ENGLISH PERDIATRIC UNIT 5 CONG. CNS
Congenital Malformation of the central nervous system.
- Explain/Define Congenital Anomalies in children
Congenital anamolis is also called a birth defect.
Congenital Anamolis: = Any metabolic, biochemical, structural and functional disorder present in a child at the time of birth.
Congenital Malformation := When only structural defects are present in the child at the time of birth, it is called “Congenital Malformation”.
Congenital anamolis affects any part of the body and results in physical and developmental disabilities. This conservative anonymity is usually at the time of the development of the Child, the Genetic Factor, and the combination of both genetic factors, genital infections. Exposure to Hamafull Substance during the time (alcohol and certain types of medication), maternal health conditions such as diabetes, and obesity etc. and a combination of both.
Congenital anomalies involve central nervous system anomalies, cleft lip, cleft palate, heart disease, club foot, Down syndrome and genetic syndrome.
Explain the Etiology/cause of the congenital Anomalies in children
Genetic factors include inherited genetic mutations and chromosomal abnormalities that are passed down from parents to their children.
Ex:=
Autosomal dominant disorder (Marfan syndrome),
Autosomal recessive disorder (cystic fibrosis),
X-linked genetic disorder (hemophilia),
and chromosomal abnormalities (Down syndrome).
Due to environmental factors
Certain types of environmental exposures during pregnancy can increase the risk of congenital anomalies, such as:
Maternal infections during intrauterine life specially STORCH (syphilis toxoplasmosis, rubella, cytomegalo virus, herpes virus),
Due to mother’s exposure to teratogenic substances like alcohol, tobacco, smoking certain medicines, etc. during pregnancy.
X-ray exposure of the mother during pregnancy.
Due to the mother taking certain types of drugs during pregnancy such as steroid hormones,
stilbestrol,
Anticonvulsants, folate antagonists, cocaine, lithium and thalidomide.
Due to maternal diseases like diabetes, obesity, cardiac failure, malnutrition, iodine deficiency, folic acid deficiency etc.
Due to abnormal environmental conditions like bicornuate uterus, septate uterus, poly hydroamnios, oligohydro amnios, fetal hypoxia etc.
Due to environmental pollution.
Explain the Clinical manifestation/ sign and symptoms of the congenital Anomalies in children
1) Physical Abnormalities
Many types of congenital anomalies are visible such as,
Cleft Leap,
cleft palette,
Limb deformities
(club foot),
Facial features being abnormal,
Abnormal growth pattern (microcephaly and macrocephaly) etc.
2) Developmental delay
Some children who are congenitally anomalous have delays in achieving developmental milestones. It usually involves motor skills, language, speech development, cognitive abilities, social and emotional development, etc.
3) Organ Dysfunction
Certain types of congenital anomalies cause dysfunction in internal organs and its signs and symptoms such as,
Congenital heart disease (cyanosis, rapid breathing, poor feeding, failure to thrive etc.).
Anomalies of the gastro-interstitial tract (including feeding difficulties, nosia, vomiting,
abdominal pain, and failure to pass meconium etc.).
4) Neurological symptoms
Certain types of congenital anamolis affect the central nervous system, causing symptoms such as seizures, abnormal reflexes, muscle weakness, paralysis, developmental regression, intellectual disabilities, etc.
5) Respiratory symptoms
Certain types of congenital anamolis affect the respiratory system viz
Respiratory symptoms like respiratory distress, breathing difficulty, due to congenital diaphragmatic hernia, choanal atresia (narrowing of the nasal airway or tissues).
Rapid breathing and cyanosis may be observed.
6) Genitourinary abnormalities
Urinary tract abnormalities such as genital abnormalities, problem with kidney function, its symptoms include urinary tract infection, difficulty in urinating, abnormal genitalia etc.
7) Sensory impairment may be congenital deafness, blindness.
Enlist the common congenital Anomalies of the children
Common Congenital Anamolis Ma
1) Central Nervous System,
2) Congenital heart diseases,
3) Gastrointestinal system,
4) Respiratory system,
5) Genito-urinary system,
6) Musculoskeletal Abnormalities,
7) Blood disorders,
8) Metabolic disorders 9) Endocrine abnormalities,
10) Chromosomal Abnormalities
etc. the involvement of the system takes place.
1) Central Nervous System,
Anencephaly in the central nervous system, spina bifida occulta, spina bifida cystica (meningocele,
meningomyelocele ),
hydrocephalus,
Microcephaly, Macrocephaly,
Porencephaly etc.
2) Congenital heart diseases,
Congenital heart diseases such as atrial septal defect (ASD), ventricular septal defect (VSD),
Tetralogy of Fallot (TOF),
Coarctation of Aorta (COA),
Patent Doctor’s Arteriosis (PDA),
Trans position of great artery.
aortic stenosis,
pulmonary stenosis,
Mitral or aortic regurgitation
etc. is involved.
3) Gastrointestinal system,
Gastrointestinal system: Cleft lip, cleft palate, tracheoesophageal fistula, esophageal atresia, congenital pyloric stenosis, duodenal atresia, congenital megacolon (Hisprung’s disease), exomphalus, umbilical hernia, anorectal malformation, diaphragmatic hernia, femoral hernia, Gertcher Cheese, Congenital Intestinal Obstruction etc Involvement takes place.
4) Respiratory system,
Respiratory system includes choanal atresia, tracheoesophageal fistula, congenital atelectasis, pulmonary agenesis, congenital stridor, congenital cyanosis etc.
5) Genito-urinary system,
Congenital hydronephrosis in the genitourinary system,
Congenital Polycystic Kidney,
Hosea Sue Kidney,
hypospadias,
Includes epispadias, congenital phimosis, congenital hydrocele, undescended testis, congenital inguinal hernia, ambiguous genitalia etc.
6) Musculoskeletal Abnormalities,
Musculoskeletal club foot, congenital dislocation of hip, developmental dysplasia of hip (DDH), osteogenesis imperfecta, polydactyly, syndactyly, Marfan syndrome, muscular dystrophy etc.
7) Blood disorders,
Thalassemia, Hemophilia, Sickle Cell Anemia, G6PD Deficiency etc.
8) Metabolic disorders
Metabolic disorders like cystic fibrosis, phenylketonuria, G6PD deficiency, congenital lactose intolerance, galactosemia, Wilson’s disease, etc.
9) Endocrine Abnormalities,
Congenital hypopituitarism (dwarfism) in endocrine abnormalities,
Congenital hypothyroidism (cretinism), congenital adrenal hyperplasia, congenital goiter, diabetes mellitus without involvement.
10) Chromosomal Abnormalities In Chromosomal Abnormalities
Down syndrome
(Trisomy 21),
Edwards syndrome (trisomy 18),
Patau syndrome
(Trisomy 13),
Turner syndrome (Xo),
Klinefelter syndrome ( XXY ,XXXY).
11) Other Anomalies
Congenital Cataract, Congenital Glaucoma, Retinoblastoma, Color Blindness, Congenital Deafness, Deaf and Dumb, Mental Retardation, Albinism, Hemangioma, Peder Willi Syndrome, Apert Syndrome.
etc. are congenital anamolis.
Explain the diagnostic evaluation of the child with the congenital anomalies
(State the diagnostic evaluation of a child with congenital anomalies).
History taking and physical examination,
imaging studies,
Ultrasound during pregnancy,
x ray,
Magnetic Resonance Imaging,
computed tomography,
genetic testing,
Laboratory testing,
blood test,
Amniocentesis in early pregnancy (14 to 16 weeks),
Assay the maternal serum alpha phytoprotein (AFP),
antenatal screening,
Cardiac evaluation,
Neurological assessment,
Explain the complication of the child with the congenital Anomalies
Physical disability,
Limb deformity,
Health problems such as arrhythmias due to congestive heart defects,
heart failure,
Develop mental retardation,
Such as motor skills, language and cognitive impairment.
