ENGLISH Unit-12-neurological Disorder(deepali)(part-5)
1) Explain/Define Spinal cord injury

The spinal cord is a part of the brain that works to control the body.
Spinal cord injury is a condition in which trauma to the spinal cord occurs and the spinal cord
This damage causes loss of sensation and reduced mobility.
When there is a sudden trauma to the spinal cord, the function of the spinal cord is temporarily and permanently changed.
When the spinal cord is injured, the spinal cord can be fractured or the vertebrae in the spinal cord can also be dislocated, this condition is called spinal cord injury.
Explain the etiology/cause of the spinal cord injury. (Give reasons for spinal cord injury)
Due to trauma.
Due to fall down.
Due to gun shot.
Road Traffic Accident (R.T.A.).
due to infection.
Due to inflammation in the spinal cord.
Due to tumor in spinal cord.
Ex:=
Meningiomas,(Meningiomas,)
Ependymomas, (Ependymomas,)
Asrocytomas,
Due to falling from a great height.
Due to electric shock.
Due to motor vehicle accident.
due to ischemia.
Due to develop mental disorder.
Due to neurodegenerative diseases.
Due to multiple sclerosis.
Because of the stroke.
Due to information.
Explain the classification of the spinal cord injury. (State the classification of spinal cord injury.)
A) Indicate Complete :=
In complete spinal cord injury, motor and sensory function is not preserved and there is involvement of sacral segment S4 and S5.
B) indicates incomplete:
In incomplete spinal cord injury below the neurological level only the sensory function is preserved, motor function is not preserved and the sacral segment is not preserved.
S4 and S5 are involved.
C) indicates incomplete:
In this incomplete spinal cord injury, only motor function is preserved below the neurological level.
D) indicate incomplete:
In this incomplete spinal cord injury, only motor function is preserved below the neurological level and only half of the key muscles are below the neurological level whose muscle grade is 3 or more.
E) indicates Normal:
Mainly sensory and motor score is normal in this. Mainly spinal cord injury but motor and sensory function is normal.
Explain the clinical manifestation / sign and symptoms of the patient with the spinal cord injury. (State the symptoms and signs of spinal cord injury.)
Paralysis.
Loss of sensation.
Breathing difficulty.
Changes in bowel and bladder function.
Loss of limb movement.
Difficulty in walking.
Symptoms mainly depend on the injury to the spinal region.
1) Cervical (Neck) injury:=
Affect the arm, legs and middle part of the body. (Affects arms, legs and mid-body.)
Breathing difficulty.
Loss of normal bowel and bladder control.
Numbness.
Sensory change. (Sense change.)
Spasticity (increased muscle tone). Spasticity (increased muscle tone).
2) Thoracic / chest level / injury. (Thoracic / chest level / injury.)
Loss of normal bowel and bladder control.
Numbness.
Sensory changes occur.
Spasticity (increased muscle tone).
weakness.
Paralysis.
3) Lumber Sacral (Lower back injury)
Loss of normal bowel and bladder control.
Numbness. (Inaction ensues.)
pain. (pain)
Sensory change. (Sense change.)
Coming to Wickness.
becoming paralyzed.
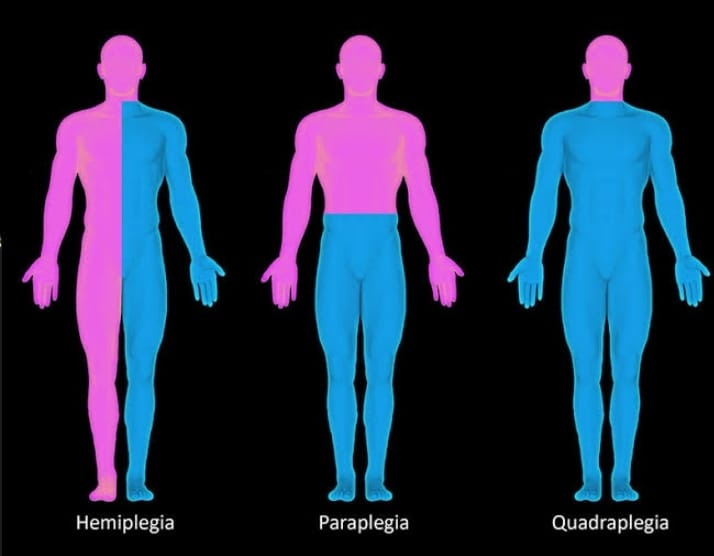
Explain the types of the spinal cord injury. (State the type of spinal cord injury.)
There are two main types of spinal cord injuries. (There are two main types of spinal cord injuries.)
1) Complete,
2) Incomplete
1) Complete Spinal cord injury has three types.
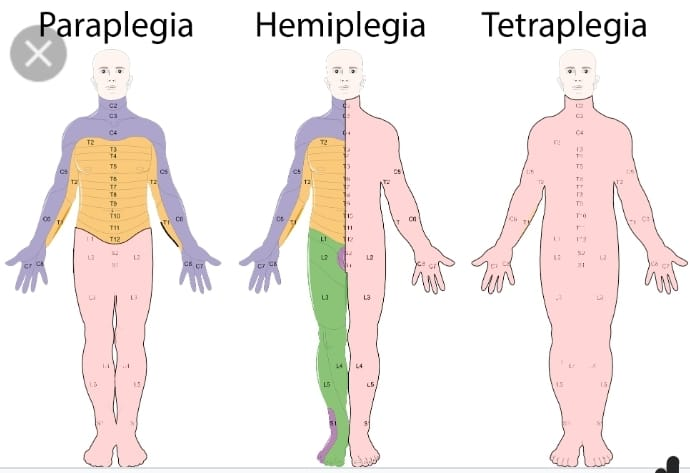
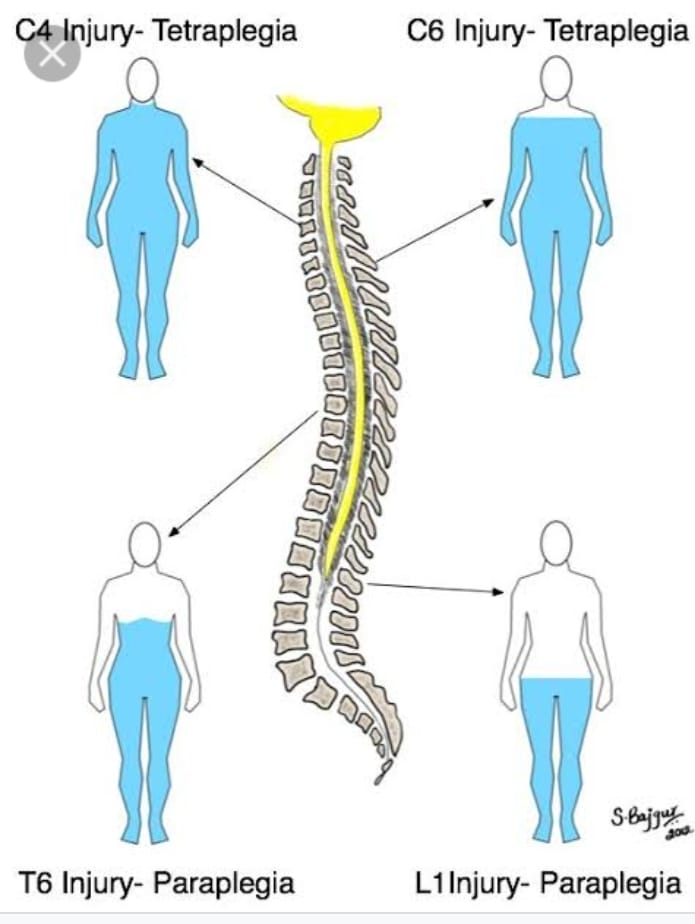
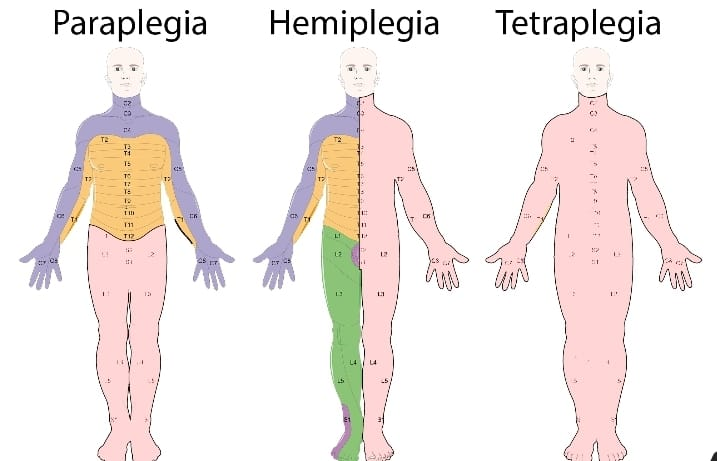
A) Paraplegia Paraplegia is mainly caused by injuries from T1-L5.
