Physio-B.sc-Unit-6-The Endocrine system
🧠 Pineal Gland – Functions and Hormones (Academic Explanation)
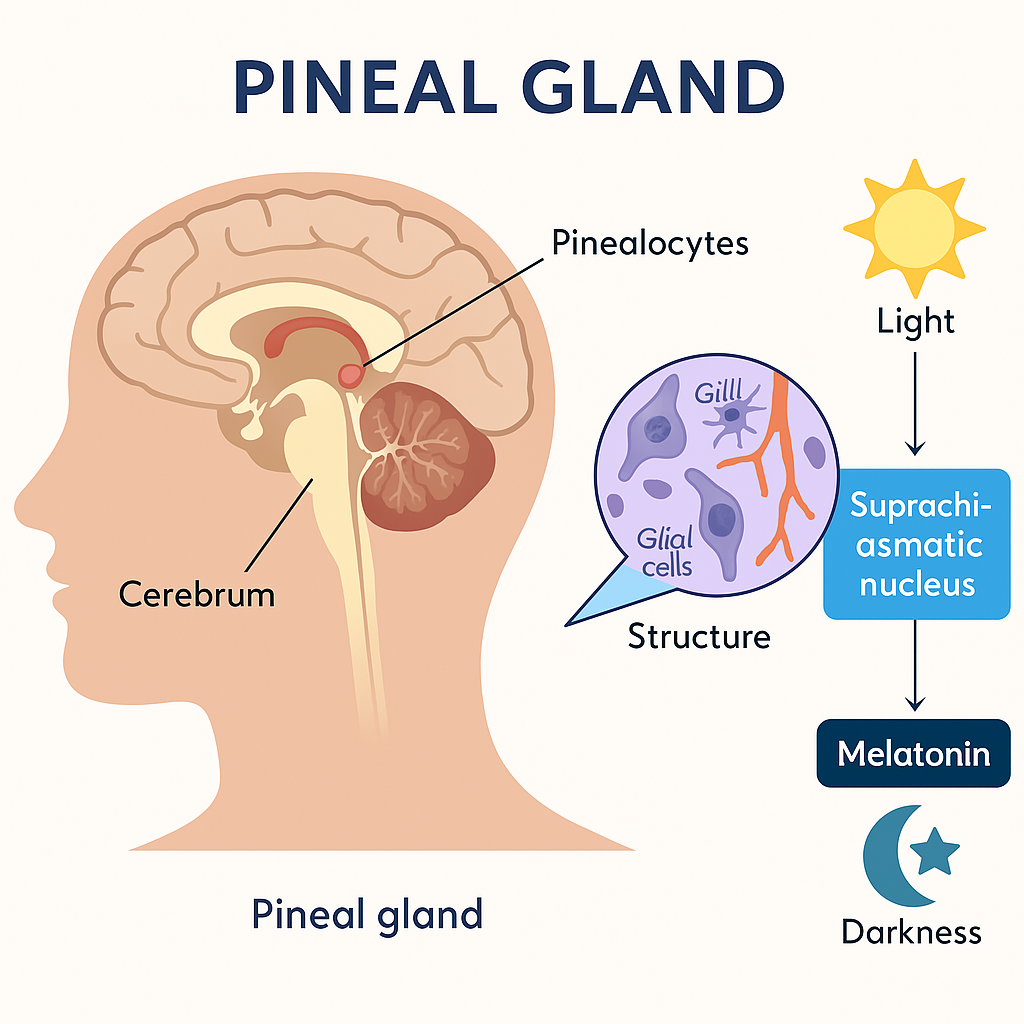
The pineal gland is a small, pea-shaped endocrine gland located near the center of the brain, between the two hemispheres, in a groove where the two halves of the thalamus join. Despite its small size, it plays a significant role in regulating circadian rhythms, reproductive functions, and seasonal biological cycles.
📍 I. Anatomy and Location
- Size: ~5–8 mm
- Location: Deep in the brain, in the epithalamus, near the third ventricle
- Often visible in brain imaging due to calcium deposits (pineal sand)
🔬 II. Structure and Histology
- Composed of:
- Pinealocytes – main cells that synthesize and secrete hormones
- Glial cells – supportive cells
- Capillaries – supply blood
- No direct nerve connections to the hypothalamus, but receives input via sympathetic fibers from the superior cervical ganglion.
🧪 III. Hormones of the Pineal Gland
🌙 1. Melatonin – Primary Hormone
- Synthesized from: Tryptophan → Serotonin → Melatonin
- Secreted in response to darkness and inhibited by light
- Regulated by: Suprachiasmatic nucleus (SCN) of the hypothalamus (body’s biological clock)
🔍 Melatonin Secretion Pattern:
| Light Condition | Melatonin Level |
|---|---|
| Daylight | Low |
| Darkness | High |
🌟 IV. Functions of the Pineal Gland
🔹 1. Regulation of Circadian Rhythms
- Melatonin controls the sleep–wake cycle (biological clock)
- Increases in the evening to induce sleepiness
- Suppressed during the day to promote wakefulness
🔹 2. Regulation of Sleep
- Aids in initiating and maintaining sleep
- Helps adjust to jet lag and shift work by resetting the biological clock
🔹 3. Antioxidant Activity
- Melatonin is a potent antioxidant
- Scavenges free radicals and protects neural tissues from oxidative stress
🔹 4. Reproductive Function Modulation
- Inhibits gonadotropin-releasing hormone (GnRH) secretion from the hypothalamus
- Can delay puberty when melatonin levels are high (e.g., in blind individuals or children)
- In animals, controls seasonal breeding patterns
🔹 5. Immunomodulatory Role
- Melatonin enhances the activity of:
- T-cells
- Natural killer (NK) cells
- Antibody production
- Supports immune surveillance
🔹 6. Role in Mood and Seasonal Affective Disorder (SAD)
- Low daylight in winter → Increased melatonin → Linked to depression, fatigue, and SAD
- Light therapy may help regulate melatonin levels and improve mood
🧾 V. Summary Table: Pineal Gland Hormones & Functions
| Hormone | Produced by | Main Functions |
|---|---|---|
| Melatonin | Pinealocytes | Regulates sleep–wake cycle, inhibits puberty, antioxidant, mood regulation |
🧠 VI. Clinical Relevance
| Condition | Effect on Pineal Function |
|---|---|
| Jet lag | Disrupts melatonin secretion → sleep disturbance |
| Seasonal Affective Disorder (SAD) | Excess melatonin in winter → mood issues |
| Sleep disorders | May benefit from melatonin supplements |
| Delayed puberty | High melatonin levels may suppress gonadotropins |
| Pineal gland tumors | Can cause hydrocephalus, visual issues, or endocrine dysfunction |
✅
The pineal gland, though small, plays a vital endocrine role in:
- Sleep regulation
- Circadian rhythm control
- Antioxidant defense
- Reproductive and immune modulation
Its primary hormone, melatonin, bridges the interaction between light exposure and biological function, making it critical in maintaining homeostasis and well-being.
🧠 Pituitary Gland – Functions and Hormones (Academic Explanation)
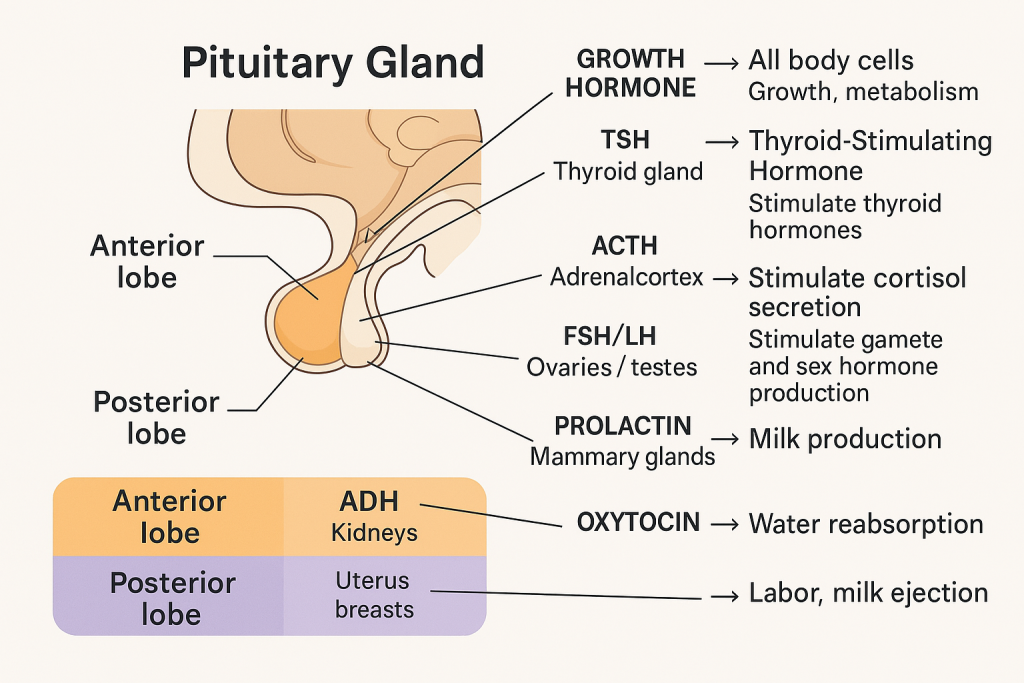
The pituitary gland, also known as the “master gland”, plays a central role in regulating the endocrine system by secreting multiple hormones that control the activity of other glands and bodily functions.