See the psychological challenge.
A psychological impact is seen,
Seeing educational challenges due to developmental delay.
Explain the management of the child with the congenital Anomalies
Children with congenital anomalies require regular medical monitoring and follow-up to monitor their growth development and overall health status. In which there is a need for regular physical assessment laboratory investigation, imaging studies etc.
Some anomalies require appropriate surgical intervention to treat and alleviate symptoms. This surgical intervention is usually a cardiac anomaly, limb deformity, cleft lip and cleft palate, any anatomical structure requiring surgical intervention for reconstruction.
Medication treatment is needed to relieve certain types of congenital anomalies such as congenital heart effects with symptoms such as arrhythmias, heart failure, medication to prevent blood clotting.
Free habilitation therapy to treat certain types of conjunctivitis requires physical therapy, speech therapy, occupational therapy, etc.
A child who has the condition of congenital abnormality needs to provide nutritious diet and feeding for the proper growth and development of the child.
To provide adequate counseling and psychological support to children with congenital anomalies and their family members to cope with the condition.
To provide complete education to the child’s family members about the child’s disease, its causes, symptoms and signs, and its treatment.
To provide proper genetic counseling to the family members of the child and his parents.
Some types of congenital anomalies require life-long treatment, so all health care providers and family members should be properly collaborative and cooperative to provide proper treatment to the child.
To provide adequate comprehensive care to children with congenital anomalies.
To provide adequate psychological support to the parents of the child.
Explain the preventive measures of the congenital Anomalies
1) Preconception care
In preconception care, providing counseling and proper education to women who are in child bearing age so that women can take proper health care during pregnancy.
It usually involves a healthy lifestyle, eating a balanced diet, maintaining an adequate weight, exercising regularly, avoiding harmful substances like alcohol and smoking, and getting proper treatment for any medical health problem.
2) Prenatal care
Early and comprehensive prenatal care is needed to properly assess maternal and child health. Due to prenatal screening, if the child has any congenital anomaly, its early detection and appropriate treatment is provided.
In which appropriate screening tests such as ultrasound and genetic testing are involved. And giving advice to women to take adequate nutritious diet, to take adequate fluids, to take folic acid supplements to prevent neural tube defects, to take adequate sleep, to avoid smoking and alcohol and not to come in contact with any harmful substance.
3) Genetic counseling and testing
By providing genetic counselling, education is provided to women and couples whether the child is at risk of any type of congenital or anomalous or not, in which family history, genetic factors, and previous pregnancies are assessed and proper counseling is provided. Congenital anomalies in children can be prevented by providing genetic counseling to women and couples.
4) Avoidance of teratogenic exposure
To provide proper education to the pregnant woman that she should not be exposed to teratogenic substances and harmful substances and any kind of radiation exposure, not to take harmful drugs due to which congenital anomalies in the child can be prevented, such as over the counter drugs, herbal supplements, Alcohol, tobacco, smoking, radiation, environmental toxins etc. are involved due to which there is risk of anomaly.
5) Optimizing Mother Health
The risk of congenital anomalies in the child can be prevented by providing appropriate health care before and during pregnancy.
If the mother has any long term diseases, it should be properly treated like diabetes mellitus, hypertension, and thyroid diseases.
If the mother has any kind of infection, treat her immediately.
Provide adequate food and vitamins supplements to the child if there is any nutritional deficiency.
6) Folic acid supplements
Adequate folic acid supplementation before pregnancy and during early pregnancy can prevent neural tube defects in the child. Like Spinabyfida, Anencephaly etc.
Women of childbearing age are advised to take daily supplements of 400 to 800 micrograms of folic acid ideally starting one month before conception and continuing through the first trimester after conception.
7) Environmental and Occupational Safety
A pregnant woman should not be exposed to any kind of hazardous chemicals and pollution, due to which anomalies can be prevented.
Occupational safety, guidelines and regulations should be followed regularly.
8) Screening and prenatal detection
Prenatal screening like ultra sound, maternal serum screening, and non invasive prenatal testing (NIPT) all these tests help in detecting any congenital anomalies and genetic abnormalities in the child. If early dissection takes place, adequate medical treatment can prevent congenital defects.
Congenital anomalies in the child can be prevented by using all these preventive measures.
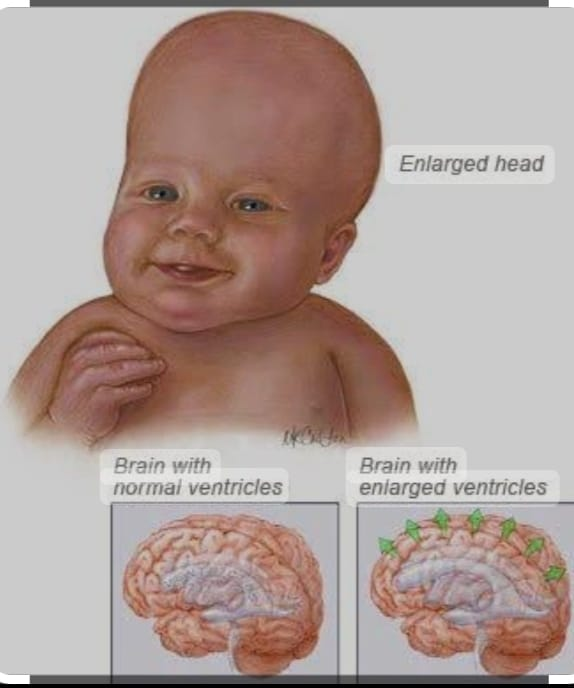
- Explain/Define Hydrocephalus in children
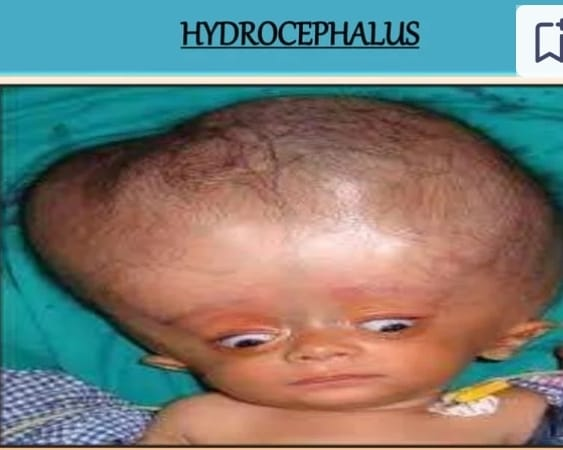
Hydrocephalus is a Greek word with hydro meaning “water” and cephalus meaning “head”. Hydrocephalus is an abnormal condition in which there is an abnormal accumulation of cerebrospinal fluid in the ventricular system and subarachnoid space. The pressure increases.
This condition of hydrocephalus usually results from an imbalance in the production and absorption of cerebrospinal fluid due to obstruction in the SCF pathway. Due to this, dilatation of the cerebral ventricles, enlargement of the head, cognitive impairment, seizures and other neurological problems are seen.
C.S.F pathway
Cerebrospinal fluid is secreted from the choroid plexuses of the ventricles by ultrafiltration and active secretion.
Cerebrospinal fluid from the lateral ventricles passes through the foramina of Monro into the third ventricle.
The cerebrospinal fluid from the third ventricles passes through the cerebral aqueduct (Aqueduct of Salvius) from the ventricles to the fourth ventricles.
The cerebrospinal fluid then passes into the basal cisterns and subarachnoid space through the foramen Luschka and foramen Magendi.
Cerebrospinal fluid is absorbed through the arachnoid wall in the venous canal and sinuses.
About 20ml of cerebrospinal fluid is secreted in one hour and 500ml / day. The total amount of cerebrospinal fluid is 100 to 150 ml.

