ENGLISH pediatric 2016(paper no.03)
2016
Q-1 🔸a. What is Tracheo Oesophageal Fistula? 02
- TEF is a congenital anomaly of the gastrointestinal system. In which there is abnormal communication between trachea and esophagus.
- Mainly this problem is seen in low birth weight or premature baby.
- Trachea and esophagus are fused by incomplete folds during the gestation period of fourth-fifth week of intrauterine life of the baby. Due to which this abnormal connection is seen between the two structures.
- It is also classified into several types based on the communication between trachea and esophagus. After the birth of the child, due to this problem, its nutritional needs are mainly compromised and complications related to the respiratory tract are seen.
🔸b. Write down etiology and clinical manifestation of Tracheo Oesophaleal Fistula. Write the causes and clinical manifestations of tracheo isocrachial fistula 05
Reasons for developing TEF.
- The main reason why TEF develops is not known but some contributory factors are as follows. In which genetic factor has a very important role.
- This problem can also be seen due to intrauterine growth failure of the baby.
Due to the teratogenic effect during fetal life, there are possibilities of this type of problem in the child.
In TEF, the structure between the esophagus and the trachea fails to grow. Due to which this problem is seen..
- Additional factors for the development of TEF include the fact that the antenatal mother did not receive proper care during the antenatal period and she has an infection or she is abusing any substance.
Clinical Manifestation of TEF.
- The clinical manifestation of TEF is based on the type of TEF developed, with different types of signs and symptoms.
Clinical features are usually seen soon after birth in this disorder. - Excessive salivation is seen in the child and bubbles are seen in his mouth.
A large amount of secretion is released from the oral cavity. - Nasal secretions are also sometimes seen and cuffing and choking sensations are also seen in the child.
Nozia and gagging are also seen in the child.
- Spasm of the child’s larynx is observed due to saliva moving into the trachea. So sometimes cyanosis is also seen.
When a baby is breastfed, the baby experiences a gagging sensation and choking reflex at the very beginning of feeding, and fluid escapes from the nasal cavity and oral cavity through cuffing. - Cyanosis is seen in the child due to cough and the child’s breathing is also temporarily abnormal.
Abdominal distention is also seen in many children. - Feeding in the baby can also lead to respiratory tract infection due to frequent trachea.
🔸c. Write down nursing management of it. 05
- Nursing management of TEF is done very carefully. Because if this condition is diagnosed as early as possible after birth, additional complications caused by it can be prevented.
- Airway is kept clear by suctioning the child from time to time. Due to which the breathing pattern remains normal and cyanosis is not seen.
- Oxygen therapy is also given when the child needs it, especially in case of cyanosis.
- Vital signs of the child should be closely monitored.
- The child is placed on Neil by Mouth (NBM) and intravenous fluid therapy is administered to maintain the child’s hydration level and nutritional status.
- It is necessary to rule out the child’s abdomen for distension.
- After the surgery, if the child has a chest tube placed, then taking proper care of this tube is very important. Monitoring and recording whether drainage is adequate.
- It is necessary to dress the chest tube with aseptic technique and take all precautions to prevent infection.
- Special care is taken of the anastomosed part of the child and care of the nasogastric tube is also very important.
- After the surgery, the child’s elbow is restrained. So proper care of drainage tube and nasogastric tube can be maintained.
- Oxygen therapy is also given as needed. The child’s vital signs are also specially monitored for early identification of any complications. If any complication develops, immediate management is undertaken.
- All equipment for emergency and critical care of the child is kept on stand by.
- After the operation the baby’s condition stabilizes, the baby is gradually started feeding and the baby’s condition is monitored.
- At the time of discharge of the child, it is necessary to explain to the mother and father about all the care to be taken at home, to explain to take precautions for infection prevention, to explain to maintain the nutritional needs of the child, and also to explain to the mother and father for any complications and for regular follow-up.
- Psychological support is also very important to reduce the anxiety of mother and father.
