ENGLISH NEW MIDWIFERY GNM TY UNIT 9 management of the high risk Labour
Unit:9 management of the high risk labor
Obstructed Labour:
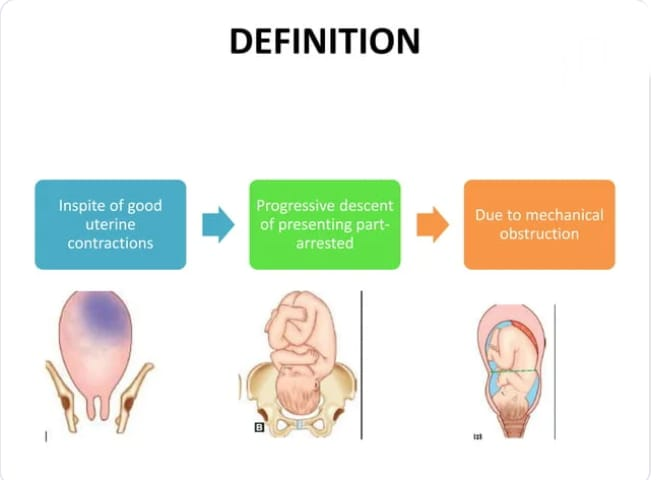
Definition
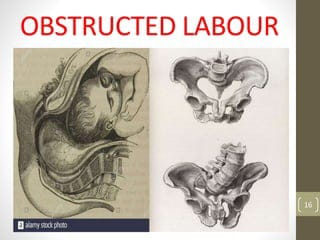
Obstructed labor is a condition in which, despite proper uterine contractions, the presenting part of the fitus, which is progressively descending, is arrested due to a mechanical obstruction, is called “obstructed labor”. Death of the fetus may also occur due to lack of supply
etiology
1) Fault in passage (birth canal),
2) Fault in passenger (fits)
1) Fault in passage (birth canal):
(a) Bonnie,
(b) Soft tissue obstruction
(a) Bonnie:
contracted pelvis,
Cephalopelvic Disproportion (CPD),
Abnormal Pelvis (Ex : Android, Anthropoid)
(b) Soft tissue obstruction:
Due to cervical dystocia caused by prolapse or prior operative scarring,
Cervical or broad ligament fibroids,
Impacted ovarian tumor,
Due to having tumors in the rectum, bladder and pelvic bone.
Being a bicornuate uterus.
Due to abnormalities in the uterus.
Having vaginal stenolosis.
Due to the vaginal septum.
Having a rigid perineum.
2) Fault in passenger (fits):
transverse lie,
bro presentation,
Due to Congenital Malformation of Fetus (Ex : Hydrocephalus),
Being a Big Baby,
Occipito-posterior position,
Compound Presentation,
Locked Twins.
Clinical Features:
Effect on Mother
Immediate
Immediate Exhaustion,
dehydration,
metabolic acidosis,
genital sepsis,
Injury to genitourinary track,
Post partum haemorrhage,
mourning
remote
Genito Urinary Fistula/ Recto Vaginal Fistula,
vaginal atresia,
Secondary amenorrhea.
Effect on the fitters
asphyxia,
acidosis,
intracranial hemorrhage,
infection.
Nursing Management
Identification of obstructed labor during the antenatal period of the mother itself so that early measures can be taken.
Proper monitoring of mother during intranatal period and proper maintenance of partograph for early detection of obstructed labour.
Prevent dehydration, ketoacidosis and sepsis in the mother and maintain the mother’s hydration status.
Administer intravenous fluids to the mother, mainly providing Ringer lactate (RL) fluid, to correct dehydration and acidosis.
If the mother has a condition of acidosis, correct it with 100 ml of 8.4% sodium bicarbonate.
Carrying out biochemical monitoring such as
Serum bicarbonate level.
Providing proper antibiotic medication to the mother like,
Administer 500 mg ampicillin and then repeat at 6 hour intervals.
Centrifuge the blood sample to the laboratory for blood grouping and cross-matching. And if operative interference is to be performed, keep a blood bottle ready.
Take a vaginal swab and send it to the laboratory for culture and sensitivity tests.
Early removal of obstruction through safe delivery in the management of obstructive labour. Do not give oxytocin or trial for safe delivery of the patient.
If the baby’s head is down and the baby is alive, perform a forceps delivery and then check for uterine rupture and tear.
If the baby is dead, deliver by destructive operation.
Not performing internal version in obstructed labor.
If the case of obstetric labor is detected early and the condition of the fetus is good, perform cesarean section.
Symphysiotomy As an alternative to caesarean section, an opening is made in the symphysis pubis to widen the pelvic cavity, during outlet contractions.
- Malposition:
Definition:
Any position other than the flexed occiput anterior position of the vertex during the intrauterine life of the fetus is called malposition.
Occipito Posterior Position:
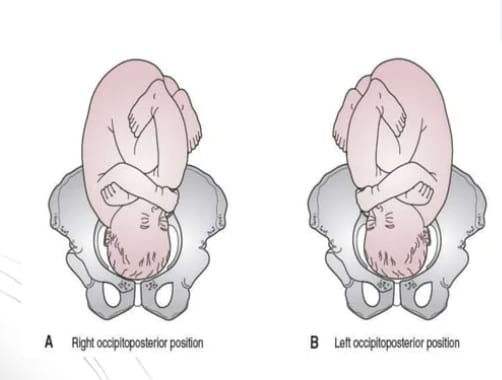
In the vertex position of fitus when the occiput is placed posteriorly at the sacro-iliac joint or directly above the sacrum, it is called the occipito-posterior position.
When the occiput is placed over the right sacroiliac joint, the condition is called right occipito posterior (R.O.P) position and when placed over the left sacroiliac joint, it is called left occipito posterior (L.O.P).
is called a position. When it points towards the sacrum it is called direct occipito posterior position.
Occipito posterior is not an abnormal presentation of the vertex but an abnormal position or malposition of the fetus during intrauterine life when the occiput of the fetus is in a posterior position (over the sacroiliac joint or direct sacrum) instead of the anterior portion in the pelvis in vertex presentation. is called occipito posterior position.

Etiology:
Often the etiology is not clear but the following factors are responsible:
- Fault in passage: Transverse narrowing of mid pelvis favors posterior position in android/anthropoid or platypeloid pelvis. In this, the anterior posterior diameter is larger, so the head engages in it rather than the transverse diameter of the bream.
- Fault in Passenger: It involves flexed head, large feet.
3.Fault in Power: Uterine inertia in it, epidural analgesia in labor favors occipito posterior position.
4.Contracted pelvis : Here, especially android pelvis leads to occipito posterior condition.
- Prematurity: Small fits can be in any part of the head with any diameter of the pelvic brim. Therefore, prematurity may predispose to an occipito-posterior position.
A poorly flexed flat sacrum leads to deflection and an occipito-posterior position.
Diagnostic Evaluation:
Abdominal Examination,
vaginal examination,
Radiography.
Abdominal Examination:
Inspection: On inspection the abdomen below the umbilicus appears flat.
Palpation: The femoral limb is palpated by gliding near the midline with the femoral back and anterior shoulder away from the medline. The fital head is not engaged and the foot is not as prominent.
ASKULSTATION: F.H.S. The right side is heard in ROP and the left side in LOP.
vaginal examination,
Bag of membrane may rupture due to increase in length of bag of membrane.
A sagittal suture lies in any oblique diameter of the pelvis.
The posterior fontanel fills toward the sacroiliac joint.
As the head is well flexed in the occipito-anterior, the posterior fontanel fills smoothly, whereas in the occipito-posterior, the head is deflected, so the anterior fontanel fills easily.
Radiography.
Mechanism of Labour:
Engagement of Head: The head is engaged through the right oblique diameter in right occipito posterior ma (ROP) and left oblique diameter in left occipito posterior position. Engaging transverse diameter of head can be biparietal (9.5 cm) and anterior-posterior diameter suboccipito-frontal (10 cm) or occipito-frontal 11.5 cm.
In favorable circumstances:
- Flexion: If there are good uterine contractions, the head flexes well and descends until the head is above the pelvic floor.
2.Internal Rotation of Head: Occiput rotates forward by 3/8 th circle (135 degrees) comes behind the QBC and neck torsion cannot stay suspended so solder rotates by about 2/8th circle ROP Right oblique in and LOP in left oblique comes in diameter.
There is still 1/8th part of torsion left on the neck.
Fits a further descent down and the head is delivered as in the occipito anterior position.
Restitution: Restitution is movement to the extent of 1/8th of a circle in the opposite direction of internal rotation of the head.
External Rotation: External rotation occurs through 1/8th of a circle in the same direction as restitution as the solder rotates from the oblique to the anterior-posterior diameter of the pelvis.
Birth of solder and trunk:
The process of expulsion is similar to the occipito-anterior position.
Unfavorable Circumstances:
Incomplete Forward Rotation/Deep Transverse Arrest: In this condition the occiput rotates anteriorly in 1/8 circle and the sagittal suture falls in the bisphenoid diameter. After that there is no forward rotation.
Non-rotation: Due to moderate deflection of the head, both the sinciput and the occiput simultaneously touch the pelvic floor. Also, there is no rotation of the occiput. The sagittal suture remains in the oblique diameter. And the forward mechanism does not happen. That condition is called Oblique Posterior Arrest.
Malrotation: In greater deflection of the head, the first sinciput touches the pelvic floor and its anterior 1/8th of circular rotation causes the occiput to fall into the sacral hollow. That position is known as occipito-sacral-position or persistent occipito-posterior position of the vertex ( POP) is called. If conditions are favorable i.e. baby’s size is average, good uterine contractions and adequate pelvis “face to ubis” delivery takes place while condition is unfavorable arrest is called occipito-sacral arrest.
Mechanism of “Face to Pubis” Delivery:
Descent: Descends forward until the root of the nose approaches the symphysis pubis.
Flexion of the head causes the brow, vertex and occiput to protrude above the perineum and is borne by face extension.
Restitution: The head rotates 1/8 circle in the direction opposite to the internal rotation and the face comes to the left of the mother in ROP and to the right in LOP.
External Rotation: The occiput is rotated 1/8 circle in the further same direction of restitution, and the face is to the left in ROP and to the right in LOP.
In persistent occipito-posterior, if it does not face to pubis by itself and goes into arrest, it is called occipito-sacral arrest.
Management:
Principals:
Early diagnosis of occipito posterior position.
Making proper observations for the progress of labor.
To provide proper and timely treatment to the patient.
Diagnosis: Fetal heart sounds are not easily located as the back flake of the fetus is over. If the membrane ruptures early, perform an internal examination and assess for an adequate pelvis.
Early caesarean section: If the pelvis is inadequate, along with obstetric complications like pre-eclampsia, post caesarean pregnancy, big baby, caesarean section is required.
First Stage:
In favorable conditions labor should be treated as normal labor but following certain instructions like starting intravenous infusion as prolonged labor is likely, monitoring progress of labor and starting oxytocin infusion for stimulation of labor in vic pain.
Cesarean section is performed in unfavorable circumstances such as labor arrest, uncoordinated uterine action, and fetal distress.
Second Stage:
Often anterior rotation of the occiput leads to delivery by itself or by low forceps or ventos.
Unrotated and Malrotated:
If the condition of the fetus and mother is good, continue continuous monitoring to watch for anterior rotation of the occiput and descent of the fetal head. Spontaneous face-to-pubis delivery can occur in the occipito-sacral position during an episode and deliver properly.
Arrested Occipito Posterior Position: Perform abdominal and vaginal examination of the patient in this condition. When the occiput is arrested in transverse or occipito oblique position, vacuum extraction or manual rotation of the head is performed in suitable cases for forceps delivery.
In unsuitable cases, delivery is done by caesarean section and craniotomy of dead babies.
Occipito-sacral arrest: If the head is engaged and the occiput is below the ischial spine, a face-to-pubis delivery is performed using Keyland forceps in the unrotated head. If the occiput is at or above the level of the ischial spine, a caesarean section is performed.
Deep transverse arrest: If vaginal delivery is safe, manual rotation of ventos or head by forceps application or rotation with forceps
Forceps delivery is performed by a skilled obstetrician. If vaginal delivery is not safe, caesarean section is performed.
Third Stage:
Administer prophylactic intravenous ergometrine 0.25 mg with delivery of anterior solder to prevent post-partum haemorrhage. Observation for injuries of cervix and lower genital tract after vaginal operative delivery.
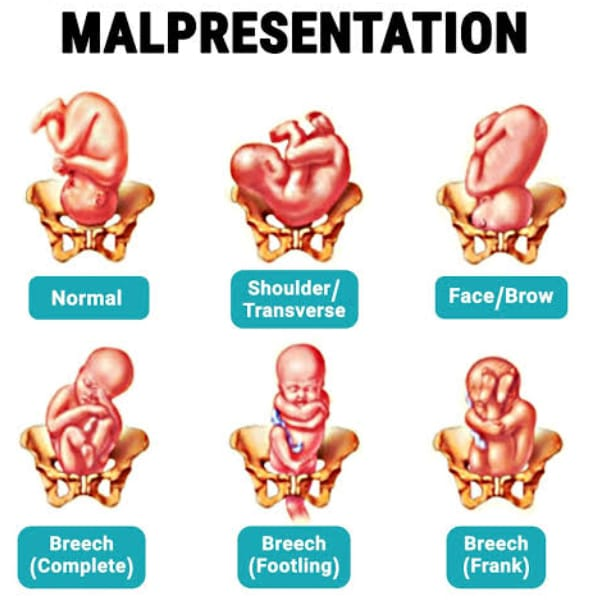
- Malpresentation:

Malpresentation is a condition in which any presentation other than the vertex as a presenting part during the intrauterine life of the fetus is called malpresentation.
Breech presentation,
face presentation,
bro presentation,
Solder Presentation,
Compound Presentation.
Breech presentation,
Definition
Breech presentation is the most common malpresentation in the uterine cavity of the fetus in which the lie of the fetus is longitudinal but the podalic pole (buttocks) is in the pelvic brim as the presenting part.
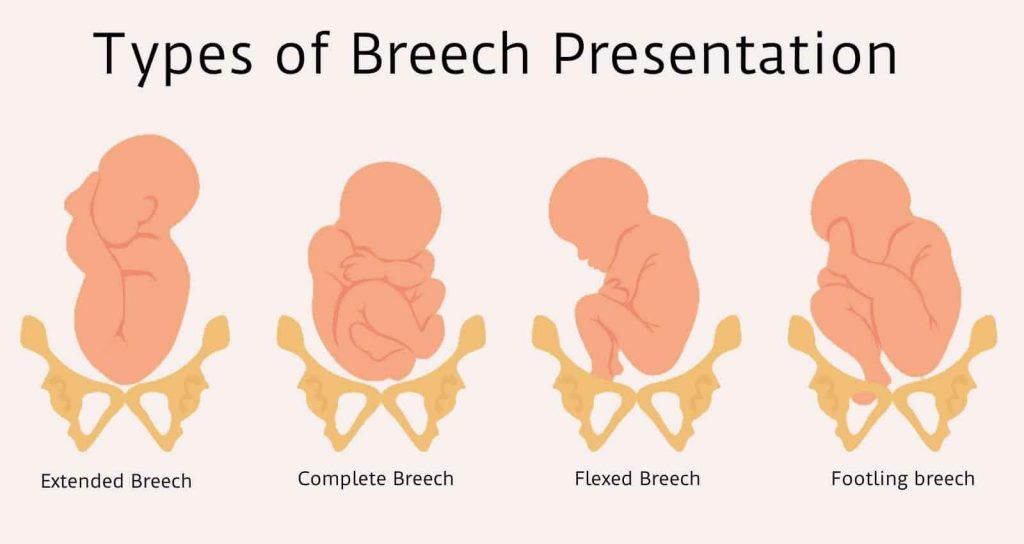
Attitudes/ Classification/ Varieties of Breach Presentation
There are mainly two types of breech presentation.
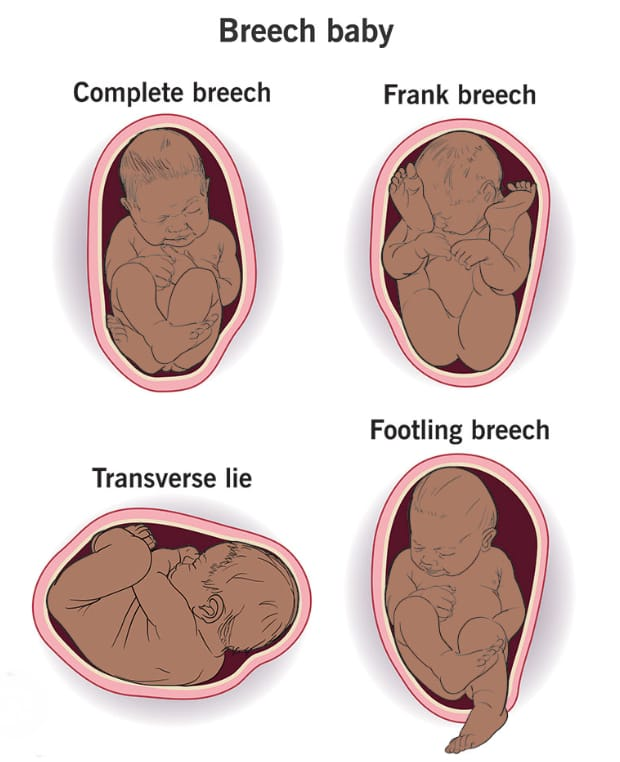
1) Complete
(flexed breech),
2) Incomplete
There are three other types of incomplete.
a) Breach with extended legs (Frank Breach).
b)Footling presentation.
C) Presentation of
1) Complete (flexed breech),
It maintains the normal attitude of full flexion. In complete breech, the leg of the fit is flexed at the thigh and the foot is flexed at the knee and the foot is presented with the buttock of the fit.
In which as presenting part:
2 Butts,
external genitalia,
And 2 fits.
2) Incomplete
In the incomplete, there are varying degrees of extension of the legs in the podleic pole.
There are three other types of incomplete.
a) Breach with extended legs (Frank Breach).
b)Footling presentation.
C) presentation of the (knee).
a) Breach with extended legs (Frank Breach).
In this condition the leg of the fit with the breech is extended i.e. the thigh of the fit is bent over the trunk of the fit and the leg is straight from the knee (knee). The presenting part consists of 2 buttocks and external genitalia. This condition is more commonly (70%) in primigravida.
b) Footling presentation:
A footling presentation occurs both and the leg is partially extended with one or both legs as the presenting part.
C) Presentation of the (knee):
In a ni (knee) presentation the ni (knee) is presented in the brim as the thigh is extended but the ni is flexed.
etiology
Fault in passenger(fits): Tema, extended legs, prematurity,
twins,
hydrocephalus,
Dead fetuses.
Fault in Passage (Birth Canal):
placenta previa,
hydroamnios,
Oligohydro amnios,
Due to less tone of uterus and abdomen.
Maternal factor
contracted pelvis,
placental malformation,
Scanty Liker Amni,
oligohydro amnios,
Uterine Abnormalities.
Diagnostic Evaluation:
History Collection,
Physical Examination,
clinical,
sonography,
Radiological
Clinical:
Fundal Grip:
If there is no part of the head of the fetus, a hard global mass is felt.
Head Ballotment.
Lateral grip: The back side of the fetus is felt at one site and the irregular extremities are felt at the other.
Pelvic Grip:
A soft broad and irregular mass like structure fills in pelvic grip.
Fetal Heart Sound:
A fetal heart sound is heard in the umbilical region.
Vaginal examination Soft and irregular parts are felt during pregnancy.
Sonography
Sonography is used to confirm the clinical diagnosis and identify any congenital abnormalities in the fetus.
In sonography, the gestational age of the fetus and its approximate weight are measured.
Radiology
Radiology is performed to confirm the diagnosis and to note the position of the head and limbs.
Mechanism of Labour
In sacro anterior position
The principal movement takes place in three places.
1)Buttx,
2) Solder,
3) Head.
1) Buttocks:
Buttocks are engaged in any one of the oblique diameters of the pelvis. Its engaging diameter is by trochanteric (10 cm) along the sacrum towards the iliopubic eminence. Breech presentation is engaged when the diameter passes through the pelvic brim. It continues to descend until the anterior buttocks touch the pelvic floor.
Then the internal rotation of the anterior buttocks is 1/8th of circular rotation behind the symphysis pubis. Along with this, the trunk descends with lateral flexion of the trunk. And the anterior hip emerges first from below the symphysis pubis. Then the posterior hip is delivered.
This is followed by delivery and restitution of the trunk and lower limbs. In it the buttocks which were in the engaging oblique diameter come into position.
Solder:
The bisacromial diameter (12 cm) is engaged in the same oblique diameter of the pelvis immediately after delivery of the buttocks and trunk. Internal rotation of the solder occurs in the anterior-posterior diameter of the pelvic outlet. With it the external rotation of the trunk is 1/8th of the circle.
Then delivery of posterior shoulder with anterior flexion of delivered trunk followed by delivery of anterior shoulder.
Untwisting of the trunk in restitution leads to left anterior solder in left sacro anterior (LSA) and left in right sacro anterior (RSA).
Then 1/8 th of circle anterior rotation of occiput followed by external rotation of solder in the same direction.
Now the femoral trunk comes in a dorso-anterior position.
Head:
The suboccipito frontal diameter of the head engages in the opposite oblique diameter or transverse diameter of the buttocks occupied.
Flexion increases with descent. Occiput forward 1/8th or 2/8th of circle internal rotation behind symphysis pubis. Next the subocciput continues to descend until it falls below the symphysis pubis. After flexion of the head, chin, mouth, fore head, vertex, occiput are delivered one after the other.
Management of breech delivery
Assessment of cases for breech delivery, especially in primigravida, age of mother, complicating factors, size of baby, pelvic capacity, CT scan,
M. Proper assessment of RI ultrasonography examination etc.
Delivery is planned by two methods when there is a breech presentation.
1) Elective caesarean section,
2) Spontaneous labor and vaginal breech delivery.
1) Elective Cesarean Section:
Indication: Bigbaby,
Hyperextension of the head, footling presentation, or preterm birth weight less than 1500 gm.
In obstetric or medical complications.
2) Spontaneous Labor and Vaginal Breech Delivery:
Indication:
Average Featal Weight,
flexed fetal head,
Adequate pelvis,
Absence of obstetric or medical complications,
Emergency caesarean section and continuous labor monitoring are facilitated with presence of experienced obstetrician.
Management of vaginal breech delivery:
First stage
Management is generally the same as for normal labor except that the onset of spontaneous labor increases the chances of vaginal delivery. Pelvic assessment and vaginal examination as cord prolapse is possible after membrane rupture.
Start an intravenous line to the mother and provide lactated Ringer’s solution.
Do not give to mother for oral intake. Then send for blood group and cross matching.
Monitor fetal status and progress of labor and provide oxytocin infusion for augmentation of labor.
First, cesarean section is indicated if there are any complications during labor, labor not progressing, fitus distress, code presentation or prolapse.
Second stage
There are three methods of vaginal breech delivery:
1) Spontaneous
Expulsion of the fetus with little assistance is not the preferred method.
2) Assisted breech
It helps in the delivery of the fetus from start to finish.
3) Breach extraction
In it, a part of the fetus or the entire body is delivered by obstetricians. As it causes trauma to the fetus and the mother, this method is rarely used.
Assisted Breech Delivery Breech delivery should be performed by a skilled obstetrician.
For that, the neonatologist should keep the anesthetist, assistant instrument and suture material, resuscitation equipment for the baby ready.
steps
When the anterior part of the fetus is visible, place the patient on the labor table and provide the patient with lithotomy position as the part distends the perineum.
After doing antiseptic cleaning and emptying the bladder through catheter.
Administer pudendal block to the patient. Episiotomy, when necessary, is performed when the perineum is distended.
Then advise the patient to wear bearing down afores.
Then do not touch the feet until the buttocks slip with the leg in the flex breech and deliver to the umbilical.
After the delivery of the trunk to the umbilical cord, take the umbilical cord downwards to one side, if the back is on the posterior side, rotate the trunk and bring it to the anterior side.
DELIVERY OF ARMS
To prevent extension of the arm, the assistant should keep his hand on the fundus and give steady pressure during uterine contractions, note the position of the hand when the scapula is visible, when the axilla is visible, deliver the arm one after the other by simple locking with a finger in each elbow and At that time, cover the baby’s legs with a stylish towel and never pull them down to hold them.
Delivery of the after coming head
The preferred time between umbilical to mouth delivery is five to ten minutes and is a more crucial stage. Following are the general methods for delivery of fitus:
1) Burn Marshall Method
This method involves letting the baby hang on its own weight and asking the assistant to apply suprapubic pressure with the hand in a downward and backward direction.
So the head flexes more and the pelvic cavity has a favorable diameter, when the nape of the neck is visible below the pubic arch, hold the baby with a finger between the two ankles.
Then keep steady traction and keep the trunk in upward and forward direction During this time hold the perineum with the left hand and allow the face and brow to be delivered from it one after the other After delivery of the mouth remove the secretion with a mucus shaker for the delivery of the rest of the head Depress the trunk.
2) Forceps delivery
In forceps delivery, the head should be in the pelvic cavity for delivery of the after coming head in the breech, Das or specially designed piper forceps are used in ordinary forceps.
3) Malar Flexion Shoulder Traction (Modified Mauriceau and Smiley Weight Technique):
Keeping the baby on the supinated left forearm and letting the limbus hang on either side. Place the middle and index fingers of the left hand on the malarbone on either side. This will maintain the flexion of the head.
Then place the ring and little fingers of the pronated right hand on the child’s right shoulder, the index finger on the left shoulder and the middle finger on the occipital region.
Apply traction in a downward and backward direction until the nape of the neck is visible below the pubic arch. and have the assistant apply suprapubic pressure to maintain flexion and
Then, by moving the baby in an upward and forward direction towards the mother’s abdomen, the face, brow will be delivered and finally the occiput and vertex will be delivered by depressing the trunk.
Resuscitate the baby immediately if there is asphyxia after delivery.
- Face Presentation:
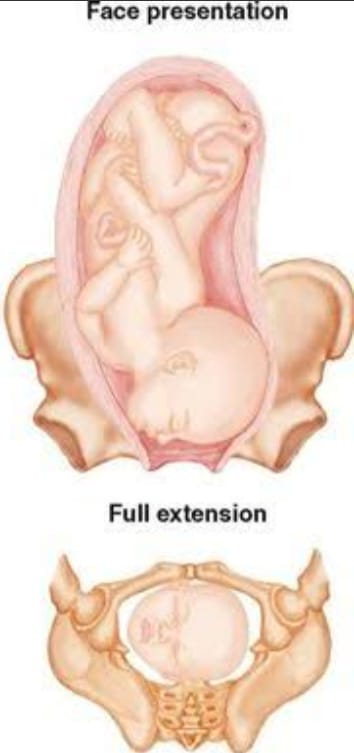
Face presentation is a malpresentation of the fetus in the uterine cavity in which the lie of the fetus is longitudinal but with the chin as the face as the presenting part while the head is in an attitude of complete extension.

Etiology:
Fault in passage: Inlet contraction of pelvis is important.
Fault in passenger:
Pendulous abdomen in large fits, multipara
Favors face presentation.
Malformed fits make up 15% incidence.
Anencephaly usually has a facial presentation.
Lateral obliquely of the uterus especially if directed towards the side towards which the occiput lies.
A contracted pelvis is associated in about 40% of cases.
A flat pelvis favors face presentation.
The etiology of face presentation is not clear but associated factors such as, multipara, contracted pelvis, flat pelvis, pelvic tumor and congenital malformation in fetal factor, congenital goiter, cord twisting around the neck, increased tone of extensor group in neck muscles lead to face presentation. is seen.
Diagnostic evaluation
history taking,
Physical Examination,
Diagnosis is sometimes made in late pregnancy and before labor.
Ultrasound to identify fetal presentation and fetal anomalies.
