Second Year Post-Basic B. Sc.Nursing December 2022~ Mental Health Nursing (upload paper no.six)
Second Year Post-Basic B. Sc.Nursing December – 2022-Mental Health Nursing
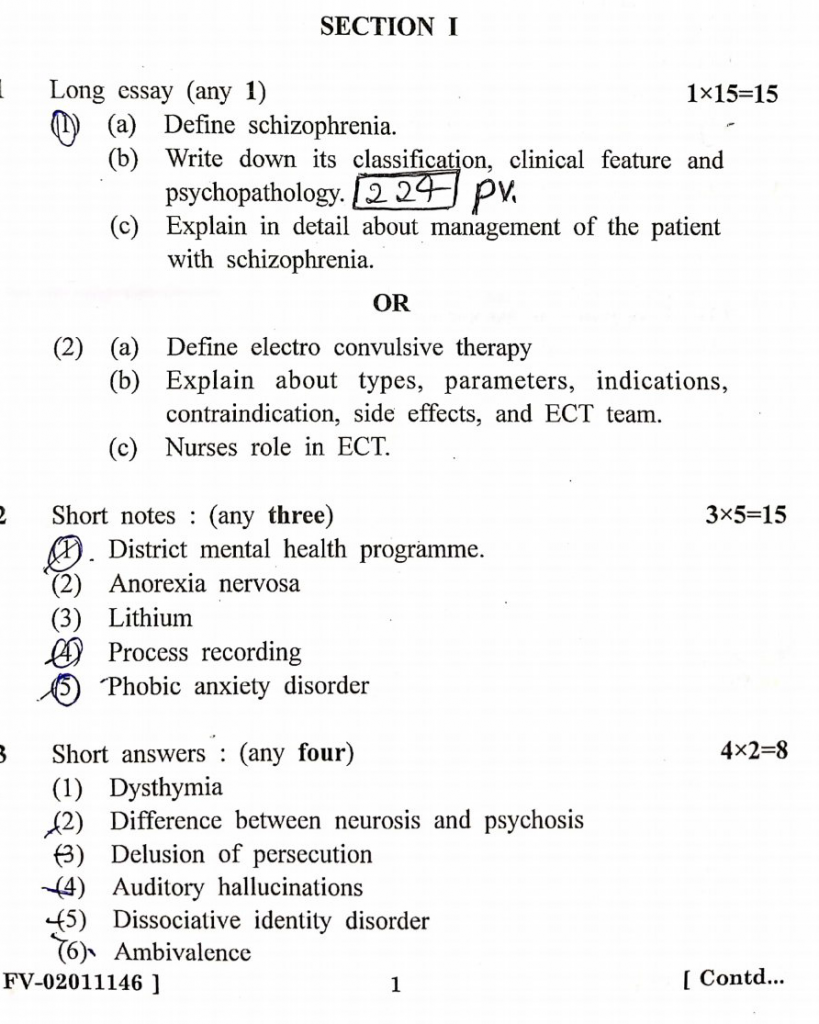
SECTION- I
1 Long essay (any 1) 1×15-15
(a) Define schizophrenia.
chizophrenia is a chronic and severe mental health disorder that affects how a person thinks, feels, and behaves. Individuals with schizophrenia may experience hallucinations (seeing or hearing things that are not present), delusions (false beliefs), disorganized thinking, and severely impaired functioning in daily life. It typically emerges in late adolescence or early adulthood and can impact speech, emotional regulation, and social interactions.
The exact cause of schizophrenia is unknown, but it is thought to result from a combination of genetic, biochemical, and environmental factors. Schizophrenia often requires long-term treatment with a combination of medications (antipsychotics), psychotherapy, and supportive care.
(b) Write down its classification, clinical feature and psychopathology.
Classification of Schizophrenia
Schizophrenia can be classified based on symptom patterns and the presentation of the disorder. The most common types include:
- Paranoid Schizophrenia
- Characterized primarily by prominent delusions and hallucinations, often with themes of persecution or grandiosity.
- Disorganized Schizophrenia (Hebephrenic)
- Marked by disorganized speech, behavior, and flat or inappropriate emotional responses.
- Catatonic Schizophrenia
- Dominated by motor symptoms, such as immobility, excessive motor activity, extreme negativism, or peculiar voluntary movements.
- Undifferentiated Schizophrenia
- A type that does not fit neatly into any one category, with mixed symptoms from different subtypes.
- Residual Schizophrenia
- Occurs when the intensity of symptoms has lessened, but some signs of schizophrenia, like emotional blunting, remain.
- Simple Schizophrenia
- Gradual onset of negative symptoms, such as apathy, emotional blunting, and withdrawal from social interactions, with few positive symptoms like delusions or hallucinations.
Clinical Features of Schizophrenia
The clinical manifestations of schizophrenia are generally divided into positive and negative symptoms, along with cognitive and affective disturbances.
- Positive Symptoms (Excess or distortion of normal functions):
- Delusions: Fixed, false beliefs not based in reality (e.g., paranoia, grandiosity).
- Hallucinations: Sensory perceptions without external stimuli, most commonly auditory (hearing voices).
- Disorganized Speech: Incoherent or fragmented thoughts and speech (e.g., tangentiality, derailment, word salad).
- Disorganized or Catatonic Behavior: Inappropriate or bizarre behavior, agitation, or stupor.
- Negative Symptoms (Reduction or loss of normal functions):
- Affective Flattening: Reduced emotional expression.
- Alogia: Decreased speech output.
- Avolition: Lack of motivation or initiative.
- Anhedonia: Loss of interest or pleasure in activities.
- Social Withdrawal: Detachment from social interactions.
- Cognitive Symptoms:
- Impaired Attention: Difficulty focusing or sustaining attention.
- Memory Deficits: Impaired working memory.
- Executive Dysfunction: Trouble planning, organizing, and abstract thinking.
- Affective Symptoms:
- Depressed Mood: Often present in the early stages or during episodes of relapse.
- Suicidal Thoughts: Due to the distress caused by the disorder.
Psychopathology of Schizophrenia
Schizophrenia involves complex alterations in brain function and structure. Key aspects of its psychopathology include:
- Neurobiological Factors:
- Dopamine Hypothesis: Schizophrenia is associated with an overactivity of dopamine in certain brain regions (positive symptoms) and underactivity in other regions (negative symptoms).
- Glutamate Hypothesis: A dysfunction in the glutamatergic system, particularly the NMDA receptor, has been implicated in cognitive deficits.
- Structural Abnormalities: Enlarged lateral ventricles, reduced gray matter, and abnormalities in the prefrontal cortex and hippocampus are often observed.
- Genetic Factors:
- A strong genetic component is associated with schizophrenia, with multiple genes contributing to the risk of developing the disorder.
- Environmental Factors:
- Prenatal Stress: Infections, malnutrition, or stress during pregnancy can increase the risk.
- Early Trauma: Childhood trauma, urban upbringing, and social stressors may contribute to vulnerability.
- Psychosocial Factors:
- Stressful life events, substance abuse (particularly cannabis), and social isolation can precipitate or exacerbate symptoms.
- Cognitive Dysfunction:
- Schizophrenia is associated with impairments in cognitive functioning, including attention, memory, and executive function, which are related to the underlying neural disturbances in the prefrontal cortex.
- Emotional Dysregulation:
- Patients often show abnormalities in emotional processing and response, potentially linked to disruptions in brain regions like the amygdala and the ventral striatum.
(c) Explain in detail about management of the patient with schizophrenia.
Management of Schizophrenia
Managing schizophrenia is complex and involves a combination of pharmacological treatments, psychotherapy, social interventions, and long-term follow-up. The goal of treatment is to reduce the severity of symptoms, improve functioning, and prevent relapse. A multidisciplinary approach is essential for optimal management.
1. Pharmacological Treatment
Medications, particularly antipsychotics, are the cornerstone of schizophrenia management. They are essential for controlling positive symptoms (e.g., delusions, hallucinations), and some newer drugs may also help with negative and cognitive symptoms.
a. Antipsychotic Medications
- First-generation (typical) antipsychotics: These include drugs like haloperidol, chlorpromazine, and fluphenazine. They primarily act by blocking dopamine D2 receptors.
- Benefits: Effective at reducing positive symptoms.
- Side effects: Can cause extrapyramidal symptoms (EPS), such as tremors, rigidity, bradykinesia, and tardive dyskinesia. Other side effects include sedation, dry mouth, and weight gain.
- Second-generation (atypical) antipsychotics: These include risperidone, olanzapine, quetiapine, aripiprazole, and clozapine.
- Benefits: Effective in treating both positive and negative symptoms, and cause fewer extrapyramidal symptoms compared to typical antipsychotics.
- Side effects: Risk of metabolic syndrome (weight gain, diabetes, dyslipidemia), sedation, and orthostatic hypotension. Clozapine is particularly useful in treatment-resistant schizophrenia but requires regular monitoring for agranulocytosis (a severe drop in white blood cells).
b. Other Medications
- Mood stabilizers (e.g., lithium, valproate): Used if there are mood disturbances such as mania or depression.
