ENGLISH SKIN DISORDERS – JUHI – SKIN-PART-8
Dermatoses
Dermatosis is a general term used to describe any skin defect and lesion. Dermatosis is a broad term denoting any disease of the skin.
While dermatitis denotes a condition with skin inflammation.
Infectious dermatoses
Infectious dermatitis is caused by bacteria, viruses, fungi, parasites and other infections. Infectious dermatitis includes skin conditions such as impetigo, folliculitis, cellulitis, warts, herpes simplex, candidiasis, scabies, etc.
Non infectious dermatoses
Non-infectious dermatitis is not caused by an infection but by some other cause.
Examples include conditions like psoriasis, seborrheic dermatitis, hyperpigmentation, vitiligo, alopecia.
Define acne vulgaris
Ekne vulgaris is the most common skin disorder. which affects the hair follicle. Which we know as acne or pimple.
Acan vulgaris is mainly found on the face, neck and upper trunk.
A vulgaris is more common in adolescents and young adults i.e. 12 to 35 years of age.
Ekne vulgaris is associated with hormonal changes, diet patterns, stress.
What is the cause of acne vulgaris
Due to excessive sebum production
A hair follicle becomes plugged due to dead skin cells or oil.
Due to abnormal keratinization of the epithelium.
Due to anaerobic bacteria
Family history
Explain pathophysiology of acne vulgaris
During puberty the sebaceous gland is stimulated due to androgen hormone.
|
The size of the sebaceous gland increases. Natural oil and sebum are produced by the sebaceous gland.
|
In the condition of Ekne vulgaris, the sebaceous gland is stimulated by many factors.
|
So sebum production increases. This sebum flows out onto the skin surface.
|
This causes the pilo sebaceous duct to become plugged, resulting in comedones.
Write sign & symptoms seen in acne vulgaris
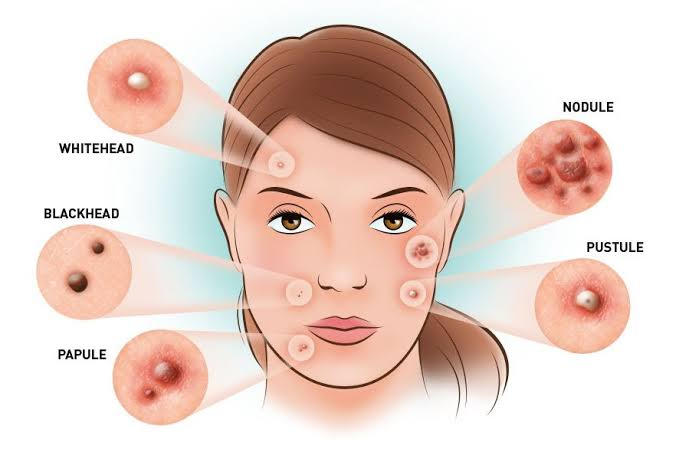
Whitehead (close plug pore), blackhead (open plug pore), papule, pustule, nodule and cyst are seen in face, neck, solder and trunk.
In more severe cases cyst formation is observed and pigmentation is observed.
Scar formation is seen.
How to diagnose acne vulgaris
History Collection
Physical Examination
Culture test (if pus present)
Write medical management of acne vulgaris
- Topical medicine
Salicylic acid and benzoyl peroxide are used as topical medicines. In which benzoyl peroxide is used more.
Benzoyl peroxide quickly reduces inflammation and reduces sebum production.
Topical antibiotics are also often used. which decreases the level of superficial fatty acids and decreases comedone papules and pustules.
Tretinoin (vitamin A acid) is also used. which clears the keratin plug from the pilosebaceous duct. Systemic medicine
Antibiotics and synthetic vitamin-A compounds are used as systemic medicine.
Estrogen therapy is also used in female patients. Estrogen progesterone preparations reduce sebum production and reduce oiliness of the scalp. This therapy is not used in mail because using this therapy in mail leads to breast enlargement. Intra lesional injection
Intralesional injection involves injecting a corticosteroid drug into the lesion. This procedure is used for the treatment of C acne. Diet therapy:
Diet plays an important role in Ekne vulgaris.
Avoid trigger foods. Like chocolate, cola, fried food, milk product and high glucose food Hygiene therapy
Wash the affected area twice a day with cleansing soap.
Use oil-free cosmetics and personal products.
Write surgical management of acne vulgaris
Comdone extraction
In comedone extraction, comedones are removed with the help of a comedone extractor. In which the opening of the comedone extractor is held over the comedone and pressure is applied on it so that the plug comes out.
Crayo surgery
Cryosurgery is used for both nodular and cystic forms.
Inscion & drainage
An incision and drainage procedure is used for large nodular cystic lesions.

Define acne rosacea
Rosacea is a chronic inflammatory skin condition that affects the central face. One finds small red papules and pustules on the face in rosacea. There is also itching and burning sensation on the face. The face is seen flushing and blushing. Along with talent ectasia is also seen i.e. spider like blood vessels are seen on the cheek.
One finds rosacea most commonly in middle-aged women and in people with fair skin. That is, 30 to 50 years of age is more common.
One has no specific treatment for rosacea but the antibiotic, azelaic acid is used.

Define acne conglobata
Acne conglobata is a rare but severe form of nodulocystic acne. The primary cause of conglomerate is unknown. But trigger factors include anabolic steroids, testosterone, leukemia and cancer.
It includes comedones, cysts, nodules and burrowing abscesses in the face, neck, back, chest and thigh. Comedones are found in groups of two to three. Offensive smelling discharge and irregular scar formation are also seen.
Anti-acne medicine is used in the treatment of acne. such as tretinoin. Systemic steroids and antibiotics are also used.

