ENGLISH PEDIATRIC UNIT 6 FLUID AND ELECTROLYTE IMBALANCE
- INTRODUCTION OF FLUID ELECTROLYTE AND ACID BASE BALANCE.
Fluid, electrolyte and acid base balance is a dynamic process and is crucial in life.
Assessing and maintaining a child’s fluid and electrolyte status is a key nursing responsibility.
If the balance of fluid and electrolyte in the body is normal then the function of the body will be normal.
But when there is even a slight alteration in fluid and electrolyte, the normal physiology of the body is also altered.
Explain the basic mechanism of Fluid and electrolyte balance.
Body weight percentage is due to dissolved organic and inorganic substances dissolved in water and is a vital part of life.
Electrolytes are minerals that are found in our body. They also have a positive (+) or negative (-) charge. Electrolytes are found in different parts of the body including blood, urine, and other body parts. are located
Electrolytes have certain specific functions.
If there is an alteration in the electrolytes of the body, the body functions are also impaired.
Mel’s body is made up of 60% electrolytes.
Whereas a female’s body is made up of 55% electrolytes.
The body of mail contains 60% water.
While female body contains 50% water.
When the body of a human being has a normal balance of electrolytes, the body’s blood chemistry, muscle actions, and other body functions remain normal.
But if there is any slight disturbance in fluid and electrolyte in the body, the body chemistry is also altered.
There are different compartments in our body.
1) Intracellular (within the cell),
2) Interstitial (between cells),
3) Intravascular (in blood vessels).
Gastrointestinal secretions, urine, sweat, all these fluids are extracellular.
Fluid and electrolyte balance and acid base balance of the body have to be kept normal to maintain the homeostasis of the body (the internal environment of the body being normal) and the cellular function, whether intracellular or extracellular.
Explain the body fluid
Body fluid is in balance if fluid intake and fluid output are normal.
Maintaining fluid and acid-base balance in the body is essential for health promotion.
Continuous dynamic changes are taking place in the body.
The body needs a proper amount of fluid to support the changes in the body and to excrete waste material. A male’s body contains 60% water, while a female’s body contains 50% water.
As much as 75% of it is water in the brain,
About 70 to 75% water in a mussel,
And 22% is in bone.
Elderly people are less than 50% water.
And an infant is 70% to 80% water.
body fluid
1)Extracellular fluid is 35-40% (14 liters).
•Interstitial fluid :=10.5liter,
Plasma:=3liter,
transcellular fluid:=0.5liter. 2) Intracellular fluid (fluid inside the cell)
60-65% (28 liter) is 6-10 liters of lymph in the body.
And 3.5 – 5 liters of blood is there.
disturbances of volume and concentration of body fluid.
General Terminology.
1) Osmolarity
The number of solute in one liter of solution is called osmolarity.
2) Osmolality
Osmolality means the number of solutes present in one kilogram of water solution is called osmolality.
3) Isotonic
An isotonic fluid is a fluid that does not change cell volume.
4) Hypotonic
A hypotonic solution is such that it causes cell swelling.
5) Hypertonic solution
This means that this solution shrinks the cell.
Explain the function of body fluid
1) Blood delivers nutrients to cells and removes waste products from cells from the body.
2) Body fluid acts to keep blood volume and blood pressure normal and maintenance between them.
3) Body fluid maintains body temperature.
4) This body fluid evaporates the fluid through sweating and maintains the homeostasis of the body.
5) Body fluid works as an aqueous medium for the cell.
6) It works for many solvents for chemical reactions.
7) It helps in digestion of food through the stomach.
8) Fluid is responsible for excretion of waste products.
9) It works as a cushion of vital organs and protects viral organs.
10) Fluids help convert food into energy.
11) Fluid acts as a waste product elimination.
12) Fluids improve the health of the intestines and thereby relieve constipation.
13) Fluid flushes the kidneys due to which the waste products of metabolism are removed from the body.
14) Fluids work to keep the vital functions of the body normal.
- Explain the fluid balance
The fluid of the body is constantly lost and the fluid balance is normalized by the intake of liquids and food by the human being.
Fluid balance is the balance in which water is taken into the body.
through any drink, food etc., and water is excreted from the body through urine and other waste products, thereby maintaining fluid balance in the body.
Fluid is excreted mainly from the kidneys, lungs and skin.
Urea and other metabolic waste products are removed from the skin and lungs by the process of evaporation of water from the body and excreted by the kidneys.
Body fluids play an important role in supplying oxygen and nutrients to cells.
Aqueous humor is the bodily fluid located in the anterior chamber of the eye.
Vitreous humor is located in the posterior chamber of the eye
bile,
blood serum,
breast milk,
cerebro spinal fluid,
gastric juice,
mucus,
Fluid around the abdomen,
Pleural fluid (the fluid around the lungs,
pamper,
semen,
sweat,
tears,
vaginal secretions,
Vomiting, etc. is situated in the body and the internal environment of the body
Maintains homeostasis.
body fluid has been divided into two compartments:=
1) intracellular fluid (ICF: = fluid inside the cell),
2) Extracellular fluid (ECF: Fluid outside the cell)
1) intracellular fluid:=
Intracellular fluid is located inside the cell. Cell membrane and cellular metabolism keep cellular constitution under control.
Intracellular fluid is equal to two by three (2/3) of the body weight. Potassium, magnesium, phosphate, organic anions, and proteins are present in intracellular fluid.
If the body is 60% water, the intracellular fluid is 40% of the body weight.
Intracellular fluid is each cell’s own mixture but is the same in all cells.
Intracellular fluid is the largest body fluid compartment of the body by volume.
2) Extracellular fluid
The fluid outside the cell is called extracellular fluid.
Extracellular is about 1/3 of body water.
Extracellular food is about 20% of body weight.
Extracellular fluid contains sodium, chloride, bicarbonate, and other substances such as oxygen, glucose, fatty acids, and amino acids, etc.
The extracellular fluid is further divided into three parts.
1) Interstitial Fluid (ISF),
2) Intravascular fluid (in plasma),
3) Intracellular fluid.
1) Interstitial fluid
Interstitial fluid is located around the cell.
This interstitial fluid is 3/4 of the extracellular fluid.
2) Intravascular Fluid (Plasma)
Fluid and electrolytes move between the interstitial and intravascular fluid and are plasma.
Plasma circulates as the extracellular component of blood.
And it makes up 1/4 of the extracellular fluid.
3) Intracellular fluid
This is the set of fluid that is outside the normal compartment and it is about 1-2 liters.
Which includes cerebrospinal fluid (CSF := CEREBRO SPINAL FLUID), digestive juice (DIAGESTIVE JUICE), MUCOUS.
Explain fluid pressure
Body fluid moves from the interstitial space to the intravascular space.
And this is mainly due to hydrostatic pressure and oncotic pressure.
Hydrostatic pressure is the pressure due to water in vessels.
Oncotic and colloidal pressure is a form of osmotic pressure that is present in the circulatory system and crosses the capillary barrier and enters the circulatory system. If the oncotic pressure is low in a child, fluid accumulates in the tissues and causes an edematous condition. happens
Filtration takes place at the arterial end of the capillary.
Because the hydrostatic pressure is greater than the oncotic pressure, fluid is pushed out of the vessels into the tissue space.
The oncotic pressure at the venous end of the capillary is greater than the hydroxy pressure, causing fluid to back up from the capillary into the interstitial space.
hydrostatic pressure (pa,N/m2)= heigt(m)×density (kg/m3)×gravity (m/s2)
Regulation of fluid balance
Fluid balance in a normal body is normal.
The term fluid balance means intracellular extracellular and plasma and the total water volume of the body is constant. In normal condition the total water volume of the body is responsible for normalizing the homeostasis body.
Regulation of body fluid occurs in the hypothalamus. The hypothalamus receives fluid from the digestive tract.
Regulation of body fluid is done by (ADH := antidiuretic hormone).
Ras (renin angiotensin aldosterone system) is activated to activate the human body when food volume or blood volume is reduced.
When blood volume or body fluid volume decreases, the juxtraglomerular cells that are located in Bauman’s capsule of the kidney secrete a hormone called renin.
Now when the angiotensin hormone is secreted from the liver.
The renin hormone then converts angiotensinogen to angiotensin one.
Now (ACE:= angiotensin covering enzyme) is secreted from the lungs.
which converts angiotensin 1 to angiotensin 2.
Angiotensin 2 works as a vasoconstrictor.
Due to this the blood vessels are constricted and the amount of blood increases and the fluid amount also increases.
And angiotensin 2 activates the adrenal gland and releases the hormone aldosterone from it.
This hormone causes sodium reabsorption, causing water retention.
Due to this, the blood volume also increases and the blood pressure also increases.
Now on the other hand, when the fluid volume in the body decreases.
Then from the posterior pituitary gland of the body. DH (ADH := antidiuretic hormone) ie antidiuretic hormone is released.
Diuretic hormone excretes retained fluid in the body.
Antidiuretic hormone is released when the body is in a condition of dehydration.
Due to this fluid remains in the body.
And the condition of dehydration in the body can be prevented.
Thus, ADH means to keep the fluid balance of the body normal
Both antidiuretic hormone and diuretic hormone play an important role.
Explain the movement of body fluid/fluid exchange processes. (Describe body fluid and process of fluid exchange)
Fluid, electrolyte gas, and small molecules can move freely across a semipermeable membrane. And this semipermeable membrane separates the two compartments.
It carries oxygen and nutrients through the cell and removes waste products from the shell.
And this process can be done by both active transport and passive transport.
An example of active transport is the sodium potassium pump.
In active transport, the substance remains on the surface of the cell and is transported inside the cell.
