ENGLISH Respiratory disorder- MSN 1 UNIT 8-juhi-part-02
Assessment of respiratory function
Health history (subjective data) :
Health history includes present health history, past health history, past surgical history, personal history, family history and occupational history.
Present health history / chief complaint
Asking the patient about their current complaints.
To know if the patient has breathing difficulty, chest pain, cuffing present or not.
If the patient has these symptoms, to know their duration, severity, intensity and associated factors.
Like when breathing difficulty is seen and in which position it is seen.
Asking if any sounds are heard while breathing.
Asking which side of the chest is the pain and whether this pain radiates or not.(If there is a cardiac related problem then the pain radiates. When there is a respiratory related problem then the pain does not radiate.)
Asking whether sputum production is observed or not.
If production is seen, know its quality and quantity.
Knowing the color of sputum.
To know if there is blood in sputum or not.
Asking how long the cough has been present. Past health history:
Ask the patient if they have experienced any such symptoms in previous years.
To know whether the patient has had conditions like TB, whooping cough, diphtheria, covid-19 in previous years.
To know whether the patient was previously admitted to the hospital or not.
Collecting information about childhood diseases and immunization. Past surgical history:
Knowing whether the patient has undergone any type of surgery in previous years.
Personal history:
Asking whether the patient has any type of allergy.
Knowing whether the patient smokes or not.
If there is a smoking history, how long have you been smoking and how many times a day you smoke.
Knowing whether any kind of medicine is on or not.
Knowing whether there is a history of alcohol or not. Family history:
Collecting the patient’s family history.
Knowing if anyone in the family has respiratory diseases or allergies. Like asthma, emphysema, cystic fibrosis
Also to know if there are any other DCs or not.
Knowing if anyone in the family smokes or not. Occupational history:
To collect the occupational history of the patient.
Like knowing what the patient is doing.
To know whether one is using protective equipment if working in industries or factories.
People working in mining, refining, manufacturing, construction, stone making, cotton and textile industries have high respiratory rate. Like Silicosis, Asthma, Asbestosis
Physical examination (physical examination) / objective data (objective data)
Respiratory assessment mainly includes head, chest, extremities, fingers and toes.
Respiratory examination uses inspection, palpation, percussion and auscultation methods.
Use adequate lighting and keep cool and cool environment while doing examination.
Carry a sputum mug while doing the examination. Hence the patient’s sputum can also be examined. ◼️Inspection (Inspection) Skin inspection (Skin inspection)
Checking the color of skin and mucus membrane.
Checking whether cyanosis is present in conjunctiva, lips, tongue.
Cyanosis is mainly due to the condition of hypoxia i.e. the condition of deoxygenated hemoglobin is present.
Cyanosis seen in lips, gums and tongue is known as ‘central cyanosis’.
Cyanosis seen in fingers and toes is known as ‘peripheral cyanosis’.


Thoracic inspection
Examination of the patient’s breathing pattern and rhythm. Also to check the effort of breathing.
Checking for restriction while breathing. Also checking whether the accessory muscles are used while breathing. (Restriction during inspiration and if it is asymmetrical, it indicates a block in the branch of the respiratory tree.)
Examining for asymmetric bulging during breathing.
Check for bulging in the intercostal space while exhaling. (If seen it indicates obstruction of expiratory flow)
Examining the chest for symmetry, shape and deformity.
Checking whether the chest has a normal shape or a barrel, pigeon or funnel shape.
👉🏻 For your knowledge
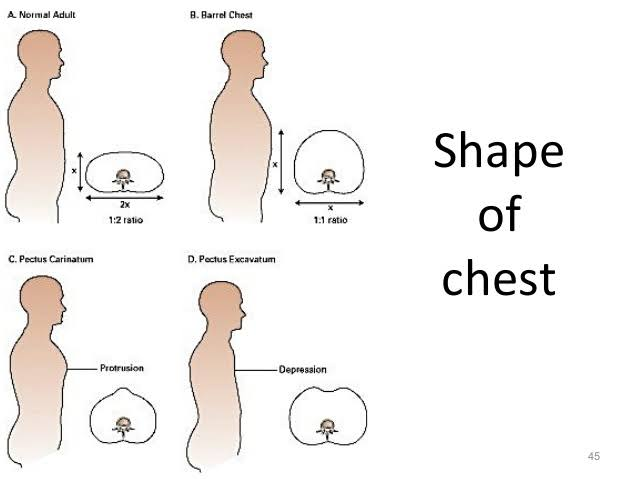
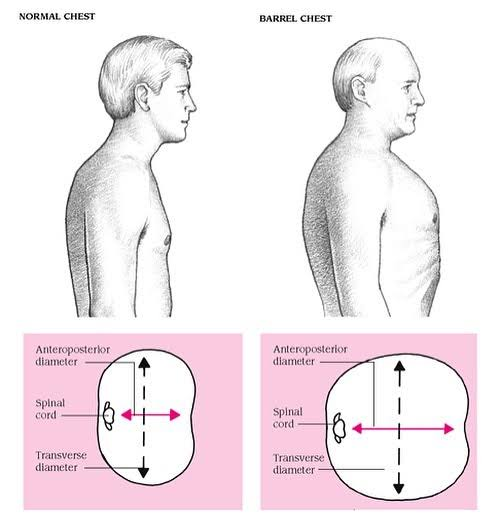
In a normal healthy person, the shape of the chest is elliptical.
