ENGLISH NEW MIDWIFERY GNM TY UNIT 8 Management of Complications During Pregnancy
Unit : 8 Management of Complications During Pregnancy
Bleeding in pregnancy
Ectopic pregnancy:
Definition
When a fertilized ovum implants and develops in the endometrial cavity of a normal uterus (outside), it is called an ectopic pregnancy.
Anatomical site of implantation of ectopic pregnancy:
Tubal pregnancy is more common. Normally the right fallopian tube is more common than the left fallopian tube. The ampulla of the fallopian tube is the most common site of implantation of an ectopic pregnancy.
If an ectopic pregnancy occurs at the isthmus of the fallopian tube, it is considered a dangerous site that can also lead to tubal rupture.
etiology
Due to certain factors, the migration of fertilized ovum into the uterine cavity is delayed.
Due to factors that provide a favorable environment for fertilized ovum to implant in the tubal mucosa.
Due to hormonal factors,
Due to birth defect,
Due to a medical condition.
Risk factors
Due to prior ectopic pregnancy,
Due to previous surgery in the uterine tube,
Due to tubal reconstructive surgery,
Intra uterine contraceptive device no use due to failure,
Due to some type of infection like,
Pelvic Inflammatory Diseases,
chlamydia infection,
Gonorrhea etc.
Having a history of infertility,
Due to Assisted Reproductive Techniques (ART),
Due to infertility treatment like,
In Vitro Fertilization (IVF),
As the mother’s age is more than 35 years,
Due to inducing prior abortion,
Having a history of endometriosis.
Signs and Symptoms:
Symptoms and signs of ectopic pregnancy are classified into two types:
1) Acute type
2) Chronic type
1) Acute type
An acute type of ectopic pregnancy presents with a triad of symptoms such as:
amenorrhea,
Sharp colicky abdominal pain,
Vaginal bleeding
Nausea and vomiting
Palency usually depends on the amount of hemorrhage.
To see signs and symptoms of mourning,
such as,
Rapid and Fable Pulse,
Falling blood pressure,
Extremities are cold and clammy.
On abdominal examination, the abdomen feels tense, tense, and tender.
Abdominal tenderness.
Bowel is distended.
Massive intraperitoneal hemorrhage occurs with tubal rupture and tubal abortion.
Cullen sign positivity: dark bluish peri-umbilical ecchymosis due to hemoperitoneum.
Vaginal area pale during pelvic examination.
The uterus appears to float in the water.
2) Chronic type
Tubal mole is common in the chronic type
It is not known at first.
Its signs include anemia, bladder irritability, tachycardia and increased temperature.
amenorrhea,
abdominal pain,
Vaginal bleeding that appears dark in color shortly after abdominal pain.
Bladder irritation such as dysuria, frequency of urination, retention of urination.
Increase in body temperature.
Examination reveals that the patient is ill,
to see the pallor,
An increase in pulse rate even at rest.
Abdominal tenderness on the affected side.
Filling of mass like structure on lower abdominal site which is irregular.
Extreme tenderness of the cervix.
Diagnostic Evaluation:
History Collection,
Physical Examination,
blood examination,
Caldosynthesis (Tapping of Pouch of Douglas),
sonography,
Assessment of hcg level,
laparoscopy,
laparotomy,
Dilatation and Curettage,
Trans vaginal ultrasonography (USG)
Management of Ectopic Pregnancy
Management of ectopic pregnancy is divided into two types,
such as,
1) Acute ectopic pregnancy management,
2) Management of chronic ectopic pregnancy
Principles of Management
To prevent complications to the mother.
In case of ectopic pregnancy, laparotomy should be performed immediately because the fertilized ovum cannot survive outside the uterine cavity so the tissues are removed to prevent serious complications.
1) Management of acute ectopic pregnancy:
Provide anti-shock treatment to patient and prepare for urgent laparotomy.
Advise the patient to lie down flat on the bed.
Provide patient with inj.morphine 15 mg (IM).
If needed, start a 5% dexrose drip.
Arrangement of blood for blood transfusion.
Even if blood is not available or arranged and the patient is in a state of shock, performing a laparotomy is imperative.
The fallopian tube containing the gestational sac is removed through a laparotomy and a partially surgical procedure.
Performing a salpingectomy. In whose step,
Referring the patient to the hospital,
Advise the patient to lie down on a flat bed.
If the patient is collapsed, raise the bed towards the foot end.
Assessing the patient’s hemoglobin level.
If the patient needs blood transfusion, keep the blood ready.
Administer adequate intravenous fluids to the patient until blood is available.
Ex:=Ringer lactate,
Dexran.
Perform a quick laparotomy under general anesthesia on the patient for salpingectomy.
Then placing the incision on the line of intra umbacus.
After that recognize the uterus and shake out the blood continuously.
Both uterine sites should then be assessed to identify gestational shock in the fallopian tubes.
After that the affected tube and ogre are observed.
Clamps are then applied.
Then the gestational sac wadi affected fallopian tubes with and without ovaries are removed.
The clamps are replaced by chromic catgut ligatures which should not be tightened.
Proper hemostasis is then ensured.
A tubectomy or salpingectomy for hydrosalpinal fluid is performed for the other fallopian tube when the patient wants sterilization.
When a blood clot is free present in the peritoneal cavity, it should be aspirated as much as possible.
Then wash the pelvic cavity properly with normal saline and quickly close the abdomen.
In case of interstitial tubal pregnancy, only the gestational scar should be removed but sometimes for the purpose of better hemostasis, quick subtotal hysterectomy is required.
2)Management of chronic ectopic pregnancy:
All cases with chronic ectopic pregnancy should be admitted to emergency.
Keeping the patient properly under observation.
To carry out all investigations of the patient properly.
Control bleeding quickly and effectively.
Keeping blood transfusion available.
Provide intravenous infusion to the patient as prescribed.
Advise the patient to perform laparotomy as early as possible.
Preparing the patient for laparoscopy or laparotomy.
Then advise to perform salpingectomy.
With medical management in ectopic pregnancy, the ectopic pregnancy is removed by making an incision on the fallopian tube or removing a section of the tube.
If the patient has suppurative pelvic hematocele, provide appropriate antibiotics and drain the pus.
Removal of tubal mole by laparotomy and partial incision on the fallopian tube.
Provide proper management of patients after surgery.
Providing systemic methotrexate 50 mg IM to patients under medical treatment.
Rh antigen is not sensitized in positive Rh women. Anti-D gamma globulin-50 micrograms should be provided to the patient immediately after operation to prevent isoimmunization.
Providing care to resuscitate the patient in acute rupture of the fallopian tube.
Properly maintain vital sign intake output chart of patient.
Providing antibiotic medication to the patient.
Anchoring the patient to early movement.
Advising the patient for proper follow-up.
- Abortion:
Definition of Abortion:
Abortion is a process in which pregnancy is terminated. In abortion, the product of conception is partially and completely separated and expelled from the uterine wall before the age of viability (28 weeks). This condition is called “abortion”. Abortion if it occurs spontaneously is called “miscarriage” and if induced abortion is called “induced abortion”.
Majority abortions or miscarriages occur during the first trimester of pregnancy i.e. during the first 12 weeks of pregnancy, then it is called “early miscarriage”. And the miscarriage that occurs after 13 weeks of pregnancy is called “late miscarriage”.
Etiology of Abortion:
The etiology of abortion is often complex and unclear but may include:
- Ovular or fetal factor
- Maternal environment
- Paternal factor
4.Unknown (25%).
Ovular or fetal factor: An autosomal trisomy in which there are three homologous chromosomes instead of two autosomes. Any chromosome other than the sex chromosome (common).
Monosomy is the condition without one missing chromosome from a pair of homologous chromosomes.
Gross congenital malformation.
Blighted ovum (ovum without embryo).
Due to hydropic degeneration of villi.
A knot, twist, or interference with the circulation of the umbilical cord may cause the death of the fitus and its expulsion.
Due to placental formation.
Twins or hydroamnios.
Maternal Environment:
- Maternal Illness: Like,
Infection:
Viral infection – rubella, cytomegalovirus, hepatitis parvovirus, influenza virus etc.
Parasitic – Malaria
Protozoal – Toxoplasmosis.
Maternal hypoxia and shock: It can be caused by the following conditions due to production of anoxic conditions.
Acute Prescription Disease,
Chronic Prescription Disease,
heart failure,
pernicious anemia,
Due to anesthesia complications,
Severe gastroenteritis,
Cholera.
Chronic Illness:
Hypertension
Chronic nephritis
Chronic wasting disease.
Endocrine factor:
hypothyroidism,
hyperthyroidism,
Diabetes mellitus.
Trauma:
Due to direct trauma to the abdominal wall,
Psychic: Emotional upset or changes in environment can lead to abortion.
c In a susceptible individual, even minor trauma, e.g.
Rough Road.
Internal Examination in Early Month.
Eliciting the Hager sign.
Sexual intercourse in the early months.
Toxic Agents: Toxic agents involve:
Environmental toxins such as:
a. Lead
b.Arsenic
c. Anesthetic gases
d. tobacco
e. Caffeine
f .Alcohol
g. Radiation in excess amount.
- Cervico Uterine Factor:
Cervical incompetence,
Congenital malformation of uterus,
Uterine tumors (fibroids),
retroverted uterus, - Immunological Factors:
Lupus anticoagulant.
Antiphospholipid antibodies.
Alloimmune factors.
6.Blood group incompatibility: It involves Rh incompatibility.
- Premature rupture of the membrane can lead to the condition of abortion.
- Diabetic factor: Due to deficiency of folic acid and vitamin C.
Paternal Factor:
Due to defective sperm.
Due to the contribution of half the number of chromosomes of the ovum.
Common Non-Causes of Abortion:
First Trimester:
Defective germ plasma,
hormonal deficiency,
trauma,
Acute infection.
Mid Trimester:
Cervical incompetence,
Due to uterine malformations,
Uterine Fibroids,
Loimplantation of placenta,
Twins and Hydroamnios
Abortion condition can arise due to causes like etc.
Types of Abortion:
The types of abortion are as follows.
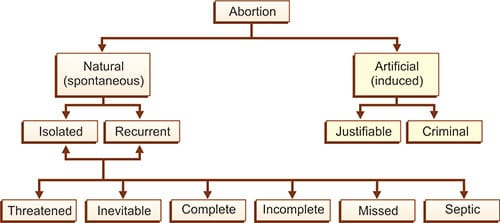
1) Spontaneous abortion
A) Threatened abortion,
B) Inevitable abortion,
C) Complete abortion,
D) Incomplete abortion,
E) Silent or missed abortion,
D) Septic abortion,
E) Recurrent abortion or habitual abortion,
2) Induced abortion
1)Spontaneous Abortion:
When abortion occurs naturally without any medical or surgical intervention, it is called spontaneous abortion. Its cause can be any genetic abnormality and maternal condition.
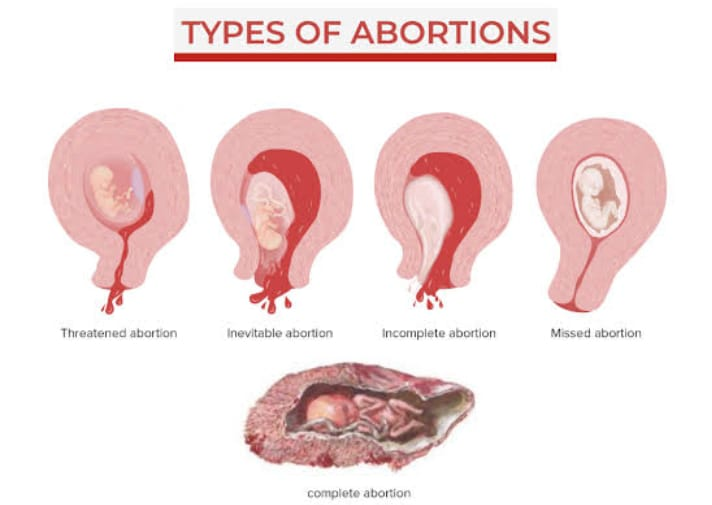
A) Threatened Abortion:
In threatened abortion, the process of abortion starts but the abortion does not reach the point where recovery is impossible, i.e. recovery can take place if proper care is taken.
B) Inevitable Abortion:
Inevitable abortion is a type of abortion in which the expulsion of the conceptus progresses with cervical dilatation. In this case, the pregnancy cannot be saved because most of the portion of the placenta is detached (from the uterine wall). This is a clinical type. is an abortion in which the changes in the abortion have progressed to the point where continuation of the pregnancy becomes impossible.
C) Complete Abortion:

Complete Abortion A type of abortion in which the product of conception is expelled in the form of mass is called complete abortion.
D) Incomplete Abortion:
Incomplete abortion is a type of abortion in which the entire product of the conceptus does not exit the uterine cavity but a small part of it remains in the uterine cavity, then this abortion is called incomplete abortion.
E) Silent or Missed Abortion:

Silent or missed abortion is said when the fetus has died in the uterine cavity and is retained in it for more than 4 weeks, then this abortion is called silent or missed abortion.
D) Septic abortion:
When the abortion is accompanied by evidence of infection of the uterus and its contents, i.e. the abortion is due to any infection, the abortion is called a septic abortion.
E) Recurrent Abortion or Habitual Abortion:
When three or more spontaneous abortions occur in sequence before 20 weeks, it is called recurrent abortion.
Other causes include immunoglobulin G, hormonal deficiency, and cervical incompetence.
genetic factor,
infection,
Also caused by endocrine and anatomical abnormalities.
2)Induced Abortion:
Induced Abortion means any medical or surgical procedure to terminate a pregnancy at will is called induced abortion.
Medical Abortion:
A medical abortion involves the use of medication to terminate a pregnancy and
Medical abortion is effective up to 10 weeks of pregnancy.
Ex:= combination of Mifeprostone and misoprostol.
Surgical Abortion:
It involves performing a surgical procedure by health care personnel and terminating the pregnancy. It is called surgical abortion Ex: vacuume Aspiration.
Threatened Abortion:

In threatened abortion, the process of abortion is started but the abortion does not reach the condition where recovery is impossible, i.e. recovery can take place if proper care is taken. And the pregnancy can continue.
Signs and Symptoms:
Vaginal erection,
Mild abdominal pain and cramping,
Bleeding to be slight,
Seeing blood no color bride red,
Mild abdominal pain,
Bleeding is painless,
mild back unite,
Dull pain in the lower abdominal area,
No fresh lump or expulsion of any kind,
having a closed cervix,
Seeing the discharge.
Sign:
Abdominally: A gravid uterus becomes soft filled and enlarged similar to a menorrhoea period.
Speculum examination or vaginal palpation: The os of the cervix is closed and a stained discharge is present.
Investigation:
Blood investigations including,
HB, ABO and Rh grouping.
urine test,
bimanual palpation,
Pelvic ultrasonography,
Transvaginal ultrasonography.
Management of threatened eruptions
Proper assessment and monitoring of pregnant women in nursing management of threatened abortion. To provide proper supportive care to women.
1) Assessment
Vital sign
To continuously monitor the mother’s vital signs. such as,
pulse,
blood pressure,
temperature,
Respiration etc.
Bleeding assessment
Assess the color, amount, intensity and consistency of vaginal bleeding.
History Collection
Collect proper history of mother including complete history about previous pregnancy and abortion.
2) Monitoring and Observation
Continuously observe the mother to assess whether she has any signs and symptoms of shock (hypotension, tachycardia, pallor).
Conduct proper investigations of mother including hemoglobin, hematocrit, ultrasonography, ABO & Rh grouping routinely.
3) Bed rest and physical activity
Advise the mother to take complete bed rest.
Advising the mother to do limited physical activity.
Advising mother not to do household work for one month.
4) Emotional support
To provide emotional support and reassurance to the mother and her family.
To properly clear the doubts and queries of the mother and her family members.
Do not give false reasons to mother and her family members.
5) Education
Providing education to the mother about the signs and symptoms of abortion such as increased bleeding, severe pain, etc. and advising her to seek immediate medical treatment if any such signs and symptoms are observed.
Provide education to mother to take proper follow up.
6) Hydration and nutrition
Advise the mother to have adequate fluid intake.
Continuously monitor mother’s intake output chart.
Advising the mother to take a properly balanced diet.
Advise the mother to consume a high fiber diet to prevent constipation.
Providing supplements to the mother with good fitting.
Ex:= Ferrous Sulphate 200 mg( BD. ),
Folic acid 5 mg/day (TDS).
Provide mother with high protein and vitamin E diet.
7) Medication administration
Providing prescribed meditation to the mother.
Provide medication to control bleeding and relieve pain.
Provide education to the mother about medication dosage, direction and side effects.
To relieve the mother if she has problem of slip and anxiety
Tab. Diazepam, (5-10 mg before night meal),
Or
Tab.Calmpose, (5-10 mg before night meal),
Or
Tab.valium (5-10 mg before night meal), should be provided.
Provide mild amount of laxative to mother at bed time for good bowel activity.
Ex:= Milk of Magnesia.
Do not provide enema to the mother as enema is responsible for stimulating uterine contractions in the mother.
Provide purgative or suppository in mild amount after 48 hours of signs and symptoms of threatened abortion to the mother to relieve constipation if present.
8) Consultancy and referral
Collaborating properly with other health care personnel for care.
To provide timely referral services to the mother if required.
9) Documentation
Timely documentation of mother’s assessment findings, interventions provided, and whether there are any changes in mother’s condition.
10) Follow up
Giving advice to take regular follow up for mother’s progress and reassessment.
Nursing management of threatened abortion is usually provided to provide properly comprehensive care to the mother and to bring about improvement in the mother’s condition.
Inevitable Abortion:
Inevitable abortion is a type of abortion in which the expulsion of the conceptus product progresses with cervical dilatation. In this abortion, the pregnancy cannot be saved/continuated because most of the portion of the placenta is detached (from the uterine wall). .This is a clinical type of abortion in which the abortive changes have progressed to the point where continuation of the pregnancy becomes impossible. It is called “inevitable abortion”.
Signs and Symbols:
Symptoms:
Increased vaginal bleeding,
This bleeding occurs due to detachment of the placenta from the uterine wall,
Severe colicky lower abdominal pain,
No exfoliation of tissues of any kind,
Dizziness due to heavy blood loss.
Sign
Vital signs are normal in majority of cases but in some cases signs of shock are seen due to excessive bleeding.
Skin is cold and clammy,
A uterus felt firm (contracted),
Cervix is seen dilating. The product of the concepts admitting the index finger is felt through the finger.
Management:
Assess the patient’s proper general condition.
Properly assess loss of product of conception.
If there is excessive amount of blood loss, properly administer intravenous (I.v.) fluids.
If the patient has lost excessive amount of blood, then proper blood transfusion should be done.
Blood Hb, ABO Rh group and random blood glucose level test if abortion has occurred.
Intramuscularly (I.m.) injection morphine to provide 15 mg.
In the case of inevitable abortion, if the cervix is fully dilated and the size of the uterus is less than 12 weeks, administer injection methargine 0.2 mg to control excessive bleeding.
If the patient is in shock condition, treat the shock condition properly by providing intravenous fluid (I.v.) or blood transfusion.
If the abortion procedure is before 12 weeks then curettage is done after providing GA (General Anesthesia) followed by dilatation and evacuation. Alternatively, suction and evacuation can be used.
If the abortion procedure is more than 12 weeks, an oxytocin drip (10 units in 500 ml of 5% dextrose) at a rate of 40-60 drops per minute enhances uterine contractions.
If the placenta is expelled and the placenta is retained, the ovum is removed with forceps.
If the placenta is not separated, GA is provided and digital separation is performed.
If bleeding is profuse due to a closed cervix (suggesting low implantation of the placenta), an abdominal hysterotomy may be required to empty the uterus.
If a condition of shock has arisen due to excessive blood loss, treat it properly.
Complete Abortion:
A complete abortion is a type of abortion in which the product of conception is expelled as a mass in which the fetus and placenta are usually completely expelled. The product of conception is not retained in the uterine cavity, i.e. the uterus is emptied. Called complete abortion.
Symptoms and signs:
A history of expulsion of flaccid mass-like structures,
Decreased abdominal pain,
Vaginal bleeding is minimal or absent,
Uterus appears smaller than during periods of amenorrhea,
Transvaginal ultrasonography showing empty ureteric VT.
Management:
Assess the patient’s proper general condition.
Properly assess loss of product of conception.
Continuously monitoring the mother’s condition.
Properly assess the amount of blood loss the patient has.
If there is excessive amount of blood loss, properly administer intravenous (I.v.) fluids.
If the patient has lost excessive amount of blood, then proper blood transfusion should be done.
Blood Hb, ABO Rh group and random blood glucose level test if abortion has occurred.
If the patient is in shock condition, treat the shock condition properly by providing intravenous fluid (I.v.) or blood transfusion.
If a condition of shock has arisen due to excessive blood loss, treat it properly.
Advise the patient to undergo uterine curettage if expulsion of the product of completely conceptus is suspected.
Advise patients for transvaginal sonography to prevent unnecessary surgical procedures.
An Rh negative patient without antibodies in her system should be protected by anti-D gamma globulin 100 micrograms I/M respectively in case of early abortion within 72 hours.
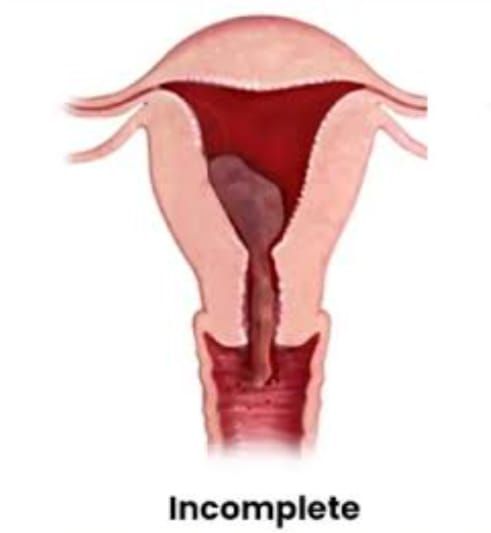
Incomplete Abortion:
Incomplete abortion is a type of abortion in which the entire (complete) product of the conceptus is not expelled from the uterine cavity but a small part of it remains in the uterine cavity, then this abortion is called incomplete abortion.
Symptoms and signs:
History of expulsion of small amount of mass like structure from vaginal area,
Colic pain in lower abdominal area,
During the internal examination.
Uterus appears smaller than during periods of amenorrhea,
Vaginal bleeding is observed,
Expulsion of incomplete mass like structure is seen during examination.
Management:
Assess the patient’s proper general condition.
Properly assess loss of product of conception.
If there is excessive amount of blood loss, properly administer intravenous (I.v.) fluids.
If the patient has lost excessive amount of blood, then proper blood transfusion should be done.
Blood Hb, ABO Rh group and random blood glucose level test if abortion has occurred.
Intramuscularly (I.m.) injection morphine to provide 15 mg.
In the case of inevitable abortion, if the cervix is fully dilated and the size of the uterus is less than 12 weeks, administer injection methargine 0.2 mg to control excessive bleeding.
If the patient is in shock condition, treat the shock condition properly by providing intravenous fluid (I.v.) or blood transfusion.
If the abortion procedure is before 12 weeks then curettage is done after providing GA (General Anesthesia) followed by dilatation and evacuation. Alternatively, suction and evacuation can be used.
If the abortion procedure is more than 12 weeks, an oxytocin drip (10 units in 500 ml of 5% dextrose) at a rate of 40-60 drops per minute enhances uterine contractions.
If the placenta is expelled and the placenta is retained, the ovum is removed with forceps.
If the placenta is not separated, GA is provided and digital separation (dilatation and evacuation) is performed.
If bleeding is profuse due to a closed cervix (suggesting low implantation of the placenta), an abdominal hysterotomy may be required to empty the uterus.
If a condition of shock has arisen due to excessive blood loss, treat it properly.
Proper removal of the product of conceptus by ovum forceps or blunt curettage in condition of incomplete abortion.
In late cases (dilatation + curettage) the tissue left behind is operated to remove bits of tissue, and the removed material is sent for histological examination.
Silent or missed abortion:
Silent or missed abortion is said when the fetus has died in the uterine cavity and is retained in the uterine cavity for more than 4 weeks, then this abortion is called silent or missed abortion.
Symptoms and signs: Persistent brownish vaginal discharge,
Subsidence of pregnancy related symptoms,
Uterine growth arrest,
Absence of fetal heart sound,
Cervix becomes firm,
Fetal skeletal collapse in radiology,
Absent fetal movement.
Investigation:
Blood investigations including,
HB, ABO and Rh grouping.
urine test,
bimanual palpation,
Pelvic ultrasonography,
Transvaginal ultrasonography.
Management:
When the uterus is less than 12 weeks:
Vaginal evacuation is done without delay.
Slow dilatation of cervix by suction and evacuation or Laminaria tent and emptying of uterus under GA.
Keep in mind the risk of hemorrhage during the operation.
Uterus more than 12 wk: For this, induction is done by following methods:
Oxytocin:
Initially start with: 10-20 units of oxytocin in 500 ml dextrose saline 5% given as a drip with 30 drops/min.
If the above regimen fails, increase the dose of oxytocin to 100 units in a pint of 5% dextrose saline at a drip rate of 30 drops/min.
Use the above method with caution.
Prostaglandins:
It is more effective than oxytocin.
Inj. 15 Methyl PG F 2α (Carboprostromethamine) 250 µg I/M every 3 hours. Such is provided at intervals for a maximum of 10
A prostaglandin E₁ analog (gemiprost pessary) is inserted into the posterior vaginal fornix up to a maximum of 5 times every 3 hours.
Proper assessment and monitoring of pregnant women in the management of abortion. To provide properly supportive care to women.
Assessment:
Vital sign
To continuously monitor the mother’s vital signs. such as,
pulse,
blood pressure,
temperature,
Respiration etc.
Bleeding assessment
Assess the color, amount, intensity and consistency of vaginal bleeding.
History Collection
Collect proper history of mother including complete history about previous pregnancy and abortion.
Monitoring and Observation
Continuously observe the mother to assess whether she has any signs and symptoms of shock (hypotension, tachycardia, pallor).
Conduct proper investigations of mother including hemoglobin, hematocrit, ultrasonography, ABO & Rh grouping routinely.
Bedrest and physical activity
Advise the mother to take complete bed rest.
Advising the mother to do limited physical activity.
Advising mother not to do household work for one month.
Emotional support
To provide emotional support and reassurance to the mother and her family.
To properly clear the doubts and queries of the mother and her family members.
Do not give false reasons to mother and her family members.
Education
Providing education to the mother about the signs and symptoms of abortion such as increased bleeding, severe pain, etc. and advising her to seek immediate medical treatment if any such signs and symptoms are observed.
Hydration and nutrition
Advise the mother to have adequate fluid intake.
Continuously monitor mother’s intake output chart.
Advising the mother to take a properly balanced diet.
Advise the mother to consume a high fiber diet to prevent constipation.
Providing supplements to the mother with good fitting.
Medication Administration
Providing prescribed medication to the mother.
Provide medication to control bleeding and relieve pain.
Provide education to the mother about the dosage, duration and side effects of the medication.
Provide mild amount of laxative to mother at bed time for good bowel activity.
Ex:= Milk of Magnesia.
Consultancy and referral
Properly collaborating for care with other health care personnel.
To provide timely referral services to the mother if required.
Documentation
Timely documentation of mother’s assessment findings, interventions provided, and whether there are any changes in mother’s condition.
Follow up
Advising the mother to follow up regularly for progress and reassessment. Management of abortion is generally provided to provide properly comprehensive care to the mother and to bring about improvement in the condition of the mother.
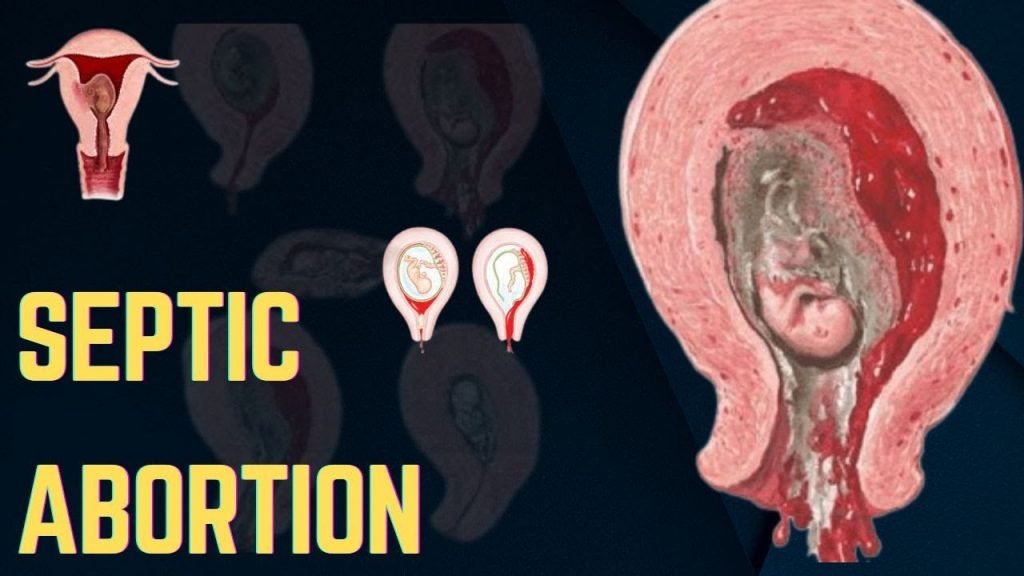
Septic abortion:
When the abortion is accompanied by evidence of infection of the uterus and its contents, i.e. the abortion is due to any infection, the abortion is called a septic abortion.
Etiology:
1.It is involved in sepsis caused by microorganisms that are normally present in the vagina (endogenous).
2.Microorganisms are:
such as,
a Anaerobic:
Bacteroides Group (Fragilis)
Anaerobic streptococci
Clostridium welchii
Tetanus bacilli
b Aerobic:
E. coli
Klebsiella
Staphylococcus
Pseudomonas
Haemolytic Streptococcus.
- The increased association of sepsis with illegal induced abortion is due to the fact that:
Proper antiseptic and asepsis are not taken.
Incomplete evacuation
Due to inadvertent injury to the genital organs and adjacent structures, especially the (gut) intestine.
Symptoms and signs
Signs of septic abortion, infection such as,
fever,
feeling cold,
Riggers coming,
Foul smelling vaginal discharge and purulent vaginal discharge.
Infection is likely to be transmitted in the blood stream.
Abdominal pain and tenderness,
Tachycardia,
An increase in the pulse rate to more than 100-120 beats per minute indicates that the infection has spread to the uterine cavity.
Vaginal bleeding is observed,
Having a history of septic shock,
A history of jaundice, oligouria and anuria should be found.
A gravid uterus feels same, small in size, firm, and tender with movement.
Foul purulent discharge from uterus.
Diagnostic Evaluation:
The main two investigations of septic abortion are:
routine investigation,
Special Investigation
Routine Investigation:
Cervical and high vaginal swabs are taken before internal examination (to find out the dominant micro-organism).
Blood test to estimate Hb.
WBC – Total and Differential Count.
Culture and urinalysis.
ABO and Rh grouping.
Special Investigation:
Pelvis and Abdomen Ultrasonography,
Pelvis and Abdomen X ray,
Blood studies: culture, serum electrolyte, and coagulation profile.
