Microbiology and infection control-April-2025- (done)-Juhi-UPLOAD
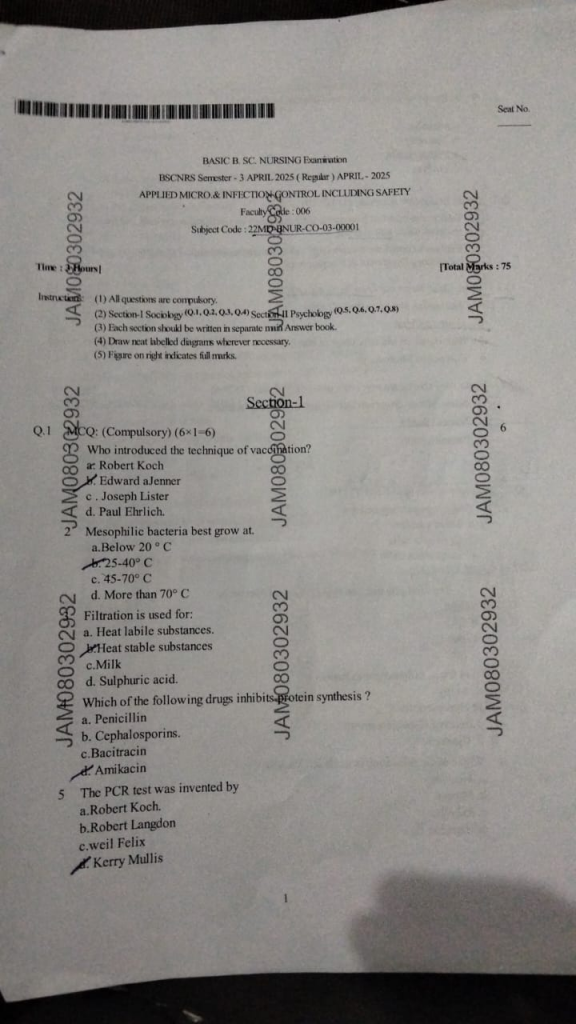
Section-1
Q.1 MCQ: (Compulsory) (6×1-6)
1.Who introduced the technique of vaccination?
a: Robert Koch
b.Edward a Jenner
c. Joseph Lister
d. Paul Ehrlich.
2.Mesophilic bacteria best grow at.
a.Below 20°C
b. 25-40° C
c. 45-70° C
d. More than 70° C
3.Filtration is used for:
a. Heat labile substances.
b.Heat stable substances
c. Milk
d. Sulphuric acid.
4.Which of the following drugs inhibits protein synthesis ?
a. Penicillin
b. Cephalosporins.
c. Bacitracin
d.Amikacin
5 The PCR test was invented by
a. Robert Koch.
b.Robert Langdon
c.weil Felix
d.Kerry Mullis
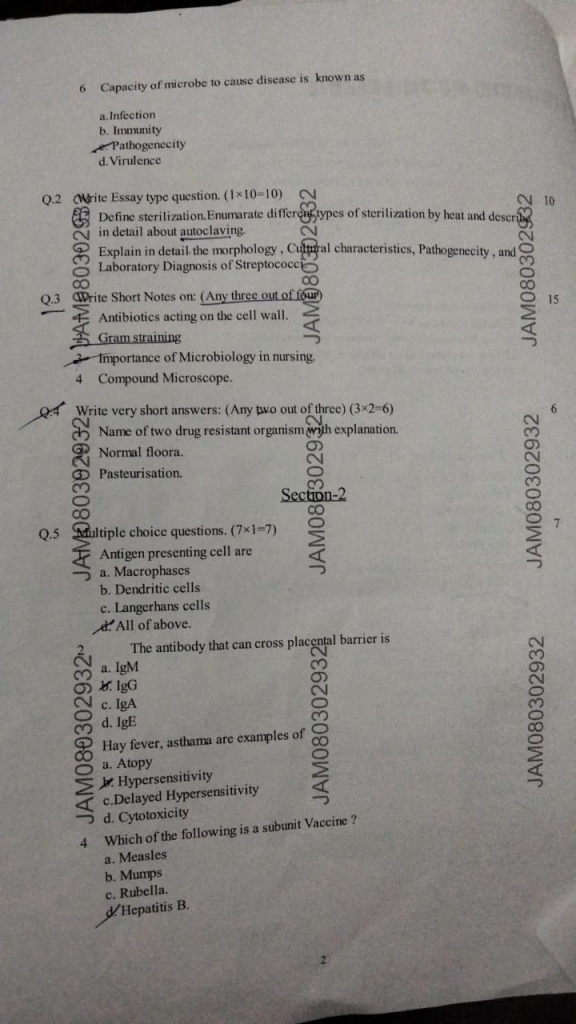
6. Capacity of microbe to cause disease is known as
a.Infection
b. Immunity
c.Pathogenecity
d. Virulence
Q.2 (Write Essay type question. (1×10-10)
1.Define sterilization. Enumarate different types of sterilization by heat and describe in detail about autoclaving
Sterilization :
Sterilization is the process of eliminating or destroying all forms of microbial life, including bacteria, viruses, fungi, and spores, from a surface, object, or fluid. It is an absolute method, meaning the item is either completely sterile or not sterile at all.
