NML-B.SC-SEM-5-NOTES-UNIT-2-Management basics appliedto Nursing
Management Basics Applied to Nursing – Definitions

Management in nursing involves the application of leadership, planning, organization, decision-making, and control to ensure effective healthcare delivery and patient safety. It focuses on the efficient use of resources, staff coordination, and policy implementation to provide quality nursing care.
General Definitions of Management
- Henry Fayol (Father of Management Theory) –
“Management is to forecast, to plan, to organize, to command, to coordinate, and to control.” - Frederick Taylor (Scientific Management) –
“Management is knowing exactly what you want men to do and then seeing that they do it in the best and cheapest way.” - Peter Drucker (Modern Management Thinker) –
“Management is doing things right; leadership is doing the right things.”
Definitions of Nursing Management
- American Nurses Association (ANA) –
“Nursing management is the process of working through staff members to provide care, achieve patient safety, and enhance nursing practice in a healthcare setting.” - Marquis and Huston (Leadership and Management in Nursing) –
“Nursing management involves planning, organizing, staffing, leading, and controlling healthcare services to ensure quality patient care.” - Nursing and Midwifery Council (NMC) –
“Nursing management ensures that nursing staff provides safe, effective, and ethical patient care through proper supervision, coordination, and resource allocation.”
Key Aspects of Nursing Management
- Clinical Management – Ensuring high-quality patient care through proper staffing, supervision, and evidence-based practice.
- Administrative Management – Managing hospital policies, human resources, budgeting, and compliance with healthcare regulations.
- Leadership in Nursing – Motivating, guiding, and supervising nursing teams for optimal performance and patient safety.
- Decision-Making in Nursing – Handling routine and emergency situations, patient care coordination, and strategic planning.
Management Basics Applied to Nursing – Concepts

Management in nursing involves the application of leadership, organization, decision-making, and supervision to ensure high-quality patient care. Nursing management integrates scientific principles of management with nursing practice to optimize healthcare delivery, staff efficiency, and patient outcomes.
Key Concepts of Nursing Management
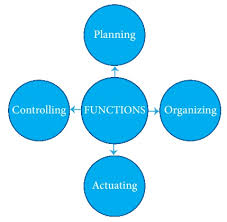
1. Functions of Nursing Management (Fayol’s Five Functions)
The core functions of nursing management align with Henri Fayol’s classical management functions, adapted to healthcare settings:
- Planning
- Setting patient care goals, staffing requirements, and resource allocation.
- Developing nursing policies and protocols to ensure smooth hospital operations.
- Example: Creating duty rosters for nurses to ensure 24/7 coverage in critical care units.
- Organizing
- Structuring nursing teams, assigning tasks, and coordinating with other healthcare professionals.
- Establishing departments, units, and hierarchy in nursing services.
- Example: Assigning a head nurse for ICU, OPD, and surgical wards for better workflow management.
- Staffing
- Recruitment, training, and retention of qualified nursing staff.
- Ensuring the right nurse-to-patient ratio to maintain quality care.
- Example: Conducting continuing education programs to enhance nursing skills.
- Directing (Leading)
- Providing guidance, supervision, and motivation to nursing teams.
- Encouraging effective communication and teamwork.
- Example: A nurse manager conducting regular team meetings to address challenges and improve morale.
- Controlling (Evaluating and Monitoring)
- Ensuring compliance with hospital policies, infection control measures, and patient care protocols.
- Monitoring nursing performance and patient outcomes.
- Example: Implementing feedback systems to evaluate patient satisfaction and improve nursing care.
2. Levels of Nursing Management
Nursing management is structured across different levels, each with specific responsibilities.
- Top-Level Management (Strategic Planning)
- Includes Chief Nursing Officers (CNO), Nursing Directors, and Hospital Administrators.
- Responsible for policy formulation, financial management, and collaboration with healthcare authorities.
- Example: Developing national nursing guidelines and standards for hospitals.
- Middle-Level Management (Operational Planning)
- Includes Nursing Supervisors, Ward Managers, and Department Heads.
- Oversees day-to-day hospital operations, staff coordination, and patient care quality.
- Example: Ensuring sufficient staff in emergency departments based on patient inflow.
- Lower-Level Management (Direct Patient Care)
- Includes Charge Nurses, Team Leaders, and Senior Staff Nurses.
- Directly involved in patient care, supervision of junior nurses, and implementing protocols.
- Example: Ensuring medication administration is error-free through proper supervision.
3. Decision-Making in Nursing Management
Decision-making is a critical component of nursing management that ensures smooth hospital operations and quality care.
- Routine Decisions – Daily staffing, medication rounds, patient admission policies.
- Crisis Decisions – Handling emergencies, ICU transfers, disaster response.
- Strategic Decisions – Implementing new nursing protocols, budget planning.
Example: During a natural disaster, the nursing manager must decide on resource allocation, patient triage, and emergency staffing.
4. Communication in Nursing Management
Effective communication is essential for coordinating patient care, maintaining teamwork, and preventing medical errors.
- Verbal Communication – Staff meetings, shift handovers, patient education.
- Non-Verbal Communication – Body language, facial expressions in patient interactions.
- Written Communication – Medical records, patient care plans, nursing documentation.
- Electronic Communication – Use of hospital management software, telemedicine, and digital charting.
Example: Using electronic health records (EHRs) to ensure accurate documentation and reduce medication errors.
5. Leadership Styles in Nursing Management
Nursing managers adopt different leadership styles based on their team, hospital policies, and patient care needs.
- Autocratic Leadership – Strict control, fast decision-making, useful in emergencies.
- Democratic Leadership – Encourages teamwork and staff participation in decision-making.
- Laissez-Faire Leadership – Hands-off approach, allowing experienced staff to work independently.
- Transformational Leadership – Inspires nurses to improve patient care, encourages innovation.
- Transactional Leadership – Focuses on structure, rewards, and performance-based management.
Example: During a COVID-19 crisis, autocratic leadership helps in quick decision-making, while democratic leadership enhances teamwork in normal hospital operations.
6. Quality Improvement and Patient Safety
Nursing management plays a key role in improving hospital safety standards and patient care outcomes.
- Risk Management – Identifying and preventing potential safety issues (e.g., falls, infections).
- Patient-Centered Care – Ensuring nurses follow ethical practices, informed consent, and cultural sensitivity.
- Evidence-Based Practice (EBP) – Applying scientific research to improve nursing protocols.
- Example: Implementing hand hygiene protocols to reduce hospital-acquired infections.
7. Challenges in Nursing Management
Despite advancements, nursing management faces several challenges:
- Nursing Staff Shortages – High patient load with fewer nurses.
- Burnout and Stress – Long working hours, high-pressure environment.
- Ethical and Legal Issues – Handling medical negligence cases, patient rights.
- Limited Career Growth – Lack of leadership roles for nurses.
- Workplace Safety Issues – Violence against healthcare workers.
Management Basics Applied to Nursing – Theories of Management
Management theories provide a structured framework for organizing, leading, and improving healthcare services in nursing. These theories guide nurse managers in decision-making, staff management, patient care coordination, and overall healthcare delivery. Management in nursing aims to balance efficiency, quality patient care, and workforce well-being.
Management theories can be broadly categorized into:
- Classical Theories – Focus on structure, efficiency, and workflow optimization.
- Behavioral Theories – Emphasize human relations, motivation, and teamwork.
- Contemporary Theories – Address modern challenges like digitalization, flexibility, and evidence-based practice.
1. Classical Management Theories
These theories were developed during the industrial revolution and focus on efficiency, productivity, and structured workflow. They provide a strong foundation for nursing administration and healthcare organization.
A. Scientific Management Theory (Frederick Taylor)
- Focus: Improving efficiency through standardization, training, and workflow optimization.
- Principles:
- Work Specialization – Assigning nurses specific tasks based on their skills.
- Training & Development – Ensuring nurses follow standardized procedures.
- Performance-Based Rewards – Encouraging productivity through incentives.
- Time and Motion Studies – Analyzing nursing tasks to minimize wasted effort.
- Application in Nursing:
- Implementing nursing protocols for patient care and medication administration.
- Streamlining ICU and emergency department workflows.
- Standardizing procedures for infection control and hygiene.
B. Bureaucratic Management Theory (Max Weber)
- Focus: Organizational structure, hierarchy, and formal rules to maintain order.
- Principles:
- Hierarchy of Authority – Nurses follow a clear chain of command.
- Standard Operating Procedures (SOPs) – Protocols ensure uniform healthcare delivery.
- Impersonal Relationships – Reducing bias by maintaining professionalism.
- Merit-Based Promotion – Recognizing nurses based on performance and experience.
- Application in Nursing:
- Hospital hierarchy: Chief Nursing Officer → Nurse Supervisors → Staff Nurses.
- Regulated policies for infection control, patient safety, and ethical nursing practices.
- Uniform documentation in patient records, reducing errors in patient care.
C. Administrative Management Theory (Henri Fayol)
- Focus: Establishing management principles applicable to all organizations.
- 14 Principles of Management (Key ones for nursing):
- Division of Work – Assigning specialized nurses to ICU, OT, OPD.
- Unity of Command – Nurses report to a single supervisor for clarity.
- Discipline – Ensuring adherence to hospital policies and professional ethics.
- Centralization & Decentralization – Balancing decision-making at different levels.
- Esprit de Corps – Encouraging teamwork and harmony among nursing staff.
- Application in Nursing:
- Task delegation among nursing teams (e.g., surgical nurses vs. general ward nurses).
- Efficient communication between nursing departments and hospital administration.
- Promoting teamwork in multidisciplinary healthcare settings.
2. Behavioral Management Theories
Behavioral theories emphasize human relations, leadership styles, motivation, and teamwork in nursing management.
