physio-b.sc-Unit-3-Digestive system
🧠 Overview of Digestive Tract Functions
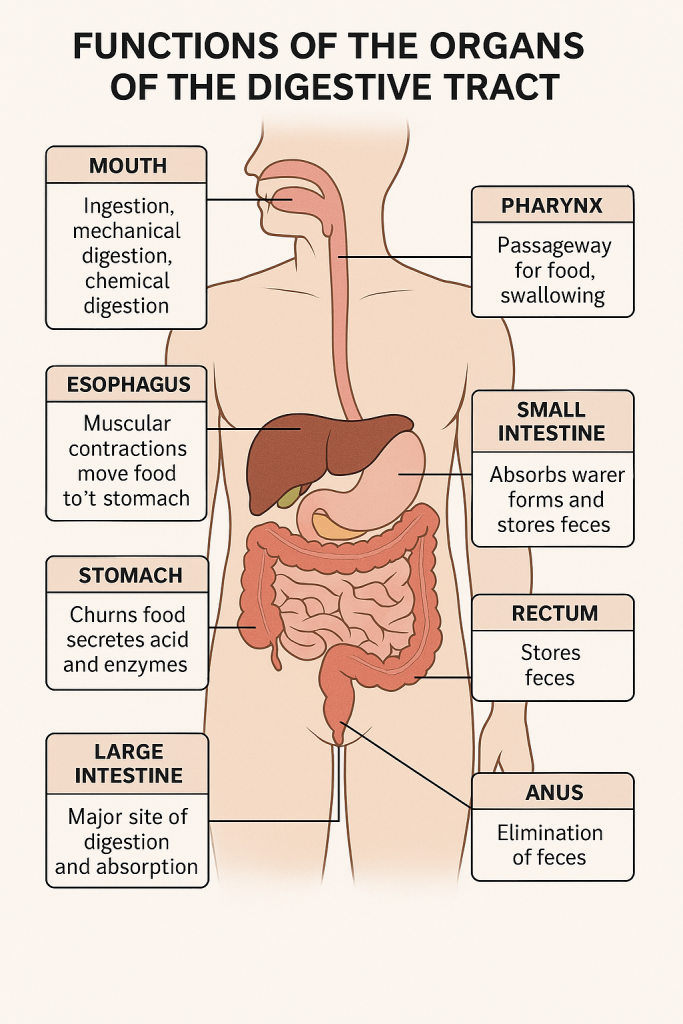
The digestive tract (also called the alimentary canal) is responsible for ingestion, digestion, absorption, and elimination. It includes the mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus.
🥄 1. Mouth (Oral Cavity)
👉 Functions:
- Ingestion: Entry point of food into the digestive system.
- Mechanical digestion: Teeth chew (masticate) food into smaller particles.
- Chemical digestion: Salivary glands secrete saliva containing:
- Amylase (ptyalin) – breaks down starch into maltose.
- Mucus – lubricates food for easy swallowing.
- Formation of bolus: Chewed food mixed with saliva forms a bolus.
- Swallowing (Deglutition): The tongue pushes bolus into the pharynx.
🧣 2. Pharynx
👉 Functions:
- Passageway for food from mouth to esophagus.
- Swallowing reflex: Involuntary phase begins here.
- Prevents choking: Epiglottis closes over the larynx to prevent food from entering the airway.
🧵 3. Esophagus
👉 Functions:
- Transport of bolus from pharynx to stomach.
- Uses peristalsis (wave-like muscular contractions) to move food downward.
- Lower esophageal sphincter (cardiac sphincter):
- Prevents reflux of stomach contents back into the esophagus.
🫙 4. Stomach
👉 Functions:
- Storage: Holds ingested food temporarily.
- Mechanical digestion: Muscular contractions churn food into chyme.
- Chemical digestion:
- Hydrochloric acid (HCl): Denatures proteins, activates enzymes, kills pathogens.
- Pepsin (from pepsinogen + HCl): Begins protein digestion.
- Intrinsic factor: Required for Vitamin B₁₂ absorption.
- Controlled release of chyme into the small intestine via the pyloric sphincter.
🧬 5. Small Intestine (Duodenum, Jejunum, Ileum)
✴️ General Function: Major site of digestion and absorption
👉 Duodenum:
- First part (25 cm long).
- Receives:
- Bile (from liver & gallbladder) – emulsifies fats.
- Pancreatic juice (enzymes + bicarbonate) – digests carbohydrates, proteins, and fats.
- Continues digestion with:
- Amylase – carbohydrate digestion.
- Trypsin & chymotrypsin – protein digestion.
- Lipase – fat digestion.
👉 Jejunum:
- Middle part (approx. 2.5 meters).
- Primary site of absorption of:
- Carbohydrates, amino acids, water-soluble vitamins, and some fats.
👉 Ileum:
- Last part (approx. 3.5 meters).
- Absorbs:
- Vitamin B₁₂, bile salts, and remaining nutrients.
- Contains Peyer’s patches for immune defense.
🪵 6. Large Intestine (Colon)
👉 Functions:
- Absorption:
- Water, electrolytes (Na⁺, Cl⁻), and vitamins produced by gut flora (e.g., Vitamin K, biotin).
- Formation of feces:
- Undigested food, dead cells, bacteria, and waste products compacted.
- Bacterial fermentation:
- Gut microbiota breaks down remaining nutrients, produces gases.
- Mucus secretion:
- Lubricates the passage of feces.
📦 7. Rectum
👉 Functions:
- Temporary storage of feces before elimination.
- Stretch receptors signal when it’s time to defecate.
🚽 8. Anus
👉 Functions:
- Defecation: Elimination of feces through the anal canal.
- Controlled by:
- Internal anal sphincter (involuntary)
- External anal sphincter (voluntary)
| Organ | Major Functions |
|---|---|
| Mouth | Ingestion, chewing, salivary digestion (amylase) |
| Pharynx | Swallowing reflex |
| Esophagus | Peristaltic transport of bolus |
| Stomach | Mechanical + chemical digestion (HCl, pepsin), storage |
| Small Intestine | Digestion & nutrient absorption |
| Large Intestine | Water & electrolyte absorption, feces formation |
| Rectum | Feces storage |
| Anus | Defecation |
🧪 Saliva: Composition, Regulation, and Functions (Narrative Explanation)
Saliva is a vital biological fluid that plays a central role in oral and digestive health. Secreted by the salivary glands, this clear, slightly alkaline fluid not only initiates digestion but also protects the oral cavity, aids in taste, and facilitates speech. On average, a healthy adult produces 1 to 1.5 liters of saliva per day under normal physiological conditions.
🔷 Composition of Saliva
Saliva is composed primarily of water (approximately 99%), making it an effective solvent for dissolving food substances and activating enzymes. The remaining 1% comprises a rich mix of electrolytes, organic substances, enzymes, and immune proteins.
● Electrolytes
Saliva contains various ions that maintain oral pH and support tooth integrity. Sodium (Na⁺) and chloride (Cl⁻) help regulate osmotic balance, while potassium (K⁺) is present in higher concentrations than in plasma. Calcium (Ca²⁺) and phosphate contribute to tooth remineralization, while bicarbonate (HCO₃⁻) acts as a buffering agent to neutralize dietary and bacterial acids.
● Organic Substances
Saliva contains several important organic molecules:
Salivary secretion is governed almost entirely by the autonomic nervous system (ANS), making it a classic example of a reflex process. Unlike many other secretions in the body, salivation is not controlled by hormones.
- Salivary amylase (ptyalin) begins the chemical breakdown of starch into maltose in the mouth.
- Lingual lipase, secreted by glands on the tongue, helps initiate fat digestion, especially important in infants.
- Mucins, glycoproteins that give saliva its slippery quality, lubricate the mouth and protect the mucous membranes.
- Antibacterial agents such as lysozyme, lactoferrin, and peroxidase inhibit bacterial growth and maintain oral hygiene.
- Immunoglobulin A (IgA) provides localized immune protection against pathogens.
- Saliva also contains trace amounts of urea and uric acid, reflecting its minor excretory role.
🔷 Regulation of Salivary Secretion
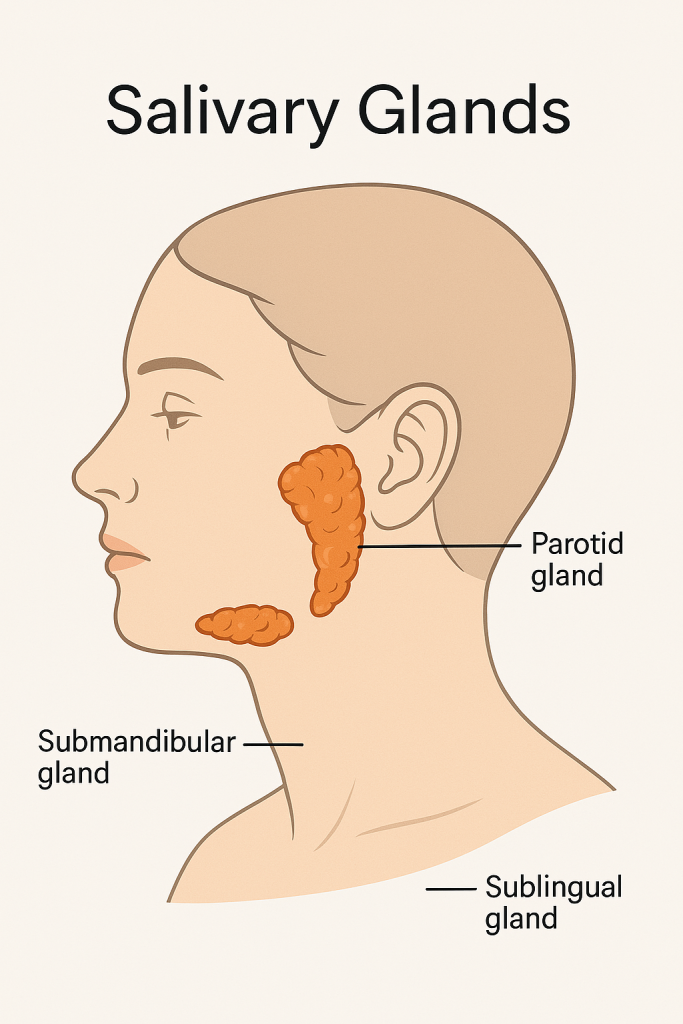
● Salivary Glands
There are three major pairs of salivary glands:
- The parotid glands produce a watery, enzyme-rich saliva.
- The submandibular glands secrete a mix of serous and mucous components.
- The sublingual glands primarily produce thick, mucous-rich saliva.
These are supported by many minor salivary glands located throughout the oral cavity, which contribute to mucosal moisture and immune defense.
● Nervous Regulation
Salivation is controlled through two divisions of the autonomic nervous system:
- Parasympathetic stimulation (via the facial nerve – CN VII, and glossopharyngeal nerve – CN IX) increases saliva production, resulting in a watery, enzyme-rich secretion.
- Sympathetic stimulation (via thoracic spinal nerves) reduces the flow but produces thicker, more mucous-rich saliva due to vasoconstriction.
● Types of Reflexes
There are two primary reflex pathways involved:
- Unconditioned reflexes are triggered directly by food in the mouth, activating taste and pressure receptors that signal the brainstem to stimulate salivary glands.
- Conditioned reflexes occur when saliva is produced in anticipation of food — for example, by the smell, sight, or thought of a meal — and are mediated by higher brain centers (cerebral cortex).
Together, these mechanisms ensure a prompt and appropriate secretion of saliva based on the body’s need, whether at rest, during eating, or even in emotional states like fear or excitement.
🔷 Functions of Saliva
Saliva performs a wide range of functions that support digestion, oral health, and communication.
● 1. Digestive Function
Saliva is the first digestive juice encountered by food. Salivary amylase initiates the breakdown of starches, and lingual lipase begins lipid digestion in neonates. Saliva softens and lubricates food, helping to form a bolus that can be easily swallowed.
● 2. Lubrication and Protection
Mucins in saliva coat the oral mucosa and make chewing, swallowing, and speaking more comfortable. The continuous washing action of saliva clears food debris and microorganisms, preventing bacterial overgrowth. It also dilutes and neutralizes acids, protecting tooth enamel from demineralization.
● 3. Antimicrobial and Immune Functions
Saliva contains a variety of antimicrobial substances. Lysozyme breaks down bacterial cell walls, lactoferrin binds iron to inhibit bacterial growth, and IgA neutralizes pathogens at the mucosal surface. These collectively reduce the risk of oral infections.
● 4. Buffering and Tooth Integrity
Bicarbonate and phosphate ions buffer the oral pH, especially after meals, maintaining an environment less favorable to acidogenic bacteria. The presence of calcium and phosphate ions helps in the remineralization of tooth enamel, which is essential for preventing dental caries.
● 5. Taste and Sensory Perception
Saliva is essential for dissolving food particles, allowing them to interact with taste buds. A dry mouth impairs the ability to taste food accurately.
● 6. Excretory Function
Though minor, saliva plays a role in the excretion of waste products like urea, uric acid, and some medications or toxins, thus supporting detoxification.
● 7. Speech and Oral Comfort
A moist oral cavity is essential for clear speech. Saliva enables the smooth movement of the tongue and lips, helping articulate words and maintain oral comfort throughout the day.
🔷 Clinical Relevance
In conditions like xerostomia (dry mouth)—caused by medications, dehydration, radiation therapy, or autoimmune diseases like Sjögren’s syndrome—the protective and digestive functions of saliva are severely compromised. This can lead to:
- Increased dental caries
- Oral infections (e.g., candidiasis)
- Halitosis (bad breath)
- Difficulty in speaking, chewing, and swallowing
Maintaining healthy salivary flow is essential for both digestive efficiency and oral defense mechanisms.Saliva is far more than just a watery secretion. It is a complex biological fluid with diverse functions—digestive, protective, excretory, and communicative. Understanding its composition and regulation not only aids in comprehending normal physiology but also in recognizing and managing various clinical conditions related to oral and systemic health.
