physio-unit-1-b.sc.General Physiology – Basic concepts
As per INC Syllabus
Topic :-
General Physiology – Basic concepts
Cell physiology including transportation
across cell membrane
Body fluid compartments, Distribution of
total body fluid, intracellular and extracellular
compartments, major electrolytes and
maintenance of homeostasis
cell cycle
Tissue – formation, repair
Membranes and glands – functions
Application and implication in nursing
🧬 CELL PHYSIOLOGY
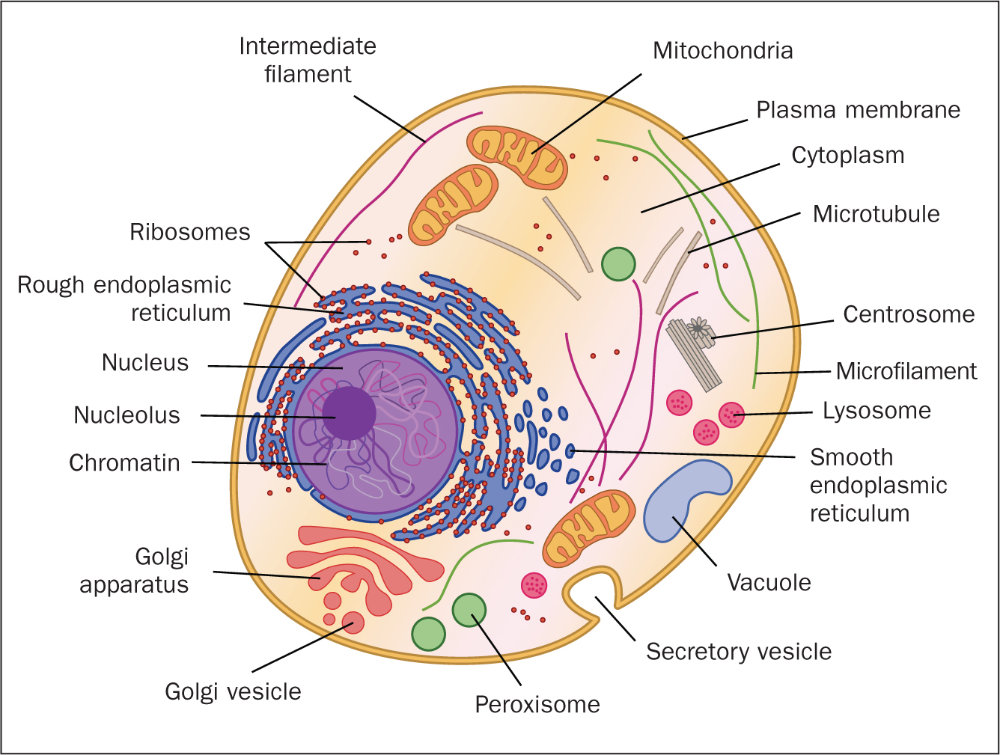
Cell physiology is the study of the vital functions and processes carried out by cells to support life. Each cell operates as a self-regulating unit, capable of performing complex biological tasks essential for survival, growth, communication, and reproduction.
📌 KEY FUNCTIONS OF CELL PHYSIOLOGY
- Transport of Substances Across Cell Membrane
- Cellular Respiration & Energy Production
- Protein Synthesis
- Cell Communication & Signal Transduction
- Cell Growth, Division, and Death
- Homeostasis and Internal Regulation
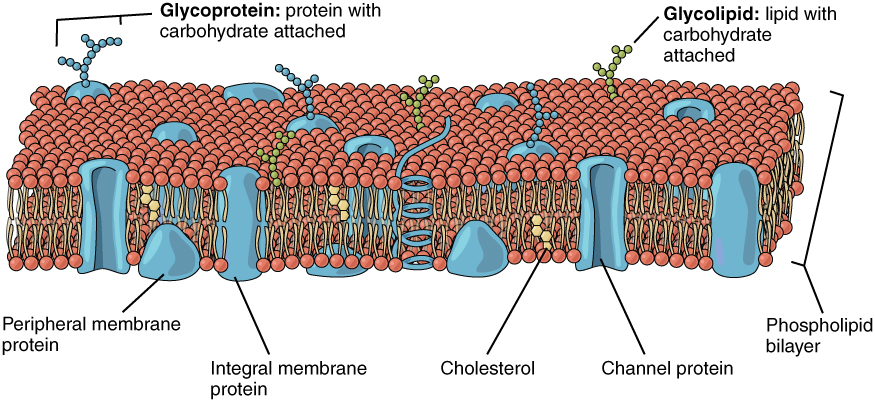
🧱 STRUCTURE OF THE CELL MEMBRANE (Plasma Membrane)
The cell membrane is semi-permeable and acts as a selective barrier.
🔹 Major Components:
- Phospholipid bilayer: Provides fluidity and barrier to polar substances.
- Membrane proteins:
- Integral proteins: Embedded across the membrane; transporters, channels.
- Peripheral proteins: Attached to membrane surface; enzymes, signaling.
- Cholesterol: Stabilizes membrane, especially in varying temperatures.
- Carbohydrates (Glycoproteins/Glycolipids): Cell recognition and immune response.
🔄 TRANSPORT ACROSS THE CELL MEMBRANE
1. ✅ Passive Transport (No Energy Required)
Movement occurs along a concentration gradient (high to low concentration).
a) Simple Diffusion
- Direct passage of small, non-polar molecules through the lipid bilayer.
- Examples: Oxygen (O₂), Carbon dioxide (CO₂), lipid-soluble drugs.
b) Facilitated Diffusion
- Involves channel proteins (for ions) or carrier proteins (for larger molecules).
- Examples: Glucose, amino acids, sodium (Na⁺), potassium (K⁺)
c) Osmosis
- Movement of water through aquaporins (water channels).
- From low solute to high solute concentration.
- Importance: Maintains fluid balance across membranes (e.g., in kidneys).
2. ⚡ Active Transport (Energy Required)
Movement against the concentration gradient, using ATP.
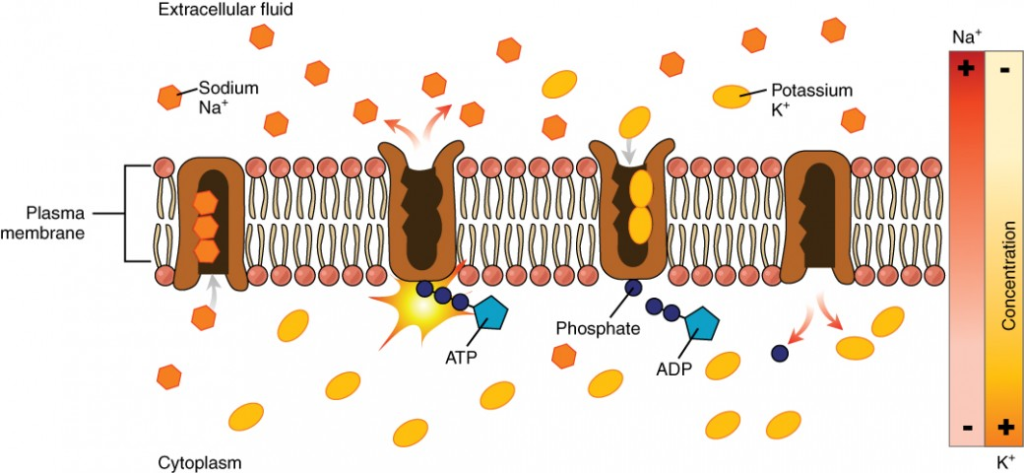
a) Primary Active Transport
- Directly uses energy from ATP to move molecules.
- Example: Sodium-potassium pump (Na⁺/K⁺-ATPase)
- 3 Na⁺ ions out, 2 K⁺ ions in
- Maintains electrochemical gradient, essential for nerve impulse conduction and muscle contraction.
b) Secondary Active Transport (Co-Transport)
- Uses the energy from another molecule’s concentration gradient.
- Symport: Both molecules move in the same direction (e.g., Na⁺ & glucose in intestinal cells)
- Antiport: Molecules move in opposite directions (e.g., Na⁺/Ca²⁺ exchange)
3. 📦 Bulk (Vesicular) Transport
Used for macromolecules (proteins, polysaccharides) or large particles.
a) Endocytosis (Substance moves into the cell)
- Phagocytosis (“cell eating”) – Engulfment of large particles by pseudopodia (e.g., WBC engulfing bacteria).
- Pinocytosis (“cell drinking”) – Uptake of fluids or dissolved substances.
- Receptor-mediated endocytosis – Specific molecules bind to receptors before being engulfed.
b) Exocytosis (Substance moves out of the cell)
- Vesicles containing substances fuse with the plasma membrane to release contents outside.
- Example: Secretion of hormones, enzymes, neurotransmitters.
⚙️ OTHER ESSENTIAL CELLULAR FUNCTIONS
🔋 1. Cellular Respiration (Energy Production)
Occurs primarily in the mitochondria, converting glucose into ATP (adenosine triphosphate).
| Type | Oxygen | ATP Yield | Byproducts |
|---|---|---|---|
| Aerobic | Yes | 36–38 ATP | CO₂, H₂O |
| Anaerobic | No | 2 ATP | Lactic acid (in humans) |
Importance: Provides energy for all metabolic and physiological activities.
🧬 2. Protein Synthesis
The process by which cells produce proteins needed for structure, enzymes, hormones, etc.
| Step | Location | Description |
|---|---|---|
| Transcription | Nucleus | DNA → mRNA (messenger RNA) |
| Translation | Ribosome | mRNA → Protein (with help of tRNA) |
Endoplasmic Reticulum & Golgi Apparatus process, fold, and package proteins for function or secretion.
📞 3. Cell Signaling & Communication
Cells communicate via:
- Chemical messengers (hormones, neurotransmitters)
- Receptors (proteins that bind specific signals)
- Second messengers (e.g., cAMP)
This helps in coordination, response to stimuli, and regulation of cell activity.
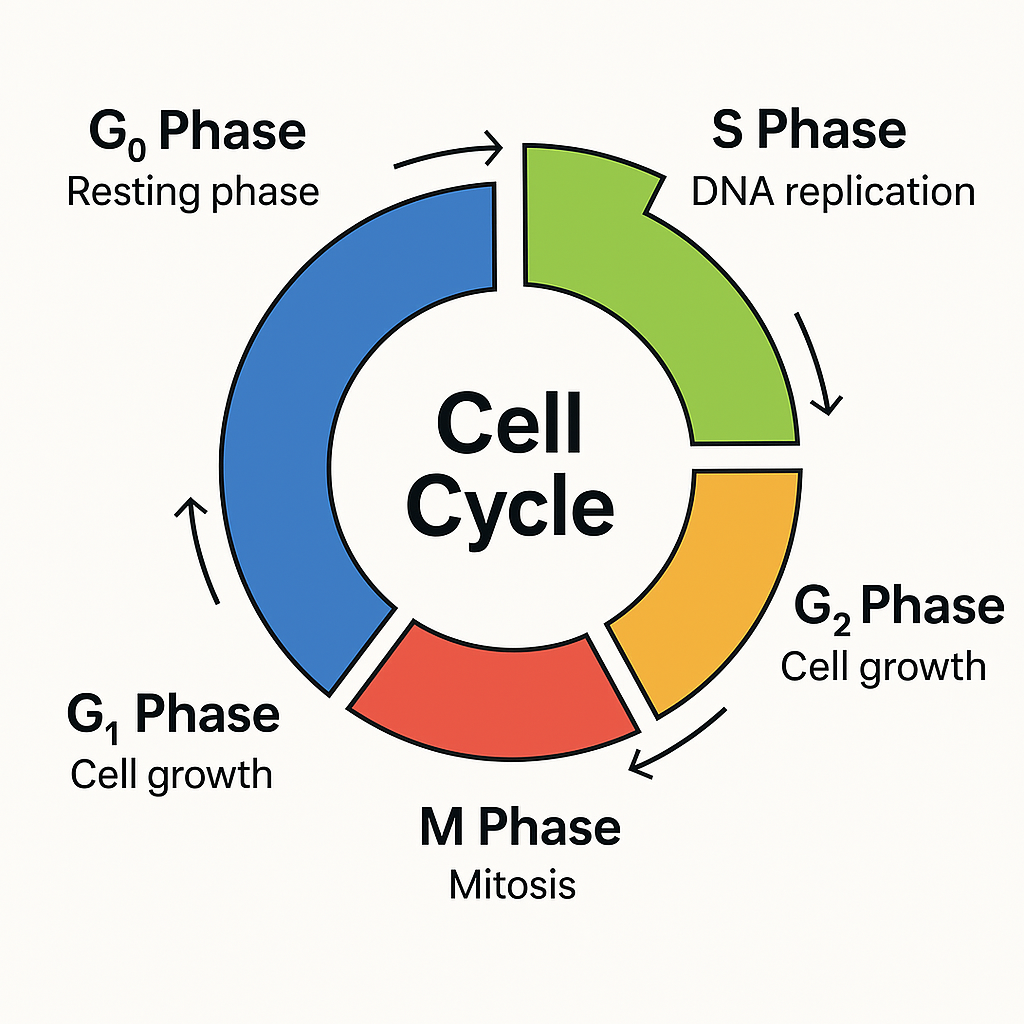
📈 4. Cell Cycle – Growth & Division
Regulated phases ensuring proper duplication and division:
| Phase | Description |
|---|---|
| G1 Phase | Cell grows and synthesizes proteins |
| S Phase | DNA replication |
| G2 Phase | Preparation for division |
| M Phase | Mitosis (division) |
- Mitosis: For somatic cell division (growth and repair)
- Meiosis: For gamete formation (reproduction)
🧬 5. Apoptosis (Programmed Cell Death)
A natural process to remove damaged or unnecessary cells. Prevents cancer and autoimmune reactions.