A. Human Relations Theory (Elton Mayo)
- Focus: Employee well-being, social interactions, and job satisfaction.
- Key Findings:
- Happy nurses provide better patient care.
- Social support and teamwork enhance efficiency.
- A positive workplace environment improves performance.
- Application in Nursing:
- Implementing stress management programs to support nurse well-being.
- Encouraging collaborative teamwork among nurses, doctors, and allied health staff.
- Conducting regular feedback sessions to enhance staff relationships and job satisfaction.
B. Maslow’s Hierarchy of Needs Theory
- Focus: Five levels of human needs influencing motivation.
| Level | Nursing Application |
|---|---|
| Physiological Needs | Providing adequate rest, meal breaks, and safe working conditions. |
| Safety Needs | Ensuring workplace safety, job security, and protective equipment (PPE). |
| Love & Belonging | Encouraging teamwork, mentorship, and supportive work culture. |
| Esteem Needs | Recognizing and rewarding nurses’ achievements. |
| Self-Actualization | Providing leadership roles, career growth, and professional development. |
- Application in Nursing:
- Recognizing and rewarding nurses for their contributions.
- Creating leadership pathways for career growth.
- Implementing wellness programs to support emotional health.
C. McGregor’s Theory X and Theory Y
- Focus: Two types of leadership styles based on motivation.
| Theory X (Strict Control) | Theory Y (Empowerment-Based Leadership) |
|---|---|
| Nurses avoid responsibility and need supervision. | Nurses are self-motivated and work better with autonomy. |
| Strict control and rigid hierarchy. | Encourages participation and innovation. |
| Authoritarian leadership. | Democratic leadership. |
- Application in Nursing:
- Theory X: Used in emergency settings requiring strict supervision.
- Theory Y: Applied in research, education, and leadership roles.
3. Contemporary Management Theories
Modern theories address complex healthcare challenges like digitalization, adaptability, and team-based decision-making.
A. Systems Theory
- Focus: Healthcare as an interdependent system where different units collaborate.
- Principles:
- Hospitals function as a system with nurses, doctors, and administration.
- Changes in one department affect others.
- Continuous feedback improves efficiency.
- Application in Nursing:
- Coordinating between ICU, OPD, and emergency units.
- Using digital health records to streamline patient care.
- Integrating mental health services with general healthcare.
B. Contingency Theory
- Focus: No single management style works in all situations. Leadership should adapt based on circumstances.
- Key Concepts:
- Flexible management strategies for different hospital settings.
- Decision-making depends on patient conditions, workload, and resources.
- Application in Nursing:
- During a pandemic, nurse managers may use an autocratic style for quick decision-making.
- In routine care, a participative leadership style is encouraged.
C. Transformational Leadership Theory
- Focus: Inspiring and empowering nurses to improve patient care.
- Key Concepts:
- Visionary Leadership – Encouraging nurses to improve and innovate.
- Encouraging teamwork and mentorship.
- Motivating staff through recognition and rewards.
- Application in Nursing:
- Implementing evidence-based nursing practices.
- Supporting continuing education and leadership development for nurses.
- Implementing innovative patient care strategies.
4. Importance of Management Theories in Nursing
- Provides structured leadership and decision-making frameworks.
- Improves patient safety, nurse-patient ratios, and workflow efficiency.
- Encourages teamwork, communication, and motivation in nursing staff.
- Enhances quality assurance, risk management, and hospital efficiency.
Importance, Features, and Levels of Management in Nursing

1. Importance of Management in Nursing
Nursing management plays a crucial role in healthcare delivery by ensuring effective patient care, workforce efficiency, and operational excellence. Effective management enhances decision-making, resource allocation, and staff coordination, leading to improved healthcare outcomes.
A. Importance of Nursing Management
- Ensures Quality Patient Care
- Organizes nursing activities to maintain high standards of care.
- Implements evidence-based nursing practices.
- Optimizes Resource Utilization
- Proper allocation of human resources, equipment, and financial resources.
- Reduces wastage and improves cost-effectiveness in healthcare facilities.
- Improves Nursing Workforce Efficiency
- Effective staffing, training, and scheduling improve productivity.
- Ensures appropriate nurse-patient ratios for better patient outcomes.
- Enhances Communication and Coordination
- Facilitates teamwork between nurses, doctors, and allied healthcare professionals.
- Encourages interdisciplinary collaboration to improve healthcare delivery.
- Strengthens Leadership in Nursing
- Develops leadership skills among nurses for better decision-making and crisis management.
- Encourages innovation in patient care and hospital administration.
- Ensures Compliance with Healthcare Regulations
- Implements policies that comply with legal, ethical, and professional standards.
- Reduces medical errors and promotes patient safety.
- Promotes Employee Satisfaction and Retention
- Supports mental health, career growth, and motivation among nursing staff.
- Reduces burnout and improves job satisfaction.
- Facilitates Crisis and Emergency Management
- Prepares healthcare teams for disasters, pandemics, and emergency situations.
- Ensures effective handling of mass casualties and sudden patient surges.
2. Features of Nursing Management
The features of nursing management define the scope, approach, and objectives of effective healthcare leadership.
A. Key Features of Nursing Management
- Goal-Oriented
- Focuses on achieving high-quality patient care and operational efficiency.
- Universal Applicability
- Applied at all levels of healthcare, from hospital administration to bedside nursing.
- Continuous Process
- Nursing management is a dynamic, ongoing process involving planning, execution, and evaluation.
- People-Oriented
- Centers around nurses, patients, doctors, and healthcare workers.
- Decision-Making Based
- Involves critical thinking, problem-solving, and informed decision-making.
- Leadership and Supervision
- Involves guiding and monitoring nursing staff to ensure compliance with protocols.
- Efficiency and Cost-Effectiveness
- Maximizes resource utilization to minimize expenses and improve service delivery.
- Flexibility and Adaptability
- Adjusts to changing healthcare needs, new medical advancements, and patient demands.
- Follows Ethical and Legal Standards
- Upholds patient rights, confidentiality, and professional ethics.
- Encourages Innovation and Research
- Promotes evidence-based practice, research, and continuous learning in nursing.
3. Levels of Management in Nursing
Nursing management operates at different levels, each responsible for specific functions and decision-making.
A. Three Levels of Nursing Management
| Level | Position/Role | Key Responsibilities |
|---|---|---|
| 1. Top-Level Management | Chief Nursing Officer (CNO), Nursing Directors, Hospital Administrators | – Policy making and strategic planning.- Financial and resource management.- Collaboration with healthcare authorities. |
| 2. Middle-Level Management | Nursing Supervisors, Ward Managers, Department Heads | – Implementing policies set by top management.- Supervising daily hospital operations.- Training and evaluating nursing staff. |
| 3. Lower-Level Management | Charge Nurses, Team Leaders, Senior Staff Nurses | – Direct patient care and bedside nursing.- Supervising junior nurses and hospital aides.- Ensuring adherence to treatment protocols. |
B. Functions of Each Level of Nursing Management
1. Top-Level Nursing Management (Strategic Planning)
- Long-term goal setting for hospital growth and patient care improvements.
- Decision-making for healthcare policies and regulatory compliance.
- Budgeting and financial planning for nursing services.
- Collaboration with government agencies, medical boards, and accreditation bodies.
✅ Example: A Chief Nursing Officer (CNO) develops hospital-wide infection control policies to reduce hospital-acquired infections.
2. Middle-Level Nursing Management (Operational Planning)
- Supervises nursing staff and hospital departments.
- Ensures patient care standards and hospital protocols are maintained.
- Conducts staff training programs and performance evaluations.
- Acts as a link between top management and lower-level nurses.
✅ Example: A Nursing Supervisor ensures that all nurses in an ICU unit follow proper ventilator management protocols.
3. Lower-Level Nursing Management (Direct Patient Care)
- Directly involved in bedside patient care.
- Monitors medication administration and nursing interventions.
- Reports patient progress and complications to higher management.
- Guides and supports junior nurses, interns, and healthcare assistants.
✅ Example: A Charge Nurse in the surgical ward ensures post-operative patients receive appropriate wound care and pain management.
4. Differences Between Levels of Management
| Aspect | Top-Level Management | Middle-Level Management | Lower-Level Management |
|---|---|---|---|
| Focus | Strategic decision-making, policy formulation | Operational supervision, policy implementation | Direct patient care, hands-on nursing |
| Decision-Making | Long-term and high-impact decisions | Medium-term, daily operations | Short-term, direct patient interventions |
| Communication Flow | Downward to middle and lower levels | Both upward (from lower level) and downward (from top level) | Upward to supervisors, patient interactions |
| Responsibility | Hospital-wide nursing services | Departmental and unit management | Individual patient care |
Summary
Nursing management is essential for efficient healthcare delivery, patient safety, and staff well-being. The importance, features, and levels of management define its scope, ensuring that healthcare institutions function smoothly.
✅ Key Takeaways:
- Nursing management ensures high-quality patient care, workforce coordination, and resource optimization.
- It is characterized by efficiency, teamwork, leadership, adaptability, and ethical responsibility.
- It operates at three levels: top (policy-making), middle (operational supervision), and lower (direct patient care).
By integrating strong leadership, effective decision-making, and structured workflows, nursing management improves healthcare services, staff satisfaction, and patient outcomes.
Management and Administration in Nursing

Management and administration are essential aspects of nursing leadership, ensuring the smooth functioning of healthcare organizations. While both concepts involve planning, organizing, directing, and controlling, management focuses on operational execution, whereas administration is more strategic and policy-driven.
In the healthcare setting, nursing management deals with day-to-day operations, resource allocation, and patient care, whereas nursing administration involves high-level decision-making, policy formulation, and financial planning.
Definitions of Management and Administration
A. Management
Management is the process of planning, organizing, leading, and controlling resources to achieve specific goals efficiently. In nursing, it refers to coordinating staff, optimizing workflows, and ensuring quality patient care.