In it, the upper body can function fully but the impairment is mainly seen in the lower leg.
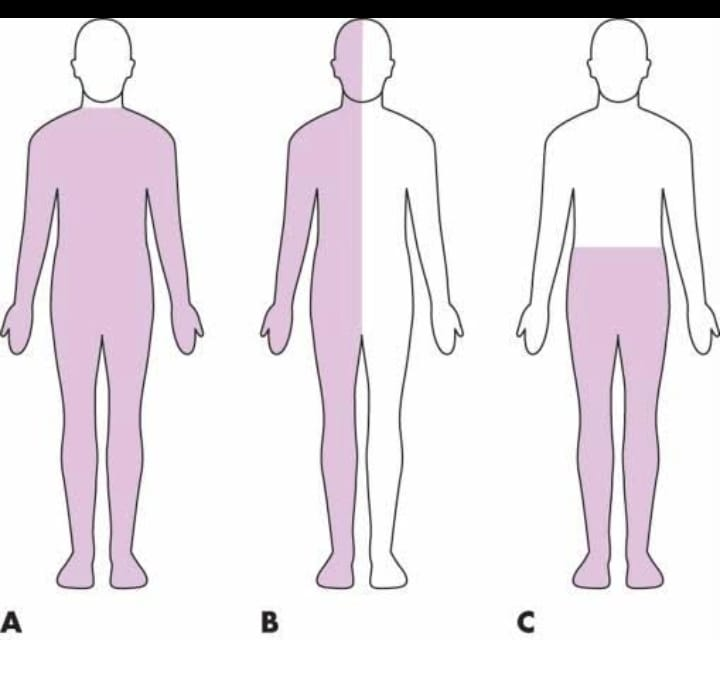
B) Hemiplegia Hemiplegia results in half body paralysis.
C) Quadriplegia Quadriplegia is also called tetraplegia.
In quadriplegia there is involvement of upper two limbs and lower limbs
2) Incomplete (incomplete) spinal cord injury again has 3 types.
A) Central cord syndrome
Cause := This is mainly due to injury and edema in cervical area and cervical lesion.
Characteristic:=
Motor deficit is seen in the upper extremities. Sensory loss varies in the upper extremities.
B) Anterior cord syndrome
Cause: This is mainly due to injury and lesion in the anterior spinal artery.
Characteristic:=
Loss of pain,
Temperature increase. (Increase in temperature.)
Impaired motor and sensory function.
poor prognosis. (Bad prognosis.)
C) Broed Sequard syndrome
Cause:=
In this the lesion is mainly due to transverse hemisection of the cord. A mainly
Because of Naif,
Caused by a missile injury, fracture.
Characteristic:=
Ipsilateral paralysis occurs. (Ipsilateral paralysis occurs.)
Contralateral loss of pain and temperature
Explain the diagnostic evaluation of the spinal cord injury. (State the diagnostic evaluation of spinal cord injury.)
History taking and physical examination. (History taking and physical examination.)
X ray. (X Ray.)
Ct scan. (CT scan.)
MRI. (MRI.)
CBC ( Hb, RBC, WBC. ).
Arterial blood gas analysis. (Arterial blood gas analysis.)
myelogram. (Myelogram)
Urodynamic Studies. (Urodynamic studies.)
Explain the treatment of the brain injury. (Write the treatment of brain injury.)
Respiratory management:=
Provide adequate amount of oxygen to the patient. (Provide adequate amount of oxygen to the patient.)
Provide adequate ventilatory support to the patient. (Provide adequate ventilatory support to the patient.)
Pharmacological management:=
Providing corticosteroid medication to the patient.
Ex:= Dexamethasone, Methyl prednisolone,
Immobilization:=
Provide spinal traction to the patient.
Provide special bed to the patient.
Properly perform surgery on the patient.
Explain the nursing management of patients with the nursing management.
Oxygenate the patient properly. (Oxygenate the patient properly.)
Assess the patient’s respiratory rate and depth properly.
Keeping the patient’s airway properly patent. (Keep the patient’s airway properly patent.)
Advise the patient to perform range of motion exercises. (Advising the patient to do range of motion exercises.)
To provide proper special bed to the patient..
Properly assess the patient’s skin integrity. (Assess the patient’s skin integrity properly.)
Change the patient’s position every two hours. (Position of the patient should be changed every two hours.)
Properly assess the patient’s bowel and bladder function. (Properly assess the patient’s bowel and bladder function.)
Provide adequate amount of fluid to the patient. (Provide fluid in adequate amount to the patient.)
Provide the patient with a high fiber and high protein diet. (Provide the patient with a high fiber and high protein diet.)
2) Explain / Define the Paraplegia. (Define paraplegia.)
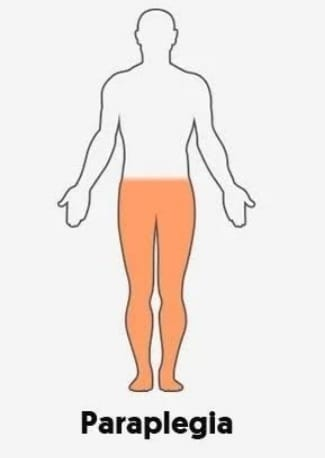
Paraplegia is a condition that mainly due to injury in the spinal cord the motor and sensory function of the lower extremities is impaired i.e. the lower extremities are paralyzed due to which the lower extremities (lower legs) cannot work properly and walking and running. This condition is called paraplegia.
Paraplegia is mainly seen due to any impairment in the thoracic, lumbar or sacral region of the spinal cord.
Explain the Etiology/cause of the Paraplegia. (Give reasons for paraplegia.)
Due to spinal injury.
due to stroke.
Due to spinal tumor.
Due to brain tumor.
due to ischemia.
Due to diabetes related new damage.
Due to spina bifida.
Due to cerebral palsy.
Due to multiple sclerosis.
Falls.
Due to accident.
Due to brain infection.
Explain the clinical manifestation / sign and symptoms of the patient with the Paraplegia. (State the symptoms and signs of a patient with paraplegia.)
Moment loss.
Loss of sensation.
Loss of bowel and bladder control.
Muscle stiffness.
tingling and burning sensation. (Tingling and burning sensation.)
Muscle spasms.
Reflexes change.
Explain the diagnostic evaluation of the patient with the Paraplegia. (State the diagnostic evaluation of a paraplegia vada patient.)
history tacking and physical examination.
Neurological examination.
imaging studies.
X ray. (X Ray.)
Ct scan.
MRI. (MRI.)
Electromyography.
Blood test (Blood test.)
Explain the medical management of the patient with Paraplegia. (State the medical management of paraplegia vada patient.)
Properly immobilize the patient’s spinal cord.
If the patient is in pain, provide analgesic medication.
Provide muscle relaxant medication to the patient.
Provide physical therapy to patients.
Provide assistive devices to patients.
Managing the patient’s bowel and bladder function.
Advising patients to prevent complications.
Advise the patient to take regular follow up.
Explain the Nursing management of patients with the Paraplegia. (State nursing management of paraplegia vada patient.)
Assess the patient’s neurological status.
Properly assess the patient’s skin integrity.
Properly assess the patient’s bowel and bladder function.
Properly assess the patient’s respiratory status.
Assess the patient’s skin care properly.
Properly assess the patient’s skin hygiene.
Advising the patient to exercise properly.
Advise the patient to exercise the bowel and bladder properly.
Provide proper respiratory support to the patient.
If the patient is in pain, provide analgesic medicine.
Provide proper psychological support to the patient.
The patient had to provide complete information about his disease, the causes of the disease, its symptoms and signs and its treatment.
Provide adequate treatment to the patient to avoid any further complications.
3) Explain/Define the Hemiplegia. (Define hemiplegia.)
Hemiplegia is a word derived from “Greek”.
Hemi means:= Half or one side of body.
Plegia means:= Paralysis or Stroke.
Hemiplegia is a condition in which total and partial paralysis of half body part occurs, which is mainly on the right side of the body or can be on the left side as well. It is caused by any illness, injury and disease in the brain and spinal cord.
(Hemiplagia Means:= Paralysis of the half part of the body.)
Explain the Classification of the Hemiplegia. (Describe the classification of hemiplegia.)
There are total five types of hemiplasia.
1) Facial hemiplegia,
2) Spinal hemiplegia,
3) contralateral hemiplegia,
4) spastic hemiplegia,
5) Alternating hemiplegia of childhood.