🧠 CLINICAL APPLICATIONS / RELEVANCE
| Condition | Related Cell Physiology Disruption |
|---|---|
| Cystic Fibrosis | Faulty Cl⁻ transport protein → thick mucus |
| Diabetes Mellitus | Impaired glucose transport and insulin signaling |
| Hyponatremia | Disturbed osmosis → brain swelling |
| Cancer | Uncontrolled cell division (mitosis failure) |
| Ischemia/Hypoxia | No oxygen → reduced ATP → active transport fails |
| Neurotoxins | Disrupt ion channels → paralysis/seizures |
📚 Summary Table: Key Cell Functions
| Function | Organelle Involved | Notes |
|---|---|---|
| Transport | Cell membrane, transport proteins | Passive & active types |
| Energy Production | Mitochondria | ATP generation via respiration |
| Protein Synthesis | Nucleus, Ribosome, ER, Golgi | DNA → mRNA → Protein |
| Communication | Receptors, signaling molecules | Hormonal & neural communication |
| Growth & Division | Nucleus, Centrosome | Cell cycle, mitosis |
| Waste Disposal | Lysosomes | Digest unwanted materials |
🔄 TRANSPORTATION ACROSS CELL MEMBRANE
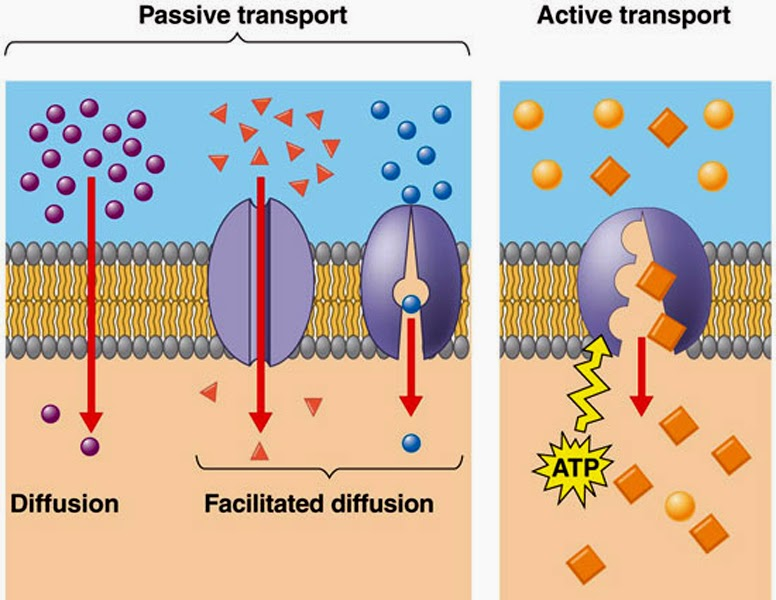
The cell membrane (plasma membrane) is selectively permeable, meaning it allows some substances to pass while restricting others. This regulation maintains the internal environment of the cell (homeostasis).
1. Passive Transport
- Does not require energy (ATP)
- Substances move from high to low concentration (down the gradient)
a) Simple Diffusion
- Movement of small, non-polar molecules (O₂, CO₂)
- Directly through the phospholipid bilayer
b) Facilitated Diffusion
- Movement via transport proteins (channel or carrier)
- For larger or polar molecules like glucose, ions (Na⁺, K⁺)
c) Osmosis
- Diffusion of water across a semi-permeable membrane
- Moves from low solute concentration to high solute concentration
2. Active Transport
- Requires energy (ATP)
- Moves substances against the concentration gradient (low to high)
a) Primary Active Transport
- Direct use of ATP
- Example: Sodium-Potassium Pump (Na⁺/K⁺ ATPase)
- Pumps 3 Na⁺ out, 2 K⁺ into the cell
- Maintains electrochemical gradient
b) Secondary Active Transport (Co-transport)
- Indirect use of ATP
- Uses energy from the gradient of one molecule to transport another
- Symport: Both substances move in the same direction
- Antiport: Substances move in opposite directions
3. Bulk Transport (Vesicular Transport)
- For large molecules like proteins, polysaccharides
a) Endocytosis (into the cell)
- Phagocytosis (“cell eating”): Engulf solid particles
- Pinocytosis (“cell drinking”): Engulf fluid
- Receptor-mediated endocytosis: Selective uptake using receptors
b) Exocytosis (out of the cell)
- Vesicles fuse with membrane to release contents outside
- Used for secretion of hormones, neurotransmitters
🌡️ Special Features of Cell Membrane Transport
- Selectivity: Only specific molecules are allowed
- Saturation: Transporters can get saturated at high concentrations
- Regulation: Some channels/gates open in response to signals (ligand-gated, voltage-gated)
- Polarization: Cells maintain electrical potential via ion gradients
⚡ Clinical Relevance
- Cystic Fibrosis: Defect in Cl⁻ channel → sticky mucus
- Diabetes: Impaired glucose transport
- Neurotoxins: Affect Na⁺/K⁺ channels → disrupt nerve transmission
- Ischemia: Lack of O₂ affects ATP → impairs active transport → cell swelling
💧 BODY FLUID COMPARTMENTS – IN DETAIL
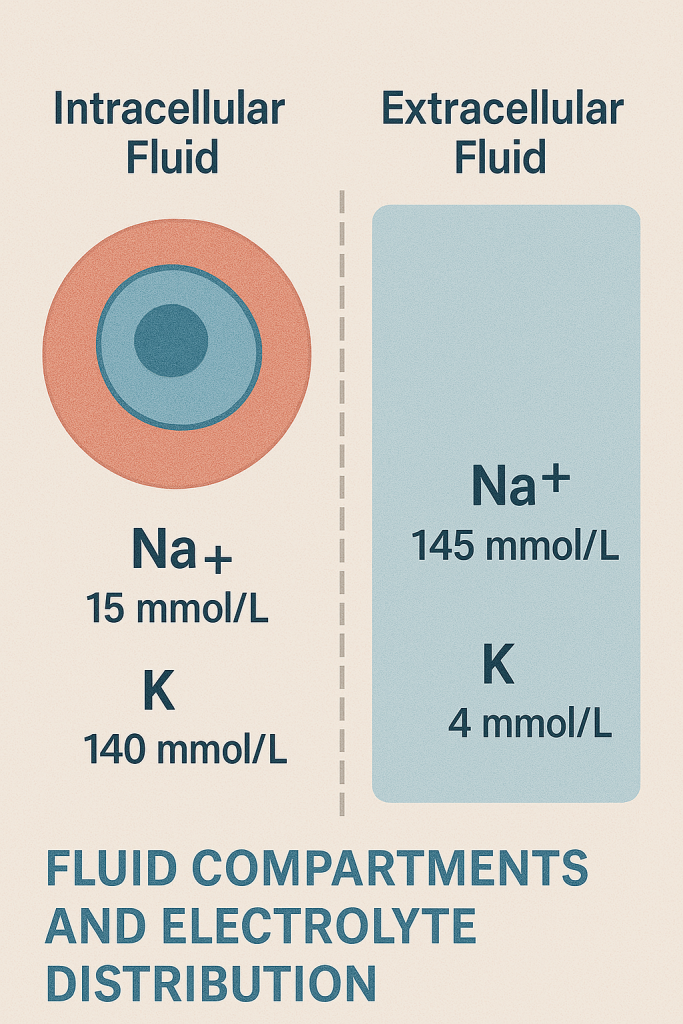
📌 Introduction
The human body is composed of approximately 60% water (varies with age, sex, body fat). This water is distributed in different fluid compartments, each with a specific volume, composition, and function.
Understanding fluid compartments is vital for managing fluid therapy, dehydration, electrolyte imbalance, shock, and renal failure.
💦 I. Major Body Fluid Compartments
📊 Total Body Water (TBW)
- Makes up ~60% of body weight in adult males (~42L)
- Lower in females (~50%) due to higher fat content
- Even lower in elderly and higher in infants (~70%)
🧊 II. Distribution of Body Fluids
Body fluids are divided into two major compartments:
🔹 1. Intracellular Fluid (ICF)
- Water inside the cells
- Makes up about 2/3 of total body water (~40% of body weight)
🔬 Key Features:
- Primary cation: Potassium (K⁺)
- Primary anions: Phosphate (PO₄³⁻), proteins
- Other ions: Magnesium (Mg²⁺)
📌 Function: Maintains cell shape, involved in enzymatic activity, cell metabolism, and electrochemical gradients
🔹 2. Extracellular Fluid (ECF)
- Water outside the cells
- Makes up 1/3 of total body water (~20% of body weight)
The ECF is further divided into:
🔸 a) Interstitial Fluid (ISF) (~15%)
- Fluid between cells in tissues
- Acts as a medium for nutrient/waste exchange
🔸 b) Intravascular Fluid (Plasma) (~5%)
- Fluid component of blood (excluding cells)
- Maintains circulating volume, blood pressure, and perfusion
🔸 c) Transcellular Fluid (minimal)
- Found in specific spaces:
- CSF (cerebrospinal fluid)
- Synovial fluid
- Peritoneal, pleural, and pericardial fluids
- Aqueous/vitreous humor (eye)
📌 Function: Specialized roles in lubrication, shock absorption, fluid exchange, and pressure balance
⚖️ III. Electrolyte Composition
| Ion | Intracellular Fluid (ICF) | Extracellular Fluid (ECF) |
|---|---|---|
| Na⁺ | Low | High (main ECF cation) |
| K⁺ | High (main ICF cation) | Low |
| Ca²⁺ | Very low | Present (important for signaling) |
| Mg²⁺ | Moderate | Low |
| Cl⁻ | Low | High (main ECF anion) |
| HCO₃⁻ | Low | Moderate |
| Proteins | High | Moderate (mainly in plasma) |
🔁 IV. Movement of Fluids Between Compartments
Fluid shifts occur by:
🔸 1. Osmosis:
- Movement of water across a semipermeable membrane from low solute to high solute concentration
🔸 2. Diffusion:
- Movement of solutes from high to low concentration
🔸 3. Filtration:
- Movement of fluid across capillary membranes due to hydrostatic and oncotic pressures
🔸 4. Active Transport:
- Uses energy (ATP) to move ions (e.g., Na⁺/K⁺ pump)
🩺 V. Clinical Implications in Nursing
✨ A. Dehydration / Fluid Volume Deficit
- Loss of ECF (e.g., vomiting, diarrhea, burns)
- Symptoms: Dry mucosa, low BP, poor skin turgor, increased HR
- Nursing Role:
- Monitor intake/output (I/O)
- Encourage oral fluids or administer IV fluids
✨ B. Edema
- Excess interstitial fluid due to:
- ↑ capillary pressure
- ↓ plasma proteins (albumin)
- ↑ capillary permeability (e.g., inflammation)
- Management:
- Diuretics
- Elevation of limbs
- Monitor daily weight
✨ C. Electrolyte Imbalances
- Common in renal failure, diarrhea, diuretics
- Examples:
- Hypokalemia – muscle weakness, arrhythmias
- Hyponatremia – confusion, seizures
- Monitor ECG, labs, and signs of imbalance
✨ D. Fluid Resuscitation and IV Therapy
- Correct hypovolemia or electrolyte loss using:
- Crystalloids (e.g., NS, Ringer’s lactate)
- Colloids (e.g., albumin)
- Choose based on which compartment needs restoration
🧠 VI. Nursing Assessments Related to Fluid Compartments
| Parameter | Purpose |
|---|---|
| Daily weight | Detect subtle fluid gain/loss |
| Intake & Output (I&O) | Monitor fluid balance |
| Skin turgor | Dehydration assessment |
| Blood pressure & HR | Detect hypovolemia or fluid overload |
| Urine output & concentration | Kidney perfusion and hydration |
| Laboratory values | Na⁺, K⁺, BUN, creatinine, osmolality |
✅ Summary
- Body fluids are divided into intracellular and extracellular compartments
- Electrolyte composition varies between compartments and is essential for cellular function
- Understanding fluid distribution helps in IV therapy, managing shock, dehydration, edema, and electrolyte imbalances
- Nurses play a critical role in assessing fluid status, administering therapy, and educating patients
💧 DISTRIBUTION OF TOTAL BODY FLUID – IN DETAIL
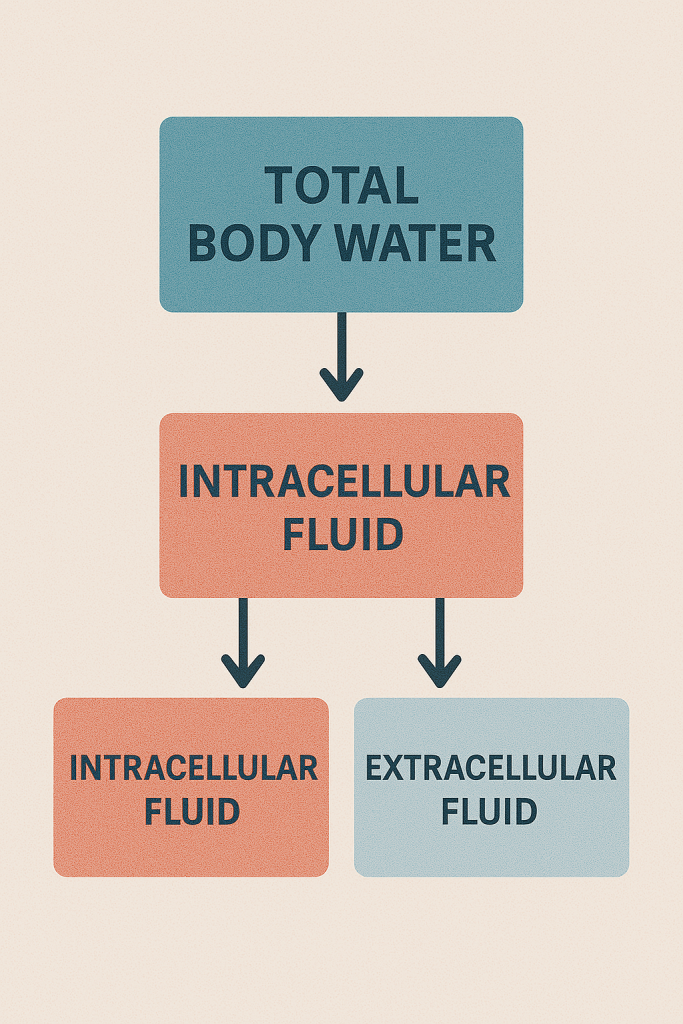
📌 Introduction
Water is the most abundant component of the human body and plays a critical role in cellular function, nutrient transport, waste removal, and temperature regulation. Total body water (TBW) refers to all the water contained in the intracellular and extracellular compartments.