🧪 GASTRIC JUICE: Composition, Function, Mechanism & Regulation
🔷 1. Composition of Gastric Juice
Gastric juice is a digestive fluid secreted by gastric glands in the stomach lining. Approximately 1.5–2 liters of gastric juice is secreted per day. It is acidic (pH ~1.5 to 3.5) and consists of both inorganic and organic components.
📌 Major Components:
| Component | Source | Function |
|---|---|---|
| Hydrochloric acid (HCl) | Parietal (oxyntic) cells | Activates pepsinogen to pepsin, kills bacteria, denatures proteins |
| Pepsinogen | Chief (zymogenic) cells | Converted to pepsin, which digests proteins |
| Mucus | Mucous neck cells | Protects mucosa from acid and pepsin |
| Intrinsic factor | Parietal cells | Essential for Vitamin B₁₂ absorption in the ileum |
| Lipase (gastric lipase) | Chief cells | Begins digestion of fats (mainly in infants) |
| Electrolytes (Na⁺, K⁺, Cl⁻, H⁺) | Gastric secretion | Maintain ionic balance and pH |
| Water | Secretory cells | Solvent for enzymes and nutrients |
🔷 2. Functions of Gastric Juice
🔹 A. Digestive Functions
- Protein digestion: Pepsin (activated by HCl) breaks proteins into peptides.
- Fat digestion (limited): Gastric lipase breaks down triglycerides (especially in infants).
- Activation of enzymes: HCl activates pepsinogen to pepsin.
- Iron absorption: Acidic pH aids in ferrous (Fe²⁺) absorption in the duodenum.
🔹 B. Protective Functions
- Bactericidal: HCl destroys most ingested pathogens.
- Mucosal protection: Mucus forms a protective barrier on the gastric lining.
🔹 C. Absorptive Function
- Intrinsic factor binds to Vitamin B₁₂, enabling its absorption in the terminal ileum.
🔷 3. Mechanism of Gastric Secretion
Gastric secretion is carried out by the specialized cells in the gastric glands:
| Cell Type | Secretions |
|---|---|
| Parietal cells | HCl and intrinsic factor |
| Chief cells | Pepsinogen and gastric lipase |
| Mucous cells | Mucus and bicarbonate |
| G cells (in pyloric antrum) | Gastrin (a hormone that stimulates secretion) |
🔷 4. Phases of Gastric Secretion
Gastric secretion occurs in three phases:
🔸 A. Cephalic Phase (30%)
- Triggered by sight, smell, taste, or thought of food.
- Mediated by the vagus nerve (parasympathetic).
- Stimulates parietal, chief, and G cells.
🔸 B. Gastric Phase (60%)
- Begins when food enters the stomach.
- Stimuli: Stomach distension, peptides, amino acids.
- Triggers:
- Gastrin release → stimulates HCl and pepsinogen secretion.
- Local reflexes and vagal reflexes.
🔸 C. Intestinal Phase (10%)
- Starts when chyme enters the duodenum.
- Initially has a stimulatory effect, then inhibitory.
- Hormones released:
- Secretin: Inhibits gastric acid.
- Cholecystokinin (CCK): Slows gastric emptying.
- Gastric inhibitory peptide (GIP): Inhibits gastric secretions.
🔷 5. Regulation of Gastric Secretion
🔹 A. Neural Regulation
- Controlled by the autonomic nervous system.
- Parasympathetic (vagus nerve): Stimulates gastric secretion via acetylcholine (ACh).
- Sympathetic nerves: Inhibit secretion under stress or fear.
🔹 B. Hormonal Regulation
- Gastrin (from G cells): Increases HCl secretion and gastric motility.
- Somatostatin: Inhibits gastrin, HCl, and pepsinogen release.
- Secretin and CCK: Decrease gastric secretion once chyme enters the duodenum.
🔹 C. Local Regulation
- Enteric nervous system (ENS) regulates local reflexes.
- Histamine (released by ECL cells): Stimulates HCl via H2 receptors on parietal cells.
🔷 6. Clinical Correlation
| Condition | Relevance |
|---|---|
| Peptic ulcer | Hypersecretion of HCl damages mucosa |
| Achlorhydria | Lack of HCl → poor protein digestion, bacterial overgrowth |
| Pernicious anemia | Absence of intrinsic factor → Vitamin B₁₂ deficiency |
| Gastritis | Inflammation of the mucosa alters secretory function |
- Gastric juice is a potent, acidic secretion essential for digestion and protection.
- Its key components include HCl, pepsinogen, mucus, intrinsic factor, and enzymes.
- Secretion is regulated by complex neural, hormonal, and local reflexes through three main phases: cephalic, gastric, and intestinal.
- Proper function is crucial for protein digestion, Vitamin B₁₂ absorption, and maintaining gastrointestinal health.
🧪 Pancreatic Juice – Composition, Functions, and Regulation (Narrative Explanation)
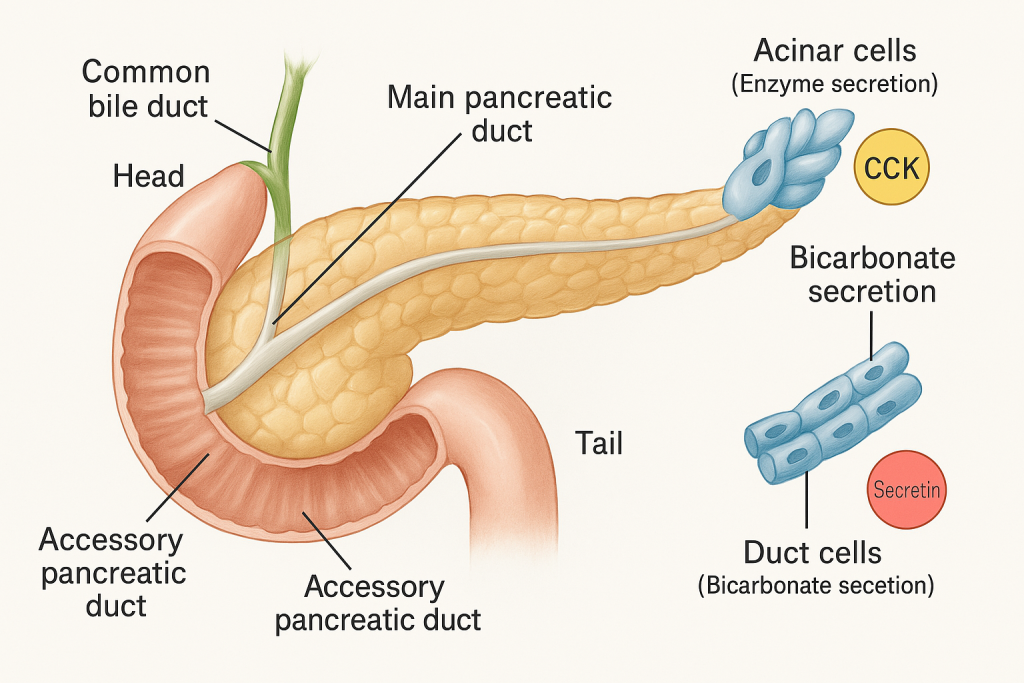
Pancreatic juice is a clear, alkaline, enzyme-rich secretion produced by the exocrine portion of the pancreas. It plays a vital role in digestion by breaking down all three major classes of nutrients—proteins, carbohydrates, and fats—and also helps neutralize the acidic chyme that enters the small intestine from the stomach. A healthy adult secretes about 1200 to 1500 mL of pancreatic juice daily into the duodenum through the main pancreatic duct, which joins the common bile duct at the ampulla of Vater.
🔷 Composition of Pancreatic Juice
Pancreatic juice is made up of two major components: an aqueous bicarbonate-rich fluid and a protein-rich enzymatic secretion. These are secreted by two different types of cells in the pancreas:
- The ductal epithelial cells produce the alkaline, bicarbonate-rich fluid.
- The acinar cells produce digestive enzymes in either active or inactive forms.
1. Aqueous Component (Alkaline Portion)
The fluid portion of pancreatic juice contains a high concentration of bicarbonate ions (HCO₃⁻). This bicarbonate is essential for neutralizing the acidic gastric juice that enters the duodenum. It also maintains the optimal alkaline pH (7.8–8.4) required for enzymatic activity in the small intestine. Other inorganic ions such as sodium (Na⁺), potassium (K⁺), and chloride (Cl⁻) are also present and help maintain osmotic and electrolyte balance in the duodenum.
2. Enzymatic Component
The enzymatic component is secreted by the acinar cells and includes a wide variety of digestive enzymes, some secreted in active forms and others in inactive precursor (zymogen) forms to prevent autodigestion of pancreatic tissues.
a. Proteolytic enzymes – Secreted as inactive zymogens:
- Trypsinogen: Activated to trypsin by the enzyme enterokinase (produced by the intestinal mucosa). Trypsin then activates other proteolytic zymogens.
- Chymotrypsinogen: Converted to chymotrypsin by trypsin.
- Procarboxypeptidase: Activated to carboxypeptidase by trypsin. These enzymes digest proteins into smaller peptides and eventually into amino acids.
b. Carbohydrate-digesting enzyme:
- Pancreatic amylase: Secreted in active form. It breaks down complex carbohydrates like starch into disaccharides (e.g., maltose) and smaller polysaccharides.
c. Fat-digesting enzymes:
- Pancreatic lipase: Breaks down triglycerides into monoglycerides and free fatty acids.
- Phospholipase A2: Digests phospholipids into lysophospholipids and fatty acids.
- Cholesterol esterase: Helps in the digestion of cholesterol esters.
d. Nucleic acid-digesting enzymes:
- Ribonuclease (RNase) and Deoxyribonuclease (DNase): Break down RNA and DNA into nucleotides.
This diverse enzyme mixture ensures that carbohydrates, fats, proteins, and nucleic acids are all digested in the small intestine.
🔷 Functions of Pancreatic Juice
The pancreatic juice is essential for complete digestion of food components and maintaining a favorable environment for enzyme action in the duodenum.
1. Digestive Function
Pancreatic enzymes are crucial for the chemical digestion of all major nutrients:
- Proteins are broken down by trypsin, chymotrypsin, and carboxypeptidase into small peptides and amino acids.
- Carbohydrates are digested by pancreatic amylase into maltose and oligosaccharides.
- Fats are emulsified (by bile) and then hydrolyzed by lipase into fatty acids and monoglycerides.
- Nucleic acids such as DNA and RNA are digested by DNase and RNase into nucleotides.
2. Neutralization of Acidic Chyme
Bicarbonate ions in the pancreatic juice play a critical role in neutralizing gastric hydrochloric acid as chyme enters the duodenum. This not only protects the delicate mucosal lining of the intestine but also creates an optimal alkaline pH for pancreatic and intestinal enzymes to function effectively.
3. Enzyme Activation
Although many enzymes are secreted in inactive forms, activation occurs in the small intestine. For instance, enterokinase (produced by duodenal mucosa) converts trypsinogen to trypsin, which then activates other zymogens. This mechanism ensures that enzymes do not harm pancreatic tissues before reaching the intestinal lumen.
🔷 Regulation of Pancreatic Secretion
The secretion of pancreatic juice is tightly controlled by neural and hormonal mechanisms that coordinate with the process of digestion. Regulation occurs in three main phases: cephalic, gastric, and intestinal.
1. Cephalic Phase
This phase is initiated by sight, smell, thought, or taste of food. It is mediated by parasympathetic impulses via the vagus nerve, which stimulate mild enzyme secretion by the pancreatic acinar cells. This prepares the pancreas in anticipation of incoming food.
2. Gastric Phase
This begins when food enters the stomach, causing gastric distension and protein breakdown. The vagus nerve and gastrin hormone (released by G-cells in the stomach) mildly stimulate the pancreas to secrete enzymes. However, this phase plays a relatively minor role in overall pancreatic secretion.
3. Intestinal Phase
This is the most significant phase of pancreatic secretion and begins when acidic chyme enters the duodenum. Two key hormones are responsible for regulating this phase:
- Secretin is released by the duodenal S-cells in response to low pH (acidic chyme). It stimulates the ductal cells of the pancreas to release a bicarbonate-rich, watery secretion to neutralize gastric acid.
- Cholecystokinin (CCK) is released by I-cells of the duodenum in response to the presence of fats and partially digested proteins. It stimulates acinar cells to release enzyme-rich pancreatic juice, aiding in digestion of fats and proteins.
4. Neural Control
Vagal (parasympathetic) stimulation continues to promote both bicarbonate and enzyme secretion throughout the digestive phases. However, during stress or fear, sympathetic stimulation can inhibit pancreatic activity.
🔷 Clinical Relevance
Proper pancreatic secretion is essential for digestion. Disorders affecting pancreatic juice can lead to serious clinical conditions:
- Acute or chronic pancreatitis occurs when digestive enzymes are prematurely activated inside the pancreas, leading to inflammation and tissue damage.
- Pancreatic insufficiency, often seen in cystic fibrosis or chronic pancreatitis, results in malabsorption of fats and proteins, leading to steatorrhea (fatty stools), weight loss, and nutritional deficiencies.
- Cystic fibrosis causes thick mucus to block pancreatic ducts, reducing enzyme delivery to the intestine.
- Zollinger-Ellison syndrome is caused by gastrin-secreting tumors, leading to excessive acid production, overwhelming pancreatic buffering capacity and altering enzyme function.
Pancreatic juice is one of the most critical secretions in the digestive process. It combines powerful enzymes capable of digesting every major class of food with an alkaline component that protects and prepares the small intestine for nutrient absorption. Its composition is intricately regulated by both neural and hormonal signals that synchronize with every phase of digestion. Any disturbance in pancreatic secretion can lead to serious digestive and absorptive disorders, highlighting the essential role of this fluid in human health.