In an example of passive transport:=
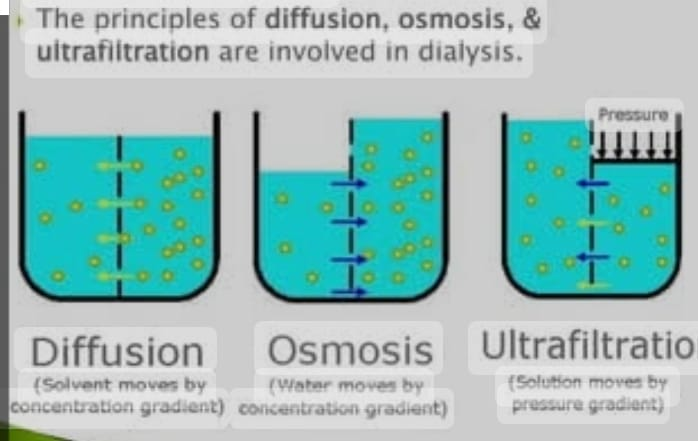
diffusion,
osmosis,
Ultrafiltration
Is included.
Active transport
Sodium potassium pump
The sodium potassium pump is in the cell membrane.
It contains ions.
In this, sodium ions are continuously released out of the cell.
And potassium ions are allowed inside the cell.
And this is mainly done by ATP (ATP:= adenosine triphosphate).
Each ATP is broken down and releases three sodium ions (3 Na+) outside the cell.
And two potassium (2k+) help keep iron inside the cell.
And because of this, the sodium inside the cell is depleted and because of this, an electrical gradient and a concentration gradient are created.
example of passive transport
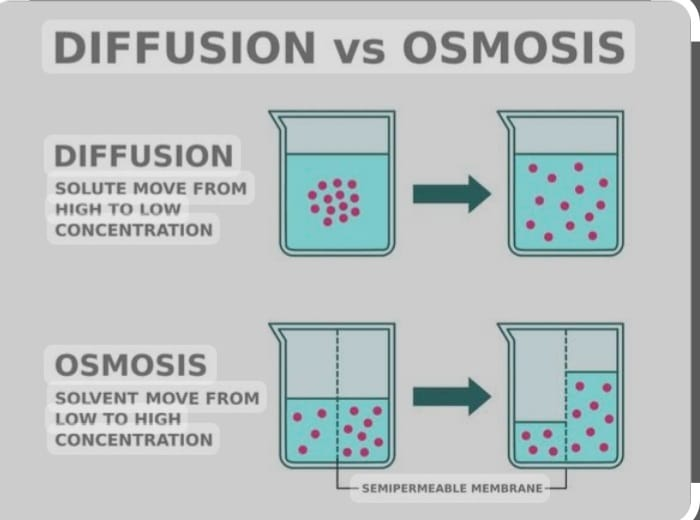
1) Diffusion
Diffusion is a process in which (atoms, ions,
molecules) are transported from higher concentration to lower concentration.
And this moment occurs along a concentration gradient.
And in this diffusion, solution molecules are transported across a semipermeable membrane from higher concentration to lower concentration.
2) Osmosis
Osmosis is the process in which water is transported from a lower concentration to a higher concentration across a semipermeable membrane.
The concentration of a solute is called osmolarity.
3) Filtration
Filtration is the process by which water and other diffusible particles can be moved from the membrane.
And this is mainly because of that.
That one side of a semi-permeable membrane has high concentration and one side has low concentration.
composition of body fluid
1) Water works as the main component of all body components.
2) Water is 45% – 75%.
3) sources of water include:=
ingested foods and liquid.
metabolic water.
4) Solutes are broadly classified into:=
electrolyte are inorganic salts, all acid, bases and some protein.
nonelectrolyte := example glucose, lipids, creatinine, and urea.
Electrolyte has greater osmotic power than nonelectrolyte.
electrolyte composition of body fluid
1)Extracellular fluid:=
Sodium (Na+) is major cation.
2)Intracellular fluid:=
Potassium (k+) is the chief cation.
Phosphate (po4-) is the chief anion.
fluid and electrolyte imbalance
Excessive amount of fluid and electrolytes from the body due to diaphoresis in the skin or due to burns, imbalance of fluid and electrolytes occurs in the body. In fluid imbalance, the level of fluid in the body is abnormal.
Fluid related complications are more common mainly in children. Excessive amounts of dehydration and fluid overload are seen in the elderly.
Fluid volume imbalance is seen due to hypovolemia, normovolemia, maldistribution of fluid, hypervolemia.
Trauma is one of the main causes of any dehydration because trauma causes excessive amount of fluid loss from the body and causes the condition of dehydration.
And another major cause of dehydration is excessive sweating from the body due to which the body fluid is reduced.
Due to continuous dehydration, blood volume decreases, as well as venous return, resulting in hypotensive conditions.
The normal osmolarity of body fluid is 275 to 295 mol/liter.
If the osmolarity of a solution is the same as the osmolarity of the body fluid (275 to 295 mol/liter), it is called an isotonic fluid.
(Isotonic solutions: = osmolarity equal to 275 to 295 mol/liter)
If the osmolarity of a fluid is greater than the osmolarity of the body fluid, it is called a hypertonic solution.
(Hypertonic solutions: = osmolarity is greater than 295 mol/ liter).
A fluid is hypotonic if its osmolarity is lower than that of the body fluid
is called a solution.
(Hypotonic solutions:= osmolarity is less than 275 mol/liter)
- Explain the fluid volume deficit/Dehydration.
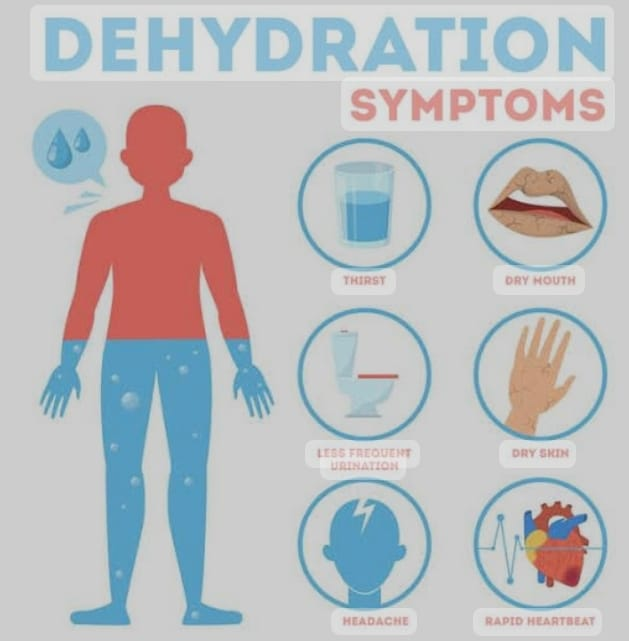
A condition of dehydration occurs in the body when there is too much fluid loss from the body.
A sign for a normal child is that the child feels very thirsty.
If a child is not able to take fluids on his own, his body activates antidiuretic hormone, which regulates osmotic pressure and extracellular fluid in the body.
A condition of dehydration occurs when the body does not have an adequate amount of fluid.
If the same amount of fluid is excreted from the child’s body, the condition of dehydration is created in the body.
Explain the Etiology/cause of Dehydration.
The main reason is excess fluid excretion from the body.
Staying oral on Nile for a long time.
Internal bleeding or hemorrhage.
Sweat profusely.
Due to taking any diuretic therapy.
Due to drainage from any hole.
diarrhea,
Gastrointestinal
instant,
vomiting,
If you have difficulty swallowing,
systemic infection,
renal failure,
fever,
Diabetic acidosis
Burns,
Frequent enemas,
Ileostomy (opening in the ileum),
chronic illness,
cystostomy,
Low fluid intake.
Diabetes
insipidus.
certain types of medicine,
Accident or trauma,
Explain the clinical manifestation/sign and symptoms of the Dehydration
(State the symptoms and signs of dehydration).
very thirsty,
weight loss,
Rapid, weak pulse,
low blood pressure,
Decreases tear formation,
dry skin,
dry mucus membrane,
Poor skin turgor,
Increase body temperature,
decreased urine output,
dehydration,
dark urine,
Constipation,
dry mouth,
Changes in mental status,
weakness,
Sunken Eye Balls,
restlessness,
dry ice,
Decreases jugular venous pressure.
Explain the diagnostic evaluation of the Dehydration.
History collection, physical examination.
Blood urea nitrogen (BUN) level,
Increase hematocrit level.
Increases the specific gravity of urine greater than 1.030.
Explain the medical management of the dehydration.
A dehydrated child’s main priority is to replace fluids in his body
So provide intravenous fluid to the child.
If the child has suffered any kind of injury or trauma and is losing a lot of fluid, apply pressure on the place where the blood is being lost so that excessive amount of blood loss can be prevented.
Give isotonic fluid to the child (ex: ringer lactate, 0.9% normal saline).
Assessment
Assess the child for any signs and symptoms of dehydration.
Assess the child’s skin integrity.
Check the child’s weight daily.
Child’s intake and output should be done every eight hours.
To assess the child’s vital signs.
Assessing the child’s mucus membrane.
Assess the child’s pulse and temperature.
Nursing diagnosis
1) Fluid volume deficit related to fluid loss or inadequate fluid intake.
2) Decrease cardiac output related to insufficient blood volume.
3) Impaired oral mucous membrane related to inadequate oral secretion.
4) ineffective tissue percussion related to insufficient blood volume.
5) Constipation related to decrease body fluid.
nursing interventions
To check vital sign of child.
Ask the child to ingest more fluids.
Checking the child’s intake output.
Provide oral fluids if the child is able to take oral fluids.
Ask the child to take fluids little by little.
If the child is unable to intake fluids orally, provide fluids through the parenteral route.
Provide fluid to the child like ringer lactate, 0.9 normal saline and dextrose 5% etc.
If the child’s dehydration is due to severe diarrhea
Providing antidiarrheal medicine to the child.
If the child is dehydrated due to vomiting, provide antiemetic medicine.
If the child has any kind of infection, provide him with antibiotic medicine.
Checking the child’s level of consciousness like anxiety, restlessness, confusion etc.
Checking the child’s skin integrity.
Changing the position of the child every two hours.
