ENGLISH PEDIATRIC UNIT 4 PART 2
COMMON BEHAVIORAL DISORDERS IN PEDIATRIC NURSING
Explain/Define Nail biting
Nail biting is also called onychophagia. Nail biting is the most common bad habit of school going children. Which is mainly found in children above 4 years.
It is a common habit in which a child engages in repetitive biting and chewing of his fingernails or toenails. Nail biting is often caused by stress, anxiety, boredom, self-punishment, nervousness.
Nail biting can result in short, uneven nails, and the skin and tissues around the nail can be damaged and infected.

Explain the etiology/cause of the nail biting. (State the reason for nail biting)
Due to biological factors,
Due to environmental factors,
Due to genetic causes,
Because of anxiety,
Due to major depressive disorder,
Due to psychological factors,
Due to stress and anxiety,
Due to behavioral factors,
Due to environmental factors,
Due to traumatic experiences during childhood,
Due to interpersonal conflict,
Due to psychiatric disorder,
Due to obsessive compulsive disorder,
Due to attention deficit hyperactivity disorder,
Due to anxiety disorder.
Explain the Clinical manifestation/ sign and symptoms of the child with the Nail biting
having short nails,
Damage to nailbeds,
Damage to surrounding tissues of nailbeds,
nail infection,
Bleeding from the nail bed,
Due to stress and anxiety,
Social withdrawal,
Infection from nail biting goes to the mouth,
Conflict between parents and caregivers,
Explain the diagnostic evaluation of the child with the nail biting. (State the diagnostic evaluation of a child with nail biting)
History taking and physical examination
Assessing the psychological level.
Conducting behavioral assessment.
Assessing the child’s family history.
Collaboration with parents.
Explain the management of the child with the nail biting. (State the management of a child with nail biting)
Providing proper cognitive behavioral therapy to the child.
Providing proper positive reinforcement to the child.
Identifying the child’s trigger factors and giving advice to reduce them.
To provide proper environmental to the child.
Properly supporting the child by the parents.
If there is any complication due to nail biting, provide proper medication.
Assessing the Psychological Environment.
Provide proper suggestion to parent to decrease stress and tension.
Advise the child’s parents not to provide any punishment by the parent if the child does nail biting. Because punishment increases anger and negativity in the child.
Provide proper positive reinforcement to the child.
Do not restrain the child.
Applying any bitter substance to the child’s fingers.
Keeping the child’s nails properly short.
Providing proper psychotherapy to the child.
- Explain/Define thumb sucking
Thumb shaking is also called finger shaking.
Thumb shaking is a common behavioral and habit disorder in infants and young children. In which they do thumb shaking to reduce tension and for comfort or self-soothing.
It involves placing the child’s thumb in the mouth and sucking rhythmically.
Thumb shaking is a natural reaction that often begins in infancy and may continue into early childhood, especially during times of stress, boredom, or fatigue.
However, after the age of 4 or 5 years, prolonged thumb sucking can lead to teething, swallowing, speech, mastication, etc. problems as well as social anxiety.
If thumb shaking develops during seven to eight years, it indicates a sign of stress.

Explain the types of the thumb sucking
There are two types of thumb shaking.
1) Normal Thumbsking,
2) Abnormal thumbsking
1) Normal thumbsking
Normal thumbsucking is mainly seen in the first and second year of life and the habit disappears as the child matures.
2) Abnormal thumbsking
When the habit of thumbsucking is observed at preschool age, it is called abnormal thumb sucking.
And that mainly
A) Psychological and
B) Due to habitual condition.
A) Psychological
A psychological mother child is of any emotional factor
Due to which the habit of thumbsking occurs. such as insecurity,
Because of loneliness, and being neglected.
B) Habitual
Habitual mother child thumbsking not because of any psychological factor but because of his normal habit.
Explain the etiology / cause of the child with thumb sucking. (Give reasons for thumb sucking)
Due to the child being unsatisfied with bottle fitting and breast feeding.
Because of infant reflexes.
A child is a very anxious, sensitive and insecure child.
Due to parenteral influence.
Due to environmental factors.
Due to genetic factor.
Working Mother.
Parent’s Occupation.
Due to emotional problems in parents and child.
Due to child maladjustment.
Explain the clinical manifestation/sign and symptoms of the child with thumb sucking. (State the symptoms and signs of thumb shaking)
Redness and irritation are seen in the thumb.
Dental problem.
Difficulty in speech.
Social and emotional impact will be seen in the child.
Visible thumb and finger shaking.
Impairment in oral hygiene is seen.
Explain the diagnostic evaluation of the child with thumb sucking.
History taking and physical examination.
Conducting behavioral assessment.
Psychological evaluation.
Dental Examination.
Speech Assessment.
Explain the medical management of the child with the Thumb Sucking
To provide a properly positive environment to the child.
Providing proper cognitive behavioral therapy to the child.
To provide proper guidance and support to the parents of the child.
To provide proper work and comfortable environment to the child.
Providing proper counseling to the child.
Advising parents not to show excessive anxiety towards the child.
Advise the parent of the child that thumb shaking is a natural process which is a natural process and then relieved.
To provide proper additional support to the child and his family members.
Giving advice to the child’s parents or the child properly
To provide love and affection.
Application of any bitter substance on the child’s thumb.
If the child is lonely and frustrated, divert his attention.
To provide proper work and comfortable environment to the child.
Define / Explain Somnambulism
Somnambulism is derived from the Latin word vada,
Somnus means “slip” and ambulus means
Also called “walking” means “slip walking”.
is coming.
Somnambulism is a sleep disorder.
Somnambulism is a condition of a child in which the child performs walking and other activities while in a sleeping state.
Sleep walking is a sleep disorder that usually occurs during deep sleep and the child wakes up forgetting all about the episode of sleep walking. And sometimes it can increase as the child gets older.
It is important for parents to maintain the safety of sleepwalking babies such as providing a safe environment and taking preventive measures like gently coaxing them back to bed if they wander, etc.

Explain the etiology/causes of the child with the somnambulism. (State the cause of somnambulism)
The exact cause of somnambulism is unknown.
But it is seen due to the combination of genetic factors, environmental factors and developmental factors.
Due to genetic factors,
Having a family history of sleep walking,
Due to the immaturity of the nervous system,
Due to any stress, anxiety and tiredness of the child,
Due to environmental factors,
Due to some type of medical condition,
Children’s Ma
due to fatigue,
And because of anxiety,
Due to certain types of medicine.
Explain the clinical manifestation / sign and symptoms of the child with the somnambulism. (State the symptoms and signs of a child with somnambulism)
Walking while sleeping.
Do routine activities at bedtime such as opening doors, rearranging things in the house, and trying to leave the house.
to do etc.
A child talks to himself,
The child wakes up from a deep sleep forgetting all about the episodes of sleepwalking that occurred.
Explain the Diagnostic evaluation of the child with the Somnambulism Explain the diagnostic evaluation of the child with the somnambulism.
History tacking and physical examination,
Assessing the child’s sleep pattern.
To assess the frequency and duration of the child’s sleep walking episodes.
Assessing the child’s neurological status.
Assessing the child’s psychological status.
Explain the management of the Somnambulism. (State the management of somnambulism)
To provide proper safety measures to the child at the time of slip. Keep away any hazardous objects and keep doors and windows closed so that the child cannot go out of the house.
To provide work and comfortable environment to the children.
Reducing stress and anxiety of the child.
To provide work and supportive environment to the child.
Provide proper reassurance and relaxation techniques to the child.
