F.Y-UNIT-2-P.B.B.SC-NOTE
1. Ethical Issues in Nursing
🔹 DEFINITION:-
Ethics refers to a branch of philosophy concerned with distiction between right and wrong , on the basis of body of knowledge not only on the basis of opinions OR the moral principles and values that guide nurses in making correct professional decisions — what is right or wrong, good or bad in patient care.
⚫MAJOR ETHICAL PRINCIPLES :-
🔹 Common Ethical Dilemmas in Nursing:
- End-of-life decisions (e.g., withdrawing life support)
- Abortion or contraception counselling
- Allocation of scarce resources (ICU beds, ventilators)
- Maintaining confidentiality in HIV-positive cases
- Truth-telling in terminal illness
⚖️ 2. Legal issue in nursing
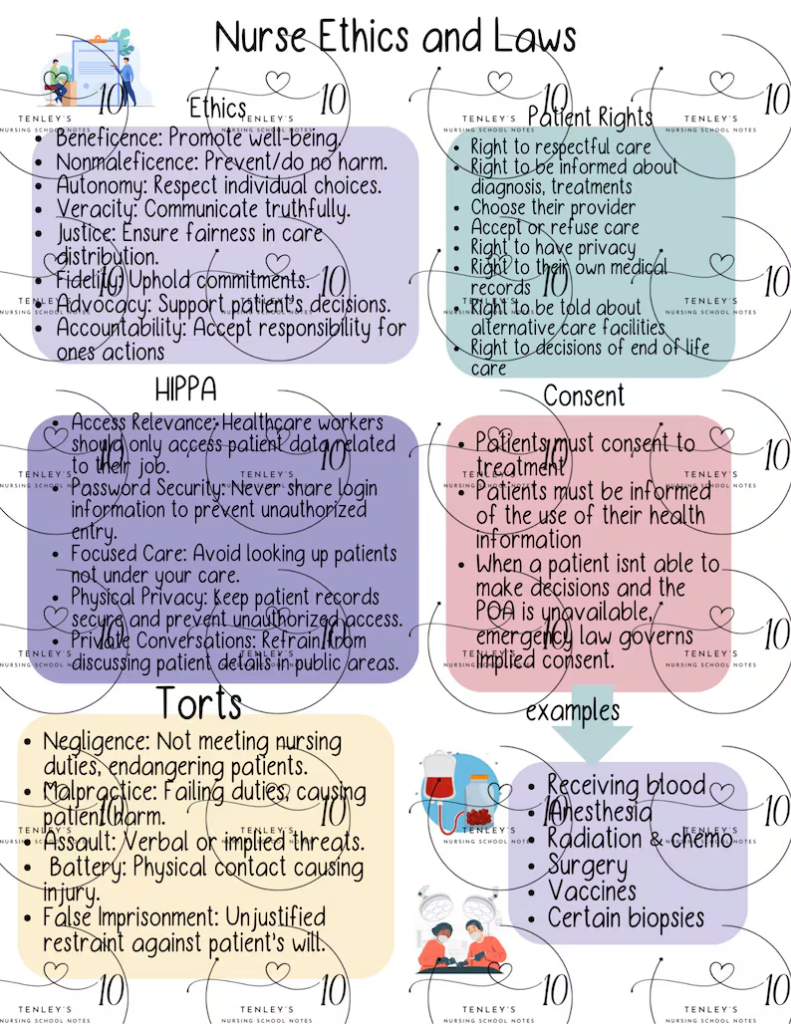
| Principle | Meaning | Example in Nursing |
|---|---|---|
| Autonomy | Respecting the patient’s right to make their OWN DECISIONS . | A nurse respects a patient’s decision to refuse blood transfusion due to religious belief. |
| Beneficence | DOING GOOD AND PROMOTING the welfare of the patient. | Giving pain relief medication to a post-operative patient to relieve suffering. |
| Non-maleficence | Avoiding harm to patients. TO TAKE CARE OF PATEINT IN SUCH A WAY THAT NO ANY INJURY HAPPEN . | Checking patient’s drug allergy before administering any injection. |
| Justice | Providing equal care to all WITHOUT NO DISCRIMINATION OF RACE , COLOUR , CASTE , RELIGION , NATIONALITY. | Giving equal priority to rich and poor patients in emergency care. |
| Fidelity | Keeping promises and MAINTAINING TRUST. | If a nurse promises to bring lab results soon, she fulfills that commitment. |
| TO BE LOYAL WITH PATIENT | ||
| Veracity | Being truthful and honest with patients. | Informing a patient truthfully about the side effects of chemotherapy. |
| Confidentiality | Keeping patient information private and confidentiel . | Not disclosing a patient’s HIV status to others without consent. |
🔹 Definition:
Legal issues relate to laws that regulate nursing practice, ensure patient safety, and protect the nurse’s professional rights.
🔹 Types of Laws Affecting Nursing:
Nurses provide safe and competent care.Patients receive ethical and lawful treatment.The nursing profession maintains accountability and integrity.
🧾 2. Objectives of Nursing Laws
- To protect the public from unqualified and unsafe nursing practices.
- To define the scope of nursing practice.
- To set educational and registration standards for nurses.
- To provide a framework for legal accountability in nursing actions.
- To promote professional discipline and ethical behavior.
| Type | Description | Example |
|---|---|---|
| Civil Law | Deals with rights of individuals and compensation for wrongs. | A patient sues a nurse for negligence during IV infusion. |
| Criminal Law | Protects society; violations are punishable by fines or imprisonment. | Administering a lethal drug dose intentionally is a criminal offence. |
| Administrative Law | Regulates the functioning of government and professional councils. | Indian Nursing Council (INC) and State Nursing Councils define nurse registration laws. |
⭐OTHER :-
🧩 B. Private Law (Civil Law)
Civil law regulates relationships between individuals, ensuring compensation for harm or injury.
🔸 1. Contract Law
- Governs agreements between nurse and employer, or nurse and patient.
Example:
- If a nurse signs a bond to serve for 2 years after training and leaves early → Breach of Contract
- A private-duty nurse failing to provide care as per contract terms → Liable for compensation.
🔸 2. Tort Law
A most important aspect of nursing in which
Tort = “a civil wrong” which causes harm to another person.
Common torts in nursing are:
| Type | Definition | Example |
|---|---|---|
| Negligence | Failure to act as a reasonably prudent nurse would or failure to achieve the basic nursing care to patient . | Not checking IV rate → patient develops pulmonary edema or forgetting administration of meds or injectable on time . |
| Malpractice | Professional negligence causing harm | Giving wrong medication → cardiac arrest . eg. asthalin liquid for inhalation given IV due to negligence instead in a nebulization. |
| Assault | Threat of touching a person without consent or threat of giving punishments . | Telling a patient, “I will give you injection even if you refuse” |
| Battery | Actual physical contact without consent. (touching or any other procedure ) | Giving injection without consent or prior alerting. |
| Defamation | *️⃣Injuring another’s reputation:- there are two types of defamation , as given below:- 1.Libel: Written or printed false statement harming someone’s reputation (e.g., writing false remarks about a nurse in a report). 2.Slander: Spoken false statement harming someone’s reputation (e.g., saying untrue things about a colleague or patient). | Spreading false rumors about a doctor or patient |
| False imprisonment | Restricting a patient’s movement without justification or without order OR admiting patient in a hospital without their consent | RESTRAINING a restless patient without doctor’s order. |
| Invasion of privacy | Disclosing patient’s personal information | Posting patient’s photo on social media OR discussing patients heath condition in lift , cafe or other then work place |
🔹 Legal Responsibilities of Nurses:
- Maintain valid registration and license under State Nursing Council.
- Provide safe and competent care within one’s scope of practice.
- Obtain informed consent before performing any procedure.
- Maintain accurate documentation of patient care.
- Respect patient rights and confidentiality.
- Report abuse or communicable diseases as required by law.
🔹 Legal Safeguards for Nurses:
🩺 Meaning:-
Legal safeguards are the protective measures and precautions that nurses take to prevent being held legally liable for mistakes, negligence, or malpractice while providing patient care.
They help nurses practice safely, ethically, and within the law.
🎯 Purpose / Importance of Legal Safeguards:-
- To protect nurses from legal action or punishment.
- To ensure safe and ethical patient care.
- To maintain professional accountability and trust.
- To reduce chances of negligence, malpractice, or abuse.
- To help nurses make legally sound decisions in complex clinical situations.
📜 Major Legal Safeguards in Nursing :-
1. Follow Standards of Care
- Standards are the minimum acceptable level of performance expected from a nurse. or nurse should know basic skills of nursing to achieve the degree.
- Defined by the Indian Nursing Council (INC), State Nursing Councils, and hospital policies.
Example:
Following the correct procedure while giving injections (e.g., checking site, dose, expiry) protects against negligence claims.
2. Proper Documentation and Record Keeping
- Accurate, complete, and timely documentation is a nurse’s best defense in court. it will help nurse from protection against legal issues ,even minor of minor incidence of patient should be documented.
- Legal saying: “If it is not written, it was not done.”
Example:
Recording vital signs, medication given, and nursing actions helps prove proper care was provided.
If doctor has given order verbally through mobile phone then also it should be recorded as “order given verbally by this/that dr via mobile phone” in nurses notes
3. Obtain Informed Consent
- Consent must be taken before performing any procedure.
- It should be voluntary, informed, and by a competent patient.
Example:
Before inserting a catheter or starting IV therapy, explain the procedure and get consent.
4. Maintain Patient Confidentiality
- Do not disclose patient’s personal, medical, or family information without consent.
- Required under Right to Privacy (Article 21) and HIV/AIDS (Prevention & Control) Act, 2017.
Example:
Never share an HIV-positive patient’s status or post patient data on social media.
5. Practice Within Legal Boundaries / Scope of Practice
- Perform only those duties for which you are qualified, trained, and authorized.
- Never act beyond your level of competence.
Example:
A GNM nurse should not perform anesthesia administration unless specially trained.
6. Maintain Valid Registration and License
- Every nurse must be registered with the State Nursing Council as per INC Act, 1947.
- Renewal must be done periodically to continue lawful practice.
Example:
If a nurse’s license has expired and she continues to work — it is illegal practice.
7. Provide Safe and Competent Care
- Use correct nursing procedures, infection control, and safety measures.
- Prevent medication errors, falls, or pressure ulcers.
Example:
Checking patient identity before drug administration prevents malpractice.
8. Use Effective Communication
- Communicate clearly with patients, relatives, and healthcare team members.
- Good communication reduces misunderstanding and lawsuits.
Example:
Informing the doctor immediately about abnormal vital signs shows responsibility.
9. Report Obligations (Mandatory Reporting)
- Nurses must report certain events as per law:
- Communicable diseases
- Child or elder abuse
- Accidental injuries, poisoning, or suicide cases
- Deaths in hospital
Example:
If a child shows signs of physical abuse, the nurse must inform the authorities.
10. Avoid Negligence and Malpractice
- Always stay alert, double-check orders, and ensure safety.
- Negligence = doing something a prudent nurse would not do.
Example:
Failing to elevate side rails of bed → patient falls → nurse held negligent.
11. Follow Institutional Policies and Protocols
- Every hospital has written policies for medication, waste disposal, emergency codes, etc.
- Following them provides legal protection.
Example:
Using proper color-coded bags for biomedical waste disposal.
12. Continuing Education and Skill Upgradation
- Regular training keeps nurses updated with new laws, drugs, and technologies.
- It helps avoid errors due to outdated knowledge.
Example:
Attending workshops on infection control or CPR updates.
13. Professional Indemnity Insurance
- It covers financial loss if a nurse is found legally liable for negligence.
- Protects nurse from heavy compensation payments.
Example:
A nurse insured under indemnity policy won’t pay from personal funds if sued.
14. Good Interpersonal Relationships
- Maintain respect and cooperation with doctors, co-workers, and patients.
- Prevents misunderstandings and complaints.
Example:
Handling a patient’s family with empathy and patience during emergencies.
15. Safeguarding Patient’s Rights
- Nurses must protect patient rights such as:
- Right to life and health care
- Right to privacy
- Right to refuse treatment
- Right to information
Example:
Respecting a patient’s decision to refuse surgery after counseling.
16. Proper Handling of Medications and Equipment
- Store, prepare, and administer medicines safely.
- Follow “10 Rights” of medication administration (right patient, drug, dose, route, etc.).
- ✅ 10 Rights of Drug Administration
Right Patient – Verify the correct patient using ID band or name before giving the drug.
Right Drug – Check the correct medication name and label before administration.
Right Dose – Give the exact prescribed amount of the drug.
Right Route – Administer the medicine by the correct route (oral, IV, IM, etc.).
Right Time – Give the drug at the correct time and frequency.
Right Documentation – Record immediately after giving the medication.
Right Reason – Know the correct purpose or indication for giving the drug.
Right Response – Observe and evaluate the patient’s reaction to the medication.
Right Education – Inform the patient about the name, purpose, and side effects of the drug.
Right to Refuse – Respect the patient’s right to refuse the medication after proper explanation.
Example:
Checking expiry date and label before injection protects from drug errors.
17. Legal Awareness and Record of Incidents
- Know local, national, and institutional laws related to nursing.
- Report and record any incidents like patient falls, needle-stick injuries, or medication errors.
Example:
Incident report serves as legal proof of immediate action taken
🌍 3. Other Issues in Nursing Practice
🔹 a) Cultural Issues
- Nurses care for patients from diverse backgrounds.
- Must respect cultural beliefs regarding food, birth, death, and gender.
- Example: A Hindu patient may refuse beef; a Muslim woman may prefer female nurse for examination.
