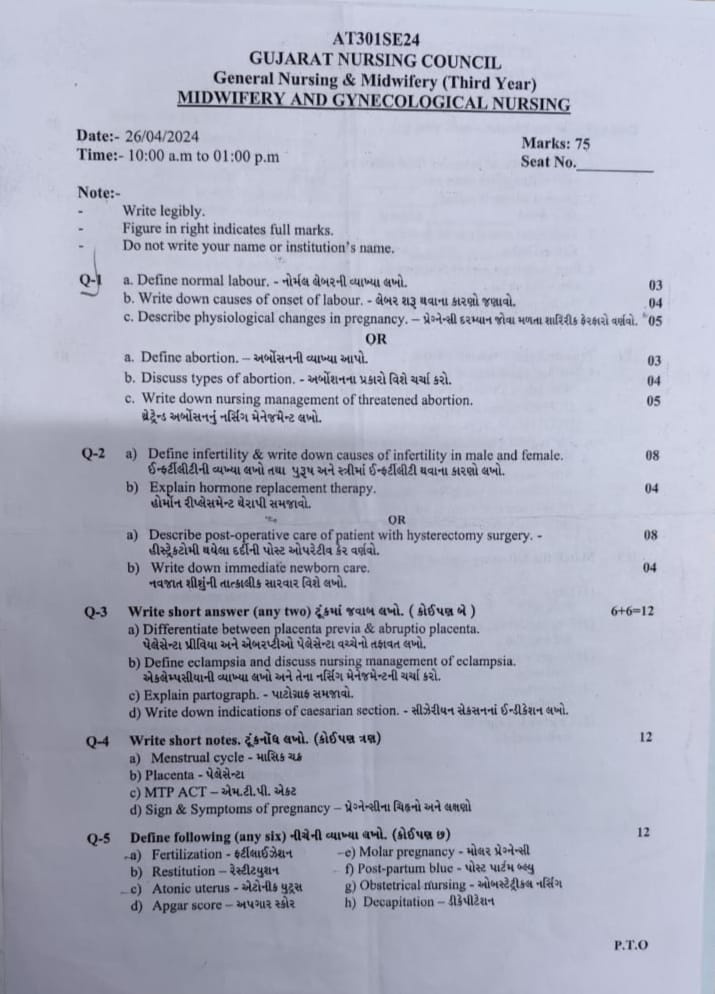
ENG.GNM.T.Y-midwifery-26/04/2024 (paper solution no .8 )-UPLOAD
ENG.GNM.T.Y-midwifery-26/04/2024
Q.1 a. Define normal labour. – નોર્મલ લેબરની વ્યાખ્યા લખો.
- Labor
The series of events that occur in the genital organs to bring out the viable product of conception from the uterus (womb) to the outside world through the vagina is called “labor”. - A woman who is in labor is called a “parturient”.
- And the process of giving birth is called “parturition”.
- Normal labor is also called euthanasia.
- Normal labor is said to be when the following criteria are fulfilled.
- 5) There should be no complications that affect the health of the mother and the baby.
- 1) The onset of labor should be spontaneous and at term (37 to 48 weeks).
- 2) The fetus should be in vertex presentation (the occiput of the fetus’s head should be in the lower part of the uterine cavity and the fetus’s chin should be tucked against its chest).
- 3) The duration of labor should not be too long (i.e. if the mother is a primary gravida, the average duration of labor should be 12 hours and if the mother is a multipara, the average duration of labor should be 6 hours)
- 4) The birth should be natural with minimal assistance.
b. Write down causes of onset of labour. – લેબર શરૂ થવાના કારણો જણાવો.
- Causes of labor onset:
- No specific cause for labor is known but it is said that many factors are responsible for the onset of labor such as,
- 1) Mechanical causes,
2) Hormonal causes,
3) Neurological causes - 1) Mechanical causes,
These include,
Heightened reflex irritability of the uterus,
Uterine distension,
Menstrual period suppression,
Prolonged pressure of the fetus. - 2) Hormonal causes:
- 1) Feto-placental contribution
The fetal hypothalamus is triggered to produce releasing factors.
These releasing factors stimulate the anterior pituitary gland to produce adrenotrophic hormone
(ACTH). - Adrenotrophic hormone
(ACTH) stimulates the fetal adrenal gland to secrete cortisol. - Cortisol causes changes in placental hormones.
Ex:=
Estrogen levels increase,
Progesterone levels decrease. - 2) Estrogen hormone: Estrogen increases the following possible mechanisms:
- 1) Oxytocin release from the maternal pituitary increases.
- 2) Oxytocin stimulates myometrial receptors to synthesize prostaglandins.
- 3) Prostaglandin synthesis increases by decidual and amnion cells.
- 4) Myometrial contraction stimulates the synthesis of the protein actomyosin.
- 3) Progesterone
Progesterone has a relaxant effect on the uterus.
Progesterone is produced first by the corpus luteum and then by the placenta.
It inhibits uterine contractility.
Fetal production of dehydroepiandrosterone sulfate (DHEA-S) and cortisol increases, which prevents the conversion of progesterone from fetal pregnenolone.
Thus, progesterone levels fall before labor while estrogen levels rise.
Then the progesterone level falls down which is associated with the synthesis of prostaglandins. - 4) Oxytocin:
Oxytocin hormone is released from the mother’s posterior pituitary gland.
Due to the increase in estrogen levels, it helps in increasing the level of oxytocin.
At the end of pregnancy, oxytocin receptors increase in the decidua vera. Oxytocin acts directly on the myometrium and causes contraction of the uterus.
Apart from this, it also acts on the endometrial tissue so that prostaglandins are released. - 5) Prostaglandins
The major sites of prostaglandin formation are the placenta, fetal membrane, decidual cells and myometrium.
It is said that due to the release of estrogen, the decidua releases prostaglandins, which act on the uterine muscles, causing the uterine muscles to contract. - 3) Neurological causes
Labor can be initiated through nerve pathways.
Both ‘α’ and ‘β’ adrenergic receptors are present in the myometrium.
Estrogen acts on the ‘α’ receptor and progesterone on the ‘β’ receptor. - 1) ‘α’:=’α’ adrenergic receptor stimulates ‘α’ receptor.
- 2) ‘β’:=’β’ adrenergic receptor stimulates ‘β’ receptor.
- Contractile response from ‘α’ receptors of prostaglandin nerve fibers located in and around the cervix and in the lower part of the uterus starts when progesterone is reduced.
- Thus, the reasons for the start of this labor are as follows.
c. Describe physiological changes in pregnancy. – પ્રેગ્નેન્સી દરમ્યાન જોવા મળતા શારિરીક ફેરફારો વર્ણવો.
- Physiological Changes During Pregnancy
- Pregnancy is a condition from the time of conception to the time of delivery. Due to certain types of specific hormones, physiological changes are observed in the mother’s body during pregnancy. These changes occur to nurture the fetus, prepare the mother’s body for labor, and to produce the best milk during the puerperium period.
- 1) Changes in Reproductive System
- A) Vulva:=
- The vulva becomes more edematous and vacuolated.
- In multipara, superficial varicosities (varicose veins: = veins become enlarged and swollen, usually found in the legs and also in the pelvic area during pregnancy) and labia minora become pigmented and hypertrophy (increase in the size of the organ).
- B) Vagina: =
- The vaginal wall becomes hypertrophied,
- edematous and more vascular.
- Increased venous blood supply to the vaginal wall gives a bluish coloration of the vaginal mucosa, which is called “Jacquemier’s sign”.
- The length of the anterior wall increases.
- The vaginal secretion is more acidic, thin and curdy white.
- The acidic pH of vaginal secretions prevents the multiplication of pathogenic microorganisms.
- (C) Uterus:= During pregnancy, the uterus grows to a greater extent. The weight and length of the uterus also increase during pregnancy.
- Weight of Uterus: In the non-pregnant state, the weight of the uterus is about 60 gm, which increases to 900 – 1000 gm during pregnancy (at term).
- Length, Width and Thickness of Uterus:
- In non-pregnant state, the length of the uterus is 7.5 cm, width is 5 cm and thickness is 2.5 cm.
- While during pregnancy (at term), the length of the uterus is 30-35 cm, width is 22.5 cm and thickness is 20 cm.
- Volume of uterine cavity: In non-pregnant state, the volume of the uterus is 10 ml, which increases to 5 liters during pregnancy.
- Body of Uterus: The body of the uterus grows and enlarges.
- Muscles
- 1) Outer:= Longitudinal layer
- 2) Middle:= Vascular layer
- 3) Inner:= Circular layer
- Hypertrophy (increase in size) and hyperplasia (increase in number) are seen in the muscles.
- After 20 weeks of pregnancy, the length of the uterine muscle fibers increases and the uterine wall becomes thinner, due to which the uterus becomes softer and more elastic in the gravid condition than in the non-gravid condition.
- Vascular system:
- Blood supply starts increasing from 20 weeks due to vasodilation caused by estradiol and progesterone.
- The diameter of the uterine artery doubles and blood flow increases and the veins dilate.
- During pregnancy, the endometrium of the uterus is called decidua.
- Braxton Hicks contractions:
- In the beginning of pregnancy, the uterus contracts spontaneously. They are irregular, infrequent, spasmodic and painless, so they do not affect the dilation of the cervix. They increase towards term (37-42 weeks) and finally merge with the painful contractions of labor.
- D) Isthmus:=
- During pregnancy, the lower segment of the uterus forms an isthmus.
- In the non-pregnant state, the length of the isthmus is 0.5 cm, which increases during pregnancy to 7.5 cm-10 cm.
- The muscle fibers of the isthmus are arranged circularly in the lower segment and form a sphincter-like structure, which helps the fetus to stay in the uterus during early pregnancy. If this sphincter is incompetent, then abortion can also occur.
- E) Cervix:=
- During pregnancy, the cervix becomes vascular, edematous, hypertrophied and hyperplastic.
- The cervix becomes soft, which is called “Goodell’s sign”.
- The length of the cervix doubles and its volume also increases.
- F) Fallopian tubes:=
- The length of the fallopian tubes increases slightly. The tubes become congested. The muscles hypertrophy and the epithelium becomes flat.
- G) Ovary:=
- Ovulation stops during pregnancy. The ovaries become hypertrophied and vascularized.
- The corpus luteum, which was the usual menstrual cycle, remains and enlarges by 2.5 cm for 8 weeks and this is due to changes in the fertilized egg (trophoblast) and helps in producing hormones. By the 12th week, acoloid degeneration occurs and the egg becomes calcified. The corpus luteum produces estrogen and progesterone hormones and provides an environment to maintain the ovum until the action of the placenta starts.