1) Facial hemiplegia,
Facial means related to “Face”
In this type, paralysis occurs in one side of the facial muscles.
And no half part of the facial muscles can work properly.
2) Spinal hemiplegia,
Spinal hemiplegia is called Brown Sequard syndrome. In this type, if one half side of the spinal cord is damaged, due to which one half part of the body is paralyzed, it is called spinal hemiplegia.
In this type, if the spinal cord is damaged in the right side, then the body of the right side is paralyzed and if the spinal cord is damaged in the left side, then the left body is paralyzed.
3) contralateral hemiplegia,
Contra lateral hemiplegia means opposite side paralysis.
This type of hemiplegia is mainly due to brain damage. In this type, if the right side brain is damaged, paralysis occurs in the left body and if there is damage in the left brain, paralysis occurs in the right body side.
4) spastic hemiplegia,
This is a type of hemiplegia in which the muscles of one half side of the body become spastic and contracted for a long time.
5) Alternating hemiplegia of childhood.
Alternating hemiplegia is mainly seen in children 18 months or older.
This mainly involves more than one episode of hemiplegia that affects one side of the body.
Explain the Etiology / Cause of the Hemiplegia. (Give reasons for hemiplegia.)
Due to brain injury.
Due to cerebral hemorrhage.
stroke.
Due to diabetic neuropathy.
Due to brain infection.
Due to meningitis.
Due to encephalitis.
Neoplastic (due to glioma-meningioma).
Due to congenital defect.
Due to injury to the spinal cord.
Due to demyelinating disease.
Due to brain cancer.
Due to brain tumor.
Due to neurological deodorization.
Due to psychological disorders.
Explain the clinical manifestation / sign and symptoms of the patient with the Hemiplegia. (State the symptoms and signs of Hemiplegia Vada patient.)
Muscle weakness and paralysis.
Impaired motor function.
Difficulty in walking, talking, work.
Changes in reflexes.
Difficulty in coordination.
Sensory changes occur.
Changes in posture.
Difficulty in speech and swallowing.
Emotional and psychological impact.
Loss of motor function.
Weakness and stiffness will be seen in one side of the body.
Difficulty grasping any object.
Explain the diagnostic evaluation of the patient with the Hemiplegia. (Give diagnostic evaluation of hemiplegia vada patient.)
History taking and physical examination
Blood test.
CT scan.
MRI.
Electromyography.
Electroencephalography.
Cerebral angiography.
Explain the medical management of the patient with Hemiplegia. (State the medical management of hemiplegiawada patient.)
Properly treat the patient due to which the condition of hemiplegia has arisen.
If the patient has a condition of hemiplegia due to any infection, provide antibiotic medication.
Ex:=
Amoxicillin,
Flucloxacillin.
Antiviral medicine should be provided to the patient if he has any viral infection.
Ex:=
Acyclovir,
Fumciclovir.
Provide anticoagulant medication if the patient has any coagulation disorder.
Ex:=
Warfarin,
Heparin.
If the patient has any plasmotic disorder, provide antispasmodic medicine to the patient.
Ex:=
Dicyclomine,
Bellaclonma.
Provide Chemotherapy drug to the patient properly.
To provide proper rehabilitation therapy to the patient.
To properly provide physical therapy, occupational therapy, psycho therapy, to the patient.
Explain the nursing management of patients with Hemiplegia. (State the nursing management of a hemiplegia patient.)
Provide proper ortho static splints like splint, cast, braces to the patient.
If the patient’s muscles are overactive, provide Botox injection to the muscles.
Provide walker, wheelchair to patient.
Provide analgesic medicine for patient pain management.
Assess the patient for any other complications or not.
Provide proper nutritional support to the patient.
Provide proper psychological support to the patient.
Provide proper medication to the patient.
Advising the patient for proper range of motion exercises.
Assess the patient properly whether there is any side effect or not.
4) Explain/Define the Quadriplegia. (Define quadriplegia.)
Quadriplegia is also called tetraplegia.
In quadriplegia there is impairment and paralysis in motor and sensory function in four i.e. Upper Extremities (Hand), Lower Extremities (foot) and trunk.
Explain the Etiology/cause of the Quadriplegia. (State the cause of quadriplegia.)
Due to spinal cord damage.
Due to traumatic injury.
Falls from the hight.
Due to spinal cord injury.
Due to motor vehicle accident.
Due to certain types of medicine.
Due to lack of blood supply.
Due to neurological disorders.
All due to injuries.
Due to an autoimmune disorder.
Due to cerebral palsy.
Spinal bifida ( Spina bifida).
Explain the types of the Quadriplegia. (State the type of quadriplegia.)
There are two types of quadriplegia.
1) Complete Quadriplagia (Complete Quadriplegia),
2) Incomplete Quadriplagia
1) Complete Quadriplagia (Complete Quadriplegia),
In complete quadriplegia, motor and sensory functions are totally lost. And the person’s voluntary muscle control is impaired. And a person who has total loss of sensation in the lower limb and upper limb is called complete quadriplegia.
2) Incomplete Quadriplagia
In incomplete quadriplegia, a person’s motor and sensory functions are partially impaired.
In complete quadriplegia the person has little voluntary muscle control and the person also has some sensation. A person with a small amount of muscle control is called incomplete quadriplegia.
Explain the clinical manifestation / sign and symptoms of the patient with the quadriplegia. (State the symptoms of quadriplegia vada patient.)
Loss of motor function.
Loss of sensory function.
Spasticity, muscle stiffness.
Absence of involuntary muscle spasms.
Impaired muscle reflex.
Respiratory complications.
Impaired balance and coordination.
Loss of bowel and bladder function.
Emotional and psychological problems.
Pressure ulcers develop.
Muscle stiffness.
Difficulty in walking.
Loss of bladder control.
Tingling and Numbness.
Loss of momentum.
Loss of sensation.
Autonomic dysreflexia occurs.
Explain the diagnostic evaluation of the patient with the quadriplegia. (State the diagnostic evaluation of a quadriplegia Vada patient.)
history taking and physical examination.
Neurological examination.
Imaging studies.
X rays.
Ct scan.
MRI.
Electromyography (EMG).
Laboratory test.
Urodynamic testing.
Autonomic function testing.
Blood test.
Lumbar puncture.
Explain the medical management of the patient with the Quadriplegia. (State the medical management of a patient with quadriplegia.)
Provide oxygen to the patient properly.
Provide proper anti-inflammatory drug to the patient.
Accurately administering cold saline to the patient.
Immobilize the patient properly.
Properly stabilize the patient if he has sustained any spinal cord injury.
If the patient is in pain, provide analgesic medicine.
If the patient has any infection then provide antibiotic medicine.
Provide proper skin care to the patient to prevent pressure ulcers from developing.
Provide proper nutritional support to the patient.
To provide proper orthopedic care to the patient.
To provide proper rehabilitation services to patients.
Provide proper psychological support to the patient.
Explain the Nursing management of patients with the Quadriplegia. (State nursing management of quadriplegia vada patient.)
Properly assess the patient.
Providing proper skin care to the patient.
Provide proper respiratory support to the patient.
Assessing the patient’s proper bowel and bladder function.
Provide properly assistive devices to Tisant.
Provide analgesic medicine to the patient for pain management.
Providing proper psychological support to the patient.
Provide proper education to the patient.
Advising the patient to exercise properly.
To provide proper work and comfortable environment to the patient
5)Explain/ Define Meningitis.
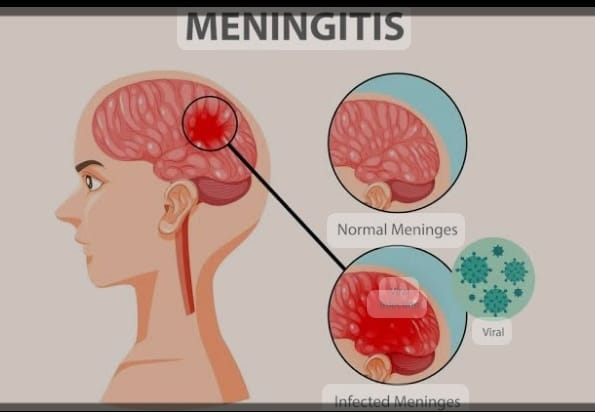
Define meningitis.
Meningies:= Meninges is the protective membrane of the brain and spinal cord that covers the brain and spinal cord.
There are three other 3 layers in this meninges.
