ENGLISH paed-II paper 2022 NITA(પેપર -5)
PAED-II 2022
🔸Q-1 a. Define Acute Renal Failure. 03
- Acute renal failure is when the kidney suddenly and completely loses its capacity to remove waste products from the body.
- A decrease in glomerular filtration rate is observed due to acute renal failure.
- There is a decrease in urine output.
- The concentration of blood urea nitrogen (BUN) in the body is high.
- Retention of sodium is seen
Hyperkalemia is seen.
Phases of acute renal failure
(1) Initial Phase
- In which kidney injury is seen from the time it starts until the death of the nephron. Which period is from few hours to days. This causes irreversible damage.
(2) Olig uric phase
- This phase can last for 8-15 days.
In which the urine output drops to 400 ml per day. - Blood urea nitrogen level increases (azotemia).
- Nausea, vomiting is observed.
(3) Diuretic phase
- This phase is observed for 1-2 weeks.
- In which hypo volemia is seen.
- Dehydration
Hypo tension
Tachycardia - Signs are seen as above.
(4) Recovery Phase
- Which is from one to two years.
In which the recovery process is slow. - There is an increase in glomerular filtration rate.
- A decrease in blood urea nitrogen levels is seen.
- But the GFR is permanently reduced by one to three percent of its previous levels.
🔸b. Write the etiology and clinical manifestations of Acute Renal Failure. 04
Causes of acute renal failure are as follows.
(1) Pre renal causes
- In which kidney failure is seen due to causes other than kidney like..
- Due to decrease in circulatory volume
- Due to cardiac insufficiency
- Due to vasodilatation
- Due to the above reasons, proper blood supply to the kidney does not reach due to which acute kidney failure is seen.
(2) Intra renal causes
- In which acute kidney failure occurs due to structural and functional damage of the kidney, it is called intrarenal failure. in which
- Prolonged Renal Ischemic Condition (due to reduced blood supply)
- Acute tubule necrosis
- Kidney stone
- Glomerulo nephritis
Renal failure is seen due to nephrotoxic drugs etc.
(3) Post renal causes
- Any obstruction or infection in the post-kidney structures is called post-renal cause.
- Cancer in the urinary tract
There is enlargement of the prostate gland - Cystolithiasis
- Renal failure is seen due to ureterolithiasis etc.
Signs and symptoms of renal failure
- Anemia
Oleg Uria
Dark colored urine
Foamy urine
Azotemia - Dehydration
Tachycardia
edema (swelling)
Flank pain
Shortness of brid
Generalize Malaise (Viknesh)
Hyperkalemia
Vomiting
Abdominal pain
Head one
Drowziness
Confusion
Dish orientation.
All the above symptoms are seen in renal failure patients.
🔸c. Write the nursing management of child with acute renal failure. 05
(1) Pharmacological
Urine output is increased by diuretics.
K binding drug (Kiczelate)
Which does not allow the absorption of potassium in the intestine, due to which hyperkalemia can be prevented.
A glucose insulin drip is given.
Sodium bicarbonate is given to treat acidosis conditions.
If the condition of continuous hyperkalemia is observed, then hemodialysis or peritoneal dialysis is done.
(2) Fluid and electrolyte replacement
- Fluid replacement should be done carefully. So that fluid overload and dehydration can be reduced
- Fluid replacement is done based on urine output. So that fluid overload can be reduced
- Check blood pressure and weight on a regular basis
(3) Nutritional therapy
- Giving a high calorie diet
- Administer potassium restricted diet
- Giving a carbohydrate rich diet
- Giving a low fat diet
- If hypovolemia occurs, give blood supply or fluid supply
- If acute kidney failure is found due to causes other than kidney, then treat that cause.
🔸Or🔸
🔸a. Define Pneumonia. -03
Pneumonia means inflammation of lung parenchyma and lung tissue. This condition is caused by bacteria and viruses. So that the air sac fills up so that the air sac becomes solid. It is also called pneumonitis.
Normally the air sac exchanges these gases but because of the pus fill in it, the exchange of gases is interfered with.
Classification of Pneumonia
(1) Based on anatomical structure
- (A) Lobar pneumonia An infection in a single lobe or section of the lung is called lobar pneumonia.
- (B) Bronchopneumonia When the infection starts in the bronchial tree and pneumonia occurs, it is called bronchopneumonia.
- (C) Interstitial pneumoniaPneumonia that occurs when the infection occurs between the alveoli and capillaries is called interstitial pneumonia.
(2) Based on etiological factors
- (A) Bacterial pneumonia Pneumonia caused by bacteria is called bacterial pneumonia. Which is caused by different types of bacteria.
- (B) Viral pneumonia Pneumonia caused by a virus is called viral pneumonia.
- It can be seen due to influenza, para-influenza, AD virus etc.