🔹 b) Religious Issues
- Religion influences treatment decisions.
- Example: Jehovah’s Witness patient refusing blood transfusion.
🔹 c) Professional Boundary Issues
- Over-involvement or personal relationships with patients can cause harm.
- Example: Sharing personal contact or accepting expensive gifts from a patient is unethical.
🔹 d) Workplace Issues
- Violence and abuse from patients or attendants.
- Staff shortage leading to burnout and negligence.
- Workplace bullying or discrimination among nursing staff.
🔹 e) Technological and Informatics Issues
- Electronic Health Records (EHRs) raise confidentiality risks.
- Example: A nurse leaving a computer screen open showing patient data is a privacy violation.
- Use of social media — nurses must not post patient photos or information.
🔹 f) End-of-Life and Ethical-Legal Overlaps
- Issues like euthanasia, withdrawal of ventilator, or Do-Not-Resuscitate (DNR) orders.
- Example: Following a legal DNR order while ensuring comfort measures to the dying patient.
⚖️ 4. Legal Issues Overlapping with End-of-Life Decisions
🔹 a) Euthanasia
- Meaning: The act of intentionally ending a life to relieve suffering.
- Types:
- Active euthanasia – giving a lethal injection → illegal in India.
- Passive euthanasia – withdrawal or withholding of life support → legal under strict conditions.
Indian Law:
- Recognized by the Supreme Court of India in 2018 (Common Cause vs. Union of India).
- Passive euthanasia and living will are permitted under medical board supervision.
Nurse’s role:
Provide compassionate care, but must not participate in active euthanasia; can support passive euthanasia if ordered legally by physician and ethics board.
🔹 b) Living Will / Advance Directive
- A written legal document made by a competent person expressing their future treatment choices.
- It becomes active when the person becomes terminally ill or unconscious.
Example:
A patient writes: “If I go into irreversible coma, I do not wish to be kept alive on ventilator.”
Legal Status:
- Recognized by the Supreme Court of India (2018).
- Must be signed before witnesses and verified by magistrate.
Nurse’s duty:
Respect living will, inform physician, and ensure decisions align with law.
🔹 c) Brain Death and Organ Transplantation
- Defined under the Human Organ Transplantation Act (1994).
- Brain death must be certified by a medical board before organ removal.
Example:
A ventilated patient declared brain-dead donates organs with family consent.
Nurse ensures legal documentation, dignity, and family support.
🔹 d) Consent and Decision-Making Capacity
- For EOL care, valid informed consent is essential.
- If the patient is unconscious, consent must come from legal guardian or next of kin.
Example:
Stopping ventilator only after consent and medical board approval.
🔹 e) Right to Refuse Treatment
A competent patient may legally refuse life-sustaining therapy.
Supported by Article 21 – Right to Life and Personal Liberty, which also includes the right to a dignified death.
CONCEPT OF HEALTH AND ILLNESS:-

* Concept of Health:-
🌿 Concept of Health
Health is not merely the absence of disease or infirmity; it is a state of complete physical, mental, social, and spiritual well-being.
The World Health Organization (WHO) defines health as:
“A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Health is a dynamic and positive concept, changing with time, environment, and individual circumstances. It depends on multiple factors — biological, psychological, social, environmental, and spiritual.
1. Physical Health

It refers to the proper functioning of body organs and systems.It means well being of body less occurence of any disease condition or infections .
- Examples: A person who eats balanced meals, exercises regularly, maintains normal weight, and is free from illness is said to have good physical health.
- Indicators: Pulse rate, blood pressure, body weight, physical endurance, absence of fatigue,absensce of infections.
2. Mental Health

It means the ability to think clearly, handle emotions, manage stress, and maintain relationships and utilising of psycological strategies in a proper way to overcome stress and other mental situations.
- Example: A nurse who can manage stressful hospital situations calmly and make decisions logically shows mental health.
- In case of large number of OPD patient still a single nurse is able to work with complete conciusness
- Indicators: Positive attitude, emotional stability, and the ability to cope with life’s difficulties.
3. Social Health

It indicates the ability to form satisfying interpersonal relationships and perform social roles effectively and able to participate in society . able to live in society with its norms and conditions.
- Example: Participating in community activities, teamwork in hospitals, and maintaining family relations show good social health.
4. Spiritual Health
It reflects inner peace, moral values, and purpose in life.

- Example: A patient who accepts illness calmly and finds meaning through faith and meditation demonstrates spiritual well-being.
5. Emotional Health

It includes recognizing and expressing emotions properly.
- Example: Expressing sadness after a loss rather than suppressing feelings is emotionally healthy behavior
Illness is the subjective feeling of being unwell — a deviation from the normal state of health in which physical or mental processes are disturbed.
It is how a person perceives and responds to disease.
- Example: Two patients with the same diagnosis may experience illness differently — one may feel severely unwell while another may cope better.
🌡️ Types of Illness — Detailed Explanation
Illness can be understood as a disturbance in the normal functioning of body or mind that affects a person’s daily activities and sense of well-being. It is not only about physical suffering but also emotional, mental, and social imbalance.
Broadly, illnesses can be classified into acute, chronic, communicable, non-communicable, mental, and occupational types.
🕒 1. Acute Illness
Definition:
An acute illness is one that develops suddenly, has a short duration, and usually resolves either with treatment or by itself lasts upto 4 weeks .
Characteristics:
- Rapid onset of symptoms
- Short course (few days to few weeks)
- May require urgent medical attention
- Full recovery is possible
Examples:
- Fever due to infection
- Influenza (flu)
- Pneumonia
- Diarrhea
- Appendicitis
Explanation:
A patient suffering from influenza feels fever, body ache, and weakness for a few days. After rest and medication, the person recovers completely — this shows the temporary nature of acute illness.
🧬 2. Chronic Illness
Definition:
A chronic illness develops slowly, continues for a long period (months or years), and often cannot be completely cured but can be managed.
Characteristics:
- Slow, gradual onset
- Long-term or lifelong duration
- Periods of remission (no symptoms) and exacerbation (worsening)
- Requires lifestyle modification and continuous treatment
Examples:
- Diabetes mellitus
- Hypertension
- Asthma
- Arthritis
- Cancer
Explanation:
A diabetic patient may live for years with the disease, needing regular insulin, diet control, and medical follow-up. Though not curable, the illness can be controlled and the person can lead a productive life.
🦠 3. Communicable (Infectious) Illness
Definition:
Communicable illnesses are caused by microorganisms such as bacteria, viruses, fungi, or parasites and can spread from one person to another directly or indirectly or we can say spread through contact.
Characteristics:
- Caused by infectious agents
- Spread through air, water, food, contact, or vectors
- Preventable through hygiene, sanitation, and immunization
- also due to fomites , utensils etc
Examples:
- Tuberculosis (airborne spread)
- COVID-19 (droplet infection)
- Cholera (water-borne)
- Malaria (mosquito-borne)
- Hepatitis B (blood-borne)
Explanation:
A nurse caring for patients must follow infection control practices like wearing gloves, masks, and maintaining hand hygiene to prevent the spread of communicable diseases in hospitals.
❤️ 4. Non-Communicable Illness
Definition:
Non-communicable illnesses (NCDs) are not caused by infections and do not spread from person to person. They are often linked to genetic, lifestyle, or environmental factors.
Characteristics:
- Non-infectious, non-transferable
- Develop slowly and progress over time
- Related to poor lifestyle, unhealthy diet, lack of exercise, smoking, or heredity
Examples:
- Diabetes
- Hypertension
- Cancer
- Heart disease
- Stroke
Explanation:
A person with an unhealthy lifestyle — eating junk food, not exercising, and under stress — may develop hypertension or heart disease. These conditions are managed through medicines, regular check-ups, and lifestyle changes rather than infection control.
🧠 5. Mental Illness
Definition:
Mental illness refers to disorders that affect mood, thinking, and behavior, interfering with daily functioning and relationships.
Characteristics:
- May be acute or chronic
- Involves emotional and behavioral disturbances
- Often misunderstood or stigmatized
- Requires psychological counseling and medication
Examples:
- Depression
- Anxiety disorders
- Schizophrenia
- Bipolar disorder
Explanation:
A psychiatric nurse caring for a depressed patient helps them express emotions, build confidence, and adhere to therapy. Mental health promotion is as important as physical health.
🧑🏭 6. Occupational Illness
Definition:
An occupational illness is caused by exposure to risk factors in the workplace such as chemicals, dust, noise, or repetitive strain.
Characteristics:
- Develops due to unsafe work environment
- Preventable through protective measures
- Often chronic in nature
- working in industrial areas like coal mine , textile industries etc
Examples:
- Silicosis (disease occurs due to silicaOR dust particles particles invaded into lungs)in miners due to dust inhalation
- Hearing loss in factory workers due to loud noise
- Skin allergies in nurses using disinfectants without gloves
Explanation:
Healthcare workers are at risk of needle-stick injuries and infections; using gloves and safe disposal of sharps can prevent occupational illnesses.
⚖️ 7. Psychosomatic Illness
Definition:
Psychosomatic illness occurs when emotional stress or psychological factors lead to physical symptoms.
Examples:
- Stomach ulcers caused by stress
- Headache due to anxiety
- High blood pressure triggered by tension
Explanation:
In hospitals, nurses often see patients whose physical symptoms are aggravated by emotional distress; holistic care includes both physical and mental support.
🌍 8. Lifestyle-Related Illness
Definition:
These illnesses result from unhealthy habits and behaviors like poor diet, lack of exercise, smoking, and alcohol use.
Examples:
- Obesity
- Type-2 diabetes
- Hypertension
- Coronary artery disease
Explanation:
A nurse’s role includes educating patients about healthy habits — balanced diet, regular exercise, and avoiding tobacco — to prevent lifestyle diseases.
🌸 Factors Affecting Health and Illness (Detailed Explanation)
Health is a dynamic and multifactorial concept — it is influenced by various internal and external factors.
These factors determine whether a person remains healthy or develops illness.
No single factor works alone; instead, all interact continuously to shape physical, mental, and social well-being.
🧬 1. Biological Factors
These include the genetic makeup, age, sex, and physiological functioning of an individual.
- Genetic inheritance:
Some people inherit genes that make them more prone to diseases.- Example: Diabetes mellitus, hypertension, sickle cell anemia, hemophilia, and certain cancers run in families.
- Age:
Each age group or vulenerable groups like elderly, paediatrics and pregnent women has different health risks.- Example: Infants are prone to infections, adolescents face hormonal issues, adults suffer from stress-related disorders, and the elderly develop degenerative diseases like arthritis.
- Sex:
Some illnesses are gender-specific or more common in one sex.- Example: Women are more prone to anemia and osteoporosis; men are more prone to heart disease and lung cancer (due to higher tobacco use).
🧠 2. Psychological Factors
Mental state, emotions, and stress play a powerful role in maintaining or disturbing health.
- Positive attitude promotes recovery and immunity, while negative emotions weaken the body’s defense.
- Example: A nurse who remains calm and optimistic during duty hours maintains better mental and physical health compared to someone constantly anxious or irritable.
- Chronic stress can lead to psychosomatic illnesses such as ulcers, hypertension, or depression.
🌍 3. Environmental Factors
The surroundings where a person lives greatly affect health.
- Physical environment: Includes air, water, housing, sanitation, waste disposal, and climate.
- Example: Poor sanitation causes diarrhea; polluted air leads to respiratory diseases like asthma.
- Social environment: Includes family, neighborhood, workplace, and community support.
- Example: A person living in a supportive family environment enjoys better mental health compared to someone in isolation.
🏠 4. Socioeconomic Factors
Economic and social status influence access to food, shelter, and healthcare.
- Income: Low income limits the ability to buy nutritious food or seek medical help.
- Example: Malnutrition and anemia are common in low-income groups.
- Education: Educated people are more aware of health practices like immunization, hygiene, and diet.
- Occupation: People working in hazardous industries (mining, construction, hospitals) face occupational health risks.
- Housing: Overcrowded or damp houses lead to tuberculosis and infections.
🥗 5. Lifestyle and Behavior Factors
How a person lives each day — habits, routines, and choices — strongly determines health.
- Diet: Unbalanced or junk food leads to obesity, diabetes, and heart disease.
- Exercise: Physical inactivity causes poor circulation and weak muscles.
- Sleep: Irregular or insufficient sleep affects immunity and concentration.
- Substance abuse: Smoking, alcohol, and drugs damage multiple organs.
- Hygiene: Poor personal hygiene spreads infections like skin diseases or parasitic infestations.
Example: A nurse maintaining a balanced diet, daily exercise, and regular rest remains healthy, whereas irregular meals and late-night shifts without rest cause fatigue and illness.
🧑⚕️ 6. Cultural and Religious Factors
Culture shapes beliefs about health, illness, diet, and treatment.
- Dietary practices: Some communities avoid certain foods due to customs, which may cause nutritional deficiencies.
- Example: A vegetarian who doesn’t include milk or pulses may develop protein deficiency.
- Health beliefs: Some people believe illness is caused by fate or evil spirits and may delay seeking medical help.
- Religious restrictions: Fasting or rejecting blood transfusion due to belief can affect health outcomes.
🧩 7. Family and Social Support Factors
Family provides emotional stability, care, and early health education.
- Positive family support: Encourages healthy habits, regular check-ups, and stress relief.
- Broken or conflicted families: Increase risk of depression, substance abuse, and poor lifestyle.
- Example: Children raised in caring families are more emotionally stable and health-conscious.
💊 8. Health Services and Access to Care
Availability and quality of healthcare determine how quickly illness is detected and treated.