📍 I. Anatomy and Location
- Size: ~0.5–1 cm (pea-sized)
- Location: At the base of the brain in a bony cavity called the sella turcica of the sphenoid bone
- Connected to the hypothalamus by the infundibulum (pituitary stalk)
🧬 II. Divisions of the Pituitary Gland
| Lobe | Alternative Name | Hormone Production |
|---|---|---|
| Anterior lobe | Adenohypophysis | Produces and secretes hormones |
| Posterior lobe | Neurohypophysis | Stores and releases hypothalamic hormones |
| Intermediate lobe | (pars intermedia) | Rudimentary in humans; secretes MSH |
🧪 III. Hormones of the Anterior Pituitary (Adenohypophysis)
🧠 Anterior Pituitary Hormones and Their Functions
The anterior pituitary gland (also called the adenohypophysis) is a major endocrine organ that secretes tropic and non-tropic hormones. These hormones regulate the function of other endocrine glands and various physiological processes such as growth, reproduction, and metabolism.
Hormone secretion is regulated by releasing and inhibiting hormones from the hypothalamus via the hypophyseal portal system.
🔬 Hormones Secreted by the Anterior Pituitary
There are six major hormones secreted by the anterior pituitary:
1. 🧬 Growth Hormone (GH or Somatotropin)
- Target Organs: Bones, muscles, liver, adipose tissue
- Stimulated by: GHRH (Growth Hormone-Releasing Hormone)
- Inhibited by: Somatostatin (GHIH)
Functions:
- Stimulates growth of long bones and skeletal muscles
- Enhances protein synthesis
- Promotes lipolysis (fat breakdown)
- Reduces glucose uptake (anti-insulin effect)
- Stimulates IGF-1 (Insulin-like Growth Factor) production in the liver
Disorders:
- ↑ GH in childhood → Gigantism
- ↑ GH in adults → Acromegaly
- ↓ GH → Dwarfism in children
2. 🦋 Thyroid-Stimulating Hormone (TSH or Thyrotropin)
- Target Organ: Thyroid gland
- Stimulated by: TRH (Thyrotropin-Releasing Hormone)
- Inhibited by: High T₃ and T₄ levels (negative feedback)
Functions:
- Stimulates the thyroid to produce and release T₃ (triiodothyronine) and T₄ (thyroxine)
- Regulates metabolism, growth, and development
Disorders:
- ↑ TSH → Hyperthyroidism (Graves’ disease)
- ↓ TSH → Hypothyroidism (e.g., Hashimoto’s thyroiditis)
3. 🧠 Adrenocorticotropic Hormone (ACTH or Corticotropin)
- Target Organ: Adrenal cortex (zona fasciculata)
- Stimulated by: CRH (Corticotropin-Releasing Hormone)
- Inhibited by: Cortisol (negative feedback)
Functions:
- Stimulates secretion of glucocorticoids (mainly cortisol)
- Helps the body respond to stress
- Regulates blood sugar, metabolism, and inflammation
Disorders:
- ↑ ACTH → Cushing’s disease (excess cortisol)
- ↓ ACTH → Adrenal insufficiency (e.g., Addison’s disease)
4. 🧬 Follicle-Stimulating Hormone (FSH)
- Target Organs: Ovaries in females, testes in males
- Stimulated by: GnRH (Gonadotropin-Releasing Hormone)
- Inhibited by: Inhibin (from gonads), estrogens/testosterone
Functions:
- In females: Stimulates follicular growth and estrogen production
- In males: Stimulates spermatogenesis in the seminiferous tubules
Disorders:
- Deficiency causes infertility, delayed puberty
5. 🔁 Luteinizing Hormone (LH)
- Target Organs: Ovaries in females, testes in males
- Stimulated by: GnRH
- Inhibited by: Estrogen/progesterone/testosterone (negative feedback)
Functions:
- In females:
- Triggers ovulation
- Promotes corpus luteum formation
- Stimulates progesterone secretion
- In males:
- Stimulates Leydig cells to produce testosterone
Disorders:
- Deficiency leads to menstrual irregularities, delayed puberty, or infertility
6. 🍼 Prolactin (PRL)
- Target Organ: Mammary glands
- Stimulated by: PRH (Prolactin-Releasing Hormone), stress, nipple stimulation
- Inhibited by: Dopamine (Prolactin-Inhibiting Hormone)
Functions:
- Initiates and maintains milk production (lactogenesis)
- Inhibits ovulation during lactation by suppressing GnRH
Disorders:
- ↑ PRL → Galactorrhea, amenorrhea, infertility
- ↓ PRL → Poor milk production postpartum
🧾 Anterior Pituitary Hormones
| Hormone | Target | Primary Function | Regulated by |
|---|---|---|---|
| GH | Bones, muscles | Growth, metabolism, protein synthesis | GHRH / Somatostatin |
| TSH | Thyroid gland | Stimulates thyroid hormone production | TRH |
| ACTH | Adrenal cortex | Stimulates cortisol secretion | CRH |
| FSH | Ovaries/Testes | Follicle growth / spermatogenesis | GnRH |
| LH | Ovaries/Testes | Ovulation / testosterone production | GnRH |
| PRL | Mammary glands | Milk production | Dopamine (inhibitory) |
The anterior pituitary gland regulates essential body functions including growth, metabolism, stress response, sexual development, fertility, and lactation. Its hormones are under strict hypothalamic control and feedback regulation, making it a central hub of the endocrine system.
💧 IV. Hormones of the Posterior Pituitary (Neurohypophysis)
🧠 Posterior Pituitary Hormones and Their Functions
The posterior pituitary, also called the neurohypophysis, is the neural part of the pituitary gland. Unlike the anterior pituitary, it does not synthesize hormones; instead, it stores and releases hormones produced by the hypothalamus.
These hormones are:
- Antidiuretic Hormone (ADH / Vasopressin)
- Oxytocin
Both are synthesized in the hypothalamic nuclei:
- ADH: Synthesized in the supraoptic nucleus
- Oxytocin: Synthesized in the paraventricular nucleus
They are transported along axons through the hypothalamo-hypophyseal tract to the posterior pituitary and released into circulation when needed.
💧 1. Antidiuretic Hormone (ADH / Vasopressin)
🔹 Production Site:
- Synthesized in the supraoptic nucleus of the hypothalamus
- Stored and released by the posterior pituitary
🧬 Target Organs:
- Kidneys (collecting ducts)
- Arterioles (in higher concentrations)
📌 Functions:
- Water reabsorption in the kidneys:
- ADH binds to V2 receptors in the renal collecting ducts
- Increases aquaporin-2 channels
- Promotes water retention, reducing urine output
- Vasoconstriction (at high doses):
- Binds to V1 receptors in blood vessels → increases vascular tone
- Maintains blood volume and pressure
🩺 Regulation:
- Stimulated by:
- ↑ Plasma osmolarity (detected by hypothalamic osmoreceptors)
- ↓ Blood volume or pressure (via baroreceptors)
- Stress, pain, certain drugs (e.g., morphine)
- Inhibited by:
- Alcohol
- Low plasma osmolarity
⚠️ Disorders:
| Condition | Cause | Effect |
|---|---|---|
| Diabetes insipidus | ADH deficiency or receptor insensitivity | Polyuria, polydipsia, dilute urine |
| SIADH (Syndrome of Inappropriate ADH Secretion) | Excess ADH | Water retention, hyponatremia |
🤱 2. Oxytocin
🔹 Production Site:
- Synthesized in the paraventricular nucleus of the hypothalamus
- Stored and released by the posterior pituitary
🧬 Target Organs:
- Uterus (during childbirth)
- Mammary glands (during lactation)
📌 Functions:
- Stimulates uterine contractions during labor:
- Binds to oxytocin receptors in the uterine myometrium
- Strengthens and coordinates contractions
- Triggers milk ejection (let-down reflex):
- Contracts myoepithelial cells surrounding alveoli in mammary glands
- Facilitates bonding and trust (psychological effects):
- Plays a role in maternal behavior, partner bonding, and social recognition
🩺 Regulation:
- Positive feedback loop:
- Uterine contractions → ↑ oxytocin → stronger contractions (until birth)
- Nipple stimulation → oxytocin release → milk ejection
- Stimulated by:
- Cervical stretch during labor
- Suckling during breastfeeding
- Emotional bonding cues
⚠️ Clinical Uses:
- Synthetic oxytocin (Pitocin) is used to:
- Induce or augment labor
- Control postpartum hemorrhage
🧾 Posterior Pituitary Hormones
| Hormone | Target | Primary Function | Stimulated by |
|---|---|---|---|
| ADH | Kidneys, blood vessels | Water reabsorption, vasoconstriction | High plasma osmolarity, low BP |
| Oxytocin | Uterus, mammary glands | Uterine contractions, milk ejection, bonding | Cervical stretch, suckling, emotional cues |
The posterior pituitary gland, though small, plays a vital role in maintaining fluid balance, regulating childbirth and lactation, and supporting social behavior through ADH and oxytocin. Their dysfunction can lead to serious clinical conditions like diabetes insipidus or labor complications, making them essential for nurses and clinicians to understand and monitor.