(3) Based on broad classification
- (A) Community acquired pneumonia When pneumonia occurs because the client lives in the community, it is called community acquired pneumonia.
- (B) Hospital acquired pneumonia When a child develops pneumonia after 48 hours of hospitalization, it is called hospital acquired pneumonia
- (C) Ventilator acquired pneumonia Pneumonia that occurs when a child is intubated or on mechanical ventilation is called ventilator-acquired pneumonia.
- (D) Aspiration pneumonia When a child aspirates any external or internal substance into the lower airways, it can cause aspiration pneumonia. The substance may be gastric content, chemical or any liquid.
🔸b. Write the etiology and clinical manifestations of Pneumonia. 04
Pneumonia is caused by the following.
Viral pneumonia including influenza, parainfluenza, adenovirus etc.
Bacterial pneumonia due to Pneumococcus, Staphylococcus, Klebsiella, E. coli etc.
Fungal pneumonia due to histoplasmosis, mycoplasma, coccidiomyosis etc.
Other Factors
- Aspiration of food
Nasal drops
Kerosene poisoning - Alter Consciousness
- Depressed cough reflex
- Impaired mucociliary transport
- Impaired alveolar macrophage function
- Andro bonyal obstruction
MU’s space condition - Low birth weight
- Mal nutrition
Poor Socio Economic Status - Large family size
- Over crowding area
Air pollution
Vitamin A deficiency
Lake of Brest Fidig
Signs and symptoms of pneumonia
- Non productive or productive cough
- Dyspnoea
- Tequipnea
- Orthopnea
- Chest pain
- Crackleous breath sound
- Means (reduced) or normal breath sound
- Chest retraction
- Paler to cyanosis
- Nasal flattening
- Weight loss
- Breasts do not fidget
- Vomiting
- Abdominal pain
Lethargy - Malays
- Diarrhea. etc. symptoms are seen.
🔸c. Write the nursing management of child with Pneumonia. 05
- Management of pneumonia can be treated by providing antibiotics
- Erythromycin and penicillin are used as antibiotics.
- Oxygen supply is given based on checking the arterial blood gases.
- The child has fever and tachypnea. Due to which there are chances of dehydration. So hydration therapy is given
- Warm most inhalations are used to relieve bronchial irritation and phlegm.
- Antihistamine and antipyretic drugs are given as per the doctor’s order.
- Regular checking of vital signs, specially oxygen level.
- If hypoxemia develops, give natural decongestants.
- Administer antitussive medication that relieves hypoxemia.
- If the respiration rate is high or the oxygen level is not maintained, the child is put on mechanical ventilation and all care is taken.
- Keep checking the child’s cyanosis level.
- Check the level of retraction in the child.
- If the baby is able to breastfeed, breastfeed with head up a little.
Q-2
🔸a. Define growth and development. Explain the various factors influencing on growth and development. 08
Growth means physical maturation in which various organs of the body increase in size and shape. Which is seen due to cell multiplication and increase in intracellular substance. Growth changes can be measured in centimeters and kilograms.
development
Development is the process by which the body matures functionally and physiologically. Development increases skill and functioning capacity. In which psychological, emotional and social changes take place. Measuring development is difficult but it can be measured.
Factors affecting growth and development
Some factors that promote or inhibit the process of growth. Which has two factors. Environmental Factors
Hereditary factor
(1) Hereditary factor
Genetic factor is an important factor. Which affects the growth and development of the child. Which affects height, body structure, skin color, eyes, and hair.
which depends on the genes of the parents. If the height of the parents is high, then the height of the child is also high, if the parents are highly intelligent, then the child will also be highly intelligent, some factors that affect the child.
Some genetic diseases that affect the growth and development of the child like thalassemia, hemophilia.
So the child has chromosomal abnormality along with that disease including Down.
Apart from this, gender also affects the growth and development of the child. While male babies are heavier and longer than female babies, girls mature earlier than boys. But height and weight are less in comparison to Bois.
Even in race and nationality, different racials have different time growth and development and their physical characteristics are different according to the national group.
(2) Environmental factors
Prenatal factors
The intrauterine environment affects fetal growth and development
Maternal Mal Nutrition
If the mother does not take a proper diet during pregnancy and if anemia is present, intrauterine growth retardation, low birth-weight, preterm baby and disturbances in its growth and development occur in later life.
Maternal infection
Some intrauterine infections such as HIV, hepatitis are transmitted to the fetus through the placenta and affect its growth and development. Due to which congenital anomalies and congenital infections are seen.
Maternal substance abuse
Some teratogenic drugs cause congenital malformation when taken during pregnancy and smoking, tobacco, alcohol also affect growth and development.
Maternal Illness
Conditions that affect fetal growth include hypertension, anemia, heart disease, hypothyroidism, diabetes, chronic renal failure, hyperpyrexia, etc. Iodine deficiency in the mother can cause mental retardation in the baby.