Clinically, vaginal examination helps to confirm the face presentation.
Abdominal Findings:
Inspection: Bulging of flanks due to S sap spine is not visible.
Palpation:
Mento Anterior:
Lateral grip: Fital limbs are forward flank back side and difficult to palpate.
Pelvic Grip: The head is not engaged because the head is large, the side with the back has a cephalic prominence, and the groove between the head and the back is not engaged.
Auscultation: Fetal heart sounds are heard anteriorly over the chest wall on the leeward side.
Vaginal examination: Vaginal examination should be done gently, as eye injury may occur. Palpate the hard alveolar margin, nose, malar eminence, supra orbital ridges and mentum in the mouth.
Sonography: Diagnosis Sonography is done to look for conformation, fetal size and congenital anomalies.
Mechanism of Labour:
Position: Mentoanterior ( 60-80%,L.M.A/R.M.A.).
Principal Movement: Principal movement follows the occipito-anterior position but with increased extension rather than flexion, delivery of the head is through flexion rather than extension.
Engagement: Engagement of the head in the oblique diameter of the pelvis with an iliopubic eminence of the mentum and the opposite sacro-iliac joint of the glabella in the right ma L.M.A. and R.M.A in Lieut. happens A sub-mento-bragmatic 9.5 cm in a fully extended head or a sub-mento-vertical 11.5 cm in a partially extended head becomes an engaging diameter.
Descent: Extension of the head increases with descent until the chin touches the pelvic floor.
Internal Rotation: 1/8th circle of the anterior chin causes the mentum to come back in front of the incisus pubis with internal rotation and continuous descent until the submentum falls below the cubic arch.
Delivery of Head: Head chin face, brow, vertex finally occiput are delivered by flexion one by one.
Submento-vertical diameter 11.5 cm distending vulval outlet.
A restitution of 1/8th circle in the opposite direction of internal rotation.
Then 1/8th circle external rotation in same side of restitution face L.M.A. Lieut in and R. M.A. In comes to right thigh followed by delivery of anterior shoulder then posterior shoulder and trunk is delivered through lateral flexion.
Management:
Patients presenting with soft presentation by vaginal examination or prolonging to 12 hours in the first stage are referred for level A care.
In the first stage, the diagnosis of face presentation is made by abdominal and vaginal examination.
Fetal size, malformation and pelvis size are assessed.
Partograph is properly maintained.
A vaginal examination is performed when the membranes are ruptured to exclude a prolapsed cord. Care should be taken to avoid infection or injury to the ice during the examination.
In case of cephalic disproportion or high risk pregnancy-Cesarean section is done.
The third stage is actively managed.
Neonates are cared for carefully and properly.
Throat is properly suctioned.
Proper oxygenation is provided.
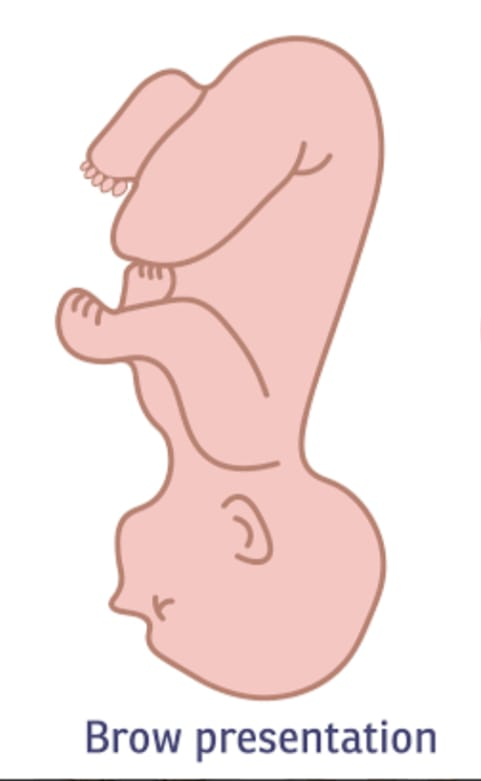
- Bro Presentation:
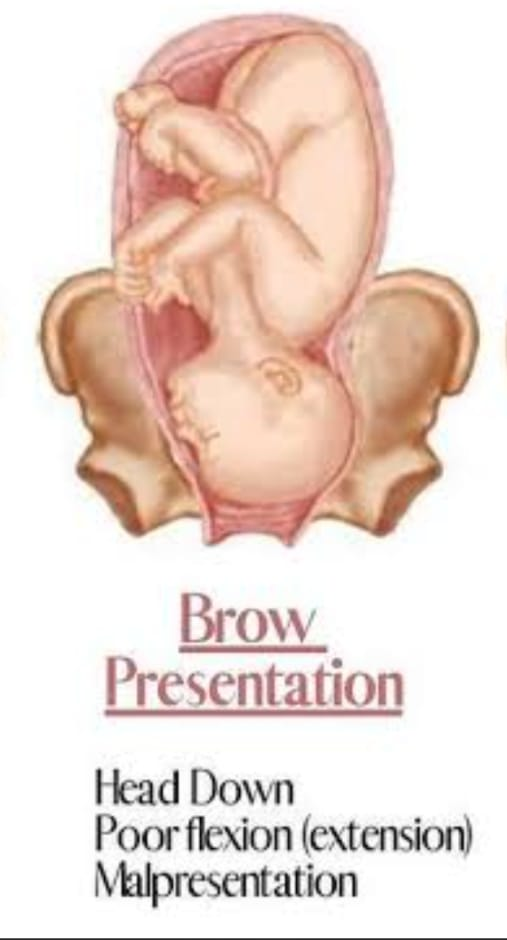
“Brow presentation is the rarest condition of cephalic presentation where the brow is the presenting part and the attitude of the head is short of the degree of extension required for presentation of the face, i.e. the head lies between full flexion and full extension.” .Brow presentation, “The head of the fetus is extended along the frontal bone in the pelvic brim. The presenting part is bounded by the anterior fontanel and orbital ridges”.
Etiology:
Fault in passage: Inlet contraction of pelvis is important.
Fault in passenger:
Pendulous abdomen in large fits, multipara
Favors face presentation.
Malformed fits make up 15% incidence.
Anencephaly usually has a facial presentation.
Lateral obliquely of the uterus especially if directed towards the side towards which the occiput lies.
A contracted pelvis is associated in about 40% of cases.
A flat pelvis favors face presentation.
The etiology of face presentation is not clear but associated factors such as, multipara, contracted pelvis, flat pelvis, pelvic tumor and congenital malformation in fetal factor, congenital goiter, cord twisting around the neck, increased tone of extensor group in neck muscles lead to face presentation. is seen.
Diagnostic evaluation
history taking,
Physical Examination,
Diagnosis is sometimes made in late pregnancy and before labor.
Ultrasound to identify fetal presentation and fetal anomalies.
Clinically, vaginal examination helps to confirm the bro presentation.
Vaginal examination: Vaginal examination should be done gently, as eye injury may occur. Palpate the hard alveolar margin, nose, malar eminence, supra orbital ridges and mentum in the mouth.
Sonography: Diagnosis Sonography is done to look for conformation, fetal size and congenital anomalies.
Mechanism of Labour:
Engagement diameter is the oblique diameter through the diameter along the anterior or posterior of the brow.
Engagement of the head is through the mentovertical diameter.
An average size baby with a normal pelvis has no mechanism of labor.
Descent down until the brow touches the pelvic floor.
Internal rotation and descent down until the hinge of the nose reaches the symphysis pubis.
Brow and vertex are followed by extension to deliver the face.
There is no mechanism in the posterior brow position.
Management:
Patients with face presentation are referred to level 2 care.
If the patient has a persistent brow presentation, cesarean section is considered the treatment of choice.
Manual correction is rarely done.
If labor is obstructed and the baby is dead, a craniotomy is performed.
In the first stage, the diagnosis of face presentation is made by abdominal and vaginal examination.
Fetal size, malformation and pelvis size are assessed.
Partograph is properly maintained.
A vaginal examination is performed when the membranes are ruptured to exclude a prolapsed cord. Care should be taken to avoid infection or injury to the ice during the examination.
In case of cephalic disproportion or high risk pregnancy-Cesarean section is done.
The third stage is actively managed.
Neonates are cared for carefully and properly.
Throat is properly suctioned.
Proper oxygen is provided to the child.
- Transverse Lie:
When the long axis of the fitus is perpendicular to the axis of the mother’s spine or the centralized uterus, it is called transverse lie”. Transverse lie is a serious complication in obstructive. In transverse lie, the long axis of the fitus is in the crotch of the mother. and the solder is usually the presenting part. The fitus lies in front of the mother or the spine. This position is dorso-anterior and dorso-posterior.

Etiology:
Multiparity: lax and pendular abdomen, imperfect uterine tone, extreme uterine obliquity.
prematurity,
twins,
hydroamnios,
Contracted pelvis,
placenta previa,
pelvic tumor,
Congenital Malformation of the Uterus,
Intra uterine death.
Diagnostic evaluation
History Collection,
Physical Examination,
Abdominal Examination:
Inspection: Uterus appears broader and asymmetric and pear form sap is not maintained.
Palpation: Fundal height is found to be less than during amenorrhoea.
Fundal grip: The fundal pole is not palpable.
Lateral Grip: A soft, broad and irregular breech is felt on one side of the midline and a smooth, hard and globular head is felt on the other side. The head is usually placed at a lower level on an iliac fossa.
A portion of the back is felt anteriorly on the long axis in a dorso-anteriorly portion or irregular small parts are felt anteriorly in a dorso-posteriorly portion.
Pelvic grip: The lower pole of the uterus becomes empty.
Auscultation: F.H.S. It is most easily heard below the umbilicus in the dorso-anterior position. dorso-posteriorly, F.H.S. are located on the higher level.
Sonar/X-ray
Ultrasonography/radiography conforms to the diagnosis.
Vaginal Examination:
The presenting part is so high that it cannot be properly identified but some soft parts can be felt.
Solder is identified by palpation
such as:
Acromion process
scapula
Clavicle
Exila
Ribs of the chest wall.
Management:
During antenatal care, women identified as having a transverse lie are referred for Level II care by 34 weeks.
In the Level II antenatal clinic, the diagnosis is confirmed clinically and its etiology is looked at.
Quality antenatal care is provided every 2 weeks till 36 weeks and then weekly until term. She is admitted to hospital from 38 weeks onwards.
As with breech presentation, external cephalic version is performed up to early labor (20%) after 37 wk.
At the end of pregnancy (39-40 weeks), a cesarean section is performed.
Perform external cephalic version if it lies transversely and with solder presentation prior to membrane rupture. If successful, A.R.M. Then perform vertex vaginal delivery. If ECV fails, delivery is by caesarean section.
Caesarean section is performed in cases with high risk factors, ie placenta previa, uterine deformity etc.
Simultaneously the mother in transverse lie is referred to a level II care hospital.
If the fitus is live, the arm is mature with or without prolapse, or the orifice is dilated completely or incompletely, a cesarean section is performed.
If the fetus is stillborn, a caesarean section is performed.
If the fitus is small, dead, and deformed, an external podalic version is performed and a breech delivery is performed.
Sometimes decapitation and aspiration are also done. Then the 3rd stage is actively managed.
- Unstable Lie:
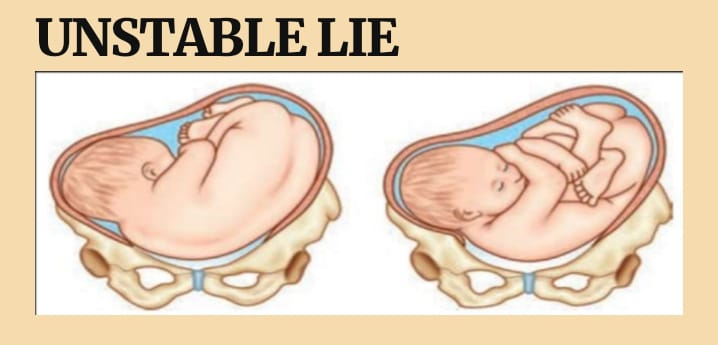
“Unstable lie” is a condition where the placenta does not remain stable within the uterine cavity. “This is a condition where the presentation of the fetus changes continuously even after the 36th week of pregnancy when it should be stable in the uterine cavity.” This word no use happens then.
When the fitus is not in a continuously stable position in the uterine cavity and there are frequent changes in position, this can make the labor process complicated. An unstable lie can cause difficulties during delivery, as the fitus is not in the optimal position for a smooth birth. Unstable fits require careful monitoring and management for safe delivery.
Etiology:
Excessive amniotic fluid (polyhydramnios),
Inadequate amniotic fluid
(oligohydramnios),
Abnormal fetal presentation,
multiple pregnancy,
Uterine Anomalies,
Abnormal uterine tone,
Due to abnormal secretion of uterine cavity,
Because of the pelvic size and sep.
Due to placental abnormalities,
Due to increased activity of fitus,
Due to decreased uterine tone and pendulous abdomen with grand multipara,
Because of the contacted pelvis,
Due to pelvic tumor,
Due to reduced muscle tone of uterine cavity due to multigravida.
Symptoms and Signs:
Abnormal fetal position,
Frequent changes in the fittal lie.
Difficulties in palpating the fetal position.
Unusual and abnormal fetal heart rate patterns.
Maternal discomfort and abnormal uterine contractions.
Diagnostic Evaluation:
History Collection,
Physical Examination,
ultrasound imaging,
Fetal heart rate monitoring,
Abdominal palpation,
Maternal History Review,
Pelvic Examination.
Management:
Properly check mother’s presentation and lie during antenatal period visit.
An external cephalic version is performed if not contraindicated.
The patient should be admitted to the hospital within 38 weeks of pregnancy.
Conduct proper investigation of the patient.
Excludes:
Placenta previa.
Contracted pelvis.
Congenital malformation of Fitus (sonography is done).
In the presence of complicating factors (as above), elective cesarean section is performed.
In the absence of complicating factors, the patient is placed for induction followed by ECV (external cephalic version). If necessary, an oxytocin drip is started.
After 1 hour, internal examination is done to exclude cord presentation and then LRM (Low Rupture of Membrane) is done.
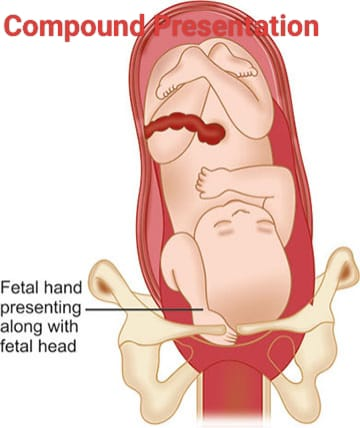
- Compound Presentation:
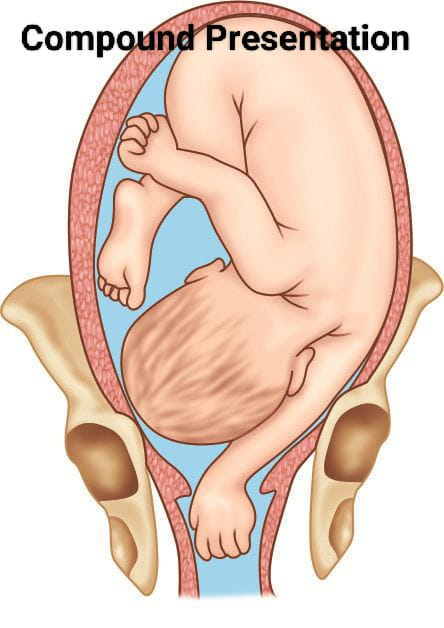
When one or more fit extremities are present along with the presenting part during intra-uterine life, it is called compound presentation. When cephalic presentation is complicated by the presence of hand or foot next to the head or both, or one or both hands next to the breech. A presence is called a compound presentation. In a compound presentation, the hand with the head is a common presentation.
Etiology:
Due to excessive amniotic fluid (polyhydroamnios),
Due to multiple gestation,
Uterine Anomalies,
Abnormal fetal presentation,
Fetal hyperactivity,
inadequate uterine tone,
prematurity,
Contracted pelvis,
pelvic tumor,
multiple pregnancy,
High head with premature or early ROM,
Hydramenios
Symptoms and signs:
Abnormal fetal presentation.
Labor progression becomes difficult and abnormal.
Increased maternal discomfort.
Fetal heart rate (FHR) becomes irregular.
Complicated delivery or engagement difficulties.
Feet hand and arm presentation.
Diagnostic evaluation
History Collection,
Physical Examination,
Abdominal palpation,
Fetal heart rate monitoring,
Pelvic Examination.
Management:
The position of the feet is properly assessed by ultrasound.
Rotation is done manually for proper repositioning of the parts of the fits.
Properly supportive care is provided to relieve the mother’s discomfort
A cesarean section is generally preferred in compound presentations.
In case of dead fetus, advice is provided for destructive operation.
Forceps and vaginal delivery are also performed in compound presentations but are generally considered high risk.
- Contracted pelvis:
A contracted pelvis is a condition in which the female bony pelvis is sufficiently abnormal in shape and size that vaginal delivery is difficult even in a normal-sized baby. That is, there are changes in the normal mechanism of labor. This is called a contracted pelvis. The female bony pelvis is divided into four sizes according to the size of the inlet.
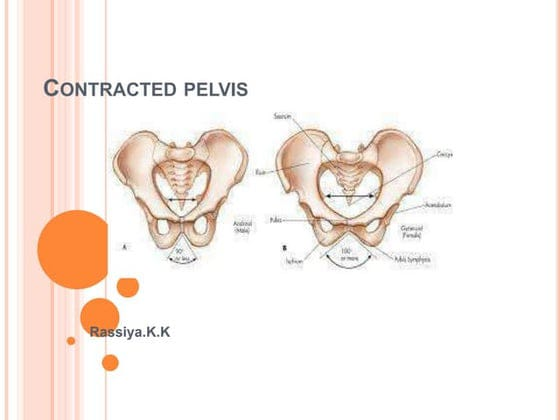
- Gynaecoid pelvis (round shape) (50%),
2.Anthropoid pelvis (oval sep) (25%), - Android Pelvis (Heart Sap)( 20 %),
4.Platypeloid pelvis (kidney sep) (5 %).
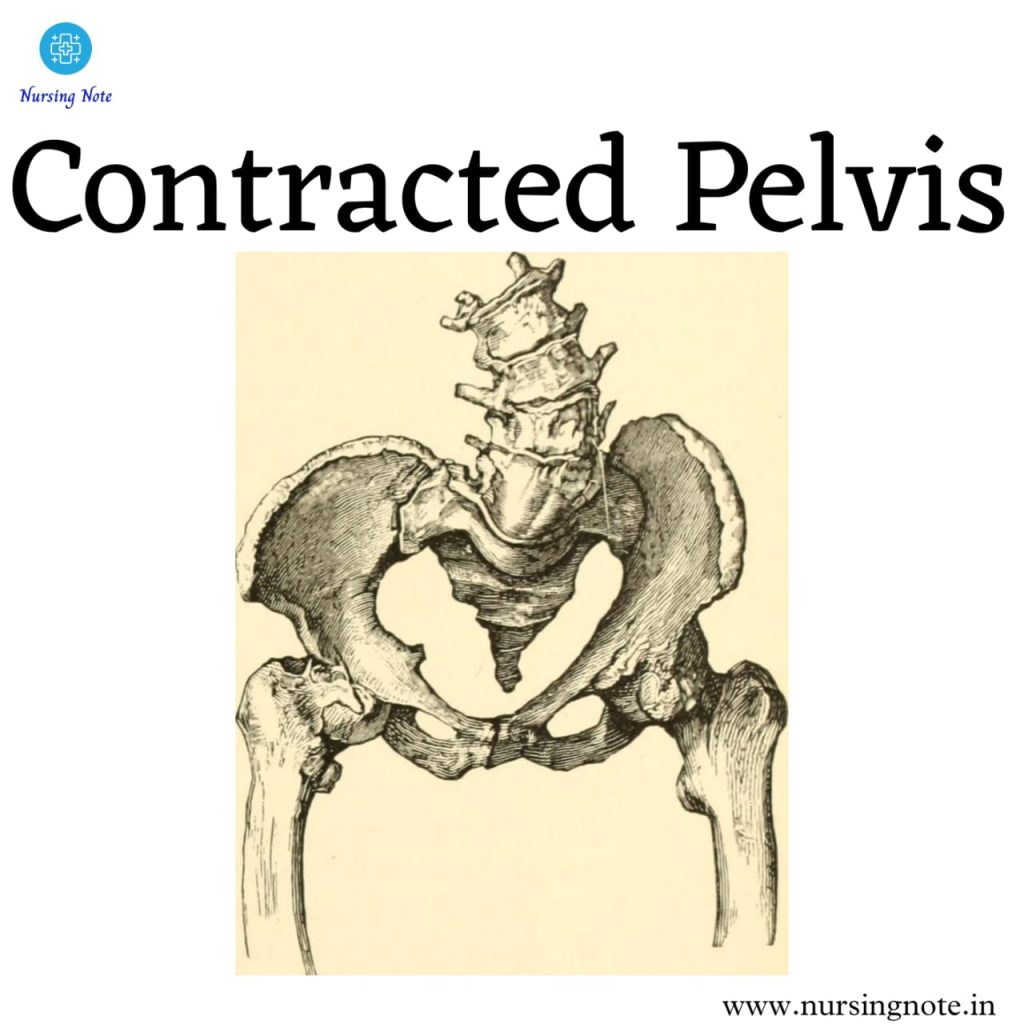
Etiology:
Developmental factors: It can be due to hereditary or congenital factors.
such as,
Nigel’s pelvis,
Robert Pelvis.
racial factor,
Nutritional factor: The condition of small pelvis arises due to poor nutrition/malnutrition.
Hormonal factor: The condition of android pelvis arises due to excessive androgen secretion.
Metabolic factors: such as rickets and osteomalacia.
Trauma, Diseases of Bone or Tumor: Fracture, Tumors, Tubercular Arthritis, Kyphosis, Scoliosis, Spondylolithiasis, Coccygeal Deformity, Poliomyelitis, Hip Joint Disease.
Degree of Contracted Pelvis:
1.Minor Degree or Minor Disproportion: Here True Conjugate 9-10 cm. Vaginal delivery is possible.
2.Moderate degree or minor disproportion: Here the true conjugate is 8-9 cm. Trial labor can be a trial. And if it fails, a caesarean section is performed.
3.Severe degree or severe disproportion: Here the true conjugate is 6 cm. is less than Cesarean section is preferred.
Symptoms and signs:
Difficult Labour,
Abnormal fetal presentation,
Maternal pelvic pain,
Frequent urinary tract infections,
Back pain.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Imaging studies such as,
x ray,
pelvic ultrasound,
Computed tomography scan (CT scan),
Magnetic Resonance Imaging (MRI),
pelvimetry,
Clinical pelvic assessment.
Management of Contracted Pelvis:
Management of a contracted pelvis, which refers to a pelvis that is abnormally small and has an abnormal shape that can make the birth of a child difficult, involves careful assessment and intervention to ensure the safety of both mother and child during labor and delivery. need of
1) Diagnosis and Assessment:
Pelvimetry
Pelvimetry is the measurement of the pelvis to assess its dimensions and shape. This measurement can be done clinically (external measurement) or radiologically (X-ray, MRI).
Take a complete history of the mother Take a complete history of the mother to assess whether any difficulties have arisen in the mother previously at the time of delivery or at the time of cesarean delivery.
Clinical Evaluation A complete physical examination of the mother including mostly pelvic measurements can be done to properly assess the condition of the contracted pelvis.
2) Antenatal Care:
Early detection
Early identification of contracted pelvis through routine antenatal checkup or ultrasound examination during the early period of pregnancy.
Consultation
Refer women with high-risk pregnancies to specialist obstetricians and perinatologists for their comprehensive management.
3) Labor Management:
Continuous Monitoring
Close monitoring of maternal and fetal condition during labour, including proper monitoring of fetal heart rate and proper assessment of maternal vital signs.
Labor Progress
Assessing the labor process continuously if labor is slow or arrested indicates a condition of cephalopelvic disproportion.
Positioning
Providing the mother with a proper position that provides optimal pelvic dimensions for labor to progress.
4) Intervention During Labour:
Artificial Rupture of Membrane
If the membrane is intake and labor is progressing slowly, the progress of labor can be improved by artificially rupturing the membrane.
Oxytocin infusion
Provide oxytocin infusion to improve contractions along with continuous monitoring of fits and uterine contractions.
Instrumental Delivery:
If the baby is in distress and vaginal delivery is possible, vacuum extraction or forceps delivery can be performed.
5) Cesarean section:
indication
When vaginal delivery is impossible, caesarean section is performed to prevent fits and any complications of mothering.
timing
When vaginal delivery is impossible, it is important to make a decision to perform a timely caesarean section to prevent complications for the fetus and the mother.
6) Postpartum Care:
Maternal monitoring
Closely monitoring the mother during the postpartum period can prevent any complications like postpartum hemorrhage.
Neonatal care
Providing newborn care immediately after the birth of the newborn especially when any condition of complicated labor arises is necessary to ensure that the newborn is properly well-being.
7) Counseling and Education:
Education
Educate the mother and her family members by providing complete information about the mother’s condition and its causes and interventions.
Future Pregnancy Planning
Discuss the effect of a contracted pelvis on future pregnancy and delivery options.
8) Multidisciplinary Approach:
Team collaboration
Obstetricians, midwives, anesthetists, neonatologists, all these specialists should be available when there is an over-complicated condition.
9) Psychological Support:
The condition of contracted pelvis is stressful and emotionally challenging for the woman, so proper psychological support should be provided to the mother and family members.
Thus, proper management of contracted pelvis is important to prevent complications to mother and child.
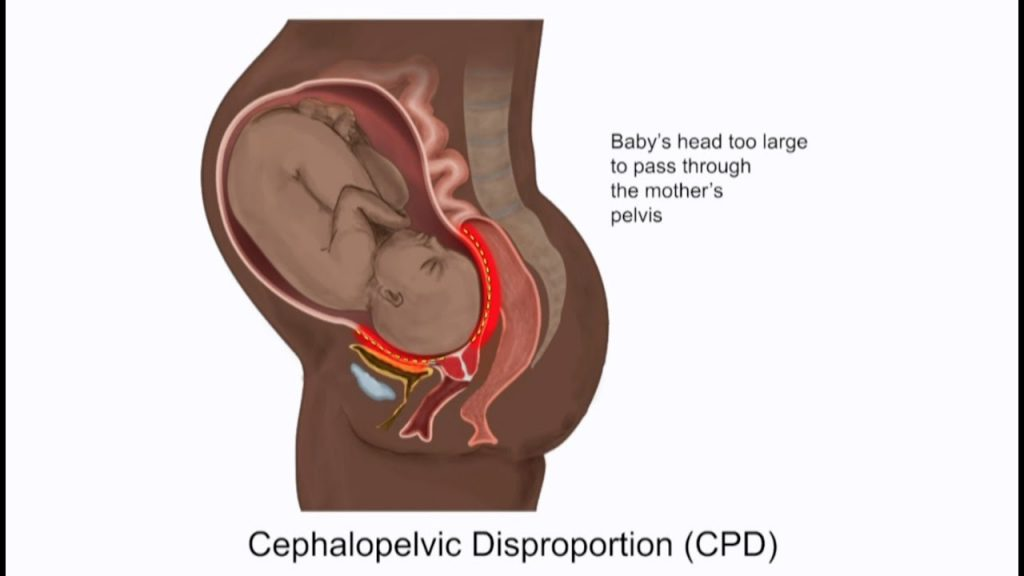
- Cephalo Pelvic Disproportion (CPD):
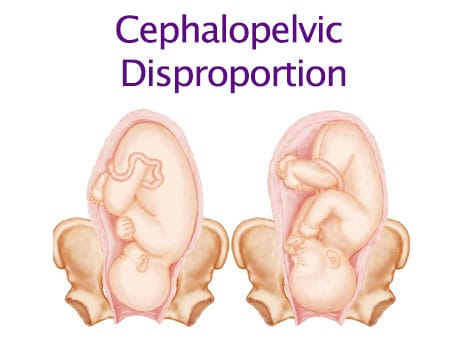
Definition:
When the normal proportion between the size of the fetus and the pelvis is disturbed, it is called cephalopelvic disproportion (CPD). If there is disparity (inequality) in the relationship between the fetal head and the maternal pelvis, this condition is called cephalopelvic disproportion (CPD). The disproportion can be either an average size baby with a small pelvis or a big baby with a normal size pelvis or a combination of both. is
In cephalopelvic disproportion (CPD),
1.Average size baby with small pelvis.
