ENGLISH paed – 2018 (paper-4) GAGIYA JAGU
PAED-2018
Q-1 🔸a. Define Tetralogy of Fallot. 03
Tetralogy of Fallot is a common birth defect. This defect consists of four other defects, which occur due to abnormalities in the developing heart during the eight weeks of pregnancy.
These four faults like,
- Ventricular septal defect :- It has an opening between right and left ventricle.
- Pulmonary stenosis :– In which the pulmonary artery becomes narrow so that the blood flow from the right ventricle is obstructed.
- Overriding of aorta:- Aorta actually originates from the left ventricle, but this aerta originates from the right side of the heart. As the aorta protrudes through this ventricular septal defect, deoxygenated blood flows into the aorta.
- Right ventricular hypertrophy:- This occurs due to obstruction of pulmonary artery and hence blood does not pass easily. Part of the right ventricle is seen to be swollen.
🔸b. Write clinical manifestations of Tetralogy of Fallot. 04
- Baby’s skin lips and nail buds turn blue when baby cries and feeds
- Dyspnoea
- Acute episodes of cyanosis and hypoxia are known as blue spells or tet spells.
- The baby’s skin is cold and clammy. Sometimes loss of consciousness also occurs.
- The child should be kept in a sitting or lying down position. The higher the better
- A two-year-old child may also develop clubbing of the fingers (clubbing means that the toes and fingers become thick and wide).
- The baby is at risk of embolism and seizures.
- If the child has severe anoxia, death can also occur.
- Difficulty in gaining weight is seen in the child, which means that the condition of failure to thrive can be seen in it.
- Tiredness is seen when the child gets tired soon while playing sports or doing movement.
- Irritability and crying are observed in the child.
- Cardiac murmurs are sometimes seen in children.
- Fanting is also seen due to insufficient blood supply and lack of oxygen in the child.
🔸c. Write the nursing management of Tetralogy of Fallot. 05
Give the child bed rest.
- Refraining the child from vigorous activity.
- To check baby’s vital signs daily.
- Administer regular medication (digoxin and diuretic) and provide nursing care and regular monitoring of his condition.
- Place the child in the semi-fowler or knee chest position to increase blood flow to the lungs.
- Check the child’s oxygen level, by pulse oximetry and administer oxygen as needed on a regular basis.
- Monitoring of conditions like hypokalemia, hemoglobin, hematocrit, cyanosis etc.
- Feed the child in small amounts and at intervals.
- Reducing the child’s anxiety and stress, and diverting the mind to other non-physical activities instead of physical activity.
- Regular checking of developmental milestones as per the child’s age.
- The baby should be given visual and auditory and tactile stimulation and the baby’s wet diaper should be changed periodically.
- Oxygen should be given immediately when a child is cyanotic.
- Provide early treatment for dehydration and anemia.
- Give IV fluid to the child.
- If tetralogy of Fallot is more severe, give IV prostaglandin E to dilate the ducts and increase pulmonary blood flow.
- Providing psychological support to the child’s parents and giving love and affection to the child.
- Giving advice to the parents on how to take care of the child on a daily basis.
- The nurse prepares the child for the surgical procedure and monitors the child at regular intervals.
🔸OR🔸
🔸a. Define Glomerulonephritis. Write the definition of glomerulonephritis. 03
- Glomerulonephritis means inflammation and infection or damage of the glomerulus. In this condition, the glomerular membrane becomes infected for any reason.
- Glomeruli are the filtering part of the kidney that act as filters to remove excess fluid and waste products from the blood and excrete them in the form of urine.
- It can be acute and chronic.
🔸b. Enlist the signs and symptoms of Glomerulonephritis. 04
(1) Acute glomerulonephritis
The child has fever and headache.
The appearance of the child is lethargic, pale and irritable.
Periorbital (area around the eye) edema (swelling) is seen. Swelling is seen on the child’s face
Urine output is reduced and the color of urine is bloody (cola).
The child may have hypertension.
(2)Chronic glomerulo nephritis
- Sometimes the child does not have any symptoms but glomerulo nephritis can be detected by urine examination.
2.Failure to thrive, growth and development is seen as age dependent.
3.Anemia is seen in the child for a long time.
4.Nocturia (abnormal excessive urine at night)
5.Moderate to severe hypertension.
- Edema (swelling)
- Pain in bones (bone pain) and bone deformity are seen.
8.There is microscopic or gross hematuria.
9.Anorexia is seen in the child.
10.Fluid and electrolyte imbalance is seen in the child.
11.Conditions of anxiety and stress can also be seen.
🔸c. Describe the nursing management of Glomerulonephritis.05
(1) Management of acute glomerulo nephritis.
