ENGLISH PEDIATRIC UNIT 4 PART 3
BEHAVIOURAL AND COMMON DISORDERS
Tic disorder in children is a neurological disorder characterized by sudden, repetitive, rapid, nonrhythmic muscle movements. Motor movement (motor tics) or vocalization (vocal tics).

Tics are involuntary disorders and occur in many parts of the body like face, head, limbs, shoulders, neck, trunk, hands etc. A tic disorder usually starts in childhood.
Explain the types of the tics in child.
There are total four types of tic disorder.
1) Motor tics,
2) vocal tics,
3) Transient tic disorder,
4) Tourette syndrome
1) Motor tics,
Movements of organs and other parts of the body are known as motor tics, such as eye blinking, head jerking etc.
2) vocal tics,
Involuntary repetitive vocalizations, such as grunting, sniffing or clearing throat, are called vocal tics.

3) Transient tic disorder
These motor or vocal tics are present and last for less than a year. Transient tic disorders are common in children and often resolve on their own without the need for treatment.
4) Giles della Tourette syndrome Tourette syndrome
It is a complex neurological disorder with multiple tics i.e. both motor and vocal involvement.
Explain the Etiology/cause of the tics disorder in child
The exact cause of tic disorder is unknown.
Due to genetic factors,
Due to neurobiological factors,
Due to neurotransmitter irregularity,
Due to environmental factors,
Due to stress and anxiety and depression in the child,
Due to immune system dysfunction,
Due to psychological factors,
Due to inflammation in the central nervous system,
Due to physiological abnormalities,
Due to head injury,
Due to stroke,
Due to infection,
Due to some kind of injury.
Explain the Clinical manifestation/ sign and symptoms of the child with the Tics Disorder
1) Motor tics
Sudden, brief, repetitive muscle movements,
Movement of muscles of different parts of the body,
Repeated eye blinking,
Repeated facial twitching,
head jerking,
Seeing shoulder movement,
Jerking and twitching movements in arms and legs.
- Vocal tics
Vocal tics are sudden, involuntary sounds or utterances made by the child.
These sounds can range from simple voices to more complex sounds or words and may involve:
throat clearing,
making a grunting sound,
sneezing,
cuffing, whistling,
Shouting, etc
Other symptoms:
Irritability,
Difficulty in attention,
Having a learning disability,
Sudden lapses, involuntary movements of body and mind,
being hyperreactive,
Stress, anxiety to the child.
Impairment in the academic performance of the child.
Child’s daily routine activity is impaired.
Explain the Diagnostic evaluation of the child with the Tics Disorder
History taking and physical examination,
Taking history about frequency and duration of tics,
laboratory test,
blood test,
Psychological, assessment,
x ray,
CT scan,
like this. RI,
Electro Encephalogram,
Blood test
Explain the medical management of the child with the Tics Disorder.
Providing the child with antipsychotic drugs This meditation modulates dopamine receptors.
Ex:=
Haloperidol Pimozide Risperidone
Aripiprazole
Fluphenazine.
Providing alpha to adrenergic agonist medication to the child. This medication helps reduce tick symptoms.
Ex:=
Clonidine,
Guanfasine.
Providing botulinum toxin injection to the child
This medication helps reduce the symptoms of a tic disorder.
Providing Proper Behavioral Therapy to the Child.
Providing Proper Cognitive Behavioral Therapy to the Child.
To provide complete education to the child and his family members about the causes, symptoms and signs, and treatment of tick diseases.
Providing proper psychological support to the child.
Advising the family members of the child to take regular, proper care of the child.
Proper monitoring of how much the child’s treatment is effective and whether it has any kind of side-effect or not.
Providing Habit Reversal Training (HRT) to the child.
Provide exposure and response prevention (ERP) therapy to the child.
Explain the Nursing management of the child with the Tics Disorder
Proper assessment of frequency, duration of child’s symptoms.
Properly assess whether there is any impairment in the child’s daily routine activities, well being due to the symptoms of tics.
To provide complete education to the child and his family members about the causes, symptoms and signs, and treatment of tick diseases.
Provide emotional support and reinforcement to the child and his family members.
To provide a properly safe and supportive environment to the child.
Providing proper behavioral therapy to the child.
Providing properly prescribed medication to the child. And continuously monitoring whether there is any kind of side effect, effectiveness of drugs or not.
Advising the family members of the child to take care of the child continuously.
Continuously monitoring the extent to which the child’s treatment is effective.
Advising the child to do daily routine activities properly, regularly and in small amounts.
Advise the child to exercise regularly in small amounts.
Advising the child to take adequate nutritious food and adequate sleep.
To provide proper counseling to the child and his parents.
Advise the child and his family members to follow up regularly.
- Explain/Define the pica in child.

Pica is an eating disorder primarily derived from the Latin word magpie.
“Magpie” means feeding on substances other than food (non-edible objects) such as dust, clay, sand, paint chips, plaster from walls, cloth, snow, etc.
Pica is the most common eating disorder in children.
Children in this condition consume a non-nutritive non-eating substance such as,
Dust, mud, sand, paint chips, plaster from the wall, chalk, hair, peppersoap, ice, plastic, thread, metal objects, etc. These non-eatable things are said to be normal till the child is two years old but after two years they convert into an abnormal habit.

Explain the Etiology/cause the child with the pica
Due to nutritional deficiency (zinc, iron, calcium),
Due to psychosocial causes,
Due to socio economic factors,
Child abuse and neglect,
Due to developmental disorders,
Due to psychological factors viz
Due to anxiety, stress, emotional distress,
Due to environmental factors,
Due to the traceful home environment,
Due to biochemical disorder,
Due to mental retardation,
Due to poor supervision,
Due to worms infestation with malnutrition,
Due to vitamin and mineral deficiency,
Due to parental neglect,
Due to poor attention provided by the caregiver,
Due to inadequate love and affection.
Explain / Define clinical manifestation / Sign and symptoms of the child with the pica.
Injecting non-edible substances,
Conceiving non-nutritive and non-food substances,
Cravings for eating non-edible substances,
Behavioral symptoms observed in the child,
Gastrointestinal symptoms such as,
nozia,
vomiting,
Abdominal pain and discomfort,
Constipation or diarrhea,
Perforation and obstruction in the gastrointestinal tract,
Finding dental problems like,
tooth erosion,
Tooth caries (KVT),
Tooth damage,
Irritation and inflammation in the gums,
Finding nutritional deficiency in the child (iron, zinc, and other essential nutrients),
Seeing psychological problems like stress, anxiety, emotional trauma, etc.
Child becomes anemic,
Deficiency of minerals and vitamins will be found in the child.
Explain the Diagnostic evaluation of the child with the pica
History taking and physical examination,
Behavioral and Developmental Assessment,
Nutritional Status Assessment,
blood test,
Psychological
assessment,
Environmental Condition Assessment,
Imaging studies.
Explain the management of the child with the pica
Identifying environmental hazards and eliminating them.
Keep non-edible items away from children.
To provide proper work and comfortable environment to the child.
Assess the nutritional status of the child especially iron, zinc and other essential nutrients.
Advising parents to provide properly nutritious food to children.
Providing proper behavioral therapy to the child.
Carrying out proper environmental modification.
Providing proper psychological support and counseling to the child.
Provide proper medication to the child if he has any psychiatric symptoms.
To provide complete information to the child and his parents about the causes of the disease, its symptoms and signs and its treatment.
If the child has any worm infestation then provide proper treatment.
If the child is deficient in vitamins and minerals, then proper supplements should be provided.
Giving advice for proper supervision of children by parents.
To provide proper work and comfortable environment to the child.
- Explain the Bite and Sting in child

“Bite” and “sting” generally refer to injuries caused by the teeth or mouth parts of an animal or insect.
A bite is a piercing or cutting of the skin, usually by an animal such as a dog, cat, snake, or human.

On the other hand, a sting is usually an insect that injects a poisonous (venom) or other irritant (irritant) substance into the skin, such as bees (honey bees), wasps (wasps) or scorpions (scorpions). Caused by an insect. Bite and sting are both types of poisoning that are most commonly seen in infants and children.

Both bites and stings can cause more serious problems, such as pain, swelling, redness, and, in some cases, a severe allergic reaction or infection. Proper wound care and, in some cases, medical treatment depending on the severity of the injury. Attention may be required.
Explain the Etiology/cause of the animals bite and insect sting to children
The etiology or causes of animal bites and insect bites in children may vary from situation to situation, but some common facts include:
- Provocation:
Children may provoke animals by inadvertently approaching them, startling them or misbehaving with them. Animals may bite in self-defense if provoked. - Territorial Behavior:
Some animals, such as dogs, may bite to protect their territory or source, especially if they believe a child is entering their space. - Fear or Anxiety:
Children’s unpredictable movements or loud voices can arouse fear or anxiety in animals, causing them to react defensively by biting. 4.Lake of Supervision:
Lack of proper supervision between children and animals increases the risk of bites, as children may not recognize warning signs from animals or understand how to react safely. - Due to Misunderstanding of Animal Behavior:
Children may not fully understand animals’ behavioral signs of stress, discomfort or aggression, causing them to unwittingly provoke animals. - Unfamiliar Environment:
Encounters with unfamiliar animals, such as stray dogs or wildlife, can result in bites if children approach them without caution or awareness of any dangerous conditions. In the case of insect stings, common causes include: - Defensive Behavior:
Insects like bees, wasps and ants perceive sudden movement as a threat and may sting in their own defense if they feel fear. - Due to nest protection:
Children may inadvertently disturb insect nests during outdoor play. Some insects sting to protect their nests or hives from potentially dangerous conditions. - Attracted by food or scent:
Some insects are attracted to food, sweet drinks, or scents, making an unexpected encounter more likely to sting. - Due to outdoor activities:
Children engaged in outdoor activities like picnics, gardening can be bitten by insects. Explain the Clinical manifestation/ sign and symptoms of the child with the animal bite and insect sting
Bite and stinging pain on the side,
to be uncomfortable,
Swelling,
redness,
itching,
irritation,
bleeding,
Bruising on bitten side,
Localized reactions like hives, redness, swelling etc.
A system reaction such as breathing difficulties may occur.
Dizziness, nausea and vomiting,
and having an anaphylactic reaction,
Increased risk of infection,
Allergic reactions like itching, swelling, redness, difficulty in breathing, rapid heartbeat, dizziness, etc.
Explain the Diagnostic evaluation of the child with the Animals bite and insect sting
History tacking and physical examination,
To properly assess the child’s signs and symptoms,
Assessing whether the child has an allergic reaction or not,
Performing laboratory assessment,
Complete blood count test,
imaging studies,
x ray,
Assess the child for any systemic reactions.
Explain the medical management of the child with the animals bite and insect sting.
To properly assess the child’s sign and its simtones.
Take proper care of the child’s wound, including cleaning the wound immediately with soap and water.
Any debris and foreign material in the wound should be removed immediately.
If there is bleeding from the wound area, apply proper cloth and provide pressure.
If the child is in pain, provide analgesic medication.
Ex:=
Acetaminophen,
Ibuprofen etc.
Antibiotic medicine should be provided if the child has any bacterial infection condition.
If the child has not received a tetanus injection in the last five years, provide a tetanus booster dose.
Provide epinephrine medication if child has any allergic reaction.
Advising the child and his parents to follow up regularly.
Explain the Nursing management of the child with the Animals bite and insect sting.
To provide properly comprehensive care to the child.
Properly assess the child’s condition and also properly assess his wound.
Properly assess the child for any sign of infection, allergic reaction and any systemic reaction.
Take proper care of the child’s wound, including cleaning the wound immediately with soap and water.
Any debris and foreign material in the wound should be removed immediately.
Application of antiseptic solution and antibiotic ointment in the wound
If there is bleeding from the wound area, apply proper cloth and provide pressure.
If the child is in pain, provide analgesic medication.
Antibiotic medicine should be provided if the child has any bacterial infection condition.
Monitoring the child properly and closely.
To provide proper emotional support to the child and his family members.
Giving advice to the child’s parents to take proper care of the child and prevent the child from going near any animal and insect.
Providing information to the child’s parents about the child’s condition, its signs and symptoms and its treatment.
Giving advice to the parents of the child to continuously and properly monitor the child.
Advising the parents to follow up the child regularly.
To provide proper psychological support to the child and his family members.
- Explain/ Define Dog bites in children (
Dog bite injuries mainly occur in children under 18 years of age due to dog bites. These dog bite injuries can range from minor punctures, wounds and scratches to more severe injuries, tissue damage and, in rare cases, even death.
Dog bites in children are usually caused by a variety of conditions, including provocation, aggressive behavior by the dog, self-protective behavior by the dog, or predatory behavior.
Dog bites can have lasting physical, psychological and emotional effects on a child.
If the dog that has bitten the child is a rabid dog, it can cause a viral disease called rabies (hydrophobia) in the child. However, rabies can also be caused by other animals such as cats, monkeys, horses, sheep, goats, etc.
The incubation period of rabies in humans is long, causing hydrophobia and rabies can be a fatal condition.