Grading:
Septic abortion is generally divided into three grades.
1) Grade 1: Infection is usually localized in the uterus and is usually associated with spontaneous abortion.
2) Grade 2: In this the infection usually spreads to the pelvic structure.
3) Grade 3: In this the infection is usually generalized peritoneum i.e. spread to the peritoneum or sometimes a condition of septic shock may also arise.
Management:
Management of the condition of a patient with septic abortion generally depends on the patient’s severity.
Obtain mother’s hi-vaginal or cervical swab culture, medication sensitivity test, and Gram stain.
Examination of the vagina is done to note the condition of abortion. If the product of conception is found loosely in the cervix, it should be removed by sponge-holding forceps.
An overall assessment of the case and grading for further treatment is done.
Conduct all investigations of the patient properly.
Provide proper treatment to the patient to remove sources of infection and sepsis.
Provide proper supportive therapy to the patient.
Administer sports therapy to the mother to restore normal homeostatic and cellular metabolism.
Grade I or mild septic abortion: Drug of choice or antibiotic used is capsule.
Ampicillin/Amoxicillin (Mox, Coymox)
500 mg TDS × 7 days
cap. Cephadroxil (Cephodar) 500 mg BD × 7 days
cap. Chloromycetin 500 mg 6 hourly.x 7 days.
While giving Cap.Chloromycetin. Blood test is done for Hb, TLC, DLC and platelets.
In grade 1 prophylactically anti-gas gangrene serum 8000 units and antitetanus serum 3000 units I/M are given.
Analgesic and sedative medications are given as per the doctor’s prescription.
To minimize oliguria, anemia or shock, blood transfusion is done.
Incomplete evacuation within 24 hours after providing antibiotics after grade 1 abortion.
Gentleness should be maintained while doing curettage, which can prevent injury.
Medicines given in Grade II are according to the type of organism, i.e. gram positive and gram negative. For gram positive:
inj. Aqueous penicillin G 5 million units every 6 hours.
Inj. Ampicillin 0.5-1 g IV every 6 hours.
For gram negative:
Inj. Gentamicin 1.5 mg/kg IV every 8 hours.
Inj. Ceftriaxone 1.5 IG, IV every 12 hours.
For anaerobes:
Inj. Metronidazole 500 mg IV every 8 hours.
Inj. Clindamycin 600 mg IV every 6 hours.
To monitor the mother’s vital signs properly.
The uterus is emptied by suction evacuation with antibiotic treatment within 6 hours.
If uterus and intestine are injured then laparotomy is done.
If the uterus is injured or infected, a hysterectomy is performed.
When the infection is localized to the pouch of Douglas, a posterior colpotomy is performed.
In grade III, it is referred to as severe septic abortion with antibiotic therapy. The mother is resuscitated and fluid and electrolyte balance is maintained.
When laparotomy is performed by a surgeon experienced, simple drainage of pus is also effective.
Recurrent Abortion or Habitual Abortion:
When a sequence of three or more spontaneous abortions occurs before 20 weeks of pregnancy, it is called recurrent abortion. Other causes include immunoglobulin G, hormonal deficiency, and cervical incompetence.
genetic factor,
infection,
Also caused by endocrine and anatomical abnormalities.
Etiology:
Due to genetic chromosomal error,
Due to anatomical defect,
Like, cervical incompetence and uterine anomalies,
Uterine infection,
endocrine disorders,
immunological factor,
idiopathic
Signs and Symtones:
Absence of fetal heart sound,
Multiple spontaneous abortions (recurrent).
Diagnostic evaluation:
History Collection,
Physical Examination,
VDRL test,
thyroid function test,
ABO & RH Grouping,
Topzoplasma IgG and IgM,
ultrasonography,
hysterosalpingography,
hysteroscopy,
laparoscopy,
endocervicals swab,
Simmons Analysis.
Management:
In nonpregnant state of the patient, complete history should be collected and properly recorded.
Assess the general health status of the patient.
Perform a pelvic examination to assess for cervical incompetence.
Laboratory tests like blood test, urine test, cervical culture,
Perform hysteroscopy, ultrasonography, and dilatation and curettage (D&C) to look for uterine KVT abnormalities.
Proper treatment of any infection during post conception.
Emphasis on health promotion in proper prenatal care of the patient.
See the patient if there is cervical in computer C then perform cerclage operation, Sirodkar or Mc Donald operation. Then remove stitches after 38th wick or before.
If the mother has a condition of bleeding then report immediately.
Provide education to patients for regular antenatal checkup and hospital delivery.
Management of abortion involves comprehensive care and support for women undergoing termination of pregnancy, whether spontaneous (miscarriage) or induced (therapeutic) abortion.
History Collection
Completing a complete history of a woman’s medical, obstetrical and gynecological conditions.
Assessing gestational age of pregnancy, identifying reasons for abortion.
Complete vital sign monitoring of the mother including,
blood pressure,
pulse,
Properly and continuously monitoring respiration and temperature etc.
Assess the client for any signs of haemorrhage eg excessive bleeding pallor etc.
Perform an abdominal examination to assess the tenderness of the uterine cavity.
Then perform a pelvic examination to assess whether cervical dilatation and products of conception are present in the uterine cavity.
Providing proper emotional support and counseling to mother and family members.
Advising the patient to explain his feelings.
Providing education about available resources for psychological support such as support groups and counseling services.
Provide prescribed analgesic medication such as NSAID or Acetaminophen to relieve the patient’s pain.
Advise the patient to use non-pharmacological measures such as heating pads and relaxation techniques to relieve the patient’s pain.
Assess the patient for signs of excessive building.
Properly assessing the amount of blood loss to the mother Preparing for blood transfusion if the patient needs it
Assess the patient for signs and symptoms of infection such as,
fever,
foul smelling,
Properly assess for symptoms like discharge and lower abdominal pain.
Provide adequate antibiotic medication to the patient as prescribed.
Properly monitor the patient for signs of incomplete abortion such as continuous heavy bleeding and camping pain.
Preparing the patient for possible surgical intervention such as dilatation and curettage (D & C).
Provide patient education about signs and symptoms requiring immediate medical care such as heavy bleeding, pain, and fever.
Provide instruction to maintain perineal hygiene to prevent infection.
Advise the patient to make a follow-up appointment one to two weeks after the abortion so that complete recovery can be properly ascertained.
Provide complete patient education about the importance of follow up visits.
Provide information to the patient about available contraceptive options to prevent unintended pregnancy.
Also provide patient education about the timing of using contraceptives after abortion.
Discharge planning involves ensuring that the patient is able to go home and that the patient can receive adequate support and a safe environment at home.
Then provide written instructions on meditation use, activity restrictions, and signs of complications. Provide information about support services and resources available in the community.
Properly and accurately document all assessments, interventions, patient responses and education provided.
Recording the emotional states of patients and providing counseling and psychological support to them.
The nurse plays a critical role in the comprehensive management of women who have had an abortion, which involves providing compassionate care, ensuring the patient’s physical and emotional well-being, and providing patient education about post-abortion care and contraceptive options. is
Proper assessment, monitoring and providing proper intervention of the patient can prevent complications and facilitate the recovery process.
Proper management of abortion plays an important role in improving the mother’s well-being.
Induced Abortion:
Induced Abortion means any medical or surgical procedure to terminate a pregnancy at will is called induced abortion.
- Medical Termination of Pregnancy (MTP)
Medical termination of pregnancy is a medical procedure in which a woman can undergo termination of pregnancy to maintain her health or well-being by considering certain criteria.
Termination of pregnancy by medical or surgical method before the stage of viability of the fetus is called induction of abortion, legal or illegal. Abortion was legalized in India as medical termination of pregnancy in August 1971 and came into effect from April 1972 and revised by Happened in 1975.
indication
When a woman’s life is in danger and her physical and mental health is severely damaged.
Child may have physical and mental abnormalities.
In the condition that the child has any congenital anomaly.
Being pregnant due to rape.
Due to social or economic reasons, mother’s health is damaged and contraceptive measures have failed.
According to Indian law, abortion is allowed up to 20 weeks, the opinion of one registered medical practitioner is required for pregnancies up to 12 weeks and two registered medical practitioners for 12 to 20 weeks.
Returned (written) consent of the patient and consent of the guardian is required in cases where the patient is under 18 years or mentally handicapped.
Contraindications
Have uncontrolled blood pressure greater than 160/100,
Having Cardio Vascular Diseases,
Women are above 35 years of age,
Have severe renal failure, liver disease or respiratory disease,
Using systemic corticosteroids,
coagulopathy or women receiving anticoagulant therapy,
Mother is anemic,
Have an uncontrolled seizure disorder.
Who can perform medical termination of pregnancy?:
The Chief Medical Officer or Civil Surgeon authorizes the following doctors for medical termination of pregnancy:
Holder of Post Graduate Degree or Diploma in Obstetrics and Gynaecology.
Six months training as a resident in obstetrics and gynaecology.
One year experience in Obstetrics and Gynecology Department.
Registered Medical Practitioner assisted in 25 cases of Medical Termination of Pregnancy (MTP).
Place for MTP (Medical Termination of Pregnancy):
A hospital established or maintained by the Government or a place approved by the Chief Medical Officer or Civil Surgeon.
Records:
Recording medical termination of pregnancy in the form. Maintain confidentiality and report to Director of Health Services.
Penalty:
A person who does not comply with this act can be punished with imprisonment of 2 to 7 years.
Methods of Medical Termination of Pregnancy (MTP):
First Trimester (up to 12 weeks):
Medical
This involves terminating the pregnancy using medication such as,
Mifepristone,
Mifepristone and Misoprostol,
Mithotrexate and Misoprostol,
Tamoxifen and misoprostol.
surgical
A pregnancy is terminated using a surgical procedure.
such as,
Menstrual Regulation, Vacuum Aspiration,
Saxan Evacuation and Curettage,
Dilatation and evacuation.
Second Trimester (13-20 wks):
prostaglandins,
Dilation and evacuation,
Intra uterine instillation of hyperosmotic solutions,
oxytocin infusion,
Hysterotomy.
Complications:
Complications usually depend on the method by which Medical Termination of Pregnancy (MTP) is performed.
Immediate complications
Cervical lacerations,
uterine perforation,
hemorrhage,
grief,
thrombosis,
embolism,
The post-abortal triad may include pain, bleeding, and low-grade fever, depending on the method used for medical termination of pregnancy.
remote
Gynecological complications,
Obstetric complications,
Failed Abortion,
Ectopic pregnancy etc.
Nursing Role with the Patient Undergoing MTP:
The nurse should provide comfort and support to the mother and her family members and provide proper reassurance by clearing all their queries.
If the mother decides to have an abortion, her husband and the patient’s own consent should be obtained along with their written permission.
Continuous monitoring and providing support to the patient before medical termination of pregnancy, during the procedure and even after the procedure is completed.
Providing proper education to the mother about the complications that may arise after abortion such as,
Continuous vaginal bleeding with clots up to three weeks after abortion,
Providing education to women about fever, continuous pain, and burning micturition etc.
First menses start 2 to 8 weeks after a woman is advised to have an abortion.
Advise women that if lactase is started, it is in mild amounts and lasts for 48 hours if the breast is not stimulated.
Provide them with education or follow-up visits two to eight weeks after medical termination of pregnancy (MTP) to ensure that the reproductive organs have returned to their prepregnancy state.
Thus, termination of pregnancy is done in medical termination of pregnancy.
APH (Ante Partum Haemorrhage):
Bleeding from the genital tract after the 28th week of pregnancy but before the birth of the child is called APH (Ante Partum Haemorrhage).
Or
“Antepartum Haemorrhage (APH) is bleeding from or in the genital tract that starts at 24 weeks of pregnancy and precedes the birth of the child” This condition is called Antepartum Haemorrhage (APH).
It is placenta previa (where the placenta is implanted abnormally low in the uterine cavity). Or it can be caused by different conditions like placental abruption (where the placenta prematurely separates from the wall of the uterine cavity).
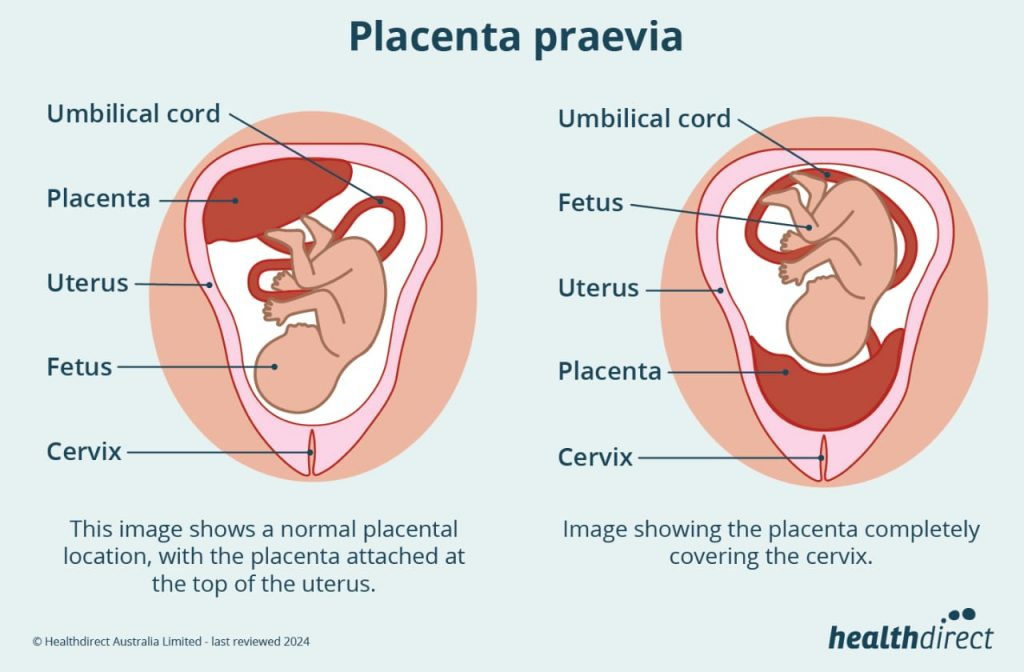
- Placenta Privia:
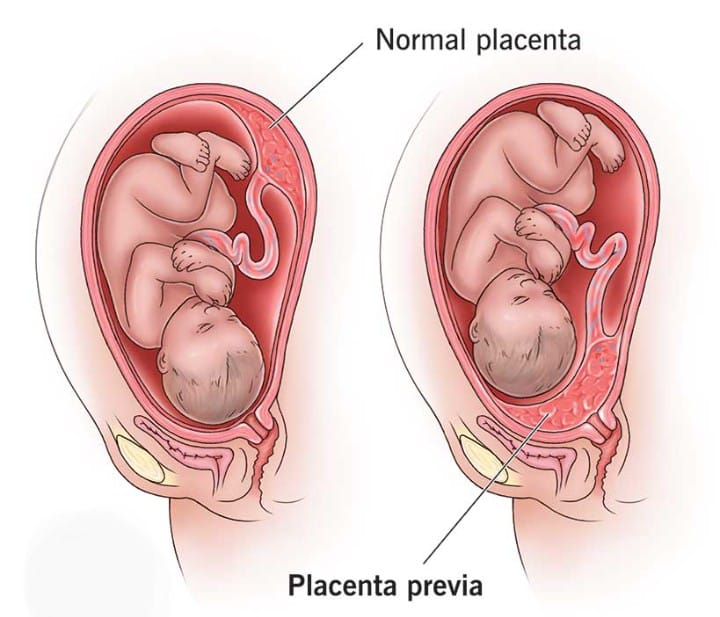
When the placenta partially or completely implants near or above the internal os of the lower segment of the uterus it is called “placenta previa”. 1/3 cases of antepartum hemorrhage are due to placenta previa.
Etiology:
The exact cause of placenta implantation in the lower uterine segment is unknown.
Some theories are given below:
Dropping Down Theory:
According to this theory, the fertilized ovum drops down in the lower uterine segment and implants in the same setting.
Persistence of chorionic activity
It explains the formation of the capsular placenta from the chorion coming in contact with the decidua vera of the lower segment of the uterus.
Defective decidua
In this the chorionic villi are spread over a large area of the uterine wall to receive nourishment.
During this process, not only does the placenta become membranous but implantation in the lower part of the uterus may occur.
Large Surface Area of Placenta:
Because of the big surface area like twins, the placenta implants in the lower segment.
High Risk Factors:
Multipara.
Increase maternal age
( > 35).
Having a history of privy lower segment caesarean section (L.S.C.S).
If any other scar is present in the uterus due to it.
Big Placental Size and Abnormalities,
Placental hypertrophy due to smoking,
Privy curettage.
Types of placenta previa:
There are four types of placenta previa depending on the degree of extension of the placenta into the lower segment of the uterine cavity.
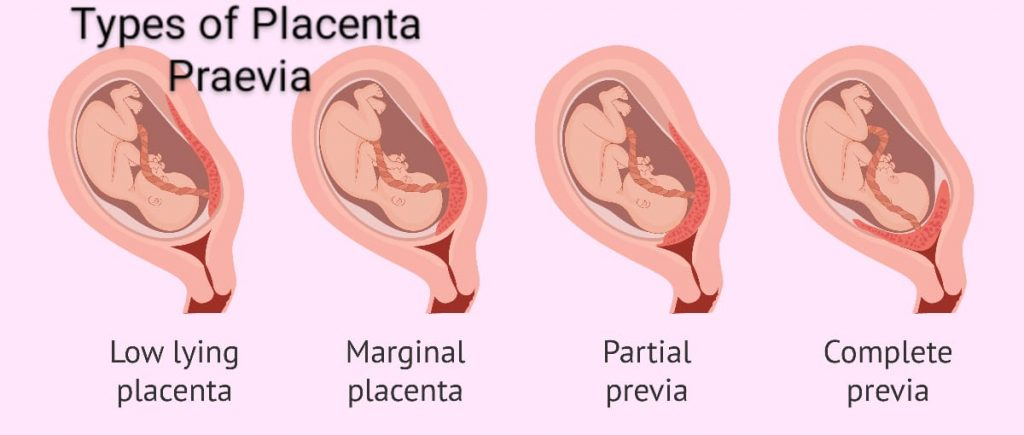
1) Type I (lateral placenta previa),
2) Type II (Marginal placenta previa),
3) Type III (Incomplete placenta previa),
4) Type IV (Complete placenta previa)
1) Type I (Lateral placenta previa):
In this type no major part of the placenta is attached to the upper segment but only the lower margin enters the lower segment but does not reach the os.
2) Type II (Marginal placenta previa):
In this type, the placenta only reaches the margin of the internal os but does not cover it. If the placenta is anterior, vaginal birth is possible, blood loss is average, and the risk of fetal hypoxia is higher than maternal shock.
3) Type III (Incomplete placenta previa): Placenta does not cover the internal os centrally but partially when the cervix begins to efface and dilate in late pregnancy, bleeding occurs due to lower stretch.
4) Type IV (Complete placenta previa): In this the placenta covers the internal os even when it is fully dilated. Severe haemorrhage occurs and caesarean section is required to save the life of mother and baby.
Sign and Symbols
symptoms
vaginal bleeding,
Bleeding is sudden.
Bleeding is painless.
Bleeding is causeless.
Bleeding is recurrent.
Bleeding is unrelated to activity and often occurs during sleep and the patient is alarmed upon waking to find himself in a pool of blood.
In placenta previa, the blood is bright red because of bleeding from a separated ytero-placental sinus. Sign
Patient has evidence of late pregnancy.
Evidence of blood loss is also seen such as shock, anemia depending on the degree of hemorrhage.
Abdomen
In this, the size of the uterus is according to the gestational period.
Uters feel soft, relaxed, and elastic.
A breech, transverse, unstable lie shows malpresentation.
The head is floating.
A fetal heart sound is often present.
Bright red blood is seen in placenta previa.
Diagnostic evaluation:
Diagnostic evaluation is done by two methods:
1) Placentography,
2) Clinically
1) Placentography: a) Sonography: Trans abdominal ultra sound
(TAS).
Trans vaginal ultra sound
(TVS).
Transperineal ultrasound.
Magnetic Resonance Imaging (MRI),
radiography,
radioactive isotope,
2) Clinically:
By Internal Examination (Double Setup Examination),
Direct visualization daring cesarean section,
Management of placenta previa:
Principles of management of placenta previa
To prevent injury to the fitus,
To reduce the risk of infection,
To control vaginal bleeding,
To promote health and reduce anxiety.
Management:
Provide adequate amount of antenatal care to the patient to improve the health status of the mother.
Perform an ultrasound at 20 weeks followed by a repeat ultrasound at 34 weeks to confirm the type of placenta previa.
Instruct the pregnant woman to rest in bed and then gently palpate the uterus for tenderness and tone.
To properly assess the amount of blood loss.
Color of bleeding and complete blood count (CBC) test.
Inj to patient as per hospital policy and prescription. Provide Morphine 15 mg IM.
Properly assess the amount of blood loss the client has suffered.
To properly note the client’s vital signs like,
temperature,
pulse,
respiration,
Blood pressure.
To properly assess the client for anemic condition or not.
To check the fetal heart sound regularly and frequently.
Abdominal examination of the pregnant woman followed by note of fetal heart sound and proper note of any tenderness present in the uterus.
Do not perform vaginal examination in the condition of placenta previa as it may increase bleeding.
Properly monitoring pregnant women for continuous or intermittent bleeding.
Arrangements should be made to shift the pregnant woman to another well equipped hospital having blood transfusion facility, caesarean section facility and neonatal care unit if required.
If the client has a hemorrhagic condition, start intravenous dextrose normal saline drips.
Advise the client to avoid stress and advise to take complete bed rest.
When the client is admitted to the hospital follow the following treatment viz.
Providing immediate attention,
Then properly planning what type of treatment is required.
In the immediate assessment, the amount of blood loss the client has suffered, his general condition, his pallor, pulse rate and blood pressure should be properly noted.
Send blood samples immediately to the laboratory for cross-matching and assessment of hemoglobin levels.
Start an infusion of normal saline to the patient.
Keeping blood ready to hand for transfusion after cross matching of blood.
Perform gentle abdominal palpation to assess the presence of any active bleeding.
Formulation of line of treatment:
In this, proper treatment should be provided according to the condition.
The hemoglobin level should be properly estimated and should be 10 gm or more.
Expectant treatment should be provided till 37 weeks are completed.
Termination in any of the following conditions viz:
Recurring hemorrhage,
dead fits,
Fetus is a congenital malformation,
India If there is uterine growth retardation (IUGR), termination is performed in such conditions.
Specific treatment is started after admission to the hospital. As such, vaginal examination is performed in the operation theater to properly prepare for cesarean section.
After examination the membrane is artificially ruptured then oxytocin is started then delivery is conducted as per condition.
If the labor process is progressing satisfactorily without any bleeding, perform vaginal delivery.
If the bleeding is continuous, the pregnant woman should undergo caesarean section.
Assess presentation if baby is malformed or dead, ventous delivery if vertex presentation and breech delivery if breech.
- Abruptio Placenta:
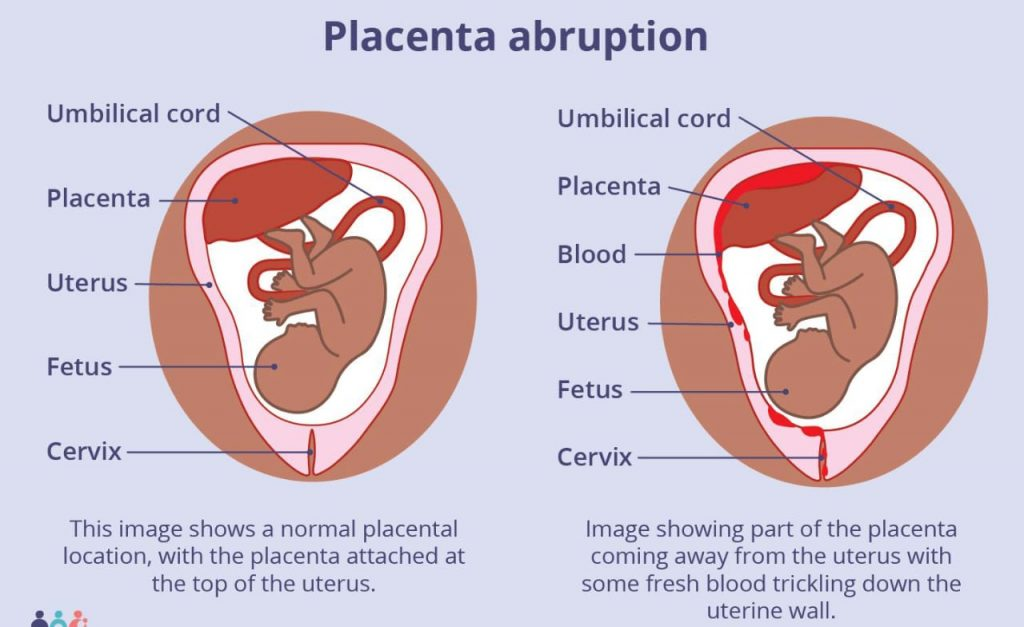
Definition:
Abruptio placenta is a form of antepartum hemorrhage (APH) in which the normally situated placenta prematurely separates from the uterine wall and causes bleeding called abruptio placenta.
Types of Abruptio Placenta:
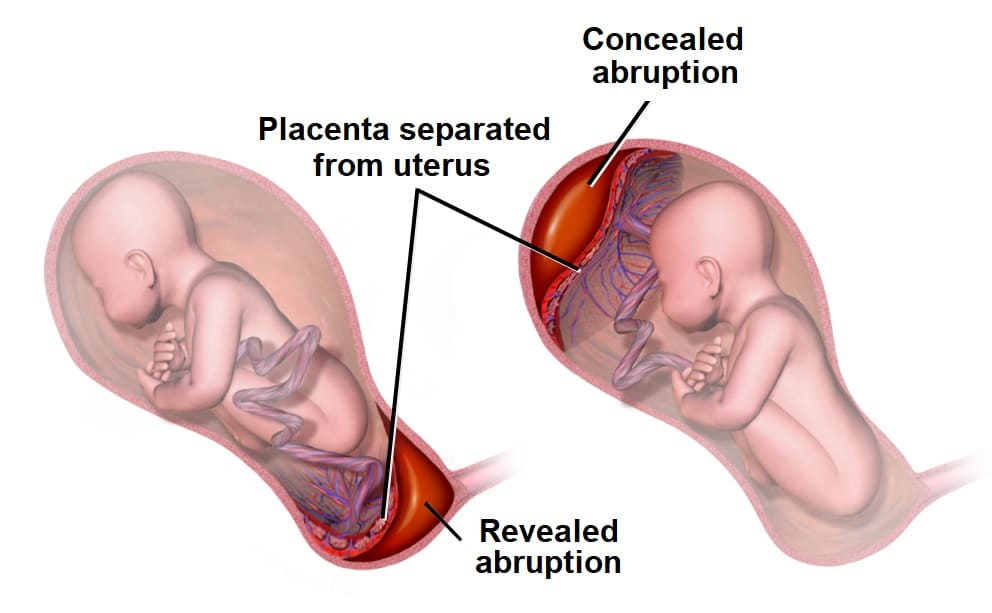
There are mainly 3 types of placental abruption namely,
1) Revealed,
2) Concealed,
3) Mix.
1) Revealed or mild type: In this type blood comes downwards between the membrane and decidua after the separation of the placenta i.e. the blood is externally visible this type is a common type of abruptio placenta.
2) Concealed: In this concealed type of abruptio placenta, the blood collects behind the separated placenta or between the membrane and decidua i.e. the blood is not externally visible. This type is a rare type of abruptio placenta.
3) Mix: In this type, the blood is partially collected inwardly (concealed) and partially visible outwardly (revealed), i.e., there are both revealed and concealed types of placental abruption. It is called mix abruptio placenta.
Etiology:
The exact cause is unknown,
5 th is more common in gravida,
Due to mother’s advanced age,
Due to poor socioeconomic condition,
malnutrition,
smoking.
Other factors like,
preeclampsia,
Sudden uterine decompression,
short cord,
Supine hypotensive syndrome,
Folic acid deficiency,
Due to torsion of the uterus,
Due to direct trauma to toe, high parity or uterine over distension.
Risk Factors:
sort cord,
Due to premature rupture of membranes,
Due to uterine leiomyomas,
chorioamnionitis,
polyhydramnios,
Anticoagulant therapy,
No use of cocaine,
smoking,
Due to trauma to the abdomen,
hypertension,
Due to intra-uterine growth retardation (IUGR),
Diagnostic evaluation
History Collection,
Physical Examination,
Blood test A hematocrit, urea, electrolyte
, to assess fibrinogen level, thrombin time, blood group and cross match.
Urine Examination,
Placentography,
ultrasound,
Cardiotocography.
Symptoms and signs:
Painful vaginal erection,
Tender board like uterus (especially when concealing hemorrhage or vaginal bleeding),
Fit bradycardia and late deceleration,
Fetal Heart Rate (FHR) being Absent,
Signs of mourning being present.
Bleeding is caused by preeclampsia or trauma.
Bleeding can be a mix of visible and invisible bleeding.
Blood is of dark red color.
In this, the condition of anemia is seen more than the amount of visible blood loss.
Abruptions of the placenta are seen in 1/3 of cases of features of preeclampsia.
In abruptio placenta, the height of the uterus is enlarged more than the gestational age.
Abruption of placenta ma uterus can be tense, tender and rigid.
Abruptio placentae malpresentation is unrelated and may also involve the head.
Heart sounds are often absent in abruptio placenta.
The placenta is found in the upper segment of the uterus.
Management:
Prevention:
The objectives of the intervention are as follows, viz.
To eliminate the responsible causes of placental separation.
Early identification of preeclampsia and hypertensive disorders and providing effective treatment.
Properly correct the patient if he is anemic.
To start early treatment to prevent patient complications.
Avoid trauma, sudden decompression of uterus, supine hypotension.
To shift the patient immediately to the maternity hospital.
Complete assessment of the patient in the hospital.
Properly assess the amount of blood loss the patient has.
Properly assessing the maturity of fits.
Assess the general condition of the patient properly.
Perform a complete diagnostic evaluation of the patient. Like, blood hemoglobin level,
Hematocrit level,
coagulation profile,
ABO and RH grouping, doing urine analysis.
Providing Ringer’s Latest (RL) solution to the patient.
Prepare the patient for proper blood transfusion.
Close monitoring of maternal or fetal condition.
Prepare the patient for delivery.
If the patient has any complication, manage it properly.
Definitive Treatment: If the patient is in labour, perform low rupture of membranes, if necessary, start oxytocin drip followed by vaginal delivery.
Provide adequate amount of antenatal care to the patient to improve the health status of the mother.
Instruct the pregnant woman to rest in bed and then gently palpate the uterus for tenderness and tone.
To properly assess the amount of blood loss.
Color of bleeding and complete blood count (CBC) test should be done.
Properly assess the amount of blood loss the client has suffered.
To properly note the client’s vital signs like,
temperature,
pulse,
respiration,
Blood pressure.
To properly assess whether the client has an anemic condition or not.
To check the fetal heart sound regularly and frequently.
Abdominal examination of the pregnant woman followed by note of fetal heart sound and proper note of any tenderness present in the uterus.
Proper monitoring of pregnant women for continuous or intermittent bleeding.
Arrangements should be made to shift the pregnant woman to another well equipped hospital having blood transfusion facility, caesarean section facility and neonatal care unit if required.