On average, total body fluid accounts for about 60% of adult body weight, though this percentage varies with age, sex, and body fat content.
🧍♂️ I. Percentage of Total Body Water (TBW)
| Group | % of Body Weight as Water | Notes |
|---|---|---|
| Adult male | ~60% | More muscle (water-rich) than fat |
| Adult female | ~50–55% | Higher fat content (less water) |
| Newborns/infants | ~70–75% | Highest water content |
| Elderly adults | ~45–55% | Lower muscle mass, higher fat |
| Obese individuals | ↓ Total body water | Fat holds less water |
🧊 II. Distribution of Body Fluids
Total body fluid is divided into two main compartments, with subdivisions:
🔹 1. Intracellular Fluid (ICF)
- Volume: ~2/3 of total body fluid or ~40% of body weight
- Location: Inside the cells of all tissues and organs
- Approximate Volume: ~25–28 liters in a 70-kg adult
🔬 Key Functions:
- Maintains cellular shape and function
- Site of metabolic reactions
- Rich in:
- Potassium (K⁺)
- Magnesium (Mg²⁺)
- Phosphate (PO₄³⁻)
- Proteins
🔹 2. Extracellular Fluid (ECF)
- Volume: ~1/3 of total body fluid or ~20% of body weight
- Approximate Volume: ~14 liters in a 70-kg adult
- Located outside the cells
- Divided into:
🔸 a) Interstitial Fluid (ISF)
- ~75% of ECF (~11 L)
- Found between cells, in tissues
- Provides medium for exchange of gases, nutrients, and waste between blood and cells
🔸 b) Intravascular Fluid (Plasma)
- ~20% of ECF (~3 L)
- Found within blood vessels
- Maintains blood pressure and perfusion
🔸 c) Transcellular Fluid
- <1% of total body fluid (~1 L or less)
- Found in specialized compartments:
- Cerebrospinal fluid (CSF)
- Pleural fluid
- Peritoneal fluid
- Synovial fluid
- Aqueous/vitreous humor (eye)
- Increases significantly in disease states (e.g., ascites, pleural effusion)
📊 III. Summary Table: Fluid Distribution in a 70-kg Adult
| Compartment | % of Body Weight | Approximate Volume |
|---|---|---|
| Total Body Water (TBW) | ~60% | ~42 liters |
| – Intracellular Fluid | ~40% | ~28 liters |
| – Extracellular Fluid | ~20% | ~14 liters |
| — Interstitial Fluid | ~15% | ~11 liters |
| — Plasma | ~5% | ~3 liters |
| — Transcellular Fluid | <1% | ~1 liter or less |
⚖️ IV. Factors Affecting Fluid Distribution
| Factor | Effect |
|---|---|
| Age | TBW decreases with age |
| Gender | Females have less TBW due to more fat |
| Body Composition | More muscle = more water; more fat = less water |
| Illness or trauma | May shift fluid into third spaces (e.g., edema, ascites) |
| Hormonal regulation | ADH, aldosterone, and ANP affect water retention or loss |
🩺 V. Clinical Significance in Nursing
🔹 1. Dehydration
- Loss of ECF (especially plasma and ISF)
- Signs: Hypotension, dry mucosa, poor skin turgor, tachycardia
- Management: Oral or IV fluid replacement
🔹 2. Edema
- Accumulation of interstitial fluid
- Due to increased capillary permeability, low plasma proteins, or lymphatic obstruction
- Requires monitoring and possible use of diuretics
🔹 3. Third Spacing
- Fluid shifts from the vascular to transcellular/interstitial space
- Seen in burns, peritonitis, sepsis
- Results in hypovolemia without weight loss
🔹 4. Shock
- Intravascular fluid loss → decreased tissue perfusion
- Requires rapid fluid resuscitation with crystalloids/colloids
🔹 5. Fluid Balance Monitoring
- Nurses assess fluid distribution via:
- I/O charting
- Daily weights
- Edema assessment
- Vital signs and lab tests
✅ Summary
The body’s fluids are distributed between intracellular and extracellular compartments, each serving vital physiological functions. Understanding the distribution of total body fluid is crucial for fluid therapy, electrolyte management, and recognizing clinical conditions like dehydration, edema, and shock.
💧 INTRACELLULAR & EXTRACELLULAR FLUID COMPARTMENTS, MAJOR ELECTROLYTES & HOMEOSTASIS
📌 I. Fluid Compartments Overview
The body’s total water is distributed between two main fluid compartments, each with distinct electrolyte composition and physiological roles.
🔹 A. Intracellular Fluid (ICF)
- Definition: Fluid within cells
- Makes up ~2/3 of total body water (~40% of body weight)
- Volume: ~28 liters in a 70-kg adult
🔹 B. Extracellular Fluid (ECF)
- Definition: Fluid outside cells
- Makes up ~1/3 of total body water (~20% of body weight)
- Volume: ~14 liters
ECF is further divided into:
- Interstitial fluid (ISF) (~11 L): Surrounds tissue cells
- Intravascular fluid (Plasma) (~3 L): Inside blood vessels
- Transcellular fluid (<1 L): Includes CSF, pleural, pericardial, synovial fluids
🧪 II. Major Electrolytes in ICF and ECF
Electrolytes are charged particles (ions) that play crucial roles in nerve impulses, muscle contraction, pH balance, and fluid regulation.
📍 A. Intracellular Fluid Electrolytes
| Electrolyte | Concentration | Function |
|---|---|---|
| Potassium (K⁺) | High | Major cation; nerve and muscle function |
| Magnesium (Mg²⁺) | Moderate | Enzyme activity, ATP use |
| Phosphate (PO₄³⁻) | High | Energy metabolism (ATP), buffering |
| Proteins (negatively charged) | High | Contribute to osmotic balance |
📍 B. Extracellular Fluid Electrolytes
| Electrolyte | Concentration | Function |
|---|---|---|
| Sodium (Na⁺) | High | Major cation; controls water distribution |
| Chloride (Cl⁻) | High | Maintains osmotic balance, electrical neutrality |
| Bicarbonate (HCO₃⁻) | Moderate | Main buffer for pH regulation |
| Calcium (Ca²⁺) | Present | Blood clotting, muscle function, nerve transmission |
💡 Key Concept:
- Sodium is the primary ECF cation
- Potassium is the primary ICF cation
🔄 III. Movement Between Compartments
Fluid and electrolyte exchange between ICF and ECF happens via:
✅ Osmosis
- Water moves from low to high solute concentration across membranes
✅ Diffusion
- Solutes move from high to low concentration
✅ Active Transport
- Uses ATP to move substances against concentration gradients
- e.g., Na⁺/K⁺ pump: Moves 3 Na⁺ out and 2 K⁺ into the cell
✅ Filtration
- Fluid movement across capillary membranes due to hydrostatic and oncotic pressure
⚖️ IV. Maintenance of Homeostasis
Homeostasis is the body’s ability to maintain a stable internal environment, including fluid and electrolyte balance. Several organ systems and hormones work together to achieve this.
🔹 1. Kidneys
- Regulate electrolyte excretion or reabsorption
- Maintain fluid volume, pH, and osmolarity
🔹 2. Hormonal Regulation
| Hormone | Origin | Action |
|---|---|---|
| ADH (Antidiuretic Hormone) | Posterior pituitary | Promotes water reabsorption in kidneys; ↓ urine output |
| Aldosterone | Adrenal cortex | Increases Na⁺ reabsorption (water follows), K⁺ excretion |
| ANP (Atrial Natriuretic Peptide) | Heart atria | Promotes Na⁺ and water excretion, lowers blood volume |
| PTH (Parathyroid Hormone) | Parathyroid glands | Regulates calcium and phosphate balance |
🔹 3. Thirst Mechanism
- Controlled by the hypothalamus
- Triggered by increased plasma osmolality or low blood volume
- Promotes fluid intake
🔹 4. Buffer Systems
- Maintain acid–base balance:
- Bicarbonate buffer (HCO₃⁻/H₂CO₃)
- Protein buffer (e.g., hemoglobin)
- Phosphate buffer (ICF)
🩺 V. Clinical Relevance for Nurses
🔸 Electrolyte Imbalance Symptoms
| Electrolyte | Deficiency (Hypo-) | Excess (Hyper-) |
|---|---|---|
| Na⁺ | Confusion, seizures | Edema, HTN, thirst |
| K⁺ | Muscle cramps, arrhythmias | Cardiac arrest, weakness |
| Ca²⁺ | Tetany, seizures | Kidney stones, bone pain |
| Mg²⁺ | Tremors, neuromuscular irritability | Respiratory depression |
| Cl⁻ | Metabolic alkalosis | Acidosis, weakness |
🔸 Nursing Interventions
- Monitor I&O, daily weight, vital signs
- Check serum electrolyte levels
- Assess for neurological changes, cardiac rhythm
- Administer electrolyte replacements (e.g., oral/IV potassium)
- Educate about hydration, diet, fluid restrictions
✅ Summary
| Feature | Intracellular Fluid | Extracellular Fluid |
|---|---|---|
| Volume | ~28 L | ~14 L |
| Main Cation | K⁺ | Na⁺ |
| Main Anion | Phosphate, proteins | Cl⁻, HCO₃⁻ |
| Functions | Cell metabolism, enzyme function | Transport, perfusion, buffering |
| Homeostasis Maintained By | Kidneys, hormones (ADH, aldosterone), buffers | Same |
Understanding the ICF and ECF composition, along with the mechanisms maintaining homeostasis, is vital in recognizing clinical symptoms, administering fluid/electrolyte therapy, and ensuring patient safety.
🧬 CELL CYCLE – IN DETAIL
📌 What is the Cell Cycle?
The cell cycle is a series of events that a cell undergoes from its formation to its division into two daughter cells. It is essential for:
- Growth and development
- Tissue repair and regeneration
- Cell replacement
- Asexual reproduction (in single-celled organisms)
🔄 Major Phases of the Cell Cycle
The cell cycle is divided into two main stages:
🔹 1. Interphase (preparation phase)
- The longest phase (~90% of the cycle)
- Includes G₁, S, and G₂ phases
🔹 2. Mitotic Phase (M phase) (division phase)
- Includes mitosis (nuclear division) and cytokinesis (cytoplasmic division)
🧪 I. Phases of the Cell Cycle
🧬 1. G₁ Phase (First Gap)
- Cell grows and synthesizes proteins, RNA, and organelles
- Prepares for DNA replication
- Duration varies by cell type
🔍 Clinical Note: Most cell cycle checkpoints occur here
🧬 2. S Phase (Synthesis)
- DNA is replicated
- Each chromosome duplicates to form sister chromatids
- Centrosomes (which help with mitosis) are also duplicated
🔍 Critical for maintaining genetic integrity during division
🧬 3. G₂ Phase (Second Gap)
- Cell grows further
- Prepares for mitosis by synthesizing enzymes and proteins needed for division
- Checks and repairs DNA replication errors
🔍 G₂/M checkpoint ensures the cell is ready to divide
⚡ 4. M Phase (Mitosis + Cytokinesis)
This is where actual cell division occurs.
