FON-VITAL SIGN-SYNOPSIS-7-PHC
🌟 VITAL SIGNS 🌟
🩺 “Vital signs are life’s signals – they reflect body function and balance.”
📘 DEFINITION
🗨️ Vital signs are the basic measurements that indicate a person’s physiological status and reflect the functioning of essential body systems. They are assessed regularly to monitor health, detect abnormalities, and guide treatment.
🧩 THE 5 MAIN VITAL SIGNS
| 🔢 No. | 📖 Vital Sign | 🔍 What it Indicates |
|---|---|---|
| 1️⃣ | Temperature (T) 🌡️ | Body heat regulation |
| 2️⃣ | Pulse (P) ❤️ | Heart rate and rhythm |
| 3️⃣ | Respiration (R) 🌬️ | Breathing rate and quality |
| 4️⃣ | Blood Pressure (BP) 💉 | Circulatory pressure |
| 5️⃣ | Oxygen Saturation (SpO₂) 🫁 | Oxygen level in blood |
Optional 6️⃣: Pain Level – sometimes referred to as the “5th or 6th vital sign”
🌡️ 1. BODY TEMPERATURE
✅ Normal Range:
| 🌍 Site | 🌡️ Normal Temp |
|---|---|
| Oral | 36.5–37.5°C (97.7–99.5°F) |
| Rectal | 37.0–38.1°C (98.6–100.6°F) |
| Axillary | 36.0–37.0°C (96.6–98.6°F) |
| Tympanic | 36.8–38.0°C (98.2–100.4°F) |
🚩 Abnormalities:
- 🔥 Fever (Pyrexia): > 100.4°F (38°C)
- 🧊 Hypothermia: < 95°F (35°C)
❤️ 2. PULSE
✅ Normal Rate:
- Adults: 60–100 bpm
- Children: 80–120 bpm
- Infants: 100–160 bpm
📍 Sites for Pulse Check:
- Radial (wrist)
- Carotid (neck)
- Brachial (arm)
- Apical (chest – with stethoscope)
- Femoral, Popliteal, Dorsalis pedis (legs/feet)
🛑 Irregularities:
- Tachycardia: > 100 bpm
- Bradycardia: < 60 bpm
- Check rhythm, strength, equality
🌬️ 3. RESPIRATION
✅ Normal Rate:
- Adults: 12–20 breaths/min
- Children: 20–30/min
- Infants: 30–60/min
⚠️ Observe:
- Rate, depth (shallow/deep), rhythm, effort
- Use of accessory muscles
- Cyanosis (blue lips/skin)
🚩 Abnormalities:
- Tachypnea: > 20/min
- Bradypnea: < 12/min
- Apnea: No breathing
💉 4. BLOOD PRESSURE (BP)
✅ Normal BP:
- Adults: 120/80 mmHg
💡 Components:
- Systolic (upper): Pressure during heart contraction
- Diastolic (lower): Pressure during heart rest
📈 BP Ranges:
| 📊 Category | 🔢 BP Reading |
|---|---|
| Normal | < 120 / < 80 mmHg |
| Prehypertension | 120–139 / 80–89 |
| Hypertension Stage 1 | 140–159 / 90–99 |
| Hypotension | < 90 / < 60 |
Use right cuff size, proper positioning (arm at heart level)
🫁 5. OXYGEN SATURATION (SpO₂)
✅ Normal Range:
- 95% – 100% (via pulse oximeter)
🚨 Below 90%: Hypoxemia
⚠️ May indicate respiratory distress or need for oxygen therapy
🌟 OPTIONAL: PAIN AS 5TH/6TH VITAL SIGN 🌟
✅ Use pain scale (0–10) or Wong-Baker Faces Scale
📝 Ask location, duration, quality (sharp, dull), triggers, and relief
👩⚕️ NURSE’S RESPONSIBILITIES DURING VITAL SIGN MONITORING
🔹 Use clean, calibrated equipment
🔹 Explain procedure to patient
🔹 Ensure correct position (sitting/lying down)
🔹 Document accurately: value, site, time
🔹 Report abnormal findings immediately
🔹 Monitor trends, not just isolated readings
🔹 Reassess if patient condition changes
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: Normal adult respiratory rate?