- H) Breast:=
- During pregnancy, due to the effects of estrogen and progesterone, the vascularity of the breast increases, along with the increase in size, nodularity and sensitivity of the breast.
- The nipple becomes enlarged, dark and erectile.
- Hypertrophy of 5 to 15 sebaceous glands, which are invisible in the non-pregnant state, is observed, which are called “Montgomery tubercles”. They are located around the nipple, and their secretion keeps the nipple and areola moist and healthy.
- The areola becomes dark and pigmented, which is called the primary areola.
- In the second trimester, a second pigmented zone forms around the primary areola, which is called the secondary areola.
- In the first three months, the ductal system in the breast increases in size and as the pregnancy progresses, its alveolar cells become secretory.
- The total weight of the breast is about 0.4 kg.
- Alveolar proliferation and fat deposition cause breast enlargement and a clear sticky fluid can be squeezed from the breast at about 12 weeks.
- At 16 weeks, this clear sticky fluid becomes thick and yellow, which is called colostrum, which is an important sign of pregnancy.
- Changes in other systems of the body.
- 1) Skin Changes:=
- A) Face: Pigmentation is seen around the cheeks, forehead and eyes which is called “graviderma masque” or “pregnancy mask” which disappears on its own after delivery.
- B) Breast: Visible pigmentation changes occur in the breast.
- C) Abdomen:
- Linea Nigra Due to melanocyte stimulating hormone, a brownish black colored line becomes visible in the midline from the zygosternum to the symphysis pubis which is called linea nigra.
- Striae Graviderum
- Depressed linear marks are seen on the abdominal wall below the umbilicus and sometimes on the breasts, which are initially pink but become glistening white after delivery and are called striae albicans or striae gravidarum.
- High estrogen levels cause vascular spider veins and palmar erythema. Skin
- Mild degree of hirsutism (excess hair) is seen and hair is lost in excess amount during the puerperium period.
- 2) Weight gain Weight loss occurs during the first weeks of pregnancy due to nausea and vomiting. Weight gain remains progressive from the following months.
- A healthy woman gains an average of 11 kg (24 lbs) of weight during pregnancy.
- During the 1st trimester: 1kg,
During the 2nd trimester: 5kg,
During the 3rd trimester: 5kg, - The amount of weight gained is:
- A) Reproductive weight gain
- 1) Weight of fetus: 3.3kg,
- 2) Weight of placenta: 0.6kg,
- 3) Weight of placenta: 0.8kg,
- 4) Weight of uterus: 0.9kg,
- 5) Weight of breast: 0.4kg.
- B) Net Maternal Weight Gain
- 1) Increase Blood Volume:=1.3kg,
- 2) Increase Extracellular Fluid:=1.2kg,
- 3) Fat and Protein:=3.5kg.
- 3) Cardiovascular System
- A) The heart has to work more during pregnancy.
Cardiac volume increases by 10% but there is no change in ECG.
Cardiac output also increases due to increase in heart rate and stroke volume.
Pulse rate also increases.
Platelet count slightly decreases due to increase in concentration rate by 40 to 45 mm. - B) Blood Pressure and Blood Volume: Blood pressure remains within normal limits. In some women, diastolic pressure drops by 5 to 10 mm during mid-pregnancy.
- C) Venous pressure: Due to the pressure of the gravid uterus on the pelvic veins, the femoral venous pressure increases by about 10 cm. After that, the blood volume also increases. The volume of red blood cells and plasma volume also increase. Blood flow increases in many parts of the body such as the uterus, pulmonary, renal, skin, and mucosa.
- 4) Respiratory system
- Hyperemia (increased blood flow) and congestion are seen in the upper respiratory mucosa.
- Due to increased inspiration, oxygen intake also increases and oxygen supply to the fetus also increases.
- Due to increased expiration, carbon dioxide is released, so due to low maternal carbon dioxide, the transfer of carbon dioxide from the fetus to the mother’s blood can easily occur.
- In the last weeks of pregnancy, the pressure of the gravid uterus on the diaphragm causes complaints of breathing difficulty, which is reduced by lightening.
- 5) Digestive system
- Due to the effect of progesterone, the muscle tone of the gastrointestinal system decreases.
- Relaxation of the cardiac sphincter leads to regurgitation of stomach contents and heartburn.
- Due to the decrease in gastric size, it empties slowly, which continues even in labor.
- In many women, the gums become spongy and vascular, which can cause bleeding during brushing.
- Decreased intestinal volume leads to better absorption of food and constipation.
- 6) Nervous system
- Mood changes occur during pregnancy and the puerperium period. Psychological conditions include nausea, vomiting, mental irritability, and insomnia.
- Depression or psychosis may also develop in women.
- Compression of the median nerve in the wrist causes pain and paresthesia (tingling) in the hands and arms. This is called carpal tunnel syndrome. It occurs in the last month of pregnancy. Similarly, sensory loss is seen in the legs due to pressure on the cutaneous nerves.
- 7) Urinary Tract
- Frequent micturition is common in early and late pregnancy.
- Stress incontinence can also occur.
- Dilatation of the uterus and pelvis continues from early pregnancy to mid-pregnancy, leading to urinary stasis and infection. Renal function also increases in pregnancy.
- 8) Locomotor System
- Thus, physiological changes are seen in women during pregnancy.
- Back pain is common due to lordosis and relaxation of joints due to the relaxin hormone in pregnancy.
- Leg cramps occur due to weight on the sacral and lumbar plexuses and difficulty in walking also occurs.
OR
a. Define abortion.-અર્બોસનની વ્યાખ્યા આપો.
- Abortion is the process by which pregnancy is terminated. In abortion, the product of conception is partially or completely separated and expelled from the uterine wall before the age of viability (28 weeks). This condition is called “abortion”.
- If abortion occurs spontaneously, it is called “miscarriage”. And if it is done purposefully, it is called “induced abortion”.
- Majority abortion or miscarriage occurs during the first trimester of pregnancy, i.e. during the first 12 weeks of pregnancy, it is called “early miscarriage”. And a miscarriage that occurs after 13 weeks of pregnancy is called a “late miscarriage.”
b. Discuss types of abortion. – અર્બોશનના પ્રકારો વિશે ચર્ચા કરો.
- The types of abortion are as follows.
- 1) Spontaneous abortion :
- A) Threatened abortion,
- B) Unavoidable abortion,
- C) Complete abortion,
- D) Incomplete abortion,
- E) Silent or missed abortion,
- D) Septic abortion,
- E) Recurrent abortion or habitual abortion,
- 2) Induced abortion
- 1) Spontaneous abortion:
- When abortion occurs naturally without any kind of medical or surgical intervention, it is called spontaneous abortion. Its cause can be any genetic abnormality and maternal condition.
- A) Threatened abortion:
- In threatened abortion, the process of abortion starts but does not reach a stage where recovery is impossible, i.e., if proper care is taken, recovery can occur.
- B) Inevitable abortion:
- Inevitable abortion is a type of abortion in which the expulsion of the conceptus progresses along with cervical dilation. In this case, the pregnancy cannot be saved because most of the placenta has detached (from the uterine wall). This is a clinical type of abortion in which the changes in the abortion have progressed to the point where continuation of the pregnancy becomes impossible.
- C) Complete Abortion:
- Complete abortion is a type of abortion in which the product of conception is expelled out in the form of a mass, it is called complete abortion.
- D) Incomplete abortion:
- Incomplete abortion is a type of abortion in which the entire product of conception is not expelled out of the uterine cavity but some part of it remains in the uterine cavity, then this abortion is called incomplete abortion.
- E)Silent or Missed Abortion:
- Silent or missed abortion is said to occur when the fetus dies in the uterine cavity and is retained in it for more than 4 weeks.
- D) Septic abortion:
- When there is evidence of infection of the uterus and its contents along with the abortion, i.e. if the abortion is due to any infection, then this abortion is called septic abortion.
- E) Recurrent abortion or habitual abortion:
- When three or more spontaneous abortions occur in a sequence before 20 weeks, then it is called recurrent abortion.
- It is caused by immunoglobulin G, hormonal deficiency, and cervical incompetence. Other causes include genetic factors, infection, endocrine, and anatomical abnormalities.
- 2) Induced abortion:
Induced abortion means the termination of pregnancy voluntarily using any medical or surgical procedure. - Medical abortion:
- Medication is used to terminate pregnancy in medical abortion and
Medical abortion remains effective up to 10 weeks of pregnancy. - Ex:= combination of Mifeprostone and misoprostol.
- Surgical Abortion:
- In this, a surgical procedure is performed by a health care personnel and the pregnancy is terminated. It is called surgical abortion Ex: vacuume Aspiration.
c. Write down nursing management of threatened abortion. થ્રેટેન્ડ એબોર્શનનું નર્સિંગ મેનેજમેન્ટ લખો.
- Nursing Management of Threatened Abortion:
- Nursing management of threatened abortion involves proper assessment and monitoring of the pregnant woman.
- Provide proper supportive care to the woman.
- 1)Assessment:-
- Vital signs
- Continuously monitor the mother’s vital signs. Such as,
- pulse,
- blood pressure,
- temperature,
- respiration etc.
- Bleeding assessment:- Assess the color, amount, intensity and consistency of vaginal bleeding.
- History collection:- Collect proper history of the mother including complete history of previous pregnancy and abortion.
- 2) Monitoring and Observation:-
- Continuous observation of the mother to assess whether she has any signs and symptoms of shock (hypotension, tachycardia, pallor).
- Proper investigations of the mother including hemoglobin, hematocrit, ultrasonography, ABO & Rh grouping should be done routinely.
- 3) Bedrest and Physical Activity:-
- Advise the mother to take complete bed rest.
- Advise the mother to limit physical activity.
- Advise the mother not to do household work for a month.
- 4) Emotional Support:-
- Provide emotional support and reassurance to the mother and her family.
- To properly clear the doubts and queries of the mother and her family members.
- Do not give false reactions to the mother and her family members.
- 5) Education:-
- Provide education to the mother about the signs and symptoms of abortion such as increased bleeding, severe pain etc. and advise her to seek immediate medical treatment if any such signs and symptoms are seen.
- Provide education to the mother to take proper follow-up.
- 6) Hydration and Nutrition:-
- Advise the mother to take adequate fluid intake.
- Continuously monitor the mother’s intake output chart.
- Advise the mother to take a properly balanced diet.
- Advise the mother to take a high fiber diet to prevent constipation.
- Provide supplements to the mother with good fitting.
- Ex:= Ferrous Sulphate 200 mg( BD. ),
- Folic Acid 5 mg/ day( TDS ).
- Provide the mother with a diet rich in high protein and Vitamin E.