If the client has a hemorrhagic condition, start intravenous dextrose normal saline drips.
Advise the client to avoid stress and advise to take complete bed rest.
When the client is admitted to the hospital, follow the following treatment such as, giving immediate attention,
Then properly planning what type of treatment is required.
In the immediate assessment, the amount of blood loss the client has suffered, his general condition, his pallor, pulse rate and blood pressure should be properly noted.
Send the blood samples immediately to the laboratory for cross-matching and assessment of hemoglobin levels.
Start an infusion of normal saline to the patient.
Keeping blood ready to hand for transfusion after cross matching of blood.
Perform gentle abdominal palpation to assess the presence of any active bleeding.
Formulation of line of treatment:
In this, proper treatment should be provided according to the condition.
The hemoglobin level should be properly estimated and should be 10 gm or more.
Expectant treatment should be provided till 37 weeks are completed.
Termination in any of the following conditions viz:
Recurring hemorrhage,
dead fits,
Fetus is a congenital malformation,
India If there is uterine growth retardation (IUGR), termination is performed in such conditions.
Specific treatment is started after admission to the hospital. As such, vaginal examination is performed in the operation theater to properly prepare for cesarean section.
After examination the membrane is artificially ruptured then oxytocin is started then delivery is conducted as per condition.
If the labor process is progressing satisfactorily without any bleeding, perform vaginal delivery.
Advise the pregnant woman to perform caesarean section if the bleeding is continuous.
Assess presentation if baby is malformed or dead, ventous delivery if vertex presentation and breech delivery if breech.
Properly assess any complications the patient has and take proper measures to prevent them.
- Vesicular Mole:
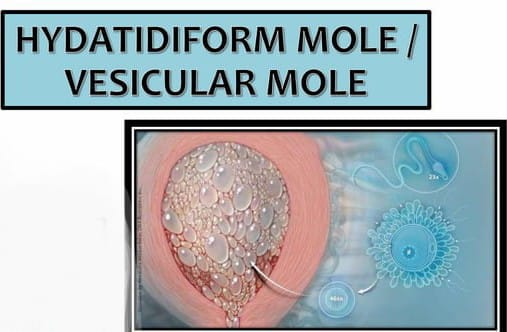
Definition
A vesicure mole is also called a hydatidiform mole (H.mole). This is an abnormal condition of the placenta. In which few degenerative and few proliferative changes occur in the young chorionic villi and due to this cluster (lump like shape) is formed in the cyst. And since it resembles a hydatid cyst, it is called a hydatidiform mole or vesicular mole. When the chorionic villi transforms into a mass of translucent vesicles, it forms a structure like a bunch of grapes, it is called a hydatidiform mole.
etiology
Its exact cause is unknown,
Due to ovular defect,
It can also be due to the following reasons:
Hemorrhagic pregnancy,
In most teenage pregnancies,
In women over 35 years of age,
Due to faulty nutrition habits such as low protein intake,
Due to low calorie intake in the diet,
Due to disturbed maternal immune mechanism,
Because of the history of hydatidiform mole,
Women whose ovulation is simulated by clomiphene,
Have poor socioeconomic condition.
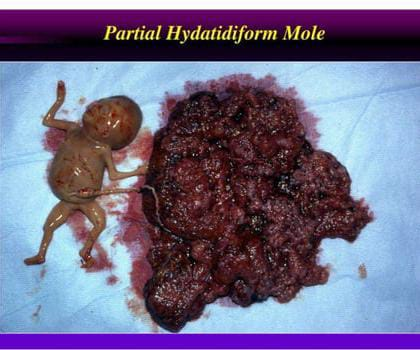
Type of vesicular mole
There are two types of vesicular mole:
1) Complete Mall,
2) Incomplete Mall
1) Complete mole: Complete or classic H. mole forms when an egg whose nucleus is lost and inactivated is formed due to fertilization.
In this the mole resembles a bunch of white grapes.
In this case, the fluid-filled vesicles grow rapidly, causing the uterus to become larger than the expected duration of pregnancy.
Complete mole involves the fetus, placenta and amniotic membrane.
A complete mole can also progress to carcinoma and does not contain an embryo.
2) Incomplete Mall
These contain embryonic or fetal parts and an amniotic sac is present.
Congenital anomalies are present in these.
These contain underdeveloped embryos that fail to survive.
Signs and Symptoms
Abnormal vaginal bleeding,
Bleeding is brownish and watery as the blood mixes with the fluid from the ruptured system giving the appearance of a discharge.
Thus, painless vaginal bleeding occurs during the fourth and fifth months of pregnancy.
Lower abdominal pain.
A patient appears to be sick without any reason.
Hyperemesis gravidarum occurs.
Early features of pre-eclampsia are seen at periods less than 20 weeks.
Pulmonary embolism causes dyspnoea.
The uterus appears larger during the gestation period.
Thyrotoxic features are observed such as,
Tremors, and anxiety etc.
Fetal heart sound and fitus patas are absent.
Expulsion of grape-like vesicles from the vaginal area.
USG:=Snow storm apparition can be seen.
Diagnostic evaluation
full blood count,
ABO and Rh grouping and blood clotting test,
Hepatic, renal and thyroid function tests,
sonography,
Straight X-ray Abdomen,
Pelvic Angiography,
CT scan and MRI.
Management
Provide proper supportive therapy to the mother so that the lost blood can be restored.
When a vesicular mole is diagnosed, the risk of choriocarcinoma can be prevented by evacuating it by suction and surgical curettage as early as possible.
To test ABO and Rh in mother’s blood investigation.
Start a fluid infusion to the mother immediately.
Provide blood transfusion to the mother if excessive amount of blood has been lost.
Emptying the uterus through a suction procedure means suctioning the mole.
After the end of suction, when no vesicles enter the suction cannula and the uterine cavity contracts, start by adding 10 units of oxytocin to the glucose drip and introduce 0.2 mg of methargin into the drip.
Oxytocin should be avoided during the Sachsen procedure because it causes embolization of vesicles in the patient’s venous channel.
Curating gently and properly from the uterine cavity by blunt curettage.
After curating, the vesicles should be properly sent to the laboratory for histological examination.
To properly monitor the mother’s vital signs like pulse rate, respiration, and blood pressure every half hour.
Administer 10 units of oxytocin to the mother intramuscularly (IM) or, if intravenously (IV), 20 units of oxytocin in 500 ml of normal saline or Ringer’s lactated solution to the patient to prevent postpartum hemorrhage.
Advise the patient to undergo hysterectomy if the patient is above 40 years of age.
Advising the mother to follow up regularly.
Administer Anti D immunoglobulin 100 microgram (IM) if mother is Rh negative.
Advising women to use contraceptive method properly.
Advising the mother to avoid pregnancy for one year.
Advise the mother to follow up the athlete for at least two years. Its aim is choriocarcinoma
Find out.
Advising women to follow up every three months after 4 to 6 weeks of follow-up and athlete for 2 years includes assessment of women’s history collection, clinical examination.
- Hyperemesis gravidarum:
Severe type of nausea and vomiting in pregnancy which adversely affects the health of the mother including dehydration, weight loss and electrolyte imbalance and impairment in the daily routine activities of the mother is called “hyperemesis gravidarum”. .
Hyperemesis gravidarum (HG) usually occurs more frequently during the first trimester of pregnancy, usually starting around 4–6 weeks of pregnancy and symptoms persist until around 9–13 weeks. This period corresponds to the time when pregnancy hormones, especially human chorionic gonadotropin (hCG), are at their highest levels.
In most cases, symptoms of hyperemesis gravidarum begin to improve by the end of the first trimester, although some women in severe cases may experience symptoms that persist into the second trimester or throw out pregnancy. Nausea and vomiting are very common in primigravida and especially in women when they wake up in the morning.
Hormones like HCG, Oestrogen, Progesterone are responsible for vomiting. Nausea and vomiting are usually more common in primigravida and in the first trimester. If persistent vomiting occurs, there is a chance of dehydration, electrolyte imbalance, and aspiration of the vomitus.
Etiology:
Hormonal causes: Due to chronic increase in the amount of gonadotrophin, estrogen, and progesterone hormones,
psychogenic,
Due to deficiency of vitamin B, carbohydrate and protein,
Allergy/Immunologies
Symptoms and signs:

nozia,
Forceful vomiting,
abdominal pain,
electrolyte imbalance,
fever,
feel tired,
loss of appetite,
dehydration,
Changes in bowel movement,
Irritability,
lethargy,
malnutrition,
Dehydration and keto-acidosis symptoms: dry coated tongue, sunken ice, systolic blood pressure less than 100 mm Hg, breath acetone smell, tachycardia, hypotension, temperature increase. Jaundice is a late feature.
Diagnostic Evaluation:
History Collection
Take proper history of frequency duration and amount of vomiting.
Assess body weight properly.
Laboratory investigation.
Complete blood count test (CBC).
Assess the electret level.
Urine analysis.
Assessing blood glucose levels properly.
Assess liver function test properly.
Imaging studies.
Abdominal ultrasound.
Management
If the woman has a condition of severe hyperemesis gravidarum, she should be properly hospitalized.
Proper assessment of women.
Properly assessing a woman’s hydration status.
Properly assessing woman’s electrite balance and continuous observation of women.
Continuously assess the consistency, frequency, and duration of vomiting experienced by women.
Properly assess the woman’s hydration status and properly assess the woman’s vital signs.
Provide intravenous fluids to maintain the woman’s hydration status and prevent electrolyte imbalance.
Providing prescribed antiemetic medication to women. For example, promethazine (Phenargan), prochlorperazine (Stamtil), triflupromazine (Sequil), metaclopramide, hydrocortisone, etc.
Proper investigation of woman’s blood.
Provide small amount and easily digestible bland food to women if vomiting subsides.
To provide proper comfort measures to the child.
To properly maintain the patient’s fluid and electrolyte balance.
Advising women to maintain proper hygienic condition.
Maintaining a proper intake-output chart of the patient
Use proper aseptic technique and maintain universal precautions to prevent cross infection.
Collaboration with other health care personnel for proper care of women.
Providing education to parents to provide proper medication to women.
If the vomiting subsides, then advise the patient to intake water in a small amount and give advice to intake carbohydrate foods like biscuits, bread and toast, provide small and frequent feeds to the patient and then provide a full diet.
Advising women to take regular follow up.
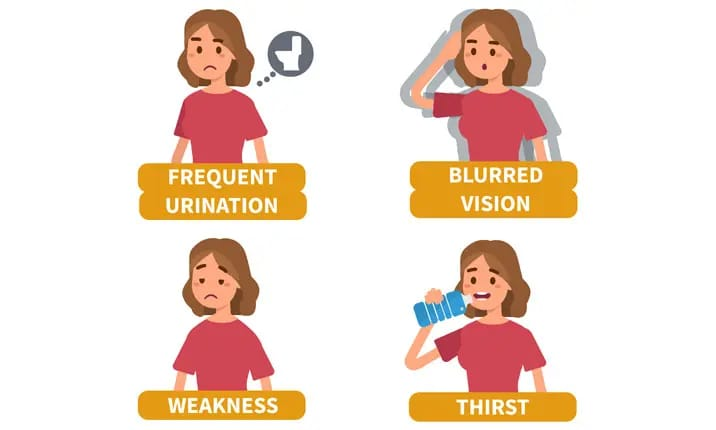
- Diabetes Mellitus

Diabetes is a chronic metabolic disorder in which carbohydrate, protein and lipid metabolism is impaired. Diabetes is a group of metabolic disorders in which the blood sugar level of a person’s blood is high. If there is an impairment, high blood sugar level is seen in the body, the “3 P” syndrome is mainly seen in diabetes mellitus.
1)P: Polyuria (passing too much urine)
2)P: Polydipsia (excessive thirst),
3)P: Polyphagia (very hungry).
GDM (Gestational Diabetes Mellitus):
Gestational diabetes mellitus is mainly seen in women and those women also develop diabetes mellitus due to glucose intolerance during pregnancy. Gestational diabetes refers to women who are diabetic during pregnancy. Gestational diabetes mellitus is a type of diabetes that occurs during pregnancy because hormonal changes during pregnancy lead to the development of insulin resistance.
Here, the mother does not have diabetes before pregnancy, so if a woman develops diabetes during pregnancy, the condition is called gestational diabetes. This condition can affect the baby’s health and development in many ways, requiring careful monitoring and management soon after birth to manage potential complications such as blood sugar, respiratory problems, jaundice and an increased risk of congenital anomalies.
Etiology:
Inherited
Environmental Factors
genetic factor,
obesity,
Due to hormonal imbalance during pregnancy.
Due to insulin deficiency.
Due to cell resistance to insulin despite insulin.
Due to too much sugar intake.
Due to sedentary life style.
Due to excess cholesterol in the body.
The growing fetus is supplied with nutrients and water by the placenta. A number of hormones are produced to maintain pregnancy (cortisol, estrogen, human placental lactogen) that can block insulin. This usually occurs at 20-24 weeks of pregnancy.
On the other hand, with the growth of the placenta, there is also an increase in hormonal production due to which insulin resistance increases. Normally, the pancreas makes extra insulin to combat insulin resistance, but when insulin production is not enough to offset the effects of placental hormones, gestational diabetes occurs.
Women with pre-existing diabetes have an increased need for insulin, e.g. An insulin dependent mother may require more insulin as the pregnancy progresses.
Symptoms and signs
Effects of Gestational Diabetes on Fits:
The effect of gestational diabetes on the fetus is of concern because the increase in maternal blood sugar levels during pregnancy is transferred to the fetus. This causes insulin to be secreted in greater amounts from the child’s body, causing tissue growth and deposition of fat, causing the newborn to be larger than expected for gestational age (macrosomia).
Newborns of diabetic mothers are at risk of congenital anomalies. Congenital anomalies such as heart, brain, spinal cord, urinary tract and gastrointestinal system problems can occur.
Other Conditions:
hypoglycemia,
macrosomia,
birth injury,
Respiratory distress.
Symptoms and signs:
Lazy size baby (due to excessive fat and glycogen accumulation in tissues),
In Face and Chikama AD,
Hyperbilirubinemia,
Signs of hypoglycemia:
twitching,
lethargy,
Caesar,
Difficulties in feeding,
apnea,
Cyanosis.
Signs of respiratory distress:
cyanosis,
nasal flaring,
grunting,
tachypnea,
Other Symptoms:
The “3 P” syndrome is predominantly seen in diabetes mellitus.
1)P: Polyuria (passing too much urine)
2)P: Polydipsia (excessive thirst),
3)P: Polyphagia (very hungry).
feeling tired
Weakness.
Difficulty seeing.
Tingling and numbness sensation in hands and feet.
Dry skin.
If sore, it heals slowly.
Frequent infections.
Nozia.
Vomiting.
Wound healing process is slow
Weight loss.
Diagnostic Evaluation:
History Collection,
Physical Examination,
1) Fasting blood sugar (FBS)
This test is done without eating or drinking anything for at least eight hours. Its normal value should be below the desiclator at 110 mg/dl and if the fasting blood glucose level is more than 125 mg/dl Diagnosed as diabetes.
Random blood sugar (RBS)
This test requires no preparation at any time the sample is taken but if the random blood glucose is greater than 200mg/dl per milliliter, it is indicated as diabetes.
PP2bs (Postprandial Blood Sugar)
This test is done after 2 hours after taking a full meal.
Normally the blood glucose level comes down to the fasting glucose level two hours after a meal, but if someone has smoked or drank caffeine, there is an alteration in it.
glycosylated HB
In this test, this test is done to assess how much glucose is attached to the blood molecule.
Glycosylated Albumin:
Glucose is usually attached to albumin so glycosylated albumin is used to assay average glucose levels.
oral glucose tolerance test.
In this, 150 mg of carbohydrate is provided to the patient for three days. After that, the fasting blood glucose level of the patient is checked. After that, the client is given 75 grams of glucose to drink, after which the glucose tolerance level of the patient is checked.
ketonuria
If ketones are present in the urine, it indicates that the body uses fat as a source of energy.
proteinuria:
If protein is present in the urine, it indicates that the protein is used as a major source of energy.
Serum lipid profile.
Serum BUN.
Serum creatinine.
Management:
Principal of Management
To eliminate the symptoms of hyperglycemia.
To reduce microvascular and macrovascular complications of diabetes mellitus.
Reducing blood glucose levels.
The patient can achieve a normal life style as far as possible.
Blood glucose levels can be reduced using patient education, dietary management, exercise and pharmacological therapy.
Patient Education
To provide proper health education to the patient and his family members.
In which to teach how to do self-monitoring of glucose.
Teach the patient how to administer insulin.
Teaching the management of hypoglycemia.
Providing education to patients about foot and skin care.
Teach diabetes management before exercise, during exercise, and after exercise.
Providing education about patient’s life style modification.
Properly check for any signs and symptoms of respiratory distress.
Dietary management
Aim of Dietary Management
To relieve the symptoms of hyperglycemia.
If treating hyperglycemia to reduce symptoms of hypoglycemia.
Reducing the overall blood glucose level of the body.
Avoiding diets that increase blood glucose levels.
Ask the patient to lose weight if he is obese.
Make the patient have regular food intake.
Ask the patient not to take sugar.
Ask to follow a diet that contains adequate amounts of protein, carbohydrates and fat.
The main goal of dietary management is to improve metabolic control in the diabetic client.
Maintaining the patient’s blood glucose level and lipid level.
Making a daily food intake plan of the patient.
Making a plan for weight management of the patient.
Provide adequate nutrition to the patient.
A person’s lifestyle and habits play an important role in controlling and managing the disease.
A balanced nutritional diet is very important in all patients.
Ask the patient to increase the protein intake in his diet. Excessive protein intake increases renal function. and glomerular filtration rate increases.
Maintaining the level of fat in the patient’s diet, maintaining the daily cholesterol level in the diet and limiting saturated fat and cholesterol.
Provide carbohydrates as per the patient’s body requirement.
Asking the patient to consume adequate amounts of carbohydrates that can maintain the body’s energy requirements.
Foods that are sweet and contain sugar should not be taken, such as cakes, ice creams, jams, etc.
Checking the patient’s blood glucose level regularly.
Carbohydrate should be taken in small amount before exercise.
The patient should be asked to check the amount of glucose, ketones and albumin in the urine and all these substances are observed during fasting.
Caloric restriction for obese clients.
Exercise:
Advise the patient to do regular exercise to prevent exacerbation of his disease condition.
Ask for regular walking.
Ask for adequate amounts of carbohydrates before and after exercise.
Pharmacological management is responsible for maintaining blood glucose levels.
If insulin is given on the abdomen, its absorption is fast. When given on arm and leg, its absorption decreases.
Oral medication is provided to the patient.
Oral Antidiabetic Agents:
1)sulfonyl urea,
2) meglitinides,
3) thiazolidinediones,
4)bigunides,
5) alpha glucoside inhibitor.
Proper teaching of the patient should be provided for proper administration of insulin because if insulin is not administered properly, tissue damage or conditions like insulin shock may occur.
Nursing Management:
1) Impaired nutritional status more than body requirement related to intake excess of activity expenditure.
The primary goal of the diet plan is to control the glucose level, thereby assessing the patient’s glucose level, and assessing the patient’s lifestyle, cultural background, activity level, dietary habit and food preference.
Ask the patient to take food in adequate amount and also to take snacks in between.
Arrange for an extra mile before the patient engages in physical activity.
Administer insulin as per doctor’s order.
2) Imbalance fluid volume related to increased stress hormone as evidenced by polyuria.
To assess the patient’s intake output chart.
Ask the patient to take oral fluids.
Provide intravenous fluid to the patient.
Checking the patient’s serum electrolyte level.
To check patient’s vital sign.
3) Activity intolerance related to weakness as evidenced by limited activities.
Assess the patient’s activity level.
Activity planning of the patient.
Provide analgesic medication to the patient before resuming activity.
Ask the patient to rest between activities.
Provide carbohydrate and protein rich food to the patient.
Providing the prescribed medicine to the patient.
4) Knowledge deficit related to cause and disease as evidence by asking questions.
Assessing the patient’s knowledge level.
Provide education to patients about diabetes diet.
Providing education to patients about foot and nail care.
Provide education to the patient or keep his feet covered with soft shoes.
Provide education to patients about self-administration of insulin.
5) Fear related to insulin injection.
Monitor the patient’s blood glucose level.
Provide education to patients about self-administration of insulin.
Provide patient education about complications of insulin therapy.
Provide education to the patient about the signs and symptoms of hyperglycemia and hypoglycemia.
- PIH (Pregnancy Induced Hypertension):
PIH is called pregnancy induced hypertension. In which the woman does not have any condition of hypertension before pregnancy but if the blood pressure of the woman increases to 140/90 mmhg or more due to pregnant uterus, this condition is called pregnancy induced hypertension.
It is generally divided into three parts viz.
- Gestational hypertension,
2.Preeclampsia, - Eclampsia
- Gestational hypertension:
A blood pressure of 140/90 mmhg or more in a normotensive pre-pregnancy woman after 20 weeks of pregnancy or in the first 24 hours of delivery is called gestational hypertension.
In its criteria,
The underlying cause of hypertension is absent.
Other signs of pre-eclampsia are not seen.
Most cases are at 37 wks gestation or more.
After delivery, the blood pressure becomes normal within 6 hours.
- Preeclampsia:

Preeclampsia is a complication of pregnancy. In which its etiology is unknown but it is a multisystem disorder. In which high blood pressure is seen along with other organs are also damaged and most commonly liver and kidney are affected. Preeclampsia occurs mainly after the 20th week of pregnancy and also differs in severity.
Among the main symptoms of preeclampsia,
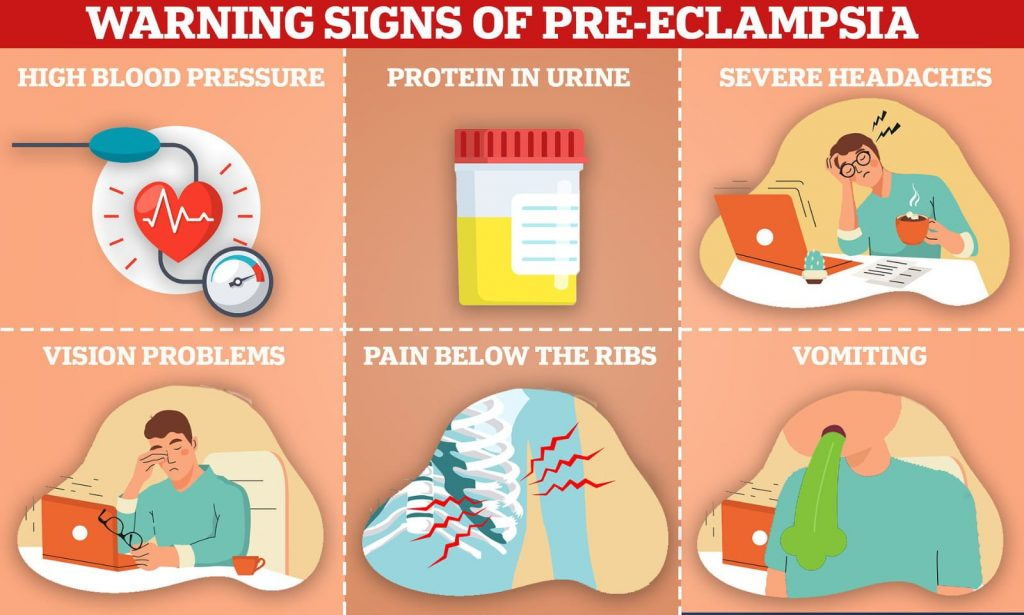
1) Hypertension that increases above 140/90 mmHg (hallmark sign of preeclampsia),
2) Edema (mainly in hands, face, and legs) and excessive weight gain.
3) Proteinuria (excess amount of protein found in urine),
4) Albuminuria (albumin present in urine).
The symptoms of preeclampsia are seen after the 20th week.
Etiology:
The exact cause is Unon.
Elderly or young primi gravida,
Due to hypertension during pregnancy,
Having a family history of hypertension,
Due to placental abnormalities like,
Hyperplacentosis: Excessive exposure of chorionic villi,
Ex: molar pregnancy, twins, diabetes,
Placental ischemia.
obesity,
Pre-existing vascular disease,
thrombophlebitis,
Complications with pregnancy like,
Multifetal pregnancy,
hydatidiform pregnancy,
hydroamniosis,
Rh.Incomplicity,
Medical diagnoses like nephritis and diabetes mellitus,
Vasospasm: Dilator depression is due to increased sensitivity of circulating pressors such as angiotensin II and prostaglandins.
Dysfunction of endothelial cells reduces placental perfusion.
It can also be caused by immune complex diseases.
It can also be caused by not having enough protein, calcium, magnesium, vitamin E and A in the diet.
Due to genetic factor
Due to immunological factors.
Due to endocrine factor.
Due to environmental factors.
Due to chronic health conditions such as hypertension, gestational diabetes, kidney disease and autoimmune disorders.
Classification of pre-eclampsia:
1.Primary 70%
- Secondary 30%
1.Primary (70%) It is of two types:
a.Pre-eclampsia.
b.Eclampsia with convulsions.
2.Secondary 30%:
a Pre-eclampsia, eclampsia superimposed on chronic hypertension (25%).
b Pre-eclampsia superimposed on chronic nephritis (5%), eclampsia.
Or
Mild : Proteinuria and hypertension present. Blood pressure is less than 170/110 mmHg.
Moderate : Proteinuria and hypertension are present. Blood pressure is greater than or equal to 170/110 mmHg.
Severe: Proteinuria and hypertension present. Blood pressure rises above 170/110 mmHg and pregnancy is less than 32 wks or with maternal complications, e.g. Help, eclamptic fit.
Symptoms and Signs:
Signs and symptoms of pre-eclampsia can vary according to severity.
It may include the following:
Main symptoms: High blood pressure (hypertension):
Blood pressure is persistently above 140/90 mmHg.
Proteinuria:
Protein is detected in urine.
Edema: Edema, especially in the arms, face, or legs. While a small amount of edema is normal during pregnancy, sudden or sudden edema, and if accompanied by other symptoms and signs, may indicate pre-eclampsia.
Albuminuria Finding albumin in urine.
Alarming Symptoms:
Headache: Often there is a dull and persistent headache that does not get relieved even with treatment.
Visual disturbances: These may include blurred vision, flashing lights or spots.
Pain in the upper part of the abdomen: especially in the upper part of the right abdomen, which suggests involvement of the liver.
Decrease in urine output:
Oliguria (reduced production of urine)
Other Symptoms:
Nausea and vomiting: especially if it is persistent and heavy.
Shortness of breath: especially if associated with fluid accumulating in the lungs (pulmonary edema).
Hyperreflexia: Exaggerated reflex response.
Thrombocytopenia: Low number of platelets, which can lead to blood clotting problems.
Decreased fetal movement: Less than normal fetal movement at that stage of pregnancy.
It is important to note that not all women with pre-eclampsia will experience all of these symptoms. The presence of hypertension and proteinuria after 20 weeks of pregnancy in previously normotensive women are the primary diagnostic criteria for pre-eclampsia.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Urine Test: To assess proteinuria.
24 hours urine collection for protein level measurement.
Ophthalmic Examination.
Blood tests for liver and kidney function such as
Serum uric acid,
blood urea level,
Serum creatinine level,
Hepatic/liver enzymes
Antenatal fetal monitoring:
Clinical Examination,
Daily Fit Kick Count,
ultrasonography,
cardiotocography,
Umbilical artery flow velocimetry,
Biophysical profile: including ultrasonography and non-stasis test to assess fetal breath test and muscle tone.
Complications:
- Maternal complications:
During pregnancy:
eclampsia,
Accidental hemorrhage,
Oliguria and Anuria,
Vision is to be demined,
Preterm labor.
HELLP Syndrome:
Hemolytic anemia, elevated liver enzymes, low platelet count,
During Labour: Eclampsia,
Shock, sepsis.
Fetal Complications: Intra uterine death, intra uterine growth restriction, asphyxia, prematurity.
Remote complications:
Residual hypertension,
severe preeclampsia,
Chronic nephritis.
Management:
Management of pre-eclampsia involves close monitoring of the mother, prevention of complications, and nursing management to improve the well-being of the mother and fetus.
1) Assessment and Monitoring
Vital sign
Continuous vital sign monitoring of the mother including,
pulse,
blood pressure,
Respiration, etc
Temperature is involved.
Fluid intake output monitoring
Monitoring mother’s intake output chart. Because of this, kidney function and fluid balance can be monitored.
Fittal assessment
Assessing fit’s heart rate and fit’s movement in fit assessment.
Assessment of symptoms
Regularly assessing the mother’s signs and symptoms
one head,
Visual Distance,
epigastric pain,
And to assess the condition of edema or not.
2) Bedrest and positioning
Advise the mother to rest on her left side to improve uteroplacental circulation and reduce vena cava compression.
Advise the mother to do limited mountain activity to prevent blood pressure from increasing.
3) Fluid management
Maintain the mother’s intravenous access so that her hydration status can be maintained and medication can be administered.
Continuously monitoring the intake output of the mother so that the hydration status of the mother can be maintained and fluid overloading of the mother can be prevented.
4) Medication administration
Providing the mother with medication properly prescribed by the healthcare provider.
such as,
Antihypertensive drug to control blood pressure
Ex:=
labetalol
(Orally 100 mg (TDS)
I.V infusion :=1-2 mg / min.),
Hydralazine (Orly
100 mg/day in four divided doses).
If the mother has a condition of fluid overload, provide diuretic medication such as,
Ex: Lasix (Frusemide) (40 mg up to 5 days).
If the mother has a condition of convulsions, provide anticonvulsive medication.
Ex:=Magnesium Sulphate.
Providing sedative meditation to the mother.
Ex:=
Diazepam 10-20 mg I.v. followed by:
Tab. Diazepam 5mg (TDS),
Tab.phenobarbitone 60 mg (hs).
If the mother has a condition of constipation, provide a mind laxative at bedtime.
Ex:= milk of magnesia.
Maintain mother’s progress chart in which,
Monitoring blood pressure four times during the day.
Daily weight monitoring of mother and condition assessment of edema.
Monitoring mother’s fluid intake and urine output.
Urine examination of mother including protein urea condition assay.
To do mother’s blood investigation in which mother’s
hematocrit,
platelet count,
uric acid,
creatinine level,
And liver function test (LFT) should be done once a week.
Ophthalmic examination of the mother.
Continually assess fit’s well-being.
5) Monitor for complications
Assessing the mother for severe pre-eclampsia and warning signs and symptoms of eclampsia including,
Scissors, severe headache,
epigastric pain,
Assess for blurred vision.
Mother’s HELLP Syndrome:
(1)H :=hemolytic anemia,
(2) EL:=elevated liver enzymes,
(3) LP:= Low Platelet Count)
Assessing complications like
6) Patient education
Advising the patient and his family members for regular antenatal checkup of pregnant women so that the condition of pre-eclampsia can be detected early.
To provide complete information and education to pregnant women and their family members about the condition of pre-eclampsia, its causes, symptoms and signs, diagnosis, complications and its treatment.
Advise the pregnant woman and her family members to seek immediate medical treatment due to
The condition of pre-eclampsia can be prevented from developing excessively.
7) Emotional support
To provide proper reassurance and psychological support to the patient and his family members.
Advising the patient and his family members to improve the proper coping mechanism.