- 1.Giving advice for bed rest.
- 2.Regular check of vital sign and urine output.
- 3.Check daily weight and make record chart.
- 4.Maintain fluid volume.
- 5.Giving the child unsweetened food and advising the parents to give the same kind of food at home.
- 6.Measure intake and output accurately and advise parents to monitor urine output at home.
- 7.To provide mind diversional and recreational facility to the child.
- 8.Careful giving of regular antibiotics to the child which may include penicillin as well as any doctor ordered.
- 9.Give frusemide when there is severe oliguria.
- 10.Peritoneal dialysis should be done as per doctor’s advice when blood urea nitrogen is high.
- 11.The nurse should make close observation of the child and record the progress of the child.
- 12.Administer the drug at regular intervals.
- 13.The nurse should plan how much fluid and food to give to the child and when.
- 14.To teach and encourage the child’s parents how to care for the child.
- 15.Giving advice to the parents on how to take care of the skin and to take timely care if any early sign of complication develops like care of respiratory problems etc.
B)Nursing Management of Chronic Glomerulo Nephritis.
1.It has no specific management but acute condition can be treated in time and complications can be prevented.
2.It can be prevented by controlling acute glomerulo nephritis. Acute glomerulo-nephritis can be controlled with steroids and other immunosuppressive drugs.
3.Control Hypertension with Antihypertensive Medication.
4.Using antibiotics for symptomatic treatment.
5.Providing psychological support to the child and family member and to the parent.
Q.2 🔸a. Define preterm baby. Describe the nursing management of preterm baby. Describe the nursing management of a preterm baby. 08
A baby born live before the completion of 37 weeks of pregnancy is called a preterm baby.
Preterm babies usually do not weigh according to gestational age i.e. less than 2.5kg.
In which the subtypes of preterm babies are found as follows.
- 1.Extremely Preterm Baby :- <28 Week of Gestation
- 2.Very preterm baby :- 28 to <32 weeks
- 3.Late preterm baby :- 32 to 37 weeks
Nursing management of preterm baby
1.Clamp the cord immediately after the birth of the baby to reduce hyperbilirubinemia and hypervolemia.
- Clear baby’s air passage with mucus suction.
- Giving oxygen to the baby through oxygen mask or nasal cannula.
- If necessary, keep the baby in a radiant warmer immediately, so that hypothermia can be prevented. Uncover the baby when keeping it in a radiant warmer.
5.Cover the baby with a cloth immediately after delivery.
- Do not give vitamin k and bath to preterm baby.
- Maintain the temperature of the baby’s body so that hypothermia can be prevented.
- Keep the baby in an incubator where the temperature and humidity of the baby remain stable and maintain the temperature of the environment around the baby.
- If necessary, insert endo tracheal tube and keep in ventilator.
- Checking ABG (arterial blood gas) and checking oxygen level by pulse oximetry.
- To check Apgar score immediately after delivery. in which
- A stands for Appearance
- P means pulse
- G stands for Grimace
- A stands for Activity
- R R means check respiration and take immediate action if necessary.
Prevent the baby from infection.
In which the baby’s infection site like umbilical cord, respiratory system, skin and gastrointestinal system should be specially monitored.
Limit visitors to the baby’s surroundings.
Nurses and doctors who are infected should be kept away from the baby. Parents and medical person should take care to wash hands by medical person whenever they touch the baby.
Keeping babies separate from each other and babies from each other’s instruments, cloths, feeding instruments and tubes etc.
Feeding:-
- Maintain aseptic technique in preparation, storage and administration of baby food.
- Tell the mother to express the milk from the breast into sterile equipment.
- Boil and autoclave baby feeding articles after every feeding.
- Give antibiotics to the baby if needed.
- Changing napkins as needed.
- Keep the infected baby in isolation.
Start feeding within one hour after delivery. - Feeding methods like nasogastric feeding, bottle feeding, spoon feeding etc.
- If the baby is kept in photo therapy, give more nutrition.
- To check daily weight and vital signs.
Burping after feeding. - Foods like breast milk, cow milk and milk powder should be given to the baby and glucose can also be given to the baby.
And giving high calorie protein and fat food. - Sit down and feed sparingly and periodically.
- Discharging the baby can be done only when the baby is pink in color and the breathing is regular and whitely stable.
Ask family members for follow-up and proper care.
🔸b. Write internationally accepted rights of child Write about internationally accepted rights of child. 04
The Rights of the Child were declared by the United Nations on 20 November 1959. They were made with the purpose of fulfilling the special needs of the child.
These rights are as follows.
No right to free education.
No right for name and nationality.