If the child has any medical condition, treat it properly.
Providing proper behavioral therapy to the child.
Advising the child to meditate properly.
Remove any dangerous objects in the child’s room.
Remove any sharp objects.
Providing proper psychotherapy to the child.
- Explain/Define Protein energy Malnutrition. (Define Protein Energy Malnutrition (PEM))

Protein Allergy Malnutrition (PEM) is a nutritional problem in a child formerly known as Protein Calorie Malnutrition (PCM) that results from inadequate intake of protein and calories in food, resulting in impaired growth, development and overall health of the child. Impairment occurs.
There are two main types of PEM.
1) Marasmus
2) Kwashiorkor

1) Marasmus
Marasmus of PEM is caused by severe calorie deficiency, resulting in weakness, loss of muscle mass, and wasting in body tissues.
Children with marasmus usually appear very thin and have an appearance of a
“Starved”.
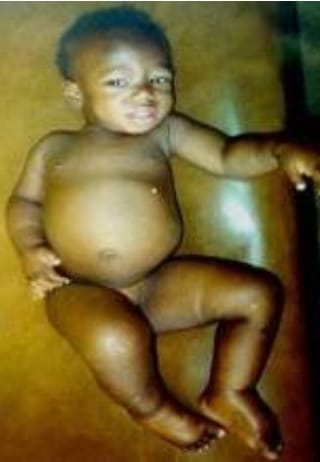
2) Kwashiorkor
Kwashiorkor is a form of PEM caused by a deficiency of solid protein, despite adequate caloric intake.
Children who have kwashiorkor have a swollen abdomen (edema), fatty liver, skin lesions, and stunted growth due to water retention. And the child with quasisurecore is normal but his body weight is higher than marasmus.
Explain the classification of the child with protein energy malnutrition. (Give classification of protein energy malnutrition)
A) Syndromal classification
There are total five types of syndromal classification.
1) Nutritional Marasmus,
2) Kwashiorkor,
3) Nutritional Dwarfing,
4) Marashmike Kwashiorkor,
5) Pre kwashiorkor
1) Nutritional Marasmus
Nutritional marasmus is a severe form of protein energy malnutrition.
In which chronic starvation is seen and the intake of both protein and calories is inadequate.
The condition of nutritional marasmus is mainly when there is extreme poverty, food insecurity, lack of access to nutritious food.
It is seen due to the presence of small amounts in the mother.
2) Kwashiorkor,
Kwashiorkor is a form of PEM caused by a deficiency of solid protein, despite adequate caloric intake.
Children who have kwashiorkor have a swollen abdomen (edema), fatty liver, skin lesions, and stunted growth due to water retention. And the child with quasisurecore is normal but his body weight is higher than marasmus.
3) Nutritional Dwarfing,
Nutritional dwarfing is also called stunted growth and growth retardation.
Nutritional dwarfing is one manifestation of protein allergy malnutrition (PEM) in children. It is a condition where children fail to achieve their expected growth due to inadequate intake of essential nutrients including protein and calories.
Nutritional dwarfing is mainly seen during the period of growth and development of the child such as infancy and early childhood.
In it, the child has skeletal growth delay, short stature,
Delayed puberty, cognitive deficits,
Symptoms like etc. are seen.
4) Marashmike Kwashiorkor,
Marasmic Kwashiorkor is a protein energy food nutrition in a solid form. It has the combined symptoms of marasmus and quasi-cerebral chorea. This condition of marasmic kwashiorkor is seen mainly when the child has prolonged and severe malnutrition.
And mainly seen due to extreme poverty and food insecurity.
5) Pre kwashiorkor
“Pre-kwashiorkor” involves the early stage or warning sign of kwashiorkor, a severe form of protein-energy malnutrition (PEM). It has early symptoms of kwashiorkor.
In prequasiorchor, children may show signs of moderate to severe malnutrition.
B) Indian Academy for Pediatrics (IAP) Classification.
Indian Academy for Pediatric classification is done mainly on the weight of the child.
Grade:=1 (Mild Malnutrition) Child weighs 80-70% of expected weight.
Grade:=2 (Moderate Malnutrition) Child weighs 70-60% of expected weight.
Grade:=3 (Severe Malnutrition) Child weighs 50-60% of expected weight.
Grade:=4 (Superior) A child weighs less than 50% of the expected weight.
When a child’s weight is more than 80% of the expected weight for age, it is called normal.
C) Gomez Classification
Gomez classification is given according to the age of the child according to his weight. In Gomez classification when the expected weight according to age is more than 90% it is called normal.
First degree: – Expected weight between 90 – 75%.
Second degree: – Expected weight between 75-60%.
Third degree: – Weight less than 60% expected.
D) International Classification
Expected weight is between 80 and 60%.
In with AD:- kwashiorkor,
In without AD :=under nutrition,
If the weight is below 60% of the expected weight and in AD := Marashmic kwashiorkor
If weight is below 60% of expected weight and without AD := Nutritional Marasmus.
E) Arnold classification
Arnold’s classification mainly depends on the mid ama circumference.
Mild to Moderate := If the mean circumference is between 12.5-13.5 cm.
Severe: If the midarm circumference is less than 12.5 centimeters.
Explain/Define the Marasmus
Marasmus word comes from the Greek word “marasmos” meaning wasting.
Marasmus in PEM (Protien Energy Malnutrition) is caused by severe calorie deficiency, resulting in weakness, loss of muscle mass and wasting in body tissues and loss of subcutaneous fat.
Children with marasmus usually appear very thin and have an appearance of a
“Starved”.
In marasmus, the child loses more than 50% of the expected weight for age.
Explain the Etiology / cause of the Marasmus
Due to the innate diet,
Due to inadequate amount of calories in the diet,
Due to poor feeding,
Due to certain medical conditions,
As due to chronic vomiting,
Due to chronic infection,
Ex := Syphilis, Tuberculosis, Upper Respiratory Infection,
Due to certain environmental factors,
Due to poverty,
Marasmus is most commonly seen in infants,
Due to congenital diseases like cleft palate hydrocephalus, Hisprung’s disease etc.
Due to certain metabolic disorders such as galactosemia.
Explain the Classification of the Marasmus. (Describe the classification of Marasmus)
There are total 4 classifications according to the grade of marasmus.
1) Grade-1 :=
In this grade, there is no loss of fat from the axilla and groin area.
2) Grade-2 :=
In this grade, there is no loss of fat from the axilla and groin area. Also, fat is lost from the abdominal and gluteal regions.
3) Grade-3 :=
In this grade, there is no loss of fat from the axilla and groin area. Also, fat is lost from the abdominal and gluteal regions. Along with this, the fat of the chest and spine is also involved.
4) Grade-4 := In this grade there is involvement of first three grades along with fat loss of bucklepad.
Explain the clinical manifestation / sign and symptoms of the child with Marasmus. (State the symptoms and signs of Marasmus)
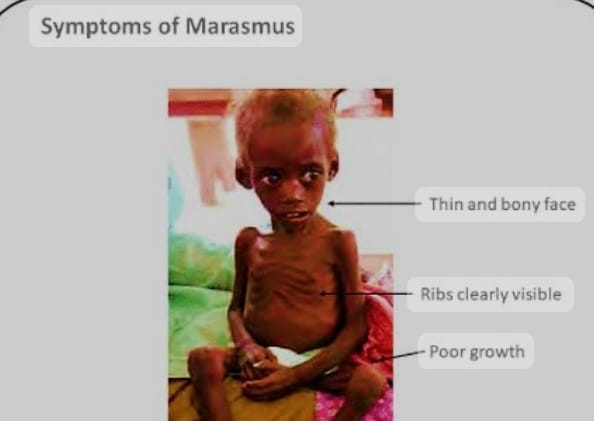
Severe wasting in body tissues,
Subcutaneous fat loss,
Child becomes very thin,
Facial features become suspicious,
Child has growth retardation,
Developmental delay of the child,
Subcutaneous fat loss from a child’s buttock abdomen, Thai.