If the child has a mild amount of dehydration, the dehydration can be removed by providing treatment at home.
If a child is dehydrated in a severe amount, he needs immediate hospitalization.
complications
If dehydration is not treated immediately, the amount of blood in the body may decrease and due to this the function of the main organs of the body may also be altered. Like brain, kidney, heart, these organs cannot function properly.
prevention
Instruct the child to maintain proper fluid intake to prevent dehydration and increase fluid intake in high-risk children such as infants.
Child education
Providing health education about the signs and symptoms of dehydration to children and their family members.
Ask the child to intake an adequate amount of fluid.
Provide health education to the child or ingest frequent amounts of fluid.
Providing education to the child or when doing excessive hard work, intake of fluid little by little in between so that the condition of dehydration can be prevented.
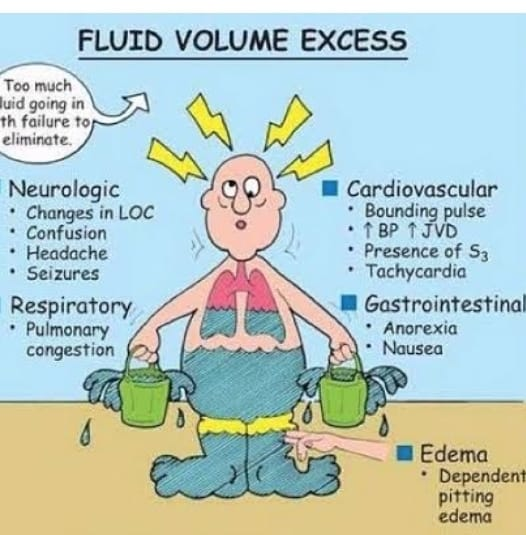
- Explain/Define hypervolemia. (Define hypervolemia)
Hypervolemia is called fluid overload or overhydration.
This is a condition in which a large amount of fluid collects in the body.
Due to the fluid overload of the child, a large amount of fluid remains in the body and due to this the electrolyte and red blood cells are diluted.
The condition of hypervolemia occurs when the amount of sodium and water in the body becomes more and due to this the condition of hypervolemia occurs.
Explain the Etiology/cause of hypervolemia.
Due to providing too much IV fluid.
Due to heart failure condition.
due to corticosteroid therapy.
Due to low intake of protein in diet.
Syndrome of Inappropriate Antidiuretic Hormone.
Renal failure.
Cirrhosis of liver,
Cushing’s syndrome,
Low dietary protein intake,
Excessive irritation of wounds and cavities.
Due to excessive fluid intake.
Explain the clinical manifestation/sign and symptoms of the hypervolemia.
Changes in Vital Sign,
ascites,
increased blood pressure,
As the pulse rate increases,
increased respiration,
Distended neck veins,
Edema in feet and legs,
Urine is diluted,
difficulty breathing,
weight gain,
Increased urine output.
Explain the Diagnostic evaluation of hypervolemia.
History Taking,
Physical Examination,
Decrease in blood urea nitrogen level (BUN),
Decreased hematocrit level,
Decrease in specific gravity of urine.
Explain the complication of the hypervolemia.
heart failure,
pulmonary edema,
Organ failure.
Explain the medical management of the hypervolemia
drug therapy,
diet therapy,
Drug therapy
Diuretic drug,
Provide diuretic (Frusemide),
Diet therapy
Ask the child to take small amounts of fluids.
Advising on a low-salt diet.
Ask the child to drink less fluid.
Oxygen therapy
Provide adequate oxygen if breathing is difficult.
Positioning
Provide semi-fowler position to the child for easy breathing and provide proper oxygen therapy if the child has difficulty breathing.
Explain the nursing management of the hypervolemia.
assessment
Assess the child’s fluid amount.
Assessing child’s intake output.
To see whether the child is in the body or not.
To assess the child’s vital signs.
Check child’s weight daily.
Nursing management
1) Excess fluid volume related to excessive fluid intake or inadequate excretion of body fluid.
2) Decrease cardiac output related to excess work on the heart from fluid retention.
3) ineffective tissue percussion related to dependent oedema.
4) Risk for Impaired gas exchange related to fluid in the lungs.
nursing interventions
To provide treatment as per the child’s need.
Check the child’s weight daily.
Checking the child’s intake output.
To check vital sign of child.
Provide the child with a semi-fowler position.
Changing the position of the child every two hours.
Provide skin care to the child as needed, do not massage the skin with too much force.
Tell the child to reduce sodium intake.
To elevate the extremities which are in ED.
Provide prescribed diuretic medicine to the child.
Check child’s intake output.
prevention
The easiest way to prevent the condition of fluid overload is to avoid excessive fluid intake.
Checking the child’s fluid amount while providing IV fluid.
patient education
Intake of low sodium food.
Provide diuretic therapy.
To provide education for the child to have low fluid intake.
Check the child’s weight daily.
- Electrolyte balance
Electrolytes are liquids that have a positive (+) or negative (-) charge and conduct electrical impulses. In addition, they are solid substances in body fluids and water that are present in body fluids and blood. Dissolves and forms solutes.
Some solutes are electrolytes and some solutes are non-electrolytes.
An electrolyte is a chemical that dissolves in water and creates an electric current.
Some of them are intracellular and some are extracellular.
Electrolyte A ( milliequivevallent/liter) meq/liter and Meq/dl
Ma is measured.
There are generally two types of electrolytes.
1) Cation ( It has positive electric charge +ve),
2) Anion ( It has negative electric charge -ve)
Explain/define electrolyte imbalance.
Sodium, potassium and calcium play an important role in the transmission of nerve impulses.
Any increase or decrease in any of these substances leads to muscle stimulation and imbalance.
sodium imbalance
Sodium imbalance occurs when the concentration of sodium in the plasma is increased or decreased.
Normal sodium concentration is 135 to 145 meq/liter.
- Explain/ define sodium deficit (hyponatremia). Define hyponatremia.
Sodium is an extracellular electrolyte. It plays an important role in water distribution. Sodium plays an important role in muscle contraction and transmission of new impulses.
The normal concentration of sodium in the blood is 135 to 145 meq/liter.
Hyponatremia is a metabolic condition in which the level of sodium in the blood is lower than the normal sodium level.
(In hyponatremia sodium concentration is less than <135 meq/liter).
Three types of hyponatremia
1) Euvolemic hyponatremia.
2) Hypervolemic hypo natremia.
3) Hypovolemic hyponatremia.
1) Euvolemic hyponatremia.
This increases the water content of the body.
But the sodium level is constant.
And this condition is caused by chronic health conditions, cancer and certain medicines.
2)Hypervolemic hyponatremia.
Both water and sodium content increases in this body.
But the amount of water is more.
Too much water dilutes sodium and lowers sodium levels.
This is mainly due to kidney failure, heart failure or liver failure.
- Hypovolemic hyponatremia
In this, the level of water and sodium from the body decreases.
But sodium levels are lost more than water.
Explain the Etiology/cause of hyponatremia.
Due to drinking too much water during exercise.
Vomiting.
Hormonal imbalance. Diarrhea.
Due to low amount of thyroid.
Syndrome of Inappropriate Antidiuretic Hormone (SIADH).
Due to excessive thirst.
Due to Oral on Nile (NPO).
Lithium therapy.
Diuretic.
Some medicine like diuretic, anti depression, pain medication.
Chronic or severe dehydration.
Due to kidney failure.
Due to kidney disease. Congestive heart failure.
Burns.
A low sodium diet can lead to hyponatremia.
Due to drinking too much water during exercise.
Climate.
Explain the clinical manifestation / sign and symptoms of the hyponatremia
(State the symptoms and signs of hyponatremia)
headache,
Muscle weakness.
feeling tired
Restlessness.
irritation.
Decrease in interest.
Muscle twitching and weakness.
Tachycardia (increases heart rate more than 100 beats/min).
Nozia.
Vomiting.
Abdominal Cramps.
Decreased urine output.
Postural hypotension.
Loss of appetite.
Mental confusion.
Delirium.
Coma.
Shock.
Confusion.
to be startled
Coma.
Cellular swelling with cerebral edema leading to headache.
Explain the Diagnostic evaluation of the Hyponatremia (tell the symptoms and signs of hypernatremia).
History Taking,
Physical Examination.
serum electrolyte level ex:= sodium, potassium, chloride.
serum sodium <135 meq/liter. Decreases urine specific gravity. Decreases serum osmolarity. Urine sodium >100 meq/24 hours.
Explain the medical management of the Hyponatremia
Cancer is the cause of some hyponatremic conditions.
So providing radiation, chemotherapy, and surgery to remove it.
So that the sodium imbalance can be corrected.
If there is a mild hyponatremia condition, it can be treated through diet, lifestyle, and medication.
If there is a condition of severe hyponatremia, treat the child with electrolyte and fluid administration.
Administer a solution such as 0.9% normal saline fluid to the child.
Provide steroid therapy to reduce intracranial swelling.
Checking the child’s intake output and daily weight check.
If the child is lethargic, provide supplementary oxygen.
Provide IV fluid to the child as needed.
Explain the nursing management of the Hyponatremia.
Take a proper health history of the child to find out the cause of the child’s condition.
Ask the child to take sodium rich food.
Provide education to child to include sodium rich fluid in diet.
If the child’s sodium level does not increase to 12 meq/liter in 24 hours, administer Ringel Latest and isotonic solution intravenously to the patient.
Maintain intake output chart of child every 24 hours.
Check the child’s weight daily.
Administer hypertonic normal saline to the child.
If the child has a fluid restriction, ask the child to take small amounts of fluids.
Checking the child’s consciousness level.
To see if the child is in a state of confusion, lethargy or not.
Assessing whether the child is oriented to time, place and person.
Assess the child’s deep tendon reflexes, muscle tone and strength.
prevention
Treating conditions that cause low sodium levels early.
To alert the person taking diuretic medicine for adverse signs and symptoms ex:= hyponatremia for taking diuretic medicine.
