Physio-Unit-11-B.sc-Nervous System
🧠 Overview of the Nervous System
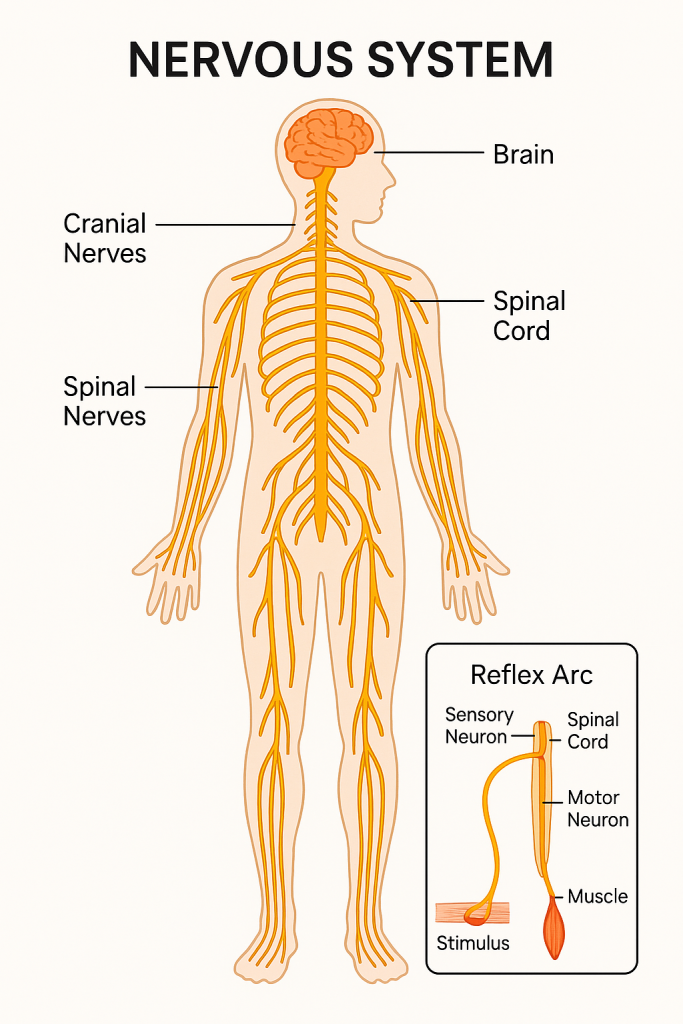
The nervous system is a highly complex and vital system responsible for controlling and coordinating all body activities. It allows the body to respond to internal and external stimuli and maintain homeostasis.
🔰 Definition
The nervous system is a specialized network of cells that transmits signals between different parts of the body to regulate bodily functions, sensation, movement, and cognition.
🧩 Major Functions
- 🧭 Sensory Input – Detects changes inside and outside the body (via receptors).
- 🧠 Integration – Processes sensory input and determines the appropriate response.
- 🏃 Motor Output – Sends commands to effectors (muscles/glands) to respond.
🏗️ Structural Classification
1️⃣ Central Nervous System (CNS)
- 📌 Brain – Control center for thoughts, memory, emotion, and decision-making.
- 📌 Spinal Cord – Connects brain to peripheral nerves and coordinates reflexes.
2️⃣ Peripheral Nervous System (PNS)
- Composed of cranial and spinal nerves.
- Divided into:
- 🌐 Somatic Nervous System (SNS) – Controls voluntary movements.
- ⚙️ Autonomic Nervous System (ANS) – Controls involuntary actions (e.g., heart rate, digestion).
🧭 Functional Classification
🌐 Somatic Nervous System (SNS)
- Transmits sensory and motor signals to/from the CNS.
- Voluntary control over skeletal muscles.
⚙️ Autonomic Nervous System (ANS)
- Regulates involuntary bodily functions.
- Divided into:
- 💢 Sympathetic Nervous System – “Fight or Flight” responses.
- 🧘 Parasympathetic Nervous System – “Rest and Digest” responses.
🧬 Basic Unit: Neuron
🔹 Structure:
- Cell Body (Soma) – Contains nucleus and organelles.
- Dendrites – Receive signals.
- Axon – Transmits impulses away from the cell body.
- Myelin Sheath – Increases impulse speed (insulation).
- Synapse – Junction where signals pass to next neuron/cell.
🔹 Types of Neurons:
- 🟢 Sensory (Afferent) – Carry impulses to CNS.
- 🔵 Motor (Efferent) – Carry impulses from CNS to effectors.
- 🟡 Interneurons – Connect sensory and motor neurons within the CNS.
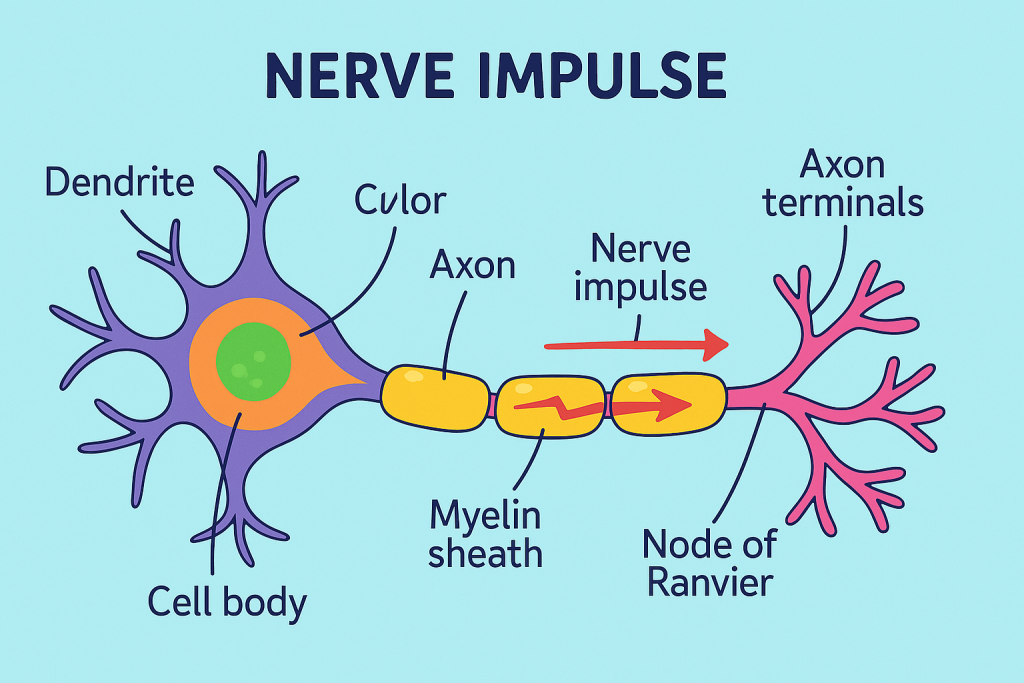
🔄 Nerve Impulse Transmission
- Stimulus triggers a nerve impulse.
- Impulse travels along the axon.
- Neurotransmitters are released at synapse.
- Signal continues to the next neuron or target cell.
🧠 Protective Structures of the CNS
- 🧱 Skull and Vertebral Column – Hard bony protection.
- 💧 Cerebrospinal Fluid (CSF) – Cushions the brain/spinal cord.
- 🧠 Meninges – Three protective membranes (dura mater, arachnoid mater, pia mater).
🧠 Brain Regions and Functions
| Region | Main Functions |
|---|---|
| Cerebrum | Thinking, memory, voluntary movement, speech |
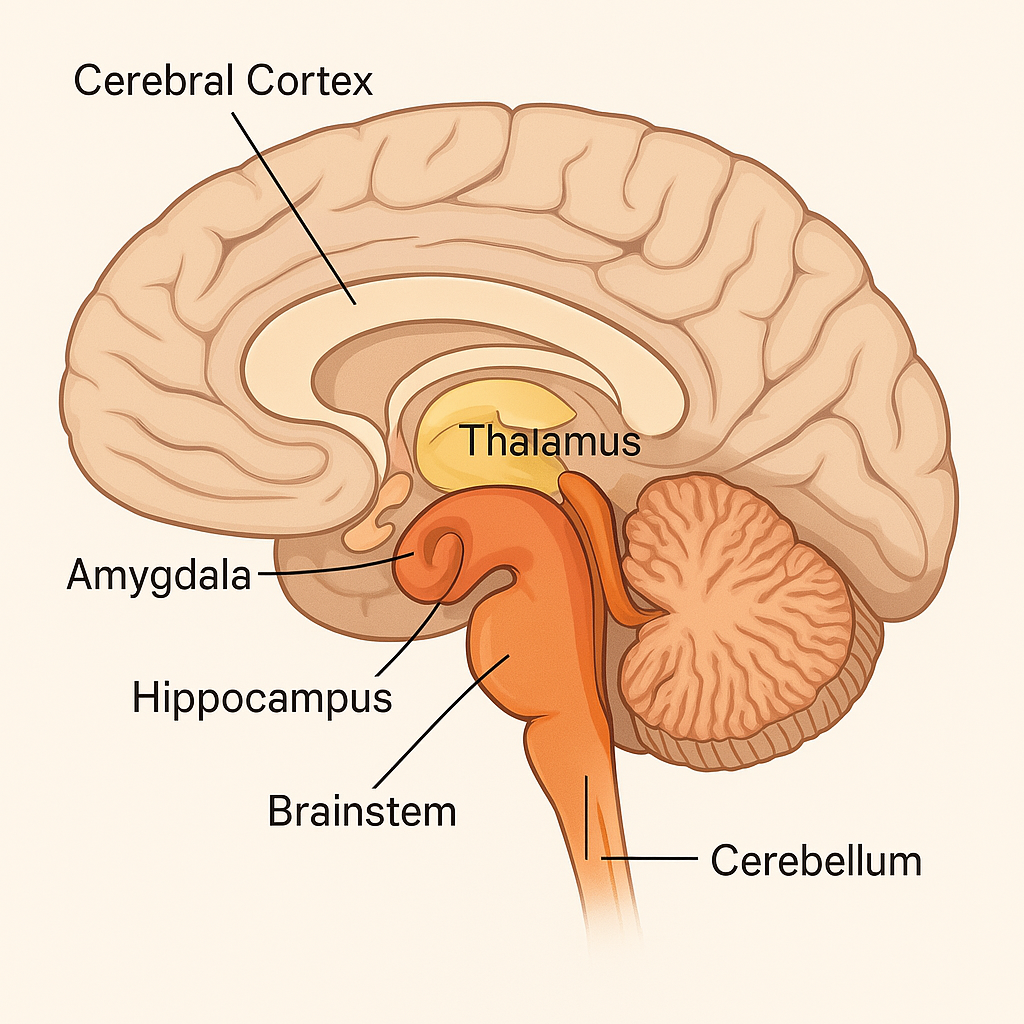
| Cerebellum | Coordination, balance, fine motor control |
| Brainstem | Autonomic functions (heart rate, breathing, sleep) |
| Diencephalon | Hormone regulation, sensory relay (thalamus, hypothalamus) |
📌 Key Terms
- Neuroglia – Supporting cells of neurons (e.g., astrocytes, oligodendrocytes).
- Reflex Arc – Simple neural pathway causing automatic response.
🏥 Applications in Nursing
- Neurological assessment (GCS, reflexes)
- Monitoring for stroke, head injury, meningitis
- Drug effects on CNS (sedatives, analgesics)
- Patient education on nervous system health (e.g., avoiding neurotoxins)
🧠 Neurons – Types & Detailed Explanation
A neuron is the structural and functional unit of the nervous system. Neurons are highly specialized cells that transmit electrical and chemical signals throughout the body. Each neuron is composed of:
- Cell Body (Soma) – contains the nucleus and organelles
- Dendrites – receive impulses from other neurons
- Axon – conducts impulses away from the cell body
- Axon Terminals – release neurotransmitters into the synaptic cleft
🔢 Classification of Neurons (Based on Function)
1️⃣ Sensory Neurons (Afferent Neurons)
- 🔹 Function: Carry sensory information from receptors (skin, eyes, ears, etc.) towards the CNS.
- 🔹 Location: Found in peripheral nervous system (PNS); cell bodies in dorsal root ganglia.
- 🔹 Example: Pain receptors detecting a sharp object and sending that signal to the spinal cord.
2️⃣ Motor Neurons (Efferent Neurons)
- 🔹 Function: Carry motor commands from CNS to effectors (muscles or glands).
- 🔹 Subtypes:
- Somatic Motor Neurons – Control voluntary muscles.
- Autonomic Motor Neurons – Control involuntary effectors (e.g., cardiac muscle, glands).
- 🔹 Example: Signal from spinal cord to biceps to contract and pull hand away.
3️⃣ Interneurons (Association Neurons)
- 🔹 Function: Connect sensory and motor neurons within the CNS; involved in integration and processing.
- 🔹 Location: Entirely within the brain and spinal cord.
- 🔹 Example: Neurons involved in reflex arcs processing the stimulus and generating a motor response.
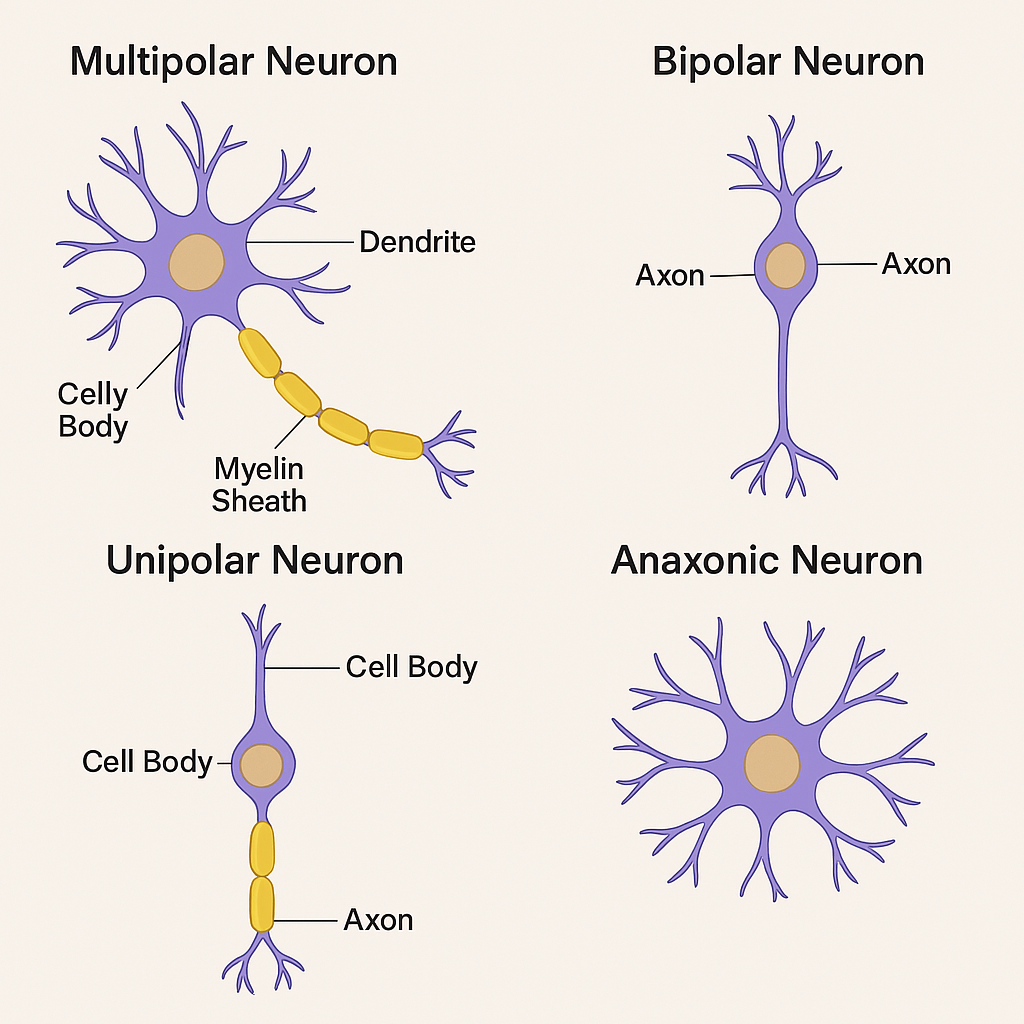
🔢 Classification of Neurons (Based on Structure)
1️⃣ Multipolar Neurons
- 🔸 Structure: One axon, multiple dendrites.
- 🔸 Most common type in the CNS.
- 🔸 Function: Typically motor or interneurons.
- 🔸 Example: Motor neurons controlling skeletal muscles.
2️⃣ Bipolar Neurons
- 🔸 Structure: One axon, one dendrite extending from opposite sides of the cell body.
- 🔸 Location: Rare – found in special sensory organs like the retina (eye), olfactory mucosa (nose), and inner ear.
- 🔸 Function: Sensory transmission in specific sense organs.
3️⃣ Unipolar (Pseudounipolar) Neurons
- 🔸 Structure: One process that splits into two branches (axon and dendrite-like extension).
- 🔸 Location: Found in dorsal root ganglia of spinal nerves.
- 🔸 Function: Mainly sensory neurons that carry impulses to the CNS.
4️⃣ Anaxonic Neurons
- 🔸 Structure: No clear axon; only dendrites.
- 🔸 Location: Found in the brain and retina.
- 🔸 Function: Act as interneurons, not producing traditional action potentials but modulating other neurons.
🧪 Comparison Table of Neuron Types
| Type | Function | Structure | Location |
|---|---|---|---|
| Sensory | Afferent (input) | Mostly unipolar | PNS, dorsal root ganglia |
| Motor | Efferent (output) | Multipolar | CNS to muscles/glands |
| Interneuron | Integration | Multipolar or anaxonic | Brain, spinal cord |
| Bipolar | Special sensory | One axon, one dendrite | Retina, olfactory system |
| Anaxonic | Modulation | No axon | Retina, some brain areas |
🩺 Applications and Implications in Nursing
- 🔍 Neurological assessment involves evaluating reflexes (interneurons), sensory perception, and motor control.
- 💉 Neurotoxic drugs may affect specific neuron types (e.g., peripheral neuropathy affects sensory neurons).
- ⚡ Diseases like Multiple Sclerosis affect motor neurons due to demyelination.
- 🧪 Understanding neuron types helps in interpreting nerve conduction studies and managing neurodegenerative conditions like ALS or Parkinson’s disease.
🧠 Structure and Functions of Neurons
🔍 “Neurons are the structural and functional units of the nervous system.”
📌 Definition:
A neuron is a specialized, excitable cell that conducts electrochemical signals throughout the nervous system. Neurons are responsible for receiving, integrating, and transmitting information between different parts of the body.
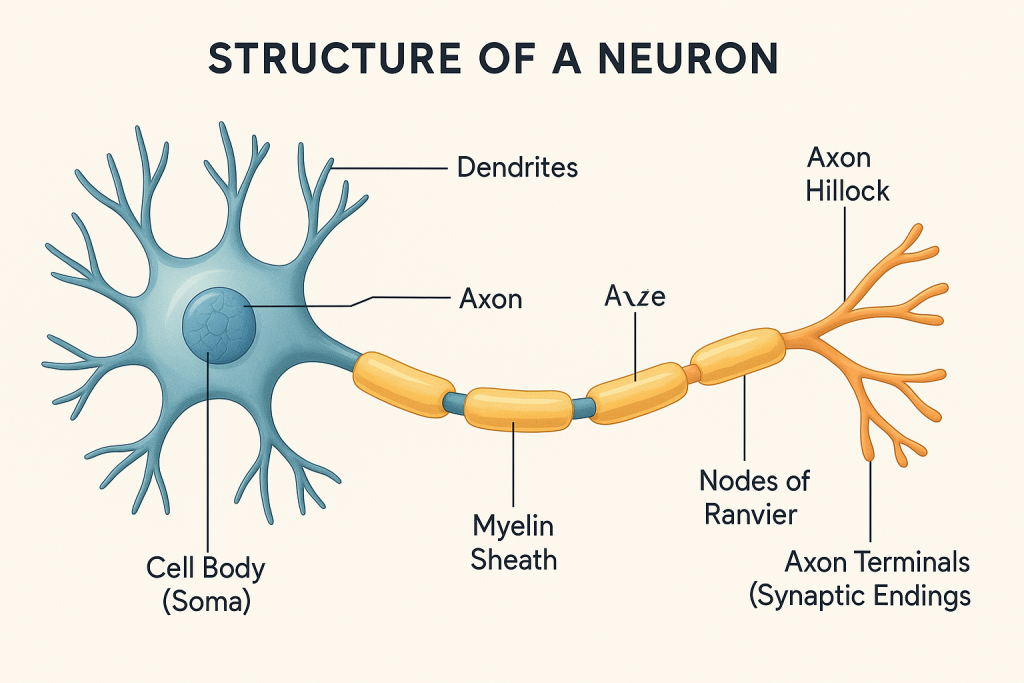
🏗️ Structure of a Neuron
A typical neuron consists of the following parts:
1️⃣ Cell Body (Soma / Perikaryon)
- 📍 Contains the nucleus, nucleolus, and cytoplasmic organelles.