🅰️ 12–20 breaths/min
✅ Q: Pulse site used in CPR in adults?
🅰️ Carotid
✅ Q: What is the normal SpO₂ range?
🅰️ 95%–100%
✅ Q: First action if BP is 80/40 mmHg?
🅰️ Report immediately to doctor
✅ Q: Which is the most accurate site for body temperature?
🅰️ Rectal (for core temp)
🌡️🌟 VITAL SIGN – TEMPERATURE 🌟
🩺 “A rise or fall in temperature can be the first whisper of illness.”
✅ Monitoring temperature is essential to assess metabolic function, immune response, and overall homeostasis.
📘 DEFINITION
🗨️ Body temperature refers to the degree of heat maintained by the body, reflecting the balance between heat produced by metabolic processes and heat lost to the environment.
- Core temperature = internal organs (e.g., rectal)
- Surface temperature = skin (e.g., axillary)
🔍 TYPES OF BODY TEMPERATURE
| 🌈 Type | 🌡️ Range | 🔎 Interpretation |
|---|---|---|
| 🌿 Normal (Afebrile) | 36.5–37.5°C (97.7–99.5°F) | Healthy regulation |
| 🔥 Fever (Pyrexia) | 38–40°C (100.4–104°F) | Infection, inflammation |
| 🌡️ Hyperpyrexia | > 41°C (105.8°F) | Medical emergency |
| 🧊 Hypothermia | < 35°C (95°F) | Cold exposure, anesthesia |
| 🔁 Intermittent Fever | Rises & falls; temp returns to normal daily | |
| 🎢 Remittent Fever | Fluctuates but does not return to normal | |
| 📈 Sustained Fever | Constantly high with little fluctuation | |
| 🔂 Relapsing Fever | Periods of fever alternate with normal temp for days |
📊 TEMPERATURE RANGES BY SITE
| 📍 Site | 🌡️ Normal Range | 🔍 Remarks |
|---|---|---|
| 🧍 Oral | 36.5–37.5°C | Most common & convenient |
| 🍑 Rectal | 37.0–38.1°C | Most accurate (core temp) |
| 🧼 Axillary | 36.0–37.0°C | Least accurate; used in infants |
| 👂 Tympanic | 36.8–38.0°C | Reflects core temp (ear canal) |
| 🌬️ Temporal Artery | 36.5–37.5°C | Non-invasive & fast |
🔺 Rectal readings are usually 0.5°C higher than oral; axillary is 0.5°C lower
🔺 Tympanic and temporal readings approximate core temperature
🔎 FACTORS AFFECTING BODY TEMPERATURE
| 🌀 Factor | 📝 Effect |
|---|---|
| 🕒 Time of Day | Lower in morning, higher in late afternoon/evening |
| 🎂 Age | Elderly = lower temp; infants = unstable regulation |
| ⚡ Activity | Increases temperature |
| 🍽️ Food/Drink | Hot/cold items can affect oral readings |
| 😰 Stress | Can increase temp slightly |
| 💊 Medications | Antipyretics, anesthetics, hormones |
| 🌬️ Environment | Hot/cold climates affect surface readings |
| 🧠 Illness | Infections, trauma, autoimmune disorders elevate temp |
🧪 TYPES OF THERMOMETERS
| 🔧 Type | 💡 Use | 🌟 Special Note |
|---|---|---|
| 🌡️ Glass (Mercury) | Oral/Rectal/Axillary | Outdated, fragile, toxic if broken |
| 📟 Digital | Oral/Rectal/Axillary | Fast, common, easy to read |
| 👂 Tympanic Infrared | Ear | Quick, suitable for children |
| 🌬️ Temporal Infrared | Forehead | Non-contact, safe for all ages |
| 🧊 Disposable (chemical dot) | Oral/Axillary | Single-use, less accurate |
⏱️ DURATION OF TEMPERATURE MEASUREMENT
| 🧪 Site | ⏱️ Time |
|---|---|
| Oral (digital) | 30–60 seconds |
| Rectal | 2–3 minutes |
| Axillary | 3–5 minutes |
| Tympanic/Temporal | 1–2 seconds |
👩⚕️ NURSE’S RESPONSIBILITIES
🟢 Before Taking Temp:
- Wash hands, gather equipment
- Explain procedure to patient
- Ask about recent hot/cold food or smoking (wait 30 mins for oral temp)
- Choose appropriate site & thermometer
🟡 During Procedure:
- Use gloves if needed
- Ensure patient comfort and privacy
- Stay with the patient (especially children)
🔴 After Taking Temp:
- Clean device properly
- Record value with site, time, and method
- Report if:
- 38°C (fever)
- < 35°C (hypothermia)
- Implement fever/hypothermia protocol as needed
📝 SAMPLE DOCUMENTATION
📝 “Temperature: 38.2°C, oral, at 10:00 AM. Patient febrile. Paracetamol 500 mg given as per doctor’s order. Reassess in 1 hour.”