A child who exercises excessively should drink as much water as needed, which is lost from the body through sweating, and should not drink more than one liter of water in an hour.
Ask the child to take sodium rich food.
Ask the child to drink enough water.
Tell the child’s parents to drink plenty of water but be careful not to cause fluid overload and ask the patient to take a sodium replacement diet.
- Explain/ define sodium excess hypernatremia.
Hypernatremia is an electrolyte imbalance in which the amount of sodium in the blood increases.
When the amount of fluid in our body is less and if the salt is more and if the renal function is less, then the amount of sodium in the body increases and the condition of hypernatremia arises.
The normal sodium level in body is 135 to 145 meq/liter.
If the value of sodium in the body exceeds the normal value, it is called hypernatremia.
(In hypernatremia the level of sodium is more than >145 meq/liter).
Explain the Etiology/cause of the hypernatremia
Due to loss of fluid from the body,
vomiting,
diarrhea,
swatting,
high fever,
dehydration,
Due to not drinking enough water,
Some types of drugs like steroids, licorice and certain blood pressure lowering drugs,
of some kind
Due to endocrine diseases such as diabetes and aldosteronism,
Due to excessive salt intake.
Due to excessive use of sodium bicarbonate.
Due to uncontrolled diabetes.
Due to heavy exercise.
Due to renal dysfunction.
Osmotic diuretic.
Explain the clinical manifestation/sign and symptoms of Hypernatremia.

feeling thirsty
Mucus membrane becoming dry and sticky.
Restlessness and agitation.
Decreased urine output.
Weight loss.
feeling weak
The tissue is firm.
Disorientation.
Tachycardia.
Confusion and personality change.
Decreased level of consciousness.
Loss of appetite.
Nozia.
Vomiting.
Fluid and electrolyte imbalance.
Pulmonary edema.
In a pitting eddy.
Abnormal skin turgor.
Postural hypotension.
Difficulty breathing.
Explain the Diagnostic evaluation of hypernatremia.
history taking,
Physical Examination,
serum electrolyte:=serum sodium level >145meq/liter.
High serum osmolarity.
Increases urine specific gravity.
Explain the management of the hypernatremia.
Infusing the child hypotonic electronic solution intravenously.
Ask the child to have adequate water intake.
Provide diuretic medicine to the child.
Maintaining intake output chart of child.
Monitor the fluid loss or gain of the child who is at risk of increased sodium level in the body.
To maintain and assess child intake output chart.
Ask the child to take a low sodium diet.
Noticing the amount of thirst the child feels.
To see if the child’s body temperature is elevated or not
To see if there is any alteration in the vital sign of the child.
Checking the child’s level of consciousness.
Checking the child for headache, nosia, vomiting and any changes in the child’s vital signs.
Monitor child’s intake output chart and assess sodium level.
If the child has any convulsions, keep the bed down and keep the siderails high on the bed.
Ask the child to drink plenty of water if he has diabetes insipidus.
Tell the child to avoid sweet foods, salty tablets, sweet liquids and spot drinks.
Teach the child to drink a lot of water during exercise.
Tell the child to drink plenty of water while taking diuretic medicine.
Assess whether the child’s sodium level increases or decreases.
Maintain aseptic technique while providing intravenous fluid.
Careful monitoring of patients with flu or uncontrollable warming.
To condition hydration and prevent immediate hospital admission of a person who is vomiting profusely.
Checking whether the patient is oriented to time, place and person.
Providing reassurance to the patient.
- Explain/Define of hypokalemia

Potassium is the major intracellular cation.
About 98% of the body’s potassium is located inside the cell.
Potassium enters the cell during the formation of new tissue and during the conversion of glucose to glycogen. As tissue breaks down, potassium is released from the cell, mainly due to any trauma, dehydration or starvation. is
Potassium acts as an important electrolyte in the conduction of new impulses and the contraction of skeletal and smooth muscles.
Normal potassium level is 3.5 to 5.5 meq/liter.
Hypokalemia A metabolic condition in which the concentration of potassium is less than the normal potassium concentration is called hypokalemia.
In the condition of hypokalemia, the potassium level is less than 3.5 meq/liter.
(In hypokalemia potassium intake is less than < 3.5meq/liter)
Explain the Etiology/cause of Hypokalemia.
Due to low dietary intake of potassium.
Due to excessive loss of potential through the kidney.
Due to increased activity of aldosterone.
vomiting,
Prolong g .i . Saxon
Due to excessive sweating.
Due to excessive fluid loss through the gastro-intestinal tract.
Due to loss of potassium from the body while giving diuretic medicine.
Due to any trauma and fluid loss.
Due to a tumor in the adrenal gland.
Eating disorder.
Diabetic ketoacidosis.
Treatment of acidosis,
metabolic alkalosis,
Aldosteronism or Cushing’s syndrome.
renal tubular acidosis,
Medication: = potassium losing diuretic, digoxin and corticosteroids.
Antibiotics := amphotericine B, carbenicillin and gentamicine.
Explain the clinical manifestation/sign and symptoms of the Hypokalemia.
dizziness,
Abnormal heart rhythm.
feeling tired
Lethargy (reduced allergy).
Confusion.
Loss of appetite.
Nausea and vomiting.
Orthostatic hypotension (dizziness that occurs when sitting or lying down).
Cardiac arrest.
hyporeflexia,
Paraesthesia (numbness and tingling),
No hunger.
Constipation.
Muscle weakness.
Pain.
Polyuria
nocturia,
Excessive thirst,
Restorative distress,
paralysis,
(Rhabdomyo lysis := breakdown of muscle tissue).
Explain the Diagnostic evaluation of the Hypokalemia.
history taking,
Physical Examination,
serum potassium <3.5meq/liter.
Metabolic alkalosis.
24 hour urine potassium excretion test.
Ecg changes.
test for kidney function (BUN and creatinine), glucose, magnesium, and phosphorous.
Explain the medical management of the Hypokalemia.
Mild to moderate levels of hypokalemia can be corrected with oral potassium supplementation.
If the child has a severe potassium deficit, he needs to take potassium intravenously. Daily 40 to 80 meq/day.
Ask the child to take potassium rich diet orally.
Ex := heavy
banana,
strawberry,
Mellon,
organ,
milk,
chicken,
beans,
Broccoli,
Carat,
potatoes,
Raisins
raisins,
raisins,
Take all these foods that are rich in potassium.
If the child cannot take it orally, slowly infuse it with intravenous potassium chloride (KCL).
To see whether the child is outputting adequate amount of urine or not.
Checking the child for signs and symptoms of hypokalemia.
Monitoring the Ecg.
In general, a child needs a low-sodium diet and a high-protein diet.
The average amount of potassium an adult should consume is 50 to 100 meq/day.
Explain the nursing management of the Hypokalemia.
Proper health history and health assessment of the child to find out the cause of the condition of hypokalemia.
Administer potassium replacement therapy to the child.
Provide potassium orally by diluting it in proper water or juice.
Checking ivy site properly.
Assess child’s intake output chart every hour.
To check vital sign of child.
Checking the child’s heart rate and rhythm.
To assess whether the child has toxicity of any digitalis group (dogitalis group) medicine or not.
Checking the child’s potassium level when taking a diuretic medicine.
To check the child’s vital sign and pulse.
Ask the child to take potassium rich food.
When administering potassium intravenously, it should not be too fast (not fast more than 10-20meq/liter) to maintain proper infusion.
To monitor the child’s muscle tone and strength.
Monitor child’s bowel sound.
Maintaining intake output chart of child.
To ensure that the child’s potassium level does not fall, the child should get enough potassium in the diet.
- Explain/Define of hyperkalemia.

Hyperkalemia is a condition in which the potassium level in the body or blood exceeds the normal potassium level.
Normal potassium level is 3.5 to 5.5 meq/liter.
In hyperkalemia potassium level is greater than 5.5meq/liter.
Explain the Etiology/causes of Hyperkalemia.
Due to excessive consumption of salt containing potassium.
The intake of potassium in the body is high and if the kidney cannot excrete that amount of potassium from the body.
Due to excessive use of oral or intravenous potassium supplementation.
Acute renal failure.
Chronic renal failure.
Adrenal gland
Insufficiency.
Glomerulonephritis: Infection and inflammation of the glomerulus, the filtering part of the kidney, is called glomerulonephritis.
Metabolic acidosis.
Rejection of kidney transplant.
Lake of aldosterone.
Additions Decs.
Type 1 diabetes. Burns.
Hemolytic conditions.
Rhabdomyolysis
(Breakdown of muscle tissues) from drugs, alcoholism, coma, or certain infection.
of some kind
Medications such as:
ACE inhibitors,
Potassium chloride,
Heparin,
captopril,
NSAIDs,
Use of potassium sparing diuretic (ex:= spironolactone).
Explain the clinical manifestation/ sign and symptoms of Hyperkalemia.
Irregular heartbeat,
low blood pressure,
chest pain,
Erythemias,
abdominal pain,
nozia,
vomiting,
Palpitation,
Muscle twitching and cramps.
Diarrhea.
Cardiac arrhythmia.
Ecg Changes.
Muscular weakness and paralysis occur.
Confusion and coma.
Ventricular dysrhythmia and cardiac arrest.
Respiratory failure.
Tingling and numbness sensation.
Cardiac arrest.
Anemia.
Muscle weakness.
Explain the Diagnostic evaluation of Hyperkalemia.
history taking,
Physical Examination,
Serum potassium levels are (greater than) > 5.5 meq.
Metabolic acidosis-serum pH falls below 7.35.
Ecg changes:=
elevated T waves,
widened qrs complex,
Prolong pR interval,
flattened or absent p waves,
Depressed St segment.
Explain the medical management of Hyperkalemia.
Treatment of hyperkalemia depends on its cause, severity of hyperkalemia, and its symptoms, and the child’s overall health.
A child should take potassium in the diet in a small amount.
Continuous cardiac monitoring of the child should be done.
Intravenous fluid should be provided properly to the child.