🩺 VI. Summary Table of Pituitary Hormones and Functions
| Hormone | Lobe | Target Organ | Primary Function |
|---|---|---|---|
| GH | Anterior | All body cells | Growth, metabolism |
| TSH | Anterior | Thyroid gland | Stimulate thyroid hormones |
| ACTH | Anterior | Adrenal cortex | Stimulate cortisol secretion |
| FSH | Anterior | Gonads | Follicle and sperm development |
| LH | Anterior | Gonads | Ovulation, testosterone production |
| PRL | Anterior | Mammary glands | Milk production |
| ADH | Posterior | Kidneys | Water reabsorption |
| Oxytocin | Posterior | Uterus, breasts | Labor, milk ejection |
| MSH | Intermediate | Skin (melanocytes) | Pigment formation (minor in humans) |
🧠 VII. Clinical Conditions Related to Pituitary Dysfunction
| Disorder | Hormonal Cause | Effects |
|---|---|---|
| Pituitary adenoma | Overproduction of GH, ACTH, or PRL | Gigantism, Cushing’s disease, galactorrhea |
| Hypopituitarism | Deficiency of one or more pituitary hormones | Fatigue, infertility, growth failure |
| Sheehan’s syndrome | Postpartum pituitary necrosis | Hypopituitarism in women after delivery |
| Diabetes insipidus | ADH deficiency | Excess urination and thirst |
✅
The pituitary gland is the central coordinator of the endocrine system, influencing growth, metabolism, stress response, reproductive function, lactation, and fluid balance. Dysfunction can lead to widespread systemic issues, which makes understanding its roles essential in patient care and clinical diagnosis.
🦋 Thyroid Hormones and Their Functions – Academic Overview
The thyroid gland is a butterfly-shaped endocrine gland located in the anterior neck, on either side of the trachea. It plays a vital role in regulating metabolism, growth, and development by secreting thyroid hormones.
🧬 I. Major Hormones of the Thyroid Gland
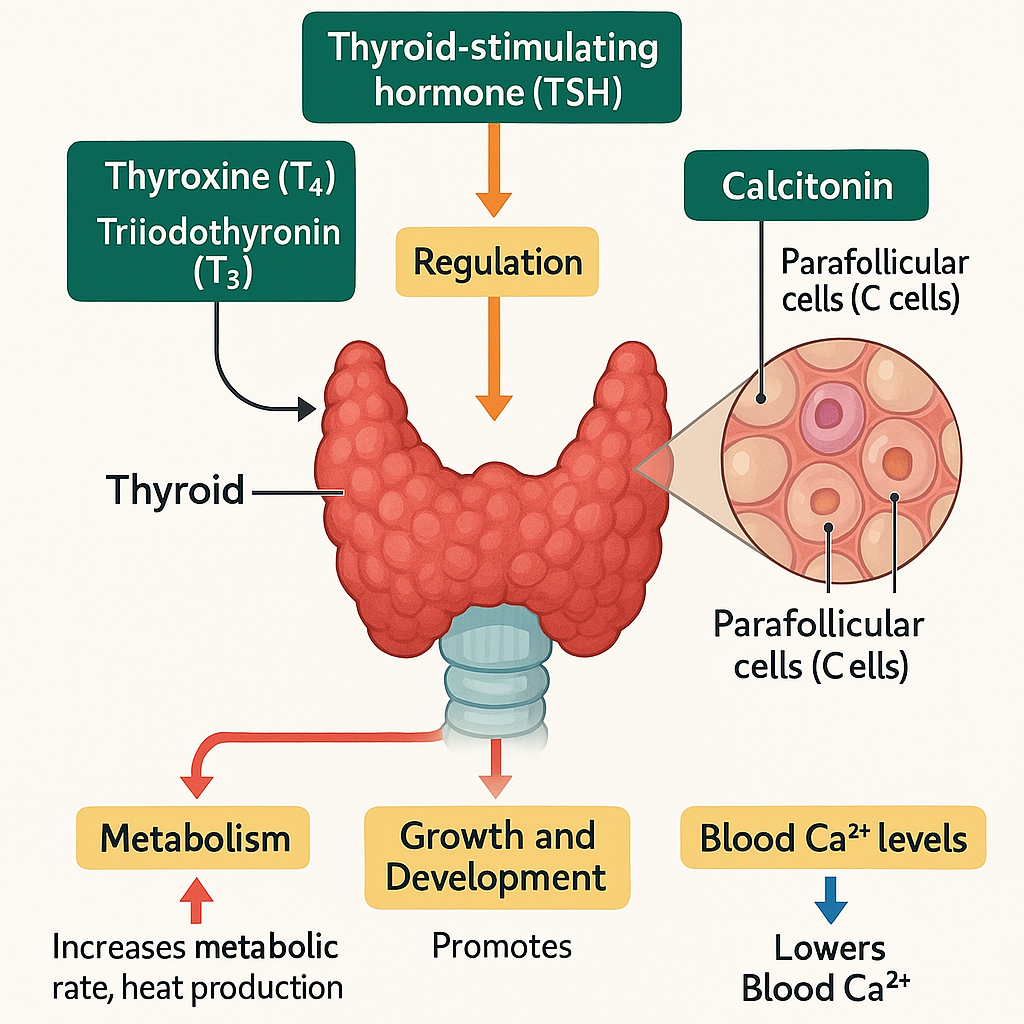
The thyroid produces three key hormones:
| Hormone | Type | Secreted by |
|---|---|---|
| Thyroxine (T₄) | Iodinated hormone | Follicular cells |
| Triiodothyronine (T₃) | Iodinated hormone | Follicular cells |
| Calcitonin | Peptide hormone | Parafollicular (C) cells |
🔹 1. Thyroxine (T₄) and Triiodothyronine (T₃)
📌 Biosynthesis:
- Synthesized from iodine and tyrosine in the thyroid follicular cells.
- T₄ is the major form secreted (~90%), but T₃ is more active.
- T₄ is converted to T₃ in peripheral tissues (especially liver and kidneys).
🧠 Regulation:
- Controlled by Thyroid Stimulating Hormone (TSH) from the anterior pituitary
- TSH is stimulated by TRH (thyrotropin-releasing hormone) from the hypothalamus
- Negative feedback: High T₃/T₄ levels inhibit TSH and TRH secretion
🔬 Functions of T₃ and T₄:
| System | Function |
|---|---|
| Metabolism | ↑ Basal metabolic rate, ↑ oxygen consumption, ↑ glucose and fat metabolism |
| Growth & Development | Essential for brain development (especially in fetus/infants); promotes skeletal growth |
| Cardiovascular | ↑ Heart rate, ↑ cardiac output by increasing sensitivity to catecholamines |
| Nervous System | Enhances alertness, reflexes, and mood |
| Gastrointestinal | ↑ GI motility and appetite |
| Reproductive | Supports normal menstrual cycle and fertility |
| Thermogenesis | Maintains body temperature by increasing heat production |
⚠️ Clinical Disorders Related to T₃ and T₄
| Condition | Hormone Status | Clinical Features |
|---|---|---|
| Hypothyroidism | ↓ T₃/T₄ | Fatigue, weight gain, cold intolerance, bradycardia, constipation, dry skin |
| Hyperthyroidism | ↑ T₃/T₄ | Weight loss, heat intolerance, tachycardia, anxiety, tremors |
| Cretinism (in infants) | Congenital ↓ T₄ | Mental retardation, growth failure |
| Myxedema | Severe adult hypothyroidism | Puffy face, lethargy, coma (in extreme cases) |
| Graves’ Disease | Autoimmune hyperthyroidism | Exophthalmos, goiter, hypermetabolism |
🔹 2. Calcitonin
📌 Produced by: Parafollicular cells (C cells) of the thyroid gland
🧠 Regulation:
- Stimulated by high blood calcium levels
- Opposes the action of parathyroid hormone (PTH)
🔬 Functions:
- Lowers blood calcium levels by:
- Inhibiting osteoclast activity (↓ bone resorption)
- Promoting calcium excretion in kidneys
- More significant in children and pregnancy (bone growth phases)
🔖 Note: Calcitonin plays a minor role in adult calcium regulation compared to PTH and vitamin D.
🧾Thyroid Hormones
| Hormone | Source | Target | Main Function |
|---|---|---|---|
| T₄ (Thyroxine) | Follicular cells | All body cells | Increases metabolism, promotes growth |
| T₃ (Triiodothyronine) | Follicular cells | All body cells | More active form of T₄ |
| Calcitonin | Parafollicular cells (C cells) | Bones, kidneys | Lowers blood calcium by inhibiting bone resorption |
✅
Thyroid hormones are essential for maintaining metabolic rate, growth, nervous system activity, and calcium balance. Abnormalities in thyroid function affect multiple organ systems and require careful monitoring, especially in pregnancy, children, and the elderly.