Henri Fayol:
“Management is to forecast, to plan, to organize, to command, to coordinate, and to control.”
Peter Drucker:
“Management is doing things right; leadership is doing the right things.”
Nursing Perspective (ANA – American Nurses Association):
“Nursing management ensures patient safety, staff coordination, and resource utilization in a healthcare setting.”
B. Administration
Administration involves policy formulation, strategic planning, and governance of an organization. In nursing, it refers to developing policies, ensuring regulatory compliance, and overseeing the overall healthcare system.
E.F.L. Brech:
“Administration is concerned with policy-making, defining objectives, and ensuring the implementation of organizational goals.”
Gulick and Urwick:
“Administration is primarily concerned with the formulation of broad policies and major decisions.”
Healthcare Administration Perspective:
“Nursing administration involves leadership in healthcare systems, ensuring quality standards, financial planning, and policy compliance.”
Differences Between Management and Administration in Nursing
| Aspect | Management | Administration |
|---|---|---|
| Definition | Execution of plans and supervision of nursing staff. | Policy formulation and strategic decision-making. |
| Focus | Day-to-day operations, patient care, and staff coordination. | Long-term goals, budgeting, and hospital policies. |
| Decision-Making | Tactical and operational decisions. | Strategic and high-level decisions. |
| Functions | Planning, organizing, staffing, directing, controlling. | Policy-making, resource allocation, financial planning, governance. |
| Authority Level | Middle and lower-level nursing managers. | Top-level executives, nursing administrators, government bodies. |
| Scope | Concerned with nurses, patients, and hospital staff. | Concerned with the entire healthcare system and regulations. |
| Example | A nursing supervisor assigns daily patient care duties and monitors staff performance. | A chief nursing officer (CNO) develops hospital-wide nursing policies and budget allocations. |
Relationship Between Management and Administration
Despite their differences, management and administration work together to ensure the effective functioning of healthcare organizations.
- Administration sets the policies, while management executes them.
- Example: Hospital administrators set infection control policies, and nurse managers implement them in clinical settings.
- Both require leadership and coordination.
- Nurse administrators plan long-term healthcare strategies, while nurse managers implement day-to-day patient care plans.
- Both involve decision-making and resource management.
- Administrators allocate financial and human resources, while managers ensure their efficient utilization.
Functions of Management and Administration in Nursing
A. Functions of Nursing Management (Fayol’s Five Functions)
- Planning – Setting nursing objectives and policies for patient care.
- Organizing – Assigning roles and responsibilities to nurses.
- Staffing – Recruiting, training, and retaining nursing personnel.
- Directing – Supervising nursing teams and ensuring compliance.
- Controlling – Monitoring nursing performance and implementing corrective actions.
✅ Example: A nursing manager schedules nurses based on patient needs and ensures adherence to hospital policies.
B. Functions of Nursing Administration
- Policy Formulation – Developing hospital-wide nursing policies.
- Financial Management – Budgeting for nursing departments.
- Regulatory Compliance – Ensuring adherence to healthcare laws and standards.
- Leadership Development – Encouraging career growth for nursing staff.
- Interdepartmental Coordination – Collaborating with medical, administrative, and government agencies.
✅ Example: A Chief Nursing Officer (CNO) establishes a policy for patient safety and infection control in hospitals.
Levels of Management and Administration in Nursing
| Level | Position/Role | Key Responsibilities |
|---|---|---|
| Top-Level (Administration) | Chief Nursing Officer (CNO), Nursing Directors, Healthcare Executives | – Policy making and strategic planning.- Financial and resource management.- Compliance with healthcare regulations. |
| Middle-Level (Management) | Nursing Supervisors, Ward Managers, Department Heads | – Implementing hospital policies.- Supervision of nursing staff.- Managing patient care units. |
| Lower-Level (Direct Nursing Care) | Charge Nurses, Team Leaders, Senior Staff Nurses | – Hands-on patient care.- Training junior nurses.- Ensuring adherence to treatment protocols. |
✅ Example: A hospital administrator approves a new nursing protocol, and nursing managers implement it in daily hospital operations.
Challenges in Nursing Management and Administration
A. Challenges in Nursing Management
- Workforce Shortages – High patient load with fewer nurses.
- Burnout and Stress – Long working hours, emotional toll.
- Operational Inefficiencies – Poor nurse-patient ratios affecting care quality.
B. Challenges in Nursing Administration
- Budget Constraints – Limited funds for staffing and training.
- Legal and Ethical Issues – Managing patient rights and hospital liabilities.
- Healthcare Policy Changes – Adapting to new laws and accreditation requirements.
✅ Example: During COVID-19, nurse managers faced staffing issues, while hospital administrators handled resource allocation and policymaking.
Importance of Management and Administration in Nursing
A. Importance of Nursing Management
- Ensures quality patient care and safety.
- Optimizes workforce efficiency and teamwork.
- Improves communication and staff coordination.
- Facilitates crisis and emergency response.
B. Importance of Nursing Administration
- Sets long-term healthcare policies and standards.
- Ensures financial sustainability and resource management.
- Promotes leadership development and career growth for nurses.
- Maintains legal compliance and accreditation.
✅ Example: A Chief Nursing Officer designs hospital policies, while nurse managers execute them for patient care improvements.
Summary
Nursing management and administration are interconnected, playing a vital role in healthcare operations. While management focuses on execution and patient care, administration involves policy-making and strategic leadership.
✅ Key Takeaways:
- Management handles daily nursing operations, while administration handles strategic hospital planning.
- Both require strong leadership, coordination, and decision-making skills.
- Effective nursing management ensures smooth patient care, while nursing administration shapes the future of healthcare policies.
By integrating effective management and administration strategies, nursing leaders can enhance healthcare quality, patient safety, and staff well-being.
Functions of Management in Nursing
Management in nursing involves planning, organizing, staffing, directing, and controlling nursing services to ensure efficient healthcare delivery. These functions, first introduced by Henri Fayol, are universally applied in nursing to enhance patient care, staff coordination, and hospital administration.
Each function plays a vital role in decision-making, resource allocation, and leadership in nursing management.
Five Key Functions of Nursing Management
The five essential functions of management, as applied in nursing, include:
| Function | Purpose in Nursing | Examples in Nursing Management |
|---|---|---|
| 1. Planning | Setting objectives, policies, and procedures. | Developing hospital infection control policies. |
| 2. Organizing | Structuring roles, responsibilities, and workflows. | Assigning nurses to different hospital departments. |
| 3. Staffing | Recruiting, training, and retaining nursing personnel. | Hiring new nurses and conducting orientation programs. |
| 4. Directing (Leading) | Supervising and guiding nursing teams. | Motivating nurses, ensuring teamwork, and handling conflicts. |
| 5. Controlling | Monitoring performance and ensuring compliance. | Evaluating patient outcomes and staff efficiency. |
Detailed Explanation of Management Functions in Nursing
1. Planning
Definition:
Planning involves setting objectives, developing policies, and forecasting future needs to ensure smooth nursing operations.
Key Aspects:
- Strategic Planning: Long-term planning (e.g., implementing a new electronic health record system).
- Tactical Planning: Short-term objectives (e.g., daily patient care plans).
- Contingency Planning: Preparing for emergencies (e.g., disaster management plans).
✅ Example: A nursing director develops a staffing plan to ensure an adequate nurse-to-patient ratio for better care.
2. Organizing
Definition:
Organizing involves structuring nursing services, defining roles, and ensuring resources are used efficiently.
Key Aspects:
- Task Allocation: Assigning nurses specific duties in ICUs, OPDs, or operation theaters.
- Departmental Coordination: Ensuring smooth collaboration between different units.
- Workflow Optimization: Implementing shift schedules for better workload distribution.
✅ Example: A nursing supervisor assigns nurses to different shifts and units based on patient needs.
3. Staffing
Definition:
Staffing ensures the right personnel are recruited, trained, and retained to provide quality healthcare.
Key Aspects:
- Recruitment & Selection: Hiring competent nurses through exams and interviews.
- Training & Development: Providing ongoing education and workshops.
- Retention Strategies: Preventing staff turnover through incentives and promotions.
✅ Example: A hospital HR team conducts training sessions on infection control for newly hired nurses.
4. Directing (Leading)
Definition:
Directing involves guiding, supervising, and motivating nursing staff to achieve hospital goals.
Key Aspects:
- Effective Communication: Encouraging open dialogue between nurses and administrators.
- Leadership in Nursing: Adopting leadership styles like transformational or democratic leadership.
- Conflict Resolution: Handling disputes and ensuring a positive work environment.
✅ Example: A nurse manager motivates staff during high-pressure situations, such as a pandemic.
5. Controlling
Definition:
Controlling involves monitoring nursing performance, evaluating patient care quality, and implementing corrections when needed.
Key Aspects:
- Quality Assurance: Monitoring patient safety and adherence to clinical protocols.
- Performance Evaluation: Assessing staff efficiency through feedback and audits.
- Compliance Monitoring: Ensuring adherence to healthcare regulations and ethical guidelines.
✅ Example: A nursing director reviews patient safety reports and implements changes to reduce hospital-acquired infections.
Importance of Management Functions in Nursing
- Ensures high-quality patient care through structured workflows.
- Improves staff efficiency and teamwork by defining clear roles.
- Enhances crisis management through effective planning and leadership.
- Reduces medical errors and ensures compliance with healthcare regulations.
The five functions of nursing management—Planning, Organizing, Staffing, Directing, and Controlling—help in delivering efficient, safe, and high-quality nursing care. These functions ensure smooth hospital operations, effective leadership, and better patient outcomes.