2.Normal size baby with big baby.
- The combination of both factors.
Etiology:
Large Baby:
Hereditary factor,
diabetes,
postmaturity,
Multiparity.
Abnormal fetal position.
Contracted pelvis.
Abnormally spaced pelvis.
Fetal macrosomia,
Abnormal fetal presentation,
hydrocephalus,
pelvic abnormalities,
Naturally Small Pelvis,
Privus Pelvic Surgery,
Ineffective uterine contractions,
Prolonged labour,
Genetic factor.
Symptoms and signs:
Difficult Labour,
Prolonged labour,
Obstructed labour,
Abnormal fetal presentation,
Fital Distress,
Abnormal fetal presentation,
Maternal pelvic pain,
Frequent urinary tract infections,
Back pain.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Imaging studies such as,
x ray,
pelvic ultrasound,
Computed tomography scan (CT scan),
Magnetic Resonance Imaging (MRI),
pelvimetry,
Clinical pelvic assessment.
Management:
Take a complete history of the mother Take a complete history of the mother to assess whether any difficulties have arisen in the mother previously at the time of delivery or at the time of cesarean delivery.
Clinical Evaluation A complete physical examination of the mother including mostly pelvic measurements can be used to properly assess the condition of the contracted pelvis.
Pelvimetry
Pelvimetry is the measurement of the pelvis to assess its dimensions and shape. This measurement can be done clinically (external measurement) or radiologically (X-ray, MRI).
Antenatal Care:
Early detection
Early identification of cephalopelvis disproportion through routine antenatal checkup or ultrasound examination during the early period of pregnancy.
Consultation
Refer women with high-risk pregnancies to specialist obstetricians and perinatologists for their comprehensive management.
Labor Management:
Continuous Monitoring
Close monitoring of maternal and fetal condition during labour, including proper monitoring of fetal heart rate and proper assessment of maternal vital signs.
Labor Progress
Assessing the labor process continuously if labor is slow or arrested indicates a condition of cephalopelvic disproportion.
Positioning
Providing the mother with a proper position that provides optimal pelvic dimensions for labor progress.
Interventions During Labor:
Artificial Rupture of Membrane
If the membrane is intake and labor is progressing slowly, the progress of labor can be improved by artificially rupturing the membrane.
Oxytocin infusion
Provide oxytocin infusion to improve contractions along with continuous monitoring of fitus condition and uterine contractions.
Instrumental Delivery:
If the baby is in distress and vaginal delivery is possible, vacuum extraction or forceps delivery can be performed.
Cesarean section:
indication
When vaginal delivery is impossible, caesarean section is performed to prevent fits and any complications of mothering.
timing
When vaginal delivery is impossible, it is important to make a decision to perform a timely cesarean section to prevent complications for the fetus and the mother.
Postpartum Care:
Maternal monitoring
Closely monitoring the mother during the post-partum period can prevent any complications like post-partum haemorrhage.
Neonatal care
Providing newborn care immediately after the birth of the newborn especially when any condition of complicated labor arises is necessary to ensure that the newborn is properly well-being.
Counseling and Education:
Education
Educate the mother and her family members by providing complete information about the mother’s condition and its causes and interventions.
Future Pregnancy Planning
Discuss the effect of a contracted pelvis on future pregnancy and delivery options.
Multidisciplinary Approaches:
Team collaboration
Obstetricians, midwives, anesthetists, neonatologists, all these specialists should be available when there is an over-complicated condition.
Psychological Support:
The condition of cephalopelvis disproportion is stressful and emotionally challenging for a woman, so proper psychological support should be provided to the mother and family members.
Thus, proper management of cephalopelvis disproportion is important to prevent complications to mother and child.
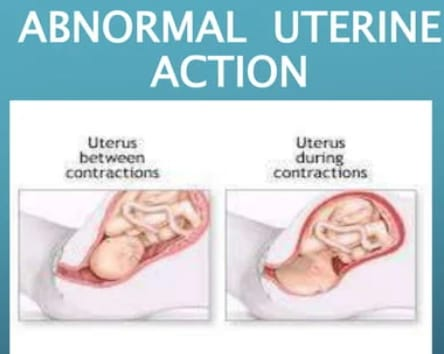
Abnormal Uterine Actions:
Normal Uterine Action:
In normal labor there is progressive dilatation of the cervix with coordinated uterine contractions and descent of the fetal head and finally successful vaginal delivery. The polarity of the uterus means that the upper segment of the uterus contracts and the lower segment relaxes. Normally, there are pacemakers on both upper sides of the uterus, due to which uterine contractions can occur properly.
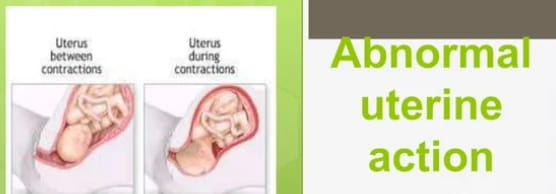
Now, Abnormal Uterine Actions means a condition in which the contraction of the uterine muscles during labor changes in its normal frequency, duration, intensity, and pattern, then this condition is called Abnormal Uterine Actions. Due to this contraction, ineffective labor occurs. , the condition of prolonged labor may arise. When there is any deviation in the normal pattern of uterine contractions, it also affects the progress of labor, which is called abnormal uterine actions. When there are any changes in the normal pattern of contractions and it affects the normal pattern of labour, it is called abnormal uterine action.
Types of Abnormal Uterine Actions:
1.Hypotonic uterine action,
- Hyper tonic uterine action,
- Un-coordinated uterine action,
- Dysfunctional uterine action,
- Prolong uterine action.
1.Hypotonic uterine action,
- Hyper tonic uterine action,
- Un-coordinated uterine action,
- Dysfunctional uterine action,
- Prolong uterine action.
1.Hypotonic uterine action: It has weak and infrequent uterine contractions due to which effective cervical dilatation cannot occur.
- Hyper tonic uterine action: It causes strong and frequent uterine contractions, due to which uterine fatigue and labor process are in adequate progress.
- In-Coordinated Uterine Action: It involves disorganized uterine contractions that do not follow the regular pattern of uterine contractions. Due to which the condition of ineffective labor progression arises.
- Dysfunctional uterine action: Dysfunctional uterine action involves the involvement of hypotonic and hypertonic uterine action. Due to which effective labor process cannot take place.
- Prolong Uterine Action: It involves uterine contractions for a long duration due to which fetal distress and uterine rupture can also occur.
Etiology:
Uterine Muscle Fatigue,
Hormonal imbalance (Ex : Oxytocin),
Uterine Abnormalities (Ex: Fibroids, Congenital Anomalies),
Fetal factors (macrosomia, abnormal presentation),
Inadequate maternal pelvic size,
Medication effect
(Analgesic, anesthetic)
Dehydration, electrolyte imbalance,
Privus uterine surgery (scarring, adhesions),
Emotional stress and anxiety,
Infection and inflammatory conditions (chorioamnionitis),
Multiple Gestation (Twins),
Maternal health conditions (eg diabetes, hypertension),
Nutritional deficiency (due to essential vitamins and minerals in adequate amounts).
Elderly primi gravida,
Prolonged pregnancy,
fibroids,
emotional factor,
Constitutional Factors,
Contracted pelvis,
malpresentation,
Due to improper use of drugs such as sedatives, analgesics, and oxytocins,
Premature attempt at vaginal delivery and instrumental vaginal delivery under light anesthesia.
Due to mother’s advanced age,
Prolonged pregnancy.
Symptoms and signs:
Prolonged labour.
ineffective uterine contractions,
Vic and infrequent uterine contractions,
Fital Distress,
Changes in fetal heart rate patterns,
Maternal discomfort and pain,
Failure to progress labor and cervical dilatation,
Diagnostic Evaluation:
history taking,
Physical Examination,
fital monitoring,
uterine monitoring,
ultrasound,
Laboratory test
Management:
Assessment and Monitoring:
Continuous fetal monitoring:
Continuous monitoring of the fetus. Assessing the well-being of the fetus. Properly assess for any signs and symptoms of fetal distress.
Regular Maternal Assessment: To properly monitor the mother’s vital signs and assess uterine contractions. To properly assess the condition of cervical dilatation of the mother.
Support During Labor:
Hydration: Advise the mother to intake water in adequate amount to prevent the condition of dehydration. Which plays an important role in affecting the uterine function.
Pain Management: Provide adequate amount of labor and comfortable environment to relieve the mother’s pain and provide epidural analgesia to the mother. Due to which the discomfort during labor can be removed.
Positioning and Mobility:
Anchorage Maternal Movement: Advising the Mother to Walk Properly. Due to which uterine contractions can occur properly. And can be easily delivered.
Medication:
Oxytocin administration: Oxytocin should be administered when urinary contractions are slow, hypotonic, or ineffective, which may increase the frequency of uterine contractions.
Tocolytic: Provide tocolytic medication when uterine action is hyper tonic.
Mechanical Intervention:
Amniotomy: Artificial rupture of membranes while labor is intact to enhance labor progress.
Surgical Intervention:
Cesarean delivery: If the labor process is a failure and there is a condition of fetal distress, there is a need for a cesarean delivery.
Postpartum Care:
Monitoring for recovery:
Properly assess if there are any complications after delivery.
Counselling: Provide support and information for future pregnancies. Assessing the potential risk of abnormal uterine contractions.
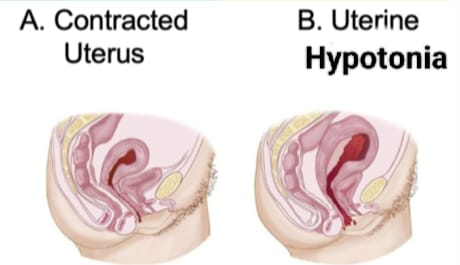
- Uterine Hypotonia/Uterine Inertia:

Uterine hypotonia condition also called uterine inertia involves low or poor tone in muscle fibers of uterine cavity. This leads to wick contraction of the uterine cavity which is infrequent and does not cause much pain. Therefore, cervical dilatation occurs slowly and the labor process is usually prolonged. Uterine inertia is a common but less serious type of uterine dysfunction that occurs early in or later in labor.
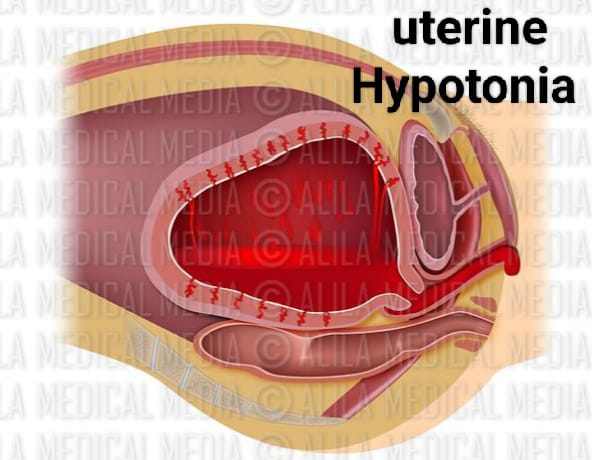
In uterine inertia, the normal pattern of uterine contractions is maintained to a lesser extent, and intrauterine pressure remains below 25 mm of Hg during contractions. The intensity and duration of contractions decrease and the relaxation and interval between two contractions increases.
Types of Uterine Inertia:
There are generally two types of uterine inertia:
1.Primary uterine inertia
- Secondary uterine inertia.
1.Primary Uterine Inertia: Primary Uterine Inertia is a condition that usually arises when the uterus cannot contract effectively during the onset of labor. This condition can usually occur due to maternal fatigue and hormonal imbalance.
- Secondary Uterine Inertia: This type usually occurs after the onset of initial effective contractions, which are usually weak and can be caused by maternal exhaust, issues in fetal position and obstructions.
Symptoms and signs:
Less pain fills during contraction time.
The uterus becomes less hard and the peak level of pain also fills the uterine wall.
After the contraction, the uterus becomes normal.
Fitter heart sound (FHS) is normal and fetal parts are well palpable.
The intensity of uterine contractions is demineralized.
Uterine contractions are of short duration.
A good amount of relaxation occurs between contractions.
The interval is incremented.
The general pattern of uterine contractions of labor is maintained.
There is limb retraction and evidence of poor cervical dilatation along with a contracted pelvis, malposition, flexed head, or mid-presentation.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Diagnosis is usually made from clinical features and associated factors such as:
Contracted pelvis,
malposition,
Deflexed head,
Misrepresentation etc.
pelvic examination,
ultra sound,
Maternal History Review,
Labor progress monitoring,
Laboratory test.
Management:
Provide proper left lateral position to mother and advise mother to avoid supine position.
Careful evaluation of mother’s condition.
Properly assess whether the patient is in labor.
Properly assess whether there is a condition of cephalopelvic disproportion or malpresentation through abdominal and pelvic examination.
Catheterization properly to empty the bladder.
Properly start the patient on an I.V. line to maintain hydration.
Provide intramuscularly (I.M.) pethidine to relieve the patient’s pain.
Perform artificial rupture of membranes (ARM) to increase contractions and start drip of oxytocin.
If uterine contractions do not increase even after starting oxytocin drip, caesarean section is preferred.
Cesarean section is planned in following cases like contracted pelvis, mal presentation and condition of fetal and maternal distress.
Increasing moral support of the patient in vaginal delivery and changing the patient’s posture including avoiding supine position and giving advice to the mother to empty the bladder properly and if unable to empty then doing catheterization and providing intravenous fluid to the woman and providing analgesics to do
Continuous monitoring of fetal heart sound (FHS).
Continuous monitoring of mother’s condition.
Properly assess the condition of mother and baby after delivery.
To provide proper reassurance to mother after delivery.
Providing proper work and quiet environment to the mother and giving advice to take proper rest.
Incoordinated Uterine Action/ Abnormal Polarity:
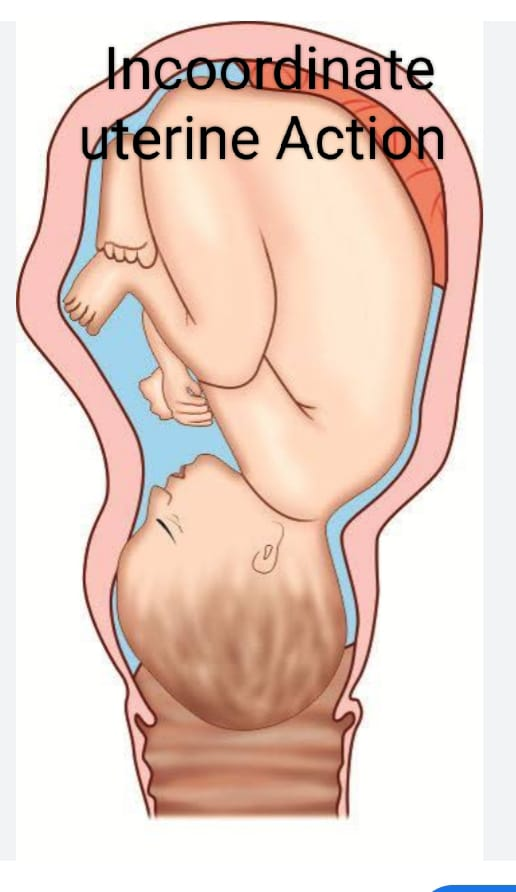
Irregular, ineffective, or poorly coordinated contractions of the uterine cavity during uncoordinated uterine action. As opposed to normal contractions which are rhythmic and help in cervical dilatation and descent of the fitus, uncoordinated uterine action of the uterus can lead to prolonged labor and complications.
This condition can be caused by factors like hormonal imbalance, maternal stress or previous uterine surgery. Incoordinated uterine action is a type of abnormal uterine action that occurs when the upper and lower parts of the uterine cavity fail to work in a coordinated manner. Due to which the condition of long, difficult and prolonged labor can occur.
This uncoordinated uterine action is mostly seen in active stage of labor due to conditions like spastic lower uterine segment, colicky uterus, asymmetric uterine contraction, constricting ring, generalized tonic contraction of uterus, cervical dystocia etc. What happens is called uncoordinated uterine actions.
Etiology:
Due to hormonal imbalance,
Due to structural abnormalities of the uterine cavity,
Due to abnormalities in pelvic shape and size,
Maternal factors such as stress, fatigue, anxiety affect the pattern of contraction.
Due to scar formation from previous surgery such as caesarean section or myomectomy.
Medication: Due to overuse of uterotonic and other medications.
Due to fitus malposition: which affects labor progress.
Fetal Position: The mal presentation of the fit affects the labor process.
Due to multiple gestation.
Symptoms and signs:
Irregular uterine contractions,
Ineffective labor progression,
Prolonged labour,
Fital Distress,
Maternal discomfort,
Increased uterine tone,
Labor progress is a failure.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Cervical Examination,
Fetal heart rate monitoring,
ultrasound,
Pelvic Examination,
laboratory test,
Bisop Score Assessment.
Management:
To provide proper position to the mother.
Careful evaluation of mother’s condition.
Properly assess whether the patient is in labor.
Properly assess whether there is a condition of cephalopelvic disproportion or malpresentation through abdominal and pelvic examination.
Catheterization properly to empty the bladder.
Properly start the patient on an I.V. line to maintain hydration.
Provide intramuscularly (I.M.) pethidine to relieve the patient’s pain.
Perform artificial rupture of membranes (ARM) to increase contractions and start drip of oxytocin.
If uterine contractions do not increase even after starting oxytocin drip, caesarean section is preferred.
Cesarean section is planned in following cases like contracted pelvis, mal presentation and condition of fetal and maternal distress.
Increasing the moral support of the patient in vaginal delivery and changing the posture of the patient including avoiding supine position and giving advice to the mother to empty the bladder properly and if unable to empty then doing catheterization and providing intravenous fluid and analgesics to the woman. to provide
Continuous monitoring of fetal heart sound (FHS).
Continuous monitoring of mother’s condition.
Properly assess the condition of mother and baby after delivery.
To provide proper reassurance to mother after delivery.
Providing proper work and quiet environment to the mother and giving advice to take proper rest.
Types of uncoordinated uterine contractions:
There are following types of uncoordinated uterine contractions viz.
1) Spastic lower segment,
2) Constriction ring or contraction ring or Schroeder’s ring,
3) Cervical dystocia,
4) Generalized tonic contraction or uterine tetany,
5)Tonic uterine contraction and retraction or Bendle’s ring.
- Spastic lower segment:
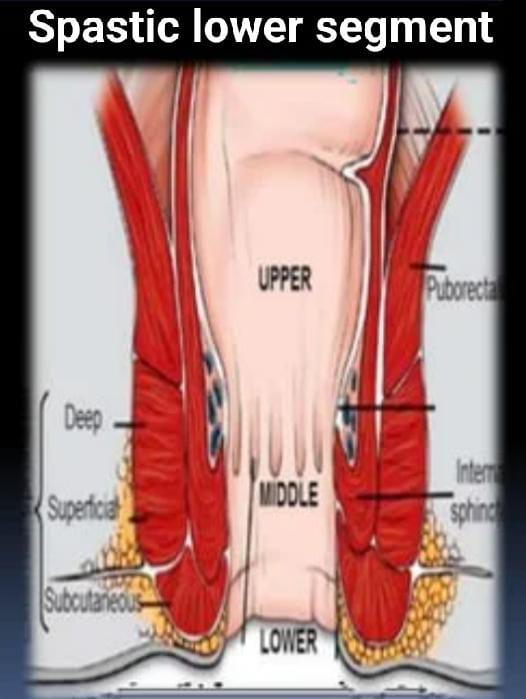
Spastic lower segment of uncoordinated uterine contractions In this type the fundal domains are reduced and reverse polarity occurs. Pacemaker does not work in proper rhythm and contraction of lower segment becomes strong. There is inadequate relaxation between the two contractions. And basal tone is raised above 20 mm Hg. Also fetal distress occurs.
Characteristic of spastic lower segment:
1) Fundal Domains: If less,
2) Polarity: Reversed,
3) Between two contractions: inadequate relaxation,
4) Basal tone is: Raised above 20 mm Hg.
Etiology:
Uterine Muscle Fatigue: Spasm may occur due to prolonged and excessive contractions.
Maternal Factor: Conditions such as dehydration, electrolyte imbalance and fatigue.
Fetal factor: Large fetal size or abnormal presentation can increase the pressure.
Pelvic Abnormalities: Abnormalities or contractures of the pelvis may increase the pressure.
Hormonal influences: An imbalance of oxytocin and other hormones can affect uterine tone.
Psychological factor: Muscle tension can increase due to stress and anxiety.
Symptoms and signs:
There is excruciating pain that is referred to the back.
Dehydration due to fatigue.
Bladder distended due to retention of urine.
Stomach and bowel are distended.
Excessive hardening of the uterine cavity in the abdomen with prolonged pain before uterine contractions.
Even after the contractions have passed, the uterus becomes tender and tense.
The vital parts become difficult to palpate.
The cervix is thickened and oedematous and hangs like a membrane.
There can be varying degrees of caput sucedaneum.
The cervix cannot dilate appropriately.
Risk is seen in fetuses due to imperfect relaxation between contractions. And distress can also occur due to placental insufficiency.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Diagnosis is usually based on clinical signs and symptoms.
The patient has excruciating pain which may also involve the back.
There is also evidence of ketoacidosis and dehydration.
The bladder is frequently distended, there is retention of urine and the stomach is distended and the bowel is visible.
Bear down is attempted prematurely.
Palpating the abdomen:
Uterus is tender filled,
Gentle manipulation stimulates the hardening of the uterine cavity with pain which further initiates uterine contractions.
It becomes difficult to palpate the fetal parts.
Fetal distress appears early.
On internal examination: Cervix that is thick, oedematous, hangs loosely like a curtain and does not apply well to the presenting part.
Inappropriate dilation of the cervix occurs.
Abscesses of membrane are seen.
Meconium may be stained liquor.
Management:
Careful evaluation of the mother to provide proper treatment to the patient.
Start the patient on an intravenous line. Then correct the patient’s condition of dehydration and ketoacidosis by rapid infusion of Ringer lactate (RL) solution.
If the patient has a pain condition, provide medication as per the prescription.
Properly assess the general condition of mother and fetus.
Continuous monitoring of fetal heart rate (FHR) and immediate reporting of any changes.
To provide proper psychological support to women.
If there are conditions like malpresentation, contracted pelvis, maternal distress, fetal distress, etc., then inform the patient to undergo urgent caesarean section.
Rapid 5% dextrose infusion to correct mother’s condition of dehydration and ketoacidosis before caesarean section.
In a conservative approach,
Advise the mother to take adequate rest.
Cidet her with Inj as Inj. Pethidine 100 mg + Inj. Aspirin 50 mg I/M.
Provide epidural analgesia if preferable.
Properly maintain the mother’s nutritional status by 5% dextrose drip.
Careful watching of fits.
Avoid oxytocin drip.
Provide proper psychological support to women and properly record and report.
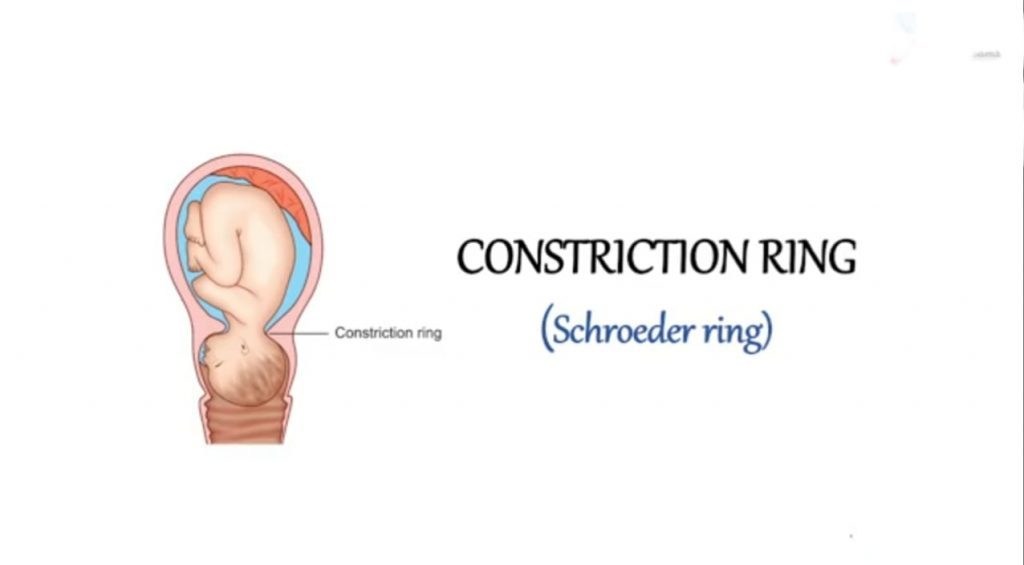
- Constriction Ring or Contraction Ring or Schroeder’s Ring:
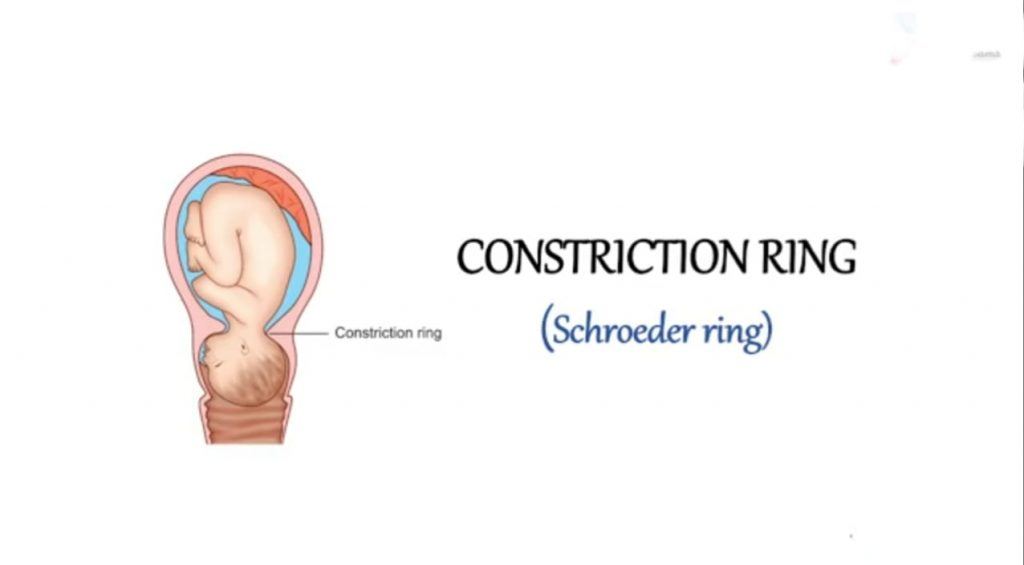
A constriction ring is a form of uncoordinated uterine action where the formation of a constriction ring occurs during the 1st, 2nd and 3rd stages of labor due to localized spasm of the uterine muscles and at the junction of the upper and lower parts of the uterus. Circular muscle fibers of the uterus Localized spastic contractions of the ring occur. A constriction ring is situated around the constricted part of the fitus at the junction of the upper and lower part of the uterus, as seen in the part of the neck in a vertex presentation.