🦠 Parathyroid Hormones and Their Functions – Academic Overview
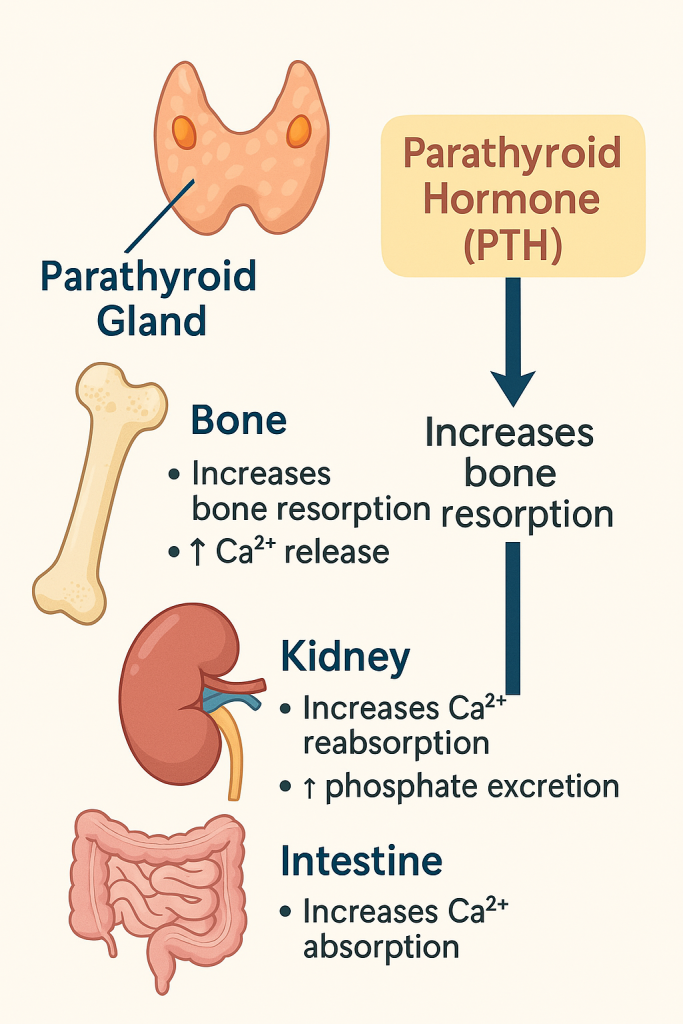
The parathyroid glands are four small, oval-shaped endocrine glands located on the posterior surface of the thyroid gland. Their primary role is to regulate calcium and phosphate metabolism in the body through the secretion of parathyroid hormone (PTH).
📍 I. Hormone Produced
| Hormone | Secreted by | Target Tissues |
|---|---|---|
| Parathyroid Hormone (PTH) | Chief cells of parathyroid gland | Bones, kidneys, and intestines |
🧪 II. Regulation of PTH Secretion
PTH secretion is tightly regulated by the blood levels of ionized calcium:
- ↓ Serum calcium → ↑ PTH secretion
- ↑ Serum calcium → ↓ PTH secretion
- Negative feedback mechanism via calcium-sensing receptors (CaSR) on parathyroid cells
🧠 III. Functions of Parathyroid Hormone (PTH)
PTH increases serum calcium and reduces serum phosphate by acting on:
1. 🦴 Bone
- PTH stimulates osteoclasts (indirectly via osteoblasts) to resorb bone matrix.
- Releases calcium and phosphate into the bloodstream.
- Increases calcium levels in the blood.
2. 🩸 Kidneys
- Increases calcium reabsorption in the distal tubules → conserves calcium.
- Decreases phosphate reabsorption in the proximal tubules → increases phosphate excretion (phosphaturia).
- Stimulates the activation of vitamin D (converts 25-OH vitamin D to 1,25(OH)₂D or calcitriol).
3. 🍽️ Intestine (Indirect Action via Calcitriol)
- PTH indirectly promotes intestinal calcium and phosphate absorption by stimulating calcitriol synthesis in the kidneys.
- Calcitriol increases expression of calcium-binding proteins in the gut.
🔁 IV. Summary of PTH Effects on Calcium and Phosphate
| Organ | Effect on Calcium | Effect on Phosphate |
|---|---|---|
| Bone | ↑ Resorption → ↑ Ca²⁺ | ↑ Phosphate release |
| Kidney | ↑ Ca²⁺ reabsorption | ↓ Phosphate reabsorption → ↑ excretion |
| Intestine | ↑ Absorption via vitamin D | ↑ Absorption via vitamin D |
⚠️ V. Clinical Conditions Related to PTH
1. Hyperparathyroidism
- Primary: Caused by parathyroid adenoma or hyperplasia
- Features:
- ↑ Serum calcium
- Bone pain, fractures (due to bone resorption)
- Renal stones (hypercalciuria)
- Abdominal groans (constipation)
- Psychic moans (depression, confusion)
2. Hypoparathyroidism
- Due to surgery (thyroidectomy), autoimmune destruction, or congenital absence
- Features:
- ↓ Serum calcium
- Tetany, muscle cramps, paresthesias
- Positive Chvostek’s and Trousseau’s signs
3. Pseudohypoparathyroidism
- Genetic disorder where organs are resistant to PTH
- PTH levels are high, but calcium remains low
🧾 VI. PTH Actions and Outcomes
| Target Organ | Action of PTH | Physiological Effect |
|---|---|---|
| Bone | Stimulates osteoclast-mediated resorption | ↑ Serum calcium and phosphate |
| Kidney | ↑ Calcium reabsorption, ↓ Phosphate reabsorption | ↑ Ca²⁺, ↓ PO₄³⁻ in blood |
| Kidney (enzyme) | Activates 1α-hydroxylase → ↑ Calcitriol | ↑ Intestinal calcium absorption |
| Intestine | Indirectly ↑ calcium absorption via calcitriol | ↑ Ca²⁺ uptake from food |
✅
The parathyroid hormone (PTH) is a key regulator of calcium homeostasis, acting on bone, kidneys, and the intestines to raise serum calcium levels while reducing phosphate. Its balanced action is essential for nerve conduction, muscle contraction, and bone health. Dysfunction in PTH secretion leads to serious metabolic and neuromuscular disorders.
🧠 Thymus Gland – Hormones and Functions (Academic Overview)
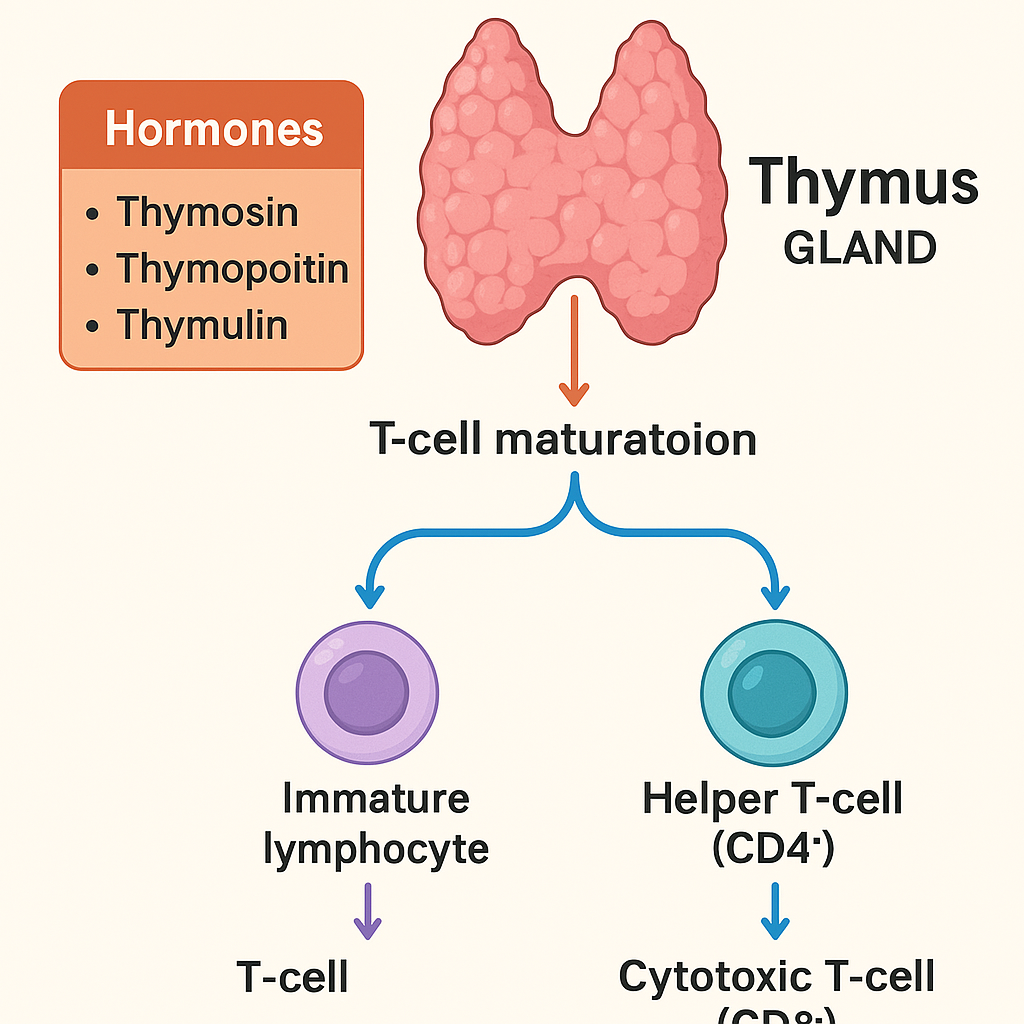
The thymus is a primary lymphoid organ that plays a vital role in the development of the immune system, particularly during childhood. It secretes hormones that regulate the maturation and differentiation of T lymphocytes, which are central to adaptive immunity.