- Access to hospitals, clinics, and trained nurses improves early diagnosis and management.
- Lack of services in rural or remote areas leads to untreated diseases and complications.
- Example: Vaccination programs in villages reduce child mortality; poor access increases preventable deaths.
🔄 9. Political and Policy Factors
Government policies affect public health directly through laws and programs.
- Health legislation: Safe water supply, pollution control, and immunization laws improve national health.
- Healthcare funding: Determines number of hospitals, staff, and availability of medicines.
- Example: National Health Mission (NHM), ICDS, and Ayushman Bharat improve accessibility to health care for all citizens.
✝️ 10. Spiritual and Moral Factors
Spiritual well-being provides peace, hope, and a sense of purpose, especially during illness.
- People with faith and moral stability recover faster due to positive coping mechanisms.
- Example: A terminally ill patient who prays and accepts reality shows better emotional adjustment than one who loses hope.
⚖️ 11. Hereditary and Genetic Factors
Certain diseases are passed down through families due to defective genes.
- Example: Sickle cell anemia, thalassemia, color blindness, and diabetes often appear in families.
- Nurses should take a family history to identify hereditary risks and educate about prevention.
💬 12. Educational and Awareness Factors
- Health education empowers people to make informed decisions.
- Example: An individual aware of hygiene practices like handwashing, vaccination, and safe food handling can prevent many communicable diseases.
⁕STRESS AND ADAPTATION :-
🌪️ STRESS — DETAILED EXPLANATION
💡 Definition of Stress
Stress is the body’s physical, mental, and emotional reaction to any demand or change that requires adjustment or response.
It is a state of tension or strain that results when external or internal pressures exceed an individual’s ability to cope.
Hans Selye (Father of Stress Research) defined stress as:
“The nonspecific response of the body to any demand made upon it.”
In simple terms — when something disturbs our balance (homeostasis), the body and mind react; this reaction is called stress.
🧠 Concept of Stress
Stress is not always harmful — it can be positive (motivating) or negative (damaging) depending on intensity and duration.
- A moderate level of stress increases alertness and efficiency.
- Excessive or prolonged stress causes illness and emotional breakdown.
This is called the “stress continuum” — from mild stimulation → healthy tension → distress → burnout.
⚖️ Types of Stress
1. Eustress (Positive Stress)
- A healthy form of stress that motivates and energizes individuals to perform better.
- It enhances focus, creativity, and performance.
- Examples:
- Preparing for an exam or job interview.
- A nurse working efficiently during an emergency shift.
2. Distress (Negative Stress)
- When demands exceed the body’s coping capacity, causing anxiety, tension, and illness.
- It leads to fatigue, depression, and burnout.
- Examples:
- Overwork, family conflict, or prolonged illness.
3. Acute Stress
- Sudden, short-term reaction to an immediate threat or challenge.
- Usually passes once the situation ends.
- Examples:
- Sudden patient emergency, minor accident, or anger episode.
4. Chronic Stress
- Long-term continuous stress due to unresolved issues or constant pressure.
- Damages physical and mental health.
- Examples:
- Prolonged job dissatisfaction, family problems, or chronic illness.
5. Physical Stress
- Stress arising from physical illness, pain, injury, or fatigue.
- Example:
- A nurse working long hours without rest develops back pain and tiredness.
6. Psychological Stress
- Related to emotional and mental conflict, fear, guilt, or frustration.
- Example:
- A nursing student worrying about exam results or future career.
7. Social Stress
- Results from poor relationships, isolation, discrimination, or societal pressure.
- Example:
- A person feeling lonely or unsupported at the workplace.
🔍 Causes (Sources) of Stress
Stressors are the factors or events that cause stress.
They may be internal (within the person) or external (environmental).
1. Physical Stressors
- Illness, pain, fatigue, noise, overcrowding, poor diet, pollution.
2. Psychological Stressors
- Fear, anger, frustration, failure, competition, guilt, anxiety.
3. Social Stressors
- Family problems, financial crisis, unemployment, death of loved ones.
4. Occupational Stressors
- Heavy workload, night shifts, lack of support, conflict with colleagues.
- Example: Nurses working long hours in ICUs experience occupational stress frequently.
5. Environmental Stressors
- Natural disasters, pandemic, extreme weather, unsafe housing.
6. Lifestyle-Related Stressors
- Lack of sleep, unhealthy eating, excessive caffeine, or addiction.
⚙️ Physiological Response to Stress (Body’s Reaction)
When stress occurs, the brain signals the hypothalamus → which activates the autonomic nervous system → releasing adrenaline and cortisol (stress hormones).
These cause the “fight-or-flight response”:
- Increased heart rate and blood pressure
- Rapid breathing
- Dilated pupils
- Sweating
- Tensed muscles
- Decreased digestion
This response helps the body prepare for action but becomes harmful if prolonged.
📉 Effects of Stress
Stress affects the body, mind, and behavior.
1. Physical Effects
- Headache, fatigue, back pain, high BP, insomnia, ulcers, decreased immunity.
2. Psychological Effects
- Anxiety, depression, irritability, loss of concentration, confusion.
3. Behavioral Effects
- Overeating or loss of appetite, smoking, alcohol use, absenteeism, withdrawal.
4. Social Effects
- Poor communication, relationship problems, isolation.
Example:
A nurse under stress due to workload may become impatient with patients or commit medication errors — showing both behavioral and performance impacts.
⏳ Stages of Stress (Hans Selye’s General Adaptation Syndrome – GAS)
Stress occurs in three main physiological stages:
Stage 1 – Alarm Reaction Stage
- The body recognizes the stressor and prepares for “fight or flight.”
- Adrenaline and cortisol are released.
- Symptoms: tacycardia, diaphoresis, xerostomia, alertness.
Stage 2 – Resistance Stage
- The body tries to adapt and resist the stressor.
- Energy is used to cope and maintain normal function.
- If the stress continues, energy reserves start depleting.
Stage 3 – Exhaustion Stage
- The body’s resources are exhausted; it can no longer fight.
- Physical and mental breakdown occurs.
- Symptoms: fatigue, illness, depression, burnout.
Example:
A nurse under continuous duty stress without rest first becomes alert (alarm), then manages somehow (resistance), but later experiences exhaustion leading to illness or absenteeism.
🌈 Coping and Stress Management
Managing stress means reducing its negative effects and maintaining balance.
1. Physical Methods
- Regular exercise (yoga, walking)
- Adequate sleep and rest
- Balanced diet
- Relaxation techniques (deep breathing, meditation)
2. Psychological Methods
- Positive thinking and self-affirmation
- Setting realistic goals
- Time management and prioritizing tasks
- Talking to trusted people or counselors
3. Social Methods
- Building supportive relationships
- Sharing feelings with family and friends
- Participating in community or spiritual activities
4. Nursing Stress Management
- Taking short breaks during shifts
- Using teamwork and delegation
- Seeking peer or supervisor support
- Practicing mindfulness in care situations
💬 Example in Nursing Context
A nurse in the ICU faces constant emergencies and long shifts.
At first, adrenaline helps her act quickly (alarm stage).
After weeks, she manages to adapt (resistance stage).
But with no rest or emotional support, she becomes fatigued, irritable, and falls sick (exhaustion stage).
→ This illustrates how continuous stress without coping leads to illness.
🌈🌸ADAPTATION:-
Definition of Adaptation
Adaptation means the process by which an individual adjusts to internal and external changes to maintain balance (homeostasis) and survival.
It is the way the body and mind respond to stressors in order to restore normal function.
🩺 In simple words: Adaptation is how we “adjust” physically, mentally, and socially to meet life’s demands and cope with stress.
🧬 Concept of Adaptation
Every person continuously interacts with their environment.
Whenever a change or challenge occurs — like illness, emotional stress, or environmental shift — the body and mind try to restore stability.
This process of adjustment is adaptation.
Adaptation is not a one-time act — it is a continuous, dynamic, and individualized process.
A person’s ability to adapt depends on:
- Their age and health,
- Personality and coping skills,
- Family and social support,
- Type and duration of stressor.
⚖️ Purpose (Need) of Adaptation
- To maintain homeostasis: Keeps the body and mind in equilibrium.
- To promote survival: Helps face threats or stress without breakdown.
- To maintain physical and mental efficiency: Allows daily functioning despite pressure.
- To support recovery from illness: Aids in healing and rehabilitation.
- To maintain social harmony: Enables individuals to fit into society and relationships.
🌍 Types of Adaptation
1. Physiological Adaptation
The body automatically adjusts to maintain internal stability when external conditions change.
- Examples:
- Sweating when it’s hot to cool the body.
- Shivering in cold weather to produce heat.
- Increase in heart rate during exercise.
- Increased red blood cells at high altitude for better oxygen transport.
These responses are involuntary and regulated by the nervous and endocrine systems.
2. Psychological (Emotional or Behavioral) Adaptation
The mind uses coping strategies to manage emotional stress and maintain mental balance.
- Examples:
- Accepting life changes such as illness or loss.
- Developing patience and self-control in difficult situations.
- Using problem-solving or relaxation techniques.
- A nurse handling an emergency calmly shows psychological adaptation.
These responses are learned and voluntary — they depend on personality, past experience, and support.
3. Social Adaptation
It involves adjusting to social norms, relationships, and community expectations.
- Examples:
- Learning new languages or customs when moving to another state.
- Cooperating with team members at work.
- A new nurse adapting to hospital culture and teamwork.
Social adaptation ensures smooth interpersonal relations and social functioning.
4. Cultural Adaptation
It is adjustment to a new cultural environment or lifestyle.
- Example: Migrant nurses adapting to hospital practices and patient behavior in a different region.
🔄 Mechanisms of Adaptation
Adaptation occurs through both biological and psychological mechanisms.
In nursing psychology, these mechanisms are often called coping or defense mechanisms.
A. Biological Mechanisms
- Hormonal regulation (adrenaline, cortisol during stress)
- Autonomic nervous system responses (heart rate, respiration)
- Immune response to infection
- Repair and healing processes after injury
These maintain physiological homeostasis.
B. Psychological Mechanisms
These include both conscious coping and unconscious defense mechanisms.
- Conscious coping:
Positive methods like planning, seeking help, meditation, or problem-solving.- Example: A student creating a study schedule before exams.
- Unconscious defense mechanisms (as per Freud):
Automatic mental processes used to reduce anxiety.- Examples:
- Denial (refusing to accept reality)
- Rationalization (giving false reasons for mistakes)
- Projection (blaming others)
- Regression (behaving childishly)
- Sublimation (converting anger into constructive work)
- Examples:
⚙️ Stages of Adaptation (According to Selye’s General Adaptation Syndrome)
Hans Selye described adaptation as a three-stage process that occurs when the body faces stress:
- Alarm Reaction Stage:
The body detects the stressor and activates “fight or flight” response — heart rate, BP, and respiration increase.
Example: A nurse becomes alert during an emergency code situation. - Resistance Stage:
The body tries to resist and cope with the stressor by adapting physiologically and psychologically.
Example: The nurse learns to manage emergencies calmly through experience.* - Exhaustion Stage:
If stress continues without rest, adaptive energy is depleted — leading to fatigue, illness, or depression.
Example: Continuous overwork without rest leads to burnout.*
Thus, adaptation is successful when the person manages stress before reaching exhaustion.
🩺 Examples of Adaptation in Nursing Context
- A patient recovering from amputation learns to use a prosthetic limb → physical adaptation.
- A nurse adjusts to night duty schedule and irregular meals → physiological and social adaptation.
- A widow coping with loss by joining a social support group → psychological adaptation.
- A diabetic patient modifying diet and lifestyle to control sugar levels → behavioral adaptation.
🌿 Factors Affecting Adaptation
- Nature and intensity of stressor – mild stress promotes adaptation; severe stress hinders it.
- Duration of stressor – short-term is manageable; long-term causes exhaustion.
- Individual’s health and personality – strong, optimistic people adapt faster.
- Previous experience – past coping skills help current adaptation.
- Social support – family, friends, and coworkers strengthen adaptive capacity.
- Cultural and spiritual beliefs – faith and meaning provide resilience.
❤️ Importance of Adaptation in Nursing
- Promotes patient recovery – Nurses assist patients to adapt to illness, disability, and hospitalization.
- Prevents stress complications – Through counseling, relaxation, and education.
- Maintains nurse’s well-being – Nurses themselves must adapt to heavy workload, emotional strain, and shift duties.
- Enhances holistic care – Adaptation includes physical, mental, and social aspects, not just disease treatment.
🩺HEALTH CARE CONCEPT AND NURSING CARE CONCEPT:-
🌿 HEALTH CARE CONCEPT
💡 Meaning
Health care is the comprehensive and organized effort made by individuals, communities, and governments to promote, maintain, and restore health.
It includes every service that helps people live a physically, mentally, and socially healthy life — from disease prevention to rehabilitation.
Health care is not only about hospitals or doctors; it begins in the family and community and extends to specialized hospitals and national health programmes.
🩹 Main Aims of Health Care
- To maintain and promote health before disease occurs.
- To prevent and control diseases through timely action.
- To cure illness and relieve suffering through effective treatment.
- To rehabilitate individuals so they can live normal, productive lives.
- To achieve the ultimate goal of “Health for All.” 🌏
🧭 Components of Health Care
- Promotive Health Care 🥦
Focuses on improving general health and well-being.
Example: health education, nutrition guidance, environmental sanitation, exercise promotion. - Preventive Health Care 💉
Aims to stop diseases before they start.