Principles of Management in Nursing

Management principles are fundamental guidelines that help nurse managers, hospital administrators, and healthcare professionals to organize, direct, and control healthcare services effectively. These principles ensure efficiency, coordination, quality patient care, and optimal use of resources.
Management in nursing is not just about supervising staff; it involves strategic planning, decision-making, communication, leadership, and problem-solving. The principles of management apply to both clinical care and administrative functions in hospitals, nursing homes, and community healthcare settings.
One of the foundational contributors to management theories, Henri Fayol, introduced 14 Principles of Management, many of which remain relevant in modern nursing services. Additionally, nursing management incorporates patient-centered care, evidence-based practice, ethical decision-making, and teamwork as core principles.
Principles of Management in Nursing
A. Fayol’s 14 Principles of Management in Nursing
Henri Fayol’s 14 Principles of Management are widely applied in hospital administration, nursing leadership, and healthcare service management.
| Principle | Definition | Application in Nursing Management |
|---|---|---|
| 1. Division of Work | Specialization improves efficiency and productivity. | Nurses are assigned specific roles (ICU nurses, surgical nurses, pediatric nurses) to improve expertise. |
| 2. Authority and Responsibility | A balance between authority (power to give orders) and responsibility (accountability for results). | A nurse manager has the authority to assign patient care tasks and is responsible for ensuring they are completed correctly. |
| 3. Discipline | Adherence to rules, ethics, and professional conduct. | Nurses follow hospital protocols for medication administration, infection control, and patient safety. |
| 4. Unity of Command | Each employee should receive orders from only one superior to avoid confusion. | A nurse reports directly to the charge nurse or nursing supervisor, preventing conflicting instructions. |
| 5. Unity of Direction | All efforts should be focused on a common goal for efficiency. | The entire nursing staff works towards improving patient recovery rates and safety standards. |
| 6. Subordination of Individual Interest | The organization’s interests must come before personal interests. | Nurses prioritize patient well-being and hospital efficiency over personal convenience. |
| 7. Remuneration (Fair Compensation) | Employees must be fairly paid for their work to motivate them. | Ensuring competitive salaries, overtime pay, and incentives for nurses to reduce attrition. |
| 8. Centralization and Decentralization | Balance between top-down control and distributed decision-making. | A hospital administrator (centralized authority) sets policies, but nurse managers (decentralized) make day-to-day decisions. |
| 9. Scalar Chain (Hierarchy) | Clear organizational structure with a proper chain of command. | Nursing hierarchy: Chief Nursing Officer → Nurse Manager → Charge Nurse → Staff Nurse. |
| 10. Order | Proper organization of resources and personnel to maintain efficiency. | Maintaining well-organized patient records, medicine storage, and staff scheduling. |
| 11. Equity (Fair Treatment) | All employees should be treated fairly and respectfully. | Ensuring equal opportunities, professional growth, and unbiased treatment for all nurses. |
| 12. Stability of Tenure | Employee retention and long-term stability lead to better performance. | Reducing high nurse turnover rates by offering career progression, training, and job security. |
| 13. Initiative | Encouraging creativity and independent thinking. | Allowing nurses to propose improvements in hospital policies and procedures. |
| 14. Esprit de Corps | Promoting teamwork and unity among employees. | Fostering a collaborative work environment where nurses, doctors, and healthcare staff support one another. |
✅ Example: A hospital’s nursing department implements a patient-centered approach, ensuring that all staff work collectively to enhance patient care, safety, and satisfaction.
B. Additional Principles Specific to Nursing Management
Apart from Fayol’s principles, modern nursing management incorporates healthcare-specific principles:
- Patient-Centered Care
- Nursing management must always prioritize patient needs, safety, and well-being.
- Encouraging compassionate care, cultural sensitivity, and personalized treatment.
✅ Example: Developing individualized nursing care plans based on patient conditions.
- Evidence-Based Practice (EBP)
- All nursing decisions should be based on research, best practices, and clinical guidelines.
✅ Example: Implementing infection control measures based on WHO guidelines.
- All nursing decisions should be based on research, best practices, and clinical guidelines.
- Ethical Decision-Making
- Nursing managers should ensure that ethical considerations and professional codes are upheld.
- Protecting patient rights, confidentiality, and informed consent.
✅ Example: Ensuring ethical handling of end-of-life care decisions.
- Flexibility and Adaptability
- Healthcare is dynamic, and nurses must adapt to new medical technologies, diseases, and patient care needs.
✅ Example: Training nurses to use AI-driven health monitoring systems.
- Healthcare is dynamic, and nurses must adapt to new medical technologies, diseases, and patient care needs.
- Effective Communication
- Ensuring clear, accurate, and timely communication between nurses, doctors, and hospital administrators.
✅ Example: Using electronic health records (EHRs) and interdepartmental communication platforms.
- Ensuring clear, accurate, and timely communication between nurses, doctors, and hospital administrators.
- Leadership in Nursing
- Nurse managers should motivate, inspire, and support their staff to improve performance.
✅ Example: Encouraging mentorship programs for junior nurses.
- Nurse managers should motivate, inspire, and support their staff to improve performance.
- Crisis and Emergency Management
- Preparing nurses for disaster response, pandemics, and medical emergencies.
✅ Example: Creating hospital contingency plans for COVID-19 and natural disasters.
- Preparing nurses for disaster response, pandemics, and medical emergencies.
Importance of Management Principles in Nursing
The application of management principles in nursing leads to better patient care, improved hospital efficiency, and professional growth for nurses. Some key benefits include:
Improved Efficiency – Standardized workflows ensure quick and accurate patient care.
Better Teamwork – Promotes cooperation among nursing staff, doctors, and allied health professionals.
Patient Safety – Ensures compliance with safety protocols, reducing medical errors.
Higher Job Satisfaction – Nurses feel valued, respected, and supported in their roles.
Enhanced Decision-Making – Enables effective leadership, problem-solving, and conflict resolution.
Workforce Stability – Reduces nurse burnout, increasing staff retention rates.
Application of Management Principles in Nursing
| Scenario | Management Principle Applied |
|---|---|
| A nurse manager developing an infection control policy | Unity of Direction & Evidence-Based Practice |
| A hospital rewarding nurses with performance incentives | Remuneration & Motivation |
| A nurse leader encouraging teamwork during emergencies | Esprit de Corps & Crisis Management |
| A nurse supervisor assigning staff based on patient needs | Division of Work & Order |
| A hospital ensuring equal job opportunities for all nurses | Equity & Stability of Tenure |
✅ Example: During COVID-19, hospitals applied Fayol’s principles by ensuring proper staffing (division of work), effective leadership (unity of command), and teamwork (Esprit de Corps).
The principles of management provide a structured approach to handling nursing operations, staff coordination, and patient care delivery. By applying these principles, nurse managers and hospital administrators can improve efficiency, promote teamwork, and ensure high-quality healthcare services.
✅ Key Takeaways:
- Fayol’s 14 Principles of Management help streamline nursing workflows, leadership, and hospital operations.
- Nursing-specific principles like Patient-Centered Care, Evidence-Based Practice, and Ethical Leadership ensure modern, high-quality nursing services.
- Applying management principles improves staff motivation, decision-making, patient safety, and overall healthcare efficiency.
Role of a Nurse as a Manager

A nurse manager plays a critical leadership role in healthcare, ensuring that nursing staff, hospital policies, and patient care function efficiently. In addition to clinical responsibilities, nurse managers oversee planning, organizing, staffing, directing, and controlling within healthcare settings.
Nurse managers work at various levels, including hospital wards, emergency departments, intensive care units (ICUs), nursing homes, community health centers, and healthcare administration offices. Their leadership impacts patient safety, healthcare quality, and staff performance.
Key Roles of a Nurse as a Manager
A nurse manager fulfills multiple roles, balancing administrative duties, leadership, patient care, and team management.
| Role | Responsibilities |
|---|---|
| 1. Leader | Guides nursing teams, sets goals, and motivates staff for better patient care. |
| 2. Planner | Develops staffing plans, workflow schedules, and care strategies. |
| 3. Organizer | Allocates nurses, resources, and facilities efficiently. |
| 4. Communicator | Acts as a bridge between nursing staff, hospital administration, and patients. |
| 5. Supervisor | Monitors patient care, ensures protocol compliance, and conducts performance reviews. |
| 6. Educator | Trains new nurses, provides continuing education, and promotes skill development. |
| 7. Patient Advocate | Ensures patient rights, ethical care, and informed decision-making. |
| 8. Financial Manager | Controls costs, manages budgets, and ensures resource availability. |
| 9. Problem Solver | Resolves conflicts, handles emergencies, and makes quick decisions. |
| 10. Evaluator | Assesses nursing staff efficiency, quality of care, and patient satisfaction. |
✅ Example: A nurse manager in an ICU ensures that all nurses follow infection control measures, maintain proper documentation, and receive ongoing training in critical care management.
Detailed Responsibilities of a Nurse Manager
A nurse manager performs essential functions across multiple domains, ensuring smooth hospital operations.
A. Leadership and Team Management
- Motivates and supports nursing teams for high-quality patient care.
- Sets clear goals, expectations, and performance standards.
- Encourages teamwork, mentorship, and professional growth.
✅ Example: A nurse manager implements peer mentoring programs, pairing senior nurses with new graduates to enhance learning.
B. Planning and Decision-Making
- Develops work schedules, patient care strategies, and hospital workflow plans.
- Implements crisis management protocols for emergencies and disease outbreaks.
- Ensures staffing levels meet patient needs.
✅ Example: A hospital’s emergency department nurse manager allocates more nurses during peak hours to handle critical cases efficiently.
C. Staffing and Human Resource Management
- Recruits, hires, trains, and evaluates nursing personnel.
- Develops competency-based training programs for professional growth.
- Addresses staff concerns, burnout, and work-life balance issues.