The face looks like an aged one.
Loss of fat from the child’s cheeks.
Child becomes irritable.
Finding severe malnutrition in the child.
Electrolyte imbalance in the child.
Neurological in Child
Symptoms are observed,
Child becomes less active,
Child’s spleen, gonads,
And reducing the size of the liver,
The child feels weak, tired, and tired.
To observe changes in the child’s behavior,
Decreased physical activity,
Child’s extreme weight loss,
Explain the diagnostic evaluation of the child with Marasmus. (Give diagnostic evaluation of Marasmus Wada child)
History taking and physical examination,
x ray,
Taking anthropometric measurements of the child,
Carrying out laboratory investigation of the child,
complete blood count,
Assay serum electrolyte and serum albumin test,
Performing imaging testing of the child properly,
Explain the management of the child with Marasmus. (Write management of child with marasmus)
Providing adequate nutritional supplements to the child,
Providing adequate high calorie feeding to the child.
Advising the child on nutritious food intake.
Maintaining adequate fluid and electrolyte levels of the child.
Provide adequate ion supplementation to the child.
Giving advice to gradually increase the child’s diet.
If the child has any infection, provide adequate antibiotic medicine.
To provide adequate psychological support to the child.
Daily recording of child no weight.
Advise the child to provide adequate breastfeeding.
Provide nutritious food like green leafy vegetables, soup, banana, pulse, cereals milk etc.
Provide diet to the child in small and quantifiable amounts.
To provide adequate work and comfortable environment to the child.
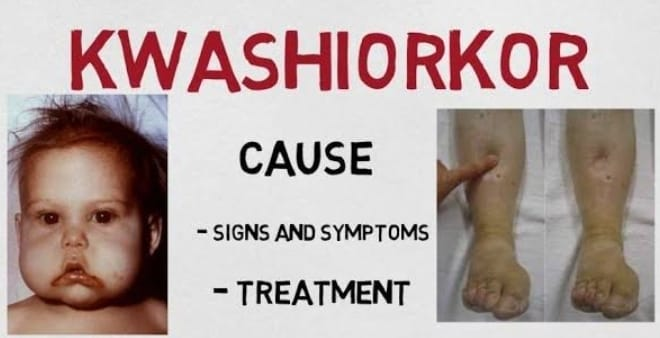
Define/Explain kwashiorkor. (Define kwashiorkor).

Quasicore is a form of solid protein energy mal nutrition (PEM). Kwashiorkor is a form of PEM. Which is caused due to deficiency of solid protein despite intake of adequate calories.
Children who have kwashiorkor have a swollen abdomen (edema), fatty liver, skin lesions, and stunted growth due to water retention. And the child with quasisurecore is normal but his body weight is higher than marasmus.
Kwashiorkor is also called “Red Hairy Boy”.
Kwashiorkor was first described by British physician Dr. Cicely Williams in 1933. But a particular kwashiorkor tumor was described in 1935.
Quasarcore’s condition is predominantly seen in preschool children.
Symptoms of kwashiorkor include edema of the body due to fluid retention
Explain the Etiology / cause of kwashiorkor.
Due to poverty,
By providing an inadequate amount of bestfitting to the child,
Due to intake of protein rich food in inadequate amount,
Due to non-availability of protein rich food,
Being of low socio economic status,
Due to faulty feeding habit,
Due to imbalance diet,
Due to not consuming nutritious diet in adequate amount,
Due to certain medical conditions such as chronic infections,
Gastro Intestinal Disorders, etc.
Due to certain metabolic disorders,
Due to environmental factors,
Due to providing adequate weaning diet to the child,
Due to intake of essential vitamins and minerals in inadequate amounts,
Explain the clinical manifestation/ sign and symptoms of the child with the Kwashiorkor.
Edema (in pitting ED) is found in the body mainly in lower extremities, upper extremities, abdomen, face etc.
A condition of bloated stomach due to collection of fluid in the abdomen,
Skin becomes dry and scaly,
Muscle wasting and muscle atrophy,
Skin changes such as pigmentation,
Hyperpigmentation, skin roughness, discolouration etc.
Hepatomegaly (liver enlargement) in a child,
Child Niapatite
to decrease,
Observe behavioral changes in the child,
Child’s growth and development deal,
Impaired skeletal growth of the child,
Finding the condition of anemia in the child,
Changes in the child’s hair,
Child should not be interested in any activity,
Muscular wasting is seen in the child,
Due to edema of the child’s face
Feeling “moon face”.
To observe psychomotor changes in the child,
Finding intellectual impairment in the child,
Explain the diagnostic evaluation of the child with Kwashiorkor.
(State the diagnostic evaluation of a child with kwashiorkor)
History tacking and physical examination,
Anthropometric measurement,
laboratory test,
Complete blood count test,
Serum albumin test,
Serum Electrolyte Test,
Arterial blood gas analysis,
Explain the medical management of the child with Kwashiorkor.
(State the medical management of Kwashiorkor Wada child)
Providing adequate protein rich diet to the child.
Advise the child for adequate calorie intake.
Advise the child to intake adequate nutritious rich food.
Provide adequate glucose solution if child has hypoglycemic condition.
If the child has anemic condition, treat it properly by blood transfusion.
Giving advice to the child to take proper skin care.
To provide proper play therapy and recreation therapy to the child.
Advise parents of children to provide nutritious rich food to the child.
Provide adequate vitamin A supplements to the child.
If Quasiorcor is in an advanced stage, hospitalize immediately.
Assess the child’s fluid and electrolyte levels properly.
Assessing child’s height, weight, and nutritional status.
Providing proper psychological support to the child.
Explain the nursing management of the child with Kwashiorkor.
(State Nursing Management of Kwashiorkor Wada Child)
To provide properly comprehensive support to the child.
Assess child’s nutritional status properly like breast fitting, weaning, food habit, balance diet,
Assessing Socioeconomic Status.
Assess the child’s growth chart properly.
Providing proper nutrition rehabilitation to the child.
Collaborate with other health care personnel for child care.
Advising the parents for adequate nutritious food intake of the child.
Maintain hydration status properly.
Provide properly prescribed medication to the child.
Providing proper psychological support to the child.
To provide complete information to the child’s parents about the causes of the disease, its symptoms and signs, and its treatment.
Providing supplementary feeding to the child.
Antibiotic medicine should be provided if the child has any infection.
Provide adequate vitamins and mineral supplements to the child.
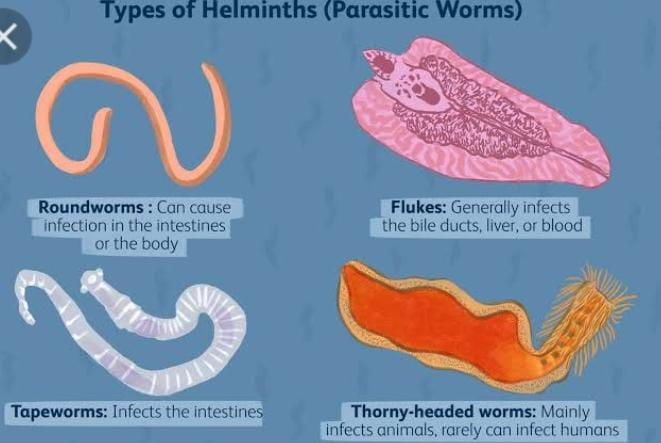
- Explain/Define Helminthic infestation

Helminthic infestation is a common health problem seen in children. It is also called worm infestation. In helminthic infestation, parasitic worms known as helminths enter the body.
