ENGLISH UNIT-4-MSN-II-OPTHALMOLOGY AND OPTHALMIC NURSING-DISORDERS (PART-3)
OPHTHALMOLOGY AND OPHTHALMIC NURSING-DISORDERS.
- Define blepharitis
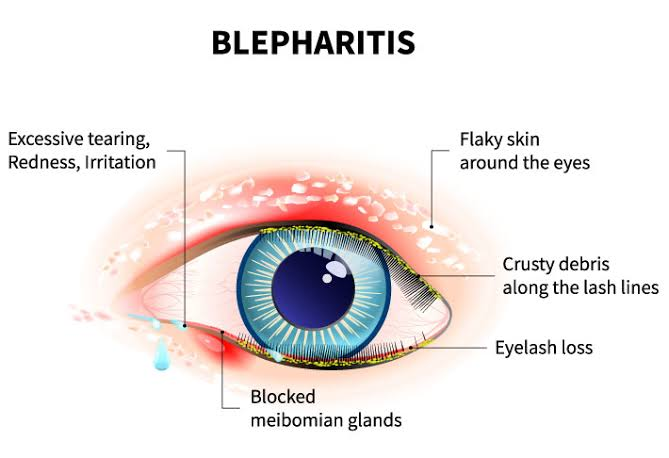
Blepharitis is an ocular condition characterized by chronic inflammation of the eyelid margin.
Inflammation of the eyelid is known as blepharitis.
Blepharitis is a common eye disorder caused by bacteria or skin conditions.
Write causes of blepharitis

Bacterial infection (staphylococcus)
Malfunctioning of oil gland in the eyelid
Allergies
Skin conditions Seborrheic dermatitis, Rosacea
Dandruff on scalp
Environmental Factors
Hormonal factor
Write clinical manifestations of blepharitis
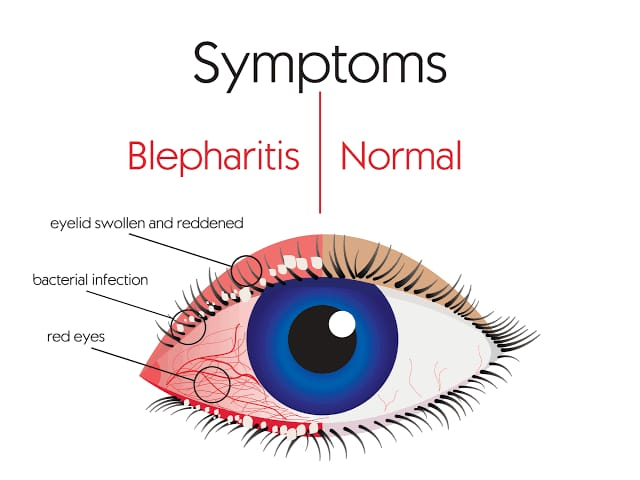
Red, Swelon Eyelid
Crusty or greasy eyelids
Red Eye
Itching and irritation in eye
Flaking or scaling around eyelashes
Gritty, burning and stinging sensation in eye
Sensitivity to light
Watery ice
Blurred vision
Loss of eyelids
Write diagnostic evaluation of blepharitis.
History Collection
Physical Examination
Slit lamp examination
Culture and sensitivity test
Write management of blepharitis
Eyelid hygiene, warm compresses, and certain medications are used for the management of blepharitis.
Eyelid hygiene: Clean the eyelids in a regular manner to manage blepharitis. To clean the eyelids, add a mild cleanser (like baby shampoo) to warm water and gently scrub the eyelids to remove debris and crusts.
Lead massage: Gently massaging the eyelids to remove the blockage in the oil gland and improve the oil flow.
Warm compresses: Applying warm compresses to the eye (5-10 minutes) loosens debris and crusts and improves circulation to the eyelids. Use a clean warmcloth for warm compresses.
Medication: Use of antibiotic ointment and steroid eye drops to reduce inflammation and control bacterial overgrowth.
Avoid eye makeup: Avoid eye makeup to prevent eye irritation and block oil glands.