In a normal healthy person the anterior posterior diameter is 1 while the lateral diameter is 2.
A normal healthy person has a ratio of anterior posterior to transverse diameter of 1:2.
Barrel chest
A barrel chest is seen due to over inflation of the lungs. Due to decreased elasticity of the alveoli, they appear inflated, due to which it appears as a round bulging chest and looks like a barrel shape.
Anterior posterior diameter increases to 2 in barrel chest. Hence the ratio of anterior posterior diameter and lateral diameter is 1:1.
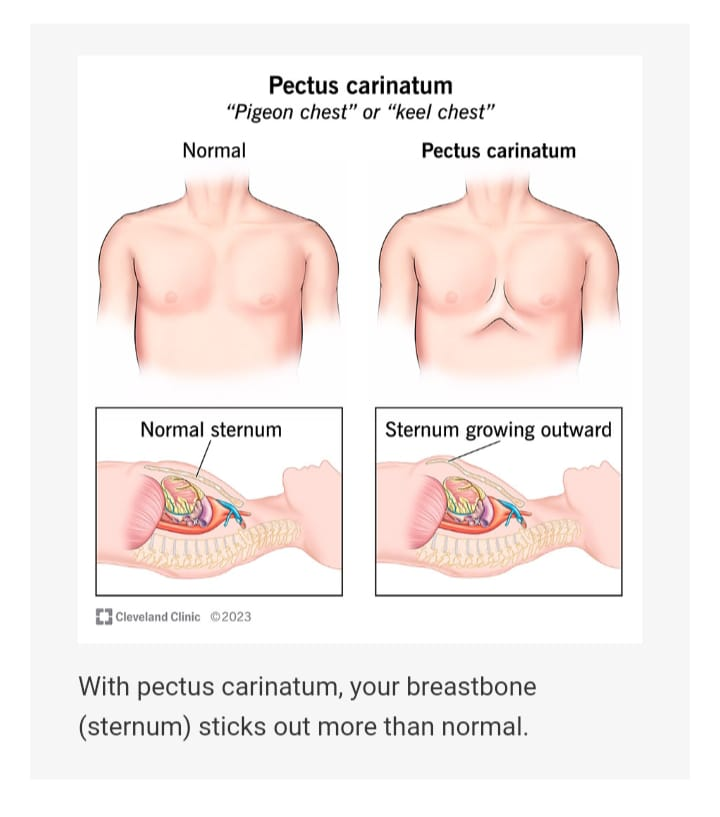
Barrel chest is seen in patients with COPD and emphysema. Pigeon chest
Pigeon Chest is also known as ‘Pectus carinatum’.
In which pectus means chest and carinatum means keel of boat.
Pectus carinatum is a deformity of the chest wall in which there is an overgrowth of the cartilage between the sternum and the ribs, causing the sternum and ribs to appear outward, i.e. protruding.
Hence there is an increase in the anterior posterior diameter.
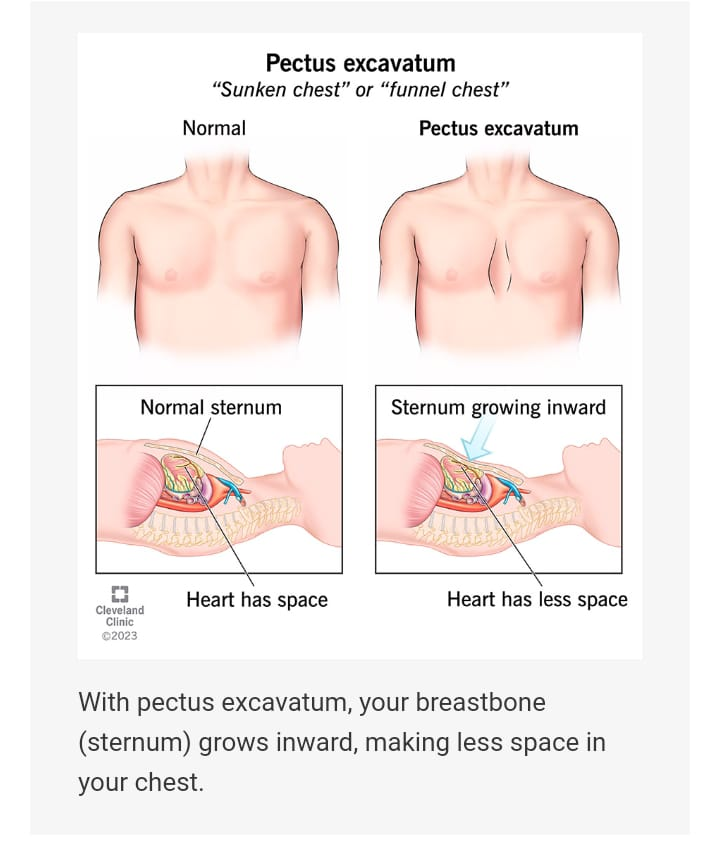
Funnel chest
Funnel chest is also known as ‘Pectus excavatum’ ‘Sunkan chest’ and ‘Cobbler’s chest’.