These worms infect various organs including the intestines, lungs, liver and blood. In common types of helminths
Round worms (nematodes),
Tapeworms (Cestodes),
Includes threadworms, hookworms and flukes (trematodes).
Helminthic infestations often enter the body through the ingestion of contaminated food or contaminated water, or by the larvae penetrating the skin.
Explain the Etiology/cause of the Helminthic infestation
The etiology of helminthic infestation in children is usually due to exposure to an environment contaminated with helminth eggs or larvae. This exposure can occur through various routes:
Ingestion:
Children due to ingestion of eggs or larvae of helminths in contaminated food or water, especially in poor sanitation and
In areas with unhygienic conditions.
Contact:
Direct contact with contaminated soil, such as playing with bare feet in areas where infected individuals have defecated, can cause helminth larvae, particularly hookworm larvae, to enter the skin.
Poor Hygiene:
Inadequate hand washing practices,
Lack of proper hand washing, especially after using the toilet or before eating, can increase the risk of helminthic infestation as children may inadvertently come into contact with helminth eggs or larvae.
Contact with animals:
Humans can acquire helminthic infestations through contact with some helminth-infected animals or by consuming undercooked food or raw meat containing helminth larvae, such as certain tapeworms.
Environmental Factors:
Environments such as warm and humid climates play an important role in the survival and transmission of helminth eggs and larvae, and children living in such areas are more likely to have helminthic infestations.
other reasons
Due to not properly disposing of human excreta.
Due to not maintaining personal hygiene.
Due to ingesting vegetables that are not properly washed.
Explain the clinical manifestation / sign and symptoms of the Helminthic infestation.
Gasterinterestine:- Abdominal pain,
Nausea and vomiting, diarrhoea,
conception,
flatulence,
loss of appetite,
weight loss,
bloody stool,
Itching in the anal area.
Fatigue and weakness:
Chronic helminthic infestation causes fatigue and weakness due to nutritional deficiency and anemia.
Anemia:
Some helminths,
Such as hookworms and whipworms, can cause chronic blood loss from the intestines, causing anemia that can cause pallor, weakness, dizziness and shortness of breath.
Skin :=
itching,
rashes,
Skin ulcers and lesions.
Respiratory Symptoms:
Infection Cough, wheezing, chest pain,
Difficulty breathing
Allergic reaction:
itching, hives,
Swelling (angio
oedema) and symptoms such as anaphylaxis
Neurological symptoms:
Neurocysticercosis, seizures,
Headache
Other symptoms:
Getting a low grade fever,
Irritability,
becoming restless,
weight loss,
feel tired,
growth failure,
Not sleeping properly,
vulvovaginitis in females,
loss of appetite,
Races can be seen in the body,
itching,
Explain the Diagnostic evaluation of the Helminthic infestation
History tacking and physical examination,
Stool examination,
blood examination,
imaging studies,
Abdominal Ultra Sound,
chest x-ray,
CT scan,
serological test,
sputum examination,
Explain the medical management of the child with the Helminthic infestation
Identifying helminthic species.
Provide antihelminthic medication to the child.
Ex:=
Albendazole,
Mebendazole.
Praziquantel meditation should be provided to the child if he has helminthic infestation by tapeworm and fluke.
If the child has stationed helminthic infestation by roundworm and threadworm then ivermectin medicine should be provided to him.
If the child has anemic condition then provide ferrous sulphate medication.
Advise the side’s parents to provide proper medication to the child.
Giving advice to the child’s parents or taking regular follow up.
Explain the Nursing management of the child with the Helminthic infestation
Proper assessment of the child.
Assessing the child’s vital signs and nutritional status.
Assess the child for anemia dehydration and any allergic reactions.
Regularly assess the child’s stool.
Giving advice to parents of child to maintain proper hygienic condition of child.
To provide education to the child that after toilet and before meals and proper hand washing.
Advise the child to drink clean water.
Provide adequate nutritious diet to the child.
If the child has anemic condition, then providing the child with proper iron supplement.
Provide proper antihelminthic medication to the child.
To provide proper comfort measures to relieve the child’s symptoms like pain, fever, fatigue, nausea.
Providing proper psychological support to the child.
Advise the child’s parents to provide properly cooked food to the child.
Advising parents to provide properly protective shoes to the child when the child goes out to play.
Advising the parents to provide the child with properly clean toys to play with.
Advise the parents to provide the child with properly heated water i.e. clean water to drink.
Advise parents to wash raw vegetables properly after consuming them.
Advising parents to keep their child’s nails short.
Advising parents to maintain cleanliness while preparing food.
Advising the parents of the child to maintain proper environmental sanitation.
Advise the child to intake high protein, low carbohydrate and fibrous food.
Advising parents to provide food in properly small and frequent amounts to the child.
To provide properly green leafy vegetables to prevent the child from anemia condition.
To provide education to the child’s parents to provide proper meditation.
Advising parents of child to take regular follow up.
- Explain/Define Round worms.

Roundworms are also known as “Ascaris lumbricoides/nematodes”.
They are a group of cylindrical worms that belong to the phylum Nematoda. They are found in a variety of habitats around the world, including soil, water, and as parasites of plants and animals.
Ascaris lumbricoides is one of the most common infestations in children. In children, it mainly affects the small intestine, the adult female roundworms are 20 to 40 centimeters. And mail worms are 12 to 30 centimeters.
These roundworm infections are mainly found in tropical and subtropical climates where environmental sanitation and hygienic conditions are poor.
A female roundworm produces 2,40,000 eggs a day.
These roundworms in the child include the intestine, liver, lungs, trachea, alveoli,
Affects bronchioles etc.
Roundworms mature in 60 to 80 days. And its life span is between 6 to 12 months and maximum life span is 1.5 to 2 years.
Infestation of roundworms is mainly transmitted through phyco-oral route i.e. in areas where sanitary facilities are scarce. It is caused by ingestion of contaminated fruits, vegetables and food.

Explain the Etiology/cause of the round worms infestation in child.
Several factors are involved in the etiology of roundworm infestation:
Transmission:
Roundworms can be transmitted through different routes, including
Contaminated food and
Ingestion of contaminated water,
Due to direct contact with infected soil,
Bite of an infected insect or animal,
Due to poor sanitation,
over crowding,
Due to compromised immune system,
Due to environmental conditions,
Due to inadequate hygiene practices,
Due to close contact with infected animals,
Due to children ingesting mud while playing outside,
Due to malnutrition,
Food is not properly cooked
due to happen.
Explain the clinical manifestation/ sign and symptoms of the child with the round worms
Symptoms and signs of roundworms include:
Abdominal pain,
Abdominal distension,
Nausea and vomiting
Diarrhea and constipation,
Malnutrition,
feel tired,
weakness,
Visible worms in the stool,
Coughing, wheezing and other respiratory symptoms,
Loeffler syndrome such as fever,
dyspnoea, cough,
Vision, Urticaria
Irritability,
abdominal discomfort,
nutritional deficiency,
Poor growth,
to see anemia,
peritonitis,
Pancreatitis,
Explain the diagnostic evaluation of the child with the round worms.