Rabies in dogs takes two forms.
1) furious
2) dumb.
The incubation period for rabies in children can vary, but is usually one to three months (20 to 90 days), although it can be shorter or longer.
Explain the Etiology/cause of the child with the dog bite.
Due to the dog being provoked by the child,
A dog may bite to protect itself,
Due to fear and anxiety in dogs,
Due to children not provoking the dog,
Due to lack of proper supervision of children by parents,
Since children are not properly aware of dog behavior,
By removing the dog,
Explain the clinical manifestation/ sign and symptoms of the child with the dog bite.
During the first one to four days,
fever,
Myalgia (muscle pain),
headache,
sore throat,
Symptoms like changes in mood etc.
A wound is visible,
Pain and tenderness,
Swelling around the wound,
Bleeding from a wound,
Signs of infection include redness, pain, vomiting, swallowing, drainage of pus from the wound, etc.
getting tetanus,
A child is emotionally distressed so that symptoms like anxiety, fear, stress, aggressive behavior can be seen in the child.
If the dog has a very deep bite, skin, tissues, nerves, muscles and tendons are also involved. Due to this, numbness, weakness,
And the function of the affected area is also lost.
A scar is visible,
If bitten by a rabid dog, symptoms of rabies may be seen such as
Hydrophobia (fear of water),
Aerophobia (fear of air),
Part of the nervous system is stimulated,
Excessive noise should not be tolerated,
Not tolerating bright light,
Muscle spasms and reflexes increase,
dilatation of the pupil,
Excessive perspiration,
Excessive salivation,
Mental changes can be seen like,
no fear of death,
anger,
irritability,
Depression etc.
If the fetal condition of rabies occurs, paralysis, coma, and even death can occur.
Explain the Diagnostic evaluation of the child with the Dog bite
History taking and physical examination,
Conducting a wound assessment,
Assessing the severity of the wound,
Assess for signs and symptoms of infection,
Assessing whether tetanus vaccine has been received or not.
imaging studies,
x ray,
To assess whether a dog bite is caused by a rabid dog and to assess the chances of rabies,
Assess for bite side paresthesias (tingling and numbness) or not. To assess whether hydrophobia is present or not.
Assessing the child’s psychological status,
Assessment of Negri bodies.
Explain the medical management of the child with the dog bite
Medical management of a child with a dog bite is to prevent infection, improve wound healing, and address any complications that may arise.
1 To properly assess the child.
An assessment of the child is performed to assess the severity of the dog bite and identify any associated injuries. Assess if the child has severe bleeding, breathing difficulties, or any other symptoms.
Wound Care:
Clean the wound thoroughly with soap and water to remove debris, microorganisms and bacteria from the dog bite wound. Remove any foreign bodies or dead skin, and assess for signs and symptoms of infection.
Close the wound properly
If the wound is large, closing the wound using sutures, staples, tissue adhesives, etc. will help the wound heal, reduce infection, and minimize scarring.
Tetanus Prophylaxis:
If the child’s tetanus vaccination is not proper and if the wound is contaminated or deep, a tetanus booster shot is given to prevent tetanus infection.
Antibiotic Therapy:
To prevent the child from bacterial infection, antibiotics are administered for treatment if there is a deep wound, a contaminated wound or signs of infection, especially the choice of antibiotics for the child.
Depending on age, allergy and identified pathogenic organisms.
Pain Management:
If the child is in pain, provide proper analgesic medicine.
Ex:= Acetaminophen,
Ibuprofen etc.
Rabies Prophylaxis:
If transmission of rabies due to dog bite is likely, rabies post-exposure prophylaxis (PEP) should be provided as per established guidelines. It mainly involves rabies vaccination and rabies immunoglobulin.
Regular monitoring:
Monitoring the child properly closely to assess for any signs of infection, signs of allergic reactions, and any other complications of dog bites. And giving advice to the child’s parents to follow up regularly.
Psychological Support:
A dog bite is a traumatic experience for a child due to which children experience symptoms like fear, anxiety, emotional distress, etc.
Provide proper psychological support and counseling to the child to relieve these symptoms. Thus, medical management of dog bites is provided to reduce complications, improve wound healing, and prevent other complications.
Explain the nursing management of the child with the dog bite.
Proper assessment of the child’s condition.
Wounds caused by dog bites and any type of infection in the child,
Allergic reaction and any other complications should be properly assessed.
Properly assessing the child’s overall health status.
Properly assess the child’s wound including washing the wound properly with soap and water.
After properly washing the wood, properly remove the debris and dead tissues in it.
After removing these dead tissues and debris, apply a proper antiseptic solution and topical antibiotic.
If the child is in pain, give analgesic medication.
If there is swelling, provide cold application to reduce it.
Properly monitor the child’s wound condition to assess for any swelling, redness, vomiting, and drainage from the wound.
To properly assess the child’s vital signs.
The schedule of tetanus is to properly assess the child and provide the child with a tetanus booster dose.
A dog bite is a traumatic experience for a child due to which children experience symptoms like fear, anxiety, emotional distress, etc.
Provide proper psychological support and counseling to the child to relieve these symptoms.
Complete education of the child and his family members about the child’s condition, the condition of the wound, its signs and symptoms and its treatment.
To provide education to the child and his parents for proper follow up.
Treat the child’s condition properly by providing proper comprehensive nursing care to the child.
To give proper work and comfortable environment to the child.
- Explain/Define Snake bite in children