Continuous ECG monitoring of the child should be done.
Medicines which reduce the amount of potassium in the body should be provided to the child.
If the child has severe hyperkalemia, dialysis is also necessary.
If the amount of potassium is not reduced by medication, calcium gluconate should be administered to the child intravenously.
Sodium bicarbonate should also be provided to the child to allow potassium to shift temporarily into the cells.
The child’s serum potassium level should be checked continuously.
Medications that increase the amount of potassium in the body should be discontinued.
The child should be administered 25% or 50% glucose and insulin intravenously to allow potassium to re-enter the cell from the extracellular space.
Intravenous calcium should be provided for a short period of time to reduce the effects of hyperkalemia to protect the heart and muscles.
Provide diuretic medicine to the child.
Explain the nursing care for hyperkalemia.
Analyzing Child No Intake Output Chart.
Avoiding potassium to the child by oral or parenteral route.
Avoiding the child to take potassium rich food eg fruit juice.
Assess the child’s pain level and provide comfort measures.
To assess the child’s vital signs.
To check the child’s heart rhythm.
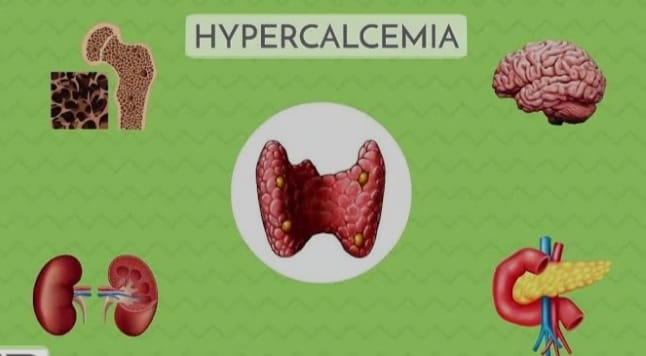
Explain the calcium imbalance.
Calcium is the most abundant mineral in the human body.
This is good for critical and health.
In body normal calcium level is 9 to 11mg/dl or 4.5 to 5.5 meq/liter.
Calcium is a mineral that is mainly found in bones and teeth.
More than 99% of calcium is found in bones. Calcium is an important component of bones and teeth. Calcium plays an important role in nerve impulses and contraction and relaxation of muscles, including cardiac muscles.
Calcium plays an important role in blood clotting, muscle and nerve function.
- Explain/define hypocalcemia

When there is not enough amount of calcium in the body and blood, it is called hypocalcemia.
Hypokalemia A condition in which the level of calcium in the body falls below the normal level is called hypokalemia.
Normal calcium level is 4.5 to 5.5 meq/liter, or 9 to 11mg/dl.
(In hypocalcemia the level of calcium in blood is less than 9 mg/dl or 4.5 meq/liter.)

Explain the Etiology/cause of Hypocalcemia.
Thyroid gland due to damage due to any disease or surgery
be underactive.
Due to excessive binding of calcium to iron.
Large amount of citrate blood.
Hypoalbuminemia
(Decreased albumin level).
Alkalosis.
Hyperphosphatemia (high amount of phosphate).
Due to not getting enough calcium in the diet.
Due to insufficient intake of vitamin D in the diet.
Due to chronic renal failure.
Due to non-absorption of proper amount of calcium in the gastrointestinal tract.
Intestinal fistula. (Fistula means abnormal connection of two organs).
Crohn’s Disease,
Chronic inflammation
Bowel Disease.
Due to deficiency of parathyroid hormone and vitamin D.
Severe burns or infection. Osteoporosis (this is a bone condition in which the bone is weak and fragile that breaks down easily).
Due to infection of the pancreas
Kidney failure.
Due to low level of magnesium in blood.
Certain medications such as diuretics, estrogen replacement therapy, glucose, calcium channel blockers, insulin, and magnesium are responsible for conditioning hypocalcemia.
Therefore, nutrition cannot be measured in adequate amounts.
Biphosphate therapy.
Certain types of leukemia (blood cancer) and blood disorders.
Toxic shock syndrome.
Explain the clinical manifestation/ sign and symptoms of Hypocalcemia.
Osteoporosis (bones become weak and fragile that break down easily due to calcium deficiency).
Anxiety and irritability,
Pathogenic fracture (any kind of disease that weakens the bone and therefore can break down easily).
Tetany (Tetanus := muscle spasm due to calcium deficiency and underactive parathyroid gland).
There is a tingling sensation around the nose and on the tips of the fingers.
Tingling and numbness sensation also occurs in hands, feet.
Muscle spasm.
Heart rate is irregular and increases.
Nausea, vomiting.
Increase in blood pressure.
Changes in mental status.
Diptendon reflexes become hyperactive.
The size of the gastrointestinal tract increases.
G.I. Diarrhea and abdominal cramps occur due to the increase in the size of the track.
Cardiac arrhythmias.
Difficulty in speech due to laryngospasm (vocal cord spasm).
Hypotension.
Dry skin.
Dermatitis (inflammation of the skin).
Skin hyperpigmentation.
Chvosticks sign :=
This sign is seen when the amount of calcium in the body is in a low amount, in which facial muscles twitch when a person is tapped on the cheek and in front of the ear.

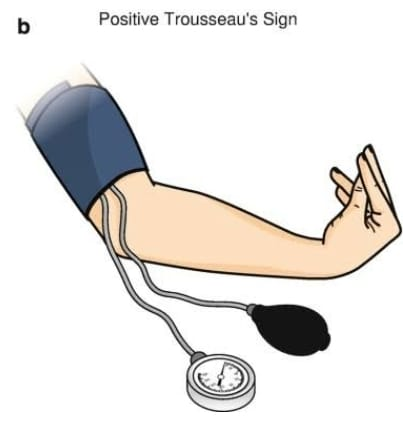
Trousseau symbol:=
This sign is seen when there is a condition of hypocalcium in the body.
Tema carpopedal spasm This involves severe spasm of the hand muscles.
Neurological symptoms like depression, personality change, seizures, loss of movement control.
Spasm in body muscles.
Explain the Diagnostic evaluation of the Hypocalcemia.
history taking,
Physical Examination.
Serum sodium level is less than <8.5 mg/dl.
Low platelet count.
Increases parathyroid hormone levels.
Ecg shows lengthened Qt interval, Prolong St segment, arrhythmias.
There are also changes in serum protein levels as serum calcium becomes less bound to albumin.
Explain the medical management of the Hypocalcemia.
A child who is deficient in calcium should take children’s calcium supplementation.
Taking vitamin D in proper amount.
Provide intravenous calcium gluconate or calcium chloride to a child with acute or severe hypocalcemia.
Calcium supplements should be provided one to two hours after meals to increase intestinal absorption.
If the child has severe hypocalcemia with cardiac arrhythmia and tetany, calcium salts should be provided to the child immediately.
Provide calcium carbonate in the initial stage of hypocalcemia.
Calcium carbonate at 250 or 500 mg/tablet.
Provide calcium gluconate and calcium chloride to the child.
If there is any serious condition, provide calcium chloride to the child.
Provide calcium carbonate in the initial stage of hypocalcemia.
Vitamin D therapy should be taken in proper amount.
Consuming foods rich in vitamin D, such as milk or dairy products, may allow calcium to be properly absorbed.
Explain the nursing management of the Hypocalcemia.
To check the child’s vital signs and blood pressure.
Administer calcium intravenously to the child.
Monitor the child’s airway and respiratory status.
Provide education to the child and his family members about sources of calcium.
If the child has undergone thyroid or neck surgery, carefully monitor the child for signs and symptoms of hypocalcemia.
Ask the child to do proper exercise.
Providing work and quiet environment to the child.
Keeping the child’s bed at a low level and providing a side rail.
Tell the child to avoid caffeine intake.
Smoking reduces the amount of calcium from the body so tell the child to avoid smoking.
Ask the child to take proper calcium diet.
- Explain/Define of hypercalcemia.
Hypercalcemia is a condition in which the level of calcium in the blood and body is
If it rises above 11 mg/dL (11mg/dl) or 5.5 equivalents per liter (5.5 meq/liter), it is called hypercalcemia.
In normal level serum calcium level is (9 to 11 mg/dl or 4.5 to 5.5meq/liter).
In hypercalcemia the level of calcium is greater than > 11mg/dl or 5.5 meq/liter)
Explain the Etiology/cause of Hypercalcemia.
Over active parathyroid gland.
Excessive release of calcium from bone due to bone cancer.
Dehydration, loss of water from the body.
multiple myeloma,
multiple fractures,
immobilization,
Intake more calcium in the diet.
Prolong bed rest.
Excessive absorption of calcium due to high amounts of vitamin D.
Tumors that destroy bone.
Excessive calcium and vitamin D intake.
Excessive consumption of milk products.
Chronic kidney failure.
Alkalosis.
Excessive dietary intake of calcium.
Vitamin D increases the amount of calcium due to absorption.
Chronic kidney disease.
Use of certain medications such as thiazide diuretics.
Inherited kidney or metabolic conditions.
Explain the clinical manifestation/sign and symptoms of the hypercalcemia
Heart rate increases.
Blood pressure increases.
Muscle weakness.
Loss of appetite.
Bone pain and pathological fractures.
Constipation.
Vomiting.
Abdominal pain.
Bodyack.
Decreased ability of blood to clot.
Nausea and vomiting.
Passing too much urine (polyuria) and feeling very thirsty (polydipsia).
Feeling tired (lethargy).
Stones are formed in the kidney and waste products build up in the body.
Confusion.
Heart block.
Difficulty speaking.
Very sleepy.
headache.
Irritability.
Depression.
Memory is impaired.
Mood swings.
Confusion.
Renal Stones.
Decreases dip tendon reflexes.
Coma.
Explain the diagnostic evaluation of the Hypercalcemia.
History taking
Physical Examination.
Serum calcium level is greater than 10.5 mg/dl.
ECG shows signs of heart block. Shortened QT interval and ST segment.