Miscellaneous
Prenatal conditions affect the growth of the fetus. In which uterine malformation, malposition of the fetus, bicornuate uterus, oligo hydro amnios, poly hydrominus etc affect growth and development.
Postnatal Environmental Factors
Growth pattern
The growth pattern is according to the size of the child at birth. If the baby’s birth weight is low, there may be complications going forward.
Nutrition
Nutrition is very important for the growth and development of the child. It should be quality and quantitative nutrition. Which should contain protein, carbohydrate, vitamins, fat and minerals in sufficient quantity which helps in the growth and development of the child. If the child is well nourished, physical and mental growth is seen well.
Childhood Illness
It affects the growth and development of the child like heart disease, kidney, liver malignancy, digestive disorder, metabolic disorder.
Physical Environment
Environment condition like housing its living condition environmental sanitation ventilation fresh air hygiene safe water supply growth and development
affects
Psychological Environment
Good psychological environment such as healthy family, good child-parent relationship and healthy interaction with other members of the family helps in emotional social and intellectual development. If the child does not get proper love, affection and security, it is seen as emotionally disturbed.
Cultural Influence
Culture affects growth and development. According to the culture its food habit, its beliefs, its living standard, education level etc. affect the growth and development.
Socio Economic States
Due to poor socio-economic status, the child will not be able to have proper growth and development and will not be able to get proper nutritional diet.
Climate and season.
Climate and season affect growth. Weight gain occurs in summer. The height increases in the spring season as compared to the rainy season.
Play and exercise
Physiological activity increases through play and exercise and muscular development takes place as well as physiological, social, moral, intellectual development and health improves due to physical exercise.
Intelligence
Which affects mental and social development. If the child has high intelligence, he will get adjusted in the environment. If there is low intelligence, it cannot be adjusted.
Hormonal influence
Hormones greatly affect the growth and development of a child. Problems are seen in growth and development due to imbalance in it.
🔸b. write down trends in Pediatric Nursing.- 04
In earlier times adults and children were given the same treatment. But nowadays due to higher mortality and morbidity in the pediatric age group, more importance has been given to children and child care.
Apart from this, the special area of child health is being focused on due to development in medical and surgical branches.
The following trends and practices are being observed in pediatric child health care.
Currently pediatric care is provided by pediatricians and trained registered nurses.
A scientific treatment approach is maintained in care from infancy to adolescence period.
Special vaccines are administered for disease prevention.
Regular assessment of the child’s growth and development is done.
Emphasis is placed on preventive services and health promotion rather than curative care.
Advancements in technology and science are seen in the medical field. So that high quality care can be provided.
Evidence-based practice of children’s karma is observed.
Institutional care is more emphasized than home care for any type of care for children. This institute i.e. hospital which has been developed through modernization with child friendly changes.
Family-centered care is provided through the support of parents and family members under the supervision of health care members at each care of the child. A child is not separated from his parents and family members even during illness.
Rooming in means keeping the child with the mother at most and moving forward with the mother in every care is being implemented.
Visiting hours have been increased and flexible hours have been kept during hospitalization of children.
There are support groups for parents, which help reduce the anxiety of parents. And the play and recreational needs of children are taken into consideration.
In the care of children, subspecialties of pediatric services such as pediatric neurology, cardiology, nephrology etc. have developed.
Cost containment means best care is provided at low cost and duplication of nursing care is prevented.
In preventive care, there are efforts to improve the health of the child at low cost and protect against diseases.
In Continuum of Care, care is provided continuously. Without any interference, if the child is hospitalized due to an acute disease, after giving treatment in the hospital for a few days, the next treatment is given to the child outdoors. Continuity of the drug is thus maintained.
Color coded management including green classification = child not requiring medicine but requiring advanced home care. PINK CLASSIFICATION = Child needs care provided as a patient. Yellow Classification=Child needs specific treatment at home.