In which pectus means chest, and excavatum means pit.
Pectus excavatum is an abnormal congenital condition. In which the sternum is pulled inward i.e. the sternum appears depressed and grows inward.
Decreased anterior posterior diameter is seen in funnel chest.
Inspection of finger & toes
Checking whether clubbing is present in fingers and toes.
Checking if cyanosis is present in fingers and toes. 👉🏻 For your knowledge Clubbing of finger (Clubbing of finger)
In clubbing of finger, the nail is abnormal and round in shape (spoon like).
Clubbing of fingers is a sign of heart and lung disease indicating chronic hypoxic condition i.e. low level of oxygen in the blood such as chronic lung infection, chronic lung malignancy
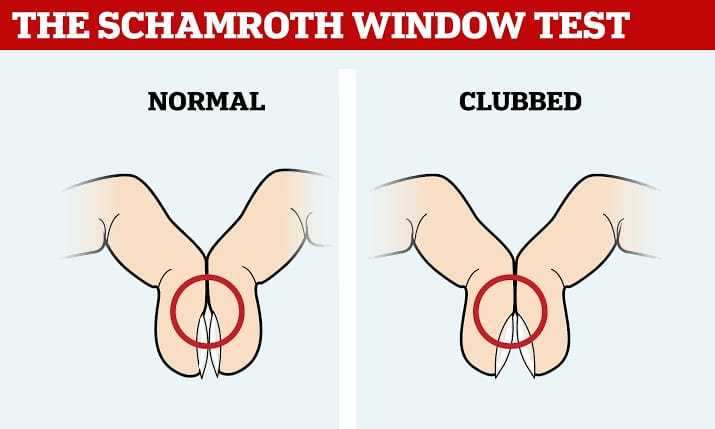
A Scharmroth window test is performed to check whether clubbing is present in the finger.
Scharmroth window test
The Scharmroth window test is used to confirm whether clubbing is present in the finger.
In the Scharmroth window test, the nail beds of one finger of both hands are held together and a diamond shape is seen between the nail boards as shown in the picture.
If a diamond shape is seen between the nail beds then it is normal whereas if there is no space between the nail beds it indicates clubbing.


Palpation
In thoracic palpation, the thoracic area is palpated.
In which the front and back of the chest are palpated for tenderness, deformity and abnormal movement.
In addition the area is palpated for pain, lesions, respiratory expansion and fremitus.
for your knowledge
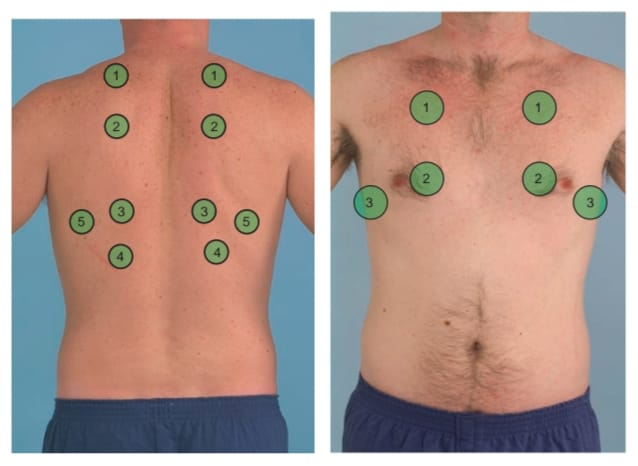
Tactile fremitus
Tactile fremitus is a palpation technique used to assess and assess the vibrations transmitted to the chest due to speech. In which the health care personnel places their hand in the area as shown in the image and asks the patient to speak and fills the chest with vibration.
An increase in fremitus indicates a condition like pneumonia but a decrease in fremitus indicates a condition like pleural effusion.