Enumeration of different types of sterilization by heat
Sterilization by heat is broadly classified into two types :
1. Moist Heat Sterilization (With Steam/Water)
Uses steam or water vapor under specific conditions to kill microorganisms by protein coagulation and denaturation.
Types
Autoclaving
121°C, 15 psi, 15–20 minutes
Used for surgical instruments, dressing, glassware, culture media
Boiling
100°C for 10–30 minutes
Not reliable for spores; used for disinfecting instruments at home
Pasteurization
63°C for 30 minutes (holder method)
72°C for 15 seconds (flash method)
Used for milk and dairy products
Tyndallization (Intermittent Sterilization)
100°C for 30 minutes on 3 consecutive days
Used for culture media with heat-sensitive components
Inspissation
75–80°C for 30 minutes on 3 successive days
Used to sterilize egg-based media (e.g., Loeffler’s serum)
2. Dry Heat Sterilization (Without Steam/Water)
Uses high temperature dry air to kill microorganisms by oxidation of cell contents.
Types
Hot Air Oven
160°C for 2 hours or 170°C for 1 hour
Used for glassware, metal instruments, powders, oils
Incineration
Burning at very high temperatures (>800°C)
Used to destroy hospital waste, infected materials
Flaming
Passing object through direct flame (e.g., Bunsen burner)
Used for inoculating loops, scalpel blades
Autoclaving
Autoclaving is a method of sterilization that uses moist heat under pressure to destroy all forms of microbial life, including bacteria, viruses, fungi, and bacterial spores. It is considered one of the most reliable and widely used methods of sterilization in medical, microbiological, and research settings.
Principle of Autoclaving :
The principle of autoclaving is based on the fact that when steam is applied under pressure, the boiling point of water increases, allowing the steam to reach higher temperatures. This moist heat causes coagulation and denaturation of microbial proteins, leading to complete sterilization.
Standard Conditions for Autoclaving :
Temperature: 121°C
Pressure: 15 pounds per square inch (psi)
Time: 15 to 20 minutes
For flash sterilization (rapid sterilization), higher temperatures (e.g., 134°C) and shorter time (3–5 minutes) are used.
Types of Autoclaves :
Gravity Displacement Autoclave – Steam displaces air by gravity.
Pre-vacuum Autoclave – Air is removed before steam is introduced, allowing better penetration.
High-speed Autoclave – Used for rapid sterilization of instruments (also called flash autoclave).
Uses of Autoclaving :
Sterilization of surgical instruments
Sterilization of glassware, dressings, rubber items
Preparation of culture media
Disposal of laboratory waste and contaminated materials
Autoclaving Procedure :
Preparation : Clean and arrange items to be sterilized.
Loading : Load items in the autoclave chamber properly, ensuring steam can circulate.
Setting Parameters : Set the required temperature, pressure, and time.
Sterilization : Start the autoclave cycle. Steam is generated and maintained under pressure.
Cooling : After the cycle, allow pressure to release and items to cool before removal.
Unloading : Carefully remove items with sterile gloves when safe.
Sterilization Indicators :
Chemical Indicators : Color-changing autoclave tapes or strips.
Biological Indicators : Use of heat-resistant spores (e.g., Geobacillus stearothermophilus) to confirm sterilization.
Mechanical Indicators : Monitors for time, temperature, and pressure during the cycle.
Advantages :
Very effective against all types of microorganisms
Economical and safe for many types of materials
Environmentally friendly (no harmful chemicals)
Disadvantages :
Not suitable for heat-sensitive or moisture-sensitive items
May cause corrosion of certain instruments if not dried properly
Requires proper training for operation and monitoring
2.Explain in detail the morphology, Cultural characteristics, Pathogenecity, and Laboratory Diagnosis of Streptococc
Morphology
Morphology is the branch of biology that deals with the form and structure of organisms and their specific structural features, including size, shape, structure, and appearance of an organism or its parts.
Types of Morphology
External Morphology (Eidonomy) :
Study of outer features of organisms like shape, color, limbs, wings, etc.
Example: Beak shape in birds, body segments in insects.
Internal Morphology (Anatomy) :
Study of internal structures such as organs, bones, and tissues.