🔸Or🔸
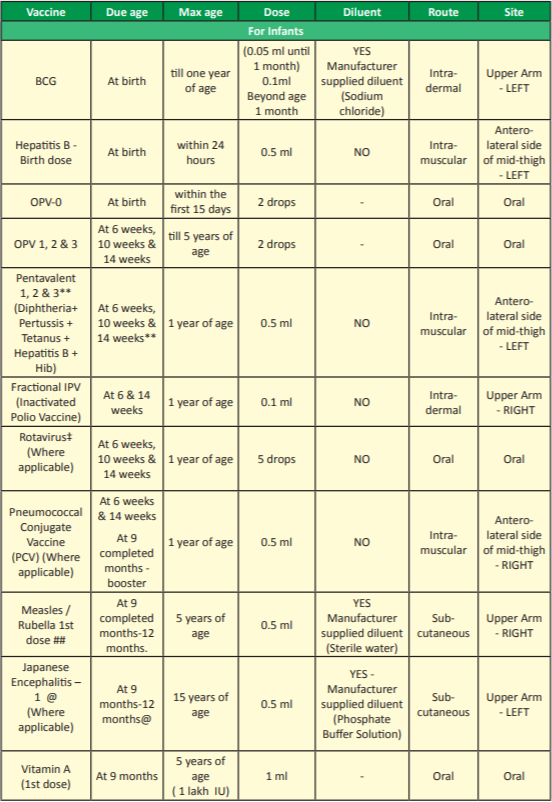
🔸a. Define immunization and write national immunization schedule for infants, children, pregnant woman and adolescent. 08
🔸b. Write the role of nurse to reduce stress in child due to hospitalization.04
The nurse helps the child and the child’s family reduce the stress of hospitalization and illness The nurse develops the relationship between the child and his parents
A pediatric nurse knows the feelings of the child and the parents. So helps to handle the problem. The nurse avoids the criticizing attitude of the parents, recognizes their anxiety and calmly listens to their complaints. The nurse helps the child and the parents to calm down and feel secure.
The nurse who provides care to the child needs a more sympathetic understanding of the parent’s needs.
Anxiety can be reduced and stress can be minimized by the following measures.
- (1) Provide family centered care
- Its stress can be reduced through family centered care which provides a home environment to the child so that the child feels comfort.
- (2) If the neonate is hospitalized, the stress of the parents can be reduced by continuous contact with the neonate and rooming in.
- (3) In the infant, the stress of the child can be reduced by reducing the separation between the parents and the child and by balancing the responsibility of the mother. In which the infant’s need is fulfilled by proper attention and handling.
- The mother is kept with the child during the procedure so that the child does not feel alone and allows the procedure to be effective. By giving toys to the infant, his tension can be relieved and his mind can be diverted.
- (4) Rooming in the toddler is provided and unlimited visit hours with the child are provided so that the child can express his feelings. All the activities like eating, bathing, sleeping are done at home.
- Familiar toys and objects should be kept with the child so that the child feels secure and the child is allowed to play. Parents should provide love and understanding to the child which helps restore the child’s trusting relationship. A child loses faith because of the Lake of Love.
- (5) When providing care to pre-school children, the anxiety can be reduced by keeping their parents together, it is planned that the child has to be hospitalized for a short duration.
- Helping the child accept stressful situations, providing love, giving the child a chance to express their feelings, and supporting careful preparation for the procedure can help. In which his privacy is maintained and it is planned according to his understanding, the child is seen to be able to participate in his hygiene and his own care.
- A proper explanation reduces his fears and reassures the child. The negative feeling of the parents towards the child is reduced. So the relationship between the child and parents can be improved.
- (6) School going children are prepared for hospitalization. Including helping the parents at that time and respecting the child’s privacy and providing him/her privacy during the examination.
- For diagnosis, the nurse takes the child’s history and provides treatment after identifying the problem. The procedure is explained and reassurance is given to the child and the child is encouraged to self-care and to continue play if possible.
- It is important to assist family members in understanding the child’s reactions when he or she is ill and to encourage parents to participate in providing care to the child and to make continuous visits with the child with the child’s friend.
- The nurse carries out activities for the promotion and restoration of the child’s health and fulfills the child’s needs by identifying them.
- (7) Assisting the adolescent child planned for hospital admission to prepare for hospitalization when ill.
- Check how illness and hospitalization have affected the child.
Introduce the hospitalized child with the nursing staff there so that anxiety can be reduced. - The nurse collects a history about the child’s illness, habits, recreation, hobbies, and respects his private needs. The procedure is explained and encouraged to cooperate. He is given recreation, peer relationships and interaction with other idols, and opportunities to express his feelings.
Q-3 Write short answers (Any Two) 2×6=12
🔸a. Define tonsillitis, writing types, etiology and the post-operative nursing care of the child with tonsillectomy.
Infection and inflammation of the tonsils is called tonsillitis.
Tonsils are located anterior to the oropharynx and posterior to the nasopharynx.
There are 2 types of tonsillitis.
- (1) Acute tonsillitis
- (2) Chronic tonsillitis
Acute tonsillitis
- Acute infection of tonsils called acute tonsillitis. This is a short term condition.
- Signs and symptoms
- It begins with a shivering and radiating pain in the throat, which moves towards the ear.
- Painful swallowing is seen.
- There is a problem in eating solid food, but there is less problem in drinking.
- Fever occurs at 39 -40 degrees Celsius
- Convulsions in young children due to fever are called febrile convulsions.
- Later tonsils are seen red and congested.
- Eustachian tube block is sometimes seen causing otitis media.