History taking and physical examination,
stool examination,
sputum examination,
Vomit Examination,
Serological test,
imaging test,
ultrasound,
Abdominal x-ray,
blood eosinophilia test,
A contrast study of the gastroenteric tract.
Explain the medical management of the child with the round worms.
Provide proper antiparasitic medication to the child.
Ex:=
Albendazole (15mg/ kg) 400 mg or
Mebendazole 100 mg twice a day for three days.
Levamisole 2.5 mg/ kg single dose.
Pyrantel pamoate 10mg/kg single dose.
The ideal drug for eradication of roundworm infestation is Piperazine citrate 100 to 150 mg/kg provided in the form of syrup, tablets, and granules at night time before sleep for one or two days. This drug paralyzes the worms so the child passes stool within 12 hours after ingesting the peperazine medicine.
If the child has any gastrointestinal symptoms such as abdominal pain, diarrhoea, constipation, nosia, vomiting, treat it properly by providing medication.
If the child has a condition of nutritional deficiency and malnutrition due to roundworms infestation, provide adequate nutritious diet to the child.
Advising the child’s parents to properly maintain the child’s hygienic condition.
Giving advice to the child and his parents that after going to the toilet, wash hands properly with soap and water.
Advise the child not to ingest any contaminated food and water.
Advise parents of child to maintain proper sanitation like proper disposal of human and animal waste.
Advise the parents to provide properly clean and safe water to the child to drink.
Advising the child’s parents to provide proper medication to the child.
Advising parents to take regular follow up.
Explain the nursing management of the child with the round worms (
To provide properly comprehensive care and support to the child.
Proper assessment of the child.
Provide complete education to the child and his parents about roundworm infestation, its causes, symptoms and signs, and its treatment.
Properly administer antiparasitic medication to the child and properly assess whether it has any kind of side effect or not.
If the child has any other type of gastrointestinal system related and other symptoms, it should be properly managed.
Provide properly nutritional food and properly cooked food to the child.
Advising the child and his parents to maintain proper good hygienic practices.
Giving advice to the child and his parents for proper hand hygiene.
Giving advice to the child and parents for proper hand washing before and after eating.
Advising parents not to provide their child with any contaminated food and drinking contaminated water.
Advise the parent to provide clean drinking water to the child and maintain proper hygienic condition and provide prepared food to the child.
To provide proper emotional support to the child and his family members.
Advising parents to avoid open defecation.
Advise parents to wash any raw vegetables and fruits properly with water.
Advise parents to keep their child’s nails short.
- Explain/Define Thread worm or pin worm infestation in child

Infestations of Enterobius vermicularis (Oxyuris vermicularis) are commonly known as pinworms or threadworms.
Pinworm or threadworm is a very common parasitic infection of infants and young children.
Pinworms and threadworms have separate sexes. Females are larger than males. It’s body is covered by a highly resistant coating called the cuticle.
Females are 8 to 13 millimeters in length and males are 2 to 5 millimeters in length.
Pinworms and threadworms mainly affect the appendix, cecum, ileum, and the ascending colon of the intestine.
Pin worms are mainly tiny, narrow and white colored worms. Pinworms and threadworms are mainly transmitted in the perianal region by scratching with nails.
Explain the Etiology/cause of the pinworm or threadworm infestation in child
Due to contaminated food,
Due to coming in contact with any contaminated surface and object like toys, towels, clothing, bedding,
Due to contact with contaminated water and soil.
Direct person-to-person transmission,
Due to environmental factors,
Due to poor hygienic practices,
Due to inadequate personal hygiene,
Due to poor environmental sanitation,
Explain the Clinical manifestation/ sign and symptoms of the pinworm or threadworm infestation in child
Itching in the anal area (pruritus ani),
Child has restlessness and irritability especially at night time,
Redness and inflammation of the skin due to scratching in the peripheral area,
Impaired sleep,
Abdominal pain,
weight loss,
loss of appetite,
Nausea and vomiting,
condition of diarrhea,
weight loss,
Area itching in female child,
Explain the Diagnostic evaluation of the child with the pinworm or threadworm
History taking and physical examination,
Early morning perianal swab,
To detect eggs of pinworms
Cellophane tape assessment (in this test cellophane tape is applied around the perianal region and then the tape is examined under a microscope to detect the presence of any pinworm eggs).
Scratch tap test assessment,
Explain the management of the child with the pinworm infestation or thread worm infestation.
Provide proper antiparasitic meditation to the child.
Ex:=
Albendazole,
Mebendazole,
Piperazine citrate,
Pyruvinium etc.
Provide proper anti-parasitic medicine to all the family members of the child who has pin worms infestation.
Advise the child’s family members to keep the child’s nails properly short.
Advising on hand washing by proper shop and water.
Dry the infected cloth properly in sunlight.
If the child is experiencing itching and irritation in the perianal region, then application of anti-pruritic cream in the perianal region.
Advising the parents of the child to maintain proper environmental sanitation.
Advising on proper hand washing before and after food intake.
Advising on proper disposal of human and animal excreta.
Advise the parents to wash the garments using proper antiseptic solution and then keep them dry in sun light.
Giving advice to parents about drinking clean and safe water.
Advise parents to keep their nails short.
Advising the parents to bathe the child daily.
Advise to keep the perianal area properly clean.
Provide proper antihelminthic medication to the child.
- Explain/Define Hook worm infection in child
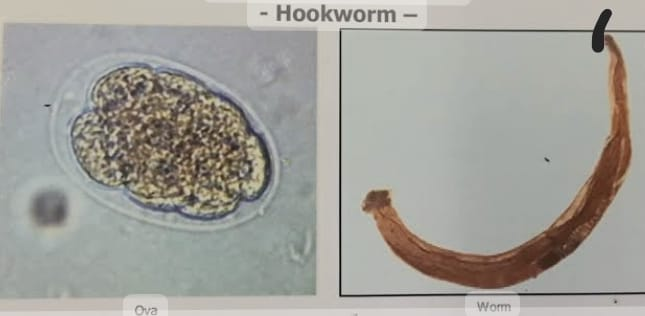
Hookworm is a roundworm infestation of the nematodes group
Hookworm infection, also known as “Ancylostoma-duodenali (ancylosto-miasis)” or nectoriasis, is a parasitic disease caused by hookworm larvae that affects the intestines of children.
Hookworms infection is mainly found in rural areas, slum areas and sub tropical areas.
Hookworm is mainly transmitted through contaminated soil and direct skin contact with a contaminated object. And due to injecting any contaminated fruits and vegetables through oral route, hookworm infestation also occurs and it affects the small intestine mainly jejunum and it also affects the lungs, bronchi and trachea in the body.
Male hookworm is 6 to 12 mm long and female hookworm is 10 to 14 mm long.
In hookworm the female hookworm is curved anteriorly dorsally. Hookworms are commonly found in agricultural areas where moist, sandy soils with deciduous vegetation are suitable for larval survival.
Iron deficiency ania is mainly seen in children due to worms infestation.
Explain the Etiology/cause of the child with the Hook worms
Due to contaminated soil and food,
Due to skin penetration,
Due to poor sanitation,
Due to inadequate sanitation,
Due to poor hygiene practices,
Due to intake of contaminated food and water,
Due to intake of contaminated food and fruits.
Explain the Clinical manifestation / Sign and symptoms of the child with the Hookworms
Finding iron deficiency anemia in children.