- Define stye

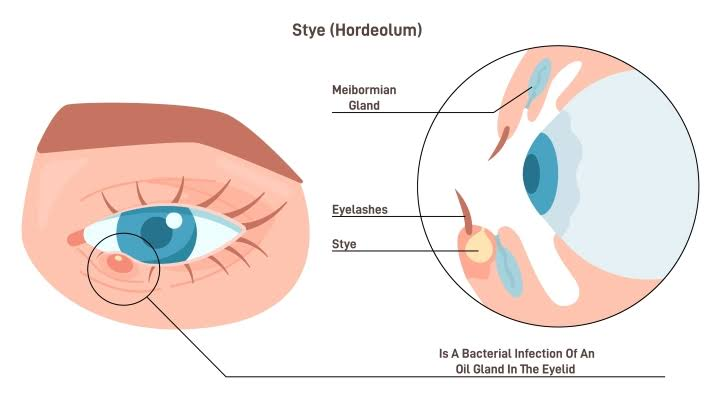
A stye is also known as a ‘hordeolum’.
A stye is a small, red painful bump on the eyelid. Write causes of stye
Stye is mainly caused by the bacterial infection Staphylococcus aureus. Apart from this it is seen due to the following factors.
Pur Eyelid Hygiene
stress
Hormonal changes
Pur nutrition
Using contaminated razor Write clinical manifestations of stye
Redness and swelling on the eyelid
Tenderness and pain in the affected area
Small pus-filled bump on the eyelid
Heaviness in eyelid
Watery ice
Sensitivity to light
Feeling Something in I
Discomfort in eye Write diagnostic evaluation of stye
History Collection
Physical Examination
Blood test
Culture and sensitivity test
Write management of stye
Warm compresses: Apply warm compresses on the affected eyelid for 10 to 15 minutes. It reduces pain and swelling and improves the drainage system.
Good eyelid hygiene-Good eyelid hygiene: Maintaining hygiene of the eyelid and avoiding frequent touching and rubbing of the affected area.
Antibiotic ointment: Antibiotic ointment and eye drops are used to treat bacterial infections.
Pain relief: Use over the counter medicines ibuprofen and acetaminophen to relieve pain.
Avoiding contact lenses and eye makeup-Avoiding contact lenses and eye makeup: Avoiding contact lenses and eye makeup until the stye heals.
Avoiding quizzing and popping: Avoiding quizzing or popping Stine. Because picking the sting spreads the infection.
Write prevention of stye
Maintaining good hygiene.
Do not touch the eyes frequently.
Wash hands before touching eyes.
Remove eye makeup before going to bed.
Avoid sharing eye makeup.
Use a clean towel.
Maintaining a healthy life style.
Avoiding stress.
Define chalazion

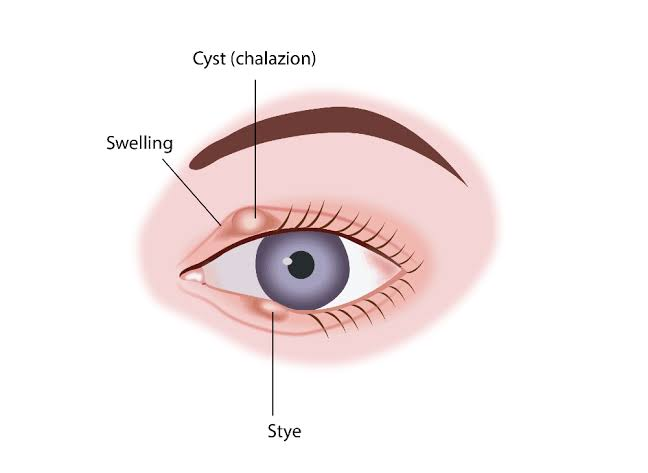
A chalazion is a small painless bump that develops on the eyelid due to a blocked meibomian gland.
A small painless bump on the eyelid is known as a chalazion.
Chalazines are also known as “eyelid cysts” because they develop on the eyelids. Also chalazion is seen due to meibomian gland blockage hence it is also known as “Meibomian cyst”.
Chalazines are mainly seen between the ages of 30 and 50 years. Write causes of chalazion
Chalazines are caused by blockage of the meibomian glands and oil glands in the eyelid. Blockage of this oil gland is seen due to the following reasons.