Example: Structure of heart, lungs, kidneys, etc.
In Microbiology :
In microbiology, morphology refers to the shape and arrangement of microorganisms, particularly bacteria.
Bacterial Shapes :
Coccus (spherical)
Example : Streptococcus, Staphylococcus
Bacillus (rod-shaped)
Example : Escherichia coli
Spirillum (spiral-shaped)
Example : Spirillum minus
Vibrio (comma-shaped)
Example : Vibrio cholerae
Bacterial Arrangements :
Diplococci – pairs
Streptococci – chains
Staphylococci – clusters
Tetrads – groups of four
Sarcinae – cube-like groups of eight
In Botany :
Morphology studies parts of the plant like:
Root (tap root, fibrous root)
Stem (aerial, underground)
Leaf (simple, compound)
Flower (calyx, corolla, androecium, gynoecium)
Fruit and seed structure
Importance of Morphology :
Helps in classification and identification of organisms.
Understanding evolutionary relationships.
Aids in diagnosing diseases (in microbiology and pathology).
Important in forensic biology, paleontology, and ecology.
Cultural characteristics
Definition :
Cultural characteristics refer to the visible features of microbial growth on different culture media under laboratory conditions. These features help in the preliminary identification and classification of microorganisms like bacteria and fungi.
Explanation :
When microorganisms are grown on artificial nutrient media (e.g., nutrient agar, blood agar, MacConkey agar), they develop colonies that show specific features. These features include :
Shape : circular, irregular, rhizoid
Size : small, medium, large
Elevation : flat, raised, convex
Margin : entire, undulate, lobate
Surface : smooth, wrinkled, mucoid
Color : white, yellow, pink, green (pigmented or non-pigmented)
Opacity : transparent, translucent, opaque
Consistency : dry, moist, brittle, sticky
Odor : characteristic smell (e.g., fruity in Pseudomonas)
Medium reaction : hemolysis on blood agar, lactose fermentation on MacConkey agar
Pathogenecity
Pathogenicity is the ability of a microorganism (such as bacteria, viruses, fungi, or parasites) to cause disease in a host organism.
Pathogenicity refers to how capable a microbe is in producing disease by overcoming the host’s defense mechanisms. It depends on several factors such as :
Invasiveness : Ability to enter, survive, and multiply in host tissues
Toxigenicity : Ability to produce toxins (e.g., exotoxins, endotoxins)
Adherence : Ability to attach to host cells using pili, fimbriae, etc.
Evasion of immunity : Ability to avoid destruction by the immune system (e.g., capsule formation, antigenic variation)
Examples :
Streptococcus pyogenes – causes sore throat and produces toxins
Mycobacterium tuberculosis – highly pathogenic, causes TB
Escherichia coli – some strains are non-pathogenic, while others (like E. coli O157:H7) are highly pathogenic
Laboratory diagnosis for streptococcus
Definition :
Laboratory diagnosis of Streptococcus aims to identify the specific species or group of Streptococcus bacteria responsible for an infection using various clinical specimens and microbiological techniques
Laboratory Diagnosis
Microscopy (Gram Staining) :
Shows Gram-positive cocci in chains
Helps in preliminary identification
Culture :
Inoculated on Blood Agar
Colony appearance: small, round with hemolysis pattern:
Alpha hemolysis – partial (green zone) (S. pneumoniae)
Beta hemolysis – complete (clear zone) (S. pyogenes)
Gamma hemolysis – no hemolysis
Biochemical Tests :
Catalase test : Negative (helps differentiate from Staphylococcus)
Bacitracin sensitivity test : S. pyogenes is sensitive
Bile solubility and optochin sensitivity for S. pneumoniae
Serological Tests :
ASO (Anti-streptolysin O) titer – used to detect recent Streptococcus infection
Q.3 Write Short Notes on: (Any three out of four)
1.Antibiotics acting on the cell wall.
Antibiotics that act on the bacterial cell wall mainly interfere with the synthesis of peptidoglycan, a crucial structural component that provides shape and rigidity to bacteria. These drugs are bactericidal in nature, meaning they kill bacteria by weakening the wall, which causes osmotic lysis of the cell.
Mechanism of action :
The main mechanism involves inhibition of penicillin-binding proteins (PBPs), which are responsible for the cross-linking of peptidoglycan strands. Disruption of this process results in a fragile cell wall.