📍 I. Anatomy and Structure
- Location: In the upper anterior mediastinum, just behind the sternum and in front of the heart
- Size: Prominent in infants and children, shrinks (involutes) after puberty
- Structure:
- Two lobes
- Outer cortex (dense with immature T-cells)
- Inner medulla (fewer, more mature T-cells and Hassall’s corpuscles)
🧬 II. Hormones Secreted by the Thymus
| Hormone | Type | Primary Role |
|---|---|---|
| Thymosin | Peptide hormone | Promotes T-cell maturation |
| Thymopoietin | Glycoprotein | Stimulates T-cell differentiation |
| Thymulin | Zinc-dependent peptide | Enhances T-cell function |
| Thymic humoral factor (THF) | Polypeptide | Aids in T-cell differentiation and immune modulation |
These hormones are not strongly differentiated in humans, but they work together to develop and maintain the immune response, especially in early life.
🔬 III. Functions of Thymic Hormones
1. 🧠 T-cell Maturation and Differentiation
- Convert immature lymphocytes (from bone marrow) into immunocompetent T-cells
- Allow for development of:
- Helper T-cells (CD4⁺)
- Cytotoxic T-cells (CD8⁺)
- Regulatory T-cells
2. 🛡️ Central Immune Tolerance
- Ensures that developing T-cells that react strongly to self-antigens are eliminated
- Prevents autoimmune diseases
3. 🧬 Immunoregulation
- Regulates balance between immunity and tolerance
- Coordinates immune responses during infections, inflammation, and stress
4. 🧒 Support of Immune Development in Infants and Children
- Critical during childhood when the immune system is still developing
- After puberty, thymic function declines, and memory T-cells maintain long-term immunity
📉 IV. Thymic Involution (Atrophy)
- After puberty, the thymus gradually shrinks and is replaced by fat
- Reduced production of thymic hormones
- Immunity becomes more dependent on existing T-cell memory than new T-cell development
🩺 V. Clinical Relevance
| Condition | Impact on Thymus or Hormones |
|---|---|
| DiGeorge Syndrome | Congenital absence of thymus → T-cell deficiency |
| Thymoma | Tumor of thymic epithelial cells; may cause myasthenia gravis |
| Autoimmune diseases | May be linked to failure of central tolerance |
| Age-related immunodeficiency | Linked to thymic involution |
🧾 Thymus Hormones & Functions
| Hormone | Main Function |
|---|---|
| Thymosin | Enhances T-cell differentiation and immune activity |
| Thymopoietin | Supports T-cell development and signaling |
| Thymulin | Involved in immune regulation and T-cell activation |
| THF | Promotes T-cell maturation and immune responsiveness |
✅
The thymus gland is essential in establishing a functional and self-tolerant T-cell population, which is crucial for adaptive immunity. Although its activity diminishes with age, the immunological foundation it lays during childhood is critical for lifelong immune competence.
🩺 Pancreas – Hormones and Their Functions
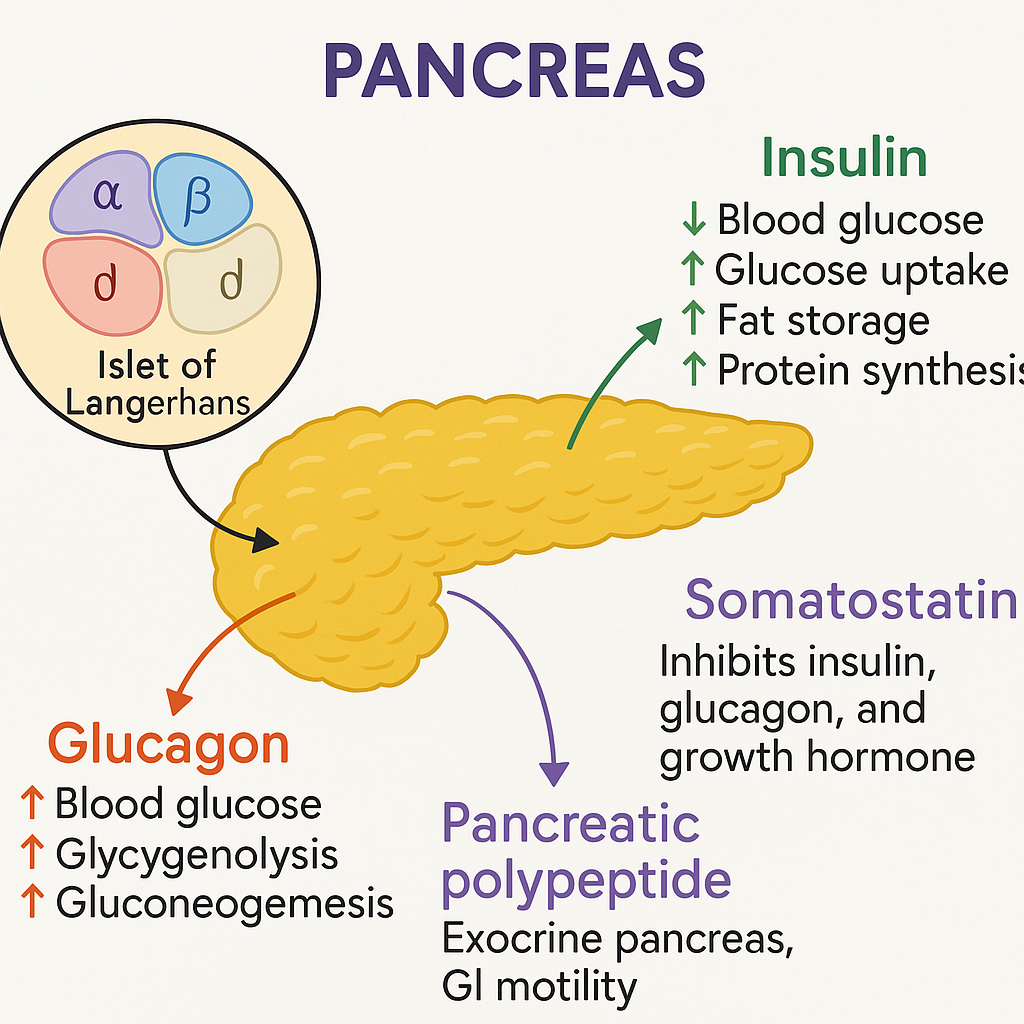
The pancreas is a dual-function gland with both:
- Exocrine functions (digestive enzyme secretion)
- Endocrine functions (hormone secretion into the bloodstream)
The endocrine portion is made up of the Islets of Langerhans, which secrete hormones that regulate blood glucose, digestion, and metabolism.
🔬 I. Islets of Langerhans – Cell Types and Hormones
| Cell Type | Hormone Secreted | Percentage of Islet Cells | Main Function |
|---|---|---|---|
| α (Alpha) | Glucagon | ~20% | Increases blood glucose |
| β (Beta) | Insulin, Amylin | ~70% | Lowers blood glucose |
| δ (Delta) | Somatostatin | ~5–10% | Inhibits insulin, glucagon, GH |
| PP (F cells) | Pancreatic Polypeptide | ~1–2% | Regulates exocrine pancreas, GI motility |
🧬 II. Pancreatic Hormones and Their Functions
🔹 1. Insulin
Secreted by: β-cells
Stimulus: ↑ Blood glucose, amino acids, parasympathetic stimulation
Inhibited by: Somatostatin, sympathetic stimulation
Functions:
- Lowers blood glucose by:
- Promoting glucose uptake (via GLUT-4 receptors) in muscle, fat, liver
- Stimulating glycogenesis (glucose → glycogen in liver)
- Inhibiting glycogenolysis and gluconeogenesis
- Increases fat storage:
- Stimulates lipogenesis, inhibits lipolysis
- Promotes protein synthesis in muscle
🩺 Deficiency or resistance to insulin leads to diabetes mellitus.
🔹 2. Glucagon
Secreted by: α-cells
Stimulus: ↓ Blood glucose, amino acids, sympathetic stimulation
Inhibited by: Insulin, somatostatin
Functions:
- Raises blood glucose by:
- Stimulating glycogenolysis (glycogen → glucose)
- Stimulating gluconeogenesis (non-carbohydrate → glucose)
- Promoting lipolysis in adipose tissue
- Acts mainly on liver to release glucose into the bloodstream
🔹 3. Somatostatin
Secreted by: δ-cells
Stimulus: Food intake, especially proteins and fats
Functions:
- Inhibitory hormone:
- Inhibits insulin and glucagon secretion
- Reduces GI motility
- Inhibits gastric acid, pancreatic enzyme, and bile secretion
🧠 Also secreted by the hypothalamus to inhibit growth hormone.
🔹 4. Pancreatic Polypeptide
Secreted by: PP cells (F cells)
Stimulus: Fasting, exercise, hypoglycemia
Inhibited by: Somatostatin, glucose
Functions:
- Regulates pancreatic enzyme secretion
- Modulates gallbladder contraction and gastric emptying
- May affect appetite and food intake
🔹 5. Amylin (Co-secreted with Insulin)
Secreted by: β-cells
Functions:
- Slows gastric emptying
- Suppresses glucagon secretion
- Promotes satiety to prevent postprandial hyperglycemia
🧾 III. Pancreatic Hormones
| Hormone | Source Cell | Function |
|---|---|---|
| Insulin | β-cells | ↓ Blood glucose, ↑ fat/protein synthesis |
| Glucagon | α-cells | ↑ Blood glucose via glycogenolysis & gluconeogenesis |
| Somatostatin | δ-cells | Inhibits insulin, glucagon, digestive secretions |
| Pancreatic Polypeptide | PP cells | Regulates exocrine function & appetite |
| Amylin | β-cells | Slows gastric emptying, ↓ glucagon, ↑ satiety |
🩺 IV. Clinical Relevance
| Condition | Hormone Involved | Effect |
|---|---|---|
| Type 1 Diabetes Mellitus | ↓ Insulin (autoimmune) | Hyperglycemia, ketoacidosis |
| Type 2 Diabetes Mellitus | Insulin resistance | Hyperglycemia, metabolic syndrome |
| Glucagonoma | ↑ Glucagon | Diabetes, weight loss, necrolytic migratory erythema |
| Somatostatinoma | ↑ Somatostatin | Diabetes, gallstones, steatorrhea |
| Insulinoma | ↑ Insulin (tumor) | Hypoglycemia |
The endocrine pancreas, through a balance of insulin, glucagon, and other hormones, plays a central role in glucose and metabolic regulation. Proper function of these hormones is critical for homeostasis, and their dysregulation leads to serious metabolic disorders like diabetes mellitus.