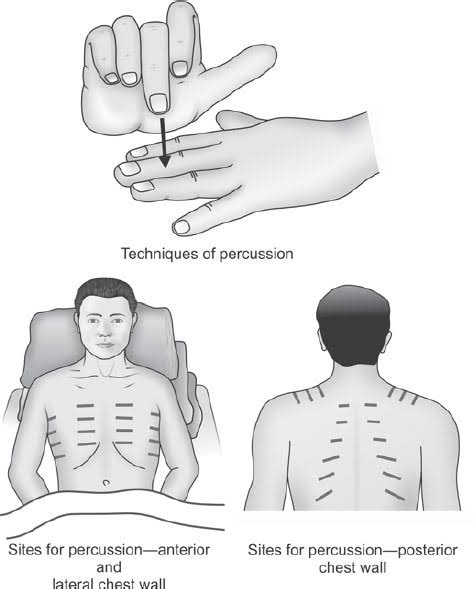
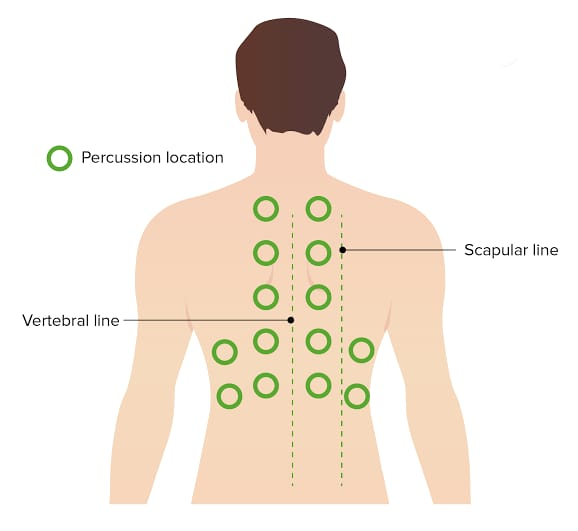
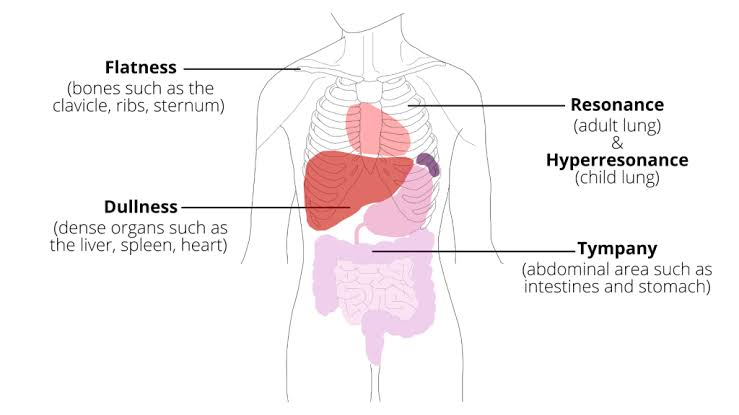
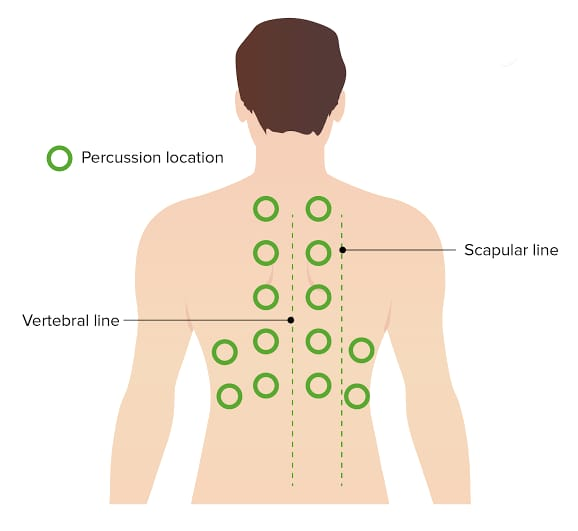
Percussion
Respiratory percussion assesses the underlying structures by tapping the chest to check for air, fluid, or solids present.
In which the anterior and posterior chest is tapped side to side and top to bottom and the sound heard through it is noted.
In addition, respiratory excursion is noted on respiratory percussion.
Respiratory percussion is useful for identifying changes in lung density and diagnosing conditions such as pneumonia, pleural effusion.
for your knowledge
- Resonance sound (Resonance sound):
Resonance is a low pitch sound. Which is mainly heard in airy areas. As in the thoracic cavity (lungus).
Dull sound
A dull sound is heard in the fluid area. like
Heart, Liver, Spleen
- Flat sound
Flat sound is heard in solid areas like bone, muscles
- Tympanic sound
A tympanic sound is a hollow, drum-like sound. Which is heard in the area of bloated stomach i.e. in the area of air pressure.
Hyper resonance sound
A hyperresonance sound is heard when there is too much air in the thoracic cavity. such as the condition of pneumothorax
•• When a dull sound is heard in the thoracic cavity it indicates that fluid has accumulated in the thoracic cavity.
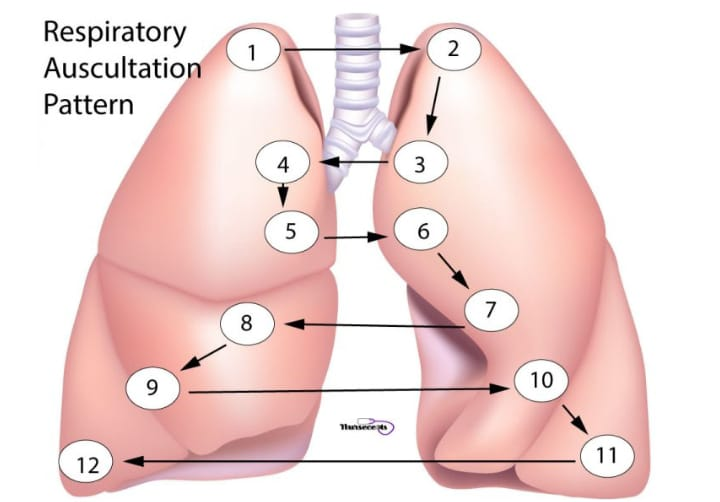
Auscultation
In auscultation, lung sounds are heard with the help of a stethoscope.
Auscultation is done by expert staff.
To note characteristic of normal lung sounds like location, quality, intensity with the help of stethoscope.