Right to receive special care if the child is handicapped.
Rite to get affection, love and better understanding.
The Right to Adequate Quality Nutrition.
Right to get first aid treatment or relief in time of any calamity or distress.
No right to get good medical care.
Right to play well and get re-creational facility.
The right to develop one’s own abilities and become a good and useful member of society.
Right to be brought up in a calm and brotherly environment.
All the above rights are also given to the children so that every child can use all the rights equally without discrimination of religion, race, caste, sex, color etc.
🔸OR🔸
🔸a. Explain the toys selection, supervision, maintenance & storage for children Write about the selection, supervision, maintenance & storage of toys for children. 08
1) Selection :-
- Choosing toys according to children’s skills, abilities and interests.
- Choosing toys that are safe for children.
- To choose age-appropriate toys, keep in mind that toys that are safe for children of one age may not be safe for children of other ages.
- Infants, toddlers and all children who are still taking toys in their mouths should avoid giving them toys with small parts, otherwise the children will have problems like choking and aspirating.
- A toy of this category should be labeled ‘not suitable for children below three years of age’.
- Do not buy long toys for infants or toys with cords and strings which may cause strangulation of the child.
- Avoid electric toys with heating elements for all children under the age of eight.
- Choose lightweight toys that should withstand rough play.
- Look at the construction of the toy structure in which the eyes, nose and small parts of the toy are securely secured or not.
- Select soft toys that will not harm the child even if they fall on him.
For children, take toys with smooth and round edges, avoid taking toys with sharp edges that can cut the baby. - If the toy is broken, remove the sharp edges to avoid injury to the child.
Avoid taking toys with shooting and throwing objects that may cause eye damage, also avoid toys like sticks and sticks. - Arrows and points used by children should be blunt and made of soft materials.
- Ensure that the contents of the toy are harmless.
- Avoid taking toys that make too much noise so as not to damage the child’s hearing.
If a gun is taken as a toy, the color of the gun should be bright to avoid the mistake of a real friend.
2). Super Vision :-
- A safe playing environment should be maintained.
- The plastic cover should be removed from the toy and thrown immediately otherwise the child may suffocate.
- Close observation of young children while they are playing.
Ask older children to keep their toys separate from younger siblings and friends. - Keep children away from stairs, hills, traffic and swimming pools etc. where children are playing with riding toys.
- Knowing and enforcing rules that are safe for children to play with.
- Instruct children to wear helmets when using bicycles and skateboards or line skates.
- Instruct children to wear gloves and use wrist, elbow and knee pads while playing.
- Also instruct children about electronic safety by teaching children how to unplug electrical toys properly, and while unplugging, pull the plug and not touch the cord.
- Teaching children about the safety of utensils that can cause injury under certain circumstances including scissors, knives, needles and hot elements, loops and long cords can also cause injury.
3). Maintenance :-
- Check new and old toys for broken and loose parts and other hazards.
- Checking whether the movable parts of the toy are securely attached to the toy,
Sometimes the parts are securely attached to the toy but can pose a danger to the child. - Repair or repair broken toys immediately and keep them out of reach of children Sharp wooden blunt toys.
Keep the toy area smooth and scratch free to avoid injury.
4). Storage :-
- Providing a safe place to store children’s toys.
- Teach children to store toys safely to avoid accidental injuries such as falling and slipping on toys.
- To safely store older children’s toys on raised shelves and in locked cupboards,
Should be stored in other areas inaccessible to small children.
🔸b. Write advantages of breast feeding – 04
- Breastfeeding develops a psychological bond between mother and baby.
- Human milk is available for the baby only as per the body temperature requirement.
- Milk is fresh and sterile and free from contamination directly into the baby’s mouth.
- Human milk is ideal if it is readily available.
- Breast milk is a safe and protective food.
There is perfect food for infants. - Meets the total nutrient requirement for the baby for the first six months.
- It is very important for baby’s brain growth because breast milk contains high amount of lactose and galactose.
- Breast milk contains vitamins, minerals, electrolytes and water which are essential for the maturation of the infant’s intestinal system.
- Breast milk provides a facility that increases the absorption of calcium so that the baby’s bone growth is good.
- Breast milk is easily digested.
- Breast milk contains all the essential nutrients that a baby needs.
- Breast milk protects the baby from infection and deficiency.
Breast milk is already prepared.
Breast feeding is a method of family planning, breast feeding is a natural contraception that has a major effect on population for developing countries. - It prevents children from diarrhea and also has laxative action.
- Breast feeding has no dangerous allergic effects.
- Breast feeding can save time and money and energy.
- Breast feeding helps in building a healthy relationship between mother and child.