🧠 Adrenal Glands – Hormones and Functions
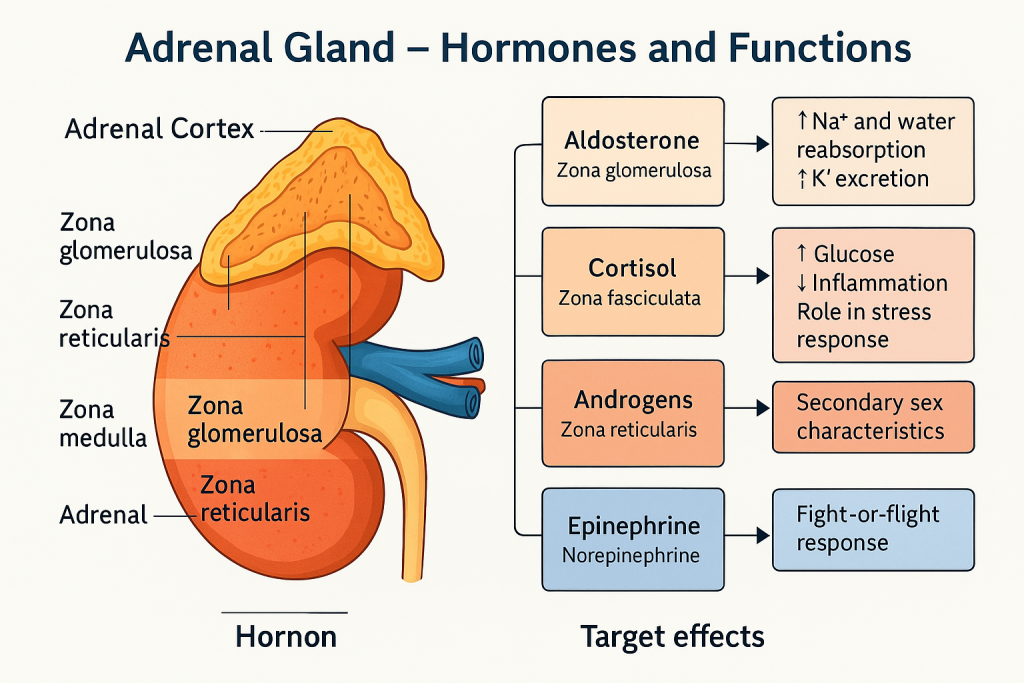
The adrenal glands (also called suprarenal glands) are paired endocrine organs located above the kidneys. Each gland consists of two functionally and structurally distinct parts:
- Adrenal Cortex (outer layer – ~90% of the gland)
- Adrenal Medulla (inner core – ~10%)
These regions produce different classes of hormones vital for metabolism, stress response, fluid balance, and fight-or-flight reactions.
🧬 I. Adrenal Cortex – Hormones and Functions
The adrenal cortex is divided into three zones, each producing a specific type of hormone:
| Zone | Hormone Type | Main Hormones |
|---|---|---|
| Zona glomerulosa | Mineralocorticoids | Aldosterone |
| Zona fasciculata | Glucocorticoids | Cortisol |
| Zona reticularis | Gonadocorticoids | Androgens (DHEA, androstenedione) |
🔹 1. Mineralocorticoids (Aldosterone)
Produced in: Zona glomerulosa
Regulated by: Renin–angiotensin–aldosterone system (RAAS), blood potassium levels
Functions:
- Promotes sodium (Na⁺) reabsorption in renal distal tubules and collecting ducts
- Promotes potassium (K⁺) excretion
- Increases water retention and blood pressure
🩺 Excess → hyperaldosteronism; Deficiency → Addison’s disease
🔹 2. Glucocorticoids (Cortisol)
Produced in: Zona fasciculata
Regulated by: ACTH (from anterior pituitary)
Functions:
- Stress response: Increases blood glucose for energy
- Promotes gluconeogenesis, protein breakdown, and lipolysis
- Suppresses immune response (anti-inflammatory)
- Maintains vascular tone and blood pressure
- Helps regulate circadian rhythm
🩺 Excess → Cushing’s syndrome; Deficiency → Addison’s disease
🔹 3. Gonadocorticoids (Adrenal androgens)
Produced in: Zona reticularis
Main hormones: DHEA (dehydroepiandrosterone), androstenedione
Functions:
- Contribute to secondary sex characteristics, especially in females (e.g., pubic and axillary hair)
- Precursor for testosterone and estrogen synthesis
- Important in postmenopausal women (major source of estrogen)
🩺 Excess → virilization in females (adrenogenital syndrome)
🔥 II. Adrenal Medulla – Hormones and Functions
The adrenal medulla contains chromaffin cells, which are modified sympathetic neurons.
| Hormones | Type | Function |
|---|---|---|
| Epinephrine | Catecholamine | Increases heart rate, dilates bronchi, mobilizes energy |
| Norepinephrine | Catecholamine | Vasoconstriction → increases blood pressure |
These hormones are released during fight-or-flight response, stimulated by sympathetic nervous system via acetylcholine.
🧬 Functions of Catecholamines (Adrenaline & Noradrenaline)
- ↑ Heart rate, cardiac output
- ↑ Blood glucose (glycogenolysis and lipolysis)
- Bronchodilation (relaxes airways)
- Vasodilation in muscles, vasoconstriction in skin/GI tract
- Pupil dilation
- ↓ GI motility, ↑ alertness
🩺 Overproduction (e.g., pheochromocytoma) → hypertension, sweating, tachycardia, headache
🧾 Summary Table: Adrenal Gland Hormones
| Region | Hormone | Function |
|---|---|---|
| Zona glomerulosa | Aldosterone | ↑ Na⁺ reabsorption, ↑ BP, ↓ K⁺ |
| Zona fasciculata | Cortisol | ↑ Glucose, ↓ Inflammation, stress response |
| Zona reticularis | Androgens (DHEA) | Secondary sex traits, sex hormone precursors |
| Adrenal medulla | Epinephrine | Fight-or-flight: ↑ HR, ↑ glucose, ↑ alertness |
| Adrenal medulla | Norepinephrine | Vasoconstriction → ↑ BP |
🩺 III. Clinical Disorders Related to Adrenal Hormones
| Disorder | Cause | Hormonal Effect |
|---|---|---|
| Addison’s disease | Autoimmune destruction | ↓ Cortisol, ↓ Aldosterone |
| Cushing’s syndrome | Cortisol excess (tumor/steroid use) | ↑ Cortisol |
| Conn’s syndrome | Aldosterone-producing tumor | ↑ Aldosterone → HTN, ↓ K⁺ |
| Congenital adrenal hyperplasia (CAH) | Enzyme defect (21-hydroxylase) | ↑ Androgens, ↓ Cortisol |
| Pheochromocytoma | Chromaffin cell tumor | ↑ Catecholamines → ↑ BP, tachycardia |
The adrenal gland is a key player in metabolism, stress regulation, blood pressure control, electrolyte balance, and sex hormone modulation. Its two regions—the cortex and medulla—coordinate short- and long-term responses to internal and external stressors, making it a critical endocrine organ.