✅ Example: In a nursing home, the nurse manager ensures proper nurse-patient ratios to improve elder care services.
D. Quality and Safety Management
- Implements patient safety measures and infection control protocols.
- Ensures adherence to national and international nursing standards (e.g., WHO, INC, ANA).
- Reduces medical errors and enhances patient recovery rates.
✅ Example: A nurse manager in a surgical ward enforces strict hand hygiene protocols to prevent post-operative infections.
E. Financial and Resource Management
- Manages departmental budgets, cost controls, and financial planning.
- Ensures availability of medical equipment, medications, and nursing supplies.
- Works with hospital administrators to optimize resource utilization.
✅ Example: A nurse manager collaborates with hospital finance teams to acquire advanced patient monitoring systems.
F. Communication and Collaboration
- Maintains effective communication between nurses, doctors, and hospital administration.
- Acts as a liaison between hospital management and nursing staff.
- Ensures patients and families understand medical procedures and care plans.
✅ Example: A nurse manager in a maternity ward arranges regular meetings with obstetricians, dietitians, and midwives to improve maternal care.
G. Conflict Resolution and Problem Solving
- Addresses interpersonal conflicts among nurses and healthcare teams.
- Manages patient complaints and staff grievances.
- Ensures a healthy work environment and job satisfaction.
✅ Example: A nurse manager mediates conflicts between senior and junior nurses to maintain a positive workplace culture.
H. Legal and Ethical Responsibilities
- Ensures compliance with nursing ethics, patient confidentiality (HIPAA), and professional standards.
- Manages medico-legal cases and ethical dilemmas in patient care.
- Enforces hospital accreditation requirements and legal policies.
✅ Example: A nurse manager ensures all nurses understand patient rights and handle informed consent properly before procedures.
Levels of Nursing Management
Nurse managers work at different levels depending on their roles and responsibilities.
| Level | Position/Role | Key Responsibilities |
|---|---|---|
| Top-Level Nursing Management | Chief Nursing Officer (CNO), Director of Nursing | – Strategic planning and policy-making.- Hospital-wide nursing leadership.- Financial and regulatory management. |
| Middle-Level Nursing Management | Nurse Supervisors, Ward Managers, Department Heads | – Implementing hospital policies.- Supervising nursing teams.- Ensuring patient care quality. |
| Lower-Level Nursing Management | Charge Nurses, Team Leaders, Senior Staff Nurses | – Direct patient care and bedside nursing.- Monitoring junior staff performance.- Maintaining treatment protocols. |
✅ Example: A Chief Nursing Officer (CNO) develops a national nursing strategy, while a Charge Nurse supervises shift duties.
Challenges Faced by Nurse Managers
Despite their vital role, nurse managers face several challenges in their profession.
A. Workforce Shortages and High Nurse-to-Patient Ratios
- Limited nursing staff increases workload, stress, and burnout.
- Solutions: Improving recruitment, staff incentives, and workload distribution.
B. Stress and Burnout
- Long working hours lead to mental and physical exhaustion.
- Solutions: Implementing mental health support, flexible scheduling, and rest breaks.
C. Ethical and Legal Issues
- Handling patient confidentiality, informed consent, and end-of-life care decisions.
- Solutions: Ensuring staff training in legal and ethical nursing practices.
D. Managing Technological Advancements
- Nurses must adapt to electronic health records (EHRs), AI-driven care, and telemedicine.
- Solutions: Providing continuous training and technology integration workshops.
✅ Example: A nurse manager in a rural clinic trains nurses in telemedicine practices for remote patient care.
Importance of Nurse Managers in Healthcare
- Enhance patient care quality and safety.
- Ensure smooth hospital operations and staff coordination.
- Improve team morale, motivation, and professional development.
- Manage budgets and optimize resource utilization.
- Ensure compliance with legal, ethical, and healthcare regulations.
✅ Example: During the COVID-19 pandemic, nurse managers played a key role in PPE distribution, crisis management, and patient triage.
Nurse managers are leaders, organizers, communicators, and problem-solvers in healthcare. Their role goes beyond bedside care, encompassing staff management, financial planning, crisis response, and quality assurance.
By balancing leadership, administration, and patient-centered care, nurse managers enhance hospital efficiency, improve patient safety, and create a positive work environment for nurses.
✅ Key Takeaways:
- Nurse managers oversee planning, staffing, supervision, budgeting, and policy implementation.
- They ensure high-quality patient care, workplace efficiency, and staff well-being.
- Effective leadership and teamwork in nursing management lead to better healthcare outcomes.
Planning in Nursing

The management process in nursing is a structured approach that ensures efficient delivery of healthcare services, proper staff utilization, and high-quality patient care. It consists of five essential functions:
- Planning – Setting goals and outlining strategies.
- Organizing – Allocating resources and assigning roles.
- Staffing – Recruiting and developing human resources.
- Directing – Leading, motivating, and supervising nursing teams.
- Controlling – Monitoring performance and making improvements.
Among these, planning is the foundational function because it establishes the direction and structure for all other management activities.
Planning in Nursing Management
A. Definition of Planning
Planning is the process of setting objectives, defining strategies, and outlining tasks to achieve specific goals. In nursing, planning involves developing strategies for patient care, workforce management, budgeting, and hospital operations.
Henri Fayol (Father of Modern Management):
“Planning is deciding in advance what to do, how to do it, when to do it, and who is to do it.”
Nursing Management Perspective:
“Planning in nursing is a systematic approach to ensuring high-quality patient care, efficient resource allocation, and smooth hospital operations.”
B. Importance of Planning in Nursing
Planning plays a crucial role in nursing as it ensures preparedness, efficiency, and effective decision-making.
- Improves Patient Care – Ensures timely interventions, treatment protocols, and safety measures.
- Optimizes Resource Allocation – Prevents wastage of manpower, medical supplies, and financial resources.
- Enhances Team Coordination – Defines roles and responsibilities, reducing confusion.
- Ensures Crisis Preparedness – Helps in disaster planning, emergency response, and pandemic management.
- Encourages Evidence-Based Practice (EBP) – Plans are based on scientific research and best practices.
- Aids in Decision-Making – Helps nurse managers set priorities and make informed choices.
C. Types of Planning in Nursing
Planning in nursing management can be classified into different categories based on time frame, scope, and flexibility.
1. Based on Time Frame
| Type | Description | Example in Nursing |
|---|---|---|
| Short-Term Planning | Immediate actions, typically lasting a few days or weeks. | Planning nurse shifts for the upcoming week. |
| Long-Term Planning | Strategic goals spanning years, focusing on hospital growth and nursing advancements. | Expanding nursing education programs and specialized training. |
| Contingency Planning | Preparing for unexpected events such as disasters or pandemics. | Developing COVID-19 or disaster response plans. |
2. Based on Scope and Function
| Type | Description | Example in Nursing |
|---|---|---|
| Strategic Planning | High-level planning involving hospital-wide goals. | Implementing electronic health records (EHRs) in all nursing departments. |
| Tactical Planning | Focuses on departmental or unit-level objectives. | Reducing nurse-patient ratios in ICUs. |
| Operational Planning | Daily and routine planning for smooth hospital functioning. | Assigning nurses to specific patients based on workload. |
3. Based on Flexibility
| Type | Description | Example in Nursing |
|---|---|---|
| Fixed Planning | Structured, well-defined planning with little room for change. | Creating strict infection control policies. |
| Flexible Planning | Allows modifications based on real-time situations. | Adjusting nurse staffing levels based on patient admission rates. |
D. Steps in the Planning Process in Nursing
Planning is a systematic process that includes multiple steps to ensure effectiveness.
| Step | Description | Example in Nursing |
|---|---|---|
| 1. Identifying Goals | Defining the main objective of the plan. | Reducing hospital-acquired infections (HAIs). |
| 2. Data Collection & Analysis | Gathering relevant information to create an informed plan. | Conducting an audit on infection rates in hospital wards. |
| 3. Establishing Priorities | Determining the most important tasks and focusing on them. | Prioritizing hand hygiene training for nurses. |
| 4. Developing Action Plans | Creating specific strategies to achieve objectives. | Implementing handwashing protocols and PPE use. |
| 5. Resource Allocation | Assigning manpower, financial support, and materials. | Ensuring adequate PPE supplies and sanitizers. |
| 6. Implementation | Executing the planned strategies. | Conducting training sessions for nurses on infection control. |
| 7. Evaluation & Feedback | Assessing outcomes and making improvements. | Monitoring infection rate reduction and revising plans if needed. |
✅ Example: A hospital aims to reduce medication errors by 30% in one year. The nurse manager collects error reports, designs training programs, implements electronic prescription systems, and evaluates progress regularly.
E. Challenges in Planning for Nursing Management
Despite its importance, planning faces various challenges in healthcare settings.
- Workforce Shortages – Limited nursing staff affects effective execution.
- Budget Constraints – Financial limitations may restrict access to medical equipment, training, and infrastructure.
- Resistance to Change – Nurses and hospital staff may be hesitant to adopt new policies.
- Unpredictable Healthcare Crises – Pandemics and disasters can disrupt planned activities.
- Lack of Technological Integration – Poor access to healthcare IT systems affects modern planning techniques.
✅ Solution: Nurse managers should adopt flexible, data-driven, and participative planning strategies to overcome these challenges.
Role of Nurse Managers in Planning
Nurse managers are key decision-makers in planning and ensure that nursing services run efficiently.
A. Responsibilities of a Nurse Manager in Planning
- Identifying nursing objectives and setting priorities.
- Coordinating staffing, scheduling, and workload distribution.
- Ensuring compliance with healthcare laws and hospital policies.
- Managing emergency preparedness plans.
- Overseeing budgeting, financial planning, and cost-effective resource use.
- Evaluating patient outcomes and staff performance to revise plans.