8) Collaboration and Communication
Proper collaboration with other health care personnel for proper treatment of the mother including communication with obstetrician, neonatologist and anesthesia provider so that the mother can be properly cared for.
Proper communication and collaboration with other health care team members for mother’s care and providing proper treatment to mother.
9) Preparation for Delivery
Maternal pre-eclampsia condition,
Preparation for timely delivery to prevent complications to mother and baby based on gestational age and severity.
Keep all necessary emergency equipments like airway, catheterization equipments, oxygen, suction apparatus, emergency medicine tray and caesarean section tray etc. properly prepared.
10) Follow up and discharge planning
Planning the post partum care of the mother and properly planning how to recover the mother from the condition of pre-eclampsia.
Advise the client and his family members for proper follow-up of the client and for continuous monitoring of blood pressure.
Thus nursing management of pre-eclampsia is provided for continuous monitoring of pregnant women, timely intervention, comprehensive care and prevention of complications for mother and baby.
- Eclampsia Definition:
Eclampsia is a life threatening complication that arises during pregnancy in women. The term eclampsia is derived from the Greek word “like a flash of lightning”. Tonic-clonic convulsions or coma as a complication of pre-eclampsia is called eclampsia. When A condition of pre-eclampsia in which,
Hypertension,
Edema (weight gain),
Proteinuria
(Protein in urine) and
If albuminuria (albumin present in urine) becomes complicated and converts to conditions like convulsions and coma, it is called “Eclampsia”. This is an obstetrical emergency. It is important to take immediate measures to manage it.
Etiology:
The exact cause is Unon.
Elderly or young primary gravida,
Due to hypertensive disorders during pregnancy: Ex: Preeclampsia,
Having a family history of hypertension,
Due to placental abnormalities like,
Hyperplacentosis: Excessive exposure of chorionic villi,
Ex: molar pregnancy, twins, diabetes,
Placental ischemia.
obesity,
Pre-existing vascular disease,
thrombophlebitis,
Complications with pregnancy like,
multifetal pregnancy,
hydatidiform pregnancy,
hydroamniosis,
Rh.Incomplicity,
Medical diagnoses like nephritis and diabetes mellitus,
Vasospasm: Dilator depression is due to increased sensitivity of circulating pressors such as angiotensin II and prostaglandins.
Dysfunction of endothelial cells reduces placental perfusion.
It can also be caused by immune complex diseases.
It can also be caused by not having enough protein, calcium, magnesium, vitamin E and A in the diet.
Due to genetic factor
Due to immunological factors.
Due to endocrine factor.
Due to environmental factors.
Due to chronic health conditions such as hypertension, gestational diabetes, kidney disease and autoimmune disorders.
Symptoms and signs:
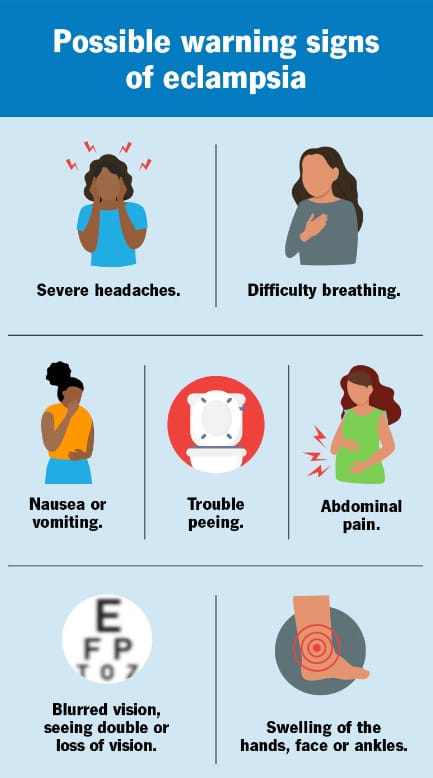
The symptoms and signs of eclampsia are divided into four stages:
1) Premonitoring stage
(30 seconds),
2) Tonic stage
(30 seconds),
3) Clonic stage
(1 to 4 minutes),
4) Stage of coma
1) Premonitoring stage
(30 seconds):
In this patient is unconscious,
There is twitching of the muscles of the face, tongue and limbus,
The eyeball is rolled, turned to one side and then fixed.
This stage lasts for 30 seconds.
2) Tonic stage
(30 seconds):
In this test, the whole body goes into a tonic spasm in this stage, trunk = opisnotonis (abnormal body posture in which the head, neck, and spine are tilted backwards.)
Limbus = Flex,
hand = clenched,
Respiration stops and the tongue protrudes between the teeth.
Cyanosis is seen,
The eyeball is fixed,
This stage lasts for 30 seconds.
3) Clonic stage
(1 to 4 minutes):
All voluntary muscles undergo alternate contraction and relaxation,
Twitching starts from the face and involves the extremities of one site,
Tongue bites,
Breathing stearatorius,
A mouth full of blood-stained frothy secretions,
Cyanosis is gradually reduced,
Respiration is labored and noisy,
Temperature increases by 40°C due to fits.
This stage lasts from 1 to 4 minutes.
4) Stage of Coma:
After a fit, the patient goes into a coma stage that lasts from minutes to hours.
Deepcoma remains until another convulsion occurs. In this the patient is seen in a state of confusion after a convulsion and the patient does not remember what happened to him.
If the fits occur consecutively, it converts to status epilepticus.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Urine Test: To assess proteinuria.
24 hours urine collection for protein level measurement.
Ophthalmic Examination.
Blood tests for liver and kidney function such as
Serum uric acid,
blood urea level,
Serum creatinine level,
Hepatic/liver enzymes
Antenatal fetal monitoring:
Clinical Examination,
Daily Fit Kick Count,
ultrasonography,
cardiotocography,
Umbilical artery flow velocimetry,
Biophysical profile: including ultrasonography and non-stasis test to assess fetal breath test and muscle tone.
Complications:
Hazards of Conversion
injury-tongue bite,
Vomiting aspiration,
exhaust,
Acute left ventricular failure,
In pulmonary AD,
pneumonia,
cerebral hemorrhage,
hyperpyrexia,
Anuria,
Disseminated Intravascular Coagulopathy (DIC),
hepatic necrosis,
postpartum depression,
Peripheral sepsis,
psychosis,
pulmonary embolism,
Abruptio placenta,
vision disturbance,
Blindness – due to optic nerve involvement,
But vision recovers four to six weeks after delivery.
Management of eclampsia
Medical and Nursing Management of Eclampsia
Aim of Management
To control fits of convulsions.
Controlling blood pressure.
Prevent complications.
Safe delivery of Fits.
Principles of Management
To maintain mother’s airway, breathing and circulation.
Properly administer 8-10 liters of oxygen to the mother.
Preventing maternal convulsions.
Provide proper ventilatory support to the mother.
Prevent injury to the mother.
All laboratory investigations of the mother should be done properly.
General Management
Hospitalization
Hospitalize the mother in a hospital with properly well-equipped facilities.
Rest Advise the mother to take adequate rest as well as advise to stop all activities and also restrict visitors.
Positioning Advise the mother to rest in a proper left lateral position to reduce Venakawa compression and prevent heel pain.
History Collection To collect the complete history of the mother including the frequency and duration of how many fits have occurred and to take the complete history of any type of medication the mother is taking or not.
Sedation and General Examination Mother should be provided with proper drug and sedated.
Ex:=phenobarbitone 15-30 mg (TDS)
Or
Diazepam 1.5 mg (TDS).
After the mother is properly sedated, perform a general and abdominal examination of the mother properly and quickly.
Vital Sign Noting the vital sign every half hour of the mother in which,
temperature,
pulse,
Respiration,
and blood pressure.
If there is any disturbance in the vital sign or if the vital sign is raised above its normal range, treat it immediately.
Urinary output
Monitor mother’s urine output hourly.
Starting nutrition mother with 10% Dextrose to maintain mother’s fluid, nutritional and caloric levels. Fluid should not be increased in an amount more than 2 liters in 24 hours.
Additionally, 50 ml 5% Dextrose should be provided to the mother at 8 hour intervals to maintain the caloric level of the mother.
Specific management or medical management
Eclampsia wadi mother can be treated by providing medication as follows:
a) Anticonvulsant,
b) Anti-hypertensive,
c) Sedatives,
d) Diuretic,
e) Antibiotics,
f) Other Medication.
a) Anticonvulsant,
Magnesium Sulphate A ( MgSO4 )
Acts as the drug of choice to treat the condition of eclampsia. Because it helps in preventing eclamptic fits in the pregnant mother.
Magnesium sulfate can be administered both IV (intravenously) and IM (intramuscularly).
Dose and route
IM (Intra Muscularly):
Initial Dose: Initially 4 gm IV (intravenously) bolus, administer magnesium sulfate very slowly over 3-5 minutes.
Continuous dose: Administer 5 gm magnesium sulfate IM (intra muscular) every four hours in alternate buttocks.
IV (Intra venously)
Initial dose:
Initial dose is 4-6 gm of magnesium sulfate administered slowly IV (intravenously) over 15-30 minutes.
Continuous Dose:
Administer 1-2 gm magnesium sulfate every hour IV (intravenously).
Magnesium sulfate is a toxic agent that can condition deep tendon reflux if not provided within therapeutic levels. The therapeutic level of magnesium sulfate (MgSO4) is 4-7 mEq/L (milliequivalents per liter). ) is In case of overdose of magnesium sulfate (MgSO4), calcium gluconate is used as an antidote.
Magnesium sulfate is administered only when nizark is present, urine output is greater than 30 ml/hr, and respiratory rate is greater than 12/min.
b) Anti-hypertensive,
Anti-hypertensives are used to control and reduce blood pressure.
Ex:
a) Hydralazine:
5 to 10 mg over 2 minutes.
b)Labetalol:
Initial dose: 20mg slowly over 2 minutes.
followed by 40-80 mg IV over 10 minutes.
The total dose should not exceed 300 mg.
c) Sedatives
Ex:=Diazepam
Dose:=5-10mg IV at the rate of 2-5mg/min.
Maximum dose: Do not increase more than 10mg dose.
d) Diuretic:
Diuretic medication should be provided during pregnancy only when pulmonary AD is present.
Ex:=Frusemide, Mannitol.
e) Antibiotics:
Antibiotics are provided as prophylaxis to reduce the complications of pulmonary and pleural infections.
Broad spectrum antibiotic medication is not used in these antibiotics.
f) Other Medication:
i) In case of pulmonary ED: Provide frusemide 40 mg IV followed by 10% mannitol.
ii) Heart failure:
Ex: Using Lasix and Digitalis medication.
iii) Hyper pyrexia:
Antipyretic medication is not used.
Nursing Management of Eclampsia
Placing a pregnant woman with eclampsia in a side-padded side rail wada cot.
Keeping a padded tongue blade between the teeth.
Keeping the mother in lateral position can avoid aspiration.
During convulsions, keep the airways patent and provide oxygen to the mother in adequate amounts.
Properly monitoring the mother’s oxygen level by pulse oximetry.
Suction properly to remove oral secretions and any vomiting, if any.
Properly note the time, duration of the convulsions the mother is experiencing.
Provide proper and regular prenatal care to mothers with pregnancy induced hypertension.
Protect the mother from self-injury.
Keep the mother in a dark room to minimize stimuli such as bright lights, noise, and visitors.
Keeping the foot side of the bed slightly elevated allows secretions to drain properly from the respiratory tract.
Assessing mother’s vital signs, ED, fundus height, presentation and position of feet and fetal heart sound and testing urine for protein.
Assessing mother’s urine output properly.
Provide intravenous infusion of glucose saline and Ringer’s lactate solution as prescribed to maintain the mother’s fluid and nutritional levels.
Advising the mother to maintain her personal hygiene.
Providing properly prescribed medication to the mother.
Assess the mother’s uterine activity, cervical status and fetal status as the membranes may rupture and delivery may occur.
Obstetrical Management:
Most of the time when a woman has convulsions she comes for labor if labor has not started then induction of labor is done by artificial membrane rupture, prostaglandins gel or oxytocin or caesarean section if the baby has died spontaneously Waited for labor.
Continuous start of hypertensive regimen as prescribed during post partum period.
Continuously monitor the mother for any other complications of eclampsia.
Advise the mother to follow up regularly.
- (PID)Pelvic Inflammatory Disease:
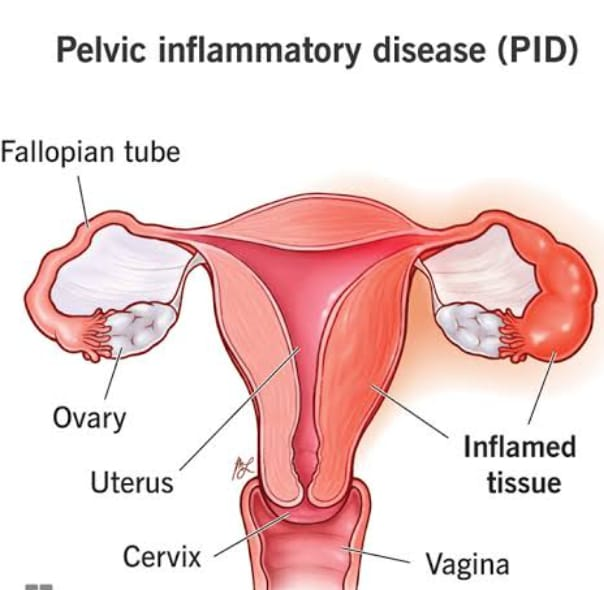
PID (Pelvic Inflammatory Disease) In which infection and inflammation occurs in the upper genital tract organs of the female reproductive system, this condition is called pelvic inflammatory disease. This infection is usually responsible for sexually transmitted diseases. The bacteria are transmitted through the vagina in an ascending (downward to upward) manner in the upper genital tract, causing infection and inflammation in the female reproductive organs, such as the uterus, vagina, cervix, uterus, fallopian tubes, ovaries, etc. Organ involvement may occur.
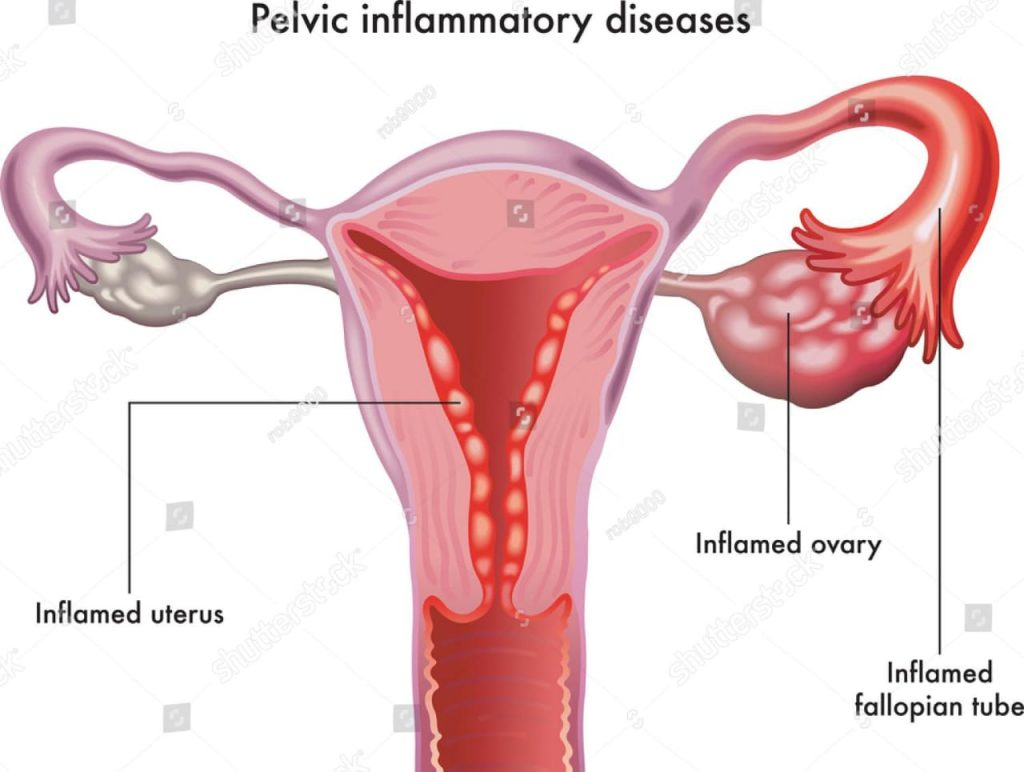
If the infection is in the vagina, it is called vaginitis.
If the infection is in the cervix, it is called cervicitis.
If the infection is in the uterus, it is called metritis.
If the infection is in the fallopian tubes, it is called salpingitis.
If the infection is in the ovary, it is called oophoritis.
Types of Inflammatory Disease:
Pelvic inflammatory diseases are generally divided into two types,
- Acute pelvic inflammatory disease
2.Chronic pelvic inflammatory disease
1.Acute Pelvic Inflammatory Disease: Acute Pelvic Inflammatory Disease means if severe symptoms are seen in a short time then this condition is called Acute Pelvic Inflammatory Disease.
2.Chronic Pelvic Inflammatory Disease: If the attacks of acute infection in Chronic Pelvic Inflammatory Disease occur frequently, this condition converts into Chronic Pelvic Inflammatory Disease.
Etiology:
Bacteria such as chlamydia and gonorrhea,
Viral infections such as herpes simplex,
Due to parasitic infection,
Due to fungal infection
Risk Factors:
Due to low socio economic status,
Due to multiple sexual partners,
Due to past history of PID,
cigarette smoking,
Due to low immunity,
Because of abortion,
Due to using IUD (Intra Uterine Device).
Symptoms and signs:
Lower abdominal pain,
fever,
one head,
Irregular menstrual bleeding,
nozia,
vomiting,
anorexia,
tenderness,
vaginal discharge,
Pain during periods,
Pain during voiding and defecation.
Diagnostic evaluation:
History Collection,
Physical Examination,
Complete Blood Count (CBC) test,
Ultrasonography (USG),
Cervical and vaginal swab cultures,
urine test,
CT scan (CT scan),
MRI,
Endometrial biopsy.
Medical Management:
The aim of medical management is to prevent infection and further transmission and to prevent complications arising.
If the patient has a bacterial infection, provide broad spectrum antibiotic medicine such as
ceftriaxone,
metronidazole,
tetracycline,
Erythromycin.
Advise the patient to take proper rest.
Advise patient to intake adequate amount of oral fluid.
If the patient has an intra-uterine device (IUD) inserted, remove it properly.
Provide the patient with a proper semi-fowler position.
Advise the patient to avoid sitz baths if they have an acute infection.
To continuously monitor the patient’s vital signs.
To provide analgesic medicine to relieve the patient’s pain.
Advise the patient to apply a hitting pad on the abdomen to relieve the pain if the patient has abdominal pain.
Advise patients to use proper barrier contraceptive methods to reduce the risk of pelvic inflammatory disease.
Advise the patient to seek medical treatment if he/she has any symptoms of pelvic inflammatory disease.
Advise the patient to avoid sexual activity during peripartum period after delivery, abortion.
Advise the patient to maintain personal hygiene.
Surgical Management:
This surgical management is done when the infection usually involves the fallopian tubes and ovaries.
Laparoscopy: A small incision is made in the abdominal wall and then a laparoscope (thin flexible tube with a camera and light) is inserted so that any infection and inflammatory conditions in the reproductive tract can be visualized on the screen.
Salpingectomy: This involves the surgical removal of the fallopian tubes.
- Multiple pregnancy

Definition:
When more than one fetus develops in the uterus simultaneously and at the same time, it is called “multiple pregnancy”.
When two fetuses develop together in the uterus, they are called twins.
When three fetuses develop simultaneously in the uterus, they are called triplets.
When four fits develop simultaneously, they are called quadruplets.
Varieties and types of twin pregnancy
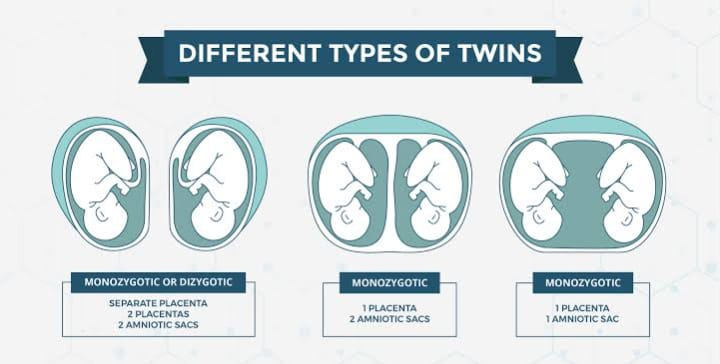
1) Dizygotic twins:
This commonest ie fertilization of two ova is the result of fertilization by two spermatozoa.
Two placentas are seen in this.
In this case, communication vessels are absent.
In this case, there may be two amnion and two chorion membranes.
Genetic features may be different in this.
They do not accept skin grafts.
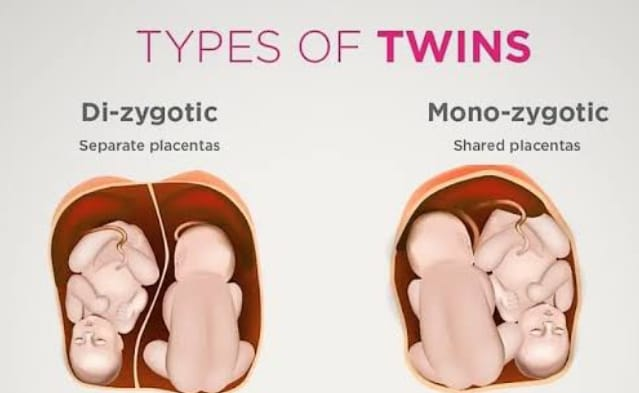
2) Monozygotic twins
Monozygotic twins develop due to fertilization of this single ovum by a single sperm.
Communication vessels are present in this.
It contains two amnion membranes.
Monozygotic twins usually have the same sex.
Genetic features are also found to be the same.
Physical features like ice, hair color, ear sap, palmar crisis etc are seen in it.
He also accepts skin grafts.
etiology
Exit cause is unknown.
Due to maternal environmental factors such as:
Race: Highest found in Negrons.
Hereditary: It is mainly transmitted from the maternal side more commonly.
Advanced Age of Mother:
Due to advanced age of mother ie 30-35 years.
Due to Influence of Parity:
Mainly 5th gravida due to increased parity.
iatrogenic
This is due to drugs used in ovulation.
2) Superfecundation
In this two different ova released in the same cycle and fertilized in a short period of time by separate acts of coitus is called superfecundation.
3) Superfitation
In this two ova are released in different menstrual cycles and fertilization takes place called super fertilization.
4) Fitters papyrus or compressus
In this a placenta has died early and a dead placenta has a flat end and is compressed between the membranes of the living placenta and the uterine wall.
5) Fetal acardiasis
This is seen in uniovular twins.
Lie and Presentation
Fitters’ Common Lie
It is usually longitudinal but malpresentation is commonly seen.
presentation
both vertices,
First vertex and second breach,
First Breach and Second Vertex,
Both breeches,
First vertex and transverse,
Both transverse.
Diagnosis of Multiple Pregnancy
History Collection,
Physical Examination,
Assessment of symptoms
Excessive enlargement of the uterus,
Nausea and vomiting are more common in the initial months.
Palpitations and shortness of breath are seen in the last months of pregnancy.
Swelling in the leg, varicose veins,
hemorrhoids,
Abnormal abdominal enlargement and excessive fetal movement.
General Examination
anemia,
Abnormal weight gain,
pre-eclampsia,
Abdominal examination
Inspection:
Barrel Sap and Large Abdomen.
Palpation:
Increased height of the uterus during amenorrhoea,
to fill the fundus of the uterus with a fit pole,
Increased abdominal girth,
Auscultation
Two fetal heart sounds are located at two different spots.
Investigation
sonography,
Biochemical tests such as maternal serum chorionic gonadotrophin,
Phytoproteins and unconjugated inst.
Management
Antenatal management
Early diagnosis and proper detection of chorionicity, amniocity, fetal growth pattern and congenital malformation if any.
Perform serial sonography, non-stress test and Doppler velocimetry for fitter surveillance.
advice
Advise mother to increase diet by 300 kcal/day.
Advising the mother to increase and moderate protein intake.
Supplement therapy
Iron therapy to the mother 100 to 200 mg /day. And advising the mother to take additional vitamins, calcium and folic acid.
Advise the mother to take adequate rest to prevent pre-term labor and other complications.
Advising the mother to make frequent antenatal visits and giving advice to the mother to do antenatal checkup at regular intervals due to which early identification can be done if the mother has a condition of anemia, or complications of preterm and if there is a condition of preeclampsia.
Regular assessment of fetal growth by ultrasound at 2-3 week intervals.
Providing adequate knowledge about breast feeding and bottle feeding to the mother during the antenatal period so that the mother can feed her baby properly.
During labor
As twin pregnancy is a high risk pregnancy, admit the patient to a well-equipped hospital facility where available. Vaginal delivery can be performed when both or one fetus is in vertex presentation.
Care during the first stage of labor
Taking additional precautions with normal conduction of singleton fetuses in the first stage.
Experience Obstetrician, Experience at Delivery,
An anesthetist, and a neonatologist should be present.
Ultrasound facility should be available in the labor room.
Adequate rest to the mother to prevent early rupture of the mother’s membrane.
Limited use of analgesic drugs and epidural if required
Administer analgesia.
Careful monitoring of the fetus.
Check for cord prolapse by doing internal examination after membrane rupture.
Starting Ringer’s lactate solution in an intravenous line.
Cross-match, group and keep 1 unit of blood ready.
Delivery of first baby
The conformational of the second stage is performed properly by vaginal examination.
Obstetricians, anesthetists and paediatricians must be present during delivery due to the increased risk of complications in multiple pregnancies.
Since multiple pregnancy is considered a high risk pregnancy, the operation theater should be properly prepared for caesarean section in case of emergency.
Continuously monitor the fetal heart sound until both babies are delivered.
Delivery of the first baby is usually spontaneous followed by a proper episiotomy.
Providing information to the mother about the sex of the first baby after delivery.
Then immediately provide the label to the baby as number 1.
Delivery of second baby
After delivery of the first baby, see the second baby in lie, presentation and fetal heart sound, abdominal examination or real time ultrasound.
Perform a vaginal examination to look for membrane and cord prolapse.
If the lie is longitudinal then look for low rupture of the membrane and again for cord prolapse.
If contractions are poor, add oxytocin to the infusion and administer to the mother.
The interval between two deliveries should be less than 30 minutes, if it is too late, interference has to be done. If the head is low down, forceps delivery, if there is no cephalopelvic disproportion in hiup, then do ventous delivery by doing internal version under general anesthesia.
Delivery of breech by breech extraction.
If the lie of the fetus is transverse, bring the fetus into a longitudinal lie by external version and if it fails, internal version and perform breech extraction under general anesthesia.
Indications of Cesarean section for second twin:
Non cephalic presentation with larger twin,
Immediate closure of cervix after delivery of first baby,
Fits distress.
The third stage
To prevent the condition of postpartum hemorrhage after delivery of the second baby, inject 10 international units (IU) IM or 20 international units (IU) of oxytocin added to 500 ml of normal saline (NS) or Ringer’s lactate solution intravenously (IV). ) to administer to the mother.
Then deliver the placenta with controlled cord traction (CCT).
Start oxytocin drip for at least one hour after delivery of second baby.
If there is excessive blood loss, give blood transfusion.
After the delivery of the mother, full care watch for two hours.
Providing additional support and health education to mothers for baby care.
Indications of Caesarean section:
Obstetric indication
placenta previa,
severe preeclampsia,
Previous caesarean section,
cord prolapse,
Abnormal uterine contractions,
Contracted pelvis.
Four Twins
Both fits or having a non-cephalic presentation (breech, transverse) in the first fit.
Conjoint twins.
Having complications like intrauterine growth retardation.
- Elderly primigravida:
Definition:
When a woman conceives her first pregnancy after the age of 30 or 35, the condition is called elderly primigravida.
Category:
Elderly primi gravidas are generally divided into two categories.
1) High fecundity: In this, women have late marriages but conceive immediately after marriage.
2) Low fecundity: Women marry early but conceive long after marriage.
Complications:
During pregnancy:
abortion,
Pre-eclampsia,
Abruptio placenta,
Uterine Fibroids,
Medical complications: Hypertension (HTN), diabetes, organic heart disease.
post maturity,
Intra uterine growth restriction (IUGR),
During Labour:
premature labor,
Pro Long Labour,
Maternal and Fetal Distress,
Retained placenta.
During Purperium:
Morbidity rate increases.
Failing lactase.
Management:
Elderly primigravida are considered high risk pregnancies.
It requires proper antenatal supervision.
The labor process is longer in elderly primigravida due to which proper supervision of the mother is required.
Abnormal uterine action converts to complicated labor.
Elderly primigravida require obstetrical intervention because the perineum is rigid and prolonged labor is likely.
Elderly primi gravidas have higher chances of neonatal morbidity and mortality rate due to increase in maternal age due to prematurity, prolonged labor hence there is a need for proper management.
Mothers should be advised to prefer hospital delivery in elderly primi gravidas.
Proper sonography should be advised for early identification of complications.
- Polyhydroamnios (Hydroamnios):
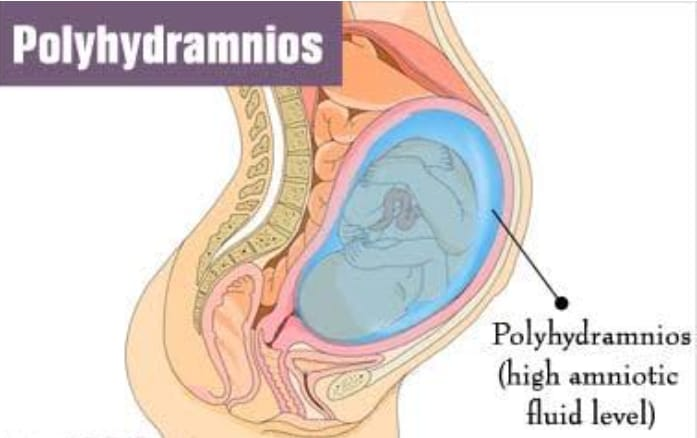
Definition:
Polly: Excessive.
Hydroamnios: amniotic fluid/like amni.
Polyhydroamnios is a condition in which the amount of amniotic fluid usually increases to more than 2000 ml. This condition is called polyhydroamnios. – equal to 800 ml).