Snake bite in children is an injury caused by the venomous bite of a snake. The snake injects venom into its prey through its specialized fangs, which usually results in symptoms and signs in the child, as well as complications, depending on the type of snake and the amount of venom injected.
Snake bite is one of the most common emergency conditions seen in children who live in slums and villages.
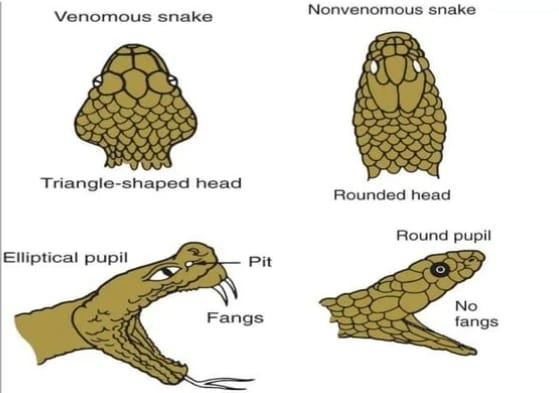
As many as 216 species of snakes are found in India. Out of which 52 species are poisonous which are members of 3 families viz.
1) Neurotoxic Elapidae (Cobra),
2) hemorrhagic hemotoxic Viperidae (vipers),
3) Neuro – hemotoxi crit
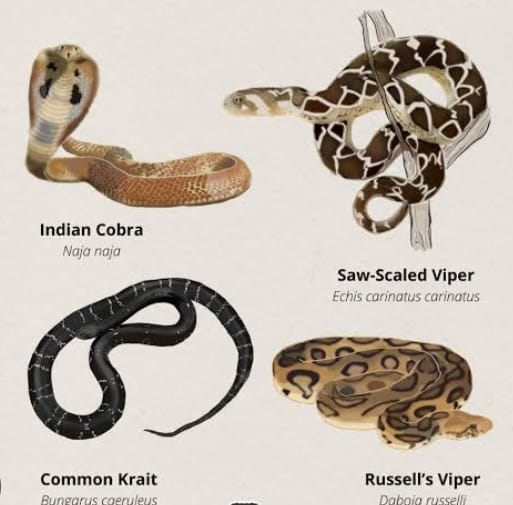
1) Neurotoxic Elapidae (Cobra),
Elapidae (Cobra) is neurotoxic. This snake venom normally blocks neuronal transmission at the neuromuscular junction, causing respiratory depression and death.
2) hemorrhagic hemotoxic Viperidae (vipers),
The venom produced by the viper is usually cytotoxic, causing cellular necrosis, tissue destruction, hemolysis, and coagulopathy, leading to hemorrhage, shock, and renal failure, and may lead to death.
3) Neuro – hemotoxi crit
Cret is both neuro and hemotoxic. This is one of the most common and dangerous snakes found in India.
Explain the Etiology/cause of the child with the Snake bite.
The etiology of a child bitten by a snake depends on factors such as geographic location, environmental factors, and human behavior.
Due to encounters in natural habitat
Children can be bitten by snakes while playing or exploring in natural habitats such as forests, fields, deserts or rural areas. 2) Unintentional provocation (provocation):
Snake bites can occur when children accidentally startle or startle a snake while exploring their surroundings. like,
stepping on or near a snake,
Reaching the hidden place where the snake is resting. And teasing the snake etc.
By disturbing and handling snakes
Curiosity and lack of awareness about the dangers of snakes lead children to handle and distaste snakes. Children trying to hold, pick up or play with a snake can cause the snake to bite, as the snake perceives the child as a threat and may bite in self-defense.
Occupational and recreational activities
Children who engage in outdoor activities such as camping, fishing, or farming are at increased risk of snakebite due to residential contact with snakes. Additionally, children living in rural or agricultural areas may be bitten by snakes while working or playing outside. can
Due to low level of awareness and education
Children who are not educated about snake safety and prevention strategies and who unknowingly provoke or approach snakes are at increased risk of being bitten. Lack of awareness about the presence of snakes in the particular environment and how to avoid them also increases the risk of snake bites. Biting incidents may occur.
Due to inappropriate clothing and footwear
Wearing open-toed slippers, sandals, or loose-fitting clothing while working in an outdoor environment can increase the risk of snakebite, as snakes are able to bite exposed skin more easily. Encouraging children to wear sturdy, closed shoes and long pants can reduce the risk of snake bites.
Environmental Factors
Environmental factors like seasonal changes,
Weather patterns can also increase the incidence of snake bites.
Thus, snakebites in children often result from accidental encounters or unexpected encounters with snakes in natural or outdoor environments.
Explain the clinical manifestation/ sign and symptoms of the child with the snake bite.
Symptoms and signs depend on the type of snake and local and systemic effects. 1) Neurotoxic Elapidae (Cobra):
In neurotoxic Elapidae (Cobra), local effects start within two to three days of the bite. like
to be in pain,
Swelling,
headache,
dizziness,
Systemic effects occur 10 minutes to 10 hours after a bite such as neurotoxic and cardiotoxic effects.
Tosis (upper eyelid
Eye drops), ophthalmoplegia (paralysis of eye muscles) with paralysis involving palate, jaw, tongue, larynx neck and respiratory muscles.
Cardiotoxicity also includes hypotension, tachycardia, ECG alterations, and hemolysis.
2) hemorrhagic hemotoxic Viperidae (vipers),
severe burning,
to be in pain,
Swelling,
cellulitis,
Bullae and ecchymosis on the bite side, redness,
Continuous oozing and bleeding,
necrosis,
Systemic signs and symptoms include bleeding on the puncture side, headache, dizziness, vomiting,
Respiratory difficulty, hemorrhage from different side,
purpura,
haematemesis,
get dirty,
having epistaxis,
Hemenorrhea,
bleeding gums,
Subconjunctival and intracranial building up,
intracranial hemorrhage,
circulatory collapse,
Renal failure, death occurs within 24 to 48 hours if intracranial bleeding occurs.
3) Neuro – hemotoxi crit
Neurological symptoms such as
muscle weakness,
Respiratory muscle weakness,
Paralysis involving facial muscles first, extremities, followed by respiratory muscles.
Respiratory distress,
Difficulty breathing,
Shortness of breath,
Respiratory failure,
Hypoxia and cyanosis,
Tossing due to muscle paralysis of the eyelids,
Difficulty in swallowing (dysphagia).
Hemotoxic effect
From the bite side,
from the nose,
Bleeding from the gums,
internal bleeding,
Petechiae (small red and purple sports) on the skin,
ecchymosis (larger bruises like petechiae) on the skin,
Cardio vascular symptoms
Hypotension,
Cardiac output decreases,
condition of mourning,
Bradycardia (slow heart rate),
Autonomic dysfunction
Excessive salivation,
Excessive sweating
(diaphoresis),
Altered mental status,
confusion,
loss of consciousness,
hypoxia,
Neurotoxicity.
Other General Symptoms
nozia,
vomiting,
palness,
cold extremities,
Burning on bite side,
On the Bite side, Macus can be seen.
Explain the Diagnostic evaluation of the child with the Snake bite
History taking and physical examination,
Snake Identification,
Laboratory Investigation,
Hemoglobin level assessment,
Complete blood count test,
platelet count,
Building Time, Clotting Time,
Blood urea nitrogen level,
Creatinine level,
electrocardiogram,
Imaging studies
Explain the medical management of the child with the snake bite
The aim of medical management of a child with snakebite is to provide timely and appropriate treatment, minimize side effects, prevent complications and promote recovery.
Immediate first aid
The first step in managing a snakebite is to ensure the safety of the child and those around him. Move the child away from the snake to prevent further snake bites
Keep the child moving and still to slow the venom from spreading into the blood stream. If possible, to the affected body part
Immobilize.
Remove any constipating clothing or jewelry from the bite site to prevent swelling and constriction.
Do not attempt to cut, suck, or apply ice to the bite site, as these steps are ineffective and may cause further damage.
Transport to Medical Facility
Attempt to transport the child to the nearest medical facility as soon as possible for further assessment and treatment.
Assessment and stabilization
Upon arrival at the health care facility, the child is assessed by the health care provider to assess the severity of the snake bite and the amount of venom present. Vital signs, heart beat, blood pressure, respiration and oxygen saturation are then closely monitored.
Intravenous (IV) access and oxygen are provided as needed to stabilize the child’s condition.
Identification and ennomination of snakes
An assessment of the type of snake bitten is done so that further treatment can be initiated.
Assessment of symptoms at the bite site such as local effects, swelling, pain etc. Systemic effects such as nausea, vomiting, neurotoxicity etc. are then assessed.
Administration of antivenom
If envenomation is reported, antivenom is provided to neutralize its effects. Antivenom is administered intravenously and depends primarily on the type of snake bite. Multiple vials may be required depending on the severity of envenomation.
Symptomatic management
Symptomatic management is provided to relieve pain, swallowing and symptoms of snakebite. If pain occurs, provide analgesic medication.
Ex:= Acetaminophen.
If there is swelling and inflammation, provide corticosteroid medication to relieve it.
Antibiotic medication should be provided if there is any bacterial infection.
Monitoring and supervision
Closely monitor the child for how effective the treatment is and for any other signs and symptoms.
Complications include allergic reaction and adverse reaction to antivenom to assess whether or not.
And provide proper respiratory support to the child.
Continuously observe the child and assess whether there are any other signs and symptoms.
Explain the nursing management of the child with the snake bite
To provide properly comprehensive support to the child.
Proper assessment and monitoring of the child.
To monitor the child’s vital signs regularly and properly.
Properly assess the bite side of the child.
And to properly assess whether the child has any systemic symptoms or not.
Closely monitoring the vital shine of the child including heart rate, blood pressure rate, respiratory rate, and oxygen saturation properly.
If the child is in pain, provide analgesic medication to relieve it.
Ex:= Acetaminophen
Relaxation techniques in non-pharmacological therapy for the child,
And providing mind diversional therapy.
Proper care of wood from snake bite involves cleaning and dressing.
Clean the wound with saline solution and antiseptic solution to properly remove debris and other foreign material if present.
Then apply dressing to properly protect the wound and tissue healing.
Closely monitoring the child to assess for signs and symptoms of any infection and energetic reaction.
To provide proper psychological support to the child and his family members.
To provide complete education to the child’s parents about the child’s condition, its signs and symptoms, its treatment, and measures to prevent it.
Advising parents of child to take regular follow up.
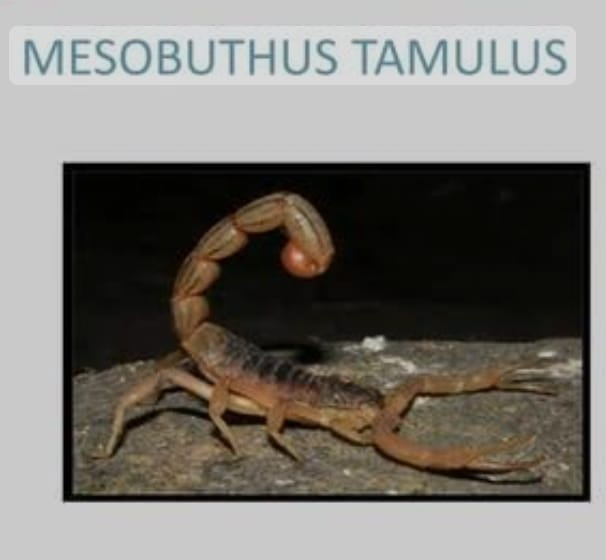
Explain/Define Scorpion sting in children.

When children are bitten by a scorpion, it is called a scorpion sting.
Children can experience symptoms ranging from mild symptoms to severe reactions due to scorpion stings.
Scorpion venom can cause pain, swelling, redness, and numbness at the site of the sting. In severe cases,
Difficulty breathing, muscle twitching, convulsions or even death may occur, especially in very young children or children with poor health status.

If children are stung by a scorpion, immediate medical treatment is required to prevent signs and symptoms and prevent other complications.
Scorpion envenomation is a major health problem all over the world but especially in developing countries and in tropical and subtropical regions.
Scorpion stings are second only to snake bites as a cause of fatal envenomation. Scorpion stings are particularly common in tropical and subtropical regions and in the summer months.

Two species of scorpions namely Mesobuthus tomulus and Palmenius swamerdani are venomous in India. Scorpion stings can often be fatal as scorpion venom is neurotoxic, cardiotoxic, hemotoxic, and myotoxic and has local and systemic signs and symptoms. Get.
Explain the etiology/cause of the child with the scorpion sting.
Due to accidental contact with scorpions,
Scorpions usually hide in certain floors or small spaces in the house and may bite a child when they come in contact with them.
When children are playing outdoor games,
slums and, due to living in tropical and subtropical areas,
Housing condition being inadequate.
Overcrowded Area Ma
Explain the clinical manifestation/sign and symptoms of the child with the scorpion sting.

Scorpion venom is neurotoxic, cardiotoxic, hematotoxic, and myotoxic. It causes local and systemic effects.
Pain at the sting site,
Redness and swelling in the area around the sting site,
Numbness and tingling sensation,
muscle spasms,
muscle twitching,
ecchymosis,
overexcitement,
tachypnea,
Nozia and
vomiting,
Increased salivation,
lacrimation,
Difficulty breathing,
Passing urine and stool frequently,
Peripheral circulatory failure,
Skin is cold and clammy,
Restlessness,
Hypotension,
tachycardia,
hepatomegaly,
Having generalized convulsions,
hemiplegia,
Confusion with neurological deficits,
Acute renal failure,
coagulopathy,
Cardiomyopathy.
Explain the Diagnostic evaluation of the child with the Scorpion sting
History tacking and physical examination,
To assess the child’s signs and symptoms,
complete blood count,
Serum electrolyte level assessment,
Coagulation studies,
Creatinine kinase level assessment,
Imaging studies to assess pulmonary edema or myocarditis
X-ray.
Explain the medical management of the child with the scorpion sting. (Give medical management of scorpion sting)
1) Immediate first aid
Take the child away from the place where the scorpion has been stung so that further stinging can be prevented.
Then apply proper tourniquet over the stung side and immobilize that part.
Wash the stung side properly with plain water.
Applying cold compresses and ice packs to reduce pain and swelling.
2) Pain management
To reduce the pain caused to the child
Provide analgesic medicine.
Ex:= Acetaminophen
Providing the child with a non-steroidal anti-inflammatory drug (NSAID).
Use local anesthetic lignocaine to relieve pain.
3) Administration of antivenom
If moderate to severe envenomation has occurred, administer antivenom to the child to neutralize the envenomation.
Antivenom is mainly provided intravenously and is provided under continuous supervision.
If the heart rate is not fast, administer adrenaline subcutaneously at 15-minute intervals and then assess whether the pulse returns or not and whether the body vomits or not.
Calcium gluconate 10% 5-10 ml intravenously with antivenom therapy should be repeated if necessary. This is mainly helpful in relieving the muscular camp.
4) Proper symptomatic management.
Provide antihistamine and corticosteroid medication to relieve allergic reactions and inflammation.
Use of muscle relaxants to reduce muscle spasms and cramps.
5) Lytic cocktail regiment
In a lytic cocktail solution,
Pethidine 100mg,
Chlorpromazine (Largactil 50 mg) and
Promethazine (Phenargan 50 mg) is prepared in 50 ml with 50e% glucose in distilled water and then 0.3 cc/kg is given intravenously every 20 minutes.
If congestive heart failure
If signs of (myocarditis) are present, provide adequate digitalis and steroid to the infant. And in case of older children, provide 100 mg every six hours.
6) Supportive care
Properly monitoring the child’s vital signs like heart rate, blood pressure, and oxygen saturation.
Provide intravenous fluids to maintain child’s hydration status and electrolyte status.
If there is breathing difficulty, provide oxygen therapy to the child properly.
Providing tetanus prophylaxis to the child.
Closely monitoring the child for any systemic signs and symptoms.
Provide proper wound care to prevent infection at the site of the child’s sting bite.
Antibiotic medicine should be provided if there is any condition of bacterial infection.
Closely monitoring the child for any other complications.
Advising parents of child to take regular follow up.
Explain the nursing management of the child with the scorpion sting
Monitoring properly in the nursing management of the child.
To prevent any further complications of the child and to enhance the recovery of the child by providing adequate treatment.
Properly and thoroughly assess the child’s symptoms.
Continuously monitoring the child’s vital signs such as heart rate, blood pressure, and oxygen saturation.
To reduce the pain caused to the child
Provide analgesic medicine.
Ex:= Acetaminophen
Non-steroidal anti-inflammatory drug (NSAID) to the child
to provide
Provide a properly cold application to the child’s wound site.
Proper care of the wound site.
Wash the wound properly with plain water and then apply a proper dressing.
Continuous monitoring of child’s condition and signs and symptoms.
Assess the child for any allergic reactions and systemic signs and symptoms.
Provide adequate intravenous fluids to maintain the child’s hydration status and electrolyte levels.
Closely monitor the child’s respiratory status and oxygen saturation.
Provide oxygen to the child properly.
To provide proper reassurance and psychological support to the child and his family members.
To provide complete education to the child and his family members about the child’s condition, its symptoms and signs, and its treatment.
To properly collaborate with other health care personnel for proper care of the child.
Complete documentation of child’s condition and medication.
Advising parents of child to take regular follow up.
Giving advice to the parents to provide a safe, working and comfortable environment to the child.
- Explain/Define Communicable disease
Communicable diseases are diseases that are transmitted by any infectious agent such as viruses, bacteria, parasites and fungi from one person to another through various routes such as direct contact, airborne droplets, and contaminated food and water. These diseases are mainly seen in school-going children, poor environmental sanitation wadi communities and children with weak immune systems.