Q-2
🔸a. Describe the nursing care of a baby having tetralogy of fallot. 08 .
- Nursing management of tetralogy of Fallot is as follows.
- A child with this cyanotic heart disease condition needs special care when cyanosis is seen in the child.
- Hypoxic spell i.e. the episode that occurs due to the child developing cyanosis due to not getting enough oxygenated blood is called hypoxic spell. Giving oxygen therapy to the child during this time, knee chest position is very important to overcome the special oxygen supplement spell. Give IV fluid to the child.
- Complete history collection from child’s mother and father and decide care plan accordingly.
Periodically take anthropometric measurements of the child so that growth failure in the child can be identified.
- Keep checking the child’s vital signs from time to time so that the child’s condition and oxygen level can be maintained.
- It is necessary to keep a special monitoring and recording of the feeding behavior of the child, its nutritional need and its intake and output chart.
- Investigate the child’s lab reports from time to time to get information about the child’s clinical condition.
- Assessment of the child’s respiratory system and heart sound should be done. So that the problem can be identified early.
- It is necessary to explain the condition of the child and its prognosis to the parents.
The child should be prohibited from playing outdoor games and excessive activities and his attention should be diverted to indoor games and games that reduce physical stress. - Fear and anxiety will develop in the child and his parents so psychological counseling of each is necessary.
Being a chronic problem, it is very important to take preventive care of the child as there are chances that the child may get frequent infections.
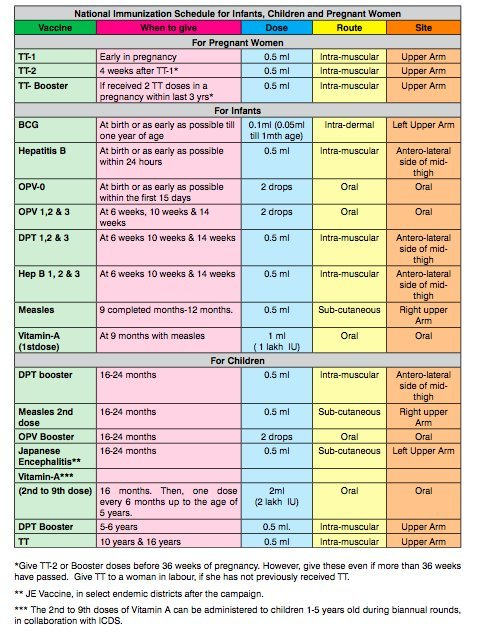
🔸b. Write down national immunization schedule for children. 04
Q-3 Answer for ANY TWO of the following:- 12
🔸a. Write the classification of Congenital Heart Disease.
- Congenital heart diseases are congenital heart abnormalities found in children.
- Structural malformations related to the heart or blood vessels arising from the heart at birth are called congenital heart diseases. Heart disease is the most common of all congenital diseases.
Congenital heart diseases are generally divided into two main categories.
Cyanotic heart disease.
Cyanosis is commonly seen in this type of heart disease. There is a decrease in pulmonary blood flow.
Right to left shunt is seen in the heart in this type of defect. So cyanosis is seen due to mixing of deoxygenated blood with oxygenated blood.
The following diseases are found in the classification of cyanotic heart diseases.
Tetralogy of Fallot
Tricuspid atresia
Trans position of great arteries
ductus arteriosus
Hypoplastic left heart syndrome
Acyanotic Heart Disease..
Cyanosis is not seen in this type of heart disease. Pulmonary blood flow increases in it and left to right shunt is seen. So oxygenated blood mixes with deoxygenated blood so that cyanosis is not usually seen in the body.
In the classification of this type of heart diseases, the following diseases are found.
Ventricular septal defect
Atrial septal defect
Patent ductus arteriosus
Atrio ventricular canal.
🔸b. Write types and causes of anemia in children.
Following are the types of anemia seen in children.
Iron deficiency anemia.
- This type of anemia is the most common type seen in children. The main cause of this anemia is iron deficiency in the child’s body. Due to which RBC maculation is not done properly and anemia is observed.