🧬 Ovaries – Hormones and Their Functions
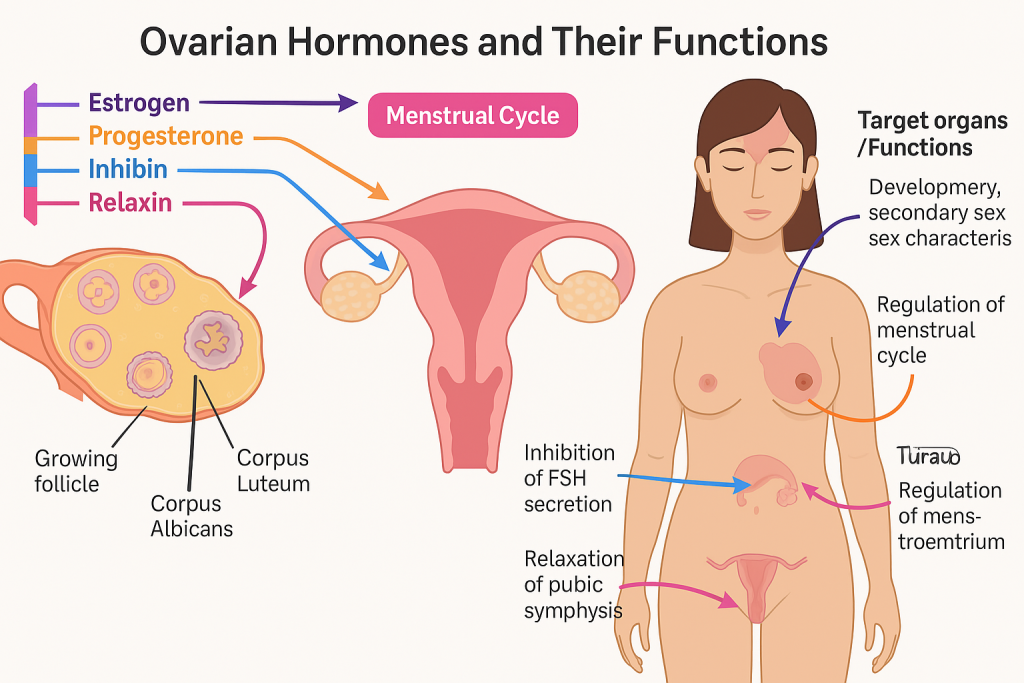
The ovaries are paired female gonads located on either side of the uterus. They serve dual functions:
- Gamete production (ova or eggs)
- Endocrine function – Secretion of female sex hormones that regulate the menstrual cycle, pregnancy, and secondary sex characteristics
🧠 I. Main Hormones Produced by the Ovaries
| Hormone | Produced By | Main Function |
|---|---|---|
| Estrogen | Granulosa cells of ovarian follicles, corpus luteum, placenta (during pregnancy) | Development of female secondary sex characteristics, regulation of menstrual cycle |
| Progesterone | Corpus luteum, placenta | Prepares and maintains endometrium, supports pregnancy |
| Inhibin | Granulosa cells | Inhibits FSH secretion |
| Relaxin | Corpus luteum and placenta | Relaxes uterine muscles and pubic symphysis during pregnancy |
🟣 II. Estrogen – The Primary Female Sex Hormone
🔬 Types of Estrogen:
- Estradiol (E2) – Most potent and predominant during reproductive years
- Estrone (E1) – Dominant after menopause
- Estriol (E3) – Predominant during pregnancy
📌 Functions:
- Stimulates development of female secondary sex characteristics:
- Breast development
- Wider pelvis
- Fat distribution
- Regulates menstrual cycle:
- Promotes proliferation of endometrium during the follicular phase
- Increases uterine sensitivity to oxytocin
- Stimulates cervical mucus production
- Maintains vaginal elasticity and bone density
🩺 Estrogen is cardioprotective and helps prevent osteoporosis.
🟡 III. Progesterone – The Hormone of Pregnancy
🔬 Secreted by:
- Corpus luteum (after ovulation)
- Placenta (during pregnancy)
📌 Functions:
- Prepares endometrium for implantation
- Maintains the uterine lining during pregnancy
- Inhibits uterine contractions to prevent premature labor
- Stimulates glandular secretion in endometrial lining
- Develops mammary glands for lactation
🩺 Low progesterone can lead to luteal phase defect and miscarriage.
🔹 IV. Inhibin
📌 Functions:
- Inhibits FSH release from the anterior pituitary
- Participates in negative feedback to regulate follicular development
🔸 V. Relaxin
📌 Functions:
- Relaxes uterine smooth muscle to prevent contractions in early pregnancy
- Relaxes the pubic symphysis and cervix during labor
- Aids in cardiovascular and renal adaptations in pregnancy
🧾 VI. Hormonal Cycle Summary – Menstrual Cycle Phases
| Phase | Dominant Hormone | Function |
|---|---|---|
| Follicular Phase | Estrogen | Follicle development, endometrial proliferation |
| Ovulation | LH surge, Estrogen | Release of ovum |
| Luteal Phase | Progesterone | Endometrial maturation, preparation for implantation |
| Menstruation | Drop in Estrogen & Progesterone | Shedding of endometrium |
🩺 VII. Clinical Relevance
| Condition | Hormonal Disruption | Manifestation |
|---|---|---|
| Polycystic Ovary Syndrome (PCOS) | ↑ Androgens, ↓ Estrogen feedback | Irregular periods, hirsutism, infertility |
| Menopause | ↓ Estrogen and Progesterone | Hot flashes, osteoporosis, mood swings |
| Amenorrhea | ↓ Estrogen or Progesterone | Absence of menstruation |
| Infertility | Luteal phase defect or FSH/LH imbalance | Anovulation |
| Ovarian tumors | Hormonal excess (e.g., estrogen-secreting) | Abnormal bleeding, early puberty |
The ovaries produce estrogen, progesterone, inhibin, and relaxin, which collectively control female reproductive function, regulate the menstrual cycle, maintain pregnancy, and influence secondary sexual development. Understanding these hormones is vital for diagnosing and managing female reproductive and endocrine disorders.
🧬 Testes – Hormones and Their Functions
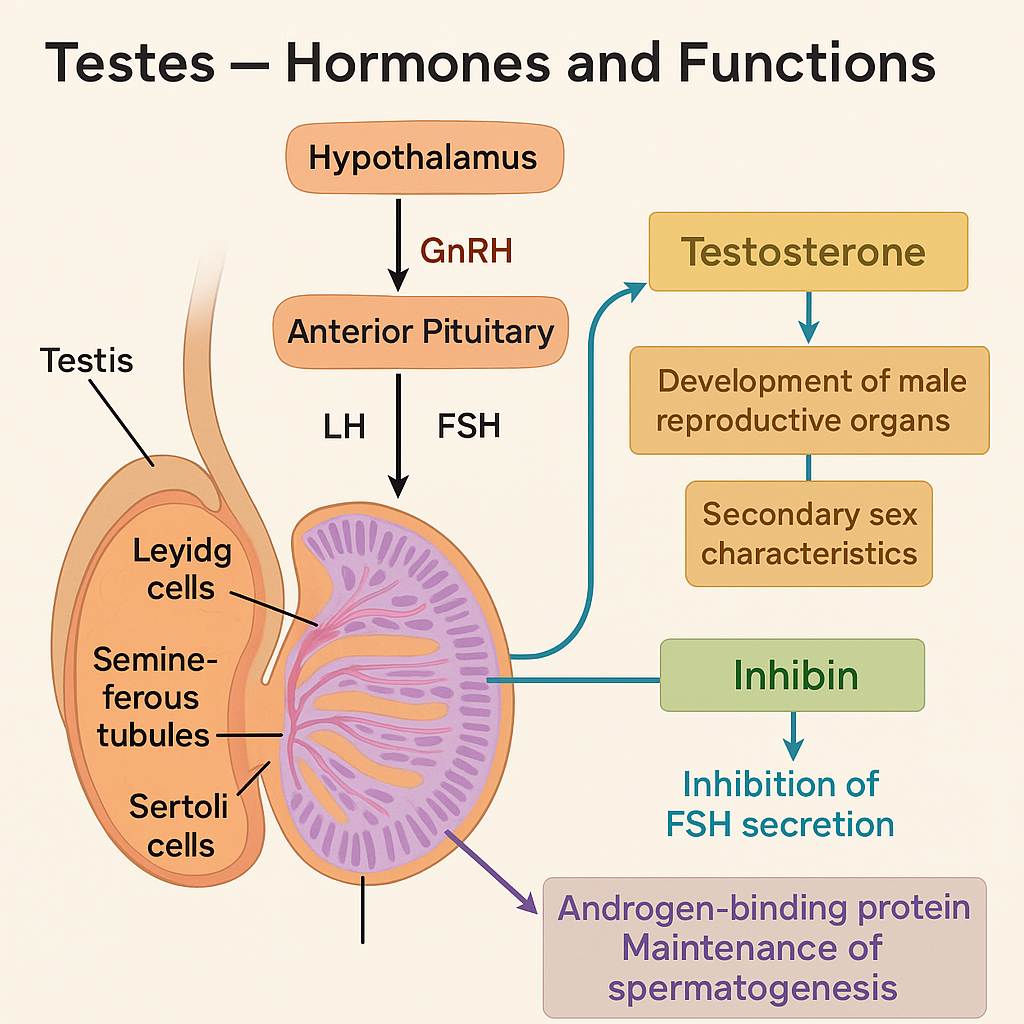
The testes are the primary male reproductive glands, housed within the scrotum. They serve two major functions:
- Spermatogenesis (production of sperm)
- Endocrine function – Secretion of male sex hormones (androgens)
These functions are tightly regulated by the hypothalamic-pituitary-gonadal (HPG) axis.
🧠 I. Cell Types of the Testes Involved in Hormone Production
| Cell Type | Location | Hormone Secreted |
|---|---|---|
| Leydig cells (interstitial cells) | Between seminiferous tubules | Testosterone (androgens) |
| Sertoli cells | Inside seminiferous tubules | Inhibin, ABP (androgen-binding protein) |
🔬 II. Major Hormones and Their Functions
🔹 1. Testosterone (Primary Male Sex Hormone)
Produced by: Leydig cells in response to LH (Luteinizing Hormone) from the anterior pituitary.