- 📍 Major site for metabolism and protein synthesis.
- 📍 Nissl bodies (clusters of rough ER) are involved in synthesizing neurotransmitters.
🔹 Function:
- Maintains the cell’s metabolic functions.
- Integrates incoming signals.
2️⃣ Dendrites
- 🌿 Short, branched, tree-like extensions from the cell body.
- Increase the surface area for receiving signals.
🔹 Function:
- Receive incoming signals from other neurons or receptors.
- Conduct graded potentials (not action potentials) toward the cell body.
3️⃣ Axon
- 📏 A single, long projection arising from the axon hillock.
- Ends in axon terminals or synaptic boutons.
🔹 Function:
- Conducts action potentials away from the cell body toward the effector organ or another neuron.
- Transmits signals using electrical impulses and neurotransmitters at synapses.
4️⃣ Axon Hillock
- 📍 Cone-shaped area of the cell body where the axon originates.
🔹 Function:
- Initiates the action potential.
5️⃣ Myelin Sheath
- 🧈 A fatty insulating layer formed by Schwann cells (in PNS) or oligodendrocytes (in CNS).
- Appears segmented due to Nodes of Ranvier.
🔹 Function:
- Increases speed of conduction via saltatory conduction.
- Protects and insulates axons.
6️⃣ Nodes of Ranvier
- 🔘 Gaps between adjacent myelin segments.
🔹 Function:
- Allow for rapid signal conduction through saltatory movement of impulses.
7️⃣ Axon Terminals (Synaptic Knobs)
- 🌐 Ends of the axon where neurotransmitters are stored and released.
🔹 Function:
- Form synapses with other neurons, muscles, or glands.
- Transmit the nerve impulse chemically to the next cell.
💡 Functions of Neurons
| 🔢 Function Type | 📝 Description |
|---|---|
| 1. Sensory Function | Detects stimuli from sensory receptors and sends to CNS (via afferent neurons) |
| 2. Integrative Function | Processes, stores, and interprets incoming sensory information (via interneurons) |
| 3. Motor Function | Transmits signals from CNS to effectors like muscles/glands (via efferent neurons) |
| 4. Conductivity | Ability to transmit electrical impulses efficiently |
| 5. Excitability | Responds to stimuli with electrical activity |
| 6. Neurosecretion | Release of neurotransmitters (e.g., acetylcholine, dopamine) for communication |
🩺 Nursing Implications
- Understanding neuron structure helps assess:
- ✅ Effects of neurodegenerative diseases (e.g., Alzheimer’s, MS)
- ✅ Neurological assessments (reflexes, motor function)
- ✅ Monitoring drug actions like anesthetics, sedatives, or anticonvulsants
- ✅ Managing nerve injury or peripheral neuropathy in diabetic patients
⚡ Nerve Impulse: Detailed & Academic Explanation
📌 Definition:
A nerve impulse (also called action potential) is a rapid, temporary electrical signal that travels along the axon of a neuron. It is essential for communication between neurons and from neurons to muscles or glands.
🧠 Basic Concept:
Neurons use electrical gradients across their membranes to transmit messages. This involves the movement of ions (Na⁺, K⁺, Cl⁻) through ion channels, leading to changes in the membrane potential.
🧪 Resting Membrane Potential (RMP)
- Normal RMP = -70 mV
- Inside of the neuron is more negative compared to the outside.
- Maintained by:
- Na⁺/K⁺ Pump (3 Na⁺ out, 2 K⁺ in)
- Selective permeability of membrane to ions (more permeable to K⁺)
🔹 Key Concept: The membrane is polarized in resting state.
🔄 Phases of Nerve Impulse (Action Potential)
1️⃣ Depolarization Phase
- Triggered when membrane potential reaches threshold (≈ -55 mV).
- Na⁺ channels open, causing influx of sodium.
- Membrane potential becomes positive (~+30 mV).
📌 Cause: Sodium influx
📌 Effect: Membrane becomes depolarized (loss of resting potential)
2️⃣ Repolarization Phase
- Na⁺ channels close.
- K⁺ channels open, and potassium exits the neuron.
- Membrane potential returns to negative.
📌 Cause: Potassium efflux
📌 Effect: Restores polarity (inside negative again)
3️⃣ Hyperpolarization (Undershoot)
- K⁺ channels stay open a bit longer.
- Membrane potential drops below -70 mV briefly.
📌 Effect: Neuron becomes less excitable for a short time
4️⃣ Restoration of Resting Potential
- Na⁺/K⁺ ATPase Pump restores ionic balance.
- RMP is re-established at -70 mV.
🔁 Propagation of Nerve Impulse
🔹 Continuous Conduction:
- Occurs in unmyelinated axons.
- Impulse moves step-by-step along entire length of axon.
🔹 Saltatory Conduction:
- Occurs in myelinated axons.
- Impulse “jumps” from one Node of Ranvier to the next.
- 🔼 Much faster than continuous conduction.
🧪 Summary of Ion Channel Activities
| Phase | Na⁺ Channels | K⁺ Channels | Membrane State |
|---|---|---|---|
| Resting | Closed | Closed | Polarized (-70 mV) |
| Depolarization | Open | Closed | +30 mV |
| Repolarization | Inactivated | Open | Returns to negative |
| Hyperpolarization | Closed | Slowly closing | Below -70 mV |
| Resting again | Restored via pumps | Restored | -70 mV reestablished |
🔄 Refractory Periods
🔒 Absolute Refractory Period:
- Neuron cannot initiate another action potential.
- Occurs during depolarization and early repolarization.
🕒 Relative Refractory Period:
- A stronger-than-normal stimulus can trigger another impulse.
- Occurs during late repolarization and hyperpolarization.
🩺 Clinical & Nursing Relevance
- ⚡ Local anesthetics (e.g., lidocaine) block Na⁺ channels → prevent impulse conduction.
- 🔥 Multiple Sclerosis affects myelin → slows or blocks saltatory conduction.
- 🧠 Epilepsy involves abnormal, excessive nerve firing.
- 💊 Electrolyte imbalances (e.g., hypokalemia or hyperkalemia) can alter nerve excitability.
- 👩⚕️ Nurses monitor neuro status via reflexes, movement, and sensory changes.
📊 Visual Analogy
Imagine a domino effect where the fall of one tile causes the next to fall. The nerve impulse behaves similarly — as one part of the neuron depolarizes, it triggers depolarization in the next segment.
🧠 Medulla Oblongata
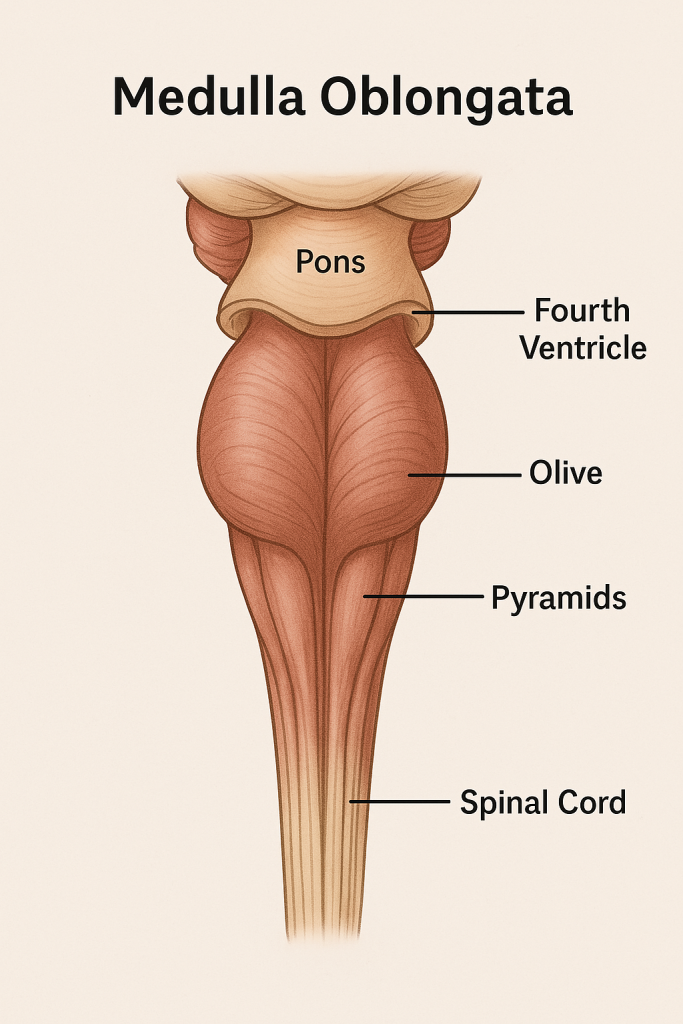
The medulla oblongata is the lowest part of the brainstem, continuous with the spinal cord. It plays a vital role in autonomic (involuntary) functions, particularly those necessary for life such as breathing, heart rate, and blood pressure regulation.
🧩 Location
- Lies between the pons (superiorly) and the spinal cord (inferiorly).
- Forms the lower half of the brainstem.
- Contains part of the fourth ventricle posteriorly.
🧬 Structural Components
- Pyramids – contain corticospinal tracts (motor fibers from cerebrum).
- Olives – relay nuclei for sensory information.
- Cranial nerve nuclei – for nerves IX, X, XI, and XII.
- Reticular formation – involved in consciousness and arousal.
- Vital centers – cardiovascular, respiratory, and vasomotor centers.
🧠 Major Functions of Medulla Oblongata
🔹 1. Cardiovascular Control Center
- Function: Regulates heart rate and force of contraction.
- Mechanism: Acts through sympathetic and parasympathetic outputs.
- Clinical relevance: Lesions can cause arrhythmias or sudden cardiac arrest.
🔹 2. Respiratory Control Center
- Function: Controls rate and depth of breathing.
- Includes: Dorsal and ventral respiratory groups.
- Works with: Pons (apneustic and pneumotaxic centers).
- Reflexes: Controlled via chemoreceptors (CO₂, O₂ levels).
🔹 3. Vasomotor Center
- Function: Regulates blood vessel diameter.
- Effect: Maintains blood pressure via vasoconstriction/vasodilation.
🔹 4. Reflex Centers (Vital Reflexes)
- Controls autonomic reflexes, including:
- Swallowing (deglutition)
- Coughing
- Sneezing
- Vomiting (emesis)
- Hiccupping
- Coordinates these reflexes with cranial nerves IX, X, and XII.
🔹 5. Cranial Nerve Functions
- Houses nuclei of:
- Glossopharyngeal (IX) – taste, baroreception.
- Vagus (X) – parasympathetic control of heart, lungs, GI.
- Accessory (XI) – head and shoulder movement.
- Hypoglossal (XII) – tongue movement.
🔹 6. Relay of Sensory and Motor Pathways
- Ascending tracts: carry sensory input from spinal cord to brain.
- Descending tracts: motor signals from brain to spinal cord.
- Decussation of pyramids: Most corticospinal fibers cross here → contralateral control.
🔹 7. Regulation of Consciousness
- Part of Reticular Activating System (RAS) – influences alertness, wakefulness.
- Injury can result in coma or reduced consciousness.
⚠️ Clinical Correlation
- Damage to medulla (stroke, trauma, tumors, demyelination) can lead to:
- Respiratory failure
- Loss of cardiovascular regulation
- Dysphagia (difficulty swallowing)
- Cranial nerve palsies
- Death if bilateral or severe
📌 Summary (Key Points)
- Medulla = vital life center.
- Controls autonomic functions: heart, lungs, blood vessels.
- Houses important cranial nerve nuclei.
- Site of motor fiber crossing (pyramidal decussation).
- Coordinates reflexes essential for survival.
🧠 Medulla Oblongata – Overview
The medulla oblongata is the lowest part of the brainstem, continuous with the spinal cord. It plays a vital role in autonomic (involuntary) functions, particularly those necessary for life such as breathing, heart rate, and blood pressure regulation.
🧩 Location
- Lies between the pons (superiorly) and the spinal cord (inferiorly).
- Forms the lower half of the brainstem.
- Contains part of the fourth ventricle posteriorly.
🧬 Structural Components
- Pyramids – contain corticospinal tracts (motor fibers from cerebrum).
- Olives – relay nuclei for sensory information.
- Cranial nerve nuclei – for nerves IX, X, XI, and XII.
- Reticular formation – involved in consciousness and arousal.
- Vital centers – cardiovascular, respiratory, and vasomotor centers.
🧠 Major Functions of Medulla Oblongata
🔹 1. Cardiovascular Control Center
- Function: Regulates heart rate and force of contraction.
- Mechanism: Acts through sympathetic and parasympathetic outputs.
- Clinical relevance: Lesions can cause arrhythmias or sudden cardiac arrest.
🔹 2. Respiratory Control Center
- Function: Controls rate and depth of breathing.
- Includes: Dorsal and ventral respiratory groups.
- Works with: Pons (apneustic and pneumotaxic centers).
- Reflexes: Controlled via chemoreceptors (CO₂, O₂ levels).
🔹 3. Vasomotor Center
- Function: Regulates blood vessel diameter.
- Effect: Maintains blood pressure via vasoconstriction/vasodilation.
🔹 4. Reflex Centers (Vital Reflexes)
- Controls autonomic reflexes, including:
- Swallowing (deglutition)
- Coughing
- Sneezing
- Vomiting (emesis)
- Hiccupping
- Coordinates these reflexes with cranial nerves IX, X, and XII.
🔹 5. Cranial Nerve Functions
- Houses nuclei of:
- Glossopharyngeal (IX) – taste, baroreception.
- Vagus (X) – parasympathetic control of heart, lungs, GI.
- Accessory (XI) – head and shoulder movement.
- Hypoglossal (XII) – tongue movement.
🔹 6. Relay of Sensory and Motor Pathways
- Ascending tracts: carry sensory input from spinal cord to brain.
- Descending tracts: motor signals from brain to spinal cord.
- Decussation of pyramids: Most corticospinal fibers cross here → contralateral control.
🔹 7. Regulation of Consciousness
- Part of Reticular Activating System (RAS) – influences alertness, wakefulness.
- Injury can result in coma or reduced consciousness.
⚠️ Clinical Correlation
- Damage to medulla (stroke, trauma, tumors, demyelination) can lead to:
- Respiratory failure
- Loss of cardiovascular regulation
- Dysphagia (difficulty swallowing)
- Cranial nerve palsies
- Death if bilateral or severe
📌 Key Points
- Medulla = vital life center.
- Controls autonomic functions: heart, lungs, blood vessels.
- Houses important cranial nerve nuclei.
- Site of motor fiber crossing (pyramidal decussation).
- Coordinates reflexes essential for survival.
🧠 Pons
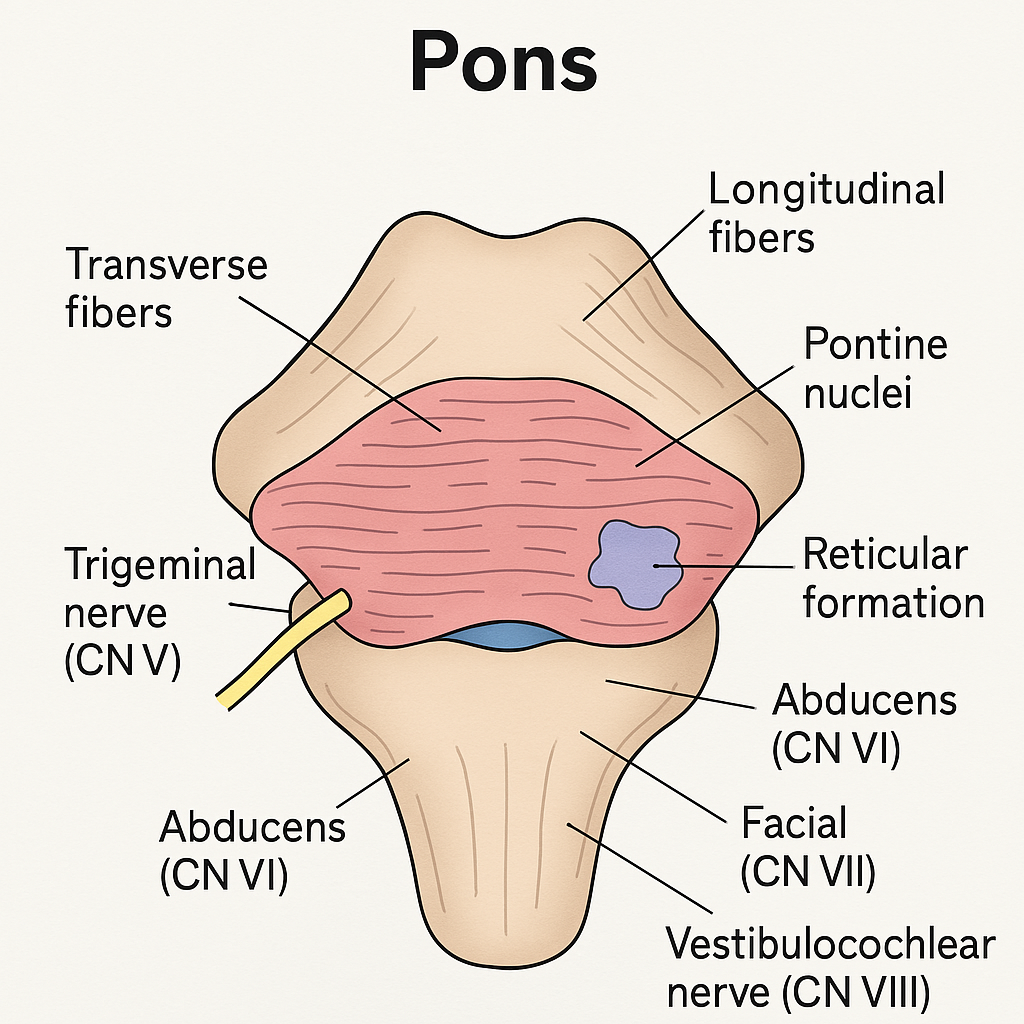
The pons is a major structure located in the brainstem, between the midbrain (above) and the medulla oblongata (below). The name “pons” means “bridge” in Latin, as it serves as a communication hub between various parts of the brain including the cerebrum, cerebellum, and spinal cord.
📍 Anatomical Location
- Anterior to the cerebellum
- Superior to the medulla oblongata
- Inferior to the midbrain
- Lies above the fourth ventricle
🧬 Structural Components
- Transverse fibers: Connect the pons to the cerebellum.
- Longitudinal tracts: Ascending (sensory) and descending (motor) tracts pass through.
- Pontine nuclei: Relay signals between the cerebrum and cerebellum.
- Cranial nerve nuclei: For CN V (trigeminal), VI (abducens), VII (facial), and part of VIII (vestibulocochlear).
- Reticular formation: Plays a role in arousal and autonomic functions.