🚩 NURSING CARE FOR FEVER (PYREXIA)
✅ Monitor temperature every 4 hours
✅ Provide tepid sponge if ordered
✅ Encourage oral fluids
✅ Remove excess clothing/blankets
✅ Administer antipyretics as prescribed
✅ Monitor for chills, sweating, confusion
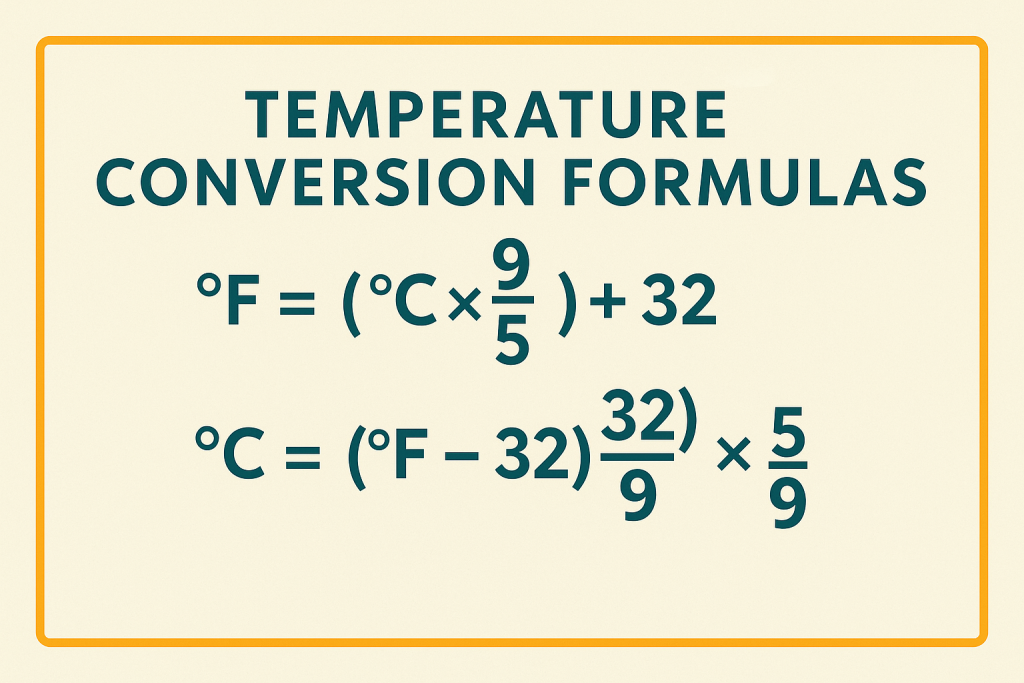
📋 Quick Reference Table (Common Values)
| °F (Fahrenheit) | °C (Celsius) |
|---|---|
| 98.6°F | 37°C (Normal Body Temp) |
| 100.4°F | 38°C (Fever Threshold) |
| 102°F | 38.9°C |
| 104°F | 40°C |
| 95°F | 35°C (Hypothermia Start) |
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the normal adult oral temperature?