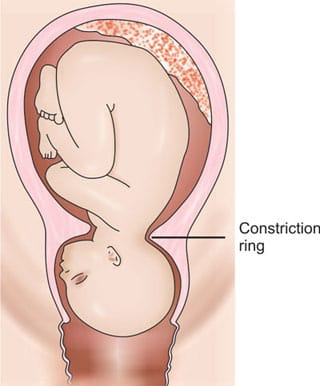
Location of Ring:
The constriction ring is above the constricted part of the fitus around the junction of the upper and lower segments of the uterus and around the neck in a cephalic presentation.
It can be seen in all stages of labor.
It is usually reversible and complete.
Etiology:
The exact cause is unknown.
But in associated etiology,
malpresentation,
malposition,
Due to rough and repeated intrauterine manipulation,
Due to improper use of uterine stimulants such as oxytocin infusion.
Due to pre-mature rupture of membranes.
Due to premature attempt at instrumental delivery under light anesthesia.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Ring contractions often precede a colicky uterus and the patient is usually a primigravida.
It is diagnosed by vaginal examination and filling with a hand inserted inside the uterine cavity.
It is suspected when the 2nd stage lasts for a long time without any reason.
In the 3rd stage, it can cause uterine contractions with retained placenta and postpartum hemorrhage.
The ring does not fill above the abdomen and the fit is at risk due to the hypertonic state but the uterus does not rupture. is
Management:
Properly assess whether the child has any condition of malpresentation and malposition or disproportion.
Provide the patient with an analgesic such as pethidine and an antispasmodic such as hyoscine.
Treatment usually depends on the stage of labor.
1st Stage:
In 1st stage, C.S. after opening the uterine cavity. Meanwhile the diagnosis is made. Therefore, the ring may have to be cut vertically to deliver the baby.
2nd Stage:
Failure to deliver the head despite correct and judicious application of forceps during the second stage of labor raises suspicion of constriction ring.
Conformation is done by palpating the ring after removing the forceps blade.
In this stage also, caesarean section is done. Otherwise forceps are reapplied.
After applying forceps, 0.5 ml of 1 in 1000 adrenaline hydrochloride is given subcutaneously.
Alternatively, 2 capsules of amyl nitrate are broken open and inhaled.
If any of these measures fail to relax the ring, general anesthesia may be provided to the patient to complete the forceps delivery.
3rd Stage:
Diagnosis is made during attempted manual removal.
A dip in anesthesia plan is usually effective.
Alternatively adrenaline/amyl nitrate may be given.
- Cervical Dystocia:
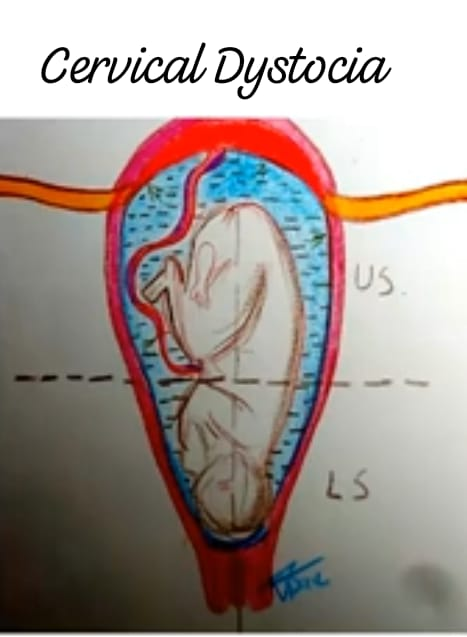
Cervical dystocia is a condition where strong, regular uterine contractions are present but there is failure to dilate the cervix in a proper and reasonable time which may lead to difficulty in the labor process, a condition called cervical dystocia. Inefficient uterine contractions, malpresentation. , malposition, and spasm in the cervix that does not progress properly in cervical dilatation is called cervical dystocia.
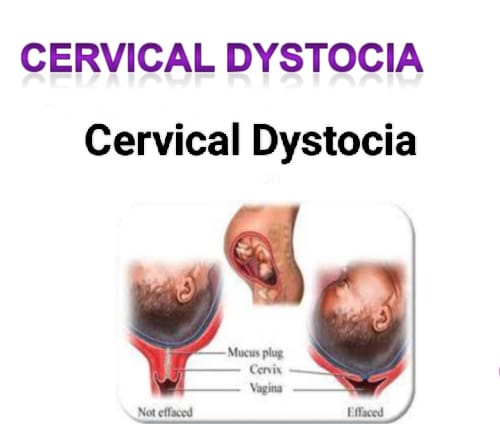
Types of Cervical Distention:
Generally there are two types of cervical dystocia namely,
1) Primary cervical dystocia,
2) Secondary cervical dystocia.
1) Primary cervical dystocia: Primary cervical dystocia usually occurs at the time of first child birth in which the normal pattern of uterine contractions is maintained but the external orifice fails to dilate.
In primary cervical dystocia,
The cervix is very thin and the head can be properly applied.
Initially uterine contractions are good but ultimately they become ineffective.
Occurs in the heel in the anterior leap.
In this, delivery can be accomplished by avulsion of the anterior leap or by annular detachment of the cervix.
2) Secondary Cervical Dystocia: Secondary cervical dystocia is usually caused by scarring or rigidity of the cervix as a result of previous operation or delivery, cervical cancer.
Symptoms and Signs:
Prolonged labour,
Failure of cervical dilatation despite good uterine contractions,
Ineffective uterine contractions,
Abnormal fetal positioning,
Maternal discomfort such as pain and increased pressure in the pelvis.
Getting fital distress.
Diagnostic Evaluation:
History Collection,
Physical Examination,
pelvic examination,
fital monitoring,
ultrasound,
laboratory test,
Beesops Score Assessment.
Treatment:
If there are complications with cervical dystocia, cesarean section is performed.
If the head is low down and the thin rim is behind the cervix, manually ventos the rim and move it up during contractions or traction, or if the cervix is thin but half dilated, place the Duhrsense incision in the 2 and 10 o’clock positions with forceps or Perform ventos extraction.
If the cervix is stenosed due to fibrosis and fails to dilate properly in a reasonable time and vaginal delivery fails, caesarean section is performed.
Cesarean section is the preferred method if there is obstruction of the cervix.
Provide analgesic like pethidine and anti spasmodic like hyoscine medication to the patient.
If the cervix is not properly dilated and there is a condition of fetal distress and the fetal head is not properly engaged, a cesarean section is performed.
- Generalized tonic contraction or uterine tetany:
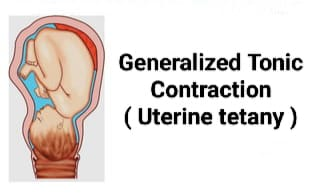
Generalized tonic contractions refers to uterine tetany characterized by prolonged (prolonged) uterine contractions. In this condition, there is retraction of the entire uterine cavity to the level of the internal os.
There is no physiological differentiation between active upper uterine segment and passive lower uterine segment.
When uterine contractions cease, the entire uterus undergoes a muscular spasm (tonic) holding the fetus inside the uterine cavity.
Uterine tetany causes active retention of the fetus.
Etiology:
Due to failure of powerful contractions of uterus to remove obstructions.
Because of irritation caused by repeated unsuccessful attempts at artificial delivery.
Due to improper use of oxytocin drugs.
Symptoms and signs:
Severe and continuous pain.
Uterine becomes tense, hard and small in size.
Fatal patches do not feel properly.
A fetal heart sound is not audible.
A head is observed during vaginal examination.
Vaginal discharge is edematous.
Dehydration and ketoacidosis occur.
On abdominal examination, the uterus is smaller in size, tense and tender.
F.H.S. not to be audible.
Vaginal Examination:
Vajaina becomes dry and oedematous.
Nursing Management:
Correct dehydration and correct ketoacidosis by I.v.infusion of the patient.
Provide antibiotics to control infection.
Provide sedatives to relieve pain.
If obstructions are suspected, a cesarean section is performed.
Provide the patient with deep sedation and intramuscularly morphine A 15 mg or pethidine drip. ie 200 mg in 500 ml 5% dextrose at a drop rate of 50-60 minutes to provide.
Advise the patient to take adequate rest.
The patient is given rest, when spontaneous delivery is possible or if there are no obstructions, spontaneous delivery is performed.
- Tonic Uterine Contractions and Retraction or Bendles Ring:
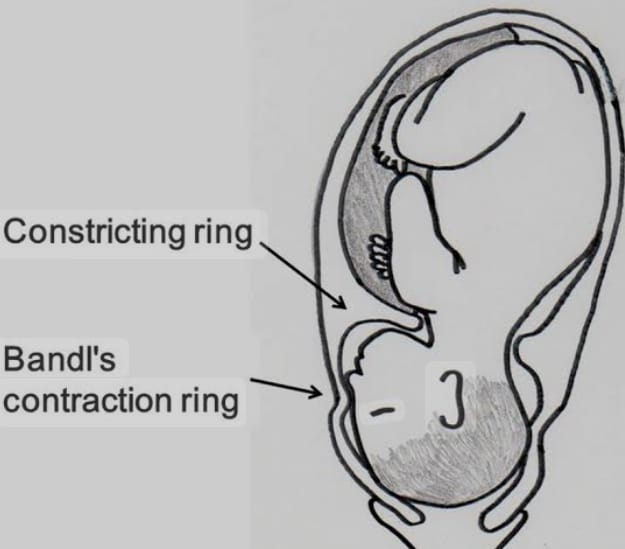
Bandle’s ring is commonly applied to the retraction ring that is usually visible above the abdomen. Bandle’s ring may cause uterine contractions due to obstructed labor. This is a transverse groove (depressed ridge) that usually occurs between the umbilicus and symphysis pubis, usually corresponding to the upper uterine segment and lower uterine segment, which is usually visible above the abdomen. The condition of obstructed labor and difficult labor can arise. Bendle’s ring is usually an abnormal junction between two segments of the uterus. It is usually called a late sign of obstructed labor.
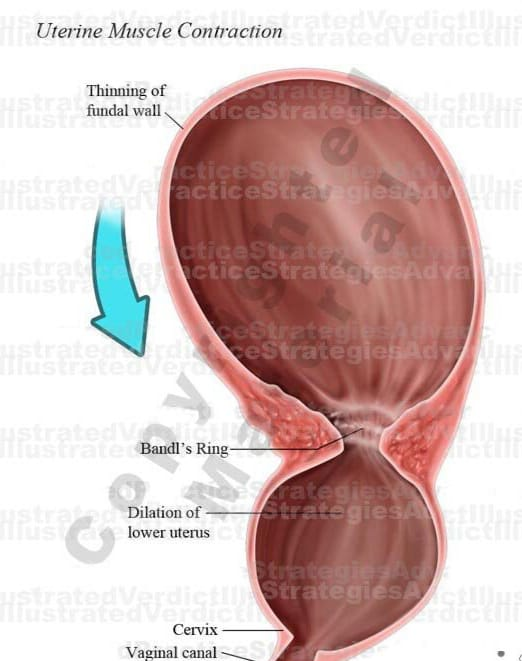
How Ring Formation Takes Place:
There is a gradual increase in the intensity, duration and frequency of uterine contractions.
In it the relaxation phase is reduced and ultimately a state of tonic contraction develops.
Retraction is usually continuous in it.
In the 1st stage the already thinned lower segment is lengthened by circumferential dilatation and progressively thinned to accommodate the fitus driven from the upper segment.
A circular groove is formed in the uterus between the active upper segment and the distended lower segment, which is called the pathological retraction ring (Bendle’s ring).
In primigravida, further retraction in response to obstruction ceases and labor stabilizes as the uterus exhausts.
In multipara, uterine retraction is continuously initiated with progressive circumferential dilatation and thinning of the lower segment.
The bundles ring moves closer and closer to the umbilicus and eventually the lower segment ruptures.
Pathophysiology: There is a gradual increase in the intensity, duration and frequency of uterine contractions, the relaxation phase diminishes and finally tonic contractions occur, although retraction remains as the lower segment lengthens and thins to accommodate the fits from the upper segment Therefore, a circular groove is formed around the uterus between the active upper segment and the distended lower segment, which is called a pathological retraction ring or Bendle’s ring. If it increases, the fetus is put in a life-threatening condition and sometimes death can also occur.
Further retraction in primi gravida causes labor to stop due to obstruction and uterine expulsion and then contractions start again whereas in multipara retraction is continuous with progressive lower segment dilatation and thinning hence Bandel’s ring of umbilicus. It gets closer and finally the lower segment is ruptured
Symptoms and signs:
The patient is restless due to continuous pain and discomfort,
A patient may see an exhaust,
Features of ketoacidosis are also seen with it.
Hypertonic contractions are observed and maternal pulse and temperature are increased.
Abdominal palpation: Upper segment is hard and tender and lower segment is distended and tender and fetal heart sound (FHS) is mostly absent.
Vital parts cannot be properly defined.
Vaginal Examination: The lower segment is compressed due to the force of the presenting part, the ring is not felt and features of obstructed labor are present, but the vagina is dry, hot and has offensive discharge, full dilatation of the cervix and membranes. Absence is observed.
Diagnostic Evaluation:
History Collection,
Physical Examination,
ultrasound,
fital monitoring,
pelvic examination,
Cardiotocography (CTG),
blood test,
Rarely, M.R.I. is used to identify anatomical abnormalities.
Management:
Supportive therapy:
It usually involves inj.morphine 15 mg I.M. provided.
A 5% dextrose drip is started.
Inj. Ampicillin 500 mg I/M is given.
Treatment of keto-acidosis is by I/V infusion of 5% dextrose and Ringer’s lactate solution.
Definitive Treatment:
Rule out the presence of uterine rupture.
If there is any kind of obstruction, relieve the obstruction in such a way as to cause minimum hazards to the mother.
Do not attempt delivery if the fetus is dead or in a dead condition.
Never do an internal version.
Routine exploration of the uterus after vaginal delivery can identify the cause of rupture.
Cesarean section is indicated in certain conditions.
Correct the condition of dehydration and ketoacidosis by infusing the patient with Ringer lactate solution.
If the patient is in pain, provide proper pain reliever/analgesic medication to relieve his pain condition.
Provide proper antibiotic medication to the patient.
Prevention: Partographical management of labor with early diagnosis for malpresentation, cephalopelvic disproportion and caesarean section.
- Difference between Constriction Ring / Contraction Ring and Retraction Ring / Bendles Ring:
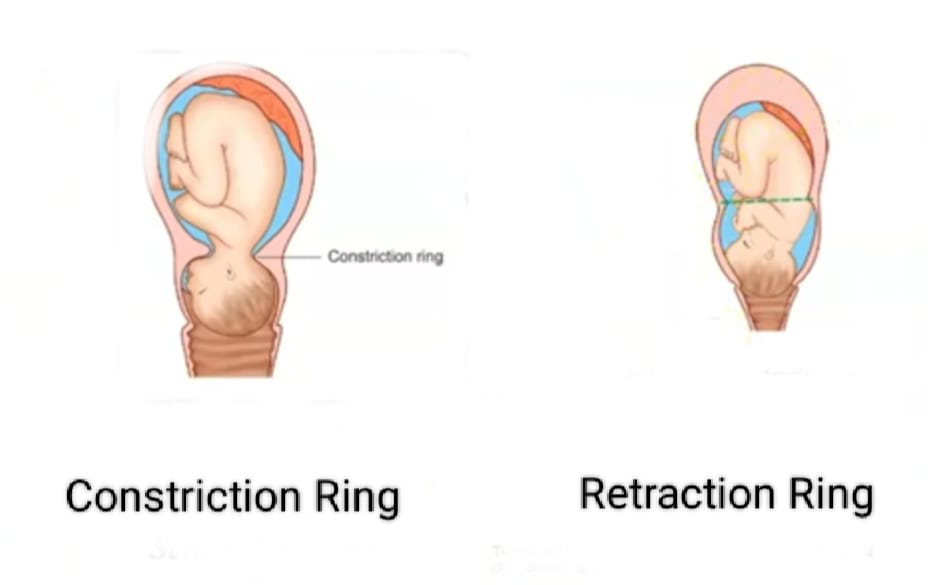
Constriction Ring/ Contraction Ring:
- Nature: Constriction ring is caused by localized incoordinate uterine contractions.
- Cause: Irritability occurs in the uterus.
- Situation: Any place but mostly above and after the junction of upper and lower segment does not change position.
4.Uterus: Abnormal polarity is seen.
- Abdominal Examination:
Uterus: Normal,
F.H.S.: Present,
Fittal part: Palpate with tenderness,
Ring: Does not fill.
Round Ligament: Does not fill.
6.Vaginal examination: Lower segment is not compressed from the presenting part.
The ring fills the head.
Features of obstructed labor are absent.
7.Result: Maternal exhaustion and fetal anoxia are late features and uterus does not rupture.
8.Treatment: Relax the ring and deliver or if necessary cesarean delivery, then cut the ring.
Retraction Ring/ Bendles Ring:
- Nature Retraction ring is the end result of tonic uterine contractions and retraction.
2.Causes: Obstructed labor occurs.
3.Situation: Always above the junction of upper and lobar segments then gradually moves upwards.
- Uterus: Normal polarity is seen.
- Abdominal Examination:
Uterus: Tense and tender.
F.H.S.: Mostly absent.
Fetal part: Not easily palpated.
Ring: Groove has a rough feel.
Roundligament: is tough and tender.
Vaginal examination: The lower segment is compressed from the presenting part.
The ring is not vaginally felt.
Features of costructured labor are present.
Results: Maternal exhaustion, sepsis, fetal anoxia are observed. The uterus usually ruptures in multigravida.
Treatment: Cesarean delivery if there is no ruptured uterus.
- Premature Rupture of Membranes (PROM):

If the membranes spontaneously rupture at any time after the 28th week of pregnancy, but before the onset of labor, the condition is called premature rupture of membranes (PROM).
When the membranes rupture after 37 weeks but before the onset of labor it is called term PROM.
If it occurs before 37 wk is completed, it is called preterm (PROM). And when the membranes rupture more than 24 hours before delivery, it is called prolonged rupture of membranes.
It is associated with cervical incompetence, pathogenicity of the vaginal canal and chorioamnionitis.

If the membranes spontaneously rupture at any time after the 28th week of pregnancy, but before the onset of labor, the condition is called premature rupture of membranes (PROM).
When the membranes rupture after 37 weeks but before the onset of labor it is called term PROM.
If it occurs before 37 wk is completed, it is called preterm (PROM). And when the membranes rupture more than 24 hours before delivery, it is called prolonged rupture of membranes.
It is associated with cervical incompetence, pathogenicity of the vaginal canal and chorioamnionitis.
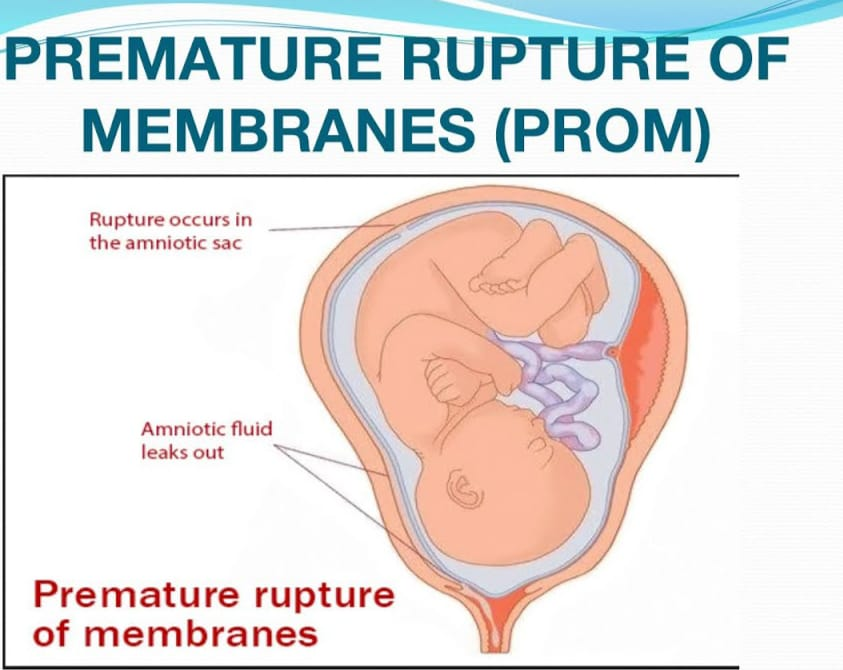
Etiology:
Its exit cell is unknown,
Possible causes include membrane friability,
Low tensile strength,
polyhydroamnios,
Cervical incompetence,
multiple pregnancy,
infection,
Short cervical length,
Low BMI,
Having a history of pre-term labor,
polyhydroamnios,
multiple pregnancy,
Due to fragile membrane,
Due to infections such as urinary tract infections and lower genital tract infections,
Symptoms and Signs:
Vaginal discharge:
Watery discharge escaping from the vaginal canal.
A sudden release of amniotic fluid, often described as a “gush” or continuous leak.
Contraction: Regular uterine contractions occur.
Vital monitoring: Changes in heart rate.
Infection-like symptoms such as,
fever,
Increase in heart rate,
Foul smelling amniotic fluid,
Cervical changes: such as cervical dilatation and effacement on examination.
Risk of Premature Rupture of Membrane:
preterm labor,
Systemic infection in mother and newborn baby,
Oligohydroamnios can usually be caused by fetal problems such as pulmonary hypoplasia.
cord prolapse,
Goods presentation due to prematurity,
Antepartum haemorrhage,
Psychological trauma in mother due to long-term hospitalization.
Diagnostic Evaluation:
History Collection,
Physical Examination,
speculum examination,
Watery discharge from vagina,
On examination of the fluid, PH >6,
Ultrasonography.
complete blood count,
urinalysis,
High vaginal swab for culture,
Ultrasonography.
Management:
First perform a speculum examination with aseptic precautions. Also check for cord prolapse and color of amniotic fluid along with diagnosis.
Do not perform vaginal examination.
Give proper bed rest to the patient.Provide sterile vulval pad.
Danger:
Start labor due to premature rupture of membranes.
There are high chances of ascending infection.
The incidence of cord prolapse is high.
A condition of dry labor is observed due to continuous escape of liquor.
Fetal pulmonary hypoplasia is a threat and is associated with oligohydroamnios.
Nursing Management:
To transfer the patient to the proper hospital.
To collect complete history of the patient.
Advise the patient to take proper bed rest.
Obstetrics examination with proper care and precautions.
Perform proper vaginal examination by maintaining sterile technique.
Proper observation of cervical dilatation and effacement.
Intracervical swab is taken for gram stain, culture and sensitivity test of bacteria.
Abdominal amniocentesis is performed under ultrasonic guidance and then a sample of liquid amnio is collected for bacterial culture and sensitivity test.
Fetal monitoring is done every 6 hours.
Vital signs of the patient are checked every four hours, especially pulse and temperature are monitored.
Antibiotics such as ampicillin 500 mg or a cephalosporin
500 mg given 6 hourly x for 6 days. Alternatively, erythromycin therapy is given and metronidazole is used continuously for 1 week.
After confirmation of the diagnosis, management is usually based on the following factors such as,
gestational age,
Whether women are in labour,
Any sepsis,
and fetal survival rate, etc.
Term PROM: Spontaneous labor starts within 24 hours of rupture in 90% of cases and during that time assess for infection and provide care if labor has not started, induction and cesarean section in complications.
Preterm PROM: Transfer the patient to a well equipped hospital if fit in utero due to risk of prematurity.
If the pregnancy is 34 weeks or more and labor does not start within 48 hours, cesarean section is performed in induction and obstetric complications.
Conservative treatment is provided if the pregnancy is less than 34 weeks and there are no maternal or fetal indications.
Proper antibiotic and steroid medication is given to the patient.
- Precipitate Labour:
Precipitate labor is called “rapid labor” and “rapid childbirth”. Precipitate labor means abnormal rapid labor in which the total duration of the first and second stages of labor is less than two hours. This leads to rapid and spontaneous expulsion of the infant. It is commonly seen in multipara women. With multipara there is a relaxed pelvic or perineal floor, with multipara there are usually strong, forceful contractions and there is no painful sensation during labour, so immediate birth. is not reported leading to precipitated labour.
Etiology:
Uterine hypertonicity,
multiparity,
Abnormal fetal presentation,
Favorable pelvic structure,
hormonal factors,
Due to premature rapid labour,
Risk of Premature Rupture of Membrane:
Maternal Risk: In which,
Extensive lacerations of cervix, vagina and perineum.
P.P.H (Post Partum Haemorrhage).
inversion,
infection.
Fatal Risks:
intracranial stress,
hemorrhage,
Serious injury to baby.
Bleeding from the cord.
A direct blow to the skull may occur.
Management:
If the patient has a prior history of precipitated labor then admit to the hospital first.
Reduction of uterine contractions during labor by magnesium sulfate.
Do not perform oxytocin augmentation.
Low Rupture of Membrane for Elective Induction Labour.
Provide libral episiotomy and control delivery of the head.
Nursing Management:
The first step is to immediately assess the situation of precipitated delivery as soon as the patient arrives in the labor room.
Call for other help and do not leave the patient alone.
Preparing a sterile obstetrics or precipitate delivery pack for delivery.
Providing condition information and psychological support to the patient.
Perform libral episiotomy and control delivery of the head.
Checking for the umbilical cord around the neck.
If the cord is loose, remove the hook and clamp the tight cord twice and make a cut between the two clamps. After that, the controlled delivery of solder should be done.
Provide comfortable position to the mother after delivery. Check the fundus every 10-15 minutes in the first hour to extend the leg and massage if the fundus is soft or boggy.
To record the delivery and examination of the placenta. To record the condition of the mother and the baby and to inform the obstetrician of any abnormalities and take measures for their treatment.
- Prolonged Labour:
When the combined duration of the first and second stages of labor is more than 18 hours, it is called prolonged labor. Cervical dilatation rate <1 cm/hr and descent of the presenting part <1 cm/hr in at least four hours of observation. It is called prolonged labor.
Etiology:
Fault in Power:
Abnormal uterine contractions like,
uterine inertia,
Can’t down a beer,
epidural analgesia,
Constriction ring.
Fault in Passage:
contracted pelvis,
cervical dystocia,
pelvic tumor,
Due to full bladder and rectum,
Cephalo Pelvic Disproportion,
android pelvis,
Spasm of the pelvic floor or perineum or resistance due to old scars.
Passenger:
malposition,
malpresentation,
big baby,
Congenital Anomalies of Fetus,
big baby,
Deflex head.
Other Causes: Due to early administration of analgesics and sedatives
Symptoms and signs:
Duration of labor should be extended.
Week and inadequate uterine contractions.
Delayed cervical dilatation.
Changes in fetal heart rate (FHR).
Maternal fatigue and exhaustion.
Pain and discomfort due to prolonged pressure on pelvic tissues.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Prolonged labor is not diagnostic but indicative of an abnormality. Abdominal examination and vaginal examination are done to identify it.
Partographic analysis is done to diagnose it, i.e. if the rate of cervical dilatation is less than 1 cm/hour in nulliparous and less than 1.5 cm/hour in multiparous, it is considered abnormal.
The head slowly descends down.
pelvic assessment,
radiography,
CT scan,
M.R.I. Intranatal imaging by.
Second stage is prolonged when it lasts more than 2 hours in primigravida and more than 1 hour in multigravida.
Danger:
Fetal Danger:
hypoxia,
intrauterine infection,
Intracranial stress/hemorrhage,
Increasing incidence of operative delivery,
Maternal Danger:
distress,
Post partum haemorrhage,
trauma to genital tract,
Increasing incidence of operative delivery,
Peripheral sepsis,
Subinvolution.
Management:
To identify the cause of prolonged labor and its effect on mother and fetus.
First stage delay: Identify the presentation, position and station of the fetus by doing vaginal examination.
If uterine activity is low, perform amniotomy, oxytocin infusion and provide analgesia.
Cesarean section is performed in conditions of malpresentation, malposition, big baby and cephalopelvic disproportion.