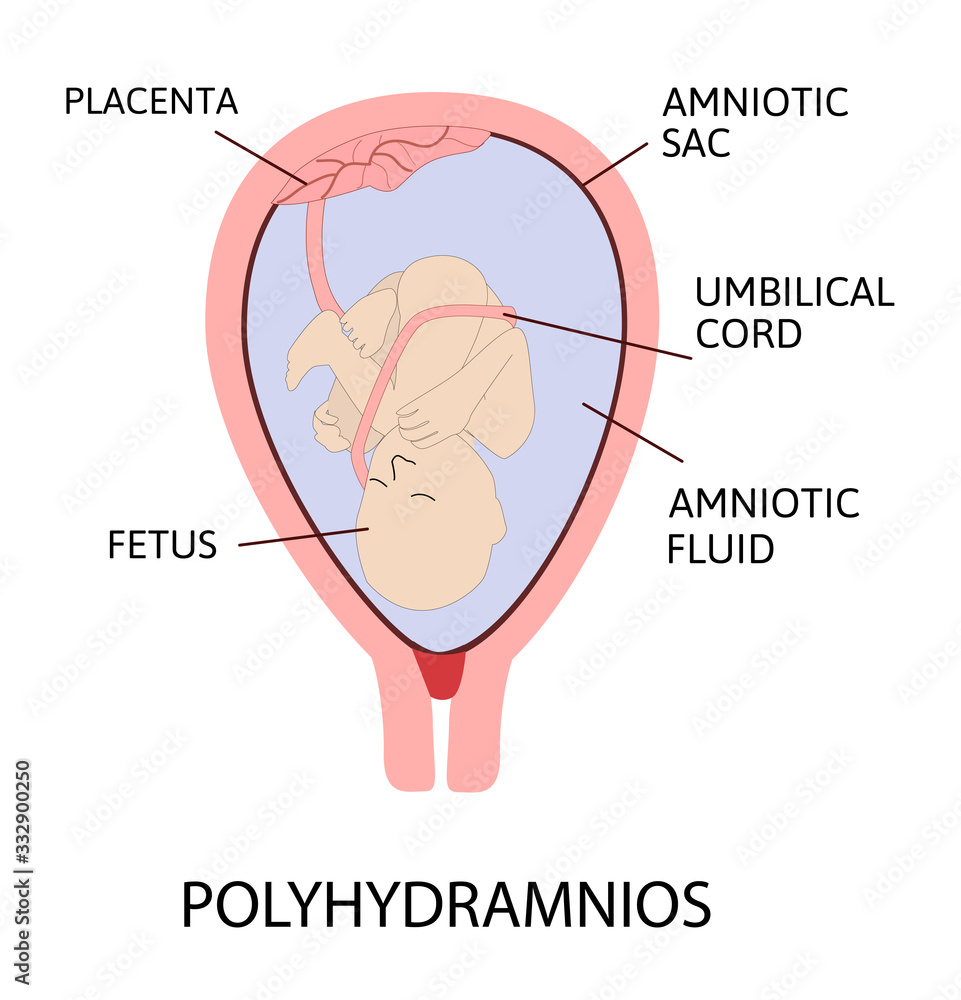
Etiology:
1) Fetal anomalous,
2) Maternal causes,
3) Placental factor,
4) Multiple pregnancy.
1) Fittal Anomalies:
anencephaly,
Open spina bifida,
Esophagia and duodenal atresia,
facial cleft,
neck massages,
Hydrops fatalis.
2) Maternal causes:
diabetes mellitus,
Cardiac and Renal Disease.
3) Placental factor:
Choriocarcinoma of the placenta.
4) Multiple pregnancy. Multiple pregnancy especially monozygotic twins.
Types of Polyhydroamnios:
Polyhydroamnios are generally divided into two categories based on the speed of their onset.
- Acute polyhydramnios
2.Chronic polyhydramnios.
1.Acute Polyhydramnios: Acute polyhydramnios this type is rare and mostly seen before 20 weeks of pregnancy i.e. this condition usually develops rapidly which usually develops during the 4th month of pregnancy due to rapid distension of the abdomen. Enlargement occurs and the abdominal girth is usually enlarged to more than 100 cm. Its onset is rapid and the uterus reaches the zyphisternum in about three to four days.
Etiology:
Gross cogenital fetal abnormality,
Uniovular twins,
Symptoms and Signs:
Severe breathlessness.
Severe abdominal discomfort.
In heel which is usually found in ankle and leg.
Varicose vein.
Abdominal symptoms such as abdominal pain, nausea and vomiting may occur.
The vital part is not filled.
The patient appears ill and features of shock are absent.
Abdomen is large and full, skin is tan, sinewy, large stria, fluid thrill is filled.
2.Chronic Polyhydromnios: This chronic polyhydromnios condition is usually a slowly developing condition that usually develops in the second half of pregnancy (30 weeks).
Symptoms and signs:
dyspnea,
Palpitation,
Abdominal discomfort,
heel in the leg,
Painful varicose veins,
The vital part should not be palpable,
Fetal heart sound (F.H.S) will not be audible.
Abdominal girth increased by more than 100 cm.
Due to accumulation of amniotic fluid.
Sign:
Signs of pregnancy being present,
Signs of pre-eclampsia such as oedema, hyper-tension and proteinuria may also be seen.
During abdominal examination:
Inspection: Abdomen appears large, globular with lateral fullness.
Skin is tan, sinewy with large striae.
Palpation: Uterus height and abdominal girth are increased during amenorrhoea.
Fluid thrill is felt in all directions of uterus and fetal parts are not well palpated.
Auscultation: Fetal heart sounds are not clear.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Internal Examination: A tense bulge membrane is felt if the cervix is dilated enough to pull and admit a finger tip.
Investigation: Sonography, radiography, blood studies like,
ABO & Rh Grouping,
Postprandial blood sugar,
glucose tolerance test,
Amniotic fluid-alpha phytoprotein.
Management
Mild polyhydroamnios:
This type is seen in the mid-trimester and usually requires no treatment, only bed rest.
Severe polyhydroamnios: Transfer this type of patient to a well-equipped hospital. The main principles of treatment are to reduce symptoms, identify the cause, and prevent complications.
Supportive therapy:
Advise patient to take adequate amount of bed rest.
Advise the patient to take a small amount of shalt in diet.
Provide analgesic and sedative medication to the patient as per the patient’s condition.
Conduct proper investigations to assess fetal malformations and complications such as diabetes and conditions of Rh isoimmunization.
If the patient is treating an associated condition such as preeclampsia or diabetes, indomethacin (25 mg every 6 hourly) provided to the mother may reduce amniotic fluid.
In uncomplicated cases: If the response is good, the pregnancy should be kept to term and the pregnancy should be allowed to continue.
In unresponsive cases with maternal distress and less than 37 days in pregnancy, amnioreduction by amniocentesis- 500 ml/hourly slowly remove (do not remove more than 1- 1.5 liters).
Labor induction if more than 37 weeks of pregnancy.
Termination of pregnancy without assessing the duration of pregnancy if there is congenital fetal anomaly.
Internal examination during labor to check for post partum haemorrhage after rupture of membranes and to prevent post partum haemorrhage and properly check for fitus nonanomalis.
Provide support in obstetrics management of patients.
Assessing the cause and degree of polyhydroamnion.
Assess mode and time of delivery according to presence of fetal abnormality.
Advise patient to take adequate amount of bed rest.
Advise patient to restrict extra salt and drink in excess amount.
To provide proper comfort measures to the patient.
Provide the patient with a properly upright position.
Provide antacid medication to the patient if he has conditions like heart burn and nosia.
Taking proper measures to prevent post partum hemorrhage and shock.
Allow reduction of amniotic fluid.
If the pregnancy is greater than 37 weeks, labor is induced and pregnancy terminated in fetal anomalies.
After delivery, check the baby for abnormalities and patency of esophagus.
Proper monitoring of mother and fetus for any complications.
- Oligohydroamnios (oligomnios):
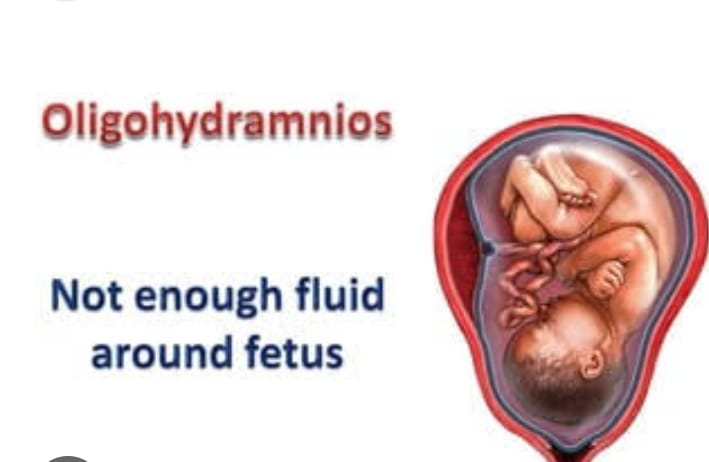
Definition:
Oligo: Reduce
Hydroamnios amniotic fluid
When the amniotic fluid at term is less than 200 ml, it is called oligohydroamnios. Oligohydroamnios is a medical condition in which the amount of amniotic fluid around the fetus is less than its normal amount during pregnancy. Amniotic fluid is important for cushioning the fetus and facilitating normal development. Oligohydroamnios may be associated with various complications, such as fetal distress, preterm birth or fetal development problems.
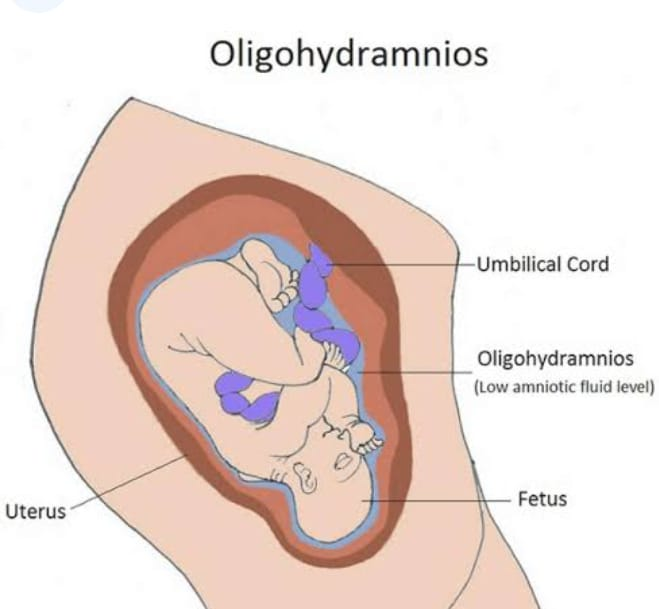
Etiology:
The exact cause is unknown, which is related to the following conditions.
Postpartum Gestation,
renal dysfunction,
From Obstratic Europe,
Failure of secretion of amniotic fluid by the amniotic cells covering the placenta.
Due to absence of kidney.
Due to decrease in fetal urine formation.
Symptoms and signs:
Uterine size becomes smaller during gestation period.
Reduced fetal movement.
Breech presentation being common.
Fetal growth retardation or deformity.
Due to less amniotic fluid, the uterus feels full of fits.
Thick meconium is passed during labor.
Complications:
Maternal: Prolonged labour, operative interference,
Maternal morbidity.
Management:
If there is a congenital malformation in the fetus then delivery should be done irrespective of the period of pregnancy.
Vaginal delivery is preferable.
In case of normal fits with third trimester, conservative management and advice for increased fluid intake along with amnio infusion in meconium liqueur.
- Intrauterine Growth Retardation (IUGR)/Intrauterine Growth Restriction (IUGR) Immaturity/Small for Date/Chronic Placental Insufficiency:
Definition:
If a baby’s birth weight is less than the tenth percentile (10%) of its average gestational age, the condition is called intrauterine growth restriction/retardation (IUGR). Growth restriction/retardation can occur in preterm, term or post-term babies. can
Incidence of IUGR
Immaturity accounts for about 1/3 of low birth weight children.
Its overall incidence in developed countries is 2-8%.
Mothers of term babies – 5%,
In post-term babies – 15%.
Types: Small fits are divided into following two types based on clinical evaluation and ultrasound examination.
1) The fetus is small and healthy but its birth weight is less than the tenth percentile (10%) of its gestational age.
2) Growth restriction is due to pathological process so again it is divided into two parts viz.
(a)Symmetrical type I (20%),
(b)Asymmetrical type II (80%).
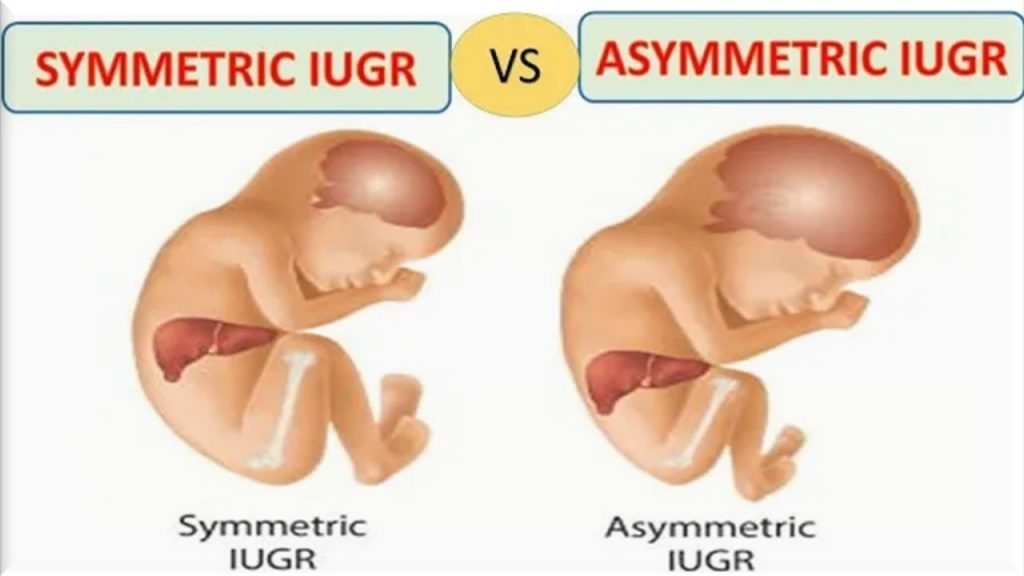
a) Symmetrical Type I (20%):
- Uniformly small size.
- Ponderal Index (Birth Weight/Crown Hill Length): Normal.
3.HC(Head Circumference): AC(Abdominal Circumference) and Femur Length (FL):AC(Abdominal Circumference) ratio is normal.
4.Etiology: Due to genetic disease or infection.
5.Total Cell Number: Less, End Cell Size: Normal.
6.Poor prognosis with neonatal-complicated.
(b)Asymmetrical Type II (80%):
1.Head is bigger than abdomen.
- Ponderal Index (Birth Weight/Crown Hill Length): Low.
3.HC(Head Circumference):AC(Abdominal Circumference) and Femur Length (FL):AC(Abdominal Circumference) ratio are elevated. - Etiology: Due to chronic placental insufficiency.
5.Total Cell Number: Normal, Smaller Size.
6.Neonatal- mostly uncomplicated with good prognosis.
Etiology:
Fetal growth retardation is generally divided into four groups namely,
- Maternal,
2.Fittle, - Placental,
- Unknown.
- Maternal:
Constitutional: Small Women Due to maternal genetic and racial factors,
Due to maternal nutrition before and during pregnancy.
Due to poor-weight gain.
Cyanotic heart disease ma
Due to low blood oxygen level.
In-adequate substrate levels
Ex. Malabsorption Syndrome.
Toxins like, alcohol, smoking, chronic renal failure, chronic urinary tract infection etc.
2.Fit:
In this, maternal blood contains enough substrates to cross the placenta but is not utilized by the fetus due to:
- Congenital Anomalies: Like, Cardiovascular, Renal and other factors.
2.Chromosomal Abnormalities: ie Trisomy 21, Trisomy 18 (Edward’s Syndrome) Trisomy 16, Trisomy 13 and Turner’s Syndrome. - Acceleration of the process of metabolism of the body due to torch agents.
- Due to multiple pregnancy.
- Placental: Due to poor uterine blood flow. Abruptio, circumvallate placenta, infraction
- Unknown. It is seen in about 40% of cases in unknown.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Clinical: Palpation of fundal height involves screening for volume and fetal mass Symphysis Fundal height correlates with gestational age at 24 weeks If it is 4 cm or less, it indicates growth restriction Abdominal girth if there is no maternal weight gain It does not increase.
Biophysical : HC, AC ration, femur length, amniotic fluid, anatomical survey ultrasound doppler parameters etc.
Biochemical markers: MSAFP and HCG levels are elevated in second trimester.
Physical Features at Birth:
Physical Features at Birth:
The birth weight deficit is about 600 gm less than the percentile standard.
Length is not affected.
Asymmetrical head circumference is greater than the body.
Dry and wrinkled skin, scaphoid abdomen, myconium-stained umbilical cord give the baby a “shriveled man” appearance. The cartilaginous ridges and plantar creses of the ear are well developed.
Baby is alert, active and cries normally, and keeps eyes open.
Reflexes are normal.
Management
Nursing management of the patient with intrauterine growth restriction usually occurs during the antenatal period, if possible.
Whenever a fit smaller than gestational age is suspected, a careful search is made to determine the presence of growth retardation by sonography.
When growth retardation is present, possible causes should be found out.
If growth retardation is present, the probable cause is identified.
If the fitus is symmetrical growth retardation, a meticulous search should be made to identify the fitus anomaly.
Fetus blood sampling and karyotyping to prevent unnecessary caesarean section in malformed babies.
The mother is given adequate rest in the pre-birth period, ie (in left lateral position).
Then there should be 2 hours after lunch and 8 hours rest period during night time.
Provide balance diet in adequate amount to correct the condition of malnutrition to the mother. Like 300 extra calories should be provided.
A low dose of aspirin (50 mg) daily is helpful in selected cases.
The patient should be properly hospitalized.
The condition of IUGR should be properly conformed.
To identify the patient for any congenital malformation and genetic disorder.
Any specific cause of intrauterine growth retardation should be treated first.
To check the fetal heart sound and mother’s condition regularly.
To check mother’s vital sign properly.
To provide proper support and reassurance to the mother.
Termination is done if the pregnancy is more than 38 weeks.
If the pregnancy is less than 38 weeks, the degree of IUGR should be checked.
If there is a condition of mild amount of retardation, advise the mother to take adequate amount of rest and provide adequate amount of supplementary therapy.
Assessing Lung Maturation of Fits in Severe Cases.
If maturity of lungs is achieved. It is assessed by L.S ratio (lecithin-sphingomyelin ratio), a value of L.S ratio greater than 2.0-2.5 is indicative of lung maturity. Delivery is done in such cases where growth of fitus cannot be improved by induction at 32-34 weeks followed by vaginal delivery/caesarean delivery.
If maturity of lungs is not achieved:
Maturity of the longus is evaluated.
Assay the level of phosphatidyl glycerol.
If the lungs are not mature, dexamethasone therapy is given and terminated.
Delivery can be made by:
Low rupture of membranes and followed by oxytocin
A casoma favorable for pregnancies of more than 34 wks is the cervix and the head is deep in the pelvis. If the cervix is favorable, prostaglandin gel can be used (PGE2).
Cesarean section is performed in unfavorable conditions.
During vaginal delivery the following are taken care of:
Delivery should take place in a well-equipped hospital where intensive intranatal monitoring is possible and has an intensive neonatal care unit.
Otherwise, the child should be transferred to a well-equipped hospital.
Precautions are taken during pregnancy.
The patient should be placed in the left lateral position.
If there is even slightly evidence of hypoxia (meconium staining and abnormal CTG), then immediate measures should be taken by caesarean section in the first stage and forceps in the second stage.
A pediatrician should also be available to care for the baby.
The baby should be cared for in an intensive neonatal care unit.
If there is a condition of hypoglycemia, special precautions should be taken for it.
To provide proper work and comfortable environment to mother.
- Post maturity/post term pregnancy/post dated pregnancy
Definition:
When a woman’s pregnancy continues beyond 2 weeks of the Expected Date of Delivery (EDD), the delivery is called a post-maturity or post-term pregnancy. “Postmaturity means the condition in which the pregnancy continues for more than 294 days calculated from the first day of the last menstrual period is called postmaturity”.
Etiology:
Apnon,
hereditary,
Last Menstrual Period (LMP) being inaccurate – due to wrong date.
Due to sedentary habit.
Due to hydroamnios.
Elderly primi gravida.
Alderley Multipara.
Fetal factors like, congenital anomalies, anencephaly.
Due to placental factors such as low estrogen levels.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Clinical findings: Weight is reduced, abdominal girth is reduced, history of false pain is noted.
Assess height of uterus, size of fitus and hardness of skull bone in palpation.
A decrease in the liker amni will cause the uterus to fill full of fits.
On internal examination, the cervix is ripe and the skull bone is hard.
Investigation: Sonography, amniosynthesis, straight X ray abdomen.
Nonstress tests every two weeks to assess fetal well-being.
biophysical profile,
Ultrasonographic to estimate amniotic fluid volume.
Modified biophysical profile.
Symptoms and signs:
Baby: Its general appearance is thin and old, wrinkled skin, vernix cassia absent, body and cord greenish-yellow in color. Longer nails are more than hard head and nail bed.
Baby’s weight is more than 3 kg and its length is about 54 cm.
Licker amni may be scanty and meconium stained.
Placenta: Infraction and calcification occur.
Cord compression occurs due to low wartner’s jelly in the cord.
Management:
Uncomplicated: Selective induction: Allow for spontaneous labor Perform modified bio physical profile twice a week.
Routine induction: Induce labor 7 – 10 days after the expected date.
Induction: If cervix is favorable (ripe), low rupture of membranes and start oxytocin infusion.
If the cervix is unfavorable (unripe), administer prostaglandin gel vaginally.
Complicated group: If postmaturity with high risk factors such as primordia, preeclampsia, Rh-incompatibility, fetal compromise or oligo hydroamnios placental insufficiency, elective caesarean section is also performed.
Any big baby and prematurity during labor may prolong labor Provide analgesics to relieve pain and careful fetal monitoring If fetal distress occurs, deliver immediately by caesarean section or forceps and ventouse.
Complications:
Fetal: Hypoxia and fetal distress due to reduced placental function, oligohydroamnios, and meconium stained liquor.
During labor: fetal hypoxia, acidosis, labor dysfunction, meconium aspiration, birth operative delivery immaturity or macrosomia.
Following birth: Meconium aspiration increases risk of chemical pneumonitis, atelectasis, and pulmonary hypotension, hypoxia, respiratory failure, hypoglycemia, still birth.
- Intra uterine death:

Intra-uterine death is also called still birth. Intra-uterine death is said when the fetus occurs after 20 weeks of pregnancy and before the delivery of the fetus and if the fetus dies during the delivery time, then this condition is called intra-uterine death (IUD). ) is called All fetuses whose weight is 500 gm or more. If the fetus dies during pregnancy antepartum or labor (intrapartum), it is called intrauterine death.
Etiology:
The exact cause is unknown.
Placental Causes:
placenta previa,
Abruptio placenta,
Placental insufficiency.
Umbilical cord problem:
Due to umbilical cord prolapse,
Due to the umbilical knot.
Due to maternal condition:
Due to preeclampsia and eclampsia,
Due to diabetes mellitus,
Infections (cytomegalovirus, toxoplasmosis),
Due to chronic diseases like hypertension, kidney disease. etc.
Fit conditions such as:
Genetic and chromosomal abnormalities,
Congenital Anomalies.
Due to infection:
Maternal infection (eg, syphilis, HIV group B, streptococcus).
Due to fetal infection.
Trauma: In Maternal Trauma (Ex: Accident and Physical Injury).
Other Factors: eg, multiple gestation eg, twins.
Due to drug and substance abuse.
Due to environmental factors (eg, exposure to toxins).
Symptoms and signs:
Absent movement of the body.
Uterine height may be found smaller than the gestational period.
Uterine tone is decreased.
Breakstone Hicks contractions are not felt.
Absence of femoral movement during palpation.
First fetal heart sound (FHS) is audible, then fetal heart sound (FHS) is absent.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Sonography: It shows fetal movement absent.
A condition of oligohydroamnios and cranial bone collapse is seen gradually in the fetus.
Straight Abdominal X-ray:
a.Spalding’s sign : Irregular overlapping of cranial bones usually seen after 7 days of fetal death.
b. Hyperflexion of the spine is seen.
C.Loss of normal parallel with crowded ribs sedo.
d.Appearance of gas shadow (Robert’s sign).
Estimation of fibrinogen level and partial thromboplastin time (especially if fit is maintained for more than 2 weeks).
Histological examination viz.
ABO and Rh Grouping.
VDRL.
Postprandial blood sugar.
HbA1C.
BUN.
Thyroid profile.
TORCH test.
Lupus anticoagulant and anticardiolipin antibody.
Management:
Prevention:
Provide pre-conception counseling and care to patients.
Proper prenatal diagnosis of the patient.
Proper screening of high risk mothers.
Termination of pregnancy if fetal compromise appears.
Expectant Management:
Spontaneous delivery occurs in 80% of cases within 2 weeks of delivery when the patient is educated for admission to the hospital.
Perform fibrinogen estimation of the patient every week.
Induction for labor by admitting to hospital in early delivery.
Oxytocin infusion is performed when the cervix is favorable.
When the cervix is unfavorable, prostaglandin gel is placed in the posterior fornix.
Misoprostol (PGE 1 ) 25-50 micrograms orally or orally is effective.
Cesarean section is usually performed when there is a major degree of placenta previa and transverse lie.
Provide proper psychological support to the patient.
Properly explaining causes of death in Fits.
As the risk of post partum depression in the patient is high, support should be provided by a psychologist or counselor when the patient needs it.
After reviewing the patient’s investigation reports, providing counseling for future pregnancy.
Advise the patient to follow up regularly.
High Risk Pregnancy:
Screening and Assessment for High Risk:
A pregnancy that has a risk of serious complications is considered a high risk pregnancy.
All pregnancies are evaluated to identify potential risk factors. By classifying pregnancies as high risk, if they require extra attention, they can be provided in an adequate amount.
Screening options are available to assess the risk for specific congenital anomalies during pregnancy and do not involve the risk of miscarriage.
If evaluation of high-risk women is done early, those high-risk pregnant women can be referred to a perinatal center before delivery, thereby reducing neonatal morbidity and mortality rates.
The most common reason for referral is preterm delivery, usually due to premature rupture of membranes.
A major benefit of screening and assessment of high-risk mothers is that early detection of any complications or problems in the mother and baby can lead to better outcomes in the health status of the mother and baby. And the mother can give birth to a healthy baby.
High risk cases like,
Obstetrical History:
privys steel berth,
Previous Neonatal Death,
Previous premature infant,
History of recurrent abortion.
Medical history of mother viz.
Maternal Illness,
chronic hypertension,
Abnormal PAP smear test,
insulin dependent diabetes,
renal diseases,
Rh- isoimmunization,
Maternal physical risk factors,
Incompetent cervix,
Uterine Malformation.
Risk factors of current pregnancy,
Moderate to severe preeclampsia (eg, hypertension, edema (weight gain), proteinuria (protein in urine), and albuminuria),
Polyhydroamnios (i.e. when the amniotic fluid amount exceeds 2000 ml),
Oligo hydroamnios (When the amount of fluid at term is less than 200 ml, it is called oligohydroamnios.),
Placenta previa (When the placenta partially or completely implants near or above the internal os of the uterus, it is called placenta previa).
Multiple pregnancy (when more than one fetus develops in the uterus simultaneously and at the same time, it is called multiple pregnancy).
Abruptio placenta (Abruptio placenta is a form of antepartum hemorrhage (APH) in which the normally situated placenta prematurely separates from the uterine wall and causes bleeding, called abruptio placenta.)
Other High Risk Pregnancies:
Abnormal fetal position,
vaginal bleeding,
malpresentation,
Fits are smaller than gestational age,
Hb level should be less than 10 g/dl,
Poor weight gain,
proteinuria,
glycosuria,
Systolic BP. Greater than 155 mm of Hg.
Vaginal infection. etc.
Things to consider during early pregnancy are —
Blood testing in which mother’s hemoglobin level, ABO and Rh group and blood sugar level are monitored.
Excessive weight gain in the mother is usually due to fluid retention. And if the mother’s weight is reduced, there is also a risk of developing the condition of intrauterine growth retardation (IUGR).
A previous history of hypertension or pregnancy induced hypertension (PIH) may be a risk factor in the mother as well as the fetus.
If the amount of amniotic fluid is high or if the amount of amniotic fluid is low, these are also called risk factors.
Another approach to be followed for high risk cases is as follows:
- Maternal Serum Alpha Phyto Protein (MSAFP):
Alpha phytoprotein (AFP) is an onco-fetal protein and is produced in the yolk sac and fetal liver.
Peak levels in fetal serum and amniotic fluid occur around 13 weeks and in maternal serum around 32 weeks.
Maternal serum and amniotic fluid are tested for alpha phytoprotein (AFP). This is usually done when there is a risk of neural tube defects and other congenital defects in the fetus. If the level of Alpha Phyto Protein (AFP) is high, it indicates fitus pathology, open neural tube defect, and if the level of Alpha Phyto Protein (AFP) is low, it suggests the condition of Down Syndrome and Gestational Trophoblastic Disease.
The amount of Maternal Serum Alpha Phyto Protein (MSAFP) is increased in some cases like Multiple Pregnancy, Open Neural Tube Defect Renal Anomalies, Rh Isoimmunization, IUFD(Intrauterine Fetal Death), Anterior Abdominal Wall Defect etc.
This test is done between 15 to 18 weeks.
- Chorionic villus sampling (CVS):
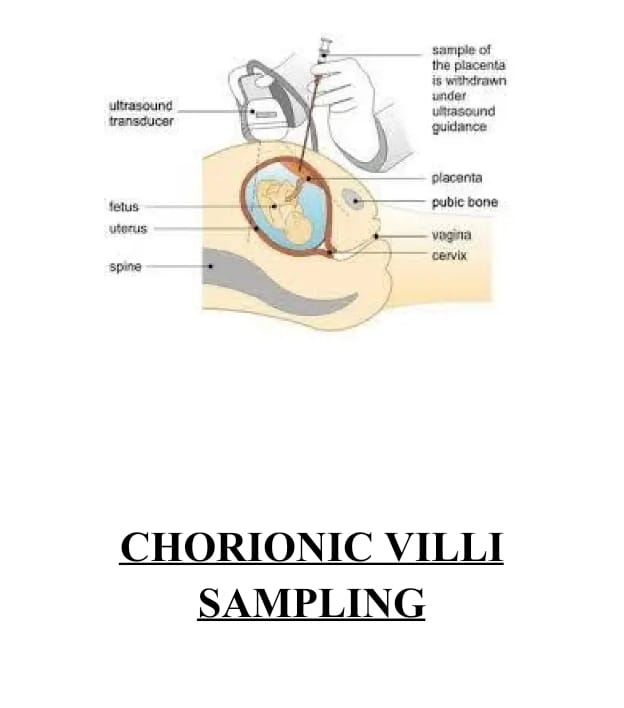
For prenatal diagnosis of genetic disorders, chorionic villus sampling is taken transcervically at 10 – 12 weeks and transabdominally at 10 weeks under ultrasound guidance.
A small amount of fluid can be collected from the chorion frondosum, transcervically (a catheter is introduced through the cervix), or transabdominally (by inserting a needle through the uterine wall of the maternal abdomen into the placental tissue). Diagnosis is obtained within 24 hours.
The positive aspect of this test is that the results are obtained early, and if termination is required, it can be done only in the first trimester. This test is also associated with fetal loss, limb deformities and vaginal bleeding etc. In addition to miscarriage, there is a risk of infection and amniotic fluid leakage.
As a result amniotic fluid can leak which can develop into a condition known as oligohydramnios which is a low amniotic fluid level.
Timing of Test – After 10 weeks.