Also auscultate for any abnormal lung sounds.
In auscultation, lung sounds are auscultated with the help of the diaphragm on the anterior and posterior sides of the chest. The chest is auscultated as shown in the picture below.
The sound is noted during both inspiration and expiration. The patient is given rest in between to prevent the condition of hyperventilation.
Thus abnormal sound is detected with the help of auscultation.
In addition, voice sound (bronchophony, egophony) is also noted in auscultation.
Normal lung sound
Bronchial sound, vesicular sound and broncho-vesicular sound are normal lung sounds.
Bronchial sound
Bronchial is a normal high-pitched hollow or tubular sound.
Heard in parts of Thrace.
In which expiratory time is more than inspiratory time. Vesicular sound
Vesicular is a normal low pitch soft sound. Which is heard in the entire lung.
In which inspiratory time is more than expiratory. Bronchovesicular sound
Broncho-vesicular is a normal medium pitch sound with equal inspiratory and expiratory times.
Abnormal lung sound
Wheezing sound
Whiz is a low pitched musical sound. Which is seen due to obstruction in the lower respiratory tract. A wheezing sound is heard only during expiration.
Stridor
A stutter is an abnormally high pitched sound. Which is seen due to obstruction in the upper respiratory tract. This sound is heard during inspiration and expiration.
Pleural friction rub
The parietal and visceral pleura become inflamed and roughened and rub against each other and produce grating and cracking sounds.
Rhonchi:
A rhonkai is an abnormal continuous low pitched breath sound. which is heard during inspiration and expiration.
Fine crackles
This is a short high pitched babbling sound. Heard during late chronic bronchitis, early pneumonia, congestive heart failure, atelectasis. Fine crackles are heard at last during inspiration.
Coarse crackles
This is a low pitch popping bubbling sound. which is heard during inspiration and expiration. Heard in chronic bronchitis, pneumonia and bronchiectasis
Diagnostic evaluation
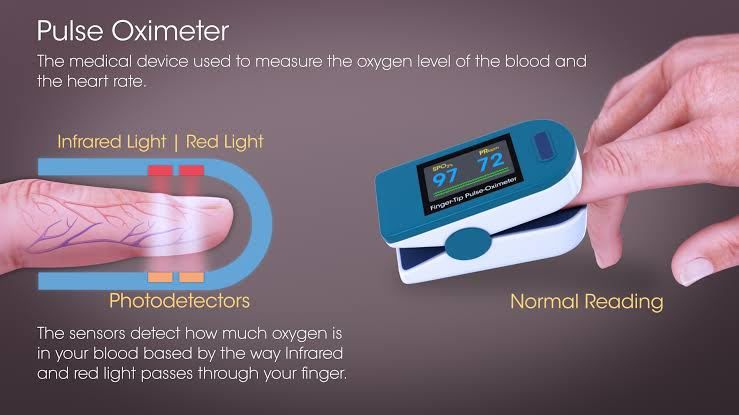
Pulse oximetry
Pulse oximetry is also known as ‘oxygen saturation test’.
Pulse oximetry is a quick, non-invasive technique for monitoring hemoglobin-linked oxygen saturation.
A pulse oximeter is used in pulse oximetry. Which is a type of electronic device.
This device consists of a light emitting diode that transmits light of two specific wavelengths (infrared light and red light) usually on the finger tip. One of these lights measures the amount of oxygenated hemoglobin while the other light measures the amount of deoxygenated hemoglobin and Finally shows the number of oxygenated hemoglobin.
A pulse oximeter is placed in the fingers, toes, feet, ears and nose and the spo2 level is checked.
A normal spo2 level is between 95-100%. If the spo2 level is less than 85%, it indicates that there is not enough oxygen reaching the cells and tissues.

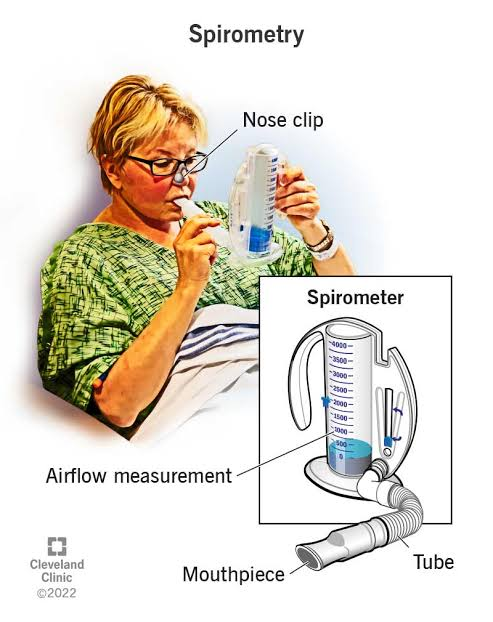
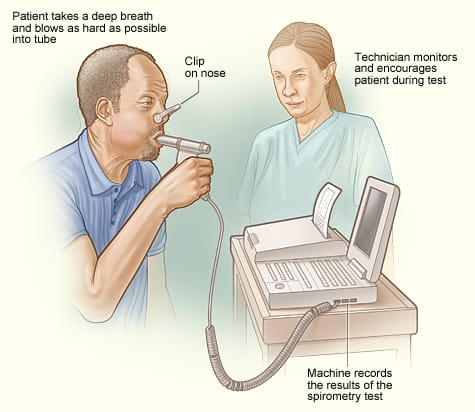
Spirometry
Spirometry is a lung function test that measures the amount of air we inhale and exhale, as well as the rate at which we inhale and exhale.