- Apart from this, symptoms like irritability, crying, weightloss etc. are also seen in the child.
Chronic tonsillitis
Inflammation of the tonsils that occurs for a long time or occurs frequently is called chronic tonsillitis.
- Signs and symptoms
- Recurrent sore throat is seen.
- Difficulty in swallowing and breathing
- Loss of appetite is seen
- Cyclic vomiting is observed
- Halitosis
- No interest in playing
- Abdominal pain
- The voice becomes thick
- The lump feels dry
- Sometimes enuresis is seen
Dyspnea occurs when the tonsils compress the airway due to chronic tonsillitis.
Chronic tonsillitis is treated with tonsillectomy if it is not treated with medical management.
Causes of Tonsillitis
- Beta hemolytic staptococcus infection
- Haemophilus influenzae type-b
- Apart from this, this condition can also be seen due to bacteria, viruses, allergens etc.
Postoperative Child Care with Tonsillectomy
- Giving the child prone and side lining position to allow drainage of secretions to prevent aspirating.
- Continuous observation of the child
- Continuous monitoring of vital signs of the child
- If the child has restlessness, frequent vomiting or regurgitation, it indicates haemorrhage.
- If there is post-operative bleeding, bring the child back to the operating room and re-corderize (re-tie) the child.
- Give ice when the child wakes up and give the child plenty of fluids to prevent dehydration
- First give synthetic fruit juice then natural fruit juice
- Do not give red and brown colored liquid as there may be confusion as to whether there is blood in the vomitus or not
- Gradually give semi-solid food from liquid
- To involve parents in child care
- Ear pain after surgery is radiating pain from throat which can be seen up to three weeks which is pain killer or chewing gum which helps to relieve the pain.
- Do not blow the nose forcefully after surgery
- Avoid crunchy and spicy food
- A post-surgery temperature of 99 degrees Fahrenheit is normal, but if it rises above 100 or 101 degrees Fahrenheit, call an ENT doctor, which is a sign of infection or dehydration.
- Oral hygiene should be maintained as bed sores are seen after surgery
- Allowing the child to play When the child is ready to play
- Keeping the child away from the infected person.
🔸b. What is diarrhea? Write its causes, clinical features and its management. What is diarrhea?
- When a child passes loose, liquid, and watery stools more than three times a day, it is called diarrhea.
- Diarrhea is the second killing disorder. Pneumonia followed by increased mortality and morbidity in the under-five age group.
- Malnutrition is seen in children due to diarrheal diseases
- Acute diarrhea is sudden diarrhea that lasts for three to seven days and is caused by an infection in the intestines.
- Acute diarrhea is seen in acute gastroenteritis
- Chronic diarrhea is more than three episodes that occur due to an organic disease
- Mucus or blood in watery and loose stool is called dysentery
Causes
- Due to viruses – rota virus, AD virus, entero virus
- Due to bacteria
- Para side, due to fungi
- It can be seen due to different environmental factors, unhygienic condition, food poisoning, food intolerance etc.
- Clinical Manifestations
- Loose and watery stools that are greenish and yellowish with an offensive smell
- Stool contains blood, pus, mucus
- Abdominal pain
- There is an increase in the frequency of passing stool, which ranges from 2 to 20 times
- Low grade fever
- Thrust
- Anorexia with vomiting
- Abdominal distension
- Behavioral changes like irritability, weakness, lethargy, sleepiness, delirium, stupor
Weight loss
- Skin turgor
- Dry lip
- Shankan I
Depressed fontanel
Low blood pressure
Tachycardia
Rapid respiration
Cold Extra Meaty - Decreases urine output
Convulsion
Symptoms like loss of consciousness are seen.
Management
Oral rehydration therapy
Hydration is maintained by ORS and breast feeding and intravenous fluids are given.
- Contains ORS
- Sodium Chloride=3.5gm
- Potassium Chloride=1.5gm
- Sodium bicarbonate=2.5gm
- Glucose=20gm
Administer antibiotic therapy as per doctor order
Symptomatic treatment is given in diarrhea
If there is fever – anti-pyretic
Skin Targer-Fluid Therapy
Vomiting-nthematic
- Providing an appropriate nutritional diet to prevent malnutrition
- Avoid high fiber rich diet and soft drinks
- Continue breast feeding
- Rice Milk,. Daliya, Saag, Khichdi should be mixed and given if the child is more than 6 months
- Maintaining hygiene while preparing food
- If the child is not breast fed, do not dilute cow’s and goat’s milk
- Can be prevented by good hand washing practices, proper disposal of stool, general cleaning
- Providing health education to the mother of the child on how to prevent diarrhea
- Changing diapers frequently can prevent skin break down and diaper rash
- Clean the baby’s clothes with an antiseptic solution and allow them to dry properly in sunlight.
🔸c. What is P.E.M? Explain in detail about kwashiorkor.