- 7) Medication Administration:-
- Provide the mother with prescribed medication.
- Provide medication to control bleeding and relieve pain.
- Provide education to the mother about the dosage, direction and side effects of the medication.
- If the mother has problems of sleep and anxiety, then provide Tab.Diazepam, ( 5-10 mg before night meal ),
Or Tab.Calmpose, ( 5-10 mg before night meal ),
Or Tab.valium ( 5-10 mg before night meal ),
to relieve it. - Provide mild amount of laxative to the mother at bed time for good bowel activity.
Ex:= Milk of Magnesia. - Do not provide enema to the mother because enema is responsible for stimulating uterine contractions in the mother.
Provide mild amount of laxative or suppository to the mother after 48 hours of signs and symptoms of threatened abortion to relieve constipation if there is any. - 8) Consultation and Referral:-
- Properly collaborate with other health care personnel for care.
- Provide timely referral services to the mother, if necessary.
- 9) Documentation:- Timely document the mother’s assessment findings, interventions provided, and any changes in the mother’s condition.
- 10) Follow-up:-
- Nursing management of threatened abortion is generally provided to provide proper comprehensive care to the mother and to bring about improvement in the mother’s condition.
- Advise regular follow-up for the mother’s progress and reassessment.
Q-2
a) Define infertility & write down causes of infertility in male and female. ઈન્ફર્ટીલીટીની વ્યખ્યા લખો તથા પુરૂષ અને સ્ત્રીમાં ઈન્ફર્ટીલીટી થવાના કારણો લખો.
- Definition:
- Infertility is a medical condition in which there is an inability to conceive a pregnancy despite having regular and unprotected intercourse for 1 year or more. Such a condition is called infertility.
- It affects about 10-15% of couples worldwide. Infertility can be due to various factors affecting the male, female or both, and it can be temporary or permanent.
- Types of Infertility
Infertility is generally of two types. - 1) Primary Infertility,
- 2) Secondary Infertility
- 1) Primary Infertility:- It refers to a patient who has not been able to conceive a pregnancy even once.
- 2) Secondary Infertility:- In this, previous pregnancy indicates that the woman has conceived but then the pregnancy fails to conceive, it is called secondary infertility.
- Causes of Infertility
- There are three main causes of infertility.
- 1) Fault in Female,
- 2) Fault in Male,
- 3) Combined Factor.
- 1) Fault in Female:-
- A) Ovarian Factor:- This is seen due to ovulatory dysfunction, mainly its three reasons are as follows.
- a) Anovulation/Oligoovulation:-
- Anovulation/Oligoovulation is usually seen due to disturbances in the hypothalamic pituitary ovarian axis.
- Ovarian activity depends on gonadotrophins and normal secretion of gonadotrophins depends on GnRH (gonadotrophin releasing hormone) released from the hypothalamus.
- (b) Luteinized Unruptured Follicle (LUF)
- (Trapped Ovum):- This is seen due to inadequate growth and function of corpus luteum.
- (C) Trapped Ovum:- In this, the ovum is trapped inside the follicles, usually due to endometriosis or hyperprolactinemia.
- 2) Tubal Factors:- In this, infertility is usually due to tubopathy (tubal infection) due to which tubal functions are impaired.
- Ex:= Defective ovum pickup and then infertility is seen.
- 3) Peritoneal Factor:- In this, one and the main factor of infertility is endometriosis.
- 4) Uterine Factor:- In this, some factors are seen due to factors that stop the fertilized ovum from implanting in the endometrium.
- These factors are like,
- a) Endometriosis,
- b) Fibroid uterus,
- c) Uterine hypoplasia,
- d) Congenital malformation of the uterus.
- 5) Cervical Factors:- In this, it is seen due to second degree uterine prolapse, retroverted uterus, and changes in the composition of the cervical nucleus.
- 6) Vaginal Factor:- This includes vaginal atresia, transverse vaginal septum, etc.
- 2) Fault in Male:
- 1) Due to defective spermatogenesis:-
- This causes infertility and is usually due to the following reasons:
- Orchitis,
- Undescended testes,
- Testicular toxins,
- Primary testicular failure,
- Due to genetic or chromosomal disorders such as 47,XXY,
- Due to endocrine factors such as thyroid dysfunction.
- 2) Due to obstruction of the afferent duct system:-
This is seen in two types. - 1) Congenital:- Due to absence of vas deferens.
- 2) Acquired: – This is usually seen due to some infections, tuberculosis, gonorrhea, and surgical trauma (during herniorrhaphy).
- 3) Failure to deposit sperm in vagina: –
- In this, sperm is deposited in the vagina due to failure.
- The reasons for this are:
- Impotence,
- Ejaculatory failure,
- Hypospadiasis,
- Bladder neck surgery.
- 4) Due to errors in seminal fluid: – In this, due to immotile sperm, due to sperm count disturbance, due to low fructose count.
- 3) Combined factor: – In this, infertility is seen due to combined factors of both male and female.
b) Explain hormone replacement therapy. હોર્મોન રીપ્લેસમેન્ટ થેરાપી સમજાવો.
- Hormonal replacement therapy (HRT) is a medical treatment that involves supplementing or replacing hormones that the body no longer produces in sufficient quantities, mainly in cases such as menopause, andropause or other hormonal imbalances. Its aim is to relieve symptoms and reduce the risks associated with hormonal imbalance.
Purpose of HRT :-
Menopause :-
Relieves symptoms such as hot flashes, night sweats , sleep disturbances, vaginal dryness. Prevents long-term effects such as osteoporosis and cardiovascular risks. - Andropause (in men): Treats testosterone deficiency, improves muscle strength, libido and energy.
Other conditions :-
Premature ovarian failure,
Hypogonadism :-
Post operative conditions such as hysterectomy, oophorectomy, gender-affirming therapy in transgender individuals. - Types of HRT
- Estrogen-only therapy (ET):
Used in women who have had a hysterectomy (no uterus).
Common forms: estradiol, combined estrogens. - Combined estrogen-progestogen therapy (EPT):
For women with an intact uterus to prevent endometrial hyperplasia or cancer.
Progestogen option:
Progesterone, medroxyprogesterone acetate.
Testosterone replacement therapy (TRT):
Used in men with low testosterone levels.
Administered by injection, gel, or patch.
Other hormonal - combination: For transgender individuals (e.g., estrogen for transfeminine individuals, testosterone for transmasculine individuals).
Root of administration Oral tablets:
Easy to use but may have a higher risk of side effects such as blood clots. Transdermal patches and gels:Applied to the skin; bypasses the liver and reduces risks. Injections:
Testosterone or other hormones given intramuscularly or subcutaneously. Vaginal preparation:
Creams, rings or pills for local symptoms such as vaginal dryness. Implants:
Long-acting hormone pills placed under the skin. Benefits of HRT For women:
Relief from menopausal symptoms. Prevention of osteoporosis. Improvement in mood, sleep and overall quality of life. For men:
Improve energy and libido, bond density and muscle mass. Improved mood and mental clarity. For transgender individuals:
Facilitates gender-affirming physical changes. Improves mental well-being and reduces gender dysphoria.
Estrogen-related risk and side effects:
Increased risk of blood clots (deep vein thrombosis, pulmonary embolism). Risk of breast cancer (combination therapy). Risk of stroke or heart disease (depending on age and time since menopause).
Progestogen-related:
Risk of mood swings, weight gain, bloating, breast tenderness.
Testosterone-related:
Acne, oily skin. Risk of sleep apnea. Possible effects on fertility.
Contraindications absolute:
Active or history of breast or endometrial cancer.
Undiagnosed vaginal bleeding. Active thromboembolic disorders. Severe liver disease.
History of cardiovascular disease, uncontrolled hypertension. Monitoring and follow-up Regular follow-ups to monitor hormone levels, side effects, and therapeutics efficiency. Regular checkups for breast and endometrial health. Bone density monitoring for osteoporosis.
OR
a) Describe post-operative care of patient with hysterectomy surgery. – હીસ્ટ્રેકટોમી થયેલા દર્દીની પોસ્ટ ઓપરેટીવ કેર વર્ણવો.
- Immediate care
:- Strictly provide care during recovery period:
Check blood pressure every 15 minutes
Record temperature every two hours
Check wound every half hour for blood loss
Place mother in left lateral position until she regains complete consciousness because general anesthesia poses a risk of airway obstruction
Regurgitation or silent aspiration of stomach contents
Change mother’s gown and towels after removing from operating table. - First 24 hours:-
Continue observation of patient for six to eight hours, periodically checking pulse, blood pressure, bleeding.
Fluids:-
Continue infusion of 2-2.5 litres of 5% dextrose, ringers lactate drip. Blood transfusion is given to anemic patients for post-operative recovery. If there is more than average blood loss during the operation, then blood transfusion is required.
Prophylactic antibiotics are given in the first 48 hours.
Analgesic such as pratidin hydrochloride 75- 100 mg is administered.
Ambulation:-
The patient can sit on his bed and can also get out of the bed for a walker if his condition is normal. Encourage the patient to move his legs and ankles so that deep vein thrombosis and pulmonary embolism can be minimized. - Second day:- The patient is given oral feeding. Slight abdominal discomfort due to intestinal paralysis is observed.
- Third day :-
Light solids are provided as per the convenience of the patient. To relieve constipation, 4-6 teaspoons of milk of magnesia are given during the night. - Discharge :-
The patient is discharged after providing health education on home care to the relatives and is explained for regular follow-up.
b) Write down immediate newborn care. નવજાત શીશુંની તાત્કાલીક સારવાર વિશે લખો.
- Immediate Newborn Care:
- Immediate Newborn Care involves properly assessing and stabilizing the newborn.
- Immediate Newborn Care is crucial for the fetus to transition from intrauterine life to extrauterine life.
- Goals of Immediate Newborn Care
- 1) To establish, maintain, and provide support for the newborn’s respiration.
- 2) To prevent the newborn from overheating and hypothermia.
- 3) To prevent the newborn from getting infections.
- 4) To provide safety to the newborn and prevent it from injury.
- 5) To provide immediate treatment for any actual or potential problem in the newborn by early identification.
Immediate newborn care is provided. - ••>Immediate Newborn Care
- 1) Establishment of Respiration:-
- When the newborn is received, immediately patent the newborn’s airway and properly clear the airway. Due to which the newborn can breathe effectively.
- As soon as the newborn’s head is turned, wipe the mouth and nose and suction the mouth and nose so that the newborn can breathe properly. Suction should be done first in the mouth and then in the nose, due to which aspiration of secretions can be prevented.