Second Stage Delay: If Fetal Heart Sound (FHS) is good then expectant management and vaginal delivery or assisted or cesarean delivery may be performed via vaginal (forceps, ventos) or cesarean delivery.
Nursing Management:
To provide proper psychological support to the mother.
Early identification of factors for prolonged labor and early detection and proper treatment.
Properly maintain the partograph. Due to which it can identify the condition of prolonged labor early.
If prescribed, provide proper sedation to the mother so that she can rest properly.
To properly maintain the nutritional status of the mother.
Give the mother properly intravenously such as Ringer’s lactate (RL).
Provide solutions to maintain his hydration status and treat the condition of ketoacidosis.
Properly maintaining patient’s vital signs like blood pressure and pulse etc.
A urine test is done to identify if acetone is present in the urine.
Properly check and record labor progress, orifice dilatation, vital signs specially blood pressure, and skin color.
- Induction of Labour:
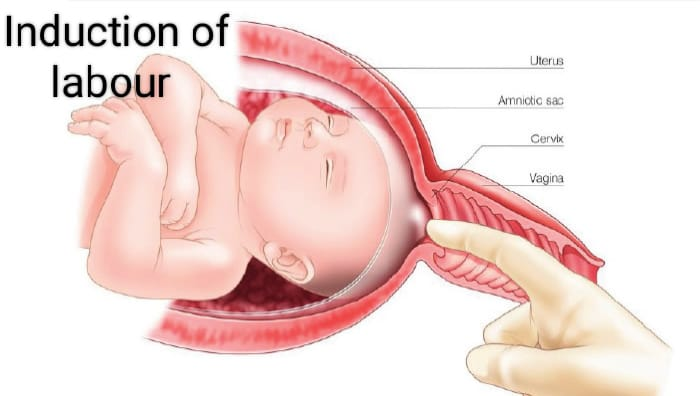
Induction of labor i.e. artificial initiation of uterine contractions after the period of viability of fits and before the spontaneous labor process starts, usually in which uterine contractions are initiated for vaginal delivery by medical, surgical or a combination of both methods. It is called induction of labor.
Purpose of Induction of Labour:
Induction is done when continuation of the pregnancy may pose a risk to the health of the mother or the fetus. So in cases of safety of both, induction is indicated.
Indications of Induction of Labour:
There is a need for induction of labor when there is any deviation in the normal physiological process of child birth.
Maternal Indication:
Prolonged pregnancy,
Pre-eclampsia and Eclampsia,
Maternal medical complications like diabetes mellitus, chronic renal failure, cardiac disease, hypertension, cholestasis, postmaturity, intrauterine death,
intrauterine growth retardation,
APH specifically abruptio placenta,
Polyhydroamnios associated with maternal distress,
oligohydroamnios,
Having a prior history of intrauterine death,
Premature Rupture of Membrane,
Due to congenital malformations in Fitus.
Fital indication:
Intrauterine growth retardation (IUGR) due to chronic placental insufficiency,
Intrauterine fetal death,
Rh-isoimmunization,
unstable lie,
Due to congenital malformation of the fetus.
Contraindications:
contracted pelvis,
Cephalopelvic Disproportion (CPD),
malpresentation,
Prior classical caesarean section or hysterotomy,
vaginal bleeding,
Waza Privya,
placenta previa,
Active genital herpes infection,
High risk pregnancy, heart disease, pelvic tumor,
Obstetrics and medical complications with elderly primigravida,
Umbilical cord prolapse,
or cord presentation,
In cervical carcinoma,
HIV-positive women who are not receiving highly active antiretroviral therapy
In cervical carcinomas.
Risks due to induction of labour:
Mother:
psychological upset,
Tendency of prolonged labour,
The need for analgesics increases,
operative interference,
Morbidity.
Fits:
Iatrogenic prematurity,
hypoxia,
uterine dysfunction,
Protong Labor,
Operative Delivery.
Method of Induction of Labour:
- Medical,
2.Surgical, - Combined.
Medical:
Prostaglandins PGE2 (prostaglandin), PGE1 (mizostol), oxytocin or mifepristone are used for medical induction.
Prostaglandins for medical induction (PGE2): act locally on contiguous cells, thereby causing biomaterial contractions. But (PGE2) survival ripening while PGF2 is responsible for myometrial contractions. PGE2 dinoprostone intracervical application is used for cervical ripening. It is repeated after 6 hours, 3 to 4 doses can be given if needed. After the application, the patient should stay in bed for 30 minutes and monitor her uterine activity and fetal heart rate.
Misoprostol (PGE1): Currently used transvaginally or orally. 25 mg vaginally every four hours is used for cervical ripening and labor induction. A total of 6-8 doses can be given.
Oxytocin: Endogenous is uterotonic. It stimulates uterine contractions. It is given as an intravenous infusion when the cervix is ripe.
Mifepristone: It is a progesterone receptor antagonist and blocks progesterone and glucocorticoid receptors. Used vaginally for cervical ripening and labor induction.
Surgical induction:
1) Artificial Rupture of Membrane (ARM),
2) Stripping the membrane
Low Rupture of Membrane (LRM):
Procedure: A small amount of amniotic fluid is drained by rupturing the membrane below the presenting part and above the internal os. It is performed in the labor room or operation theater with full aseptic precautions followed by emptying of the bladder and lithotomy position with long couture forceps or amnion hook followed by placement of a sterile vulval pad and administration of antibiotics. After membrane rupture, amniotic fluid should be assessed for color, station of cervix, cord prolapse and fetal heart rate.
Indications: Anti-partum haemorrhage (APH),
Hydroamnios, severe preeclampsia, eclampsia.
Contraindications: Intra-uterine fetal death, maternal AIDS, genital active herpes infection.
Advantages:
Low blood pressure in pre-eclampsia and eclampsia,
Maternal distress is reduced in hydroamnios,
Leakermany can be assessed,
Internal fetal monitoring can be done,
Uterine CVD is assessed,
Blood sample taken from fetal scalp,
Catheter placement to measure intra-uterine pressure,
Bleeding is controlled in ante partum haemorrhage (APH) and
Abruption of the placenta and initiation of labor reduces tension.
Risk: Cord prolapse, excessive amniotic fluid escape, placental abruption, injury amnionitis etc.
Stripping the Membranes: This procedure is useful for cervical re-opening, before ARM and for induction of labour. Digital separation of the chorioamniotic membrane from the wall of the cervix and lower uterine segment is called stripping of the membrane. It causes the release of endogenous prostaglandin A from the membrane and decidua. This method is simple, safe and beneficial in its criteria that the fetal head is applied to the cervix and the cervix should be as dilated as the examiner’s finger can reach.
Mechanical: Dilator
The membrane releases prostaglandins from the decidua for labor induction and survival ripening.
Transcervical balloon catheter (Follis catheter): Extra amniotic saline infusion is performed for cervical repair.
Combined Method: In this method both medical and surgical methods are used. Its advantages include being more effective than a single procedure, shortening the induction-delivery interval, thereby reducing infection, and shortening the observation period.
- Dystocia:
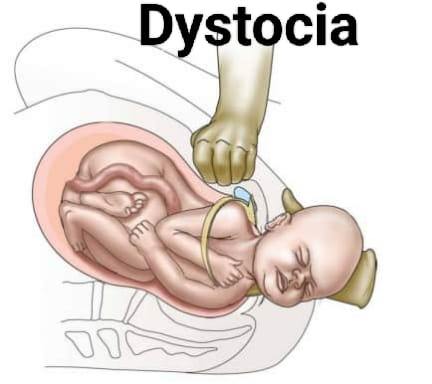
Dystocia is a condition of difficult labor or difficult child birth in which the labor process is slow and progress associated with labor is slow and failure.
The condition of dystocia is usually,
Abnorlity in the passage,
Abnormalities in the passenger,
and due to abnormalities in power and associated with a combination of all these factors.
- Fetal Macrosomia:
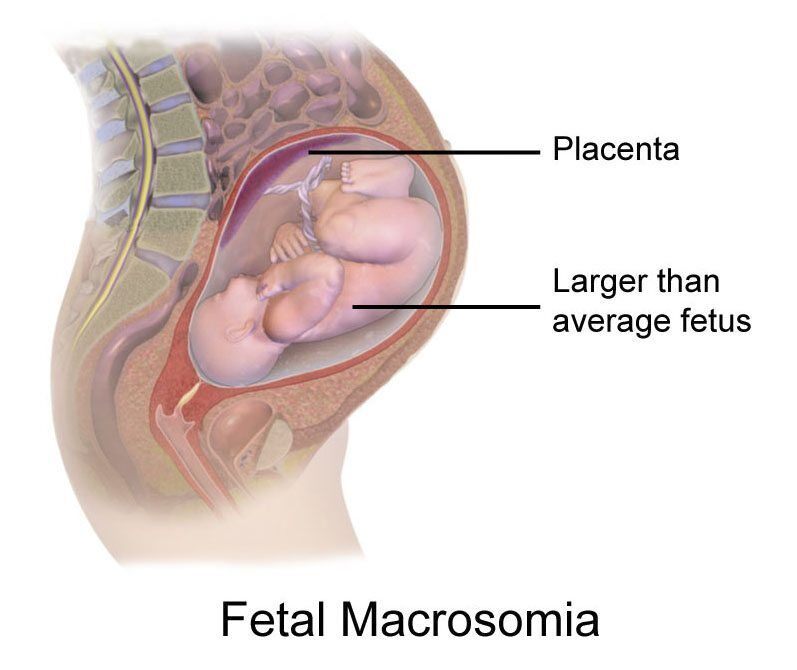
Fetal macrosomia is called generalized fetal enlargement. When the fetal birth-weight is usually 4 kg (4000 gm) and more, the condition is called fetal macrosomia.
Etiology:

hereditary,
Maternal diabetes mellitus,
Gestational Diabetes Mellitus,
obesity,
Size of parents,
postmaturity,
multiparity,
Prolong pregnancy,
maternal age,
Male Fitus.
Symptoms and signs:
Prolonged labour,
Vic and infrequent uterine contractions,
Fital Distress,
maternal fatigue,
Abnormal fetal presentation.
pelvic discomfort,
In cervical swelling and AD.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Pelvic Examination,
ultrasound,
Fetal heart rate monitoring,
amniotomy,
Blood test.
Management:
Monitoring:
Regular assessment of fits and regular monitoring of growth and well-being of fits through ultrasound.
Maternal Management:
Blood Glucose Control: Advise mothers with gestational diabetes to properly maintain their blood glucose levels.
Nutritional Guidance:
Advising the mother to have a balanced diet intake during pregnancy. And giving advice for weight management.
Delivery Planning:
Vaginal delivery: If the fetus is of manageable size and correctly positioned, trial labor is attempted.
Cesarean section:
If the fetus is of a large size, vaginal delivery is impossible, the patient is advised for caesarean section.
Intrapartum monitoring:
Continuous physical monitoring during the intrapartum period to monitor for any signs and symptoms of fitus distress.
Post Partum Care:
Continuously monitoring the condition of the mother and fetus after delivery and properly monitoring for any complications like hypoglycemia in the newborn.
Multidisciplinary Approaches:
Properly collaborate with obstetricians, endocrinologists, nutritionists, and pediatricians for comprehensive care.
- Hydrocephalus:
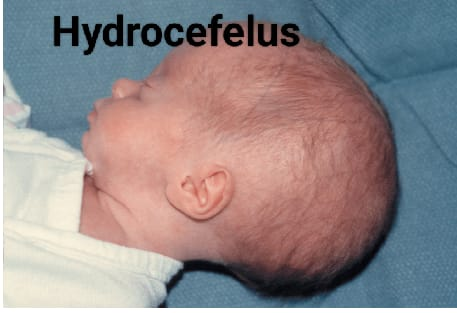
Hydrocephalus is a Greek word consisting of hydro meaning “water” and cephalus meaning “head”. Hydrocephalus is an abnormal condition in which the cerebrospinal
Abnormal accumulation of fluid (CSF) occurs in the ventricular system and subarachnoid space. Due to this, the pressure inside the skull increases. This condition of hydrocephalus usually results from an imbalance in the production and absorption of cerebrospinal fluid due to obstruction in the SCF pathway. Due to this, dilatation of cerebral ventricles, enlargement of head, cognitive impairment, seizures and other neurological problems are seen.
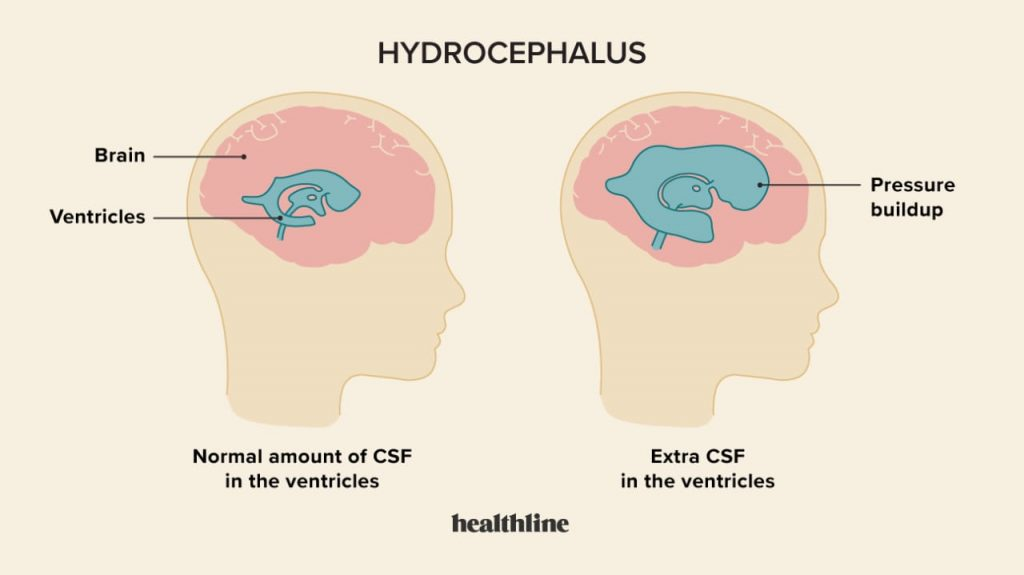
C.S.F pathway
Cerebrospinal fluid is secreted from the choroid plexuses of the ventricles by ultrafiltration and active secretion.
Cerebrospinal fluid from the lateral ventricles passes through the foramina of Monro into the third ventricle.
The cerebrospinal fluid from the third ventricles passes through the cerebral aqueduct (Aqueduct of Salvius) from the ventricles to the fourth ventricles.
The cerebrospinal fluid then passes into the basal cisterns and subarachnoid space through the foramen Luschka and foramen Magendi. Cerebrospinal fluid is absorbed through the venous channel and arachnoid wall in the sinuses. About 20ml of cerebrospinal fluid is secreted in one hour and 500ml / day. The total amount of cerebrospinal fluid is 100 to 150ml.
Etiology:
The condition of hydrocephalus is mainly of two types, congenital hydrocephalus and acquired hydrocephalus.
1) Congenital Hydrocephalus:
Due to infection during intra-uterine life like,
STORCH (syphilis, toxoplasmosis, rubella, cytomegalo virus, herpes virus.),
Caused by a congenital brain tumor that obstructs the flow of cerebrospinal fluid.
Malformation at birth
because of,
Due to intracranial hemorrhage,
Due to stenosis and maldevelopment of the duct,
Arachnoid no
Due to maldevelopment,
Due to displacement of the brain stem and cerebellum from the foramen magnum (Arnoldchiri malformation),
Due to genetic factors.
2) Acquired hydrocephalus:
Due to brain infection like,
Meningitis, encephalitis.
Due to trauma eg, birth trauma, head injury, intracranial haemorrhage.
Neoplasms like, tuberculoma, subdural hematoma and abscess, gliomas, ependymoma, astrocytoma, choroid plexus papilloma, pseudotumor cerebri.
Due to chemicals such as hypervitaminosis A.
Connective tissue disorders such as Hurler syndrome, achondroplasia,
Degenerative Atrophy of Brain,
Arteriovenous malformation, ruptured aneurysm.
3) Communicating hydrocephalus:
Bacterial meningitis,
Malignant Meningitis,
hemorrhage,
Increased venous pressure.
4) Noncommunicating hydrocephalus:
Due to congenital causes,
Due to Acquired Cause.
Types of Hydrocephalus:
There are total four types of hydrocephalus.
1) Congenital hydrocephalus,
2) Acquired hydrocephalus,
3) Communicating hydrocephalus,
4) Noncommunicating hydrocephalus.
1) Congenital Hydrocephalus :
Congenital hydrocephalus is present at birth. And it is usually caused by some environmental factor and genetic factor during fetal development.
2) Acquired hydrocephalus:
Acquired hydrocephalus develops at birth. And even then it develops. Acquired hydrocephalus is caused by any birth injury and birth trauma.
3) Communicating Hydrocephalus:
In communicating hydrocephalus there is no blockage of the ventricular system, basal cisterns, and spinal subarachnoid space. In this communicating hydrocephalus, excessive production of cerebrospinal fluid (CSF) and inadequate absorption of cerebrospinal fluid (CSF) does not occur, resulting in accumulation of fluid in the brain which is responsible for creating hydrocephalus.
4) Noncommunicating hydrocephalus:
This noncommunicating hydrocephalus occurs due to obstruction in any of the ventricular systems (usually the aqueduct, foramen Luschka, and Magendi). The obstruction can be usually partial, intermittent, or even complete. This obstruction usually develops due to inflammation and obstructive lesions. Due to this blockage, the flow of spinal fluid into the brain is impaired. Due to this there is an accumulation of fluid in the brain which creates the condition of hydrocephalus.
Symptoms and signs:
Accumulation of cerebrospinal fluid in the ventricles of the brain.
Excessive enlargement of the head.
To become a sine skull.
Separation of cranial sutures due to head enlargement.
bulging of the fontanelles,
Scalp is singed and vein is dilated.
Percussion of the skull produces a “cracked pot” resonance (Macewen’s sign).
See the sunset sign (sclera visible above the iris).
His face looks small compared to his head.
Increased intracranial pressure.
Having hemiplegia.
Cry is hoarseness.
Often occurring in papilloae.
Spasticity occurs.
Ataxia.
Urinary incontinence.
Progressive deterioration of mental function.
Nozia.
Vomiting.
Restlessness.
Irritability.
Irregular and decreased respiration.
The pulse will decrease.
Having a convulsion.
feeling tired
Stupor and coma.
Head one.
Lethargy.
from the app.
Changes in personality.
Irritability.
Confusion.
Visual problem.
Diagnostic Evaluation:
History Collection,
Physical examination,
Antenatally: sonography
Measuring head circumference.
Cranial ultrasonography.
x ray
CT scan.
M.R.I.
Neurological examination.
Ventriculography.
Pneumoencephalography.
Intracranial pressure monitoring.
Neuropsychological assessment.
Genetic testing.
Intracranial pressure monitoring.
Management:
In breech presentation, the arrested head can be decompressed by perforating the sub-occipital region using a perforator or sharp pointed scissors under the guidance of two fingers of the left hand securing the anterior vaginal wall. Other methods of head decompression are:
Laminectomy in the cervical region to open the spinal canal.
During the procedure the anterior vaginal wall is retracted by two Landens retractors.
Dressing forceps of the uterus or a Drew-Smith catheter are pushed through the open spinal canal into the ventricle to drain fluid (eg open spina bifida).
If the condition of hydrocephalus is mild and stable, then continuous monitoring of the child by healthcare personnel. Continuous monitoring of the child’s head circumference, developmental milestones etc.
If the child has mild symptoms, provide adequate medication to reduce the symptoms.
A carbonic anhydrase inhibitor, acetazolamide (Dymox), is used to reduce the production of CSF.
Oral glycerol and isorbital are used in children to reduce increased intracranial pressure.
If the child has the condition of hydrocephalus due to any obstruction, there is a need for surgical management.
Perform lumbar puncture to maintain cerebrospinal fluid pressure.
The most common method to treat the condition of hydrocephalus is stent placement. such as abdominal VT.)
Endoscopic third ventriculoostomy (ETV) is performed in certain cases such as non-communicating hydrocephalus in which the obstruction leads to hydrocephalus condition.In this procedure, a hole is formed in the third ventricle, which allows cerebrospinal fluid to flow out. Obstruction of the pathway is bypassed and can move into the subarachnoid space where it is absorbed.
Types of shunt procedures:
1) Ventriculoperitoneal shunt: In this procedure, one part of the shunt catheter is inserted into the anterior border of the lateral ventricles in the brain while the other end of the shunt is inserted into the skin of the peritoneal cavity. and pathways of cerebrospinal fluid are diverted from the ventricles into the peritoneal cavity.
2) Ventriculo pleural shunt (VPL): This shunt is similar to the ventriculo peritoneal shunt in that one end of the shunt catheter is inserted into the ventricles and the other end of the shunt catheter is inserted into the pleural cavity (around the lungs). is done. This shunt allows cerebrospinal fluid to flow into the pleural cavity where it is absorbed.
3) Ventriculo atrial shunt: To collect cerebrospinal fluid in a ventriculo atrial shunt, the distal end of the shunt catheter is inserted into one ventricle of the brain and then the other end of the shunt catheter is inserted into the atrium of the heart through the jugular vein. By performing this shunt procedure, the pathway of cerebrospinal fluid is entered into the blood stream where it is absorbed.
4) Long peritoneal shunt: In a long peritoneal shunt, the cerebrospinal fluid is diverted from the lumbar subarachnoid space (lower spine) into the peritoneal cavity. which may lead to absorption of cerebrospinal fluid into the abdominal cavity.
5) Ventriculo ureter shunt:
This type of shunt is usually used in older children when all other types of shunts have failed to divert cerebrospinal fluid from the ventricles to the ureters.
Nursing Management:
Preoperative nursing management
Properly and continuously assess the child including baseline health status, vital signs, neurological status and hydration status of the child.
Continuously monitor the child’s intracranial pressure.
Continuously measure the child’s head circumference.
Palpate the child’s fontanelles to assess for any increased intracranial pressure.
Assess the child’s pupillary response and level of consciousness.
To continuously monitor the child’s vital signs.
To provide proper work and quiet environment to the child.
Maintain aseptic technique while handling the child to prevent nosocomial infection.
Changing the child’s position continuously.
To properly maintain the nutritional status of the child.
Provide proper intravenous fluid to the child.
Keeping the child Nil Per Oral (Nil Per Oral).
Continuously monitor child’s intake output chart.
To properly collaborate with other health care personnel for proper care of the child.
Surgery is a stressful condition for the child and its family members, so proper education and psychological support should be provided to the child’s parents.
To provide proper assurance and emotional support to the parents of the child.
Post operative management:
Monitoring the child continuously and closely after the surgery.
To monitor the child’s vital signs frequently every fifteen to twenty minutes.
Properly monitoring the neurological status of the child.
Monitoring the child frequently if there is an alteration in body temperature.
Position the child at the non-operative site to prevent pressure on the shunt.
After surgery, the child is usually provided with a flat position on the bed for 24 hours.
Assess the child’s photoreceptors to immediately notice if depressed.
If the child is in pain, provide analgesic medication to relieve it.
Do this if the child has any complications after the surgery.
Provide proper fluid to the child and maintain his hydration status. To continuously monitor the intake output chart of the child. And continuously maintain the child’s electrolyte level.
Provide dressing to the child by maintaining proper aseptic technique on the surgical side.
To provide proper support and education to the child and his family members.
- Shoulder Dystocia:

The term shoulder dystocia has been defined to describe a wide range of difficulties encountered in the delivery of the shoulder during labor. In which, during the labor process, the head of the fetus is delivered but due to its shoulder being stuck in the pelvic bone of the mother, difficulty arises in delivery, i.e. the shoulders of the fetus cannot be delivered, then this condition is called shoulder dystocia. is
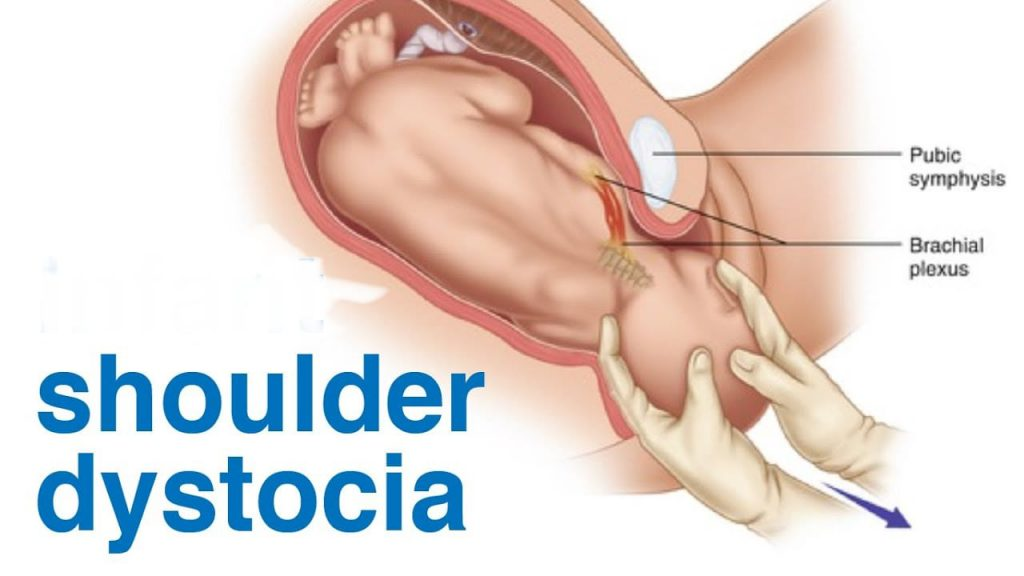
Shoulder dystocia is an emergency in which the child’s shoulder gets stuck behind the mother’s pelvic bone after the head is delivered during birth. Due to this, complications can arise in both the mother and the baby, in which the risk of potential nerve damage or fracture in the child and hemorrhage in the mother can increase.
In Solder’s dystocia, the problem is in the pelvic inlet.
The anterior solder lies above the symphysis pubis.
While the posterior solder lies in the sacral promontory.
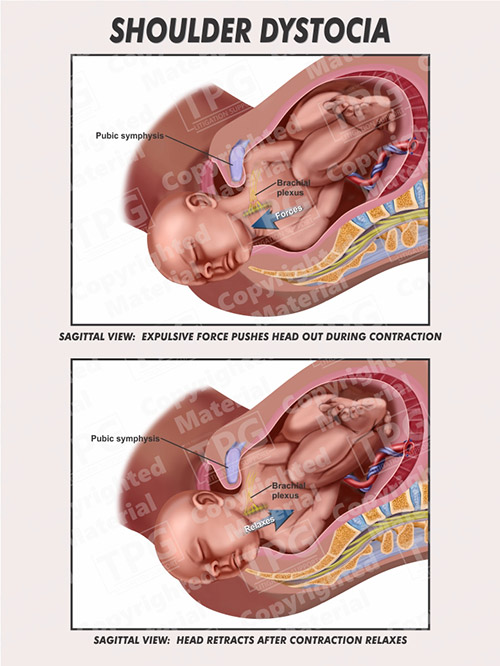
Etiology:
macrosomia,
Abnormal fetal presentation,
Narrow pelvic shape or deformities,
maternal obesity,
Diabetes mellitus, (gestational or pre-existing)
Privus solder dystocia,
rapid labor,
Due to the prolongation of the second stage of labour,
induction of labour,
Assisted delivery (forceps or vacuum extraction).
Predisposing factors:
Fetal macrosomia (fetus weight at birth greater than 4 kg (4000 gm)),
Maternal diabetes mellitus,
obesity,
Midpelvic instrumental delivery,
post maturity,
multiparity,
anencephaly,
Fits ascites,
Maternal age should be more than 35 years.
Fital Distress,
A short cord or cord tightly looped around the neck.
Symptoms and signs:
Turtle Sign: Involves a phenomenon seen during childbirth where, after delivery of the head of the fetus, the body retracts back towards the perineum instead of holding the start of delivery. This condition indicates a potential solder dystocia condition, which suggests that the solder is stuck behind the pelvic bone.