X-ray may reveal the presence of osteoporosis, bone cavitation or urinary calculi.
Urinalysis.
Decreased parathyroid hormone.
Salkovich urine test shows increased calcium precipitation.
Explain the medical management of the Hypercalcemia.
If a child has a severe hypercalcemia condition, it needs immediate hospitalization.
Maintain the hydration status of a child with severe or acute hyperkalemia by providing normal saline.
If the child has nosia, vomiting, polyuria, provide normal saline.
Provide the child who is taking diuretic medicine or Lasix (Frusemide) so that the amount of calcium is excreted from the body.
Avoid using medications that bind calcium and release it from the body.
Ask the child to undergo ambulation.
Ask the child to provide plenty of fluids.
Providing reinsurance to the client and his family members.
Calcitonin helps lower serum sodium levels.
Biphosphate helps to absorb the amount of calcium in the bone.
Administer glucocorticoid.
Dialysis.
Explain the Nursing management of the Hypercalcemia.
To maintain intake output chart of child.
Ask the child to increase fluid intake.
Telling the child to take a low calcium diet, intake.
To provide reassurance to the parents and family members of the child.
Ask the child to increase fluid intake.
If the child’s serum calcium level rises above 5.5 meq/liter, check the child for cardiac arrhythmias.
If the child is using a diuretic or normal saline, check the child for signs and symptoms of heart failure.
If the child is receiving a glycoside, observe for toxicity such as loss of appetite, nosia, vomiting, bradycardia, etc.
If the child’s bone is weak, change the child’s position carefully.
If the child is bedridden, change the child’s position frequently and ask the child to do range of motion exercises.
To check vital sign of child.
Assess the child’s respiratory status.
To check the child’s heart sound.
Asking the child to do physical activity to maintain no weight.
Ask the child to take enough fiber-rich food to relieve constipation.
Ask the child to take low calcium diet and fluid intake.
Asking the child to do activities so that calcium can be reduced from the body.
Introduction of magnesium
Magnesium is an essential component that regulates over 300 enzymes that are responsible for many body functions.
Magnesium works as a cofactor for many body enzymes.
Magnesium plays an important role in the metabolic activity of the body.
Magnesium is important for the relaxation of smooth muscles, such as those surrounding the bronchial tubes, and skeletal muscle contraction, and for neurons in the brain.
Magnesium converts what is in the body into energy and helps build up in protein and maintains calcium levels in the blood.
Magnesium prevents cardiovascular diseases and regulates irregular heart beat.
Magnesium helps to prevent the condition of heart attack.
Magnesium prevents the condition of stroke.
(The normal value for serum magnesium is 1.5 to 2.5 meq/liter)
or
(1.8-3.0mg/dl)
If in magnesium
Hypomagnesia if there is an imbalance
Or called hypermagnesium.
- Explain/ define Magnesium deficit (hypomagnesemia).
Hypomagnesemia is an electronic disturbance.
Those who have abnormally low levels of magnesium have less than normal magnesium levels in the blood.
(The normal adult value of magnesium is 1.5-2.5meq/liter.)
(In hypomagnesemia level of magnesium is less than <1.5 meq/liter.)

Hypomagnesemia is an electronic disturbance.
Those who have abnormally low levels of magnesium have less than normal magnesium levels in the blood.
(The normal adult value of magnesium is 1.5-2.5meq/liter.)
(In hypomagnesemia level of magnesium is less than <1.5 meq/liter.)
Explain the Etiology/cause of Hypomagnesemia.
Due to excessive loss of magnesium from the body.
Due to low magnesium intake.
Due to protein calorie mal nutrition.
Due to lack of proper absorption in intestine.
due to malnutrition or starvation.
Due to excessive fluid loss from the body.
Due to excessive excretion of urine from the body.
Severe diarrhea.
Crohn’s disease.
Due to giving too much diuretic.
Use of certain medications including amphotericin,
Cisplatin,
Aminoglycoside.
Gastrointestinal fistula.
Renal damage.
Total parenteral nutrition.
Excessive urination (polyuria).
Alcoholism.
Malabsorption.
Due to high blood calcium level in the body.
Hyperaldosteronism.
Explain the Clinical manifestation/sign and symptoms of Hypomagnesemia
Positive Trousseau’s and Chovostek signs.
Loss of appetite.
Nozia.
Vomiting.
weakness.
from the app.
Muscle weakness.
Paraesthesia
(Tingling or numb sensation).
Movement is slow and involuntary.
Irritability,
tetanus,
Leg and foot cramps.
to be startled
Trams,
Ataxia: Absence of normal coordination.
Carpopedal spasm (spasm in hand muscles).
Depression.
Irritability.
Psychotic behavior.
to be startled
Vertical nystagmus := Involuntary movement of the eyeball.)
Cardiac dysrhythmias.
Extreme agitation.
Insomnia
Delirium.
Auditory and visual hallucinations.
Explain the diagnostic evaluation of the Hypomagnesemia.
History taking.
Physical Examination.
Serum magnesium lower than 1.5 meq/liter.
Nuclear magnesium resonance spectroscopy.
Electrocardiogram may show:=
A.) Prolong PR and QT interval,
B) widening QRS,
c)ST segment depression.
D)flattened T waves.
E) prominent U wave.
Explain the medical management of the Hypomagnesemia.
Treatment of hypomagnesemia is provided based on its deficiency and clinical effect.
The goal of treatment is to identify and eliminate the cause of hypomagnesemia and replace the amount of magnesium in the body.
Provide oral magnesium replacement to children with mild symptoms.
Which is a very black sign to the child and
Intravenous magnesium A replacement for those with symptoms.
And asking the child who has a condition of mild hypomagnesia to take a diet rich in magnesium.
Like := green leafy vegetable,
Nuts (almonds),
Legumes (legumes),
Wall Gain (whole grain),
sea food,
Ask to take magnesium rich diet like etc.
Magnesium preparations such as magnesium oxide should be taken as they contain higher amounts of magnesium.
Provide magnesium sulfate intravenously (10 to 40 meq/liter) to the child who has severe hypomagnesemia condition.
If the child
cardiac arrhythmia,
Obstetrics problem,
Electrolyte disturbance,
Asthma.
If there are conditions like etc. then intravenously provide magnesium sulphate.
Explain the nursing management of the Hypomagnesemia.
Ask the child to take magnesium rich food.
Monitoring the child’s level of consciousness.
Monitoring the child’s breathing pattern.
To assess the changes in the E.C.G. of the child.
Advise the child to avoid excessive amounts of diuretics and laxatives.
Monitor the child’s bowel sounds and abdominal distension.
Check the child’s reflexes before infusing magnesium.
Provide work, quiet and dark room to the child.
Provide a low bed to the child and keep its side wells high to prevent fall down if the patient faints.
- Explain/ define hypermagnesemia: (Define hypermagnesemia).
Hypermagnesia is an electronic imbalance in which magnesium levels in the body exceed 2.5 meq/liter.
A normal level of magnesium in the body is important for the function of the heart and nervous system.
(In hypermagnesemia the level of magnesium is greater than > 2.5 meq/liter).
Explain the Etiology/cause of the Hypermagnesemia.
hemolysis,
Renal insufficiency,
High magnesium vada due to overuse of antacids and laxatives.
Hypothyroidism.
Lithium therapy.
Diabetic ketoacidosis.
Adrenal insufficiency
Overdose of magnesium salts.
Severe dehydration.
Chronic renal insufficiency.
Explain the clinical manifestation / sign and symptoms of the Hypermagnesemia.
Nausea and Vomiting,
weakness,
difficulty breathing,
Low blood pressure (hypotension),
bradypnea,
feel tired,
fall asleep,
Skeletal muscle weakness,
Deminized reflexes,
facial paresthesia,
flaccid muscle paralysis,
hypercalcemia,
arrhythmia,
Decreased diptendon reflex.
Bradycardia.
Bridging is a cell.
Bradycardia.
Cardiac failure.
Explain the diagnostic evaluation of the Hypermagnesemia.
history taking,
Physical Examination,
Serum magnesium level is greater than 2.5 meq/liter.
Elevated potassium and calcium levels.
ECG changes:= prolonged PR interval,
tall t waves,
Prolonged QT interval and Widened QRS.
Explain the medical management of the Hypermagnesemia.
Ask the child to increase fluid intake.
Provide diuretic medicine to the child.
Infuse calcium gluconate to prevent magnesium toxicity.
If the child is unable to pass magnesium through urine, i.e. if his kidney function is impaired, he should be provided with diet.
Explain the Nursing management of the Hypermagnesemia.
Careful monitoring of the child.
To maintain intake output chart of child.
Tell the child not to take magnesium rich food.
To assess the child’s reflexes.
Monitor the child for lethargy or drowsiness.
Avoid over-the-counter drugs that contain magnesium.
To check vital sign of child.
Assess the child’s respiratory function.
monitor Ecg changes like:=( prolonged PR, Prolonged QRS, and prolonged QT.)
Ask the child to take food with low magnesium.
- Explain/Define burns.
Burn injury is the most severe trauma to the body. Burn injuries are caused by direct contact with thermal, chemical, electrical, friction, heat, and radiation.
The injury seen in skin and tissue coming in contact with hot liquid, hot object, stream, fire, sun, electricity and chemical is known as ‘burn injury’.
A burn injury occurs due to the transfer of energy from the hit resource to the body. This hit is transferred by means of conduction and radiation.
Human skin can tolerate temperatures up to 42-44 C. But when it comes in contact with temperature higher than this temperature, tissue destruction is seen.
Burn injury is a major global public health problem with physical, psychological and financial impact on people.
Most burns are accidental.
Burn injuries occur in people of all ages and socioeconomic groups.

Explain the Etiology/causes of burns
Thermal Burns:
Thermal burns are most commonly seen. Thermal burns are caused by contact with fire, flame, hot, liquid, hot object and steam. The severity of thermal burns depends on the temperature of the object and the duration of exposure. For example residential fire, automobile accident.