- 2) Initiation of Cry:-
Normally 99% of newborns cry immediately and spontaneously after delivery, this cry is known as a good sign for the newborn’s breathing. - If the newborn does not cry properly, then
- Follow the following steps:
- a) If the baby does not cry spontaneously or if the cry is weak, then lightly simulate the baby to cry.
- b) To stimulate the baby’s cry, rub the soles of his feet lightly instead of slapping his bottom. After removing the secretions of the newborn, stimulate the baby to start crying.
- C) The cry of the newborn is usually loud and husky and if there is any abnormal cry as follows, then the newborn should be properly monitored like,
- •>High pitch cry:= Due to hypoglycemia and increased intracranial pressure,
Weak cry:= Prematurity,
Hosacry:= Laryngeal strider - 3)Care of cord:-
- Cord care is an important immediate care of the newborn.
- The cord of the newborn should be clamped within 30 seconds of birth and then cut properly.
- After the newborn is delivered, place the newborn on the mother’s abdomen.
- Then clamp the cord properly at two opposite sites using a cord clamp.
- Apply the first clamp 5 cm away from the umbilicus, then apply the second clamp 2.5 centimeters from the first clamp.
- Then cut the cord properly between the two clamps.
- Do not apply anything to the cord, let it dry and fall naturally.
- The cord naturally falls off within seven to ten days after birth.
- Prevent the cord from getting wet with water and urine.
- If any discharge or bleeding is present in the cord, immediately assess the cord clamp and then loosen it properly.
- If the following signs and symptoms are seen from the cord, then report it immediately like foul odor coming from the cord, no discharge is seen, redness is seen around the cord, the cord is wet, the cord does not fall down in 7-10 days, inflammation, fever etc.
- 4) Maintain Position of the Newborn:-
- The newborn is usually prone to choke, cough and gag during the first 12-18 hours after birth. Therefore, the newborn should be provided with a proper position.
- In which, the fitters should be provided with a proper side lining position so that the mucus can be removed and drained.
- 5) Identification and Banding: – After the baby is born, put a proper identification band on the baby so that the baby can be identified properly.
- 6) Eye Care: – Clean the eyes of the newborn properly with sterile gauze from the inner canthus to the outer canthus.
- If necessary, apply erythromycin or tetracycline eye ointment from the lower lid of the eye.
- 7) Attachment and Warmth (Bonding): – After the baby is born, place the baby on the mother’s abdomen so that bonding with the mother occurs and proper skin to skin contact can occur so that the mother and baby can be attached and the baby can be prevented from hypothermia.
- 8) APGAR Score:-
- APGAR score is the most important part of immediate newborn care.
- APGAR score is assessed at 1 minute and then at 5 minutes after birth.
- In APGAR score,
- A:= Appearance (skin color),
P:=Pulse (heart rate),
G:=Grimes (reflux irritability),
A:=Activity (muscle tone),
R:=Respiration (respiratory efforts) are assessed.
The total score of the APGAR score is 0-10. - APGAR score at 1 minute after birth:
- If the Apgar score is 7-10, it is considered normal, i.e. no depression, in which the baby is provided with normal post-delivery routine care.
- If the APGAR score is between 4-6, it indicates mild depression, in which the child requires assistance for breathing.
- If the APGAR score is between 0-3, it indicates severe depression in which the child needs resuscitation.
- APGAR score at 5 minutes after birth:
- Immediate care of the newborn after birth is done as follows.
- If the APGAR score is between 7-10, it is called normal, but if the Apgar score is below 7, then the baby needs to be monitored for another half an hour.
03 Write short answer (any two) ટૂંકમાં જવાબ લખો. (કોઈપણ બે)
a) Differentiate between placenta previa & abruptio placenta. પેલેસેન્ટા પ્રીવિયા અને એબરપ્ટીઓ પેલેસેન્ટા વચ્ચેનો તફાવત લખો.
- Difference between placenta previa and abruptio placentae:
- 1) Clinical features
- •>Placenta previa
- Nature of bleeding:-Painless, causeless and recurrent bleeding.
Bleeding is always visible. - Abruptio placentae:-Bleeding occurs due to painful, preeclampsia or trauma.
Bleeding can be visible, invisible or mixed. - •>Placenta previa
- Character of blood:- Bright red colored blood is seen.
- Abruptio placentae:- Dark red colored blood is seen.
- •>Placenta previa
- General condition and anemia:- Anemia is seen in proportion to visible blood loss.
- Abruptio placentae:- In this, the condition of anemia is more common than the amount of visible blood loss.
- •>Placenta previa
- Features of preeclampsia:- The condition of preeclampsia is not related to placenta previa.
- Abruptio placentae:- In abortio placentae, features of preeclampsia are seen in 1/3 of the cases.
- 2) Abdominal Examination
- •>Placenta previa
- Height of uterus:- The height of the uterus is found according to the gestational age.
- Abruptio placentae:- In abortio placentae, the height of the uterus is larger than the gestational age.
- •>Placenta Previa:-
- Feel of Uterus:- In placenta previa, the uterus feels soft and relaxed.
- Abruptio placentae:- In placenta previa, the uterus can be tense, tender and rigid.
- •>Placenta Previa
- Malpresentation:- In placenta previa, malpresentation is common and the head is high-floating.
- Abruptio placentae:- In placenta previa, malpresentation is unrelated and the head may also be engaged.
- •>Placenta Previa
- FHS(Fetal heart sounds):- Heart sounds are often present in placenta previa.
- Abruptio placentae:- In abruptio placentae, the heart sound is mostly absent.
- 3) Placentography (USG)
- Placenta previa:- The placenta is found in the lower segment of the uterus.
- Abruptio placentae:- The placenta is found in the upper segment of the uterus.
- 4) Vaginal Examination
- Abruptio placentae The placenta is not felt in the lower segment of the uterus.
- Placenta previa The placenta is felt in the lower segment of the uterus.
b) Define eclampsia and discuss nursing management of eclampsia. એકલેમ્પસીયાની વ્યાખ્યા લખો અને તેના નર્સિંગ મેનેજમેન્ટની ચર્ચા કરો.
- Eclampsia Definition
- Eclampsia is a life-threatening complication that occurs in women during pregnancy.
- The term eclampsia is derived from the Greek word for “like a flash of lightning”. Tonic-clonic convulsions or coma are complications of pre-eclampsia.
- When the condition of pre-eclampsia, which includes,
hypertension,
edema (weight gain),
proteinuria (protein in urine) and
albuminuria (albumin present in urine), is complicated and converts into a condition like convulsions and coma, it is called “eclampsia”.
This is an obstetric emergency. To manage which immediate measures are important. - Management of Eclampsia:-Medical and Nursing Management of Eclampsia
- Aim of Management:-
- To control the convulsive fits.
- To control blood pressure.
- To prevent complications.
- To deliver the fetus safely.
- Principles of Management
- To maintain the mother’s airway, breathing and circulation.
- To administer oxygen to the mother properly, about 8-10 liters.
- To prevent convulsions to the mother.
- To provide the mother with proper ventilatory support.
- To prevent injury to the mother.
- To conduct all laboratory investigations of the mother properly.
- General Management:-
- Hospitalization:- Hospitalize the mother in a hospital with properly equipped facilities.
- Rest:- Advise the mother to take adequate rest, along with advising her to stop all activities and restrict visitors.
- Positioning:- Advise the mother to take rest in the proper left lateral position to reduce vena cava compression and prevent heel spurs.
- History Collection: Collect a complete history of the mother including the frequency and duration of the fits and any medications the mother is taking.
- Sedation and then general examination:-
- Properly provide the mother with drugs and sedate her.
- Ex:=phenobarbiton 15-30 mg ( TDS)
- Or
- Diazepam 1.5 mg ( TDS).
- After the mother is properly sedated, do a general and abdominal examination of the mother properly and quickly.
- Vital signs
- Note the mother’s vital signs every half hour, including,
- Temperature,
- Pulse,
- Respiration,
- And blood pressure.
- If there is any abnormality in the vital signs or if the vital signs are raised above their normal range, treat them immediately.
- Urinary output: Monitor the mother’s urine output every hour.
- Nutrition:-
- Start the mother on 10% Dextrose to maintain the mother’s fluid, nutritional and calorie levels.
- Fluid should not increase by more than 2 liters in 24 hours.
- Additionally, to maintain the mother’s calorie levels, provide the mother with 50 ml of 5% Dextrose at an interval of 8 hours.
- Specific Management or Medical Management Eclampsia can be treated by providing the mother with the following medications:
- a) Anticonvulsants,
- b) Antihypertensives,
- c) Sedatives,
- d) Diuretics,
- e) Antibiotics,
- f) Other medications.
- a) Anticonvulsant:- ,
- Magnesium Sulphate ( MgSO4 ):-
- It acts as the drug of choice to treat the condition of eclampsia. As it helps in preventing eclamptic fits in the pregnant mother.
- Magnesium Sulphate can be administered both IV (intravenously) and IM (intramuscularly).
- Dose and route:-
- IM (intramuscularly):
- Initial dose: Initially 4gm IV (intravenously) bolus, Magnesium Sulphate should be administered very slowly for 3-5 minutes.
- Continuous dose: Administer 5 gm magnesium sulphate IM (intramuscular) every four hours in alternate buttock.
- •>IV (intravenous):-
- Initial dose: Administer 4-6 gm magnesium sulphate IV (intravenous) slowly over 15-30 minutes.
- Continuous dose: Administer 1-2 gm magnesium sulphate IV (intravenous) every hour.
- Magnesium sulphate is a toxic agent and if not provided within therapeutic levels, it may cause a condition called deep tendon reflux.
- The therapeutic level of magnesium sulfate (MgSO4) is 4-7 mEq/L ( milliequivalents per liter ).
- In case of magnesium sulfate overdose (MgSO4), calcium gluconate is used as an antidote.
Magnesium sulfate is administered only when there is no urine present,
urine output is increased to more than 30 ml/hr and respiratory rate is more than 12/min. - b) Antihypertensives: Antihypertensives are used to control and reduce blood pressure.
- Ex:
a) Hydralazine: 5 to 10 mg over 2 minutes.
b) Labetalol:
Initial dose: 20mg slowly over 2 minutes.
Then 40-80 mg IV over 10 minutes.
Total dose should not exceed 300 mg. - c) Sedatives:-
Ex:=Diazepam
Dose:=5-10mg IV at the rate of 2-5mg/minute. - Maximum dose: Should not be increased more than 10mg.
- d) Diuretics: Diuretic medication should be provided only when pulmonary edema is present during pregnancy.
Ex:=Frusemide, Mannitol. - e) Antibiotics:
- Antibiotics are provided as prophylactic to reduce the complications of pulmonary and pleural infections.
- Broad spectrum antibiotic medications are used in these antibiotics.