- Antidepressants (e.g., SSRIs): May be added for treating comorbid depression.
- Benzodiazepines (e.g., lorazepam): Sometimes used to reduce agitation and anxiety, especially in the acute phase.
c. Long-acting Injectable Antipsychotics (LAIs)
- For patients who struggle with medication adherence, long-acting injectable antipsychotics (e.g., fluphenazine decanoate, risperidone LAI) are beneficial, as they only need to be administered once every 2-4 weeks.
2. Psychotherapy
Psychotherapy, when combined with medication, plays a critical role in improving insight, coping strategies, and adherence to treatment. Common types include:
a. Cognitive Behavioral Therapy (CBT)
- Focuses on changing distorted thinking patterns and behaviors. Helps patients recognize delusional thinking and develop more realistic interpretations of situations.
b. Family Therapy
- Schizophrenia significantly affects the patient’s family. Family therapy aims to improve communication, reduce stress, and educate the family about the illness, thereby creating a supportive home environment.
c. Cognitive Remediation Therapy
- Targets cognitive deficits such as attention, memory, and executive function, helping patients improve their ability to function in daily life.
d. Psychoeducation
- Educates the patient and family about schizophrenia, medication adherence, coping strategies, and early warning signs of relapse.
3. Psychosocial Interventions
Psychosocial treatments are crucial in helping patients integrate into society and improve their quality of life.
a. Social Skills Training
- Focuses on improving interpersonal communication, daily living skills, and social interactions. This helps the patient maintain personal relationships and engage in community activities.
b. Vocational Rehabilitation
- Assists the patient in gaining and maintaining employment, which can provide structure, purpose, and financial independence.
c. Supported Employment Programs
- These programs help individuals with schizophrenia find jobs that suit their abilities and provide on-the-job support.
d. Assertive Community Treatment (ACT)
- A comprehensive, community-based treatment model where a team of mental health professionals provides personalized care. The team might include psychiatrists, social workers, nurses, and vocational therapists.
e. Housing Support
- Stable housing is essential. Supported housing programs offer residential environments where patients can live independently with access to mental health care.
4. Hospitalization
In cases of acute psychotic episodes or when there is a risk of harm to self or others, inpatient hospitalization may be required. This allows for intensive treatment, stabilization with medications, and protection in a safe environment.
a. Indications for Hospitalization
- Acute psychosis with severe delusions or hallucinations.
- Suicidal or homicidal ideation.
- Severe aggression or agitation.
- Inability to care for basic needs, such as eating or personal hygiene.
- Medication non-adherence leading to relapse.
b. Inpatient Treatment Goals
- Stabilizing acute symptoms through medication adjustments.
- Providing a safe and structured environment.
- Developing a long-term care plan and reintroducing outpatient services post-discharge.
5. Relapse Prevention and Long-term Management
Schizophrenia is often a lifelong condition, so continuous management is essential to prevent relapses and maintain quality of life.
a. Medication Adherence
- Ensuring adherence to prescribed medications is key to relapse prevention. LAIs may be useful for patients with a history of non-adherence.
b. Regular Psychiatric Follow-up
- Routine appointments with a psychiatrist or mental health team for medication management and to monitor for early signs of relapse.
c. Early Warning Signs of Relapse
- The patient and their family should be educated about recognizing early warning signs such as increased agitation, social withdrawal, or disturbances in thought patterns. Early intervention can prevent a full-blown relapse.
d. Smoking Cessation and Substance Abuse Counseling
- Smoking and substance abuse are more common in schizophrenia patients and can interfere with treatment. Counseling and support are crucial for addressing these issues.
6. Management of Comorbid Conditions
Many patients with schizophrenia have comorbid physical or mental health conditions (e.g., diabetes, hypertension, depression). Treating these conditions is crucial for improving overall health outcomes.
7. Self-care and Wellness Strategies
- Encouraging a healthy lifestyle, including regular exercise, a balanced diet, and adequate sleep, can help manage stress and improve overall well-being.
8. Legal and Ethical Considerations
- Involuntary Commitment: In some cases, patients may need to be involuntarily hospitalized if they pose a risk to themselves or others. This requires careful consideration of patient rights and legal procedures.
- Guardianship: In severe cases where the patient cannot make informed decisions, legal guardianship may be necessary to manage their care and financial decisions.
OR
(2) (a) Define electro convulsive therapy
Electroconvulsive Therapy (ECT) is a medical treatment in which controlled electrical currents are passed through the brain to intentionally trigger a brief seizure. This procedure is primarily used to treat severe mental health conditions, such as major depression, schizophrenia, and bipolar disorder, especially when other treatments like medications and psychotherapy have not been effective. ECT is performed under general anesthesia and is considered safe, with modern techniques minimizing side effects. It works by altering brain chemistry, potentially providing rapid relief from severe symptoms.
(b) Explain about types, parameters, indications, contraindication, side effects, and ECT team.
Electroconvulsive Therapy (ECT): Types, Parameters, Indications, Contraindications, Side Effects, and ECT Team
Types of Electroconvulsive Therapy (ECT)
- Bilateral ECT:
- Electrodes are placed on both sides of the head, targeting both hemispheres of the brain.
- It is more effective for severe mental health conditions but has a higher risk of cognitive side effects, such as memory loss.
- Unilateral ECT:
- Electrodes are placed on one side of the head (typically the non-dominant hemisphere).
- It has fewer cognitive side effects compared to bilateral ECT but may be less effective in some patients.
- Brief-Pulse ECT:
- Involves delivering short electrical pulses to the brain.
- This is the most commonly used type in modern ECT due to its lower risk of cognitive side effects.
- Ultra-brief Pulse ECT:
- Uses an extremely short pulse duration, reducing the cognitive side effects further.
- It is considered less effective than standard brief-pulse ECT but is used in certain patient populations to minimize memory impairment.
Parameters of ECT
- Electrical Stimulus:
- The stimulus is typically in the range of 70-120 volts, and the duration can vary between 0.5 to 2 seconds, depending on the type of pulse used.
- Pulse Width:
- Modern machines typically use pulse widths of 0.5-1.5 milliseconds. Ultra-brief pulse widths are generally 0.3 milliseconds.
- Frequency:
- The frequency of ECT sessions is generally 2-3 times per week.
- The number of sessions varies depending on the condition but generally ranges from 6 to 12 treatments.
- Seizure Duration:
- The goal is to induce a seizure that lasts 20-60 seconds. Seizures shorter than 15 seconds are usually considered inadequate, and adjustments to parameters may be made.
Indications for ECT
ECT is used primarily when other treatments have been ineffective or when rapid response is necessary. Indications include:
- Major Depressive Disorder:
- Especially in cases with severe depression, psychotic features, suicidal tendencies, or when medications are ineffective or contraindicated.
- Bipolar Disorder:
- Used for severe manic or depressive episodes, especially when medications or psychotherapy are not effective.
- Schizophrenia:
- Primarily in cases with catatonia, treatment-resistant schizophrenia, or when rapid improvement is required.
- Catatonia:
- ECT is considered highly effective for treating catatonic states associated with various psychiatric or medical conditions.
- Suicidal Behavior:
- When rapid symptom control is essential, ECT can be lifesaving by reducing suicidal ideation.
- Parkinson’s Disease:
- In some cases, ECT is used to treat severe depression associated with Parkinson’s or as a symptomatic treatment for Parkinsonian symptoms.
- Neuroleptic Malignant Syndrome:
- ECT is sometimes used to treat this life-threatening condition associated with antipsychotic medications.
Contraindications of ECT
While ECT is generally safe, some conditions warrant caution or avoidance. Contraindications include:
- Absolute Contraindications:
- Increased Intracranial Pressure (ICP): ECT can exacerbate this condition due to elevated cerebral blood flow.
- Recent Myocardial Infarction (Heart Attack): ECT can stress the cardiovascular system, increasing the risk of complications.
- Relative Contraindications:
- Severe Cardiovascular Disease: Patients with unstable angina, arrhythmias, or congestive heart failure require careful monitoring.
- Aneurysms: Cerebral or aortic aneurysms may increase the risk of rupture during the seizure.
- Severe Respiratory Disease: Patients with conditions such as severe COPD need special attention during anesthesia.
- Osteoporosis or Fragile Bones: The convulsions induced by ECT can increase the risk of fractures in vulnerable patients.
Side Effects of ECT
- Short-term Side Effects:
- Headache: Common after ECT sessions, usually mild and treatable with over-the-counter pain relievers.
- Nausea: Can occur due to the anesthesia used during the procedure.
- Muscle Soreness: Mild muscle aches due to the induced seizure are common but typically short-lived.
- Confusion: Patients may experience confusion immediately after the procedure, especially older individuals.
- Memory Loss: Short-term memory loss is common, particularly with bilateral ECT. Anterograde (new memories) and retrograde (past memories) amnesia can occur, but memory generally returns within weeks to months.
- Long-term Side Effects:
- Cognitive Impairment: Long-term cognitive deficits, particularly memory problems, can persist in some patients, especially with frequent bilateral ECT.