Loss of appetite.
Epigastric pain and cramping.
Paika.
Passing black color stool.
Diarrhea and constipation.
Irritant papulo-vesicular lesions and itching.
Child Malnutrition.
Growth retardation in the child.
Hypoproteinemia occurs.
Found in heels in the body.
nozia,
vomiting,
diarrhea,
Restlessness,
Cuffing, sneezing, wheezing and chest discomfort.
Impaired cognitive development of the child.
feeling tired
Explain the Diagnostic evaluation of the Hook worms
History tacking and physical examination,
Stool examination,
blood examination,
serological test,
imaging studies,
Abdominal ultrasound,
Abdominal X Ray
Explain the management of the child with hookworm infestation
Give proper antiparasitic medication to the child.
Ex:=
Albendazole.
Mebendazole.
Pyrantel pamoate,
Bephenium hydroxynaphthoate,
Levamisole
If the child has anemic condition, provide iron supplement. And provide iron rich food to the child.
Providing proper nutritional support to the child. And providing it with nutritious diet.
Advising the parents of the child to maintain proper hygienic condition of the child.
Advising the child’s parents to provide the child to wear properly protective shoes when playing outdoor games.
Advise the child to do regular handwashing.
Advising parents of child to maintain environmental sanitation.
Advise parents of children to prepare food in a properly clean and hygienic condition and provide clean water to the child to drink.
Advising child’s parents to wash hands properly with soap and water before and after food intake.
Advise child’s parents for proper disposal of excreta.
Advise the child’s parents to provide properly cooked food for the child’s intake.
Provide daily bathing to the child.
Giving advice to China parents to keep the child’s nails short.
Providing education to parents to wash all child’s garments properly in antiseptic solution and dry them in sunlight.
Giving advice to the parents or providing regular medication of the child.
Advising parents to take regular follow up.
- Explain/Define Tapeworm.

Tapeworms are a type of parasitic flatworm of the class “Cestoda”. Which is mainly seen in children. They are long, ribbon-like worms.
Tapeworms are separated by the structure of their segmented bodies, in which each segment is called a proglottid.
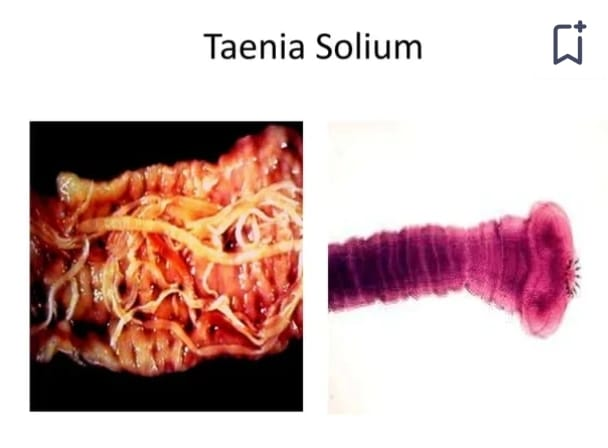
Tapeworms are mostly “Taenia solium” and “Taenia saginata”, pork tapeworms are Taeniasolium and beef tapeworm is Taenia saginata.

Taenia solium tapeworm has suckers, hooks and scolex but Taenia saginata does not have hooks.
These sugar hooks allow tapeworms to attach to children’s intestines.
Taenia saginata is 5 to 12 meters in length and Taeniasolium is 2 to 6 meters in length.
Tapeworms are primarily transmitted by ingesting water contaminated by improperly cooked meat and infected pork and beef, by improperly washed vegetables, food, and fruits, by eggs.
Tapeworms are swallowed orally by animals and then invade the striated muscles of the animal’s intestine where they develop into cysticerci. These cysticerci remain in the animal for several years and are then ingested by humans through raw and undercooked infected meat. Humans are infected due to ingestion.
Explain the Etiology / cause of the Tapeworm in child.
through contaminated food,
Due to ingestion of undercut and romit that is contaminated by tapeworms,
Due to poor hygienic conditions,
Due to exposure to contaminated environment,
Due to non-proper handling of food materials,
Due to contaminated water and soil,
Due to lack of proper hand hygiene,
Explain the Clinical manifestation/ sign and symptoms of the child with the Tapeworms.
Abdominal discomfort,
Abdominal pain and cramping,
Abdominal distension,
Nausea and vomiting,
Changes in bowel habit,
Diarrhea and constipation,
weight loss,
Visible worms in stool,
Itching and irritation,
Deficiency of vitamin B12 and iron will be observed.
Fatigue, weakness, pale skin,
pale skin,
Shortness of breath,
Certain types of allergy creations such as AD, difficulty in bridging and skin rashes,
Proglottids of tapeworms can be found in schools,
Child having headache,
Explain the Diagnostic evaluation of the child with the tape worm.
History taking and physical examination,
stool examination,
ultrasound,
CT scan,
like this. RI
CSF Examination,
serological test,
endoscopy test,
Explain the management of the child with the tape worm
Providing proper antiparasitic meditation to the child.
Ex :=
Albendazole,
Mebendazole.
Provide Prazequantel and Niclosamide medication to the child.
Providing Mepacrine, Niclosamide meditation to the child.
Advise the child’s parents to provide properly cooked food and clean food to the child.
Giving advice to the child’s parents to maintain the child’s hygienic condition.
Advise the child’s parents to provide properly clean drinking water to the child.
Advise the parents or provide education to the child for proper hand washing before and after eating.
To provide complete information to the child’s parents about the child’s disease, its causes, its symptoms and signs and its treatment.
Advise child’s parents for proper disposal of excreta.
Giving advice to parents or providing education to their child or washing hands properly with soap and water after going to the bathroom.
Advise parents to wash all vegetables and fruits with proper water.
Advise parents to consume raw fruits vegetables and meat.
Advise parents to provide their child with properly clean/boiled water intake.
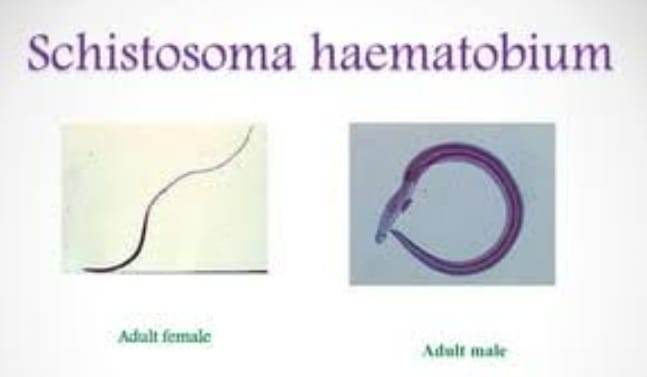
- Explain/Define schistoma Hematobiun (Flukes).
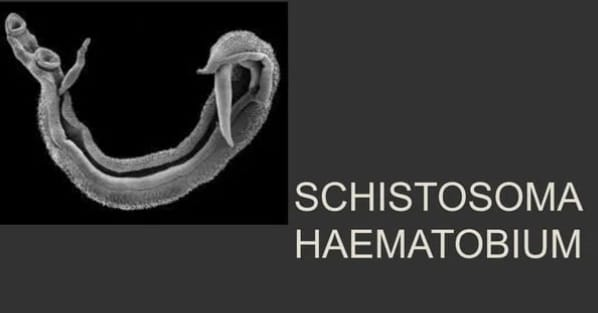
Schistoma haematobium is a worm infection in children caused by flukes (trematodes).