🧠 Functions of the Liver (Detailed Explanation)
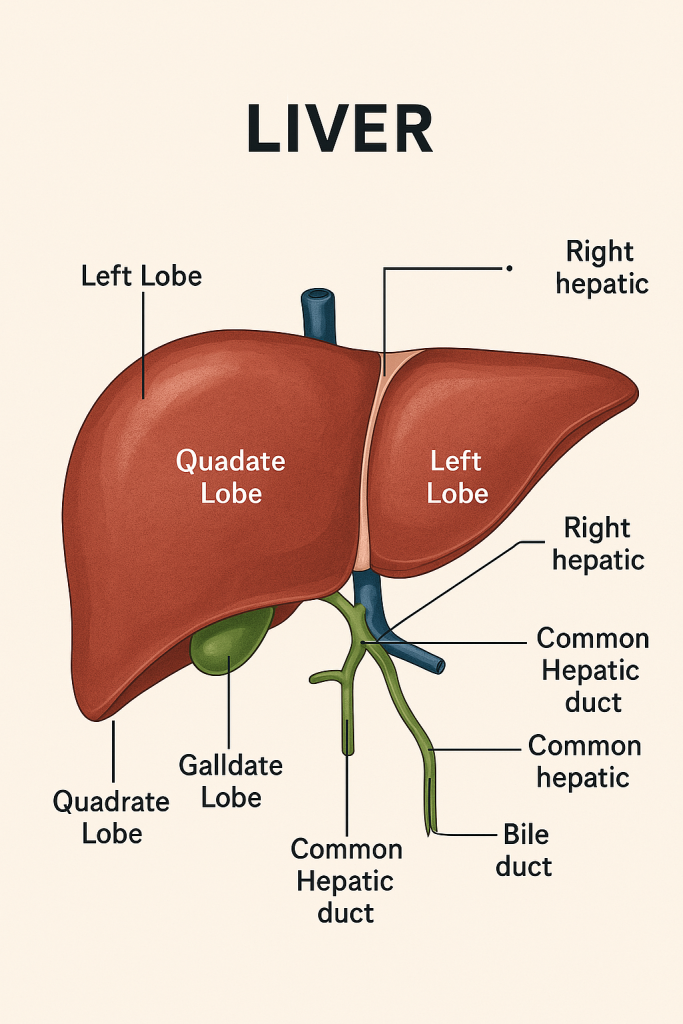
The liver is the largest internal organ and one of the most metabolically active organs in the body. Located in the right upper quadrant of the abdomen, it weighs about 1.2–1.5 kg in an average adult. It performs over 500 essential functions, broadly classified into metabolic, secretory, synthetic, detoxification, storage, and immune roles.
🔷 1. Metabolic Functions
The liver plays a central role in metabolism of carbohydrates, proteins, and fats.
🧁 A. Carbohydrate Metabolism
- Glycogenesis: Converts excess glucose to glycogen for storage.
- Glycogenolysis: Breaks down stored glycogen to glucose during fasting or low blood sugar.
- Gluconeogenesis: Synthesizes glucose from non-carbohydrate sources (amino acids, lactate, glycerol) during prolonged fasting.
- Maintains blood glucose homeostasis, especially between meals.
🍗 B. Protein Metabolism
- Deamination: Removes amino groups from amino acids, forming ammonia.
- Urea formation: Converts toxic ammonia into urea (less toxic), which is excreted by kidneys.
- Synthesis of plasma proteins: Produces albumin, fibrinogen, prothrombin, and other clotting factors.
- Transamination: Interconversion of amino acids for metabolic needs.
🧈 C. Fat Metabolism
- Lipogenesis: Converts excess carbohydrates and proteins into fatty acids and triglycerides.
- Fatty acid oxidation: Breaks down fatty acids to produce energy (especially during fasting).
- Synthesis of cholesterol and phospholipids.
- Formation of lipoproteins (VLDL, LDL, HDL) for fat transport in blood.
🔷 2. Detoxification Functions
The liver is the body’s detoxifier, converting harmful substances into less toxic forms.
- Detoxifies drugs, alcohol, and metabolic waste products.
- Converts ammonia to urea, which is excreted by the kidneys.
- Modifies and inactivates hormones (e.g., estrogen, cortisol, aldosterone).
- Processes bilirubin, a breakdown product of hemoglobin, into conjugated bilirubin for bile excretion.
🔷 3. Bile Production and Excretory Function
The liver secretes bile, essential for digestion and excretion.
- Produces about 600–1000 mL of bile per day.
- Bile contains bile salts, bile pigments (mainly bilirubin), cholesterol, phospholipids, electrolytes, and water.
- Bile salts emulsify fats, aiding in digestion and absorption in the small intestine.
- Bilirubin is excreted via bile into the intestine and gives feces its brown color.
- Bile also serves as a route of excretion for drugs, heavy metals, and hormones.
🔷 4. Synthetic Functions
The liver synthesizes many essential compounds needed for homeostasis.
- Albumin: Maintains oncotic pressure and transports hormones, drugs.
- Clotting factors: Fibrinogen, prothrombin, factors VII, IX, X — all essential for blood coagulation.
- Angiotensinogen: Involved in blood pressure regulation.
- Transport proteins: For lipids, vitamins, hormones.
🔷 5. Storage Functions
The liver stores several important nutrients and substances:
- Glycogen: Stored glucose for energy.
- Vitamins: A, D, E, K (fat-soluble) and B12.
- Minerals: Iron (as ferritin), copper, and zinc.
- Blood: Acts as a blood reservoir (can store 200–400 mL).
🔷 6. Hematological Functions
- Fetal hematopoiesis: In fetal life, the liver produces red blood cells.
- Removes old or damaged red blood cells (in cooperation with the spleen).
- Produces clotting factors and regulates platelet function indirectly.
🔷 7. Immunological Functions
The liver contains Kupffer cells, specialized macrophages that play a role in immune defense.
- Kupffer cells engulf pathogens, old red cells, and debris from the blood.
- The liver also acts as a filter for bacteria and antigens from the portal blood.
🔷 8. Hormonal Functions
- Metabolizes and clears steroid hormones (estrogen, testosterone, cortisol).
- Participates in the activation of Vitamin D (along with the kidney).
- Produces angiotensinogen, which helps regulate blood pressure via the renin-angiotensin system.
- Modulates levels of insulin and glucagon through uptake and degradation.
🔷 9. Conversion of Ammonia to Urea
One of the critical detox functions of the liver is the urea cycle, where:
- Toxic ammonia (a byproduct of protein metabolism) is converted into urea.
- Urea is water-soluble and is excreted by the kidneys.
- Failure of this process in liver disease can lead to hyperammonemia and hepatic encephalopathy.
🔷 10. Miscellaneous Functions
- Participates in heat production due to its high metabolic rate.
- Plays a role in drug metabolism through oxidation, reduction, hydrolysis, conjugation.
- Maintains lipid and cholesterol balance in blood.
📌 Clinical Importance of Liver Functions
Any disturbance in liver function can result in:
- Jaundice: Accumulation of bilirubin.
- Bleeding disorders: Due to decreased clotting factor synthesis.
- Hypoalbuminemia: Leading to edema and ascites.
- Hepatic encephalopathy: Due to ammonia buildup.
- Malabsorption of fats: Due to lack of bile salts.
- Drug toxicity: Impaired detoxification of drugs and toxins.
The liver is an essential metabolic powerhouse, responsible for:
- Carbohydrate, protein, and fat metabolism
- Detoxification of harmful substances
- Synthesis of vital proteins and clotting factors
- Storage of nutrients and minerals
- Immune defense through Kupffer cells
- Regulation of blood composition, pH, and hormone levels
Its proper functioning is crucial for overall health, and liver diseases can have wide-reaching systemic effects.
🟡 Functions of the Gallbladder – Detailed Academic Explanation
The gallbladder is a small, pear-shaped organ located beneath the liver in the right upper quadrant of the abdomen. Though small in size, it plays a critical role in the digestive system—particularly in the storage and regulation of bile flow. While the liver continuously produces bile, the gallbladder acts as a reservoir and control center for its release into the small intestine when needed.
🔷 1. Storage of Bile
The primary function of the gallbladder is to store bile produced by the liver. Bile is a yellowish-green alkaline fluid composed of:
- Bile salts
- Bilirubin (a bile pigment)
- Cholesterol
- Phospholipids (mainly lecithin)
- Electrolytes and water
The liver secretes bile continuously, but it is not always immediately needed for digestion. Instead of flowing directly into the duodenum, excess bile is diverted into the gallbladder via the cystic duct and stored there between meals.
The gallbladder can hold approximately 30–50 mL of bile, and during storage, the epithelial lining absorbs water and electrolytes, concentrating the bile by up to 10-fold, making it more potent for fat digestion.
🔷 2. Concentration of Bile
One of the key functions of the gallbladder is to concentrate the bile during its storage phase. This is achieved by the active absorption of sodium and chloride ions from bile by the gallbladder mucosa, followed by passive water reabsorption. This process significantly reduces the volume while increasing the concentration of:
- Bile salts (needed for fat emulsification)
- Cholesterol
- Lecithin
- Bilirubin
This concentrated bile is more effective in facilitating the digestion and absorption of lipids.
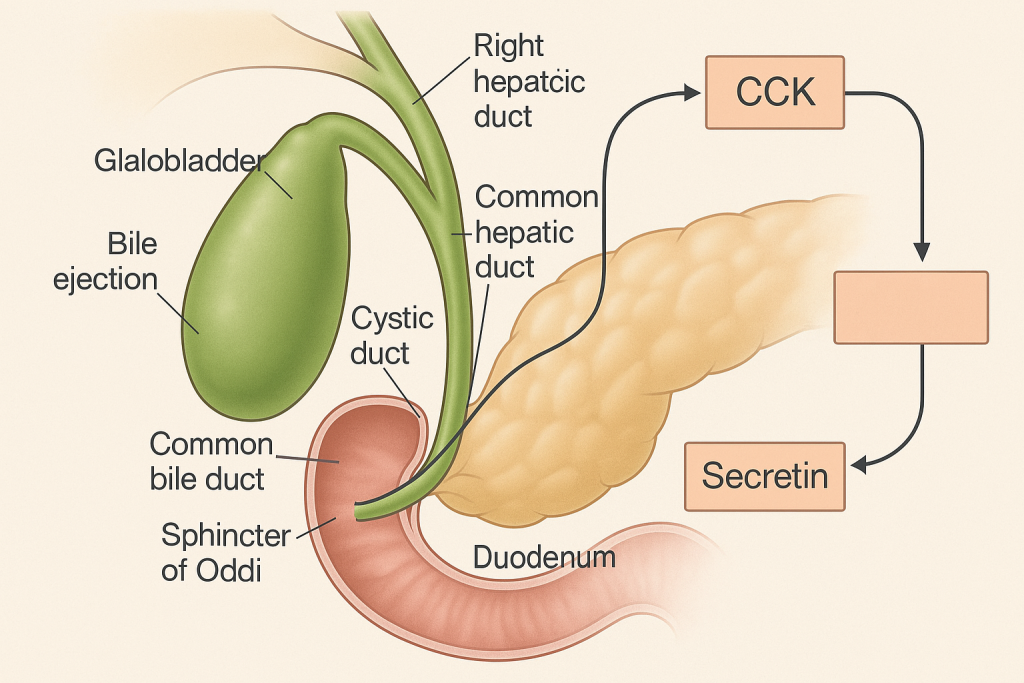
🔷 3. Release of Bile (Ejection into Duodenum)
When food, especially fatty food, enters the duodenum, it triggers a neurohormonal reflex leading to gallbladder contraction and bile ejection.
👉 Mechanism of Bile Release:
- The presence of fat and amino acids in the duodenum stimulates the I cells of the intestinal mucosa to secrete the hormone cholecystokinin (CCK).
- CCK causes the smooth muscles of the gallbladder wall to contract.
- Simultaneously, CCK relaxes the sphincter of Oddi (a muscular valve controlling bile flow into the duodenum).
- This coordinated action allows bile to flow from the gallbladder into the cystic duct, then the common bile duct, and finally into the duodenum.
This process ensures that bile is released exactly when it is needed, i.e., during digestion of fatty meals.
🔷 4. Role of Bile in Digestion (Indirect Function of Gallbladder)
Although the gallbladder does not produce bile or digest nutrients, it facilitates fat digestion through regulated bile delivery.
Bile stored and released by the gallbladder performs the following:
- Emulsification of fats: Bile salts break down large fat globules into smaller micelles, increasing the surface area for enzyme action.
- Solubilization of lipids and fat-soluble vitamins (A, D, E, K): Helps in their absorption through the intestinal mucosa.
- Neutralization of gastric acid: Bile contributes to alkaline intestinal pH, optimal for enzyme activity.
- Excretion: Bile carries bilirubin, excess cholesterol, drugs, and toxins from the liver to be eliminated in feces.
Hence, by controlling bile availability, the gallbladder plays a key role in lipid digestion, absorption, and excretion of waste products.
🔷 5. Regulation of Gallbladder Function
Gallbladder activity is controlled by both hormonal and nervous mechanisms.
A. Hormonal Regulation
- Cholecystokinin (CCK): The most important hormone that stimulates gallbladder contraction and bile ejection.
- Secretin: Stimulates bicarbonate-rich bile secretion from the liver but indirectly aids bile flow.
B. Neural Regulation
- Vagal stimulation (parasympathetic): Promotes mild contraction of the gallbladder during the cephalic and gastric phases of digestion (e.g., at the smell or taste of food).
- Enteric nervous system also plays a role in local reflex control.
🔷 6. Role in Waste Excretion
Bile stored in the gallbladder acts as a route of excretion for substances not handled by the kidneys. These include:
- Bilirubin: The end product of hemoglobin breakdown.
- Excess cholesterol
- Xenobiotics: Certain drugs and toxins. These are eliminated from the body in feces via bile.
🔷 Clinical Relevance of Gallbladder Function
Gallbladder dysfunction can lead to several clinical conditions:
- Cholelithiasis (Gallstones):
- Formed from cholesterol, bile salts, or bilirubin.
- Can block bile flow → biliary colic, cholecystitis.
- Cholecystitis:
- Inflammation of the gallbladder, usually due to gallstones.
- Leads to pain, fever, vomiting, and requires medical or surgical intervention.
- Biliary Dyskinesia:
- Functional motility disorder where the gallbladder does not empty properly.