- Chances of conception decrease during lactation.
- Best feeding helps in involution of uterus (i.e. bringing uterus to pre-pregnant state).
- Breast feeding reduces the chances of sunstroke, gastrointestinal infections and ectopic eczema.
And the chances of scurvy and rickets are also reduced. - Breast feeding reduces the chances of breast cancer.
- Breast milk contains IgA and IgM macrophages, lymphocytes, lysosomes, etc. due to which diarrhea and acute respiratory infections can be prevented in babies.
And prevents against malaria and viral and bacterial infections. - Breast milk protects against conversion, hypocalcemia, tetanus, deficiency of vitamin E and zinc.
- Exclusive breast feeding can prevent malnutrition in children.
- Breast feeding increases the intelligence of the baby, and gives the baby a sense of security (due to the infant-mother bond).
- The chances of illness in the child are reduced.
- Breast feeding reduces the chances of postpartum hemorrhage (excessive bleeding from the genital tract after delivery).
- Chances of ovarian cancer are also reduced.
- Helps in reducing the excess fat that is stored in the mother during pregnancy.
Q.3 Write Short Answers (Any Two) Answer in short. (any two) 2X6=12
🔸Write the advantages of breast feeding.
🔸a. Write common puberty changes occur in boys & girls. Write about the common changes of puberty in boys and girls.
Puberty changes in girls:-
- 1.Height and weight increase.
- 2.Breast changes occur in which pigmentation of the areola occurs and the size of the breast tissue and nipple increases.
- 3.Pelvic girth increases in transverse form.
- 4.Pubic hair is seen.
- 5.There are changes in vaginal discharge.
- 6.Axillary sweet gland is activated, axillary hair is seen.
- 7.Menstruation period occurs which is called menarche.
- 8.One (acne) is seen in some girls.
Puberty changes in boys :-
- Increase in weight and height.
- The size of the external genitalia increases.
- Pubic hair is found in the armpit, upper lip, groin area, thigh, chest and umbilical area.
- Facial hair is seen after two years of pubic hair.
- There are changes in the voice which becomes darker.
- Simeon is discharged while sleeping.
🔸b. Write down nurses responsibilities while administering blood transfusion to Thalassemia patient.
- Taking vital signs before blood transfusion.
- Verify that the physician has ordered it or not.
- Obtaining patient’s signed consent.
- Explaining blood transfusion to parents and child.
- Ensure patient name and registration number are checked.
- Check blood type and Rh type.
- Cross matching of donor blood with thalassemia patients.
- Blood should be fresh and not more than five days old.
- Checking Expiry Date of Blood Bag
- Give the patient npo (oral on neel) four hours before the blood transfusion procedure.
- Warm the blood before blood transfusion to body temperature, do not transfuse cold blood.
- Maintain aseptic technique, wearing gloves when puncturing a patient’s venipuncture, and maintaining aseptic technique during blood transfusion and when removing articles after blood transfusion.
Record the time of initiation of blood transfusion.
Observation of patient during blood transfusion and observation of infusion site and blood bag and flow rate.
Blood transfusion should be started slowly in which the transfusion rate should be kept at 2ml/min for the first fifteen minutes and not more than that.
Advise patient to report chills, itching, fever, shortness of breathing, pain in transfusion site and rash, fast heart rate and low blood pressure and other untoward signs.
If these symptoms appear, the nurse should inform the doctor immediately.
Keep emergency drugs and instruments ready so that we can treat any emergency immediately.
After the blood transfusion, the material should be properly carded.
If necessary, give antipyretics and other drugs to the patient after blood transfusion as per doctor’s instructions.
Recording and reporting after blood transfusion.
🔸c. Write preventive measures of accident up to 2 years of age in children.
- Due to the increase in the child’s range of motion, the child may fall and fall, so it is necessary to supervise the child continuously and make sure that no place is touched or bumped.
- It is common for a child to be shocked by an exposed electric wire or wire, so check the wiring periodically and avoid having exposed plugs or wires.
- A child can put anything in the mouth, so keep any poisonous or harmful substances away from the child’s reach and do not put any other harmful substances in the child’s food container.
- If there is an open water tank or a place full of water on the opposite side of the house, cover it and keep it because the child can die due to drowning.
- Health education is very important to prevent accidents among children. Through which information can be given about safety precautions and awareness.
Parents of children need to be specially persuaded to maintain constant supervision and discipline of children.
- Along with parents, family members, school teachers and the general public also need to be informed about safety precautions.
- It is necessary for the nurse to explain to the parents that along with the increase in age of the child, his mobility and his capabilities also increase so that the chances of accidents also increase. So, with the increase in age, the child needs to be taken care of more.