Prolong second stage of labor.
Maternal perineal pressure and discomfort are increased.
Changes in fetal heart rate are seen, such as bradycardia.
Delay in solder delivery.
Risk of brachial plexus injury increases in newborns.
A potential clavicular or humeral fracture may occur in the newborn.
Maternal hemorrhage.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Fetal heart rate monitoring,
ultrasound,
pelvic examination,
x ray,
M.R.I.
Management:
During management should:
Calling for additional help.
Clearing the infant’s mouth and nose.
Abduct the maternal thigh and flex it spirally towards the abdomen.
Perform a wide mediolateral episiotomy if an earlier mediolateral episiotomy has not been performed.
During management should not:
Do not panic if you have the condition of solder dystocia.
Do not apply Traxon on the baby’s head.
Do not apply fundal pressure.
Step – I: The head and neck of the fitus are grasped and moved in a posterior position and suprapubic pressure is applied towards the fitus’ chest.
Step – II Roberts Maneuver: It involves abduction of the mother’s thigh and the thigh is sharply flexed on the mother’s abdomen.
Step-III Woods Maneuver: It involves inserting two fingers into the posterior vagina and then rotating the posterior solder towards the anterior.
Step: IV Delivery of Posterior Arm:
Identifying the location of the posterior arm.
Directing the hand into the hollow of the sacrum.
Grasp and splint the wrist and forearm.
Sweeping over the chest and hand delivery.
Delivery of posterior arm.
Step: V Cleidotomy: In this the girth of the solder is reduced. And one and both one clavicles are cut.
Zavanellis Maneuver: Used to manage certain cases of solder dystocia during childbirth. In this maneuver, when the placental solder becomes stuck after the head comes out, the placental head is pushed back into the birth canal to relieve pressure on the cord and then delivered by cesarean section.
Obstetrical Emergencies:
- Cord prolapse:
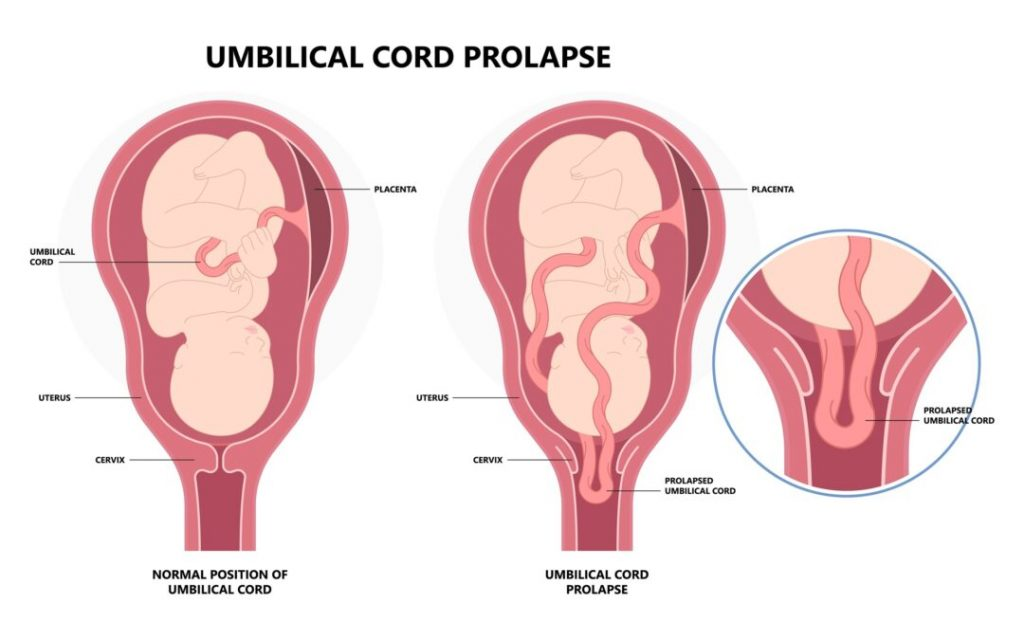
Cord prolapse is a condition where the umbilical cord slips past the presenting part of the fetus during labor, and the membranes are not intact. This can lead to compression of the cord and impairment of blood flow and oxygen supply to the fetus. This can increase the risk of fetal distress. Cord prolapse is considered an obstetric emergency and often requires immediate intervention to ensure the safety of the fetus, such as providing the mother with a proper position or performing a cesarean delivery.
When the umbilical cord comes before the presenting part of the fetus and the umbilical cord is the presenting part but the membrane is not intact and due to this the circulating blood and oxygen supply in the cord is clamped off while passing through the birth canal. A cord prolapse is called an obstetric emergency.
Cord Presentation: Cord presentation is a condition in which the umbilical cord is present before the presenting part of the fetus i.e. the umbilical cord is present as the presenting part and the membrane is also intact. is called
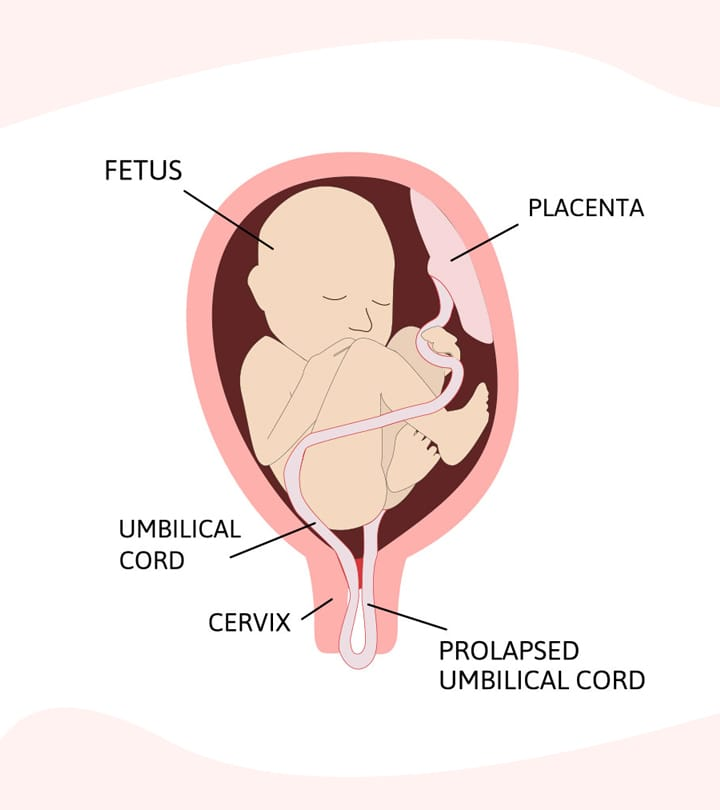
Types of Cord Prolapse:
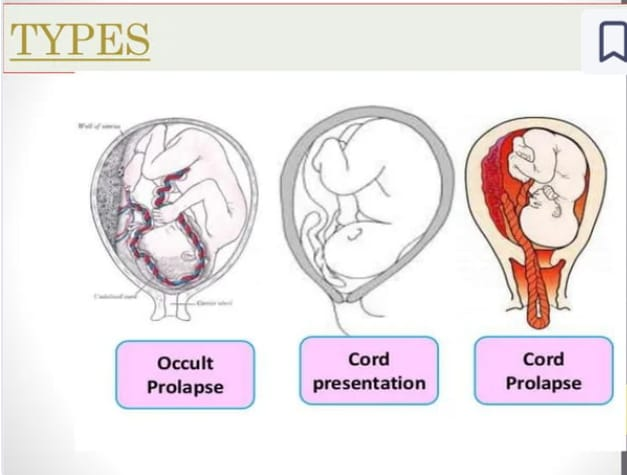
There are generally 3 types of cord prolapse.
1) Occult prolapse,
2) Chord presentation,
3) Cord prolapse.
1) Occult prolapse: Umbilical cord is compressed but not palpable and visible through percussion. It can be detected when there are changes in fetal heart rate monitoring.
The cord falls on the presenting side but is not filled by the fingers on internal examination.
2) Cord Presentation: Cord presentation is a condition in which the umbilical cord is present before the presenting part of the fetus i.e. umbilical cord is present as the presenting part and the membrane is also intact. is called a cord presentation.
3) Cord prolapse: When the umbilical cord comes before the presenting part of the fetus and the umbilical cord is the presenting part but the membrane is not intact and due to this the circulating blood and oxygen supply in the cord while passing through the birth canal. That clamped off is called cord prolapse.
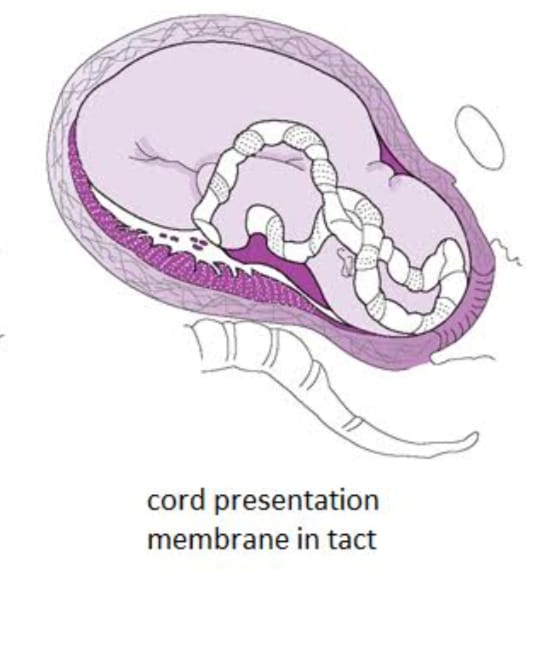
malpresentation,
Contracted pelvis,
prematurity,
Low birth weight <2.5kg,
Fetal Congenital Anomalies
twins,
hydroamnios,
Minor degree placenta previa,
Low Rupture of Membrane,
Manual rotation of the head,
version,
induction,
Long cord (having a long cord more than 100 cm),
Due to abnormal presentation and position of the fetal head, such as
Breech presentation,
Face and brow presentation,
Solder Presentation,
Occipito posterior position,
highhead,
polyhydroamnios,
Multiple pregnancy.
Diagnostic Evaluation:
History Collection,
Physical Examination,
ultrasound,
vaginal examination,
1) Occult prolapse: Diagnosis is difficult. If there is continuous variable deceleration in fetal heart sound (FHS) pattern, occult prolapse may be present.
2) Cord presentation: Pulsation of the cord from the intact membrane fills.
3) Cord prolapse: The cord fills directly, and if the fitus is live, the cord pulsates. Many times the cord does not pulsate but the fitus may be live.
Fits A death is declared to be conformed by USG and auscultation.
Management:
Management usually depends on whether the baby is alive or dead.
If the baby is dead then its conformation should be done by ultrasound and wait for spontaneous delivery.
If the baby is live and vaginal delivery is possible, deliver it by forceps and ventos.
If vaginal delivery is not possible,
First aid management is done by minimizing the pressure in the cord and stopping the infusion of oxytocin.
Observe for cord prolapse in all cases after membrane rupture.
Surgical induction: watch for cord accident before and after amniotomy and, if possible, prepare for caesarean section in the amniotomy operation theatre.
After diagnosis of cord presentation, if immediate delivery is not possible, prepare the patient for caesarean section. Until then, give exaggerated Sims lateral position. Rarely, cervix is 7-8 cm dilated, watch and forceps if there is no fetal distress. And breech delivery.
Cord prolapse: First properly assess whether the baby is live or dead. Look for maturity and survival dilatation.
If the baby is live, cesarean section is the best method. Before preparing for cesarean section, fill the bladder with 400 to 750 ml of normal saline inserted through the catheter and empty the bladder before cesarean delivery.
If immediate safe vaginal delivery is possible then perform forceps delivery in vertex presentation and breech extraction in breech presentation If baby is death then wait for spontaneous delivery after conformation of diagnosis.
Inform the supervisor immediately if the midwife feels the possibility of cord prolapse on vaginal examination.
Taking action immediately after diagnosis of cord problem.
Inform the mother and her family members for immediate action such as caesarean section.
If safe vaginal delivery is not possible, first aid should include minimal pressure on the cord and provide intravenous fluids and oxygen.
If the cord is outside the vagina, cover it with warm normal saline gauze and gently replace it with a gloved hand.
Exaggerated and elevated position of the patient. and placing pillows under the hip or knee-chest or Trendelen Berg position and sending for caesarean section.
Properly assisting the patient and obstetrician in the steps of management.
Careful monitoring of the condition of the fetus.
To properly record the Fetal Heart Sound (F.H.S.) and maintain a proper record of every action.
- Amniotic fluid embolism:
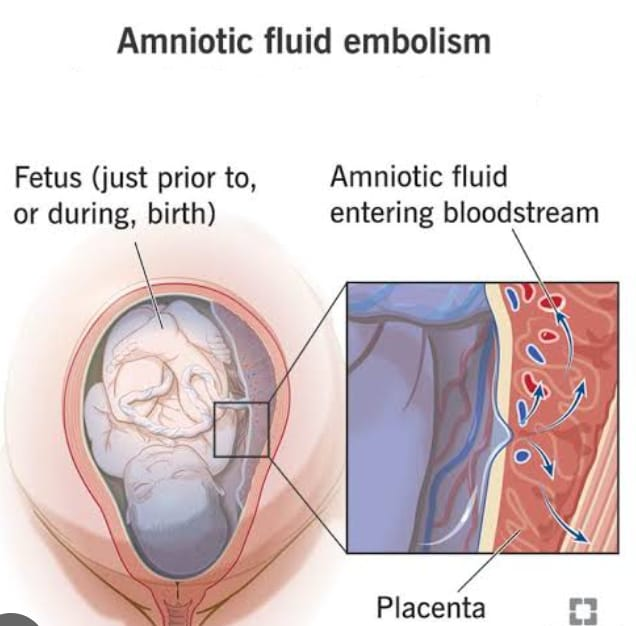
Amniotic fluid embolism is a condition in which the accidental infusion of amniotic fluid from the pressure of the contracting uterus into the mother’s bloodstream or maternal circulation from the uterus or placental site. This condition can usually be fatal to the mother, because Amniotic fluid containing debris deposits in the pulmonary arterioles and produces symptoms of pulmonary embolism. This condition is a common cause of maternal death during labor.
Etiology:
A defect in the membrane,
After membrane rupture or premature separation of the placenta (abruptio placenta),
Rapid or precipitate labor,
multiparity,
Advance Maternal Age,
drug,
Due to uterine trauma in manipulation,
During Caesarean section.
Symptoms and Signs:
Sudden onset of maternal respiratory distress such as
Severe dyspnoea and cyanosis,
chest pain,
frothy pink sputum with cuffing,
Pro-found hypotension and tachycardia,
Grief greater than blood loss,
vomiting,
Restlessness and anxiety,
convulsions,
scissors,
heart failure,
In pulmonary AD,
Fetal bradycardia,
If delivery does not take place, the condition of fetal distress may occur.
Maternal or fetal death can occur within minutes if immediate treatment is not provided.
Complications can include disseminated intravascular coagulation (DIC).
Diagnostic Evaluation:
History Collection,
Physical Examination,
Blood Gas Analysis,
Complete Blood Count (CBC),
coagulation profile,
fibrinogen,
Arterial blood gases,
Electrolyte level monitoring,
Imaging studies (chest x-ray),
electrocardiogram,
echocardiogram,
MRI (if further evaluation is required),
serum tryptase,
Cervical histopathology.
Management:
Call for medical help and provide treatment to the patient immediately.
To immediately start emergency or resuscitative measures to maintain the patient’s life.
Give oxygen 8-10 liter/minute through face mask or 100% oxygen through resuscitation bag and assist in resuscitation immediately.
To prepare the patient for intubation and mechanical ventilation.
Intravenous crystalloid (Ringer’s) or colloids (hemacell) and fresh frozen plasma (FFP), platelet concentrates, packed red blood cells and autotransfusion (patient’s own blood collected from the operated area) for volume replacement.
Administer aminophylline for respiratory distress and heparin in acute condition of disseminated intravascular coagulation (DIC) as per instructions.
Properly monitor maternal and fetal condition.
Hourly urine output monitoring by placing an indwelling urinary catheter.
Provide proper side lining position to the patient.
Making preparations for an emergency birth when the mother’s condition stabilizes.
Properly record and report monitoring.
Provide reassurance and emotional support to mother and family members pro-wide.
Complications of Amniotic Fluid Embolism:
Disseminated intra vascular.
Cardiopulmonary collapse.
Coagulation.
Acute renal failure.
Atonic uterus.
Hypotension.
Fatal distress/death.
- Obstetric shock:
Obstetric shock is a condition in which due to the incapacity of the mother’s circulatory system, there are difficulties in getting the oxygen and nutrients required by the body and in removing the waste substances and circulation is in inadequate amount resulting in poor tissue perfusion hence generalized. Cellular hypoxia occurs, this condition is called shock.
Shock is a condition that can arise due to the inability of the circulatory system to provide oxygen and nutrients to the tissues as required./Shock is generally a state in which tissue perfusion is compromised, causing cellular hypoxia and It is defined as a syndrome initiated by acute hypoperfusion that can lead to a condition of tissue hypoxia. and conditions of vital organ dysfunction may arise. Shock is usually a systemic disorder that can affect multiple organ systems.
Classification/Etiology of Shock:
1.Hypovolemic shock: It may be hemorrhagic or nonhemorrhagic in which the circulatory blood volume decreases.
Post partum/ post abortive haemorrhage,
ectopic pregnancy,
placenta previa,
Abruptio placenta,
Rupture uterus, and obstetric surgery cause hemorrhagic shock.
Nausea, vomiting, diuresis, supine hypotensive syndrome, and amniotic fluid with rapid removal of clod loss lead to nonhemorrhagic shock.
- Septic shock (endotoxic shock): Due to septic abortion, chorioamnionitis, pyelonephritis, postpartum endometritis, the patient goes into septic shock.
- Cardiogenic shock: Cardiogenic shock is seen in myocardial infarction, cardiac arrest, cardiac tamponade.
- Extra cardiac shock: Pulmonary embolism, amniotic fluid embolism, anaphylactic drug, neurogenic, chemical injury etc. are responsible for shock.
Antepartum Causes:
abruptio placenta,
placenta previa,
trauma.
Postpartum Causes:
retained placenta,
atonic uterus,
ruptured uterus,
coagulopathy,
Laceration
Symptoms and signs:
Grey’s Blue/ Pale Skin,
Cold and clammy skin,
sieving,
perspiration,
drymouth,
pyrexia,
Sub-normal temperature,
Rapid and Vic Pulse,
slow bounding pulse,
Rapid breathing but as mother’s condition worsens breathing becomes deep, slow and finally unconscious.
Blood pressure is initially normal then low, but 40% volume loss is not recorded.
Urine output decreases.
Management:
Early diagnosis of signs of shock and provision of comfortable position to the patient. Ex: Providing lateral position in supine hypotensive syndrome.
Start resuscitative measures immediately and maintain the airway and elevate the foot end.
Provide 6-8 liter/min oxygen to the patient.
Correcting the patient’s condition of acidosis.
Stopping bleeding in hemorrhagic shock.
To replace fluid I.V. Provide infusion and transfusion to expand the volume. Ex : blood transfusion, provide normal saline in crystalloid, Hemasil in colloid, etc.
Check cardiac efficiency and prevent circulatory overload and cardiac failure.
Provide instructions on medications, antibiotics, vasodilators, diuretics, corticosteroids, and insulin to maintain normal blood glucose in septic shock.
Provide support, encouragement, and emotional security if grief is due to psychological stress.
To provide proper psychological support to the family members of the patient.
To check and properly record vital sign and fetal heart sound (FHS) of mother every 15 minutes.
To properly maintain patient intake output and other recordings.
Vasa previa:
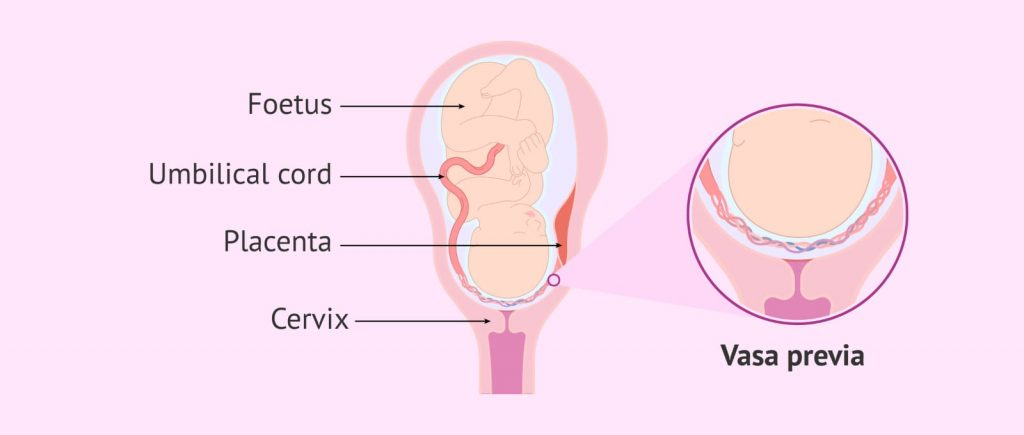
Vasa previa is an obstetrics complication in which the fetal blood vessels pass out through or near the internal orifice of the uterus and in front of the presenting part. When the supporting membrane ruptures, these vessels can rupture. The risk remains because it is unsupported by the umbilical cord or placental tissues. These complications can arise during labor and during delivery.
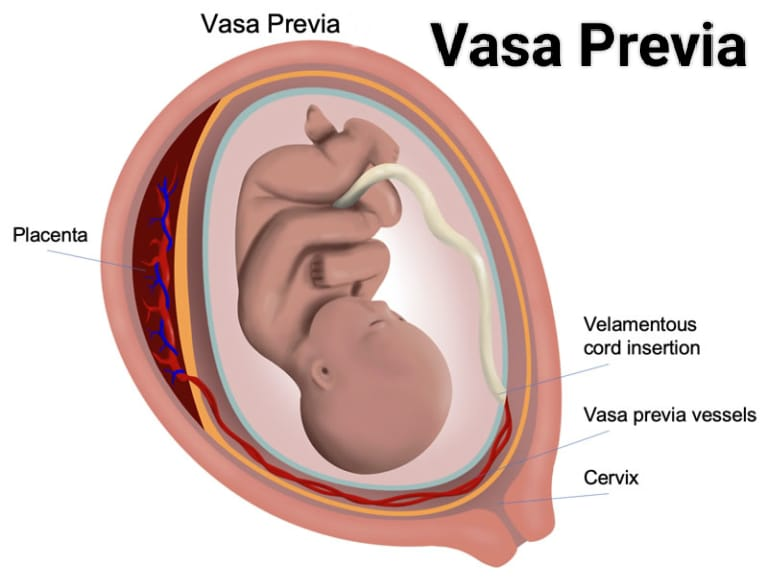
Etiology:
A low lying placenta may be due to scarring of the uterus as a result of previous miscarriages and D and C (dilatation and curettage).
An abnormally or unusually formed placenta may be a bilobed placenta or a sesscenturate-low placenta.
In-vitro fertilization pregnancies and multiple pregnancies (twins and triplets).
Due to velamentous insertion of umbilical cord.
Risk Factors of Vasa Previa:
placenta previa,
Velamentous insertion of umbilical cord,
Multilobed placenta,
Multiple pregnancy.
Symptoms and signs:
Painless vaginal bleeding (2nd and 3rd trimester).
Darker red color blood (because baby’s blood is dark color, bright red blood means mother’s blood).
Fetal bradycardia.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Ultrasonography:
Transvaginal sonography in combination with color Doppler helps detect vasa previa as early as the 16th week of pregnancy.
Noting the triad sign:
Painless vaginal bleeding,
membrane rupture,
Fetal bradycardia or death.
Treatment:
Hospitalize the mother in the 3rd trimester to ensure rapid access to medical care if blood vessels rupture.
A cesarean section is performed around 35 weeks of pregnancy.
A healthy delivery by caesarean section is the only treatment plan to follow. A cesarean section should be planned as early as possible to avoid emergencies and late enough to prevent problems related to prematurity. Usually at 35-36 weeks if the mother is normal without any risk a caesarean section is recommended.
- Rupture of the uterus:
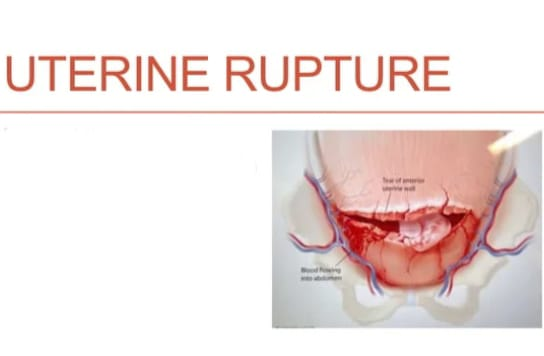
If the continuity of the uterine wall breaks down at any time during pregnancy, this condition is called rupture of the uterus. This is an obstetric emergency that occurs during labor, sometimes in late pregnancy.
A breakdown in the continuity of the uterine wall (endometrium, myometrium, and cirrhosis) occurs after 28 weeks of pregnancy. This is called rupture of the uterus. In which the small rupture occurring in the early month is called perforation.
Types of Uterine Rupture:
- Complete Rupture,
- Incomplete rupture
- Complete Rupture:
Complete rupture is the sudden rupture of the uterus with its peritoneal covering. It is usually caused by the release of scar in the upper segment and spontaneous rupture of obstetrics and non-obstructive type. Complete rupture can occur with or without placental abruption. comes out of the uterus.
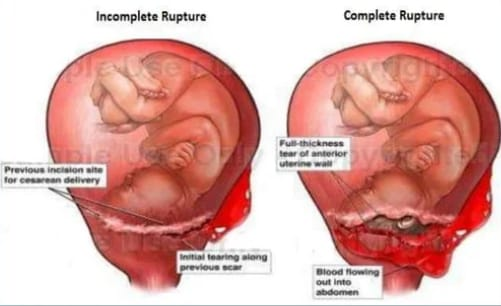
2.Incomplete Rupture: In complete rupture the peritoneum is intact i.e. there is no involvement of the peritoneal membrane and it mostly occurs due to extension of the lower segment scar/cervical tear. In this, the fetus and placenta remain inside the uterine cavity. or parts of the fitus occupying the interlayers of the broad ligament.
Etiology:
Spontaneous rupture,
scar rupture,
Iatrogenic/traumatic rupture.
Spontaneous Rupture:
Dilatation and curettage operation or manual removal of placenta from previous damage to uterine wall,
Grand Multipara,
If there is a congenital malformation in the uterus, spontaneous rupture occurs during pregnancy. It usually occurs during the last trimester.
During labor, the uterus can rupture due to obstructed labor (obstructive rupture) and grand multipara (non-obstructive rupture).
Scar Rupture:
Rupture of the uterus occurs during pregnancy and labor by classical caesarean section or hysterotomy.
Iatrogenic/traumatic rupture:
oxytocin,
prostaglandin,
Forcible External Version,
By pressing on the abdomen,
Internal podleic version,
Manual removal of placenta,
Forceps or breech extraction,
A uterus ruptures due to oxytocin and destructive operation.
Warning sign of ruptured uterus:
Intermittent pain on the right side as the uterus rotates on its axis and tilts to the right side.
Lower abdominal pain.
A pulse rate of less than 100/min.
Chances of shock increase.
In these cases, when the abdomen is opened, the baby is found to be dead.
Vaginal bleeding.
Dull abdominal pain.
Symptoms and signs:
acute abdominal pain,
Burning and severe pain in abdomen.
Vaginal bleeding.
Profuse and sudden vaginal bleeding.
Decreased fetal heart rate.
Decreased or absent fetal movement.
Hypotension (low blood pressure due to blood loss).
Tachycardia (increase in mother’s heart rate due to grief).