- The main causes of iron deficiency in children are as follows.
- Due to low storage of iron in the mother during intra-uterine life, it is not available to the child in sufficient quantity.
- Even if the mother is malnourished during pregnancy, the baby will not get enough iron.
- Iron deficiency is also seen in the child of a mother with twins pregnancy or multiple pregnancy.
- Apart from this, by continuing breast feeding in children for a long time, starting weaning late, not getting enough nutritious food due to poverty, lack of proper balance diet also causes iron deficiency in the child and due to this the condition of anemia is created.
- Iron deficiency is also seen in children due to some diseases such as diarrhoea, malabsorption syndrome and worm infestation and iron deficiency anemia is also seen due to any chronic illness.
Megaloblastic anemia…
- Megaloblastic anemia occurs due to deficiency of folic acid and vitamin b12. Due to lack of folic acid and vitamin b12 in these RBCs during their erythropoiesis stage, immature RBCs are large in size and megaloblastic anemia is observed due to their early division.
- The causes of folic acid and vitamin B12 deficiency are as follows.
- In order to develop this type of anemia, if the intrinsic factor secreted from the wall of the stomach is not secreted, then due to this, this type of anemia is seen to develop.
- This type of enema can also be seen due to vitamin C deficiency.
Sickle cell anemia..
- This type of anemia is an autosomal recessive disorder. This is a condition caused by a genetic abnormality. In which abnormal hemoglobin synthesis occurs. Due to which RBCs with abnormal sickle-shaped shape of C sep (C shape) are prepared. Due to which it is called sickle cell anemia.
- When the RBCs with this abnormal shape get plugged in the small capillaries and obstruct the blood circulation, there is a decrease in the oxygen situation in the blood and a lot of pain is seen at the place where the RBCs are plugged, it is seen as sickle cell crisis or vaso occlusive crisis. Due to this there is also a possibility of developing infarction.
- Hemolytic crisis also occurs due to simultaneous destruction of many RBCs.
- Genetic and chromosomal abnormalities are the reasons for developing this type of anemia.
Aplastic anemia…
- This type of anemia occurs due to bone marrow depression.
- The blood cells produced by the bone marrow are produced in very small quantities. Due to which the number of all blood cells in the body decreases. This is known as pancytopenia.
- If only decrease in number of RBCs is observed due to this, it is known as hypoplastic anemia.
- Anemia occurs due to bone marrow not being able to produce sufficient number of RBCs and is called aplastic anemia. Genetic and chromosomal abnormalities are the main causes of congenital aplastic anemia.
- Among the causes of acquired plastic anemia are viral infection, bacterial infection, any type of malignancy, radiation therapy or exposure to any type of radiation, harmful chemical and medicine also there are possibilities of this type of anemia.
🔸c. Write fractures and accidents seen in children.
Fracture means a break in the continuity of the bone in the body from any place.
Fractures seen in children are slightly different from fractures seen in adults.
Fractures in children are usually caused by a fall or any other type of injury.
Sometimes due to any disease condition, it is common to get faeces in children.
Following are the types of common faeces seen in children.
Complete fracture.
When there is a complete fracture in the bone and no connection between the two ends is attached, it is called a complete fracture. This fracture can be oblique, spiral or transverse.
Incomplete fracture.
When the bone is not completely broken i.e. its two ends are not completely separated from each other then it is called incomplete fracture.
Open fracture.
This fracture is also called compound fracture. In which after breaking the bone, it breaks the skin and tissue and is seen on the outside.
Close fracture.
When after the fracture in the bone, it penetrates the skin or tissue and is not visible on the outside but is fractured inside the bone, it is called a closed fracture.
Green Stick Fracture..
These bones are partially fractured and the bone is bent, but the fracture does not cross the bone completely.
plastic deformation.
It is also called bending fracture. In children, this type of fracture is usually seen in the ulna bone.
Part of this bone is seen to be banded and microscopic fracture lines are seen along the bone.