- Post-Cholecystectomy (Gallbladder Removal):
- Bile flows continuously into the intestine (instead of being stored and released in pulses).
- Patients may experience fat digestion issues initially.
Gallbladder Functions
- Stores bile produced by the liver.
- Concentrates bile by absorbing water and electrolytes.
- Releases bile into the duodenum in response to CCK.
- Coordinates with liver and intestine to aid in fat digestion.
- Serves as an excretory route for waste products like bilirubin and cholesterol.
🌟 The Pancreas – A Dual-Function Life Regulator
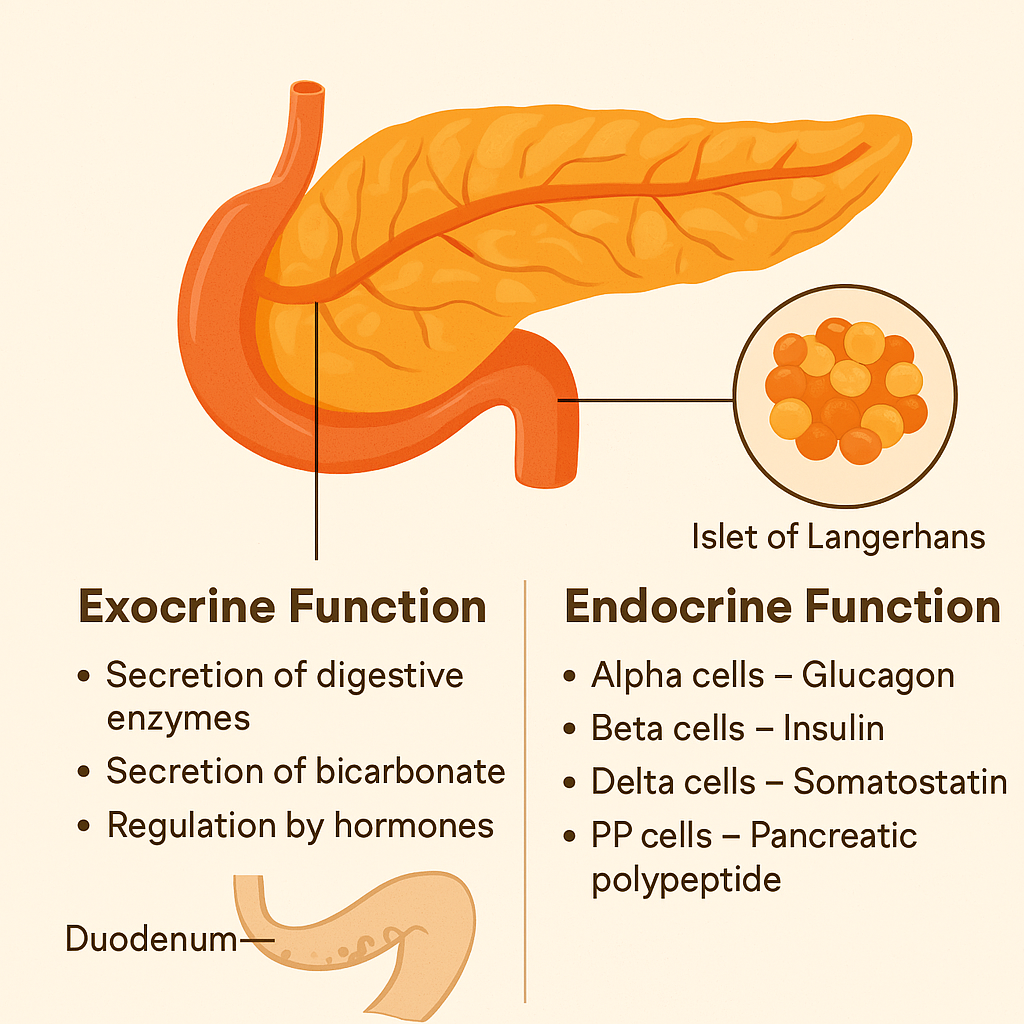
The pancreas is a soft, elongated organ located deep in the abdomen, behind the stomach. Though modest in size, it plays two mighty roles that are essential to human survival: one in digestion and the other in metabolic regulation. These two distinct roles are carried out by its exocrine and endocrine parts.
Let’s explore these two faces of the pancreas in detail.
🍽️ I. Exocrine Function: The Digestive Helper
The exocrine part makes up nearly 98% of the pancreatic tissue and is made up of acinar cells and ductal cells. These cells produce and secrete digestive enzymes and alkaline fluids that are essential for breaking down the food we eat.
🔍 Key Functions:
1. Secretion of Digestive Enzymes
The pancreas produces powerful enzymes that are released into the duodenum (first part of the small intestine) via the pancreatic duct. These enzymes include:
- Amylase – breaks down starch into simple sugars.
- Lipase – breaks down fats into fatty acids and glycerol.
- Proteases (like trypsin and chymotrypsin) – break down proteins into amino acids.
🧠 These enzymes are secreted in inactive form to prevent self-digestion of the pancreas and become active only in the intestine.
2. Secretion of Bicarbonate (Alkaline Juice)
- Ductal cells release sodium bicarbonate (NaHCO₃) which neutralizes stomach acid in the chyme.
- This protects the intestinal lining and creates an alkaline environment ideal for enzyme function.
3. Regulation by Hormones
- Secretin (from the small intestine) stimulates bicarbonate release.
- Cholecystokinin (CCK) stimulates enzyme secretion when fats or proteins are detected in the small intestine.
➡️ Together, these processes ensure proper digestion and absorption of nutrients.
🩸 II. Endocrine Function: The Sugar Balancer
The endocrine part of the pancreas consists of tiny clusters of hormone-producing cells called the Islets of Langerhans, which form about 2% of the gland. These cells secrete hormones directly into the bloodstream to regulate blood glucose levels and metabolism.
🧬 Types of Islet Cells and Their Functions:
| Cell Type | Hormone | Function |
|---|---|---|
| Alpha (α) cells | Glucagon | Raises blood sugar by promoting glycogen breakdown and glucose release from the liver. |
| Beta (β) cells | Insulin | Lowers blood sugar by promoting glucose uptake into cells and storage as glycogen. |
| Delta (δ) cells | Somatostatin | Inhibits insulin and glucagon release; helps regulate the timing of digestion and hormone release. |
| PP (F) cells | Pancreatic polypeptide | Regulates both exocrine secretion and appetite control. |
➡️ The balance between insulin and glucagon ensures the body has a steady energy supply without causing blood sugar extremes.
🔁 Integrated Function: Harmony Between Digestion and Metabolism
The pancreas acts like a master coordinator, synchronizing digestion with metabolic needs:
- After a meal: it increases enzyme and insulin secretion to digest food and store energy.
- During fasting: it slows down enzyme production and releases glucagon to mobilize stored glucose.
⚠️ Clinical Insight: Why Pancreatic Health Matters
When the pancreas malfunctions, it can lead to serious health issues:
- Diabetes Mellitus – due to insulin imbalance.
- Pancreatitis – inflammation caused by premature enzyme activation.
- Exocrine Pancreatic Insufficiency (EPI) – poor digestion due to lack of enzymes.
- Pancreatic Cancer – often silent until advanced, affecting both digestive and endocrine roles.
| Function | Type | Secretions | Role |
|---|---|---|---|
| Digestion | Exocrine | Enzymes (amylase, lipase, protease) + Bicarbonate | Breaks down food, neutralizes acid |
| Metabolism | Endocrine | Insulin, Glucagon, Somatostatin, Pancreatic Polypeptide | Regulates blood sugar and energy use |
🌿 Bile: The Digestive Gold from the Liver
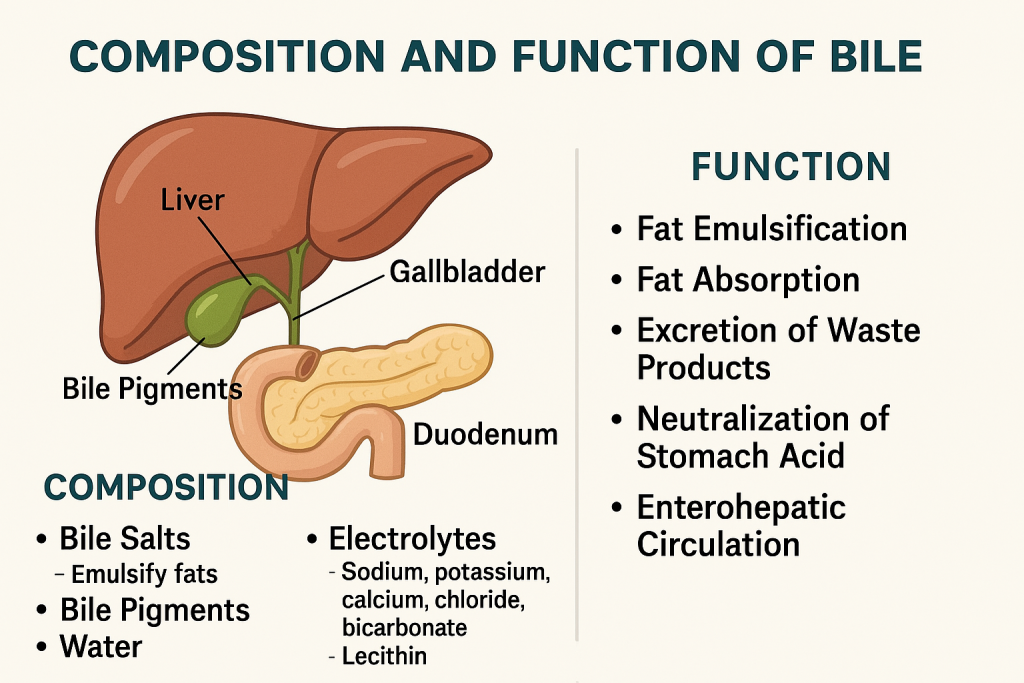
Bile is a yellowish-green alkaline fluid produced by the liver and stored in the gallbladder. It plays a crucial role in digestion and absorption of fats, and in the elimination of waste products from the body. Although not an enzyme, bile acts as a biological detergent that emulsifies fats, making them easier for digestive enzymes to break down.
🧪 Composition of Bile
Bile is a complex aqueous secretion, made up of both organic and inorganic substances. Its main components include:
🌟 1. Bile Salts (Primary Active Components)
- Derived from cholesterol (cholic acid and chenodeoxycholic acid).
- Function: Emulsify large fat globules into tiny droplets (micelles), increasing the surface area for lipase action.
🌈 2. Bile Pigments
- Mainly bilirubin (a breakdown product of hemoglobin).
- Function: Excretory role—gives bile its yellow-green color and is eliminated in feces.
💧 3. Water
- Makes up 90–95% of bile.
- Function: Solvent that allows bile to flow easily and dissolve other components.
🧂 4. Electrolytes
- Include sodium, potassium, calcium, chloride, and bicarbonate.
- Function: Maintain the bile’s alkalinity and support fat digestion.
🍬 5. Cholesterol and Phospholipids
- Mainly lecithin (a phospholipid).
- Function: Aid in fat transport and emulsification; excess cholesterol is excreted through bile.
🛠️ Functions of Bile: Role in Digestion and Beyond
1. 🧈 Fat Emulsification
- Bile salts break down fat globules into tiny droplets.
- This emulsification increases the surface area for enzymes (especially lipase) to act.
2. 🔄 Fat Absorption
- Bile helps form micelles—tiny complexes that transport fatty acids and fat-soluble vitamins (A, D, E, K) to the intestinal lining for absorption.
3. 🚮 Excretion of Waste Products
- Bile carries waste products like:
- Bilirubin (from old red blood cells)
- Excess cholesterol
- Toxins and drugs
- These are eliminated through feces, giving stool its characteristic brown color.
4. 🧪 Neutralization of Stomach Acid
- Bile contains bicarbonate ions that help neutralize acidic chyme entering the duodenum from the stomach, creating a favorable pH for intestinal enzymes.
5. 🔄 Enterohepatic Circulation
- Most bile salts are reabsorbed in the ileum and returned to the liver via the portal vein for reuse—this recycling saves energy and resources.
📦 Composition & Function of Bile
| Component | Origin/Type | Function |
|---|---|---|
| Bile Salts | Organic (cholesterol) | Emulsify fats, form micelles, aid fat absorption |
| Bile Pigments | Bilirubin | Excrete hemoglobin waste, color bile/feces |
| Water | Inorganic solvent | Dissolves other components, facilitates bile flow |
| Electrolytes | Na⁺, K⁺, Cl⁻, HCO₃⁻ | Maintain alkaline pH and ionic balance in bile |
| Cholesterol | Organic lipid | Excreted via bile, also aids micelle formation |
| Lecithin (Phospholipid) | Organic | Helps with emulsification and micelle stability |
⚠️ Clinical Insight
- Gallstones may form when bile becomes too concentrated with cholesterol or bile pigments.
- Obstructive jaundice results when bile flow is blocked, causing bilirubin buildup.
- Fatty stool (steatorrhea) can occur in bile deficiency, as fats are poorly absorbed.