The ECT Team
ECT is performed by a specialized team of professionals to ensure safety and effectiveness. The team typically consists of:
- Psychiatrist:
- Oversees the treatment, decides on the ECT protocol, adjusts parameters, and monitors the patient’s mental health response to the treatment.
- Anesthesiologist:
- Administers general anesthesia and ensures the patient is unconscious and pain-free during the procedure. They also monitor the patient’s vitals (blood pressure, heart rate, oxygen saturation) throughout the treatment.
- Nurse:
- Assists the team in preparing the patient, administering medications, and monitoring the patient before, during, and after the procedure. The nurse also ensures the patient’s comfort and safety post-procedure.
- Electroencephalogram (EEG) Technician:
- Monitors brain activity and ensures that a therapeutic seizure has occurred. EEG technicians also assist in adjusting the ECT machine settings as required.
- Support Staff:
- Often include psychiatric social workers and other support personnel who assist in patient care, provide psychoeducation, and offer post-treatment support.
(c) Nurses role in ECT.
Nurses’ Role in Electroconvulsive Therapy (ECT)
Nurses play a crucial role in the safe and effective administration of Electroconvulsive Therapy (ECT), ensuring that patients are prepared, monitored, and cared for before, during, and after the procedure. The nurse’s role encompasses several responsibilities, including patient education, preparation, observation, and post-procedure care.
1. Pre-ECT Responsibilities
a. Patient Education and Preparation
- Explanation of Procedure: The nurse educates the patient and their family about the ECT process, explaining its purpose, how it works, potential side effects, and the expected outcomes to alleviate anxiety and foster cooperation.
- Consent Process: Ensure that informed consent has been obtained by the psychiatrist or physician. The nurse ensures the patient understands the procedure and clarifies any doubts.
- Pre-ECT Fasting: The patient is instructed to fast for about 6-8 hours before the procedure to prevent aspiration during anesthesia.
- Pre-procedure Checklist: Verify that all pre-ECT investigations (e.g., ECG, chest X-ray, electrolyte levels) have been completed and are within normal limits.
- Removal of Personal Items: Ensure the patient removes dentures, jewelry, contact lenses, hearing aids, and other prosthetics before the procedure.
- Vital Signs Monitoring: Take and record baseline vital signs (blood pressure, heart rate, respiratory rate, oxygen saturation) to ensure the patient is medically stable for the procedure.
b. Emotional Support
- Addressing Anxiety: Many patients may feel anxious before the procedure. The nurse provides reassurance, emotional support, and encouragement to reduce anxiety and create a calming environment.
c. Medication Administration
- Pre-medications: The nurse administers pre-ECT medications as prescribed, such as:
- Anticholinergic agents (e.g., atropine) to reduce secretions and prevent bradycardia.
- Muscle relaxants (e.g., succinylcholine) to minimize the risk of injury due to muscle contractions during the seizure.
- Sedatives or anxiolytics (if ordered) to ease patient anxiety before the anesthesia is administered.
2. Intra-ECT Responsibilities
a. Assisting the ECT Team
- Assisting the Anesthesiologist: Help administer general anesthesia, ensuring the patient is properly sedated before the ECT stimulus is given.
- Positioning the Patient: Ensure the patient is properly positioned on the treatment table, typically in the supine position with the head slightly elevated.
- Monitoring Vital Signs: Continuously monitor and document vital signs, including blood pressure, heart rate, oxygen saturation, and respiratory rate, throughout the procedure.
b. Safety and Comfort
- Protecting the Patient: Ensure that safety measures are in place, such as placing a bite block in the patient’s mouth to prevent injury to the teeth and tongue during the seizure.
- Observing the Seizure: Assist in monitoring the seizure duration and ensuring that it is within the therapeutic range (typically 20-60 seconds).
c. Documentation
- The nurse records key observations during the procedure, including:
- The time and duration of the seizure.
- Medications administered.
- Vital signs during the procedure.
- Any adverse reactions or complications.
3. Post-ECT Responsibilities
a. Post-Procedure Care
- Monitoring and Observation: Once the procedure is complete, the nurse monitors the patient in the recovery area until they regain consciousness and are stable.
- Monitor vital signs regularly (every 15 minutes until stable).
- Assess the level of consciousness, neurological status, and cognitive function.
- Check for any signs of post-ECT complications, such as prolonged confusion, agitation, or nausea.
b. Reorientation and Emotional Support
- Reorienting the Patient: Many patients may feel confused or disoriented upon waking up from anesthesia. The nurse reassures and orients the patient by reminding them of the time, place, and reason for the procedure.
- Providing Comfort: Address any discomfort the patient may experience, such as headache or muscle soreness, by administering prescribed analgesics or applying cold compresses.
c. Ensuring Safety
- Fall Prevention: The nurse ensures that the patient is safe and secure in the post-ECT recovery area, particularly if they are confused or disoriented, to prevent falls or injuries.
d. Emotional and Psychological Support
- Assessing the Patient’s Emotional State: Provide continued emotional support and answer any questions the patient or family may have about how the procedure went.
4. Discharge and Follow-up Care
a. Preparing for Discharge
- Ensuring Stability: The nurse ensures that the patient is fully awake, stable, and coherent before discharge. The patient must be able to walk, talk, and eat without difficulty.
- Family Education: Educate the family or caregiver about post-ECT care, including potential short-term side effects (e.g., headache, memory loss) and instructions on what to do in case of emergencies (e.g., confusion or prolonged disorientation).
b. Follow-up Instructions
- Medication Adherence: Reinforce the importance of continuing prescribed medications as part of the overall treatment plan.
- Appointment Scheduling: Ensure the patient has scheduled follow-up appointments for continued care and monitoring.
5. Managing Complications
If complications arise during or after ECT, the nurse should be prepared to:
- Manage Seizures: In case of prolonged seizures, the nurse may assist the medical team in administering anticonvulsants as prescribed.
- Treat Cardiovascular Complications: Be vigilant for signs of cardiac irregularities, such as arrhythmias or hypotension, and ensure immediate medical intervention if needed.
- Handle Respiratory Issues: Be prepared to assist in managing airway and breathing difficulties, particularly in patients with respiratory compromise.
6. Ongoing Support and Documentation
- Documentation: The nurse thoroughly documents all aspects of care before, during, and after ECT, including medications given, vital signs, seizure duration, patient’s response, and any side effects.
- Psychoeducation: The nurse continues to educate the patient and family about the treatment process and its long-term management.
2 Short notes: (any three) 3×5-15
1.District mental health programme.
District Mental Health Programme (DMHP) in India
The District Mental Health Programme (DMHP) is an initiative under the National Mental Health Programme (NMHP) of India, launched by the Ministry of Health and Family Welfare in 1982. The objective of the DMHP is to integrate mental health services into the primary healthcare system and make mental health care accessible at the community level.
Objectives of DMHP
- Provide Mental Health Services at the District Level:
- Establish mental health services in district hospitals, community health centers (CHCs), and primary health centers (PHCs).
- Make basic mental healthcare accessible to the population, especially in underserved areas.
- Reduce the Burden of Mental Disorders:
- Identify, diagnose, and treat common mental health disorders, such as depression, anxiety, schizophrenia, and bipolar disorder, at early stages.
- Provide outpatient and inpatient services for people with mental illness.
- Promote Mental Health Awareness:
- Conduct awareness and education programs to reduce stigma around mental illness and promote understanding of mental health issues in the community.
- Training of General Healthcare Workers:
- Train medical officers, healthcare workers, and community workers to recognize and treat mental health conditions at the grassroots level.
- Equip healthcare workers to identify mental health issues early and refer complex cases to specialized services.
- Ensure Continuity of Care:
- Provide follow-up services, rehabilitation, and support for patients with chronic mental illnesses.
- Collaborate with NGOs, rehabilitation centers, and families for long-term care and reintegration of patients into society.
Key Components of DMHP
- Mental Health Services:
- Outpatient Services: Offering consultation and treatment for common psychiatric disorders.
- Inpatient Services: Providing hospitalization for acute psychiatric cases.
- Referral Services: Referring complex cases to specialized psychiatric centers.
- Rehabilitation Services: Focusing on the rehabilitation of people with mental illnesses through therapy, vocational training, and community-based rehabilitation.
- Training of Human Resources:
- Training of Medical Officers and Healthcare Workers: Enhancing the skills of general practitioners and healthcare workers at PHCs and CHCs to diagnose and treat basic mental health conditions.
- Sensitization of Teachers, Police Personnel, and Others: Training various stakeholders to recognize and manage mental health issues in the community.
- IEC (Information, Education, and Communication) Activities:
- Public Awareness Campaigns: Increasing awareness about mental health, reducing stigma, and encouraging early treatment-seeking behavior.
- School Mental Health Programs: Promoting mental health awareness in schools and addressing issues like childhood depression, bullying, and substance abuse.
- Monitoring and Evaluation:
- A system for ongoing monitoring and evaluation to ensure that mental health services are effectively delivered and the programme is achieving its objectives.
- Support for Severe Mental Disorders:
- Providing specialized services for patients with severe mental illnesses, such as schizophrenia, bipolar disorder, and psychosis.