Following are the common accidents seen in children
When any child gets any kind of damage or injury suddenly it is called an accident. Children also die due to many accidents among young children. Certain types of accidents also create emergency situations in children.
Following are the common accidents seen in children.
- During the infertile period, the child cannot walk or run much, but it can walk and move from one place to another. So it is likely to happen due to the following accidents.
- A child falls from any place and the injury caused by impact is seen. Because at this time the child does not have control over coordination and motor movement. So, running and hitting injuries are commonly seen.
- Aspiration of foreign body i.e. in small child this stage is known as oral state. In which the child mouths whatever object is around. There are chances of aspirating or getting trapped in the respiratory tract or digestive tract.
- Any of these foreign bodies can enter the child’s eyes, nose, ears anywhere, which should be taken care of.
- Apart from this, it is common for a small child to get burned or burned by anything. Causes of buns include burns from hot water, burns from fire, shot at any place in the plug etc.
- A child can drown by falling into water anywhere, including falling into a tub, open drain, or water tank and drowning. So drowning injuries are commonly seen in children.
- Toddler, preschool and school going children are very active and their maximum time is spent running around and playing outdoor games. So sports injuries, fall down injuries, vehicle accidents, drowning etc. injuries are commonly seen in children of this age.
Q.4 Write Short notes on ANY THREE of the following:- 12
🔸1.Marasmus-–
Marasmus…
Marasmus is a severe form of protein energy malnutrition. In which, especially in children, due to deficiency of protein and energy i.e. calories, severe muscle wasting and fat loss are seen in the body.
50% weight loss is seen according to the age of this child.
Causes of Marasmus
- This condition develops when the child does not get enough protein and calories because its nutritional requirements are not met.
- This child does not get enough food in terms of quality and quantity.
- This type of condition can be seen if the child is taking artificial feeding or is given diluted feeding.
- If the child is exclusively breastfed even after six months, this condition can develop in the long run.
- This condition can occur when a child has an inflammatory disease or serious disease condition involving a gastrointestinal tract.
- A child may also develop this condition due to prolonged vomiting and diarrhoea.
- This condition can also develop when the child has any chronic diseases or diseases related to structural mal formation or mal absorption syndrome.
- This condition is more commonly seen in infants than in older children. During this time, the child has a high requirement of energy i.e. carbohydrates. Due to lack of which, this condition is seen developing especially in infants.
Classification of Marasmus..
According to the degree of fat and muscle loss from the body in this condition, it is classified into different grades.
- Grade 1. Fat loss occurs from the axilla and groin area.
- Grade 2. In addition to the axilla and groin, there is fat loss from the abdomen and gluteal areas.
- Grade 3. In addition to Grades 1 and 2, fat loss occurs from the chest and spine.
- Grade 4. In this last grade, all fat is lost from around the mouth.
Clinical Manifestations of Marasmus.
In this condition, fat loss occurs gradually from every part of the body and the weight of the child decreases continuously.
The child looks aged. The child’s face looks like a monkey. The child is constantly irritable.
Constipation and diarrhea alternate in the child.
Signs and symptoms of severe electrolyte imbalance are seen in the child. Due to which many neurological and cardiological complications also develop.
The child is less active.
Due to loss of weight and not getting enough nutritional food in the child, many diseases and many infections are also caused. Due to some complications, the child may also die.
- Diagnosis..
- History Collection
- Physical Examination
- X-ray (to detect systemic diseases and disorders)
- management..
In this condition, children are given high calorie diet. A diet with double calories than its requirement can also be given to the child if it is tolerated. It is necessary to gradually increase the quality and content of the diet.
Gradually increase the amount of carbohydrates in the food. If there is diarrhoea, the sugar intake is gradually increased.
Concentrated thick formula feeding should be given to the baby.
Antibiotics or medicine can be given as per doctor order for infection.
If any surgical condition is identified, surgical correction can be done.
The psychological condition of the child is also taken care of.
Continuous monitoring of baby’s abdomen and growth chart is kept for weight if needed.