- To provide a safe environment around the child and to remove harmful things from that environment. By creating this kind of environment at home, school and community and hospital everywhere, the child can be saved from accidents.
- The parents should be convinced that the child does not get injured by the sports equipment and that no part of it gets stuck in the mouth or respiratory track.
- Hospital facilities and emergency and trauma care are also essential for survival. So by improving these services also disability can be prevented.
🔸d. Describe nursing care of neonate with hypothermia.
Mild Hypothermia :-
- Clean and dry the baby immediately after delivery.
- Keep the baby on mother side, advise not to bathe the baby.
- Ask to start breast feeding within 30 minutes after delivery, so the body temperature becomes normal as the bond between the neonate and the mother increases.
- Cover neonate properly especially head, chest and fit.
- Keeping the neonate warm,
By the following method viz.
- Skin to Skin (which includes counseling mothers about Kangaroo Mother Care) contact,
- Warm room and warm bed
- Radiant warmer and incubator.
- Take the temperature at regular half-hourly intervals until the temperature reaches 36.5°C, then take the temperature at hourly intervals thereafter.
- 2.Moderate Hypothermia :- (32 degree centigrade to < 36 degree centigrade)
- Keep the room warm, keep the bed and surrounding environment warm.
- Maintain normal temperature of neonate by using incubator.
- Radiant warmer should also be used so that the body temperature remains normal
And can treat hypothermia. - Continue rewarming the baby until the body temperature is in the normal range.
- Monitor temperature every 15 to 30 minutes.
- Telling mothers about Kangaroo Mother Care.
- Management of severe hypothermia;-
(< 32 degree centigrade)
- Keep the room warm by a room heater or by a 200 watt bulb.
- Use an air-heated incubator that has an air temperature of 35-36 degrees Celsius.
- Monitor heart rate, temperature and glucose level of neonate.
- Measuring whether hitloss has decreased or not.
- Start IV dextrose 10% at 60-80 ml/kg/day.
- Give oxygen if the baby needs it.
- Administer 1mg vitamin k injection to term neonates and 0.5 mg vitamin k to preterm neonates.
Q.4 Write Short notes (ANY THREE) 3X4=12
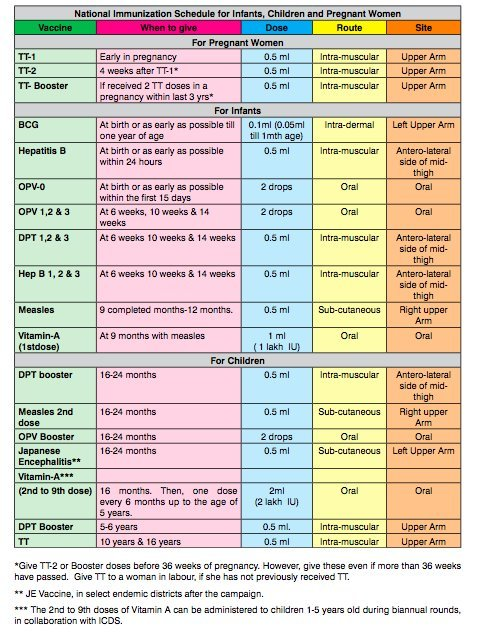
🔸a. Recent Immunization schedule of India.
🔸b. Megacolon/Hirschsprung disease.Megacolon Hirschsprung disease
Megacolon
This is a type of congenital anomaly of the gastrointestinal system.
It is also known as Herschprung’s disease.
When there are no ganglionic nerve cells in the wall of the intestine, the defect causes the part to swell and widen. This disorder is known as mega colon or aganglionic mega colon.
These nerve cells are absent in the muscular layer and submucosal layer of the intestine.
This problem can be limited to a part of the intestine or even spread to the whole intestine. Mainly this problem is seen near the part of rectum and sigmoid colon.
- Causes of megacolon
- Genetic and Hereditary
- Intra uterine growth failure
- Chronic constipation
- Anorectal atresia and mal formation etc. are responsible.
Symptoms of megacolon
The clinical manifestation of the child depends on which part of the intestine is affected and how many parts are defective.
The symptoms and sign base of this disease condition are seen differently in neonates and children.
After birth, a child with this condition usually does not pass stool i.e. meconium or passes very late.
Vomiting with bile and fecal matter is also seen due to the backflow of the contents of the intestine in the child.
Abdominal distension and constipation are seen in the child.
Anorexia and dehydration are seen in the child. So the condition of failure to thrive is also seen due to non-fulfillment of its nutritional needs. In which there is less increase in the growth characteristics of the child according to age.