- Collaboration with NGOs and Other Sectors:
- Partnering with non-governmental organizations (NGOs) and other sectors to provide comprehensive care, rehabilitation, and mental health promotion in the community.
Challenges Faced by DMHP
- Human Resource Shortages:
- Lack of trained mental health professionals, such as psychiatrists, psychologists, and psychiatric social workers at the district level.
- Stigma and Awareness:
- Widespread stigma surrounding mental health issues prevents individuals from seeking help.
- Low awareness of mental health services available under DMHP, especially in rural areas.
- Resource Allocation:
- Limited financial and infrastructural resources for mental health services in many districts.
- Limited Integration into Primary Health Care:
- Full integration of mental health services into primary care settings has been slow due to the lack of training and infrastructure at the grassroots level.
Recent Initiatives and Progress
- Manodarpan:
- A program initiated during the COVID-19 pandemic to address the mental health challenges faced by students, offering psychological support and counseling services.
- Expansion of Tele-Mental Health Services:
- Introduction of telemedicine and digital mental health services to improve access to mental healthcare, especially in remote areas.
- National Mental Health Policy (2014):
- Strengthening mental health services across all levels, with a particular focus on rural and underdeveloped districts.
(2) Anorexia nervosa
Anorexia Nervosa
Anorexia Nervosa is a serious and potentially life-threatening eating disorder characterized by self-imposed starvation and excessive weight loss. Individuals with anorexia nervosa have an intense fear of gaining weight and a distorted body image, leading them to restrict their food intake, engage in extreme dieting, and sometimes excessive exercise. Despite being underweight, they may perceive themselves as overweight.
Key Features of Anorexia Nervosa
- Restrictive Eating:
- Patients severely limit their food intake to control their weight. They often avoid high-calorie foods and may follow extreme dieting patterns.
- Intense Fear of Gaining Weight:
- Even though they are underweight, individuals with anorexia nervosa are terrified of gaining weight or becoming fat, and this fear drives their behaviors.
- Distorted Body Image:
- Patients have a distorted perception of their body size and shape. They may see themselves as overweight, even when they are dangerously underweight.
- Low Body Weight:
- Weight is significantly below the normal range for age, sex, and physical health status.
Types of Anorexia Nervosa
- Restricting Type:
- Individuals with this type reduce their caloric intake drastically, engaging in restrictive dieting and excessive fasting to lose weight.
- Binge-eating/Purging Type:
- Individuals with this type may engage in episodes of binge eating followed by purging behaviors, such as self-induced vomiting, misuse of laxatives, diuretics, or excessive exercise.
Clinical Features
- Physical Signs:
- Extreme weight loss.
- Thin appearance.
- Fatigue and weakness.
- Dizziness or fainting.
- Brittle hair and nails.
- Dry, yellowish skin.
- Lanugo (fine hair growth on the body).
- Amenorrhea (absence of menstruation in females).
- Cold intolerance due to low body fat.
- Low blood pressure, slow heart rate (bradycardia).
- Psychological and Behavioral Signs:
- Preoccupation with food, dieting, and body weight.
- Refusal to maintain a normal body weight.
- Social withdrawal and isolation.
- Irritability and mood swings.
- Obsessive rituals around food (e.g., cutting food into tiny pieces).
- Denial of the seriousness of low body weight.
- Excessive exercise.
Complications
- Malnutrition: Leads to weakened immune system and poor wound healing.
- Cardiovascular issues: Bradycardia, hypotension, arrhythmias, heart failure.
- Bone problems: Osteoporosis or osteopenia due to reduced calcium and vitamin D.
- Fertility issues: Amenorrhea and infertility.
- Electrolyte Imbalance: Especially in the binge-purge subtype, which can cause life-threatening heart issues.
- Mental health issues: Depression, anxiety, and a high risk of suicide.
Causes and Risk Factors
- Genetic Factors: A family history of eating disorders, depression, or anxiety can increase the risk.
- Psychological Factors: Perfectionism, obsessive-compulsive tendencies, low self-esteem, and a need for control may contribute.
- Cultural and Social Factors: Societal pressure to be thin, media influence, and cultural norms related to beauty can trigger the development of anorexia.
- Environmental Factors: Traumatic events, such as bullying or abuse, or involvement in professions or activities that emphasize thinness (e.g., modeling, athletics).
Diagnosis
Anorexia nervosa is typically diagnosed through clinical evaluation and meeting specific criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which includes:
- Restriction of Energy Intake: Leading to significantly low body weight.
- Intense Fear of Gaining Weight: Or becoming fat, despite being underweight.
- Distorted Body Image: Distorted perception of body weight or shape, or denial of the seriousness of low body weight.
Management and Treatment
The management of anorexia nervosa is multidisciplinary, involving medical doctors, mental health professionals, dietitians, and sometimes social workers.
- Medical Treatment:
- Nutritional Rehabilitation: Restoring the patient’s nutritional health and achieving a healthy weight is the primary focus. This may require hospitalization in severe cases to monitor vital signs and stabilize physical health.
- Monitoring for Complications: Regular monitoring for cardiovascular issues, electrolyte imbalances, and other complications is essential.
- Medications: While no medications specifically target anorexia nervosa, antidepressants or anti-anxiety medications may be prescribed to address associated mental health conditions.
- Psychotherapy:
- Cognitive Behavioral Therapy (CBT): A common therapeutic approach that helps patients address distorted thoughts related to body image, eating, and weight, and develop healthier attitudes and behaviors around food.
- Family-Based Therapy (FBT): Especially useful for adolescents, this approach involves family members in the recovery process to help support and encourage healthy eating behaviors.
- Interpersonal Therapy (IPT): Focuses on improving interpersonal relationships and emotional regulation, addressing underlying social and emotional triggers.
- Nutritional Counseling:
- Dietitians play a key role in helping patients understand the importance of balanced nutrition and guide them in healthy meal planning, portion control, and overcoming food-related fears.
- Hospitalization:
- In cases of severe malnutrition, dehydration, or when the patient is at risk of suicide, hospitalization may be required. Inpatient or outpatient treatment programs provide intensive monitoring and structured meals to help the patient recover.
Prognosis
- Anorexia nervosa is a chronic condition with a high rate of relapse. Early diagnosis and intervention significantly improve the prognosis.
- Long-term follow-up is essential to ensure continued recovery, monitor for relapses, and support the patient in maintaining a healthy lifestyle.
- Recovery can take months or years, and relapses are common, so ongoing psychological and medical support is often needed.
(3) Lithium
Lithium: Overview, Uses, Mechanism, Side Effects, and Nursing Considerations
Lithium is a mood stabilizer commonly used to treat psychiatric conditions, particularly bipolar disorder. It is considered the gold standard treatment for managing the manic and depressive episodes associated with bipolar disorder. Lithium is also sometimes used for schizoaffective disorder and to augment antidepressant treatment in major depressive disorder.
Uses of Lithium
- Bipolar Disorder:
- Lithium is primarily used to control acute mania, hypomania, and to prevent manic and depressive episodes in bipolar disorder.
- Schizoaffective Disorder:
- In combination with antipsychotic medications, lithium helps stabilize mood in patients with schizoaffective disorder.
- Augmentation Therapy in Depression:
- Lithium is sometimes used to augment the effects of antidepressants in treatment-resistant depression.
- Suicide Prevention:
- Lithium has been shown to reduce suicidal ideation and behavior in patients with mood disorders, making it a valuable part of long-term treatment.
Mechanism of Action
The exact mechanism by which lithium works is not completely understood, but it is believed to act through several pathways, including:
- Modulation of Neurotransmitters:
- Lithium alters the balance of neurotransmitters such as dopamine, serotonin, and norepinephrine, which play a role in mood regulation.
- Effects on Signal Transduction:
- Lithium inhibits the enzyme inositol monophosphatase, leading to reduced availability of inositol, which impacts second messenger systems involved in neurotransmission.
- It also stabilizes excitatory and inhibitory neurotransmitter release, helping to balance mood swings.
- Neuroprotective Effects:
- Lithium has been shown to promote neurogenesis (formation of new neurons) and prevent neurodegeneration, potentially reducing the cognitive decline associated with mood disorders.
Therapeutic Range
- The therapeutic serum concentration of lithium is 0.6 to 1.2 mEq/L for maintenance treatment and 0.8 to 1.5 mEq/L for acute mania. Regular monitoring of blood levels is required due to its narrow therapeutic window.
Side Effects of Lithium
Common Side Effects
- Gastrointestinal Issues:
- Nausea, vomiting, diarrhea, and abdominal pain.
- Tremors:
- Fine hand tremors are common, especially early in treatment.
- Increased Thirst and Urination (Polyuria):
- Lithium can cause excessive thirst and frequent urination (diabetes insipidus), requiring increased water intake.
- Weight Gain:
- Some patients experience weight gain while on lithium therapy.
- Cognitive Issues:
- Mild cognitive difficulties, such as memory problems and decreased concentration, may occur.
- Hypothyroidism:
- Long-term use of lithium can interfere with thyroid function, leading to hypothyroidism in some patients.