Bacterial infection
Chronic blepharitis
Rosacea
Seborrhoea
Meibomian gland dysfunction
Write clinical manifestations of chalazion
Small painless bump or lump on the eyelid (upper & lower eyelid)
Tenderness or swelling around the affected area
Redness or irritation in the eyelid
Blurred vision
Sensation of pressure and heaviness in the eyelid
If it is infected, it will be painful.
Write diagnostic evaluation of chalazion
History Collection
Physical Examination
Sleet lamp examination
Optical Coherence Tomography
Biopsy
Write management of chalazion
Warm compresses: Apply warm compresses on the affected eyelid. This oil softens the gland and promotes drainage as well as reduces inflammation.
Eyelid massage: Gently massage the eyelid area around the chalazion. Which helps to drain the blocked gland.
Topical medication: Antibiotic and corticosteroid ointment and eye drops are administered as topical medicine. Which prevents secondary infection and reduces inflammation.
Steroid injection: In cases with larger chalazines, corticosteroid injections are injected directly into the chalazines. which reduces inflammation and promotes resolution.
Incision and drainage: Surgical procedure incision and drainage is performed when conservative treatment fails to resolve the chalazion. In which local anesthesia is administered in the affected area and a small incision is made there and the blocked contents are drained.
Excision: Surgical excision is performed in rare cases when other treatments fail to treat the chalazion. In which the entire part of the chalazion is removed.
Define antropion
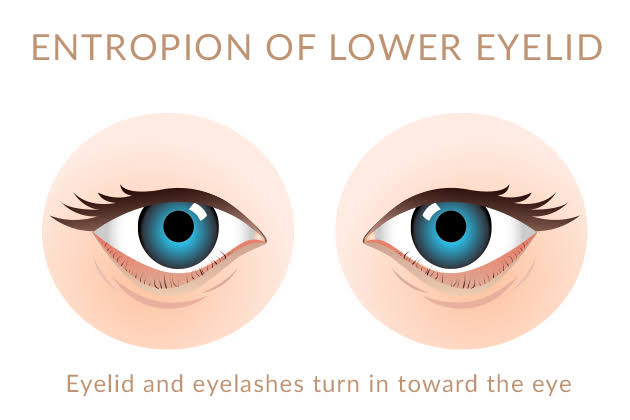
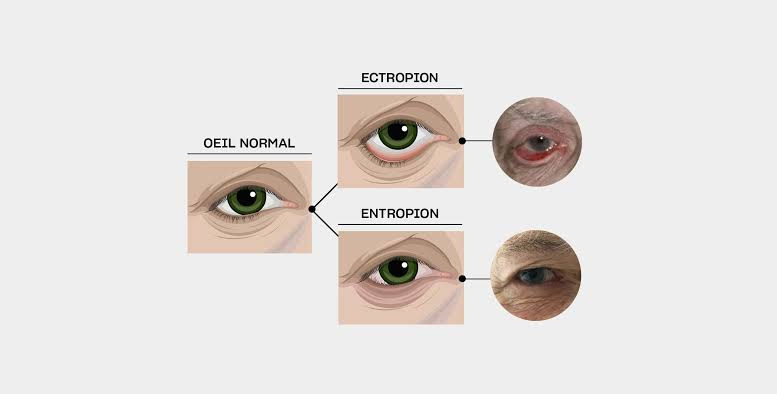
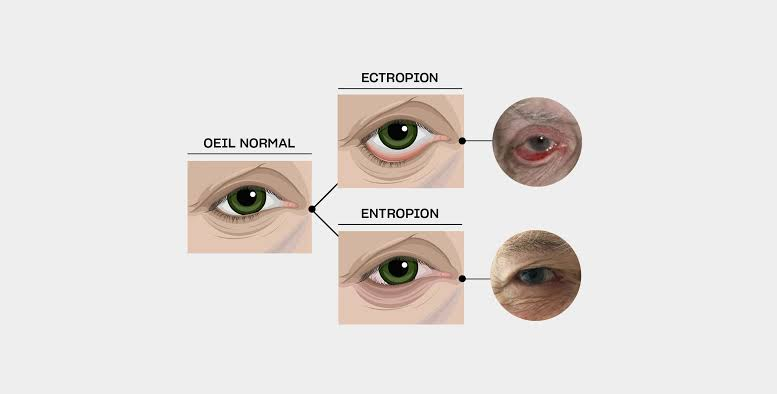
In entropion the eyelid margin is rolled inward.