A spirometry test uses a spirometer instrument with a tube connected to a mouth piece and through this mouth piece the patient is asked to inhale and exhale air and the changes in the spirometer are observed.
The nose is clipped while doing this test.
Respiratory conditions such as asthma and COPD can be assessed with the help of spirometry.
Pulmonary function test
A pulmonary function test is a group test that measures how well the lungs are working.
These include spirometry, lung diffusion test, lung volume test and exercise test.
A pulmonary function test measures lung volume, capacity, flow rate, and gas exchange.
Pulmonary function tests are used to diagnose certain types of lung disease. Like asthma, emphysema
Arterial blood gas analysis (ABGs)
Arterial blood gas analysis is an important diagnostic method. It is useful for measuring the level of oxygen and carbon dioxide in the blood as well as blood pH and blood bicarbonate.
In which blood is mainly collected from the radial artery by expert health care personnel, in addition blood is often collected from the brachial or femoral artery (blood is not collected from the vein).
Through this test, the capacity of the lungs to dissolve oxygen in the blood and remove carbon dioxide from the blood can be known.
This test is preceded by an Allen test which is used to check the patency of the arteries that supply blood to the hand (radial and ulnar arteries). Normal value of ABGs
✓ partial pressure of oxygen – Pao2
- 75 – 100 mmHg
✓ partial pressure of carbon dioxide – Paco2
- 35 – 45 mmHg
✓ PH : 7.35 – 7.45
✓ Bicarbonate – Hco3-
- 22 – 26 mEq/L
✓ Oxygen content – O2CT
- 15 – 23% per 100 ml of blood
✓ Oxygen saturation
- 95 – 100%
Abnormal ABGs values indicate respiratory and metabolic disorders.
Culture
Cultural tests include blood culture and sputum culture. So that which type of micro organism is present in it can be identified
Sputum studies
A sputum study involves studying the sputum (mucus cough). So that bacteria, viruses and abnormal cells in the sputum can be identified. Conditions like pneumonia, tuberculosis can be identified with the help of sputum study.
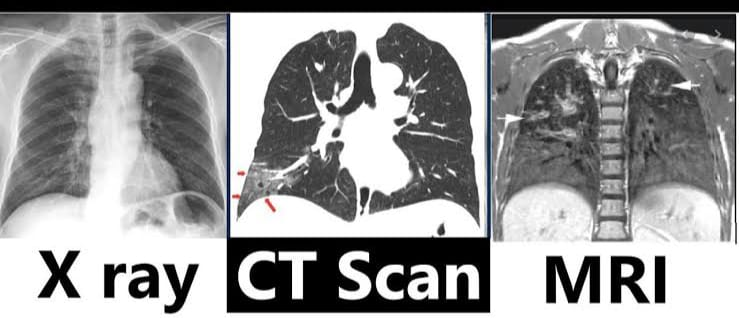
Imaging studies
Imaging studies are performed to evaluate anatomic structures.
In which X-ray, CT scan, m. R. Includes eye, angiography and ventilation perfusion lung scan. Chest x-ray
A chest x-ray uses small amounts of x-rays to create a 2D image of the area and visualize bone and tumors.
It mainly involves anterior-posterior and lateral side view.
Before the X-ray, the patient is asked to take a full inspiration so that the lungs can be well visualized.
Pneumonia, lung cancer, tumor, foreign body and rib fracture can be identified with the help of X-ray. CT-scan
A CT scan is an imaging study that provides more detailed information and a 3D image than an X-ray.
In a CT scan, X-rays are taken from different angles of the body and a cross-section picture of the body is created with the help of a computer.
With the help of CT scan, the condition of organs and soft tissue can be known.
CT scan can identify lung cancer, pulmonary embolism and infection. MRI
MRI – Magnetic Resonance Imaging
MRI uses powerful magnets and radio waves to create a cross-section image of a given area.
MRI provides detailed information of the heart, lungs and blood vessels.
MRI can detect pulmonary nodules, fibrosis, pleural disease and vascular abnormalities.
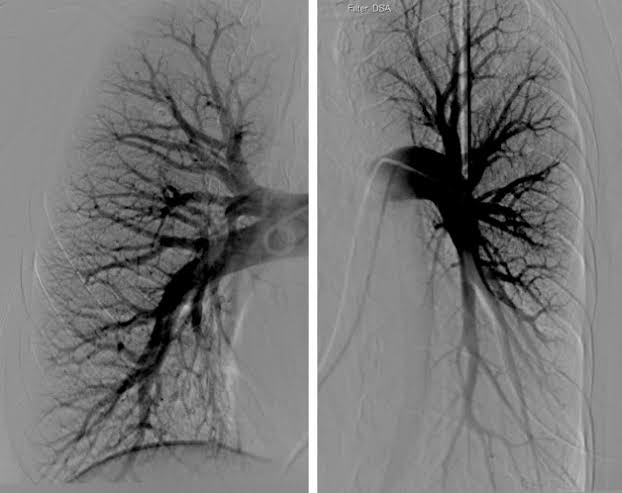
Pulmonary angiography
This is an invasive fluoroscopic procedure with which the pulmonary vein and pulmonary artery can be visualized.