Signs of shock like pallor, diaphoresis, confusion etc.
Vital body parts to be palpable.
Abdominal tenderness.
Changes in uterine tone such as uterine hypertonicity or hypotonicity.
Diagnostic Evaluation:
History Collection,
Physical Examination,
ultrasound,
Fetal heart rate monitoring,
laboratory test,
Complete blood count test,
CT scan,
MRI (Magnetic Resonance Imaging),
Laparotomy.
Management:
To provide proper antenatal care to pregnant women.
Screening of cases of obstructed labour, prior caesarean section, hysterotomy, myomectomy and grand multipara, etc. and referred for level II care.
Resuscitation is done if the patient is conscious. It is life saving.
such as,
a.Inj. Morphine sulfate 15 mg I.M. is given.
b.Infusion of 5% dextrose and Ringer’s lactate is started.
c Blood is arranged for immediate transfusion.
Patients are given antibiotics such as:
Inj. cefotaxime 1g I/V × 6 hourly.
Inj. Gentamicin 80 g I/M × 8 hourly.
To check the patient’s pulse and blood pressure every 15 minutes.
The patient and her husband should be informed about the possibility of hysterectomy and sterilization and their consent should be obtained.
The patient is prepared for laparotomy.
Immediate and quick laparotomy is performed through a longitudinal incision under general anesthesia.
If the patient’s condition is low, do quick subtotal hysterectomy.
When the patient’s condition permits and there is colporrhexis, a complete hysterectomy is performed.
Depending on the clinical condition, either resuscitation is followed by laparotomy or in acute conditions resuscitation and laparotomy are performed simultaneously.
After laparotomy, hysterectomy is surgery for rupture of the uterus unless there is sufficient reason to preserve it.
In cases of scar rupture where the margins are clear, the repair is done.
Repair and sterilization are performed in clean cut scar rupture patients with desired number of children.
If rupture occurs outside the hospital, the patient is immediately shifted to a larger hospital.
The patient is kept awake and comfortable.
Provide proper pain relieving drug to the patient like,
Pethidine (100 mg)
If the sterile solution mentioned above is not available, shock is treated by raising the feet in bed and giving rectal infusion of saline or glucose-saline or tap water in intravenous infusion.
Nursing Interventions:
Compulsory hospital delivery of high risk mothers.
Maternal shock or fetal distress is a warning sign for the midwife.
To monitor mother’s vital sign and fetal heart sound (F.H.S.).
To keep Mother’s Nile by mouth.
Call the doctor in signs of complete or incomplete rupture.
Transfer the mother to a well-equipped hospital in the community.
Assist in resuscitation, medical and surgical management of mother.
To provide reinsurance to mother, husband and family members.
- Post Partum Hemorrhage (PPH):
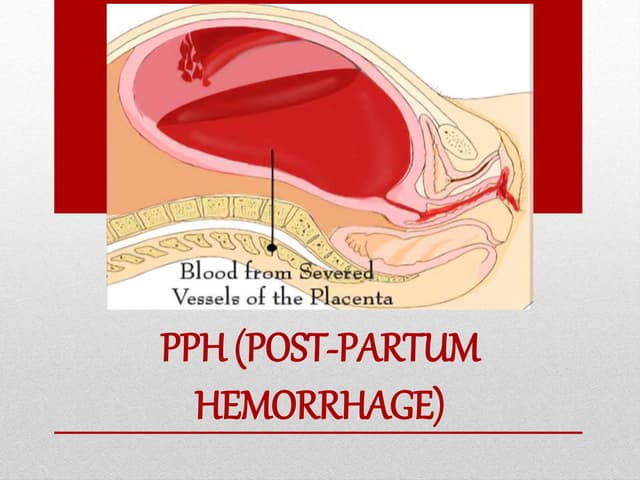
Postpartum haemorrhage is a condition that occurs from the birth of the baby to the end of the peripartum period (after birth of the baby up to 6 weeks period) from the genital tract in excessive amount which adversely affects the general condition of the mother. , in which pulse rate increases and blood pressure falls down as evidence. So this condition is called Post Partum Haemorrhage (PPH).
If 500 ml or more after vaginal delivery, 1000 ml or more after cesarean section,
and ,
If there is blood loss of 1500 ml or more after caesarean hysterectomy, the condition is called post partum haemorrhage (PPH).

Types of Postpartum Haemorrhage (PPH).
There are mainly two types of post partum haemorrhage:
1) Primary Postpartum Haemorrhage,
2) Secondary post partum haemorrhage.
1) Primary Postpartum Haemorrhage: Bleeding occurring within 24 hours after the birth of the baby is called Primary Postpartum Haemorrhage. It usually occurs in the first two hours after delivery. There are two other types:
a)Third stage hemorrhage
b)True post partum haemorrhage
a) Third stage haemorrhage:
Third stage hemorrhage occurs before the expulsion of the placenta.
b) True Postpartum Haemorrhage: True postpartum haemorrhage occurs within 24 hours after the expulsion of the placenta.
2) Secondary Postpartum Haemorrhage: Bleeding after 24 hours after delivery of the baby (occurring up to 6 weeks) is called Delayed Peripheral Haemorrhage, Late Peripheral Haemorrhage or Secondary Postpartum Haemorrhage.
- Etiology of Primary Postpartum Haemorrhage:
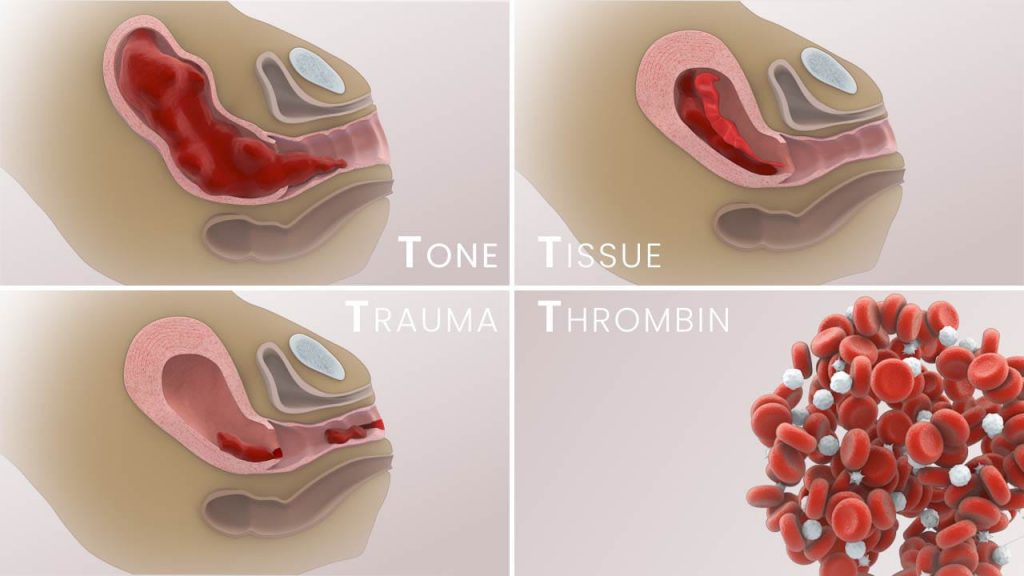
1) Atonic uterus(tone),
2) traumatic (trauma),
3) Retained tissue(s),
4) Blood coagulation disorder (thrombin).
1) Atonic Uterus: About 80% of post partum haemorrhage is caused by atonic uterus. In this, the uterine sinuses rupture after the separation of the placenta, due to which the uterine muscles do not contract and retraction properly, the building continues due to the condition of post partum haemorrhage. It can be seen in the following conditions:
grandmultipara,
multiple pregnancy,
hydroamnios,
Due to over distension of uterus in large baby,
Malnutrition and anemia,
Antepartum haemorrhage, prolonged labour,
anesthesia,
have used oxytocin for induction or augmentation of labour,
Due to malformation of uterus,
Uterine Fibroids,
The third stage of labor is not properly managed,
Retained placenta
2) Traumatic: Up to 20% of post-partum haemorrhage (PPH) is bleeding after operative delivery in the genital tract after delivery and involves the cervix, vagina, perineum, periurethral region and rupture of the uterus.
3) Retained Tissues: Placenta bits and blood clots left in the uterus can lead to postpartum hemorrhage.
4) Blood Coagulation Disorder: Abruptio Placenta, Jaundice, Thrombocytopenic Purpura, HELLP Syndrome, Intra Uterine Death or Sepsis.
Signs and Symptoms of Primary Postpartum Hemorrhage:
Vaginal bleeding is mostly external.
Effects due to blood loss depend on the predelivery hemoglobin level, the degree of hypervolemia, and the rate of blood loss.
Changes in the mother’s vitals, i.e., blood pressure, are seen after a blood volume loss of 20 to 25%. Rarely, rapid blood loss results in death within minutes.
On Abdomen Uterus:
Contracted in traumatic hemorrhage and flabby and hard by massage in atonic hemorrhage.
Management of Primary Postpartum Haemorrhage:
Postpartum hemorrhage is a major cause of maternal morbidity and mortality and is not always preventable but its incidence can be reduced by identifying risk factors.
Measures to prevent post partum haemorrhage:
Antenatal:
To improve the health status of women and make efforts to prevent anemia.
Delivery of high risk multipara in well equipped hospital.
Getting the blood group of each patient done.
Ultra sonography of previous cesarean delivery KM. R. I. By looking at the location of the placenta, placenta accreta can be detected.
Delivery in morbid adherent placenta to a senior obstetrician.
Intranatal:
Active management of the third stage can reduce postpartum hemorrhage by approximately 60%.
If induction or augmentation of labor is done with oxytocin, oxytocin infusion should be given to the athlete for one hour after delivery.
Observe for utero vaginal canal trauma after delivery in difficult labor or instrumental delivery.
After delivery, observe for about two hours to check whether the uterus is hard and contracted, and then send to the ward.
Administer local or epidural anesthesia in forceps, ventos or breech delivery.
Spontaneous separation and delivery of placenta in caesarean section.
Examination of placenta and membranes after delivery.
Antenatal Management:
Assessing the health status of the patient specially maintaining the hemoglobin level of the patient properly.
If the hemoglobin level is properly maintained, then any complications due to blood loss can be prevented.
Transfer the high risk mother to a well equipped hospital.
Intranatal Management:
Sedative and analgesic drug administration during the intranatal period.
Avoid Hasty Delivery After the baby’s head is delivered, it takes at least 2 to 3 minutes for the truck to deliver it.
Managing third stage care in high risk patients.
After the delivery of the placenta, properly assess whether the placenta has been delivered completely or not and assess whether any bits of the placenta are retained in the uterus or not.
Injection oxytocin is 10 unit / IM or if 20-40 Unit oxytocin is added to 1000 ml of normal saline or Ringer lactate solution by infusion.
Exploration of the uterovaginal canal to note whether or not there is any trouma due to difficult labor or instrumental delivery.
After delivery of the patient, keep the athlete under observation for two hours.
Continuously note the mother’s vital signs during that time.
Calling health care personnel for extra health.
Intravenous cannula administration of two large doses.
Sending the blood to the laboratory for blood grouping and cross-matching.
Adequate amount of intravenous fluid administration to the mother.
To properly note the mother’s vital sign.
If bleeding is due to an atonic uterus, gently rub the fundus with finger tips.
If soft and relaxed, gently massage the fundus in a circular motion so that the blood clots can be properly removed.
If bits of placenta or clots are retained in the uterine cavity, remove them properly.
Further repeat the injection oxytocin.
Administer methyl PGF2 intramuscularly or transabdominally into the myometrium to return the uterus to its tone and repeat as needed.
If the uterus is still atonic, perform manual compression.
Applying pressure on the placental side in manual compression can help control bleeding.
Tight intrauterine packing is performed under general anesthesia to control postpartum hemorrhage.
If the above measures fail then hysterectomy is done as a last option.
General Steps for Management of Postpartum Hemorrhage:
Starting intravenous therapy,
Catheterize the mother properly.
If necessary, start a blood transfusion.
To note whether the placenta has delivered properly and if the placenta has not delivered, to properly assess whether it is separated or unseparated.
Remove the placenta bimanually if the placenta has not separated.
If the placenta is undelivered but separated, assess where the patient is present in the uterine cavity. That is, to assess whether it is present in the lower segment of the uterine cavity, in the part of the cervix or on the vagina.
If the placenta is present in the lower segment of the uterine cavity, remove it by controlled cord traction.
If control cold traction fails then perform bimanual compression and if that also fails then perform hysterectomy last.
If the separated placenta is on the cervix or vagina, grasp and remove it, if that fails, remove the placenta by bimanual compression and if that fails, perform hysterectomy last.
To properly remove retained bits of placenta in the uterine cavity if the placenta is delivered.
If placental clots cannot be removed, provide injection Syntocin 40 IU International Unit 1 Liter Intravenous Infusion. Due to which the patient’s clots can be removed.
Then complete vital sign assessment of the mother.
Provide a properly comfortable position to the mother and advise her to take proper rest.
To provide proper reassurance to the mother.
2) Secondary post partum haemorrhage:
Bleeding in the peripartum period (occurring up to 6 weeks) after 24 hours after the birth of the baby is called delayed periperal hemorrhage, late periperal hemorrhage, or secondary postpartum hemorrhage. The building in it can be done mostly during 8 to 14 days.
Etiology of Secondary Postpartum Haemorrhage:
If bits of cotyledon or membrane remain inside the uterine cavity,
Due to infection,
Due to endometritis,
If there is placental site subinvolution, due to
Due to caesarean section wound,
Due to estrogen therapy,
Due to carcinoma of the cervix,
Due to placental polyps,
Due to parietal inversion of uterus,
Signs and symptoms of secondary postpartum hemorrhage:
Heavy lochia discharge that appears bright red in color,
Local discharge being offensive,
fever,
Elevated pulse rate,
Subinvolution of uterus,
anemia,
sepsis,
Nursing Management of Secondary Postpartum Hemorrhage:
To properly assess the amount of blood loss.
To provide proper blood transfusion to the patient.
Properly identifying the causes of postpartum hemorrhage.
Administer 10 units of oxytocin IM (intracellular) or if intravenously (IV) to the patient by adding 20 units of oxytocin to 500 ml of normal saline or regurgitated solution for infusion to prevent post partum haemorrhage.
Provide proper antibiotic medication to the patient.
Advise the patient to take complete bed rest.
If the patient has any retained bits of placenta to remove it properly.
If the patient is bleeding even in a minor amount, do not ignore it as it can be an alarm symptom of post partum haemorrhage.
Properly remove retained product by sponge holding, ovum forceps or gentle curettage.
If bleeding is due to trauma to the cervicovaginal canal, control it with hemostatic sutures.
If the delivery of the patient took place in an unhygienic environment, then administration of anti-tetanus serum and anti-gangrene serum to the patient.
Provide blood transfusion if patient is anemic.
Properly monitor the patient’s vital signs including monitoring vital signs every four hours initially and then twice throughout the day.
Provide the patient with ferrous gluconate (300 mg TDS) or ferrous sulfate (200 mg TDS) orally.
Provide proper folic acid (5 mg) meditation to the patient.
To provide proper work and comfortable environment to the mother.
Advising the mother to take proper follow up.
General Management of Postpartum Haemorrhage:
Postpartum hemorrhage is a major cause of maternal morbidity and mortality, so proper and effective management of postpartum hemorrhage remains important to prevent complications.
The management of postpartum hemorrhage involves a systemic approach that involves controlling bleeding, stabilizing the mother, and identifying the cause of postpartum hemorrhage.
1) Immediate Action:
Early recognition
Early identification of signs and symptoms of postpartum haemorrhage such as excessive bleeding (more than 500 ml if vaginal delivery and more than 1000 ml if cesarean section), tachycardia, hypotension, pallor and signs of shock Identify why.
Call for help
Notify senior obstetricians, anesthesiologists and other necessary health care personnel to assist in the management of postpartum hemorrhage.
assessment
Quantity of blood loss
To properly assess the amount of blood loss.
Clinical assessment
Perform a focused clinical examination to assess for uterine tone, size, and any signs of trauma and whether a retained product is present.
Establish intravenous (IV) access
Large intravenous (IV) access for rapid fluid administration and administration of medications in women with postpartum hemorrhage.
Oxygen administration
Provide supplemental oxygen to maintain tissue oxygenation.
2) Pharmacological management
Uterotonic medication
Administer uterotonic agents to stimulate uterine contractions and control bleeding.
Oxytocin
Oxytocin is a first-line agent with a bolus dose of 10 to 40 units added to 1 liter of crystalloid solution and provided as an infusion over 10 to 30 minutes.
Followed by
Infusion of 40 units in 1 liter of IV fluid over 4-6 hours.
Misoprostol
If oxytocin is not available, administer 800 mcg rectally and 600 orally.
3) Non pharmacological management:
Uterine massage
Gently massage the uterine fundus to enhance uterine contractions and control bleeding.
Balloon tamponade
In post-partum haemorrhage, if there is continuous bleeding even after giving utratonic drugs and uterine massage, then use balloon tampons (Bakery balloon and Follis catheter) to apply pressure to the uterine wall again, thereby achieving hemostasis and controlling the bleeding. can be done
4) Surgical intervention
Manual removal of placenta
If placental tissue appears to be present in the uterine cavity, provide anesthesia and manually remove the placenta.
Compression sutures
Apply uterine compression sutures to mechanically compress the uterus and control bleeding.
Uterine artery ligation
In some cases, uterine artery ligation is performed as a surgical option to reduce blood flow to the uterus.
Hysterectomy
Hysterectomy is performed as an emergency measure when the bleeding is not controlled by any other measures and the patient’s condition is deteriorating.
5) Supportive care and monitoring:
Fluid administration
Adequate intravenous fluid administration to the patient to improve tissue perfusion such as:
Normal saline
Or Ringer lactate solution.
Blood transfusion
Provide blood transfusion as per patient’s need when excessive amount of bleeding has occurred.
monitoring
Continuously monitor the patient’s vital signs, urine output, and level of consciousness.
Repeat hematological and biochemical tests to assess response to treatment.
Psychological support
Post Partum Haemorrhage (PPH) is a traumatic condition so proper psychological support should be provided to the patient and her family members.
6) Prevention
Antenatal care
Early identification of risk factors for post-partum haemorrhage during the antenatal period can lead to early management and prevention of complications.
Active management of third stage of labor
Use of prophylactic uterotonic medication to prevent post-partum haemorrhagic conditions and reduce the risk of uterine atony.
Skilled birth attendance should be available to train personnel to recognize and manage obstetrical emergencies immediately.
7) Follow up and Documentation:
Post management care
Advising the patient to take proper follow up so that the recovery can be monitored and if the patient has anemic condition it can also be assessed.
Documentation
Proper documentation of the event occurred, the interventions performed for it, and the patient’s response to treatment etc.
Thus, proper management of postpartum hemorrhage is important to prevent complications caused by conditions such as postpartum hemorrhage in women after child birth.
- Atonic uterus:
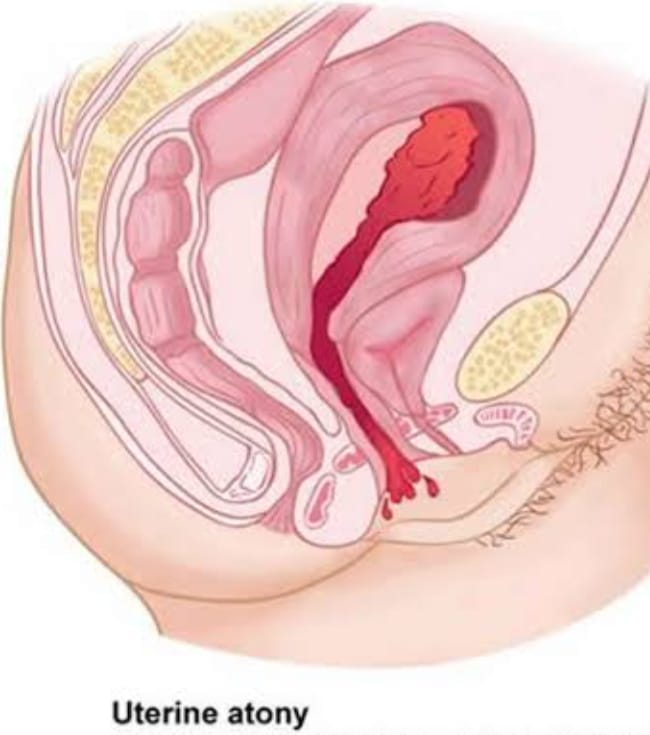
Atonic uterus is a condition in which the uterus fails to contract with normal strength, duration and intervals during childbirth. In other words, the uterus is prolapsed and lacks normal tone. It can arise due to serious complications of the third stage of pregnancy. Uterus without tone end which is the cause of PPH. In which the uterus relaxes.
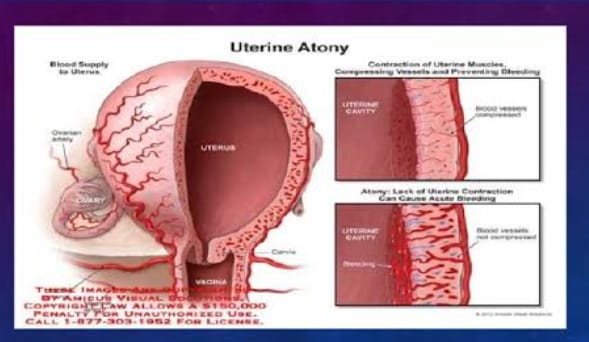
Risk Factors or Causes of Atonic Uterus:
Placenta previa or abruptio placenta,
retained placenta,
Incomplete separation of placenta,
Having a full bladder,
Due to high parity,
multiple pregnancies,
polyhydroamnios,
Being a large baby,
Due to prolonged labour,
Due to anemic mother.
Symptoms and Signs:
excessive bleeding,
Increase heart rate,
low blood pressure,
uterine enlargement,
Pelvic pain and discomfort,
Madwa to see the sign of mourning.
Diagnostic Evaluation:
History Collection,
Physical Examination,
vital sign monitoring,
Hemoglobin and hematocrit level assessment,
ultrasound,
Bimanual Examination,
Blood coagulation test.
Management:
- Uterine Massage:
Uterine massage is the first step in the management of an atony uterus. Uterine massage is done until uterine contractions start continuously.
- Pharmacological therapy:
Oxytocin: This initiates rhythmic contractions.
The uterus compresses the spiral arteries which helps prevent bleeding.
Methylergometrine:
It is not used because of its side effects like hypertension.
Carboprost can be used in cases where oxytocin cannot be used. Prostaglandin is never given intravenously as this may prove fatal.
Arrange for blood and provide blood transfusion if required.
If bleeding continues:
Examining the placenta for completeness.
If the placenta has some missing fragments such as the absence of part of the maternal surface, then properly remove the remaining placental tissues.
Properly Assessing Clotting Status If a clot does not form after 7 minutes or a soft clot breaks down easily, it suggests a condition of coagulopathy. Which should be managed immediately.
If the bleeding continues even after taking the above measures, follow the points below.
Perform manual compression until the bleeding stops and the uterus begins to contract.
Alternatively compressing the aorta.
If still bleeding continuously, ligation of uterus or utero-ovarian artery.
If bleeding does not stop even after ligation, subtotal hysterectomy is performed.
- Injuries to the birth canal
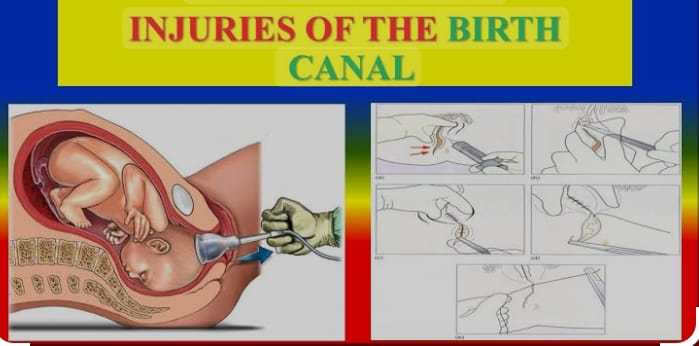
Birth canal i.e. any structure that forms the birth canal during delivery, during labor or during child birth, if there is an injury to those structures, it is called a birth canal injury. In this injury,
Injury to the vulva
Injury to the perineum
Vaginal injury
Injury to the cervix
Pelvichematoma
Rupture of the uterus
Visceral injuries involving bladder, rectum and urethra.
Injuries to Vulva:
If the vulva is injured during child birth and during labor, this condition is called injury to the vulva.
In that common site,
Posteriorly vulvar skin laceration,
Involvement of the para-urethral tear occurs on the inner-aspect of the labia minora.
Injury to the Perineum:
Perineum injuries are usually caused by mismanagement of the second stage of labor.
Etiology:
The reasons may be:
Excessive stretching of the perineum due to:
Large baby
Face to pubis arch
Shoulder delivery (posteriorly one)
Forceps delivery
Rapid stretching of the perineum causes:
Due to rapid delivery of head during uterine contractions.
Precipitate labor.
Due to breech delivery.
Due to inelastic perineum and rigid perineum during elderly primi gravida period.
Due to formation of scar during previous operation.
Ex: Episiotomy or Perineorrhaphy,
Vulval edema.
Degree of Perennial Terrain:
Degree of perineal tear
There are three degrees of perineal tear:
1 St degree: in it
There is involvement of the laceration, involving the hymen, forechette, lower part of the vagina and perineal skin, but the perineal body remains intact.
2nd degree: It involves laceration of the posterior vaginal wall and various degrees of ter involvement of the perineal body and anal.
The sphincter follows.
3rd Degree (Complete): It involves major laceration of the posterior vaginal wall and also involves the ter of the perineum body and the anal sphincter and may or may not involve the anal canal and sometimes the rectum. But involvement can happen.
Management:
The recent tear should be repaired immediately after delivery of the placenta as this reduces the chance of infection and minimizes blood loss.
If the wound is delayed, i.e. repaired after more than 24 hours.
However, if there is a delay of more than 24 hours, the tire should be completely repaired after 3 months.
A 3rd degree scar requires good light exposure, adequate support including an anesthetist, and the necessary instruments.
Repair is done in lithotomy position. The vagina, vulva and perineal region are swabbed with an antiseptic Dettol solution.
The perineal skin, vaginal mucosa, and perineum muscles surrounding the tar are infiltrated with 1% lignocaine hydrochloride (10-20 ml).
In a complete perineal tear, the rectum and anal canal are first closed from top to bottom with chromic catgut No. 00 with interrupted stitches using a covered or traumatic needle, and the note is placed inside the lumen.
The muscle wall and pararectal fascia are then sutured with interrupted stitches using a traumatic needle.
The torn end of the sphincter anii externus exposed by Ellis forceps is reconstructed with a figure of eight stitch supplemented by other interrupted sutures using a 0′ chromic catgut number. ‘
Thus, a 3rd degree perineal tear converts to a 2nd degree.
If the ter is incomplete, the vaginal mucosa should be sutured first. The first suture is placed at or above the apex of the ter.
The wall of the vagina is sutured by interrupted sutures with a chromic catgut number. Using ‘0’ curved round body needle from top to bottom until reaching the fourchette.
Next, repair of the perineal muscles is performed through interrupted sutures using No. 0 catgut.
The perineal skin is sutured with chromic catgut or nylon silicone gut using a cutting needle.
After suturing, daily care of perineal skin is done.
Every time after urination and defecation dressing should be done to keep the wound clean and dry. Dressing is done by swabbing with a cotton swab soaked in antiseptic solution followed by application of antiseptic powder or ointment. (Furacin or Neosporin).
To relieve pain, magnesium sulfate compresses or infrared heat can be used. Analgesic medication can be given when needed.
After 24 hours the patient is allowed to leave the bed.
The patient is given a low residual diet consisting of milk, bread, eggs, biscuits, fish, sweets etc. from the second day.
The patient is given milk of magnesia 8 ml twice a day starting on the second day and increasing to 15 ml on the third day.