🅰️ 36.5–37.5°C
✅ Q: Which thermometer gives the most accurate reading?
🅰️ Rectal thermometer
✅ Q: What type of fever returns to normal between episodes?
🅰️ Intermittent fever
✅ Q: Which site is safest for children under 3?
🅰️ Axillary or tympanic
✅ Q: When is temperature highest during the day?
🅰️ Evening
🌟 VITAL SIGN – PULSE 🌟
❤️ “Each beat speaks of life – feel it, count it, understand it.”
📘 DEFINITION
🗨️ Pulse is the rhythmic expansion and contraction of an artery as blood is forced through it by the beating of the heart. It reflects heart rate, rhythm, and strength, and is an essential indicator of circulatory health.
🧠 PHYSIOLOGY OF PULSE
🩺 Pulse is generated by:
- Left ventricular contraction
- Felt in peripheral arteries as a pressure wave
- Provides info on cardiac output & peripheral circulation
📍 COMMON SITES FOR PULSE ASSESSMENT
| 🔍 Site | 📌 Location | 💡 Use |
|---|---|---|
| ✋ Radial | Wrist (thumb side) | Most common site |
| 🧠 Temporal | Forehead | Used in infants |
| 👂 Carotid | Neck | CPR in adults |
| 💪 Brachial | Elbow fold | BP & infant pulse |
| 🦵 Femoral | Groin | Circulation check |
| 🦶 Popliteal | Behind knee | Leg circulation |
| 👣 Dorsalis pedis | Top of foot | Peripheral perfusion |
| 🧦 Posterior tibial | Inner ankle | Circulatory status in diabetics |
| 💓 Apical | Chest (5th intercostal space, midclavicular line) | Most accurate; used in children, irregular HR |
✅ NORMAL PULSE RATES (Resting)
| 👶 Age Group | 💓 Normal Pulse |
|---|---|
| Newborns | 120–160 bpm |
| Infants | 100–160 bpm |
| Children (1–10 yrs) | 70–120 bpm |
| Adults | 60–100 bpm |
| Older adults | 60–100 bpm |
🚩 ABNORMAL PULSE FINDINGS
| 🚨 Condition | 🔍 Description |
|---|---|
| 🔼 Tachycardia | Pulse > 100 bpm (fever, anxiety, dehydration, anemia) |
| 🔽 Bradycardia | Pulse < 60 bpm (athletes, heart block, meds) |
| ❌ Irregular rhythm | Uneven beats – may indicate arrhythmia |
| ❗ Thready or weak pulse | Low volume – shock or blood loss |
| 💪 Bounding pulse | Strong pulse – fever, anxiety, fluid overload |
👩⚕️ CHARACTERISTICS OF PULSE TO ASSESS
| 🧩 Characteristic | 🔍 What to Check |
|---|---|
| 🔢 Rate | Number of beats/min |
| 🔄 Rhythm | Regular or irregular |
| 💪 Strength | Weak, strong, bounding |
| ✋ Equality | Compare both sides (e.g., radial pulses) |
| ⏱️ Volume | Full, normal, thready |
🧰 METHOD OF ASSESSING PULSE (Radial)
1️⃣ Wash hands & explain procedure
2️⃣ Position patient comfortably with arm supported
3️⃣ Use index and middle fingers (not thumb)
4️⃣ Feel the radial pulse at wrist
5️⃣ Count for 30 seconds × 2 (if regular) or 60 seconds (if irregular)
6️⃣ Observe rate, rhythm, strength
7️⃣ Record findings accurately
🔬 APICAL PULSE
✔️ Use a stethoscope
✔️ Locate at 5th intercostal space, left midclavicular line
✔️ Count for 1 full minute
✔️ Preferred for:
- Infants & children
- Cardiac meds (e.g., digoxin)
- Irregular or faint radial pulse
📝 SAMPLE DOCUMENTATION
📝 “Pulse: 86 bpm, regular, strong, radial site, recorded at 8:00 AM. No abnormalities noted.”
📝 “Apical pulse: 72 bpm, regular, assessed prior to digoxin administration.”