Protein energy malnutrition is a disorder caused by a nutritional deficiency. Which is caused due to low intake of protein and calories.
- There are 2 main types of PEM.
- Kwasiorkor
- Marasmus
Kawasikor
- Quasiorchor is mainly caused by protein deficiency. It is usually seen in children between six months and three years of age.
- There is no loss of subcutaneous fat and swelling in the body.
- In them, the child’s ribs are not very prominent and the child is lethargic.
- Muscle wasting is absent or normal in the child. It is seen that the child’s appetite is less.
- The baby’s face is seen in a moon shape. Baby hair changes gray or red color.
- In this condition, when adequate protein amount is given to the child, the condition of the child often seems to improve.
Management Of PEM (Kwashiorkor)
- Preventive, promotive and rehabilitative services by the nursing staff for protein energy mal nutrition is a very important responsibility for the child to get in the hospital and at home.
- A nutritional history of the child with all its dietary aspects should be collected and physical examination and anthropometric assessment should be done to know its nutritional deficiency status.
- Additional investigation should be done if necessary.
- To monitor the growth of the child, it is necessary to maintain regular growth charts. By which children with growth failure can be identified early.
- To participate in crisis management of children with PEM in hospital.
- Implementing a nutritional rehabilitation program.
- To promote the child’s parents to take good care of the child in terms of nutritional and other health aspects.
- Convince the mother and father for regular follow-up of the child.
- Breast feeding, weaning, balance diet, appropriate feeding practice, good health habits etc. Nutritional education and demonstration should be explained to mother and father.
- Explain the preventive measures of PEM to the mother and father.
- Explain the nutritional services available at village level to children from lower socio economic background.
- Monitoring the availability of nutritional services at community and individual level and record reports on nutritional program implementation.
- It is necessary to participate in the nutritional research project and work to bring awareness to the family and community.
👉Q-4Write short note (Any Three) 3×4=12
🔸1.Rights of the children usi.
The Rights of the Child were declared by the United Nations on 20 November 1959. They were made with the purpose of fulfilling the special needs of the child.
These rights are as follows.
- No right to free education.
- No right for name and nationality.
- Right to receive special care if the child is handicapped.
- Rite to get affection, love and better understanding.
- The Right to Adequate Quality Nutrition.
- Right to get first aid treatment or relief in time of any calamity or distress.
- No right to get good medical care.
Right to play well and get re-creational facility.
The right to develop one’s own abilities and become a good and useful member of society.
Right to be brought up in a calm and brotherly environment.
All the above rights are also given to the children so that every child can use all the rights equally without discrimination of religion, race, caste, sex, color etc.
🔸2.ICDS scheme –
This is an important program for the welfare of children at present. Which was started in 1975 by the Government of India.
ICDS scheme is found in every area, tribal and urban.
Initially, when starting this program, this program was started only at some selected places. But currently there are more than 5,000 functioning centers.
Objective of ICDS Scheme.
Improving the nutritional status of zero to six year old children.
To work for compensatory growth and development of children.
To reduce mortality, morbidity and mal-nutrition in children
Also reduce school drop out rate.
To establish a policy and coordination between different departments working for the promotion of children.
To increase the health capacity of the mother and supplement her nutritional diet.
The above objective is delivered to the beneficiaries through the following package services. Following are the services provided to the beneficiaries of icds programme.
- Services provided to children from zero to six years of age.
- Immunization, Health Checkup, Supplementary Nutrition, Referral Services, Non Formal Preschool Education.
- Services provided to adolescent girls.
- Supplementary Nutrition and Health Education.
- Services provided to mother.
- Health Checkup, Immunization, Supplementary Nutrition.
Dietary services are mainly provided by Anganwadi workers to the above beneficiaries. This Anganwadi worker has a population of 1000. It mainly handles this program at the village level and is involved in providing all types of services related to dietary services, preventive services, antenatal care as well as postnatal care and immunization care.
There is a supervisor i.e. head sevika for the supervision of these Anganwadi workers. Which is given some special training. who supervises all activities in coordination with the Project Officer of the ICDS programme.
Due to this program, the amount of mal nutrition is low. Immunization coverage is high. Also there is a reduction in mortality and morbidity rates in children.
🔸3.Advantages of breast feeding
- Breastfeeding develops a psychological bond between mother and baby.
- Human milk is available for the baby only as per the body temperature requirement.
- Milk is fresh and sterile and free from contamination directly into the baby’s mouth.
- Human milk is ideal if it is readily available.
- Breast milk is a safe and protective food.
There is perfect food for infants. - Meets the total nutrient requirement of the baby for the first six months.
- It is very important for baby’s brain growth because breast milk contains high amount of lactose and galactose.
- Breast milk contains vitamins, minerals, electrolytes and water which are essential for the maturation of the infant’s intestinal system.