- Skin Conditions:
- Acne, psoriasis, and other skin rashes can be exacerbated by lithium.
Serious Side Effects
- Lithium Toxicity:
- Lithium toxicity occurs when lithium levels exceed the therapeutic range. Symptoms of toxicity include:
- Severe nausea and vomiting.
- Coarse tremors.
- Confusion, drowsiness, and slurred speech.
- Ataxia (impaired coordination), seizures, and coma.
- Lithium toxicity is a medical emergency and requires immediate treatment, typically with IV fluids to enhance excretion.
- Kidney Dysfunction:
- Chronic use of lithium can lead to nephrogenic diabetes insipidus (a kidney disorder that affects water balance), and long-term use may cause kidney damage. Regular monitoring of kidney function is required.
- Cardiac Arrhythmias:
- Lithium can cause changes in heart rhythm, especially in patients with pre-existing cardiac conditions.
- Hypercalcemia:
- Lithium can increase calcium levels in the blood, potentially causing hypercalcemia.
Contraindications and Precautions
- Pregnancy and Breastfeeding:
- Lithium should be used with caution in pregnancy, especially during the first trimester, as it is associated with an increased risk of congenital malformations, particularly Ebstein’s anomaly (a heart defect). Lithium can also pass into breast milk and affect the infant.
- Kidney Disease:
- Since lithium is excreted by the kidneys, individuals with kidney disease should avoid lithium, or its use should be carefully monitored.
- Cardiovascular Disease:
- Lithium can cause arrhythmias, so it must be used cautiously in patients with heart conditions.
- Sodium Depletion:
- Patients on low-sodium diets or those taking diuretics are at increased risk of lithium toxicity, as lithium levels can rise when sodium levels decrease.
- Drug Interactions:
- Certain medications, such as NSAIDs, ACE inhibitors, diuretics, and antipsychotics, can increase lithium levels and the risk of toxicity. These interactions need careful management.
Nursing Considerations for Lithium
- Monitoring Serum Lithium Levels:
- Regular blood tests are necessary to ensure that lithium levels remain within the therapeutic range (0.6–1.2 mEq/L). Blood samples should be taken 12 hours after the last dose of lithium.
- Monitoring Renal and Thyroid Function:
- Regular assessment of kidney function (serum creatinine and electrolyte levels) and thyroid function (TSH levels) should be conducted to detect early signs of nephrotoxicity and hypothyroidism.
- Educating the Patient:
- Instruct patients to maintain adequate fluid and sodium intake, as dehydration and sodium loss can increase lithium levels and cause toxicity.
- Teach patients about the symptoms of lithium toxicity (e.g., severe tremor, confusion, vomiting) and the importance of reporting them immediately.
- Inform patients about potential side effects, including weight gain, tremors, and increased urination.
- Monitoring for Side Effects:
- Assess for early signs of toxicity such as confusion, tremors, and gastrointestinal disturbances.
- Monitor for symptoms of hypothyroidism (e.g., fatigue, weight gain, cold intolerance) and refer the patient for appropriate tests if necessary.
- Compliance and Follow-Up:
- Encourage adherence to prescribed doses, as missing doses or taking too much can lead to severe consequences.
- Ensure regular follow-up appointments for blood monitoring and evaluation of mental health status.
- Managing Drug Interactions:
- Assess the patient’s medication regimen for possible drug interactions that could alter lithium levels, especially with NSAIDs, diuretics, and antihypertensive medications.
- Safe Medication Administration:
- Administer lithium with food or milk to reduce gastrointestinal irritation.
- Avoid abrupt discontinuation, as it can lead to relapse of manic or depressive episodes.
4) Process recording
A process recording is a detailed account of interactions between a nurse (or other health care professionals) and a patient during the care process. It is typically used in nursing education to help students reflect on their communication skills, understand patient interactions, and improve therapeutic techniques. The process recording serves as a learning tool to analyze communication and emotional dynamics in a clinical setting.
Key Components of a Process Recording:
- Patient Information:
- Patient initials or ID number (to maintain confidentiality)
- Age, gender, diagnosis, and other relevant background information
- Setting:
- Description of the location and context where the interaction took place (e.g., hospital room, clinic, community setting)
- Date and time of the interaction
- Purpose of Interaction:
- The reason for the interaction (e.g., assessing patient needs, providing education, or supporting the patient emotionally)
- Verbatim Dialogue:
- Exact words spoken by both the nurse and the patient during the interaction
- The verbatim dialogue helps capture the actual communication dynamics
- Nurse’s Thoughts and Feelings:
- The nurse’s internal thoughts, feelings, and reactions during the interaction
- This part reflects the emotional responses and clinical reasoning at various points
- Analysis of Communication Techniques:
- Review and analysis of the types of communication techniques used (e.g., therapeutic techniques like active listening, open-ended questions, or non-verbal cues)
- Evaluation of whether the communication was effective or ineffective in promoting understanding, trust, or therapeutic goals
- Patient’s Response:
- Patient’s verbal and non-verbal responses to the nurse’s actions
- Any changes in the patient’s mood, behavior, or condition during the interaction
- Evaluation of the Interaction:
- Reflection on how the interaction went, what went well, and areas that could be improved
- Analysis of the therapeutic relationship and patient outcomes based on the communication
- Follow-up or Next Steps:
- What further actions need to be taken following the interaction (e.g., scheduling another session, adjusting treatment plan, providing further education)
- Any planned follow-up based on the interaction’s outcome
Example Format of a Process Recording:
| Time | Nurse’s Dialogue/Actions | Patient’s Dialogue/Actions | Nurse’s Thoughts/Feelings | Analysis (Techniques) |
|---|---|---|---|---|
| 10:00 AM | “How are you feeling today?” | “I am okay, just a bit tired.” | The patient seems calm. | Open-ended question |
| 10:05 AM | “Can you tell me more about your tiredness?” | “I didn’t sleep well last night because of the pain.” | I wonder if the pain is from their condition or due to stress. | Exploring patient feelings |
| 10:10 AM | “Would you like some pain relief?” | “Yes, that would help, I think.” | I should check if pain medication is due. | Offering choices to promote autonomy |
Process recording encourages self-awareness, critical thinking, and reflection in nurses, allowing them to continuously improve their therapeutic communication skills.
Would you like to discuss a specific example or need further details?
5)Phobic anxiety disorder
Phobic Anxiety Disorder is a type of anxiety disorder characterized by an excessive, irrational fear of specific objects, situations, or activities that typically pose little or no real danger. Individuals with this disorder recognize their fears as irrational but feel powerless to control or stop them. Phobic anxiety can significantly impair a person’s daily functioning and quality of life.
Types of Phobic Anxiety Disorders:
- Specific Phobia:
- Intense fear of a specific object or situation (e.g., heights, spiders, flying).
- Common subtypes include:
- Animal Type: Fear of animals or insects (e.g., dogs, snakes, spiders).
- Natural Environment Type: Fear of natural phenomena (e.g., heights, storms, water).
- Blood-Injection-Injury Type: Fear of blood, injections, or injury.
- Situational Type: Fear of specific situations (e.g., flying, elevators, enclosed spaces).
- Other Type: Fear of choking, vomiting, or loud sounds.
- Social Phobia (Social Anxiety Disorder):
- Fear of social situations where the person may be embarrassed, judged, or scrutinized by others.
- Common situations include public speaking, meeting new people, or eating in public.
- Social anxiety disorder can severely limit an individual’s ability to work, attend school, or maintain relationships.
- Agoraphobia:
- Fear of being in places or situations where escape may be difficult or help unavailable if anxiety symptoms occur.
- Common fears include open spaces, crowded places, or traveling alone.
- It is often linked with panic disorder, where individuals fear having a panic attack in such situations.
Symptoms of Phobic Anxiety Disorder:
- Emotional Symptoms:
- Intense fear or anxiety triggered by exposure to the phobic stimulus.
- A strong desire to avoid the object or situation causing fear.
- Panic attacks in some cases, with symptoms like rapid heartbeat, sweating, trembling, shortness of breath, and a sense of impending doom.
- Physical Symptoms:
- Increased heart rate and palpitations.
- Sweating and shaking.
- Shortness of breath or choking sensations.
- Dizziness or lightheadedness.
- Gastrointestinal discomfort.
- Behavioral Symptoms:
- Avoidance of the feared object or situation.
- Interference with daily activities or normal functioning.
- Need for reassurance or presence of someone trusted to face the fear.
Causes of Phobic Anxiety Disorder:
- Genetics: Phobic disorders can run in families, suggesting a genetic predisposition to anxiety disorders.
- Environmental Factors: Traumatic experiences, such as being bitten by a dog or being trapped in an elevator, can trigger the development of phobias.
- Learned Behavior: Children may develop phobias by observing anxious behavior in parents or others.
- Biological Factors: Abnormalities in neurotransmitter systems (e.g., serotonin and dopamine) in the brain may contribute to anxiety disorders.
Diagnosis:
- A diagnosis is typically made based on clinical interviews, including detailed history of the individual’s fears, anxiety triggers, and avoidance behaviors.
- Diagnostic criteria are outlined in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders), which guides mental health professionals.