Main Classes of Antibiotics Acting on Cell Wall :
Penicillins – e.g., Penicillin G, Amoxicillin
Cephalosporins – e.g., Ceftriaxone, Cefazolin
Carbapenems – e.g., Imipenem, Meropenem
Monobactams – e.g., Aztreonam
Glycopeptides – e.g., Vancomycin, Teicoplanin
Clinical Uses :
These antibiotics are used to treat infections like :
Pneumonia
Meningitis
Skin infections
Urinary tract infections
Septicemia
Resistance Mechanisms :
Production of beta-lactamase enzymes
Altered PBPs (e.g., in MRSA)
Decreased permeability of bacterial cell wall
2.Gram straining
Definition :
Gram staining is a differential staining technique developed by Hans Christian Gram in 1884 to classify bacteria into two major groups: Gram-positive and Gram-negative, based on differences in their cell wall structure.
Principle :
The stain differentiates bacteria based on the thickness of the peptidoglycan layer.
Gram-positive bacteria retain the crystal violet stain due to a thick peptidoglycan layer.
Gram-negative bacteria lose the violet stain and take up safranin, appearing pink/red.
Reagents Used :
Primary Stain : Crystal violet
Mordant : Iodine solution
Decolorizer : Alcohol or acetone
Counterstain : Safranin
Steps of Gram Staining :
Apply crystal violet for 1 minute → all cells purple
Apply iodine for 1 minute → forms complex with crystal violet
Decolorize with alcohol (15–20 seconds) → Gram-positive retain color; Gram-negative lose it
Counterstain with safranin for 30–60 seconds → Gram-negative appear pink/red
Results :
Gram-positive : Purple or Blue in colour, Peptidoglycan Layer-Thick
Gram-negative : Pink or Red in colour, Peptidoglycan Layer-Thin
Examples :
Gram-positive : Staphylococcus aureus, Streptococcus pyogenes
Gram-negative : Escherichia coli, Salmonella typhi
Uses :
Quick bacterial classification
Helps guide antibiotic selection
First step in bacterial diagnosis in microbiology labs
3.Importance of Microbiology in nursing.
Microbiology is the study of microscopic organisms such as bacteria, viruses, fungi, and protozoa. For nurses, understanding microbiology is essential in delivering safe and effective care, especially in infection prevention, diagnosis, and patient education.
1. Infection Control
Helps nurses understand sources, transmission, and prevention of infections.
Essential for maintaining aseptic techniques, hand hygiene, sterilization, and disinfection procedures.
Crucial in managing nosocomial (hospital-acquired) infections.
2. Safe Nursing Procedures
Knowledge of microbiology guides safe handling of wounds, injections, catheters, IV lines, and surgical care.
Prevents cross-contamination during dressing changes, IV infusions, and specimen collection.
3. Identification of Pathogens
Nurses assist in collecting, transporting, and labeling clinical specimens for lab diagnosis (e.g., blood, urine, sputum).
Enables early detection and reporting of infections such as tuberculosis, MRSA, sepsis, etc.
4. Antibiotic Use and Resistance
Microbiology knowledge helps nurses understand antibiotics, sensitivity reports, and drug resistance (e.g., MRSA, VRE).
Educate patients about completing antibiotic courses and avoiding misuse.
5. Immunization and Disease Prevention
Nurses provide vaccinations and counsel on immunity against infectious diseases like hepatitis, influenza, and measles.
Understands the role of microbial antigens and vaccine-preventable diseases.
6. Understanding Emerging Diseases
Helps recognize and care for patients with new infections (e.g., COVID-19, Zika, Nipah virus).
Enhances response to outbreaks and public health emergencies.
7. Role in Health Education
Educates patients and communities about personal hygiene, sanitation, food safety, and disease prevention.
Promotes infection awareness and healthy behaviors.
4 Compound Microscope.
Definition :
A compound microscope is an optical instrument used to magnify small objects that are not visible to the naked eye. It uses two sets of lenses – objective lens and eyepiece (ocular) lens – to produce a highly magnified image of the specimen.
Parts of a Compound Microscope :
1. Optical Parts :
Eyepiece (Ocular lens) : Located at the top; usually 10x magnification
Objective lenses : Usually 3 or 4 lenses (e.g., 10x, 40x, 100x oil immersion)
Condenser : Focuses light onto the specimen
Mirror or Illuminator : Provides light for viewing
2. Mechanical Parts :
Body tube : Connects eyepiece to objective lenses
Arm: Supports the tube and connects to base
Stage : Flat platform where slides are placed
Coarse adjustment knob : Moves stage up/down for focusing
Fine adjustment knob : Sharpens the focus
Base : Bottom support of the microscope
Working Principle :
Light from the mirror or illuminator passes through the condenser to the slide.
The objective lens magnifies the image.
The image is further magnified by the eyepiece.
Total magnification = Eyepiece × Objective lens (e.g., 10x × 40x = 400x)
Uses in Nursing/Microbiology :
Observing microorganisms (bacteria, protozoa)
Examining blood cells, urine sediments
Diagnosing infections and parasites
Viewing stained slides like Gram stain, acid-fast stain
Q.4 Write very short answers: (Any two out of three) (3×2=6)
1.Name of two drug resistant organism with explanation.