Mitosis is divided into 4–5 stages:
| Stage | Key Events |
|---|---|
| Prophase | Chromosomes condense, spindle fibers form, nuclear envelope breaks down |
| Metaphase | Chromosomes align at the cell equator |
| Anaphase | Sister chromatids separate and move to opposite poles |
| Telophase | Nuclear membranes re-form around each set of chromosomes |
| Cytokinesis | Cytoplasm divides → 2 genetically identical daughter cells |
🔍 Occurs in somatic (body) cells, ensuring equal genetic material distribution
⏸️ II. G₀ Phase – Resting Phase
- Cells that exit the cycle (temporary or permanently) enter G₀
- Metabolically active but do not divide
- Examples: neurons, skeletal muscle, cardiac muscle (mostly in G₀)
🔍 Some cells can re-enter the cycle when stimulated (e.g., liver cells after damage)
🧠 III. Cell Cycle Regulation
Tightly controlled by:
- Cyclins (proteins that rise/fall during the cycle)
- Cyclin-dependent kinases (CDKs) – enzymes activated by cyclins
- Checkpoints – monitor DNA integrity and cell readiness
🔍 Major Checkpoints:
| Checkpoint | Function |
|---|---|
| G₁/S checkpoint | Checks for DNA damage, adequate size |
| G₂/M checkpoint | Ensures DNA is fully replicated, no damage |
| Metaphase checkpoint | Confirms chromosomes are properly aligned |
Tumor suppressor genes like p53 stop the cycle if errors are found
🧬 IV. Importance of the Cell Cycle
| Function | Example |
|---|---|
| Growth | Embryonic development, childhood |
| Repair | Wound healing, tissue regeneration |
| Replacement | Skin cells, blood cells, GI lining |
| Reproduction | In single-celled organisms via mitosis |
🩺 V. Clinical Relevance for Nursing
✅ 1. Wound Healing
- Cell cycle is activated in epidermis and connective tissue
- Guides proliferation of epithelial and fibroblast cells
✅ 2. Cancer
- Uncontrolled cell division due to failed checkpoints or mutations
- Cancer cells bypass G₁ and G₂ controls
- Chemotherapy and radiation target rapidly dividing cells
✅ 3. Stem Cell Therapy
- Uses controlled cell cycles of multipotent or pluripotent cells to regenerate tissues
✅ 4. Tissue Engineering
- Requires knowledge of cell cycle timing and control to grow functional tissues
✅ 5. Antibiotics & Antivirals
- Some drugs act on cellular replication, useful in treating infections and cancer
📊 VI. Summary Table
| Phase | Description | Key Outcome |
|---|---|---|
| G₁ | Cell grows, prepares for DNA synthesis | Prepares machinery |
| S | DNA replication | Two copies of genome |
| G₂ | Prepares for mitosis | Ensures readiness |
| M | Cell division | 2 identical daughter cells |
| G₀ | Resting phase | Cell not dividing |
🧬 TISSUE FORMATION (HISTOGENESIS) – IN DETAIL
📌 I. What is Tissue Formation (Histogenesis)?
Tissue formation, or histogenesis, refers to the development and specialization of cells into organized tissue types during embryonic development. It is a crucial part of organogenesis — the process by which organs are formed in the embryo.
This also occurs (to a lesser extent) during tissue repair, regeneration, and stem cell therapy in adults.
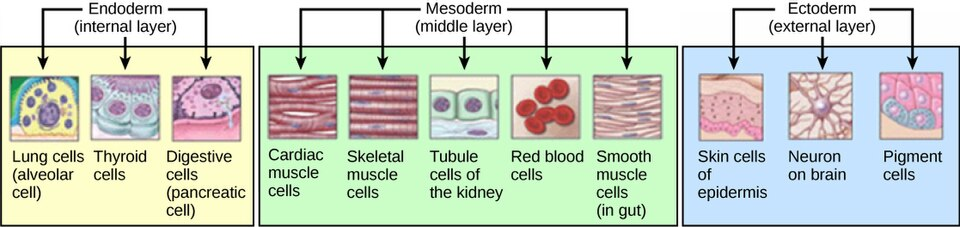
🌱 II. Embryonic Origins – Germ Layers
In early embryonic development (around 3rd week), the embryo forms three primary germ layers, from which all tissues of the body originate:
| Germ Layer | Derived Tissues |
|---|---|
| Ectoderm | Skin, nervous tissue, sense organs |
| Mesoderm | Muscle, bone, blood, connective tissue, kidneys, heart |
| Endoderm | Lining of GI tract, respiratory tract, liver, pancreas, glands |
🧫 III. Steps of Tissue Formation
🔹 1. Cell Differentiation
- Totipotent cells (zygote) → differentiate into pluripotent stem cells
- Pluripotent cells specialize into specific lineages based on gene expression and signaling
- Each cell becomes structurally and functionally adapted to its role
🔹 2. Proliferation
- Cells undergo controlled mitosis to increase in number
- Controlled by growth factors, hormones, and genes
🔹 3. Migration
- Cells move to specific regions to form layers and structures
- Example: Neural crest cells migrate to form parts of the nervous system
🔹 4. Aggregation
- Cells that share function group together
- Begin producing extracellular matrix (ECM) and adhere to one another
🔹 5. Maturation
- Tissues begin to express specialized proteins, structures, and functions
- Blood vessels grow into the tissue (angiogenesis) to supply nutrients
🧩 IV. Primary Tissue Types Formed
| Tissue Type | Description | Function |
|---|---|---|
| Epithelial | Layers of tightly packed cells | Protection, absorption, secretion |
| Connective | Cells + ECM (collagen, elastin) | Support, transport, defense |
| Muscle | Elongated contractile cells | Movement, posture, heat |
| Nervous | Neurons + glial cells | Communication, control, response |
⚙️ V. Molecular and Genetic Control of Tissue Formation
Tissue formation is tightly regulated by:
🔸 A. Gene Expression
- Determines which proteins a cell makes → affects structure/function
🔸 B. Transcription Factors
- Control which genes are active (e.g., HOX genes guide body patterning)
🔸 C. Growth Factors
- FGF (Fibroblast growth factor) – skin, limb formation
- TGF-β (Transforming growth factor beta) – ECM and wound healing
- VEGF (Vascular endothelial growth factor) – blood vessel growth
🔸 D. Cell Signaling Pathways
- WNT, Notch, Sonic Hedgehog (Shh) – involved in organ patterning and tissue boundaries
🔁 VI. Tissue Renewal and Adult Tissue Formation
Though most tissue formation occurs in the embryo, some tissues continue forming or renewing in adults:
| Tissue | Renewal Rate | Example |
|---|---|---|
| Skin epithelium | Rapid | Constant renewal |
| Blood cells | Rapid | From bone marrow stem cells |
| Liver cells | Moderate | Regeneration after injury |
| Nerve & cardiac cells | Minimal/None | Limited repair capacity |
🧠 VII. Clinical Relevance
✨ A. Congenital Malformations
- Abnormal tissue formation (e.g., cleft palate, neural tube defects)
- Caused by gene mutations, toxins, maternal malnutrition
✨ B. Cancer
- Uncontrolled cell proliferation due to failed regulation of tissue formation
✨ C. Stem Cell Therapy
- Uses pluripotent/multipotent cells to regenerate damaged tissues (e.g., bone marrow, cornea)
✨ D. Wound Healing
- Adult tissue formation occurs through:
- Cell proliferation
- ECM remodeling
- Angiogenesis
✅ Summary Table
| Phase | Description |
|---|---|
| Differentiation | Stem cells become specialized cells |
| Proliferation | Cell numbers increase via mitosis |
| Migration | Cells move to where they are needed |
| Aggregation | Similar cells cluster to form tissue |
| Maturation | Tissue develops its final form and function |
🧬 PHYSIOLOGY OF TISSUE – IN DETAIL
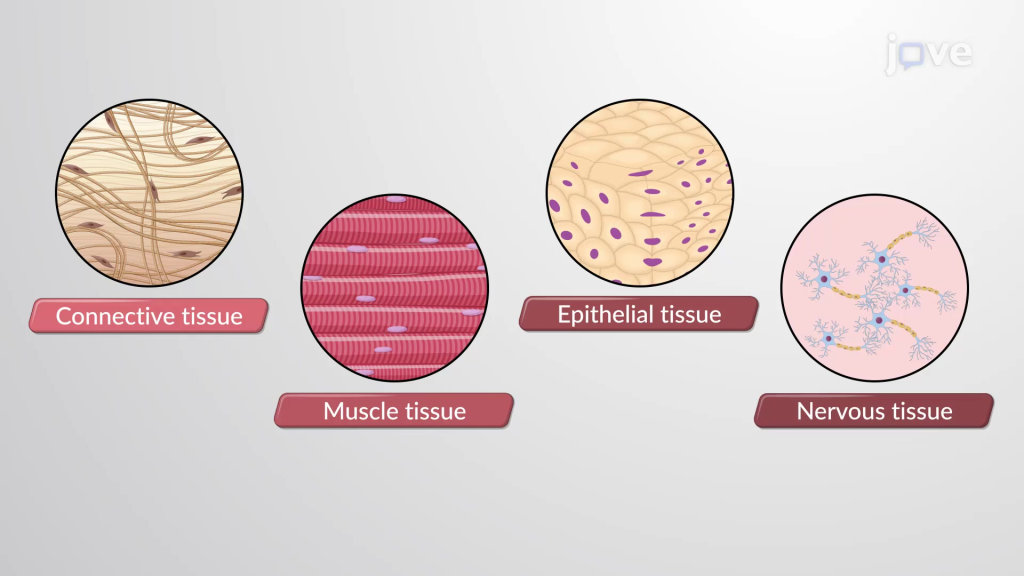
📌 Introduction
A tissue is a group of similar cells and their intercellular substances that perform a specific function. The human body is made up of four primary types of tissues, each with specialized roles that support body structure, function, and communication.
Understanding tissue physiology is essential for recognizing how organs work, and how injury, disease, or aging affects body systems.
🧠 I. The Four Basic Types of Tissues
- Epithelial tissue
- Connective tissue
- Muscle tissue
- Nervous tissue
🧬 PHYSIOLOGY OF EPITHELIAL TISSUE – IN DETAIL
📌 Introduction
Epithelial tissue is one of the four fundamental tissue types in the body (along with connective, muscle, and nervous tissues). It forms the covering and lining surfaces of the body and its organs, as well as the glands. It plays crucial roles in protection, secretion, absorption, excretion, filtration, and sensation.
🧠 Understanding epithelial tissue is essential in studying skin function, organ linings, glandular secretions, and many disease processes (e.g., carcinomas).
🧱 I. Structural Features of Epithelial Tissue
🔹 1. Cellularity
- Epithelial tissue is composed of closely packed cells with minimal or no intercellular space.
🔹 2. Polarity
- Cells have an apical surface (free/exposed side) and a basal surface (attached to basement membrane).
🔹 3. Basement Membrane
- A thin extracellular layer that anchors epithelial cells to underlying connective tissue.
- Composed of basal lamina + reticular lamina
🔹 4. Avascularity
- Epithelial tissue has no blood vessels.
- Nutrients and waste exchange occur through diffusion from underlying capillaries.
🔹 5. High Regenerative Capacity
- Cells divide rapidly to replace damaged or dead cells.
- Especially prominent in skin, GI tract, and respiratory epithelium
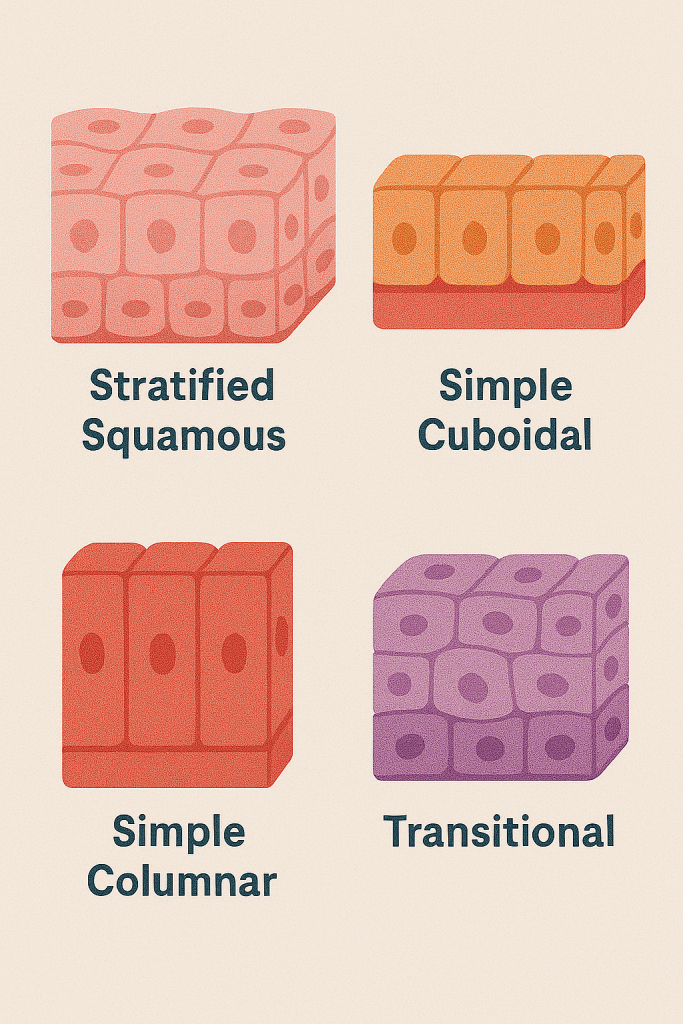
🧬 II. Classification of Epithelial Tissue
Epithelia are classified based on:
- Number of layers:
- Simple – one layer
- Stratified – multiple layers
- Pseudostratified – appears layered but isn’t
- Cell shape:
- Squamous – flat
- Cuboidal – cube-shaped
- Columnar – tall and column-like
| Type | Description | Example |
|---|---|---|
| Simple Squamous | Thin, flat | Alveoli of lungs, blood vessels |
| Simple Cuboidal | Cube-shaped | Kidney tubules, glands |
| Simple Columnar | Tall cells, may have cilia | GI tract lining |
| Stratified Squamous | Multiple layers | Skin, mouth, esophagus |
| Pseudostratified Columnar | Appears layered, often ciliated | Respiratory tract |
| Transitional | Stretchable cells | Urinary bladder |
⚙️ III. Physiological Functions of Epithelial Tissue
🔹 1. Protection
- Stratified squamous epithelium in the skin protects against:
- Mechanical injury
- Microbial invasion
- Dehydration
🔹 2. Absorption
- Simple columnar epithelium (e.g., in intestines) absorbs:
- Nutrients
- Water
- Electrolytes
🔹 3. Secretion
- Glandular epithelium (exocrine & endocrine) secretes:
- Mucus (e.g., goblet cells)
- Enzymes (e.g., pancreas)
- Hormones (e.g., thyroid, adrenal)
🔹 4. Excretion
- Kidney tubule epithelium excretes waste products into urine
🔹 5. Filtration
- Simple squamous epithelium in glomeruli of kidneys filters blood
🔹 6. Sensation
- Specialized epithelial cells are involved in sensory perception:
- Taste buds (tongue)
- Olfactory epithelium (nose)
🔹 7. Diffusion
- Alveolar epithelium in the lungs facilitates gas exchange (O₂, CO₂)
🧪 IV. Glandular Epithelium
Specialized epithelial cells form glands that secrete substances.