Chemical Burns:
Chemical burns are caused by coming into contact with household or industrial chemicals such as strong acids, alkalis and organic compounds. Examples include sulfuric acid, phosphoric acid, spirits, petroleum products, sodium and calcium hypochlorite. The severity of chemical burns depends on the concentration, volume and duration of exposure to the chemical.
Electrical Burns:
Electrical burns are caused by electrical energy or electrical shock. The severity of electrical burns depends on the intensity of the current and the duration of exposure. For example, contact with faulty electrical wiring can cause electrical burns due to shock. Electric burns are difficult to diagnose. Because no symptoms are seen on the skin but internal damage is seen.

Radiation Burns:
Radiation burns are caused by contact with a radioactive source. Like UV light, X Ray, Gamma Ray. For example a nuclear bump explosion. The severity of radiation burns depends on the strength, duration, distance and surface area of the radiation.
Inhalation Burns:
Inhalation burns are caused by exposure to smoke. For example carbon monoxide poisoning.
Explain the Types & classification of burns.
Based on the depth of the burn and its severity, it is classified as follows.
According to burn depth & severity of penetrate the skin surface
Burns are classified into first degree burns, second degree burns, third degree burns and fourth degree burns based on their depth.
The depth of burning depends on the temperature of the burning object and the duration of exposure to it.
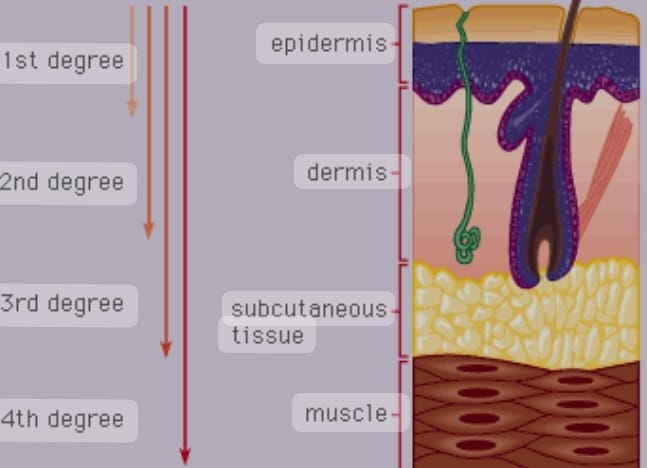
First degree burns / superficial partial thickness

In first degree burns, the epidermal layer of the skin is affected and there is minimal tissue injury.
The burned area is pink to reddish in color with erythema, dryness and pain. That area is found to be overly sensitive.
(Hyperesthesia). Blister formation is not observed.
First degree burns heal within a week and scar formation is not seen.
First degree burns can also be treated at home.
A sunburn is an example of a first degree burn.
Second degree burns / deep partial thickness
Second degree burns are also known as ‘dermal burns’.
In second degree burns, the epidermis and dermis layers are affected and the epidermal layer is destroyed.
Apart from this, hair follicles and sweat glands are also affected.
It involves redness, pain, swelling and blister formation at the burn site.
Second degree burns heal within 2-3 weeks and scar formation is seen.
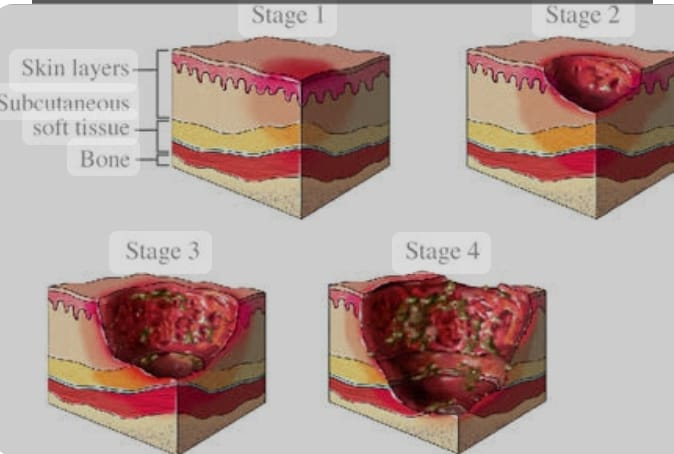
Third degree burns / full thickness
In third degree burns, the epidermis, dermis and subcutaneous layers are affected. Epidermis and dermis layers are destroyed.
Apart from this, bones, muscles, tendons and organs are also often affected. The burnt area looks waxy, white, i.e. the area looks burnt and blackened. The area is found to be firm, leathery and dry.
Pain and sensation are not seen due to nerve endings being destroyed and damaged. Apart from this conditions like hematuria and shock are seen.
Third degree burns can result in deep scars, so cosmetic or reconstructive surgery and skin grafts are used.
Third degree burns are slow-healing.
Forth degree burns
Fourth degree burns are those that have extended to the fascia. Bones, muscles, tendons and organs are also damaged.
In which the affected area looks like a dry chard and the area is painless and eschar is also seen.
These types of burns are caused by deep flame and electrical burns.
If the extremities are affected in the fourth degree, mutation is required.
According to burn severity
Depending on the severity of the burn and how much body surface area is affected, burns are divided into minor burns, moderate burns and severe burns.
Minor burns
If less than 10% of the total body surface area is affected in children and less than 15% of the total body surface area in adults, it is known as minor burns.
Patients with minor burns can be treated on opd basis.
All first degree and second degree burns are included in minor burns.
Moderate burns:
In moderate burns, the area affected is 20 to 25% of the total body surface area. In adults, the affected area is 15 to 25% of the total body surface area, while in children, the affected area is 10 to 20 percent of the total body surface area.
Severe burns:
In severe burns, an area greater than 20 to 25 percent of the total body surface area is affected. In adults, more than 25% of the total body surface area is affected.
While in children more than 20% of the area is affected.
Severe burns include inhalation and electrical burns.
Third degree burn and fourth degree burn are included in severe burns.
How does calculate percentage of burns
Or
Extent of body surface area injured
Different methods are used to calculate how much of the total body surface area is affected in burns. Like Rule of Nine, Lund and Browder Method, Palm Method
Rule of nine
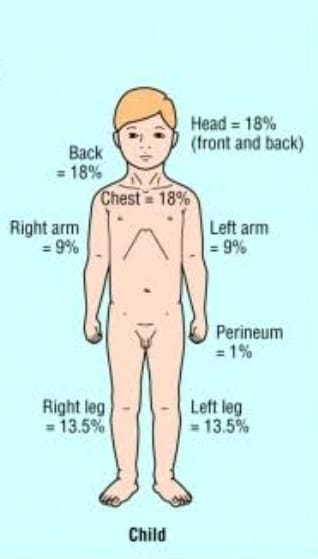
The Rule of Nine is a quick method for calculating the percentage of burns in a child.
Rule of Nine is given by Alexander Wallace hence Rule of Nine is also known as ‘Wallace of Nine’.
The Rule of Nine divides the different areas into percentages as follows:
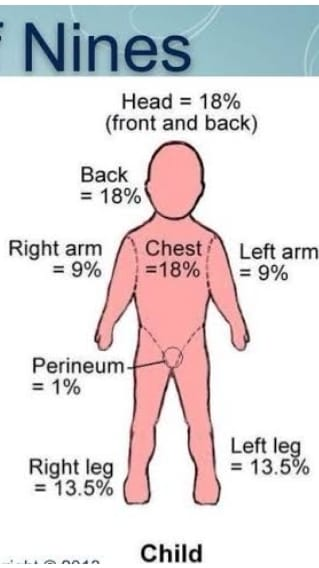
Head = 18%
(Anterior 9%,
posterior 9%).
Chest = 18%
(Anterior 9%,
posterior 9%).
Abdomen = 18% (Anterior 9%
,posterior 9%).
Right arm = 9%
Left arm = 9%.
(Total Leg Area 27 %) Right Leg = 13.5%
Left leg = 13.5%.
Genital Area = 1%
As shown above, the percentage of total body surface area affected can be determined.
Lund & browder method
The Lund and Browder method is the most accurate and precise method for estimating total body surface area in children and adults.
Because in this method percentages are given according to the size of different body areas of children and adults. As in children the head is big while the size of the extremities is small. Hence in children the head is given a higher percentage whereas in adults the head is given a lower percentage than that.
The percentage is calculated as shown in the table below.
Palmar method
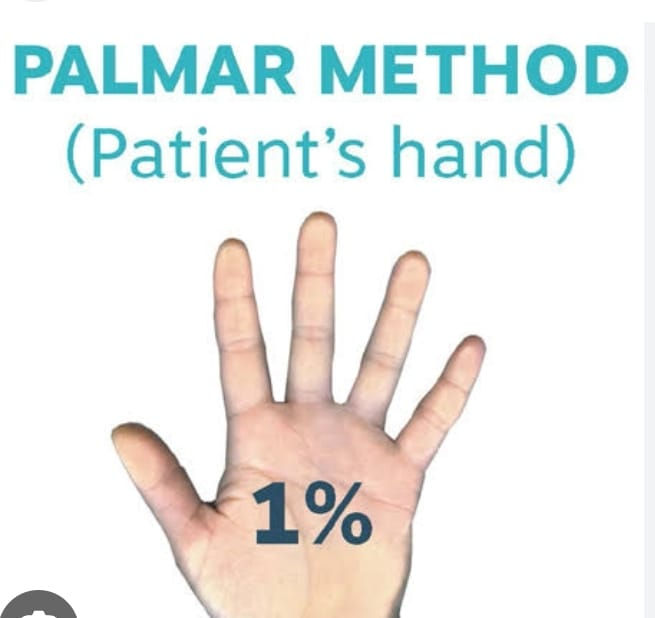
The Palmer method becomes more useful and effective when the burn injury is small, irregular or patchy.
In this method, the palm of the patient’s hand is considered to be 0.5% of the total body surface area and the palm and fingers are considered to be 1%.
Thus burn injuries at different places in the body are calculated using the Palmer method.