🧠 Functions of the Pons
🔹 1. Bridge Between Brain Regions
- Acts as a relay station for signals traveling:
- Between cortex and cerebellum
- Between forebrain and medulla
- Between spinal cord and higher brain centers
🔹 2. Regulation of Respiration
- Houses the:
- Pneumotaxic center: Controls rate of breathing by limiting inspiration.
- Apneustic center: Promotes deep, prolonged inspiration.
- Works with the medullary respiratory centers for rhythmic breathing.
🔹 3. Cranial Nerve Functions
- Cranial Nerve V (Trigeminal):
- Facial sensation
- Chewing movements (mastication)
- Cranial Nerve VI (Abducens):
- Controls lateral eye movement
- Cranial Nerve VII (Facial):
- Facial expressions
- Salivation
- Lacrimation (tear production)
- Taste from anterior 2/3 of tongue
- Cranial Nerve VIII (Vestibulocochlear):
- Hearing and balance (partially)
🔹 4. Motor Control
- Contains descending motor tracts that pass through to the medulla and spinal cord.
- Coordinates voluntary motor signals.
🔹 5. Sensory Pathway Relay
- Carries ascending sensory information from the spinal cord to the thalamus and higher centers.
🔹 6. Sleep and Arousal (Reticular Formation)
- Part of the Reticular Activating System (RAS).
- Maintains wakefulness, alertness, and regulates sleep cycles.
🔹 7. Hearing, Balance, and Equilibrium
- Part of CN VIII nucleus lies here.
- Coordinates vestibular functions.
🔹 8. Facial Expressions and Reflexes
- Coordinates reflexes like blinking, salivating, and facial expressions via facial nerve.
⚠️ Clinical Correlation
- Damage to pons can cause:
- Loss of motor coordination
- Breathing irregularities
- Locked-in syndrome (conscious but paralyzed)
- Cranial nerve deficits (e.g., facial paralysis, diplopia)
📌 Summary (Key Points)
- 🧠 Pons = communication bridge of brainstem.
- 🔁 Relays sensory and motor signals.
- 💨 Helps control breathing rhythm.
- 🧍 Coordinates facial movements, chewing, and eye motion.
- 🌙 Involved in sleep and alertness.
🧠 Cerebrum
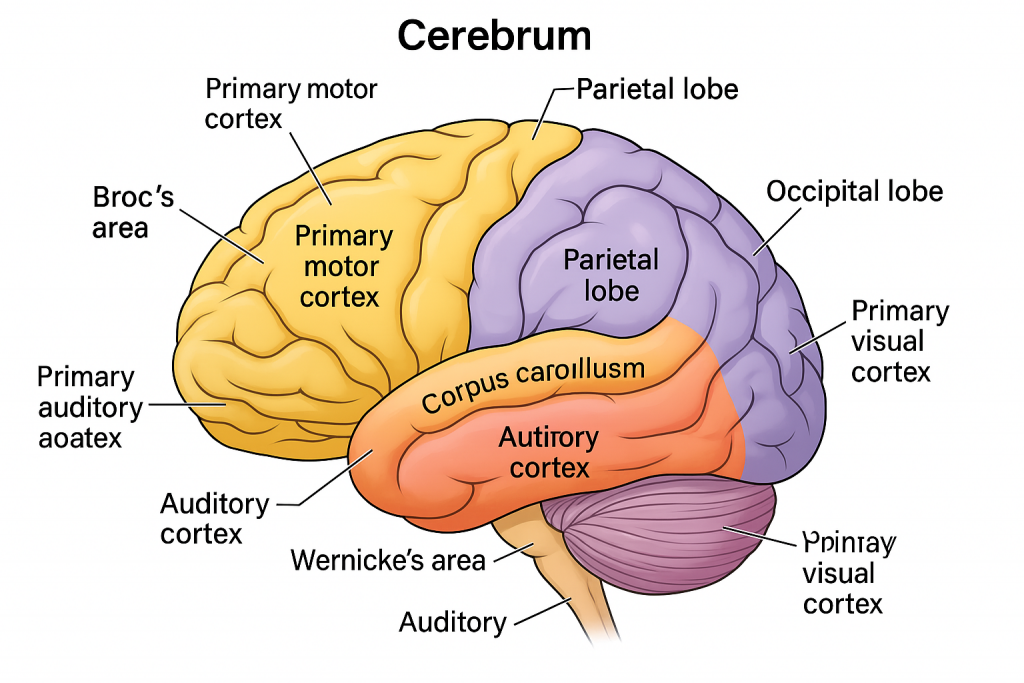
The cerebrum is the largest and most developed part of the human brain, making up nearly 80% of total brain weight. It is responsible for higher-order brain functions such as thought, emotion, memory, voluntary movement, sensation, and decision-making.
🧩 Anatomical Structure
🧠 1. Divisions
- Divided into two cerebral hemispheres: Left and Right
- Separated by longitudinal fissure
- Connected by corpus callosum (a band of white matter)
🧠 2. Lobes of Each Hemisphere
Each hemisphere is divided into four lobes, based on overlying skull bones:
| Lobe | Main Functions |
|---|---|
| Frontal | Voluntary movement, speech (Broca’s area), decision-making, problem-solving, emotions |
| Parietal | Somatic sensation (touch, pressure, pain, temperature), spatial orientation |
| Temporal | Hearing, memory, language comprehension (Wernicke’s area) |
| Occipital | Vision and visual interpretation |
🧠 3. Cerebral Cortex
- Outer layer of gray matter
- Site of conscious thought, perception, voluntary movement
- Contains gyri (ridges) and sulci (grooves) for increased surface area
🧠 4. White Matter
- Located beneath the cortex
- Contains myelinated axons that connect various parts of the brain
🧠 5. Basal Ganglia
- Group of nuclei deep inside white matter
- Involved in motor control and movement coordination
🎯 Functions of the Cerebrum
🔹 1. Motor Functions
- Primary motor cortex (frontal lobe) controls voluntary skeletal muscle movements.
- Premotor and supplementary motor areas help plan and coordinate movement.
🔹 2. Sensory Processing
- Primary somatosensory cortex (parietal lobe) interprets tactile sensations.
- Visual cortex (occipital lobe) processes visual data.
- Auditory cortex (temporal lobe) processes sound.
- Olfactory cortex (frontal/temporal) for smell.
- Gustatory cortex (parietal lobe) for taste.
🔹 3. Speech and Language
- Broca’s area (frontal lobe, usually left hemisphere): motor aspect of speech.
- Wernicke’s area (temporal lobe): comprehension of spoken and written language.
🔹 4. Cognition and Intellect
- Prefrontal cortex: Responsible for logic, judgment, planning, problem-solving, and personality.
🔹 5. Emotions and Behavior
- Integrates with limbic system to control emotional expression and behavior.
🔹 6. Memory
- Hippocampus (temporal lobe): crucial for forming and retrieving long-term memories.
🔹 7. Consciousness and Awareness
- Cerebrum integrates signals from various systems to produce awareness and conscious thought.
⚠️ Clinical Relevance
Damage to specific lobes of the cerebrum can result in distinct neurological deficits:
| Lobe Affected | Resulting Deficit |
|---|---|
| Frontal | Paralysis, personality change, Broca’s aphasia |
| Parietal | Sensory loss, spatial disorientation |
| Temporal | Hearing loss, Wernicke’s aphasia, memory loss |
| Occipital | Vision loss or visual hallucinations |
📌 Key Points
✔️ Cerebrum = largest and most complex brain region
✔️ Controls voluntary movement, sensation, memory, emotion, and intellect
✔️ Composed of cortex, white matter, basal ganglia, and lobes
✔️ Left hemisphere: logic, language; Right hemisphere: creativity, spatial skills
🧠 Cerebellum
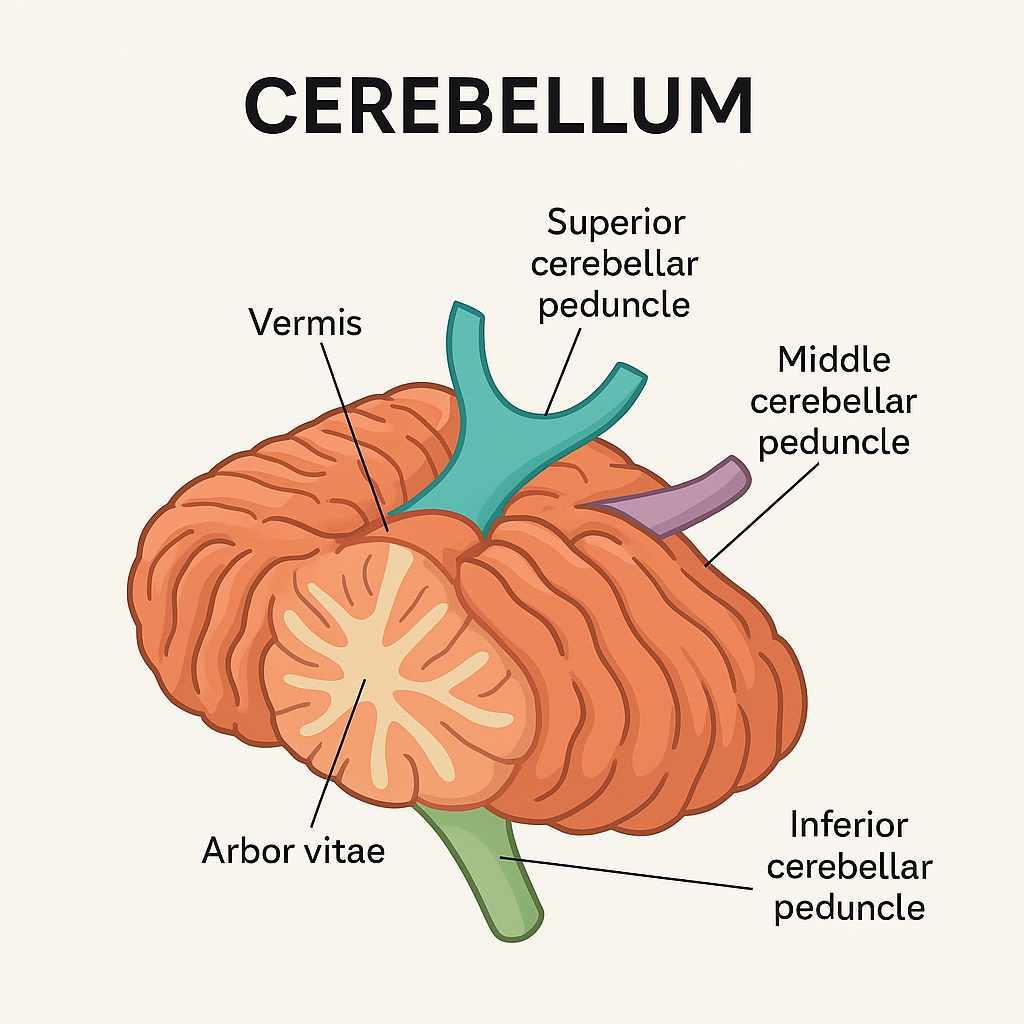
The cerebellum, also known as the “little brain”, is a major structure located at the back of the brain, underneath the cerebrum and behind the brainstem. It is primarily responsible for coordinating voluntary movements, maintaining posture, balance, and muscle tone.
📍 Anatomical Location
- Located in the posterior cranial fossa
- Lies posterior to the pons and medulla
- Separated from the cerebrum by the tentorium cerebelli
- Forms the roof of the fourth ventricle
🧩 Structural Features
🔹 1. Two Hemispheres
- Right and Left cerebellar hemispheres
- Connected by a central vermis (worm-like structure)
🔹 2. Three Lobes
- Anterior lobe – involved in posture and limb movement
- Posterior lobe – coordinates fine voluntary movements
- Flocculonodular lobe – regulates balance and eye movement
🔹 3. Cerebellar Cortex
- Outer gray matter with highly folded gyri (called folia)
- Inner white matter arranged in a tree-like pattern (arbor vitae)
🔹 4. Deep Cerebellar Nuclei
- Dentate, emboliform, globose, and fastigial nuclei
- Relay motor outputs to other parts of the brain and spinal cord
🔹 5. Peduncles
Connect cerebellum to brainstem:
- Superior cerebellar peduncle → midbrain (efferent)
- Middle cerebellar peduncle → pons (afferent)
- Inferior cerebellar peduncle → medulla (afferent/efferent)
🧠 Functions of the Cerebellum
🔸 1. Coordination of Voluntary Movements
- Smoothens and coordinates movements initiated by the motor cortex
- Ensures fluid, purposeful muscle activity (e.g., walking, writing)
🔸 2. Balance and Equilibrium
- Integrates sensory input from vestibular system, eyes, and proprioceptors
- Maintains upright posture and coordinates movements to prevent falls
🔸 3. Muscle Tone Regulation
- Monitors muscle stretch and adjusts tone via spinal cord reflex arcs
🔸 4. Motor Learning
- Plays a role in learning new motor skills (e.g., riding a bicycle, typing)
- Adjusts motor plans based on feedback (error correction)
🔸 5. Eye Movement and Gaze Stability
- Coordinates smooth pursuit and saccadic eye movements
- Controls vestibulo-ocular reflex (VOR) for gaze stabilization
⚠️ Clinical Relevance
🔻 Damage to the cerebellum may cause:
| Condition | Manifestations |
|---|---|
| Ataxia | Uncoordinated, clumsy movements (gait or limb) |
| Dysmetria | Inability to judge distance (overshooting or undershooting) |
| Dysdiadochokinesia | Inability to perform rapid alternating movements |
| Hypotonia | Decreased muscle tone |
| Nystagmus | Involuntary eye movement |
| Tremors | Intention tremor (occurs during movement, not at rest) |
| Vertigo & balance problems | Especially in flocculonodular damage |
📌 Key Points
✔️ Located behind the brainstem, beneath the cerebrum
✔️ Responsible for coordination, posture, balance, and fine motor control
✔️ Connected to brainstem via three peduncles
✔️ Integrates sensory inputs with motor commands
✔️ Lesions lead to ataxia, tremors, and motor control issues
🌐 Sensory Nervous System –
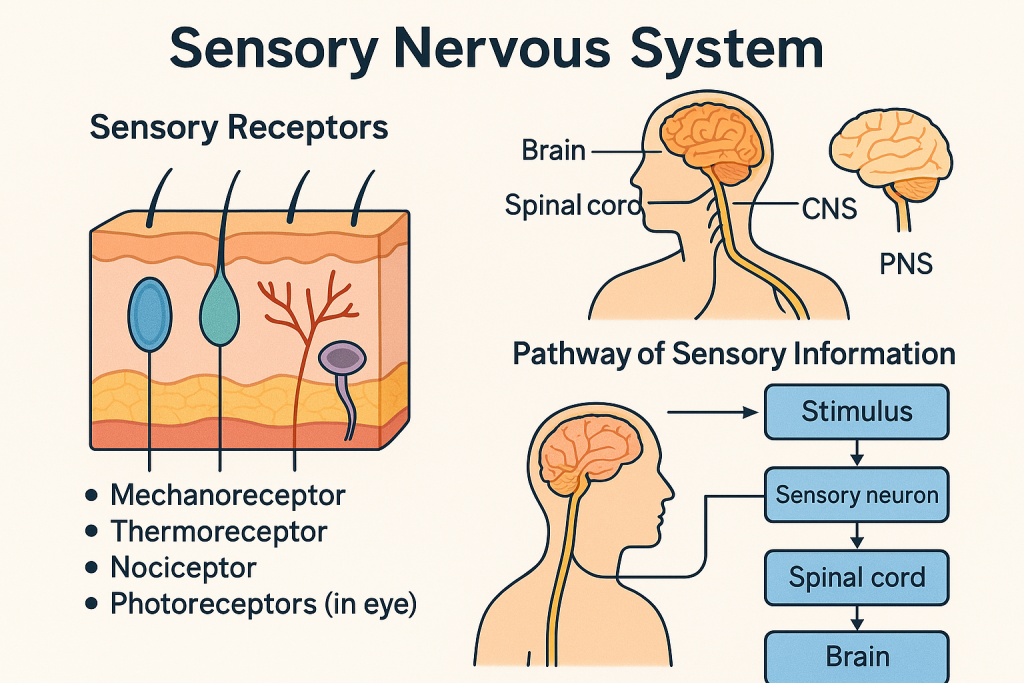
The Sensory Nervous System, also known as the afferent division of the Peripheral Nervous System (PNS), is a vital subsystem responsible for conveying information from the environment (external or internal) to the Central Nervous System (CNS), which includes the brain and spinal cord. It is foundational to perception, reflexes, motor control, and maintaining homeostasis.
🔬 1. Definition
The sensory nervous system is the part of the nervous system that detects sensory stimuli from the external or internal environment and transmits that information to the CNS for processing, integration, and response.
🧩 2. Structural Components
a. Sensory Receptors
These are specialized neurons or epithelial cells capable of detecting changes in the environment. They initiate a sensory impulse in response to:
- Mechanical changes (pressure, stretch)
- Temperature
- Chemical substances
- Light (photons)
- Tissue damage (pain)
b. Afferent Neurons
Also known as sensory neurons, these carry the impulses from receptors to the CNS. Most are pseudo-unipolar neurons, where the cell body lies in a dorsal root ganglion (DRG) or cranial sensory ganglia.
c. Sensory Nerve Pathways
These consist of nerve fibers bundled together that travel through spinal nerves or cranial nerves, reaching the spinal cord or brainstem.
d. CNS Integration Centers
After the impulses reach the CNS, structures like the thalamus, reticular formation, and cerebral cortex (especially the postcentral gyrus in the parietal lobe) process and interpret the stimuli.
🔍 3. Classification of Sensory Modalities
✅ a. General Senses
These are widely distributed throughout the body:
- Somatic Senses: Touch, pain, pressure, temperature, proprioception (sense of body position and movement).
- Visceral Senses: Stretch, chemical changes, temperature, and pain from internal organs.
🌟 b. Special Senses
These are localized to specialized organs:
- Vision (eyes – retina)
- Hearing & Balance (ears – cochlea and vestibular system)
- Olfaction (nose – olfactory epithelium)
- Gustation (tongue – taste buds)
🧠 4. Classification of Sensory Receptors by Stimulus Type
| Receptor | Stimulus Detected | Examples/Location |
|---|---|---|
| Mechanoreceptors | Mechanical deformation (touch, pressure) | Skin, blood vessels, inner ear |
| Thermoreceptors | Temperature changes | Skin (free nerve endings) |
| Nociceptors | Pain (due to damage or inflammation) | Throughout body |
| Photoreceptors | Light (photons) | Retina of eye (rods and cones) |
| Chemoreceptors | Chemical stimuli (O₂, CO₂, pH, taste) | Tongue, nose, medulla oblongata |
| Proprioceptors | Position and movement of body parts | Muscles, tendons (muscle spindles, Golgi tendon organs) |
📤 5. Pathway of Sensory Transmission (Three-Neuron Chain)
🧷 First-order Neuron:
- Originates in the sensory receptor
- Travels through peripheral nerve to spinal cord or brainstem
🧷 Second-order Neuron:
- Located in spinal cord or medulla
- Axon crosses (decussates) to the opposite side and ascends to the thalamus
🧷 Third-order Neuron:
- Arises in thalamus
- Projects to the primary somatosensory cortex (postcentral gyrus)
🛠 6. Functional Role of the Sensory Nervous System
- 🧭 Homeostasis Maintenance: Detects and reports internal changes (e.g., blood pressure, CO₂ levels).
- 🤕 Pain Perception: Protects body by initiating reflexes or conscious responses to harmful stimuli.
- ✋ Touch and Pressure: Allows for tactile discrimination and interaction with environment.
- 🦵 Proprioception: Helps coordinate movement and posture.
- 🧠 Sensory Integration: Assists the brain in decision-making, memory, and motor planning.