🔸 A. Exocrine glands – Secrete into ducts
- Sweat glands, salivary glands, pancreas (digestive enzymes)
🔸 B. Endocrine glands – Secrete into bloodstream
- Pituitary, thyroid, adrenal glands (hormones)
🧠 V. Specializations of Epithelial Cells
| Feature | Description | Function |
|---|---|---|
| Cilia | Hair-like projections | Move mucus and particles (e.g., in respiratory tract) |
| Microvilli | Finger-like extensions | Increase surface area for absorption (e.g., intestines) |
| Tight junctions | Seal cells together | Prevent leakage between cells |
| Desmosomes | Strong connections | Provide mechanical strength |
| Gap junctions | Protein channels | Allow communication between cells |
🩺 VI. Clinical Relevance in Nursing
| Condition | Affected Epithelium | Nursing Focus |
|---|---|---|
| Pressure ulcers | Stratified squamous (skin) | Prevent skin breakdown, repositioning |
| Burns | All layers | Fluid balance, infection control |
| Cancer (e.g., carcinoma) | Epithelial origin | Early detection, biopsy support |
| GERD | Esophageal lining | Monitor for dysphagia, acid suppression |
| Asthma | Respiratory epithelium | Inhaler education, airway assessment |
| UTI | Transitional epithelium | Hygiene education, fluid intake |
✅ Summary
| Feature | Epithelial Tissue |
|---|---|
| Main role | Protection, secretion, absorption |
| Location | Covers body surfaces, lines cavities, forms glands |
| Structure | Tightly packed cells, avascular, regenerative |
| Types | Simple, stratified, squamous, cuboidal, columnar |
| Specializations | Cilia, microvilli, tight junctions |
🧬 PHYSIOLOGY OF CONNECTIVE TISSUE – IN DETAIL

📌 Introduction
Connective tissue is one of the four basic tissue types of the human body (along with epithelial, muscle, and nervous tissue). It is the most abundant and widely distributed tissue type and plays essential roles in support, protection, transport, energy storage, and immune defense.
Unlike epithelial tissue, connective tissue is not cellularly dense. It contains cells scattered within an extracellular matrix (ECM) of fibers and ground substance, providing structure and strength to organs and systems.
🧱 I. Basic Structural Components of Connective Tissue
Connective tissue consists of three key elements:
1️⃣ Cells
These vary by tissue type:
| Cell Type | Function |
|---|---|
| Fibroblasts | Produce fibers (collagen, elastin) and ground substance |
| Adipocytes | Store fat (energy reserve, insulation) |
| Macrophages | Phagocytose pathogens/debris; immune defense |
| Mast cells | Release histamine and heparin; involved in allergic reactions |
| Plasma cells | Produce antibodies |
| Chondrocytes | Maintain cartilage matrix |
| Osteocytes | Maintain bone matrix |
| Blood cells | Transport (RBCs), defense (WBCs), clotting (platelets) |
2️⃣ Extracellular Fibers
Produced by fibroblasts:
| Fiber | Characteristics | Function |
|---|---|---|
| Collagen fibers | Thick, strong, unbranched | Provide strength and flexibility |
| Elastic fibers | Thin, branched, stretchable | Allow tissue recoil (e.g., lungs, skin) |
| Reticular fibers | Thin collagen fibers forming networks | Support in soft organs (e.g., spleen, liver) |
3️⃣ Ground Substance
- A gel-like material composed of water, glycosaminoglycans (GAGs), and proteoglycans
- Fills space between cells and fibers
- Acts as a medium for nutrient and waste exchange
- Provides lubrication, resistance to compression
🧬 II. Classification of Connective Tissue
🔹 A. Connective Tissue Proper
| Type | Description | Examples |
|---|---|---|
| Loose CT | Loosely packed fibers, more ground substance | Areolar, adipose, reticular tissue |
| Dense CT | Densely packed collagen fibers | Tendons (dense regular), dermis (dense irregular) |
🔹 B. Specialized Connective Tissues
| Type | Description | Function |
|---|---|---|
| Adipose Tissue | Fat storage; cells = adipocytes | Energy storage, insulation |
| Cartilage | Chondrocytes in firm ECM | Flexible support, cushioning |
| Bone | Osteocytes in mineralized matrix | Structural support, movement |
| Blood | Cells suspended in plasma | Transport, immune response, clottin |
⚙️ III. Physiological Functions of Connective Tissue
🔸 1. Support and Structure
- Forms the framework of the body (bones, ligaments, cartilage)
- Maintains organ shape and integrity
🔸 2. Binding and Connection
- Connects tissues and organs
- Tendons: muscle to bone
- Ligaments: bone to bone
🔸 3. Protection
- Bone protects brain, lungs, spinal cord
- Adipose tissue cushions organs
- White blood cells defend against pathogens
🔸 4. Insulation and Energy Storage
- Adipose tissue stores triglycerides for energy
- Helps maintain body temperature
🔸 5. Transport
- Blood transports oxygen, nutrients, waste, hormones
- Lymph returns interstitial fluid to circulation
🔸 6. Healing and Repair
- Fibroblasts produce collagen for scar formation
- Mast cells and macrophages initiate inflammation and cleanup
🔸 7. Immune Surveillance
- Reticular connective tissue in lymph nodes and spleen filters pathogens
- Leukocytes provide defense in CT
🔄 IV. Connective Tissue Remodeling & Homeostasis
- Bone remodeling: Dynamic process involving osteoblasts (build bone) and osteoclasts (break down bone)
- Wound healing: Fibroblasts lay down collagen fibers to form a scar
- Adipose turnover: Fat stored or broken down based on energy needs
- Cartilage regeneration: Limited due to avascular nature
🩺 V. Clinical Relevance in Nursing
| Condition | Affected CT | Nursing Concern |
|---|---|---|
| Osteoporosis | Bone | Fracture prevention, calcium/Vit D intake |
| Arthritis | Cartilage, synovial tissue | Joint mobility, pain management |
| Edema | Loose areolar tissue | Monitor fluid balance, limb elevation |
| Obesity | Excess adipose tissue | Nutritional counseling, comorbidity care |
| Wound healing | Fibrous CT | Monitor for infection, promote healing |
| Ehlers-Danlos Syndrome | Defective collagen | Skin/joint protection, bleeding risk |
| Anemia, Leukemia | Bone marrow (blood CT) | Monitor blood counts, infection control |
✅ Summary Table
| Feature | Connective Tissue |
|---|---|
| Main Components | Cells + fibers + ground substance |
| Function | Support, binding, transport, protection, storage |
| Types | Loose, dense, cartilage, bone, blood, adipose |
| Major Cells | Fibroblasts, adipocytes, macrophages, mast cells |
| Clinical Role | Injury repair, immune defense, nutrient transport |
💪 PHYSIOLOGY OF MUSCLE TISSUE – IN DETAIL
📌 Introduction
Muscle tissue is one of the four major tissue types in the human body, specialized for contraction and movement. It allows the body to move, maintain posture, and generate heat, and it also contributes to the function of internal organs like the heart and digestive system.
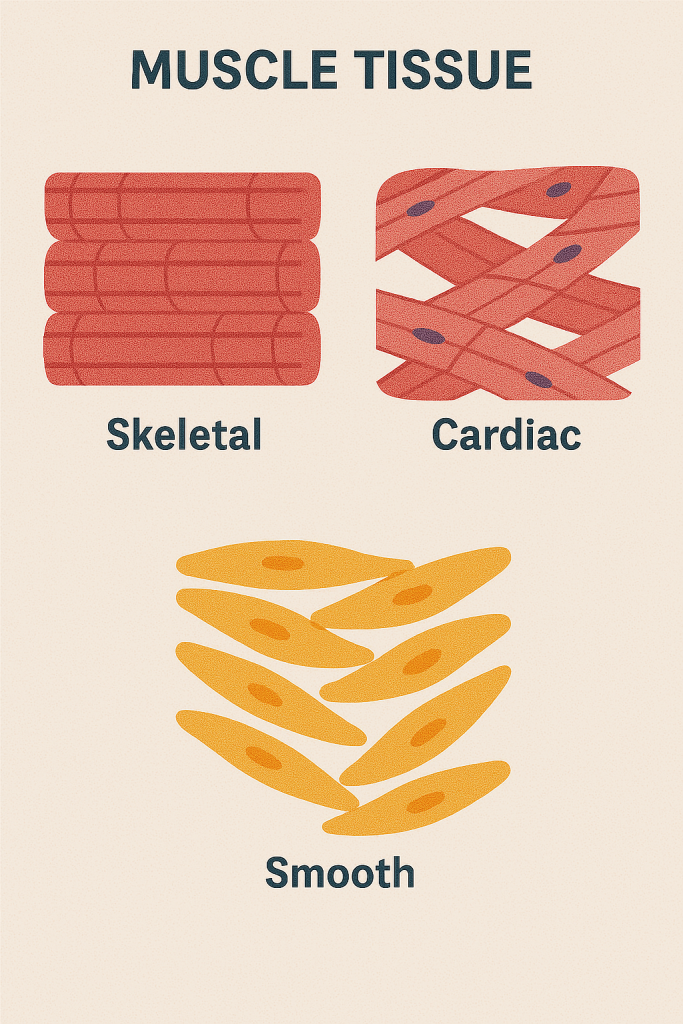
🧠 I. Types of Muscle Tissue
| Type | Structure | Control | Location | Function |
|---|---|---|---|---|
| Skeletal | Striated, multinucleated | Voluntary | Attached to bones | Body movement, posture |
| Cardiac | Striated, branched, intercalated discs | Involuntary | Heart wall | Pumping blood |
| Smooth | Non-striated, spindle-shaped | Involuntary | Walls of hollow organs (e.g., intestines, blood vessels) | Movement of substances, vasodilation, peristalsis |
🔬 II. Structure of Muscle Tissue
🔹 1. Muscle Fibers (Cells)
- Long, cylindrical cells
- Contain myofibrils made up of:
- Actin (thin filaments)
- Myosin (thick filaments)
🔹 2. Sarcomere – Functional Unit
- The smallest contractile unit of muscle fiber
- Organized in repeating units along the myofibril
- Contains:
- Z lines, A bands, I bands, H zone, M line
⚙️ III. Physiology of Muscle Contraction (Sliding Filament Theory)
Muscle contraction occurs via interaction between actin and myosin filaments within the sarcomere.