MRSA (Methicillin-Resistant Staphylococcus aureus)
MRSA is a strain of Staphylococcus aureus that has developed resistance to methicillin and most beta-lactam antibiotics (e.g., penicillin, cephalosporins). It is commonly found in hospital settings and causes infections like wound infections, pneumonia, bloodstream infections, and surgical site infections.
It spreads through direct contact and requires strict infection control.
MDR-TB (Multi-Drug Resistant Mycobacterium tuberculosis)
MDR-TB is a form of tuberculosis caused by Mycobacterium tuberculosis that is resistant to at least isoniazid and rifampicin, the two most powerful first-line anti-TB drugs. It arises due to improper or incomplete treatment, and is harder and more expensive to treat, requiring second-line drugs for a longer duration.
2.Normal floora.
Definition :
Normal flora (also called normal microbiota) refers to the non-pathogenic microorganisms (bacteria, fungi, and sometimes viruses) that naturally live on or inside the human body without causing harm under normal conditions.
Normal flora is found on various parts of the body such as:
Skin – Staphylococcus epidermidis, Corynebacterium
Nose and throat – Streptococcus viridans, Neisseria species
Mouth – Lactobacillus, Streptococcus mutans
Intestine – Escherichia coli, Bacteroides, Lactobacillus
Vagina – Lactobacillus, Candida (in small numbers)
Functions :
Prevents colonization by pathogens (competitive exclusion)
Produces vitamins (e.g., Vitamin K by E. coli)
Stimulates immune system development
Helps in digestion (intestinal flora)
3.Pasteurisation.
Definition :
Pasteurization is the process of heating liquids, especially milk, to a specific temperature for a short time to kill harmful microorganisms such as Mycobacterium tuberculosis, Brucella, and Salmonella, without changing the taste or nutritional value.
Common Methods :
Low Temperature Long Time (LTLT) : 63°C for 30 minutes
High Temperature Short Time (HTST) : 72°C for 15–20 seconds
Ultra-High Temperature (UHT) : 135°C for 2–5 seconds
Uses of Pasteurization :
Milk (most common)
Juices (fruit juices, vegetable juices)
Wine and beer
Egg products
Advantages :
Increases safety by killing pathogens
Extends shelf life
Maintains nutritional quality
Limitations :
Does not kill spores
Not a substitute for refrigeration after treatment
Section-2
Q.5 ultiple choice questions. (7×1-7)
1.Antigen presenting cell are
a. Macrophases
b. Dendritic cells
c. Langerhans cells
d. All of above.
2.The antibody that can cross placental barrier is
a. IgM
b. IgG
c. IgA
d. IgE
3. Hay fever, asthama are examples of
a. Atopy
b. Hypersensitivity
c. Delayed Hypersensitivity
d. Cytotoxicity
4. Which of the following is a subunit Vaccine?
a. Measles
b. Mumps
c. Rubella.
d. Hepatitis B.
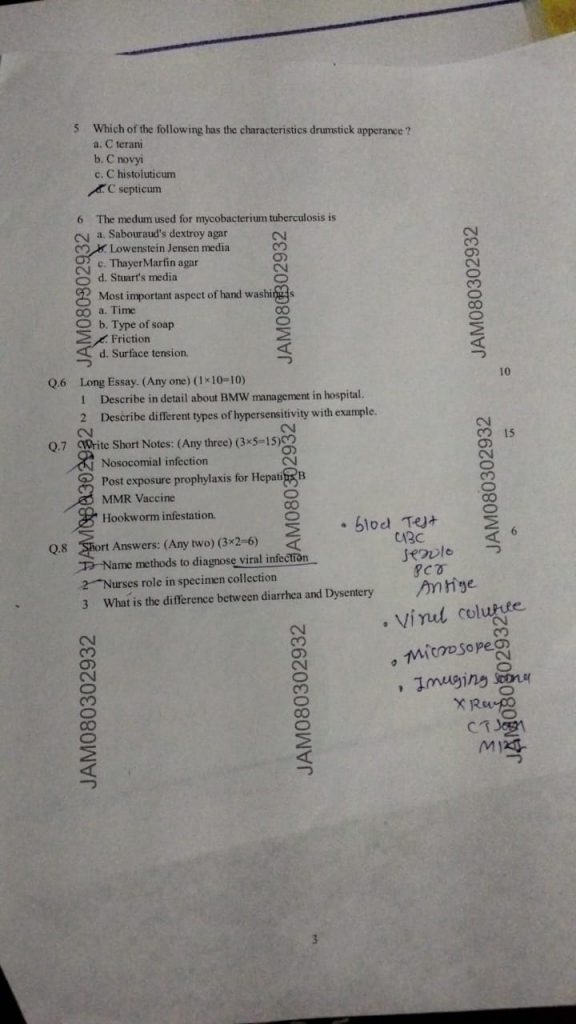
5. Which of the following has the characteristics drumstick apperance?
a. C tetani
b. C novyi
c. C histoluticum
d. C septicum
6. The medum used for mycobacterian tuberculosis is
a. Sabouraud’s dextroy agar
b. Lowenstein Jensen media
c. Thayer Marfin agar
d. Shart’s media
7. Most important aspect of hand washings
a. Time
b. Type of soap
c. Friction
d. Surface tension.