Older children do not show immediate symptoms like newborns and the affected part of the colon is smaller or less visible. The symptoms of which..
Abdominal distention and abdominal discomfort and irritability are especially common in children.
Chronic constipation is seen in the child.
Peristalsis movement can be felt in the child’s abdomen and it can be observed that the superficial veins of that part are also dilated.
Diarrhea and constipation are seen alternately in children. In which the stool is a special ribbon-like, liquid-like stool passed.
Malnutrition, anemia and failure to thrive are seen in the child.
Management of the patient with megacolon
- Mega colon is a congenital anomaly of the gastrointestinal system seen in children. Which is specially treated surgically. In it, the part of the colon with the distended portion is removed and an end-to-end anastomosis is performed.
Perioperative nursing management for this condition is as follows.
Vital signs of the child should be checked regularly, so that its general condition can be assessed.
Administer antibiotics as per doctor order.
Maintain the child’s hydration level.
- A daily rectal voce is given with a prescribed solution. The frequency, color and amount of stool returned after washing is noted.
- It is very important to maintain the nutritional level of the child.
- Special post-operative care of the child is necessary to prevent infection at the surgical site. Daily dressing with aseptic technique is essential.
- An opening is made on the abdomen after the baby’s surgery. The opening is called a stoma. This procedure is called colostomy. It is necessary to take special care of the opening part of colostomy i.e. stoma. In which it is necessary to take special care in its dressing, its skin care, its drainage care and not to get an infection in that part.
- Regular checks are necessary for the normal function of the colostomy.
- Explain to apply zinc paste on colostomy site.
- Explain to maintain hygiene and cleanliness.
- After the discharge of the child from the hospital, persuade the mother and father to do all these care related procedures at home. Encourage follow-up care and hospital visits when needed. Daily assessment of the child. Ask to contact the hospital immediately if any complications occur.
🔸c. Principles of post-operative care of infant
Immediate post operative care :-
- Keeping the operation bed ready so that the patient can rest there after the surgery.
- Immediately shift the patient to the recovery room after surgery.
- Monitor vital signs such as blood pressure, oxygen content and temperature.
- Keep the child’s airway clear by giving it side line position.
- If necessary, suction the airway to remove secretions.
- Maintaining intake and output chart.
- Restrain the child so that no injury occurs.
- Do not give anything by mouth until the child is conscious.
2). Care after 24 hours of surgery :-
- To monitor vital signs.
- To observe the patient’s level of consciousness and hydration status, intake and output and any discharge from the surgical site.
- Administering medications prescribed by a physician such as antibiotics and analgesics to the patient.
- Dressing the operative side with strict aseptic technique.
- To maintain personal hygiene of the child.
- Advise the child to get enough rest and sleep.
- Simple nursing interventions such as early movement and active or passive exercise help prevent post-operative complications.
- Planning the child’s discharge from the hospital.
- Advising on child feeding and regular care, medication and follow-up.
🔸d. Diarrhoea-
Diarrhea is a condition in which the frequency of passing stool increases. It is a major health problem in young children.
Diarrhea means passing liquid or watery stools and generally passing watery stools more than four times a day or increasing the frequency of passing stools is called diarrhoea.
It is also normal for a neonate to pass semi-solid or watery stools four to five times a day.
Causes of diarrhea
- Unhygienic condition
- Unhealthy feeding practices
- Diarrhea can also be caused by bacteria, viruses, parasites, fungi etc. This condition is especially seen due to infection and inflammation.
- Diarrhea can also occur due to antibiotic therapy.
Diarrhea can also occur due to any type of food allergy, food poisoning or over feeding or food intolerance. - Diarrhea can also occur due to a serious disease condition in children.
Clinical Manifestations of Diarrhea.
- In case of mild diarrhea the child passes stool three to six times during the day. Dehydration is not seen in them.
- In moderate diarrhea, stool is passed eight to ten times during the day. Along with fever abdominal pain, anorexia, vomiting, nosia etc. symptoms are also seen.
- Symptoms of mild dehydration can also be seen in them.
- In severe diarrhea, stool is passed more than 10 times during the day. They show symptoms of moderate to severe dehydration. Along with this, the following common manifestations are also seen in the child.
- Fever, Irritability, Nosia, Vomiting, Abdominal pain and discomfort, Abdominal bloating, Weakness, Anorexia, Wet loss, Decreased urine output, Dry skin, Loss of skin elasticity, Tachycardia, Hypo tension etc.
Diagnosis.
- History and Physical Examination
- School Examination
- Blood examination
- Ultra sonography
Management.
- Antibiotic and anti-viral medicines are given as per the doctor’s order to treat the infection.