✅ Example: A nurse manager in a maternity ward develops a plan to improve postpartum care, ensuring adequate staff, educational resources for mothers, and strict monitoring of newborns.
Importance of Planning in Nursing Leadership
Planning is essential for leadership in nursing as it enhances efficiency, decision-making, and patient safety.
- Ensures smooth hospital operations by defining responsibilities.
- Improves crisis management in disaster or pandemic situations.
- Enhances team coordination by structuring work shifts and patient assignments.
- Reduces medical errors by enforcing evidence-based protocols.
- Facilitates career development by ensuring staff training programs.
Summary
Planning is the backbone of nursing management, setting the stage for efficient patient care, effective resource utilization, and organizational success. By implementing structured, evidence-based, and flexible planning strategies, nurse managers can improve healthcare outcomes, enhance team performance, and ensure long-term hospital growth.
✅ Key Takeaways:
- Planning in nursing establishes goals, organizes resources, and prepares for challenges.
- It can be short-term, long-term, strategic, operational, or contingency-based.
- Effective planning leads to better patient care, optimized staffing, and crisis preparedness.
- Nurse managers play a vital role in executing and refining healthcare plans.
Organizing in Nursing

Organizing is one of the key functions of management that ensures the efficient use of resources, clear role allocation, and smooth workflow in healthcare settings. In nursing management, organizing involves structuring nursing teams, assigning responsibilities, and optimizing patient care delivery.
A well-organized nursing department ensures better coordination, reduced errors, and improved patient safety. It is a fundamental process that connects planning to execution, ensuring that goals set during the planning stage are properly implemented.
Definition of Organizing in Nursing Management
Henri Fayol (Father of Modern Management):
“To organize is to bring together the physical, financial, and human resources and arrange them in a way to achieve goals.”
Healthcare Perspective:
“Organizing in nursing involves structuring healthcare services, allocating duties, and ensuring seamless teamwork to enhance patient care and hospital efficiency.”
Importance of Organizing in Nursing
Organizing is essential for effective healthcare management and ensures smooth hospital operations.
- Enhances Efficiency – Proper distribution of duties reduces workload stress and duplication of tasks.
- Improves Patient Care – Ensures continuous monitoring, better response time, and quality nursing services.
- Defines Roles and Responsibilities – Prevents confusion among nursing staff and enhances accountability.
- Facilitates Teamwork and Communication – Ensures smooth interaction between nurses, doctors, and support staff.
- Optimizes Resource Utilization – Avoids wastage of time, manpower, and medical supplies.
- Improves Decision-Making – Helps nurse managers make informed choices regarding staff assignments and patient care priorities.
✅ Example: In an ICU, organizing ensures that specialized nurses handle critical cases, patient monitoring follows a structured approach, and emergency protocols are in place.
Principles of Organizing in Nursing Management
The organizing function follows certain principles that ensure structured healthcare operations.
| Principle | Definition | Application in Nursing |
|---|---|---|
| 1. Unity of Objective | All staff should work towards a common goal. | Ensuring zero patient falls in a hospital ward. |
| 2. Division of Work | Specialization increases efficiency. | Assigning nurses based on expertise (ICU, maternity, pediatric care, etc.). |
| 3. Chain of Command | There should be a clear reporting hierarchy. | Staff nurses report to charge nurses, who report to nurse managers. |
| 4. Span of Control | A manager should only oversee a reasonable number of staff. | A nurse manager supervises 6-8 nurses in a ward for effective management. |
| 5. Coordination | Different departments should work together. | Nurses, doctors, and physiotherapists collaborate for post-surgical patient care. |
| 6. Flexibility | The structure should adapt to changing healthcare needs. | Modifying staffing patterns during a pandemic to accommodate more patients. |
| 7. Authority and Responsibility | Authority should be matched with accountability. | A nurse in charge of medication rounds is responsible for accuracy. |
✅ Example: In an Emergency Department (ED), nurses, paramedics, and doctors work under an organized triage system, ensuring patients with critical conditions receive immediate care while non-critical cases are handled systematically.
Steps in the Organizing Process in Nursing
Organizing in nursing follows a structured approach to ensure optimal patient care and efficient hospital management.
| Step | Description | Example in Nursing |
|---|---|---|
| 1. Identifying Objectives | Defining goals for patient care and nursing efficiency. | Reducing hospital-acquired infections (HAIs). |
| 2. Analyzing Activities | Identifying key nursing functions and dividing them into manageable tasks. | Assigning nurses for medication administration, wound care, and patient education. |
| 3. Classifying Roles and Responsibilities | Grouping tasks based on departments and expertise. | Creating teams for ICU, OPD, surgical wards, and maternity care. |
| 4. Delegating Authority | Assigning decision-making powers to appropriate personnel. | Charge nurses handle staff allocation, while senior nurses supervise clinical procedures. |
| 5. Coordination and Communication | Ensuring smooth interaction between departments. | Regular meetings between nurses, doctors, and hospital administration. |
| 6. Monitoring and Evaluation | Assessing staff performance and making improvements. | Reviewing nurse-patient ratios and adjusting shifts accordingly. |
✅ Example: A nurse manager in a surgical ward organizes the team by assigning pre-op nurses, post-op recovery nurses, and wound care nurses to ensure smooth patient transitions.
Types of Organizational Structures in Nursing
Different hospitals use various organizational models based on their size, staffing, and patient care needs.
| Type | Description | Example in Nursing |
|---|---|---|
| 1. Hierarchical Structure | A top-down system with clear reporting lines. | A Chief Nursing Officer (CNO) → Nurse Supervisor → Charge Nurse → Staff Nurse. |
| 2. Functional Structure | Nurses are divided based on specialization. | Separate teams for ICU, pediatric, and surgical wards. |
| 3. Matrix Structure | Combines both hierarchical and team-based structures. | A nurse may report to both a department head and a project manager. |
| 4. Flat Structure | Minimal management levels with more autonomy for nurses. | Community health nursing teams working independently. |
✅ Example: A multi-specialty hospital may have a functional structure where nurses are divided into specific departments like Oncology, Cardiology, and Neonatal Care.
Challenges in Organizing Nursing Services
Despite its importance, organizing in nursing faces several challenges.
A. Common Challenges
- Staff Shortages – Affects proper division of work and workload balance.
- Poor Communication – Leads to errors in patient care and inefficient teamwork.
- Lack of Coordination – Departments may work in silos, causing delays in patient treatment.
- Rigid Structures – Inflexible hospital policies limit adaptability in emergencies.
- Technology Gaps – Lack of hospital management software affects organization.
B. Solutions to Overcome Challenges
- Optimize Staffing – Maintain proper nurse-patient ratios to reduce workload stress.
- Improve Communication Channels – Use electronic health records (EHRs) and interdisciplinary team meetings.
- Encourage Cross-Training – Train nurses to handle multiple roles for better adaptability.
- Implement Flexible Work Schedules – Adjust shift timings based on hospital needs.
- Use Technology for Resource Management – Adopt nursing informatics systems.
✅ Example: A hospital facing staff shortages during a pandemic cross-trains nurses to work in multiple departments, ensuring continuity of patient care.
Role of Nurse Managers in Organizing
Nurse managers play a critical role in organizing healthcare teams and operations.
A. Key Responsibilities of Nurse Managers in Organizing
- Assigning nursing staff to different departments based on their expertise.
- Ensuring proper resource allocation (manpower, equipment, and medical supplies).
- Developing shift schedules to maintain adequate coverage.
- Coordinating with doctors, administrators, and allied healthcare professionals.
- Implementing technology-driven organization methods (EHRs, hospital workflow software).
✅ Example: A nurse manager in an oncology unit organizes staff by designating chemotherapy nurses, patient education nurses, and post-treatment care specialists.
Organizing is a vital function in nursing management that ensures proper structuring, staffing, and workflow optimization. An effective organizational system enhances patient safety, improves team coordination, and maximizes efficiency in healthcare delivery.
✅ Key Takeaways:
- Organizing connects planning to execution in nursing management.
- It ensures clear role allocation, teamwork, and smooth hospital operations.
- Different organizational structures (hierarchical, functional, matrix, flat) exist in nursing.
- Nurse managers play a key role in organizing staff, schedules, and resources.
Staffing in Nursing

Staffing is one of the core functions of nursing management, ensuring that the right number of nurses with the right skills are available to provide high-quality patient care. It is a continuous process that involves recruitment, selection, training, development, deployment, and retention of nursing personnel.
Proper staffing ensures efficient workload distribution, prevents burnout, enhances patient safety, and improves overall healthcare service delivery. Nurse managers play a crucial role in workforce planning, maintaining nurse-patient ratios, and ensuring a competent nursing team.
Definition of Staffing in Nursing Management
Koontz & O’Donnell (Management Theorists):
“Staffing is the process of acquiring, developing, and retaining human resources to achieve organizational goals.”
Healthcare Perspective:
“Staffing in nursing ensures that qualified nurses are recruited, trained, assigned, and retained to meet patient care needs efficiently.”
Importance of Staffing in Nursing
Effective staffing ensures smooth hospital operations, patient satisfaction, and staff well-being.
- Ensures Quality Patient Care – Proper staffing levels prevent medical errors and delays in care.
- Reduces Nurse Burnout – Prevents overwork and stress by maintaining balanced workloads.
- Maintains Legal Compliance – Meets mandatory nurse-patient ratio regulations.
- Enhances Efficiency – Ensures timely and coordinated healthcare delivery.
- Increases Job Satisfaction – Retains qualified and motivated nurses.
- Facilitates Crisis Management – Prepares for emergencies, pandemics, and disaster response.
✅ Example: In an ICU, maintaining a nurse-to-patient ratio of 1:1 ensures intensive monitoring and better patient outcomes.