Explain the Etiology/cause of the Hydrocephalus
The condition of hydrocephalus is mainly of two types, congenital hydrocephalus and acquired hydrocephalus.
1) Congenital hydrocephalus
Due to infection during intra-uterine life like,
STORCH (syphilis, toxoplasmosis, rubella, cytomegalo virus, herpes virus. ),
Caused by a congenital brain tumor that obstructs the flow of cerebrospinal fluid.
Due to malformations at birth,
Due to intracranial hemorrhage,
Due to cerebral malformation,
Due to stenosis and maldevelopment of the duct,
Due to maldevelopment of arachnoid villi,
Due to displacement of brain stem and cerebellum from foramen magnum (Arnoldchiri malformation),
Due to genetic factors.
2) Acquired hydrocephalus
Due to brain infection like,
Meningitis, encephalitis.
Due to trauma eg, birth trauma, head injury, intracranial haemorrhage.
Neoplasms like, tuberculoma, subdural hematoma and abscess, gliomas, ependymoma, astrocytoma, choroid plexus papilloma, pseudotumor cerebri.
Due to chemicals such as hypervitaminosis A.
Connective tissue disorders such as Hurler syndrome, achondroplasia,
Degenerative Atrophy of Brain,
Arteriovenous malformation, ruptured aneurysm.
3) Communicating hydrocephalus
Bacterial meningitis,
Malignant Meningitis,
hemorrhage,
Increased venous pressure.
4) Noncommunicating hydrocephalus
Due to congenital causes,
Due to Acquired Cause.
Explain the types of the Hydrocephalus
There are total four types of hydrocephalus.
1) Congenital hydrocephalus,
2) Acquired hydrocephalus,
3) Communicating hydrocephalus,
4) Noncommunicating hydrocephalus.
1) Congenital Hydrocephalus,
Congenital hydrocephalus is present at birth. And it is usually caused by some environmental factor and genetic factor during fetal development.
2) Acquired hydrocephalus,
Acquired hydrocephalus develops at birth. And even then it develops. Acquired hydrocephalus is caused by any birth injury and birth trauma.
3) Communicating hydrocephalus,
In communicating hydrocephalus there is no blockage of the ventricular system, basal cisterns, and spinal subarachnoid space. In this communicating hydrocephalus, excessive production of cerebrospinal fluid (CSF) and inadequate absorption of cerebrospinal fluid (CSF) does not occur, resulting in an accumulation of fluid in the brain that is responsible for creating hydrocephalus.
4) Noncommunicating hydrocephalus.
This noncommunicating hydrocephalus occurs due to obstruction in any of the ventricular systems (usually the aqueduct, foramen Luschka, and Magendi). This obstruction can usually be partial, intermittent, or even complete. This obstruction usually develops due to inflammation and obstructive lesions. Due to this blockage, the flow of spinal fluid within the brain is impaired. Due to this there is an accumulation of fluid in the brain which creates the condition of hydrocephalus.
Explain the Clinical manifestation/ sign and symptoms of the Hydrocephalus
Accumulation of cerebrospinal fluid in the ventricles of the brain.
Excessive enlargement of the head.
To become a sine skull.
Separation of cranial sutures due to head enlargement.
Fontanels are bulging, scalp is singed and veins are dilated.
Percussion of the skull produces a “cracked pot” resonance (Macewen’s sign).
See the sunset sign (sclera visible above the iris).
His face looks small compared to his head.
Increased intracranial pressure.
Having hemiplegia.
Cry is hoarseness.
Often occurring in papilloae.
Spasticity occurs.
Ataxia.
Urinary incontinence.
Progressive deterioration of mental function.
Nozia.
Vomiting.
Restlessness.
Irritability.
Irregular and decreased respiration.
The pulse will decrease.
Having a convulsion.
feeling tired
Stupor and coma.
Head one.
Lethargy.
from the app.
Changes in personality.
Irritability.
Confusion.
Visual problem.
Explain the Diagnostic evaluation of the child with the Hydrocephalus
History taking and physical examination.
Measuring head circumference.
Cranial ultrasonography.
x ray
CT scan.
M.R.I.
Neurological examination.
Ventriculography.
Pneumoencephalography.
Intracranial pressure monitoring.
Neuropsychological assessment.
Genetic testing.
Intracranial pressure monitoring.
Explain the medical management of the child with the Hydrocephalus.
If the condition of hydrocephalus is mild and stable, then continuous monitoring of the child by healthcare personnel. Continuous monitoring of the child’s head circumference, developmental milestones etc.
If the child has mild symptoms, provide adequate medication to reduce the symptoms.
A carbonic anhydrase inhibitor, acetazolamide (Dymox), is used to reduce the production of CSF.
Oral glycerol and isorbital are used in children to reduce increased intracranial pressure.
If the child has the condition of hydrocephalus due to any obstruction, there is a need for surgical management.
Perform lumbar puncture to maintain cerebrospinal fluid pressure.
The most common method to treat the condition of hydrocephalus is stent placement. such as abdominal VT.)
Endoscopic third ventriculoostomy (ETV) is performed in certain cases such as non-communicating hydrocephalus in which the obstruction causes hydrocephalus. Obstruction of the pathway is bypassed and can move into the subarachnoid space where it is absorbed.
Explain the types of shunt procedures
1) Ventriculo peritoneal shunt
In this procedure, one part of the shunt catheter is inserted into the anterior border of the lateral ventricles in the brain while the other end of the shunt is inserted into the skin of the peritoneal cavity. and pathways of cerebrospinal fluid are diverted from the ventricles into the peritoneal cavity.
2) Ventriculo pleural shunt (VPL)
This shunt is similar to a ventriculoperitoneal shunt in that one end of the shunt catheter is inserted into the ventricles and the other end of the shunt catheter is inserted into the pleural cavity (around the lungs). Due to this shunt, cerebrospinal fluid flows into the pleural cavity and is absorbed there.
3) Ventriculo atrial shunt
To collect cerebrospinal fluid in a ventriculo-atrial shunt, the distal end of the shunt catheter is inserted into one ventricle of the brain and the other end of the shunt catheter is inserted into the atrium of the heart via the jugular vein. By performing this shunt procedure, the pathway of cerebrospinal fluid is entered into the blood stream where it is absorbed.
4) Long peritoneal shunt
A long peritoneal shunt involves diverting cerebrospinal fluid from the lumbar subarachnoid space (lower spine) into the peritoneal cavity. which may lead to absorption of cerebrospinal fluid into the abdominal cavity.
5) Ventriculo ureter shunt
This type of shunt is usually used in older children when all other types of shunts have failed to divert cerebrospinal fluid from the ventricles to the ureters.
Explain the Nursing management of the child with the Hydrocephalus
Preoperative nursing management
Properly and continuously assess the child including baseline health status, vital signs, neurological status and hydration status of the child.
Continuously monitor the child’s intracranial pressure.
Continuously measure the child’s head circumference.
Palpate the child’s fontanelles to assess for any increased intracranial pressure.
Assess the child’s pupillary response and level of consciousness.
To continuously monitor the child’s vital signs.
To provide proper work and quiet environment to the child.
Maintain aseptic technique while handling the child to prevent nosocomial infection.
Changing the child’s position continuously.
To properly maintain the child’s nutritional status.
Provide intravenous fluid to the child properly.
Keeping the child Nil Per Oral (Nil Per Oral).
Continuously monitor child’s intake output chart.
To properly collaborate with other health care personnel for proper care of the child.
Surgery is a stressful condition for the child and its family members, so proper education and psychological support should be provided to the child’s parents.
To provide proper assurance and emotional support to the parents of the child.
Post operative management
Monitoring the child continuously and closely after the surgery.
To monitor the child’s vital signs frequently every fifteen to twenty minutes.