It is very important to maintain the temperature of the child’s body.
After the baby starts gaining weight, the baby can be gradually shifted to a home made all balance diet.
Give the child exclusive best feeding for six months. After that, the child is shifted to compulsory weaning diet and breast feeding is given as and when required.
🔸2.Meningitis-
Meningitis..
The tissue layer surrounding the brain and spinal cord is called the meninges. Inflammation of this tissue layer due to any reason is known as meningitis.
A high mortality and morbidity rate is seen due to this problem in children.
Bacteria, viruses and many pathogens are responsible for causing meningitis.
Types of Meningitis..
Bacterial meningitis.
- This type of meningitis is caused by different types of bacteria like meningococcal, pneumococcal, streptococcal etc.
Viral meningitis.
- It is caused by different types of viruses such as Haemophilus influenzae type B virus.
- TB meningitis is also seen due to the causative organism of TB.
Causes for meningitis.
- Bacteria, viruses, chronic infections, diabetes, patients taking immunosuppressive drugs, different types of malignancy, etc. cause meningitis.
Sign ad symptoms..
- Excessive crying, nosia, vomiting, irritability are seen in the child.
- Sometimes convulsions can also be seen in the child.
- Cyanosis, apnea can also be seen in the child.
- Fever and sleep disturbance are seen due to infection.
- Feeding proper is not observed in the child. Nutritional imbalance is observed.
- All the symptoms of increased intracranial pressure are seen. This leads to bulging frontanles.
- Muscular rigidity and headache are seen in the child.
- In severe cases the child may also have signs and symptoms of neurological abnormality.
- There are two main signs especially seen in children with meningitis which are as follows.
Kerning sign.
- When the child is placed upright in the supine position and the hip is flexed to 90 degrees, pain is observed on passive extension of the ankle, then this sign is positive. Such a child cannot straighten his leg completely.
Broodzinki sign.
- When this child is placed upright and the neck is flexed, both extremities are flexed. When passive flexion of any one extremity is done, flexion of the other extremity is also observed. Pain is also seen during movement of the activity.
If both the above signs are positive, there is a possibility of having meningitis.
- Diagnosis..
- History Collection
- Physical Examination
- Neurological examination
- Clinical Examination
- Lumbar puncture
- Blood investment etc
management..
In the management of meningitis, antibiotic therapy, intravenous fluid therapy is given as per the doctor’s order.
Intravenous fluid therapy is given to the child to maintain fluid and electrolyte balance.
Antipyretic medicine is given to reduce fever.
Apart from this, the child is given supportive medicine based on his signs and symptoms like antacid, anti emetic etc. as per the doctor’s order.
Oxygen therapy is also given as a support therapy if the child needs it.
Isolate the child to prevent infection to him and other health care team members.
To monitor the baby’s vital signs regularly.
Stop additional stimulation from outside environment Provide work and comfortable environment to the child.
Specially monitor the child’s neurological function and notify any abnormality.
Keep changing the baby’s position and keeping the side rails of the bed high.
Maintain intake and output chart of the child specially.
To maintain general hygienic care and skin care of the child.
Provide psychological and emotional support to the child through the use of recreational care and mind divert therapy. Explain the child’s prognosis to the child’s parents and counsel them to reduce their emotional and psychological anxiety.
🔸3.Leukemia-
Leukemia is a common disorder seen in children. In which there is continuous production of uncontrolled immature abnormal WBC of BC.
Due to the abnormal function of these bone marrows, the normal production of RBCs, WBCs and other cells is affected.
Leukemia is the most common neoplastic disease in children.
Causes of Leukemia
- There is no known exact cause of leukemia. But following risk factors can lead to leukemia.
- Genetic factors
- Environmental factors
- virus
- Exposure to ionizing radiation
- Leukemia is also common due to certain genetic and chromosomal diseases.
The types of leukemia are as follows.
Acute Lymphocytic Leukemia..