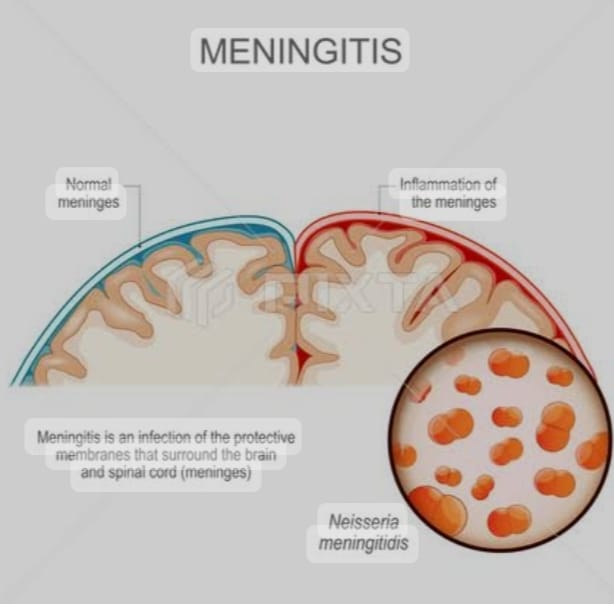
1) Duramater (outer most layer),
2) Arachnoid mater (intermidiate layer),
3) Pia Mater (Innermost layer)
Thus, there are three layers of meninges that cover and protect the brain and spinal cord.
Meningitis: If there is infection and inflammation in the meninges layer surrounding the brain and spinal cord, the condition is called meningitis. This infection can be caused by bacteria, viruses, and microorganisms.
{ Meningitis:= infection and inflammation of the Meningies layer that should be covered to the brain and Spinal cord }
Explain the etiology/cause of the meningitis. (State the cause of meningitis.)
Due to bacterial infection.
Ex:=
Mycobacterium Tuberculosis,
Streptococcus pneumoniae,
Neisseria meningitidis,
Haemophilus influenzae,
Listeria monocytogenes.
Due to viral infection.
mumps,
Herpes simplex virus,
Epstein barr viral,
Varicella-zoster viral,
Measles,
Influenza.
Due to fungal infection.
Candida, due to systemic lupus erythematosus (SLE),
Due to certain types of medication.
Due to head injury.
Due to trauma in the head and spinal cord.
Cancer.
due to tobacco use.
Due to impaired immune system.
Due to over crowding.
Due to brain surgery.
Explain the clinical manifestation / sign and symptoms of the patient with the Meningitis. (State the symptoms and signs of meningitis.)
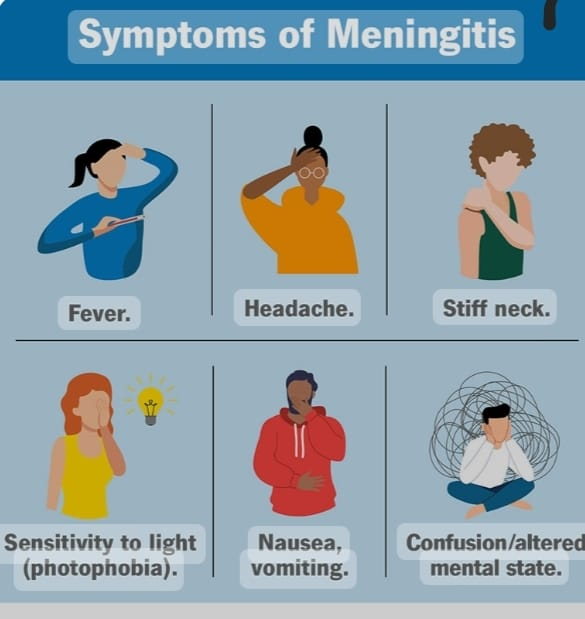
Headache,
very high fever,
Alteration of maintain status.
Confusion.
Altered consciousness.
Vomiting.
Photophobia (An inability to tolerate light).
Irritability.
Drowsiness.
Confusion.
Altered Consciousness.
Vomiting.
Sign of meningeal irritation.
Nuchal rigidity (Neck Stiffness).
headache.
Altered mental status.
to be startled
Joint pain.
Muscle ache.
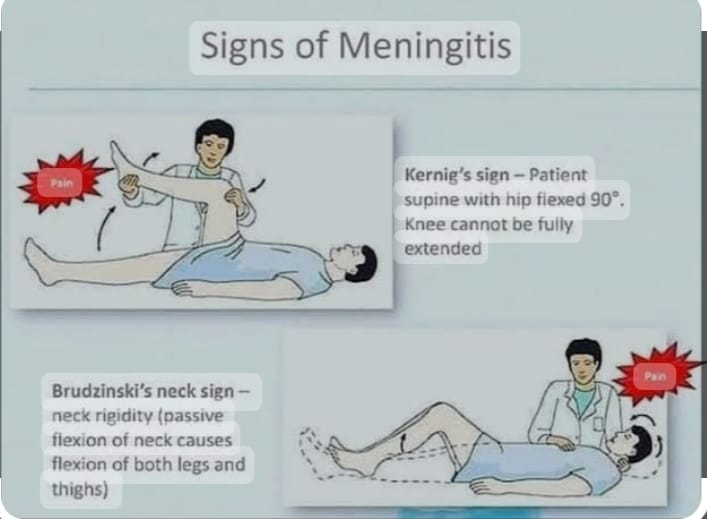
Positive Brudzinski Sign:=
Brudzinski’s sign When the patient is placed in the supine position and his neck is flexed towards the chest, his hip and ankle are automatically flexed, this is called Brudzinski’s sign.

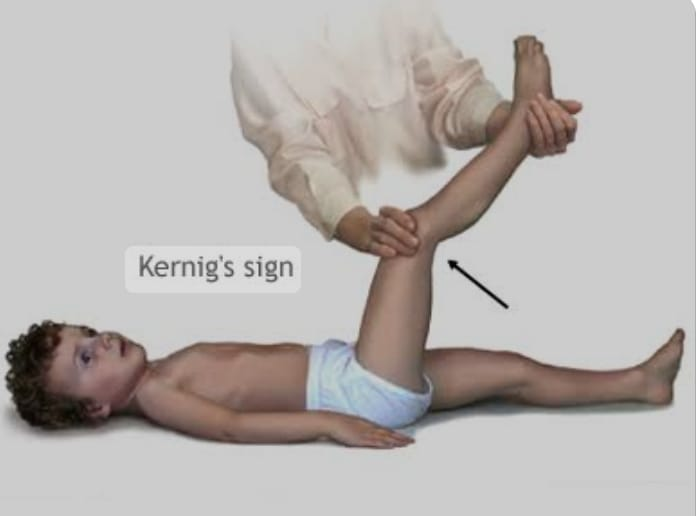
Kerning sign:= (kerning sign)
In the kerning sign, when the patient is provided with supine position and then the patient’s knee and hip are flexed, if the patient’s knee is again extended, it is called kerning sign.
K:= Knee,
E:= Extent
R:= Resistance
That is, directly extending the knee causes pain to the patient.
Explain the diagnostic evaluation of the patient with Meningitis. (State the diagnostic evaluation of a patient with meningitis.)
History taking and physical examination.
Blood culture.
Lumbar puncture.
Chest x-ray.
CSF examination.
ct scan.
Gram stain.
CSF culture.
MRI test.
Explain the management of the patient with Meningitis. (State the management of a patient with meningitis.)
Provide antibiotic medicine if the patient has any bacterial infection.
Ex:=
Rifampicin,
Cefotaxime,
Vancomycin.
Provide antiviral medicine if the patient has any viral infection.
If the patient is in pain, provide analgesic medicine.
Ex:= Acetaminophen, NSAID (Non steroidal anti inflammatory drug).
Provide intravenous fluid to the patient.
If the patient has fever, then give antipyretic medicine.
If the patient has fever, provide anticonvulsant medication.
Continuous close monitoring of the patient.
Continuously close monitoring of patient’s vital signs.
If the patient has inflammation, provide corticosteroid medicine.
If the patient has the condition of meningitis, keep him properly isolated.
Properly monitor patient’s hydration status.
Provide proper nutritional support to the patient.
Provide proper intravenous fluid to the patient.
Explain the nursing management of patients with Meningitis. State the nursing management of a patient with meningitis.
Properly assess the patient.
To continuously monitor the patient’s vital signs.
Properly assess the patient’s hydration status.
Maintain proper fluid and electrolyte levels of the patient.
If the patient is in pain, provide analgesic medicine.
Properly assess the neurological status of the patient.
If the patient has seizures, provide anti-convulsion medicine.
Provide proper nutritional support to the patient.
Providing proper psychological support to the patient.
To provide proper education to the patient about his disease, its causes, and its symptoms and signs.
Continuously monitor the patient’s intake output.
Continuous monitoring of patient’s vital signs and neurological status.
Continuously monitor the patient’s level of consciousness.
Advising the patient to take medicine regularly.