🏥 7. Clinical Relevance (Neurological and Nursing Perspective)
| Condition | Description | Nursing Considerations |
|---|---|---|
| Peripheral Neuropathy | Loss of sensory nerve function (e.g., diabetes mellitus) | Assess sensory loss, prevent injury, monitor feet |
| Phantom Limb Pain | Perception of pain in an amputated limb | Emotional support, mirror therapy |
| Stroke (Sensory Loss) | Damage to sensory cortex or pathways → loss of proprioception or touch | Fall risk, rehabilitation, tactile stimulation |
| Multiple Sclerosis | Demyelination affects sensory transmission | Sensory testing, temperature sensitivity management |
| Spinal Cord Injury | Disruption of ascending tracts → sensory deficits below injury level | Pressure sore prevention, neurological checks, positioning |
📌 Insights
- Sensory nerves are exclusively afferent and transmit impulses towards the CNS.
- Sensory input is critical for motor control, reflex arcs, and higher-level processing (e.g., memory, attention).
- Damage to any level of the sensory pathway (receptor, neuron, or CNS) results in sensory impairment.
🧠 Motor Nervous System
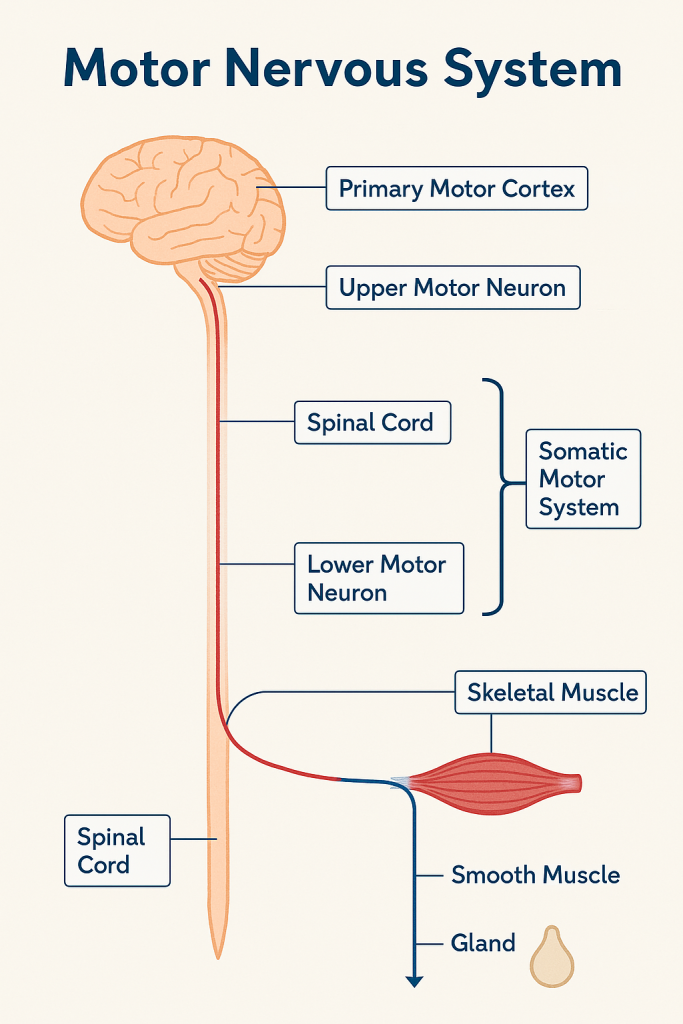
The Motor Nervous System is a subdivision of the Peripheral Nervous System (PNS) that transmits efferent impulses from the Central Nervous System (CNS) to the effector organs (i.e., skeletal muscles, cardiac muscles, smooth muscles, and glands). This system governs both voluntary and involuntary motor activity, thereby enabling movement and internal organ function.
🔍 1. Functional Division of the Motor Nervous System
The motor division is broadly classified into:
🔸 A. Somatic Motor System
- Controls voluntary movements
- Consists of motor neurons that innervate skeletal muscles
- Origin of impulse: Motor cortex (precentral gyrus)
- Final output: Neuromuscular junction releases acetylcholine (ACh), leading to muscle contraction
🔸 B. Autonomic Motor System (Visceral Efferent System)
- Regulates involuntary activities of smooth muscle, cardiac muscle, and glands
- Maintains homeostasis
- Subdivided into:
- Sympathetic Nervous System: Prepares body for “fight or flight”
- Parasympathetic Nervous System: Maintains “rest and digest” functions
- Enteric Nervous System: Regulates the gastrointestinal tract (can function independently or under autonomic control)
🧩 2. Components of the Motor System
| Component | Description |
|---|---|
| Upper Motor Neurons (UMNs) | Originate in cerebral cortex or brainstem; modulate lower motor neurons |
| Lower Motor Neurons (LMNs) | Originate in spinal cord or brainstem; directly innervate muscle fibers |
| Neuromuscular Junction | Specialized synapse where motor neuron communicates with skeletal muscle |
| Effectors | Skeletal muscle (somatic); smooth/cardiac muscle, glands (autonomic) |
🧠 3. Motor Pathways (Descending Tracts)
Motor impulses travel from the brain through descending tracts in the spinal cord:
🔹 Corticospinal Tract (Pyramidal Tract)
- Originates in primary motor cortex
- Passes through internal capsule → medulla (pyramidal decussation) → spinal cord
- Controls voluntary fine motor movements
🔹 Extrapyramidal Tracts
- Originate in brainstem nuclei (e.g., rubrospinal, reticulospinal)
- Involved in posture, balance, and gross motor control
🔁 4. Mechanism of Voluntary Motor Control
- Initiation: Motor cortex plans and initiates the movement
- Transmission: UMNs carry impulse to LMNs
- Execution: LMNs innervate muscles via motor nerves
- Contraction: At neuromuscular junction, ACh binds receptors → depolarization → muscle contracts
🧪 5. Neurotransmitters Involved
| Neurotransmitter | Function |
|---|---|
| Acetylcholine (ACh) | Released at neuromuscular junction (somatic system) |
| Norepinephrine (NE) | Primary neurotransmitter in sympathetic division |
| Acetylcholine (ACh) | Also acts in parasympathetic division (postganglionic neurons) |
⚕️ 6. Clinical Correlation – Motor Deficits
| Disorder | Pathophysiology | Characteristics |
|---|---|---|
| Upper Motor Neuron Lesion | Damage to cortex, internal capsule, corticospinal tract | Spastic paralysis, hyperreflexia, Babinski sign |
| Lower Motor Neuron Lesion | Damage to anterior horn, spinal nerves, cranial nerves | Flaccid paralysis, muscle atrophy, fasciculations |
| Myasthenia Gravis | Autoimmune destruction of ACh receptors at NMJ | Muscle weakness, fatigability |
| Amyotrophic Lateral Sclerosis (ALS) | Degeneration of both UMN and LMN | Mixed spastic and flaccid paralysis |
🩺 7. Relevance in Nursing and Medical Practice
- Assessment of motor function is essential in neurological exams (e.g., reflexes, tone, strength)
- Rehabilitation relies on understanding motor pathways (stroke, SCI)
- Drug administration (e.g., anticholinergics, sympatholytics) targets motor/autonomic nerves
- Patient safety depends on identifying motor impairments (fall risk, aspiration risk)
📌 Key Takeaways
- The motor nervous system transmits efferent signals from the CNS to effectors.
- Divided into somatic (voluntary) and autonomic (involuntary) systems.
- UMN and LMN lesions present with distinct clinical signs.
- Neurotransmitters like ACh and NE play crucial roles in neuromuscular transmission.
- Critical for movement, posture, reflexes, and internal organ regulation.
🌐 Peripheral Nervous System (PNS)
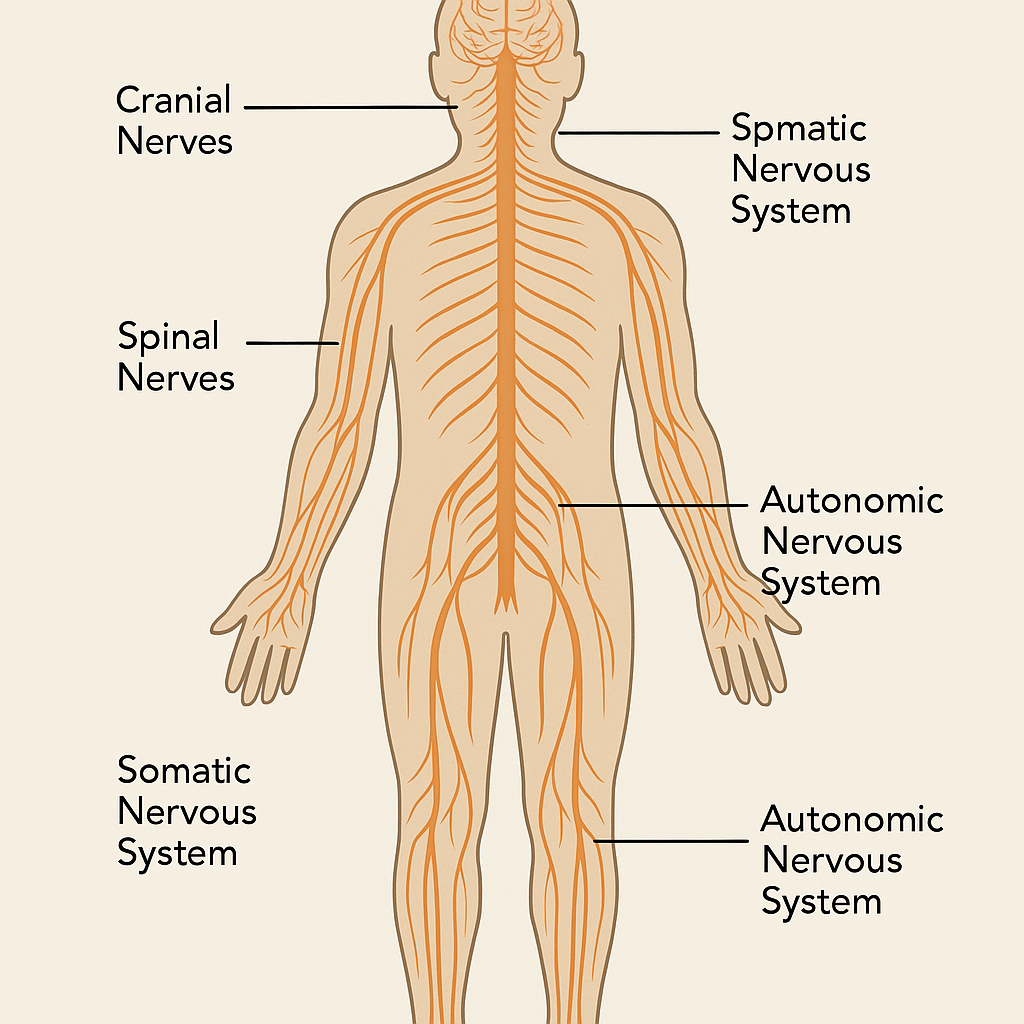
The Peripheral Nervous System (PNS) is a vital component of the human nervous system, working in perfect harmony with the Central Nervous System (CNS) to ensure communication between the brain, spinal cord, and the rest of the body. While the CNS acts as the control center, the PNS serves as a vast network of communication lines that extend out to every organ, limb, and tissue. It enables the body to sense the environment, react to stimuli, and regulate internal functions.
By definition, the Peripheral Nervous System comprises all neural structures located outside the brain and spinal cord. This includes the cranial nerves, which emerge from the brain, and the spinal nerves, which exit the spinal cord. It also includes ganglia (clusters of neuron cell bodies) and peripheral sensory and motor neurons.
In essence, the PNS connects the CNS to every part of the body, ensuring that signals from the brain reach the target organs, and information from the environment or internal organs reaches the brain.
🌟 Structure and Divisions of the PNS
Functionally, the PNS is divided into two main divisions:
🔸 Sensory (Afferent) Division
This division is responsible for carrying information toward the CNS. It includes somatic sensory neurons, which transmit signals like touch, pain, temperature, and proprioception (body position) from the skin, joints, and muscles. It also includes visceral sensory neurons, which monitor internal conditions such as blood pressure, stretch in organs, and chemical changes.
🔸 Motor (Efferent) Division
This is the output system, carrying commands from the CNS to muscles and glands. The motor division is further subdivided into:
- Somatic Nervous System, which controls voluntary movements of skeletal muscles. For instance, walking, picking up a cup, or writing all rely on this system.
- Autonomic Nervous System, which governs involuntary functions such as heart rate, digestion, and respiratory rate. The autonomic system is further split into:
- The Sympathetic Nervous System, which activates the “fight or flight” response during stress, increasing heart rate, dilating pupils, and redirecting blood to muscles.
- The Parasympathetic Nervous System, which promotes “rest and digest” activities, slowing the heart rate and enhancing digestion.
- The Enteric Nervous System, which operates independently to regulate the gastrointestinal tract.
🧩 Anatomy of Peripheral Nerves
Peripheral nerves are like electrical cables, consisting of bundles of axon fibers encased in protective layers. Each individual axon is wrapped in a delicate layer called the endoneurium. Several axons are grouped into bundles known as fascicles, surrounded by the perineurium. The entire nerve, made up of multiple fascicles, is enclosed by the tough epineurium.
These nerves can be:
- Sensory nerves, carrying signals to the brain.
- Motor nerves, sending commands from the brain.
- Or mixed nerves, doing both jobs simultaneously.
⚙️ Functions of the Peripheral Nervous System
The PNS plays several critical roles:
- It enables sensory detection, letting the body perceive stimuli like heat, cold, pain, or balance.
- It facilitates motor control, activating muscles to allow voluntary movements.
- It supports autonomic regulation, keeping vital processes like heartbeat and digestion running smoothly.
- It also mediates reflex actions, which are rapid, automatic responses to stimuli—often bypassing the brain entirely for faster reactions (like pulling your hand away from a hot surface).
⚕️ Clinical Relevance and Nursing Insight
Damage or disease affecting the peripheral nervous system can result in significant functional impairment. For example:
- Peripheral neuropathy, commonly seen in diabetic patients, causes numbness, tingling, and pain in the limbs.
- Guillain-Barré Syndrome, an autoimmune condition, results in rapid-onset muscle weakness due to peripheral nerve demyelination.
- Bell’s palsy involves inflammation of the facial nerve, leading to sudden one-sided facial paralysis.
- Radiculopathy, often caused by herniated discs, can cause sharp pain and weakness along the path of a spinal nerve.
In such conditions, nurses play a vital role in assessing sensory-motor function, preventing complications, supporting rehabilitation, and educating patients about protective measures.
📚
The Peripheral Nervous System is the dynamic communication highway of the body. It serves as the vital link between the central command center (CNS) and the rest of the body, making sure every organ, muscle, and sense is synchronized and responsive. From enabling us to move and feel to ensuring our heart beats and stomach digests, the PNS is indispensable in maintaining both our survival and quality of life.
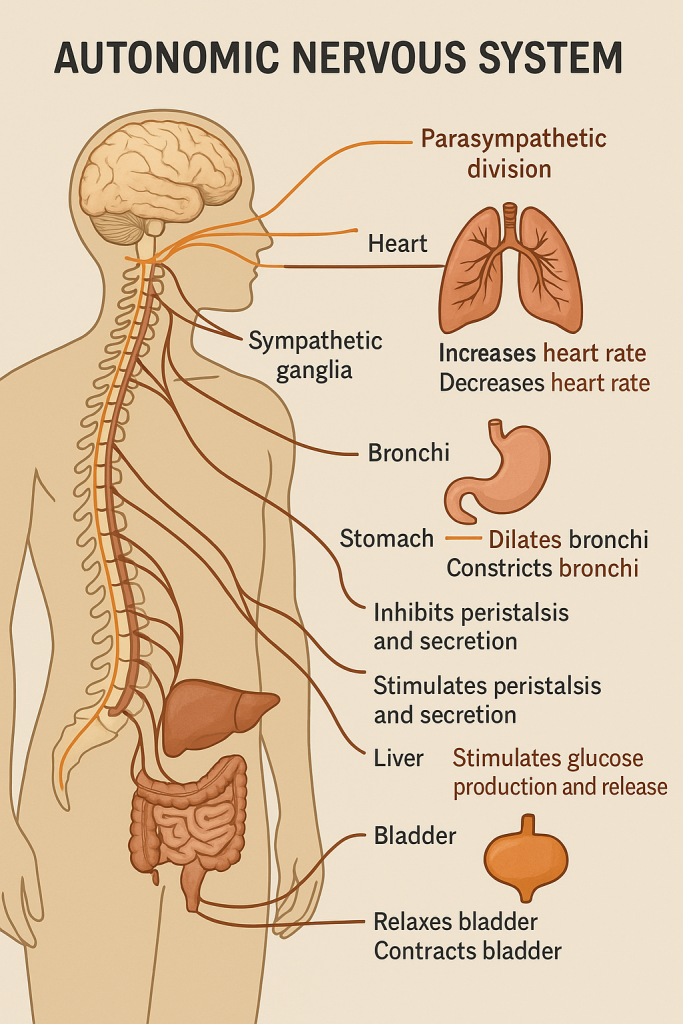
🌐 Autonomic Nervous System (ANS)
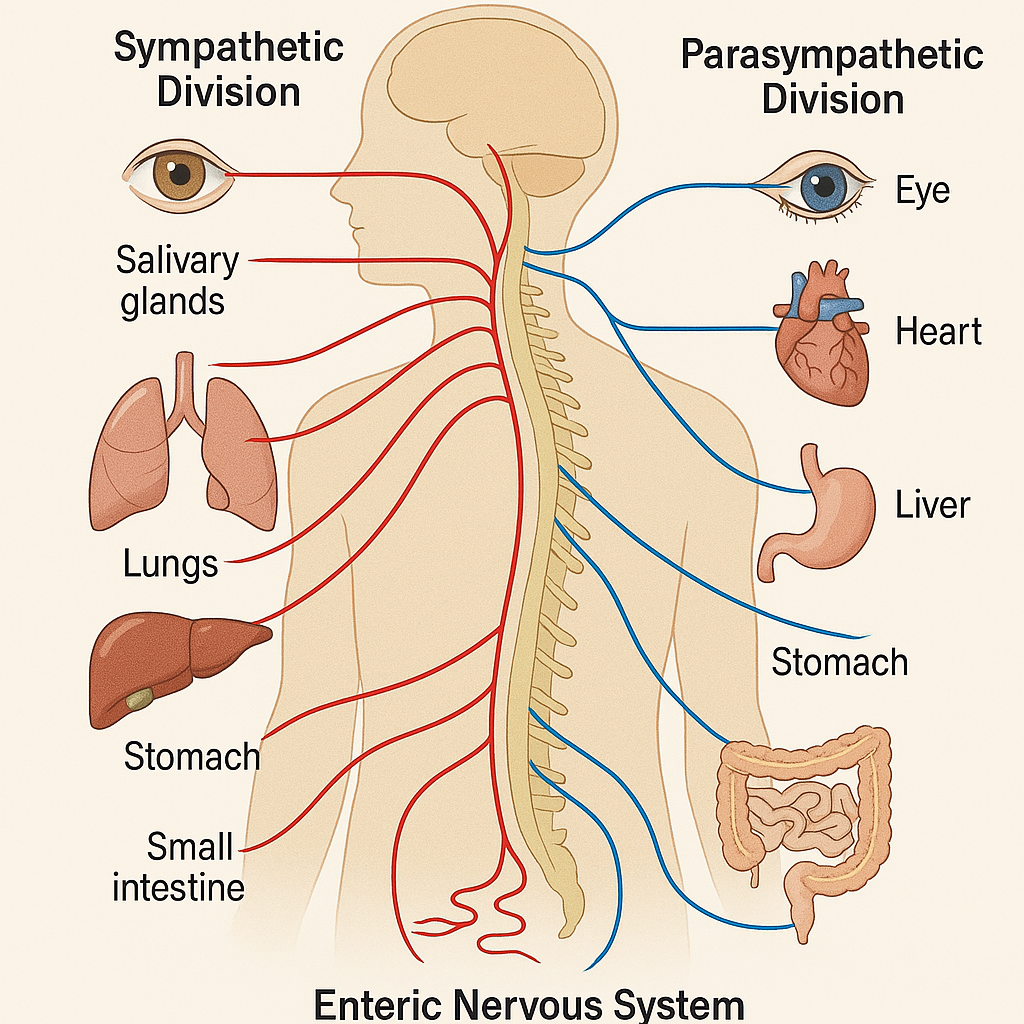
The Autonomic Nervous System (ANS) is a magnificent part of the human body’s communication network — often called the “silent controller” — because it operates in the background, without our conscious awareness. From maintaining heartbeat rhythm to adjusting pupil size and regulating digestion, the ANS keeps our internal environment stable, supporting the body’s homeostasis.