Common examples are Haemophilus influenzae, chickenpox, measles, German measles, mumps, poliomyelitis, dengue fever, rabies, malaria, diphtheria, pertussis (whooping cough), epidemic typhus, typhoid fever (enteric fever), brucellosis, tetanus, leprosy, tuberculosis. , involvement of meningococcal infection etc.
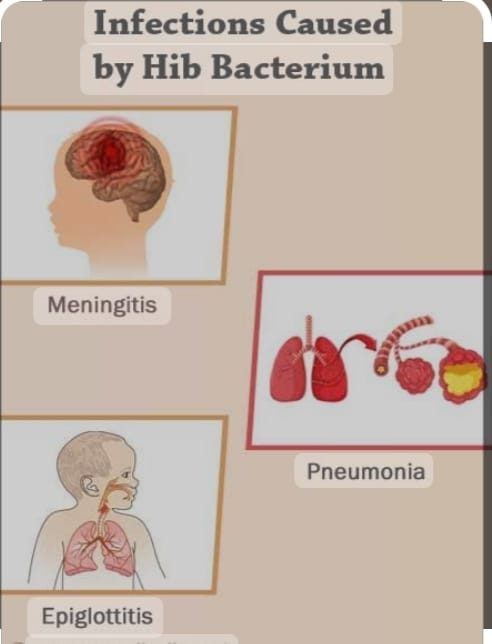
- Explain/Define Haemophilus influenzae- B (HIb)Disease

Haemophilus influenzae-B is a bacterial infection caused by Haemophilus influenzae type-B bacteria.
These diseases usually affect young children, especially children under five years of age. And serious complications can occur if left untreated.
It is a gram-negative pleomorphic coccobacillus that is commonly present in the nasopharynx and in unimmunized children.
There are 6 different serotypes of Haemophilus influenzae namely Haemophilus influenzae A,B,C,D,E,F.
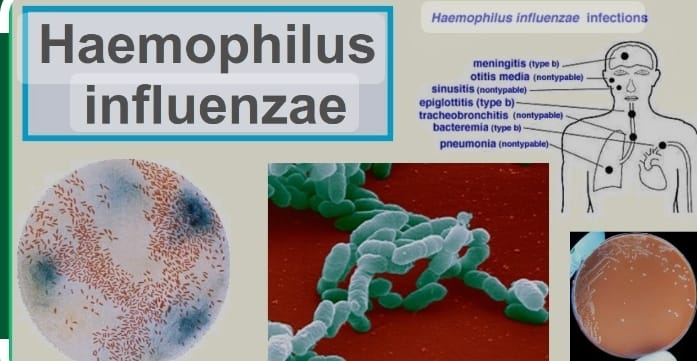
Explain the mode of transmission of the child with the Haemophilus influenzae
by Haemophilus influenzae bacteria,
Through direct contact,
by droplet infection
through respiratory droplets,
Due to direct contact of any contaminated surface and object,
Explain the Etiology/cause of child with the Haemophilus influenzae
by Haemophilus influenzae bacteria,
To unimmunized children,
Immuno Deficiency Wada Children,
Due to poor sanitation,
- Explain the clinical manifestation/ sign and symptoms of the child with the Haemophilus influenzae
Upper respiratory tract infection,
Otitis media
Earache, fever,
Irritability, sleeping difficulty, discharge from ear.
Sinusitis
Nasal congestion,
Facial pain and pressure,
Headache, cough and fever.
Pharyngitis
sore throat,
Difficulty in swallowing,
fever,
Swollen neck lymph nodes,
Lower respiratory tract infection
Pneumonia
Fever, Cough, Breathing Difficulty, Chest Pain Fatigue,
Bronchitis
persistent cough,
Chest discomfort, mild fever and fatigue.
Invasive type signs and symptoms
meningitis,
pericarditis,
epiglottis,
cellulitis,
Suppurative arthritis,
septicemia,
Other signs and symptoms
conjunctivitis,
glottis,
osteomyelitis,
peritonitis,
endocarditis,
Explain the Diagnostic evaluation of the child with the Haemophilus influenzae
History taking and physical examination,
clinical examination,
laboratory test,
blood culture,
Cerebrospinal fluid analysis,
nasopharyngeal swab or throat culture,
imaging studies,
chest x-ray,
Polymerase chain reaction test.
Explain the management of the child with the Haemophilus influenzae
Provide proper antibiotic medicine to the child.
Ex:=
Cefotexime,
Ceftriaxone,
Cifixine,
Amoxicillin,
Ampicillin,
Chloramphenicol.
To provide properly supportive care to the child.
Supportive care is usually provided to relieve symptoms and signs of the disease, prevent complications, and promote recovery.
If the child has a febrile condition, provide antipyretic medicine.
Administer analgesic medication if the child has penile contusion.
Ex:= Acetaminophen,
Ibuprofen.
Encouraging adequate fluid intake to maintain the child’s hydration status.
To properly assess the child’s vital signs like pulse, blood pressure, temperature.
Properly assess the neurological status of the child.
If the child has an invasive disease like meningitis, epiglottis then provide proper care to the child like provide respiratory support and provide intravenous fluid.
Prevention

Providing Haemophilus influenza vaccine to the child to prevent Haemophilus influenzae.
Monitoring the child properly and closely.
Giving advice to the parents of the child to take proper care of the child.
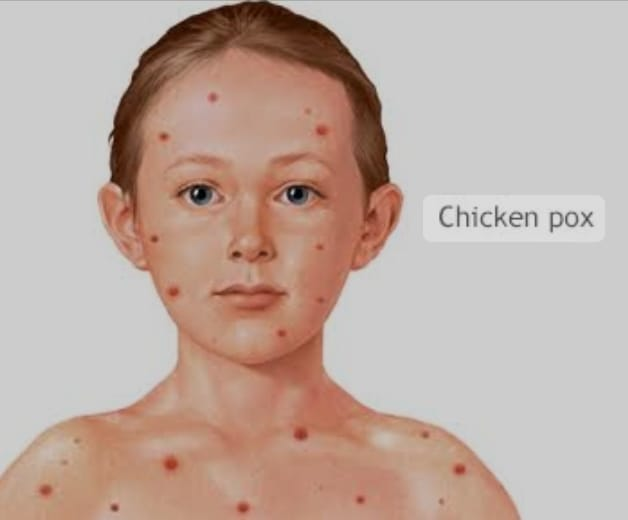
- Explain/Define Chickenpox Diseases in children

Chickenpox is a highly communicable disease. Chickenpox is also known as varicella.
Chickenpox is a viral, acute and highly infectious disease usually caused by the varicella zoster virus (VZV). A child who gets chickenpox has a low grade fever, ‘pleomorphisms’ over the child’s body and looks like blisters. This is usually more common in children under 12 years of age (5-10 years).
Explain the Etiology/cause of the child with the Chickenpox
Due to varicella zoster virus (VZV),
Due to respiratory droplets,
Due to direct contact of infection,
Due to DNA virus,
herpes zoster,
Due to a weakened immune system.
Explain the mode of the transmission of the Chickenpox
Coughing, sneezing by an infected individual due to contact with its fomites.
Due to coming in direct contact with an infected person.
Due to direct and indirect contact,
Due to airborne infection.
Explain the Clinical manifestation/sign and symptoms of the child with the Chickenpox
feel tired,
Getting a low grade fever,
headache,
be together
feeling cold,
Scarring of the skin,
To see skin lesions,
hemorrhage,
Occurrence of ophthalmic and meningeal lesions