- Anti emetic medicines are given to relieve abdominal pain.
- Antipyretic medicine is given in case of fever.
- In addition, depending on the degree of vomiting and dehydration, intravenous fluid therapy is given to maintain fluid and electrolyte balance.
- If there is no vomiting and mild to moderate dehydration, oral rehydration solution (ORS) is given to maintain fluid and electrolyte balance.
- Add this ORS packet in one liter of water and use it for 24 hours as per the age and requirement of the child. With the help of this fluid and electrolyte balance is maintained in the child. If it increases after 24 hours of use, it is discarded. Oral rehydration solution can also be prepared by home methods.
- During episodes of diarrhea, give the baby easily digestible food, keep breast feeding continuous.
- Avoid milk and milk products, avoid fresh fruit juice, avoid outside food and cold drinks.
- To explain measures for personal hygiene and food hygiene.
- Avoid bottle feeding and avoid pacifiers.
- Explain about hand hygiene and personal hygiene.
- Explain the importance of hand washing.
- Advising to feed food only after it is properly cooked.
- Daily monitoring of child’s fluid and electrolyte balance and child’s body weight.
- Feed the baby little by little.
- Advise to take after boiling and cooling the water.
- Explain to the child as well as his mother and father about the measurement of diarrhea and food hygiene and preventive strategies etc.
- Explain to follow up.
🔸e. Enuresis-
- Enuresis i.e. bedwetting after 5 years is difficult to determine, as children gain bladder control at different ages. This behavioral disorder is usually seen in children after the age of 5 years.
- When bladder control is achieved and urine is passed voluntarily after 5 years, it is called enuresis. It is necessary to note that the child passes urine 2 times during the night when he is awake.
Cause of enuresis :-
- Developmental causes :-
- Those who have no bladder muscle control, those who have nerve and muscle immaturity and incoordination, who have no bladder control for 6 to 8 years.
2.Organic causes :-
- In which there is a defect in the formation of the urinary track,
- Having a UTI infection (urinary tract infection),
- Neurogenic deficiency causes increased urine output in diabetes.
- Psychological causes :-
- Due to strict family and parents
- When a female child is rejected by her parents
- Due to Shibling,
- Due to too late and too early or inadequate training of bladder control by parents.
- Physical factor :-
- Worm infestation
- Genitourinary infection, anatomical defect etc. are the reasons.
Types of enuresis :-
- Which clinically has two types
- Primary en uresis
- Secondary and Eurasias
A). Primary Enuresis :-
- That is, the child has already passed involuntary urine, in which the child has not received proper bladder control training by the parents and because the parents are not very close with the child. Bladder control is never developed in this child.
B). Secondary Enuresis :-
- Such a child has once acquired bladder control but due to some diseases and stressful events like marital problems, parental quarrels, death, sibling and shifting to a new house, involuntary passing of urine is seen again.
Diagnostic Evaluation :-
History Collection
Physical examination investigations such as urine culture and urinalysis
Management :-
- Nursing Tips:
- We can manage it through some therapeutic techniques.
- Providing bladder training,
Restriction of fluid in the evening mill. - Do not give the child too much fluids or ask him to pass urine before sleep.
- Pass urine at intervals during sleep so that bedwetting does not occur during sleep
2.Drug:- Giving imipramine, amitriptyline and anticholinergic drugs to reduce bladder contraction.
Desmopressin nasal spray is a vasopressin analog that reduces urine output during the night.
3.Psychotherapy and Training:-
- Reassuring parents and child.
- Parents should be told to encourage the child to have dry nights.
- Sometimes the child should also be rewarded and anchored by the parents when they do not wet the bed.
- Advise less fluid intake at night and pass urine before sleep and encourage the child to drink more fluid during the day.
- Training to retain urine in the bladder for a long time.
- Waking him once or twice to pass urine during the night.
- Parents spend time with the child.
- By designing electrical devices that the child
Instruct parents to use this type of electrical bell circuit that wakes the baby up by recognizing the reflex response, which wakes the baby up before going to bedwetting.
Q.5 Write Definition (ANY SIX) Give the definition. (any six) 6×2=12
🔸a. Thumb sucking- —
- Sucking is an infant’s main joy. By which they get affection, love and satisfaction. According to the psycho-analytical theory, if the reason why a child thumbsucks is not getting enough satisfaction from the food taken by mouth or when the child is anxious or stressed, he starts sucking the thumb.
- Lack of adequate oral feeding leads to malnourished thumb sucking in the child.
- According to psychiatrists, thumb sucking reflects or acts as a substitute for the mother.