Entropion is a medical condition in which the eyelid usually turns downward, inward, causing the eyelid and the underlying skin to rub against the eye surface. Write causes of antropion
Entropy is observed due to variance factor. Which are as follows.
Age Related Changes in the Eyelid Tissue
Scarring or trauma to the eyelid
Genetic predisposition
Inflammation or infection of the eyelid
Neurological conditions that affect the eyelid
Chronic eye conditions (blepharitis, chronic conjunctivitis)
Previous Eyelid Surgery Write types of entropion (Write types of entropion)
Congenital entropion: Congenital entropion is an air condition that is seen by birth.
Involutional Entropion / Senile Entropion: Involutional entropion is the most common type that occurs due to age related changes in the eyelid tissue. Involutional entropion primarily affects the lower eyelid.
Cicatricial entropion: Cicatricial entropion occurs due to the development of scar tissue on the eyelid margin.
Spastic entropion: The eyelid turns inward due to spasm in the muscles of the eyelid margin. Write clinical manifestations of entropion
Eye irritation
Eye pain
Redness in eyes
Epiphora (Watery Ice)
Foreign body sensation in eye
Photo phobia
Corneal damage Write management of entropion
Conservative major as well as surgical intervention are used for the management of entropion.
A conservative major
Lubricating eyedrops and ointments – Lubricating eyedrops and ointments: Lubricating eyedrops and ointments smooth the cornea and relieve discomfort.
Tape or adhesive strip: Tape or adhesive strip is applied on the eyelid. which provides temporary support to the lead and prevents inward turning.
Botox injection: In some cases, Botox (botulinum toxin) injection is administered in the muscles around the eye which causes a temporary week of massage and the eyelid relaxes so that the eyelid returns to its original position.
Surgical intervention:
Surgical intervention is the treatment of choice as conservative measures provide temporary relief. Several surgical methods are used for the treatment of entropion. Which surgical method to use depends on the entropion’s cause and anatomy.
Eyelid tightening: In eyelid tightening, the muscles and tissue of the eyelid are tightened and brought to its normal position.
Tarsorrhaphy: In severe cases when other surgical procedures are not possible or effective, the eyelids are partially sutured together to relieve symptoms and protect the cornea.
Wheeler’s Operation: Wheeler’s operation is mainly used to correct the lower eyelid. In which a segment of the lower eyelid is cut due to which the eyelid becomes short and the tissue there is tightened.
Define Ectropion
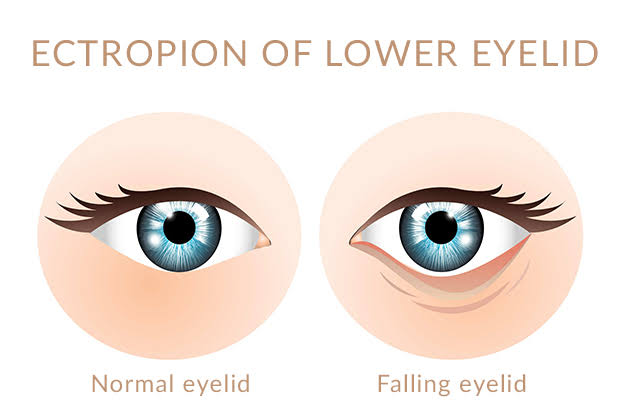
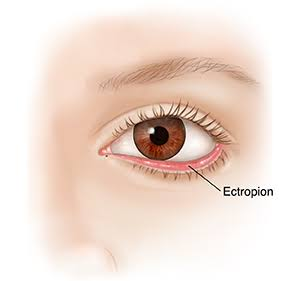
Ectropion mainly affects the lower eyelid. Write causes of ectropion
Age Related Changes-Age Related Changes
Facial nerve palsy
Scaring – Scaring
Eyelid luxury
Eyelid tumor-eyelid tumor
Sun damage
Previous Eyelid Surgery Write types of ectropion (Write types of ectropion)
Congenital ectropion: Congenital ectropion is rare. In which abnormality is seen in the eyelid at the time of birth.