Example: immunization, periodic screening, antenatal check-ups, safe-water campaigns. - Curative Health Care 🏥
Deals with diagnosis and treatment once disease has appeared.
Example: giving medicines, surgery, hospitalization. - Rehabilitative Health Care 🤝
Helps people recover after illness and regain independence.
Example: physiotherapy, occupational therapy, counselling, social reintegration.
🏗️ Levels of Health Care
- Primary Level 🏡 – The first contact of the individual with the health system; includes sub-centres, PHCs, and health workers providing basic services.
- Secondary Level 🏥 – District hospitals or CHCs providing specialist care and laboratory support.
- Tertiary Level 🏛️ – Advanced, super-specialty hospitals such as medical colleges or AIIMS, offering complex treatment and research facilities.
🎯 Goals and Principles
- Equitable Distribution: Health services must reach every person, especially the poor and rural population.
- Community Participation: People should take part in planning and maintaining their own health.
- Inter-sectoral Coordination: Health improvement requires cooperation between health, education, agriculture, and social sectors.
- Appropriate Technology: Use methods that are simple, scientifically sound, and affordable for the community.
- Accessibility and Quality: Health care must be available, acceptable, and of good quality for all.
- Promotive Health Care 🥦
Focuses on improving general health and well-being.
Example: health education, nutrition guidance, environmental sanitation, exercise promotion. - Preventive Health Care 💉
Aims to stop diseases before they start.
Example: immunization, periodic screening, antenatal check-ups, safe-water campaigns. - Curative Health Care 🏥
Deals with diagnosis and treatment once disease has appeared.
Example: giving medicines, surgery, hospitalization. - Rehabilitative Health Care 🤝
Helps people recover after illness and regain independence.
Example: physiotherapy, occupational therapy, counselling, social reintegration.
🏗️ Levels of Health Care
- Primary Level 🏡 – The first contact of the individual with the health system; includes sub-centres, PHCs, and health workers providing basic services.
- Secondary Level 🏥 – District hospitals or CHCs providing specialist care and laboratory support.
- Tertiary Level 🏛️ – Advanced, super-specialty hospitals such as medical colleges or AIIMS, offering complex treatment and research facilities.
🩺 NURSING CARE CONCEPT
💡 Meaning
Nursing care is the art and science of caring for individuals, families, or communities to help them attain, maintain, or recover optimal health and quality of life.
It is based on compassion, knowledge, skill, and critical thinking, and focuses on the whole person — body, mind, and spirit.
🌸 Nature of Nursing Care
- It is holistic, addressing physical, emotional, social, and spiritual needs.
- It is individualized, respecting every person’s culture, beliefs, and values.
- It is scientific, based on evidence and professional knowledge.
- It is continuous, from admission to discharge and follow-up.
- It is humanistic, rooted in empathy, understanding, and moral responsibility.
🔶 Aims of Nursing Care
- To promote health and prevent illness.
- To restore health through care, comfort, and education.
- To support rehabilitation and adaptation after disease or disability.
- To provide emotional support to the patient and family.
- To assist in a dignified death when recovery is not possible.
🔄 Nursing Process (Core of Nursing Care)
- Assessment 🔍 – Collecting detailed information about the patient’s physical, psychological, social, and spiritual status.
- Nursing Diagnosis 🧠 – Identifying the actual or potential health problems based on assessment data.
- Planning 🎯 – Setting goals and determining nursing interventions to achieve desired outcomes.
- Implementation 👐 – Carrying out nursing actions such as medication administration, hygiene, teaching, and counselling.
- Evaluation ✅ – Checking whether the goals were met and modifying the plan if needed.
This process ensures systematic, safe, and effective patient care.
💕 Principles of Nursing Care
- Respect for life and dignity of each person.
- Effective communication with patients and families.
- Evidence-based practice for best outcomes.
- Safety first — preventing errors and infections.
- Teamwork — collaborating with doctors, paramedics, and the community.
🌼 Essence of Nursing
Nursing care is not only giving medicine or injections; it is caring from the heart 💖, understanding human suffering, and using professional skill to heal, comfort, and guide patients toward wellness.
A nurse’s touch, words, and presence can bring hope, courage, and healing — making nursing one of the noblest professions in the world. 🌷
⁕ DEVELOPMENT OF CONCEPTS , NEEDS , ROLES AND PROBLEMS OF DEVELOPMENT STAGES OF HUMAN AT DIFFERENT AGE GROUP :-
⁕DEVELOPMENTAL STAGES OF NEWBORN :-
👶 Concept: “Newborn” & Early Development
Newborn:- a born baby is define as newborn till 24 hours
Neonate = a baby from birth to 28 days. This short period is packed with physiological adaptation from intra-uterine to extra-uterine life.
🧠 Core idea
- The newborn undergoes rapid systemic transitions—breathing air, thermoregulating, feeding by mouth, independent glucose control, bilirubin handling, and immune protection.
- Development in this stage is mostly neuro-behavioral organization and reflex-driven actions (not learned skills).
- We often view the neonatal period in three windows:
- Immediate (birth–24 h),
- Early (0–7 d),
- Late (8–28 d).
📏 Normal characteristics (orientation for assessment)
- Weight: ~2.5–3.5 kg (↓ up to 10% in first 5–7 days; regained by day 10–14).
- Length: 👉 48–52 cm (mean ≈ 50 cm ≈ 19.7 in)
- Head circumference: ~35 cm (≈2 cm > chest).
- Vital signs: RR 30–60/min, HR 100–160/min, temp 36.5–37.5 °C (axillary).
🍼 Neuro-behavioral features
- Primitive reflexes: rooting, sucking, Moro, grasp, stepping, tonic-neck, Babinski.
- Vision: best focus 20–30 cm, prefers faces/high contrast. 👀
- Hearing: functional at birth; startles to loud sounds. 👂
- Smell/taste: recognizes mother’s scent; prefers sweet. 👃😋
- Sleep: ~16–18 h/day in short cycles (active/REM and quiet sleep). 😴
🌱 Developmental Needs of the Newborn (Birth–28 Days)
Think “B.R.E.A.T.H.E. & B.O.N.D.” to remember core needs:
🫁 B – Breathe & Basic life support
- Immediate airway: clear secretions if obstructed; ensure effective breathing within the first minute.
- Apgar at 1 & 5 min guides urgency of support.A-P-G-A-R (each 0–2 pts): short revision of apgar score below
- (A – Appearance (color): blue/pale 0 • pink body/blue limbs 1 • all pink 2 🎨
- P – Pulse (HR): absent 0 • <100/min 1 • ≥100/min 2 ❤️
- G – Grimace (reflex irritability): no response 0 • grimace 1 • cough/sneeze/cry 2 😮💨
- A – Activity (muscle tone): limp 0 • some flexion 1 • active movement 2 💪)
- R – Respiration: absent 0 • slow/irregular 1 • good cry 2 📣
- How to read it:
- 7–10 👉 baby generally doing well
- 4–6 👉 needs some support/stimulation/oxygenation
- 0–3 👉 urgent resuscitation required
- Notes 📝: Start resuscitation without waiting for the score. Preterm babies may score lower due to immaturity. APGAR reflects immediate adaptation, not long-term outcomes.
- Resuscitation (only if needed): warm, position, clear airway, stimulate, PPV as per protocol.
🌡️ R – Regulation of temperature
- Prevent hypothermia from minute 1: dry → skin-to-skin (KMC), cap, warm room (≈25–28 °C), delay first bath 24 h+.
- Target temp 36.5–37.5 °C. Cold stress quickly leads to hypoglycaemia, acidosis, respiratory distress.
🍯 E – Energy (glucose) and early feeding
- Initiate breastfeeding within 30 minutes if stable; colostrum = immunity & laxative for meconium.
- On-demand 8–12 feeds/24 h; ensure deep latch & effective suck-swallow-breathe.(in short ; feed baby every 2 hourly in alternate breast)
- Watch for hypoglycaemia (jitteriness, lethargy, poor feeding).
🛡️ A – Anti-infective protection
- Clean cord care (keep dry; no harmful substances).
- Hand hygiene for all handlers; minimize visitors/crowding.
- Immunization at birth per national schedule (e.g., BCG, OPV-0, Hep B-1). 💉
- Vitamin K at birth prevents hemorrhagic disease (per local protocol).
🚽 T – Toileting & transition (elimination)
- Urine usually within 24 h; meconium within 24–48 h then transitional stools.
- Monitor for failure to pass urine/meconium, abdominal distension, bilious vomiting.
🧴 H – Hygiene & skin care
- Delay bathing, gentle sponge if needed; protect vernix (natural barrier).
- Diaper care to prevent dermatitis; air time; barrier creams if needed.
🧠 E – Emotional security & sensory regulation
- Skin-to-skin, rooming-in, responsive caregiving build attachment. 🤱
- Calm environment: soft light/sound, swaddling/containment, paced handling.
🤝 B.O.N.D. – Bonding, Orientation, Nurture, Developmental care
- Bonding: encourage eye contact, voice, scent familiarity.
- Orientation: teach parents newborn cues (hunger, overstimulation, pain).
- Nurture: exclusive breastfeeding, warmth, gentle touch.
- Developmental care: cluster procedures, support flexed midline posture, non-nutritive sucking for comfort.
🧑⚕️ Roles in Newborn Care (Who does what?)
👩🍼 Parents/Caregivers
- Provide skin-to-skin, frequent exclusive breastfeeding, burping after feeds.
- Recognize danger signs (listed below) and seek care early.
- Keep cord clean & dry, maintain warmth, safe sleep (supine, firm surface, no loose bedding).
- Attend birth immunizations, register baby, follow-up visits.
🧑⚕️ Nurses/ANMs (facility & community)
- Immediate care: warm-dry-stimulate; support early latch; Vit K & immunizations per policy.
- Assessment: full head-to-toe (fontanelles, hips, palate, reflexes, heart/lungs, umbilicus, genitalia).
- Screening: jaundice check, feeding adequacy, weight trend; hearing/CHD/metabolic screening as available.
- Parent education: feeding cues, satiety signs, hand hygiene, cord care, danger signs, safe sleep.
- Home-based newborn care (HBNC/IMNCI): scheduled home visits, growth monitoring, early referral.
- Documentation & referral: prompt stabilization and transport if red flags.
🧑⚕️ Doctors/Pediatric team
- Manage resuscitation, respiratory distress, sepsis, jaundice requiring phototherapy, hypoglycaemia, congenital anomalies, preterm/LBW protocols.
- Ensure screening tests, counsel families, arrange follow-up.
🏘️ Community health workers (e.g., ASHA)
- Early postnatal visits, reinforce breastfeeding, warmth, hygiene; track immunizations; identify danger signs and facilitate referral.
🚩 Common Problems by Stages:-
1) ⏱️ Immediate (Birth–24 h)
Key risks: asphyxia, respiratory distress, hypothermia, hypoglycaemia, birth injury.
- Birth asphyxia: poor cry/respiration, cyanosis; needs resuscitation per steps (warm, position, clear airway, ventilate).
- Respiratory distress: RR > 60, grunting, chest indrawing, nasal flaring. Consider TTN, RDS, MAS; oxygen/CPAP, referral.
- Hypothermia: cool skin, lethargy; re-warm (skin-to-skin, warm room), check glucose.
- Hypoglycaemia: jittery, poor feeding; early feeds/buccal glucose as protocol; investigate if persistent.
- Birth injuries: cephalohematoma, clavicle fracture, brachial plexus injury—gentle handling, pain management, pediatric review.
2) 🌄 Early Neonatal (0–7 days)
Key risks: sepsis, jaundice, feeding issues, excessive weight loss, dehydration fever.
- Neonatal sepsis: poor feeding, fever/low temp, lethargy, fast breathing, abdominal distension, umbilical redness with pus—urgent evaluation, antibiotics per protocol.
- Jaundice (often day 2–3): assess onset, progression to palms/soles, risk factors (prematurity, ABO/Rh incompatibility, G6PD deficiency). May need bilirubin levels, phototherapy, rarely exchange transfusion.
- Feeding problems: shallow latch, sore nipples, sleepy baby—lactation support, wake-and-feed, compressions, assess tongue-tie if suspected.
- Dehydration: ↓wet diapers, weight loss > 10%, sunken fontanelle—urgent feeding plan, possible IV fluids if severe.
3) 🌙 Late Neonatal (8–28 days)
Key risks: late-onset sepsis, persistent jaundice, GI problems, skin/oral infections, colic.
- Late-onset sepsis: fever, irritability, poor feeding—prompt referral.
- Prolonged jaundice (>14 days term): evaluate for breast-milk jaundice, hypothyroidism, biliary atresia, UTI.
- GI issues: reflux/regurgitation (usually benign), projectile vomiting → rule out pyloric stenosis; constipation uncommon in breastfed infants—check hydration.
- Oral thrush: white plaques; treat baby and consider maternal nipple care.
- Diaper dermatitis: frequent changes, air-drying, barrier ointments.
- Infantile colic: inconsolable crying, typically evening—reassure, soothing measures (swaddle, rocking, white noise), check red flags.
🆘 Universal Neonatal Danger Signs (IMNCI-style) to Teach Parents
- Dyspnea/tacypnea (≥60/min), severe chest indrawing.
- Fever (≥37.5 °C) or hypothermia (≤35.5 °C).
- Convulsions, abnormal movements, or very sleepy/unconscious.
- Poor feeding/not able to breastfeed, or vomits everything.
- Yellow palms/soles or jaundice on day 1.
- Umbilical redness with pus, or ≥10 skin pustules.
- Reduced/absent movement, persistent high-pitched cry.