In which a contrast dye is injected into the femoral artery or pulmonary artery with the help of a catheter and the pulmonary vessels are visualized and studied.
With the help of pulmonary angiography, pulmonary embolism, pulmonary vasculature, pulmonary hypertension and abnormalities of the pulmonary vascular tree can be detected and pulmonary blood flow, blockage, pressure and abnormalities are evaluated.
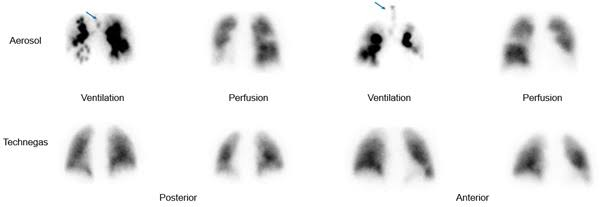
Ventilation perfusion lung scan
A ventilation perfusion lung scan is a nuclear medicine test that evaluates air flow and blood flow to the lungs.
In which radioactive subtons are inhaled and air flow is detected with its help. Similarly, radioactive subtons are administered intravenously to detect blood flow.
Endoscopic procedure
An endoscopic procedure involves direct inspection and examination of the organ using an endoscope.
Endoscopic procedures include bronchoscopy and thoracoscopy. Bronchoscopy
Bronchoscopy involves direct inspection and examination of the larynx, trachea, bronchi and bronchioles with the help of a bronchoscope.
In which the bronchoscope is inserted into the airway through the nose or sometimes the mouth and the light and small camera in the bronchoscope visualizes the organs and identifies the secretions and tumors.
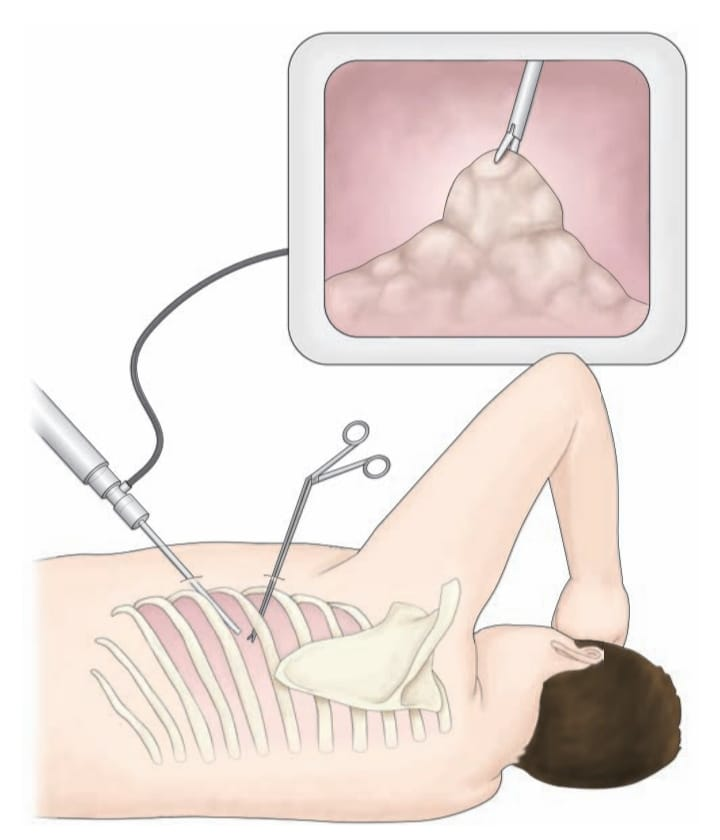
In addition, secretions and foreign bodies in the tracheo-bronchial tree can be removed. Thoracoscopy • Thoracoscopy is a diagnostic procedure in which the pleural cavity is examined using an endoscope.
In this procedure, a small incision is made in the chest wall and through this incision an endoscope is inserted into the pleural cavity and direct examination of the area is performed.
This specialized endoscope has a narrowing tube and a built-in camera and light to visualize the thoracic area.
Thoracoscopy can be used to diagnose pleural effusion, pleural disease and staging of tumours, and biopsies are also collected using thoracoscopy.
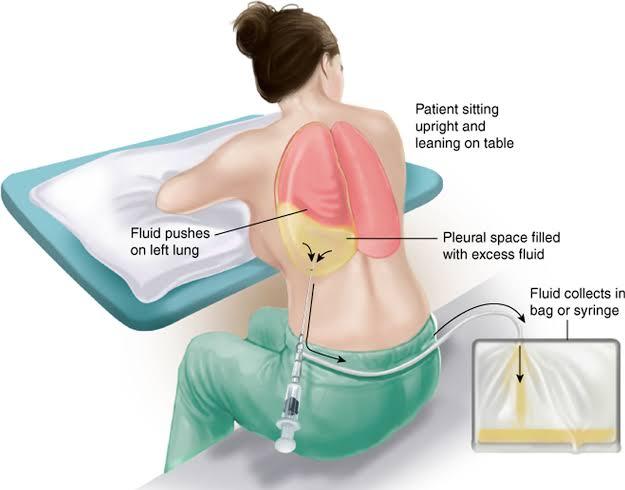
Thoracocentesis
Thoracocentesis is a diagnostic and therapeutic procedure.