Fungal infection of skin
Fungal infections are also known as ‘mycosis’.
The fungus is more common in warm and moist areas. Hence, fungal infections are more common in moist areas such as feet, armpits and skin folds.
Fungal infections are spread by direct or indirect contact with an infected person.
Infections are more common in people who use systemic corticosteroids and antibiotics, who use birth control pills, who are immunosuppressed, who have systemic diseases, who live in warm climates.
Fungal infections include tinea and candidiasis.
What is Tinea
Tinea is also known as ‘dermatophytosis’.
Tinea is the most common fungal infection.
Tinea is also known as ‘ring worm infection’ because of the red colored ring shaped patches.
Explain type of tinea
Depending on which part of the body is involved, tinea is of the following types:
Tinea pedis
Tinea corporis
Tinea capitis
Tinea cruris
Tinea unguium
Tinea barbae
Tinea faciei
Tinea manuum

Tinea pedis
Tinea pedis is also known as ‘ringworm of foot’ or ‘athlete’s foot’.
Tinea pedis affects the area between the sole of the foot and the toes.
Explain sign & symptoms seen in tinea pedis
Scaly, peeling and cracked skin can be seen between tosses.
Itching is seen in that area.
Stinging and burning sensations are observed.
Skin becomes inflamed and discolored.
In more severe cases, pain fills the fissure and a foul odor is seen. Write medical management of tinea pedis
Soaking the foot in boro solution, vinegar solution, potassium permagnet solution or saline solution to remove crust, scale and debris and reduce inflammation.
Applying a topical antifungal agent to the infected area. Like Clotrimazole, Miconazole Write nursing management of tenia pedis
To assess vital signs.
Checking the area between the toss and the toss.
Apply topical medicine on the affected area.
Advise the patient to avoid wearing rubber and plastic shoes.
Wear cotton socks.
Keep the toss part dry.
To clean the toss properly with a shop.
Administer the medicine prescribed by the doctor.
To maintain records and reports.

Tinea corporis
Tinea corporis is also known as ‘ring worm of body’.
Tinea corporis is an infection of the body. In which mainly the face, neck, trunk and extremities are affected.
Tinea corporis can occur at any age but is more common in children.
Sign & symptoms seen in tenia corporis
Initially, small red macules are seen.
Then a large papule, pustule or vesicle of ring shape is seen.
In which red color rice border is seen.
These lesions appear as clusters.
There is itching and erythema in the affected area. Write management of tenia corporis
Apply topical antifungal cream on the affected area. For example Clotrimazole
Provide oral antifungal medicine in severe cases. For example griseofulvin, terbinafine
Applying cold compresses. Write nursing management of tinea corporis
To assess vital signs.
Note the color, type and size of the lesion.
Apply topical medicine on the infected area.
Advise the patient to keep the folded area dry.
Avoid wearing tight fitting clothes.
Wear cotton clothes.
Maintaining proper hygiene.
Administer the medicine prescribed by the doctor.
To maintain records and reports.

Tinea capitis
Tinea capitis is also known as ‘ring worm of scalp’.
Tinea capitis is a highly contagious fungal infection that infects the hair shaft.
Tinea capitis is more common in children between two and ten years of age.
Explain sign & symptoms seen in tinea capitis
Erythematous patches of oval shape of red color are seen on the scalp.
Small papules and pustules are seen on the scalp.
Etching is seen at that place.
Hair becomes brittle hence temporary hair loss is seen. Write medical management of tinea capitis
Using anti-fungal drugs to treat fungal infections.
Apply topical anti-fungal ointment on the infected area.
Wash your hair with shampoo two or three times a week.
Using nizoral or selenium sulfamide as a shampoo. Write nursing management of tinea capitis
To do vital sign ss.
To note the characteristic of the lesion.
Provide isolation to the patient.
To retrack a visitor.
Maintaining proper hygiene.
Wash hands twice in a wick.
Advise the patient and his family members that each family member should use a separate towel, comb and brush.
Apply the medicine prescribed by the doctor.
To maintain records and reports.

Tinea cruris
Tinea cruris is also known as ‘ringworm of groin’ or ‘jock itch’.
Tinea cruris is a ringworm infestation of the groin area, affecting the inner and groin areas.
Tinea cruris is more common in obese persons and in people who wear tight underwear.
Explain sign & symptoms seen in tinea cruris
Small red colored scaling patches and circular elevated plaques are seen in the groin area.
Severe itching is seen in the affected area.
Clusters of pastuals are seen around the border. Write management of tinea cruris
Apply topical antifungal cream on the affected area.
Administering oral anti-fungal medicine in severe cases.
Advise the patient to avoid wearing tight underwear.
Keep the groin area dry and clean.

Tinea unguium
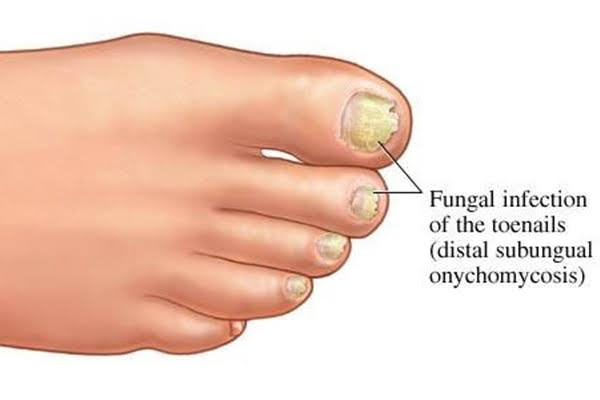
Tinea ungium is also known as ‘Onychomycosis’.
Tinea ungium is an infestation of the fingernail or toenail. But the toe nail is more affected. Explain sign & symptoms seen in tinea unguium
The nail is found to be thick, brittle and deformed.
Nails are seen in yellow color and luster.
Debris collects under the nail plate due to which it separates from the nail plate.
If the infection persists for a long time, the nail is completely destroyed. Write management of tinea unguium
Using antifungal medicine to treat fungal infections.
Applying a topical antifungal cream to the infected area.
In chronic conditions nail avulsion is done i.e. the nail is removed.
Tinea barbae
Tinea barbae is a rare fungal infection. In which the skin, hair and hair follicles in the beard and mustache are affected and red ring-shaped skin rashes are seen there.

Tinea faciei
Tinea faeces is a facial ringworm infestation. In which the super facial skin on the face is affected. In which scaly plaque is seen in cheek, nose, chin, forehead.

Tinea manuum
Tinea manum is an infection of the superficial skin of the hand. In which round and oval shape races are seen in the hand.