- Most children stop thumb-sucking by the time they are two years old. While other preschoolers quit at the same time, and if the child continues to suck the thumb after four years, the parents should inform the doctor.
🔸b. Oesophageal Airesia-Esophageal atresia
- Esophageal atresia is a common birth defect. In which a part of the baby’s esophagus is not fully developed or a part of the esophagus is found to be narrower than normal.
- OR
- A baby’s esophagus fails to develop as a continuous canal or tube.
- Esophageal atresia can also occur alone or with tracheoesophageal fistula.
- The esophagus connects the mouth to the stomach.
- Due to esophageal atresia, the baby is not able to pass food from the mouth to the stomach, and has difficulty in breathing.
🔸c. Pneumonia
- Pneumonia is an infection of the lower respiratory tract and lungs. which affects one or both lungs. Pneumonia causes air sacs or alveoli to become filled with fluid or pus, which can be caused by bacteria, viruses, or fungi.
- Pneumonia is spread when an infected person coughs, sneezes or touches their objects, or is spread by airborne droplets. The bean is spread by inhalation by infected individuals.
- High fever, cough, cyanosis and shortness of breath are seen in pneumonia.
🔸d. Hydrocephalus –
- Hydrocephalus is an abnormality of a child’s nervous system.
- In which there is an abnormal collection of fluid in the ventricles inside the child’s brain.
- This fluid is the cerebrospinal fluid, the reason for its filling is either its absorption is not normal or its production is more than normal.
- Thus, due to the imbalance of cerebrospinal fluid, its filling in the ventricles of the brain is known as hydrocephalus. Hydrocephalus is also caused by obstruction of the CSF pathway.
- Due to this condition enlargement of brain ventricle and head is seen. Due to which the circumference of the head increases and the head appears larger than normal.
🔸e. Acromegaly
- Acromegaly is a hormonal disorder. Acromegaly occurs during adulthood when the pituitary gland produces too much growth hormone.
- Where, acro means extremity.
- And Megali means enlargement.
- Acromegaly is a chronic disease.
In which there is enlargement in the bones of head, hand, feet and swelling and enlargement in soft tissue. - Bone size increases due to excess growth hormone is called gigantism. The increase in bone size is seen only during childhood. Bone height does not increase during adulthood.
- Acromegaly is caused by a pituitary tumor.
🔸f. Extrophy of bladder
- Exstrophy of the bladder in which the bladder protrudes above the skin or the outside bladder is seen. Exstrophy of the bladder is a rare birth defect. In which the bladder is visible from the outside of the abdominal wall and pelvic cavity and is extremely open.
- The bladder is visible from the outside. Because the bladder is exposed, it does not store urine and does not function normally, leading to leakage of urine.
- Bladder exstrophy occurs when the skin of the lower abdominal wall does not form properly, leaving the bladder open.
🔸g. Growth
- Growth is physical maturation in which there is an increase in the number and size of body tissues and an increase in the size or number of body organs.
- In which the increase in growth is due to the division of the cell and the increase in the components inside the cell causes the growth of the body.
- Changes due to body growth are measured in inches/centimeters and pounds/kilograms.
- Growth is progressive and measurable with increases in height and weight.
- Good nutrition leads to proper growth with age, so good food intake leads to good growth.
🔸h. Preventive paediatrics –
- In preventive pediatrics, health care providers provide preventive care to children rather than treating diseases in children.
- Through preventive care, children are prevented from diseases and disabilities.
- In which health promotion and preventive activities are done.
- Preventive pediatric care like
- 1.Primary Preventive Care
- 2.Secondary Preventive Care
- 3.Tertiary Preventive Care is provided.
- Care JVK, 1. Prevention of Diseases 2. Promotion of Physical, Mental and Social Wellbeing of Child 3. Improve Health Care Activities like Growth Monitor, ORS, Nutrition and Immunization and Promote Breast Feeding and Prevention of Communicable Diseases and Accidents etc. is included.
🔸Q.6 A. Fill in the blanks. – 05
1.Measles vaccine is administered by _ route.
subcutaneously
2.Weaning diet should be started with__ type of food. Liquid
3.Electronic toys should be avoided for children below_____ years of age. eight years
4.Infection of the middle ear is known as____ Otitis media
5.Child is able to crawl at the age of________ months. 11 months
🔸B. State whether the following statements are True or False. 05
- Large head is also known as microcephaly. Big head is also known as mycocephaly. wrong
- First booster dose of DPT vaccine is given at 3 years of age. wrong
- The green stick fractures are commonly occur in young children. correct
- Meningocele is less severe than meningomyelocele. . correct
- Diphtheria is commonly seen during first 6 months of age. wrong