- Acute lymphocytic leukemia is a disorder of the bone marrow. In which elements of the bone marrow are replaced by immature blast cells. Due to this, anemia, thrombocytopenia and decrease in other blood cell numbers are seen.
- This disorder is commonly seen in children between the ages of 3 and 7 years. Male child is more commonly affected than female child.
Mainly this condition is seen due to leukemic cells replacing normal bone marrow cells.
Acute Non Lymphocytic Leukemia…
This is a common malignant disorder of bone marrow. In which the proliferation of immature monocytes and myelocytes takes place in the bone marrow, due to which this condition arises.
Clinical features…
Fever, Building, Anemia, Bone pain, Hepato splenic megali, Thrombocytopenia, Purpura ecchymosis, Gastrointestinal bleeding, Cerebral hemorrhage, Pallor, Joint pain, Anorexia, Malaise, Decrease activity level, Weight loss, Muscle wasting, Malaina, Hemechua, Headache, Drowsiness, Nosia, Vomiting, Unconsciousness etc..
- Diagnostic evaluation
- Blood examination
- Low blood counts
- Low W Bisi Countess
- Peripheral blood examination
- CSF study etc..
management..
- Antibiotic therapy
- Corticosteroids and Immunosuppressive Medicines
- Chemotherapy
- Radiation therapy
- Bone marrow transplantation
Nursing Management..
- Informing the child and his parents about the prognosis of the disease and giving him psychological support and making efforts to reduce anxiety.
- As a nurse you should spend your time with the child and plan the treatment according to his needs.
- Prevention of infection and pain management in children
- Administer antibiotic therapy.
- Taking measurements for hygiene and cleanliness.
- Restricting entry of visitors.
- Intravenous fluid therapy is given to maintain fluid and electrolyte balance in the child.
- Intramuscular injection should be avoided.
- No precautions should be taken during blood transfusion.
- Take special care and attention so that the child does not get hurt in any part of the body. Advise the child to use a soft toothbrush. Take special care of baby’s lips and face as baby has developed bleeding tendency.
- The nutritional level of the child should be closely monitored and maintained normal.
To record the child’s vital signs and report any abnormalities immediately.
Due to chemotherapy and radiation therapy of the child, image changes, hair loss, taking psychological and emotional care of the child and boosting his confidence. - Advise the mother father for regular follow up and convince the child to visit the hospital immediately for any complications.
🔸4.APGAR score –
- An important immediate assessment after the birth of a newborn baby is the Apgar score assessment. This scoring system is given by Dr. Virginia Apgar. In which the following parameters of the child are measured immediately after birth viz
- Respiration, heart rate, muscle tone, reflex response and skin color are the five parameters that the neonate is monitored for one to five minutes.
- Each parameter is given a score of 2, 1, and 0 for its normal, subnormal, and absent function.
- After 5 minutes of assessment, the score of each parameter is totaled. The total score is given out of 10.
- If the newborn’s Apgar score is between 7 and 10 after the five-minute assessment, the child is found to have no adjustment or physical problem.
- If a child’s Apkar score is between 4 and 6, it indicates that the child has some difficulty. This score indicates mild to moderate depression.
- If the child’s score is found to be 3 or below 3, this condition indicates severe depression in the child and indicates that the child needs immediate emergency management.
- As this Apgar score is monitored immediately after birth, every parameter in the first minute is associated with extra-uterine life adjustment, so the parameter that occurs at five minutes is known as the true parameter. Because within five minutes the child has adjusted enough with the external environment. So that the normal function of each parameter can be well assessed.
- A room with a comfortable environment should be present while assessing the above Apgar score. There should be enough light. Infection prevention measures should be taken and every information should be recorded. The mother should accompany the child if possible during Apgar assessment.
- It is necessary to rule out the obstetrical history of the mother, her physical condition, presence of any disease condition, presence of any risk factor before the birth of the child.
Q-5 Define ANY SIX of the following terms. 12 .
🔸1.Croup
This is a type of upper respiratory tract and laryngeal infection. Because of that absolutely
A loud and hoarse cough, hoarseness of voice, stridor and fever are seen.