The Autonomic Nervous System is a subdivision of the Peripheral Nervous System (PNS) that controls the involuntary functions of our body. It sends motor commands from the Central Nervous System (CNS) to smooth muscles, cardiac muscles, and glands. Unlike the somatic nervous system, which allows voluntary control over skeletal muscles (like walking or waving), the ANS works automatically, managing vital functions even when we are asleep or unconscious.
⚙️ Core Functions of the ANS
The ANS regulates and integrates the following essential activities:
- ❤️ Heart rate
- 💨 Respiration rate
- 💧 Sweating
- 🌡️ Body temperature
- 🧬 Metabolic processes
- 🍔 Digestive function
- 🧃 Secretion of glands (saliva, hormones, enzymes)
Every second, the ANS makes thousands of adjustments to keep the internal environment balanced — whether you’re resting, running, eating, or emotionally stressed.
🧩 Main Divisions of the Autonomic Nervous System
The ANS has three primary subdivisions, each with distinct but interconnected roles:
🔹 1. Sympathetic Nervous System (SNS) – “Fight or Flight”
This division prepares the body to face emergencies. It’s active during stress, fear, or physical activity.
Key actions include:
- ⬆️ Increases heart rate and blood pressure
- ⬆️ Dilates bronchi for faster breathing
- ⬆️ Dilates pupils to enhance vision
- ⬇️ Slows down digestion
- ⬆️ Stimulates sweat glands
- Releases adrenaline (epinephrine) from the adrenal medulla
This system ensures your body is energized and alert to deal with danger — whether it’s escaping a threat or reacting quickly to a crisis.
🔹 2. Parasympathetic Nervous System (PNS) – “Rest and Digest”
This division restores energy and promotes calm and relaxation. It takes over when you’re at rest or after eating.
Key actions include:
- ⬇️ Slows down heart rate
- ⬇️ Constricts pupils
- ⬇️ Promotes digestive secretions and gut motility
- ⬆️ Stimulates urination and defecation
- Enhances glandular secretions (e.g., saliva)
This system helps the body to conserve energy, recover from stress, and support healing.
🔹 3. Enteric Nervous System (ENS) – “Gut Brain”
Sometimes called the “second brain”, the enteric nervous system is a vast network of neurons embedded in the wall of the gastrointestinal (GI) tract. It controls:
- Intestinal motility (peristalsis)
- Secretion of digestive enzymes
- Absorption and excretion
The ENS can function independently of the brain and spinal cord but usually operates in coordination with the sympathetic and parasympathetic systems.
🧪 Anatomical and Physiological Characteristics
- The autonomic pathway typically involves two neurons:
- A preganglionic neuron, which arises from the brainstem or spinal cord and ends in a ganglion.
- A postganglionic neuron, which carries the impulse from the ganglion to the target organ (e.g., heart, lung, gland).
- Neurotransmitters used by the ANS:
- Acetylcholine (ACh): Used by all preganglionic neurons and most parasympathetic postganglionic neurons.
- Norepinephrine (NE): Secreted by most sympathetic postganglionic neurons, causing actions like vasoconstriction and increased heart rate.
⚕️ Clinical Relevance – Why Nurses and Clinicians Must Understand the ANS
Understanding the ANS is crucial in both acute and chronic care. Many conditions are directly linked to autonomic function, including:
- Autonomic Dysreflexia in spinal cord injury patients — a life-threatening condition.
- Orthostatic Hypotension, where standing up suddenly causes a drop in BP.
- Diabetic Neuropathy, where poor blood sugar control damages autonomic fibers.
- Use of drugs like beta-blockers, anticholinergics, and sympathomimetics—all affect ANS targets and pathways.
- Stress management, patient comfort, pain perception, and even emotional support involve autonomic regulation.
📚 Key Takeaways
✅ The Autonomic Nervous System is automatic, essential, and ever-active.
✅ It governs the inner workings of organs without conscious effort.
✅ It is split into sympathetic (emergency) and parasympathetic (recovery) systems, along with the enteric nervous system in the gut.
✅ It uses neurotransmitters like ACh and NE to carry out its tasks.
✅ From emergency response to digestion and rest, the ANS protects, balances, and restores the body continuously.
🧠 Limbic System and Higher Mental Functions
The human brain is not just an organ of logic and memory — it is the center of emotion, creativity, decision-making, and personality. Deep within its folds lies a powerful network of structures collectively known as the limbic system, the seat of emotion and memory. Surrounding and interacting with it are higher mental functions, the abilities that define what it means to be human — thinking, reasoning, learning, and feeling.
The limbic system is a group of interconnected deep brain structures located just beneath the cerebral cortex and surrounding the brainstem. The word “limbic” comes from the Latin limbus, meaning “border,” reflecting its location at the border between the cerebrum and the diencephalon.
Though traditionally known for emotion, the limbic system is essential for memory formation, learning, instinctive behavior, and even motivation and olfaction.
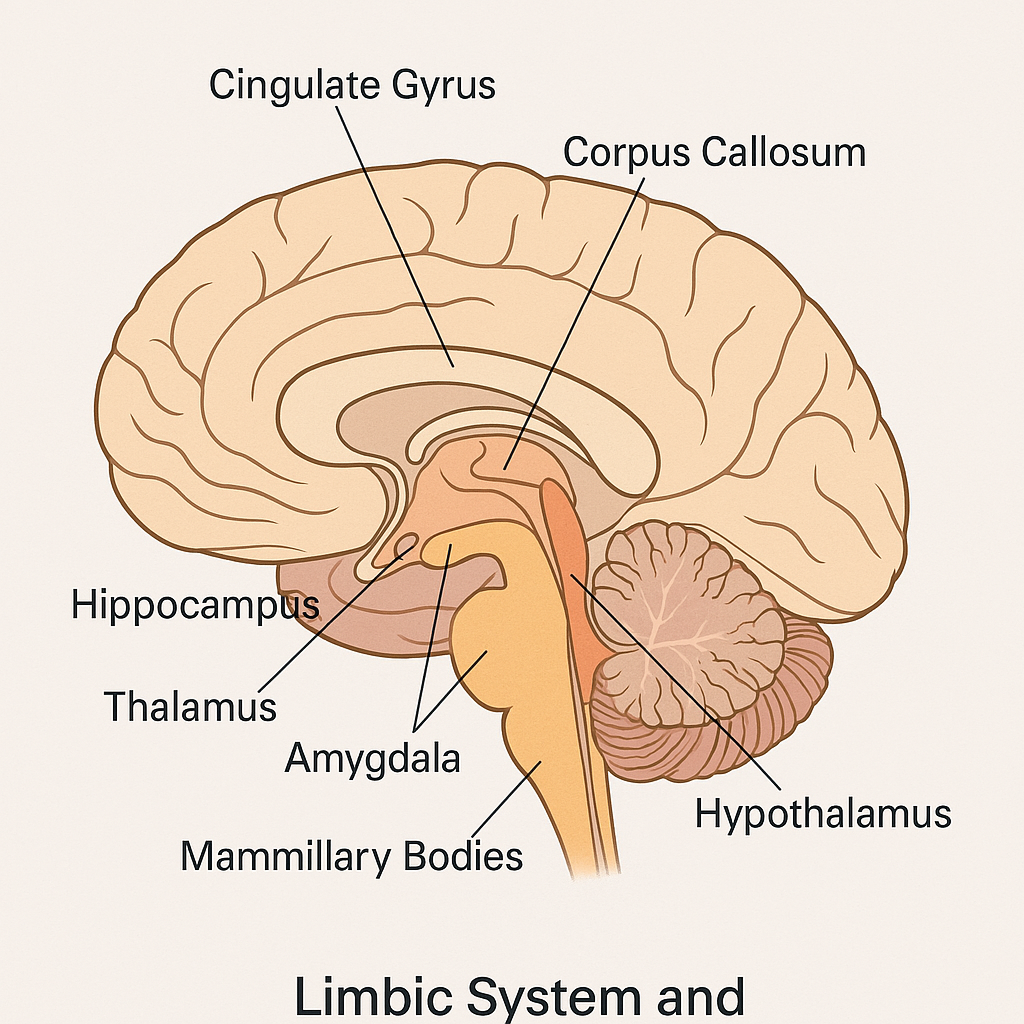
🧩 Major Structures of the Limbic System
- Hypothalamus – The master regulator of the autonomic nervous system and endocrine system. It links emotion to physiological responses (like increased heart rate when afraid).
- Amygdala – Known as the “fear center.” It processes emotions like fear, anger, and pleasure, and plays a role in aggressive behavior and emotional memory.
- Hippocampus – Essential for forming new long-term memories and spatial navigation. Damage can cause short-term memory loss.
- Thalamus – Acts as a relay station, channeling sensory information to appropriate cortical areas.
- Cingulate Gyrus – Involved in emotional regulation and linking behavioral outcomes to motivation.
- Mammillary Bodies – Involved in recollective memory.
- Olfactory Bulbs – Closely linked to the limbic system, explaining why smells often trigger emotional memories.
💭 Functions of the Limbic System
The limbic system contributes to:
- 🌈 Emotions (fear, anger, love, pleasure)
- 🔁 Memory formation and retrieval
- 🚨 Behavioral responses to stimuli
- 🧃 Hormonal regulation (through the hypothalamus)
- 🧠 Autonomic nervous system responses
- 🧩 Learning and motivation
- 👃 Olfactory processing
Its deep interconnections with both autonomic and cognitive systems make it central to integrating emotional and physiological responses — such as crying when sad or blushing when embarrassed.
🧠 Higher Mental Functions
Beyond emotions, the cerebral cortex — especially the frontal, parietal, temporal, and occipital lobes — orchestrates higher mental functions, which are unique to humans and some primates. These functions allow us to reason, reflect, learn, create, and express conscious awareness.
📘 Key Higher Mental Functions and Their Brain Centers
🔹 1. Consciousness
- Maintained by the reticular activating system (RAS) and cortex.
- Represents alertness, awareness, and the ability to respond to the environment.
🔹 2. Memory
- Short-term memory is associated with the prefrontal cortex.
- Long-term memory is stored across the cortex but requires the hippocampus to form.
- Emotional memories are closely tied to the amygdala.
🔹 3. Learning
- Involves hippocampus, cortex, and cerebellum (especially for motor learning).
- Influenced by repetition, emotional state, and motivation.
🔹 4. Language
- Broca’s area (frontal lobe): Speech production
- Wernicke’s area (temporal lobe): Language comprehension
🔹 5. Reasoning and Judgment
- Managed by the prefrontal cortex, responsible for decision-making, impulse control, and planning.
🔹 6. Personality
- Also shaped by the frontal lobe, particularly the orbitofrontal cortex.
🧠✨ The Mind-Emotion Connection
The interaction between the limbic system and higher cortical areas is what gives rise to complex behaviors. For example:
- A memory (hippocampus) can trigger a strong emotional reaction (amygdala).
- An emotion (fear) can influence decision-making (prefrontal cortex).
- Logical thought can suppress emotional reactions, showing cognitive control over feelings.
This integration is what makes human behavior so nuanced — we don’t just react; we feel, think, remember, and choose.
⚕️ Clinical Insight and Relevance
A deep understanding of the limbic system and higher functions is essential for recognizing and treating many conditions:
- Alzheimer’s Disease: Begins in the hippocampus, leading to memory loss.
- Anxiety and PTSD: Linked to overactivity of the amygdala and impaired inhibition from the prefrontal cortex.
- Frontal Lobe Injuries: Affect judgment, personality, and decision-making (seen in head trauma or stroke).
- Depression: Related to altered activity in limbic and prefrontal areas.
Nurses and health professionals play a key role in assessing cognitive function, emotional regulation, and memory in patients through both observation and structured assessments.
📌 Summary in a Nutshell
- The limbic system is the emotional and memory center of the brain.
- It includes the amygdala, hippocampus, hypothalamus, thalamus, and others.
- Higher mental functions such as consciousness, learning, memory, language, and judgment are coordinated by the cerebral cortex, especially the frontal lobe.
- These systems are interconnected, and their harmony is essential for emotional balance, rational thinking, and memory.
- Dysfunction can lead to neuropsychiatric and cognitive disorders, making this topic critical for clinical practice.
🧠 Hippocampus – The Memory Maker of the Brain
Tucked deep within the folds of the temporal lobe lies a seahorse-shaped structure that plays a starring role in how we form, store, and retrieve memories — this is the hippocampus. More than just a memory center, the hippocampus is a navigation guide, a learning engine, and a bridge between the past and present. Its elegant role in the brain is essential to our identity, experience, and even survival.
📍 What Is the Hippocampus?
The hippocampus is a paired, curved structure situated in the medial temporal lobe, forming a crucial part of the limbic system, the brain’s emotional and memory-processing hub. Its name comes from the Greek word hippokampos, meaning “seahorse,” due to its unique curved shape.
It is bilaterally located — with one hippocampus in each hemisphere — and lies beneath the cortical surface, just under the cerebral cortex and near the amygdala.
🔬 Anatomical Structure of the Hippocampus
The hippocampus consists of:
- Dentate Gyrus – Involved in new memory formation and pattern separation.
- Cornu Ammonis (CA1–CA4) – Subregions critical for memory encoding and consolidation.
- Subiculum – Acts as an output structure, relaying hippocampal signals to other brain areas.
These interconnected zones form a trisynaptic circuit — a looped network that processes, refines, and sends information to and from the hippocampus.
🧠 Functions of the Hippocampus
The hippocampus plays multiple essential roles, especially in:
📌 1. Memory Formation
The most well-known role of the hippocampus is in converting short-term memories into long-term memories. It acts like a biological recording system, taking experiences, encoding them, and preparing them for storage across the cerebral cortex.
📌 2. Spatial Navigation
The hippocampus allows us to navigate physical spaces by creating cognitive maps. It helps us remember directions, layouts of rooms, or routes between places. Specialized neurons called place cells become active when we’re in or recalling specific locations.
📌 3. Learning
It is central to declarative learning — especially learning facts and events (episodic and semantic memory). Students and professionals alike rely heavily on hippocampal function when studying or remembering clinical procedures.
📌 4. Emotional Regulation
Through its connections with the amygdala, the hippocampus contributes to the emotional coloring of memories, such as remembering a joyful celebration or a traumatic event.
🧪 Neurochemical Aspects
Neurotransmitters important to hippocampal function include:
- Glutamate – The primary excitatory neurotransmitter involved in memory encoding.
- Acetylcholine – Vital for learning and attention; heavily active during memory tasks.
- GABA – Helps regulate excessive excitatory activity.
- Cortisol – Chronic stress and high cortisol levels can shrink the hippocampus and impair memory.
⚠️ Clinical Relevance
Damage or degeneration of the hippocampus can lead to severe cognitive impairments, especially involving memory:
🧠 Alzheimer’s Disease
- One of the earliest brain regions affected.
- Leads to progressive memory loss, especially of recent events.
🧠 Anterograde Amnesia
- Patients are unable to form new long-term memories following damage (as seen in classic cases like patient H.M.).
🧠 Stress and Depression
- Prolonged stress and high cortisol levels shrink the hippocampus, contributing to memory difficulties and mood disorders.
🧠 Temporal Lobe Epilepsy
- Often originates in the hippocampus; surgical removal may be needed but can impair memory further.
👩⚕️ Nursing and Medical Application
Healthcare professionals must understand hippocampal function to:
- Assess cognitive and memory impairments
- Provide patient-centered care in neurodegenerative diseases
- Recognize early signs of dementia
- Support memory-boosting strategies through mental stimulation, nutrition, and stress management
📚 Fascinating Facts
- The hippocampus is one of the few brain areas capable of neurogenesis (creating new neurons) throughout life — especially during learning and exercise.
- Physical activity, sleep, and a rich learning environment can boost hippocampal health.
- Emotional trauma can impair hippocampal function, underscoring the mind-body connection.
🧾 In Summary
The hippocampus is the heart of memory — an elegant, complex structure that allows us to learn, remember, and navigate our world. It is small in size but enormous in influence, linking our past to our present and guiding our actions into the future. Its preservation and protection are critical for cognitive health, emotional stability, and personal identity.
🧠 Thalamus – The Brain’s Grand Central Station
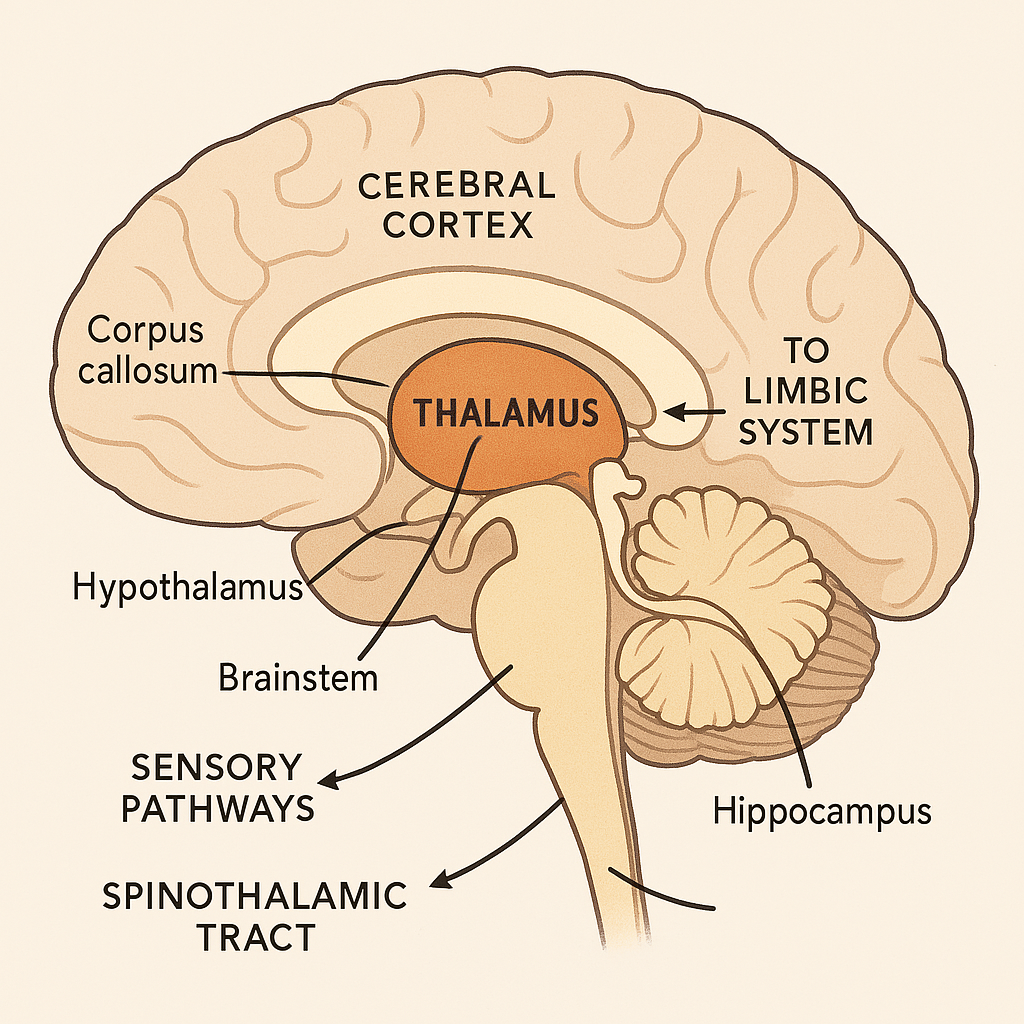
Imagine a train station at the heart of a bustling city — sorting, directing, and coordinating information to and from every corner. That’s the thalamus for the human brain. Acting as the relay center and gateway to consciousness, the thalamus plays a pivotal role in sensation, attention, alertness, and coordination. Every time you see, hear, feel, or even think clearly, your thalamus is working behind the scenes — managing the traffic of data flowing between the body and brain.