If the patient fails to pass stool even with milk of magnesia, the patient is given a compound enema (olive oil, liquid paraffin, glycerin and normal swine).
For 5-7 days, one of these intestinal antiseptics is to be continued or as prescribed by the doctor, namely:
Tab. Neomycin 250 mg four times a day.
Cap. Sulphathiazole 1 mg BD daily.
Tab. Metronidazole 2 tablets four times a day.
Tab. Sulphaguanidine 2 tablets four times a day.
Vaginal Terr:
Isolated vaginal tears/lacerations without involvement of the perineum or cervix are commonly seen after instrumental or manipulative delivery. In these cases, the tar is extensive and often associated with brisk hemorrhage. Terri can extend in any direction, be either superficially limited or diffuse into the paravaginal tissues.
Treatment and Nursing Management
Teres associated with brisk hemorrhage require exploration under general anesthesia with good light.
The tear is usually repaired using chromic catgut No. 0 with interrupted and continuous sutures.
In cases of extensive lacerations in addition to sutures, hemostasis can be achieved by intravaginal plugging with roller gauze soaked in glycerin and acriflavine.
The plug should be removed after 24 hours.
Calporaxis:
Rupture of the vaginal vault is called colporaxis.
Types:
1.Primary : Where only volt is involved.
2.Secondary: When it is associated with cervical ter (common).
When the peritoneum is opened it is said to be complete.
Treatment:
If the tear is limited to the vault including the accessible part of the cervix, the repair is done from below.
If the cervical ter extends into the lower segment or high up to the major branches of the uterine vessels. After damage, laparotomy is performed along with resuscitative measures.
- Cervical ter:
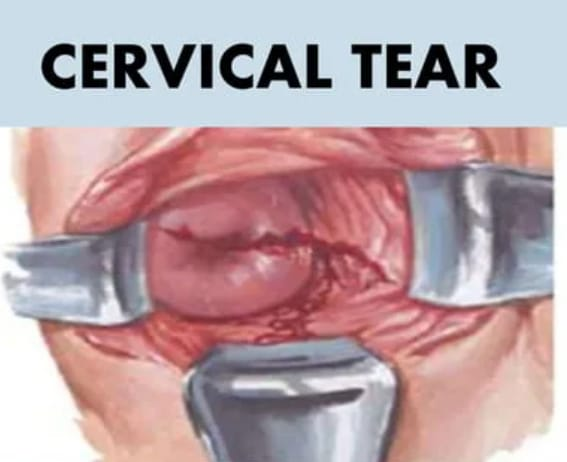
During the first delivery, a minor degree of cervical tear is inevitable. Extensive injuries are rare. Cervical tears involve a laceration or injury to the cervix, which is the lower part of the uterus that connects to the vagina. This can happen during child birth, especially if there is a prolonged labor or if there is significant pressure.
Cervical tears can vary in severity, ranging from minor lacerations to more extensive lacerations that may require medical intervention. Symptoms may include bleeding, pain and difficulties in urination or difficulties in intestinal movement. Proper assessment and care are important to prevent complications.
Etiology:
Due to prolonged labor process,
Due to forceps or vacuum expression,
Due to large fit size,
Due to multiple pregnancy,
Due to abnormal fetal position,
Due to prior cervical surgery,
Due to rigid cervix,
Due to strong uterine contractions.
Symptoms and signs:
vaginal building,
pelvic pain,
Abnormal discharge,
Difficulties in bowel movement and urination.
Look for visible tar.
Diagnostic Evaluation:
History Collection,
Physical Examination,
speculum examination,
ultrasound,
colposcopy,
Laboratory test.
Danger:
Early Danger,
Late Danger
Early Danger:
Deep cervical tear leads to involvement of major blood vessels which can condition severe postpartum haemorrhage.
Pelvic cellulitis.
Thrombophlebitis.
Late Danger:
ectropion,
Cervical incompetence with mid-trimester abortion.
Management:
Cervical tears associated with bleeding should be repaired immediately after delivery of the placenta.
Repair should be done under general anesthesia in lithotomy position with good light.
In this, the anterior and posterior margins of the torn cervix are grasped with sponge holding forceps.
The assistance gently pushes the fundus downward. This makes the tar more accessible for effective suturing.
First the apex has to be identified and the first vertical matrix is sutured and placed just above the apex using a covered round body needle and chromic catgut number ‘0’. Cervix wall thickness is taken.
Bleeding is stopped immediately.
Similar mattress sutures are used to repair the remaining tears. (These sutures prevent rolling of the edges).
If there is condition of cervical tear, lithotomy position should be provided to the woman.
Provide general anesthesia and properly repair the tar.
Exposing the local area and cleaning it properly.
Properly grasp the anterior and posterior margins of the cervix with sponge holding forceps.
Ask the assistant to lower the fundus. Due to this, the tar remains more accessible and sutures can be performed effectively.
Identifying the apex and suturing through the first vertical matrix above the apex with a chromic Catgut No. O using a round body needle. Make sure you take the entire thickness of the cervix.
Nursing Management:
To properly assess the condition of women.
To check vital sign of woman properly.
To properly check the amount of blood loss.
Inform the obstetrician and provide assistance in repairing the terr immediately.
Maintain proper aseptic technique while performing repairs.
Proper antibiotic medication should be provided after providing the test dose.
To provide proper psychological support to women and their family members.
To provide proper work and environment to women.
- pelvic hematoma

Pelvic hematoma is a condition in which blood collects anywhere between the pelvic peritoneum and the perineal skin, this condition is called pelvic hematoma.
Anatomical Type:
Depending on the hematoma, whether it is present below or above the levator ani, it is called:
- Infralevator Hematoma (Common)
- Supralevator hematoma (rarely)
- Infralevator hematoma (common): Most common is vulvar hematoma. A vulvar hematoma is a form of concealed traumatic hemorrhage in the connective tissues of the vulva and vagina.
Etiology:
It can be caused by:
Due to improper hemostasis during repair such as vaginal or perineal tears or episiotomy wounds.
Due to failure to take precautions while suturing apex of tar.
Due to failure to eliminate dead space while suturing the vaginal wall.
Rupture of the paravaginal venous plexus either spontaneously or after instrumental delivery
Due to rupture of subcutaneous veins.
Symptoms and signs:
Persistent and severe pain in the perineal region.
There may be rectal tenesmus or bearing down afters when extension occurs in the ischio-rectal fossa.
Retention of urine can also occur.
In Sign of Pelvic Hematoma:
Variable degree of shock.
On local examination, there may be a tense swelling on the vulva that is dusky purple in color and tender to the touch.
Treatment:
Early detection of hematoma within the operation theater by providing general anesthesia.
Perform all procedures properly maintaining aseptic precautions.
At the same time resuscitative measures are taken.
The wound is reopened or an incision is made along the line of maximum distension, usually near the introitus.
The blood clot is scooped out and the bleeding point is secured.
Usually, an oozing surface is seen near the sutures and a rubber drain can be left in place for 24 hours.
Prophylactically, antibiotics are given or drainage of the hematoma is done under general anesthesia. Analgesic medication is provided to manage pain.
Supralevator Hematoma:
This is a rare type of hematoma and is not commonly seen.
Etiology:
Causes of supralevator hematoma are:
Cervical laceration or primarily colporrhexis (vault rupture)
Lower uterine segment rupture
Spontaneous rupture of the paravaginal venous plexus adjacent to the vault.
Diagnosis:
Diagnosis is usually late (as pain, vaginal bleeding appears late).
After delivery, features of unexplained shock and internal hemorrhage raise suspicion.
On abdominal examination: there is swelling over the inguinal ligament pushing the uterus to contact the lateral side.
A vaginal examination may reveal:
Occlusion of the vaginal canal by a bulge.
Boggy swallowing belt through fornix.
Management:
If there is a shock condition, treat it immediately.
Making Proper Arrangements for Laparotomy
Broad ligament is the anterior leaf of peritoneum is incised and blood is scooped out.
Bleeding points are securely ligated if visible.
To prevent uterine damage, random blind sutures should not be applied.
If the oozing is continuous, the anterior division of the internal iliac artery is tied.
- Rupture of the uterus:
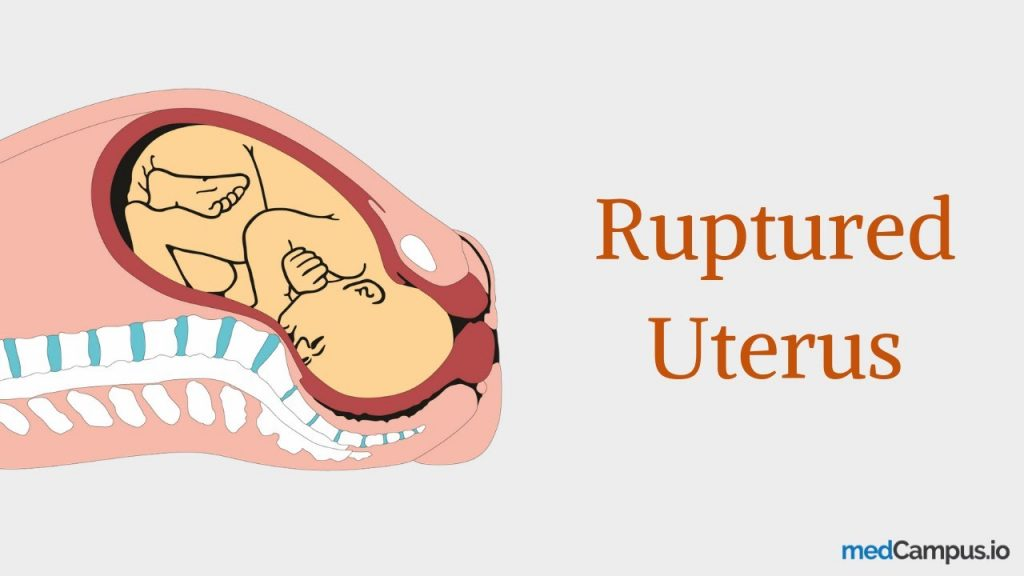
If the continuity of the uterine wall breaks down at any time during pregnancy, this condition is called rupture of the uterus. This is an obstetric emergency that occurs during labor, sometimes in late pregnancy.
A breakdown in the continuity of the uterine wall (endometrium, myometrium, and cirrhosis) occurs after 28 weeks of pregnancy. This is called rupture of the uterus. In which the small rupture occurring in the early month is called perforation.
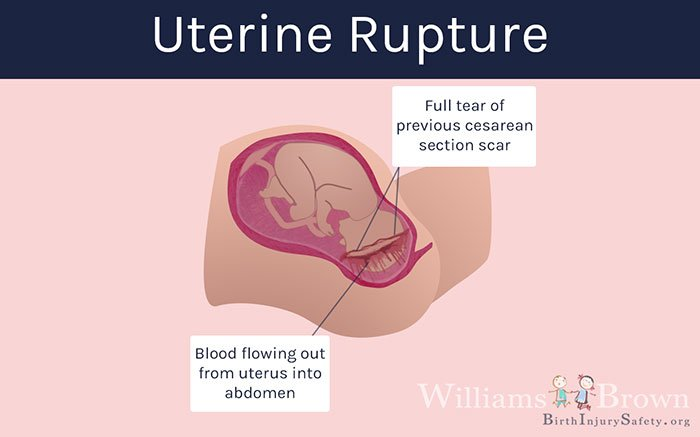
Types of Uterine Rupture:
- Complete Rupture,
- Incomplete rupture.
- Complete Rupture:
Complete rupture is the sudden rupture of the uterus with its peritoneal covering. It is usually caused by the release of scar in the upper segment and spontaneous rupture of obstetrics and non-obstructive type. Complete rupture can occur with or without placental abruption. comes out of the uterus.
2.Incomplete Rupture: In complete rupture the peritoneum is intact i.e. there is no involvement of the peritoneal membrane and it mostly occurs due to extension of the lower segment scar/cervical tear. In this, the fetus and placenta remain inside the uterine cavity. or parts of the fitus occupying the interlayers of the broad ligament.
Etiology:
Spontaneous rupture,
scar rupture,
Iatrogenic/traumatic rupture.
Spontaneous Rupture:
Dilatation and curettage operation or manual removal of placenta from previous damage to uterine wall,
Grand Multipara,
If there is a congenital malformation in the uterus, spontaneous rupture occurs during pregnancy. It usually occurs during the last trimester.
During labor, the uterus can rupture due to obstructed labor (obstructive rupture) and grand multipara (non-obstructive rupture).
Scar Rupture:
Rupture of uterus by classical caesarean section or hysterotomy during pregnancy and labor.
Iatrogenic/traumatic rupture:
oxytocin,
prostaglandin,
Forcible External Version,
By pressing on the abdomen,
Internal podleic version,
Manual removal of placenta,
Forceps or breech extraction,
A uterus ruptures due to oxytocin and destructive operation.
Warning sign of ruptured uterus:
Intermittent pain on the right side as the uterus rotates on its axis and tilts to the right side.
Lower abdominal pain.
A pulse rate of less than 100/min.
Chances of shock increase.
In these cases, when the abdomen is opened, the baby is found to be dead.
Vaginal bleeding.
Dull abdominal pain.
Symptoms and signs:
acute abdominal pain,
Burning and severe pain in abdomen.
Vaginal bleeding.
Profuse and sudden vaginal bleeding.
Decreased fetal heart rate.
Decreased or absent fetal movement.
Hypotension (low blood pressure due to blood loss).
Tachycardia (increase in mother’s heart rate due to grief).
Signs of shock like pallor, diaphoresis, confusion etc.
Vital body parts to be palpable.
Abdominal tenderness.
Changes in uterine tone such as uterine hypertonicity or hypotonicity.
Diagnostic Evaluation:
History Collection,
Physical Examination,
ultrasound,
Fetal heart rate monitoring,
laboratory test,
Complete blood count test,
CT scan,
MRI (Magnetic Resonance Imaging),
Laparotomy.
Management:
Providing proper antenatal care to pregnant women.
Screening of cases of obstructed labour, prior caesarean section, hysterotomy, myomectomy and grand multipara, etc. and referred for level II care.
Resuscitation is done if the patient is conscious. It is life saving.
such as,
a.Inj. Morphine sulfate 15 mg I.M. is given.
b.Infusion of 5% dextrose and Ringer’s lactate is started.
c Blood is arranged for immediate transfusion.
Patients are given antibiotics such as:
Inj. cefotaxime 1g I/V × 6 hourly.
Inj. Gentamicin 80 g I/M × 8 hourly.
To check the patient’s pulse and blood pressure every 15 minutes.
The patient and her husband should be informed about the possibility of hysterectomy and sterilization and their consent should be obtained.
The patient is prepared for laparotomy.
Immediate and quick laparotomy is performed through a longitudinal incision under general anesthesia.
If the patient’s condition is low, do quick subtotal hysterectomy.
When the patient’s condition permits and there is colporrhexis, a complete hysterectomy is performed.
Depending on the clinical condition, either resuscitation is followed by laparotomy or in acute conditions resuscitation and laparotomy are performed simultaneously.
After laparotomy, hysterectomy is surgery for rupture of the uterus unless there is sufficient reason to preserve it.
In cases of scar rupture where the margins are clear, the repair is done.
Repair and sterilization are performed in clean cut scar rupture patients with desired number of children.
If rupture occurs outside the hospital, the patient is immediately shifted to a larger hospital.
The patient is kept awake and comfortable.
Provide proper pain relieving drug to the patient like,
Pethidine (100 mg)
If the sterile solution mentioned above is not available, shock is treated by raising the feet in bed and giving rectal infusion of saline or glucose-saline or tap water in intravenous infusion.
Nursing Interventions:
Compulsory hospital delivery of high risk mothers.
Maternal shock or fetal distress is a warning sign for the midwife.
To monitor mother’s vital sign and fetal heart sound (F.H.S.).
To keep Mother’s Nile by mouth.
Call the doctor in signs of complete or incomplete rupture.
Transfer the mother to a well-equipped hospital in the community.
Assist in resuscitation, medical and surgical management of mother.
To provide reinsurance to mother, husband and family members.
Visceral injury to other organs:
Visceral injuries including,
bladder,
rectum,
the urethra.
Bladder Causes:
trauma,
Slugging fistula
Trauma: It can be due to:
Instrumental vaginal delivery such as destructive operation or forceps delivery especially with Killand forceps.
Abdominal operative procedures such as hysterectomy or caesarean section for ruptured uterus.
Sloughing Fistula:
This is gradually becoming rare in developing countries.
It results from the effect of prolonged compression on the bladder between the head and symphysis pubis in obstructed labour.
Diagnostic evaluation
History Collection,
Physical examination,
Diagnosis is made by:
Dribbling of urine immediately after operative delivery.
Passing blood stained urine after cesarean section or hysterectomy.
Clean cut with margin oozing surface.
In sloughing fistula:
History of Prolonged Labour
Dribbling of urine occurs after various intervals
After delivery (5-7 days).
As the margins become devitalized and necrosed.
Chunks of tissue are missing.
Nursing Management:
Immediate local repair is preferable in traumatic fistula.
In favorable conditions, a self-retaining catheter is introduced and kept in place for 10-14 days or longer.
Comes on urinary antiseptics.
The patient is advised to wash the bladder daily (not more than 30 ml). The lotion is provided with acriflavineline 10,000.
In favorable conditions, the fistula may close spontaneously. If it goes to failure, then after 3 months repair has to be done.
In sloughing fistulas, repair should not be attempted, instead a self-retaining catheter is placed.
Repair is to be done after 3 months.
- Retained placenta

Retained placenta means a condition in which the placenta is not expelled even for 30 minutes during the 3rd stage of labor i.e. after the birth of the baby, i.e. it is retained (held) in the uterine cavity, this condition is called retained placenta. comes
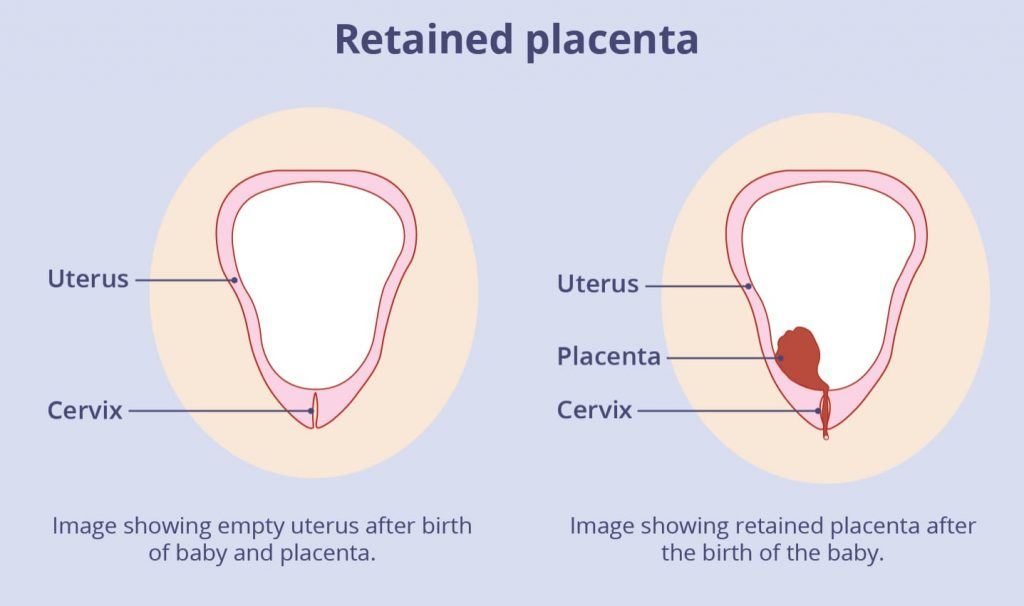
Etiology:
Causes of retained placenta are:
The placenta is completely separated but the placenta remains retained due to poor voluntary expulsive effects, especially due to exhaustive and prolonged labour.
Simple persistent placenta due to uterine atonicity:
Grand Multipara,
Over distension of uterus,
Due to the condition of prolonged labour,
Uterine Malformation,
Due to larger placental surface.
Placenta Partial/Complete Separation A retained placenta can occur due to:
Constriction ring (hour-glass constriction), hour-glass constriction occurs due to mismanagement of the 3rd stage of labour, i.e. due to fiddling with the uterus or overzealous massage of the uterus.
Morbid Adherent Placenta: Partially or Rarely Complete.
Due to faulty technique for expelling the placenta before it separates.
Adequate uterine contractions and retraction are stopped due to full bladder due to which difficulties in expulsion of placenta may arise.
Other causes like,
Poor Voluntary Explosive Afters,
Atonic uterus: due to grand multipara, over distension of uterus, prolonged labour, uterine malformation, large placental surface area.
Morbid adherent placenta: partial or rarely, complete.
Constriction ring (due to hour-glass construction).
Due to trying to deliver the placenta prematurely.
Symptoms and signs:
Post partum haemorrhage,
uterine atony,
Foul smelling vaginal discharge,
Abdominal pain and tenderness,
Having the condition of lokia present for a prolonged period of time.
Due to blood loss, symptoms of anemia such as fatigue, weakness and pallor can be seen.
Danger:
hemorrhage,
grief,
Peripheral sepsis,
Risk of recurrence in next pregnancy.
Management:
Complete observation for bleeding at the time of delivery of the placenta.
If the bladder is bloated, empty it through a catheter.
If bleeding occurs during this period, manage as for third stage hemorrhage.
If the placenta is separated, remove it by controlled cord traction.
To properly note the mother’s vital sign.
If the placenta is un-separated and retained in the uterine cavity, remove it manually.
If there are complications with retained placenta, provide treatment and remove the placenta manually.
To provide proper work and comfortable environment to the patient.
- Inversion of uterus
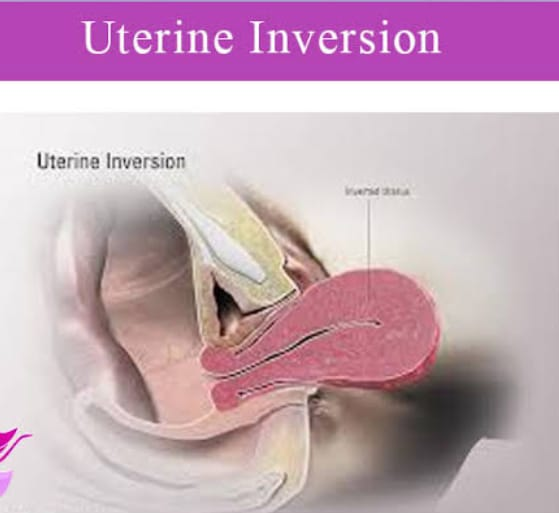
Inversion of uterus is a rare third-stage serious complication in which the uterus protrudes slightly or completely from the inside to the outside. It is called inversion of uterus. Inversion often starts from a dimple in the fundus of the uterus and The uterus continues to invert until it is completely inverted. Its incidence is approximately 1 in 20,000 deliveries.
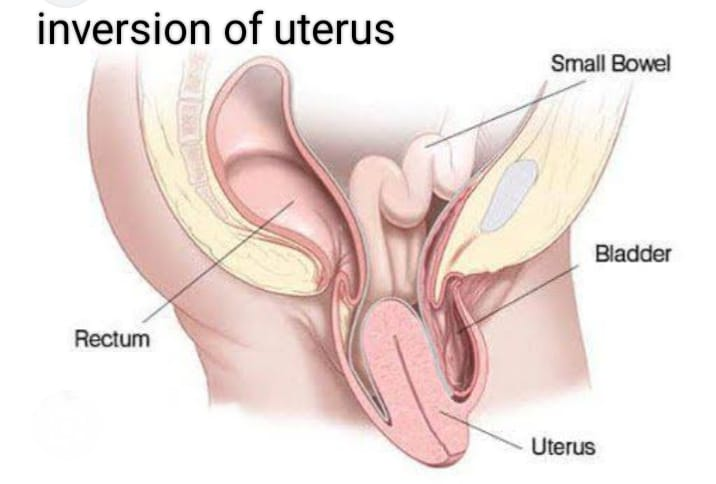
Degree of puerperal inversion of the uterus
There are three degrees of inversion of uterus namely:
- First degree
- Second degree
- Third degree
1.First degree: In the first degree, the depressed fundus reaches the internal orifice or there is dimpling in the fundus.
- Second degree: In this, the body of the uterus is inverted up to the level of the internal orifice. The fundus protrudes into the vagina through the external orifice. First and second degrees have incomplete inversion
- Third Degree (Completely Inversion):
In this stage the uterus and cervix are completely inverted.
The fundus protrudes into the outside of the vaginal introitus.
It involves inversion of playing in advanced 3rd degree.
The endometrium is visible on the outside of the vulva with or without the placenta.
Etiology:
Spontaneous (40%),
induced (60%).
Spontaneous (40%): Spontaneous inversion of the uterus is rare but if present, local tone of the placental site at the fundus associated with a sharp rise in intra-abdominal pressure as in cases of sneezing, cuffing or bearing down afterts. may be due to It is sometimes linked to such as:
short cord,
placenta accreta,
Fundal attachment of the placenta.
Induced (60%):
Mismanagement of the 3rd stage of labor leads to inversion in the uterus.
Stretching (pulling) of the cord when the uterus is atonic.
Improper cradle cap on an atonic uterus.
Due to use of improper/faulty technique of placenta in manual removal.
Due to short cord pulling on fundus during delivery.
Due to forced expulsion of placenta due to downward pressure on uterus.
Symptoms and signs:
Acute lower abdominal pain with bearing down sensation.
grief,
Cupping or dimpling of the fundus on abdominal examination.
On bimanual examination when there is a complete degree of peer sap, redis purple color mass is seen outside the vulva which can be diagnosed by sonography.
Inversion is usually caused by 3rd stage labor.
Due to blood loss in acute inversion, the condition of shock can also arise.
In symptoms of chronic inversion,
Persistent vaginal bleeding,
pelvic pain,
Something protrudes from the top of the head.
Difficulty in passing urine.
Sign:
There may be evidence of grief.
A condition of anemia can occur in mild to moderate degree.
First degree inversion involves cupping of funds.
Bimanual examination shows protrusion of the fundus within the uterine cavity.
In 2nd degree, the fundus cannot be felt bimanually.
A round and firm swelling with a soft bleeding surface is felt as the cervix protrudes into the vagina, and the swelling is often covered by the placenta.
In the 3rd degree, the abdominal fundus cannot be felt. The mass protrudes outside the vulva.
Nursing Management:
Proper management of the third stage is important in this condition so that complications can be prevented.
Provide intravenous fluid such as Ringer’s lactate solution to prevent the patient from going into shock condition.
To arrange proper blood transfusion for the patient.
Immediate treatment in recent cases is replacement of the uterus under general anesthesia.
Provide patient with inj.Retrodrine IV over 15 min.
The part of the uterus lying near the cervix should be pushed in first and then the part of the fundus should be pushed in.
If the placenta is still adherent, it should not be removed before manual replacement unless a large portion of the placenta interferes with manual replacement.
After replacement, the hand is placed in the uterus while Methergin 0.2 mg is administered intravenously.
Inj. Oxytocin is an I.v. Drip is provided to prevent recurrence of inversion.
To provide proper blood transfusion to the patient.
Elevate the patient’s feet if symptoms of shock are observed.
Replacement of uterus by providing general anesthesia to the patient.
Controlling the condition of vaginal haemorrhage by tight gouge plugging.
Oxytocin should not be provided while the uterus is still inverted.
If a recent case occurred after a few days, manual replacement is attempted as soon as possible.
If that fails, Sullivan’s hydrostatic method is performed under general anesthesia.
The uterus is pushed into the vagina.
A vaginal douche is given with an antiseptic solution by placing a douche nozzle in the posterior vaginal wall and the douche is prevented from escaping.
Inj. Oxytocin is provided.
In case of chronic cases, operative treatment is advised by incision of the posterior part of the ring by Holten’s method per abdomen or anterior part of the ring by Spinelli’s method per vagina.