🔄 Steps of Contraction:
- Nerve impulse reaches neuromuscular junction
- Acetylcholine (ACh) is released → binds to receptors on muscle fiber
- Depolarization of sarcolemma → triggers Ca²⁺ release from sarcoplasmic reticulum
- Calcium binds to troponin, moving tropomyosin, exposing binding sites on actin
- Myosin heads bind to actin forming cross-bridges
- ATP is hydrolyzed → myosin head pulls actin (power stroke)
- New ATP attaches → myosin releases, re-cocks → cycle repeats
💡 ATP and calcium are essential for:
- Initiating, maintaining, and ending muscle contraction
🔋 IV. Muscle Energy Sources
| Energy Source | Duration | Use |
|---|---|---|
| ATP stored in muscle | Few seconds | Immediate energy |
| Creatine phosphate | 10–15 sec | Rapid ATP regeneration |
| Anaerobic glycolysis | 30–60 sec | No oxygen needed, produces lactic acid |
| Aerobic respiration | Long duration | Oxygen required, efficient |
🏃 V. Functions of Muscle Tissue
🔹 1. Movement
- Voluntary (e.g., walking, writing)
- Involuntary (e.g., digestion, heart pumping)
🔹 2. Posture and Stability
- Skeletal muscles maintain body posture
🔹 3. Heat Production
- Thermogenesis from muscle activity maintains body temperature
🔹 4. Circulation
- Cardiac muscle pumps blood
- Smooth muscle regulates vessel diameter and blood flow
🔹 5. Control of Openings
- Smooth and skeletal muscles regulate sphincters (e.g., bladder, anus)
🔄 VI. Muscle Tone and Reflexes
- Muscle tone: Continuous partial contraction to maintain posture
- Controlled by reflex arcs and spinal cord neurons
- Hypertonia or hypotonia indicates neurological dysfunction
VII. Neuromuscular Junction (NMJ)
- Junction between a motor neuron and a muscle fiber
- Transmits signals via acetylcholine (ACh)
- Target of certain drugs/toxins (e.g., curare, botulinum toxin)
🩺 VIII. Clinical Significance in Nursing
| Disorder | Affected Muscle | Nursing Focus |
|---|---|---|
| Muscle cramps | Skeletal | Hydration, electrolyte balance |
| Myasthenia gravis | Skeletal (NMJ) | Monitor fatigue, respiratory status |
| Muscle atrophy | All types (esp. skeletal) | Physical therapy, mobilization |
| Cardiac failure | Cardiac muscle | Monitor vitals, medication adherence |
| Paralysis | Skeletal (nerves) | Fall prevention, passive ROM |
| Smooth muscle spasms | GI or urinary tract | Antispasmodics, pain relief |
✅ Summary Table
| Feature | Skeletal Muscle | Cardiac Muscle | Smooth Muscle |
|---|---|---|---|
| Control | Voluntary | Involuntary | Involuntary |
| Striations | Yes | Yes | No |
| Nuclei per cell | Multinucleated | Single (central) | Single (central) |
| Location | Attached to bones | Heart | Walls of organs |
| Special features | Fast contraction | Intercalated discs | Slow, sustained contraction |
🧠 NERVOUS TISSUE – IN DETAIL
📌 Introduction
Nervous tissue is a highly specialized tissue designed for the transmission of electrical impulses throughout the body. It is the main tissue of the nervous system, which includes the brain, spinal cord (central nervous system – CNS), and nerves (peripheral nervous system – PNS).
It plays a critical role in sensory perception, motor control, cognition, reflexes, and maintenance of homeostasis.
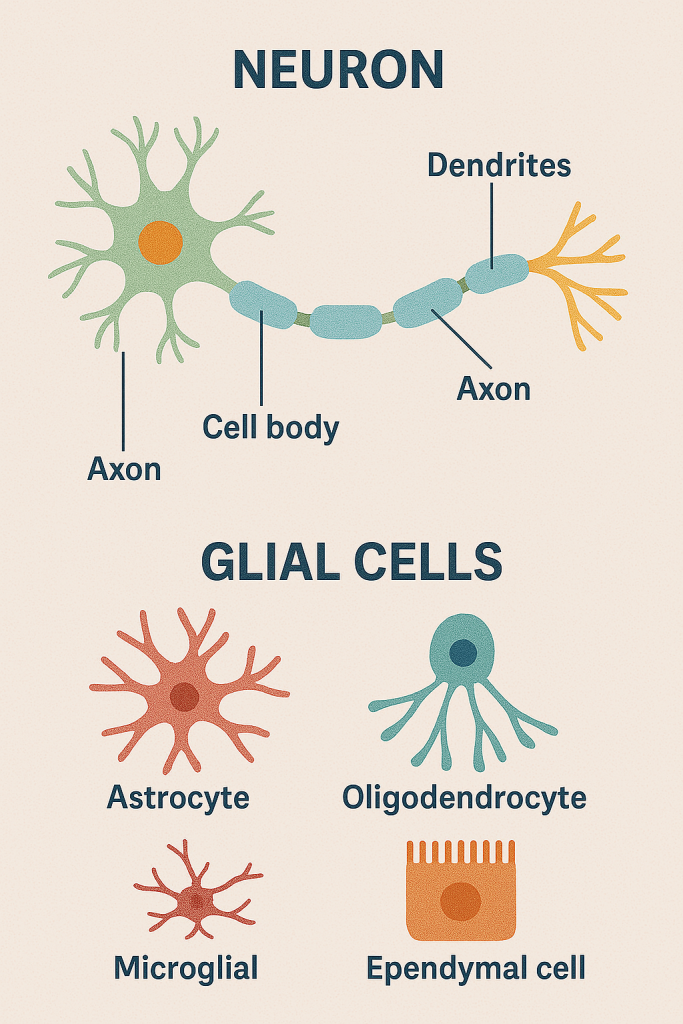
🧬 I. Components of Nervous Tissue
Nervous tissue is composed of two main types of cells:
🔹 1. Neurons (Nerve Cells)
- Functional and structural unit of nervous tissue
- Specialized to generate and transmit nerve impulses
✨ Structure of a Neuron:
| Part | Description | Function |
|---|---|---|
| Cell body (soma) | Contains nucleus and organelles | Integrates information |
| Dendrites | Branched projections | Receive signals from other neurons |
| Axon | Long extension (may be myelinated) | Transmits impulses away from cell body |
| Axon terminals | End branches of axon | Release neurotransmitters to communicate with next cell |
| Myelin sheath | Fatty insulating layer (formed by Schwann cells or oligodendrocytes) | Increases speed of impulse transmission |
| Nodes of Ranvier | Gaps in the myelin sheath | Facilitate rapid saltatory conduction |
🔹 2. Neuroglia (Glial Cells)
- Supporting, nourishing, and protecting neurons
- 10x more numerous than neurons
✨ Types of Glial Cells:
| Type | Location | Function |
|---|---|---|
| Astrocytes | CNS | Maintain blood–brain barrier, support neurons |
| Oligodendrocytes | CNS | Produce myelin sheath |
| Microglia | CNS | Act as macrophages (immune defense) |
| Ependymal cells | CNS | Line ventricles, produce CSF |
| Schwann cells | PNS | Produce myelin in peripheral nerves |
| Satellite cells | PNS | Support neuron cell bodies in ganglia |
⚙️ II. Functions of Nervous Tissue
| Function | Description |
|---|---|
| Sensory input | Detects internal and external stimuli |
| Integration | Processes and interprets sensory input |
| Motor output | Triggers responses via muscles/glands |
| Homeostasis | Maintains internal stability via feedback |
| Mental activities | Enables thought, memory, emotion, learning |
🧠 III. Types of Neurons (Based on Function)
| Type | Function | Example |
|---|---|---|
| Sensory (afferent) | Transmit impulses from receptors to CNS | Pain, temperature sensors |
| Motor (efferent) | Carry signals from CNS to effectors (muscles/glands) | Spinal motor neurons |
| Interneurons | Connect sensory and motor neurons within CNS | Reflex arcs, brain integration |
⚡ IV. Nerve Impulse Transmission (Physiology)
Resting Membrane Potential:
- Inside of neuron is negatively charged compared to outside
- Maintained by the Na⁺/K⁺ pump
Action Potential:
- Stimulus causes depolarization (Na⁺ enters cell)
- If threshold is reached, action potential fires
- Repolarization follows (K⁺ leaves cell)
- Refractory period resets ionic balance
Saltatory Conduction:
- In myelinated axons, impulses jump between Nodes of Ranvier
- Much faster than unmyelinated conduction
🔗 V. Synaptic Transmission
- At synapses, electrical signals are converted to chemical signals
- Neurotransmitters (e.g., acetylcholine, dopamine, serotonin) are released from axon terminals
- Bind to receptors on next neuron or effector cell to propagate or modulate signal
🧩 VI. Divisions of the Nervous System (In Relation to Tissue)
| Division | Components | Function |
|---|---|---|
| Central Nervous System (CNS) | Brain, spinal cord | Integrates information, controls activity |
| Peripheral Nervous System (PNS) | Cranial and spinal nerves | Communication lines |
| Somatic Nervous System | Voluntary | Controls skeletal muscles |
| Autonomic Nervous System | Involuntary | Regulates glands, heart, smooth muscles |
| – Sympathetic | “Fight or flight” | |
| – Parasympathetic | “Rest and digest” |
🩺 VII. Clinical Relevance in Nursing
| Condition | Tissue Affected | Nursing Focus |
|---|---|---|
| Stroke | CNS neurons | Monitor neuro signs, rehab support |
| Multiple sclerosis | Myelin sheath (CNS) | Fatigue, motor support, medication adherence |
| Alzheimer’s disease | Neuron degeneration (brain) | Cognitive care, safety |
| Parkinson’s disease | Dopaminergic neurons | Fall prevention, mobility, medication |
| Peripheral neuropathy | Sensory nerves (PNS) | Sensory checks, skin care, pain management |
| Spinal cord injury | CNS tracts | Bladder/bowel care, mobility, pressure ulcer prevention |
✅ Summary
| Feature | Nervous Tissue |
|---|---|
| Main cells | Neurons, glial cells |
| Functions | Sensory input, integration, motor output, communication |
| Impulse type | Electrical (within neuron), chemical (between neurons) |
| Regeneration | Limited in CNS, better in PNS |
| Control | Voluntary (somatic) and involuntary (autonomic) |
✨ Conclusion
Nervous tissue is the control and communication tissue of the body. It enables rapid response, coordination, and adaptation. Understanding its structure and function is key for assessing and managing neurological conditions, neurotrauma, reflexes, and cognitive disorders in nursing and clinical practice.
🧬 PHYSIOLOGY OF MEMBRANES – IN DETAIL
📌 Introduction
In physiology, the term “membrane” refers to either:
- Biological (cellular) membranes – at the cellular level (e.g., plasma membrane)
- Tissue-level body membranes – found covering organs, cavities, and joints
This explanation focuses primarily on the physiology of biological membranes, particularly the plasma (cell) membrane, and also briefly covers tissue-level membranes used in anatomy and nursing.
🧫 I. Physiology of the Plasma (Cell) Membrane
🔹 Definition:
The plasma membrane is a semipermeable barrier that surrounds every cell, separating its internal environment (cytoplasm) from the extracellular space.
🔬 II. Structure of the Plasma Membrane (Fluid Mosaic Model)
The plasma membrane is made of a phospholipid bilayer with proteins, cholesterol, and carbohydrates embedded in or attached to it.
🔸 Key Components:
| Component | Description | Function |
|---|---|---|
| Phospholipids | Form bilayer with hydrophilic heads & hydrophobic tails | Create semipermeable barrier |
| Proteins | Integral (span membrane) or peripheral (surface) | Transport, enzymes, receptors |
| Cholesterol | Inserted between phospholipids | Adds stability, fluidity |
| Carbohydrates | Attached to proteins/lipids (glycoproteins/glycolipids) | Cell recognition and signaling |
⚙️ III. Functions of the Plasma Membrane
| Function | Description |
|---|---|
| Selective permeability | Controls what enters/leaves the cell (e.g., nutrients, ions, waste) |
| Communication | Receptors for hormones, neurotransmitters |
| Protection | Physically protects internal cell components |
| Cell signaling | Interacts with other cells via proteins and glycoproteins |
| Transport | Facilitates movement of substances |
| Structural support | Anchors the cytoskeleton and helps maintain cell shape |
🔄 IV. Membrane Transport Mechanisms
Substances cross the membrane via passive or active processes.
🔹 A. Passive Transport (No energy required)
- Moves substances down their concentration gradient
| Type | Description | Example |
|---|---|---|
| Simple diffusion | Movement of small, nonpolar molecules | O₂, CO₂ |
| Facilitated diffusion | Uses channel or carrier proteins | Glucose, ions |
| Osmosis | Movement of water | Water entering a dehydrated cell |
🔹 B. Active Transport (Requires ATP)
- Moves substances against the gradient
| Type | Description | Example |
|---|---|---|
| Primary active transport | Uses ATP directly | Na⁺/K⁺ pump |
| Secondary active transport | Uses gradient created by another pump | Na⁺-glucose symport |
🔹 C. Bulk Transport (Vesicular Transport)
| Type | Description | Example |
|---|---|---|
| Endocytosis | Cell engulfs substances into vesicles | Phagocytosis (eating), Pinocytosis (drinking) |
| Exocytosis | Releases substances from cell | Neurotransmitter release, hormone secretion |
🧠 V. Membrane Potentials and Excitability
In excitable cells (neurons, muscle cells):
- The plasma membrane maintains a resting membrane potential via:
- Ion gradients (Na⁺ outside, K⁺ inside)
- Active Na⁺/K⁺ ATPase pump
- Essential for:
- Nerve impulses
- Muscle contraction
- Synaptic transmission
🧩 VI. Tissue-Level Body Membranes
These are multicellular sheets lining or covering body surfaces:
🔹 1. Mucous Membranes
- Line body cavities open to exterior (e.g., respiratory, digestive)
- Secrete mucus → protection, lubrication
🔹 2. Serous Membranes
- Line closed cavities (e.g., pleura, peritoneum, pericardium)
- Secrete serous fluid → reduces friction
🔹 3. Cutaneous Membrane
- The skin (epidermis + dermis)
- Protects, prevents dehydration, senses environment
🔹 4. Synovial Membranes
- Line joint cavities
- Secrete synovial fluid for lubrication
🩺 VII. Clinical Relevance in Nursing
| Condition | Affected Membrane | Nursing Implication |
|---|---|---|
| Cystic fibrosis | Defective chloride channels in membrane | Respiratory care, chest physiotherapy |
| Burns | Damaged cutaneous membrane (skin) | Fluid resuscitation, infection prevention |
| Edema | Altered membrane permeability in capillaries | Monitor fluid status, elevate limbs |
| Meningitis | Inflammation of meninges (meningeal membranes) | Neuro checks, antibiotics |
| Neuromuscular disorders | Defective membrane ion channels | Monitor respiration, assistive care |
✅ Summary
| Feature | Plasma Membrane |
|---|---|
| Structure | Phospholipid bilayer with proteins and carbs |
| Main Functions | Selective transport, signaling, protection |
| Transport Types | Diffusion, osmosis, active transport, endo/exocytosis |
| Membrane Potential | Important in nerve/muscle function |
| Tissue Membranes | Mucous, serous, synovial, cutaneous |
✨ Conclusion
The cell membrane is essential for maintaining the internal environment of the cell, regulating communication, transport, and response. At the tissue level, body membranes serve to protect, lubricate, and separate structures. A strong understanding of membrane physiology is vital in fluid balance, infection control, drug delivery, and neuro-muscular function.