Clinical manifestation in chickenpox is divided into two parts.
1) Pre-eruptive,
2) Eruptive
1) Pre-eruptive,
Mild to moderate fever,
back pain,
feeling cold,
feel tired,
2) Eruptive
Recesses in the body,
fever,
Mascule,
papule,
vesicle,
pustule,
the crusts
Explain the Diagnostic evaluation of the child with the Chickenpox
History taking and physical examination,
laboratory test,
polymerase chain reaction test,
varicella virus test,
serological test,
Immuno fluorescent staining,
fluorescent antibody,
Latex agglutination and ELISA test,
Serological test.
Explain the management of the child with chickenpox
To relieve symptoms
If the child is experiencing pain and discomfort, provide analgesics.
Ex:= Acetaminophen
Ibuprofen.
If the child has fever, provide antipyretic medicine.
Ex:
Paracetamol,
Aspirin.
If the child is itching, give antihistamine medicine.
If the child has a fever, advise adequate water intake to prevent dehydration.
Provide antipruritic and mild sedation to the child.
Provide antiviral medicine to the child.
Ex:= Acyclovir.
If the child has an infection, provide antibiotic medicine.
Provide the child with calamine lotion, potassium permanganate lotion, antiseptic lotion and sponge bath properly.
Keeping the child’s nails properly short to prevent scratching.
Advise the child to properly maintain oral hygiene.
Advise the use of a soft toothbrush to prevent nasal mucosal injury.
Advise the child to maintain general cleanliness to prevent further infection.
Proper isolation of the child so that further child can be prevented from getting infected. And advising the child to avoid going to school for a minimum of six days.
Advise the child to maintain proper good hand hygiene.
Advise the child not to come in contact with a person who has not had chicken pox to prevent infection.
Provide two doses of proper varicella vaccination to the child.
First dose := at 12-15 month,
Second dose := at 4-6 years.
To provide proper work and comfortable environment to the child.
Provide complete education to the child and his family members about Chandni’s condition, its symptoms and signs and its treatment.
Providing proper psychological support to the child.
Advising the child’s parents to take proper care of the child.
Advise the child to take medication regularly and follow up.
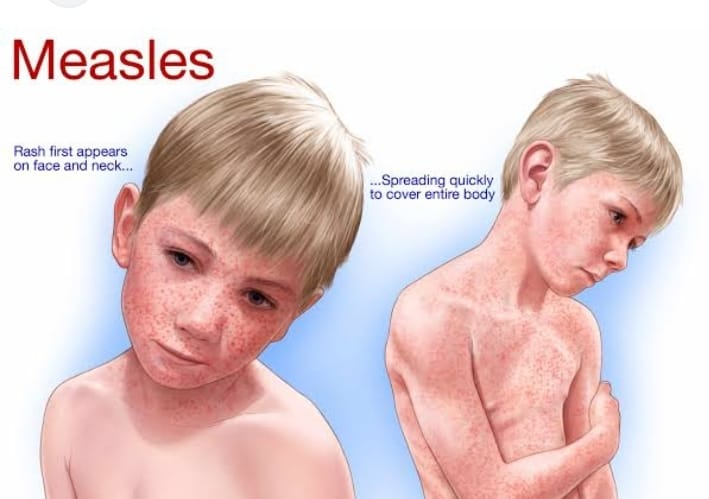
- Explain/Define Meseals in children. (Define Measles)
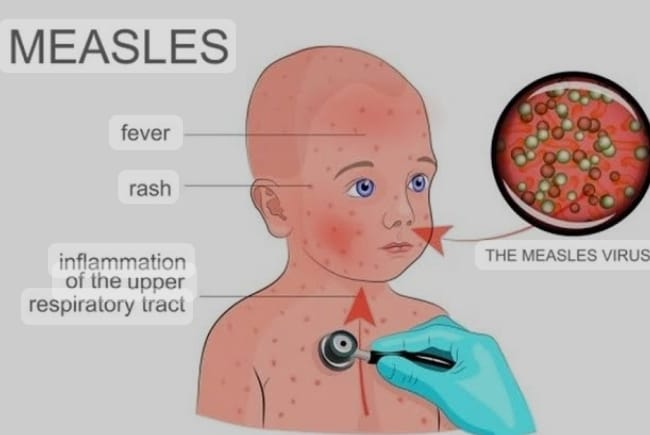
Measles (measles) is a highly contagious and viral infectious disease mainly caused by the measles virus that is mainly seen in children.
Measles usually presents with body fever, catarrhal symptoms in the upper respiratory tract, and maculopapular rashes on the body’s neck, face, trunk, neck, and legs.
However, measles is commonly seen in children under three years of age and mainly in malnourished children.
Explain the Etiology/cause of the child with the measles.
Mussels virus-a RNA Virous (Paramyxo virus group),
Due to coming in contact with droplets from an infected person,
A child who has not been vaccinated against measles.
Explain the mode of transmission of the Meseals
Incubation period:= 4-10 days.
Due to direct and indirect contact.
Due to droplet infection.
Due to respiratory droplets.
Explain the Clinical manifestation/Sign and symptoms of the Meseals
Symptoms and signs of measles are divided into three parts.
1) Prodomal (catarrhal) or preeruptive stage,
2) Eruptive Stage,
3) Convulsant stage or postmeasles stage.
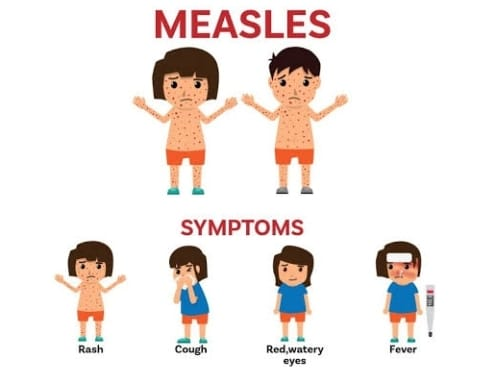
1) Prodomal stage (catarrhal) or pre-eruptive stage,
Prodomal stage (catarrhal) or preeruptive stage starts 10 days after infection and lasts for 3 to 5 days.
common cold,
coryza,
Ice is red,
lacrimation, and photophobia,
lymphadenopathy,
Vomiting and diarrhoea,
sneezing,
nasal discharge,
fever,
Bracey cough,
to be nosed,
feel tired,
sneezing,
nasal discharge,
Koplik Sports
(This sports a bluish white center with small white spots and is usually found inside the mouth and inner lining of the cheeks).
2) Eruptive stage
Maculopapularresis is seen in the wall body. The race usually starts from the mouth and then moves down the body to the trunk, mouth, and legs.
anorexia,
malays,
Cervical lymphadenopathy,
fever,
3) Convulsant stage or postmeasles stage.
fever,
to race,
fever,
Explain the Diagnostic evaluation of the child with Meseals.
History tacking and physical examination,
serological test,
ELISA test,
Leukocyte count assessment,
Routine blood examination,
blood culture,
Complement fixator antibody titer,
vaccination history,
Explain the management of the child with the measles.
To provide properly supportive and comprehensive care to the child.
1) Isolation
Measles is a highly infectious and contagious disease. Therefore, to prevent it from spreading, the child who has measles should be properly isolated. Isolation is usually done up to 4 days after rash appears.
2) Rest and hydration
Advise the child to take adequate rest.
Advise for adequate fluid intake to maintain hydration status and prevent dehydration.
3) Fever management
Provide antipyretic medication to the child to relieve the child’s fever.
Ex:= Acetaminophen,
Ibuprofen.
4) Symptomatic management
If the child has the condition of runny nose, cough, and conjunctivitis, then provide proper medication to the child.
If the child has nasal congestion, instill the child with nasal drops.
5) Nutrition
Provide adequate nutritional support to the child
6) Monitoring for complications
Closely monitor the child for any complications such as pneumonia and encephalitis.
Child has breathing difficulty, chest pain,
Get immediate medical treatment if you have conditions like severe headache, confusion, seizures.
7) Vitamin A Supplement
Provide vitamin A supplement if the child has vitamin A deficiency.
8). Preventive measures
Provide measles vaccine 0.5 ml as immunization to the child.
1st dose:=9-12month,
subcutaneously, right upper arm 0.5 ml
2nd dose:= 16-24 months
subcutaneously, right upper arm 0.5 ml. To provide proper work and comfortable environment to the child.
Explain / Define German Meseals in children (Define German measles in children.)
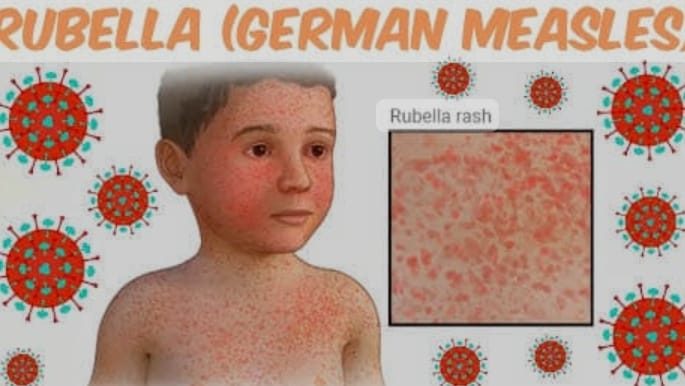
German measles is also called rubella. Which is called 3 day measles. It is a viral infection caused by rubella virus/myxovirus.
German Mussels is a Latin word meaning little red. This disease was first described by the German physician Friedrich Hoffmann in the mid-eighteenth century.
Measles usually affects children. And it is usually more common in children aged 3 to 10 years.
German measles causes low grade fever, cervical lymph node enlargement, sore throat, runny nose, red rash that starts from the face and spreads to the wall body. But if German measles occurs in a pregnant mother, the infection can be transmitted to the unborn child, causing serious birth defects called congenital rubella syndrome.

Explain the Etiology/cause of the child with the German Meseals.
Myxovirus / rubella virus
Explain the mode of transmission of the German Meseals
through respiratory droplets,
Due to coming in contact due to coughing and sneezing by an infected person.
Due to direct contact with respiratory secretions such as saliva and mucus.
Due to contact with contaminated surfaces.
Due to direct and indirect contact.
Explain the incubation period of the German Meseals
The incubation period of German measles (the first signs and symptoms after exposure to the infectious agent) is 14 to 21 days.
Explain the Clinical manifestation/ sign and symptoms of the child with the German Meseals.
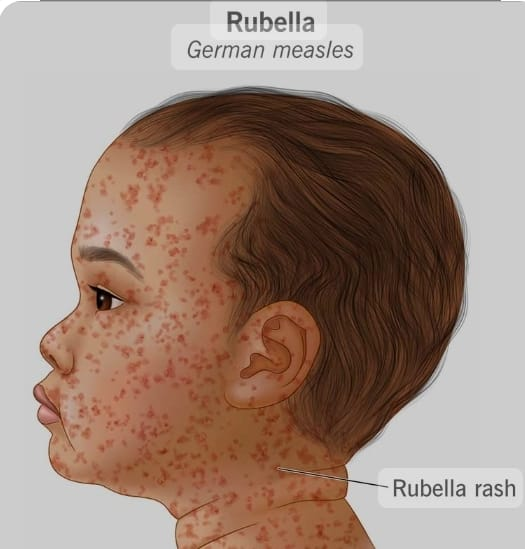
Recesses can be seen in the body.
fever,
lymphadenopathy,
Upper respiratory symptoms like cough, sore throat, runny nose, expectoration.
general discomfort,
one head,
fatigue,
General Malays,
joint pain,
Slight Malayalam,
Congenital rubella syndrome
growth retardation,
Congenital heart disease,
mental retardation,
Hepato splenomegaly,
hepatitis,
pancreatitis,
pneumonitis,
cleft pallet and foot,
retinal lesions,
Chronic encephalitis.

Explain the Diagnostic evaluation of the child with the German measles.
History tacking and physical examination,
serological test,
Laboratory testing,
blood test,
viral isolation,
Throat swab culture,
Haemagglutination Inhibition Test (HAI),
Explain the Management of the child with the German Meseals.
1) Symptomatic management
If there is fever, cough, sore throat, general discomfort, provide proper over the counter medicine to the child.
If the child is in pain, provide analgesic medicine.
Ex:=
Acetaminophen,
Ibuprofen,
2) Rest and hydration
Advise the child to take adequate rest.
Advise the child to take adequate fluids to keep them well hydrated.
3) Isolation
If a child gets German measles, it is a contagious disease, so keep the child in proper isolation. Keeping the child in eye isolation for a minimum of seven days after resection.
Advise the child to provide adequate rest to prevent any other complications.
4) Vaccination
Provide rubella vaccination to prevent the disease. Provide measles, mumps, and rubella (MMR) vaccination to the child.
Like providing two doses in measles,
1st dose:=9-12 month, subcutaneously, 0.5ml, is provided in right upper arm.
2nd dose:= 16-24 month, 0.5 ml, is provided subcutaneously.
To provide proper work and comfortable environment to the child.
To provide proper psychological support to the child and his family members.
- Explain/Define Mumps in children

Mumps is a viral infection and contagious disease caused by the mumps virus. And it affects the salivary gland (one or both parotid glands). It causes the salivary gland to become swollen and painful.
Children have fever, headache, muscle aches, fatigue, loss of appetite, and swallowing of cheeks and jaw. Mumps is usually caused by respiratory droplets from coughing, sneezing, and close contact with an infected person.
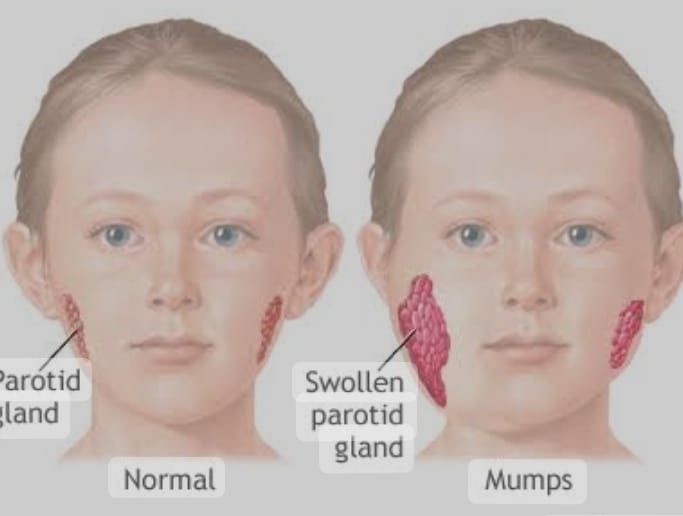
Explain the Etiology/cause of the child with the Mumps.
Mumps virus (paramyxovirus family),
RNA Viruses,
through respiratory droplets,
Due to coming in direct contact with the saliva and mucus of an infected person,
Explain the mode of transmission of the Mumps in children
Due to contact with respiratory droplets from sneezing and coughing of infected persons.
Due to coming in direct contact with saliva and mucus of infected person.
Explain the incubation period of Mumps in children
The incubation period of mumps is 12 to 24 days.
Explain the Clinical manifestation/ Sign and symptoms of Mumps in children