Treatment for Phobic Anxiety Disorder:
- Cognitive Behavioral Therapy (CBT):
- The most effective treatment for phobias.
- Exposure Therapy: A key component of CBT, involves gradual exposure to the feared object or situation in a controlled manner to reduce fear over time.
- Cognitive Restructuring: Helps patients identify and challenge irrational thoughts related to their phobia.
- Medications:
- Antidepressants (SSRIs): Selective serotonin reuptake inhibitors like fluoxetine or sertraline can help reduce anxiety.
- Benzodiazepines: These are used on a short-term basis for immediate relief of anxiety, but they carry the risk of dependency.
- Beta-Blockers: Can reduce physical symptoms like rapid heart rate and trembling in anxiety-provoking situations (e.g., public speaking).
- Relaxation Techniques:
- Practices such as deep breathing, progressive muscle relaxation, and mindfulness can help reduce anxiety symptoms and panic attacks.
- Support Groups:
- Support from others with similar experiences can be beneficial for individuals facing phobic anxiety, offering a sense of community and shared strategies.
Prognosis:
- Phobic anxiety disorders are highly treatable, especially when identified early.
- With appropriate therapy and, if necessary, medication, many individuals can manage or overcome their phobias, allowing them to lead normal, fulfilling lives.
Would you like more information on specific phobias or details on a treatment approach?
3 Short answers: (any four)4×2-8
(1) Dysthymia
Dysthymia, also known as persistent depressive disorder (PDD), is a chronic form of depression characterized by a consistently low mood lasting for at least two years. While the symptoms are less severe than major depression, they are long-lasting and can interfere with daily functioning.
- Depressed mood most of the day, more days than not, for at least 2 years.
- Symptoms include low energy, poor appetite or overeating, insomnia or oversleeping, low self-esteem, and difficulty concentrating.
- Individuals with dysthymia may experience episodes of major depression (double depression).
Treatment:
- Psychotherapy (especially cognitive behavioral therapy)
- Medications, such as antidepressants (SSRIs or SNRIs)
- Lifestyle changes, including regular physical activity and stress management.
Dysthymia tends to be long-term, but with proper treatment, many individuals can manage the symptoms effectively.
(2) Difference between neurosis and psychosis
differentiation between psychosis and neurosis:
Psychosis:
- Definition: Psychosis refers to a severe mental disorder characterized by a loss of contact with reality, often involving hallucinations (perceiving things that aren’t there) and delusions (false beliefs).
- Symptoms: Hallucinations (auditory, visual, tactile, etc.), delusions (paranoid, grandiose, etc.), disorganized thinking, disorganized or catatonic behavior, and negative symptoms such as lack of motivation or emotional expression.
- Types: Psychotic disorders include schizophrenia, schizoaffective disorder, brief psychotic disorder, and substance-induced psychotic disorder.
- Onset: Psychosis typically develops in late adolescence or early adulthood, although it can occur at any age.
- Duration: Psychotic episodes may last for weeks, months, or even years, depending on the underlying cause and treatment effectiveness.
- Reality Distortion: Individuals experiencing psychosis may have a distorted perception of reality and may struggle to differentiate between what is real and what is not.
- Treatment: Treatment often involves antipsychotic medications, psychotherapy (such as cognitive-behavioral therapy), and supportive interventions to help manage symptoms and improve functioning.
Neurosis:
- Definition: Neurosis refers to a milder mental disorder characterized by excessive anxiety, irrational fears, obsessions, compulsions, and other distressing symptoms that interfere with daily functioning but do not involve a loss of contact with reality.
- Symptoms: Symptoms of neurosis include excessive worry, anxiety, phobias, obsessive-compulsive behaviors, somatic symptoms (physical complaints with no underlying medical cause), and difficulties coping with stress.
- Types: Neurotic disorders include generalized anxiety disorder, obsessive-compulsive disorder (OCD), phobias, panic disorder, and somatic symptom disorder.
- Onset: Neurosis can develop at any age, with symptoms often starting in childhood or adolescence and persisting into adulthood.
- Duration: Symptoms of neurosis may be chronic or episodic, depending on the specific disorder and individual factors.
- Reality Contact: Unlike psychosis, individuals with neurosis maintain contact with reality and are aware that their symptoms are irrational or excessive.
- Treatment: Treatment for neurosis typically involves psychotherapy, such as cognitive-behavioral therapy (CBT), exposure therapy, and medication (e.g., antidepressants or anti-anxiety medications) to alleviate symptoms and improve coping skills.
(6) Delusion of persecution
A delusion of persecution is a false, irrational belief that one is being targeted, harassed, or conspired against by others. Individuals with this type of delusion believe that they are being wronged, spied on, or plotted against, even when there is no evidence to support these beliefs. It is commonly associated with psychiatric conditions like schizophrenia and paranoid disorders.
- Persistent belief that one is being persecuted, despite contrary evidence.
- May lead to feelings of fear, mistrust, and hostility.
- Can severely impact the individual’s daily functioning and relationships.
Treatment:
- Antipsychotic medications
- Psychotherapy, especially cognitive behavioral therapy (CBT)
Treatment helps to manage the delusion and improve the individual’s quality of life.
(4) Auditory hallucinations
Auditory hallucinations are perceptions of hearing sounds, typically voices, that are not present in the external environment. These hallucinations are often associated with psychiatric conditions like schizophrenia, but can also occur in mood disorders, substance abuse, and neurological conditions.
- Hearing voices, music, or other sounds when no external source exists.
- The voices may be commanding, critical, or neutral.
- Common in mental health conditions, particularly schizophrenia and severe depression.
Treatment:
- Antipsychotic medications to reduce hallucinations.
- Cognitive-behavioral therapy (CBT) to help patients manage their reactions to hallucinations.
- Addressing underlying causes, such as substance abuse or neurological issues.
Proper diagnosis and treatment can help reduce or eliminate auditory hallucinations.
(5) Dissociative identity disorder
Dissociative Identity Disorder (DID), formerly known as multiple personality disorder, is a mental health condition characterized by the presence of two or more distinct personality states or identities within an individual. These identities may have their own names, behaviors, memories, and ways of interacting with the world.
- Two or more distinct identities or personality states that take control of the individual’s behavior at different times.
- Gaps in memory (amnesia) for everyday events, personal information, or traumatic experiences.
- Often associated with severe childhood trauma or abuse.
Treatment:
- Psychotherapy (long-term therapy focused on integrating the identities and processing trauma)
- Medications (to manage symptoms like depression or anxiety, but no specific medication for DID)
- Supportive care and stress management strategies.
DID is a complex disorder, but with appropriate therapy, individuals can work toward integrating their identities and improving functioning.
(6) Ambivalence
Ambivalence refers to having mixed or conflicting feelings or attitudes about a person, object, or situation. It involves experiencing opposing emotions simultaneously, such as love and hate, or indecision about making a choice. Ambivalence can lead to difficulty in decision-making and internal tension because of the contradictory desires or thoughts.
Example:
- Feeling both excitement and fear about starting a new job.
Ambivalence is common in everyday situations and can be a normal part of emotional experiences. However, if persistent, it may impact decision-making and emotional well-being.
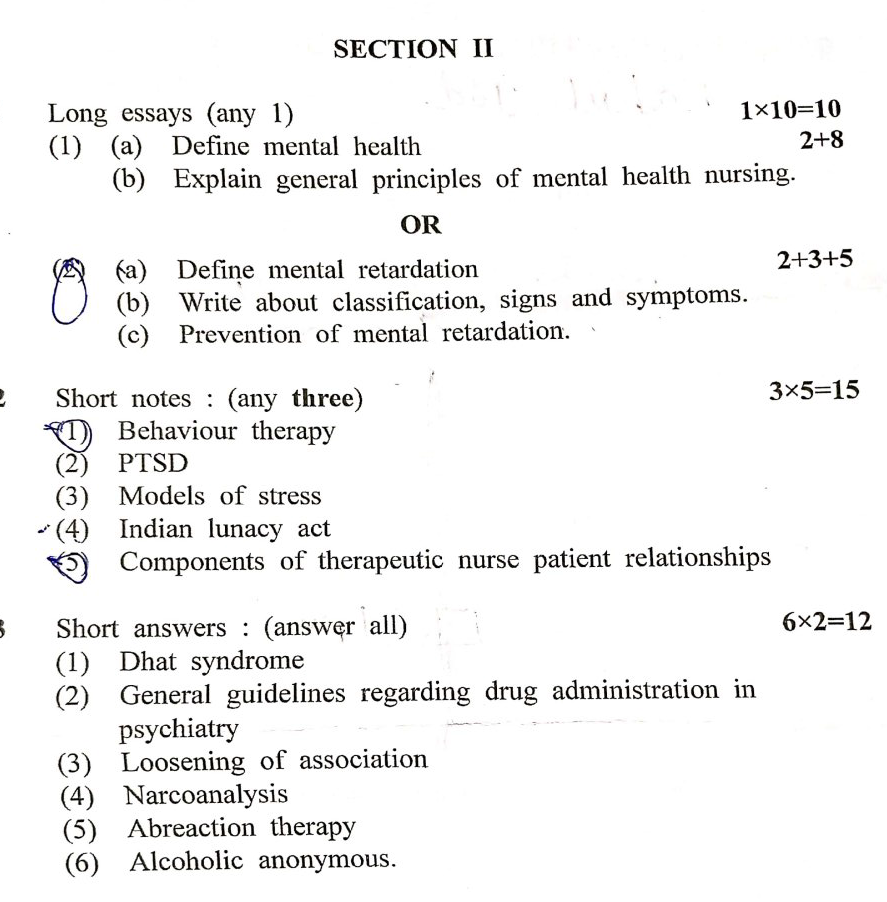
SECTION- II
1.Long essays (any 1) 1×10=10
( 1) (a) Define mental health 2×8
Mental health refers to a state of well-being in which an individual realizes their abilities, can cope with normal life stresses, work productively, and contribute to their community. It encompasses emotional, psychological, and social well-being, influencing how people think, feel, and act. Mental health affects how we handle stress, relate to others, and make choices. Good mental health is not merely the absence of mental illness but also the presence of positive qualities like resilience, emotional regulation, and strong interpersonal relationships.