- Breast milk provides a facility that increases the absorption of calcium so that the baby’s bone growth is good.
- Breast milk is easily digested.
- Breast milk contains all the essential nutrients that a baby needs.
- Breast milk protects the baby from infection and deficiency.
Breast milk is already prepared.
Breast feeding is a method of family planning, breast feeding is a natural contraception that has a major effect on population for developing countries.
- It prevents children from diarrhea and also has laxative action.
- Breast feeding has no dangerous allergic effects.
- Breast feeding can save time and money and energy.
- Breast feeding helps in building a healthy relationship between mother and child.
- Chances of conception decrease during lactation.
- Best feeding helps in involution of uterus (i.e. bringing uterus to pre-pregnant state).
- Breast feeding reduces the chances of sunstroke, gastrointestinal infections and ectopic eczema.
And the chances of scurvy and rickets are also reduced.
- Breast feeding reduces the chances of breast cancer.
- Breast milk contains IgA and IgM macrophages, lymphocytes, lysosomes, etc. due to which diarrhea and acute respiratory infections can be prevented in babies.
And prevents against malaria and viral and bacterial infections. - Breast milk protects against conversion, hypocalcemia, tetanus, deficiency of vitamin E and zinc.
- Exclusive breast feeding can prevent malnutrition in children.
- Breast feeding increases the intelligence of the baby, and gives the baby a sense of security (due to the infant-mother bond).
- The chances of illness in the child are reduced.
- Breast feeding reduces the chances of postpartum hemorrhage (excessive bleeding from the genital tract after delivery).
- Chances of ovarian cancer are also reduced.
- Helps reduce excess fat stored in the mother during pregnancy.
🔸4.Define Esophageal atresia and Tracheoesophageal fistula, Write the signs and nursing management of Tracheoesophageal fistula.
- TEF is a congenital anomaly of the gastrointestinal system. In which there is abnormal communication between trachea and esophagus.
- Mainly this problem is seen in low birth weight or premature baby.
- Trachea and esophagus are fused by incomplete folds during the gestation period of fourth-fifth week of intrauterine life of the baby. Due to which this abnormal connection is seen between the two structures.
- It is also classified into several types based on the communication between the trachea and the esophagus. After the birth of the child, due to this problem, its nutritional needs are mainly compromised and complications related to the respiratory tract are seen.
Clinical Manifestation of TEF.
- The clinical manifestation of TEF varies depending on the type of TEF developed, with different types of signs and symptoms.
Clinical features are usually seen soon after birth in this disorder. - Excessive salivation is seen in the child and bubbles are seen in his mouth.
A large amount of secretion is released from the oral cavity. - Nasal secretions are also sometimes seen and cuffing and choking sensations are also seen in the child.
Nozia and gagging are also seen in the child.
- Spasm of the child’s larynx is observed due to saliva moving into the trachea. So sometimes cyanosis is also seen.
When a baby is breastfed, the baby experiences a gagging sensation and choking reflex at the very beginning of feeding, and fluid escapes from the nasal cavity and oral cavity through cuffing. - Due to cough, cyanosis is seen in the child and breathing of the child is also temporarily abnormal.
Abdominal distention is also seen in many children. - Feeding in the baby can also lead to respiratory tract infection due to repeated trachea.
Write its nursing management.
- Nursing management of TEF is done very carefully. Because if this condition is diagnosed as early as possible after birth, the additional complications caused by it can be prevented.
- Airway is kept clear by suctioning the child from time to time. Due to which the breathing pattern remains normal and cyanosis is not seen.
- Oxygen therapy is also given when the child needs it, especially in case of cyanosis.
- Vital signs of the child should be closely monitored.
- The child is placed on Neil by Mouth (NBM) and intravenous fluid therapy is administered to maintain the child’s hydration level and nutritional status.
- It is necessary to rule out the child’s abdomen for distention.
- After the surgery, if the child has a chest tube placed, then taking proper care of this tube is very important. Monitoring and recording whether drainage is adequate.
- It is necessary to dress the chest tube with aseptic technique and take all precautions to avoid infection.
- Special care is taken of the anastomosed part of the child and care of the nasogastric tube is also very important.
- After the surgery, the child’s elbow is restrained. So proper care of drainage tube and nasogastric tube can be maintained.
- Oxygen therapy is also given as needed. The child’s vital signs are also specially monitored for early identification of any complications. If any complication develops, immediate management is undertaken.
- All equipment for emergency and critical care of the child is kept on stand by.
- After the operation the baby’s condition stabilizes, the baby is gradually started feeding and the baby’s condition is monitored.
- At the time of discharge of the child, it is necessary to explain to the mother and father about all the care to be taken at home, to explain to take precautions for infection prevention, to explain to maintain the nutritional needs of the child, and also to explain to the mother and father for any complications and for regular follow-up.