📘 Secretion and Function of the Small Intestine:
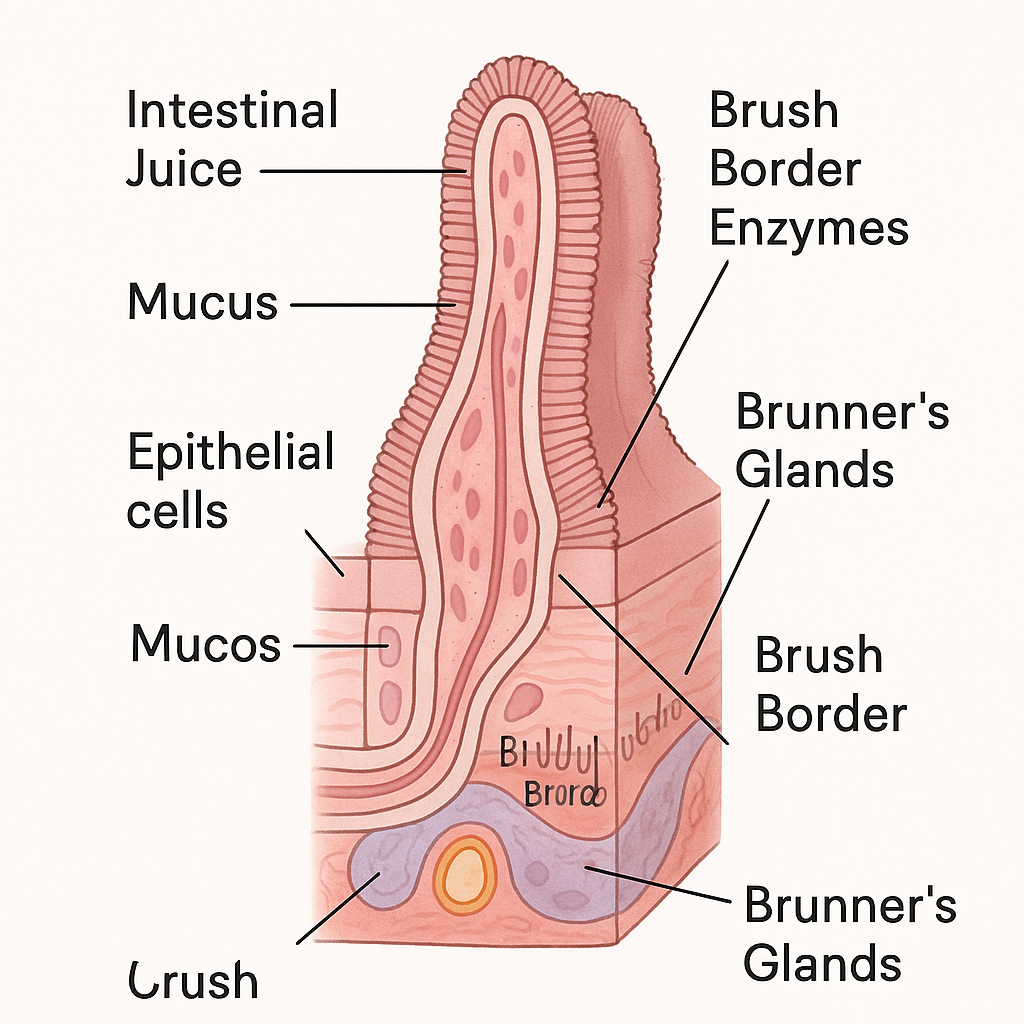
The small intestine is the primary site for digestion and absorption of nutrients in the human body. It is about 6 meters long and divided into three parts: duodenum, jejunum, and ileum. Each part contributes to various functions through mechanical actions, secretions, enzymatic activity, and absorptive roles.
🧪 I. Secretions of the Small Intestine
The intestinal glands (crypts of Lieberkühn) and duodenal (Brunner’s) glands in the mucosa of the small intestine secrete a variety of substances essential for digestion and protection.
🌟 Major Secretions:
1. Intestinal Juice (Succus Entericus)
- A clear, slightly alkaline fluid (pH ~7.6).
- Secreted by the crypts of Lieberkühn.
- Daily secretion: ~1.5 to 2 liters.
🔬 Contents:
| Component | Function |
|---|---|
| Water & Electrolytes | Solvent medium for digestion and absorption |
| Mucus (from goblet cells) | Protects mucosa; lubricates chyme |
| Enzymes | Final breakdown of nutrients |
2. Digestive Enzymes in the Brush Border
Located on the microvilli of epithelial cells:
- Disaccharidases (e.g., maltase, sucrase, lactase): break down disaccharides into monosaccharides.
- Peptidases: break down peptides into amino acids.
- Nucleotidases & Nucleosidases: digest nucleic acids.
- Enterokinase (enteropeptidase): activates trypsinogen → trypsin (essential for protein digestion).
3. Brunner’s Gland Secretions (in Duodenum)
- Produce alkaline mucus rich in bicarbonate ions.
- Neutralizes acidic chyme from the stomach to protect the mucosa and provide an optimal pH for enzymes.
4. Hormonal Secretions
The mucosa of the small intestine also secretes important hormones:
| Hormone | Source | Function |
|---|---|---|
| Secretin | Duodenum | Stimulates bicarbonate secretion from pancreas; inhibits gastric acid |
| Cholecystokinin (CCK) | Duodenum | Stimulates pancreatic enzyme secretion and gallbladder contraction |
| Enterogastrone | Duodenum | Inhibits gastric motility and secretions |
| Gastric Inhibitory Peptide (GIP) | Duodenum & Jejunum | Slows gastric emptying; stimulates insulin release |
🧠 II. Functions of the Small Intestine
The small intestine is an efficient organ designed for:
- Digestion
- Absorption
- Hormonal regulation
- Immunological defense
🌟 Major Functions:
1. Digestion
- Enzymes from the pancreas and small intestine act on proteins, carbohydrates, and fats.
- Final digestion occurs on the brush border of the intestinal epithelium.
2. Absorption
The small intestine is lined with villi and microvilli, increasing surface area for absorption.
- Duodenum and Jejunum absorb:
- Glucose, amino acids, fatty acids, vitamins, minerals.
- Ileum absorbs:
- Vitamin B12, bile salts, and remaining nutrients.
3. Protection and Immune Defense
- Mucus protects from mechanical and chemical injury.
- Peyer’s patches (lymphoid tissue in the ileum) form part of the gut-associated lymphoid tissue (GALT), defending against pathogens.
4. Motility and Mixing
- Segmental contractions mix chyme with enzymes.
- Peristalsis pushes chyme forward for further digestion and absorption.
5. Hormonal Regulation
- Secretin, CCK, and other gut hormones regulate:
- Pancreatic secretions
- Gallbladder contraction
- Gastric emptying
- Appetite and insulin release
📝 Secretion & Function of Small Intestine
| Secretion | Source | Function |
|---|---|---|
| Intestinal Juice | Crypts of Lieberkühn | Lubrication, enzyme action |
| Mucus | Goblet cells, Brunner’s glands | Protection, alkalinity |
| Disaccharidases | Brush border enzymes | Breakdown of sugars |
| Peptidases | Brush border enzymes | Breakdown of peptides |
| Enterokinase | Duodenum (epithelial cells) | Activation of trypsinogen |
| Secretin | Duodenal mucosa | Stimulates bicarbonate, inhibits acid |
| CCK | Duodenum | Pancreatic enzyme release, bile secretion |
| GIP | Small intestine | Inhibits gastric secretion, stimulates insulin |
📚 Clinical Correlation
- Lactose intolerance: Deficiency of lactase leads to poor digestion of lactose, causing bloating and diarrhea.
- Celiac disease: Autoimmune reaction damages villi, reducing nutrient absorption.
- Peptic ulcers: If Brunner’s glands don’t neutralize acid, duodenal ulcers may form.
- Malabsorption syndromes: Damage to the intestinal lining leads to failure in nutrient uptake.
📘 Large Intestine: Secretions and Functions
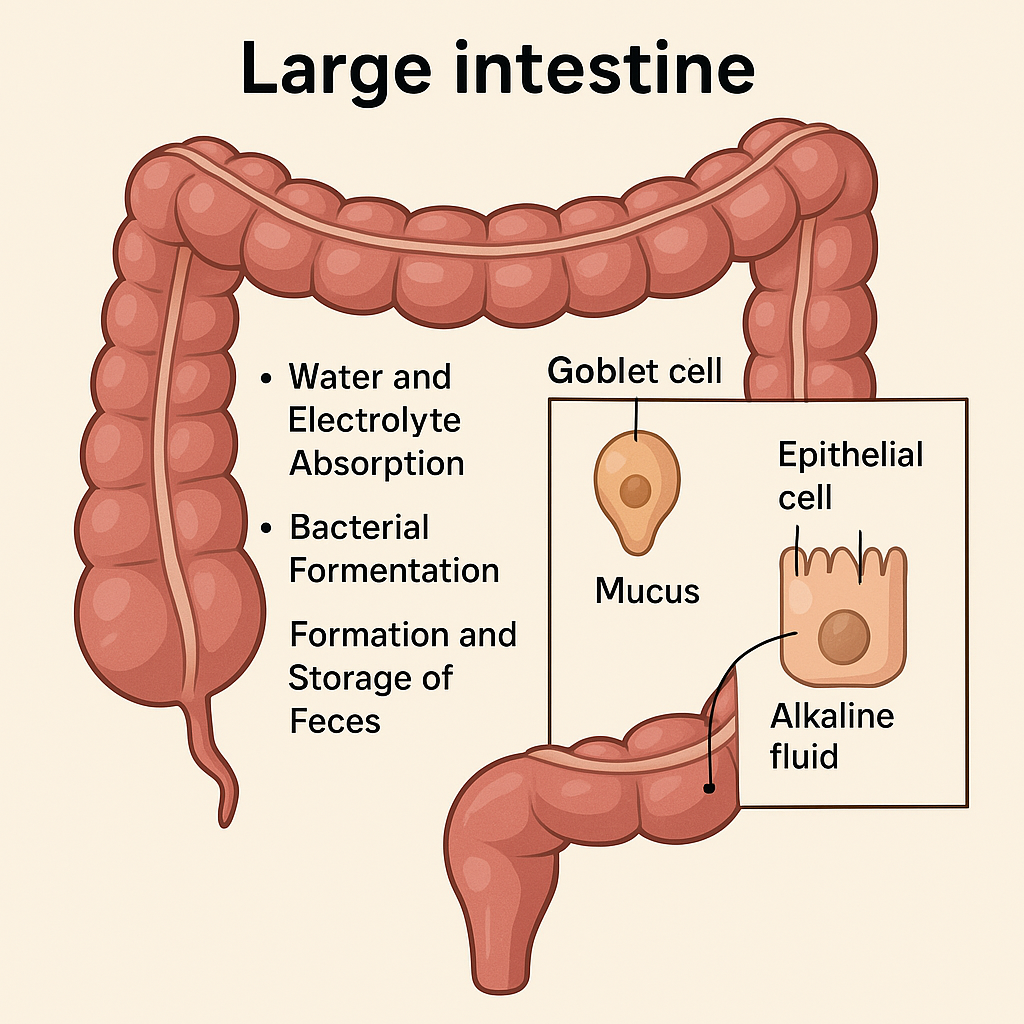
The large intestine, or colon, is the final segment of the digestive tract, approximately 1.5 meters long, extending from the ileocecal valve to the anus. Although not primarily involved in digestion, it plays an essential role in water and electrolyte absorption, formation of feces, and gut immunity.
🧪 I. Secretions of the Large Intestine
Unlike the small intestine, the large intestine does not secrete digestive enzymes. Its secretions are mostly protective and lubricative, facilitating the passage of fecal material and maintaining mucosal integrity.
🌟 Major Secretions:
1. Mucus
- Secreted by goblet cells in the mucosal lining.
- Function:
- Lubricates feces to ease movement.
- Protects the mucosa from mechanical and chemical irritation.
- Binds fecal particles for easier expulsion.
2. Alkaline Fluid
- Contains bicarbonate ions (HCO₃⁻).
- Secreted by epithelial cells.
- Function:
- Neutralizes acids produced by bacterial fermentation (e.g., short-chain fatty acids, lactic acid).
- Maintains mucosal pH balance to prevent inflammation.
3. Potassium and Electrolyte Secretion
- Some potassium (K⁺) and chloride (Cl⁻) ions are actively secreted into the lumen.
- Especially relevant during diarrhea when these losses can lead to hypokalemia.
🧠 II. Functions of the Large Intestine
Though the large intestine lacks digestive enzymes, its mechanical, absorptive, excretory, and microbial roles are crucial to maintaining health and homeostasis.
🌟 Major Functions:
1. 💧 Water and Electrolyte Absorption
- The colon absorbs:
- Water (up to 1.5 liters/day)
- Electrolytes such as sodium and chloride
- This process converts liquid chyme into solid feces.
2. 🦠 Bacterial Fermentation (Microbial Function)
- The colon houses over 100 trillion bacteria (gut microbiota).
- These bacteria:
- Ferment undigested carbohydrates to produce short-chain fatty acids (SCFAs) like acetate, butyrate, and propionate.
- Synthesize vitamins, especially vitamin K and biotin (B7).
- Contribute to immune system regulation and mucosal protection.
3. 🧻 Formation and Storage of Feces
- Indigestible residues are compacted into semisolid feces.
- The rectum stores feces until defecation is triggered via reflex pathways.
4. ⚖️ pH Regulation
- The alkaline secretion of bicarbonate helps counteract acidic by-products of fermentation, keeping the environment slightly alkaline to neutral (pH ~6.8–7.3).
5. 🧬 Immunity and Barrier Protection
- Gut-associated lymphoid tissue (GALT) in the large intestine provides immune surveillance.
- Mucus and tight junctions in the epithelium serve as a physical barrier to pathogens.
📦 Secretions and Functions of the Large Intestine
| Secretion | Source | Function |
|---|---|---|
| Mucus | Goblet cells | Lubricates feces, protects mucosa |
| Bicarbonate ions | Epithelial cells | Neutralizes acidic waste, maintains pH |
| Electrolytes (K⁺, Cl⁻) | Epithelial cells | Electrolyte balance; potassium secretion |
| Function | Description |
|---|---|
| Water & Electrolyte Absorption | Conserves fluid, forms solid feces |
| Bacterial Fermentation | Digests fiber, synthesizes vitamins, produces SCFAs |
| Vitamin Synthesis | Especially Vitamin K and Biotin by gut flora |
| Immunological Role | GALT and epithelial barrier protect against infection |
| Fecal Storage & Defecation | Stores waste until voluntary elimination |
🧬 Clinical Relevance
- Constipation: Reduced motility leads to excessive water reabsorption.
- Diarrhea: Increased motility or reduced absorption results in water and electrolyte loss.
- Ulcerative Colitis & Crohn’s Disease: Inflammatory bowel diseases affecting mucosal function.
- Colorectal Cancer: One of the leading causes of cancer-related deaths; early screening is vital.