(b) Explain general principles of mental health nursing.
Mental health nursing is a specialized field of nursing practice that focuses on the care of individuals with mental illnesses or emotional difficulties. The goal is to support patients in their recovery while promoting optimal mental health and well-being. The following are the general principles that guide mental health nursing practice:
1. Individualized Care:
- Patient-Centered Approach: Care must be tailored to the unique needs of each individual, taking into consideration their mental health condition, personality, preferences, culture, and life experiences.
- Holistic Care: Mental health nursing addresses not only the psychological but also the physical, social, and emotional aspects of the patient’s health.
2. Therapeutic Communication:
- Building Trust and Rapport: Establishing a trusting relationship is fundamental. Active listening, empathy, and non-judgmental communication help patients feel valued and understood.
- Open and Supportive Dialogue: Encourage patients to express their thoughts and feelings. Clear communication helps in understanding their condition and identifying treatment needs.
3. Maintaining a Safe Environment:
- Safety First: Ensure the physical and emotional safety of both the patient and healthcare providers. This includes reducing risks of harm (e.g., self-harm, violence, or suicide).
- Therapeutic Milieu: Create a therapeutic environment that supports healing and recovery, such as calming surroundings and routine activities.
4. Respecting Patient Dignity and Rights:
- Respect for Autonomy: Always respect the patient’s autonomy and right to make decisions regarding their treatment, within the limits of their mental capacity.
- Confidentiality: Protect patient information and maintain confidentiality unless there is a risk of harm to the patient or others.
5. Promoting Independence and Empowerment:
- Encouraging Self-Care: Help patients to engage in self-care activities, build self-esteem, and develop coping mechanisms for managing their mental health.
- Empowerment: Involve patients in their care plans and encourage them to take an active role in their recovery process.
6. Using Evidence-Based Practices:
- Best Practices: Mental health nurses should use evidence-based approaches in diagnosis, intervention, and treatment. This involves keeping up to date with the latest research and treatment modalities.
- Evaluation: Regularly assess the patient’s progress and the effectiveness of interventions, adjusting care plans as necessary.
7. Cultural Competence:
- Culturally Sensitive Care: Nurses should provide care that is respectful and responsive to the cultural and linguistic needs of the patient. Understanding cultural backgrounds helps in creating effective and appropriate care plans.
- Eliminate Stigma: Nurses should work to eliminate mental health stigma and promote acceptance of mental health issues.
8. Crisis Intervention and De-escalation:
- Crisis Management: Mental health nurses must be trained in recognizing and managing psychiatric emergencies, such as suicidal ideation or acute psychosis.
- De-escalation Techniques: Use non-violent communication and calming strategies to prevent aggressive behavior or reduce patient agitation during crises.
9. Medication Management:
- Adherence to Medication: Educate patients about their medications, including the importance of adherence, potential side effects, and how the medication works.
- Monitoring and Side Effects: Monitor patients for the therapeutic effects of medications and any adverse reactions, adjusting the treatment plan as needed.
10. Family Involvement and Support Systems:
- Family Education: Involving the patient’s family in the care process can enhance treatment outcomes. Educate families on the nature of the illness, the importance of their support, and how they can contribute to the patient’s recovery.
- Building a Support System: Encourage patients to build strong support systems outside of their families, including friends, mental health groups, or community organizations.
11. Promoting Recovery and Rehabilitation:
- Recovery-Oriented Care: Mental health nursing should focus on long-term recovery, helping individuals regain control of their lives, reintegrate into society, and maintain their mental health.
- Rehabilitation Programs: Assist patients in accessing vocational rehabilitation, skill-building, and social support programs that aid their recovery process.
12. Ethical and Legal Responsibilities:
- Legal Awareness: Mental health nurses must be aware of the legal aspects surrounding mental health care, such as the Mental Health Act, involuntary admissions, and patients’ rights.
- Ethical Considerations: Uphold ethical standards in all practices, such as obtaining informed consent, maintaining patient dignity, and advocating for the patient’s well-being.
OR
(a) Define mental retardation 2+3+5
Mental retardation, now commonly referred to as intellectual disability (ID), is characterized by significant limitations in both intellectual functioning and adaptive behavior, which covers a range of everyday social and practical skills. This condition originates before the age of 18 and results in challenges with learning, reasoning, problem-solving, and performing everyday tasks. Intellectual functioning is typically measured through standardized IQ tests, while adaptive behavior refers to the ability to perform age-appropriate daily living activities.
(b) Write about classification, signs and symptoms.
Intellectual disability is classified based on the severity of the impairment in intellectual functioning and adaptive behavior. These classifications often rely on IQ scores and the degree of support needed for daily living.
1. Mild Intellectual Disability (IQ 50-70):
- Individuals can often live independently with some assistance.
- May experience difficulty in school and learning but can acquire academic skills up to the 6th-grade level.
- Social skills are usually functional, and they can work in regular jobs with limited support.
- Able to perform basic self-care but may require guidance in complex tasks.
2. Moderate Intellectual Disability (IQ 35-49):
- Individuals require more supervision and support in daily living activities.
- They can achieve academic skills equivalent to 2nd-grade level and can learn simple communication and daily living skills.
- Social interactions may be limited, and they may have difficulty understanding social norms.
- Can work in supervised environments and live in group homes or with family support.
3. Severe Intellectual Disability (IQ 20-34):
- Individuals need constant supervision and support for most activities.
- Communication is usually limited, and they may use basic language or gestures.
- Adaptive behavior, such as self-care, is limited, and they require significant assistance with daily tasks.
- They may be able to perform simple tasks in highly structured environments.
4. Profound Intellectual Disability (IQ below 20):
- Individuals require 24-hour care and supervision.
- They have very limited communication abilities, often relying on non-verbal cues.
- Motor skills may be impaired, and they may have co-existing physical disabilities.
- Adaptive behaviors are minimal, requiring extensive support in all aspects of life, including feeding, dressing, and mobility.
Signs and Symptoms of Mental Retardation (Intellectual Disability):
- Cognitive Symptoms:
- Delayed milestones in speech and motor development.
- Difficulty in learning new information and skills.
- Poor problem-solving abilities.
- Difficulty in understanding abstract concepts.
- Behavioral Symptoms:
- Trouble with social interactions and forming relationships.
- Difficulty following rules or understanding social cues.
- Limited capacity for judgment and decision-making.
- Difficulty managing emotions and behavior, which may result in frustration or aggression.
- Communication Challenges:
- Delayed language development.
- Limited vocabulary and difficulty forming sentences.
- Difficulty understanding and following complex instructions.
- Non-verbal communication may be relied upon in more severe cases.
- Motor Skills Impairment:
- Delays in gross and fine motor skill development (e.g., walking, grasping objects).
- In severe cases, coordination problems may be present.
- Adaptive Behavior Challenges:
- Difficulty performing everyday tasks, such as dressing, bathing, and feeding independently.
- Difficulty in managing finances, handling transportation, or planning daily routines.
- Poor personal hygiene and lack of awareness about health and safety.
- Educational Challenges:
- Difficulty with academic learning, such as reading, writing, and math.
- Need for specialized education programs or special classrooms in school.
(c) Prevention of mental retardation.
Preventing intellectual disability involves addressing potential risk factors at various stages, from prenatal care to early childhood development. The following are key strategies for prevention:
1. Prenatal Care:
- Proper Nutrition: Adequate maternal nutrition, including the intake of folic acid, iron, and vitamins, helps reduce the risk of birth defects and brain development issues.
- Avoidance of Harmful Substances: Pregnant women should avoid alcohol, smoking, and recreational drugs, as these can cause fetal alcohol syndrome and other developmental issues.
- Control of Chronic Conditions: Proper management of maternal health conditions such as diabetes, hypertension, and infections during pregnancy can reduce the risk of intellectual disability in the child.
- Genetic Counseling: Families with a history of genetic disorders should seek genetic counseling before conceiving, which can help identify potential risks for intellectual disabilities.