Swelling in one or both parotid glands.
Tenderness in the parotid gland.
Getting a fever.
Head one and ear one.
Pain while chewing and swallowing.
Fatigue and generalized malaise.
Do not feel hungry.
Pain in the muscles.
Submaxillary and sublingual gland enlargement of the gland.
Explain the Diagnostic evaluation Mumps in children
History taking and physical examination,
CSF examination,
blood test,
Laboratory Investigation,
serological test,
Imaging studies.
Complement fixation test.
Explain the management of Mumps in children
1) Symptomatic management
If the child is in pain, provide analgesic medicine.
Ex:= Acetaminophen,
Ibuprofen.
If the child has fever, provide antipyretic medicine.
Giving advance to child to take adequate rest.
Advise the child to take adequate fluids.
2) Comfort measures
If the child’s salivary gland is swollen, provide compresses and compresses.
Provide the child to properly intake soft food.
3) Isolation
Provide proper isolation to the child who has the condition of mumps.
4) Proper hospitalization of the child to prevent complications.
5) Vaccination
Proper measles, mumps, and rubella (MMR) vaccine should be provided to the child so that mumps condition can be prevented.
Advise the child to gargle with mouth saline mouth wash.
Explain/Define Poliomyelitis in children
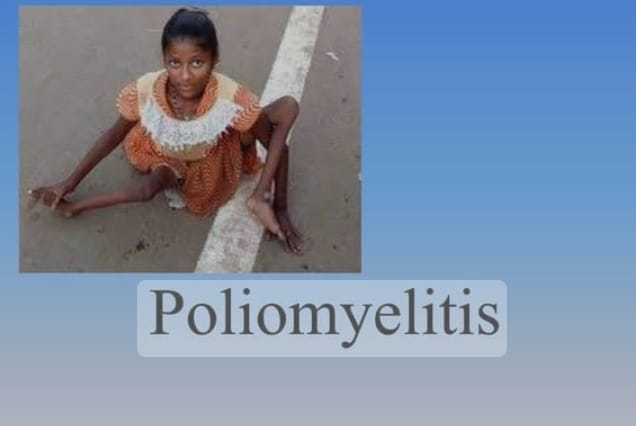
Poliomyelitis is also commonly called polio. Poliomyelitis is a highly contagious, acute viral and infectious disease. It is usually caused by an RNA enterovirus called poliovirus. The poliovirus usually destroys the anterior bone cells of the spinal cord and the nuclei of the cranial nerves and causes paralysis.
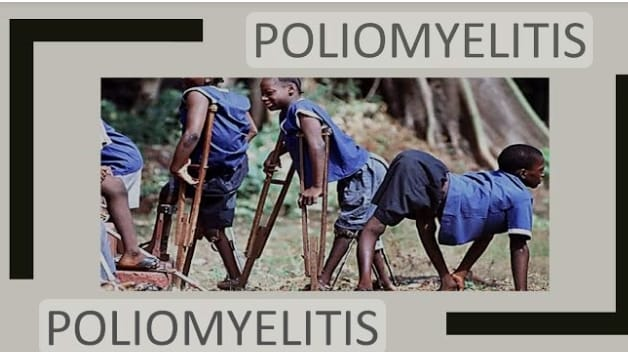
Polio usually affects children under the age of five. Polio virus is usually caused by coming into contact with contaminated food, contaminated water, and the feces of an infected person. Polio usually causes paralysis with involvement of the lower legs, along with the involvement of the alimentary tract, and also involvement of the central nervous system if the respiratory muscles are involved, a life threatening condition arises.
Explain the Etiology /causes of Poliomyelitis in children
Caused by poliovirus (type I,II,III)/ RNA enterovirus,
Due to coming in contact with infected person’s physis,
If an infected person coughs and sneezes, due to coming in contact with its droplets,
By fico oral route,
Due to intake of contaminated food and contaminated water,
Due to poor sanitation and unhygienic conditions,
In unimmunized children,
Due to a weakened immune system due to malnutrition,
In over crowded areas,
Due to non-immunization of polio.
Due to traveling to an area where polio is an outbreak.
Explain the mode of transmission of Poliomyelitis in children
Mainly by the oropharyngeal route,
Due to coming into contact with infected person’s physis,
Due to contact of contaminated surfaces with impacted bodies,
By fico oral route,
Due to ingestion of contaminated food and water,
Due to coming into contact with its droplets due to coughing and sneezing of an infected person,
Explain the incubation period of Poliomyelitis in children
The incubation period of poliomyelitis in children is 7 to 14 days.
Explain the Clinical manifestation/ Sign and symptoms of Poliomyelitis in children
The symptoms and signs of polio myelitis depend on the different types such as,
1) Asymptomatic poliomyelitis (silent/inapparent/subclinical infection),
2) Abortive poliomyelitis
(Minor Illness),
3) Non Paralytic Polio Myelitis,
4) Paralytic polio myelitis
subtype:=
A) Spinal form,
B) Bulbar form,
C) Bulbospinal form,
D) encephalitis form

) Asymptomatic Poliomyelitis (Silent/Inapparent/Subclinical Infection)
Approximately in asymptomatic poliomyelitis
90 to 95% of infected persons are infected with the virus and the infection is asymptomatic.
2) Abortive poliomyelitis (minor illness),
Abortive poliomyelitis is a mild and self-limiting illness and accounts for 4-8% of cases. These viruses usually invade the blood stream and cause the condition of viremia. Its signs and symptoms typically include,
Fever, sore throat, headache, nosia, vomiting, loss of appetite, abdominal pain, body pain are seen.
3) Non Paralytic Polio Myelitis,
In nonparalytic poliomyelitis, the poliovirus usually enters the urinary system. And its 1% cases are seen.
Its symptoms include neck stiffness, headache, back pain, pain in legs, neck pain and nosia and vomiting. Paralysis does not occur in this. The symptoms are
Occurs for 1 to 2 weeks and then resolves.
4) Paralytic polio myelitis
Paralytic polio myelitis is the most severe form of polio. In which paralysis occurs in one or more limbs, the virus enters the central nervous system (CNS) and subsequently creates a condition of paralysis. Its most important feature is acute asymmetric flaccid paralysis (AFP). There is muscle stiffness, muscle pain, stiffness in a child with the condition of Chinese lighting polio.
A) Spinal form
Paralytic poliomyelitis of the spinal form involves the extremities, neck, abdomen, diaphragm and intercostal muscles.
Then there are symptoms like fever, muscle pain, tremors, deep tendon reflex being demineralized.
Flaccid paralysis occurs predominantly in the lower limb followed by the upper limb. And large muscles are more affected than small muscles. And due to the involvement of bladder and bowel, the condition of urinary retention and constipation is seen. In the spinal form, respiratory difficulty is seen due to the involvement of the diaphragm and intercostal muscles.
B) Bulbar form
The bulbar form is a less common but more severe form because it involves the vital medullary center and
It involves paralysis in the muscles supplied by the cranial nervous and vital respiratory and circulatory centers. In its symptoms and signs
dysphagia,
dyspnea,
nasalspeech,
Facial paralysis occurs.
Paralysis of the vagus nerve causes weakness in the soft palate, pharyns and vocal cords, resulting in nasal speech and hoarseness of voice.
Difficulty occurs in bridging and swallowing.
There is a chance of aspirating due to regurgitation
Atelectasis and pneumonia develop. Involvement of the respiratory center leads to cellular irregular breathing, and oxygen saturation is demineralized.
Child mother
restlessness,
Confusion and unconsciousness are seen.
C) Bulbospinal form,
Bulbar form and spinal form are seen in this. And 25% of paralytic cases are seen.
D) encephalitis form
A less common form of encephalitis presents in patients with irritability, tremors, drowsiness, convulsions, unconsciousness.
Other symptoms
feel tired,
fever,
one head,
vomiting,
Diarrhea and constipation,
sore throat,
Neck Stephenish,
Sensitivity to light,
muscle pain,
wickness,
paralysis,
Difficulty in breathing, swallowing and talking.
Explain the Diagnostic evaluation of the child with the Poliomyelitis
History taking and physical examination
Clinical assessment,
laboratory test,
stool examination,
throat swab,
viral culture,
Polymerase chain reaction testing (PCR test),
throat swab,
Cerebrospinal fluid (CSF) assessment,
serological test,
imaging studies,
x ray,
M.R.I. testing,
Lumbar puncture (spinal tap),
electromyography,
Explain the management of the child with the Poliomyelitis

Providing properly supportive treatment to the child.
Advise the child to take proper bed rest.
Giving advice to maintain proper nutritional status of child.
Advise the child to have adequate fluid intake. So that the child’s fluid and electrolyte levels can be properly maintained.
Proper medication should be provided if the child has symptoms like fever, pain and discomfort.
Provide proper physical therapy if the child has muscle weakness, paralysis.
Provide proper rehabilitation therapy to strengthen muscles, improve flexibility.
Provide supportive devices such as braces, orthoses, crutches, and wheelchairs to improve the child’s mobility and independence.
Provide proper respiratory support if the child has respiratory muscle weakness.
Closely monitor the child’s respiratory function.
If the child has joint pain, muscle pain, joint stiffness, then analgesic medicine should be provided.
Provide proper relaxation techniques to the child.
To provide adequate care to prevent the child from secondary complications.
Providing education to the child to maintain good hygiene practices.
Proper polio vaccination should be provided to the child so that the condition of poliomyelitis can be prevented.
Provide proper polio vaccination to child as per immunization.
Provide mild sedative to child for pain relief.
Any child
To assess whether the condition of respiratory distress is present or not.
To provide proper emotional support to the child and his family members.
- Explain/Define Dengue fever.