Properly monitoring the neurological status of the child.
Monitoring the child frequently if there is an alteration in body temperature.
Position the child at the non-operative site to prevent pressure on the shunt.
After surgery, the child is usually provided with a flat position on the bed for 24 hours.
Assess the child’s photoreceptors to immediately notice if depressed.
If the child is in pain, provide analgesic medication to relieve it.
Do this if the child has any complications after the surgery or not.
Provide proper fluid to the child and maintain his hydration status. To continuously monitor the intake output chart of the child. And continuously maintain the child’s electrolyte level.
Provide dressing to the child by maintaining proper aseptic technique on the surgical side.
To provide proper support and education to the child and his family members.
- Explain/Define Cerebral palsy (CP)
Cerebral :=mins brain related
Palsy : = Minus weakness and problem in body movement.
Cerebral palsy is a medical condition. It is usually seen due to abnormal development of the brain before birth and due to injury to parts of the brain after birth due to which the normal movement of the body is lost.
Cerebral palsy is a group of disorders of permanent movement, posture and muscle tone that usually occur during early childhood.
Cerebral palsy is usually caused by abnormal development and injury to the central nervous system (CNS) pathways that control movement, balance and posture.
Cerebral palsy usually affects muscle movement, coordination, muscle tone, and motor skills, leading to difficulties in movement and posture.
Cerebral palsy is a non-progressive neuromuscular disorder of the cerebral region that usually occurs as a result of brain injury, affecting muscle control, strength, posture, and movement.
Explain the Etiology/cause of Cerebral palsy
Prenatal causes
Due to genetic factors,
Due to the structural malformation of the nervous system,
Due to brain malformation,
Due to brain infection,
Due to cytomegalovirus infection,
Due to maternal health conditions such as diabetes, hypotension, thyroid diseases, and exposure to any toxic substance during pregnancy.
Perinatal causes
Due to hypoxic ischemic injury,
Due to pre-mature birth,
Due to low birth weight,
Due to intrauterine infection,
Due to introversion at birth,
Due to electrolyte disturbance,
Due to respiratory distress syndrome,
Due to jaundice,
Due to birth asphyxia,
Due to intracranial hemorrhage,
Due to hyperbilirubinemia,
Due to hypoglycemia,
Due to infection in the central nervous system.
Postnatal causes
Due to intracranial injury,
Due to infection in the central nervous system like meningitis, encephalitis etc.
Due to hypoxia.
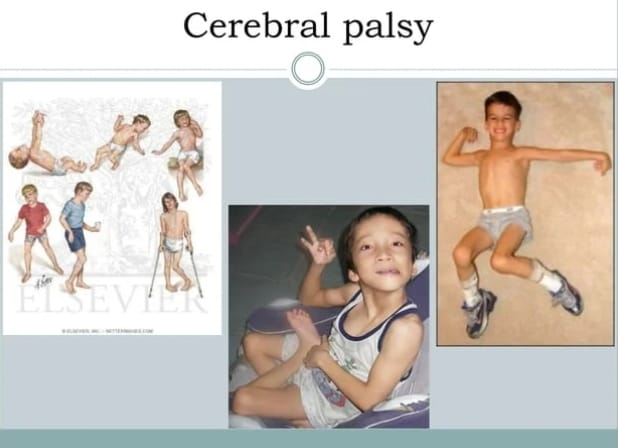
Explain the Classification of the cerebral palsy
1) Pyramidal cerebral palsy,
2) Extra pyramidal cerebral palsy,
3) Mixed type cerebral palsy.
••>
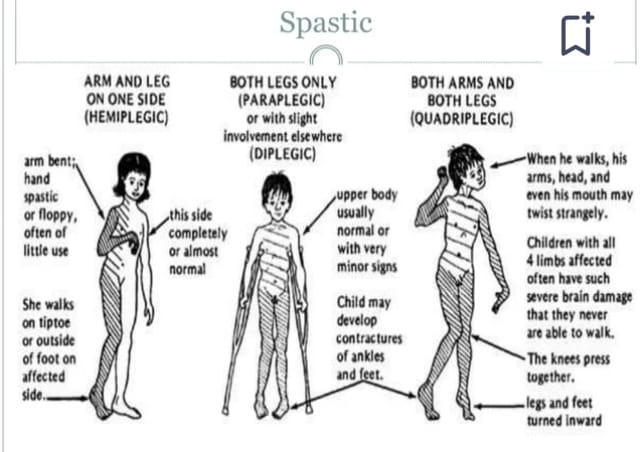
1) Pyramidal cerebral palsy,
Pyramidal cerebral palsy, also known as spastic cerebral palsy,
It causes stiffness and tightness of muscles,
Which is caused due to the damage of the pyramidal track of the brain.
This track is responsible for transmitting motor signals from the brain to the spinal cord and muscles.
Features:
Individuals with pyramidal CP typically,
spasticity,
Reflexes become exaggerated,
Voluntary movement is impaired. Muscle stiffness often results in jerking and stiff movements and affects fine motor skills and gross motor skills.
Type: Pyramidal cerebral palsy can be further classified based on motor impairment, such as hemiplegic (affects one side of the body), diplegic (primarily affects both legs), or quadriplegic (affects all four extremities). ).
2) Extra pyramidal cerebral palsy,
Extrapyramidal cerebral palsy is characterized by involuntary, uncontrolled movement and posture caused by damage to the extrapyramidal system, which is caused by damage to the parts of the brain that control movement and muscle tone.
Features:
Individuals with extrapyramidal cerebral palsy ma
Dyskinetic movement
can occur, such as athetosis,
Dystonia (continuous muscle contractions causing abnormal posture), or chorea (rapid, jerking movements). This movement often affects the arms, legs and face and its intensity can also change.
Reasons:
Extrapyramidal cerebral palsy is often caused by damage to the basal ganglia or other subcortical structures of the brain caused by perinatal hypoxia, kernicterus (bilirubin-induced brain damage). or due to some genetic factor.
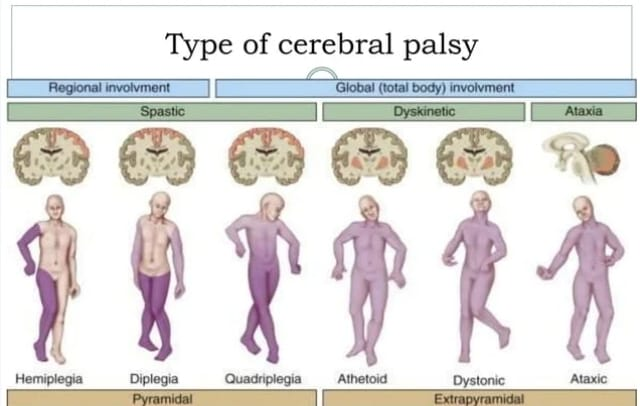
A) Coryeth cerebral palsy
Coryeth cerebral palsy has abnormal, involuntary movements and postures.
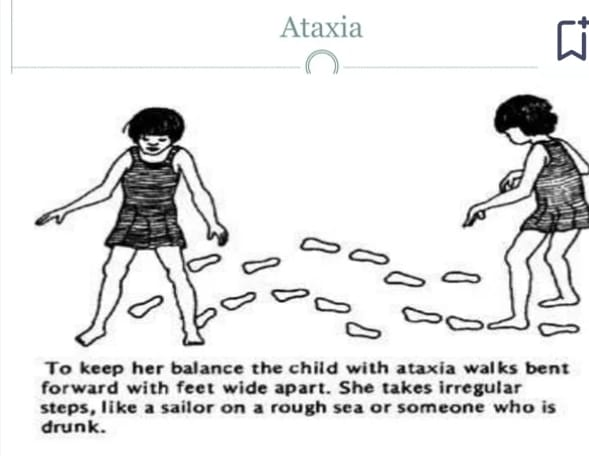
B) Ataxic cerebral palsy
Balance and coordination are impaired in ataxic cerebral palsy. Tremors are an important and prominent sign in ataxic cerebral palsy.