Schistoma haematobium, also known as bladder fluke or blood fluke, can infect children just as it infects adults.
When children get an infection with Schistoma haematobium, children may also experience symptoms similar to those seen in adults, such as blood in the urine (hematuria),
Symptoms like pain (dysuria) during urination are seen.
In children, if not given immediate attention, infection can lead to stunted growth, cognitive impairment and other developmental problems.
After malaria and intestinal helminthiasis, schistosomiasis is the third most devastating tropical disease in the world.
Schistoma haematobium affects organs like skin, brain, muscles, adrenal gland, ice, bladder, urinary tract, kidney etc. Schistoma haematobium is caused by contact with fresh water contaminated by parasitic larval cercaraie (cercariae).
These larvae are released from infected fresh water snails, can penetrate the skin of children exposed to contaminated water during activities such as swimming, bathing or washing. Therefore, contact with contaminated water rather than fresh water is the primary source of transmission of Schistosoma haematobium in children and adults. Schistosoma haematobium is more common in South America and Africa.
Explain the Etiology/cause of the Schistoma Hematobiun in child.
Contaminated water:
Infected individuals pass out the eggs of Schistoma haematobium through their urine into fresh water bodies like lakes, rivers.
Once in the water, Schistoma haematobium is released from the eggs, which release larvae called miracidia. The miracidia then infect specific freshwater snails, where they undergo development and multiplication. Inside the snail, the larvae are free-swimming cercariae. devop in, which is released into water.
When children come into contact with contaminated water while playing, swimming or bathing, cercariae penetrate their skin, entering their blood stream. Inside the body, cercariae migrate into the blood vessels around the bladder and reproductive organs, where they develop into adult worms. and schistoma haematobium develops.
Explain the clinical manifestation / sign and symptoms of the child with the Schistoma Hematobiun. (Explain the symptoms and signs of a child with schistoma haematobium.)
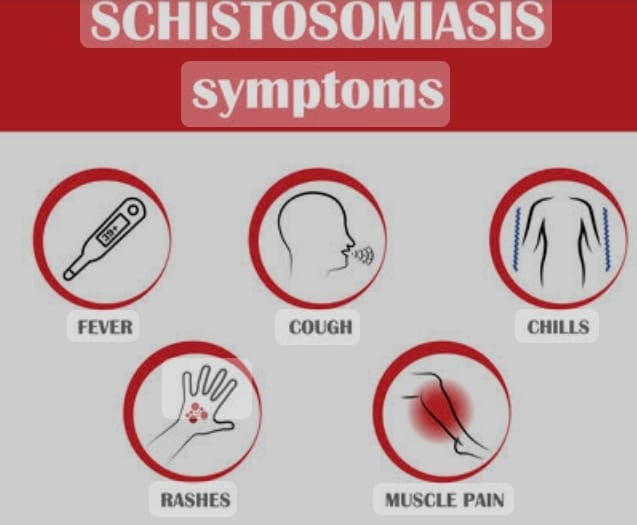
Passing blood in the urine (hematuria),
Pain during urination,
(dysuria),
Increased urinary frequency,
Urinary tract infection,
Abdominal pain,
feel tired,
weakness,
Delay in child’s growth and development,
fever,
expectoration,
muscle contraction,
Abdominal pain,
diarrhea,
hepatosplenomegaly,
eosinophilia,
passing blood in the stool,
Finding anemia in a child,
Child malnourishment,
Recesses in the skin and itching in the skin,
acute dermatitis,
Nausea and vomiting.
Explain the Diagnostic evaluation of the child with the Schistoma Hematobiun
History tacking and physical examination,
Stool examination,
Urine Examination,
serological test,
imaging studies,
ultrasound,
computed tomography,
biopsy,
Explain the management of the child with the Schistoma Hematobium
Complete assessment of the child.
Provide antiparasitic medication to the child.
Ex:= Prazequantel .
Proper symptomatic management of the child.
If the child has condition of abdominal pain and dysuria then provide painkiller medication.
Ex:= Acetaminophen,
Non-steroidal anti-inflammatory drug (NSAID).
Properly monitoring whether the child’s treatment is effective or not.
Advising the parents of the child to prevent the child from coming into contact with contaminated water.
Advise the parents to provide the child with boiled clean water intake.
Advise parents or provide education to their child about hand hygiene.
Advise parents to provide their child to wear properly protective shoes.
To provide complete education to the child’s parents about their child’s disease condition, its causes, symptoms and signs, and its treatment.
To provide proper psychological support to the child’s parents and the child.
Giving advice to the child’s parents to maintain the child’s personal hygiene.
Advise the child’s parents to provide medical treatment to the child immediately.
To provide proper education to the parents to take proper care of the child.
Advising the parents to follow up the child regularly.
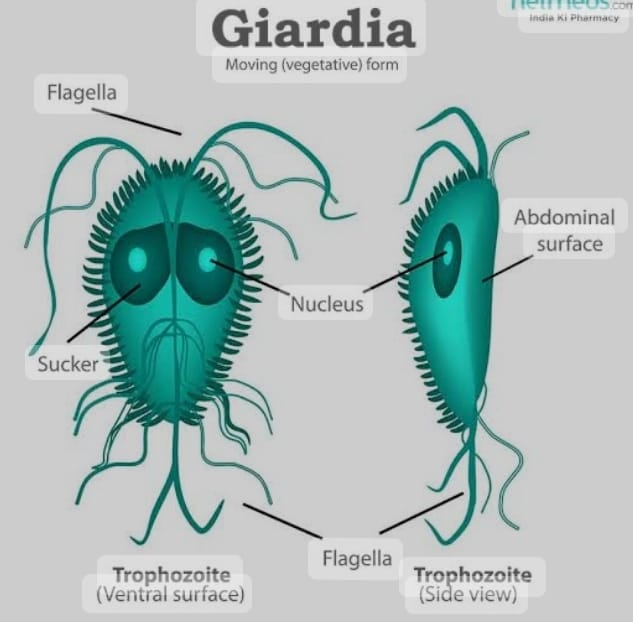
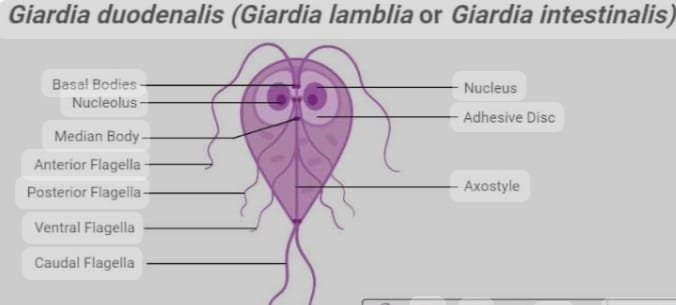
- Explain/Define Giardiasis.
Giardiasis is an infection of the upper small intestine caused by the microscopic parasite Giardiamblia. (also known as “Giardia intestinalis” or “Giardia duodenalis”) can affect children and adults alike, but is especially common in children in areas with poor sanitation or contaminated water sources, malnutrition and immunodeficiency. It is especially seen in children.
Giardiasis is an important cause of morbidity in infancy and childhood. Giardiasis can be a fatal condition if not properly treated.
Giardiasis is usually transmitted by ingestion of water or food contaminated with Giardia cysts (cycts). Cysts can survive in water, soil and surfaces for long periods of time, making transmission easy, especially in areas with poor sanitation conditions.