🧠 Movements of the Alimentary Tract:
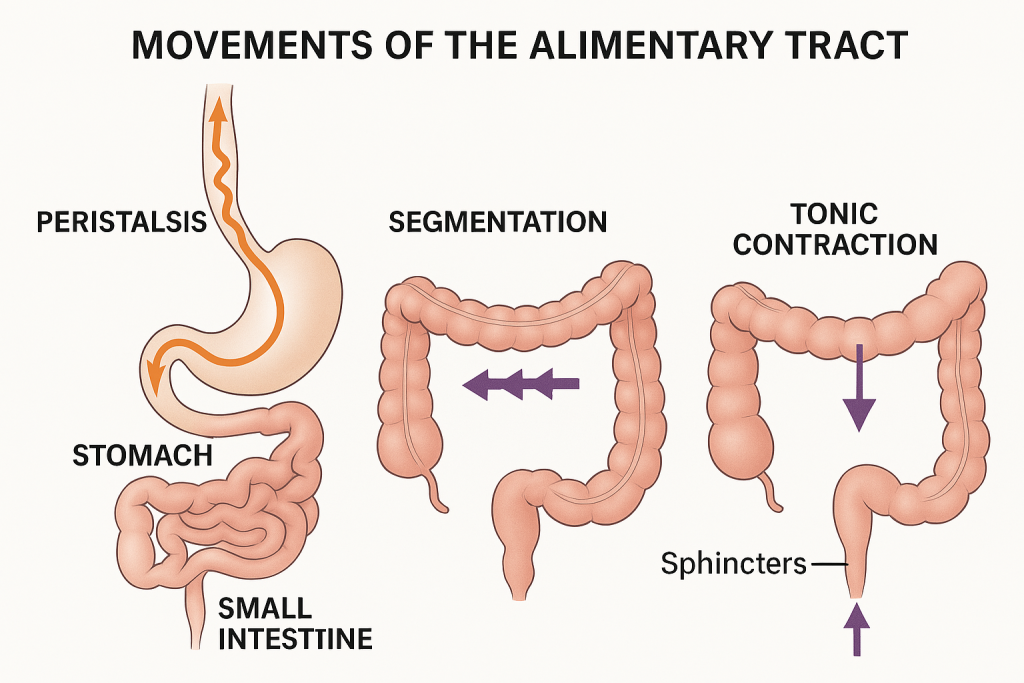
The alimentary tract (or gastrointestinal tract) is a long, muscular tube that extends from the mouth to the anus. It performs mechanical functions that facilitate ingestion, digestion, absorption, and elimination. These functions are driven by coordinated muscular contractions—collectively known as gastrointestinal motility.
🧬 Types of Muscles Involved
The alimentary tract consists of smooth muscles, organized in two layers:
- Inner circular layer
- Outer longitudinal layer
In certain areas like the pharynx and upper esophagus, skeletal muscle is also involved (for voluntary swallowing).
🚶♂️ Types of Movements in the Alimentary Tract
1. Propulsive Movements (Peristalsis)
- Definition: Rhythmic, wave-like contractions that push contents forward through the GI tract.
- Occurs in: Esophagus, stomach, small and large intestines.
- Mechanism: Contraction of circular muscle behind the bolus and relaxation in front of it.
🧠 Peristalsis is involuntary and controlled by the enteric nervous system and influenced by hormones.
2. Mixing Movements (Segmentation)
- Definition: Localized contractions that churn and mix intestinal contents with digestive juices.
- Occurs in: Small and large intestines.
- Function: Enhances digestion and absorption by increasing contact with mucosa.
3. Tonic Contractions
- Definition: Sustained contraction of sphincters or specific areas.
- Occurs in: Lower esophageal sphincter, pyloric sphincter, ileocecal valve, anal sphincter.
- Function: Acts as valves, controlling the flow of contents and preventing backflow.
4. Receptive Relaxation
- Definition: Relaxation of the stomach and esophagus in response to swallowing.
- Function: Allows food to enter without resistance and prepares the tract for incoming contents.
5. Mass Movements
- Definition: Strong peristaltic waves occurring a few times a day.
- Occurs in: Colon (especially transverse and descending parts).
- Function: Moves fecal matter toward the rectum for defecation.
6. Swallowing (Deglutition)
- Phases:
- Oral Phase – voluntary
- Pharyngeal Phase – involuntary
- Esophageal Phase – involuntary peristalsis
- Function: Transfers food from mouth to stomach safely and efficiently.
7. Defecation Reflex
- Triggered by stretch receptors in the rectum.
- Involves voluntary relaxation of external anal sphincter and involuntary contraction of the rectal wall.
- Requires coordinated action of abdominal muscles, diaphragm, and pelvic floor.
🧪 GI Tract Movements
| Type of Movement | Location | Function |
|---|---|---|
| Peristalsis | Esophagus → Anus | Propels food forward |
| Segmentation | Small & large intestine | Mixes chyme with enzymes, enhances absorption |
| Tonic Contractions | Sphincters (LES, pyloric, etc.) | Controls passage between GI segments |
| Receptive Relaxation | Stomach, esophagus | Prepares organs to receive contents |
| Mass Movements | Large intestine | Drives feces toward rectum |
| Swallowing | Mouth → Esophagus | Transfers food to stomach |
| Defecation | Rectum and anus | Eliminates waste |
⚠️ Clinical Relevance
| Disorder | Related Movement Problem |
|---|---|
| Achalasia | Failure of lower esophageal sphincter to relax |
| GERD | Weak lower esophageal sphincter; causes reflux |
| Ileus | Absence of intestinal movement; often post-surgery |
| Constipation | Decreased motility or mass movement |
| Diarrhea | Increased intestinal motility, reducing absorption time |
🧠 Digestion in the Mouth –
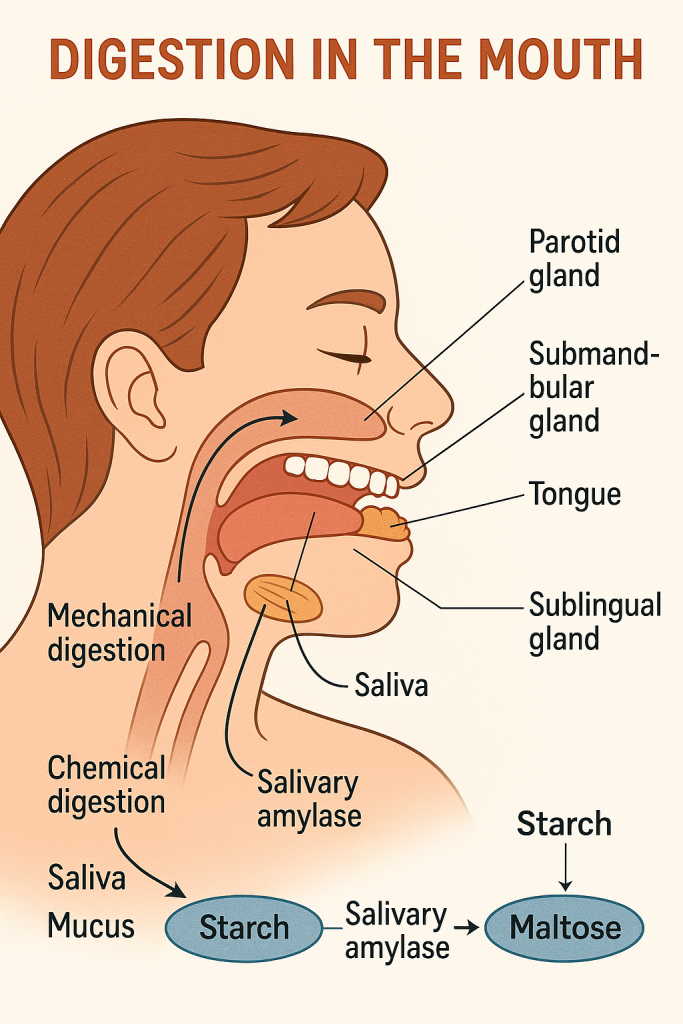
The mouth (oral cavity) is the first site of digestion in the alimentary canal. It plays a vital role in both the mechanical and chemical breakdown of food. The aim is to prepare the food into a semi-liquid mass called bolus, making it easier to swallow and digest further in the stomach and intestines.
🦷 I. Mechanical Digestion in the Mouth (Mastication)
🔹 Mastication (Chewing)
- Performed by teeth, assisted by tongue, cheeks, and jaw muscles.
- Breaks large food particles into smaller ones, increasing surface area for enzyme action.
- Forms bolus—a soft, moist mass ready for swallowing.
🔹 Role of the Tongue
- Moves food between teeth for thorough chewing.
- Helps in taste sensation and bolus formation.
- Pushes the bolus toward the pharynx during swallowing.
💧 II. Chemical Digestion in the Mouth (Salivary Enzymes)
🔹 Saliva – The Digestive Fluid
- Secreted by three pairs of salivary glands:
- Parotid glands (serous)
- Submandibular glands (seromucous)
- Sublingual glands (mucous)
- Daily secretion: ~1 to 1.5 liters
🌟 Composition of Saliva:
| Component | Function |
|---|---|
| Water (99%) | Moistens food, helps dissolve substances |
| Mucus (mucin) | Lubricates and binds food particles |
| Salivary amylase (ptyalin) | Begins starch digestion (polysaccharides → maltose) |
| Lingual lipase | Minor role in fat digestion (more active in stomach) |
| Lysozyme | Antibacterial action |
| Bicarbonate ions | Maintain pH (~6.7–7.4), neutralize acids |
🔬 Enzymatic Action in the Mouth
🧪 Salivary Amylase (Ptyalin)
- Substrate: Starch
- Product: Maltose (a disaccharide)
- Optimal pH: 6.7 to 7.0
- Action Site: Mouth (inactivated in acidic stomach)
🧪 Lingual Lipase
- Secreted by lingual glands on the tongue.
- Starts the digestion of triglycerides, although it becomes more effective in the acidic environment of the stomach.
🛠️ III. Functions of the Mouth in Digestion
| Function | Description |
|---|---|
| Ingestion | Food enters the body via the mouth. |
| Mechanical digestion | Chewing breaks down food into smaller particles. |
| Chemical digestion | Salivary enzymes begin digestion of starch and lipids. |
| Taste perception | Taste buds detect sweet, sour, salty, bitter, umami. |
| Speech assistance | Teeth, lips, and tongue help articulate sounds. |
| Swallowing preparation | Food is formed into a bolus and passed to the pharynx. |
🧬 Digestion in the Mouth
| Aspect | Details |
|---|---|
| Mechanical | Mastication by teeth and tongue movement |
| Chemical | Saliva contains amylase (starch digestion) and mucin |
| Salivary glands | Parotid, Submandibular, Sublingual |
| Enzymes | Salivary amylase, lingual lipase |
| End product | Partially digested starch (maltose), soft bolus |
⚠️ Clinical Insight
| Condition | Description |
|---|---|
| Xerostomia (dry mouth) | Reduced saliva secretion affects digestion and oral hygiene. |
| Mumps | Viral infection of the parotid gland causing swelling and pain. |
| Dental caries | Enzymes and sugars in food promote acid production and tooth decay. |
🧠 Digestion in the Stomach –
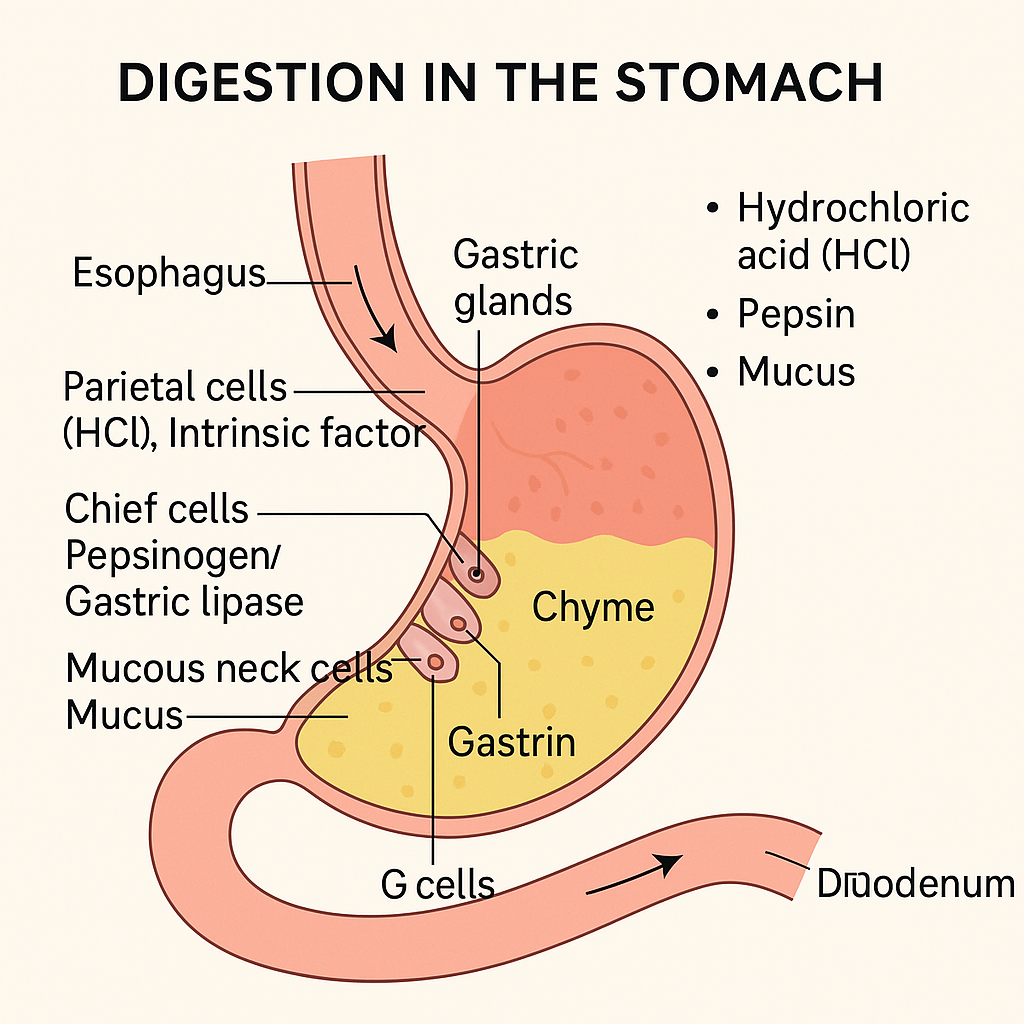
The stomach is a muscular, J-shaped organ located in the upper abdomen between the esophagus and small intestine. It serves as a temporary food reservoir and a powerful chemical processor, playing a key role in both mechanical and chemical digestion.