➡️ Immediate facility care—don’t wait. 🚑
🧭Daily Care(Birth → 28 Days)
Day 0–1 🌤️
- Skin-to-skin, delayed cord clamping as per policy, initiate breastfeeding within 1 h.
- Vitamin K, birth immunizations, complete newborn exam.
- Teach: latch, hunger cues, hand hygiene, cord care, safe sleep.
- No early bath; keep warm.
Days 2–7 📈
- Frequent feeds, track wet diapers (≥6–8/day by day 5), stool transition.
- Weight check (acceptable loss ≤10%), jaundice surveillance.
- Home visit (HBNC/IMNCI): reinforce warmth, feeding, hygiene; screen for danger signs.
Days 8–28 🌟
- Continue exclusive breastfeeding, KMC especially for LBW/preterm.
- Monitor growth, skin/oral health, crying patterns; ensure follow-up.
- Start vitamin D supplementation if advised by local pediatric guidance. ☀️
👶 INFANT DEVELOPMENT: CONCEPT:-
🧠 What “development” means in infancy
- Development = qualitative changes in function and capability (sensing, moving, thinking, relating).
- Growth = quantitative changes in size (weight, length/height, head circumference).
- Both run together but are not the same.
📏 Core principles (remember these!)
- Cephalocaudal 👉 control develops head → toe.
- Proximodistal 👉 control develops center → periphery (shoulder → hand → fingers).
- General → specific 👉 big, global movements → precise, refined skills.
- Sequential & orderly 👉 milestones follow a predictable path (but timing varies).
- Critical periods 👉 early months are highly plastic for vision, hearing, attachment, and language.
- Individual variation 👉 normal range is broad; rate ≠ sequence.
🧩 Theoretical anchors (helpful for care planning)
- Erikson: Trust vs. Mistrust—consistent, warm care builds basic trust. 🤝
- Piaget: Sensorimotor stage—learning through senses & action (object permanence begins ~8–9 mo). 🧸
- Bowlby: Attachment forms with responsive caregiving; stranger/separation anxiety are normal signs of bonding (peak ~8–10 mo). 💞
- Temperament: inborn style (easy, difficult, slow-to-warm); guides individualized care. 🌈
🗓️ DEVELOPMENTAL STAGES & KEY MILESTONES
Milestones are guides (not exams). Look for progress over time.
🌤️ Neonate (birth–28 days)
- Adaptation: breathing starts, circulation transitions, thermal regulation immature.
- Motor: flexed posture; primitive reflexes (Moro, rooting, suck, grasp, stepping).
- Sensory: prefers faces/voice, sees best at 20–25 cm; tracks briefly.
- Social: quiet alert periods; calms to touch/voice.
- Growth norms: ~birth wt 2.5–3.5 kg (varies), HC ~35 cm. ⚖️
🌱 Early infancy (1–3 months)
- Gross motor: better head control (especially by 3 mo), tummy time lifts head/chest.
- Fine motor: hands open more; follows objects across midline.
- Language: cooing, different cries.
- Social: social smile (~6–8 weeks), watches caregiver intently.
🌿 Middle infancy (4–6 months)
- Gross motor: rolls front↔back, sits with support by ~6 mo.
- Fine motor: palmar grasp, brings objects to mouth, hand-to-hand transfer (near 6 mo).
- Language: laughs, squeals, explores sounds.
- Cognitive: reaches intentionally, explores cause–effect.
- Growth: weight roughly doubles by ~5–6 mo. 🍼
✨ Late infancy (7–9 months)
- Gross motor: sits without support; starts crawling/creeping; pulls to stand (end of this period for some).
- Fine motor: raking grasp → evolving inferior pincer near 9 mo.
- Language: babbles (ba-ba/da-da, nonspecific); responds to name.
- Social: stranger anxiety & separation anxiety appear (healthy attachment signs).
- Cognitive: object permanence emerging; loves peek-a-boo.
🌟 Late-late infancy (10–12 months)
- Gross motor: cruises holding furniture; may stand alone; some first steps.
- Fine motor: pincer grasp refined; bangs two blocks; points.
- Language: understands simple commands, first words near 12 mo (varies).
- Social/Play: waves bye-bye, claps, imitates; goal-directed problem solving.
- Growth: weight roughly triples by ~12 mo; length ↑ ~25 cm in year; HC ~46 cm (avg). 🎈
- Teeth: ~6–8 teeth by 12 mo (individual variability).
🧰 NEEDS OF THE INFANT (0–12 months):-
🍼 Nutrition:-
- Exclusive breastfeeding for first 6 months (on demand, day & night).
- Vitamin D supplementation is commonly recommended in infancy; follow local guidance. 🌞
- At 6 months: start complementary feeding while continuing breastfeeding to 12–24 mo+.
- Start soft & thick (not watery), 2–3×/day then increase to 3–4×/day + 1–2 nutritious snacks by 9–12 mo.
- Include iron-rich foods (mashed pulses/legumes, egg where culturally acceptable, fortified cereals).
- Introduce one new food at a time; watch for allergy signs.
- Iron needs rise after 6 mo; prioritize heme/non-heme sources + vitamin-C foods for absorption. 🍊
😴 Sleep & routines:-
- Total 14–17 h/day (newborns often 16–18 h, consolidates by 3–4 mo).
- Establish day–night rhythm gradually; calm bedtime routine.
- Safe sleep: supine position, firm flat surface, no pillows/loose bedding, no overheating, no smoking. 🌙
🌡️ Warmth, hygiene, & skin:-
- Thermal protection (layers, skin-to-skin esp. early).
- Cord care: keep clean & dry; no powders/pastes unless advised.
- Gentle bathing, fragrance-free emollients for dry skin.
- Oral care: wipe gums; soft brush when teeth erupt; avoid bottle in bed. 🪥
💉 Immunization & prophylaxis:-
- Follow your national immunization schedule (birth, 6/10/14 wk, 9–12 mo, etc.).
- Counsel on adverse event recognition (fever, local swelling) and comfort care.
- Micronutrients (e.g., vitamin A) per local program once eligible.
🧠 Stimulation & bonding:-
- Responsive caregiving: talk, sing, cuddle, eye contact; comfort promptly.
- Tummy time daily (supervised) for motor development and head shape.
- Age-appropriate play: rattles, soft books (0–6 mo); peek-a-boo, blocks, cause-effect toys (6–12 mo).
- Read aloud and narrate routines; name objects & feelings. 📚
🛡️ Safety :-
- Never shake an infant; protect the head/neck.
- Choking prevention: no nuts, hard pieces, coins, small batteries; always supervise feeding.
- Falls/burns prevention: never leave on high surfaces; check water temp; keep hot liquids & cords away.
- Car safety: age-appropriate rear-facing seat.
- Poisoning: lock meds/chemicals; store safely.
🔎 Screening & follow-up :-
- Growth monitoring: plot weight/length/HC at each visit; look at the trend.
- Developmental surveillance at every contact; formal screening as per clinic schedule.
- Vision/hearing risk assessment (family history, infections, NICU stay).
- Maternal mental health check—caregivers need care too. 💗
👩⚕️ ROLES (Who does what?)
👨👩👧 Parents/Caregivers
- Provide consistent, loving, responsive care (foundation of trust).
- Practice on-demand feeding (0–6 mo), introduce safe complementary foods (6–12 mo).
- Maintain immunization appointments; growth & development check-ins.
- Play & talk daily; follow safe-sleep and home-safety measures.
- Seek help early for feeding, illness, or developmental concerns.
🧑⚕️ Nurse/Health Worker (PHC/CHC/Clinic/Hospital)
- Assess growth, development, feeding, attachment, and caregiver well-being.
- Educate & coach: breastfeeding technique (position, latch, burping), complementary feeding textures and frequency, safe sleep, stimulation, and injury prevention.
- Plot charts, monitor trends, identify red flags, and refer when indicated.
- Atraumatic care: minimize procedures/pain; support kangaroo care.
- Document & follow up: immunizations, supplementation, screening results.
- Community role: organize well-baby clinics, Mother–Infant counselling, and home visits when available.
🧑⚕️ Pediatric Team
- Diagnose/manage medical issues, guide nutrition for LBW/ill infants, assess developmental delays, order tests/referrals (audiology, ophthalmology, therapy).
🚩 COMMON PROBLEMS & WHAT TO WATCH FOR ?
🌡️ Early neonatal risks
- Hypothermia (cool extremities, lethargy)—skin-to-skin, warm room, check infection.
- Breastfeeding difficulties (poor latch, sore nipples, inadequate transfer)—urgent lactation support.
- Jaundice beyond physiologic range (very yellow palms/soles, poor feeding)—needs assessment.
- Sepsis signs: poor feeding, fever/hypothermia, fast breathing, lethargy, grunting—emergency.
- Hypoglycemia risk (SGA/LGA, maternal diabetes)—prompt feeding and monitoring.
🍼 Feeding & growth issues (0–12 mo)
- Regurgitation/GER (usually benign): upright after feeds, avoid overfeeding; alarm if projectile, bilious, poor weight gain.
- Colic (crying ≥3 h/day, ≥3 days/week): soothing routines, caregiver breaks; exclude illness.
- Undernutrition/faltering growth: assess feeding technique, frequency, illness, micronutrient intake; consider medical causes.
- Anemia risk after 6 mo—ensure iron-rich complementary foods/supplements per guidance.
- Rickets risk—adequate vitamin D, sunlight exposure per advice.
🤧 Infections
- ARI: fast breathing, chest indrawing, poor feeding, cyanosis—urgent care.
- Diarrhea: danger signs = blood in stool, sunken eyes, very thirsty/lethargic; give ORS, continue feeds, seek care early.
- Skin/oral issues: thrush, diaper rash—gentle care, treat as indicated.
🧠 Developmental & neurological concerns
- Tone abnormalities (very stiff/floppy), persistent fisting after 4–5 mo, asymmetry in movements.
- Not smiling by 3 mo, no babble by 8–9 mo, no sitting by 9 mo, no pincer by 12 mo.
- Regression (loss of acquired skills) = red flag.
- Hearing/vision: not startling to loud sound (newborn), not turning to sound by ~6 mo, poor eye contact or tracking—screen & refer.
- Early social communication concerns by 9–12 mo (limited joint attention, little response to name) → early evaluation.
😴 Behavior & sleep
- Sleep fragmentation is common; watch for apnea, snoring with poor growth, or excessive daytime sleepiness.
- Stranger/separation anxiety is typical; support with predictable routines and warm transitions.
🦷 Teething & oral health
- Irritability, drool are common; fever/diarrhea ≠ teething—look for infection.
- first lower incision is arised as a teeth.
- Start tooth brushing with a smear of fluoride toothpaste once teeth erupt; avoid sweetened bottles.
🧯 Injuries & AEFI
- Choking (nuts, grapes, hard candy, coins), burns, falls, drowning in small buckets—anticipatory guidance at every visit.
- AEFI: fever, soreness—reassure and advise when to return (high fever, persistent crying, swelling spreading, allergic signs).
🧭 QUICK “RED FLAGS”.
- No social smile by 3 mo 😊
- Persistent head lag after 4–5 mo 🧷
- Not rolling by 6–7 mo; not sitting by 9 mo 🪑
- No babbling by 8–9 mo; no response to name by 9–10 mo 🗣️
- No pincer grasp or no single words by 12 mo ✋
- Any loss of previously acquired skills 🔁
- Poor feeding, lethargy, fever <3 mo, breathing difficulty, cyanosis, seizures—emergency. 🚑
📝 NURSING CARE FLOW (practical)
- Assess: birth history, feeding pattern, elimination, sleep, growth trend, milestone progression, safety environment, caregiver mood.
- Plan: feeding support (BF coaching; complementary plan), immunization catch-up, stimulation prescription (tummy time minutes/day, play ideas), safety checklist.
- Implement: demonstrate latch/position, show food textures/portions with caregiver’s utensils, model play, give safe sleep handout.
- Evaluate: weight/length gain trajectory, milestone progress, caregiver confidence; re-plan and refer as needed.
- Document & schedule follow-ups.
👶 TODDLER: Developmental Concept (1–3 years)
🌱 What “toddler” means
A toddler is a child in the rapid transition from infancy to early childhood, typically 1–3 years. This stage is marked by fast growth, motor independence, language explosion, emerging self-identity, and the psychosocial struggle of “Autonomy vs. Shame & Doubt” (Erikson). The toddler’s favorite word is often “No!” — a healthy sign of autonomy.
🧠 Core developmental domains (how toddlers typically progress)
- Gross motor: From walking independently ➝ running ➝ climbing ➝ kicking a ball, jumping with both feet, and stairs (initially one step at a time, often with support).
- Fine motor: From pincer perfection ➝ stacking blocks, scribbling then copying simple strokes/circles, turning pages, using a spoon/cup with minimal spillage, large-piece puzzles.
- Language/communication: From single words at ~12–15 months ➝ 50+ words & 2-word phrases by ~24 months ➝ follows 2-step commands, names common objects & body parts, uses I/me/mine, enjoys songs and rhymes.
- Cognitive (Piaget): Late sensorimotor ➝ beginnings of pre-operational thought at ~2 years. Object permanence is solid; cause-effect is enjoyed; symbolic/pretend play blossoms; thinking is egocentric and intuitive.
- Social–emotional: Strong attachment, separation anxiety (peaks then eases), parallel play (alongside peers, not yet cooperative), temper tantrums, pride/shame beginnings, imitative behavior.
- Personal–social/self-help: Feeds self, drinks from cup, helps undress, starts toilet readiness signs, tries simple chores (bringing shoes, putting toys away).