2. Perinatal Care (During Birth):
- Skilled Birth Attendants: Having a skilled healthcare professional during delivery helps reduce the risks of birth complications, such as oxygen deprivation (hypoxia), which can lead to brain damage.
- Immediate Newborn Care: Proper care after delivery, such as resuscitation and monitoring for signs of distress, is crucial in preventing complications that may result in intellectual disability.
3. Postnatal Care and Early Childhood:
- Vaccinations: Immunization against infectious diseases like rubella, meningitis, and measles can prevent brain damage that leads to intellectual disability.
- Early Screening and Intervention: Early identification of developmental delays through regular pediatric check-ups allows for timely interventions like speech therapy, physical therapy, and special education.
- Adequate Nutrition: Ensuring proper nutrition in infancy and early childhood, including breastfeeding, helps in brain development and prevents malnutrition-related cognitive impairments.
- Avoiding Exposure to Toxins: Limiting children’s exposure to environmental toxins, such as lead and mercury, is crucial in preventing intellectual impairment.
4. Prevention of Head Injuries:
- Safety Measures: Using car seats, helmets, and other protective gear can prevent traumatic brain injuries that may lead to intellectual disability.
- Supervision: Ensuring proper supervision of young children to prevent accidents that could result in head injuries.
5. Prevention of Infections and Illnesses:
- Timely Treatment of Illnesses: Prompt treatment of illnesses such as meningitis and encephalitis, which can cause brain damage if left untreated.
- Healthy Environment: Maintaining a clean living environment to prevent infections and promote healthy development.
2.Short notes: (any three)3×5=15
1)Behaviour therapy
Behavior therapy is a type of psychotherapy that focuses on changing maladaptive behaviors through various techniques based on the principles of learning theory. It primarily uses classical conditioning, operant conditioning, and social learning to address psychological problems. The goal is to replace unhealthy behaviors with positive ones by reinforcing desirable behaviors and eliminating unwanted ones.
Techniques:
- Systematic Desensitization: Gradually exposing patients to their fears while teaching relaxation techniques to reduce anxiety.
- Operant Conditioning: Using positive reinforcement, punishment, or extinction to modify behavior.
- Exposure Therapy: Helping patients confront and reduce their fears through controlled exposure to anxiety-producing situations.
- Token Economies: Rewarding patients with tokens for positive behavior that can be exchanged for privileges.
Behavior therapy is effective in treating conditions such as anxiety disorders, phobias, obsessive-compulsive disorder (OCD), and addictions.
2)PTSD
PTSD is a mental health condition that can develop after a person experiences or witnesses a traumatic event, such as war, natural disasters, serious accidents, or violent personal assaults. The disorder causes intense fear, helplessness, or horror.
Symptoms:
- Re-experiencing: Flashbacks, nightmares, or intrusive thoughts about the traumatic event.
- Avoidance: Avoiding reminders of the trauma, such as places, people, or activities.
- Hyperarousal: Increased alertness, irritability, difficulty sleeping, or being easily startled.
- Negative Cognitions and Mood: Feelings of guilt, isolation, or detachment from others, as well as negative beliefs about oneself or the world.
Treatment:
- Cognitive Behavioral Therapy (CBT), particularly trauma-focused CBT.
- Eye Movement Desensitization and Reprocessing (EMDR).
- Medications, such as selective serotonin reuptake inhibitors (SSRIs).
- Support groups and family therapy.
(3) Models of stress
Stress models help explain the relationship between stressors (external events) and stress responses (psychological and physiological reactions).
a) General Adaptation Syndrome (GAS):
Proposed by Hans Selye, GAS outlines three stages of stress response:
- Alarm: Initial reaction to a stressor where the body activates the fight-or-flight response.
- Resistance: The body attempts to adapt to the stressor by releasing stress hormones like cortisol to cope.
- Exhaustion: Prolonged stress can deplete the body’s resources, leading to burnout, illness, or depression.
b) Cognitive Appraisal Model (Lazarus and Folkman):
This model suggests that stress is a result of how individuals appraise a situation:
- Primary Appraisal: Determining whether an event is a threat or challenge.
- Secondary Appraisal: Assessing one’s ability to cope with the stressor. Stress results from the imbalance between the perceived demands and one’s ability to cope.
c) Transactional Model of Stress:
This model focuses on the dynamic interaction between individuals and their environment. Stress arises when environmental demands exceed personal resources, leading to feelings of overwhelm.
(4) Indian lunacy act
The Indian Lunacy Act of 1912 was one of the earliest laws enacted to regulate the treatment and care of people with mental illness in India. Its primary focus was on the legal framework for the detention and treatment of individuals with mental disorders.
Key Points:
- The act defined procedures for admitting mentally ill persons into asylums.
- It provided for the appointment of “managers” to oversee asylums.
- The law primarily focused on the custodial care of patients rather than treatment or rehabilitation.
- It was replaced by the Mental Health Act of 1987, which emphasized human rights and aimed to de-stigmatize mental illness.
The Indian Lunacy Act is considered outdated and was more about controlling and confining individuals with mental illness rather than focusing on their treatment and reintegration into society.
5) Components of therapeutic nurse patient relationships
A therapeutic nurse-patient relationship is a professional, goal-directed relationship that promotes the patient’s well-being and recovery. It is based on mutual respect, trust, and empathy. The following components are essential for fostering a successful therapeutic relationship:
a) Trust:
- Foundation of the relationship: The patient must trust that the nurse will provide care that is in their best interest.
- Built through consistency, honesty, and reliability.
b) Empathy:
- The nurse must understand the patient’s feelings and experiences from their perspective.
- Empathy helps the nurse connect with the patient emotionally and offer personalized care.
c) Respect:
- Recognizing the patient’s autonomy and dignity.
- The nurse must respect the patient’s values, beliefs, and choices, and promote their independence.
d) Professional Boundaries:
- Clear boundaries must be maintained to avoid personal involvement or bias.
- Nurses should be caring but remain professional to ensure that the relationship stays therapeutic.
e) Active Listening:
- Nurses must actively listen to patients’ concerns, feelings, and needs without judgment or interruption.
- This helps patients feel heard, understood, and valued.
f) Confidentiality:
- Maintaining patient confidentiality is critical to fostering trust and creating a safe space for the patient to share personal information.
- Nurses should only share patient information with those involved in their care, and only when necessary.
g) Patient-Centered Care:
- Involve the patient in decision-making and care planning.
- The nurse should empower the patient by acknowledging their role in managing their health and treatment.
3.Short answers: (answer all) 6X2=12
1) Dhat syndrome
Dhat syndrome is a culture-bound psychiatric disorder prevalent in South Asian countries. It is characterized by anxiety and somatic symptoms, including fatigue, weakness, and feelings of loss, attributed to the loss of “Dhat” (semen) through urine, masturbation, or nocturnal emissions. It is often associated with guilt, shame, and sexual dysfunction. Treatment includes education, counseling, and addressing underlying anxiety or depression.
(2) General guidelines regarding drug administration in psychiatry
Start Low, Go Slow: Psychiatric medications should often begin with a low dose, gradually increasing based on patient tolerance and response.Monitor Side Effects: Regular monitoring for side effects like weight gain, sedation, or movement disorders is crucial.Adherence: Ensure patient compliance by educating them on the importance of consistent use.Individualized Treatment: Tailor the medication based on the patient’s specific condition, response, and medical history.Drug Interactions: Be aware of potential interactions with other medications or substances.
4) Narcoanalysis
Narcoanalysis is a therapeutic and investigative technique in which a patient is administered a sedative drug (such as sodium pentothal) to lower inhibitions and enable them to talk freely. It is used to recover repressed memories or investigate facts in forensic settings. The reliability of information gathered through narcoanalysis is debated, as it may be influenced by suggestion.
(3) Loosening of association
Loosening of associations refers to a thought disorder where a person’s ideas and thoughts become disorganized and disconnected. This results in incoherent or fragmented speech, making it difficult to follow their line of thinking. It is often seen in schizophrenia and other psychotic disorders.
(5) Abreaction therapy
Abreaction therapy involves recalling and reliving a past traumatic experience with the aim of releasing the repressed emotions associated with it. This is done in a controlled therapeutic setting where the patient expresses pent-up emotions, leading to catharsis. It is often used in the treatment of trauma, anxiety, and PTSD.
(6) Alcoholic anonymous.
Alcoholics Anonymous (AA) is a worldwide fellowship of individuals who have struggled with alcohol addiction. It follows a 12-step program that promotes abstinence and recovery through group support, self-reflection, and spiritual development. AA emphasizes peer support and shared experiences to help individuals maintain sobriety. Meetings are free and open to anyone seeking help for alcohol dependence.
💥☺☺☺ALL THE BEST ☺☺☺💥💪
નોંધ :-MCQ ANSWER APP ની યુનિક પેટર્ન માં બંને ભાષા માં આગળ paper solution /click here ની નીચે આપેલા છે. ” અ ” પર ક્લિક કરવાથી ભાષા ચેન્જ થશે.

IF ANY QUERY OR QUESTION,REVIEW-KINDLY WATSAPP US No. – 84859 76407