🧬 PHYSIOLOGY OF KEY BODY MEMBRANES – IN DETAIL
I. 🔸 Anatomical and Protective Membranes
1. Mucous Membrane
- Location: Lines body cavities that open to the outside (e.g., respiratory, GI, urinary, reproductive tracts)
- Structure: Epithelial layer + lamina propria (loose connective tissue)
- Function:
- Secretes mucus for lubrication, moisture, and protection
- Traps dust/pathogens (e.g., respiratory tract)
- Involved in absorption and secretion
- Clinical Note: Inflamed in conditions like gastritis, rhinitis, bronchitis
2. Serous Membrane
- Location: Lines closed internal cavities (pleura, pericardium, peritoneum)
- Structure: Simple squamous epithelium (mesothelium) + areolar connective tissue
- Function:
- Produces serous fluid → reduces friction between moving organs
- Protects internal organs
- Clinical Note: Pleuritis, peritonitis, pericarditis occur when these membranes become inflamed
3. Synovial Membrane
- Location: Lines freely movable joints, tendon sheaths, bursae
- Structure: Loose connective tissue with synoviocytes (no epithelium)
- Function:
- Secretes synovial fluid to lubricate and nourish articular cartilage
- Clinical Note: Involved in arthritis, synovitis, and joint injuries
4. Cutaneous Membrane (Skin)
- Location: Covers the entire external surface of the body
- Structure: Stratified squamous epithelium (epidermis) + dermis (CT)
- Function:
- Barrier to pathogens, UV radiation, water loss
- Involved in thermoregulation, vitamin D synthesis, sensation
- Clinical Note: Skin diseases include eczema, psoriasis, burns
5. Basement Membrane
- Location: Between epithelial tissue and underlying connective tissue
- Structure: Made of collagen, laminin, and proteoglycans
- Function:
- Provides support and anchorage
- Regulates cell growth and filtration (e.g., in glomerulus)
- Clinical Note: Damaged in diabetic nephropathy, cancer invasion
6. Tympanic Membrane (Eardrum)
- Location: Separates external ear from middle ear
- Structure: Thin connective tissue membrane covered by skin on outside and mucosa on inside
- Function:
- Vibrates in response to sound waves
- Transmits vibrations to ossicles → hearing
- Clinical Note: Perforation leads to hearing loss, infection
II. 🔸 Functional/Respiratory/Developmental Membranes
7. Alveolar-Capillary Membrane
- Location: Interface between alveoli and pulmonary capillaries in lungs
- Structure: Alveolar epithelium + basement membrane + capillary endothelium
- Function:
- Facilitates gas exchange (O₂/CO₂)
- Clinical Note: Thickening in pulmonary edema, ARDS, or fibrosis impairs gas diffusion
8. Fetal Membranes (Amnion & Chorion)
- Location: Surround the fetus within the uterus
- Structure:
- Amnion: Inner layer, thin & transparent
- Chorion: Outer layer, vascularized, forms part of placenta
- Function:
- Amnion: Holds amniotic fluid → cushions, protects, allows fetal movement
- Chorion: Enables nutrient/gas exchange, hormone secretion
- Clinical Note: Rupture = “water breaking”; chorioamnionitis is a serious infection
III. 🔸 Serous Membranes – Detailed
9. Pleural Membrane
- Location: Lines thoracic cavity and covers lungs
- Structure: Visceral pleura (on lung), parietal pleura (on cavity wall)
- Function:
- Secretes pleural fluid → reduces friction during breathing
- Clinical Note: Pleural effusion, pneumothorax, pleurisy
10. Pericardial Membrane
- Location: Surrounds the heart
- Structure: Visceral pericardium (on heart), parietal pericardium (outer layer)
- Function:
- Produces pericardial fluid → cushions heart, prevents friction
- Clinical Note: Pericarditis, cardiac tamponade
11. Peritoneal Membrane
- Location: Lines the abdominal cavity and abdominal organs
- Structure: Visceral peritoneum (on organs), parietal peritoneum (on cavity wall)
- Function:
- Allows movement of intestines, secretes lubricating fluid
- Clinical Note: Peritonitis, ascites, peritoneal dialysis
IV. 🔸 Cellular and Subcellular Membranes
12. Endothelial Membrane
- Location: Lines blood and lymph vessels
- Structure: Simple squamous epithelium (endothelium)
- Function:
- Controls permeability, inflammation, blood clotting
- Clinical Note: Dysfunction in atherosclerosis, hypertension, sepsis
13. Nuclear Membrane (Envelope)
- Location: Encloses the nucleus
- Structure: Double membrane with nuclear pores
- Function:
- Regulates transport of RNA and proteins
- Maintains nuclear integrity
- Clinical Note: Disrupted in some genetic diseases and during cell division
14. Cell Membrane (Plasma Membrane)
- Location: Outer boundary of all cells
- Structure: Phospholipid bilayer with proteins and cholesterol (fluid mosaic model)
- Function:
- Selective permeability, signal transduction, cell recognition
- Clinical Note: Site of action for hormones, drugs, and toxins; involved in transport and immunity
✅ Summary Table
| Membrane | Main Function | Clinical Note |
|---|---|---|
| Mucous | Protection, secretion | Respiratory & GI infections |
| Serous | Friction reduction | Serositis (e.g., pericarditis) |
| Synovial | Joint lubrication | Arthritis, joint swelling |
| Cutaneous | Barrier & sensory | Burns, dermatitis |
| Basement | Anchoring & filtration | Nephropathy, cancer spread |
| Tympanic | Sound transmission | Perforation, otitis media |
| Alveolar | Gas exchange | ARDS, fibrosis |
| Amnion/Chorion | Fetal protection/nutrition | PROM, infection |
| Pleural | Lung movement | Pleural effusion |
| Pericardial | Heart protection | Cardiac tamponade |
| Peritoneal | Abdominal organ support | Peritonitis |
| Endothelial | Vascular integrity | Sepsis, clotting issues |
| Nuclear | Genetic regulation | Cell cycle control |
| Plasma Membrane | Selective transport, signaling | Transport disorders, drug action |
🧠 GLANDS – FUNCTIONS IN DETAIL
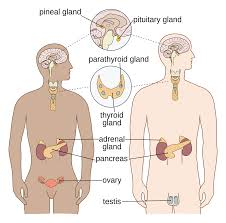
🔶 I. ENDOCRINE GLANDS
Secrete hormones directly into the bloodstream, regulating growth, metabolism, reproduction, etc.
1. Pituitary Gland (“Master Gland”)
Location: Base of brain, below hypothalamus
Lobes: Anterior & Posterior
🔹 Functions:
| Hormone | Function |
|---|---|
| GH (Growth Hormone) | Stimulates growth of bones/muscles |
| TSH | Stimulates thyroid gland |
| ACTH | Stimulates adrenal cortex |
| FSH/LH | Regulate ovaries/testes |
| PRL | Stimulates milk production |
| ADH (from posterior) | Conserves water in kidneys |
| Oxytocin | Triggers labor contractions, milk ejection |
🔍 Clinical Note: Disorders include gigantism, dwarfism, diabetes insipidus
2. Pineal Gland
Location: Deep in brain (epithalamus)
Secretion: Melatonin
🔹 Functions:
- Regulates sleep–wake cycle (circadian rhythm)
- Influenced by light/dark cycles
🔍 Clinical Note: Pineal tumors may affect sleep or puberty
3. Thyroid Gland
Location: Neck, in front of trachea
Hormones: T3, T4, Calcitonin
🔹 Functions:
- T3/T4: Regulate metabolism, heart rate, body temp
- Calcitonin: Lowers blood calcium by promoting bone storage
🔍 Clinical Note: Hyperthyroidism (Graves’), hypothyroidism (Hashimoto’s)
4. Parathyroid Glands
Location: Posterior surface of thyroid (4 glands)
Hormone: Parathyroid hormone (PTH)
🔹 Functions:
- Increases blood calcium by:
- Stimulating bone resorption
- Enhancing Ca²⁺ reabsorption in kidneys
- Activating vitamin D
🔍 Clinical Note: Disorders include tetany, bone demineralization
5. Adrenal Glands
Location: On top of kidneys
Parts: Cortex & Medulla
🔹 Cortex Hormones:
| Hormone | Function |
|---|---|
| Aldosterone | Regulates Na⁺/K⁺ balance, BP |
| Cortisol | Manages stress, glucose metabolism, inflammation |
| Androgens | Supplement sex hormones |
🔹 Medulla Hormones:
| Hormone | Function |
|---|---|
| Adrenaline/Noradrenaline | Fight-or-flight response |
🔍 Clinical Note: Disorders include Addison’s disease, Cushing’s syndrome
6. Thymus Gland
Location: Behind sternum (active in childhood)
Hormone: Thymosin
🔹 Function:
- Matures T-lymphocytes (immune function)
🔍 Clinical Note: Shrinks after puberty; dysfunction affects immunity
🔷 II. MIXED (ENDOCRINE + EXOCRINE) GLANDS
7. Pancreas
Location: Behind the stomach
Endocrine (Islets of Langerhans):
| Hormone | Function |
|---|---|
| Insulin | Lowers blood glucose |
| Glucagon | Raises blood glucose |
| Somatostatin | Regulates insulin/glucagon |
Exocrine:
- Secretes digestive enzymes into the duodenum (via pancreatic duct)
🔍 Clinical Note: Diabetes mellitus, pancreatitis
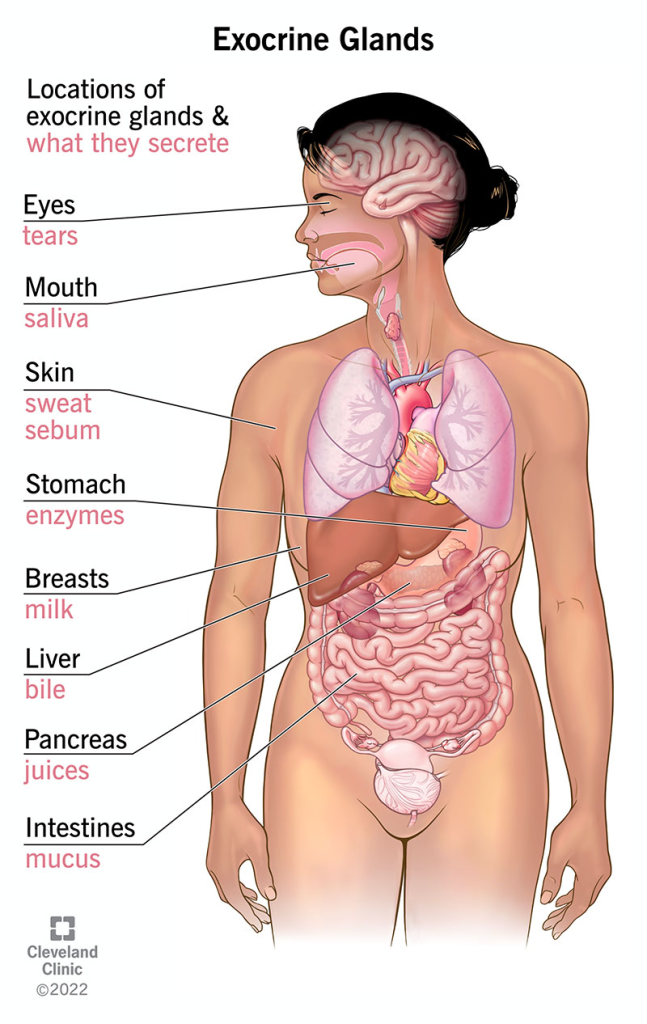
🔷 III. EXOCRINE GLANDS
Secrete substances via ducts to specific body surfaces or cavities
8. Salivary Glands
- Types: Parotid, submandibular, sublingual
- Secretion: Saliva
🔹 Functions:
- Lubrication, digestion of starch (amylase), oral hygiene
🔍 Clinical Note: Sialadenitis, dry mouth in dehydration
9. Sebaceous Glands
Location: Dermis of skin, associated with hair follicles
Secretion: Sebum
🔹 Function:
- Lubricates skin/hair, antibacterial action
🔍 Clinical Note: Acne, sebaceous cysts
10. Sweat Glands
Types: Eccrine (throughout body) and Apocrine (axilla, groin)
🔹 Functions:
- Eccrine: Regulate body temperature
- Apocrine: Secrete thick sweat (active after puberty)
🔍 Clinical Note: Hyperhidrosis, body odor, heat stroke prevention
11. Mammary Glands
Location: Breasts
Secretion: Milk
🔹 Function:
- Lactation – Provides nutrition and immunity to newborn
🔍 Clinical Note: Mastitis, galactorrhea, breast cancer
12. Lacrimal Glands
Location: Upper outer corner of eye orbit
Secretion: Tears
🔹 Functions:
- Lubricate eyes, protect from dust, antimicrobial via lysozyme
🔍 Clinical Note: Dry eye syndrome, dacryocystitis
13. Prostate Gland
Location: Surrounds male urethra below bladder
Secretion: Part of seminal fluid
🔹 Function:
- Enhances sperm mobility, neutralizes vaginal acidity
🔍 Clinical Note: Benign Prostatic Hyperplasia (BPH), prostate cancer
14. Bartholin’s Glands (in females)
Location: Vaginal opening
Secretion: Mucus
🔹 Function:
- Lubricates vaginal canal during arousal
🔍 Clinical Note: Bartholin cyst or abscess
15. Cowper’s Glands (Bulbourethral Glands)
Location: Below prostate in males
Secretion: Pre-ejaculate fluid
🔹 Function:
- Lubricates urethra, neutralizes acidity before ejaculation
🔍 Clinical Note: Infection or blockage can cause urethral pain
16. Gastric Glands
Location: Stomach lining
Secretion: HCl, pepsinogen, mucus, intrinsic factor
🔹 Functions:
- Digest proteins, protect lining, absorb B12
🔍 Clinical Note: Peptic ulcers, pernicious anemia
17. Intestinal Glands (Crypts of Lieberkühn)
Location: Intestinal lining
Secretion: Digestive enzymes, mucus
🔹 Functions:
- Aid in digestion and absorption, mucosal renewal
🔍 Clinical Note: Malabsorption syndromes, diarrhea
18. Liver (as an exocrine gland)
Secretion: Bile
🔹 Function:
- Emulsifies fats for digestion in the duodenum
🔍 Clinical Note: Hepatitis, bile duct obstruction, fatty liver
✅ SUMMARY CHART – GLANDS & THEIR FUNCTIONS
| Gland | Type | Main Function |
|---|---|---|
| Pituitary | Endocrine | Master control, regulates other glands |
| Thyroid | Endocrine | Metabolism regulation |
| Adrenal | Endocrine | Stress, BP, metabolism |
| Pancreas | Endo/Exocrine | Glucose regulation & digestion |
| Salivary | Exocrine | Digestion (amylase) |
| Sebaceous | Exocrine | Skin/hair lubrication |
| Sweat (eccrine/apocrine) | Exocrine | Thermoregulation, scent |
| Mammary | Exocrine | Milk production |
| Lacrimal | Exocrine | Tear secretion |
| Prostate | Exocrine | Sperm activation |
| Bartholin’s/Cowper’s | Exocrine | Reproductive lubrication |
| Gastric/Intestinal | Exocrine | Digestion |
| Liver | Exocrine | Bile secretion |
| Pineal | Endocrine | Circadian rhythm |
| Parathyroid | Endocrine | Calcium balance |
| Thymus | Endocrine | T-cell maturation |
🧬 TISSUE REPAIR – IN DETAIL
📌 I. What is Tissue Repair?