📍 What is the Thalamus?
The thalamus is a paired, egg-shaped structure located deep in the center of the brain, just above the brainstem and nestled between the two cerebral hemispheres. It is part of the diencephalon, which also includes the hypothalamus, epithalamus, and subthalamus.
Composed of gray matter, the thalamus consists of multiple nuclei, each with specific roles and connections to different parts of the brain. Its central location and widespread connections make it indispensable for sensory and motor processing, as well as cognitive and emotional functions.
🧩 Anatomical Connections and Structure
Each thalamus (one on either side of the third ventricle) connects to almost all parts of the cerebral cortex. It is divided into multiple functional nuclei:
- Sensory relay nuclei (e.g., lateral geniculate nucleus for vision, medial geniculate nucleus for hearing)
- Motor relay nuclei (connected to basal ganglia and cerebellum)
- Association nuclei (linked to memory, learning, and attention)
- Intralaminar nuclei (involved in arousal and consciousness)
These nuclei make the thalamus a hub that filters, processes, and relays information to the appropriate cortical area.
🔬 Functions of the Thalamus
The thalamus is more than a passive relay — it actively shapes the information we perceive, prioritizing some inputs while downplaying others.
🔹 1. Sensory Relay
Almost all sensory signals (except smell) pass through the thalamus before reaching the cerebral cortex. Whether it’s a gentle breeze on the skin or the color of the sunset, the thalamus processes and forwards this information to the appropriate sensory cortex.
🔹 2. Motor Integration
The thalamus works with the basal ganglia and cerebellum to regulate voluntary motor control by relaying motor signals from these structures to the motor cortex.
🔹 3. Consciousness and Alertness
Through connections with the reticular activating system (RAS) and cerebral cortex, the thalamus regulates wakefulness, alertness, and levels of consciousness. When thalamic activity is disrupted, consciousness can fade (e.g., coma).
🔹 4. Pain Perception
It plays a role in processing pain signals, especially emotional and affective responses to pain, linking it to limbic structures like the cingulate gyrus.
🔹 5. Memory and Emotion
Thalamic nuclei also help process emotional experiences, and some are closely connected to the hippocampus and amygdala, supporting learning and emotional memory.
🧠 Thalamus and the Limbic System
The thalamus is not just a sensory filter — it’s also a part of the limbic system, involved in emotions, behavior, and motivation. Its links to the prefrontal cortex and limbic structures help it contribute to complex functions like attention, judgment, and affect regulation.
⚠️ Clinical Relevance and Nursing Significance
Damage to the thalamus, though rare, can have devastating effects. Conditions associated with thalamic dysfunction include:
🧠 Thalamic Stroke
- May cause sensory loss, hemiparesis, or thalamic pain syndrome
- Symptoms: burning, aching, or stabbing pain on the opposite side of the body (Dejerine–Roussy syndrome)
🧠 Thalamic Tumors or Lesions
- Can affect consciousness, coordination, and language processing
🧠 Coma and Disorders of Consciousness
- Since the thalamus regulates arousal, damage can lead to coma, vegetative states, or disorientation
🧠 Neurodegenerative Disorders
- In Alzheimer’s disease and schizophrenia, thalamic nuclei show volume reduction and connectivity loss, affecting memory and cognition.
Nursing professionals should be alert to changes in sensory perception, mental status, consciousness level, and movement coordination in patients with suspected thalamic involvement. Understanding the thalamus’ role aids in neurological assessments and early intervention.
📚 In Summary
- The thalamus is the brain’s relay and filtering station, crucial for directing sensory, motor, cognitive, and emotional information to the right places.
- It determines what sensory information reaches your conscious mind.
- Beyond a relay, it is an integrator, a gatekeeper, and a consciousness coordinator.
- Its dysfunction may lead to sensory loss, pain disorders, or even altered states of awareness.
🎯 Vestibular Apparatus – The Balance System of the Inner Ear
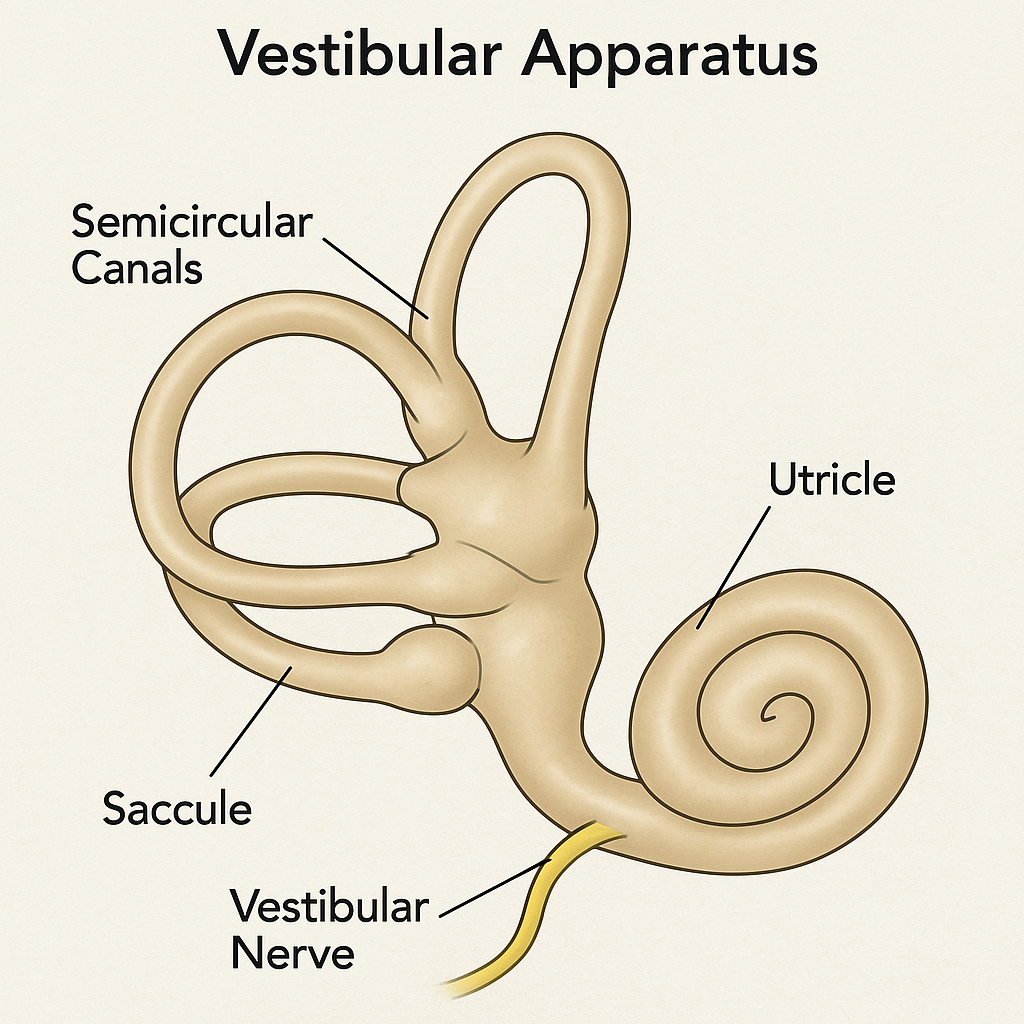
Have you ever wondered how you stay upright while walking, dancing, or even standing on one foot with your eyes closed? The answer lies deep within your inner ear — in a structure no bigger than a grape — called the vestibular apparatus. This finely tuned system allows the brain to detect motion, gravity, and spatial orientation, ensuring balance, posture, and coordinated movement.
It’s not just about standing still — it’s about surviving gravity and maintaining stability through every step, tilt, and turn.
🧠 What is the Vestibular Apparatus?
The vestibular apparatus is a specialized structure located within the inner ear (labyrinth). It is a part of the vestibular system, which includes:
- The peripheral sensory structures in the inner ear
- The vestibular nerve
- Brainstem vestibular nuclei
- The cerebellum and cerebral cortex
Together, these components help the body sense and respond to changes in head position and motion. It is housed within the bony labyrinth of the temporal bone and filled with fluid, hair cells, and nerve fibers that detect movement.
🧩 Structural Components of the Vestibular Apparatus
The vestibular apparatus consists of two main types of structures:
🔹 1. The Semicircular Canals – Detect rotational (angular) movement
There are three semicircular canals arranged in three planes (horizontal, anterior, posterior) — like a 3D gyroscope.
Each canal contains:
- Endolymph fluid
- A widened area called the ampulla, which houses the crista ampullaris
- Hair cells in the crista, topped with stereocilia and kinocilium, detect head rotation
When you rotate your head, the fluid lags behind, bending the hair cells, and sending impulses via the vestibular nerve to the brain.
🔹 2. The Otolith Organs – Detect linear acceleration and gravity
These include the:
- Utricle: Detects horizontal movement (e.g., walking forward)
- Saccule: Detects vertical movement (e.g., jumping or going in an elevator)
Each contains:
- A sensory epithelium called the macula
- Calcium carbonate crystals called otoliths sit atop a gelatinous layer
- When the head moves or tilts, gravity causes these otoliths to shift, bending the hair cells beneath them and triggering nerve signals
🎢 How Does the Vestibular Apparatus Work?
- Head movement causes fluid displacement or otolith movement in the vestibular organs
- This movement bends hair cells, which generate electrical impulses
- Impulses travel through the vestibular portion of the vestibulocochlear nerve (CN VIII)
- Signals are processed in the vestibular nuclei in the brainstem and relayed to:
- Cerebellum (for coordination)
- Oculomotor centers (for eye movement)
- Spinal cord (for postural adjustments)
- Cerebral cortex (for perception of balance)
🔁 Vestibulo-Ocular Reflex (VOR) – Stabilizing Vision
This reflex keeps your gaze steady while your head moves. For example, when you turn your head to the right, your eyes automatically move to the left to maintain visual fixation. This reflex is crucial for balance, reading, and navigating your environment.
🧪 Neurophysiological Integration
The vestibular system is intricately connected to:
- The Cerebellum – for refining motor activity and equilibrium
- The Brainstem (Vestibular Nuclei) – for integrating sensory input
- The Spinal Cord – to adjust posture via vestibulospinal tracts
- The Extraocular Muscles – for coordinated eye movements
It works hand-in-hand with visual and proprioceptive inputs to maintain overall balance.
⚠️ Clinical Relevance – Vestibular Dysfunction
Disorders of the vestibular system can lead to disturbing and disabling symptoms, such as:
🌀 Vertigo
A sensation of spinning caused by disturbances in the semicircular canals (e.g., Benign Paroxysmal Positional Vertigo – BPPV)
🌊 Meniere’s Disease
Increased endolymph pressure causes hearing loss, tinnitus, and episodic vertigo
🤕 Labyrinthitis or Vestibular Neuritis
Inflammation of inner ear structures or vestibular nerve, leading to acute vertigo, imbalance, nausea
⚖️ Vestibular Hypofunction (Unilateral/Bilateral)
Results in chronic dizziness, imbalance, and motion sensitivity
👩⚕️ Importance in Nursing and Medical Practice
Nurses and clinicians must assess vestibular function when patients report:
- Sudden dizziness or vertigo
- Imbalance or unsteadiness
- Nausea without gastrointestinal cause
- Falls or difficulty walking
Bedside tests like the Romberg test, head thrust test, and Dix-Hallpike maneuver help evaluate vestibular function. Early recognition aids in referral to ENT or neurology and implementation of vestibular rehabilitation therapy.
📚 In Summary
- The vestibular apparatus is the body’s balance and motion detector located in the inner ear
- It includes the semicircular canals (detect rotational movement) and otolith organs (detect linear acceleration and gravity)
- It communicates with the brainstem, cerebellum, and eyes to maintain balance, posture, and spatial orientation
- Vestibular disorders can cause vertigo, nausea, unsteadiness, and fall risk
It’s a silent guardian — keeping you upright, steady, and oriented with every step and turn you take.
🧠 Cranial Nerves – The Twelve Pairs of Neural Pathways Connecting the Brain to the Body
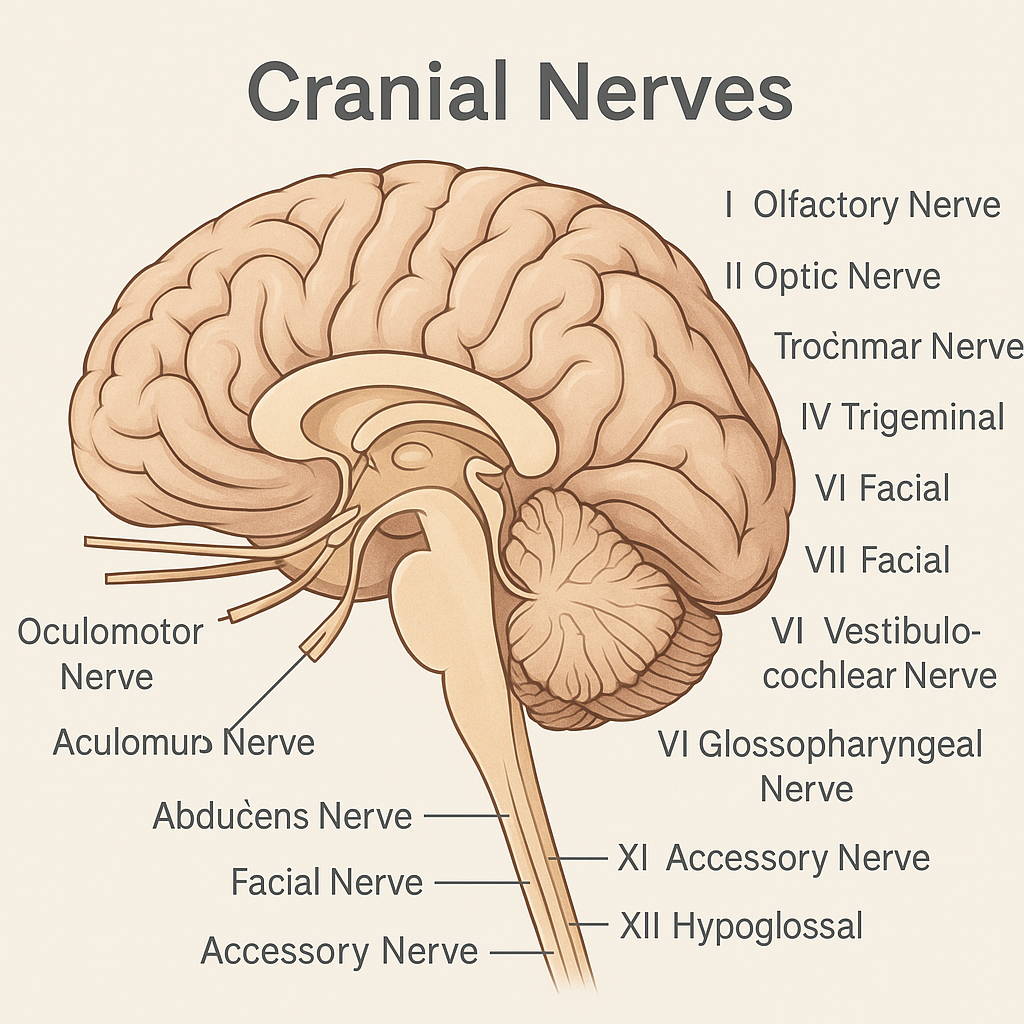
The human body is orchestrated by a sophisticated nervous system, and among its most remarkable components are the cranial nerves — twelve pairs of nerves that arise directly from the brain and brainstem. These nerves serve as direct communication lines between the brain and structures of the head, neck, and trunk, regulating vital sensory, motor, and autonomic functions.
Cranial nerves allow you to smell, see, blink, smile, taste, speak, swallow, and even digest. In essence, they are responsible for much of what makes us humanly expressive and functionally adaptive.
🧩 Overview of the Cranial Nerves
There are 12 pairs of cranial nerves, numbered I through XII, based on their attachment site to the brain (from anterior to posterior). Some are purely sensory, others are purely motor, and many are mixed — performing both sensory and motor functions.
🧠 Mnemonic for names:
“Oh, Oh, Oh, To Touch And Feel Very Green Vegetables, AH!”
🧠 Mnemonic for function (Sensory/Motor):
“Some Say Marry Money, But My Brother Says Big Brains Matter Most.”
📘 Detailed Functions of Each Cranial Nerve
🔹 I. Olfactory Nerve (Sensory)
- Function: Smell
- Location: Originates in the olfactory bulb and projects to the nasal mucosa
- Clinical relevance: Damage results in anosmia (loss of smell)
- Nursing Tip: Test with aromatic substances (e.g., coffee, vanilla)
🔹 II. Optic Nerve (Sensory)
- Function: Vision
- Location: Connects retina to the brain’s visual cortex
- Clinical relevance: Lesions cause visual field defects, blindness
- Nursing Tip: Visual acuity and visual field testing are key
🔹 III. Oculomotor Nerve (Motor)
- Function: Controls most eye movements, pupil constriction, and eyelid elevation
- Clinical relevance: Paralysis causes ptosis, diplopia, and pupil dilation
- Nursing Tip: Assess extraocular movements and pupillary response to light
🔹 IV. Trochlear Nerve (Motor)
- Function: Moves the eyeball down and laterally via the superior oblique muscle
- Clinical relevance: Lesions cause vertical diplopia
- Nursing Tip: Have patient look downward and inward
🔹 V. Trigeminal Nerve (Mixed)
- Function:
- Sensory: Face, scalp, cornea, nasal & oral cavities
- Motor: Muscles of mastication (chewing)
- Clinical relevance:
- Trigeminal neuralgia causes excruciating facial pain
- Corneal reflex lost in lesions
- Nursing Tip: Test light touch/pain across face and ability to chew
🔹 VI. Abducens Nerve (Motor)
- Function: Abducts the eyeball (lateral movement via lateral rectus)
- Clinical relevance: Strabismus or diplopia due to loss of lateral eye movement
- Nursing Tip: Observe for eye deviation on lateral gaze
🔹 VII. Facial Nerve (Mixed)
- Function:
- Motor: Facial expressions, eyelid closure
- Sensory: Taste from anterior 2/3 of tongue
- Autonomic: Lacrimal and salivary glands
- Clinical relevance:
- Bell’s palsy = unilateral facial paralysis
- Dry eyes, loss of taste
- Nursing Tip: Ask patient to smile, raise eyebrows, puff cheeks
🔹 VIII. Vestibulocochlear Nerve (Sensory)
- Function:
- Vestibular: Balance
- Cochlear: Hearing
- Clinical relevance: Hearing loss, vertigo, tinnitus, balance problems
- Nursing Tip: Perform Rinne and Weber tests, assess gait and equilibrium
🔹 IX. Glossopharyngeal Nerve (Mixed)
- Function:
- Sensory: Taste from posterior 1/3 of tongue, pharynx sensation
- Motor: Swallowing
- Autonomic: Parotid salivary secretion
- Clinical relevance: Absent gag reflex, difficulty swallowing
- Nursing Tip: Elicit gag reflex, assess taste and swallowing
🔹 X. Vagus Nerve (Mixed)
- Function:
- Motor: Swallowing, speech
- Sensory: Sensation from thoracic/abdominal organs
- Autonomic: Heart rate, digestion, bronchial secretion
- Clinical relevance: Hoarseness, loss of gag reflex, GI disturbances
- Nursing Tip: Monitor voice, cough, swallowing, and heart rate
🔹 XI. Accessory Nerve (Motor)
- Function: Controls sternocleidomastoid and trapezius muscles (head and shoulder movement)
- Clinical relevance: Shoulder droop, head turning weakness
- Nursing Tip: Ask patient to shrug shoulders or turn head against resistance
🔹 XII. Hypoglossal Nerve (Motor)
- Function: Controls tongue movement for speech and swallowing
- Clinical relevance: Tongue deviation, dysarthria, dysphagia
- Nursing Tip: Ask patient to stick out tongue and move side-to-side
🧠 Clinical Integration for Nurses and Clinicians
Understanding cranial nerve function is essential in:
- Neurological examinations
- Identifying stroke syndromes
- Diagnosing tumors, infections, and nerve palsies
- Evaluating head trauma
- Assessing swallowing, speech, facial symmetry, and eye function
Each cranial nerve test is a clue in the neurological puzzle — helping pinpoint where dysfunction lies and guiding further evaluation or emergency intervention.