- f) Other medications:
- i) In case of pulmonary ED: Provide frusemide 40 mg IV followed by 10% Mannitol.
- ii) Heart failure: Use Ex: Lasix and Digitalis medications.
- iii) Hyper pyrexia:
- Antipyretic medications are used.
- Nursing Management of Eclampsia
- Pregnant woman with eclampsia should be placed in a padded side railed bed.
- Place a padded tongue blade between the teeth.
- Place the mother in a lateral position to avoid aspiration.
- Maintain a patent airway during convulsions and provide adequate amounts of oxygen to the mother.
- Monitor the mother’s oxygen level properly with pulse oximetry.
- Suction the mother’s mouth properly to remove oral secretions and any vomiting.
- Note the time and duration of the mother’s convulsions properly.
- Provide proper and regular prenatal care to the mother with pregnancy-induced hypertension.
- Protect the mother from self-injury.
- Keep the mother in a dark room to minimize stimuli such as bright light, noise, and visitors.
- Keep the foot side of the bed slightly elevated so that secretions can drain properly from the respiratory tract.
- Assess the mother’s vital signs, including the ED, fundal height, presentation and position of the fetus, and fetal heart sound, and test the urine for protein.
- Assess the mother’s urine output properly.
- Provide intravenous infusions of glucose saline and Ringer’s lactate solution as prescribed to maintain the mother’s fluid and nutritional levels.
- Advise the mother to maintain personal hygiene.
- Provide the mother with properly prescribed medications.
- Assess the mother’s uterine activity, cervical status and fetal status as membranes may rupture and delivery may occur.
- Obstetrical management:
- Advise the mother to have regular follow-up.
- Often, when a woman has convulsions, she comes for labor. If labor has not started, artificial membrane rupture, prostaglandin gel or oxytocin is used to induce labor, or a cesarean section is also performed. If the baby has died, spontaneous labor is waited for.
- Continue the hypertensive regimen as prescribed during the postpartum period.
- Continuously monitor the mother for any complications other than eclampsia.
c) Explain partograph. – પાટોગ્રાફ સમજાવો.
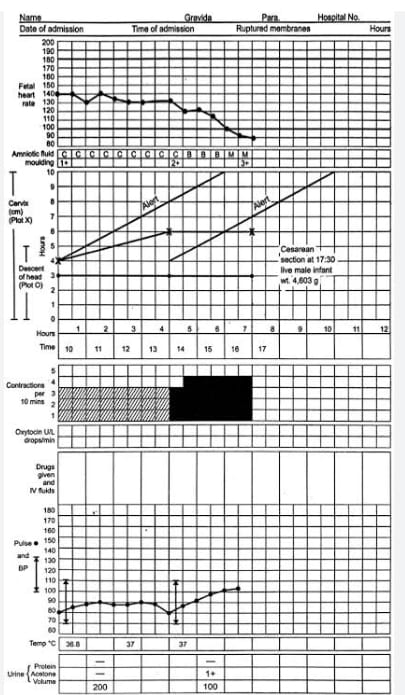
- Definition:
Partograph is a graphic recording and tool for cervical dilation, fetal head descent and labor progress and the condition of the mother and fetus. Partograph can provide immediate and relevant information about the condition of the mother and fetus. It recognizes the need to take action at the appropriate time and for timely referral. Partograph can also improve the morbidity and mortality rate of the mother and fetus. - Objectives or Advantages:
- 1) To make proper observations and record during labor.
- 2) To understand the latent and active phases of labor.
- 3) To interpret the partograph and identify any deviation from normal and take appropriate action.
- 4) To know the progress of labor and take action at the right time and refer.
- 5) To see the record at a glance in a single sitting and to hand over easily.
- 6) To avoid having to record labor events repeatedly.
- 7) To reduce the rate of prolonged labor and education.
- Observation Charted on Partograph:
- 1) Pregnant Woman Information:
- A) Name,
- B) GTPAL Score
- G: Gravida,
- T:=Tomb Birth,
- P:=Par,
- A:=Abortion,
- L:=Living Children.
- C) Name of the hospital,
D) Hospital registration number,
E) Date and time of admission,
F) Time of membrane rupture,
G) Period of gestation,
H) Date and time of onset of labour. - 2) Fetal condition:
A) Fetal heart rate,
B) Amniotic fluid,
C) Molding. - 3) Progress of labour
A) Cervical dilation,
B) Descent of head,
C) Uterine contractions. - 4) Maternal condition
A) Oxytocin, drugs and I.v. fluid administration
B) Pulse,
C) Blood pressure,
D) Temperature,
E) Urine volume, acetone and protein. - All this information is filled in the partograph.
- Points to keep in mind while filling the partograph:
- 1) When the woman reaches the active phase of labor, the partograph should be maintained and the pregnant woman should not be left alone.
- 2) Fetal heart rate should be counted and recorded every half hour,
Fetal heart sounds should be counted for a full 1 minute and should be counted immediately after the uterine contractions are completed. - 3) When the dilation of the cervix is 4 cm or more, the frequency, intensity, duration, pulse, fetal heart rate of uterine contractions should be monitored every 30 minutes.
- 4) Blood pressure and cervical dilation (in cm) should be monitored every two hours.
- 5) Descent of head and temperature should be monitored every four hours.
- Partograph
- 1) Patient identification data
This includes the woman’s name, age, GTPAL score, date and time of admission, registration number, time of membrane rupture and time and date of onset of labor. - 2) Fetal condition
Fetal heart rate should be counted and recorded every half hour.
Fetal heart rate should be counted for a full 1 minute.
Fetal heart rate should be counted immediately after uterine contractions are detected.
If fetal heart sound (FHS) is < 120/Minutes or if (FHS) is > 160/Minutes, it indicates fetal distress. If there is a condition of fetal distress, immediate action should be taken.
The vertical column in each small box shows the interval of half an hour. - 2) Condition of Membrane
Along with the fetal condition, the condition of the amniotic membrane and the color of the amniotic fluid should also be recorded every 30 minutes. - A) If the amniotic membrane is intact: = I (Intect),
- B) If the liker is clear: = C (Clear),
- C) If the liker is absent: = A (Absent),
- D) If the amniotic membrane is ruptured: = R (Rupture),
- E) If the liker is meconium stained: = M (meconium),
- F) If blood is present in the liker: B (Blood)
- Thus, the condition of the amniotic membrane and amniotic fluid should be marked as follows in the partograph.
- 3) Molding (The bones of the fetal head are separated by sutures and fontanelles, but when it passes through the birth canal, the bones of the fetal head overlap each other and the shape of the head changes for a while, due to which the fetal head can pass easily through the birth canal. This condition is called molding.)
Molding is recorded by grade. - A) 0 -> If the bones are separated and the sutures are easily felt.
- B) + -> When the bones just touch each other.
- C) ++ -> When the bones overlap but easily separate.
- D) +++ -> When the bones are severely fixed and overlapping.
- 4) Progress of Labor
- Start plotting labor progression on the partograph only after the woman is in active labor.
Active labor is when the cervical dilation is 4 cm or more and at least two good contractions occur in every 10 minutes.
Record cervical dilation in cm every four hours.
Record the onset of cervical dilation starting from the left alert line (when the mother is in active labor). Normally the graph line remains continuously above the left alert line, indicating the proper time each time.
If the alert line is crossed, i.e. if the graph moves to the right of the alert line, it indicates prolonged labor. Hence, the midwife is immediately alerted that there is something abnormal in labor. Note the time when the alert line is crossed and immediately start taking measures for immediate treatment or referral.
When the graph crosses the action line i.e. if it goes to the right side of the action line, immediately start treatment or refer the mother to the appropriate medical service.
The difference between the alert and action lines is 4 hours. - 5) Uterine contractions
Uterine contractions should be recorded every half hour. Contractions occurring twice in ten minutes indicate good uterine contractions. - Mark them in the box of the partograph as follows.
- -> Mild uterine contractions < 20 seconds,
- -> Moderate uterine contractions 20 – 40 seconds,
- -> Strong uterine contractions > 40 seconds.
- 6) Cervical Dilation and Descent of Fetal Head
- The descent of the fetal head down through the out labor process occurs simultaneously with cervical dilation.
- Until the cervix is 7 centimeters dilated, the assessment of the fetal head descent is done by abdominal palpation, which assesses the fifth (5) digit of the fetal head above the pelvic brim.
- In the partograph, cervical dilation is plotted by (x) while the descent of the fetal head is plotted by (O).
- 7) Maternal Condition
The maternal pulse is recorded on the partograph every half hour
and is plotted on the partograph by a dot (•). - Maternal blood pressure is recorded every 4 hours, both systolic blood pressure and diastolic blood pressure are indicated by vertical arrows (↕) where the upper end of the arrow indicates systolic BP. While the lower end of the arrow indicates diastolic blood pressure.
Maternal temperature should be recorded every four hours on the partograph.
Maternal urine volume, urine acetone and protein levels should be recorded properly on the partograph.
If any drug or oxytocin medication is given to the mother during the labor process, its dose, route and time of administration should be recorded properly. - Thus, early, quick and relevant information about the labor progress and the condition of the mother and fetus can be obtained through the partograph.
d) Write down indications of caesarian section. – સીઝેરીયન સેક્સનનાં ઈન્ડીકેશન લખો.
- Indications for cesarean section are divided into two categories:
- 1) Absolute, (in which vaginal delivery is not possible)
- 2) Relative (in which vaginal delivery is possible but there is a risk to the mother and baby)
- 1) Absolute, (in which vaginal delivery is not possible):
- Central placenta previa,
- Severe degree of contracted pelvis,
- Cervical or broad ligament fibroids,
- Vaginal atresia/obstruction,
- Advanced cervical carcinoma,
- Cephalopelvic disproportion,
- Obstruction due to pelvic mass,
- Fats have died.
- 2) Relative (in which vaginal delivery is possible but there is risk to mother and baby):
- Cephalopelvic disproportion,
- Contracted pelvis,
- Previous cesarean delivery,
- Fetal distress,
- Abnormal uterine contractions,
- Large fetus,
- Small pelvis,
- Failed induction,
- Antepartum hemorrhage such as placenta previa, abruptio placentae.
- Malpresentation or abnormal lie (transverse lie).
- Bad obstetric history,
- Hypertensive disorders such as preeclampsia,
- Prolapse of umbilical cord,
- Elderly primigravida,
- Medico-gynecological disorders:
- Chronic hypertension,
- Chronic nephritis,
- Diabetes,
- Heart disease,
- Pelvic tumor,
- Vaginal atresia,
- Carcinoma of cervix,
- Cervical dystocia.