Advising the patient to follow up regularly.
Provide proper psychological support to the patient.
6) Define/Explain Encephalitis. (Define encephalitis.)
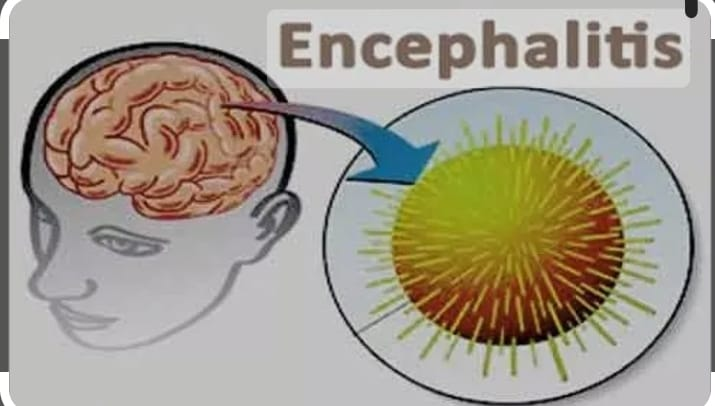
If there is infection and inflammation in the brain, the condition is called encephalitis. Encephalitis is a condition that causes infection and inflammation in the white and gray matter of the brain and mainly affects the cerebrum, brain stem and cerebellum.
Encephalitis is caused by any viral infection, bacterial infection and allergic condition.
The condition of encephalitis is mainly seen in young age and old age people.
Explain the Etiology/cause of the patient with Encephalitis. (Give reasons for encephalitis.)
Caused by bacteria.
Ex:=
Mycobacterium Tuberculosis,
Streptococcus,
Due to viral infection.
Ex:=
Due to herpes simplex virus,
Epstein Barr
Due to virus,
Varicellazoster
Due to virus,
Due to enterovirus
(polio virus and coxsackie virus),
Arab virus
for this reason,
Arthropod – Bony virus,
tick-borne virus,
Mumps, Measles and Rubella (MMR)
Rabies viral.
Due to parasitic infection.
•Ex:=
•Roundworm,
- Cysticercosis,
Toxoplasmosis.
Due to a weakened immune system.
Due to fungal infection.
Ex:=
Aspergillus Species,
Cryptococcus neoformans,
Due to autoimmune diseases,
Due to any allergic conditions.
Explain the types of Encephalitis. (State the type of encephalitis.)
There are total six types of encephalitis.
1) infectious encephalitis,
2) Postinfectious encephalitis,
3) Autoimmune encephalitis,
4) Japanese encephalitis,
5) Allergic encephalitis,
6) Chronic encephalitis
A) Subacute sclerosing panencephalitis
B) Progressive Multifocal Leukodystrophy (PML)
1) infectious encephalitis,
Infectious encephalitis is any type of infection
caused by The condition of infectious encephalitis arises due to microorganisms like bacteria, viruses, fungal parasites etc.
2) Postinfectious encephalitis,
Postinfectious encephalitis The condition of infectious encephalitis occurs two to three weeks after the initial infection. Postinfectious encephalitis is also seen as a complication of vaccination of any viral infection.
3) Autoimmune encephalitis,
In autoimmune encephalitis, if our body’s own immune system damages our brain, it is called autoimmune encephalitis. In this condition, the antibody of our body crosses the blood brain barrier and then damages the brain tissues and causes encephalitis.
Called autoimmune encephalitis.
4) Japanese encephalitis,
Japanese encephalitis is mainly spread by mosquitoes. This condition is mainly found in south, east, Asia, the far east and the Pacific island. And this condition is more common among people who do farming.
5) Allergic encephalitis,
Allergic encephalitis is mainly caused by any allergic reaction.
6) Chronic encephalitis
Chronic encephalitis develops slowly and gradually over several months. If the condition of encephalitis persists for a long period of time, it is called chronic encephalitis.
The condition of chronic encephalitis is mainly seen in patients with HIV when the immunity is down.
There are two other types of chronic encephalitis.
A) Subacute sclerosing panencephalitis
Subacute sclerosing panencephalitis is an inflammatory complication of measles infection.
B) Progressive Multifocal Leukodystrophy (PML)
Progressive multifocal leukodystrophy (PML) is mainly caused by John Cunningham viral (JC viral) inflammation.
Explain the clinical manifestation / sign and symptoms of the patient with the Encephalitis. (State the symptoms and signs of encephalitis vada patient.)
Fever,
headache,
Confusion and altered mental status,
startle,
Neurological deficits.
Behavior changes.
Nausea and vomiting.
stiff neck
Photophobia (Sensitivity to the bright lights).
Hallucination (Falls Sensory Perception).
Difficulty in speech and language.
Motor disturbance.
Body aches.
Caesar is coming.
Aphasia (Inability in Speaking).
Aphagia (Inability in Swallowing).
Disorientation.
Joint pain.
Loss of sensation in some part of the body.
In a person’s personality and behavior
Changes happen.
Muscle weakness.
Vision can be partial or total loss.
Loss of eye movement.
Involuntary loss of Face, Arm, and Legs.
Anxiety.
Unusual behavior.
Delusion:= believing things that are Obvious untrue.
Explain the diagnostic evaluation of the patient with the patient with the Encephalitis. (State the diagnostic evaluation of a patient with encephalitis vada.)
History taking and physical examination.
Brain MRI.
Ct scan.
Brain biopsy.
Culture of the Cerebro spinal fluid (CSF).
Serology test.
Lumber puncture.
CSF Examination.
PCR Test (Polymerase Chain Reaction).
Explain the medical management of the patient with Encephalitis. (State the medical management of a patient with encephalitis.)
Provide proper supportive care to the patient.
Advise the patient to take proper rest.
Advising the client to take proper nutrition.
Advise the patient to take proper fluids.
Antiviral medicine if the patient has a viral infection.
Ex:=
Acyclovir (Zovirax),
Foscavir (foscarnet).
Provide proper anti-inflammatory drug to the patient.
Ex:= Acetaminophen,
Ibuprofen,
Naproxen.
If the patient has a bacterial infection, provide antibiotic medicine to the patient.
If the patient has any parasitic infection then give antiparasitic medicine.
If the patient has seizure condition, provide anticonvulsant medicine.
Provide proper supportive care to the patient.
If the patient has any pain condition then provide analgesic medicine.
Monitor the patient’s neurological status.
Monitor the patient’s mental status and consciousness level.
To provide proper rehabilitation services to patients.
Provide proper psychological support to the patient.
Provide oxygen to the patient properly.
Provide proper intravenous fluids to the patient.
Explain the nursing management of patients with Encephalitis. (State the nursing management of a patient with encephalitis.)
To provide properly comprehensive care to the patient.
Properly assess the patient.
Properly assess the patient’s neurological status, mental status and level of consciousness.
To assess patient’s vital signs properly.
Continuously monitor the patient’s fluid and electrolyte levels.
Continuously monitor the patient’s electrolyte levels.
If the patient has seizure condition, provide anticonvulsant medicine.
If the patient has a viral infection, provide antiviral medicine.
If the patient has any bacterial infection then provide antibiotic medicine.
Antifungal medicine should be provided if the patient has any fungal infection.
If the patient has any parasitic infection then provide antiparasitic medicine.
Provide proper respiratory support to the patient.
Provide proper nutritional support to the patient.
Maintaining proper hydration status of the patient.
Properly assess the patient if any kind of complication has occurred.
To provide proper education to the patient and his family members.
Provide emotional support to the patient.
To monitor the patient’s vital signs frequently.
Properly monitoring the patient’s intake output chart.
To properly monitor patient’s vital signs.
Closely monitor the patient’s neurological status.
Keeping the patient’s airway properly patent.
Providing a properly calm and comfortable environment to the patient.
Keep the patient away from noisy environment.
Properly monitor the patient’s skin integrity.
Advise the patient to perform proper range of motion exercises.
Provide proper standard precautions and isolation to the patient.
Provide proper antipyretic medicine to the patient.
Provide proper psychological support to the patient.
Advising the patient to take proper medication.
Advising the patient to follow up regularly.