Q.6 Long Essay. (Any one) (1×10=10)
1 Describe in detail about BMW management in hospital.
Definition :
Biomedical waste refers to any waste generated during the diagnosis, treatment, or immunization of humans or animals, or during research activities and production/testing of biologicals. It may be infectious, hazardous, or radioactive.
Sources of Biomedical Waste in Hospitals :
Operation theatres
Wards and ICUs
Laboratories and pathology departments
Radiology and chemotherapy units
Central sterile supply department (CSSD)
Categories of Biomedical Waste (as per rules) :
Yellow
Waste Type : Human anatomical waste, soiled waste, expired drugs
Disposal Method : Incineration or deep burial
Red
Waste Type : Contaminated plastics (tubing, bottles, gloves)
Disposal Method : Autoclaving/Microwaving, shredding
White
Waste Type : (Translucent) Sharps (needles, scalpels, blades)
Disposal Method : Autoclaving followed by shredding
Blue
Waste Type : Glassware, broken vials, ampoules
Disposal Method : Disinfection/autoclaving then recycling
Steps in BMW Management in Hospital :
Segregation at Source :
Waste is separated immediately at the point of generation into color-coded bins.
Collection & Transportation :
Collected in leak-proof, labeled containers and transported safely to the temporary storage area.
Storage :
Stored for not more than 48 hours in a designated and secure area.
Treatment & Disposal :
Treated using autoclaving, incineration, deep burial, chemical disinfection, etc.
Final disposal in authorized common biomedical waste treatment facility (CBWTF).
Personal Protective Equipment (PPE) :
Staff involved in handling BMW must wear gloves, masks, aprons, goggles, and boots.
Record Keeping :
Hospitals must maintain daily logs, treatment records, and manifest copies for waste tracking.
Training and Awareness :
Regular training for healthcare staff on segregation, handling, and emergency measures.
Labeling and Signage :
Each container must be labeled with the biohazard symbol and relevant information.
1 Describe different types of hypersensitivity with example.
Hypersensitivity refers to an exaggerated or inappropriate immune response to an antigen (allergen), which results in tissue damage, inflammation, or disease. It occurs in previously sensitized individuals and involves immunological mechanisms such as antibody or T-cell mediated reactions.
Classification of Hypersensitivity
Hypersensitivity reactions are classified into four types (I–IV) by Gell and Coombs based on the immunologic mechanism and time course.
Type I – Immediate (Anaphylactic) Hypersensitivity
Mediated by : IgE antibodies
Onset : Within minutes of exposure
Mechanism : Allergen binds to IgE on mast cells → release of histamine & other mediators
Examples :
Anaphylaxis
Asthma
Hay fever (Allergic rhinitis)
Urticaria (hives)
Clinical features : Bronchospasm, hypotension, itching, swelling
Type II – Antibody-Mediated Cytotoxic Hypersensitivity
Mediated by : IgG or IgM antibodies
Mechanism : Antibodies target antigens on cell surfaces → cell lysis via complement or phagocytosis
Examples :
Hemolytic anemia
Blood transfusion reaction
Rh incompatibility (Erythroblastosis fetalis)
Myasthenia gravis
Outcome : Destruction of host cells
Type III – Immune Complex-Mediated Hypersensitivity
Mediated by : Immune complexes (antigen-antibody complexes)
Mechanism : Complexes deposit in tissues → activate complement → inflammation
Examples :
Systemic lupus erythematosus (SLE)
Rheumatoid arthritis
Serum sickness
Post-streptococcal glomerulonephritis
Symptoms : Fever, rash, joint pain, nephritis
Type IV – Delayed-Type (Cell-Mediated) Hypersensitivity
Mediated by : T-lymphocytes (no antibody involved)
Onset : 24–72 hours after exposure
Mechanism : Sensitized T-cells release cytokines → macrophage activation → tissue damage
Examples :
Tuberculin skin test (Mantoux test)
Contact dermatitis (e.g., poison ivy)
Graft-versus-host disease
Type 1 Diabetes Mellitus
Hallmark : Delayed inflammatory response
Q.7 Write Short Notes: (Any three) (3×5=15)
1.Nosocomial infection
Definition :
Nosocomial infection, also known as hospital-acquired infection (HAI), refers to an infection that is not present or incubating at the time of hospital admission but develops 48 hours or more after admission or within 30 days after receiving healthcare.