⚠️ NURSE’S RESPONSIBILITIES
🔹 Choose correct site based on age/condition
🔹 Ensure patient is resting before measurement
🔹 Use accurate counting method
🔹 Reassess if irregular or abnormal
🔹 Report if:
- < 60 bpm or > 100 bpm
- Irregular or thready pulse
🔹 Monitor closely before administering cardiac meds
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the normal pulse rate in adults?
🅰️ 60–100 bpm
✅ Q: Which pulse site is used during adult CPR?
🅰️ Carotid
✅ Q: Which pulse site is used in infants?
🅰️ Brachial
✅ Q: What is a bounding pulse?
🅰️ Very strong/full pulse (often seen in fever or fluid overload)
✅ Q: Where is the apical pulse located?
🅰️ 5th intercostal space, midclavicular line
🌬️🌟 VITAL SIGN – RESPIRATION 🌟
🫁 “Each breath is a rhythm of life – calm, clear, continuous.”
✔️ Monitoring respiration provides key insight into a patient’s oxygenation, ventilation, and respiratory health.
📘 DEFINITION
🗨️ Respiration is the process of inhaling oxygen and exhaling carbon dioxide, involving both external (lung exchange) and internal (tissue exchange) respiration.
In vital signs, we assess the rate, rhythm, depth, and effort of breathing.
✅ NORMAL RESPIRATORY RATES BY AGE
| 👶 Age Group | 🌬️ Normal Rate (breaths/min) |
|---|---|
| Newborn | 30–60 |
| Infant (1 yr) | 30–40 |
| Children (1–7 yrs) | 20–30 |
| Adults | 12–20 |
| Elderly | 12–24 |
📊 CHARACTERISTICS OF RESPIRATION TO ASSESS
| 🔍 Aspect | 💡 What to Observe |
|---|---|
| 🔢 Rate | Breaths per minute |
| 🔄 Rhythm | Regular or irregular breathing pattern |
| 📏 Depth | Shallow, normal, or deep |
| 🔺 Effort | Easy, labored, noisy, or use of accessory muscles |
| 👂 Sounds | Wheezing, stridor, crackles (on auscultation) |
🚨 ABNORMAL BREATHING PATTERNS
| ⚠️ Type | 📝 Description |
|---|---|
| 🔼 Tachypnea | Rapid breathing (> 20/min in adults) |
| 🔽 Bradypnea | Slow breathing (< 12/min in adults) |
| ⛔ Apnea | Absence of breathing |
| 📈 Hyperventilation | Deep, rapid breathing (anxiety, fever) |
| 📉 Hypoventilation | Shallow, slow breathing (drug overdose) |
| 📊 Cheyne-Stokes | Periodic breathing with gradual increases and decreases, followed by apnea (seen in dying patients, brain injury) |
| 🔁 Kussmaul’s | Deep, labored breathing (metabolic acidosis, DKA) |
| 💨 Orthopnea | Difficulty breathing unless sitting upright (seen in CHF) |
👩⚕️ METHOD OF RESPIRATION ASSESSMENT
1️⃣ Explain procedure (without focusing too much on breathing – may alter pattern)
2️⃣ Position patient comfortably (semi-Fowler’s ideal)
3️⃣ Watch chest/abdomen movement silently
4️⃣ Count breaths for 1 full minute if irregular, or 30 sec × 2 if regular
5️⃣ Observe rhythm, depth, effort
6️⃣ Record and report findings
📉 NURSE’S RESPONSIBILITIES
🔹 Do not tell the patient you’re counting respiration (may affect rate)
🔹 Use watch with second hand
🔹 Assess after pulse check (continue to observe chest)
🔹 Look for nasal flaring, use of accessory muscles, cyanosis
🔹 Document rate, depth, rhythm, and abnormalities
📝 SAMPLE DOCUMENTATION
📝 “Respiration: 18 breaths/min, regular rhythm, normal depth, no signs of respiratory distress. Monitored at 10:00 AM.”