- Cordosynthesis (percutaneous umbilical blood sampling):
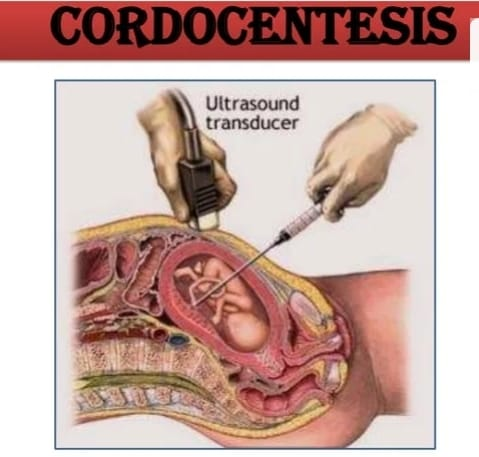
In this test, blood sample of the fetus is collected during pregnancy and then any chromosomal abnormality or blood disorder is diagnosed. In it, under the guidance of ultrasound, the umbilical vein is punctured and the needle is inserted. And then 0.5 to 2 ml of fetal blood is collected. Preterm labor, abortion or intrauterine fetal death may occur due to this test.
The time to do this test is after 18 weeks.
- Triple Test:
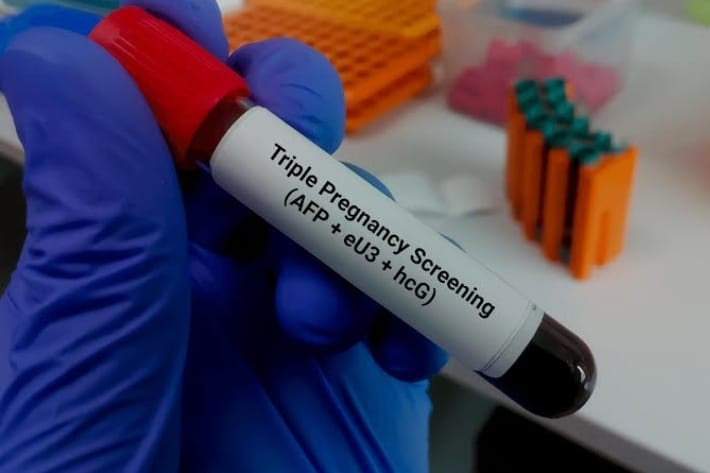
In this test, a combination of three tests is done in which,
Maternal serum alpha-fetoprotein (MSAFP), human chorionic gonadotrophin (HCG), and unconjugated estrol (UE) are involved.
This test is used to detect Down syndrome.
If pregnancy is affected, maternal serum alpha phytoprotein (MSAFP) and estrogen levels are low and human chorionic gonadotrophin (HCG) levels are high.
- Amniocentesis:
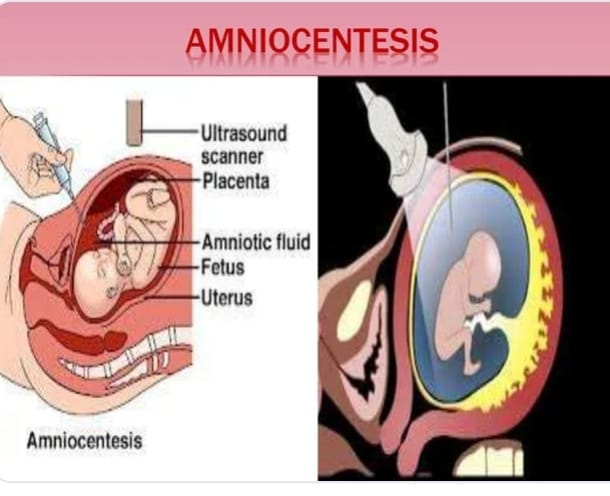
This is an invasive procedure usually performed at 16 – 18 weeks under ultrasonography guidance for cytogenetic analysis of fetal cells DNA analysis and biochemical tests of fluid.
In this procedure, a fine needle is inserted transabdominally into the amniotic cavity and aspiration of amniotic fluid is performed.
Procedure –
Before the actual procedure, a local anesthetic is given to relieve pain during the needle insertion used to withdraw the amniotic fluid.
Needle insertion is done through the abdominal wall of the mother and into the amniotic sac through the wall of the uterus.
Using ultrasound-guidance, the needle is guided to an area of the sac that is away from the fetus and approximately 20 ml of amniotic fluid is withdrawn for testing. Amniotic fluid contains cells that are shed by the developing fetus.
Cells are checked for the number and size of chromosomes (karyotype) to see if there are any problems that put the baby at risk for certain conditions. After the amniotic fluid is removed, the cells of the fetus are separated from it.
Cells are grown in culture medium, then fixed and stained.
Chromosomes are examined under a microscope for abnormalities.
This test detects most common abnormalities including mostly chromosomal disorders like Down syndrome, Edward syndrome (trisomy 18) and Turner syndrome, neural tube defects like spina bifida and anencephaly.
Hundreds of genetic disorders can be identified through this test.
Amniocentesis can also detect whether the mother or baby is Rh-negative and whether the baby’s lungs are mature enough for birth if immediate termination is needed. Amniosynthesis cannot detect every type of abnormality – for example, it cannot tell whether a baby has a cleft lip or a cleft palate.
Amniocentesis is performed during pregnancy when:
It is done to determine if a woman has previously had a chromosomally affected pregnancy or genetic disorder, has Down syndrome and other defects.
Chromosomal abnormalities detected by ultrasound examination may indicate an increased risk of developing chromosomal abnormalities.
When parents have a history of any genetic disorder or birth defect in the family.
In women who are older than 35 years.
Due to the request of a woman who is concerned about a chromosomal abnormality in her child.
Risks Associated with Amniocentesis:
Maternal and fetal haemorrhage,
infection,
fital injury,
Miscarriage.
During late pregnancy:
Biophysical
Biophysical investigations like fetal movement count, cardiotocography, non-stress test, fetal bio physical profile (BPP), Doppler ultrasound, contraction stress test (CST), amniotic fluid volume etc. are done for uteroplacental insufficiency.
Fittal Movement Count:
Cardiff Count 10 Formula:
In this, the patient starts counting the fetal movements from 9.am and stops when 10 movements are done, he is asked to inform the doctor if he does not have less than 10 movements within 12 hours in two consecutive days or no movement in one day.
Daily Fatal Movement Count (DFMC):
In this test, counting three counts in each period of morning, noon and evening and multiplying it by four, if it is more than 10 in 12 hours or less than three fetal movements in each period, then it is indicated that there is a problem with the fetus.
Diagnosis Modalities Invasive and Noninvasive:
Different invasive and non-invasive methods are used for prenatal screening and diagnosis.
In which non-invasive method (a method that does not require any instrument to open and insert inside the body),
Examination of the uterus from the outside of the body.
Ultra sound detection.
Listen for fetal heart sounds (FHS).
External fetal monitoring involves tests such as the non-stress test (NST).
Invasive method (a medical procedure that invades (enters) the body, usually by cutting or puncturing the skin or inserting an instrument into the body)
such as,
Chorionic villus sampling,
amniocentesis,
chordosynthesis,
Methods such as maternal serum alpha phytoprotein (MSAFP) are involved.
- Ultrasound Scan (USG):

An ultrasound scan is generally a safe, non-invasive, accurate and cost-effective investigation. In an ultrasound scan, high frequency sound waves are transmitted into the uterus.
In ultrasound, the baby’s bouncing off and returning echoes are translated by a computer into an image on a screen that shows the baby’s position and movements. Hard tissues such as bone reflect the greatest echoes and are white in the image, and smooth tissues appear gray and mottled. Fluid (such as the amniotic fluid that contains the baby) does not reflect any echoes and therefore appears black.
It is the difference between these different shades of white, gray and black that allows the sonographer to interpret the image.When scanning the abdomen in early pregnancy, the procedure often requires a full bladder.
Uses of Ultrasound:
To check the viability of the fetus
Heart beats of fetuses can be checked by ultra sound.* To check how many fetuses are surviving in the uterine cavity / to check the number of fetuses usually before 14 weeks of pregnancy it tells that a woman is a baby. Along with pregnancy, ultrasound scanning is used to check if the fetus is live and if it is a single fetus or one of twins or triplets.
To detect ectopic pregnancy
It is used to detect any abnormality, such as a condition of ectopic pregnancy, in which the fetus implants outside the uterine cavity, mainly in the fallopian tube. .
Doppler umbilical velocimetry Doppler ultrasonography measures the speed at which RBCs travel in the blood vessels of the uterus and fetus. This is helpful in determining whether vascular resistance is present in women with diabetes or gestational hypertension and consequent placental insufficiency.
Placental Grading:
Placental grading usually depends on the amount of calcium deposited in the placenta. Grading can be provided as
Amniotic fluid volume assessment
If the fetus is stressed in utero as the amniotic fluid decreases, the fetus is placed at risk of umbilical cord compression and thus interferes with its nutritional level.
At less than 20 wk, the uterus divides into two vertical lines along the midpoint (line nigra). The vertical diameter of the largest pocket of amniotic fluid present on each side is measured in centimeters (cm). The amniotic fluid index (AFI) is the sum of the two. After 20 wk, the uterus is divided into four parts and the sum of the four is taken. Average AFI: 12-15 cm (28-40 wicks); 5-6 (oligohydramnios), 20-24 (polyhydramnios).
To detect the cause of vaginal bleeding
Ultrasound helps the mother find the cause of any bleeding. Fetus viability is measured by ultrasound in cases of vaginal bleeding. Visible heart beats can be seen and detected by pulse Doppler ultrasound at about 6 wk and are usually clearly depictable (pictured) at 7 wk. .
To find out the exact date of pregnancy
The exact date of pregnancy can also be known by measuring the baby. For patients with uncertainty of the last menstrual cycle, such measurements should be done as early as possible in pregnancy to arrive at a suitable dating. Measurements made are:
a) Crown-rump length (CRL):
This measurement can be done between 7 and 13 weeks and gives a very accurate estimate of gestation.
b) Biparietal diameter (BPD)
Diameter between 2 sides of head. This is measured after 13 weeks. It went from about 2.4 cm at 13 wks to about 9.5 cm at term. increases up to
c) Femur Length (FL)
Measures the longest bone in the body and reflects the longitudinal growth of the fitus. Its utility is similar to that of BPD. It grows from about 1.5 cm at 14 wk to about 7.8 cm at term.
d) The Abdominal Circumference ( AC )
It is the single most important measurement to make in late pregnancy. It reflects the size and weight of the fetus more than the age.
To assess the risk of Down syndrome
At 11-14 weeks the presence of Down syndrome can be detected by measuring the fluid from the back of the child’s neck (called a nuchal translucency scan). Some major abnormalities can also be detected at this stage. At 11 to 14 weeks, a measurement of the thickness of the skin on the back of the neck (known as a nuchal translucency measurement) can be used to measure the risk of a fetus having a chromosomal abnormality. Why is the blur test abnormal? To find out.
To assist in performing diagnostic tests
Some tests to assess the well-being of the fetus, such as CVS or amniocentesis, are performed safely with the help of ultrasound to show the position of the baby and the placenta.
Development of Fits
After 18 weeks it is possible to examine the fetus in more detail. Examination of most organ systems can be performed to ensure that the development of the fetus appears to be occurring normally.
To diagnose certain types of abnormalities
such as spina bifida. Many structural abnormalities in the fetus can be reliably diagnosed by ultrasound scan, and this can usually be done before 20 weeks.
To assess the amount of amniotic fluid and locate the placenta
Liker i.e. high or low amount of amniotic fluid can be clearly detected by ultrasound and both these conditions can adversely affect the fetus. Ultrasonography is also important to detect the location of the placenta. Due to which any abnormal site of the placenta can be detected early such as placenta previa.
Ultrasonography is also important for other obstetrical conditions such as,
a) When intrauterine death is a conforming requirement.
b) To check fetal presentation in certain cases.
C) When there is a need to evaluate fetal movement, tone and breathing in the biophysical profile.
d) To diagnose uterine and pelvic abnormalities during pregnancy.
Ex: Fibromyomata, Ovarian cyst.
An ultrasound scan can be performed both vaginally and abdominally
Vaginal scan
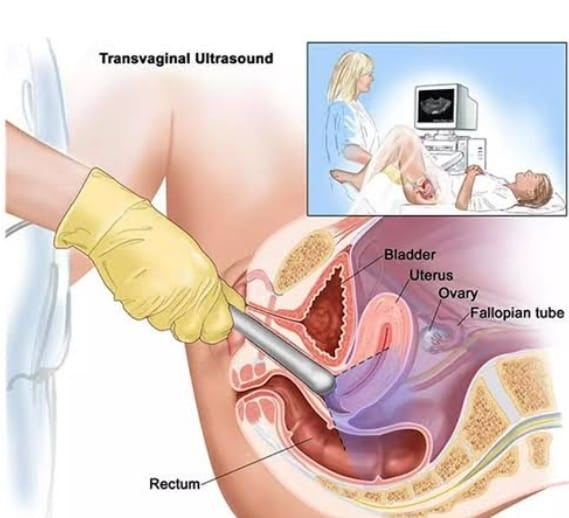
A vaginal scan is only done during the first 12 – 14 weeks of pregnancy. Because the fit is very small at this stage, vaginal scan provides a better view compared to abdominal scan. In vaginal scan, the mother is asked to lie down on her back and then a lubricated sensor is inserted into the vagina. The sensor is usually covered by a condom.
Abdominal scan
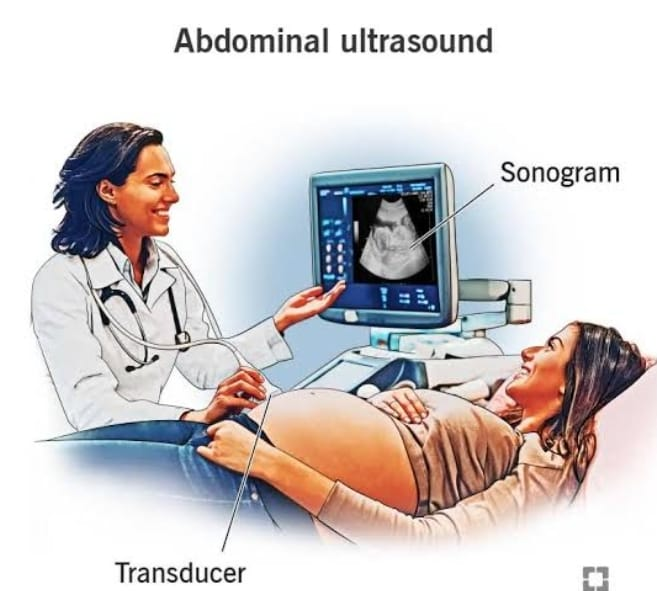
An abdominal scan is usually used after 12 to 14 weeks of pregnancy. In an abdominal scan, the mother is asked to lie on her back. A gel is applied to her skin over her lower abdomen. The gel allows the sensor to slide smoothly over the skin and helps produce clear images. The sensor is held firmly against his skin and moved over the abdominal surface.
Doppler ultrasound
Doppler ultrasound is currently most widely used to detect fetal cardiac pulsations and pulsations in various blood vessels of the fetus. Further developments in Doppler ultrasound technology in recent years have enabled a great expansion in its application in obstetrics, particularly In the area of assessment and monitoring of fit’s well-being, its progression faces the diagnosis of intrauterine growth restriction and cardiac malformations.
Cardiotocography (CTG):
Cardiotocography (CTG) graphically records the fetal heart beat and uterine contractions.
It is generally done during the third trimester. The machine used for monitoring is called a cardiotocograph and is also known as an electronic fetal monitor (EFM) or external fetal monitor (EFM).
Two transducers are used externally by strapping to the abdominal wall. One measures the heart rate of the fetus and the other measures the contractions of the uterus.
Internal measurement can also be done. It requires a certain degree of cervical dilatation, as it involves inserting a pressure catheter into the uterine cavity and attaching a scalp electrode to the head of the fetus to adequately measure the pulse. It is preferred when there is a possibility of complicated birth. is Cardiotocography is also used to perform a non-stress test (NST) as well as a contraction stress test (CST).
- Non Stress Test (NST):
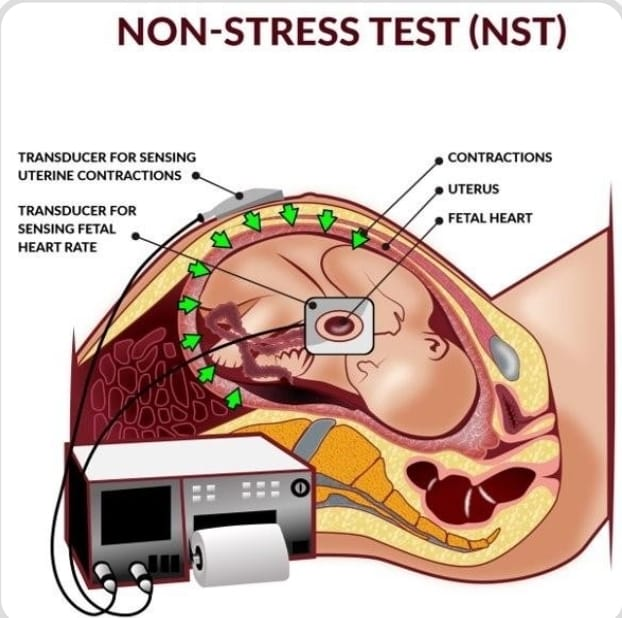
Fetal well-being is evaluated by monitoring fetal heart rate (FHR) in response to fetal movement in the non-stress test (NST). Doing this test does not put any special stress on the fetus. In the non-stress test, a belt is attached around the mother’s abdomen to monitor the fetus’s heart rate and uterine contractions.
Non-stress is a common prenatal procedure that is usually performed during the third trimester to assess fetal health. The heart rate is recorded for about 20-30 minutes, during which time the mother indicates that she is fit. Do you feel any movement? Short-term variation from baseline should be between 10 and 15 bpm. And if the variation with other abnormalities cannot be reduced for a long time, there may be fitous distress.
Purpose:
The primary goal of the NST (Non Stress Test) is to monitor the baby’s heart rate and assess how the fetal heart rate (FHR) responds to movement. It helps evaluate the well-being of the fetus and can provide insight into the baby’s oxygen levels and overall health. NST is usually used in cases where there are concerns about the health of the fetus or when there is a risk for complications.
Position and Preparation of Mother:
Non-Stress Stress (NST) is usually performed by providing the mother in a properly comfortable position. While performing this test, the fetus should not be in sleeping condition as it may lead to variation in fetal heart rate i.e. in fetal heart rate. A decrease may be observed. Fits are elicited by abdominal palpation or buzzing. Advise the woman to press the button when she feels fetal movement and monitor the fetal heart rate (FHR).
Advantages:
This is a non-invasive test.
This test is simple,
It is inexpensive and less time consuming.
There is no contraindication or complication of this test.
No special expertise is required to perform this test.
Immediate answer can be obtained through this test.
Interpretation of Test:
Reactive Test (Normal Stress Test (NST)):
The test is considered reactive when the fetal heart rate (FHR) accelerates to 15 beats/min above baseline for 15-30 seconds in relation to fetal movement. When two or more such events occur within a 10-minute period or 20 – When there are five or more accelerations in a minute period, the test is considered normal.
Non Reactive Test (Abnormal Non Stress Test):
A non-reactive test is performed when the fetal heart rate is absent in response to fetal movements. When the fetal heart rate is less than 15 beats/min in response to fetal movement and lasts for less than 15 seconds, the test is called abnormal.
Suspicious non-stress test
These include an acceleration of the heart rate of the fit in relation to the movement of the fit, but the number of beats above baseline, or the length of the duration, does not meet the criteria for being reactive or non-reactive.
Indication of Non Stress Test (NST):
Women who have any pre-existing medical conditions like diabetes or conditions that arose during pregnancy like,
Have a condition of hyper tension.
When a pregnant woman reports that the fetal movement is less than usual. Intrauterine growth retardation (IUGR) is a condition in which the child does not grow properly according to its normal age. When the amount of amniotic fluid is too high or the amount of amniotic fluid is reduced. In lost condition.
This test is performed to check the babbling of the baby in the condition that the pregnancy of the woman is continuous even after 40 weeks of pregnancy.
After a woman undergoes a procedure such as an external cephalic version (to turn a breech baby) or an amniocentesis in the third trimester (to determine whether the baby’s lungs are mature enough for birth or to rule out an infection of the uterus), the health care practitioner may A non stress test (NST) is done to ensure that the baby is well-being.
- Contraction Stress Test (CST):

Contraction stress test
(CST) is used to assess the condition of the health of the fetus and the condition of the fetal heart rate (FHR) in women when the fetal oxygen level is reduced during uterine contractions. In this test, the fetal heart rate response to uterine contractions induced by oxytocin is assessed.
External heart monitoring is done in this test. During uterine contractions, the blood and oxygen supply to the fetus drops for a short period of time. This condition is not a problem for most babies, but in some babies, their heart rate slows down. These changes in heart rate are monitored on an external fetal monitoring device. This test is usually performed when a woman is 34 weeks or more weeks pregnant.
Preparation of Mother:
In this, semirecumbent position, lateral tilt position, and properly comfortable position are provided to women. Uterine contractions are then recorded for 20 to 30 minutes. If the uterine contractions are three or more than three in 10 minutes and their duration is usually longer than 40 seconds, no stimulation is needed. If spontaneous stimulation is absent, stimulation is induced by providing oxytocin. In the oxytocin challenge test, a diluted oxytocin solution is administered intravenously. Then increase the infusion rate at small intervals until three or more than three uterine contractions in 10 minutes are observed for more than 30 minutes, then stop the oxytocin infusion after recording.
Contraction stress test is done to check the condition of the following such as,
Used to assess fetal welling and fetal heart rate (FHR) during the process of labor or during uterine contractions when the amount of oxygen is low.
Contraindication
If a woman has the condition of placenta previa,
Women have the condition of Antepartum Haemorrhage (APH),
Privus classic caesarean section is performed,
Clients who are at high risk of preterm labor
Risk
Labor can usually start early after the expected date of delivery.
Prolonged contractions can cause problems in the baby.
Interpretation:
The contraction stress test (CST) is used to assess the health status of the fetus due to reduced blood and oxygen supply to the fetus for a short period of time when the woman is in labor. is
Normal Contraction Stress Test (CST)
The result of a normal test is called negative. In which the baby’s heart rate is not low (decelerate). But after the contraction (late decelerate) it is low.
Abnormal Contraction Stress Test (CST)
Abnormal contraction stress test (CST) results are positive in which the heart rate of the fetus slows down and remains continuously slow even after the contractions, which means that problems can arise during normal labor in the fetus. It can also mean that if there is a delay during the delivery time, then the baby may have a problem.
Hyperstimulation
Contractions in hyperstimulation last 90 seconds or longer.
Suspicious
There is a late declaration of the fetal heart rate, but this is not repetitive and does not occur with continuous contractions.
Unsatisfactory
The quality of this recording is not that good.
- Anemia.
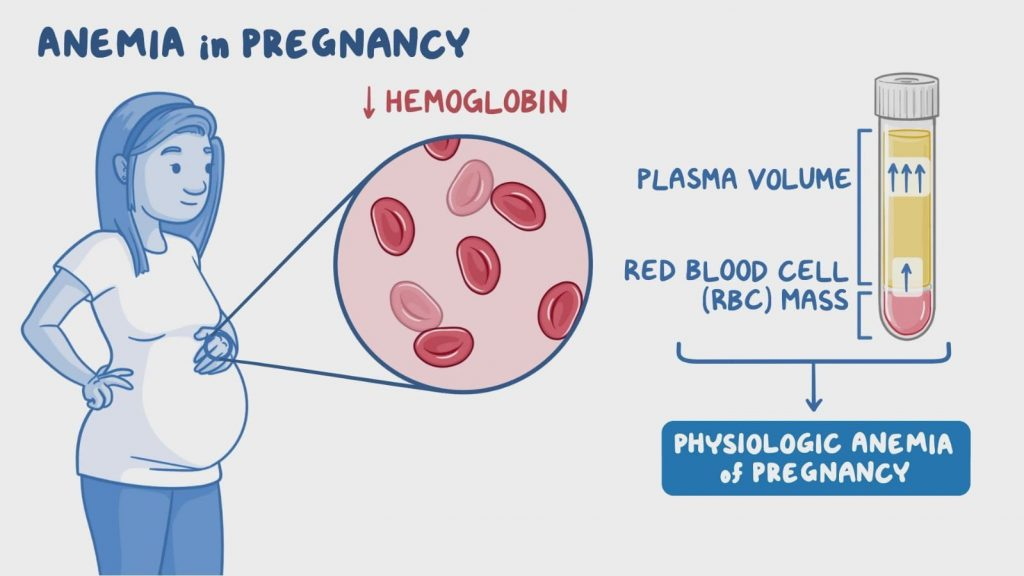
Anemia is the most common blood disorder seen in women during pregnancy. It is generally more prevalent in areas with poor socioeconomic conditions. Anemia is a condition in which the circulating red blood cell and hemoglobin levels are lower than their normal levels (reduced numbers). Due to this, the oxygen carrying capacity of red blood cells decreases. It is usually seen due to different reasons such as nutritional deficiency (ion, vitamin B12, or folate), chronic disease, genetic condition, and blood loss.
Female Ma Normal Hb : 12-16 gm/ dl.
If the hemoglobin level in a female is between 10 gm/ dl – 11.9 gm/ dl then it is called mild anemia.
If the hemoglobin level in a female is between 7 gm/ dl – 9.9 gm/ dl then it is called moderate anemia.
If the level of hemoglobin in a female is less than 7 gm/dl, it is called severe anemia.
Classification:
- Physiological anemia.
- Pathological anemia.
1.Physiological Anemia: In pregnancy plasma volume red blood cells (RBC) volume and hemoglobin mass increase hence pregnancy demand increases specially in second half trimester with adequate amount of diet even extra demand of iron is not fulfilled hence pregnancy time Meanwhile physiological iron deficiency is observed. Hence hemoglobin concentration falls down in pre-pregnancy due to effect of hemodilution and negative iron balance.
- Pathological Anemia:
Deficiency anemia: due to iron deficiency, folic acid deficiency, vitamin B 12 deficiency, protein deficiency etc.
Hemorrhagic:
Acute: due to bleeding or antepartum haemorrhage (APH) in the early months.
Chronic: Hookworm infestation, bleeding piles etc.
Hereditary: Thalassemia, Sickle Cell Hemoglobinopathy, Other, Hemoglobinopathy, Hereditary Hemolytic.
Bone marrow insufficiency: hypoplasia or aplasia due to radiation, drugs (aspirin, indomethacin.
Anemia of infection (malaria, tuberculosis).
Chronic disease (renal) or neoplasm.
Etiology:
Due to nutritional deficiency.
Due to chronic diseases.
Due to genetic factors.
Due to blood loss.
Due to infection.
Due to Bonemarrow disorder.
Due to vitamin deficiency.
Due to impaired production of red blood cells.
Due to excessive amount of blood loss.
Due to decreased production of red blood cells.
Symptoms and signs:
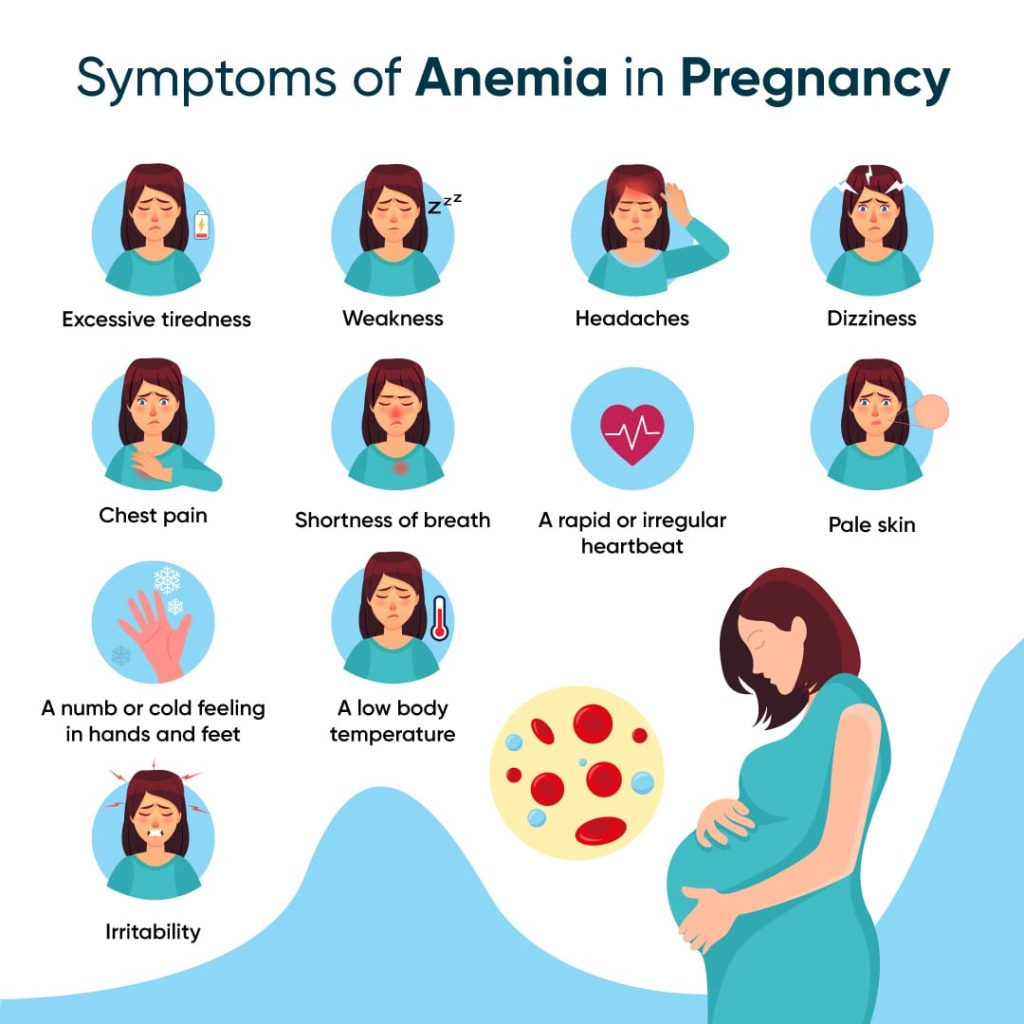
feel tired,
weakness,
Paleness of skin, conjunctiva and mucous membrane,
Shortness of breathing,
dizziness,
headache,
Rapid and irregular heartbeat,
Cold hands and feet.
Nails become brittle.
Poor concentration.
Cognitive difficulties.
Growth and development will be delayed.
Loss of appetite.
Dizziness.
tachypnea.
Tachycardia.
Palpitation.
Diarrhea and vomiting.
Cardiac enlargement with murmur sound.
Jaundice, petechiae and ecchymosis are also present in some cases.
Hepatomegaly.
Diagnostic evaluation
history taking,
Physical Examination,
Complete blood count test.
Peripheral blood smear.
Additional blood test.
Bone marrow aspiration and biopsy.
Imaging test.
x ray
CT scan.
M.R.I.
Genetic testing.
Stool examination
Management:
Assessing the causes of anemia in women.
If a woman’s anemic condition is due to nutritional deficiency, provide the child with adequate nutritional supplements such as iron, vitamin B12 and folate.
Providing women with a nutritious diet containing proper iron.
To provide adequate supplementary diet to women according to nutritional deficiency.
If a woman has anemic condition due to any infection or chronic disease, then the condition of the woman should be treated immediately.
If a woman has a condition of severe anemia, proper blood transfusion should be done.
Monitoring women regularly.