Involutional Ectropion / Senile Ectropion– Involutional Ectropion / Senile Ectropion : This is the most common type which is seen due to age related changes in the eyelid tissue.
Spastic ectropion: Spastic ectropion occurs due to spasm in the orbicularis muscles.
Cicatricial ectropion: Occurs due to the development of scar tissue near the eyelid margin. This scar tissue occurs due to trauma, injury.
Paralytic ectropion: Paralytic ectropion occurs due to paralysis of the orbicularis muscles.
Mechanical ectropion: Mechanical ectropion occurs due to mechanical factors such as tumors, masses, and facial paralysis that result in outward turning. Write clinical manifestations of entropion
Eyelid turning outward
Redness and irritation
Excessive tearing (epiphora)
Foreign body sensation
Blurry vision
Eyeless irritation Write management of ectropion
A conservative major
Lubricating eyedrops and ointments: Lubricating eyedrops and ointments smooth the cornea and relieve discomfort.
Tape or adhesive strip: A tape or adhesive strip is applied to the eyelid to temporarily support the lead and prevent it from turning outward.
Botox injection: In some cases, Botox (botulinum toxin) injection is administered in the muscles around the eye which causes a temporary week of massage and the eyelid relaxes so that the eyelid returns to its original position.
Eyelid tightening: In eyelid tightening, the muscles and tissue of the eyelid are tightened and brought to its normal position.
Tarsorrhaphy: In severe cases when other surgical procedures are not possible or effective, the eyelids are partially sutured together to relieve symptoms and protect the cornea.
Wheeler’s Operation: Wheeler’s operation is mainly used to correct the lower eyelid. In which a segment of the lower eyelid is cut due to which the eyelid becomes short and the tissue there is tightened.
Dacryocystitis:-
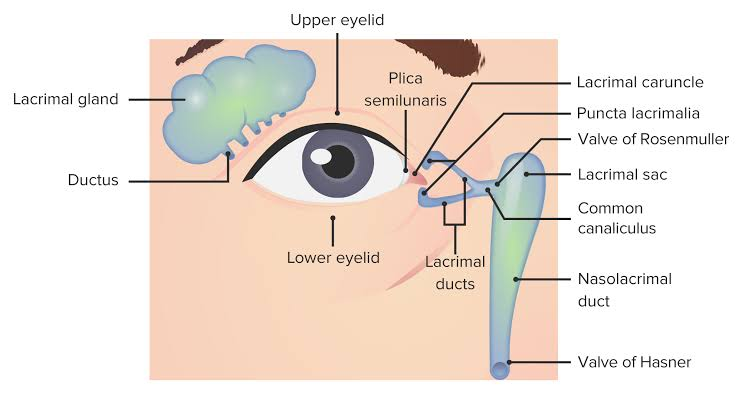

Write causes of dacryocystitis
Dacryocystitis is mainly due to nasolacrimal duct narrowing or blockage.
Obstruction in nasolacrimal duct
Bacterial and viral infection to the duct
Injury around the duct
Tumor around the duct
Inflammatory condition Write sign and symptoms seen in dacryocystitis
Excessive tearing (watery ice)
Pain and tenderness
Discharge from the affected eye
Crusting on the eye lead
Blurred vision
Fever Write diagnostic evaluation of dacryocystitis
History Collection
Physical Examination
Fluorescein dye test
Dacryocystography
Nasal endoscopy
Diagnostic nasolacrimal irrigation
Blood test
Culture and sensitivity test
Write management of dacryocystitis
Antibiotic therapy: Providing antibiotic medicine to treat underlying infection.
Warm compresses and massage: Apply warm compresses to the affected area and gently massage the area to promote drainage.
Nasolacrimal Duct Irrigation: Flushing the tear duct with a saline solution that clears the obstruction and improves drainage.
Topical steroid: Use topical steroid eye drops to reduce swelling and inflammation. Surgical management
Dacryocystorhinostomy (DCR): In a dacryocystorhinostomy, a new drainage pathway is created and the blocked portion of the tear duct is bypassed.