In which fluid is aspirated from the pleural space between the lung and chest wall with the help of a needle or plastic catheter and the analysis of this pleural fluid is done.
Normally there is a small amount of pleural fluid in the pleural space. If present in excess, it indicates a diseased condition.
The pleural fluid is studied for gram stain culture and sensitivity, acid fast sensitivity and culture, differential cell count, cytology PH, specific gravity and total protein.
This procedure is done under the guidance of ultrasound.
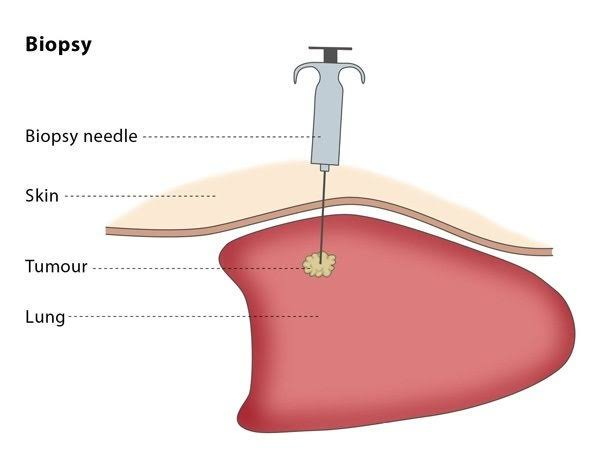
Biopsy
In a biopsy, a small sample of tissue is collected from the suspected area and microscopically examined. So that it can be identified whether malignancy is present or not.
Pleural biopsy
A pleural biopsy involves collecting a small sample of tissue from the pleura.
(The thin membrane surrounding the lungs and chest cavity is called the pleura)
A pleural biopsy is collected using needle biopsy or thoracoscopy. Lung biopsy
In a lung biopsy, a sample of lung tissue is collected from the lungs and examined. So lung cancer, lung infection and disease can be identified.
Different methods are used to collect lung biopsies.
Bronchoscopic biopsy
Open lung biopsy
Mediastinoscopy
Needle biopsy
Common nursing diagnosis & care for respiratory disorders
Impaired gas exchange related to bronchospasm, pulmonary obstruction, altered oxygen supply as evidenced by hypoxia, hypercapnia, cynosis, abnormal ABG
Improve gas exchange
(improving gas exchange)
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports. Ineffective airway clearance related to bronchoconstriction, increase mucus production as evidenced by hypoxia, hypercapnia, abnormal ABG
Maintain patent airway
(Maintaining airway patent)
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports. Ineffective breathing patterns related to shortness of breath, mucous production, bronchospasm Improve breathing pattern
(Improving Breathing Pattern)
To monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assessing breath sound and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide Fowler position to the patient and restrict his activities.
Explain and anchor the patient about deepbreathing and cuffing exercises.
To provide knowledge to patients about pursed lip breathing and diaphragmatic breathing.
Anchoring the patient to cough expectorate if secretions are present.
Provide oxygen therapy if spo2 level is low.
Providing nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
To maintain records and reports. Acute pain related to inflammatory condition of lung
Relieve pain
(relieving pain)
Assessing pain level.
To assess location, duration and intensity of pain.
To assess factors that trigger pain.
Provide a comfortable position to the patient.
Provide warm moist compression to the patient.
Providing Mind Diversional Therapy to the patient. So that the patient’s attention is diverted from the pain.
Advise the patient about relaxation therapy.
Administering prescribed analgesic medicine. Knowledge deficit related to disease condition and its prognosis
Improve knowledge level
(Improving Knowledge Level)
Assess the patient’s condition.
Assessing the patient’s knowledge of the disease condition and its treatment.
To provide knowledge to the patient about the disease condition and its prognosis.
Providing knowledge in a language the patient can understand.
To resolve patient’s doubts and queries. Anxiety related to disease condition, hospitalization
Reduce anxiety
(relieving anxiety)
Assess the patient’s condition.
Paying attention to the psychological needs of the patient and listening carefully to the patient.
Encouraging the patient to express his feelings, discomfort and anxiety.
To solve all doubts and queries of patients.
Providing knowledge to the patient about his condition and treatment so that his anxiety is removed and the patient becomes confident.
Providing psychological support to the patient.
Providing mind diversion therapy and recreational therapy to patients. Activity intolerance related to fatigue, dyspnea
Increase activity level
Assess the patient’s condition.
Checking the patient’s activity level.
Provide bed rest to the patient initially.
Then gradually anchor the patient to range of motion exercises.
Assisting the patient with his activities.
2 Provide rest to the patient between activities.
To check if the patient has any breathing difficulty during the activity.
If breathing difficulty is found, stop the patient’s activity and provide rest.