If the woman has an anemic condition due to excessive blood loss, stop it and start the intravenous infusion immediately.
To provide complete education to the woman and her family members about the condition, its causes, symptoms and signs and its treatment.
To carry out all laboratory investigations of women.
Screening women regularly to prevent them from anemic conditions.
Ion Deficiency Anemia:
Iron deficiency anemia is the most common nutritional and hematological disorder seen in pregnancy. It is generally more prevalent in areas with poor socioeconomic conditions.
Iron deficiency anemia is a condition in which the production of red blood cells decreases due to deficiency of iron in children. The condition of anemia caused by deficiency of iron which helps in the production of hemoglobin is called iron deficiency anemia.
Etiology:
Inadequate iron storage during the intrauterine period,
prematurity,
tween baby,
maternal anemia,
poverty,
Due to certain disease conditions eg
diarrheal disease,
Infection, malabsorption syndrome,
hookworm infestation,
Due to chronic illness,
Due to insufficient ion supply at birth.
Due to impaired ion absorption.
Due to blood loss.
Due to nutritional deficiency.
Due to chronic diseases.
Due to genetic factors.
Due to blood loss.
Due to infection.
Due to Bonemarrow disorder.
Due to vitamin deficiency.
Due to impaired production of red blood cells.
Due to excessive amount of blood loss.
Due to increased requirement of iron in the body.
Due to intensive breastfeeding.
Due to hereditary and genetic factors.
Symptoms and signs:
feel tired,
weakness,
Paleness of skin, conjunctiva and mucous membrane,
Shortness of breathing,
dizziness,
headache,
Rapid and irregular heartbeat,
Cold hands and feet.
Nails become brittle.
Poor concentration.
Cognitive difficulties.
Growth and development will be delayed.
Loss of appetite.
Dizziness.
tachypnea.
Tachycardia.
Palpitation.
Diarrhea and vomiting.
Cardiac enlargement with murmur sound.
Jaundice, petechiae and ecchymosis are also present in some cases.
Hepatomegaly.
Irritability.
Tiredness.
Atrophy of tongue papilla.
Diagnostic evaluation
history taking,
Physical Examination,
Complete blood count test.
Peripheral blood smear.
Additional blood test.
Bone marrow aspiration and biopsy.
Serum ferritin level test.
Total Iron Binding Capacity Test.
Imaging test.
x ray
CT scan.
M.R.I.
Genetic testing.
Stool examination
Management
Pregnant women have their hemoglobin levels checked during the first antenatal visit, then at 28 weeks and finally at 36 weeks.
Advise the mother to have an adequate well-balanced diet involving iron, protein and vitamins such as
liver
meat
egg
Green vegetables
Peas
fig
Beans
whole wheat
Green plantain
gourd
Groundnut etc.
The mother should be advised to use iron utensils for cooking and not to discard water used for cooking rice and vegetables.
In addition to a well-balanced diet, supplementary iron should be given regularly when the mother is free of nozia. It involves the following:
Ferrous Sulphate – 200 mg containing 60 mg of elemental iron.
Tablet folic acid 1 mg (it should be given with ferrous sulphate).
This tablet should be given until the hemoglobin level does not exceed 13 g/dl.
It is necessary to advise the mother to avoid frequent child birth and to advise the woman to maintain a minimum interval of three years during pregnancy so that the lost iron can be replaced again.
If the mother’s hemoglobin level is less than 10 g/100 ml, she should be admitted for investigation.
She should be given medication or oral preparations in the form of capsules.
There are preparations available such as:
Ferrous Gluconate,
Ferrous fumate,
Ferrous succinate
Give with or after Mills (meal) three times a day.
A widely used tablet is a fursolate tablet containing 200 mg (3 gm) of ferrous sulfate and 60 mg of elemental iron, copper, and manganese.
The initial dose is one tablet given three times a day with or after food, if larger amounts are required, a maximum of six tablets are given daily, which is usually stopped after 3-4 days. And this treatment is continued until the blood level is normal.
Advise the mother to start iron preparations as a maintenance dose for at least 3 months after delivery to re-maintain iron stores.
Provide parenteral therapy in cases where mother is unable to administer oral therapy.
Mother is provided by intravenous (i.v.) route or intramuscularly.
To provide adequate supplementary diet to women according to nutritional deficiency.
If a woman has anemic condition due to any infection or chronic disease, the woman’s condition should be treated immediately.
If a woman has a condition of severe anemia, proper blood transfusion should be done.
Monitoring women regularly.
If the woman has an anemic condition due to excessive blood loss, stop it and start the intravenous infusion immediately.
To provide complete education to the child and his family members about the child’s condition, its causes, its symptoms and signs and its treatment.
To carry out all types of laboratory investigations of women.
Regular screening of children to prevent women from anemic conditions.
Advising women to take adequate rest.
To provide proper emotional support to the woman and her family members.
Properly monitoring the woman’s condition including vital sign intake output chart properly recording.
- Sickle cell anemia
“Sickle cell anemia” is a severe hemolytic anemia and a hereditary and genetic blood disorder that usually affects red blood cells in which the red blood cells have an abnormal sickle cell. In this disease, red blood cells are rigid, sticky and abnormal crescent and sickle sep. The abnormal shape of these red blood cells blocks blood flow, which increases the risk of pain, organ damage, and infection. Sickle-shaped red blood cells have a life span of 30-40 days and their oxygen Carrying capacity is also decreased.
Etiology:
Due to genetic mutation.
Due to hereditary condition.
Having a family history of sickle cell disease.
Symptoms and signs:
mild jaundice,
fever,
headache,
feel tired,
weakness,
Paleness of skin, conjunctiva and mucous membrane,
Shortness of breathing,
dizziness,
Vision problems,
Leg ulcers,
Absence of speech,
Having pain episodes,
headache,
Rapid and irregular heartbeat,
Cold hands and feet.
Nails become brittle.
Poor concentration.
Cognitive difficulties.
Growth and development will be delayed.
Loss of appetite.
Dizziness.
tachypnea.
Tachycardia.
Palpitation.
Diarrhea and vomiting.
Cardiac enlargement with murmur sound.
Jaundice, petechiae and ecchymosis are also present in some cases.
Hepatomegaly.
Irritability.
Tiredness.
Pneumonia.
Traumatic rupture of an enlarged spleen.
Diagnostic evaluation
history taking,
Physical Examination,
Complete blood count test.
Peripheral blood smear.
Additional blood test.
Hemoglobin solubility test,
Bone marrow aspiration and biopsy.
Serum ferritin level test.
Total Iron Binding Capacity Test.
Genetic testing.
Management
Regular health super vision of women.
Providing adequate hydroxyurea medication to women.
Properly maintaining the hydration status of women.
To properly maintain a woman’s blood and electrolyte levels.
Providing proper antibiotic medication to women.
Improving the dietary intake of women, especially providing iron and protein containing food to the child.
If a woman’s condition of anemia is due to nutritional deficiency, then providing the child with adequate nutritional supplements such as iron, vitamin B12 and folate.
Providing women with a nutritious diet containing proper iron.
To provide adequate supplementary diet to women according to nutritional deficiency.
If a woman has anemic condition due to any infection or chronic disease, then the condition of the woman should be treated immediately.
If a woman has a condition of severe anemia, proper blood transfusion should be done.
Regular monitoring of women.
If the woman has an anemic condition due to excessive blood loss, stop it and start the intravenous infusion immediately.
If the woman has a condition of pain, provide analgesic medication.
To provide complete education to the woman and her family members about the child’s condition, its causes, symptoms and signs and its treatment.
To carry out all types of laboratory investigations of women.
Screening women regularly to prevent women from anemic conditions.
Advising women to take adequate rest.
To provide proper emotional support to the woman and her family members.
Properly monitoring the woman’s condition including vital sign intake output chart properly recording.
- Thalassemia
Thalassemia is a group of hereditary hemolytic anemias. which is an autosomal recessive genetic disorder in which the synthesis of hemoglobin is reduced/inadequate amount of production. Thalassemia is a genetic blood disorder in which the body does not produce sufficient amount of hemoglobin (protein in red blood cells that carry oxygen into the body). These red blood cells are destroyed in large amounts due to which the condition of anemia arises.
There are mainly two types of thalassemia.
1) Alpha Thalassemia,
2) Beta Thalassemia,
1) Alpha Thalassemia,
Alpha thalassemia is caused by missing or mutated alpha chain of hemoglobin.
1) Silent Carrier
In this one or both alpha globin genes are missing or mutated but no symptoms are seen.
2)Alpha thalassemia trait
These two alpha globin genes are missing or mutated, and this causes the condition of mild anemia, with mild symptoms such as fatigue or pale skin.
3) Hemoglobin H disease
In this, the condition of moderate to severe anemia arises due to missing and mutation of three alpha globin chains. It has more pronounced anemia, jaundice,
Enlarged spleen and other symptoms are seen.
4) Alpha thalassemia major
In this, all i.e. all four alpha globin genes are missing and severely mutated. Due to this, severe anemia and other health problems can be seen.
2) Beta Thalassemia,
Beta thalassemia is caused by missing or mutation of the beta chain of hemoglobin.
1) Beta thalassemia trait
A beta globin gene is missing and mutated and most of the symptoms are not seen.
2) Beta thalassemia intermedia
In this two beta globin genes are affected to a moderate degree symptoms are very wide. Due to this condition of mild to severe anemia is seen. Sometimes it also requires transfusion.
3) Beta thalassemia major (Cullis anemia)
In this both beta globin genes are severely affected. Due to which the condition of severe anemia arises. In this, transfusion is a life long requirement starting from childhood.
Another classification of the thalassemia
1) Thalassemia Major,
2) Thalassemia intermedia,
3) Thalassemia minor
- Thalassemia Major (Culis Anemia):
Thalassemia major is the most severe form of thalassemia.
It occurs when a child inherits two mutated beta globin genes, one from both parents. This results in a significant reduction or absence of the beta globin chain, a condition of severe anemia.
A person with thalassemia major requires lifelong blood transfusions from childhood to maintain hemoglobin levels and prevent complications.
Without treatment, thalassemia major can lead to growth delay, organ damage and bone problems and other health related conditions. - Thalassemia intermedia:
Thalassemia intermedia is an intermediate form of thalassemia, less severe than thalassemia major but more severe than thalassemia minor. A person with thalassemia intermedia has two mutated beta globin genes, but the degree of chromosomal abnormalities varies.
Symptoms may range from mild to moderate anemia, and some patients may require blood transfusions to manage symptoms. The need for treatment varies according to the severity of symptoms in patients with thalassemia intermedia. Patients with thalassemia intermedia may develop complications such as bone deformities, enlarged spleen, and gallstones, but these are usually less severe than with thalassemia major. - Thalassemia minor (trait):
Thalassemia minor, also known as thalassemia trait, is the mildest form of thalassemia. It occurs when a child inherits a mutated beta globin gene from one parent and a normal beta globin gene from the other parent. Patients with thalassemia minor usually have no symptoms or only mild symptoms of anemia.
Thalassemia minor carriers usually have slightly lower hemoglobin levels than normal, but they usually do not require treatment. However, carriers of thalassemia minor can pass the gene mutation on to their children.
Causes of Thalassemia:
Due to genetic mutation,
Due to impairment in alpha globin and beta globin.
Being a family history.
Symptoms and Signs of Thalassemia:
feel tired,
Pale skin, conjunctiva and mucous membrane.
Shortness of breath,
Spleen and liver enlargement (hepatosplenomegaly),
jaundice,
Growth and development are delayed,
Bone abnormalities,
heart problem,
Endocrine complications,
Getting infected.
Loss of appetite (anorexia),
Poor feeding habit,
Abdomen is distended,
Failure to Thrive,
Facial Features – Upper maxilla hypertrophoid, exposing of upper teeth, depressed nasal bridge,
mal occlusion of teeth,
lymphadenopathy or hypogonadism,
Osteoporosis of
Metacarpals and Metatarsals.
Recurrent respiratory infection,
lymph node enlargement,
Poor nutritional status.
Diagnostic Evaluation of Thalassemia:
history taking,
Physical Examination,
Complete blood count test,
Hemoglobin electrophoresis,
Peripheral blood smear,
Iron Studies,
genetic testing,
Bone marrow examination,
common
Serum bilirubin test,
Serum iron level,
Bone marrow studies,
Osmotic fragility test,
radiological findings,
Management of Thalassemia:
The patient requires repeated blood transfusions. A patient needs blood transfusion starting from early childhood and throughout the throwout life.
Provide proper iron chelating therapy to the patient. Patients are prone to iron overload due to long-term transfusions, which is why iron chelation therapy is provided to patients to prevent this condition.
This involves the involvement of iron chelating therapy (deferoxamide, deferiprone, deferasirox).
Provide proper folic acid supplementation to the patient.
Performing bone marrow transplantation on the patient.
Providing proper gene therapy to the patient.
Provide proper supportive care to the patient.
Nursing Management of Thalassemia:
Provide complete education to the patient about the condition, its causes, symptoms and signs, and its treatment.
Continuous monitoring of the patient.
Provide proper blood transfusion to the patient.
Assess whether the patient has any reaction at the time of blood transfusion.
Regular health supervision of the patient.
Properly maintain the patient’s hydration status.
Properly maintain the patient’s blood and electrolyte levels.
Provide proper antibiotic medication to the patient.
Improving the patient’s dietary intake, especially providing iron and protein containing food to the child.
If the patient’s anemic condition is due to nutritional deficiency, provide the patient with adequate nutritional supplements such as iron, vitamin B12 and folate.
Provide the patient with a nutritious diet containing proper iron.
Providing adequate supplementary diet to the patient according to nutritional deficiency.
If the patient has anemic condition due to any infection or chronic disease, treat the child’s condition immediately.
If the patient has a condition of severe anemia, then proper blood transfusion should be done.
Monitoring the patient regularly.
If the patient has an anemic condition due to excessive blood loss, stop and start intravenous infusion immediately.
If the patient has a pain condition, provide analgesic medication.
To provide complete education to the patient and his family members about the child’s condition, its causes, its symptoms and signs and its treatment.
To perform all types of laboratory investigations of the patient.
Screening the child regularly to prevent the patient from anemic conditions.
Advise the patient to take adequate rest.
Provide proper emotional support to the patient and his family members.
Properly monitoring the patient’s condition including vital sign intake output chart properly recording.
- Jaundice during pregnancy (jaundice):

Jaundice is also called icterus. Jaundice is not a disease but it is seen as a sign of disease after many diseases. Jaundice is a condition that when the amount of bilirubin in the body increases, the skin, mucus membrane, sclera of the body becomes yellow in color, it is called jaundice. Jaundice is seen when the amount of bilirubin in the body increases above 2 mg/dl, the condition of jaundice is seen.
(Note: = Normal bilirubin level is 0.8 to 1.2 mg/dl.) In Jaundice: Bilirubin level increases above 2mg/dl.
{Direct/unconjugated/fat soluble bilirubin level is 0.1-0.3 mg/dl.}
{Indirect/conjugated/water soluble bilirubin level is 0.2-0.8mg/dl.}
Bilirubin is a natural product that is released as a byproduct due to the breakdown of red blood cells and is excreted out of the body by the liver. The condition of jaundice arises when the amount of conjugated bilirubin is not used by the liver in the biliary system. Bilirubin is not excreted from the body. And due to the accumulation of bilirubin in the body itself, the condition of jaundice arises.
Type of jaundice
There are total four types of jaundice:
- Haemolytic Jaundice,
- Obstructive Jaundice,
- Hepatocellular jaundice
- Hereditary jaundice
- Haemolytic Jaundice:
Him Mins: “Blood”
Lytic Mins:
“Breakdown of Sale”
Haemolytic Mins:
“Breakdown of Sale”
Hemolytic jaundice is also called prehepatic jaundice. Raised level of bilirubin in jaundice is seen due to excessive breakdown of red blood cells.
Etiology:
sickle cell anemia,
transfusion reaction,
malaria,
thalassemia,
Autoimmune disorders.
- Obstructive Jaundice:
Obstructive jaundice is called extrahepatic type of jaundice.
Obstructive jaundice occurs when the bile duct is blocked and bilirubin is not excreted by the liver and remains in the liver. Hence it is called cholestatic jaundice because bilirubin cannot be excreted from the liver due to obstruction of the bile duct.
Obstructive jaundice causes extreme levels of body itching due to salt buildup in the body.
Etiology:
Due to carcinoma in gall bladder and bile duct,
Because gallstones are present in the biliary system,
Due to infection and inflammation.
- Hepatocellular Jaundice:
Hepatocellular jaundice is the most common type of jaundice.
Hepatocellular jaundice occurs when the cells of the liver are damaged due to any reason, the liver is unable to excrete bilirubin from the body and due to this, bilirubin increases in the blood.
Hepatocellular jaundice is mainly
liver failure,
liver diseases,
liver cancer,
hepatitis,
Viruses such as
yellow fever,
Epstein Barr virus is caused by certain types of drugs.
- Hereditary jaundice
Hereditary jaundice is mainly found in any person from his family. Hereditary jaundice is mainly due to impairment in the metabolism of bilirubin from the time of birth, excessive amount of bilirubin accumulates in the body. It is mainly seen when bilirubin is overproduced or not excreted from the body.
1) Dubin/Johnson Syndrome:
This is an inherited disorder. In this jaundice, the level of conjugated bilirubin increases in the liver.
2) Gilbats syndrome
Gilbert’s syndrome is an inherited condition mainly caused by a benign condition in which the level of bilirubin increases to a mild level.
- Rotors Syndrome:
It is an inherited disease characterized by intermittent jaundice.
Etiology:
Due to accumulation of excessive amount of bilirubin in the body.
Due to any liver cell abnormality.
Due to blockage of bile duct.
Due to inflammation in liver and bile duct.
1) Pre hepatic causes:
Due to the destruction of red blood cells,
Conditions in which red blood cells break down such as:
malaria,
sickle cell anemia,
thalassemia,
glucose 6 phosphate,
Due to drugs and other toxins,
Due to auto immune disorder.
2) Hepatic causes:
Hepatic jaundice is mainly seen when there is incapacity of the liver which leads to the condition of jaundice.
Due to hepatitis,
Cirrhosis of liver,
Due to certain drugs,
Gilbert’s syndrome,
Cancer
3) Post hepatic causes:
This is mainly due to any obstruction.
Because of Golston.
Because of cancer.
Due to stricture of bile duct.
Cholangitis
Symptoms and signs:
Yellowish discoloration of skin, mucus membrane and sclera is seen in the body.
Stools are light in color.
Yellow discoloration of urine.
Itching in the skin.
feeling tired
Abdominal pain.
Nozia
Vomiting
get a fever
Weakness.
Loss of appetite
headache
Confusion.
Swelling in leg and abdomen.
Loss of appetite.
Diagnostic evaluation
history taking,
Physical Examination,
Blood test
Complete blood count test
Liver function test
Urine analysis
Liver biopsy
Imaging study
ct scan.
MRI.
Abdominal Ultra Sonography.
Hepatitis A,B,C test.
Management:
Provide intravenous fluid to the patient to prevent the condition of dehydration.
If the patient is experiencing nausea and vomiting, provide antiemetic medicine.
If the patient is in pain, provide analgesic medicine.
Antibiotic medicine should be provided if the patient has any bacterial infection.
Provide antiviral medicine to the patient.
Transfusion of blood when required by the patient.
Providing chemotherapy and radiation therapy to patients.
Provide steroid and immunoglobulin to the patient.
Provide high carbohydrate and low protein diet to the patient.
Providing nutritional supplementation to the patient.
Provide vitamin K injection to prevent bleeding.
Any drug, toxic chemical, and alcohol cause the condition of jaundice, so avoid these things.
Surgical Management:
If there is a cancerous condition, there is a need for surgical treatment.
If the condition of jaundice is due to obstruction of the bile duct, surgically opening it.
Liver transplantation is often required.
If the patient has gallstones, then surgery to remove them.
If the patient has hemolytic jaundice, treat him by providing medication.
Nursing Management
Advise the patient to drink plenty of fluids.
Ask the patient to take adequate rest.
Tell the patient to avoid things like coffee, alcohol, junk food, drink soda, etc.
Ask the patient to take fruits and vegetables.
Avoid foods that contain preservatives.
Tell the patient to avoid meat and animal fat.
Do not ask the patient to take dairy products like cheese, milk etc.
Patient should avoid fats like ghee, butter, cream, oil for 2 weeks.
Soybean, egg, according to the patient’s condition. Dale, milk should be provided sparingly.
Ask the patient to eat small amounts of carbohydrate rich food like roti, bread, boiled potato etc.
Taking medicine as prescribed by health care personnel.
- Hepatitis:
Hepatitis is a condition characterized by infection and inflammation of the liver. Viral hepatitis is mainly
Hepatitis A viral,
Hepatitis B virus,
Hepatitis C virus,
Hepatitis D virus,
Hepatitis E is caused by viruses.
epstein barr virus,
Yellow fever virus
Rubella virus
Herpes simplex
Varicella virus
AD virus
All these viruses also cause hepatitis.
The hepatitis virus enters the liver and multiplies there, then damages the liver and causes inflammation and necrosis of the hepatocytes. When the hepatitis virus enters the body, its signs and symptoms are seen in three phases.
- Preicterus phase or prodomal phase
- Icterus face
- Convolescent face
- Preecterous Phase or Prodomal Phase:
This phase can be seen for one to two weeks. In this phase, the patient has flu-like symptoms.
such as,
feel tired,
loss of appetite,
body aches,
nozia,
vomiting,
Diarrhea, and
Constipation.
- Icterus face:
An icterus face begins five to ten days after exposure to the hepatitis virus and signs and symptoms appear. This phase is seen from two to six weeks. In this phase, the level of bilirubin increases in the body, due to which the skin, mucus membrane of the body is seen in a yellowish color.
Jaundice condition is seen in this phase.
In this phase there is itching due to bile salt deposits in the patient’s skin.
In this phase, stool is light brown and clay in color due to non-excretion of bile through the normal fecal pathway.
- Convalescent phase:
The convalescent phase is followed by the icterus phase. This phase is seen for a few weeks and even for a few months. In this phase there is a gradual improvement in its signs and symptoms.
- Hepatitis A During Pregnancy:
Hepatitis A (A) is a viral infection that causes infection or inflammation of the liver, mainly R. N. A (RNA Viral) is caused by a virus. Hepatitis A is transmitted mainly through the oral route. It is mainly transmitted through food or liquid contaminated with the hepatitis A virus. It is transmitted by a person who has not properly washed their hands after a bowel movement and prepares food.
The incubation period of hepatitis A is between 15 to 50 days. And the average is 30 days.
Hepatitis A (A) virus can be seen from four to eight weeks (4 to 8 weeks).
Etiology:
- Contaminated food or water:
Transmitted through food and food materials prepared by an infected person. - Person to Person Contact:
Due to coming in direct contact with any infected person or due to coming into contact with his items.
3) Due to poor sanitation.
4) Due to poor hygiene.
5) Due to over crowding.
6) Due to not washing hands properly after bowel movement.
7) Drinking contaminated water.
8) Due to eating under cooked selfies.
9) Due to blood transfusion.
By not reusing a contaminated needle due to sexual contact with a person who has hepatitis A virus infection.
Symptoms and signs:
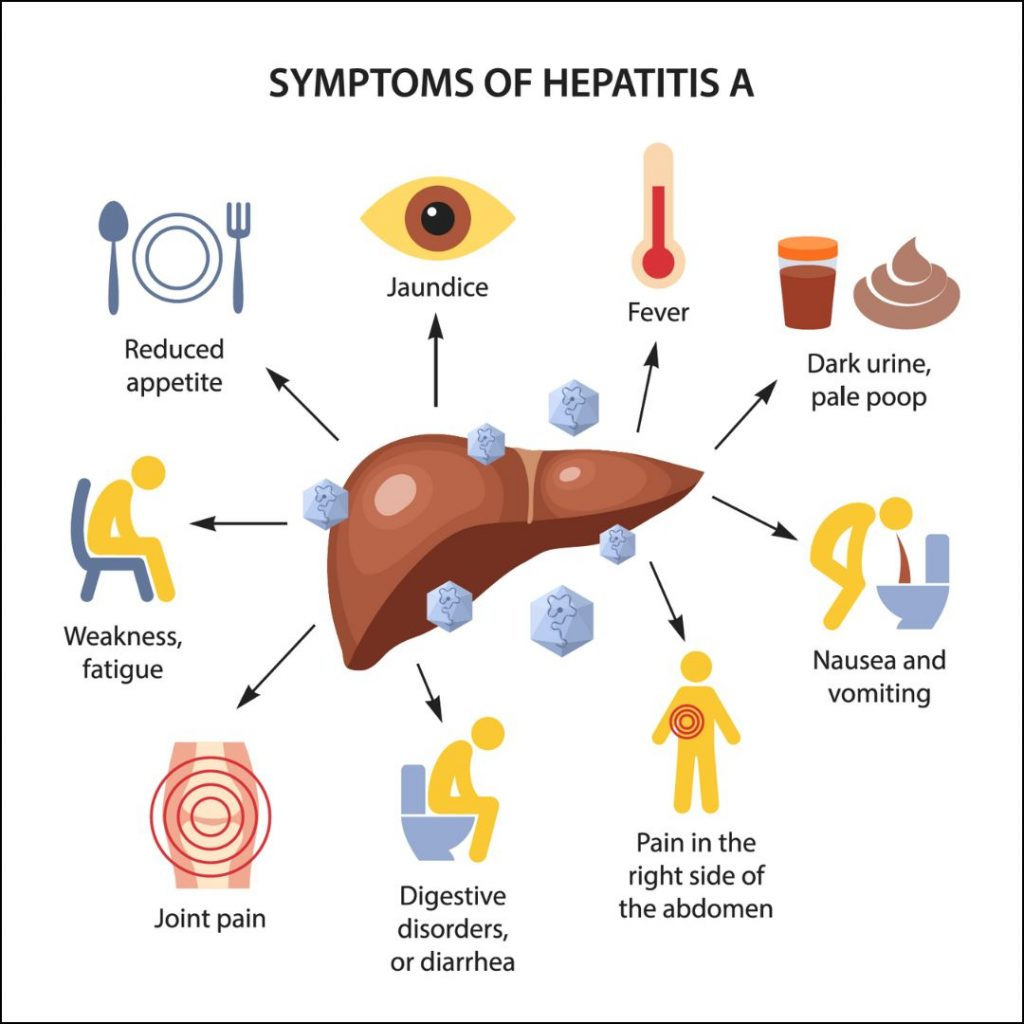
In this the patient has flu like symptoms.
Upper respiratory tract infection
Getting a low grade fever.
Loss of appetite.
Indigestion.
nozia,
Vomiting
Diarrhea
Clay colored stools
Become a heart
Jaundice
Weakness.
headache
feeling tired
Generalized Weakness
Stomach clamps
Diagnostic Evaluation:
History Collection,
Physical Examination,
blood test,
Assay the immunoglobulin level,
Assess the liver function test
Ultrasound
ct scan.
MRI.
Management:
Do not ask the patient to take alcohol.
Ask the patient to avoid eating fatty food.
Ask the patient to maintain personal hygiene.
Ask the patient to do proper hand washing.
Ask the patient to avoid unprotected sex.
Ask the patient to take a nutritional diet.
Provide intravenous glucose to the patient.
Advise patient to maintain no body weight.
Ask the patient to take adequate bed rest.
Ask the patient to avoid physical activity.
Ask the patient to do small amounts of activity.
If the patient has nosia and vomiting, provide antiemetic medicine.
Nursing Management:
To monitor patient’s vital signs frequently.
Monitor the patient’s weight daily.
Assessing the patient’s frequent stools.
Provide oral fluids to the patient frequently.
Providing intravenous feed to the patient.
Monitoring the patient’s intake-output chart.
Monitoring the nutritional status of the patient.
Ask the patient to eat in a sitting position.
Providing patients with small, free quantitative dietary supplements.
Maintaining oral hygiene of the patient.
Provide oral care to the patient.
Ask the patient to take diet in small and frequent amounts.
Provide work and quiet environment while feeding the patient.
Ask the patient to take adequate rest.
To monitor patient’s daily intake output chart.
Provide proper oxygen to the patient.
- Hepatitis B During Pregnancy:
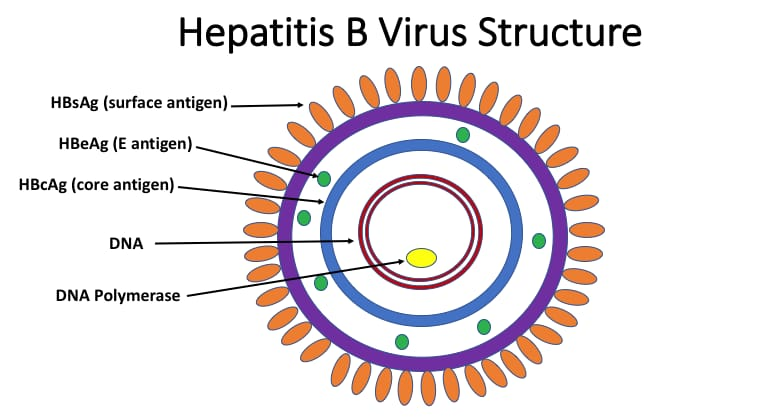
Hepatitis B is also called serum hepatitis. Hepatitis B is mainly transmitted by the hepatitis B virus. The hepatitis B virus is mainly present in the blood, saliva, semen and vaginal secretions of an infected person. Hepatitis B virus creates infection and inflammation in the liver which is called severe form life threatening infection. Hepatitis B virus is a life long infection due to
Liver cirrhosis
Liver failure
Liver cancer
And death can also happen.
Hepatitis B occurs in both acute (acute: rapidly developing) and chronic (chronic: long lasting) forms. The incubation period of hepatitis B ranges from one to six months. Hepatitis B is primarily transmitted by the hepatitis B virus which Mainly present in blood, semen, and other body fluids.
Etiology:
Caused by hepatitis B virus.
Transmitted through blood, saliva, semen, vaginal secretions etc. of an infected person.
Unprotected sexual contact
by.
Through contact with infected needles and syringes.
Mother to Child Transmission.
Intravenous drug users.
Health care workers.
A person who undergoes frequent blood transfusions.
By coming into sexual contact with an infected person.
Due to sexual contact with multiple partners.
Due to intravenous drug abuse.
Due to repeated exposure to blood.
Due to sharing toothbrushes and razors.
Dialysis patients.
Due to repeated any medical procedure.