What is candidiasis
Candidiasis is also known as ‘yeast infection’.
Candidiasis is a fungal infection caused by Candida albicans.
Candida albicans is a yeast type fungus. Hence it is also called yeast infection.
Candida albicans is mainly found in our body in small amounts in the mouth, throat, vagina and GI tract. But when it gets a favorable environment, it multiplies and creates the condition of candidiasis. Write types of candidiasis
Depending on the location of infection, candidiasis is of the following types:
i) Vaginal candidiasis
Vaginal candidiasis occurs due to overgrowth of yeast in the vagina.
Vaginal candidiasis causes swelling and redness of the vagina and vulva.
Burning and itching is seen in that area.
Vaginal discharge like cottage cheese of thick white color is seen.
Pain during urination and intercourse.
Antifungal suppositories, tablets or creams are used as treatment.

ii) Oral candidiasis
Oral candidiasis is also known as ‘oral thrush’.
In oral candidiasis, Candida yeast spreads in the mouth and throat.
Oral thrush is mainly seen in newborns and older adults.
Oral thrush causes white or yellow sores on lips, mouth, tongue, throat and esophagus.
Oral thrush is treated with the antifungal medicines clotrimazole, fluconazole.
Rinse with chlorhexidine mouth wash.

iii) Cutaneous candidiasis
Cutaneous candidiasis is an infection of the skin.
Cutaneous candidiasis is more common in warm and moist areas. Such as underarm, under the breast, groin area, in the space between fingers and toes.
In which small raised red colored pin point satellite lesions are seen on the skin.
Antifungal creams are used as treatment.

iv) Candida granuloma
Candida granuloma is a chronic infection that affects different parts of the body such as the face, mouth, skin, scalp and nails.
In which white cheesy plaques are seen in the mouth and pin point satellite lesions and papules are seen on the skin.

v) Invasive candidiasis
Invasive candidiasis is also known as ‘systemic candidiasis’.
In invasive candidiasis, Candida reaches the blood, heart, brain, eye, and bone through treatment or instruments. And due to that serious life threatening condition is seen.
How to diagnose candidiasis
History Collection
Physical Examination
Culture
Skin scraping
Wood Lamp Examination
Write medical management of candidiasis
Antifungal medicines are used to treat fungal infections.
Apply topical antifungal cream on the affected area.
Antifungal suppositories are used in vaginal candidiasis.
Write nursing management of candidiasis
To assess the patient’s vital signs.
Note which part of the body is affected.
Applying topical medicine on the affected area.
Do not give patient advice or share personal information.
All people should use a separate towel and wash cloth.
Avoid wearing rubber and plastic shoes.
Avoid wearing tight and fitting clothes.
Wear cotton clothes.
Maintain proper hygiene and keep skin dry.
Administer the medicine prescribed by the doctor.
To maintain records and reports
Parasite infestation of skin
Skin infections caused by parasites (lice, mites) are known as parasite infestations.
In a parasitic infestation, the insect or worm resides in the burrows on the skin, multiplies and receives nutrition from there.
Parasite infestation is spread through direct and indirect contact with an infected person.
Parasitic skin infestations include pediculosis and scabies.
What is pediculosis
Pediculosis is a lice infestation.
This parasite lives on the outside of the animal or human body and receives nourishment from the blood, hence the lice are also known as ‘ectoparasites’.
Anticoagulants are present in the saliva of lice so that when the lice pierces the skin to draw blood from the host, the host’s blood does not clot.
Lies in celebration can be seen in people of any age. But it is more common in school going children.
There are three main types of pediculosis:
pediculosis capitis
pediculosis corporis
pediculosis pubis
Pediculosis capitis
Pediculosis capitis is a scalp infestation caused by head lice. Which in our language is called tola or lice in the head.
These lice are found behind the ears and on the nape of the neck.
We can see the eggs (nits) laid by louse with the naked eye. Which appears silvery and glistening oval shaped and sticks to the hair. Explain sign & symptoms seen in pediculosis capitis
Feels like something is moving in the hair.
Itching occurs in the scalp due to which there is scratching.
Erythema is seen in that area. Write management of pediculosis capitis
Washing hair with shampoos or shampoos containing permethrin or lindane subtons.
Washed hair with a fine toothed comb to remove nits and lice.
Soak the comb in hot water for 10 minutes after using the comb.
Washing towels, cloths and other items used by an infected person in hot water

Pediculosis corporis
Pediculosis corporis is also known as ‘Vagabond Disease’.
Pediculosis corporis is a body infestation caused by body lice.
Pediculosis corporis is seen in people with poor hygiene and people who do not bathe for long periods of time. Explain sign & symptoms seen in pediculosis corporis
Erythematous macules are seen on the trunk, neck, shoulders and buttocks.
Then a wheal and papule are seen at that place.
Etching and scratching are seen at that place. Write management of pediculosis corporis
Applying permethrin or lindane lotion to the affected area.
Wash towels, cloths and other items used by the patient with hot water.

Pediculosis pubis
Pediculosis pubis is an infestation of the pubic area caused by pubic louse.
Pubic louse is also known as ‘crabs’.
In which the pubic lice lays its eggs on the pubic hair and receives nourishment from there. Explain sign & symptoms seen in pediculosis pubis
Intense itching is observed in the groin area and the itching increases at night.
Scratch marks and crusting are seen at that place.
It appears to be area gray or bluish in color. Write management of pediculosis pubis
Apply permethrin lotion on the affected area.
Wash the comb and clothes used by the patient with warm water.

What is scabies
Scabies is also known as ‘sarcoptic mange’.
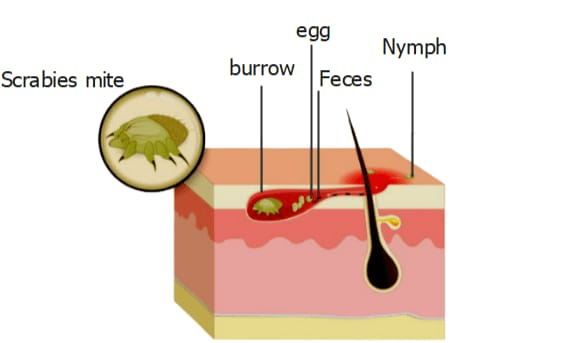
Scabies is a highly contagious parasitic skin infestation. Which is caused by ‘Sarcoptic mange mite’.
Scabies is mainly found in the area between the fingers and toes, under the fingernails, in the folds of the thighs and genital area, around the nipples, armpits, wrists, elbows and knees.
Explain pathophysiology of scabies
Coming in contact with an infected person
|
The scabies mite lives on the burrows in the skin.
|
The adult female lays eggs in the burrow.
|
The larvae hatch from the egg in three to four days and become adult mites in one to two weeks.
|
After four to six weeks, the patient develops symptoms of scabies.
Explain sign & symptoms seen in scabies
Severe itching is seen in places with mite burrows and increased itching at night.
A pimple like race is seen on the skin.
Tiny blisters and bumps appear on the skin that look like wavy tunnels.
Vesicles, crusts and excoriations are seen as secondary lesions
How to diagnose scabies
History Collection
Physical Examination
Skin scraping
Write management of scabies
Ask the patient to bathe with warm soapy water.
Then apply the scabicidal lotion on the area other than the face and scalp i.e. below the neck.
Using lindane or permethrin as a scabicidal lotion.
Keep this lotion for 12 to 24 hours and then take a bath.
Do this procedure for a week. Write nursing management of scabies
Assess the patient’s condition.
Advise the patient to apply scabicidal lotion to the lower neck.
Do not apply lotion frequently as it causes irritation.
Giving patient advice or maintaining proper hygiene.
Ask the patient to use clean towels and clean clothes.
Wash the towel cloth used by the patient with hot water.
Administering medicine prescribed by a doctor.
To maintain records and reports.