Common Sites of Nosocomial Infections :
Urinary Tract Infections (UTIs) – often due to catheterization
Surgical Site Infections (SSIs)
Pneumonia – especially ventilator-associated
Bloodstream Infections (BSIs) – often related to IV lines or catheters
Gastrointestinal infections – e.g., due to Clostridium difficile
Causative Microorganisms :
Bacteria :
Staphylococcus aureus (including MRSA)
Pseudomonas aeruginosa
Escherichia coli
Klebsiella pneumoniae
Fungi : Candida albicans
Viruses : e.g., norovirus, influenza (less common)
Risk Factors :
Indwelling devices (catheters, IV lines, ventilators)
Prolonged hospital stay
Immunocompromised state
Poor hand hygiene practices
Invasive surgical procedures
Prevention and Control :
Standard Precautions
Hand hygiene (before & after patient care)
Use of PPE (gloves, masks, gowns)
Sterile technique in invasive procedures
Safe injection practices
Environmental cleaning
Isolation precautions for patients with contagious infections
Proper sterilization and disinfection of medical equipment
Antibiotic stewardship – rational use of antibiotics to prevent resistance
2.Post exposure prophylaxis for Hepatitis B
Post-exposure prophylaxis (PEP) for Hepatitis B virus (HBV) refers to preventive measures taken after accidental exposure to blood or body fluids potentially infected with HBV. Common exposures include needle-stick injuries, mucosal contact, or perinatal transmission.
Key Components of PEP :
Immediate Wound Care :
Wash the exposed area with soap and water.
Avoid squeezing or scrubbing the wound.
Assessment of Source and Victim :
Determine HBsAg status of the source.
Check the vaccination and antibody status (anti-HBs) of the exposed individual.
Vaccinated Person with Adequate Antibody (>10 mIU/mL) :
No PEP required.
Vaccinated Person with Unknown or Inadequate Antibody (<10 mIU/mL) :
One dose of Hepatitis B vaccine booster ± 1 dose of HBIG (Hepatitis B Immune Globulin) depending on risk.
Unvaccinated or Incompletely Vaccinated Person :
Start full Hepatitis B vaccination series (0, 1, 6 months).
Give HBIG 0.06 mL/kg IM within 24 hours, preferably within 7 days of exposure.
Newborn of HBsAg Positive Mother :
Administer HBV vaccine + HBIG within 12 hours of birth.
Follow-up :
Test for HBsAg and anti-HBs after 6 months.
Monitor for clinical signs of hepatitis.
3.MMR. Vaccine
Definition :
The MMR vaccine is a combined live attenuated vaccine that provides protection against three viral diseases:
Measles
Mumps
Rubella
Composition :
Live attenuated strains of :
Measles virus (Edmonston strain)
Mumps virus (Jeryl Lynn strain)
Rubella virus (Wistar RA 27/3 strain)
Schedule (as per National Immunization Guidelines) :
9 months : First dose (as MMR or MR)
15–18 months : Second dose
4–6 years (booster) : Third dose (in some schedules or schools)
Route & Site of Administration :
Route : Subcutaneous (SC)
Site : Anterolateral aspect of the thigh (infants) or upper arm (older children)
Storage :
Stored at 2–8°C in the refrigerator
Protect from light (photosensitive)
Indications :
Prevention of :
Measles (highly contagious viral disease)
Mumps (causes swollen salivary glands and orchitis)
Rubella (can cause congenital rubella syndrome in pregnancy)
Contraindications :
Severe allergic reaction to neomycin or gelatin
Immunocompromised individuals (e.g., leukemia, HIV/AIDS with low CD4)
Pregnancy – live vaccine can harm the fetus
Common Side Effects :
Mild fever
Rash
Pain or swelling at injection site
Mild joint pain (especially rubella component in adolescent females)
Serious Adverse Effects (Rare) :
Febrile seizures
Thrombocytopenia
Anaphylactic reaction
Nursing Responsibilities :
Ensure vaccine cold chain maintenance
Obtain informed consent
Screen for contraindications
Educate parents about minor side effects
Advise to avoid pregnancy for at least 1 month after vaccination
4.Hookworm infestation.
Definition :
Hookworm infestation is a parasitic infection caused by intestinal nematodes (roundworms), primarily Ancylostoma duodenale and Necator americanus, which attach to the small intestine and feed on the host’s blood, leading to anemia and malnutrition.