This is mainly seen in laryngitis. Due to which sometimes breathlessness, restlessness and cyanosis are also seen due to blocking of respiratory passages.
Croup is also known as laryngotracheobronchitis.
🔸2.Convulsion-convulsion
Convulsion occurs due to involuntary movement of voluntary muscles. Due to disturbances in the function of the brain, more electrical impulses are sent by the brain to the skeletal muscles and involuntary rapid movement of these muscles is seen.
Convulsions are accompanied by changes in the level of consciousness. Convulsions are also called seizures.
Convulsions are common in young children. Convulsions can occur in young children for many reasons such as febrile convulsions due to fever.
Motor movements in convulsions are seen in different ways and are also classified differently according to their patterns.
🔸3.Intussusception-
Intussusception is when the wall of the intestine is indented like a telescope. In it, a part of the intestine gets trapped inside.
This is a condition of intestinal obstruction seen in children. This is a type of medical emergency. This is usually seen near the ileocecal region.
Due to this obstruction there is blockage of gas and secretion and due to not proper blood circulation edema i.e. swelling is seen. Sometimes necrosis and gangrene can also develop due to it.
🔸4.Diphtheria–
Diphtheria is a bacterial infection caused by the corny bacterium diphtheria bacilli. This causes inflammation in the mucous membrane of the oral cavity and upper respiratory tract.
Bacterial toxins cause severe inflammation in this membrane.
Laryngeal diphtheria can also cause more severe symptoms.
Signs and symptoms such as fever, hoarseness of voice, white patches on mucus membrane, cuffing etc. are also seen.
🔸5.Bronchitis —
Inflammation in the mucus membrane of the bronchi and bronchial tree is called bronchitis. It is a common condition for children.
Causes include bacteria, viruses and certain allergic substances that can cause this condition.
Along with cuffing and mucus production, sometimes breathing difficulties are also seen.
🔸6.Pyloric stenosis –
It is a congenital anomaly of the gastrointestinal tract. In which there is hypertrophy of the pyloric muscles located in the lower part of the stomach. Due to hypertrophy of these circular muscles, its size decreases and its lumen becomes narrow. This condition is known as hypertrophic pyloric stenosis.
This narrows the opening of the pyloric sphincter muscle. Due to which the content of the stomach has difficulty in going to the small intestine and it follows back and is seen in the form of vomiting.
🔸7.Hypospadiasis-
This is a type of congenital anomaly of the urinary system. In which the opening of the urethra in the child is seen on the ventral surface i.e. under the part of the penis instead of the normal place of the penis.
This urethral opening is found on the underside of the penis. It is a common congenital anomaly of the urinary system seen in males. In which the child has difficulty passing urine in a normal flow.
This type of problem is also seen in female child. In which the urethral opening opens downward into the vaginal cavity so that urine drips down from the vagina.
🔸Q-6 A. Fill in the blanks :- 10
1.NICU temperature should be —-_and humidity is,_ —–NICU (Temp. 22 to 26’C, and humidity 30 to 60%)
2.Beri-Beri occurs due to ——deficiency. (Vitamin B1)
3.Acute tonsilities is caused by__________
(Beta Haemolytic Streptococcal)
4.Surgical operation for undescended testes is called_____
(Orchiopexy)
5.Umberical cord has________ vein and artery. Umbilical cord contains __ vein and ______artery. (1 vein and 2 arteries)
6.Posterior fontanel is shaped and closes at_ month.
(Triangle shape, 2 months)
7.Father of pediatric nursing is __
(Abraham Jacoby)
🔸B. State whether following statements are ‘True’ or ‘False’s 05
Gestational assessment can be done by Bellard scale (correct)
There is no tear formation in the neonate. (false)
Patient care area in PICU should be approximately 20m ^ 2(false)
Pleural effusion means collection of fluid in pleural space. (correct)
Blood volume in normal new born is doubled by age of one year. (false)