Principles of Staffing in Nursing
Staffing must follow certain principles to ensure efficiency and fairness.
| Principle | Description | Application in Nursing |
|---|---|---|
| 1. Right Number of Nurses | The correct number of staff should be available. | Ensuring 1:5 nurse-patient ratio in general wards. |
| 2. Right Skill Mix | A combination of experienced and junior nurses ensures balanced care. | Assigning senior nurses for critical care and junior nurses for routine tasks. |
| 3. Flexibility in Scheduling | Staff schedules should adapt to patient needs. | Increasing staffing during peak admission periods. |
| 4. Continuous Training | Nurses should receive ongoing education to stay updated. | Conducting monthly CPR and emergency response workshops. |
| 5. Legal and Ethical Compliance | Staffing must follow healthcare laws and ethical guidelines. | Adhering to government-mandated nurse-patient ratios. |
| 6. Employee Welfare | Ensuring nurses have a balanced workload and career growth. | Providing rest breaks, career promotions, and incentives. |
✅ Example: A nurse manager schedules more nurses during flu season to handle higher patient loads.
Steps in the Staffing Process in Nursing
The staffing process includes several key steps to ensure the selection and development of a competent nursing workforce.
| Step | Description | Example in Nursing |
|---|---|---|
| 1. Manpower Planning | Assessing staffing needs based on patient load and hospital policies. | Reviewing bed occupancy rates and workload distribution. |
| 2. Recruitment | Attracting potential candidates through job postings and referrals. | Hiring nurses through campus placements and job fairs. |
| 3. Selection | Evaluating applicants through exams, interviews, and background checks. | Conducting practical skill tests for ICU nursing candidates. |
| 4. Placement & Orientation | Assigning nurses to departments and providing hospital orientation. | Conducting a one-week onboarding program for new recruits. |
| 5. Training & Development | Enhancing skills through workshops, simulations, and certifications. | Organizing monthly infection control training. |
| 6. Performance Evaluation | Assessing staff efficiency through feedback and appraisals. | Conducting yearly performance reviews and patient feedback analysis. |
| 7. Retention & Career Progression | Providing promotions, incentives, and professional growth opportunities. | Offering higher education sponsorships for advanced nursing roles. |
✅ Example: A hospital with high patient volume implements a recruitment drive for emergency nurses and trains them through simulation-based learning.
Nurse-Patient Ratio Standards
Maintaining the correct nurse-to-patient ratio is crucial for patient safety and nurse well-being.
| Healthcare Setting | Recommended Nurse-Patient Ratio |
|---|---|
| ICU | 1:1 |
| General Ward | 1:5 |
| Emergency Department | 1:4 |
| Maternity Ward | 1:3 |
| Pediatric Unit | 1:4 |
✅ Example: A nurse-patient ratio of 1:1 in ICUs allows continuous monitoring of critically ill patients.
Challenges in Nursing Staffing
Despite its importance, staffing faces several challenges in healthcare settings.
A. Common Challenges
- Nurse Shortages – Many hospitals face a lack of qualified nurses.
- High Workload & Burnout – Excessive patient loads lead to stress and job dissatisfaction.
- Budget Constraints – Limited funds restrict recruitment and training programs.
- Irregular Shifts & Overtime – Leads to physical and mental exhaustion.
- Staff Retention Issues – Many nurses migrate abroad for better salaries.
B. Solutions to Overcome Staffing Challenges
- Recruit More Nurses – Government and hospitals should increase hiring efforts.
- Improve Work-Life Balance – Implement fixed shifts and sufficient rest periods.
- Offer Competitive Salaries – Higher pay improves job retention.
- Promote Career Growth – Providing training and specialization opportunities.
- Use Technology for Scheduling – Automated shift planners can optimize workforce allocation.
✅ Example: A hospital facing high nurse turnover introduces incentives, flexible scheduling, and wellness programs to retain staff.
Role of Nurse Managers in Staffing
Nurse managers play a key role in staffing by ensuring hospitals maintain adequate and competent nursing teams.
A. Responsibilities of a Nurse Manager in Staffing
- Assessing staffing needs based on patient volume and healthcare demand.
- Coordinating recruitment, interviews, and hiring processes.
- Ensuring proper nurse-patient ratios for effective workload distribution.
- Developing training programs to improve staff skills.
- Managing nurse scheduling and shift allocations.
- Addressing staff grievances, burnout, and job satisfaction issues.
✅ Example: A nurse manager in a surgical unit ensures proper staffing before major operations by scheduling extra nurses for post-operative care.
Importance of Technology in Staffing
Technology can improve nurse staffing efficiency by automating processes and predicting workforce needs.
A. Tech-Based Solutions for Nurse Staffing
- Electronic Health Records (EHRs): Monitor patient data and predict workload.
- Automated Shift Scheduling: Software tools optimize nurse scheduling.
- AI-Powered Predictive Analytics: Forecast staffing needs based on patient admissions.
- Telehealth & Remote Monitoring: Reduce workload by managing non-critical patients remotely.
✅ Example: A hospital uses AI-based scheduling software to ensure balanced nurse workloads.
Staffing is a crucial management function that ensures hospitals maintain a well-trained, adequately staffed nursing workforce. Proper staffing enhances patient care, reduces nurse burnout, and optimizes hospital efficiency.
✅ Key Takeaways:
- Staffing involves recruitment, training, scheduling, and retention of nurses.
- Maintaining proper nurse-patient ratios improves patient care and staff well-being.
- Nurse managers play a critical role in workforce planning and job satisfaction.
- Technology can enhance staffing efficiency through AI-based scheduling and predictive workforce planning.
Directing/Leading in Nursing

Directing (also known as Leading) is a critical management function in nursing that focuses on guiding, motivating, supervising, and influencing nursing staff to achieve healthcare goals effectively. It ensures that nurses perform their roles efficiently, professionally, and ethically, leading to improved patient care, teamwork, and organizational success.
Effective leadership in nursing is not just about giving orders but involves inspiring, mentoring, and empowering nurses to provide the best possible care.
Definition of Directing/Leading in Nursing
Henri Fayol (Father of Modern Management):
“Directing means influencing people so that they contribute to organizational and group goals.”
American Nurses Association (ANA):
“Nursing leadership is the ability to inspire and guide individuals or groups to achieve common healthcare objectives through motivation, communication, and ethical decision-making.”
Healthcare Perspective:
“Directing in nursing involves providing clear instructions, setting expectations, and motivating nursing staff to deliver high-quality patient care while fostering teamwork and professional growth.”
Importance of Directing/Leading in Nursing
Effective directing (or leadership) is essential in healthcare settings to maintain efficiency, ensure patient safety, and improve nurse satisfaction.
- Enhances Patient Care Quality – Ensures proper supervision and adherence to healthcare protocols.
- Improves Nurse Motivation & Job Satisfaction – Encourages a positive work environment and team collaboration.
- Facilitates Effective Communication – Reduces misunderstandings and promotes teamwork.
- Encourages Innovation & Problem-Solving – Inspires nurses to develop new strategies for patient care improvement.
- Reduces Workplace Conflicts – Promotes teamwork, fairness, and professionalism.
- Strengthens Decision-Making Abilities – Empowers nurses to take initiative in critical situations.
- Ensures Ethical and Professional Nursing Practices – Guides nurses in maintaining ethical standards and legal compliance.
✅ Example: A nurse manager in an ICU ensures that all nurses understand emergency protocols, communicate effectively, and work together under pressure to provide the best critical care.
Principles of Directing/Leading in Nursing
The principles of directing in nursing focus on effective supervision, clear communication, and motivation.
| Principle | Description | Application in Nursing |
|---|---|---|
| 1. Principle of Leadership | A leader should guide, inspire, and empower the team. | Encouraging senior nurses to mentor junior nurses. |
| 2. Principle of Communication | Clear and open communication enhances teamwork. | Conducting daily shift handovers to update patient progress. |
| 3. Principle of Motivation | Staff should be encouraged through rewards and recognition. | Recognizing nurses’ hard work with “Nurse of the Month” awards. |
| 4. Principle of Unity of Command | A nurse should receive instructions from one immediate supervisor to avoid confusion. | A charge nurse gives directions to staff nurses without conflicting orders. |
| 5. Principle of Participation | Involving nurses in decision-making improves engagement. | Allowing nurses to suggest improvements in hospital policies. |
| 6. Principle of Supervision | Continuous monitoring ensures quality control. | A nurse manager evaluates staff performance through regular audits. |
| 7. Principle of Follow-Up | Leaders should check if instructions are properly implemented. | A ward supervisor ensures nurses follow infection control protocols. |
✅ Example: A nurse leader in a maternity ward ensures that staff follows safe childbirth protocols, communicates well with mothers, and provides compassionate care.
Elements of Directing/Leading in Nursing
Effective directing in nursing involves four key elements:
| Element | Description | Example in Nursing |
|---|---|---|
| 1. Supervision | Continuous guidance and monitoring of nursing staff. | A nurse manager oversees medication administration rounds. |
| 2. Motivation | Encouraging nurses through incentives and career growth. | Providing scholarships for nurses to pursue higher education. |
| 3. Communication | Ensuring clear, transparent interaction among healthcare teams. | Holding daily briefings to discuss patient cases. |
| 4. Leadership | Inspiring and influencing nurses to excel. | A senior nurse setting an example through excellent bedside manners. |
✅ Example: A nurse director ensures proper communication between departments, avoiding confusion in critical patient transfers.