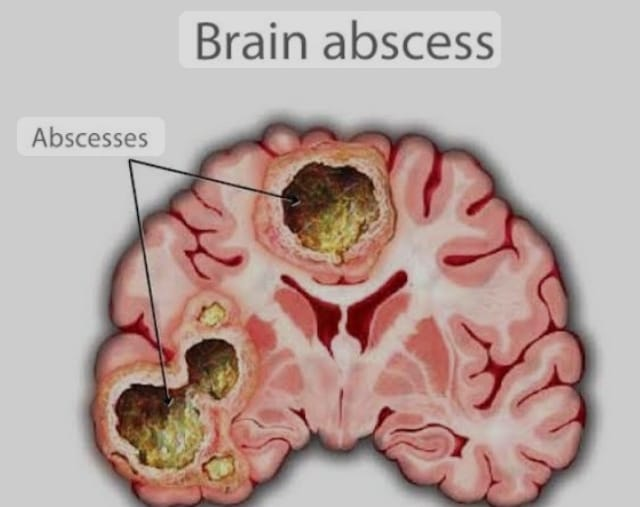
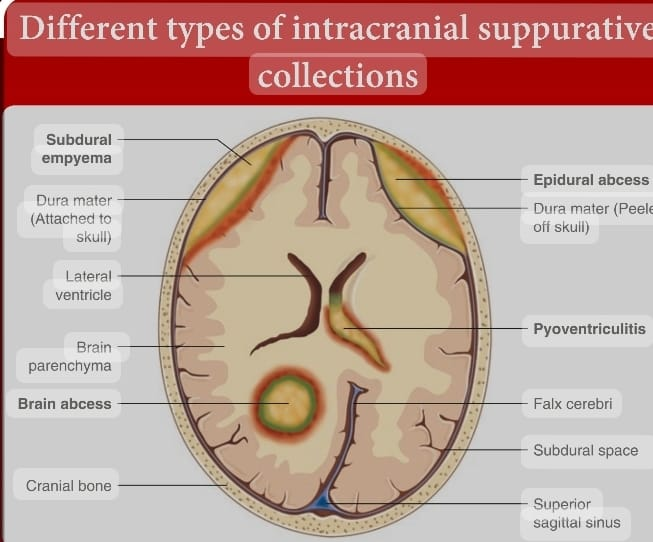
6) Define/ Explain Brain Abscess. (Define brain abscess.)
A brain abscess is a bacterial brain infection.
It is also called cerebral abscess. In this condition, the bacteria reach the brain and then the bacteria create an infection in the brain. When the infection occurs in the brain and the body responds to it, inflammation occurs in the brain. Due to this inflammation, pus formation occurs in the brain. This condition is called brain abscess.
Any bacterial or other microorganism causes infection in the brain tissues. Due to this infection, inflammation occurs in the brain. Due to this inflammation, pus is formed in the brain. is
Explain the etiology/cause of the patient with the brain abscess.
State the causes of brain abscess.
Due to bacterial infection.
Due to fungal infection.
Due to parasitic infection.
Due to direct trauma and injury.
Due to blood stream infection.
Due to compromised immune system.
Due to ear infection.
Due to dental abscess.
Due to infection of paranasal sinuses.
Due to lung, heart and kidney infection.
Due to penetrating injury.
Being a chronic disease.
Due to taking immune system suppressive drugs.
Due to any fungal infection.
Explain the clinical manifestation / sign and symptoms of the patient with the brain abscess. (State the symptoms and signs of a patient with brain abscess.)
.
headache,
fever,
Neurological impairment.
Altered mental status.
Nausea and vomiting.
seizure.
Visual disturbance.
Difficulty in speaking.
Difficulty in swallowing.
Personality change.
Increased intracranial pressure in the skull.
If the abscess occurs in the cerebellum, the person’s balance is lost.
If the abscess occurs in the frontal lobe of the brain, memory loss occurs, attention span is shortened and speech disorder occurs.
If the abscess occurs in the temporal lobe, vision is partially lost.
Confusion.
Siezer to come.
Irritability.
Drowsiness.
Loss of sensation.
Loss of coordination.
Movement decreases.
Having a language difficulty.
Weakness.
Loss of muscle function.
Stiff neck.
Explain the diagnostic evaluation of the patient with the brain abscess. (State the diagnostic evaluation of a patient with brain abscess.)
history taking and physical examination.
ct scan.
MRI.
Blood culture.
Chest and Skull x-rays.
Complete blood count.
Electroencephalogram (EEG),
needle biopsy,
lumbar puncture,
Explain the medical management of the patient with the Brain Abscess. (State the medical management of a patient with brain abscess.)
Provide proper antibiotic medicine to the patient.
Ex:= Penicillin,
Metronidazole.
Provide proper corticosteroid medicine to the patient.
If the patient is in pain, provide analgesic medicine.
If the patient has fever then provide antipyretic medicine.
If the patient has seizures, provide antiepileptic medicine.
To continuously monitor the patient’s vital signs.
Properly assess the patient’s neurological status.
Explain the surgical management of patients with brain abscess. (State the surgical management of a patient with brain abscess.)
In the condition of brain abscess, the abscess is drained surgically.
Abscess is properly aspirated.
A brain abscess is surgically opened and any infectious material is removed.
Brain abscesses are removed using CT scan and MRI.
Explain the Nursing management of patients with the Brain Abscess. (State the nursing management of a patient with brain abscess.)
Assess the patient’s neurological status properly.
To properly assess the patient’s vital signs.
Properly assess the pupillary response and motor response of the patient.
Assess the patient for any signs and symptoms of increased intracranial pressure such as headache, altered mental status, and any changes in vital signs.
To monitor patient’s vital signs regularly.
If the patient is in pain, provide analgesic medicine.
If the patient has seizures, provide antiepileptic medicine.
Antibiotic medicine should be provided if the patient has any infection.
Properly assess the patient’s fluid and electrolyte levels.
Provide proper nutritional support to the patient.
Provide proper psychological support to the patient.
To provide complete information to the patient about his disease, its causes, its symptoms and signs, and its treatment.
Assess the patient for any other complications.
Advising the patient to take regular medication.
Advising the patient to follow up properly.
To provide proper working and comfortable environment to the patient.
Advising the patient to take regular follow up
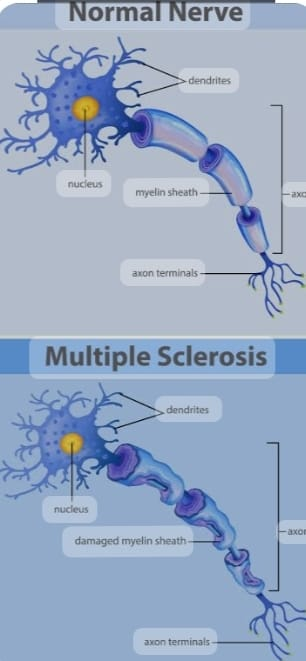
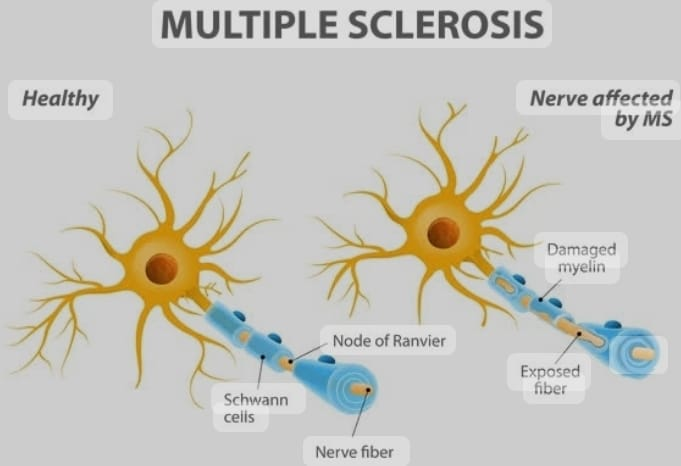
7) Define/Explain Multiple Sclerosis. (Define multiple sclerosis.)
MS is the abbreviation for multiple sclerosis. Also called Multiple sclerosis is a type of autoimmune disease in which the myelin sheath over the neurons of the brain and spinal cord is degenerative, demyelinating, scarring and destruction due to which the neurons cannot function properly due to which the electrical impulses are transmitted properly. does not occur and body function is impaired. Multiple Sclerosis
Neurological symptoms are also seen due to destruction of the myelin sheath. Like, feeling tired, feeling weak, Numbness and Tingling sensation, Impairment in balance and coordination.
Symptoms like This DCS is mainly seen in young adults and is more common in females.
Explain the etiology/cause of the multiple sclerosis. (State the causes of multiple sclerosis.)
Due to genetic factor.
Due to environmental factors.
Due to viral infection.
Due to low vitamin D.
Because of smoking.
Due to genetic and environmental factors.
Due to having a history of disease in family members.
Because of Smocking.
environmental exposure to pollution, toxins,
Explain the types of multiple sclerosis. (State the type of multiple sclerosis.)
There are total four types of multiple sclerosis.
1) Relapsing Remitting Multiple Sclerosis; (RRMS),
2) Primary Progressive Multiple Sclerosis (PPMS),
3) Secondary Progressive Multiple Sclerosis (SPMS),
4) Progressive Relapsing Multiple Sclerosis (PRMS).