📏 Growth & physical pointers (clinically useful)
- Weight: ~tripled by 1 year; quadrupled by ~2 years.
- Height/length: ~75 cm at 1 year, ~85–90 cm at 2 years; roughly +10–12 cm/year.
- Head vs chest: Head ≈ chest at ~1 year; chest surpasses head during toddlerhood.
- Teeth: Most or all 20 primary teeth erupt by ~2½–3 years; begin tooth-brushing habits.
- Fontanel: Anterior fontanel typically closes by ~18 months.
🧩 Development of “Concepts” in Toddlers (how ideas form)
🪞 Self & body concept
- Builds a sense of “me”: says “mine”, recognizes self in the mirror, asserts choices (food, clothes, toys).
- Learns body parts (nose, eyes, tummy), begins body image; curiosity about genitals is normal — respond with calm, non-shaming guidance.
⏱️ Time, space, number & size
- Understands immediate time (“now/soon/later”), not clock time.
- Knows in/out, up/down, and near/far gradually.
- May rote-count small numbers and compare big vs small by ~2½–3 years.
- Colors and shapes recognition begins (names a few common ones toward the end of toddler period).
🎭 Symbolic thought & play
- Pretend play (feeding a doll, driving a toy car) shows symbolic thinking.
- Imitation is key: toddlers copy adult routines (sweeping, cooking play).
- Egocentrism is normal — sees world from own perspective.
🧭 Moral & social concepts (early seeds)
- Operates in pre-conventional morality (Kohlberg): behavior guided by rewards, consequences, and adult approval.
- Learns simple rules (don’t touch hot, wait your turn) via consistent limits and modeling.
🍎 Needs of the Toddler (holistic, practical)
🥗 Nutrition & hydration
- Offer 3 small meals + 2 healthy snacks daily; variety & routine reduce picky eating.
- Emphasize iron-rich foods (pulses, eggs, green leafy veg), protein, healthy fats, seasonal fruits/veg, milk/curd/paneer.
- Limit juice/sugary drinks; prefer plain water; avoid bottle-to-bed to prevent dental caries.
- Vitamin D & calcium support bone growth; iron prevents anemia (follow local guidance).
💤 Sleep & routines
- Needs ~11–14 hours/24h (often 1 daytime nap).
- Consistent bedtime routine (bath–book–bed), calm environment, limited screen exposure before sleep.
🚼 Toilet training (readiness, not rush)
- Look for readiness signs: stays dry ≥2 hours, follows simple instructions, pulls pants up/down, interest in potty, communicates need to go.
- Use positive reinforcement, no punishment; expect accidents during learning.
🧸 Play & stimulation
- Free, active, exploratory play daily: blocks, balls, push-pull toys, large crayons, nesting cups, picture books, pretend kitchen, simple puzzles.
- Play is the toddler’s work — it builds motor, language, cognition, social skills.
🧼 Hygiene, oral care & skin
- Hand-washing before eating/after toileting; short nails; daily bath as climate allows.
- Brush teeth twice daily with a smear of fluoride toothpaste; first dental visit during toddler years.
- Sun protection and gentle moisturizers for sensitive skin.
🛡️ Safety (top priority)
- Choking prevention: cut foods small; avoid nuts/whole grapes/hard candies.
- Burns/falls/drowning: kitchen & bathroom safety, never leave near water, use stair gates, hot liquids out of reach.
- Poisoning: lock medicines/cleaners/kerosene/pesticides; label containers; keep battery items secure.
- Transport: age-appropriate car seat; road safety habits early.
- Animal bites: supervised contact; teach gentle handling.
💬 Emotional needs & behavior guidance
- Provide warmth, predictable routines, choices (“blue cup or red cup?”), and clear limits.
- Use emotion coaching: name feelings (“you’re angry because the toy broke”), and redirect.
- Tantrums are communication — stay calm, ensure safety, ignore minor outbursts, praise calm behaviors.
🩺 Health services & surveillance
- Keep immunizations up-to-date (boosters typically due in this window; follow your national schedule).
- Growth monitoring: weight, height, MUAC, head circumference; track on growth charts.
- Deworming & Vitamin A as per local programs.
- Developmental screening at regular visits; autism-specific screens often at ~18 and 24 months.
👩👦 Roles in Toddler Care (who does what)
👨👩👧 Parents/Caregivers
- Create safe, loving, structured home; provide nutritious meals, sleep schedules, daily play, reading aloud, toilet-training support.
- Model language (talk, sing, name objects), and pro-social behavior (sharing, waiting turns).
- Use positive discipline (clear rules, natural consequences, praise); avoid corporal punishment.
- Maintain health visits, immunizations, dental checks; seek help for red flags (see below).
🧑⚕️ Nurse/ANM/Health worker (community & clinic)
- Assess growth & development; plot on charts; identify risk or delay.
- Guide feeding, address picky eating/anemia, counsel toilet training, sleep hygiene, injury prevention.
- Ensure immunization, Vitamin A, deworming, oral health education.
- Teach home management of minor illnesses (fever, cough, diarrhea with ORS/zinc), and danger signs needing referral.
- Provide parent coaching for tantrums, separation anxiety, and toilet training; screen for developmental delay/autism; coordinate referrals (ENT/ophthalmology/physio/early intervention).
🧑🏫 Anganwadi/ECCE/Preschool & Community
- Offer play-based learning (songs, stories, group play), monitor nutrition, and coordinate supplementation per programs.
- Support parental education sessions on safety, nutrition, and responsive caregiving.
⚠️ Common Problems in Toddlerhood:-
😤 Behavioral & emotional
- Temper tantrums/negativism: Normal assertion of autonomy. Stay calm, reduce triggers (hunger/tiredness), offer choices, set limits, praise calm recovery.
- Separation anxiety: Practice brief separations, predictable good-bye rituals, reassure with return.
- Sleep issues/night waking: Consistent bedtime, soothing routine, no screens pre-bed, respond calmly with minimal stimulation.
- Toilet training difficulties/constipation: Ensure readiness, fiber & fluids, toilet stool for feet support, reward sitting practice, treat constipation early.
🥣 Feeding & nutrition
- Picky eating: Normal. Offer small portions, repeat exposures (10–15x), no force-feeding, routine mealtimes, family modeling.
- Anemia/under-nutrition: Encourage iron-rich foods; review milk overuse (can displace iron foods); consider supplements as advised.
- Bottle caries: Avoid bottle in bed; brush twice daily; prefer cup.
🤧 Common illnesses
- URIs, fever, otitis media, diarrhea: Know home care basics, hydration, red flags (poor feeding, lethargy, fast breathing, chest indrawing, persistent vomiting, blood in stool, seizures).
- Skin issues: diaper rash (keep dry, barrier creams), eczema (gentle cleansers, moisturize).
- Wheezing/reactive airway: Recognize respiratory distress signs; follow care plans if diagnosed.
🧩 Developmental concerns (red flags worth acting on)
- 12–15 mo: no single words, no gestures (pointing/waving), no response to name.
- 18 mo: no pretend play, no 6–10 words, limited eye contact or joint attention.
- 24 mo: no two-word phrases, loss of language/social skills at any time, persistent toe-walking or stiff/floppy tone.
- Any age: regression, poor hearing/vision, not walking by ~18 mo, no interest in play.
👉 Early evaluation (hearing, vision, developmental/ASD screening) and early intervention change trajectories.
🧯 Injuries & poisoning (most preventable issue)
- Choking, burns, falls, road injuries, drowning, dog bites, chemical/med ingestion are high risk.
- Child-proofing, supervision, safe storage, and early teaching of “stop/wait/hold hands” save lives.
✅care frameworks
🛑 Tantrum T-A-M-E
Trigger control (sleep/food); Acknowledge feeling; Minimize attention to outburst; Engage after calm with a simple choice/redirect.
🚽 Toilet training 1–2–3
1: Wait for readiness; 2: Routine sits after meals; 3: Reward successes, ignore accidents, never punish.
🥗 Picky eating 5S
Schedule meals/snacks; Small portions; Serve variety; Stay neutral (no pressure); Show (model eating the same foods).
🌡️ Diarrhea/fever home care ABC
Amounts of fluids/ORS; Beware red flags (blood stool, lethargy, fast breathing, sunken eyes); Consult/visit if flags or poor intake.
🌸 PRESCHOOLER (3 – 6 YEARS): DEVELOPMENTAL CONCEPT
💡 Concept of Development
The preschool stage — often called the “foundation age” — bridges the gap between infancy and formal schooling.
At this age, the child’s growth is steady rather than rapid, and development focuses mainly on refining motor, social, language, emotional, and intellectual abilities.
This is the age of initiative, curiosity, imagination, and play.
According to Erik Erikson, the psychosocial stage is “Initiative vs Guilt.”
The child learns to initiate activities, explore the environment, and develop confidence; if discouraged, feelings of guilt and inadequacy may appear.
🌿 1️⃣ Physical Development
⚖️ Growth
- Weight: Increases about 2 kg per year.
- Height: Increases about 5 – 7 cm per year.
- Body Proportion: Legs lengthen, abdomen flattens, and the child looks slimmer and taller.
- Teeth: All 20 deciduous teeth usually erupted by 3 years.
🏃♀️ Gross Motor Development
- 3 yrs – runs, climbs stairs with alternate feet, rides tricycle.
- 4 yrs – hops on one foot, throws and catches ball.
- 5 yrs – skips, balances on one foot for > 5 seconds.
- 6 yrs – rides bicycle, ties shoelaces, starts coordinated sports.
✋ Fine Motor Development
- Can draw circles, squares, stick figures.
- Dresses self with little help.
- Builds towers, uses scissors, buttons, spoons, toothbrush.
- Begins to copy letters and numbers.
💬 2️⃣ Language Development
- Rapid vocabulary growth: from about 900 words at 3 yrs to 2000+ words by 6 yrs.
- Forms full sentences, tells short stories, asks endless “Why?” questions.
- Can express needs, ideas, and imagination clearly.
- Pronunciation improves; some sounds may still be imperfect.
- Reading readiness develops — recognizes letters, pictures, and rhymes.
🧠 3️⃣ Cognitive (Intellectual) Development
- According to Piaget, this is the Preoperational Stage (2 – 7 yrs).
- Thinking is egocentric, magical, and non-logical — they believe their thoughts can cause events.
- Understands time in simple terms like “after lunch” or “tomorrow.”
- Develops imagination and symbolic play (using a stick as a horse).
- Begins to classify objects by shape or color.
- Learns basic counting, colours, shapes, and opposites.
💞 4️⃣ Emotional & Social Development
- Learns to cooperate, share, and make friends through group play.
- Shows affection, empathy, and beginning sense of morality (“good” vs “bad”).
- Imitates adults’ behavior — wants to be like parents and teachers.
- Begins to control temper but still shows outbursts if frustrated.
- Fear of darkness, strangers, or imaginary creatures is common.
- Gains independence but needs love, security, and reassurance.
🎭 5️⃣ Moral Development
- Based on Kohlberg’s Pre-conventional Level:
- Behaviour guided by reward and punishment.
- Understands simple moral rules (“don’t hit,” “say thank you”).
- Moral values learned mainly from parents, teachers, and observation.
🕊️ 6️⃣ Spiritual Development
- Learns about right and wrong in connection with pleasing parents or God.
- Can learn simple prayers, blessings, or good-deed habits.
- Develops awe and curiosity toward nature and religion.
🩺 7️⃣ Health and Nutritional Needs of Preschooler
🍲 Nutritional Needs
- Balanced diet with proteins, carbohydrates, fats, vitamins, and minerals.
- Require about 1500–1800 kcal/day.
- Encourage fruits, vegetables, milk, and small frequent meals.
- Teach self-feeding, good table manners, and avoidance of junk food.
🪥 Hygiene and Health Needs
- Regular bathing, hair and nail care, teeth brushing twice daily.
- Annual health check-ups, immunization completion (booster doses).
- Safe environment to prevent accidents and burns.
- Regular sleep (10–12 hours/day) with quiet bedtime routine.
🎓 8️⃣ Educational and Play Needs
🎨 Play Needs
- Play is the work of the preschooler! 🧩
- Promotes physical, intellectual, and emotional growth.
- Types of play:
- Imaginative play: pretending to be doctor, nurse, teacher.
- Constructive play: blocks, puzzles, drawing.
- Co-operative play: group games, singing, dancing.
- Through play, children learn sharing, patience, and problem-solving.
📚 Learning Needs
- Basic skills for school: recognition of alphabet, colors, counting, storytelling.
- Develop concentration and memory.
- Encourage curiosity through questioning and exploration.
🫶 9️⃣ Role of Parents and Nurses
👨👩👧 Role of Parents
- Provide love, security, and consistent discipline.
- Encourage independence (dressing, feeding, toileting).
- Avoid comparing child with others.
- Answer questions honestly and patiently.
- Promote socialization through play groups or nursery school.
👩⚕️ Role of Nurse
- Guide parents regarding nutrition, hygiene, safety, and immunization.
- Detect early developmental delays and refer if needed.
- Encourage positive reinforcement instead of punishment.
- Educate about pre-school readiness, emotional support, and health promotion.
- Teach injury prevention — burns, falls, choking, poisoning.
⚠️ 🔟 Common Problems in Preschool Stage
1️⃣ Behavioral Problems 😠
- Temper tantrums, stubbornness, jealousy, aggression.
- Usually due to over-control or lack of attention.
➤ Management: Ignore minor misbehavior, reward good conduct, provide love and consistency.
2️⃣ Sleep Disturbances 😴
- Nightmares, fear of dark, bedtime resistance.
➤ Management: Maintain bedtime routine, provide comfort item, avoid frightening stories.