- Common indications of cesarean section
- 1) Failure to progress in labor:
- Prolonged labor in which the cervix does not dilate properly and the fetus does not descend properly into the birth canal, requiring cesarean section.
- 2) Fetal distress:
A sign that the fetus is not able to tolerate labor properly, such as an abnormal fetal heart rate, indicating reduced oxygen supply to the fetus, which may necessitate a cesarean section. - 3) Malpresentation of the baby:
When the baby is in a breech presentation (buttocks as the presenting part), transverse position, making vaginal delivery impossible and requiring a cesarean section. - 4) Placental abnormality:
Placenta previa:
In which the placenta is partially or completely implanted in the lower uterine segment, i.e., the placenta is present as the presenting part. - Placental abruption, in which the patient separates prematurely from the uterine wall, also requires a cesarean section.
- 5) Maternal health conditions such as genital herpes, heart disease, severe hypertension, etc.
- 6) Previous cesarean section:
If a cesarean section has been performed before, then the need for a repeat cesarean section depends on the scar of the previous cs and the duration of the pregnancy. - 7) Multiple pregnancy:
When there are multiple pregnancies such as twins, triplets and the presenting part and position of the fetuses, a cesarean section is required. - 8) Umbilical Cord Prolapse:
In which the umbilical cord slips down through the cervix, which can cut off the blood supply to the fetus. - 9) Maternal Request:
In some cases, the mother herself chooses a cesarean section due to personal and psychological reasons. - 10) Emergencies During Labor:
Complications during labor such as uterine rupture, severe bleeding, and maternal illness require an immediate cesarean section to protect the health and safety of the mother and baby. - Thus, a cesarean section is required in all these conditions.
Q-4 Write short notes. ટૂંકનોંધ લખો. (કોઈપણ ત્રણ)
a) Menstrual cycle – માસિક ચક્ર
- Definition: Menstruation comes from the word “moon”. The menstrual cycle is a visible cyclic process of physiological changes in the endometrium of the uterus and bleeding from the vagina due to the interconnection of hormones. Which is caused by the HPO process
- (H: Hypothalamus,
- P: Pituitary gland,
- O: Ovaries).
- H: Hypothalamus:
- The hypothalamus secretes gonadotropin-releasing hormone (GnRH) which stimulates the anterior pituitary gland to secrete FSH (Follicle Stimulating Hormone)
- LH (Luteinizing Hormone).
- P: Pituitary Gland:
Pituitary gland secretes FSH (Follicle Stimulating Hormone)
LH (Luteinizing Hormone). It works on the ovaries. - O: Ovaries:
FSH (Follicle Stimulating Hormone) secreted by the pituitary gland causes maturation of ovarian follicles, secretion of estrogen and ovulation.
While LH (Luteinizing Hormone) causes development of corpus luteum and secretion of progesterone. - The hormones secreted during the menstrual cycle are regulated by a negative feedback mechanism.
The hypothalamus responds to changes in the blood levels of estrogen and progesterone. For example, the hypothalamus is depressed by high levels of estrogen and progesterone in the blood, while the hypothalamus is stimulated by low levels of estrogen and progesterone. - The average length of the menstrual cycle is 28 days.
- Menstrual Cycle:
The menstrual cycle has two phases. - 1) Ovarian Phase
- 2) Uterine Phase
- 1) Ovarian Phase:
The ovarian phase involves two further phases. - a) Follicular Phase,
- b) Luteal Phase
- a) Follicular Phase:
- The follicular phase starts from the first day of menstruation and ends with ovulation. This phase usually lasts for 14 days.
- In this phase, follicles grow due to follicle stimulating hormone (FSH).
- One of these follicles (dominant follicle) matures.
- This mature follicle becomes a Graafian follicle. It releases estrogen.
- Then estrogen acts on both follicle stimulating hormone (FSH) and luteinizing hormone (LH).
- Estrogen suppresses follicle stimulating hormone (FSH) and stimulates luteinizing hormone (LH).
- Then luteinizing hormone (LH) ruptures the Graafian follicle that is formed from the dominant follicle, and the ovum comes out of it, and then the work of the corpus luteum increases.
- b) Luteal Phase:
- The luteal phase is the period from ovulation to the start of the next menstrual cycle, usually lasting 14 days.
- In this phase, the corpus luteum develops, which is formed from the remaining ovarian follicles after ovulation.
- The corpus luteum produces progesterone, which prepares the lining of the uterine cavity for implantation of a fertilized egg.
- The luteal phase can have two possibilities:
- I: Fertilization absent
- II: Fertilization present
- I: Fertilization absent
- If fertilization is absent, the corpus luteum converts to the corpus luteum.
- The corpus menstrualis converts into corpus albicans and then disappears after 28 days.
- II: Fertilization present
- If fertilization is present, the corpus luteum converts into corpus luteum verum which also contains progesterone hormone and it remains for three months.
- Progesterone hormone suppresses the immunity of the mother due to which the growth of the fetus in the uterine cavity can occur and the condition of abortion is prevented.
- 2) Uterine Phase:
- The uterine phase is further divided into three phases:
- 1) Bleeding Phase (4 days)
- 2) Proliferative Phase (10 days)
- 3) Secretory Phase (14 days)
- 1) Bleeding Phase (4 days):
- When the ovum is not fertilized, the increased level of progesterone hormone in the blood causes vasoconstriction of the blood vessels of the endometrium (innermost layer of the uterus).
Due to this, the blood supply to the endometrial layer of the uterine cavity decreases.
And a condition of hypoxia arises.
Due to this, necrosis and death of the cells and tissues of the endometrial layer occurs.
Now due to necrosis and death of these cells and tissues, the condition of hematometra (collection of blood in the uterine cavity) arises.
Due to this condition, the nerve supply goes to the hypothalamus, after which it stimulates the pituitary gland. The pituitary gland releases oxytocin, which is responsible for uterine contraction.
Due to this uterine contraction, blood flow becomes visible at the vaginal site. And menstruation starts. In which there is blood from the endometrial gland, endometrial cells, and capillaries and unfertilized ovum. - When the reduced progesterone level reaches a critical level, the second ovarian follicle is stimulated by follicle-stimulating hormone (FSH) and the proliferative phase begins.
- 2) Proliferative Phase (10 days):
- The proliferative phase is also called the follicular phase.
- In this stage, the ovarian follicles grow due to follicle-stimulating hormone (FSH) and mature and produce estrogen.
- Estrogen stimulates the proliferation of the endometrium and prepares it to receive the fertilized ovum.
- Thus, the endometrium becomes thick (2 to 3 mm) due to rapid cell multiplication.
- And due to the increase in mucus secreting glands and blood capillaries, ovulation occurs at the end of this phase due to the effect of luteinizing hormone (LH) and the production of estrogen decreases.
- 3) Secretory Phase (14 days):
- Thus, the menstrual cycle is explained in two phases namely ovarian phase and uterine phase.
- This phase is also called luteal phase.
- Immediately after ovulation, the lining cells of the ovarian follicle are stimulated by luteinizing hormone (LH) and its corpus luteum is formed.
- Now this corpus luteum produces progesterone.
- Due to the effect of this progesterone hormone, the endometrium of the uterine cavity secretes more mucus from the secretory glands and becomes edematous i.e. thick (5 to 6 mm) and the endometrium provides a favorable environment for the implantation of the fertilized ovum.
b) Placenta – પ્લેસેન્ટા
- Placenta:
- Introduction
The placenta is a mass-like structure. It develops from two sources, the fetal component, the chorion frondosum, and the maternal component, the decidua basalis, usually on the anterior or posterior side of the upper uterine segment.
The placenta is connected to the fetus by the umbilical cord and maintains the pregnancy. The placenta supports the life of the embryo by supplying oxygen and food to the embryo and removing toxic materials. - Definition
The placenta is “discoid shaped” due to its septum,
It is “hemochorionic” because its chorion is in direct contact with maternal blood, and it is “deciduous” because the placenta is shed after birth. - Placental Origin
The placenta originates from the trophoblastic layer of the fertilized ovum.
The placenta is closely linked to the maternal circulation to properly perform functions that the fetus is unable to perform during intrauterine life.
The survival of the fetus depends on the integrity and efficiency of the placenta. - Attachment of Placenta
The placenta is attached to the uterine wall of the mother and establishes a connection between the mother and the fetus through the umbilical cord. - Placenta at term
The placenta at term is a flat and round or oval shaped disc-like spongy, flaky structure. The placenta is thick in the centre and thin at the edges. - Diameter and Thickness of Placenta
- 1) Average weight of placenta: = 500 gm
- 2) Ratio between fetus and placenta: = 1/6( 3kg / 500 gm).
- 3) Diameter of placenta: = 15-20 cm.
- 4) Surface area of placenta: = 243 sq cm (square centimeter).
- 5) Placenta volume:= 500 ml.
- 6) Placenta is thick in the center while thin at the edges.
Central part of placenta:=2.5 to 3 cm.
Peripheral part of placenta:= 1 to 1.5 cm - The umbilical cord connects the fetus to the placenta, which has one umbilical vein and
two umbilical arteries. - Parts of placenta
- The placenta has two surfaces.
- 1) Fetal surface (80%),
- 2) Maternal surface (20%)
- 1) Fetal surface (80%):
The fetal surface is smooth, sinuous and transparent, covered by a smooth and glistening amnion.
In which the umbilical cord is connected at the center.
Umbilical vessels are visible on this surface.
Fetal surface is bright red in color. - 2) Maternal surface (20%):
Maternal surface is “rough and spongy”.
It is dull red in color.
Maternal surface is divided into 15 to 30 cotyledons which are separated by sulci.
Small calcified infarcts are visible on the maternal surface. - Structure of placenta
The placenta has two plates. Chorionic plate is on the inner side which is covered by amniotic membrane. Umbilical cord is attached to this plate. On the maternal side is basal plate.
Between the chorionic plate (fetal site) and the basal plate (maternal site) is the intervillous space.
In this intervillous space, the stem cells and their branches are located and the space contains maternal blood. - 1) Amniotic membrane
The amniotic membrane is a single layer of cubical epithelium and connective tissue. And the amniotic membrane is loosely attached to the chorionic plate.
It does not play any part in the formation of the placenta. - 2) Chorionic plate
The chorionic plate is a seat of connective tissue. It contains the branches of the umbilical vessels. This chorionic plate is covered by the amniotic membrane at the fetal site.
Stem cells arise from the chorionic plate which forms the inner boundary of the choriodecidual space. - 3) Basal plate.
The basal plate is formed by cytoblast, syncytoblast, and decidua basalis.
It is a compact and spongy layer.
The basal plate is present near the maternal surface.