- Psychological support is also very important to reduce the anxiety of mother and father.
Q-5 Define following (Any Six) 6×2=12
🔸1.Juvenile Delinquency-
Juvenile means childhood and delinquency means anti-social.
Antisocial and criminal behavior by children during childhood is called juvenile delinquency.
In which boys are below 16 years and girls are below 18 years.
- reasons
- Turmoil between parents
- Divorce
- There is less recreation in school
- The relationship between student and teacher is unhealthy
- Having a physical defect
- Have heredity
- Management
- Giving love and affection to the child
- Recreation is optional
- Improving the relationship between student and teacher
🔸2.Enuresis –
Enuresis means bed wetting which is a behavioral disorder seen after 5 years. It is difficult to determine because a child gains bladder control at different ages.
When bladder control is achieved and urine is passed involuntarily after 5 years, it is called enuresis.
Which clinically has two types.
- Primary enuresis
- Secondary enuresis
- Primary enuresis means that the child already passes involuntary urine
- Secondary enuresis means that the child has regained bladder control but passes urine involuntarily again due to some illness.
- Which can be managed through some therapy techniques such as drugs
- By training the bladder
- By restriction of evening meal ma fluid
- Through a designed electrical device that wakes up the child by recognizing the child’s reflex response.
- Enuresis can be prevented by making the child wake up in a regular manner and make the urine fast
🔸3.Infant Mortality Rate – IMR stands for Infant Mortality Rate.
- IMR = number of children who died within 1 year of age × 1000
- Total children born in that year
- IMR e.g.Gujarat=23, India=26
🔸4.Anthropometry-
Anthropometric means measurement of height, weight, head circumference, chest circumference. This is a sine measuring the parameters of the body. Which helps to know the growth and development of the child.
If the growth and development of the child is good then it can be said from its measurement that the child is healthy.
- Type of anthropometric
- Static anthropometric
- Dynamic anthopometric
Static means measuring the child’s body and function while at rest is called static anthropometric.
Body measurements taken when the child’s body is moving or working is called dynamic anthropometric.
🔸5.Hydrocephalus –
Accumulation of excessive CSF in the ventricles of the brain is called hydrocephalus.
which occurs due to excessive production of CSF in the choroid plexus or blockage in the pathway of CSF circulation
- It happens for two reasons.
- congenital
- And
- Acquired
The head circumference is more than normal.
The production of CSF is reduced by using medicines in its treatment. In addition, CAF is drained from the brain by surgery (VP shunt).
🔸6.Battered Child syndrome
When a child is subjected to physical injury or sexual abuse or psychological harm by their parents or another adult, it is called battered child syndrome. This is a non-accidental injury.
reasons
- Violence against pregnant wife by husband
- A forceful grasping of a child by a parent that causes nail scratches to appear on the child’s skin
- Force feeding the child by opening the mouth
- When having unwanted children
- This is managed by doing investigations with the help of a special agency.
🔸7.Restraints
Restraints are protective and mechanical devices that minimize movement and protect the child from injury. Resten is made of linen, canvas, leather, plastic, metal, and wood.
purposes
- To carry out physical examination of the child
- To provide safety to the child
- For diagnosis and therapeutic procedures
- To prevent injury to the child
- The restraint should not be too tight to interfere with circulation
- Use cotton pads to make the baby comfortable
- Keep checking the restraint at 20 to 30 minute intervals
- Type of restraint
- Mom Restrain
- Elbow restraint
- Abdominal Restraint
- Jacket Restraint
- Restrain the safety belt
🔸8.Mental Retardation –
Mental retardation is a generalized disorder. In which cognitive function is impaired and two or more adaptive behavior deficits are observed before 18 years of age.
- Type of mental retardation
- Mild=50-70 I q
- Moderate=35-50 Iq
- Severe=20-35 I cu
- Pro found=less than 20 i q
🔸Q-6 (A) Fill in the blanks. 05
1) In under five clinic the central triangle which is red in color indicates___ family planning
2)____Shock occurs as a result of an ante allergic reaction. . Anaphylactic shock
3) B.C.G vaccination is done to prevent the disease. BCG vaccine is given to prevent __ disease. Tuberculosis
4) ____disease is called “Like the joints and bite the heart”. Rheumatic fever
5) The full form of UNICEF is___ UNITED NATIONS CHILDREN’S EMERGENCY FUND
🔸(B) State whether the following statements are True or False. 05
1) Bulging fontanel suggests dehydration.- . wrong
2) Lumber puncture procedure is used to diagnose the meningitis. correct
3) IQ below 20 is considered as profound mental retardation. correct
4) Rabies is a fatal viral infection of central nervous system. correct
5) One Anganwadi covers 5000 population in each village. wrong