1) Relapsing Remitting Multiple Sclerosis; (RRMS),
Relapsing remitting multiple sclerosis is the most common form of multiple sclerosis. In this type, a person develops multiple sclerosis, then recovers, and the person has relapses of multiple sclerosis.
2) Primary Progressive Multiple Sclerosis (PPMS),
In primary progressive multiple sclerosis, there is continuous progression of the disease after a person develops the disease. This type of multiple sclerosis is mainly seen after 40 years.
3) Secondary Progressive Multiple Sclerosis (SPMS),
In this type there will be relapsing-remitting attacks initially. But like this
After two to three attacks, the disease begins to progress continuously. If the patient does not receive proper treatment of relapsing remitting multiple sclerosis, it is transmitted to secondary progressive multiple sclerosis.
4) Progressive Relapsing Multiple Sclerosis (PRMS).
After the onset of progressive relapsing multiple sclerosis, its continuous progression is seen.
Explain the clinical manifestation / sign and symptoms of the patient with the Multiple Sclerosis. (State the symptoms and signs of Multiple Sclerosis Wada patient.)
Numbness and tingling sensation.
Burning sensation.
Weakness and paralysis.
Stiffness and spasticity in the muscles.
Tremors and involuntary muscle movements.
Visual disturbance.
Blurred vision.
Loss of color vision.
Double vision (Diplopia).
Difficulty in balance and coordination (Ataxia).
Dizziness.
feeling tired
Impairment in concentration.
Changes in mood.
Bowel and bladder dysfunction.
Sexual dysfunction.
Pain and sensory disturbance.
Difficulty in speech and swallowing.
Eye movement becomes involuntary.
Mood disturbance.
Weakness and numbness are both extremes.
Explain the diagnostic evaluation of the patient with multiple sclerosis. (State the diagnostic evaluation of a patient with multiple sclerosis.)
History taking and physical examination.
history taking and physical examination.
Ct scan.
M.R.I.
PET test.
C.S.F.Analysis.
Neuropsychological testing.
Evoked potential.
Neurological Studies.
Blood test.
Explain the medical management of the patient with Multiple Sclerosis. (Write the medical management of a patient with multiple sclerosis.)
Disease modifying therapy.
Disease modifying therapy is the main treatment for relapsing remitting multiple sclerosis and secondary progressive multiple sclerosis.
This medication reduces inflammation, suppresses the disease, and prevents the disease from relapsing.
Ex:=
Interferon beta,
Glatirmate Acetate,
Dimethyl fumarate,
Fingolimod,
Teriflunomide,
Ocrelizumab.etc.
Provide proper symptomatic treatment to the patient.
Provide physical therapy and occupational therapy to patients.
If the patient has muscle stiffness, provide antispasmodic medicine to the patient.
If the patient has a condition of depression, provide antidepressant medicine.
Provide anti-cholinergic medicine to the patient.
Provide proper physical therapy and speech therapy to the patient.
If the patient has a condition of inflammation, he should be provided with corticosteroid medicine properly.
Monitoring the patient properly.
To provide proper rehabilitation to the patient.
Advising patients to adopt healthy lifestyle habits.
Advise the patient to take regular exercise, balance diet, adequate sleep, and reduce stress.
Advise the patient to avoid smoking and alcohol.
Provide proper bowel and bladder training to the patient.
Explain the Nursing management of patients with Multiple Sclerosis. (State the nursing management of a patient with multiple sclerosis.)
Properly assess the patient.
Properly assess the physical, psychological, neurological and cognitive status of the patient.
Properly assess the symptoms of the patient.
Advising the patient to take medication properly.
Provide proper psychological support to the patient.
Advise the patient to exercise properly.
Advise the patient to take proper rest.
Provide proper muscle relaxant medicine to the patient.
Advise patient to change position frequently to hourly.
Advise the patient to maintain proper aseptic technique.
Advising patients to provide proper skin care.
Provide proper corticosteroid medicine to reduce the oedema and inflammation in the patient’s body.
Advising the patient for proper life style modification.
Advising the patient to follow up properly.
Advising the patient to take proper medication.
Providing a properly calm and conformable environment to the patient.
8) Define/Explain Myasthenia Gravis. (Define myasthenia gravis.)
Myasthenia gravis is a compound word.
Mys:= Muscles,
Aesthesis:= Sensation.
Myasthenia gravis is a chronic autoimmune disorder MG (Myesthenia Gravis) disease mainly affects the neuromuscular junction and in Myesthenia Gravis chronic progressive neuromuscular junction is damaged and muscle weakness occurs.
In myasthenia gravis, an inappropriate antibody is produced in the patient’s body and this antibody binds to the Ach receptor (Acetylecoline receptor). And this antibody blocks the Ach receptor. And due to this, the number of Ach receptor decreases and its function is also impaired. And the nerve impulses cannot be transmitted properly and the muscles of the body become weak and the voluntary muscle control of the body is impaired. And due to this, muscle weakness and fatigue occur.
Explain the Etiology/ Cause of the patient with the Myasthenia Gravis. (State the cause of a patient with myasthenia gravis.)
The exact cause of myasthenia gravis is unknown.
Due to thymus gland tumor.
Due to abnormality of thyroid gland.
Autoimmune attack:= thyrotoxicosis, rheumatoid arthritis,
Systemic lupus erythematosus,
Myasthenia Crisis,
Due to acetylcholine deficiency.
Due to abnormality in Thyroid gland.
Due to environmental factors.
Due to genetic factors.
3) Explain the clinical manifestation/sign and symptoms of the patient with the Myesthenia Gravis. (State the symptoms and signs of myasthenia gravis vada patient.)
Muscle weakness,
Ptosis (Drooping of the eye lids),
Diplopia (Double vision),
Weakness in facial muscles.
Mask-like facial expressions.
Changes in voice.
Arm, Hands,
Weakness in fingers, legs and neck.
Dysphagia (difficulty in swallowing),
Dysarthia (Weakness in the muscles of the mouth and throat can cause Slurred Speech),
feel tired,
Respiratory impairment.
Facial weakness.
Weakness in the extremities.
Breathing difficulty.
Difficulty in swallowing.
Difficulty in talking.
Speech impairment.
Shortness in bridging.
Having double vision.
Weakness in leg and hand.
Facial paralysis.

Explain the diagnostic evaluation of the patient with the Myasthenia Gravis. (State the diagnostic evaluation of a patient with myasthenia gravis.)
History taking and physical examination.
Ct scan.
MRI.
Repetitive nerve stimulation.
Single fiber electromyography
(EMG).
Pulmonary function test.
Endophonium test.
Neurological examination.
Explain the medical management of the patient with the Myasthenia Gravis. (Give medical management of myasthenia gravis vada patient.)
1) Cholinestase inhibitor:=
Ex:= pyridostigmine
It is the first line treatment of myasthenia gravis.
This medicine prevents the breakdown of acetyl, due to which muscle concentration increases and neuromuscular transmission also increases.
2) Immuno suppressive therapy:=
Provide immunosuppressive medicine to individuals who have moderate to severe MG and cholinesterase inhibitor medicine cannot work properly.
Ex:=
Corticosteroids
Azathioprine, (Azathioprine,)
Methotrexate, (Methotrexate,)
Mycophenolate mofetil. (Mycophenolate mofetil.)
3) Monoclonal antibody:=
Provide proper monoclonal antibody to the patient.
4) Intravenous immunoglobulin and plasma exchange (Plasmaphresis)
This medicine decreases acute exacerbations or myasthenia gravis and circulating antibodies.
5) Thymectomy:=
In this the thymus gland is removed.
6) Supportive therapy:=
Provide proper supportive therapy to the patient.
7) Regular Monitoring:=
Monitor the patient regularly.
8) Lifestyle monitor:=
Giving advice for proper life style modification to T-shirt.
Explain the nursing management of patients with the Myasthenia Gravis. (State the nursing management of a patient with myasthenia gravis.)
Proper assessment of the patient.
Properly assess the patient’s neurological status.
Provide proper respiratory support to the patient.
Advising the patient to do proper physical activity.
Provide proper nutritional support to the patient.
Provide proper psychological support to the patient.
Keep the patient’s airway properly patent.
Assess the patient’s fluid and electrolyte levels properly.
Provide proper nutritional support to the patient.
Provide proper psychological support to the patient.
Provide proper calm and comfortable environment to the patient.