🧾 In Summary
- There are 12 cranial nerves, each with unique sensory, motor, or autonomic functions
- They originate from the brain, not the spinal cord
- They govern everything from smell and sight to speech, swallowing, heart rate, and balance
- Cranial nerve assessment is a core skill in nursing, neuro, and ENT practice
🌐 Autonomic Functions – The Silent Controllers of Body Physiology
Your heart beats, your lungs breathe, your stomach digests — all without a single conscious thought. This silent symphony is orchestrated by the autonomic nervous system (ANS), a remarkable division of the nervous system that regulates the body’s involuntary functions. From sweating in the heat to your pupils dilating in the dark, the ANS ensures that the internal environment remains stable and responsive.
It’s like having an internal autopilot that reacts, regulates, and restores — 24 hours a day, without sleep or break.
🧠 What Are Autonomic Functions?
Autonomic functions are those that are carried out automatically, without conscious control, to maintain homeostasis (internal balance). These functions are mediated by the autonomic nervous system, which innervates smooth muscle, cardiac muscle, and glands.
They include essential physiological processes such as:
- Heart rate and rhythm
- Blood pressure regulation
- Breathing rate and depth
- Digestive motility and secretion
- Pupillary responses
- Body temperature control
- Bladder control
- Sexual arousal and reproduction
- Metabolic and hormonal regulation
🧩 Divisions of the Autonomic Nervous System and Their Roles
The ANS is functionally divided into three parts, each with distinct yet complementary roles:
🔹 1. Sympathetic Nervous System (SNS) – “Fight or Flight”
This division prepares the body for action in response to stress or danger. It increases energy expenditure and prioritizes survival.
Key sympathetic functions include:
- 🫀 Increased heart rate and force of contraction
- 🫁 Bronchodilation – more air to lungs
- 👁️ Pupil dilation – improved vision in darkness
- 💧 Sweating
- ⬆️ Blood flow to muscles, ⬇️ to GI tract
- 🧃 Inhibition of digestion and urine formation
- ⚠️ Release of adrenaline from adrenal medulla
🔹 2. Parasympathetic Nervous System (PNS) – “Rest and Digest”
This division promotes energy conservation and recovery. It is most active during rest and after meals.
Key parasympathetic functions include:
- 💓 Slowed heart rate
- 🫁 Bronchoconstriction
- 👁️ Pupil constriction
- 🍽️ Increased digestive secretion and motility
- 🧃 Salivation, lacrimation, and urination
- 🧠 Promotion of calmness and healing
🔹 3. Enteric Nervous System (ENS) – “The Gut Brain”
Embedded in the wall of the gastrointestinal tract, the ENS operates semi-independently to control:
- 🌀 Peristalsis (gut movement)
- 🧃 Secretion of digestive enzymes and hormones
- 🧠 Local reflexes in digestion Though it communicates with the sympathetic and parasympathetic systems, it can function autonomously.
🔄 How Autonomic Functions Are Controlled
The control centers for autonomic functions are located in:
- Hypothalamus – the master regulator of autonomic output
- Brainstem centers (e.g., medulla oblongata for cardiovascular and respiratory control)
- Spinal cord – especially for sympathetic output and reflexes
- Cerebral cortex and limbic system – influence autonomic responses to emotions (e.g., blushing when embarrassed)
The autonomic reflex arc is similar to the somatic one, but it involves two neurons:
- Preganglionic neuron: Originates in CNS
- Postganglionic neuron: Extends to target organ
Neurotransmitters involved:
- Acetylcholine (ACh) – used by parasympathetic neurons and some sympathetic neurons
- Norepinephrine (NE) – mainly used by sympathetic postganglionic neurons
- Epinephrine – secreted by adrenal medulla into the bloodstream during stress
🏥 Clinical Relevance of Autonomic Function
Understanding autonomic functions is vital in medical and nursing practice, especially for monitoring and managing:
- 🔺 Blood pressure and heart rate in critical care
- 💊 Drug effects on sympathetic/parasympathetic tone (e.g., beta-blockers, atropine)
- 🧠 Autonomic dysfunction in diabetes (e.g., postural hypotension, gastroparesis)
- ⚡ Neurogenic shock in spinal cord injury
- 🔄 Vasovagal syncope from parasympathetic overdrive
- 🌡️ Thermoregulatory issues in hypothalamic disorders
👩⚕️ Importance in Nursing Assessment
Nurses routinely observe and assess autonomic signs, such as:
- Changes in heart rate or rhythm
- Abnormal breathing patterns
- Skin temperature and sweating
- Bowel and bladder control
- Pupil responses
- Level of consciousness and arousal (especially in neurological cases)
Monitoring and documenting these signs help detect early autonomic instability, which can be life-saving.
📚 In Summary
- Autonomic functions are involuntary processes controlled by the autonomic nervous system
- They regulate cardiac, respiratory, digestive, urinary, and reproductive systems
- The ANS is divided into:
- Sympathetic (fight/flight),
- Parasympathetic (rest/digest),
- Enteric (gut control)
- These systems work in dynamic balance to maintain homeostasis
- Nurses and clinicians must understand autonomic regulation to effectively manage patients in acute and chronic conditions
🧠 Physiology of Pain – Understanding the Language of Distress
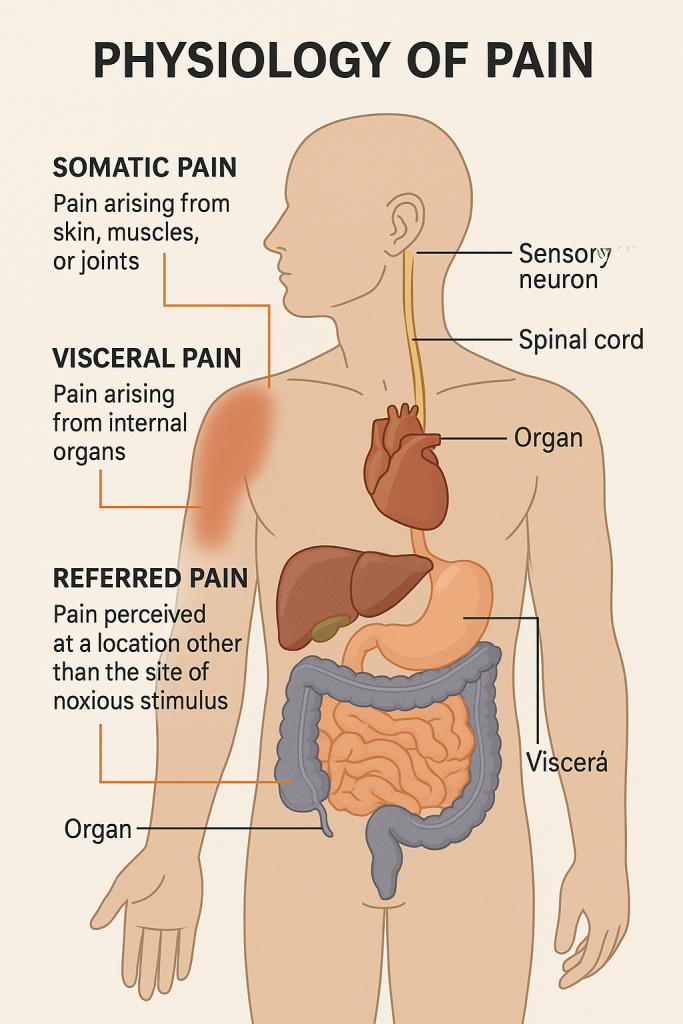
Pain is not merely a symptom — it is the body’s protective alarm system, an essential biological signal that alerts us to injury, disease, or dysfunction. Whether it’s the sharp sting of a needle, the dull ache of internal inflammation, or the puzzling discomfort felt in an area far from the actual injury, pain is a complex physiological and emotional experience.
At its core, pain is the brain’s interpretation of nociceptive signals — and these signals can arise from various tissues and travel through different neural pathways, leading to distinct types of pain: somatic, visceral, and referred.
🔬 What Is Pain? (Physiologically)
Pain is defined by the International Association for the Study of Pain (IASP) as:
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
Pain arises through a process called nociception, which includes:
- Transduction – Conversion of harmful stimuli (mechanical, thermal, chemical) into electrical impulses by nociceptors
- Transmission – Impulses travel through afferent nerve fibers (Aδ and C fibers) to the spinal cord and then to the brain
- Perception – The brain (thalamus, cortex, limbic system) processes and interprets the signal as “pain”
- Modulation – The body may amplify or inhibit pain via endogenous substances (e.g., endorphins, enkephalins)
🧩 Types of Pain Based on Origin
🔹 1. Somatic Pain – From the Body Wall and Muscles
Somatic pain arises from skin, muscles, joints, bones, and connective tissue. It is usually sharp, well-localized, and easily described.
There are two forms:
- Superficial Somatic Pain: Originates from the skin or subcutaneous tissues
– e.g., cuts, burns, insect bites - Deep Somatic Pain: Originates from muscles, tendons, ligaments, or bones
– e.g., sprains, arthritis, muscular injuries
Characteristics:
- Easily localized
- Sharp or throbbing
- Triggered by mechanical or inflammatory damage
- Conducted through A-delta fibers (sharp pain) and C fibers (dull ache)
🧠 Clinical Example: A patient with a fractured wrist feels deep, throbbing somatic pain directly over the injury site.
🔹 2. Visceral Pain – From Internal Organs
Visceral pain originates from the viscera (internal organs) such as the stomach, intestines, bladder, or heart. It is often diffuse, dull, and poorly localized, and may be accompanied by autonomic symptoms like sweating, nausea, or changes in heart rate.
Characteristics:
- Poorly localized (spread over a large area)
- Cramping, pressure-like, or aching
- Often associated with autonomic symptoms (vomiting, pallor, bradycardia)
- Transmitted primarily by C fibers
🧠 Clinical Example: A patient with appendicitis may initially feel a vague, central abdominal pain (visceral), which later becomes localized (somatic) as inflammation spreads.
🔹 3. Referred Pain – Pain Felt Away from the Actual Source
Referred pain occurs when pain from a visceral organ is perceived at a distant somatic site, typically due to converging sensory pathways in the spinal cord.
This happens because visceral afferent fibers and somatic afferent fibers enter the spinal cord at the same segment, leading the brain to misinterpret the origin of pain.
Mechanism:
- Spinal cord neurons receive signals from both visceral and somatic areas
- The brain associates the stimulus with the more commonly stimulated somatic region
🧠 Classic Clinical Examples:
- Cardiac pain felt in the left arm, jaw, or shoulder
- Diaphragmatic irritation from gallbladder inflammation felt in the right shoulder
- Renal colic referred to the groin
🧠 Neural Pathways Involved in Pain
- First-order neurons: Carry impulses from the nociceptors to the spinal cord (dorsal horn)
- Second-order neurons: Cross to the opposite side and ascend in the spinothalamic tract to the thalamus
- Third-order neurons: Project from the thalamus to the somatosensory cortex (pain perception area)
Additionally, limbic system activation gives pain its emotional component, and the hypothalamus triggers autonomic responses.
⚠️ Clinical Relevance and Nursing Implications
Understanding different types of pain is essential for:
- Accurate pain assessment (e.g., using pain scales)
- Differentiating superficial from deep or referred pain
- Evaluating the source of internal pathology
- Implementing appropriate pain management strategies
💊 Treatment may include:
- NSAIDs and local anesthetics for somatic pain
- Opioids for visceral pain
- Antispasmodics, nerve blocks, or epidural analgesia for severe or referred pain
📚 In Summary
- Somatic pain is sharp, localized, and originates from skin or musculoskeletal tissues.
- Visceral pain is dull, cramping, and arises from internal organs; often poorly localized.
- Referred pain is pain perceived in a distant somatic site due to shared neural pathways.
- Understanding these pain types enhances diagnosis, assessment, and targeted interventions in clinical settings.
⚡ Reflexes – Nature’s Rapid Protective Responses
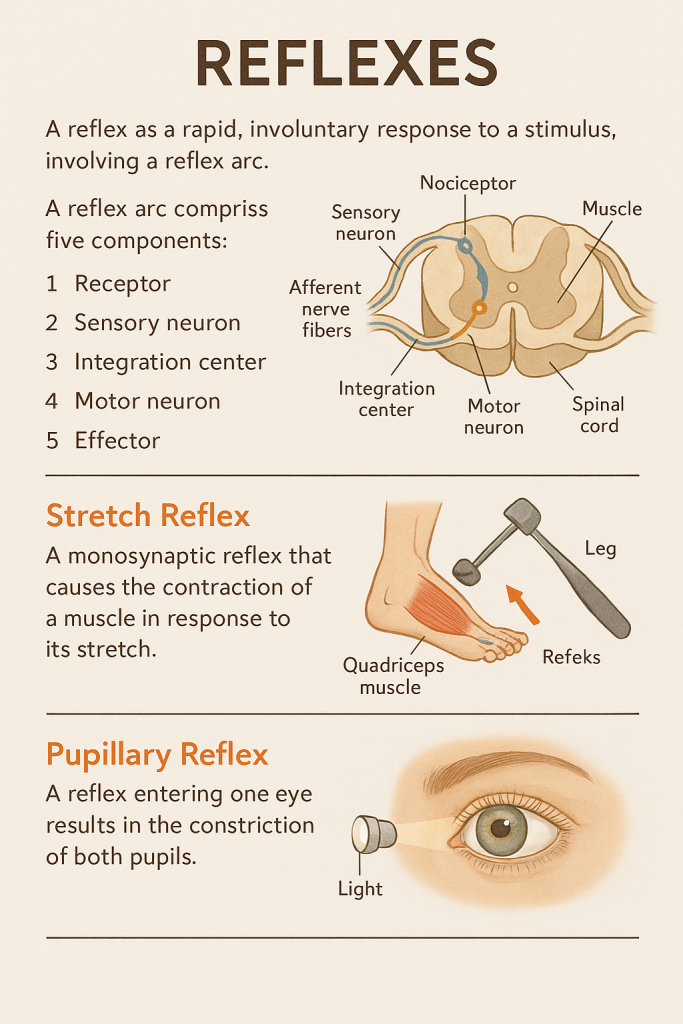
Before your brain even registers danger, your body is already reacting — pulling your hand away from a hot stove, blinking when something comes close to your eye, or balancing your posture after a slip. These automatic, rapid responses are called reflexes, and they are among the most elegant examples of how the nervous system protects and preserves the body.
Reflexes are predictable, stereotyped, involuntary responses to specific stimuli, involving precise neural pathways that bypass conscious thought to ensure immediate action.
🧠 What is a Reflex?
A reflex is a fast, involuntary, and predictable motor response to a specific sensory stimulus, often for protection or functional regulation. Most reflexes are mediated by the spinal cord or brainstem, allowing quick responses without the need for higher brain processing.
Reflexes are the nervous system’s “emergency protocols” — they bypass complex decision-making to ensure swift action.
🔄 The Reflex Arc – The Neural Blueprint of Reflexes
Every reflex action follows a fixed neural pathway known as the reflex arc, composed of five essential components:
- Receptor – Detects the stimulus (e.g., pain, pressure)
- Sensory (Afferent) Neuron – Carries the impulse toward the spinal cord
- Integration Center – Located in the spinal cord or brainstem; processes the signal
- Motor (Efferent) Neuron – Sends impulses to the effector
- Effector – Muscle or gland that responds (e.g., contracts or secretes)
This process occurs in milliseconds — far quicker than any voluntary reaction.
📘 Types of Reflexes Based on Location and Function
🔹 1. Spinal Reflexes
- Mediated through the spinal cord without brain involvement
- Examples:
- Stretch Reflex (e.g., patellar or knee-jerk reflex)
- Withdrawal Reflex (e.g., pulling hand away from heat)
🔹 2. Cranial Reflexes
- Mediated by the brainstem
- Involve cranial nerves
- Examples:
- Pupillary Light Reflex
- Corneal Reflex
- Gag Reflex
🧩 Classifications of Reflexes
✅ By Response Type
- Somatic Reflexes: Involve skeletal muscles (e.g., stretch reflex, withdrawal reflex)
- Autonomic (Visceral) Reflexes: Involve smooth muscle, cardiac muscle, or glands (e.g., heart rate regulation, digestive secretions)
✅ By Number of Synapses
- Monosynaptic Reflex: Involves one sensory and one motor neuron (e.g., patellar reflex)
- Polysynaptic Reflex: Involves interneurons between sensory and motor neurons (e.g., withdrawal reflex)
🌟 Examples of Major Reflexes
🦵 1. Stretch Reflex (e.g., Patellar Reflex)
- Trigger: Tap on patellar tendon
- Response: Quadriceps muscle contracts, causing leg extension
- Function: Maintains muscle tone and postural stability
✋ 2. Withdrawal Reflex (Flexor Reflex)
- Trigger: Painful stimulus (e.g., touching something hot)
- Response: Immediate withdrawal of the body part
- Function: Protects from injury
🧠 3. Crossed Extensor Reflex
- Paired with withdrawal reflex
- Example: One leg withdraws (flexes), the opposite leg extends to maintain balance
- Function: Maintains postural control
👁 4. Pupillary Light Reflex
- Stimulus: Light shone in the eye
- Response: Pupil constricts
- Cranial nerves: CN II (optic) and CN III (oculomotor)
- Function: Protects retina from excessive light
🧃 5. Baroreceptor Reflex (Autonomic)
- Stimulus: Rise in blood pressure
- Response: Heart rate decreases to lower blood pressure
- Function: Maintains blood pressure homeostasis
⚕️ Clinical Relevance of Reflex Testing
Reflex testing is a vital component of neurological examination. Reflexes provide insights into:
- Spinal cord integrity
- Peripheral nerve function
- Upper vs. lower motor neuron lesions
Reflex Grading Scale (0 to 4+):
- 0: Absent reflex
- 1+: Hypoactive
- 2+: Normal
- 3+: Brisk
- 4+: Hyperactive with clonus
🧠 Examples:
- Hyperreflexia: Suggests upper motor neuron lesion
- Hyporeflexia or areflexia: Suggests lower motor neuron lesion or peripheral neuropathy
- Babinski Reflex (Plantar Reflex): In adults, extension of big toe = abnormal, indicating CNS damage
👩⚕️ Nursing Insight
As a nurse or clinician:
- Know how to test reflexes properly (e.g., patellar hammer, light source)
- Document asymmetry, absence, or exaggeration
- Use reflex responses to assist in diagnosis and monitoring neurological disorders
- Recognize reflex changes in infants, trauma patients, or those with spinal injury
📚 In Summary
- Reflexes are involuntary, fast, and protective responses to stimuli.
- They are mediated by the reflex arc, involving sensory and motor pathways.
- Reflexes are vital for survival, posture, and homeostasis.
- Testing reflexes provides critical diagnostic clues in neurological assessments.