Leadership Styles in Nursing
Nurse managers and administrators adopt different leadership styles based on the situation and team dynamics.
| Leadership Style | Characteristics | Example in Nursing |
|---|---|---|
| 1. Autocratic Leadership | Strict control, quick decision-making, minimal staff involvement. | Used in emergency situations like cardiac arrests. |
| 2. Democratic Leadership | Encourages team participation and shared decision-making. | Nurses collaborate on developing new patient care guidelines. |
| 3. Transformational Leadership | Inspires nurses to grow, innovate, and excel. | Encouraging evidence-based nursing practices. |
| 4. Laissez-Faire Leadership | Minimal supervision, trusts nurses to make decisions independently. | Used in experienced research teams. |
| 5. Transactional Leadership | Focuses on structure, rewards, and discipline. | Giving bonuses for excellent performance in nursing care. |
✅ Example: During a mass casualty event, an autocratic leadership style is effective, while a democratic approach is useful for routine hospital decision-making.
Steps in Directing/Leading in Nursing
Effective directing in nursing follows a systematic approach to ensure clear guidance and motivation.
| Step | Description | Example in Nursing |
|---|---|---|
| 1. Setting Objectives | Defining clear goals for patient care and nursing efficiency. | Aiming for zero medication errors in a month. |
| 2. Assigning Responsibilities | Delegating tasks based on nurse expertise. | Assigning ICU-trained nurses to critical cases. |
| 3. Providing Guidance | Giving instructions and feedback to staff. | A nurse manager explains new patient monitoring guidelines. |
| 4. Motivating Staff | Using rewards, encouragement, and career growth plans. | Organizing team-building activities for nurses. |
| 5. Monitoring and Evaluating | Assessing nurse performance and making improvements. | Conducting monthly patient satisfaction surveys. |
✅ Example: A nurse supervisor in an oncology unit motivates nurses by recognizing their efforts in providing compassionate care to terminally ill patients.
Challenges in Directing/Leading in Nursing
Despite its importance, directing faces several challenges in healthcare settings.
- Staff Resistance to Change – Some nurses hesitate to adopt new protocols.
- Communication Barriers – Miscommunication affects teamwork and patient safety.
- High Workload and Burnout – Overworked nurses struggle to stay motivated.
- Lack of Leadership Training – Many nurses lack formal leadership skills.
- Ethical Dilemmas in Decision-Making – Leaders must navigate complex patient rights issues.
✅ Solution: Providing leadership training, mentorship programs, and stress management initiatives.
Role of Nurse Managers in Directing
Nurse managers play a critical role in leadership by:
- Providing clear instructions and maintaining team discipline.
- Resolving conflicts and fostering a positive work environment.
- Ensuring open communication between staff and administration.
- Encouraging continuous learning and professional growth.
- Making quick, informed decisions during emergencies.
✅ Example: A nurse director implements leadership workshops to train junior nurses in effective decision-making
Directing (or leading) is a vital function of nursing management that ensures efficient team coordination, effective communication, and high-quality patient care. A strong leader inspires, motivates, and empowers nurses, leading to better healthcare outcomes and professional growth.
Key Takeaways:
- Leadership in nursing enhances patient safety, teamwork, and motivation.
- Effective communication and motivation are key elements of directing.
- Different leadership styles (autocratic, democratic, transformational) are used in nursing.
- Nurse managers play a crucial role in guiding and supervising nursing teams.
Controlling in Nursing

Controlling is a fundamental function of nursing management that ensures healthcare services are delivered as planned, policies are followed, and patient care meets quality standards. It involves monitoring, evaluating, and taking corrective actions to improve nursing performance, patient safety, and overall healthcare efficiency.
Effective controlling helps nurse managers maintain high-quality care, compliance with healthcare regulations, and efficient hospital operations.
Definition of Controlling in Nursing Management
Henri Fayol (Father of Modern Management):
“Controlling is ensuring that activities conform to plans, policies, and instructions to achieve objectives.”
Koontz & O’Donnell:
“Control is the process of measuring actual performance against the set standards and taking corrective action when needed.”
Nursing Perspective:
“Controlling in nursing involves monitoring staff performance, ensuring adherence to hospital protocols, and making necessary adjustments to improve patient care and organizational efficiency.”
✅ Example: A nurse supervisor checks medication administration records to ensure that all nurses follow correct dosage protocols and documentation procedures.
Importance of Controlling in Nursing
Controlling is essential for maintaining efficiency, accountability, and patient safety in healthcare settings.
- Ensures Quality Care – Monitors nursing performance and adherence to protocols.
- Reduces Medical Errors – Prevents medication errors, patient mismanagement, and procedural mistakes.
- Improves Resource Utilization – Ensures optimal staffing, equipment use, and budget management.
- Enhances Patient Safety – Maintains infection control measures and emergency response preparedness.
- Increases Staff Accountability – Encourages nurses to follow ethical and professional standards.
- Facilitates Decision-Making – Provides data for making informed improvements in nursing practice.
✅ Example: A hospital uses patient satisfaction surveys to assess and improve nursing care quality.
Principles of Controlling in Nursing
The controlling function is based on key principles that ensure systematic performance monitoring.
| Principle | Description | Application in Nursing |
|---|---|---|
| 1. Setting Standards | Define benchmarks for performance. | Aiming for zero hospital-acquired infections (HAIs). |
| 2. Measuring Performance | Monitor nursing efficiency and compliance. | Conducting monthly audits on patient care documentation. |
| 3. Comparing Results with Standards | Identify gaps between expected and actual performance. | Checking nurse-patient ratio compliance in different wards. |
| 4. Corrective Actions | Take steps to improve deficiencies. | Conducting training sessions on infection control if hygiene standards are not met. |
| 5. Feedback Mechanism | Regular feedback improves nursing efficiency. | Implementing patient feedback surveys for service evaluation. |
✅ Example: A hospital implements a checklist system to ensure nurses follow hand hygiene protocols before and after patient care.
Steps in the Controlling Process in Nursing
Controlling in nursing follows a structured approach to identify areas of improvement and maintain high-quality care.
| Step | Description | Example in Nursing |
|---|---|---|
| 1. Setting Performance Standards | Establishing clear objectives and expected outcomes. | Ensuring all patients receive pain assessment every 4 hours. |
| 2. Measuring Actual Performance | Monitoring staff work and collecting performance data. | Reviewing electronic health records (EHRs) for timely documentation. |
| 3. Comparing Performance with Standards | Identifying gaps between desired and actual performance. | Checking if patient discharge times meet the hospital’s 6-hour policy. |
| 4. Identifying Causes of Deviation | Analyzing why standards are not met. | Investigating why medication errors increased in a specific ward. |
| 5. Taking Corrective Actions | Implementing solutions to resolve issues. | Providing extra medication safety training for nurses. |
| 6. Continuous Monitoring | Regular follow-up ensures improvements are sustained. | Conducting quarterly reviews on patient fall incidents. |
✅ Example: A hospital’s quality control team analyzes nurse-patient communication errors and implements an active listening workshop to enhance communication.
Types of Controlling in Nursing
There are different types of control measures used in nursing management to ensure smooth hospital operations.
| Type | Description | Example in Nursing |
|---|---|---|
| 1. Preventive Control | Prevents problems before they occur. | Training nurses in infection control before an outbreak. |
| 2. Concurrent Control | Monitors performance in real-time. | Supervising medication administration rounds. |
| 3. Corrective Control | Implements actions after a problem is detected. | Revising emergency response protocols after a patient safety review. |
| 4. Internal Control | Self-monitoring by employees. | Nurses conducting double-checks on patient prescriptions. |
| 5. External Control | Regulations imposed by external bodies. | Compliance with Joint Commission International (JCI) or WHO guidelines. |
✅ Example: A hospital conducts regular fire safety drills as part of preventive control to ensure staff readiness in emergencies.
Challenges in Nursing Control Processes
Despite its importance, controlling in nursing faces several challenges.
- Resistance to Change – Nurses may hesitate to adopt new protocols.
- High Workload – Increased monitoring adds extra responsibilities to nurses.
- Limited Resources – Some hospitals lack technology for proper tracking.
- Data Accuracy Issues – Errors in record-keeping affect performance measurement.
- Lack of Leadership Support – Weak leadership reduces enforcement of standards.
✅ Solution: Hospitals should use digital monitoring tools, offer leadership training, and ensure fair evaluation systems.
Role of Nurse Managers in Controlling
Nurse managers play a crucial role in implementing control measures to maintain high standards of nursing care.
A. Key Responsibilities of Nurse Managers in Controlling
- Ensuring compliance with healthcare regulations and hospital policies.
- Monitoring nurse performance and providing constructive feedback.
- Identifying gaps in patient care and implementing corrective actions.
- Ensuring staff adherence to safety protocols and infection control guidelines.
- Managing hospital resources to prevent misuse or shortages.
- Maintaining accurate documentation and auditing nursing records.
✅ Example: A nurse manager conducts weekly rounds to ensure proper pain management protocols are followed.
Use of Technology in Nursing Control
Technology plays a vital role in improving control mechanisms in healthcare settings.
| Technology | Purpose |
|---|---|
| Electronic Health Records (EHRs) | Tracks patient data and nursing documentation. |
| Real-Time Monitoring Systems | Provides live updates on patient conditions. |
| Automated Medication Systems | Reduces medication administration errors. |
| Artificial Intelligence (AI) Analytics | Predicts staffing needs and patient risk factors. |
✅ Example: A hospital uses AI-powered predictive analytics to identify units experiencing high patient fall rates, leading to targeted interventions
Controlling is a vital nursing management function that ensures quality care, regulatory compliance, and efficiency in healthcare settings. It allows nurse managers to monitor staff performance, correct deficiencies, and enhance patient safety.
Key Takeaways:
- Controlling in nursing ensures high-quality patient care and staff accountability.
- It involves setting standards, measuring performance, identifying gaps, and taking corrective actions.
- Different types of control (preventive, concurrent, corrective) are used in hospitals.
- Nurse managers play a crucial role in supervising and improving nursing practices.
- Technology enhances nursing control by improving data accuracy and monitoring systems.