🧠 FACTORS AFFECTING RESPIRATION
| ⚙️ Factor | 📈 Effect |
|---|---|
| 🧒 Age | Higher in infants, slower in adults |
| ⚡ Activity | Increases rate |
| 😰 Emotions | Stress/anxiety increase rate |
| 🧪 Medications | Narcotics slow breathing; bronchodilators may ease it |
| 🌡️ Fever | Increases metabolic rate → ↑ respiratory rate |
| 🩸 Anemia | Increases rate due to low O₂ transport |
| 💔 Heart/Lung Disease | May cause dyspnea, altered patterns |
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the normal respiratory rate for a healthy adult?
🅰️ 12–20 breaths/min
✅ Q: Which breathing pattern is seen in diabetic ketoacidosis?
🅰️ Kussmaul’s respiration
✅ Q: What is apnea?
🅰️ Absence of breathing
✅ Q: What signs indicate respiratory distress?
🅰️ Nasal flaring, cyanosis, accessory muscle use
✅ Q: How should a nurse count respiration accurately?
🅰️ Without informing the patient to avoid altered breathing
💉🌟 VITAL SIGN – BLOOD PRESSURE (BP) 🌟
🩺 “Blood pressure is a silent indicator of cardiovascular health — check it, respect it.”
📘 DEFINITION
🗨️ Blood pressure is the force exerted by circulating blood on the walls of arteries. It reflects the efficiency of the heart, blood vessels, and overall circulatory system.
✅ It is measured in millimeters of mercury (mmHg) and has two components:
- Systolic Pressure (SBP): Peak pressure during heart contraction
- Diastolic Pressure (DBP): Minimum pressure during heart relaxation
📊 NORMAL BLOOD PRESSURE VALUES (ADULTS)
| 💡 Component | 🌡️ Normal Range |
|---|---|
| ✅ Systolic | 90–120 mmHg |
| ✅ Diastolic | 60–80 mmHg |
| 📊 Normal BP | 120/80 mmHg |
📈 BP CLASSIFICATION (According to AHA)
| 🩸 Category | 🔢 BP Reading |
|---|---|
| ✅ Normal | < 120 / < 80 mmHg |
| ⚠️ Elevated | 120–129 / < 80 mmHg |
| 🚨 Stage 1 Hypertension | 130–139 / 80–89 mmHg |
| 🚨 Stage 2 Hypertension | ≥ 140 / ≥ 90 mmHg |
| 🆘 Hypertensive Crisis | > 180 / > 120 mmHg |
| 🔽 Hypotension | < 90 / < 60 mmHg |
🔍 TYPES OF BLOOD PRESSURE
| 🔢 Type | 📖 Description |
|---|---|
| 📉 Hypotension | Low BP → Dizziness, fainting |
| 📈 Hypertension | High BP → Risk of stroke, heart disease |
| 🔁 Postural (Orthostatic) Hypotension | Drop in BP on standing up |
| ⚖️ White Coat Hypertension | Elevated BP in clinical settings only |
| 📉 Shock BP | Critically low due to blood loss or sepsis |
🧠 FACTORS AFFECTING BLOOD PRESSURE
| 🔄 Factor | 📊 Effect |
|---|---|
| 🎂 Age | ↑ with age |
| ⚡ Activity | ↑ during exercise |
| 🍵 Caffeine/Smoking | Temporary ↑ |
| 💊 Medications | Some raise, some lower BP |
| 😰 Emotions | Stress/anxiety ↑ |
| 🧂 Sodium intake | ↑ BP |
| 🩸 Blood loss | ↓ BP |
| 🌡️ Temperature | Cold ↑ / Heat ↓ |
🧰 EQUIPMENT USED
✔️ Sphygmomanometer (Manual – mercury or aneroid)
✔️ Stethoscope
✔️ Automatic digital BP machine
✅ METHOD OF MEASURING BLOOD PRESSURE (Manual)
1️⃣ Wash hands & explain procedure
2️⃣ Ensure patient is resting 5 minutes, seated, arm supported at heart level
3️⃣ Select correct cuff size (covering 2/3rd of upper arm)
4️⃣ Place cuff 2.5 cm above elbow crease
5️⃣ Palpate brachial artery
6️⃣ Inflate cuff while auscultating → note first sound (systolic)
7️⃣ Note when sound disappears → diastolic
8️⃣ Deflate cuff slowly
9️⃣ Record reading with site, position, arm, and time
📝 SAMPLE DOCUMENTATION
📝 “BP: 128/78 mmHg, right arm, sitting, at 8:00 AM. No abnormalities noted.”