Causative Agents :
Ancylostoma duodenale
Necator americanus
Mode of Transmission :
Infective larvae in contaminated soil penetrate intact skin, especially through bare feet.
Poor sanitation, open defecation, and barefoot walking increase the risk.
Life Cycle :
Eggs excreted in feces contaminate soil
Hatch into larvae → become infective
Larvae penetrate skin → migrate via blood to lungs
Ascend to throat → swallowed → reach small intestine
Mature into adult worms and suck blood
Signs and Symptoms :
Ground itch at skin penetration site
Abdominal cramps, bloating, diarrhea
Iron-deficiency anemia (pallor, fatigue)
Growth retardation in children
Protein loss, weakness
Diagnosis :
History collection
Physical examination
Microscopic stool examination → detects hookworm eggs
CBC → shows low hemoglobin (anemia)
Treatment :
Albendazole (400 mg single dose)
Mebendazole (100 mg twice daily for 3 days)
Iron and folic acid supplements for anemia
Nutritional support
Prevention :
Wear shoes to prevent skin contact with soil
Promote sanitation and use of toilets
Health education on hygiene and safe defecation
Deworming programs in schools and communities
Q.8 Short Answers: (Any two) (3×2=6)
1.Name methods to diagnose viral infection
Several methods are used to diagnose viral infections based on clinical samples like blood, throat swabs, CSF, urine, etc.
Common Diagnostic Methods :
Polymerase Chain Reaction (PCR) :
Detects viral genetic material (DNA or RNA)
Highly sensitive and specific
Used for viruses like HIV, COVID-19, Hepatitis B/C
Antigen Detection Tests :
Detect viral proteins (antigens) in samples
Rapid test kits (e.g., Dengue NS1, COVID-19 antigen test)
Serological Tests :
Detect antibodies (IgM, IgG) produced by the immune system
Example : ELISA test for HIV, Hepatitis B
Viral Culture :
Growing viruses in cell cultures
Time-consuming, used for research or special cases
Electron Microscopy :
Direct visualization of viruses using powerful microscope
Used in research labs
Rapid Diagnostic Tests (RDTs) :
Point-of-care tests providing results within minutes
Example : Rapid influenza test
2 Nurses role in specimen collection
1. Patient preparation
Explain the purpose and procedure of patient.
Ensure privacy, comfort, and informed consent.
Verify pre-test instructions (e.g., fasting, medication restrictions).
2. Proper Collection Technique
Use correct technique for each specimen type (urine, stool, blood, sputum, etc.).
Maintain aseptic technique to avoid contamination.
Collect specimen at the right time (e.g., early morning sputum).
3. Labeling and Documentation
Label specimen containers with patient name, ID, date, and time immediately.
Fill out lab request forms correctly.
Record the procedure in nurse’s notes.
4. Safe Handling and Transport
Handle specimens carefully to prevent spillage or contamination.
Send to the laboratory promptly using proper biohazard containers.
Maintain specific temperature if required (e.g., ice for some blood samples).
5. Infection Control and Waste Disposal
Perform hand hygiene and wear appropriate PPE.
Dispose of used materials as per biomedical waste guidelines.
Clean the area and equipment after use.
3 What is the difference between diarrhea and Dysentery
1. Definition :
Diarrhea :
It is the frequent passage of loose or watery stools, typically without blood or mucus. It may be caused by infections, food intolerance, or medications.
Dysentery :
It is an inflammatory disorder of the intestine, especially the colon, resulting in bloody, mucus-filled stools along with abdominal pain and fever. It is usually caused by bacterial or amoebic infections.
2. Causative Organisms :
Diarrhea :
Commonly caused by viruses (e.g., Rotavirus, Norovirus), some bacteria (e.g., E. coli, Vibrio cholerae).
Dysentery :
Caused by Shigella (bacillary dysentery) or Entamoeba histolytica (amoebic dysentery).
3. Stool Characteristics :
Diarrhea :
Watery, large-volume stools with no visible blood or mucus.
Dysentery :
Small-volume stools that contain blood and mucus.
4. Abdominal Pain :
Diarrhea :
Usually mild or crampy abdominal discomfort.
Dysentery :
Severe abdominal pain with tenesmus (painful straining during defecation).
5. Fever and Systemic Symptoms :
Diarrhea :
Fever may be mild or absent.
Dysentery :
Often accompanied by high fever, fatigue, and dehydration.
6. Duration and Severity :
Diarrhea :
Often self-limiting, especially viral diarrhea.
Dysentery :
Requires prompt treatment with antimicrobials to prevent complications.
7. Treatment Approach :
Diarrhea :
Focus is on rehydration therapy (ORS) and dietary management.
Dysentery :
Requires antibiotic/antiparasitic therapy in addition to fluid replacement.