Tissue repair is the body’s biological process of restoring tissue integrity and function following injury, disease, or surgery. It may involve:
- Regeneration – restoring original tissue structure
- Fibrosis (scarring) – replacing damaged tissue with connective tissue
The goal is to re-establish homeostasis and prevent infection or further damage.
🔁 II. Types of Tissue Repair
1. Regeneration
- Damaged cells are replaced by the same type of cells
- Structure and function are fully restored
- Requires intact extracellular matrix (ECM) and proliferative capacity
✔ Occurs in:
- Epithelial tissues (skin, mucosa, liver)
- Bone tissue
- Blood and hematopoietic tissues
2. Fibrosis (Scar Formation)
- Replacement with fibrous connective tissue (collagen)
- Occurs when:
- The original tissue cannot regenerate
- The damage is extensive
- Basement membrane/ECM is destroyed
✘ Leads to:
- Loss of normal function
- Formation of scar tissue
✔ Seen in:
- Cardiac muscle after infarction
- Chronic liver damage (cirrhosis)
- Spinal cord injuries
🔄 III. Phases of Tissue Repair
🩸 1. Hemostasis (Immediate to Few Minutes)
- Vasoconstriction → stops bleeding
- Platelet aggregation → forms clot
- Clot releases growth factors (PDGF, TGF-β) → triggers repair
🔥 2. Inflammation (0–3 Days)
- Vasodilation → increases blood flow
- Neutrophils & macrophages:
- Remove debris, pathogens
- Release cytokines (IL-1, TNF-α) and growth factors
- Prepares site for healing
🌱 3. Proliferation (3–21 Days)
Key processes:
- Fibroblast proliferation → synthesize collagen & ECM
- Angiogenesis → new capillary growth for nutrient delivery
- Granulation tissue forms: rich in fibroblasts, collagen, and new vessels
- Re-epithelialization – epithelial cells migrate to cover wound
🧱 4. Remodeling (21 Days to 1 Year)
- Collagen reorganization (type III → type I)
- Blood vessels regress
- Scar tissue gains tensile strength (up to 80% of original strength)
⚙️ IV. Cells Involved in Tissue Repair
| Cell Type | Function |
|---|---|
| Platelets | Clot formation and release of growth factors |
| Neutrophils | Initial inflammation, phagocytosis of microbes |
| Macrophages | Debris cleanup, stimulate fibroblasts |
| Fibroblasts | Produce collagen and ECM |
| Endothelial cells | Form new capillaries (angiogenesis) |
| Epithelial cells | Cover wound surface (re-epithelialization) |
🔬 V. Mediators & Growth Factors
| Factor | Role in Repair |
|---|---|
| VEGF (Vascular Endothelial Growth Factor) | Stimulates angiogenesis |
| TGF-β (Transforming Growth Factor-β) | Stimulates ECM deposition, fibrosis |
| PDGF (Platelet-Derived Growth Factor) | Attracts fibroblasts |
| EGF (Epidermal Growth Factor) | Stimulates epithelial cell growth |
| IL-1, TNF-α | Promote inflammation, cell recruitment |
🧠 VI. Factors Affecting Tissue Repair
| Factor | Positive Influence | Negative Influence |
|---|---|---|
| Nutrition | Protein, vitamin C, zinc → collagen synthesis | Malnutrition delays healing |
| Oxygenation | Necessary for ATP, collagen cross-linking | Ischemia (e.g., diabetes, smoking) slows repair |
| Age | Young tissues heal faster | Aging slows regeneration |
| Infection | Mild inflammation helps healing | Chronic infection delays repair |
| Blood supply | Delivers nutrients and immune cells | Poor perfusion slows healing |
| Hormones/Drugs | Some support healing (e.g., GH) | Steroids suppress inflammation & fibroblasts |
| Chronic diseases | — | Diabetes, kidney/liver disease impair healing |
🏥 VII. Types of Wound Healing (Tissue Repair in Skin)
| Healing Type | Description | Examples |
|---|---|---|
| Primary Intention | Clean, surgical wound edges brought together; minimal scarring | Sutured wound |
| Secondary Intention | Wound left open; more inflammation and granulation; more scarring | Ulcers, burns |
| Tertiary Intention | Delayed closure after infection cleared | Infected surgical wounds |
🩺 VIII. Clinical Relevance for Nurses
- Monitor wounds for signs of infection, delayed healing
- Promote adequate nutrition & hydration
- Assist with dressing changes to maintain moist wound environment
- Educate patients about smoking cessation, diabetes control
- Use pressure-relieving devices to prevent pressure ulcers
- Recognize signs of abnormal healing:
- Keloid or hypertrophic scar
- Chronic wounds
- Dehiscence (wound reopening)
✅ Summary Table
| Phase | Key Events | Outcome |
|---|---|---|
| Hemostasis | Clot forms, platelets release factors | Bleeding stops |
| Inflammation | Neutrophils/macrophages clean site | Site prepared |
| Proliferation | Fibroblasts, angiogenesis, granulation | Tissue forms |
| Remodeling | Collagen realignment, scar formation | Final healing |
✨ Conclusion
Tissue repair is a dynamic and tightly regulated process involving inflammation, cellular growth, and remodeling. While regeneration restores original tissue, fibrosis replaces it with scar tissue. Nurses and clinicians play a crucial role in monitoring, supporting, and promoting effective healing through wound care, nutrition, and infection control.
🧬 PHYSIOLOGY OF CELL, TISSUES, MEMBRANES & GLANDS – APPLICATION & IMPLICATION IN NURSING
I. 🧫 CELL PHYSIOLOGY – Application in Nursing
🔬 Overview
- The cell is the basic structural and functional unit of all living organisms.
- It carries out essential processes: metabolism, growth, reproduction, communication, transport, and repair.
💡 Key Cellular Functions:
| Function | Nursing Application |
|---|---|
| Cell membrane transport | Important for understanding fluid/electrolyte therapy, IV infusions, osmosis and diffusion in dehydration, edema |
| Mitochondria (ATP production) | Guides energy needs in healing, fever, critical care |
| Protein synthesis | Important in tissue repair, immune response |
| Cell division (mitosis) | Crucial for wound healing, regeneration |
| Apoptosis (programmed cell death) | Relevant in cancer, immune regulation, tissue turnover |
🩺 Implications in Nursing:
- Administer correct IV fluids based on osmolality
- Recognize signs of cellular hypoxia (e.g., cyanosis, fatigue)
- Monitor lab values (electrolytes, glucose) that affect cellular function
- Educate patients on nutrition for cellular health and recovery
II. 🧬 TISSUE PHYSIOLOGY – Application in Nursing
🔬 Tissues are organized groups of similar cells performing a specific function.
💡 Types of Tissues & Nursing Relevance:
| Tissue Type | Key Function | Nursing Implication |
|---|---|---|
| Epithelial | Protection, absorption, secretion | Skin integrity, wound care, infection prevention |
| Connective | Support, transport, immunity | Joint support, fracture care, edema management |
| Muscle | Movement, heat, contraction | Assess mobility, maintain posture, prevent pressure sores |
| Nervous | Sensory & motor coordination | Neurological checks, reflex testing, communication support |
🩺 Implications in Nursing:
- Promote tissue healing through wound dressing, repositioning
- Support tissue perfusion (oxygen, nutrition)
- Understand the tissue-specific response to trauma, infection, inflammation
- Manage patients with degenerative diseases (e.g., Parkinson’s, multiple sclerosis)
III. 🧫 MEMBRANE PHYSIOLOGY – Application in Nursing
🔬 Membranes are layers of cells or tissues that cover surfaces, line cavities, or separate structures.
💡 Types & Functions:
| Membrane Type | Function | Nursing Application |
|---|---|---|
| Plasma (cell) membrane | Controls entry/exit of substances | Explains drug action, electrolyte therapy, cell swelling/shrinkage |
| Mucous membrane | Lubrication, protection | Oral care, GI/respiratory tract management |
| Serous membrane | Reduces friction | Manage pleuritis, pericardial effusion, ascites |
| Synovial membrane | Joint lubrication | Joint care, arthritis management |
| Cutaneous (skin) | Barrier, sensory | Prevent pressure ulcers, ensure hygiene, skin integrity |
| Basement membrane | Anchoring epithelium | Important in understanding wound healing, tumor spread |
🩺 Implications in Nursing:
- Prevent breakdown of skin/mucosa (e.g., in unconscious patients)
- Manage inflammation and fluid buildup (e.g., pleural, pericardial)
- Educate patients on skin care, joint protection, hydration
IV. 🧪 GLAND PHYSIOLOGY – Application in Nursing
🔬 Glands secrete substances like hormones, enzymes, sweat, or mucus either into the bloodstream (endocrine) or via ducts (exocrine).
💡 Types & Examples:
| Gland Type | Examples | Nursing Relevance |
|---|---|---|
| Endocrine | Pituitary, thyroid, pancreas (insulin) | Manage diabetes, monitor thyroid disorders, hormone therapy |
| Exocrine | Salivary, sweat, mammary, gastric glands | Oral hygiene, thermoregulation, lactation support, digestion |
| Mixed | Pancreas (insulin + enzymes) | Blood sugar monitoring, enzyme supplementation in pancreatitis |
🩺 Implications in Nursing:
- Administer hormonal drugs (e.g., insulin, thyroxine)
- Educate patients on diabetes care, hydration, glandular health
- Monitor body temperature and fluid loss (via sweat)
- Support gland-related disorders (e.g., goiter, adrenal crisis, hormonal imbalances)
🧠 V. Integrated Nursing Applications – Case Scenarios
| Scenario | Application |
|---|---|
| Wound care | Involves cell repair, epithelial tissue healing, basement membrane reformation |
| Diabetes | Involves endocrine gland (pancreas), cell glucose uptake, membrane transport |
| Stroke patient | Nervous tissue damage → need for neuro checks, skin protection, membrane care |
| Dehydration | Involves cell osmosis, mucous membrane dryness, exocrine gland reduction |
| Fever | Sweating → fluid/electrolyte loss → monitor membranes and tissues for dehydration |
| Hormonal therapy | Understanding gland secretion, cell receptor action, homeostasis |
✅ SUMMARY TABLE
| System | Physiological Concept | Nursing Application |
|---|---|---|
| Cell | Metabolism, transport, division | IV fluids, medication action, tissue repair |
| Tissue | Function-specific roles | Wound healing, mobility, neuro care |
| Membrane | Protection, secretion, diffusion | Infection control, respiratory, skin care |
| Glands | Hormone/enzyme secretion | Endocrine disorders, thermoregulation, digestion |