C) Dystonic cerebral palsy
In dystonic cerebral palsy, muscle tone is increased and postural disturbance occurs.
3) Mixed type cerebral palsy.
In mixed type cerebral palsy there is involvement of pyramidal and extrapyramidal symptoms, where individuals have symptoms of both spasticity and dyskinesia.
Explain the Classification according to severity
a) Mild cerebral palsy
In this the child is ambulatory and only has impairment in his fine movements.
b)Moderate cerebral palsy
In this child, gross motor, fine motor and speech development is impaired.
c) Severe cerebral palsy
In this the child presents multiple defects and the child is not able to perform his daily routine activities.
Explain the sign and symptoms/ clinical manifestation of the child with the cerebral palsy.
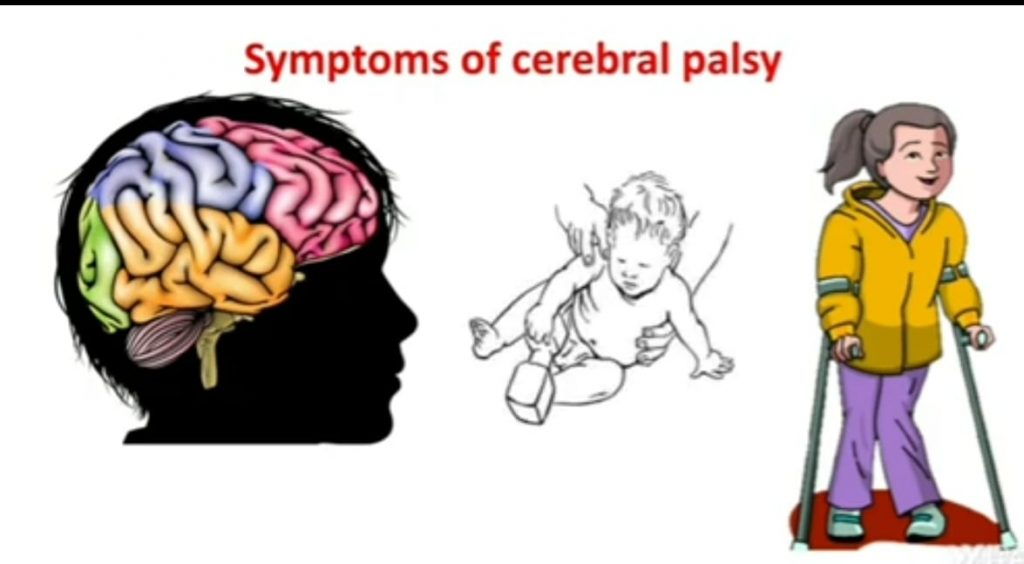
Asymmetrical movement,
lightness,
Irritability,
Difficulty in feeding and swallowing,
Excessive high pitch and fibbling cry,
Poor head control,
Weight gain slows down,
Gross motor development delay,
coming to wickness,
Abnormal posture,
drooling,
Recurrent infection,
Stool incontinence,
Malocclusion of teeth,
Tooth decay,
Having speech difficulty,
Mental retardation,
Gastroesophageal reflux,
Visual defect,
Hearing impairment,
having a speech disorder,
Behavioral problems are observed.
1) Pyramidal cerebral palsy,
quadriplegia,
paraplegia,
hemiplegia,
tri plegia,
Dy plegia,
monoplegia,
Persistent reflexes may be observed.
feeding difficulty,
Voluntary moment restriction occurs,
A child with multiple handicaps,
Neurological deficits,
Behavioral problems are observed.
2) Extrapyramidal cerebral palsy
dyskinesia,
athetosis,
dystonia,
tremors,
Rigidity, including involvement of the legs, neck, and trunk,
Involuntary, uncoordinated,
An uncontrollable moment,
3) Atonic cerebral palsy
hypotonia,
hyporeflexia,
ataxia,
Tremors
4) Mixed type cerebral palsy
Both pyramidal and extrapyramidal are involved.
Look for neurological symptoms.
Deformity Associated Cerebral Palsy
Disturbance in mental development,
growth retardation,
Caesar,
Sensory impairment,
Vision impairment,
Hearing impairment,
Speech impairment,
Gait disturbance.
Explain the Diagnostic evaluation of the child with the cerebral palsy
History tacking and physical examination,
A screening test to assess metabolic defects,
Neurological examination,
Developmental Assessment,
Blood test for VDRL,
electromyography,
electroencephalography,
Intelligence Quotient Test,
Hearing Ability Test,
vision test,
Psychological Disorders Assessment,
cityscan,
MRI,
psychometry test,
Urine and blood examination.
Explain the management of the child with the cerebral palsy
Drug therapy
If the child has spasticity and hypotonia, provide diazepam medication.
If the child has athetosis, provide chlordizepoxaad and levodopa medication.
Carbamazepine medication should be provided if the child has the condition of dystonia.
If the child has epilepsy, provide anticonvulsant medication.
If child has behavioral problems and provide tranquilizer medicine as muscle relaxant and improve muscle function.
Physical therapy
Providing the child with proper orthodic devices like braces, splints and castings.
Providing properly adaptive equipment to the child like bicycle, suitable vehicle and wheelchair.
Occupational therapy
Providing proper occupational therapy to the child.
Providing proper computer education to the child.
Speech / Language Therapy
Using motor skills to improve speech therapy.
Adopting communication techniques.
Social Education Therapy
Providing education about early intervention and programs.
Providing education about individualized education programs.
Running specialized learning programs and support services in schools.
Surgical management
Orthopedic surgery of child like tendon transfer, muscle strengthening.
Perform selective rhizotomy to decrease spasticity.
Provide orthopedic support by providing splints and orthopedic devices.
Explain the Nursing management of the child with the cerebral palsy.
Health Assessment and Monitoring
Continuously monitoring the child’s nutritional level, hydration level, growth assessment and overall health assessment of the child.
To monitor the child’s vital signs properly.
Properly monitoring the neurological status of the child.
Monitor child’s respiratory status properly.
Continuously monitoring the child for any other complications.
Assess the child’s musculoskeletal function including muscle tone, range of motion, and continuously assess whether any contractures and deformities are present.
Providing properly prescribed medication to the child.
Providing complete education to child’s care giver about medication dosage, timing, side effects.
Providing nutritious diet to the child to maintain the nutritional status of the child.
Assisting the child in mobility in small amounts can prevent pressure sores.
To provide orthopedic devices to improve the mobility of the child.
Provide physical therapy to improve child’s muscle strength, flexibility, muscle tone.
To provide complete education about the child’s condition to the child’s parents and their care givers.
To provide proper psychological support and counseling to the child and his family members.
Communicate properly with the child to improve his communication skills.
To properly collaborate with other health care personnel for proper care of the child.
- Explain/Define Spina bifida
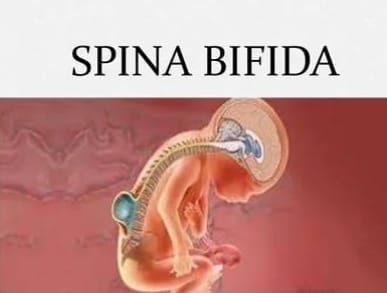
Spina bifida is a congenital neural tube defect. The neural tube is normally responsible for foaming and closing the spinal cord and brain during early embryonic development.
When the spinal cord is formed, it does not close completely and there is a gap between the vertebrae. Due to this incomplete spinal cord closure, different types of malformation of the spinal cord and spinal column are seen.