Dengue fever is a viral disease caused by group B arbovirus. Dengue fever is caused by mosquito bites such as Aedes aegypti, Aedes albopictus. Children with dengue fever have high fever, purpuric sports, headache, joint and muscle pain, seizures and vomiting, irritability, lethargy, and decreased appetite. Dengue fever is also called “backbone fever”.
Explain the Etiology/cause of the dengue fever
dengue virus,
flavi virus,
Explain the mode of transmission the dengue fever
Dengue fever is usually transmitted by mosquitoes.
Addis Egypt,
Aedes albopictus.
Explain the incubation period of the dengue fever
The incubation period of dengue fever is 3 to 15 days.
Explain the clinical manifestation/ sign and symptoms of the dengue fever.
Getting high fever,
pharyngitis,
rhinitis,
diarrhea,
black head,
Muscle, bone and joint pain,
Maculopapular lesions in the trunk and upper limbs of the body,
feel tired,
Generalized quickness occurs,
Pain in the back of the ice (retro orbital pain),
Nausea and vomiting
loss of appetite,
Bad test coming from the mouth,
Flushing of the face,
Cervical lymphadenopathy,
hepatosplenomegaly,
bradycardia,
Profuse sweating.
Explain the diagnostic evaluation of the dengue fever
(State the diagnostic evaluation of dengue fever)
History taking and physical examination,
laboratory test,
blood examination,
stool examination,
Enzyme linked immunosorbent assay (ELISA) test,
Complete blood count
Liver function test,
imaging studies,
x ray,
Serological monitoring.
A positive Hess test,
raised hematocrit,
leukopenia,
Reduce platelet counts,
IGM antibody test
Explain the management of the dengue fever.
Proper assessment of the child.
Proper symptomatic management of the child.
Maintain child’s hydration status to prevent child from dehydration.
Give proper antipyretic medication to the child.
Ex:= Acetaminophen,
(Paracetamol),
If the child is in pain, provide analgesic medicine.
Ex:= Acetaminophen,
Ibuprofen.
Advise the child to take adequate rest.
Closely monitoring the child to assess whether he has any signs of dehydration, decrease in urine output, dry mouth, burnt ice, etc.
To monitor the child’s vital signs properly.
Maintaining Child No Intake Output Chart.
Advise the child to intake easily digestible food.
Providing education to parents to prevent their child from mosquito bites. Like using insect repellent, giving advice to wear long-sleeved clothes, giving advice to use mosquito nets and screens.
To provide complete education to the child and his parents about the child’s condition, its symptoms and signs, and its treatment.
To provide education to the parents of the child to take proper care of the child.
To provide work and comfortable environment to children.
Advising parents of child to provide regular medication of child.
Advising parents of child to take regular follow up.
- Explain/Define Rabies in children
Rabies is also known as hydrophobia (fear of water). Rabies is a fatal viral disease that affects the central nervous system. And when symptoms are present, it can be a fatal condition. In children, rabies is usually caused by bites and scratches from infected animals, usually dogs, cats, jackals, and wolves.
The rabies virus is usually transmitted through the saliva of an infected animal through the bite of an infected animal.
Symptoms of rabies in children are initially flu-like, including fever, headache, and general malaise.
As the disease progresses, more symptoms appear, such as anxiety, confusion, hallucinations, difficulty swallowing, and hydrophobia (fear of water). Eventually, if left untreated, rabies can lead to paralysis, coma, and even death.
Explain the Etiology/cause of the Rabies in children
Caused by Lysa virus type I
Explain the mode of transmission of the Rabies in children
Due to bites and scratches from infected animals,
1) Byte
Due to the bite of an infected animal, its saliva enters the child’s body and creates the condition of rabies.
2) Scratch
When infected animals scratch the child, the infection is transmitted and the child can become infected.
3) Due to contact of infected mucous membrane.
Infected saliva from animals comes into contact with mucus membranes such as child’s mouth, nose and eyes.
Explain the incubation period of the Rabies in children.
Incubation period
It is from 1 to 3 months.
Explain the clinical manifestation/ sign and symptoms of Rabies in children
(State the symptoms and signs of rabies in children)
1) Prodomal phase
This phase lasts from 2 to 10 days.
These include pyrexia, malaise,
vomiting,
anorexia,
one head,
Anxiety, and pain and paresthesia are seen towards the wound site.
2) Acute neurological stage
Hydrophobia (fear of water),
Aerophobia (fear of air),
Excessive salivation,
hyperreactivity,
agitation,
Restlessness.
Hallucinations: Visual and auditory hallucinations.
Confusion and disoriented := changes in mental status.
Paralysis.
3) Coma and death
Coma and death can also occur due to rabies.
Brust, hyperreactivity, hoarseness of voice,
dysphagia,
pharyngeal pain,
convulsions,
Meningeal irritation.
Explain the management of Rabies in
Management of rabies in children
explain)

1) Local treatment
The suspected wound is immediately washed with soap and water followed by the application of alcohol and tincture of iodine.
Then apply dressing and bandage.
2) Observe the animal for 10 days.
Keep the biting animal under close observation for three days or if the animal dies within 10 days after the bite, signs of illness are seen. Therefore, antirabies treatment should be started immediately.
3) Antirabies treatment
Rabies vaccine prepared from central nervous tissue of infected animals. The vaccine is provided subcutaneously in the anterior abdominal wall.
A dose of 2 to 5 ml is provided for 7 to 14 days.
4) Post Exposure Prophylactic (PEP)
However, contact with saliva and body secretions of animals with suspected rabies should provide immediate medical attention.
Properly clean the wound in post-exposure prophylaxis.
Then provide proper rabies vaccination and often provide rabies immunoglobulin.
5) Supportive care
The child’s surface is usually provided to prevent infection, reduce pain, reduce fever and anxiety.
Advise the child to have adequate fluid intake to prevent dehydration.
Provide proper oxygen therapy to the child.
Providing nutrition to improve the child’s immune system and overall health.
To provide proper comfort measures to the child.
To provide proper comfort measures to the child and his family members.
Properly vaccinate any pet to control rabies.
Explain/Define whooping cough in children
Whooping cough is also known as pertussis. Whooping cough is a highly contagious, communicable and acute bacterial infection of the respiratory tract whose causative organism is Bordella pertussis.
This is mainly seen in pre-schoolers and newborns, especially in children who have not been properly immunized.
Whooping Cough Children in the paroxysmal stage of pertussis have episodes of coughing accompanied by a distinctive “whooping” sound when breathing. Children with this disease initially have symptoms similar to those of the common cold, but it is known as whooping cough because of the wheezing sound that progresses with coughing. Whooping cough is also known as “100 day cough”.
The habit pattern of cuffing can last for a long period of time, even weeks and months, so the Chinese call it “100 day fever”.
Explain the Etiology/cause of the whooping cough
Bordella pertussis,
Bordella parapertussis,
Haemophilus
hemolyticus,
Bordella bronchiseptica,
Adenovirus infection.
Due to over crowded place,
Due to low sanitation,
Due to poor environmental hygiene,
Due to decreased immunity of a person,
Due to non-vaccination of whooping cough,
Due to winter and spring season.
Explain the mode of transmission of the whooping cough
Due to droplets through the mouth and nose of an infected person,
Other droplets due to infection,
Due to coming in contact with a contaminated object.
Due to contact with oral secretions and droplets.
Due to coming in contact with any contaminated surface.
Explain the incubation period of the whooping cough
The incubation period for whooping cough is 7-14 days, but no longer than 3 weeks.
Explain the clinical manifestation/ Sign and symptoms of the whooping cough
Symptoms and signs of whooping cough are divided into 3 stages.
1) Catarrhal stage (0-2 week),
2) Paroxysmal stage and spasmodic stage (2-4 weeks),
3) Convalescent stage (last 2 weeks)
1) Catarrhal stage (0-2 week),
Early symptoms in the catarrhal stage include,
fever,
rhinitis,
sneezing,
Anorexia (loss of appetite),
Nausea and vomiting,
lacrimation,
Irritating cough at night time,
2) Paroxysmal stage and spasmodic stage (2-4 weeks),
Paroxysmal cough,
vomiting,
Whooping sound while breathing,
laryngospasm,
Baby is cyanosis with congestion (red face) feeling suffocated.
Excited look,
sweating,
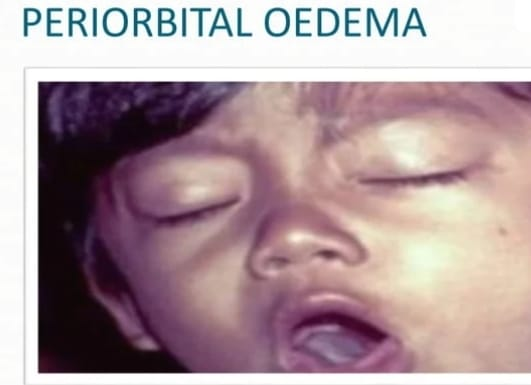
occurring in peri-orbital AD,
Subconjunctival hemorrhage,
Ulcers and frenulum in the tongue,
Dehydration,
exhaustion,
convulsions,
Neck and scalp vein congestion,
Confusion and restlessness,
Paroxysms are triggered with eating, yawning, sneezing.
3) Convalescent stage (last 2 weeks)
Disturbing Cough,
Vomiting stops,
Appetite is greatly improved,
Cough is present for more than a week and a month.
The Chinese call it “100 day fever”.
atelectasis,
Bronchopneumonia.
Explain the Diagnostic evaluation of the child with the whooping cough.
History tacking and physical examination,
White Blood Cells (W.B.C Count) Assessment,
Erythrocyte sedimentation rate (ESR) assessment,
chest x-ray,
ELISA test (to detect the IGM, IgG, or IgA),
nasopharyngeal swab culture,
blood examination,
Explain the management of the whooping cough.
1) Supportive care
Advise the child to take plenty of rest.
Advise adequate fluid intake to maintain child’s hydration status.
Keep the child away from smoke and other respiratory irritants.
2) Providing antibiotic medication
Ex:=
Azithromycin,
Clarithromycin and Roxythromycin up to 5-7 days,
Erithromycine 50 mg/kg/day in four divided doses twice weekly,
3) Isolation
Keep the infected child properly isolated. So that transmission to other children can be prevented.
4) Bronchodilators
Provide nebulization bronchodilator if child has severe paroxysmal cough
Ex:= salbutamol (0.3-0.5 mg /kg / day in three divided doses), albuterol.
If the child has severe cuffing, provide Betamethasone (0.75 mg/ kg/ day).
5) Supportive nursing care
Keeping the child properly isolated,
Provide oxygen to the child to prevent the condition of hypoxia.
If there is secretion, remove it properly.
Provide proper positioning of the child to relieve respiratory discomfort.
Provide adequate fluids to maintain child’s hydration and electrolyte levels.
Advise the child to take small, frequent amounts and easily digestible food intake.
Advising parents to maintain proper hygienic condition of child.
Advising parents to provide meditation to a child.
To provide complete education to the child and his family members about the child’s disease, its causes, symptoms and signs and its treatment.
Explain the preventive measures of the whooping cough.