The uterine artery and vein enter the intervillous space from the basal plate.
The basal plate forms the boundary of the maternal surface. - 4) Intervillous space
Which has the chorionic plate on the inner side and the basal plate on the outer side. The two plates are connected around it.
Internally, it is lined on all sides by syncytiotrophoblast and filled with slow-flowing maternal blood.
These intervillous - 5) Stem villi
Stem villi originate from the chorionic plate and grow to the basal plate.
Primary, secondary and tertiary villi are formed in progressive development.
The functional unit of the placenta is the fetal cotyledon or placentome. It is formed from the major primary stem villi.
These major stem villi pass through the intervillous space and are anchored to the basal plate. The functional subunit is called the lobule. Which is formed from the tertiary villi.
There are about 60 stem villi in the human placenta. Therefore, each cotyledon (total:=15-20) has three to four major stem villi. Some villi anchor the placenta and some remain free in the intervening space, which are called nutritive villi. The blood vessels in the villi do not connect with each other. - Circulation through the placenta
- There are two types of circulation in the placenta.
- 1) Phytoplacental circulation,
- 2) Uteroplacental circulation
- 1) Phytoplacental circulation,
- In the phytoplacental circulation, two umbilical arteries bring impure blood from the fetus and it enters the chorionic plate, which supplies each half of the placenta.
- The arteries break into small branches and enter the stem of the chorionic villi, which divide into primary, secondary, and tertiary vessels. Maternal and fetal blood flow side by side in opposite directions.
The fetal blood flow is 400 ml/minute which is mainly due to the pumping action of the fetal heart rate. The blood from the umbilical artery gives carbon dioxide to the placenta and absorbs oxygen and returns to the fetus through the umbilical vein. - 2) Uteroplacental circulation (maternal circulation) In the uteroplacental circulation, the uterine artery and vein enter the intervillous space through the basal plate and transmit blood and nutrients from the mother to the intervillous space.
- Functions of Placenta
- 1) Respiratory function
The fetus obtains oxygen and excretes carbon dioxide through the placenta. - Just as oxygen passes from the mother’s blood to the fetal blood, carbon dioxide in the fetus is transmitted to the maternal blood through the placenta.
- 2) Nutritive function
All types of nutrients such as amino acids, glucose, vitamins, minerals, lipids, water and electrolytes are transmitted from the mother to the fetus. - The food taken in the maternal diet reaches the placental side, where it becomes a simple form, after which the placenta selects the substances required by the fetus and transmits them to the fetus.
- 3) Storage function
The placenta stores glucose, iron and vitamins. And the placenta provides them to the fetus when it needs them. - 4) Excretory function
The waste products in the fetus are transmitted to the placenta. - 5) Protection
The placental membrane has a limited barrier function. Some antibodies pass from the mother to the fetus, providing immunity to the baby for three months after birth. - 6) Immunological function
The antigens of the fetus and placenta act as foreign to the mother. However, graft rejection does not occur because the placenta provides immunological protection against rejection. - 7) Hormonal function
- Steroid hormones
Oestrogen,
Progesterone. - Protein hormones
HCG (Human Chorionic Gonadotropin),
HPL (Human Placental Lactogen),
Relaxin,
PAPPA (Pregnancy Associated Plasma Protein:= A). - •>HCG (Human Chorionic Gonadotropin),
HCG (Human Chorionic Gonadotropin) is produced by the cytotrophoblastic layer of the chorionic villi.
HCG (Human Chorionic Gonadotropin) is high during the 7th to 10th week of pregnancy and then decreases as the pregnancy progresses. It maintains the corpus luteum.
HCG (Human Chorionic Gonadotropin) is used in pregnancy tests because it is excreted in the mother’s urine.
HCG (Human Chorionic Gonadotropin) is detected in the blood 7 days after fertilization and in the urine 9 days after fertilization, which indicates a positive pregnancy test. - ••> HPL (Human Placental Lactogen)
HPL (Human Placental Lactogen) is produced by the placenta and is involved in the lactogenic and metabolic processes of pregnancy. When the level of human chorionic gonadotropin trophin decreases, the level of human placental lactogen (HPL) increases and continues throughout pregnancy.
Human Placental Lactogen (HPL) acts as an anti-insulin which increases the glucose level in the blood and helps in supplying glucose to the fetus. - ••>Relaxin
Relaxin is produced by decidua cells. And it softens the cervix and helps relax the pelvic ligaments and symphysis pubis during the labor process. - ••>PAPPA (Pregnancy Associated Plasma Protein:= A)
Pregnancy Associated Plasma Protein:= A works as an immunosuppressant and works to maintain pregnancy. - ••> Estrogen
Estrogen is produced by the placenta throughout pregnancy. It is essential for the well-being of the fetus.
Estrogen increases during labor, which helps in the release of oxytocin, which increases uterine contractions. - ••> Progesterone
Progesterone is produced by the syncytial layer of the placenta and acts as a tocolytic agent and prevents uterine contractions, as well as acting as an immunosuppressant to help maintain pregnancy.
c) MTP ACT – એમ.ટી.પી.એક્ટ
- ••> Progesterone
ProgesteroneMedical Termination of Pregnancy (MTP) - Medical termination of pregnancy is a medical procedure in which a woman can terminate her pregnancy to maintain her health or well-being, taking into account certain criteria.
- Termination of pregnancy by medical or surgical methods before the stage of viability of the fetus is called induction of abortion and is legal or illegal. Abortion was legalized in India as a medical termination of pregnancy in August 1971 and was implemented from April 1972 and revised in 1975.
- Indications
- When the woman’s life is in danger and her physical and mental health is seriously damaged.
- The child is at risk of physical and mental abnormalities.
- In a condition where the child has any congenital anomaly.
- Pregnancy due to rape.
- Mother’s health is damaged due to social or economic reasons and contraceptive measures have failed.
- According to Indian law, abortion is allowed up to 20 weeks. In pregnancy up to 12 weeks, the opinion of one registered medical practitioner is required and in 12 to 20 weeks, the opinion of two registered medical practitioners is required.
- Written consent of the patient and in cases where the patient is under 18 years or mentally handicapped, the consent of the guardian is required.
- Contraindications
- Uncontrolled blood pressure of more than 160/100,
- Cardiovascular disease,
- Woman is more than 35 years of age,
- Severe renal failure, liver disease or respiratory disease,
- Use of systemic corticosteroids,
- Coagulopathy or woman is receiving anticoagulant therapy,
- Mother has anemia,
- Uncontrolled seizure disorder.
- Who can perform medical termination of pregnancy?
- The Chief Medical Officer or Civil Surgeon grants permission for medical termination of pregnancy to the following doctors:
- Holding a Post Graduate Degree or Diploma in Obstetrics and Gynaecology.
- Six months training as a Resident in Obstetrics and Gynaecology.
- One year experience in the Department of Obstetrics and Gynaecology.
- Assisted a Registered Medical Practitioner in 25 cases of Medical Termination of Pregnancy (MTP). Place for MTP (Medical Termination of Pregnancy): Hospital established or maintained by the Government or the place approved by the Chief Medical Officer or Civil Surgeon. Records: Medical Termination of Pregnancy to be recorded in the form. Confidentiality should be maintained and the same should be reported to the Director of Health Services. Penalty:
A person who fails to comply with this Act can be punished with imprisonment for a term ranging from 2 to 7 years. Methods of Medical Termination of Pregnancy (MTP): First Trimester (up to 12 weeks): Medical
In this, pregnancy is terminated using medication such as,
Mifepristone,
Mifepristone and Misoprostol,
Mithotrexate and Misoprostol,
Tamoxifen and misoprostol. Surgical
In this, pregnancy is terminated using surgical procedures.
Such as,
Menstrual regulation, Vacuum aspiration,
Suction evacuation and curettage,
Dilatation and evacuation. Second Trimester (13-20 weeks): - Prostaglandins,
- Dilation and evacuation,
- Intrauterine instillation of hyperosmotic solutions,
- Oxytocin infusion,
- Hysterotomy.
- Complications:
- Complications generally depend on the method of medical termination of pregnancy (MTP) performed.
- Immediate complications
- Cervical lacerations,
- Uterine perforation,
- Hemorrhage,
- Shock,
- Thrombosis,
- Embolism,
- Post-abortive triad pain, bleeding, and low-grade fever may occur and depend on the method of medical termination of pregnancy used.
- Remote
- Gynecological complications,
- Obstetric complications,
- Failed abortion,
- Ectopic pregnancy etc.
- Nursing Role with the Patient Undergoing MTP:
- Thus, in medical termination of pregnancy, the pregnancy is terminated.
- The nurse should provide comfort and support to the mother and her family members and provide proper reassurance by clearing all their queries.
- If the mother has decided to have an abortion, then take her written permission along with her husband and the patient’s consent.
- Continuous monitoring of the patient and support should be provided before, during and after the procedure for medical termination of pregnancy.
- Provide proper education to the mother about the complications that may arise after abortion, such as,
Continuous vaginal bleeding with clots for three weeks after abortion,
Fever, continuous pain, and burning urination. - Advise the woman that the first menstruation starts between 2 and 8 weeks after abortion.
- Advise the woman that lactation, if it starts, is in a mild amount and if the breasts are not stimulated, it lasts only for 48 hours.
- Provide them with education or have them come for a follow-up visit two to eight weeks after undergoing medical termination of pregnancy (MTP) to ensure that the reproductive organs have returned to their pre-pregnancy state.
d) Sign & Symptoms of pregnancy ગર્ભાવસ્થાના ચિહ્નો અને લક્ષણો
- There are three main signs of pregnancy which are as follows.
- Presumptive Signs
- Probable Signs
- Positive Signs
- Presumptive Signs:
- Mostly subjective i.e. the mother herself feels that she is pregnant when it could also be due to other illnesses.
- Amenorrhea,
- Nausea and vomiting,
- Morning sickness,
- Tingling sensation in 3 to 4 weeks,
- Enlargement of breast and nipple, Appearance of Montgomery tubercles in the breast.
- Increased urination, Colostrum expressed from the nipple.
- Pigmentation of the face and breast (Chloasma, Linea Nigra, Striae Gravidarum),
- Quickening: The first movement of the mother and fetus is felt at about 16 – 20 weeks.
- Probable Signs:
- Probable signs are maternal physiological changes. They can be detected during examination. They are objective but cannot be said to be a definite confirmation of pregnancy.
- Visualization of fetal movement in late pregnancy.
- Enlargement of the abdomen. Pregnancy can be detected by abdominal palpation.
- Changes in the size and shape of the uterus and enlargement of the uterus.
- External and internal miscarriage.