When the vertebral column has a defect in closure and there is a space between them, the tissues are exposed from this bony space and the sac (sac) like structural protrusion is called spina bifida.

Explain the types of the spina bifida
There are mainly three types of spina bifida.
1) Spina bifida occulta.
2) Spina bifida meningocele.
3) Spina bifida meningomyosele.
••>
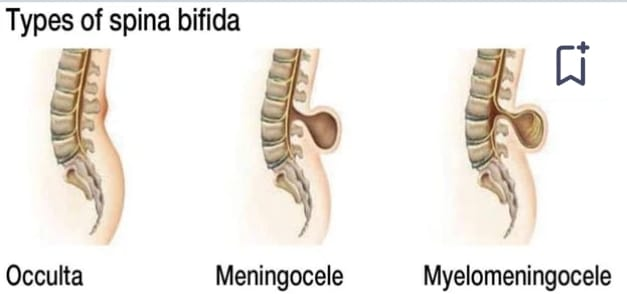
1) Spina bifida occulta.
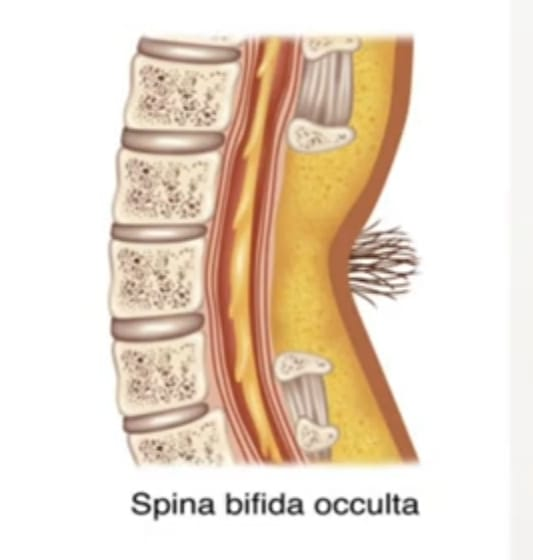
Spina bifida occulta is the mildest and more common form of spina bifida, where the spinal cord and nerves are usually unaffected. In spina bifida occulta, there is a small gap or opening in one or more spinal cords but it is covered by a layer of skin, so there is no visible protrusion of the spinal cord or meninges. Often, this form of spina bifida does not even show symptoms.
2) Meningocele:
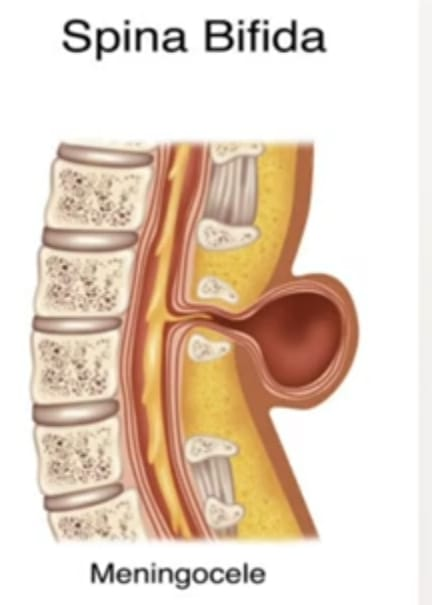
In this form, the protective layer surrounding the spinal cord (meninges) herniates (protrudes) outward from the lower back area through a gap or opening in the spinal cord, forming a sac or cyst filled with the meninges layer and cerebrospinal fluid. . As with myelomeningocele, the spinal cord itself is not involved, and the neurological deficit is less severe.
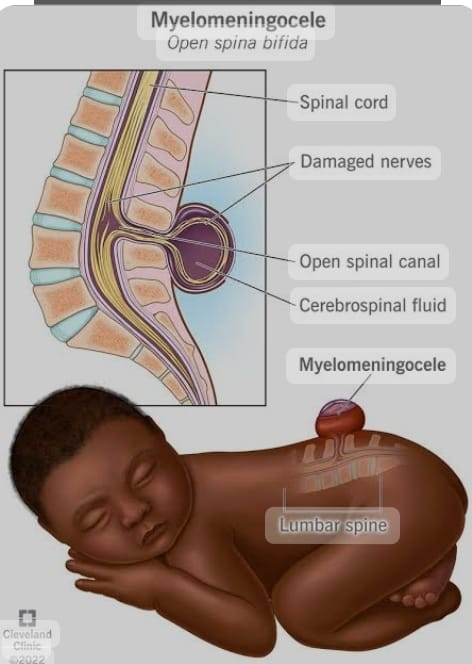
3) Spina bifida meningomyosele.
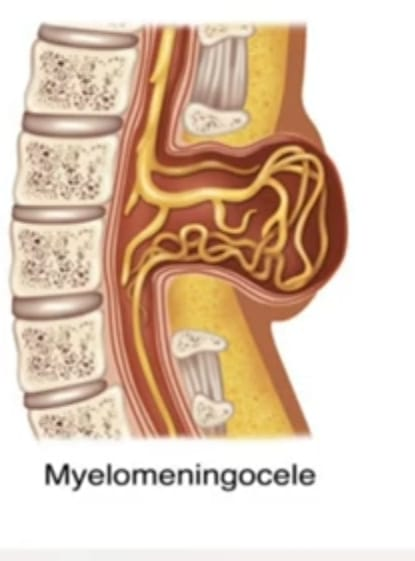
Meningomyelocyle is the most severe form of spina bifida, where the spinal cord, meninges and nerves protrude through a gap or opening in the spinal cord, the lower back area covered by a thin layer of skin, a sac or cyst. Makes.
Neurological deficits are often seen in meningomyelocyles leading to functional impairment. Individuals with meningomyelocyles develop paralysis, muscle weakness, sensory loss, bowel and bladder dysfunction, and other complications such as hydrocephalus (fluid accumulation in the brain), Chiari, and malformations.
Explain the Etiology/cause of the Spina bifida
The exact cause of spina bifida is unknown.
Due to genetic factors,
Due to environmental factors,
Due to intake of folic acid (vitamin B9) in inadequate amount by the mother during the first trimester.
Due to maternal disease conditions like diabetes, obesity,
Due to mother’s exposure to teratogenic substances (smoking, alcohol, tobacco, drugs) during pregnancy,
Due to advanced maternal age,
Due to hyperthermia condition in mother during pregnancy.
Due to the mother taking certain types of anticonvulsant medication during pregnancy.
Explain the clinical manifestation/ sign and symptoms of the child with the spina bifida.
Symptoms and signs of spina bifida usually depend on its type.
1) Spina bifida occulta.
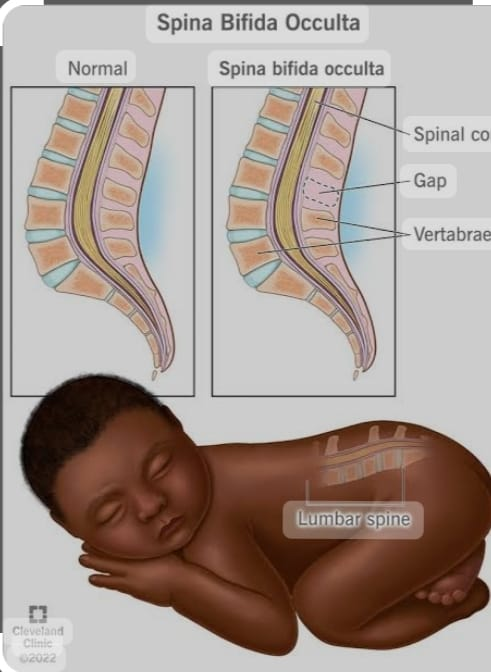
Spina bifida occulta usually has no noticeable signs and symptoms. But some children may have a small dimple, birthmark, hair lump or fatty lump on the skin on the lower back area due to spinal cord defect.