- Vaccination
Proper diphtheria, pertussis and tetanus (DPT) vaccine should be provided to the child so that whooping cough can be prevented.
DPT Vaccine 0.5ml,
IM (Intra Muscular),
3 doses and 2 booster doses
antero lateral side of the mid-thigh.
DPT 1st dose:=
at 6 weeks,
DPT 2nd dose:=
at 10 weeks,
DPT 3rd dose:=
at 14 weeks,
DPT 1st booster dose:=
at 16-24 months,
DPT 2nd booster dose:=
at 5-6 years (upper arm),
Whooping cough can be prevented in children by providing vaccination.
Explain/Define Epidemic typhus.
Epidemic typhus is called louse-born typhus. This is a rare but serious bacterial infection caused by the bacterium Rickettsia provezekii (gram-negative non-flagellated coccus bacillus).
Epidemic typhus is usually caused by the bite of an infected lice. Epidemic typhus is more common in persons living in overcrowded areas and in unhygienic conditions.
Explain the Etiology/cause of the Epidemic typhus
The bacterium Rickettsia provezekii,
By biting an infected body lichen,
Due to over crowded area,
Due to unsanitary conditions,
Due to unhygienic conditions.
Explain the mode of transmission the Epidemic typhus
Due to the bite of infected bodylice,
Due to overcrowded area,
Due to unsanitary conditions,
Due to unhygienic conditions.
Explain the incubation period of the Epidemic typhus.
The incubation period of epidemic typhus is 14 days.
Explain the Clinical manifestation/ sign and symptoms of the Epidemic typhus.
Getting a very high fever,
severe headache,
Muscle pain and body aches,
feeling cold,
abdominal tenderness,
Races can be seen in the body,
muscle aches,
joint pain,
Loss of appetite (anorexia),
Non productive cough,
Nausea and vomiting
Diarrhea and constipation,
abdominal pain,
hear the tinnitus sound,
Meningismus (neck stiffness, headache, photophobia, nozia and vomiting).
Central nervous system signs and symptoms such as confusion,
Photophobia
delirium,
Sometimes coma can also occur due to central nervous system involvement.
Visual disturbance,
Myocarditis (infection and inflammation of the middle layer of the heart i.e. myocardium).
Explain the Diagnostic evaluation of the Epidemic typhus
History taking and physical examination,
clinical assessment,
laboratory test,
blood test,
Serological test (immunofluorescence assay (IFA) or enzyme linked immunosorbent assay (ELISA)), polymerase chain reaction testing (PCR testing),
imaging studies,
chest x-ray,
skin biopsy,
Weyl-Felix reaction,
Explain the management of the Epidemic typhus
1) Provide proper antibiotic therapy.
Ex:=
Doxycycline:= orally/intravenously
Dose := 2.2 mg/ kg/ 24 hour in two divided doses,
Chloramphenicol:= 50-100 mg/24 hours/ Qd up to 5 days
And tetracycline.
2) Suppository care
Provide proper supportive treatment to the child so that complications can be prevented.
In which giving advice to the child to take adequate rest.
Advise adequate fluid intake to maintain child’s hydration status.
If the child has fever, provide antipyretic medication.
3) Isolation and infection control
If the child has the condition of epidemic typhus, keep him properly isolated so that its transmission to other children can be prevented.
Advise the child to maintain proper hygienic condition.
Advise the child to maintain proper environmental sanitation.
4) Monitoring for complications
Close monitoring of the child to assess for any complications like pneumonia, dehydration, and neurological signs and symptoms.
5) Preventive measures
Control lice infestation and improve hygienic conditions and living standards.
To provide proper psychological support to the child and his family members.
Explain/Define Precocious puberty
Puberty is a biological process in which a child
Many physical and hormonal changes take place in the body
is Due to this sexual maturity and reproduction
Abilities are developed.
Normal puberty time is between 8 and 13 years
And normal puberty time in boys is 9 to 14 years
Between and if puberty is normal in a child
If it develops earlier than age, it is called precocious puberty
is called
The term ‘precocious’ refers to physical and mental development occurring earlier than the expected time.
Precocious puberty means when puberty starts before 8 years in girls i.e. breast development, growth of pubic hair and menstruation cycle starts before 8 years in girls and puberty starts before 9 years in boys i.e. enlargement of testicles and penis. If growth, growth of pubic hair, changes in voice start before 9 years, it is called precocious puberty.
Precocious puberty means when the secondary sexual characteristic in girls and boys starts earlier than its normal time, it is called precocious puberty.
Explain the type of the Precocious puberty
There are two types of precocious puberty.
1) Central Precocious Puberty (CPP), (True Precocious Puberty),
2) Peripheral Precocious Puberty (PPP), (Pseudo Precocious Puberty)
1) Central Precocious Puberty (CPP), (True Precocious Puberty),
Central precocious puberty is usually caused by premature activation of the hypothalamic pituitary gonadal (HPG) axis. Central precocious puberty usually occurs due to excessive secretion of gonadotrophin releasing hormone (GTRH).
Central precocious puberty is usually seen as a complication of brain abnormalities such as congenital anomalies, cranial irradiation, hydrocephalus, central nervous system tumors, central nervous system trauma, and central nervous system infections.
A common cause of precocious puberty is a hypothalamic hamartoma (the formation of a tumor-like structure over the hypothalamus).
In central precocious puberty, spermatogenesis and ovulation are premature and physical and sexual maturation are similar to normal puberty.
2) Peripheral Precocious Puberty (PPP), (Pseudo Precocious Puberty)
Peripheral precocious puberty is usually caused by increased secretion of sex steroid hormones (androgens and estrogens) from the adrenal glands and gonads (ovaries and testes). This peripheral precocious puberty is independent of the hypothalamic pituitary gonadal (HPG) axis.
In this type, spermatogenesis and ovulation are incomplete and partially developed but other signs of sexual maturation are present and somatic growth is rapid.
Explain the Etiology/cause of the Precocious puberty
1) Central Precocious Puberty (CPP), (True Precocious Puberty),
idiopathic,
Due to abnormalities of the central nervous system,
A) Congenital Anomalies of Central Nervous (CNS) System
Due to hydrocephalus,
Due to hypothalamic hamartoma,
Due to porencephaly (a cystic CVT present in the brain matter, this CVT communicates with the ventricular system and the subarachnoid space),
B) Acquired lesions of central nervous system
Due to inflammation,
Due to radiation therapy,
due to chemotherapy.
Due to trauma,
Due to any surgery,
due to granuloma.
C) Due to tumors in the central nervous system
In Opticaglio,
pineal tumor,
In craniopharyngio,
In ependymo.
2) Peripheral Precocious Puberty (PPP), (Pseudo Precocious Puberty)
Girls :=
Due to tumor in adrenal gland,
Ovarian causes
Due to granulosa thecacell tumor,
Due to gonadoblastoma,
Due to benign follicular cyst,
Boyce:=
Due to a testis bearing cell (cell that releases the male hormone testosterone) tumor,
Due to adrenal tumors,
testotoxicosis,
Due to hormonal imbalance.
Explain the Clinical manifestation/ sign and symptoms of the Precocious puberty
Girls:=
Premature development of the breast (thalarchy),
Early growth of pubic hair (puberty),
Menstruation cycle (menarche) starts early,
Rapid growth,
Advance bone maturation,
Emotional and behavioral changes,
Increased production of sweat and sebum in the body,
Passing vaginal discharge due to hormonal changes.
Boyce:=
Dislocation of testicles and penis,
Early growth of pubic hair,
Height increase,
Weight gain,
darkening of voice,
Early growth of hair on face, chest, under
Early bone maturation,
Emotional and behavioral changes such as mood swings, irritability, low self-esteem etc.
Increased production of sweat and sebum,
Linear growth and muscle growth,
Explain the Diagnostic evaluation of the Precocious puberty
History taking and physical examination,
blood test,
Hormonal level testing (including Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), Estradiol in girls and Testosterone in boys)
imaging studies,
x ray,
like this. R.I.,
Gonadotrophin releasing hormone testing,
genetic testing,
Gonadal biopsy to identify the cause and identify associated problems.
Explain the management of the Precocious puberty
1) Treatment of underlying condition
If precocious puberty is any kind of medical condition like tumor, hormonal imbalance then it should be properly treated. Radiation therapy, chemotherapy and surgery are also used to treat this medical condition.
2) Gonado trophin releasing hormone (GnRH) analogs
Gonadotrophin releasing hormone (GnRH) analogues such as leuprolide or triptorelin suppress the release of gonadotrophins (luteinizing hormone (LH) and follicle-stimulating hormone (FSH)) from the pituitary gland, thus delaying puberty growth.
3) Peripheral precocious puberty ma
Medroxy progesterone Acetate 100mg/m2 every 2-3 weeks to treat the underlying cause
intramuscular,
Provide an oral dose of 10 mg twice a day.
Cyproterone Acetate 100- 150 mg /m2/ day in two to three divided doses This medication stops the cyclical bleeding leading to regressing of the secondary sexual characteristic.
4) Monitoring and follow up
Regularly monitoring how effective the treatment provided to the child is.
4) Psychological support
To provide proper psychological support and counseling to the child to cope up with his condition.
5) Educational support
To provide complete education to the child and his family members about the causes of the child’s condition, its symptoms and signs and its treatment.
To provide proper guidance and counseling to the child and his parents.
6) Lifestyle modification.
Giving advice to the child for proper life style modification.
Advise the child to do regular exercise.
Advise the child to take a nutritious diet.
Advise the child to get adequate sleep.
To provide proper work and comfortable environment to the child.
- Explain/Define Gynecomastia
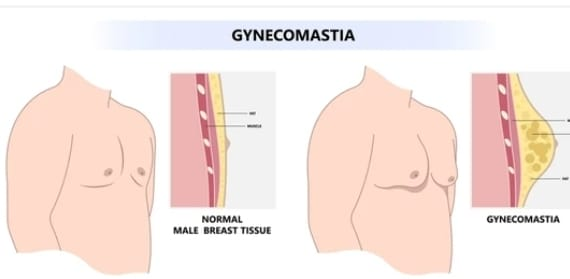
Gynecomastia is a medical condition in which there is an enlargement of the breast tissues in the male. Gynecomastia is usually seen due to hormonal imbalance i.e. imbalance of estrogen and testosterone hormone, in which the level of estrogen increases in comparison to testosterone. Gynecomastia is usually seen in infancy and
A higher proportion is seen during puberty.
Pseudogynaecomastia Pseudogynaecomastia is an enlargement of the male breast but is usually due to fat deposits.
Synonyms of pseudogynecomastia include adipomastia and lipomastia.
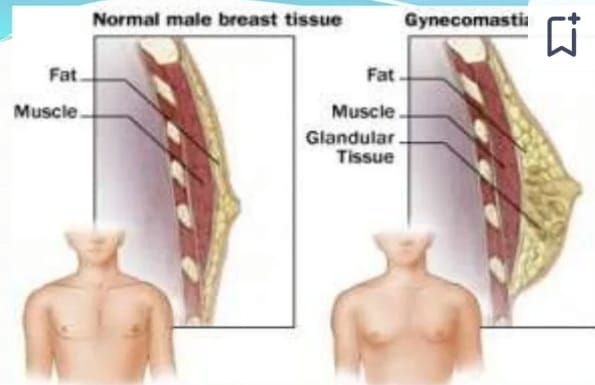
Explain the etiology/causes of the gynecomastia
Due to hormonal imbalance.
Estrogen and testosterone hormone are responsible for the development of breast tissues, when the amount of estrogen increases than testosterone hormone, breast enlargement takes place.
Due to certain medical conditions like,
liver disease,
liver cirrhosis,
kidney failure,
testicular disorder,
Due to testicular tumor,
Due to obesity,
Explain the clinical manifestation/ Sign and symptoms of the gynecomastia
Male breast enlargement,
Nipple A Swollen and firm.
Discomfort and pain in affected breast,
Tenderness and sensitivity present,
Discharge from the nipple,
Enlargement of axillary lymph nodes,
Psychological symptoms are seen,
Low self esteem.
Explain the Diagnostic evaluation of the gynecomastia
History taking and physical examination,
hormonal testing,
Blood test to assess hormonal levels (luteinizing hormone, follicle stimulating estrogen, testosterone),
imaging studies,
CT-scan,
mammography,
ultrasound,
MRI,
biopsy,
Explain the management of the gynecomastia
Proper assessment of the child’s condition.
If gynecomastia is due to any medical condition like hormonal imbalance, medication side effect, treat the cause properly.
To provide proper reassurance and psychological support to the child and his family members.
To provide proper psychological support to the child and his family members.
Providing children with hormonal modulating medications such as selective estrogen receptor modulators (SERMS) or aromatase inhibitor medications.
If the child has a condition of persistent and severe gynecomastia, tamoxifen and raloxifene medication should be provided.
Gynecomastia in children is transient and resolves within one to two years.
To provide proper psychological support to parents and child to remove their anxiety and stress.
Advising the parents to provide proper work and comfortable environment to the child.
To provide complete education to the child’s parents about the child’s condition, its symptoms and signs, and its treatment.