3️⃣ Toilet Training Issues 🚽
- Enuresis (bed-wetting), encopresis (soiling).
➤ Management: Avoid punishment, maintain regular toilet schedule, limit fluids before bed.
4️⃣ Nutritional Problems 🍬
- Poor appetite, picky eating, anaemia, or obesity.
➤ Management: Provide variety, involve child in food choice, offer small frequent meals.
5️⃣ Injury and Accidents 🩹
- Falls, burns, choking, poisoning — major cause of morbidity.
➤ Prevention: Supervision, safe environment, teach danger awareness.
6️⃣ Emotional Problems 😢
- Fear, sibling rivalry, separation anxiety, low confidence.
➤ Support: Reassurance, emotional bonding, storytelling, involvement in daily activities.
🎒 SCHOOL-AGE (SCHOOLER) — DEVELOPMENTAL CONCEPT
🌱 What “development” means here
- Growth slows but stays steady: bones lengthen, muscles strengthen, stamina improves.
- Development shifts toward skills, competencies, habits, and identity that make the child a successful student, friend, and team-member.
- Core theme: “Doing and achieving” → a sense of competence.
🧩 Domains you’ll observe
- Physical/Motor: improved coordination, fine motor skill (writing, instruments, crafts), team sports readiness.
- Cognitive/Academic: reading fluency, numeracy, problem solving, rule-based games, understanding time/money/space.
- Language/Communication: richer vocabulary, narratives, jokes/puns, classroom discussion.
- Psychosocial: peer approval rises, self-concept refines (strengths/weaknesses), self-esteem becomes grades/skills-linked.
- Emotional regulation: better impulse control, uses rules & routines to feel secure.
- Body-image & puberty preview: interest in body function and modesty; pre-pubertal changes may start late in this stage.
🧩 DEVELOPMENTAL NEEDS (HOLISTIC)
🥗 1) Physical & biological needs
- Balanced nutrition 🥦: whole grains, pulses, fruits/veg, dairy/alternatives, lean proteins; limit ultra-processed snacks/sugary drinks.
- Sleep 😴: consistent routine; typical need ~9–12 hours/night; no screens before bed.
- Activity 🏃♀️: daily play/sport, endurance + strength + flexibility; limit screen time.
- Hygiene & oral health 🪥: brush 2× daily, floss/clean between teeth, periodic dental checks; safe water & hand hygiene.
- Safety 🛡️: road safety, helmet use, water safety, safe internet, safe touch/personal boundaries.
- Immunization 💉: age-appropriate booster doses per national schedule; deworming/vision/hearing checks as advised.
🧠 2) Cognitive & school needs
- Structured learning with clear expectations, feedback, and practice.
- Reading culture 📚: daily reading, library exposure, puzzles, constructive hobbies (music, art, coding, crafts).
- Homework scaffolding ✏️: chunk tasks, planners, quiet study space, praise effort (growth mindset).
❤️ 3) Emotional & mental-health needs
- Warm, predictable relationships 🤗; consistent rules.
- Emotion coaching 🫶: name feelings, normalize mistakes, problem-solve together.
- Self-esteem 🌟: celebrate process and persistence, not just marks.
🫂 4) Social & moral needs
- Peer engagement 👯: team games, group projects; learn fairness, sharing, conflict resolution.
- Values & empathy 💬: discuss fairness, honesty, consequences; model respectful behavior.
- Digital citizenship 💻: kindness online, privacy awareness, reporting bullying, time limits.
🧭 5) Sexuality & body-safety education (age-appropriate)
- Correct body terms, personal boundaries, consent, safe/unsafe touch, whom to tell.
- Puberty prep (especially 9–12): normalize changes, hygiene, periods/wet dreams, mood shifts.
🏥 6) Health-system interface (nursing/public health)
- Periodic screening: growth/BMI trend, vision, hearing, dental, posture/backpack ergonomics, anemia risk.
- Anticipatory guidance: safety, media use, sleep, nutrition, sport readiness, mental-health red flags.
- School health linkage: teacher collaboration, referral pathways, inclusive education.
🧑🎓 EMERGING ROLES OF THE SCHOOLER
- Student/learner 📖: follows routines, completes tasks, seeks mastery, owns mistakes, asks for help.
- Friend/peer 🤝: learns cooperation, turn-taking, loyalty, handles peer pressure.
- Family member 🏠: contributes with age-appropriate chores, care for belongings, basic self-care independence.
- Team-mate/citizen 🏅: plays fair, respects rules, accepts diversity, participates in community/school events.
- Digital citizen 🌐: responsible device use, protects privacy, avoids harmful content, balances screen time.
- Self-manager ⏱️: packs bag, manages timetable/homework, basic money-time organization, personal hygiene.
⚠️ COMMON DEVELOPMENTAL PROBLEMS (WHAT TO WATCH & WHY)
🧬 1) Growth & nutrition
- Under-nutrition / micronutrient deficiencies (e.g., iron) → fatigue, poor attention, frequent infections.
- Overweight/obesity → low self-esteem, bullying risk, metabolic concerns; often linked to sedentary life + diet.
- Feeding struggles/picky eating → inadequate variety; needs behavioral shaping & family modeling.
👁️🦷 2) Sensory & dental
- Uncorrected vision/hearing issues 👓👂 → “inattention,” poor grades; needs screening & timely correction.
- Dental caries/malocclusion 🦷 → pain, speech issues, absenteeism; stress daily care + dental visits.
🧠 3) Learning & neurodevelopment
- Specific learning disorders (dyslexia, dysgraphia, dyscalculia) ✍️➗
- Clues: uneven skills (smart orally but weak in reading/writing/math), avoids tasks, slow work.
- Needs assessment, remediation, accommodations (extra time, audiobooks, multisensory teaching).
- ADHD ⚡: inattention, hyperactivity/impulsivity across settings; support via structure, behavior plans, specialist care.
- Autism spectrum (higher-functioning) 🧩: social communication differences, restricted interests; requires individualized supports.
🧠💬 4) Emotional–behavioral
- Anxiety (tests, separation, social), low mood, somatic complaints (headache, tummy-ache).
- Oppositional behaviors when demands are high or routines inconsistent.
- Bullying (victim or perpetrator) 🛑: watch for school avoidance, mood changes, secrecy online.
🛡️ 5) Safety & lifestyle
- Injuries (roads, water, sports) → need rules, equipment, supervision.
- Screen overuse & gaming dependency 🕹️ → sleep loss, irritability, academic dip.
- Online risks 🧨: cyberbullying, scams, exposure to harmful content; enforce family media plan.
🚻 6) Somatic/functional
- Enuresis/encopresis, constipation; often behavioral + physiological; respond with non-shaming, routines, medical review.
- Allergy/asthma, recurrent infections, posture issues (heavy backpacks), scoliosis signs.
🧒 7) Early/late puberty concerns
- Precocious signs or delayed changes → pediatric evaluation and supportive counseling.
🩺 NURSING INTERVENTIONS
🔍 Assessment & screening
- Track growth trends (not single points), diet, sleep, activity, school performance, mood/behavior, family stress.
- Routine vision/hearing/dental checks; observe posture and backpack ergonomics.
💬 Anticipatory guidance (child + parent)
- Routines: sleep, homework, chores, device limits.
- Nutrition: family meals, healthy swaps, lunchbox planning, hydration.
- Safety: roads, water, sports gear, kitchen tools, dog safety, “stranger & body-safety” rules.
- Media literacy: co-view, discuss content, teach pause-think-check.
🏫 School partnership
- Communicate with teachers; promote Individualized Education Plans where needed.
- Advocate inclusive classrooms, anti-bullying policies, and mental-health first aid awareness.
🧰 Skill-building for the child
- Teach study strategies (chunking, spacing, note-making), emotion regulation (deep breathing, “name it to tame it”), friendship skills (assertive “I-statements”).
🧭 When to refer (red flags)
- Persistent academic decline, teacher concerns despite support.
- Marked behavior change, self-harm talk, sleep/appetite disruption.
- Hearing/vision complaints, frequent headaches, squinting, very close reading.
- Growth faltering or rapid weight gain; early/late puberty signs.
- Recurrent wheeze, exertional breathlessness, syncope.
🌱 What is Adolescence?
Adolescence is the transitional period between childhood and adulthood, typically 10–19 years (many educators also consider “youth” up to 24). It’s marked by rapid biological (pubertal), cognitive, emotional, and social change. Nurses view adolescence through a bio-psycho-social lens: growth of the body 🧬, growth of the mind 🧠, and growth of relationships & roles 🤝.
Key developmental frameworks
- Erikson: Identity vs. Role Confusion—forming a stable sense of “Who am I?” 🪞
- Piaget: shift to formal operational thinking—abstract reasoning, hypothesis testing, future orientation 📈
- Kohlberg: progression in moral reasoning—from “rules” to principles & values ⚖️
- Elkind: adolescent egocentrism—imaginary audience & personal fable (feeling invincible) 🎭
- Marcia: identity statuses—diffusion, foreclosure, moratorium, achievement 🧭
🧭 Staging Overview (used in nursing & adolescent medicine)
- Early adolescence (≈10–13 yrs)
- Middle adolescence (≈14–16 yrs)
- Late adolescence (≈17–19+ yrs; “emerging adulthood” may extend to ≈24)
Below, each stage covers: developmental concept, needs, role expectations, common problems, and nursing focus.
1) 🌤️ Early Adolescence (≈10–13 years)
🔬 Developmental Concept
- Biological: Pubertal onset; growth spurts; secondary sex characteristics. Body changes are visible and fast, driving curiosity and self-consciousness.
- Cognitive: Mostly concrete thinking; beginning to question but still literal; short-term focus.
- Psychosocial: Heightened self-awareness and body image; same-sex peer bonding strong; seeking a bit more privacy; testing rules.
- Emotional: Fluctuating mood due to hormones and novelty; heightened sensitivity to peer feedback.
- Moral/Values: Rules still matter, but starting to recognize exceptions; “Is it fair?” becomes important.
🧡 Needs
- Accurate, age-appropriate body education about puberty & hygiene 🚿
- Nutritional support (iron, calcium, protein) for growth; regular meals & hydration 🥗
- Sleep hygiene (≈9–10 hours/night) to support growth & learning 😴
- Physical activity & play for musculoskeletal health and self-esteem 🏃♀️
- Basic digital literacy & boundaries (screen time, online safety) 📱
- Safe spaces & trusted adults for questions about body, emotions, friendships 🛟
🎭 Role Expectations (home–school–peers)
- Home: Learn self-care (hygiene, organizing schoolwork), share small chores, respect boundaries 🏡
- School: Build study habits, participate in group learning, explore interests 📚
- Peers: Practice inclusion, empathy, conflict resolution; avoid bullying 🤗
- Self: Begin identity exploration—likes/dislikes, talents, values 🧩
⚠️ Common Problems
- Body image worries, early/late maturation stress, acne, growth pains 🪞
- School adjustment issues, concentration difficulties, procrastination 📝
- Bullying/cyberbullying; low self-esteem; social withdrawal 😔
- Beginning risk exposure: unsupervised internet use, curiosity about substances or sexuality (usually informational stage) 🚫
🩺 Nursing Focus (Stage-Specific)
- Gentle, brief education on puberty, menstrual hygiene, nocturnal emissions, personal care 🗣️
- HEADSSS screening lite (Home, Education/Employment, Activities, Drugs, Sexuality, Suicide/Depression, Safety) to open dialogue 🧩
- Reinforce nutrition, WASH, deworming schedules, immunization boosters (per local program) 💉
- Parental guidance: warmth + structure; monitoring without shaming; positive reinforcement 👨👩👧
- Promote sport/play and sleep routines; address bullying pathways & school coordination 🛡️
2)🌦️ Middle Adolescence (≈14–16 years)
🔬 Developmental Concept
- Biological: Puberty advances toward completion; body shape and strength increase.
- Cognitive: Rising abstract thinking; experimenting with ideals, causes, and logic; risk–reward sensitivity peaks.
- Psychosocial: Peer approval is powerful; trying out multiple identities (clothes, music, groups).
- Emotional: High emotional intensity; sensation-seeking; developing romantic interest 💞
- Moral/Values: Challenges to authority, debating fairness, rights, and autonomy.
🧡 Needs
- Autonomy with guidance: choices in academics, hobbies, time; adult scaffolding 🧗
- Skills training: study skills, time management, assertive communication, refusal skills 🗓️
- Sexual & reproductive health (SRH) education: consent, boundaries, STI awareness, safe behaviors, respect and equality 🫶
- Mental health literacy: understanding stress, anxiety, low mood; coping skills 🧘
- Substance use prevention: factual information, peer-led models 🚭
- Career exposure: talks, internships, role models, volunteering 🧑💼
🎭 Role Expectations
- Home: Increased responsibility (younger sibling support, budgeting basics), collaborative decision-making 🏠
- School: Goal setting, exam discipline, joining teams/clubs; academic honesty 🎯
- Peers/Relationships: Healthy friendships & dating norms: consent, respect, boundaries; bystander action against violence 💬
- Community/Online: Digital citizenship; community service; safe mobility 🚲
⚠️ Common Problems
- Risk behaviors: truancy, unsafe rides, early substance experimentation, unsafe sexual activity 😟
- Academic stress & perfectionism, sleep deficit, screen overuse 📵
- Eating problems (skipping meals, fad dieting), disordered eating patterns 🍽️
- Mental health: anxiety, depressive symptoms, self-harm ideation; peer pressure; identity conflict 🧨
- Violence & harassment: bullying, dating violence, cyber exploitation, discrimination 🛑
🩺 Nursing Focus
- Confidential, non-judgmental counselling; ensure privacy & trust 🤝
- Structured HEADSSS with risk assessment; screen for anemia, BMI-for-age, vision/hearing, mood (e.g., brief tools), and substance risk (age-appropriate tools) 🧪
- Skill-building sessions: stress management, problem-solving, negotiation, refusal skills 💬
- SRH counselling: anatomy, consent, delaying & safer choices, respect; address myths clearly 📘
- Coordinate with school health, peer educators, community groups; facilitate referrals (mental health, dermatology, dental, etc.) 🔗
3) ☀️ Late Adolescence (≈17–19+ years; often to ≈24)
🔬 Developmental Concept
- Biological: Puberty completed; growth stabilizes; focus shifts to fitness and body competence.