Neurological symptoms like weakness, numbness, bowel and bladder dysfunction are seen.
2) Meningocele.
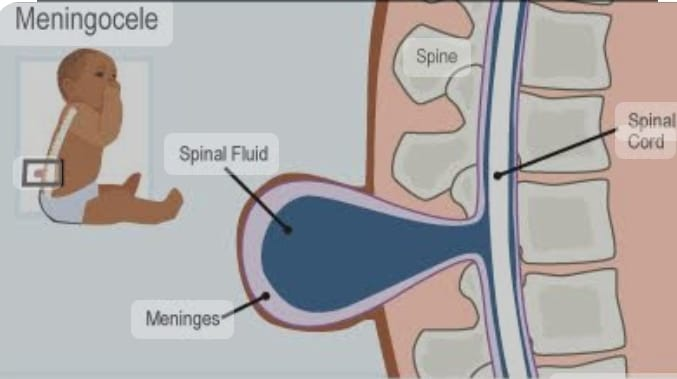
A meningocele is a protruding sac or cyst filled with cerebrospinal fluid, usually through an opening in the spinal cord. A sac is covered by a thin layer of skin and usually occurs in the lower back or sacral region.
Neurological symptoms are usually few or absent because there is no involvement of the spinal cord. However, associated bowel and bladder dysfunction is seen.
3) Meningomylosil.
Meningomyelocyle is the most severe form of spina bifida and involves protrusion of the spinal cord, its protective layer (meninges), and the spinal cord into the lower back region.
A sac or cyst that contains an exposed spinal cord is usually covered by a thin layer of skin and is prone to rupture or infection.
Neurological symptoms are seen and include paralysis, muscle weakness, sensory loss, and bowel and bladder dysfunction. Other symptoms in meningomyelocyles may include hydrocephalus (accumulation of fluid in the brain), Chiari malformations, orthopedic deformities (eg, scoliosis), and skin breakdown or pressure ulcers.
Other symptoms
Orthopedic abnormalities such as club foot,
Finding hip displacement,
Impaired bowel and bladder function such as urinary incontinence, urinary tract infection,
Impaired renal function,
Pressure sores and skin irritation,
Abnormal eye movement,
68% of children with spina bifida have a latex allergy.
paralysis,
scoliosis,
back pain,
Partial and complete loss of sensation,
Weakness in the body,
Other symptoms
Dimpling is seen in lower back region i.e. mainly sacral region,
Hey look,
Difficulty in swallowing leads to conditioning of choking,
Hosannas of Voice,
Breathing difficulty while sleeping,
Impaired intelligence level,
Impaired cognitive level.
Explain the Diagnostic evaluation of the child with the Spina bifida
Pre natal screening
Maternal Serum Alpha Phyto Protein (MSAFP)
screening,
prenatal ultrasound,
Amniocentesis,
Alpha Phytoprotein (AFP) Assessment,
imaging studies,
ultrasound,
Laboratory testing,
radio graph,
myelogram,
spinal tomogram,
Neurological assessment,
Explain the management of the child with the Spina bifida
Medical management
Surgical repair of the condition of spina bifida after birth can prevent the child from infection and maintain neurological function.
If the child has a condition of hydrocephalus, divert the flow of cerebrospinal fluid by providing a proper ventricular catheter.
If the child has any orthopedic complication, treat it properly surgically and provide physical therapy.
If the child has bowel and bladder dysfunction, treat it properly.
Provide proper physical therapy to the child like exercises, stretches and great training.
If the child has any other complication then treat it immediately.
To provide complete education to the child and his family members about the child’s condition, its causes, symptoms and signs, and its treatment.
To provide proper psychological support and counseling to the child and his family members.
To properly maintain the nutritional status of the child.
Providing properly assistive devices like orthosis, braces, to the child.
To provide proper work and comfortable environment to the child.
Explain the nursing management of the child with the spina bifida
A child with spina bifida needs to be provided with holistic nursing management.
To properly assess the child.
Proper assessment of physical, psychological, developmental and psychosocial needs of the child.
To properly assess the child’s vital signs.
Assessing the neurological status of the child.
Child’s Bowel and Bladder Function,
Properly assess skin integrity and musculoskeletal health.
Continuously monitoring the child’s nutritional status, hydration status, no growth.
If the condition of spina bifida has been surgically repaired, maintain aseptic technique and provide proper dressing in the wound area to prevent infection of the child.
To maintain the nutritional status of the child.
To provide properly assistive devices to the child to improve his mobility.
To provide complete education to the child’s family members and parents about the condition of spina bifida, its causes, symptoms and signs, and its treatment.
Providing proper emotional support and counseling to parents.
To have proper therapeutic communication with the child’s parents.
Advising parents to follow up regularly.
- Explain/Define meningocele.
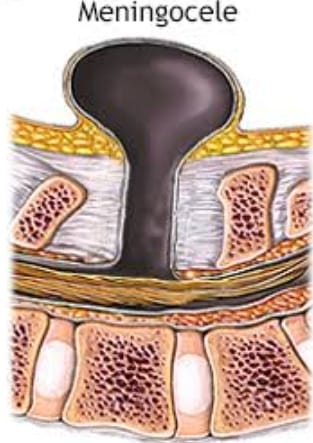
Meningocele is a type of congenital neural tube defect in which the meninges, the protective layer of the spinal cord, protrude (herniate) through a defect (gap or opening) in the spinal column, resembling a sac filled with cerebrospinal fluid (CSF). Structural A forms in the lower back area. And it is covered by a thin layer of skin. Even if there is minimal trauma, CSF can leak and infection can also occur.
As in meningocele, the spinal cord itself is usually not involved and the nerve does not protrude, so the neurological deficit is less severe in meningocele.
Explain the Etiology/cause of the child with the meningocele
The exact cause of meningocele is unknown.
Due to genetic factors,
Due to environmental factors,
Due to intake of folic acid (vitamin B9) in inadequate amount by the mother during the first trimester.
Due to maternal disease conditions like diabetes, obesity,
Due to mother’s exposure to teratogenic substances (smoking, alcohol, tobacco, drugs) during pregnancy,
Due to advanced maternal age,
Due to hyperthermia condition in mother during pregnancy.
Due to the mother taking certain types of anticonvulsant medication during pregnancy.
Explain the clinical manifestation/ sign and symptoms of the child with the meningocele.
A meningocele is a protruding sac or cyst filled with cerebrospinal fluid, usually through an opening in the spinal column. A sac is covered by a thin layer of skin and usually occurs in the lower back or sacral region.
Neurological symptoms like weakness and paralysis,
Bowel and bladder dysfunction may occur.
A visible sac-like structure in the lower back region i.e. mainly sacral region which is covered by skin,
Hey look,
Difficulty in swallowing leads to conditioning of choking,
Hosannas of Voice,
Sensory deficits such as numbness and tingling sensation in legs and feet,
Breathing difficulty while sleeping,
Impaired intelligence level,
Respiratory difficulty,
Impaired cognitive level.
Explain the Diagnostic evaluation of the child with the meningocele.
History taking and physical examination,
skull radiography,
genetic testing,
Computerized Axial Tomography (CAT)
Maternal Serum Alpha Phyto Protein (MSAFP)
screening,
prenatal ultrasound,
Amniocentesis,
Alpha Phytoprotein (AFP) Assessment,
imaging studies,
ultrasound,
MR. i.,
city scan,
Laboratory testing,
radio graph,
myelogram,
spinal tomogram,
Neurological assessment,
Explain the management of the child with the meningocele.
Surgical repair of the meningocele condition after birth can prevent the child from infection and maintain neurological function.
Prone position should be provided to the child who has Mangosheel condition due to which the back pressure can be prevented and it can be prevented from rupturing.