⚠️ NURSE’S RESPONSIBILITIES
🔹 Use correct cuff size
🔹 Avoid taking BP on injured, IV, or post-mastectomy arm
🔹 Compare both arms on first assessment
🔹 Retake if result is abnormally high or low
🔹 Report:
- 140/90 (Hypertension)
- <90/60 (Hypotension)
🔹 Monitor trends, not just one reading
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the normal adult blood pressure?
🅰️ 120/80 mmHg
✅ Q: What is the name of the device used to measure BP?
🅰️ Sphygmomanometer
✅ Q: What causes postural hypotension?
🅰️ Sudden drop in BP when standing
✅ Q: First sound heard while deflating BP cuff indicates?
🅰️ Systolic pressure
✅ Q: Which artery is used in BP measurement?
🅰️ Brachial artery
🌟 VITAL SIGN – SpO₂ (OXYGEN SATURATION) 🌟
🫁 “Every cell needs oxygen — monitoring SpO₂ tells us how well the lungs are doing their job.”
📘 DEFINITION
🗨️ SpO₂ (Peripheral Oxygen Saturation) is the percentage of hemoglobin in the blood that is saturated with oxygen.
✅ It is a non-invasive, quick, and reliable method to assess a patient’s oxygenation status.
✅ NORMAL SpO₂ VALUES
| 🩸 Condition | 📊 SpO₂ Range |
|---|---|
| ✅ Normal (Healthy Adults) | 95%–100% |
| ⚠️ Mild Hypoxemia | 91%–94% |
| 🚨 Moderate Hypoxemia | 86%–90% |
| 🆘 Severe Hypoxemia | < 85% |
❗ SpO₂ < 90% requires immediate medical attention!
📌 Special Considerations
- COPD patients may maintain 88%–92% as acceptable baseline
- Always assess SpO₂ along with respiratory rate & effort
🧰 EQUIPMENT USED
🔹 Pulse oximeter
– Device clips to finger, toe, earlobe, or foot (infants)
– Uses infrared light to measure oxygen levels
👩⚕️ STEPS TO MEASURE SpO₂
1️⃣ Explain the procedure to the patient
2️⃣ Ensure patient is at rest and comfortable
3️⃣ Select site: index/middle finger, toe, or ear lobe
4️⃣ Remove nail polish, cold hands, or fake nails if present
5️⃣ Place pulse oximeter probe correctly
6️⃣ Wait for a stable reading (typically 10–30 seconds)
7️⃣ Note SpO₂ (%) and pulse rate
📝 SAMPLE DOCUMENTATION
📝 “SpO₂: 98% on room air, stable. Pulse: 82 bpm. Recorded at 10:00 AM.”
📝 “SpO₂: 91% with nasal oxygen @ 2 L/min. Patient monitored for respiratory distress.”
🧠 FACTORS AFFECTING ACCURACY
| ⚠️ Interference | 💡 Result |
|---|---|
| 💅 Nail polish/artificial nails | False low reading |
| ❄️ Cold extremities | Weak signal |
| 🚫 Poor circulation | Unreliable reading |
| 💍 Movement/tremors | Fluctuating readings |
| 🧠 Carbon monoxide poisoning | False normal SpO₂ |
🧯 NURSING ACTIONS FOR LOW SpO₂
✅ Reposition patient in semi-Fowler’s or high-Fowler’s
✅ Encourage deep breathing or coughing
✅ Administer oxygen therapy as prescribed
✅ Monitor respiratory rate, effort, and color
✅ Inform physician if SpO₂ remains below 92% or declines suddenly
✅ Recheck SpO₂ every 15–30 minutes if unstable
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the normal SpO₂ range for a healthy adult?