Balloon Dilation: A balloon catheter is used in some cases. The balloon catheter is inserted through a narrow portion of the tear duct and the balloon is dilated to widen the area and improve drainage.
Probing and Irrigation: Probing and irrigation is done in cases of congenital dacryocystitis. This involves gentle probing and irrigation of the tear duct under general anesthesia to clear the obstruction.
Define trachoma
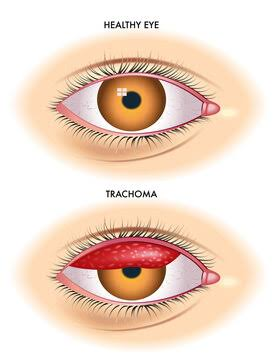
Trachoma is a contagious bacterial eye infection. It is caused by a bacterium called Chlamydia trachomatis.
Trachoma is the world’s leading cause of infectious blindness.
Trachoma is spread by direct contact with the eye, nose and throat secretions of an infected person. Write clinical manifestations of trachoma
Cloudy cornea
Blurred vision
Corneal scarring
Discharge from the eye
Sensitivity to light
Eye pain
Itching and irritation
Swallowing in the Eyelid
Illesis Abnormality (Illesis Turned Inward)
Write diagnostic evaluation of trachoma
History Collection
Physical Examination
Swab test
Visual acuity testing
Photography
Blood test
Culture and Suncity Test
Write management of trachoma
The SAFE strategy for the treatment of trachoma is given by WHO which is as follows:
S: Surgery: In cases with advanced trachoma, surgery is performed to correct trachomatous trichiasis (iliacs turned inward) if present. Hence blindness and visual impairment can be prevented.
A : Antibiotic : Using antibiotic medicine to treat bacterial infection. For example azithromycin and tetracycline
F : Facial Cleanliness : Promoting facial cleanliness especially in children, which minimizes bacterial transmission. Anchoring to face washing with regular soap and water.
E : Environmental Improvement : To implement environmental measures like clean water supply, sanitation. Improving the environment can prevent bacterial transmission.
Define pterygium
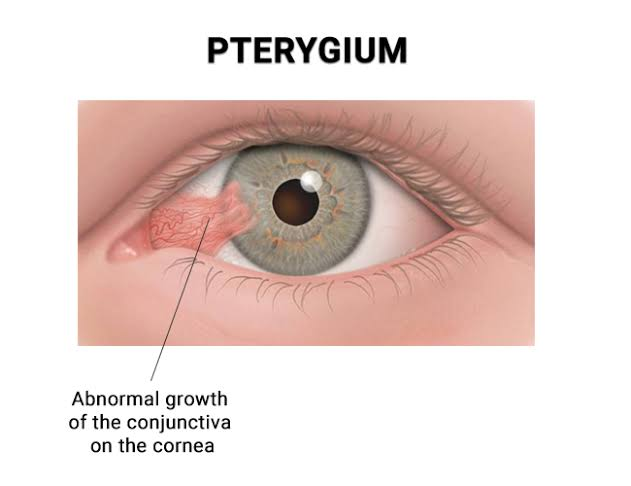

Pterygium is known as another ‘eye web’ and ‘surfer’s eye’.
A pterygium is a noncancerous triangular growth on the conjunctiva and the growth is seen spreading to the cornea.
In pterygium one or both eyes are affected. Write causes of pterygium
The exact cause of pterygium is unknown. But the factors to cause pterygium are as follows.
Exposure to UV light
Exposure to dust, wind
Environmental Factors
Dry eye
Chronic irritation Write clinical manifestation of pterygium
Pink and flaky tissue develop on conjunctiva
Redness and inflammation
Irritation or gritty sensation
Blurred vision
Dryness or excessive tearing Write diagnostic evaluation of pterygium
History Collection
Physical Examination
Visual examination
Visual acuity test
Fluorescein staining
Write management of pterygium
Non surgical management:
Use lubricating eye drops to relieve dryness and irritation.
Using corticosteroid eye drops to reduce inflammation. Surgical Management:
If the pterygium causes vision problems or discomfort, remove it. Pterygium is removed by placing excision