🦾 I. Mechanical Digestion in the Stomach
🔹 Churning and Mixing
- The stomach wall undergoes rhythmic muscular contractions known as peristalsis.
- These contractions mix food with gastric juices, producing a semi-liquid mass called chyme.
- The pyloric sphincter controls the slow release of chyme into the duodenum.
🧪 II. Chemical Digestion in the Stomach
The inner lining of the stomach (gastric mucosa) contains gastric glands that secrete gastric juice, a combination of enzymes, acid, mucus, and hormones.
🌟 Composition of Gastric Juice
Produced by the gastric glands in the fundus and body of the stomach:
| Cell Type | Secretion | Function |
|---|---|---|
| Parietal (oxyntic) cells | Hydrochloric acid (HCl) | Activates pepsinogen to pepsin; provides acidic pH (1.5–3.5); kills microbes |
| Intrinsic factor | Essential for vitamin B₁₂ absorption in the ileum | |
| Chief (peptic) cells | Pepsinogen | Inactive enzyme activated to pepsin, which digests proteins |
| Gastric lipase | Weak fat digestion (mainly active in infants) | |
| Mucous neck cells | Mucus | Protects stomach lining from acid and pepsin |
| G cells | Gastrin (hormone) | Stimulates secretion of HCl and gastric motility |
🧬 Enzymatic Actions in the Stomach
🧪 Pepsin
- Source: Chief cells (as pepsinogen)
- Activated by: HCl
- Function: Breaks down proteins into smaller peptides
- Optimal pH: 1.5 to 2.0
🧪 Gastric Lipase
- Acts on triglycerides to produce fatty acids and monoglycerides
- Plays a minor role in adults but more significant in infants
🔁 Role of Stomach Acid (HCl)
- Activates pepsinogen
- Kills bacteria and pathogens
- Denatures dietary proteins for easier enzyme access
- Creates acidic environment essential for enzyme function
🛠️ III. Overall Functions of the Stomach in Digestion
| Function | Details |
|---|---|
| Mechanical digestion | Churning mixes food with gastric juice to form chyme |
| Protein digestion | Initiated by pepsin |
| Minimal fat digestion | Gastric lipase acts on some lipids |
| Antibacterial defense | HCl destroys most ingested microbes |
| Secretion of intrinsic factor | Essential for vitamin B₁₂ absorption (prevents pernicious anemia) |
| Hormonal regulation | Gastrin stimulates gastric secretions and motility |
| Storage | Temporarily holds food before gradual release into the duodenum |
⚠️ Clinical Relevance
| Disorder | Effect |
|---|---|
| Gastritis | Inflammation of the stomach lining due to HCl/microbial damage |
| Peptic ulcers | Erosion of mucosal lining by excess acid or H. pylori |
| Achlorhydria | Absence of HCl, impairing protein digestion |
| Pernicious anemia | Due to intrinsic factor deficiency → vitamin B₁₂ malabsorption |
🧪 Digestion in the Stomach
| Aspect | Details |
|---|---|
| Mechanical | Mixing of food with gastric juice through peristaltic contractions |
| Chemical | Enzyme action by pepsin and gastric lipase |
| pH level | Highly acidic (1.5 to 3.5) |
| End product | Chyme – a semifluid mixture of partially digested food and gastric juice |
📘 Digestion in the Small Intestine –
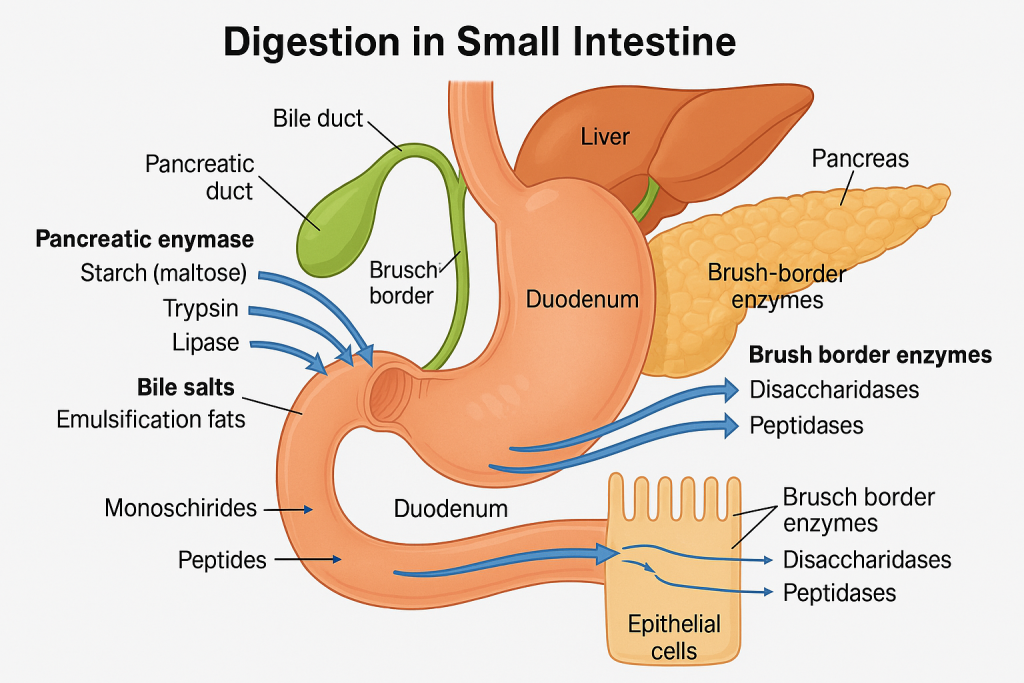
The small intestine is the main site for digestion and absorption in the human gastrointestinal tract. It is approximately 6 meters long and is divided into three parts: duodenum, jejunum, and ileum. Digestion in the small intestine involves mechanical mixing, chemical breakdown, and enzyme activity from both intestinal secretions and accessory digestive organs (pancreas and liver).
🧬 I. Mechanical Digestion in the Small Intestine
🔁 Segmental Contractions
- Rhythmic contractions of circular muscles that mix chyme with digestive juices.
- Facilitate exposure of food particles to enzymes and absorptive surfaces.
➡️ Peristalsis
- Wave-like contractions that propel chyme forward through the intestine.
🧪 II. Chemical Digestion in the Small Intestine
Chemical digestion in the small intestine depends on:
- Pancreatic enzymes
- Bile from the liver
- Brush border enzymes of the intestinal wall
📍 A. Enzymes from the Pancreas
Secreted into the duodenum via the pancreatic duct:
| Enzyme | Substrate | End Product |
|---|---|---|
| Amylase | Starch | Maltose, maltotriose |
| Lipase | Triglycerides (fats) | Fatty acids, monoglycerides |
| Trypsin, Chymotrypsin | Proteins | Peptides |
| Carboxypeptidase | Peptides | Amino acids |
| Nucleases | DNA/RNA | Nucleotides |
📍 B. Bile from the Liver (Stored in Gallbladder)
- Released into the duodenum via the common bile duct.
- Contains bile salts that:
- Emulsify fats into micelles.
- Increase surface area for lipase activity.
📍 C. Brush Border Enzymes
Located on the microvilli of enterocytes (intestinal lining cells):
| Enzyme | Substrate | End Product |
|---|---|---|
| Disaccharidases (maltase, sucrase, lactase) | Maltose, sucrose, lactose | Glucose, fructose, galactose |
| Peptidases | Peptides | Amino acids |
| Nucleotidases | Nucleotides | Nitrogen bases, sugars, phosphate |
| Enterokinase | Trypsinogen | Trypsin (activates other proteases) |
🌟 III. Functions of the Small Intestine in Digestion
| Function | Details |
|---|---|
| Completion of digestion | Final breakdown of carbohydrates, proteins, and lipids |
| Activation of enzymes | Enterokinase activates trypsin → cascade of protease activation |
| Emulsification of fats | Bile salts emulsify fats to aid digestion and absorption |
| Nutrient absorption | Villi and microvilli maximize surface area for efficient absorption |
| Neutralization of chyme | Bicarbonate from pancreas and Brunner’s glands neutralizes gastric acid |
🧪 IV. Summary Table: Digestion in the Small Intestine
| Digestive Agent | Source | Target Nutrient | End Product |
|---|---|---|---|
| Pancreatic amylase | Pancreas | Starch | Maltose, disaccharides |
| Disaccharidases | Brush border | Maltose, sucrose, lactose | Monosaccharides (glucose, etc.) |
| Pancreatic proteases | Pancreas | Proteins | Peptides |
| Peptidases | Brush border | Peptides | Amino acids |
| Lipase + bile salts | Pancreas + Liver | Triglycerides | Fatty acids, monoglycerides |
| Nucleases + nucleotidases | Pancreas + Intestinal cells | DNA/RNA | Nucleotides → bases + sugars |
⚠️ Clinical Correlation
| Condition | Effect |
|---|---|
| Lactose intolerance | Deficiency of lactase; causes bloating, diarrhea |
| Celiac disease | Autoimmune reaction damages villi; affects digestion and absorption |
| Pancreatic insufficiency | Inadequate enzymes; causes maldigestion, especially fats |
| Chronic diarrhea | May result from poor digestion or absorption of nutrients |
📘 Digestion in the Large Intestine – Academic Explanation
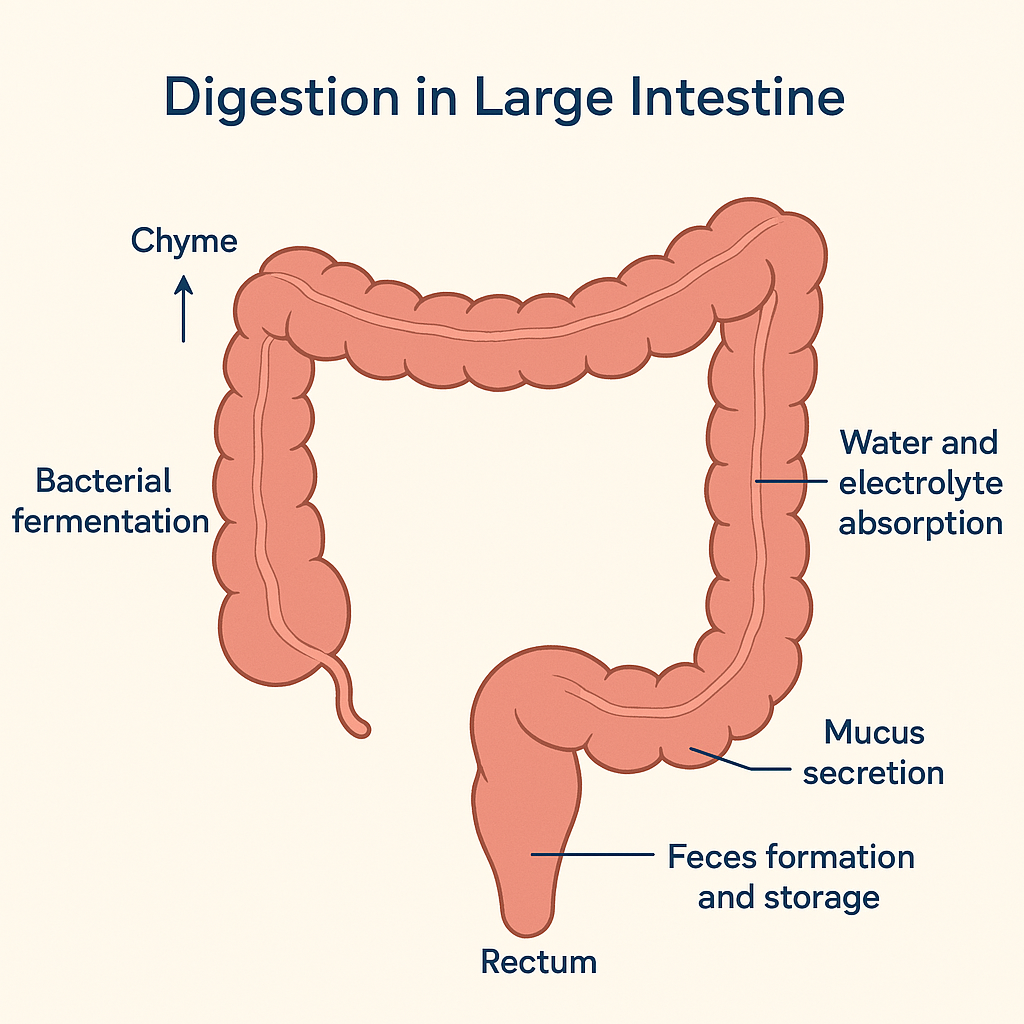
The large intestine, also known as the colon, is the final segment of the digestive tract. It measures approximately 1.5 meters in length and extends from the ileocecal valve to the anus. Unlike the stomach and small intestine, the large intestine does not play a major role in enzymatic digestion. However, it is essential for water absorption, electrolyte balance, bacterial fermentation, and formation and elimination of feces.
🧠 Overview of the Process
After chyme (partially digested food) passes through the ileocecal valve, it enters the cecum, the first part of the large intestine. By this stage, most nutrients have already been absorbed in the small intestine. The contents are now mostly undigested carbohydrates, fiber, water, salts, mucus, dead cells, and bacteria.
Digestion in the large intestine primarily involves mechanical movement, water and electrolyte absorption, and bacterial action rather than enzymatic activity from the body.