What is pemphigus vulgaris (What is pemphigus vulgaris)
The word pemphigus is derived from the Greek word ‘pemphix’ which means ‘blister’.
Pemphigus vulgaris is an autoimmune disease in which the immune system mistakenly attacks epidermal cells and mucus membranes resulting in painful blisters.
In which a reaction is seen between desmoglein (antigen) and antibody (IgG) in epidermal cells.
A type 2 hypersensitivity type reaction is seen in pemphigus vulgaris.
Pemphigus vulgaris mainly occurs in the mouth, nose, eyes, back, chest, umbilicus and genital area. Explain sign & symptoms seen in pemphigus vulgaris
Painful blisters and sores appear first in the mouth and scalp.
The blister then spreads to other parts of the body.
Erosions and ulcerations are seen at the blistered site.
There is oozing, crusting and peeling.
A musty order is seen from the blisters.
A Nikolsky sign is positive (applying pressure on the blister causes it to spread to the underlying skin).
The skin is a slow hill.
Bacterial superinfection occurs and often a septicemia-like condition arises.
How to diagnose pemphigus vulgaris (How to diagnose pemphigus vulgaris)
History Collection
Physical Examination
Skin biopsy (punch biopsy)
Immunofluorescence
Tzank Samier
Write management of pemphigus vulgaris
Corticosteroids: Administer systemic corticosteroids. Initially give high dose and provide antacid medicine along with it. Apply topical corticosteroid to the affected area.
Immunosuppressive Agents: Immunosuppressive agents are used to suppress immunity. Hence intravenous immunoglobulin is given. Methotrexate, cyclophosphamide are used as immunosuppressive agents.
Plasmapheresis: Plasmapheresis is used to reduce serum antibody levels.
In case of severe mouth ulcer, IV fluid should be provided.
Write nursing management of pemphigus vulgaris
To assess vital signs.
Assess the patient’s condition.
Provide a comfortable position to the patient.
Providing oral care to the patient.
Applying lip balm on the lips. So that the lips remain moist and can be prevented from drying.
Providing warm moist compression.
Apply wet dressing on the affected area.
Observe for signs and symptoms of infection.
Provide psychological support to the patient.
Reassuring the patient and his family members.
Apply topical medicine prescribed by the doctor.
Administer the medicine prescribed by the doctor.
To maintain records and reports.

What is Stevens Johnson syndrome (What is Stevens-Johnson syndrome)
Stevens-Johnson syndrome is also known as ‘erythema multiforme mass’.
Stevens-Johnson syndrome is a rare and serious skin reaction disorder. In which a reaction is seen on the skin due to taking some medicine.
Painful blisters and lesions are seen mainly on the skin and mucous membranes.
Stevens-Johnson syndrome has the following drug reactions.
Antigout medicine, anticonvulsant medicine, antipsychotic medicine, antibacterial medicine (especially sulfonamides) pain reliever medicine, non-steroidal anti-inflammatory drug
It is more common in people who are HIV positive and have pneumonia as well as in immunosuppressed patients.
Explain sign & symptoms seen in stevens johnson syndrome
Initially, flu-like symptoms such as high temperature, headache, cough, throat pain, joint pain are observed.
Painful blisters are found on the skin, mouth, eyes, nose and genital area. After a few days, the blisters appear as scabies.
Swelling is seen in mouth, lips, tongue and face.
There is pain in the eye. Even when looking at bright light, the pen is seen in the eye.
How to diagnose stevens johnson syndrome (How to diagnose Stevens-Johnson syndrome)
History Collection
Physical Examination
Skin biopsy
Write management of stevens johnson syndrome
Administer IV immunoglobulin.
Provide systemic corticosteroids.
Provide antibiotics to control infection.
Provide analgesic medicine to relieve pain.
Provide iv fluids to maintain fluid and electrolyte balance.
Providing eye care and wound care.
Cleansing the skin and removing dead tissue. Covering the wound with a non-adhesive dressing.
Write nursing management of stevens johnson syndrome
To assess vital signs.
Maintaining intake output chart.
Provide a comfortable position to the patient.
Change position every two hours
Providing iv fluids to the patient.
Providing eye care and wound care to patients.
Noting whether signs of infection are present or not.
Administer the medicine prescribed by the doctor.
To maintain records and reports.
Write complications of Stevens Johnson syndrome
Dehydration
Sepsis
Pneumonia
Multiple organ failure