💧 Cerebrospinal Fluid (CSF) – The Brain’s Crystal Clear Lifeline
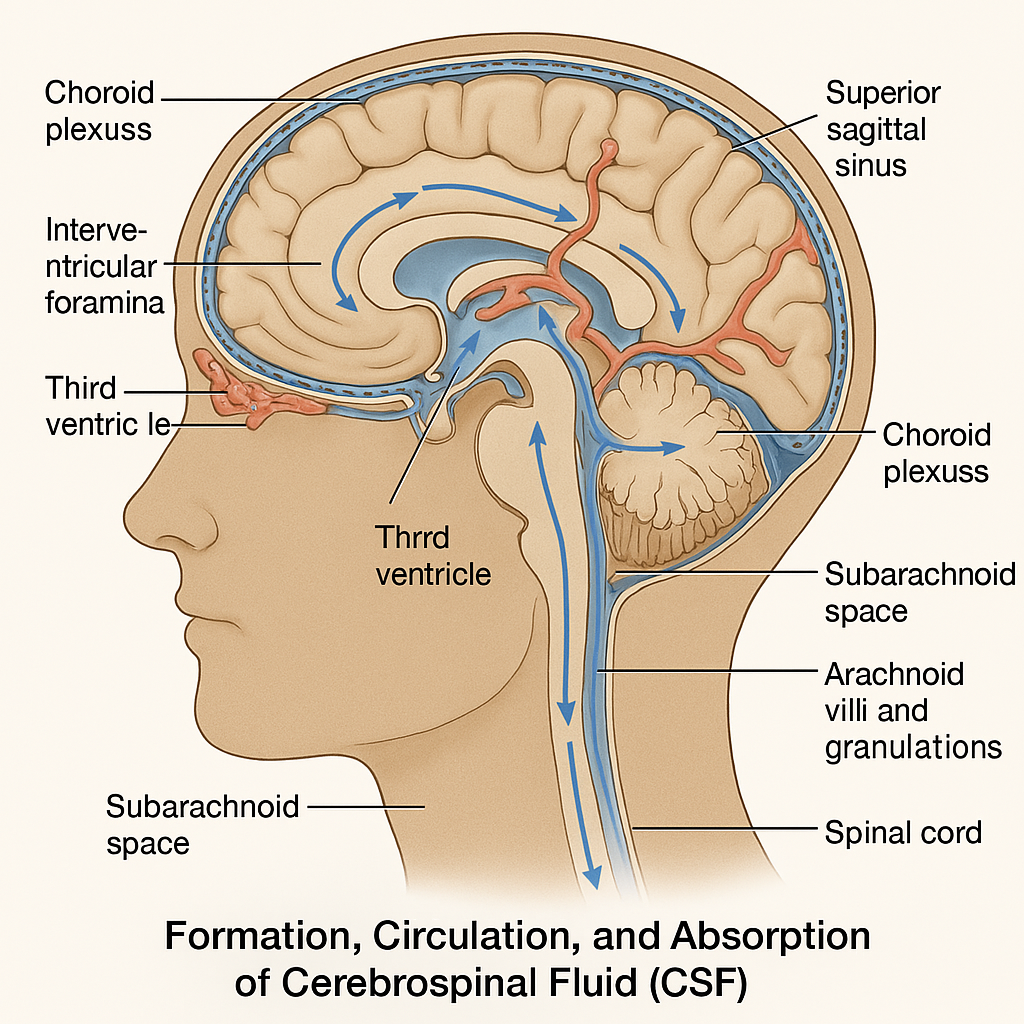
Floating in a bath of clear, protective fluid, the human brain is cushioned, nourished, and cleansed — all thanks to Cerebrospinal Fluid (CSF). Much more than just a buffer, CSF is an essential element in maintaining neural health, protecting delicate brain tissue, and removing waste. Its production, flow, and reabsorption are tightly regulated to keep the central nervous system functioning in perfect harmony.
🧠 What is CSF?
Cerebrospinal Fluid (CSF) is a clear, colorless, watery fluid that circulates through the ventricles of the brain, the central canal of the spinal cord, and the subarachnoid space surrounding the brain and spinal cord.
It acts as:
- 🛡 A protective cushion
- 🚰 A nutrient delivery system
- ♻ A waste removal channel
- ⚖ A pressure stabilizer within the cranial cavity
🧪 1. Formation of CSF
The main site of CSF production is the choroid plexus, a specialized network of capillaries and ependymal cells located in the walls of the lateral, third, and fourth ventricles of the brain.
- 80–90% of CSF is produced by the choroid plexus
- The rest is secreted by ependymal lining cells and brain interstitial fluid
CSF is formed by filtration of blood plasma, followed by selective secretion and active transport by the choroid plexus.
Daily volume produced: ~500 mL
Normal volume in circulation: ~150 mL
(This means CSF is turned over 3–4 times per day)
⚗️ 2. Composition of CSF
| Component | CSF Level | Significance |
|---|---|---|
| Appearance | Clear, colorless | Cloudy = infection; Bloody = hemorrhage |
| Specific Gravity | ~1.005 | Slightly lighter than water |
| pH | ~7.32 | Slightly more acidic than plasma |
| Proteins | Low (15–45 mg/dL) | ↑ in infections or tumors |
| Glucose | 50–80 mg/dL | 2/3 of blood glucose; ↓ in meningitis |
| White Blood Cells | 0–5 cells/µL | ↑ indicates infection or inflammation |
| Electrolytes | Na⁺, Cl⁻, HCO₃⁻, K⁺ | Helps maintain CNS ionic environment |
🔄 3. Circulation of CSF
The flow of CSF is unidirectional, ensuring constant movement and filtration. Here’s the journey:
🧭 CSF Circulation Pathway
- Choroid Plexus in Lateral Ventricles
⬇ - Interventricular Foramina (of Monro)
⬇ - Third Ventricle (at midline of diencephalon)
⬇ - Cerebral Aqueduct (of Sylvius)
⬇ - Fourth Ventricle (between pons and cerebellum)
⬇ - Foramina of Luschka & Magendie
⬇ - Subarachnoid Space surrounding brain & spinal cord
⬇ - Arachnoid Villi & Granulations (in superior sagittal sinus)
⬇ - Venous Circulation – via dural venous sinuses
🌀 Key Concept: CSF flows from the ventricles to the subarachnoid space, then drains into the venous system.
🚰 CSF Drainage and Reabsorption
- CSF is reabsorbed into the bloodstream through arachnoid granulations (finger-like projections of the arachnoid mater into dural sinuses)
- This process is pressure-dependent — higher CSF pressure promotes faster absorption
⚠️ Clinical Relevance
Disruption in CSF production, flow, or reabsorption can lead to significant neurological disorders:
🔹 Hydrocephalus
- Excess CSF accumulation in the ventricles
- Can be communicating (reabsorption defect) or non-communicating (obstruction)
- Presents with increased intracranial pressure, enlarged head in infants, and mental status changes in adults
🔹 Meningitis
- Infection inflames meninges → cloudy, high-protein, low-glucose CSF
- CSF sampling via lumbar puncture (LP) is diagnostic
🔹 CSF Leak
- Caused by trauma or surgical injury
- Results in low pressure headache, clear nasal or ear discharge (testable with beta-2 transferrin protein)
🔹 Subarachnoid Hemorrhage
- Blood in CSF; “thunderclap headache”
- CSF appears xanthochromic (yellowish) after a few hours
👩⚕️ Nursing Application and Importance
Nurses are involved in:
- Assisting with lumbar punctures
- Monitoring CSF drainage (e.g., via ventriculostomy)
- Recognizing signs of increased intracranial pressure (ICP):
- Headache, vomiting, papilledema, altered consciousness
- Evaluating post-lumbar puncture care: Prevent CSF leak by keeping the patient in supine position
📚 In Summary
- CSF is produced by the choroid plexus, circulates through the ventricles and subarachnoid space, and is absorbed into venous circulation.
- It provides protection, nourishment, and waste removal for the brain and spinal cord.
- Its composition is carefully regulated and abnormalities can signal infection, hemorrhage, or obstructive conditions like hydrocephalus.
🧠 Blood-Brain Barrier (BBB) & Blood-CSF Barrier – The Brain’s Gatekeepers
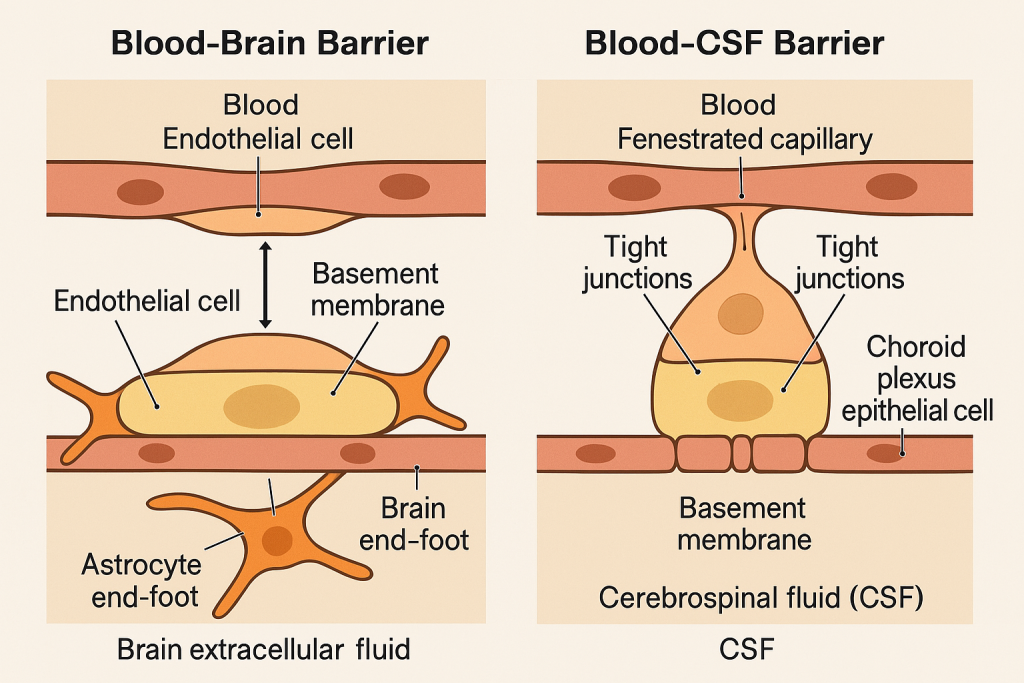
The human brain is a delicate and highly specialized organ. To preserve its function, it is shielded by selective defense systems that regulate what enters and exits the central nervous system (CNS). These systems — the Blood-Brain Barrier (BBB) and the Blood-CSF Barrier — act as vigilant sentinels, guarding the internal environment of the brain from toxins, pathogens, and fluctuations in blood composition, while still allowing the passage of essential nutrients.
🧱 1. Blood-Brain Barrier (BBB) – The Wall of Selectivity
🌟 What is the BBB?
The Blood-Brain Barrier is a specialized, semipermeable physiological barrier that separates the bloodstream from the brain’s extracellular fluid (ECF). It serves as the primary shield protecting neurons from harmful substances in the blood, while carefully regulating the transport of necessary molecules such as oxygen and glucose.
🧩 Anatomical Components of the BBB:
- Endothelial Cells of brain capillaries:
- Joined by tight junctions, preventing paracellular transport
- Basement Membrane:
- A thin layer of extracellular matrix supporting the endothelium
- Astrocyte End-feet:
- Specialized glial cells that surround capillaries, regulating permeability and nutrient exchange
- Pericytes:
- Embedded in the capillary walls, they stabilize the structure and regulate blood flow
🧠 Functions of the BBB:
- 🛡 Protects the CNS from toxins, pathogens, and harmful drugs
- 🔄 Regulates ionic balance for synaptic transmission
- 💧 Maintains fluid composition of the brain’s microenvironment
- ⛔ Prevents neuroinflammation by blocking immune cell infiltration
- ✅ Permits the entry of essential substances like glucose (via GLUT1 transporters), amino acids, O₂, and CO₂
🧪 Permeability Characteristics of the BBB:
Allowed to cross easily:
- Lipid-soluble molecules (e.g., ethanol, nicotine)
- Gases (O₂, CO₂)
- Small molecules via transport proteins (e.g., glucose, amino acids)
Restricted or denied:
- Proteins
- Most drugs
- Pathogens
- Immune cells and antibodies
⚠️ Clinical Importance of the BBB:
Disruption or dysfunction of the BBB is implicated in:
- Meningitis (bacterial toxins can increase permeability)
- Multiple sclerosis (autoimmune cells cross into the CNS)
- Brain tumors (abnormal vessels with leaky barriers)
- Alzheimer’s disease (BBB breakdown contributes to amyloid accumulation)
- Drug delivery challenges in treating CNS disorders (e.g., chemotherapy, antibiotics)
💧 2. Blood-CSF Barrier – The Brain’s Fluid Filter
🌟 What is the Blood-CSF Barrier?
The Blood-CSF Barrier is a selective barrier located at the choroid plexus, which separates the circulating blood from the cerebrospinal fluid (CSF) in the ventricles. It ensures that the CSF — which bathes and protects the brain and spinal cord — maintains its precise composition for neuronal function.
🧩 Anatomical Components of the Blood-CSF Barrier:
- Choroid Plexus Epithelial Cells:
- Formed by cuboidal epithelial cells with tight junctions
- Capillaries within the Choroid Plexus:
- These are fenestrated (leaky) to allow plasma filtration
- Basal Lamina:
- Provides structural support and filtration
Unlike the BBB, the capillaries in the choroid plexus are leaky, but the epithelial cell layer forms the real barrier that filters what gets into the CSF.
🧠 Functions of the Blood-CSF Barrier:
- 🎯 Controls entry of substances into CSF
- 🛡 Protects CNS from toxic metabolites and pathogens
- 🔁 Regulates ion balance in CSF for optimal neuronal activity
- ♻ Facilitates removal of waste products
⚖️ Comparing BBB and Blood-CSF Barrier
| Feature | Blood-Brain Barrier (BBB) | Blood-CSF Barrier |
|---|---|---|
| Location | Brain capillaries | Choroid plexus of ventricles |
| Barrier Formed By | Endothelial cells with tight junctions | Choroid plexus epithelial cells |
| Primary Role | Protects neurons from blood-borne agents | Regulates composition of CSF |
| Capillary Type | Non-fenestrated (tight) | Fenestrated (leaky) capillaries |
| Transport Mechanisms | Active & facilitated diffusion | Active transport and secretion |
| Disruption Consequence | Edema, neurodegeneration | Altered CSF composition, hydrocephalus risk |
⚕️ Clinical Relevance
- Infections (e.g., meningitis) can affect both barriers, leading to brain swelling and impaired function.
- Lumbar puncture can assess CSF composition to detect barrier damage.
- New drug formulations (e.g., liposomal delivery) are being designed to bypass these barriers for effective CNS treatment.
👩⚕️ Nursing & Medical Insight
Understanding these barriers is critical in:
- Monitoring neuroinfections
- Administering medications that may/may not cross into the CNS
- Evaluating CSF reports in diagnostic procedures
- Caring for patients with CNS disorders (e.g., epilepsy, MS, brain tumors)
📚 In Summary
- The Blood-Brain Barrier and Blood-CSF Barrier serve as critical regulators that shield the brain from harmful agents while maintaining internal stability.
- They are anatomically distinct, but functionally integrated to protect the CNS environment.
- Their integrity is vital to brain health, and their dysfunction is linked to many neurological diseases.
🧠 Nervous System – Application & Implication in Nursing Practice
The nervous system is the master controller of the human body — governing movement, sensation, thought, emotion, and vital organ function. For nurses, an in-depth understanding of the nervous system is not just theoretical knowledge — it is practical, essential, and life-saving. From assessing a stroke patient’s response to managing pain or interpreting a reflex, nursing care often begins and ends with the nervous system in mind.
🌐 I. Why the Nervous System Matters in Nursing
The nervous system includes the central nervous system (CNS) — brain and spinal cord — and the peripheral nervous system (PNS), which includes cranial and spinal nerves. Nurses engage with the nervous system across:
- Neurological assessment
- Pain management
- Emergency and critical care
- Rehabilitation
- Mental health
- Medication administration and monitoring
Understanding its structure and function enables nurses to:
- Detect early signs of neurological dysfunction
- Respond to emergencies
- Provide appropriate interventions
- Educate and support patients and families
🔍 II. Applications of Nervous System Knowledge in Nursing
🩺 1. Neurological Assessment
Nurses routinely assess mental status, cranial nerves, reflexes, motor and sensory function, and level of consciousness using tools like:
- Glasgow Coma Scale (GCS)
- Pupil size and reactivity
- Sensory testing (touch, pain, temperature)
- Motor strength and coordination
🔔 Early detection of changes can signal stroke, increased intracranial pressure, or neurodegeneration.
💊 2. Pain Management
Understanding nociceptive pathways, types of pain (somatic, visceral, neuropathic), and neurotransmitters helps nurses:
- Assess pain using appropriate scales
- Administer analgesics effectively
- Monitor responses and side effects
- Implement non-pharmacological techniques like distraction, massage, or cold therapy
Pain is a neurological perception, and managing it is a core nursing responsibility.
🚨 3. Emergency Nursing (Stroke, Seizures, Head Injury)
In emergencies, quick neurological evaluation is critical:
- FAST assessment for stroke (Face, Arms, Speech, Time)
- Seizure precautions (padding rails, airway protection)
- Post-head injury monitoring for signs of brain edema or hemorrhage
The nervous system dictates vital reflexes like breathing and consciousness — every minute matters.
🧠 4. Caring for Patients with Neurological Disorders
Conditions like:
- Parkinson’s disease (movement and autonomic dysfunction)
- Multiple sclerosis (nerve conduction loss)
- Spinal cord injury (paralysis, sensory loss)
- Alzheimer’s or dementia (cognitive decline)
- Meningitis (infection of CNS linings)
Nurses need to:
- Monitor symptoms and progression
- Provide supportive care and positioning
- Prevent complications like aspiration or pressure ulcers
- Promote mobility, independence, and patient safety
🧬 5. Autonomic Nervous System Regulation
Understanding sympathetic and parasympathetic responses is vital when:
- Monitoring blood pressure, heart rate, and respiration
- Managing stress responses
- Administering drugs that affect autonomic tone (e.g., atropine, beta-blockers)
Autonomic imbalance can result in life-threatening instability — nurses must act quickly.
💉 6. Pharmacological Considerations
Many drugs affect neurotransmitters, including:
- CNS depressants/stimulants
- Anesthetics
- Antiepileptics
- Antipsychotics/antidepressants
- Cholinergic and adrenergic agents
Nurses must understand:
- Mechanism of action
- Side effects (e.g., drowsiness, tremors, dizziness)
- Monitoring parameters
- Safe administration techniques
🧘 7. Mental Health and Psychosocial Support
The brain controls emotion, cognition, and behavior. Nurses in mental health must:
- Understand how neurotransmitter imbalances affect mood and perception
- Support patients with depression, anxiety, psychosis, and PTSD
- Use therapeutic communication and emotional regulation techniques
Emotional care is neurologically rooted — a vital part of holistic nursing.
🧾 III. Implications in Nursing Practice
| Area | Nursing Implication |
|---|---|
| Assessment | Perform and interpret neurological assessments regularly |
| Intervention | Implement prompt care for neuroemergencies |
| Patient Safety | Prevent injury in patients with seizures, falls, or confusion |
| Education | Teach patients/families about stroke, medications, memory care |
| Multidisciplinary Care | Collaborate with neurologists, physiotherapists, and occupational therapists |
The nervous system is central to nursing practice — whether you’re in ICU, mental health, medical-surgical, or community care. Understanding its anatomy, physiology, and pathology equips nurses to:
- Deliver competent, compassionate care
- Recognize and respond to critical changes
- Promote recovery and independence
- Serve as educators and advocates for patients with neurological needs
✅ A nurse who understands the nervous system is empowered to care for the whole patient — body, mind, and spirit.