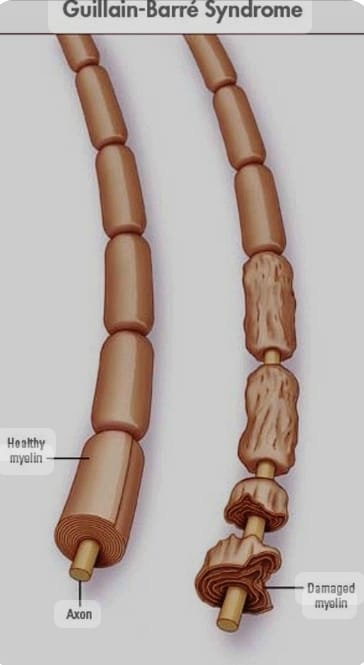
9) Explain/Define Gillian Barre Syndrome. Explain/Define Guillain Barre Syndrome.
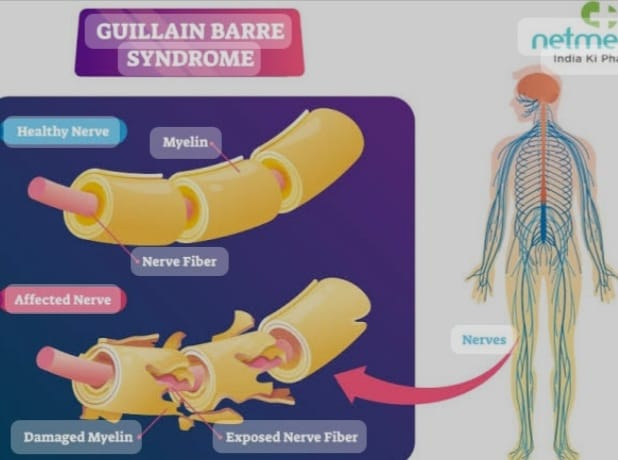
Guillain Barre syndrome is named after George’s Guillian, Jan Alexander Bare and Strohl. Guillain Barre syndrome was first described in 1916.
Guillain Barre syndrome is also called acute inflammatory polyneuropathy or polyradiculoneuritis.
Guillain Barre Syndrome is also called G.B.Syndrome.
Guillain Barre syndrome affects the peripheral nervous system (which affects the cranial nerve and spinal nerve).
Guillain Barre syndrome is an autoimmune disorder. It is a disorder in which the body’s immune system affects the peripheral nervous system and spinal nerves.
In this condition, the swan cell is damaged.
Due to the damage of the swan cell, the neuron is demyelinated, damaged and destroyed, due to which the transmission of the nerve is disturbed and the transmission of nerve impulses cannot take place. So nerve impulses cannot be transmitted from one neuron to another. So this is called Guillain Barre syndrome disease.
Explain the Etiology/Cause of the Guillian Barr Syndrome. (Give no cause for Guillain Barre syndrome.)
Exact causes are unknown.
Due to lung infection and gastrointestinal infection.
Campylobacter jejuni.
Caused by cytomegalovirus.
Caused by Epstein Barr virus.
Zika virus.
Due to swine flu infection.
Due to general surgery and epidural anesthesia.
Due to certain types of auto immune diseases.
Due to certain types of medication
like:= Thrombolytic and immunosuppressive.
Explain the classification of the patient with the Guillian bare syndrome. State the classification of Guillain Barre syndrome.
There are 6 classifications of Guillain Barre syndrome.
1) Acute inflammatory demyelinating polyneuropathy (AIDP),
2)Miller Fisher Syndrome (MFS),
3) Acute Motor Axonal Neuropathy (AMAN),
4) Acute Motor Sensory Axonal Neuropathy (AMSAN),
5) Acute Panotonomic Neuropathy (APN),
6) Bickerstaff brainstem encephalitis (BBE).
1) Acute inflammatory demyelinating polyneuropathy (AIDP), Acute inflammatory demyelinating polyneuropathy (AIDP),
This acute inflammatory demyelinating polyneuropathy is the most common form and subtype of Guillain Barre syndrome. This is mainly due to the direct response of auto immune response mainly on Schwann cells.
2) Miller Fisher Syndrome (MFS), Miller Fisher Syndrome (MFS),
Miller Fisher syndrome is a rare variant of Guillain Barre syndrome. It mainly involves descending paralysis. It mainly affects the first eye muscles. And Triad like, Opthelmoplagia, Ataxia (Loss of the Muscles Control), and Areflexia (Absence of the deep tendon Reflexes) are seen. In this type Anti-GQ1b antibodies are 90% cases. Ma is seen.
3) Acute motor axonal neuropathy (AMAN),
In this type, the motor nodes are attached to the Ranvier. This is primarily an autoimmune response that occurs directly in the exoplasm of the peripheral nerve. This type is seasonal and recovery is also rapid, Anti-GD3 antibodies can be seen in this.
4) Acute Motor Sensory Axonal Neuropathy (AMSAN)
This is similar to AMAN. But there is severe axonal damage to the sensory nerve. This type gives a direct response to the peripheral nerve just like AMAN. Recovery is slow and incomplete.
5) Acute Panotonomic Neuropathy (APN),
This is a rare variant type of GBS. Encephalopathy is also involved. This type has a high mortality rate due to cardiovascular involvement.
Symptoms like impaired sweating, lack of tear formation, photophobia, dryness of nasal mucosa, itching or peeling of skin, nausea, dysphagia, constipation, lethargy, fatigue are seen in this patient.
6) Bickerstaff brainstem encephalitis (BBE). (Bickerstaff brainstem encephalitis (BBE).)
This is another variant of Guillain Barre syndrome.
These are mainly ophthalmoplegia, ataxia, consciousness disturbance, hyperreflexia, and Babinski sign. BBE has a more severe initial presentation and a good prognosis.
Explain the clinical manifestation / sign and symptoms of the patient with the Guillian bare syndrome. (State the symptoms and signs of Guillain Barre syndrome.)
Muscle weakness.
Tingling and numbness.
Areflexia (Deminished and Absence of the deep tendon reflexes).
Pain
Fluctuating blood pressure.
Heart rate abnormality.
A swatting disturbance occurs.
Bowel and bladder function disturbance.
Impaired respiratory function.
Difficulty in swallowing (Dysphagia).
Facial weakness.
Double vision (Diplopia).
Difficulty in speaking (Dysarthia).
Progressive muscle weakness in arms, legs, and face on both sides.
Reflexes in the lower extremities are demineralized.
Tingling sensation in hands and feet.
Stiffness and muscle pain.
Having an uncoordinated moment.
Muscle spasms.
Palpitation.
Changes in heart rate.
Cardiac arrhythmias.
Difficulty in eye movement, facial movement, speaking, chewing and swallowing
Explain the diagnostic evaluation of the patient with the Guillain bare syndrome. (State the diagnostic evaluation of Guillain Barre syndrome.)
History taking and physical examination. (History taking and physical examination)
Laboratory test. (Blood test.)
Cytomegalo virus test (CMV),
Epstein Barr Virus (EBV) Test
Cerebro spinal fluid analysis
Electro Physiological Test
Electromyography (EMG),
Imaging studies. (MRI test.) (Imaging studies. (MRI test.) )
Autoimmune function test.
Pulmonary function test (PFT test).
Nerve conduction velocity test.
Explain the medical management of the patient with the Guillian bare syndrome. (State the medical management of Guillain Barre syndrome.)
Provide proper supportive care to the patient.
Proper close monitoring of the patient.
Provide proper supportive care to the patient.
Monitor patient’s vitals properly.
Provide proper respiratory support to the patient.
Provide intravenous immunoglobulin to the patient.
Properly Plasmaphresis (In this process plasma is removed from the patient’s body and its antibodies are removed and then the plasma is replaced back in the patient’s body.)
Provide proper mechanical ventilation to the patient.
If the patient is in pain, provide analgesic medicine.
To provide proper therapy and rehabilitation therapy to the patient.
Provide proper nutritional support to the patient.
Provide proper psychological support to the patient.
Explain the nursing management of patients with the Guillian bare syndrome. (State the nursing management of Guillain Barre syndrome.)
Provide proper respiratory support to the patient.
Properly assess the patient.
To properly assess the patient’s vital signs.
Provide proper respiratory support to the patient.
Advise the patient to perform proper range of motion exercises.
Provide proper nutritional support to the patient.
Properly managing the patient’s pain.
Provide proper psychological support to the patient.
Provide proper education to the patient.
To provide proper rehabilitation to the patient.
Provide proper mechanical ventilation to the patient.
Advise the patient to perform proper deep breathing and cuffing exercises.
Advise the patient to perform proper active range of motion exercises.
Advise patient to take high calorie high protein diet.
Advise the patient to have adequate fluid intake.
Advising patients to take medicine properly.
Advising the patient to follow up properly.
Provide a properly calm and comfortable environment to the patient.
.
.