What is psoriasis
Psoriasis is an autoimmune condition. In which skin cells grow and multiply rapidly due to which keratin overproduction is seen and white silvery plaque is seen in the skin.
Psoriasis can occur at any age but is more common between the ages of 15 and 35.
The exact cause of psoriasis is unknown but family history and certain trigger factors can cause psoriasis.
Factors that trigger psoriasis are as follows:
Emotional stress
Anxiety
trauma
infection
Seasonal and hormonal changes
Cold and dry weather
Sun burn
Explain pathophysiology of psoriasis
Due to etiological factor
|
T-cell becomes hyper activated.
|
This results in epidermal infiltration and keratinocyte proliferation. That means normally skin cells are replaced in 10 to 30 days but in such condition it is replaced in three to four days.
|
This results in the production of various cytokines in large quantities.
|
Also an inflammatory response is observed. Superficial blood vessels dilate and vascular engorgement is seen.
|
Epidermal hyperplasia causes insufficient lipid release and causes flaking and scaling of the skin.
Write types of psoriasis
Plaque Psoriasis:
Plaque psoriasis is also known as ‘vulgar psoriasis’. Plaque psoriasis is the most common form of raised inflamed lesions on the skin. It is called plaque. which are covered with silvery white scales. These lesions are seen symmetrically. Which is mainly found in the scalp, trunk, limbs, elbows and knees.
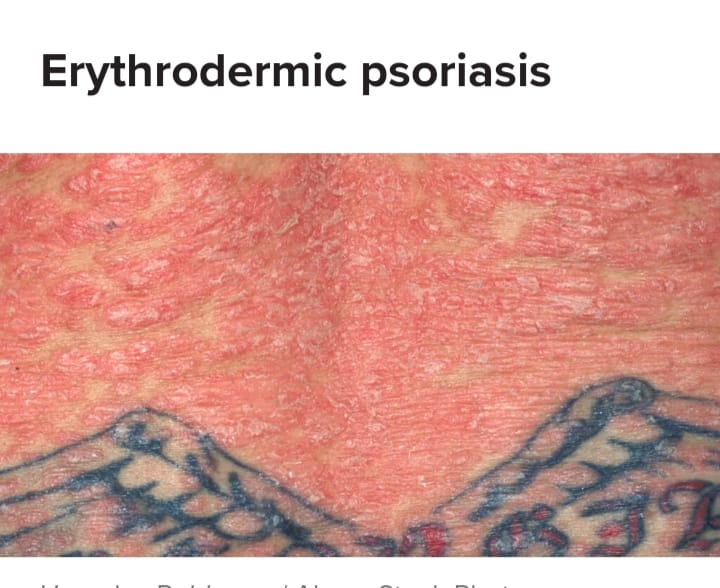
Erythrodermic psoriasis:
Erythrodermic psoriasis is a rare but more severe form. In which red scaly skin is seen in the body and severe itching, burning and peeling are seen.
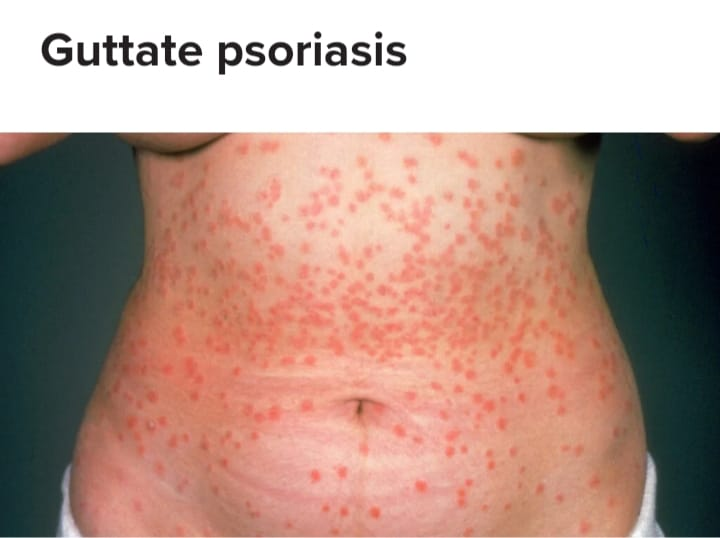
Guttate psoriasis
In guttate psoriasis, small pink-red colored spores are seen on the torso and limbs. Guttate psoriasis is mainly seen in children and young adults.
Inverse Psoriasis
Smooth sinus red patches are seen in inverse psoriasis. Which is mainly found in folded areas. Like under the breast, armpit and groin area
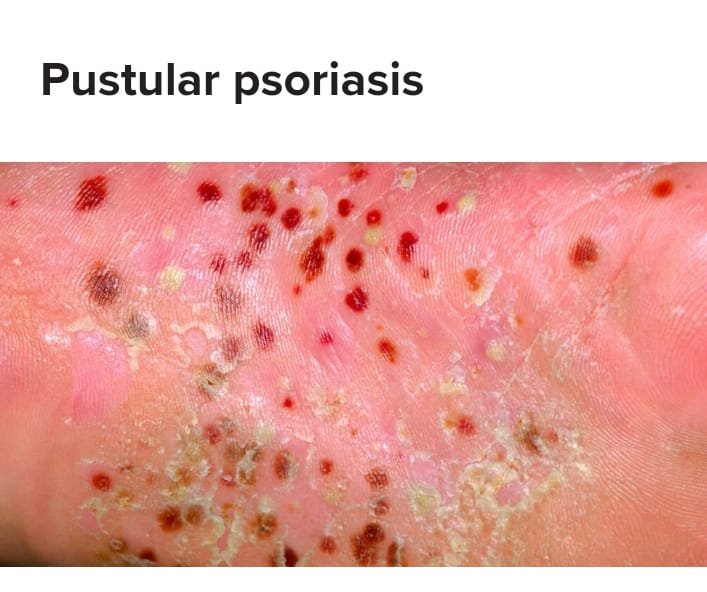
Pustular psoriasis
Pustular psoriasis is a rare form of pustular or pus-filled blisters with red skin surrounding them. Pustular psoriasis occurs mainly on the hands and feet.
Nail psoriasis
Fingernails and toenails are affected in nail psoriasis. In which the nails are white, yellow or brown in color and there seems to be a drop of blood or oil under the nail plate. The skin inside the nail becomes thicker and the nail separates from the nail plate.
How to diagnose psoriasis
History Collection
Physical Examination
Biopsy
Immunofluorescence
Ultrasound
Write management of psoriasis
Topical corticosteroids:
Topical corticosteroids are used in the treatment of mild and moderate psoriasis. Corticosteroids reduce the information and
Vitamin D analogues:
Vitamin D analog creams are applied with steroid creams that reduce skin cell production. For example calcitriol, calcipotriol
Calcineurin inhibitor:
Calcineurin inhibitors decrease the activity of the immune system and reduce inflammation. For example tacrolimus ointment
Coal tar :
Call Tar is used when other topical treatments are not effective. Charcoal reduces scaling, itching and inflammation.
Retinoid cream:
Retinoid cream is a synthetic form of vitamin A. which is administered with steroids.
Immunosuppression drugs:
Immuno suppressants such as methotrexate, cyclophosphamide are used to suppress immunity.
Phototherapy:
In phototherapy, the skin is exposed to UV light which decreases the growth rate of epidermal cells.
Systemic corticosteroids:
Systemic corticosteroids are used in severe cases.
Write nursing management of psoriasis
To assess vital signs.
Assessing skin integrity.
Provide a comfortable position to the patient.
Educate the patient about skin care.
Advise the patient to bathe with warm water instead of hot water.
Advise the patient to avoid rubbing and friction on the affected area.
Clean the affected area and apply topical medicine.
Providing psychological support to the patient.
Reassuring the patient and his family members.
Administer the medicine prescribed by the doctor.
To maintain records and reports.