- Cognitive: Stronger executive functions—planning, impulse control, weighing long-term outcomes.
- Psychosocial: Consolidating identity (values, politics, spirituality, orientation), intimacy and commitment grow.
- Emotional: Better self-regulation; reflective thinking; resilience building.
- Moral/Values: Move toward principle-based reasoning and social responsibility.
🧡 Needs
- Career & vocational clarity: mentorship, internships, application coaching, financial literacy 💼
- Transition skills: leaving home/hostel life, cooking, budgets, time & stress management 🧳
- Relationship skills: communication, consent, contraception literacy (as per local policies), conflict resolution 🧷
- Maintaining mental health: coping, seeking help early, relapse prevention 🌿
- Civic engagement: volunteering, voting literacy, leadership, environmental responsibility 🌍
- Healthy lifestyle maintenance: sleep, nutrition, exercise, substance-free living 🏋️
🎭 Role Expectations
- Self: Independent decision-making, ethical conduct, self-care & health maintenance 🧭
- Family: Adult-to-adult communication, shared planning for finances/career, respect for generational values 💬
- Education/Work: Professionalism, accountability, teamwork, lifelong learning 🎓
- Relationships/Community: Mutual respect, safe intimacy, boundary-setting, service leadership 🕊️
⚠️ Common Problems
- Career/academic pressure, burnout, test anxiety, failure fear 😥
- Substance misuse escalation (parties, hostels), risky driving/road injuries 🚗
- Intimate partner issues: coercion, unsafe sex, unintended pregnancy, STIs 💔
- Mood disorders, suicidal ideation, loneliness (especially after transitions) 🌧️
- Financial stress, poor work–life balance, digital addiction, gambling/gaming risks 💸
🩺 Nursing Focus
- Transition-to-adulthood counselling: health insurance basics, when/where to seek care, self-advocacy 🗺️
- Career & stress clinics with time-management and test-prep strategies ⏱️
- Substance & injury prevention: peers as safety champions; helmet/seatbelt adherence 🪖
- SRH services in a rights-respecting, confidential manner; routine testing when indicated; stigma-free care 🩻
- Mental-health first aid: screening, brief interventions, strong referral pathways 🌉
🧩Cross-Cutting “Big Rocks” Every Nurse Should Address
🥗 Nutrition & Anemia
Rapid growth + poor diet = iron deficiency, calcium deficit, vitamin D gap. Promote iron–folic, protein, fruits/veg, hydration; address menstrual blood loss in girls and skip-meal culture in boys and girls.
🛏️ Sleep
Teen circadian shift → late sleep. Aim 8–10 hours; discourage all-night study & doomscrolling.
🧠 Mental Health Literacy
Normalize feelings, teach coping skills, foster help-seeking. Watch for red flags: persistent low mood, anhedonia, major sleep/appetite change, self-harm talk, withdrawal.
💬 Communication that Works
Use open questions, validate feelings, avoid lecturing. Confidentiality (within safety limits) builds trust. Encourage parent–adolescent dialogue that is warm, firm, & fair.
🛡️ Safety & Violence Prevention
Bullying, dating violence, harassment (including cyber) require zero tolerance and clear pathways: report, protect, support, refer.
🧭 Ethical–Legal Awareness
Provide adolescent-friendly, non-judgmental care. Follow local laws and organizational guidelines on privacy, consent/assent, safeguarding and mandatory reporting where applicable.
🧑⚕️ Role of the Nurse/ANM with Adolescents (Practical Checklist)
Document & Follow-up: set goals; review after 2–4 weeks; celebrate small wins 🎉.
Screen & Educate: HEADSSS; vitals, BMI-for-age, vision, oral health; anemia screening when feasible.
Counsel: puberty, menstrual health, hygiene, acne care; SRH & consent (age-appropriate); substance refusal skills.
Mental Health First Line: empathic listening; brief interventions; safety planning; referral for risk.
Build Skills: study habits, stress tools, problem-solving, digital hygiene, peer-support.
Engage Family & School: create supportive environments; anti-bullying policy; safe campus.
Link to Programs/Services: adolescent clinics, peer educator clubs, nutrition & deworming days, helplines.
🧠ERIKSON THEORY OF PSYCOSOCIAL DEVELOPMENT:-
1) 👶 Infancy (0–1 yr): Trust vs. Mistrust → Virtue: Hope
- Core need: Consistent warmth—feeding, touch, timely response to cries ❤️
- Hallmarks: Attachment, soothing, sensory exploration; stranger anxiety emerges
- Risk if unmet: Insecure attachment, withdrawal, difficulty self-soothing 😟
- Nursing cues & actions: Promote rooming-in, skin-to-skin, responsive feeding, teach caregivers sensitive attunement; pain control; stable routines 🍼
2) 🚼 Toddlerhood (1–3 yrs): Autonomy vs. Shame & Doubt → Virtue: Will
- Core need: Safe chances to “do it myself” (toilet training, dressing) 🎯
- Hallmarks: Parallel play, negativism (“No!”), emerging self-control
- Risk if unmet: Shame, doubt, compulsivity or over-dependence
- Nursing cues & actions: Offer choices, simple tasks, positive toilet guidance, praise effort; avoid ridicule for accidents; teach calm limit-setting 🚽
3) 🧒 Early Childhood (3–6 yrs): Initiative vs. Guilt → Virtue: Purpose
- Core need: Permission to imagine, lead small games, ask “why?” 🌈
- Hallmarks: Fantasy play, planful behavior, gender-role exploration
- Risk if unmet: Excess guilt, inhibition, fear of trying
- Nursing cues & actions: Therapeutic play, allow role-play (nurse/doctor kits), give small “helper” jobs; frame rules as safety, not shame 🎭
4) 🧑🎒 Middle Childhood (6–12 yrs): Industry vs. Inferiority → Virtue: Competence
- Core need: Opportunities to master skills and be recognized 🏆
- Hallmarks: School tasks, teamwork, hobbies; compares self with peers
- Risk if unmet: Inferiority, inertia, “I’m not good at anything”
- Nursing cues & actions: Set achievable goals, sticker charts, teach self-care routines (asthma, diabetes), celebrate progress; anti-bullying support 📚
5) 🧭 Adolescence (12–18 yrs): Identity vs. Role Confusion → Virtue: Fidelity
- Core need: Space to explore values, careers, body image, relationships 🔎
- Hallmarks: Abstract thinking, peer salience, cause-driven interests
- Risk if unmet: Role confusion, repudiation, risky experimentation
- Nursing cues & actions: HEADSSS screening, confidential & non-judgmental counselling, SRH education, coping skills, peer-support programs 🧑⚕️
6) 💞 Young Adulthood (18–40 yrs): Intimacy vs. Isolation → Virtue: Love
- Core need: Build mutual, committed relationships while keeping identity 🤝
- Hallmarks: Deeper friendships, partnership, career launch
- Risk if unmet: Isolation, exclusivity or superficial “promiscuity” of attachments
- Nursing cues & actions: Teach communication, consent, mental-health literacy, work–life balance; support for infertility, SRH, and relationship stress 💬
7) 🌱 Middle Adulthood (40–65 yrs): Generativity vs. Stagnation → Virtue: Care
- Core need: Contribution—parenting, mentoring, community service 🌍
- Hallmarks: Productivity, legacy, guiding the next generation
- Risk if unmet: Stagnation, self-absorption, rejectivity
- Nursing cues & actions: Screen NCD risks; encourage volunteering/mentoring, caregiver-stress support, midlife mental-health checks, purpose-building programs 🧩
8) 🕊️ Late Adulthood (65+): Integrity vs. Despair → Virtue: Wisdom
- Core need: Life review with acceptance—“I lived meaningfully.” 📖
- Hallmarks: Reminiscence, reconciliation, spiritual growth
- Risk if unmet: Despair, bitterness, fear of death, disdain
- Nursing cues & actions: Guided life-review, legacy projects, grief support, dignity-conserving care, advance-care planning, pain & symptom control 🌟
🌟SIGMUND FREUD ; PSYCOSEXUAL DEVELOPMENT:-
1) 👶 Oral Stage (0–1 year) — Mouth focus
Zone: mouth (sucking, swallowing, biting)
Task/Conflict: Weaning & basic trust—tolerating delay of gratification, soothing without constant oral input
Caregiver keys: warm, predictable feeding; don’t underfeed/overfeed; allow non-nutritive soothing appropriately 🍼
If well resolved: basic trust, openness, ability to give/receive nurture 🤍
If fixated:
- Oral-receptive: dependency, seeking comfort via mouth (over-eating, nail-biting, smoking)
- Oral-aggressive: biting sarcasm, verbal hostility
Nursing pearls: teach responsive feeding, skin-to-skin, avoid using the bottle as the only comfort tool; support caregivers to read hunger vs comfort cues. 👩⚕️
2) 🚽 Anal Stage (1–3 years) — Control & autonomy
Zone: anus (retention/expulsion)
Task/Conflict: Toilet training + autonomy vs control—learning self-control without shame
Caregiver keys: patient, non-shaming approach; celebrate attempts; respect readiness signs; predictable routines ⏱️
If well resolved: autonomy, willpower, healthy pride in mastery 💪
If fixated:
- Anal-retentive: over-orderly, stingy, perfectionistic
- Anal-expulsive: messy, impulsive, defiant
Nursing pearls: coach parents on readiness (dry intervals, interest in toilet), positive reinforcement, avoid punishment or ridicule. 🌟
3) 🎭 Phallic Stage (3–6 years) — Identity & curiosity
Zone: genitals (self-exploration; noticing sex differences)
Task/Conflict: managing Oedipal/Electra dynamics (affection toward opposite-sex parent; rivalry with same-sex parent) and identification with same-sex parent; beginning of superego formation
Caregiver keys: calm answers to body questions, teach privacy & boundaries without shame, model respectful adult relationships 👨👩👧
If well resolved: initiative, confidence, identification with positive role models, conscience development 🧭
If fixated: vanity, boastfulness, or conversely sexual guilt/anxiety; difficulties with authority
Nursing pearls: normalize curiosity, use simple body-safety rules (“bathing suit areas are private”), avoid scolding; guide parents to respond matter-of-factly. 🛟
4) 🧑🎒 Latency Stage (6–12 years) — Energy goes to learning
Zone: drives are sublimated into school, hobbies, and friendships
Task/Conflict: build industry, skills, and peer bonds; consolidate superego values
Caregiver keys: structure + encouragement; chances to master academics, arts, sports; teamwork 🤝
If well resolved: competence, focus, cooperation, self-esteem 🏅
If fixated (or poorly supported): feelings of inferiority, disengagement, school avoidance
Nursing pearls: reinforce hobbies, anti-bullying strategies, praise effort, set realistic goals; screen for learning or attention issues early. 📚
5) 🌱 Genital Stage (12+ years into adulthood) — Mature intimacy & work
Zone: genitals, now oriented to mutual, age-appropriate intimacy
Task/Conflict: integrate earlier stages to form mature sexuality, capacity for love, and productive work
Caregiver keys (and clinicians too): balanced guidance on relationships, consent, responsibility, values, and long-term goals 🧭
If well resolved: stable relationships, empathy, creativity, responsibility, balance of Id–Ego–Superego ❤️🩹
If conflicts persist: unstable intimacy, identity confusion, guilt or anxiety around sexuality, or compulsive sensation-seeking
Nursing pearls: provide adolescent-friendly, confidential counselling; teach consent, respect, contraception literacy (as per local law/policy), and mental-health coping. 🩺
🧩 Fixation & Regression (why it matters clinically)
- Fixation: unmet needs or over-gratification at a stage → enduring traits (e.g., oral comfort-seeking under stress).
- Regression: under stress, people may revert to earlier patterns (thumb-sucking, tantrums, comfort eating).
Nursing tip: When you see “younger” coping behaviors during illness, view them as stress signals, not “misbehavior,” and add comfort + skill-building. 🌤️
🛡️ Defense Mechanisms (Ego’s toolset)
Common, often unconscious ways the Ego manages conflict:
- Repression (burying painful thoughts) 🙈
- Projection (attributing one’s feelings to others) 🎯
- Displacement (redirecting feelings to a safer target) 🔁
- Reaction formation (showing the opposite feeling) 🔄
- Rationalization (justifying to avoid discomfort) 🧮
- Sublimation (channeling drives into creative/socially useful work) 🎨
- Regression (temporary return to earlier behaviors) ⏪
Clinical use: teach healthy sublimation, problem-solving, and communication to replace less helpful defenses. 🌱
⚖️ Erikson vs. Freud (quick clarity)
- Freud = Psychosexual (oral, anal, phallic, latency, genital; focus on drives and bodily zones).
- Erikson = Psychosocial (social relationships & identity across the entire lifespan).
Erikson extends development beyond childhood, emphasizing social roles, culture, and virtue formation. 🌐