🦠 Role of Gut Microbiota (Bacterial Digestion)
The large intestine hosts trillions of beneficial bacteria, which play a critical role in the fermentation of undigested carbohydrates and in producing essential nutrients.
These gut bacteria:
- Ferment dietary fibers and resistant starches to produce short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate. These SCFAs are absorbed and used as an energy source by colon cells.
- Produce gases (hydrogen, methane, carbon dioxide) as by-products of fermentation.
- Synthesize vitamins such as vitamin K and some B vitamins (e.g., biotin and folate).
- Help modulate immune function and maintain intestinal barrier integrity.
💧 Water and Electrolyte Absorption
A significant function of the large intestine is the reabsorption of water and electrolytes such as sodium and chloride. This process transforms the liquid contents received from the small intestine into semi-solid feces. Up to 1.5 liters of water may be absorbed daily, preventing dehydration and maintaining homeostasis.
🧬 Mucus Secretion and Protection
The lining of the large intestine secretes mucus from numerous goblet cells. Mucus plays a key role in:
- Lubricating the fecal material, facilitating its movement.
- Protecting the intestinal lining from mechanical damage and microbial invasion.
- Binding waste material together for proper fecal formation.
Importantly, the large intestine does not secrete digestive enzymes. All enzymatic digestion concludes in the small intestine.
🪵 Feces Formation and Storage
As undigested material and waste products pass through the colon, they are gradually dehydrated and compacted into feces. This fecal matter is temporarily stored in the rectum until defecation occurs. The process is coordinated by voluntary and involuntary muscle actions.
🧠 Regulation of Defecation
The presence of feces in the rectum stimulates stretch receptors, initiating the defecation reflex. This leads to:
- Relaxation of the internal anal sphincter (involuntary).
- Voluntary control of the external anal sphincter.
- Conscious action supported by abdominal muscles and diaphragm to expel the feces.
⚠️ Clinical Notes
- In constipation, slow movement through the colon leads to excessive water reabsorption and hard stools.
- In diarrhea, rapid transit prevents sufficient water absorption, resulting in loose stools.
- Dysbiosis (imbalance in gut bacteria) can affect vitamin synthesis, immunity, and even mental health.
- Antibiotics can disrupt the gut flora, reducing vitamin K production and increasing susceptibility to infections like Clostridium difficile.
While the large intestine does not perform significant enzymatic digestion, it is indispensable for:
- Fermentation of undigested residues
- Synthesis of essential vitamins
- Water and electrolyte reabsorption
- Formation, storage, and controlled elimination of feces
These functions support not only digestion but also fluid balance, nutrient recycling, and overall gut health.
📘 Absorption of Food –
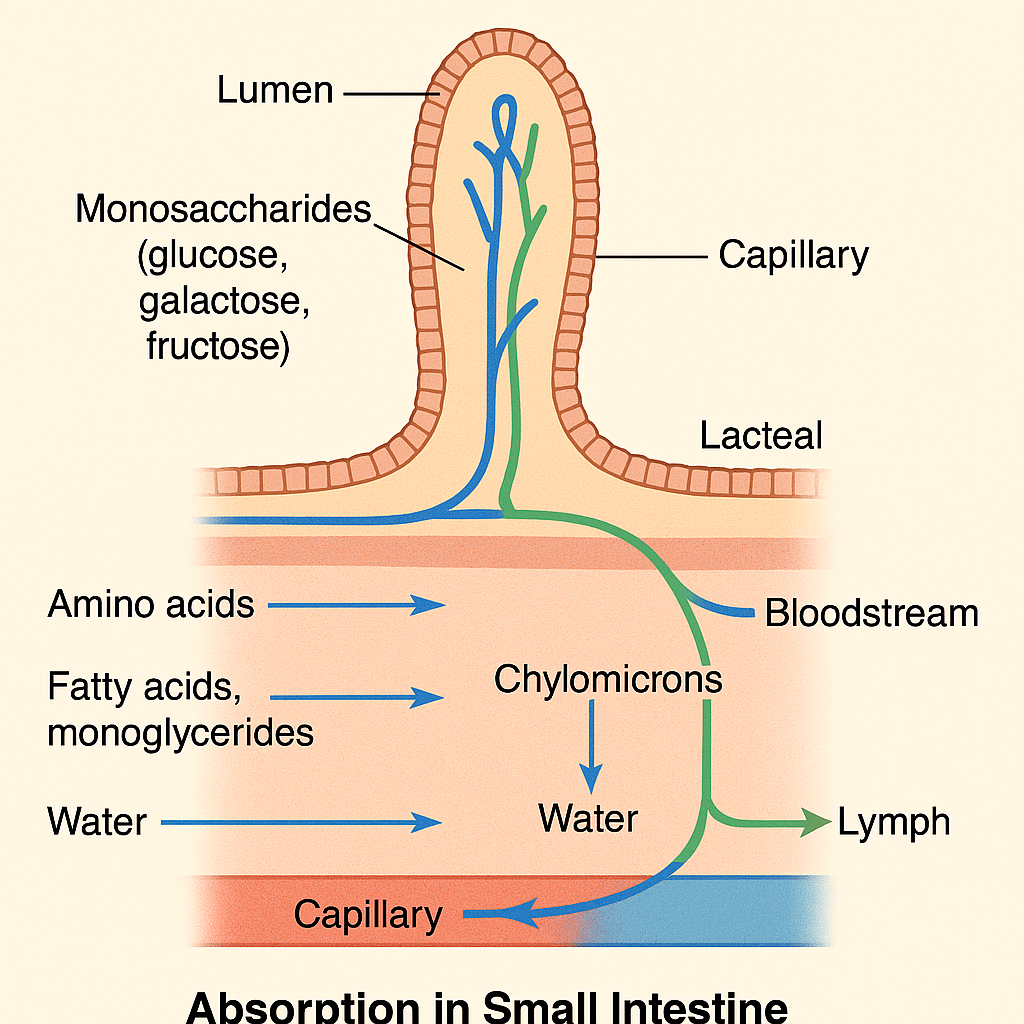
Absorption is the process by which digested nutrients pass from the lumen of the gastrointestinal tract into the blood or lymphatic system, allowing the body to utilize them for energy, growth, repair, and cellular functions. This process occurs mainly in the small intestine, although limited absorption happens in the mouth, stomach, and large intestine.
🧠 Key Sites of Absorption
- Mouth – negligible, except for some drugs (e.g., nitroglycerin).
- Stomach – minor absorption of water, alcohol, aspirin, and lipid-soluble drugs.
- Small Intestine – major site of nutrient absorption.
- Large Intestine – absorption of water, electrolytes, and some vitamins (e.g., vitamin K, biotin).
🧬 Structure Adapted for Absorption (Small Intestine)
The small intestine is specially designed to maximize absorption:
- Villi: Finger-like projections of the mucosa.
- Microvilli (brush border): Tiny hair-like extensions on epithelial cells.
- Crypts of Lieberkühn: Invaginations that help regenerate intestinal cells.
- Capillaries and lacteals: Present in each villus to absorb nutrients into the blood (hydrophilic) or lymph (lipophilic).
These structures increase the surface area of the intestine over 600 times, enhancing its ability to absorb nutrients efficiently.
🍽️ Absorption of Nutrients: Site-Wise and Nutrient-Wise
1. Carbohydrates
- End product: Monosaccharides (glucose, galactose, fructose)
- Site: Mainly in the jejunum
- Mechanism:
- Glucose & galactose: Active transport with sodium (SGLT-1)
- Fructose: Facilitated diffusion (GLUT-5)
- Enters capillaries → hepatic portal vein → liver
2. Proteins
- End product: Amino acids, dipeptides, tripeptides
- Site: Duodenum and jejunum
- Mechanism:
- Amino acids: Active transport
- Dipeptides/tripeptides: Secondary active transport, then broken down intracellularly
- Enters capillaries → portal circulation
3. Fats (Lipids)
- End product: Fatty acids, monoglycerides, glycerol
- Site: Duodenum and jejunum
- Mechanism:
- Bile salts form micelles to help lipid absorption.
- Inside epithelial cells: reassembled into triglycerides, coated with proteins → form chylomicrons.
- Chylomicrons enter lacteals (lymphatic capillaries) → lymph → thoracic duct → bloodstream
4. Water
- Absorbed throughout the small intestine and colon
- Absorption is passive, by osmosis
- Approximately 8–9 liters/day of water are absorbed in the small intestine.
5. Electrolytes
- Sodium (Na⁺): Actively absorbed, often with glucose or amino acids
- Chloride (Cl⁻): Passively follows Na⁺
- Potassium (K⁺): Absorbed by diffusion in the small intestine
- Calcium and Iron:
- Absorbed in the duodenum
- Calcium absorption is vitamin D dependent
- Iron absorption is enhanced by acidic pH and vitamin C
6. Vitamins
- Fat-soluble (A, D, E, K): Absorbed with dietary fat via micelles
- Water-soluble (B-complex, C): Absorbed via active or passive transport
- Vitamin B₁₂:
- Binds to intrinsic factor (from the stomach)
- Absorbed in the ileum
🔄 Transport After Absorption
- Bloodstream (Portal circulation): Transports water-soluble nutrients (sugars, amino acids, water-soluble vitamins) directly to the liver for metabolism and distribution.
- Lymphatic system: Transports fat-soluble nutrients (lipids and fat-soluble vitamins) via lacteals in villi → enters bloodstream through thoracic duct.
⚠️ Clinical Relevance
- Malabsorption syndromes (e.g., celiac disease, Crohn’s disease): Lead to nutrient deficiencies.
- Lactose intolerance: Poor absorption of lactose causes diarrhea and gas.
- Vitamin B₁₂ deficiency: Due to intrinsic factor loss (pernicious anemia).
- Steatorrhea: Fat malabsorption causes fatty stools.
Absorption is a highly specialized and efficient process, primarily occurring in the small intestine, with help from:
- Villi and microvilli for surface area expansion,
- Enzymes and transporters for breaking down and moving nutrients,
- Lymphatic and vascular systems for nutrient transport.
Together, these systems ensure the body receives all essential nutrients for proper physiological functioning.
📘 Applications and Implications in Nursing – Digestive System
The digestive system plays a central role in nutrient breakdown, absorption, metabolism, and waste elimination. For nurses, understanding this system is crucial for monitoring nutritional status, recognizing gastrointestinal disorders, and administering appropriate care interventions.
🧠 I. Applications of Digestive System Knowledge in Nursing Practice
1. 🩺 Comprehensive Health Assessment
- Nurses assess for symptoms like nausea, vomiting, diarrhea, constipation, abdominal pain, bloating, or indigestion.
- Abdominal examination (inspection, auscultation, percussion, palpation) helps detect organ enlargement, masses, bowel sounds, or tenderness.
2. 🧪 Monitoring Nutritional Status
- Assess dietary intake and correlate with digestion and absorption efficiency.
- Monitor signs of malnutrition, especially in patients with GI diseases (e.g., Crohn’s, ulcerative colitis, celiac disease).
- Use tools like BMI, mid-arm circumference, and serum albumin levels to evaluate nutritional status.
3. 💊 Drug Administration
- Nurses need to understand:
- Absorption sites for oral medications (e.g., some drugs are absorbed in the stomach, others in the small intestine).
- The effect of food on drug absorption (e.g., calcium affects iron absorption).
- Enteral feeding implications for drug compatibility and timing.
4. 🏥 Enteral and Parenteral Nutrition
- Nurses manage:
- Nasogastric (NG) feeding
- PEG tube care
- Parenteral nutrition (TPN) in critically ill patients
- Must monitor for complications like aspiration, blockage, diarrhea, or infection.
5. 💩 Elimination and Bowel Care
- Monitor bowel patterns; promote healthy elimination.
- Administer enemas, laxatives, or assist with bowel retraining programs.
- Educate patients with colostomy or ileostomy care.
6. 🦠 Infection Control
- Educate and implement hygiene measures for patients with gastrointestinal infections (e.g., Clostridium difficile, hepatitis A).
- Monitor for dehydration and electrolyte imbalance in patients with persistent vomiting or diarrhea.
7. 🔬 Pre and Post-operative Care
- Prepare patients for endoscopy, colonoscopy, abdominal surgeries.
- Monitor bowel sounds and peristalsis post-operatively.
- Prevent complications like paralytic ileus, constipation, or surgical site infection.
⚠️ II. Nursing Implications in Gastrointestinal Disorders
1. Peptic Ulcer Disease
- Monitor pain, bleeding signs, dietary habits.
- Educate on avoidance of NSAIDs, alcohol, spicy foods.
- Administer antacids, proton pump inhibitors (PPIs).
2. Gastroesophageal Reflux Disease (GERD)
- Position patient upright after meals.
- Educate on small meals, low-fat diet, avoiding late-night eating.
- Monitor for esophagitis or aspiration risks.
3. Hepatitis and Liver Disease
- Observe for jaundice, ascites, bleeding, mental status changes.
- Ensure low-protein, high-carbohydrate diet in hepatic encephalopathy.
- Practice infection control and drug safety.
4. Malabsorption Syndromes (e.g., Celiac Disease)
- Monitor for weight loss, anemia, diarrhea.
- Educate on gluten-free diet and nutritional supplements.
5. Constipation and Diarrhea
- Assess causes (diet, drugs, immobility).
- Promote hydration, high-fiber diet, mobility.
- Prevent complications like electrolyte imbalance or skin breakdown.
6. Colorectal Cancer
- Encourage screening (FOBT, colonoscopy), especially in at-risk patients.
- Monitor post-op patients for bowel function, bleeding, stoma care.
🧬 III. Nursing Education and Patient Counseling
- Educate on:
- Balanced diet and hydration
- Hygiene and handwashing
- Safe food preparation
- Early signs of digestive issues
- Support patients with:
- Chronic GI diseases
- Lifestyle modifications
- Coping with stoma or feeding tubes
Understanding the digestive system has direct applications in almost every area of nursing care—from bedside assessments to complex medical-surgical management. It enables nurses to:
- Promote nutritional health
- Prevent complications
- Implement targeted interventions
- Deliver holistic patient care