🅰️ 95%–100%
✅ Q: Which instrument is used to measure SpO₂?
🅰️ Pulse oximeter
✅ Q: What is the acceptable SpO₂ range in a COPD patient?
🅰️ 88%–92%
✅ Q: Which factors interfere with SpO₂ readings?
🅰️ Nail polish, poor circulation, movement
✅ Q: What is the first nursing action for SpO₂ of 89% on room air?
🅰️ Reassess and administer oxygen if prescribed
🌟 PAIN ASSESSMENT – THE 5th VITAL SIGN 🌟
⚠️ “Pain is what the patient says it is — assess it, believe it, manage it.”
🩺 Pain is now widely recognized as the 5th vital sign, and accurate assessment is essential to provide quality patient care.
📘 DEFINITION
🗨️ Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, as described by the patient.
✅ It is subjective, meaning only the person experiencing pain can truly describe it.
🧩 CHARACTERISTICS OF PAIN (PQRST METHOD)
| 🔠 Letter | ❓ Meaning | 💡 Nurse’s Questions |
|---|---|---|
| P | Provocation | What causes or worsens the pain? |
| Q | Quality | What does the pain feel like? (sharp, dull, burning) |
| R | Region/Radiation | Where is the pain? Does it move? |
| S | Severity | Rate pain on a scale of 0 to 10 |
| T | Timing | When did it start? Constant or intermittent? |
📊 PAIN INTENSITY SCALES
1️⃣ Numerical Rating Scale (NRS)
🔢 0 = No pain | 10 = Worst possible pain
🧑 Used for: Adults who can rate pain
2️⃣ Visual Analog Scale (VAS)
📏 A straight line from “No pain” ➡️ “Worst pain”
🧑 Used in: Adults or older children
3️⃣ Wong-Baker Faces Pain Scale 😊😐😢😭
📸 Patient points to a face that represents their pain
🧒 Used in: Children aged 3+, language barriers, elderly
4️⃣ FLACC Scale (For Non-verbal Patients)
🧸 Stands for:
- F = Face
- L = Legs
- A = Activity
- C = Cry
- C = Consolability
✅ Each category scored 0–2
✅ Total score out of 10
🧑🍼 Used in: Infants, unconscious, or non-verbal patients
🎯 TYPES OF PAIN
| 🔍 Type | 💡 Description |
|---|---|
| 🩸 Acute Pain | Sudden onset, short duration (injury, surgery) |
| ♾️ Chronic Pain | Lasts > 3 months (arthritis, cancer) |
| 🧠 Neuropathic Pain | Nerve-related (burning, tingling) |
| 🦴 Somatic Pain | Skin, muscle, bone (localized, sharp) |
| 🧘 Visceral Pain | Internal organs (cramping, pressure) |
| ❓ Referred Pain | Pain felt in different area than origin |
👩⚕️ NURSE’S ROLE IN PAIN ASSESSMENT
✅ Believe the patient – pain is subjective
✅ Use standard pain scales
✅ Assess before and after interventions
✅ Observe non-verbal cues (grimace, guarding, moaning)
✅ Document location, intensity, quality, duration, relief
✅ Collaborate for pharmacologic (meds) and non-pharmacologic (massage, repositioning, heat/cold) interventions
✅ Reassess regularly (esp. post-analgesia)
📝 SAMPLE DOCUMENTATION
📝 “Patient reports sharp pain in lower back, rated 8/10 on NRS. Analgesic (Tab Paracetamol 500 mg) given at 10:00 AM. Reassessed at 10:45 AM — pain reduced to 3/10. Patient comfortable.”
📌 MOST ASKED EXAM QUESTIONS (MCQ STYLE)
✅ Q: What is the 5th vital sign in nursing?
🅰️ Pain
✅ Q: Which scale is best for assessing pain in children above 3 years?
🅰️ Wong-Baker Faces Scale
✅ Q: What does the “P” in PQRST stand for?
🅰️ Provocation
✅ Q: When should pain be reassessed after medication?
🅰️ 30–60 minutes after administration
✅ Q: What type of pain results from nerve damage?
🅰️ Neuropathic pain