Explain the Etiology/cause of the child with the Giardiasis
Due to intake of contaminated water,
Due to poor sanitation,
Due to contaminated food,
Due to coming in contact with contaminated object,
Due to coming in contact with contaminated surface
Due to intake of raw food, fruits and vegetables,
Infected person to person transmission,
Due to coming in contact with infected animals,
Due to coming in contact with infected animals and their physes.
Due to unhygienic conditions.
Explain the Clinical manifestation/ sign and symptoms of the child with the Giardiasis
Foul smelling diarrhoea,
Dehydration
Abdominal distension,
flatulence,
epigastric cramps,
nozia,
vomiting,
poor appetite,
Steatorrhea (excretion of abnormal quantity of fat in stool due to reduced absorption of fat by intestine),
malabsorption of lactose,
loss of appetite,
Absence of blood and mucus present in stool,
feel tired,
weight loss,
headache,
abdominal pain,
Explain the Diagnostic evaluation of the Giardiasis in child
History tacking and physical examination,
Findings of Giardia lamblia by aspiration of duodenal material,
stool examination,
Faecal antigen ELISA test (ELISA) for parasitic dissection,
Intestinal biopsy,
imaging studies,
computed tomography,
Explain the medical management of the child with the Giardiasis
Provide antibiotic medication to the child.
Ex:= Metronidazole 15mg/ kg/ day in 3 divided doses for 10 days.
Tinidazole 50 to 75 mg/kg single dose,
or 20 mg/ kg/ day in divided doses for five days.
Nitazoxanide up to 3 day medication is a popular option for children as it is available in liquid form.
If the child has the condition of giardiasis
Mepacrine,
Secnidazole
Ornidazole Or
Provide Albendazole medication.
Child no
Perform symptomatic management.
If the child has the condition of diarrhea and abdominal colic, give advice to avoid milk items.
Advise child to provide adequate protein and calorie rich diet along with liberal diet.
Advise the child to provide proper vitamin supplements i.e. vitamin A rich diet.
Giving advice to the child’s parents that the child should avoid high spicy and fried food.
Advising parents to maintain good personal hygiene of child.
Provide intravenous fluid to maintain child’s hydration status.
If the child has a condition of diarrhea, provide antidiarrheal medication.
If the child has abdominal pain, provide antispasmodic medication.
Provide a nutritious diet to the child to prevent malnutrition and weight loss.
Giving advice to parents of child to maintain good hygienic condition of child.
Advise the parents of the child to provide clean drinking water to the child.
Advising the child’s parents to provide regular medication to the child.
Explain the Nursing management of the child with the Giardiasis
To properly assess the child’s symptoms.
To properly assess the child’s vital signs.
To the child and his parents
Complete information about the causes, symptoms and signs of giardiasis, and its treatment.
Advising the parents of the child to practice proper hygiene.
Advise the child to wash hands properly with soap and water.
Advising parents of children on safe food handling.
Advise the parents to provide proper antiparasitic medication to the child.
To provide education to the parents to provide nutritional status to the child.
Advise the child’s parents to maintain the child’s hydration status.
Provide proper psychological support to the child.
Advise the child to do proper handwashing.
Advise the child to ingest properly cooked food.
Advise the child’s parents to keep the child’s nails properly trimmed.
To provide proper medication to the child’s parents.
To provide proper follow-up to the parents of the child.
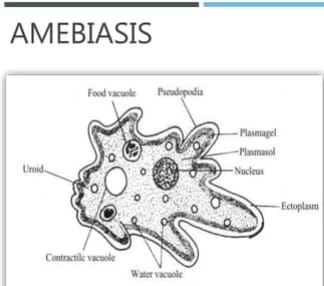
Explain/Define Amebiasis
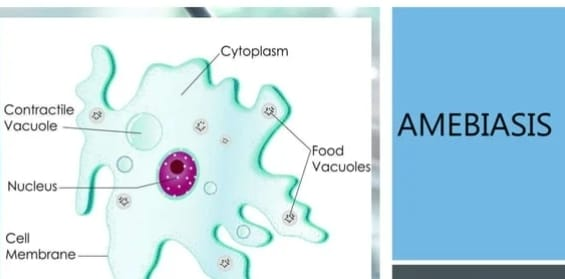
Amebiasis is a major protozoal infection seen in children.
Amebiasis in children is an infectious disease caused by the protozoan parasitic Entamoeba histolytica.

These diseases mainly affect the intestines but other organs are also involved, such as the liver, lungs affecting the gastrointestinal system.
Amoebiasis is more commonly found in areas with poor hygienic and sanitation conditions.
Explain the Etiology/cause of the Amebiasis
Caused by the protozoa Entamoeba histolytica,
Due to ingestion of contaminated food and water,
Due to poor hygienic conditions,
Due to poor sanitation and unhygienic conditions,
Due to direct person-to-person transmission,
Due to contact with contaminated surfaces,
Due to low socio economic status,
Due to ingestion of raw contaminated vegetables,
Due to putting contaminated fingernails in the mouth,
By phyco-oral route
Explain the clinical manifestation / sign and symptoms of the child with the Amebiasis.
Abdominal pain,
Abdominal cramps,
Getting a low grade fever,
feeling cold,
diarrhea,
Passage of blood and mucus in the stool,
feel tired,
Nausea and vomiting,
weight loss,
fever,
hepatomegaly,
Abdominal cramps,
weight loss,
Abdominal discomfort,
Tenesmus (tenesmus is a filling that requires emptying of stool even though the bowel is already empty. It involves straining, pain, and cramping.)
Explain the Diagnostic evaluation of the child with the Amebiasis.
History tacking and physical examination,
Laboratory Investigation,
stool examination,
sigmoidoscopy,
mucosal biopsy,
ultrasonography,
chest x-ray,
CT scan,
like this. R. eye test,
blood examination,
Serological test (ELISA),
Endoscopic examination.
Explain the medical management of the child with the Amebiasis
Provide antimicrobial therapy to the child.
Ex:
Metronidazole 20 to 50 mg/ kg per day after meals in 3 divided doses for 10 to 14 days.
Tinidazole 50 to 60 mg/ kg / day in 3 divided doses for 3 days.
Diloxanide furoate 20 mg/kg/day in three divided doses for ten days.
Amebiasis drugs along with other drugs viz
Imidazole,
Ornidazole,
Secnidazole,
Paromomycine etc.
Other symptomatic management of the child with antimicrobial therapy.
Maintain child’s hydration status properly.
If the child has pain condition then provide analgesic medication.
If the child has a condition of diarrhea, provide antidiarrheal medicine.
Provide proper nutritional support to the child.
Advising the child’s parents to provide proper medication to the child and take regular follow up.
Explain the Nursing management of the child with Amebiasis. (State the nursing management of a child with amoebiasis).
Take a complete history of the child.
To provide complete information to the child and his family members about the causes of emesis, its symptoms and signs, and its treatment.
To provide education to the parents to provide proper medication to the child.
Properly monitoring whether the treatment provided to the child is effective or not.
Properly maintaining the nutritional status of the child. And giving advice to the child’s parents to balance the child well.
To provide proper psychological and emotional support to the child and his family members.
Advise the child’s parents to provide clean fluid food to the child.
Maintain child’s hydration status.
Advise the child to intake properly boiled water.
Advise the parents to provide properly cooked food to the child.
Giving advice to child’s parents to intake properly washed fruits and vegetables.
To keep the child’s nails properly short
Giving advice to parents.
Advising parents to maintain child’s personal hygiene.
Advising the parents to take proper medication of the child and giving advice for regular follow up.