This method is used in both children and adults.
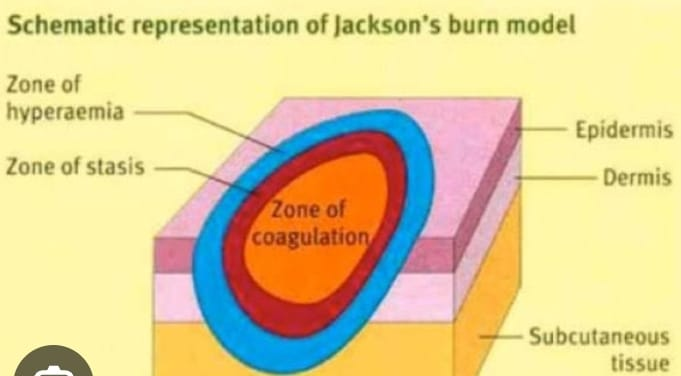
Jackson burn model (Jackson burn model).
The Jackson burn model helps to understand the pathophysiology of burn wounds.
In this model, the damaged tissue is divided into 3 zones:
Zone Coagulation, Zone Stasis and Zone Hyperemi
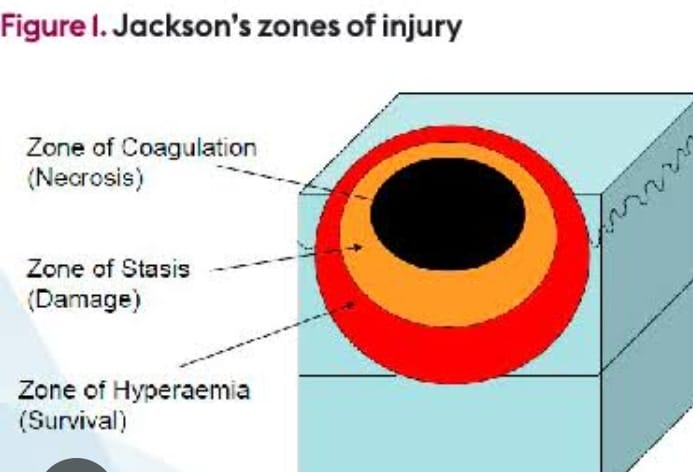
Zone Coagulation:
The zone of coagulation is the most central area of the burn in which the tissue is severely damaged and is irreversible.
Zone Stasis:
The area surrounding the zone of coagulation is known as the zone of stasis. There is less damaged tissue and there is vascular transudate, inflammatory reaction and impaired tissue perfusion. If a good environment is provided then the tissue recovers otherwise necrosis occurs.
Zone Hyperemia:
Zone hyperemia is the outermost layer of the burn where increased blood flow due to vasodilation leads to faster tissue recovery and reduced chances of necrosis.
Explain pathophysiology of burns
A burn injury occurs due to the transfer of heat resources or energy to the body.
The severity of a burn injury depends on the temperature of the heating agent and the duration of exposure.
A primary local response occurs if the area affected is less than 25% of the total body surface area, but a local and systemic response occurs if the area affected is greater than 25% of the total body surface area.
First 24 to 48 hours after burn injury
Burn injury
|
\/
Coagulation necrosis is seen in the soft tissue.
|
\/
Vasoactive substances and inflammatory mediators are released. (eg cytokines, histamine, oxidase, catecholamine)
|
\/
This results in increased vascular integrity and capillary permeability and vasodilation.
|
\/
Hence the fluid shifts from the intracellular space to the interstitial space.(Most of the fluid is shifted within 12 hours and this process is seen to be continuous for 30 hours)
|
\/
Peripheral edema develops due to fluid shift and increases tissue colloid osmotic pressure and fluid electrolyte imbalance.
|
\/
On the other hand, there is a decrease in intravascular volume so that blood volume decreases and cardiac output also decreases.
|
\/
Thus this stage is also known as hypovolemic stage.
48 to 72 hours after the burn
48 to 72 hours after the burn
|
\/
Vascular integrity and capillary permeability return and normalize.
|
\/
Fluid returns from the interstitial space to the intravascular space thereby reducing peripheral edema.
|
\/
Intravascular volume increases. (Fluid overload can also occur often.) (Hence this fluid is excreted through urine. Hence this stage is also known as diuretic stage.
|
\/
This also increases blood volume and cardiac output.
|
\/
This results in increased blood flow to all organs and tissues.
Explain local & systemic effect of burns
Local Effect of Burns:
In a burn injury, if the area affected is less than 25 percent of the total body surface area, a local effect is seen.
Tissue damage
Exposure to high temperature causes tissue and cell damage and necrosis.
Edema
Fluid shifts from the intravascular space to the interstitial space causing edema.
Inflammation
A burn injury causes our body to respond by releasing inflammatory mediators and causing inflammation. Redness, erythema, swelling and blister formation are observed in the affected area.
infection
Microorganisms grow and enter the body due to tissue destruction and breakdown of skin integrity. Hence infection is seen.
Systemic Effect of Burns:
Local and systemic response is observed in burn injury if the area affected is more than 25% of the total body surface area.
This systemic effect is due to release of vasoactive substances and inflammatory mediators. Like histamine, cytokines, oxidase, catecholamine
Cardio Vascular Alterations:
There is a decrease in cardiac output.
This results in hypotension and tachycardia.
RBCs are destroyed.
The hematocrit level increases and the plasma level decreases.
Abnormalities in coagulation are seen.
Cardiac dysrhythmias are seen in electrical burns.
Pulmonary Ulceration:
Pulmonary alteration occurs due to inhalation burns.
Bronchoconstriction is seen.
There is increased secretion and congestion.
Obstruction is seen in the airway.
Stider and horseness sounds are seen.
Pulmonary edema is seen.
Hypoxia is observed.
Renal Alteration:
Renal function is altered due to decreased renal blood flow.
A decrease in glomerulo filtration rate is observed.
Blood is seen in the urine.
GI Ulceration:
Intestinal paralysis results in decreased movement and decreased bowel sounds.
Metabolism increases.
Bleeding in the GI tract causes vomiting and blood in the stool.
Stress and ulceration are seen.
Immunologic Alterations:
Damage to the skin barrier allows micro-organisms to grow and enter the body and cause tissue infection.
Thermoregulatory disturbance:
Due to loss of skin, the function of regulating body temperature is altered, hence the condition of hypothermia is seen.
Fluid and Electrolyte Alterations:
Conditions such as hyponatremia and hyperkalemia are seen.
Explain the first aid care of burns injury (Right first aid care of burns injury)
Take the child away from the scene and check that the child does not come in contact with the burning material.
To remove burnt cloth and ornaments worn by the child. If the cloth is stuck to the body area, do not remove it.
Then check the child’s airway, breathing and circulation.
If breathing is not present, clear the airway and provide CPR.
If the child is breathing, apply full running water to the affected area.
If the fingers are stuck together due to burns, gently separate them.
Then cover the wound loosely with a clean cloth. So that contamination can be prevented and air can be prevented from coming in contact with the surface.
Avoid friction and pressure on the burned area.
Do not apply any kind of ointment or cream on that area.
Explain the Immediate care of burns patients (Immediate care of burns child)
Move the victim away from the scene.
To remove burnt cloth and jewelery worn by the child.
Assess the child’s airway, breathing and circulation.
If breathing is not present, clear the airway and provide CPR.
Flush the burn area with full running water and cover the wound.
Transfer the child to the nearest hospital.
If necessary, provide oxygen therapy to the child.
Securing the child’s iv line.
Administer intravenous fluids.
Explain the management of the child with the burn.
In the management of a burnt child, it is managed in 3 ways.
1) Airway Management,
2) Hyperbaric oxygen therapy,
3) Fluid management.
Chemotherapy
Wound care.
1) Airway Management,
A child whose face and neck
Properly observe the airway of the child who has been burned in the region or has inhaled the flame.
Monitor the child’s airway properly and closely.
Closely monitor the child for any bronchial asthma.
If the child has minor pulmonary injury, advise for cuffing so that the secretion can be properly removed.
If the child is not able to do the cuffing, then do the proper training.
Providing proper bronchodilator medication to the child so that the medication can dilate the bronchi and widen the airways so that the child can breathe easily.
A proper mucolytic medication is also provided to the child due to which the mucus is thinned due to which the mucus can be removed and the child can breathe easily.
2) Hyperbaric oxygen therapy,
Hyperbaric oxygen therapy is a non-invasive medical treatment used to properly provide oxygen to a burned child.
It consists of a hyperbaric oxygen therapy device that has a pressure chamber with a field of 100% pure oxygen.
3) Fluid management.
Fluid management is essential in the burned child. Because fluid is lost more in a burnt child. Plasma is lost in excess in a burned child.
Proper fluids are provided to properly maintain electrolytes in the burned child.
Proper fluids are provided to prevent the child from shock condition.
Fluids are provided for a duration of 48 hours in a burnt child.
4ml Ringer lactate ( RL)×wt.in kg×percentage of TBSA burn to calculate child’s 24 hour fluid intake.
Half amount of fluid is provided to the child in the first eight hours.
After that half amount of fluid is provided in next 16 hours.
Then in the next 24 hours fluid equal to 2ml Rl × wt in kg × percentage of burn is provided.
Continuously assess the child’s vital signs.
Properly assessing child’s intake output chart.
Chemotherapy
Provide crystalline penicillin to the child for 5 days.
Provide proper antibiotic medication to the child.
Provide proper sedative medication to the child.
Like pethidine 1 to 2 mg/ kg intravenously.
Provide adequate protein and calorie rich diet to the child.
Wound care.
Taking proper care of the wound due to burn can prevent the child from infection.
Provide proper dressing to the wound.
To remove dead tissues and debris in the wound by maintaining proper aseptic technique.
Wrap the child in a proper figure of 8 shape with a bandage to improve the venus return.
Apply topical antimicrobial and antibiotic to the child properly.
To provide proper work and comfortable environment to the child.