Protect the protruding sac-like structure with sterile dressing.
Prone proper position should be provided to the child due to which the pressure in the lower back area can be prevented.
If the child has a condition of hydrocephalus, divert the flow of cerebrospinal fluid by providing a proper ventricular catheter.
If the child has any orthopedic complication, treat it properly surgically and provide physical therapy.
If the child has bowel and bladder dysfunction, treat it properly.
Provide proper physical therapy to the child like exercises, stretches and great training.
If the child has any other complication then treat it immediately.
To provide complete education to the child and his family members about the child’s condition, its causes, symptoms and signs, and its treatment.
To provide proper psychological support and counseling to the child and his family members.
To properly maintain the nutritional status of the child.
Providing properly assistive devices like orthosis, braces, to the child.
To provide proper work and comfortable environment to the child.
Explain the nursing management of the child with the meningocele.
A child with meningocele needs to provide holistic nursing management.
To properly assess the child.
Proper assessment of physical, psychological, developmental and psychosocial needs of the child.
To properly assess the child’s vital signs.
Assessing the neurological status of the child.
Child’s Bowel and Bladder Function,
Properly assess skin integrity and musculoskeletal health.
Continuously monitoring the child’s nutritional status, hydration status, no growth.
If the condition of meningocele is surgically repaired, maintain aseptic technique and provide proper dressing in the wound area to prevent infection of the child.
To maintain the nutritional status of the child.
To provide properly assistive devices to the child to improve his mobility.
To provide complete education to the child’s family members and parents about the condition of meningocele, its causes, symptoms and signs, and its treatment.
Providing proper emotional support and counseling to parents.
To have proper therapeutic communication with the child’s parents.
Advising parents to follow up regularly.
- Explain/Define meningomyelocele
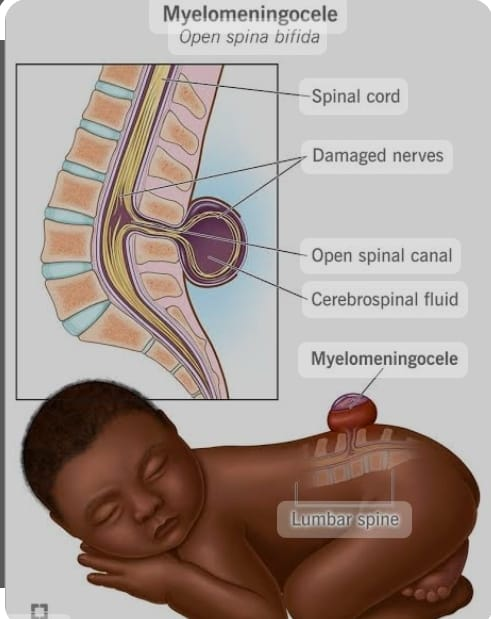
Meningomyelocyle is the most severe form of spina bifida, where the spinal cord, meninges and nerves protrude (protrusion) through a gap or opening in the spinal column, the lower back area covered by a thin layer of skin, a sac or cyst. Makes. Neurological deficits are often seen in meningomyelocyles and function is also impaired. A child with meningomylosil has paralysis, muscle weakness, sensory loss,
Bowel and bladder dysfunction and other complications such as hydrocephalus (fluid accumulation in the brain), Chiari, and malformations occur.
Explain the Etiology/cause of the meningomyelocele
The exact cause of meningomylosing is unknown.
Due to genetic factors,
Due to environmental factors,
Due to intake of folic acid (vitamin B9) in inadequate amount by the mother during the first trimester.
Due to maternal disease conditions like diabetes, obesity,
Due to mother’s exposure to teratogenic substances (smoking, alcohol, tobacco, drugs) during pregnancy,
Due to advanced maternal age,
Due to hyperthermia condition in mother during pregnancy.
Due to the mother taking certain types of anticonvulsant medication during pregnancy.
Explain the clinical manifestation/ sign and symptoms of the child with the meningomyelocele.
Meningomyelocyle is the most severe form of spina bifida and involves protrusion of the spinal cord, its protective layer (meninges), and the spinal cord into the lower back region.
A sac or cyst that contains an exposed spinal cord is usually covered by a thin layer of skin and is prone to rupture or infection. Neurological symptoms are seen and include paralysis, muscle weakness, sensory loss, and bowel and bladder dysfunction.
Other symptoms in meningomyelocyles may include hydrocephalus (accumulation of fluid in the brain), Chiari malformations, orthopedic deformities (eg, scoliosis), and skin breakdown or pressure ulcers.
Orthopedic abnormalities such as club foot, hip displacement, impaired bowel and bladder function such as urinary incontinence, urinary tract infection, poor renal function,
Pressure sores and skin irritation,
Abnormal eye movement,
paralysis,
scoliosis,
back pain,
Partial and complete loss of sensation,
Weakness in the body,
A sac-like structure is found in the lower back region i.e. mainly in the sacral region.
Hey look,
Difficulty in swallowing leads to conditioning of choking,
Hosannas of Voice,
Breathing difficulty while sleeping,
Impaired intelligence level,
Impaired cognitive level.
Explain the Diagnostic evaluation of the child with the meningomyelocele
History taking and physical examination,
Radiography of skull, hip and chest,
genetic testing,
Urine and CSF culture,
Computerized Axial Tomography (CAT)
Maternal Serum Alpha Phyto Protein (MSAFP)
screening,
prenatal ultrasound,
Amniocentesis,
Alpha Phytoprotein (AFP) Assessment,
imaging studies,
ultrasound,
MR. i.,
city scan,
Laboratory testing,
radio graph,
myelogram,
spinal tomogram,
Neurological assessment,
Explain the management of the child with the meningomyelocele.
Surgical repair of the meningomyelocyle condition after birth can prevent the child from infection and maintain neurological function.
Prone position should be provided to the child who has the condition of mangomyelosyl, due to which the pressure in the back can be prevented and it can be prevented from rupturing.
Protect the protruding sac-like structure with sterile dressing.
Prone proper position should be provided to the child due to which the pressure in the lower back area can be prevented.
If the child has a condition of hydrocephalus, divert the flow of cerebrospinal fluid by providing a proper ventricular catheter.
If the child has any orthopedic complication, treat it properly surgically and provide physical therapy.
If the child has bowel and bladder dysfunction, treat it properly.
Provide proper physical therapy to the child like exercises, stretches and great training.
If the child has any other complication then treat it immediately.
To provide complete education to the child and his family members about the child’s condition, its causes, symptoms and signs, and its treatment.
To provide proper psychological support and counseling to the child and his family members.
To properly maintain the nutritional status of the child.
Providing properly assistive devices like orthosis, braces, to the child.
To provide proper work and comfortable environment to the child.
Explain the nursing management of the child with the meningomyelocele
A child with meningomyelocyle needs to be provided with holistic nursing management.
To properly assess the child.
Proper assessment of physical, psychological, developmental and psychosocial needs of the child.
To properly assess the child’s vital signs.
Assessing the neurological status of the child.
Child’s Bowel and Bladder Function,
Properly assess skin integrity and musculoskeletal health.
Continuously monitoring the child’s nutritional status, hydration status, no growth.
To prevent infection and injury to the child after bathing the child with meningomylosil.
After the birth of the child, providing the child with a left room and an incubator immediately.
If the condition of meningomyelocele has been surgically repaired, maintain aseptic technique and provide a properly sterile antibiotic dressing in the wound area to prevent infection of the child.
Continuous observation of the child.
To maintain the nutritional status of the child.
To provide properly assistive devices to the child to improve his mobility.
To provide complete education to the child’s family members and parents about the condition of meningomyelocele, its causes, symptoms and signs, and its treatment.
Providing proper emotional support and counseling to parents.
To have proper therapeutic communication with the child’s parents.
Advising parents to follow up regularly.