Functions:
🧔 A. Developmental & Reproductive Functions
- Stimulates differentiation of male reproductive organs (fetal stage)
- Initiates spermatogenesis in puberty
- Promotes development of secondary sexual characteristics:
- Deepening of voice
- Facial/body hair growth
- Muscle mass and strength
- Growth of penis and scrotum
- Maintains libido and sexual function
🧬 B. Metabolic Functions
- Anabolic effect: promotes protein synthesis and muscle growth
- Erythropoietic effect: increases red blood cell production
- Influences bone growth and closure of epiphyseal plates
🧠 C. Feedback Regulation
- Negative feedback on hypothalamus and pituitary to regulate GnRH and LH levels
🔸 2. Inhibin
Produced by: Sertoli cells
Stimulated by: High FSH levels
Functions:
- Inhibits FSH release from the anterior pituitary
- Helps regulate spermatogenesis
- Provides negative feedback to maintain sperm production balance
🔸 3. Androgen-Binding Protein (ABP)
Produced by: Sertoli cells in response to FSH
Function: Binds testosterone and maintains high local concentration within the seminiferous tubules to support spermatogenesis
🔸 4. Estrogen (small amount)
- Formed from testosterone via aromatase enzyme in Sertoli and Leydig cells
- May play a role in:
- Sperm maturation
- Fluid reabsorption in efferent ductules
- Feedback regulation
🧾 III. Summary Table – Testicular Hormones
| Hormone | Secreted By | Main Function |
|---|---|---|
| Testosterone | Leydig cells | Male development, spermatogenesis, libido, muscle mass |
| Inhibin | Sertoli cells | Inhibits FSH, regulates spermatogenesis |
| ABP | Sertoli cells | Maintains high testosterone in seminiferous tubules |
| Estrogen (minor) | Sertoli/Leydig cells | Supports sperm maturation, fluid balance |
🔁 IV. Hormonal Regulation – HPG Axis
- Hypothalamus secretes GnRH
- GnRH stimulates anterior pituitary to secrete:
- LH → stimulates Leydig cells to produce testosterone
- FSH → stimulates Sertoli cells to support sperm development and produce inhibin
- Testosterone and inhibin exert negative feedback on GnRH, LH, and FSH
🩺 V. Clinical Significance of Testicular Hormones
| Condition | Hormonal Basis | Manifestations |
|---|---|---|
| Hypogonadism | ↓ Testosterone | Delayed puberty, infertility, decreased libido |
| Klinefelter Syndrome (XXY) | Primary testicular failure, ↓ Testosterone | Infertility, gynecomastia, reduced facial hair |
| Androgen Insensitivity Syndrome | Defective testosterone receptors | Female phenotype despite XY genotype |
| Anabolic steroid abuse | Excess synthetic androgens → ↓ endogenous LH/FSH | Testicular atrophy, infertilit |
The testes are essential for producing testosterone, which governs male sexual development, spermatogenesis, and overall male physiology. Other hormones like inhibin and ABP fine-tune the regulation of FSH and support sperm production. Disruption in these hormones leads to reproductive, metabolic, and developmental disorders.
🧠 Alterations in Disease of the Endocrine System – Academic Overview
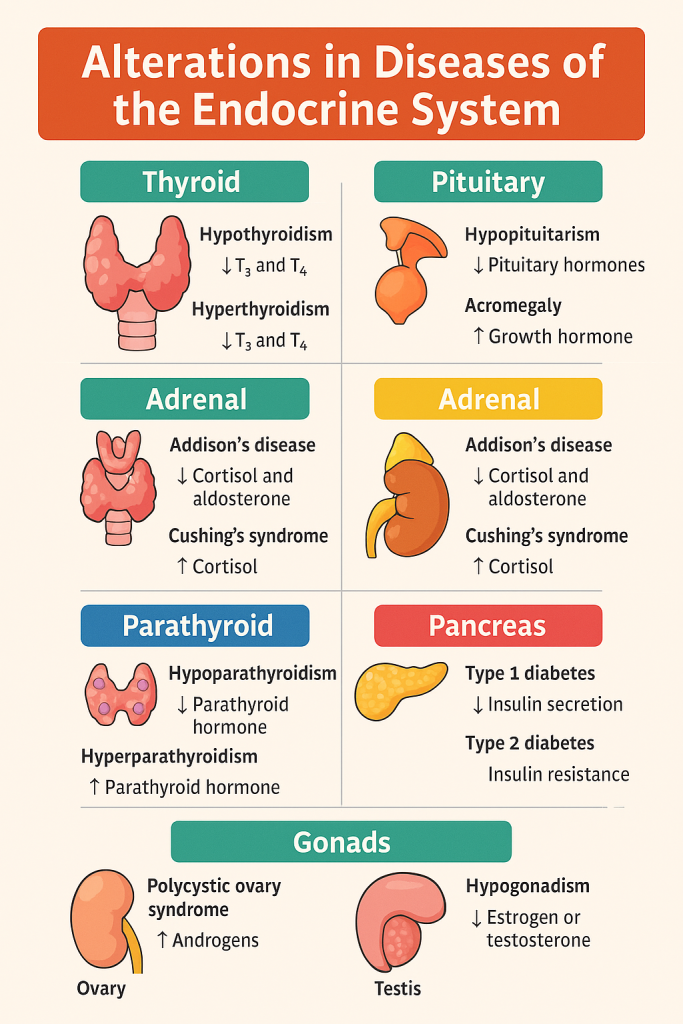
The endocrine system regulates essential body processes like metabolism, growth, reproduction, fluid balance, and stress response through the release of hormones. Diseases of the endocrine system lead to either:
- Hyperfunction – Excessive hormone production
- Hypofunction – Inadequate hormone production
These alterations can affect any endocrine gland and result in systemic manifestations.
🔬 I. General Types of Endocrine Alterations
| Type of Alteration | Description | Example |
|---|---|---|
| Hyposecretion | Underproduction of a hormone | Hypothyroidism, Addison’s disease |
| Hypersecretion | Overproduction of a hormone | Hyperthyroidism, Cushing’s syndrome |
| Hormone resistance | Tissues become insensitive to normal hormone levels | Type 2 Diabetes Mellitus |
| Hormone excess from tumors | Non-glandular tissues secrete hormones | Pheochromocytoma, paraneoplastic syndromes |
| Autoimmune destruction | Immune system attacks endocrine tissues | Type 1 Diabetes, Hashimoto’s thyroiditis |
🦋 II. Common Endocrine Disorders and Their Alterations
🔹 Thyroid Disorders
1. Hypothyroidism
- ↓ T₃ and T₄
- Causes: Hashimoto’s thyroiditis (autoimmune), iodine deficiency
- Symptoms: Fatigue, weight gain, cold intolerance, dry skin, bradycardia
2. Hyperthyroidism
- ↑ T₃ and T₄
- Causes: Graves’ disease (autoimmune), thyroid nodules
- Symptoms: Weight loss, heat intolerance, anxiety, tremors, tachycardia
🔹 Pituitary Disorders
1. Hypopituitarism
- ↓ GH, TSH, ACTH, LH/FSH, PRL
- Causes: Tumor, trauma, infarction (Sheehan’s syndrome)
- Symptoms: Growth failure, fatigue, amenorrhea, infertility
2. Pituitary Adenomas (Hyperpituitarism)
- ↑ GH → Acromegaly (adults), gigantism (children)
- ↑ ACTH → Cushing’s disease
- ↑ Prolactin → Galactorrhea, amenorrhea
🔹 Adrenal Disorders
1. Addison’s Disease (Adrenal Insufficiency)
- ↓ Cortisol and aldosterone
- Causes: Autoimmune destruction, TB
- Symptoms: Hypotension, hyperpigmentation, fatigue, hyponatremia
2. Cushing’s Syndrome
- ↑ Cortisol
- Causes: Tumor, long-term steroid therapy
- Symptoms: Moon face, truncal obesity, striae, hypertension, glucose intolerance
3. Pheochromocytoma
- ↑ Catecholamines (epinephrine/norepinephrine)
- Symptoms: Paroxysmal hypertension, palpitations, sweating
🔹 Parathyroid Disorders
1. Hypoparathyroidism
- ↓ PTH → ↓ Ca²⁺
- Symptoms: Tetany, muscle cramps, Chvostek & Trousseau signs
2. Hyperparathyroidism
- ↑ PTH → ↑ Ca²⁺
- Symptoms: Bone pain, kidney stones, abdominal discomfort
🔹 Pancreatic Disorders (Endocrine)
1. Type 1 Diabetes Mellitus
- Autoimmune destruction of β-cells → ↓ insulin
- Symptoms: Polyuria, polydipsia, weight loss, DKA
2. Type 2 Diabetes Mellitus
- Insulin resistance ± relative insulin deficiency
- Symptoms: Hyperglycemia, fatigue, poor wound healing
🔹 Gonadal Disorders
1. Hypogonadism (Male or Female)
- ↓ Testosterone or estrogen/progesterone
- Symptoms: Infertility, amenorrhea, loss of secondary sex characteristics
2. Polycystic Ovary Syndrome (PCOS)
- ↑ Androgens, insulin resistance
- Symptoms: Irregular menses, hirsutism, acne, infertility
🩺 III. Summary Table of Endocrine Alterations
| Gland | Disease | Hormone Altered | Effect |
|---|---|---|---|
| Thyroid | Hypo/Hyperthyroidism | T₃, T₄ | Metabolic slowdown/speedup |
| Pituitary | Adenoma, Sheehan’s, Hypopituitarism | GH, ACTH, TSH, LH/FSH | Growth, reproduction, cortisol |
| Adrenal | Addison’s, Cushing’s | Cortisol, Aldosterone | BP, metabolism, stress response |
| Parathyroid | Hyper/Hypoparathyroidism | PTH | Calcium balance |
| Pancreas | Type 1 & 2 Diabetes | Insulin | Blood glucose regulation |
| Gonads | PCOS, Hypogonadism | Estrogen/Testosterone | Fertility, sexual development |