- A positive pregnancy test means the detection of the hormone human chorionic gonadotropin (HCG) in the urine. The following signs are seen in it:
- Jacquemier sign or Chadwick sign:
- This sign appears during the 8th week of pregnancy. In this, bluish discoloration of the vulva, vagina and cervix is called Chadwick sign, while bluish discoloration of the vagina is called Jacquemier sign.
- Heartman sign:
- This sign is seen between the 1st and 3rd month of pregnancy. In this, slight bleeding is seen when the fertilized egg implants in the uterine cavity.
- Palmar sign:
This sign is seen during 4-8 weeks of pregnancy. In this sign, regular and rhythmic contractions of the uterus occur when bimanual examination is done. - Goodell’s sign:
Goodell’s sign is seen up to 6 weeks and it shows softening of the lower part of the cervix. - Hegar’s sign:
This sign is seen between 6 and 10 weeks and it shows enlargement of the upper part of the uterus i.e. the body part of the uterus with the growth of the fetus and softening of the lower part of the uterus. Hegar’s sign is a cyanosis and softening of the cervix, a softening of the cervix between the uterus and the cervical isthmus (Around 6-8 weeks). - Piskacek’s sign:
This sign is seen during 6-8 weeks in which the uterus enlarges asymmetrically due to lateral implantation in the uterus. - Osiander’s sign:
This sign is seen during 6-8 weeks. In this sign, pulsation is felt in the lateral fornix in the vaginal area. - Braxton Hicks Contractions:
In early pregnancy, the uterus contracts spontaneously. They are regular, infrequent, spasmodic, painless, and do not affect the dilation of the cervix. They increase near term and eventually merge with the painful contractions of labor. The expulsion of the fetus includes,
Internal expulsion and external expulsion: - Internal expulsion: After the sixteenth week, vaginal examination shows the presence of a body that moves on tapping and then returns to its place with a thrust.
- External ballotment: Around 20 weeks of pregnancy, a ballotment is felt in the uterus under the hand palpating the uterus. This is known as external ballotment.
- Positive Signs: Positive signs confirm pregnancy. In which the examiner detects and documents the fetus.
- Visualization of fetuses by ultrasound: This test confirms pregnancy and also assesses the fetus’s lie, presentation, fetal heart sound, location of the placenta, amount and distribution of amniotic fluid, and internal os. Fetal abnormalities such as encephalitis, spina bifida, myelomeningocele, etc., and uterine and ovarian abnormalities are detected by this method.
Routinely, a scan is recommended during the mid-trimester before the 20th week of pregnancy. In case of serious fetal abnormalities, the patient may be advised to terminate the pregnancy. - Pregcolor and pregcolor-card test: These are mostly used as home-kits to confirm pregnancy. These color-changing-card-tests are simple and can be done by the woman herself. The presence of 2 lines in the card test on the 5th day after missed periods confirms pregnancy.
- Hearing the fetal heart sound: The fetal heart sound can be heard on a fetoscope after 20 weeks.
- Fetal movements: Fetal movements are felt at 22 weeks.
- Palpation of fetal parts: Fetal parts are palpable after 24 weeks
- Frequency of micturition: It is usually experienced at the end of term in which frequency of micturition occurs due to engagement of the fetal head.
- Radiography: It is not usually advocated in pre-natal practice.
- Radiographic pelvimetry is rarely indicated in selected cases of suspected cephalopelvic disproportion.
- Radioimmunoassay: This is a very sensitive method and can be used to detect the presence of hCG in maternal serum and urine 7-8 days after ovulation or at the time of implantation.
It confirms the presence of pregnancy after 3 weeks of conception. The concentration of hCG in maternal serum doubles every 2-3 days until it reaches a peak value 2-3 months after conception (Black-Burn 2007). - The embryo can be seen on ultrasonography by 6 weeks, after which the fetus can be seen.
- Radiological appearance of the skeletal system of the fetus.
- Visualization of the fetal skeleton on X-ray.
Q-5 Define following (any six) -કોઈપણ છ
a) Fertilization – ફર્ટીલાઈઝેશન
Fertilization is the process in which a spermatozoon and a mature ovum fuse. Fertilization is the union of a single spermatozoon with an ovum in the ampulla tubule.
b) Restitution – રેસ્ટીયુશન
It is a visible passive movement of the head that occurs due to the untwisting of the neck during internal rotation. This movement, which is a 1/8 circle head rotation in the opposite direction of internal rotation, is called restitution.
c) Atonic uterus – એટોનીક યૂટ્રસ
It is a condition in which the uterus does not contract properly after childbirth, resulting in excessive building after delivery and a life-threatening condition.
d) Apgar score – અપગાર સ્કોર
The Apgar score, developed in 1952 by obstetrician anesthesiologist Virginia Apgar, is the standard tool for the assessment of newborn babies. The Apgar score is a practical method for quickly and instantly performing a complete assessment of neonates and newborns.
-e) Molar pregnancy – મોલર પ્રેગનન્સી
Molar Pregnancy, also known as Hydatidiform Mole. Hydatidiform mole (H.Mole) is also called vesicular mole.
This is an abnormal condition of the placenta. In which some degenerative and proliferative changes occur in the young chorionic villi and due to this, a cluster (cluster-like shape) is formed in the cyst. And since it resembles a hydatid cyst, it is called hydatidiform mole or vesicular mole.
When the chorionic villi transform into a mass of translucent vesicles, they form a structure like a bunch of grapes, which is called hydatidiform mole.
Types of Vesicular Mole
There are two types of vesicular moles:
1) Complete mole,
2) Incomplete mole
1) Complete mole:
A complete or classic H. mole forms when an egg whose nucleus is lost and inactivated undergoes fertilization.
In this, the mole resembles a bunch of white grapes.
In this, the fluid-filled vesicles grow rapidly, causing the uterus to become larger than the expected duration of pregnancy.
In complete moles, the fetus, placenta, and amniotic membranes are involved.
Complete moles can also progress to carcinoma and do not contain an embryo.
2) Incomplete mole
This contains embryonic or fetal parts and the amniotic sac is present.
This contains congenital anomalies.
This contains an underdeveloped embryo that fails to survive.
f) Post-partum blue – પોસ્ટ પાર્ટમ બ્લયુ
Many women experience postpartum blues due to hormonal changes, usually three to seven days after delivery. It lasts for one to two weeks. This is due to the drop in estrogen and progesterone hormone levels. The mother usually cries easily, feels irritable, sad, and confused.
g) Obstetrical nursing – ઑબ્સ્ટેટ્રિકલ નર્સિંગ
Obstetric nursing, also known as perinatal nursing, is a nursing specialty that focuses on caring for patients who are pregnant, are pregnant, or have recently delivered. Obstetric nurses help with prenatal care testing, pregnancy complications, and the care provided to patients during delivery and labor.
h) Decapitation – ડીકેપીટેશન
Decapitation is a destructive delivery.
This destructive delivery is performed when the fetus has died in the womb (uterus) and to expel the dead fetus from the womb through the vaginal canal, this type of destructive delivery is performed in which some body parts of the dead fetus are reduced. Due to which the dead fetus can be easily delivered through the birth canal.
In decapitation delivery, the head of the dead fetus in the womb (uterine cavity) is cut from its trunk and then the fetus is delivered along with the extraction of the trunk of the fetus. This procedure is called decapitation.
Q-6(A) Fill in the blanks – ખાલી જગ્યા પૂરો
- Golden color of amniotic fluid indicates……… એમ્નિઓટીક ફ્લુઈડનો ગોલ્ડન કલર ……………સુચવે છે.
Ans:–rh incompetability
- Normal labour is called …………………….. નોર્મલ લેબરને …………………………..કહેવાય છે
Ans:-eutocia
- Fetal heart sound can be heard in…………..weeks. ફીટલ હાર્ટ સાઉન્ડ……………….. અઠવાડીયે સાંભળી શકાય છે.
Ans . 18–20 weeks
- First menstrual period is known as………………….. પ્રથમ માસિક આવે તે………………………….. તરીકે ઓળખાય છે.
Ans:-menarche
- During pregnancy endometrium is known as………………….. પ્રેગનન્સી દરમ્યાન એન્ડોમેટ્રીયમ ……………………તરીકે ઓળખાય છે.
Ans:-desidua
(B) True or False – ખરા ખોટા જણાવો.
1. Bishop score is used to assess the progress of labor. બીશપ સ્કોરનો ઉપયોગ લેબરનો પ્રોગ્રેસ જાણવા થાય છે.
FALSE
2. HCG hormones is responsible for hyperemesis gravidarum. HCG હોર્મોન એ હાયપર એમેસીસ ગ્રેવીડેરમ માટે જવાબદાર છે.
True
3. Per vaginal examination is contra indicated in abruptio placenta. એબરપ્ટીઓ પ્લેસન્ટામાં વજાઈનલ એકઝામીનેશન ના કરવી જોઈએ.
True
4.Artificial rupture of membrane is a method of surgical induction of labor. આર્ટીફીશીયલ રપ્ચર ઓફ મેમ્બ્રેનએ સર્જીકલ ઈન્ડકશન ઓફ લેબરની એક પધ્ધતી છે.
True
5.HCG is secreted from cytotrophoblast layer of placenta. HCG એ પ્લેસન્ટાના સાયટોટ્રોફોબ્લાસ્ટ લેયર માંથી સ્ત્રાવ થાય છે.
FALSE
(C) Match the following – જોડકા જોડો
A B
(1) Hegar’s sign હેગાર્સ સાઈન (1) Absence of menstruation મેન્સ્ટ્રુએશનની ગેરહાજરી
(2) Polymenorrhagia પોલીમેનોરેજીયા (2) Irregular menstruation અનિયમિત મેન્સ્ટ્રુએશન
(3) Palmer’s sign પામર્સ સાઈન (3) Softening of isthmus ઈસ્થમસનું નરમ થવું SUMMOS
(4) Menorrhagia મેનોરેજીયા (4) Frequent menstruation વારંવાર મેન્સ્ટ્રુએશન આવવું
(5) Chadwick’s sign ચોડવીકસ સાઈન (5) Rhythmic and regular painless contraction લયબધ્ધ અને નિયમિત કોન્ટ્રાકશન
(6) Bluish discoloration of cervix and vagina સર્વિશ અને વજાઈના વાદળી રંગની થવી
Answer
Q-1 . Hegars sign :- 3. Softening of isthmus
Q-2. Polymenorrhagia:- 4. Frequent menstruation
Q-3. Palmers sign :-5. rhythmic and regular painless contraction
Q-4 . Menorrhagia :- 2. Irregular menstruation
Q-5 . Chadwick ‘s Sign :- 6. bluish discoloration of cervix and vagina