Define skin cancer
Skin cancer is the most common cancer. Abnormal cell growth found in skin tissue is known as skin cancer.
Write cause & risk factor of skin cancer
People with light skin and fair skin
People exposed to UV light and X-rays
People with family history
People with weak immune systems
Old Age
Explain types of skin cancer
There are mainly three types of skin cancer:
1) Basal cell carcinoma
2) Squamous cell carcinoma
3) Malignant melanoma
1) Basal cell carcinoma
- Basal cell carcinoma is the most common skin cancer. In which carcinoma is seen in the basal cells in the lower part of the epidermis.
Basal cell carcinoma does not usually spread to other areas.
In which round growths of flash color are seen in the skin as well as pear like bumps and pinkish color patches are seen.
Basal cell carcinoma is more commonly seen in people with fair skin.
Basal cell carcinoma mainly affects the head, neck, arms, chest, abdomen and legs. 2) Squamous cell carcinoma
Squamous cell carcinoma is the second most common skin cancer. In which carcinoma is seen in the squamous cells of the outside layer in the skin.
In which red bumps and scaly patches are seen. Sores that heal but return to the same site.
These symptoms are mainly seen in the ears, face, neck, arms, chest and back.
Squamous cell carcinoma is more common in people with light skin color. 3) Malignant melanoma • Malignant melanoma is the most serious type of skin cancer because it spreads to surrounding areas.
In which malignancy is seen in melanocyte cells rather than producing melanin.
Malignant melanoma frequently develops moles on the screen and dark spots on the skin.
Apart from this, there are some types of cancer:
Kaposi sarcoma
Kaposi’s sarcoma is a type of skin cancer in which malignancy occurs in endothelial cells in lymph and blood vessels. In which lesions of different colors are seen in skin, lymph, oral cavity, GI tract and respiratory tract.
Markel cell carcinoma
Merkel cell carcinoma is a rare form of skin cancer. In which over growth is seen in Markel cells. Merkel cells are a special type of cell found in the epidermis.
Sebaceous carcinoma
Sebaceous carcinoma is a rare type of skin cancer that occurs in the oil glands of the skin. In which the eye lead is mainly affected and lumps and thickness are seen on the skin.
Dermatofibrosarcoma protuberans
Dermatofibrosarcoma protuberance is a rare soft tissue tumor that affects the dermis and subcutaneous tissue and often involves muscle and fascia. In which firm plaque is seen on the skin.
Explain sign & symptoms seen in skin cancer
ABCDE symptoms are mainly seen in skin cancer.
Asymmetry: Lesions are irregular in shape and lesions or moles are not similar to each other.
Border: Blurry or irregular shaped edges are seen.
Color : Spots or moles are found in different colors like white, pink, black, blue and red
Diameter: Diameter is found to be greater than that of a pencil. (6mm)
Evolving: Changes in shape, size, color and symptoms are seen.
Write management of skin cancer
Management depends on the stage of the cancer. Biopsy is also effective for small and limited cancerous cells.
Chemotherapy:
Chemotherapy consists of orally, topically, and intravenously administered drugs that kill cancerous cells.
Radiation therapy:
Radiation therapy uses strong beam energy to kill cancerous cells.
Immunotherapy:
Immunotherapy uses certain medicines that stimulate the immune system so that it kills cancerous cells.
Photodynemic therapy:
In photodynamic therapy, cancerous cells are killed by light and photosensitizing chemicals.
Crayotherapy:
Cryotherapy uses liquid nitrogen to freeze and kill cancerous cells.
Mohs surgery:
In Mohs surgery, layers are removed one by one and lastly the layer containing cancerous cells is removed.
Excisional surgery:
Excisional surgery involves removing the tumor and surrounding healthy skin through an incision.
Currete & electrodessication:
In electrodesiccation, cancerous cells are destroyed by electric current.
Burns & its management
Introduction of burns
Burn injury occurs due to direct contact with thermal, chemical, electrical and radiation.
Injuries seen in skin and tissue in contact with hot liquids, hot objects, streams, fire, sun, electricity and chemicals are known as ‘burn injuries’.
A burn injury occurs due to the transfer of energy from the hit resource to the body. This hit is transferred by means of conduction and radiation.
Human skin can tolerate temperatures up to 42-44 C. But when it comes in contact with temperature higher than this temperature, tissue destruction is seen.
Burn injury is a major global public health problem with physical, psychological and financial impact on people.
Most burns are accidental.
Burn injuries occur in people of all ages and socioeconomic groups.
Write causes of burns
Thermal burns:
Thermal burns are the most commonly seen. Thermal burns are caused by coming into contact with fire, flame, hot, liquid, hot object and steam. The severity of thermal burns depends on the temperature of the object and the duration of exposure. For example residential fire, automobile accident.
Chemical burns:
Chemical burns are caused by coming into contact with household or industrial chemicals such as strong acids, alkalis and organic compounds. Example sulfuric acid, phosphoric acid, sodium and calcium hypochlorite Chemical burns Severity depends on the concentration of the chemical, volume and duration of exposure.
Electrical burns:
Electrical burns are caused by electrical energy or electrical shock. The severity of electrical burns depends on the intensity of the current and the duration of exposure. For example, electrical burns can occur due to a hobby coming into contact with faulty electrical wiring. Electric burns are difficult to diagnose. Because no symptoms are seen on the skin but internal damage is seen.
Radiation burns:
Radiation burns are caused by contact with a radioactive source. Like UV light, X Ray, Gamma Ray. For example a nuclear bump explosion. The severity of radiation burns depends on the strength, duration, distance and surface area of the radiation.
Inhalation burns:
Inhalation burns are caused by exposure to asphyxiants, smoke. For example carbon monoxide poisoning.
Types & classification of burns
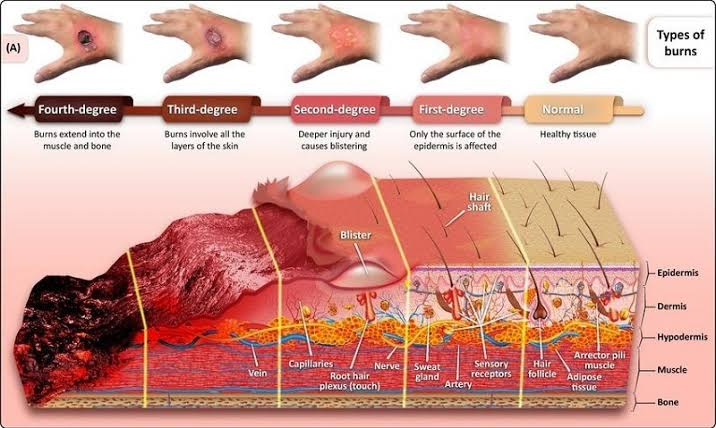
Based on the depth of the burn and its severity, it is classified as follows.
According to burn depth & severity of penetrate the skin surface
Burns are classified into first degree burns, second degree burns, third degree burns and fourth degree burns based on their depth.
The depth of burning depends on the temperature of the burning object and the duration of exposure to it.
First degree burns / superficial partial thickness
In first degree burns, the epidermis, the superficial layer of the skin, is affected and there is minimal tissue injury.
In it, the burned area is pink to reddish in color and erythema, dryness, and pain are seen at the site. That area is found to be overly sensitive (hyperesthesia).
Blister formation is not observed.
First degree burns heal within a week and car formation is not seen.
First degree burns can also be treated at home.
A sunburn is an example of a first degree burn.
Second degree burns / deep partial thickness
Second degree burns are also known as ‘dermal burns’.
In second degree burns, the epidermis and dermis layers are affected and the epidermal layer is destroyed.
Apart from this, hair follicles and sweat glands are also affected.
It involves redness, pain, swelling and blister formation at the burn site.
Second degree burns heal within 2-3 weeks and scar formation is seen.
Third degree burns / full thickness
In third degree burns, the epidermis, dermis and subcutaneous layers are affected. Epidermis and dermis layers are destroyed. Apart from this, bones, muscles, tendons and organs are also often affected.
Burned area looks waxy white and charred i.e. the area looks burnt and blackened. The area is found to be firm, leathery and dry.
Pain and sensation are not seen due to nerve endings being destroyed and damaged. Apart from this conditions like hematuria and shock are seen.
Third degree burns result in deep scars, so cosmetic or reconstructive surgery and skin grafts are used.
Third degree burns are slow-healing. Fourth degree burns
Fourth degree burns are those that have extended to the fascia. Bones, muscles, tendons and organs are also damaged.
In which the affected area looks like a dry chard and the area is painless and eschar is also seen.
These types of burns are caused by deep flame and electrical burns.
If the extremities are affected in the fourth degree, mutation is required.
According to burn severity
Depending on the severity of the burn and how much body surface area is affected, burns are divided into minor burns, moderate burns and severe burns.
Minor burns:
If less than 10% of the total body surface area is affected in children and less than 15% of the total body surface area in adults, it is known as minor burns.
Patients with minor burns can be treated on opd basis.
All first degree and second degree burns are included in minor burns.
Moderate burns:
In moderate burns, the area affected is 20 to 25% of the total body surface area. In adults, the affected area is 15 to 25% of the total body surface area, while in children, the affected area is 10 to 20 percent of the total body surface area.
Severe burns:
In severe burns, more than 20 to 25 percent of the total body surface area is affected. In adults, more than 25% of the total body surface area is affected, while in children, more than 20% of the area is affected.
Severe burns include inhalation and electrical burns.
Third degree burns and fourth degree burns are included in severe burns.
How does calculate percentage of burns
Or
Extent of body surface area injured
Different methods are used to calculate how much of the total body surface area is affected in burns. Like Rule of Nine, Lund and Browder Method, Palm Method
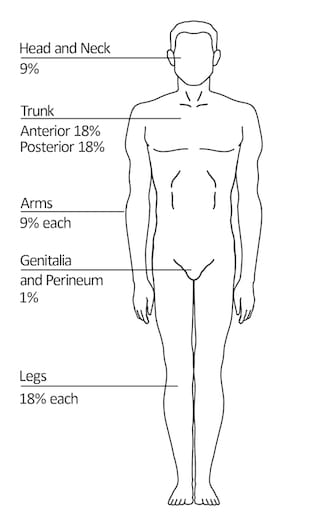
Rule of nine
The Rule of Nine is a quick method for calculating the percentage of burns in adults.
Rule of Nine is given by Alexander Wallace hence Rule of Nine is also known as ‘Wallace of Nine’.
The Rule of Nine divides the different areas into percentages as follows:
Head = 9%
Right arm = 9%
Left arm = 9%
Right leg = 18%
Left Leg = 18%
Chest = 18%
Back = 18%
Genital Area = 1%
As shown above, the percentage of total body surface area affected can be determined.
This method is not used in infants and children because the body area size of children is less than that of adults.
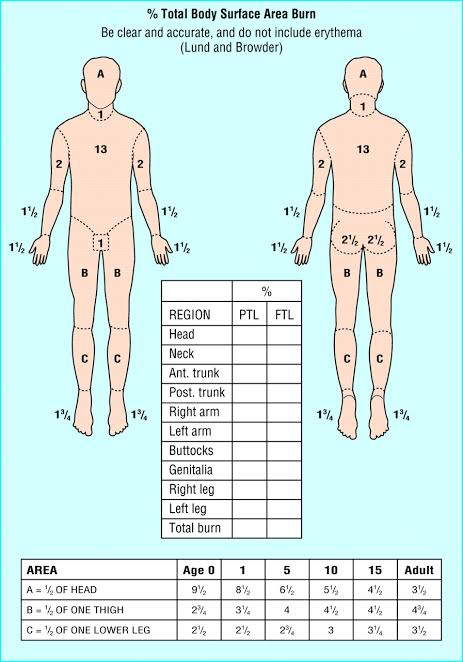
Lund & browder method
The Lund and Browder method is the most accurate and precise method for estimating total body surface area in children and adults.
Because in this method percentages are given according to the size of different body areas of children and adults. As in children the head is big while the size of the extremities is small. Hence in children the head is given a higher percentage whereas in adults the head is given a lower percentage than that.
The percentage is calculated as shown in the table below.
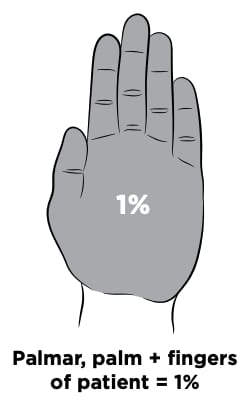
Palmar method
The Palmer method becomes more useful and effective when the burn injury is small, irregular or patchy.
In this method, the palm of the patient’s hand is considered to be 0.5% of the total body surface area and the palm and fingers are considered to be 1%.
Thus the burn injury at different places in the body is calculated with the help of Palmer method.
This method is used in both children and adults.
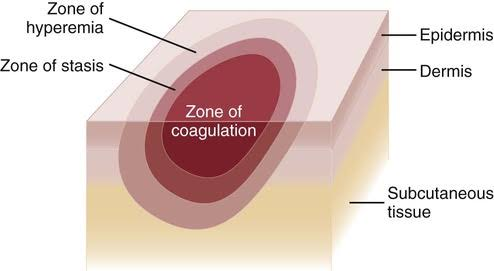
Jackson burn model
The Jackson burn model helps to understand the pathophysiology of burn wounds.
In this model, the damaged tissue is divided into 3 zones:
Zone Coagulation, Zone Stasis and Zone Hyperemia Zone coagulation:
The zone of coagulation is the most central area of the burn in which the tissue is severely damaged and is reversible.
Zone stasis:
The area surrounding the zone of coagulation is known as the zone of stasis. There is less damaged tissue and there is vascular transudate, inflammatory reaction and impaired tissue perfusion. If a good environment is provided then the tissue recovers otherwise necrosis occurs.
Zone hyperaemia:
Zone hyperemia is the outermost layer of the burn where increased blood flow due to vasodilation leads to faster tissue recovery and reduced chances of necrosis.
Explain pathophysiology of burns
A burn injury occurs due to the transfer of heat resources or energy to the body.
The severity of a burn injury depends on the temperature of the heating agent and the duration of exposure.
A primary local response occurs if the area affected is less than 25% of the total body surface area, but a local and systemic response occurs if the area affected is greater than 25% of the total body surface area. First 24 to 48 hours following burn injury Coagulation necrosis is seen in the soft tissue.
|
Vasoactive substances and inflammatory mediators are released. (eg cytokines, histamine, oxidase, catecholamine)
|
This results in increased vascular integrity and capillary permeability and vasodilation.
|
Hence the fluid shifts from the intracellular space to the interstitial space.(Most of the fluid is shifted within 12 hours and this process is seen to be continuous for 30 hours)
|
Peripheral edema develops due to fluid shift and increases tissue colloid osmotic pressure and fluid electrolyte imbalance.
|
On the other hand, there is a decrease in intravascular volume so that blood volume decreases and cardiac output also decreases.
|
Thus this stage is also known as hypovolemic stage. After 48 to 72 hours of burn
48 to 72 hours after the burn
|
Vascular integrity and capillary permeability return and normalize.
|
Fluid returns from the interstitial space to the intravascular space thereby reducing peripheral edema.
|
Intravascular volume increases. (Fluid overload may also occur often.) (Hence this fluid is excreted through urine. Hence this stage is also known as the diuretic stage.)
|
This also increases blood volume and increases cardiac output.
|
This results in increased blood flow to all organs and tissues.
Explain local & systemic effect of burns
Local effect of burns:
In a burn injury, if the area affected is less than 25 percent of the total body surface area, a local effect is seen.
Tissue damage:
Exposure to high temperature causes tissue and cell damage and necrosis.
Edema:
Fluid shifts from the intravascular space to the interstitial space causing edema.
Inflammation:
A burn injury causes our body to respond by releasing inflammatory mediators and causing inflammation. Redness, erythema, swelling and blister formation are observed in the affected area.
Infection:
Microorganisms grow and enter the body due to tissue destruction and breakdown of skin integrity. Hence infection is seen.
Systemic effects of burns:
Local and systemic response is observed in burn injury if the area affected is more than 25% of the total body surface area.
This systemic effect is due to release of vasoactive substances and inflammatory mediators. Like histamine, cytokines, oxidase, catecholamine
Cardio vascular alteration:
There is a decrease in cardiac output.
This results in hypotension and tachycardia.
RBCs are destroyed.
The hematocrit level increases and the plasma level decreases.
Abnormalities in coagulation are seen.
Cardiac dysrhythmias are seen in electrical burns.
Pulmonary alteration:
Pulmonary alteration occurs due to inhalation burns.
Bronco constriction is seen.
There is increased secretion and congestion.
Obstruction is seen in the airway.
Stider and horseness sounds are observed.
Pulmonary edema is seen.
Hypoxia is observed.
Renal alteration:
Renal function is altered due to decreased renal blood flow.
A decrease in glomerular filtration rate is observed.
Blood is seen in the urine.
GI alteration:
Intestinal paratalaxis is decreased in movement and bowel sounds are also decreased.
Metabolism increases.
Bleeding in the GI tract causes vomiting and blood in the stool.
Stress and ulceration are seen.
Immunologic alteration:
Damage to the skin barrier allows micro-organisms to grow and enter the body and cause tissue infection.
Thermoregulatory alteration:
Due to loss of skin, the function of regularizing body temperature is altered, hence the condition of hypothermia is seen.
Fluid & electrolyte alteration:
Conditions such as hyponatremia and hyperkalemia are seen.
Immediate care of burns patients
Move the victim away from the scene.
To remove burnt cloth and jewelery worn by the patient.
Assess the patient for airway, breathing and circulation.
If breathing is not present, clear the airway and provide CPR.
Flush the burn area with running water and cover the wound.
Transfer the patient to the nearest hospital.
Provide oxygen therapy to the patient if required.
Securing patient iv line.
Administer intravenous fluids.
Write first aid care of burns injury
Move the victim away from the scene and check that the patient does not come in contact with burning material.
To remove burnt cloth and ornaments worn by the victim. If the cloth is stuck to the body area, do not remove it.
Then check the victim for airway, breathing and circulation.
If breathing is not present, clear the airway and provide CPR.
If the patient is breathing, apply full running water to the affected area.
If the fingers are stuck together due to burns, gently separate them.
Then cover the wound loosely with a clean cloth. So that contamination can be prevented and air can be prevented from coming in contact with the surface.
Avoid friction and pressure on the burned area.
Do not apply any kind of ointment or cream on the area.
.