Symptoms and signs:
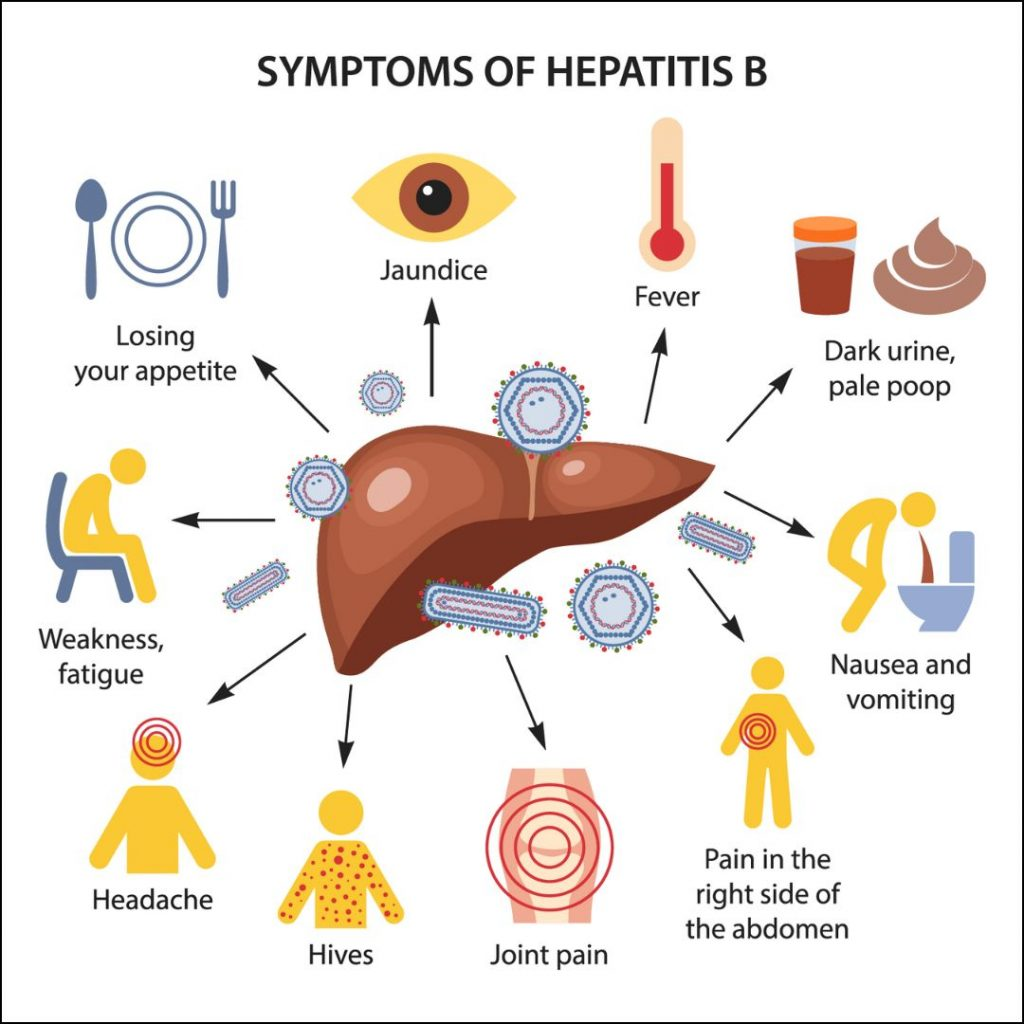
Hepatitis B virus after exposure to the virus
12 wicks are found.
Jaundice
get a fever
Loss of appetite.
Respiratory symptoms are observed.
Abdominal discomfort.
races.
Abdominal pain.
Nozia.
Vomiting.
Generalized pain.
Weakness.
Dark yellow urine.
Liver a tender, enlarged.
Clay colored stools
Lethargy.
Adjudication of the spleen occurs in some cases and is palpable
Diagnostic evaluation
History Collection,
Physical Examination,
Assay the albumin level,
Assess the liver function test,
Assay the prothrombin time,
Assay about the presence of antibody HBsAG (anti-HBs).
antibody to hepatitis B core antigen (Anti-HBc).
hepatitis B surface antigen (HBsAG).
hepatitis E surface
Antigen (HBeAG).
Management.
medical management
If the patient has acute hepatitis, lifestyle modification should be done.
Ask the patient to take proper bed rest.
Ask the patient to take adequate fluids.
Advise patient to take nutritional diet.
Ask the patient to avoid alcohol if he has a chronic hepatitis condition.
Tell the patient to avoid over the counter medicine.
Providing interferon alpha medication to patients with chronic hepatitis B conditions.
Interferon-alpha increases the activity of the body’s immune system and impairs the reproduction of the hepatitis-B virus.
Interferon-alpha tablets are taken daily or three times a week for six months.
Provide the patient with lamivudine and adenovir medication.
Ask the patient to take adequate bed rest.
Properly maintain the nutritional status of the patient.
Provide adequate fluid to the patient.
Liver transplantation if the patient has severe condition.
Nursing Management:
Maintain patient’s skin integrity.
Providing good skin care to patients.
Tell the patient not to use irritating ointments.
Ask the patient to apply an emollient.
Ask the patient to keep fingernails short.
Assess the patient for any bleeding.
If the patient has itching, provide medication to reduce it.
Changing the patient’s position frequently to prevent pressure ulcers.
Assess the patient for any neurological signs and symptoms.
To provide work and quiet environment to the patient.
Ask the patient to report any bleeding immediately.
Monitor the patient’s prothrombin time and bleeding time and administer vitamin K.
Do not perform any procedure that causes any trauma to the patient.
Take proper care to avoid any needle stick injury to the patient.
Prevention:
Getting the hepatitis B vaccine properly to prevent hepatitis B.
Proper screening of donated blood.
Use of disposable series-needle.
Ask the patient to maintain good personal hygiene.
Daily disinfection of the working area.
Wear gloves when working with any body fluid.
Asking individuals who are health care personnel and high-risk individuals to receive hepatitis B vaccine.
A total of three doses of hepatitis B are taken.
After one month after taking the first dose, the second dose (2nd dose) and then six months after the first dose, the 3rd dose of hepatitis B is taken.
If anyone has come in contact with hepatitis B virus due to needle stick injury, get vaccinated immediately.
Avoid sexual contact with a person who has acute or chronic hepatitis.
Use of barrier method as contraceptive during sexual activity.
Avoid sharing personal items like toothbrushes and razors.
Do not use any needles or syringes that have not been disinfected and use disposable series and needles.
Avoid coming in contact with body fluids of an infected person.
- Hepatitis C During Pregnancy:
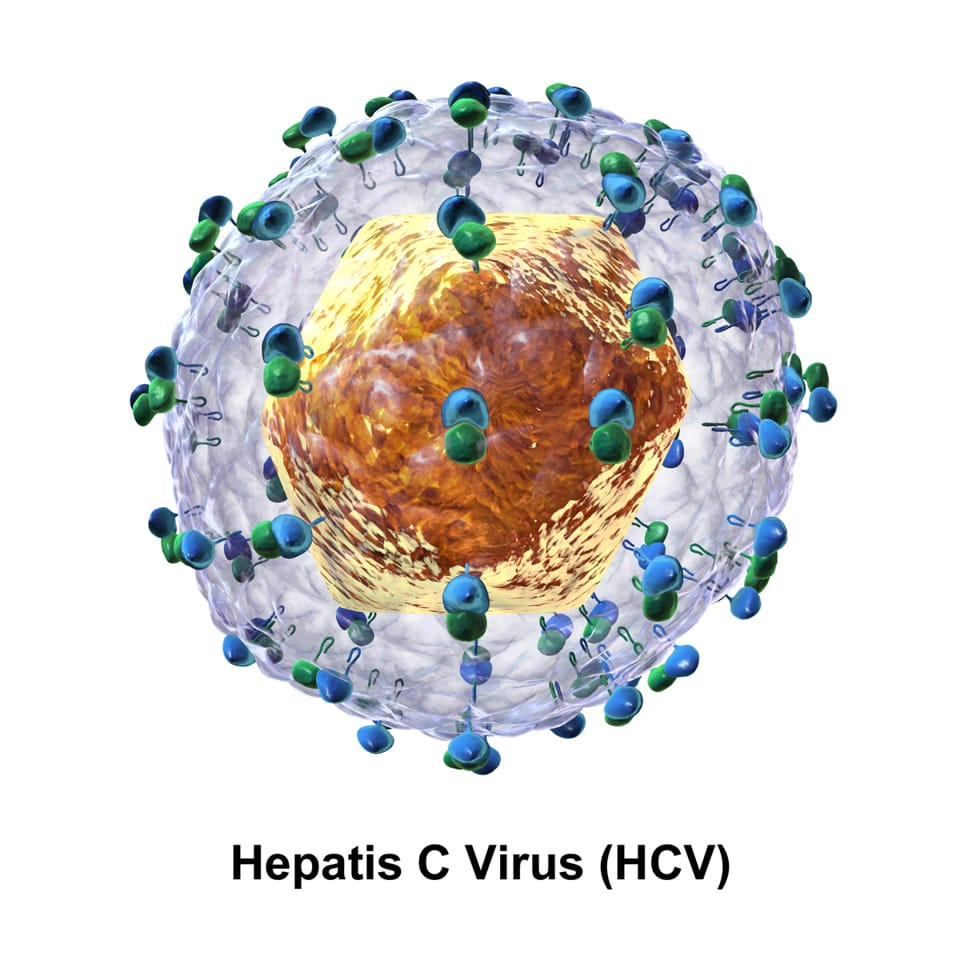
Hepatitis C is an infection and inflammation of the liver and is mainly caused by the hepatitis C virus.
occurs through Hepatitis C is a viral infection caused by the hepatitis C virus, an RNA virus belonging to the family of viruses of the Flaviviridae group. Hepatitis C was first identified in 1989. Hepatitis C is spread primarily by direct contact with the blood of an infected person. Hepatitis C is different from Hepatitis A and B.
Incubation period of hepatitis C
It is 15-160 days.
Etiology:
Due to hepatitis C virus,
Due to prolonged dialysis,
Due to working with blood regularly.
Due to having unprotected sexual activity with a person who has hepatitis C infection.
Due to contact with any body fluid of a person who has hepatitis C infection.
Due to any needle stick injury.
Due to blood transfusion.
Due to tattooing by any infected instrument.
Due to any accidental needle stick injury.
Due to any organ transfusion.
Due to sharing of personal items such as toothbrushes and razors.
Due to giving birth to her child by a mother who has hepatitis C infection.
Among individuals who are sexually active.
Among individuals who have multiple partners.
Symptoms and Signs:
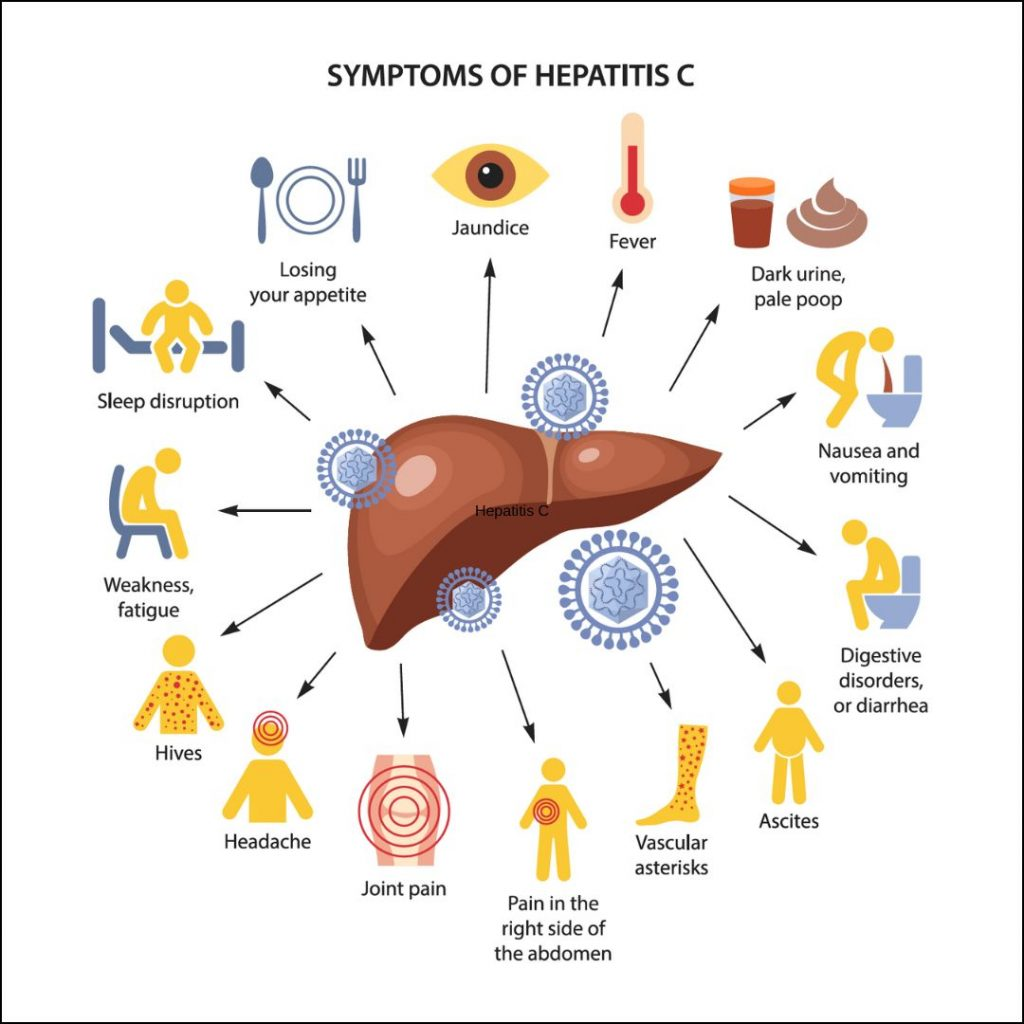
liver failure,
Cirrhosis of liver,
Abdominal pain (right upper abdomen),
Abdominal swelling.
jaundice,
Dark urine and
Passing pale and clay colored stools.
Building up from the esophagus and stomach.
Dark urine.
feeling tired
Etching.
Muscle and joint pain.
Getting a fever.
Loss of appetite.
Nozia.
Vomiting.
Liver cancer.
Diagnostic Evaluation:
History Taking,
Physical Examination,
Liver function test,
Assay EIA (enzyme immunoassay) to detect hepatitis C antibody.
hepatitis c genotypes.
Assay the albumin level.
Assess the liver function test
Assay the prothrombin time
Liver biopsy.
Management:
Advise the patient to take adequate rest.
Keep the patient properly isolated.
Properly disposable syringe should be used while handling the patient.
Proper disposal of patient excreta.
To provide proper work and comfortable environment to the patient.
Advise the patient to properly intake safe drinking water.
To check patient’s vital sign properly.
Providing antiviral medicine to the patient to treat hepatitis C virus
Ex: pegylated interferon alfa and ribavirin
Ask the patient to maintain good hand washing technique.
Ask the patient to follow streak aseptic technique.
Follow strict aseptic technique when visiting a person who has an infection.
Provide patient education not to scratch the area where the itching is occurring.
If the patient has abdominal discomfort, feels very tired, has skin rashes and has fever and vomiting, then inform the doctor immediately.
Providing education to the patient or doing tattooing and skin piercing can also cause transmission of Hepatitis B.
Provide education to the patient or don’t donate blood after hepatitis C infection.
Ask the patient to take rest between activities.
Ask the patient to come for regular checkup.
Advise a person who is infected with hepatitis C to avoid sexual activity.
Ask the patient to use a barrier method of contraception during sexual activity.
- Hepatitis D During Pregnancy:

Hepatitis D is also called delta virus. Hepatitis D is an infection and inflammation of the liver mainly caused by the hepatitis D virus. Hepatitis D is a viral infection caused by the hepatitis D virus. Hepatitis D is also called a satellite infection because hepatitis D occurs primarily in individuals who have hepatitis B. Hepatitis D increases the severity of hepatitis B and damages the liver to a greater extent. It is mainly transmitted through contact with any infected blood.
Etiology:
Due to coming into contact with infected blood and body fluid.
In individuals who have hepatitis B.
Due to sharing of needles, saws, and personal utensils like toothbrushes, razors of infected persons.
Due to sexual activity with an infected person.
Due to unprotected sexual activity.
Intravenous drug users.
Due to direct contact with the blood of an infected person.
Due to the birth of a baby by an infected mother.
Due to having hepatitis B infection in the past.
Due to receiving blood transfusion.
Symptoms and signs:
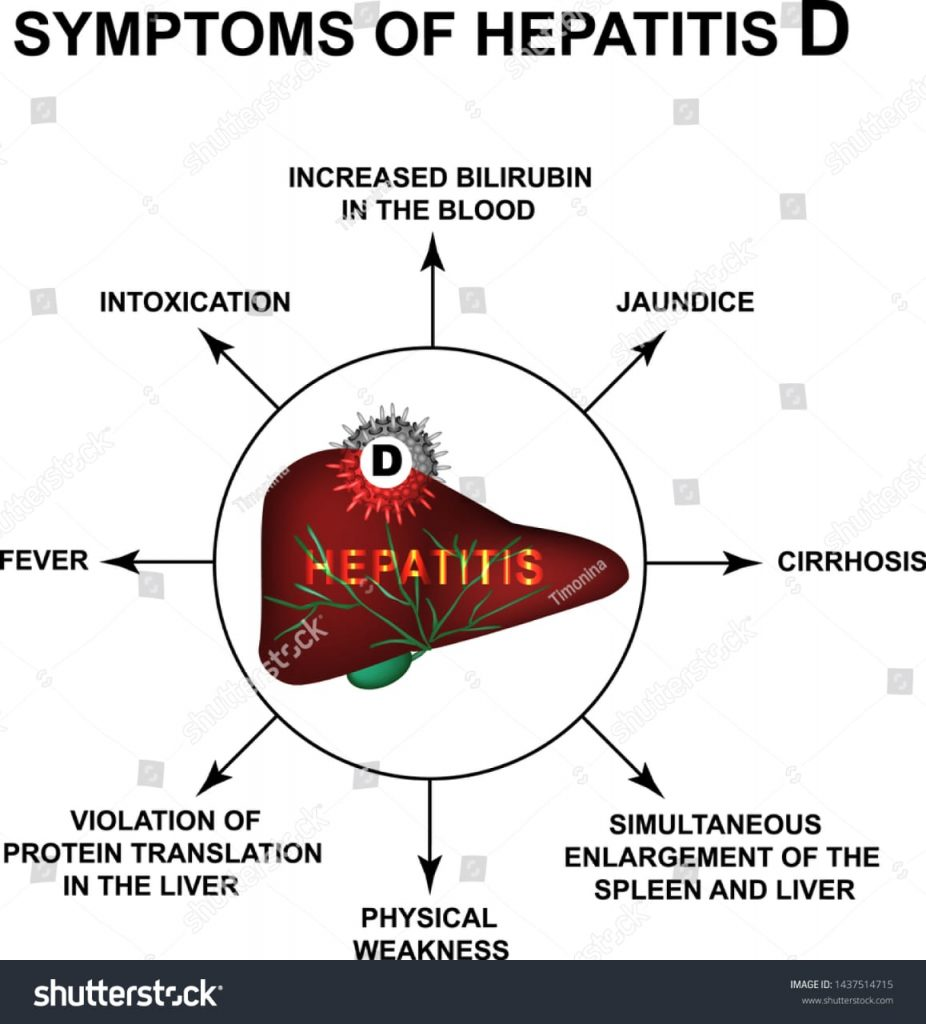
1) Flu like symptoms:
feel tired,
weakness,
Pain in the muscles,
fever,
2)Jaundice:
Due to accumulation of bilirubin in the body, yellowish discoloration of skin, mucus membrane and sclera is seen.
3) Abdominal Pain:
Pain and discomfort in the upper right quadrant of the abdomen occurs due to inflammation of the liver.
4) Dark urine:
Urine is dark in color due to the buildup of bilirubin in the body.
5) Pale or clay colored stool
Due to non-excretion of bilirubin from the body, the stool is pale and clay colored.
6) Nausea and Vomiting:
Many times patients with hepatitis D have nosia and vomiting condition.
7) Loss of Appetite:
A person does not feel hungry due to hepatitis D.
8) Joint pain
A person experiences joint pain due to disease.
9) Confusion.
10) Itching.
11) Fever.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Liver biopsy
Blood test
Liver function test
Liver enzymes
Abdominal ultra sound
Anti delta agent antibody test
Management:
Medical Management:
Provide antiviral medication to the patient.
Ex: = tenoflovir,
Entecavir.
Patient ne interferon -alpha
Provide medication.
Monitor the patient’s liver function test regularly.
Ask the patient to take an adequate nutritional diet.
If the patient has nosia and vomiting condition then provide antiemetic medicine.
If the patient’s condition has worsened, liver transplantation should be done.
Providing vaccines to patients.
Ask to avoid drugs that alter liver function or damage liver cells.
Ask the patient to take high carbohydrate foods like bread, jam, wheat, biscuits, rice, vegetables, potatoes, etc.
Ask the patient not to share his personal equipment like toothbrush, razor etc.
Advise to avoid sexual contact with an infectious person.
Nursing Management:
Assessment:
Ask about the patient’s thorough medical history and signs and symptoms of the disease.
To monitor patient’s vital signs.
Assess the patient for jaundice, abdominal pain, and any other signs and symptoms.
Symptoms Management:
If the patient has nosia and vomiting, provide antiemetic medicine.
If the patient is in pain, provide analgesic medicine.
Maintaining the patient’s comfort level.
Advise on maintaining the client’s nutritional status
Ask the patient to take a well-balanced diet that contains adequate amounts of calories and vitamins so that the liver can function properly.
Monitor the patient for any signs and symptoms of malnutrition.
4) Maintain fluid balance properly.
Maintaining patient no intake output chart.
Ask the patient to take adequate amount of fluids.
Maintain patient’s hydration status.
If the patient has a condition of severe dehydration, provide intravenous fluids and maintain the patient’s hydration status.
5) Infection control:
Providing education to patients to maintain proper hygienic condition.
Provide education to patients for proper hand washing.
Ask the patient to maintain aseptic technique.
6) Rest and Activity:
Adequate to the patient
Ask to take a rest.
Ask the patient to do small amounts of physical activity.
Ask the patient to do moderate daily routine activities.
7) Psychological Support:
Provide proper psychological support to the patient.
To clear all the draughts of the patient.
To give complete information to the patient about the disease and its treatment.
8) Medication Administration:
Provide proper antiviral medicine to the patient.
Providing education to patients for lifestyle modification.
To monitor patient’s vital signs.
Liver function test of the patient.
Perform all laboratory investigations of the patient.
Provide education to patients to receive hepatitis B vaccination.
Patient is regular
Ask to follow-up.
- Hepatitis E (E) during pregnancy

Hepatitis E is a viral infection that is transmitted by the hepatitis E virus. Hepatitis E is an infection and inflammation of the liver and is mainly transmitted by the hepatitis E virus. Hepatitis E was mainly discovered in 1990. Hepatitis E is mainly transmitted through the phyco-oral route ie through contaminated/infected food and water.
Incubation period of hepatitis E
It ranges from two to nine weeks. Hepatitis E is self-limited but it can severely affect pregnant women. It can also cause abortion and intrauterine death in pregnant women.
Etiology:
by hepatitis E virus.
genotypes:=1,2,3,4
Genotype := 1,2 are associated with the human infection.
Due to intake of contaminated food and water.
Due to poor sanitation.
Due to poor hygienic conditions.
Due to low socio economic condition.
During the third trimester of pregnancy.
In International Travelers.
A person who lives in an area with an outbreak of hepatitis E.
A person who has sexual activity with an infected person.
Due to unprotected sexual activity.
Symptoms and signs:
weakness,
feel tired,
fever,
Pain in the muscles,
nozia,
vomiting,
Loss of appetite (anorexia),
abdominal pain,
Pain in right upper quadrant part of abdomen.
Jaundice: Jaundice causes yellowish discoloration of skin, mucous membrane and sclera.
Passage of dark colored urine due to bilirubin.
Passing pale and dark colored stools.
Liver enlargement (hepatomegaly).
Itching due to accumulation of bilirubin in the skin,
weakness,
malays,
Joint pain
Pain in the muscles,
Weight loss.
Diagnostic Evaluation:
history taking,
Physical Examination
Blood test
Anti-HEV igM
Antibody test.
Liver function test
Serological test
Stool examination
Imaging study
assess the hepatitis A,
hepatitis B,
hepatitis c test.
Management:
There is no specific treatment for hepatitis E but it subsides on its own.
Keep the patient on a nutritious diet.
Administer antiemetic medicine to treat the patient’s condition of nausea and vomiting.
Provide the patient with high carbohydrate foods such as bread, jam, wheat, biscuits, rice, vegetables, and potatoes.
Ask to maintain good hygienic condition of patient.
Avoid eating uncooked food.
Do not drink contaminated water.
Complete health history and physical examination of the patient.
Ask the patient about any signs and symptoms of hepatitis.
Ask the patient to take some rest between activities.
Assess the patient’s working ability.
To provide work and quiet environment to the patient.
Provide high calorie diet to the patient.
Monitor patient’s intake output chart.
Serving food to the patient in an attractive manner.
Providing a relaxing environment to the patient.
Ask the patient to maintain oral hygiene.
Ask the patient to avoid carbonated drinks.
Ask the patient to adopt proper hand washing technique.
Ask the patient to maintain personal hygiene.
Ask the patient to avoid unprotected sexual activity.
Avoiding sexual activity with someone who is infected.
Use of barrier method as contraceptive during sexual activities.
Providing education to patients on proper skin care.
Asking the patient to bathe with warm water, do not use hot water as it increases skin dryness.
Ask the patient to avoid using alcohol-based soaps.
Ask the patient to apply a proper emollient.
Ask the patient to keep his fingernails short.
Urinary tract infection
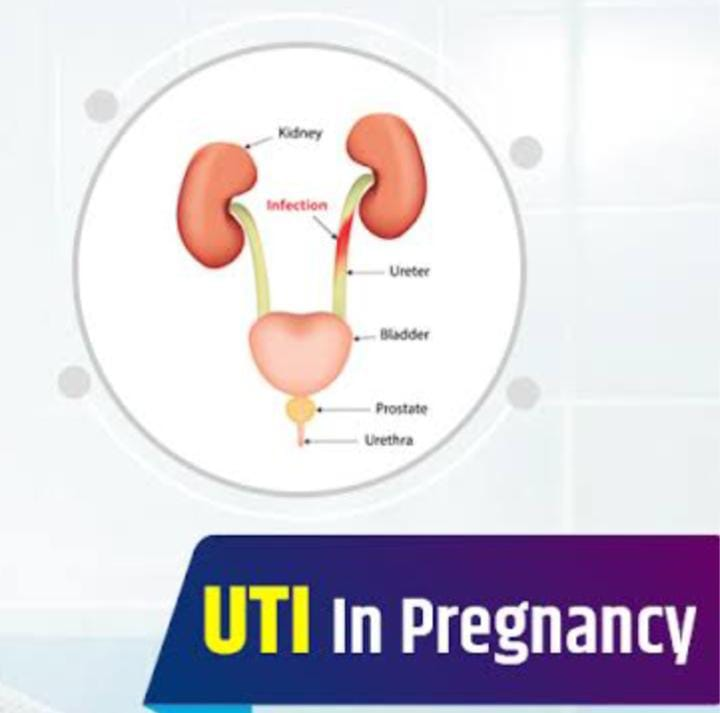
Urinary tract infection is mainly infection and inflammation in the part of urinary system. The urinary system mainly consists of the kidneys, ureters, bladder, and urethra. If infection and inflammation occurs in this system, it is called urinary tract infection. Urinary tract infections are mainly caused by pathogenic microorganisms. If the urinary tract infection mainly affects the upper urinary tract, it is called pyelonephritis. If the urinary tract infection mainly affects the lower urinary tract, it is called simple cystitis.
Types of urinary tract infection:
There are two main types of urinary tract infections.
1) Upper urinary tract infection
2) Lower urinary tract infection
1) Upper urinary tract infection,
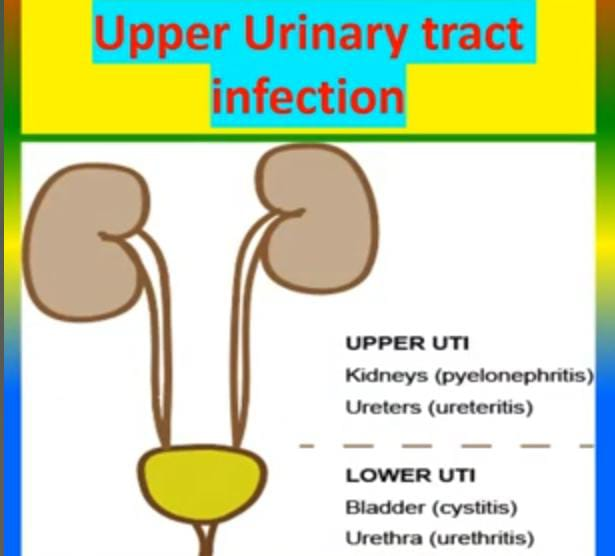
Upper urinary tract infections are mainly called pyelonephritis. Upper urinary tract infection mainly involves the kidneys and ureters. It causes fever, chills, nausea, vomiting and other symptoms.
2) Lower urinary tract infection.
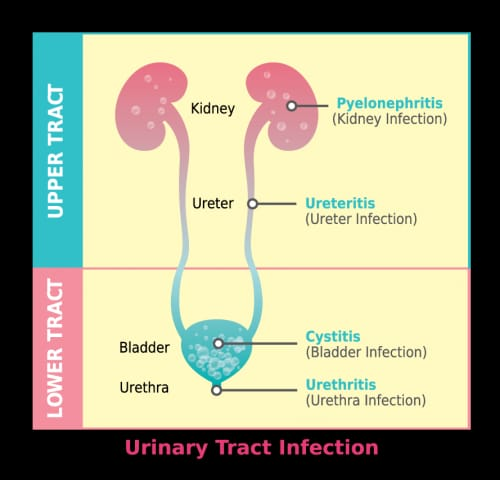
Lower urinary tract infection is called simple cystitis.
Lower urinary tract infections mainly involve the bladder and urethra.
Etiology:
Escherichia coli,
Klebsiella,
enterococcus,
enterobacter,
pseudomonas,
proteus,
staphylococcus,
mycoplasma,
Chlamydia,
risk factor
1) Female :
short urethra,
Structural abnormality due to line.
Due to urethral stricture.
Due to urethral vesical function abnormality.
Due to obstruction
Due to tumor being present.
Being calculi present.
Due to prostatic hypertrophy.
Impaired Bladder Innervation:
Due to multiple sclerosis.
Due to urinary stasis. Due to neurogenic bladder.
Due to chronic diseases:
immuno suppression,
Glomerulo
Due to nephritis,
Due to hyper tension.
Due to sickle cell anemia.
Edge:
Due to anemia.
Due to malnutrition.
Symptoms and signs
dysuria,
Increased frequency of urination.
Urgency for urination.
Hematuria (blood in urine).
Cloudy and foul smelling urination.
Pelvic pain.
Flank pain.
Fever
Chills
Nozia
Vomiting
Urinary incontinence.
Lower back pain.
headache
Pain during urination.
Diagnostic Evaluation:
History Collection,
Physical Examination.
Complete blood count.
Urine analysis.
Urinary microscopy.
Urine culture.
Ultrasound.
X ray.
MRI.
Cytoscopy.
Medical Management:
Monitor patient’s intake output chart.
To assess whether the patient has any kind of adverse reaction or not.
Advise the patient to increase fluid intake.
Provide antibiotic medicine to the patient.
Ex:=
ciorofloxacin,
Norfloxacine,
Nitrofurantoin/trimethoprime.
If the patient is in pain, provide analgesic medicine.
Ex:=
Acetaminophen,
Ibuprofen
Advise patient to avoid irritating food like alcohol, tea coffee, spicy food, hot food.
Advise the patient to maintain personal hygiene.
Provide psychological support to patients.
Advising the patient to take proper medication.
Nursing Management of Patient:
Properly assess the patient.
Advise the patient for proper fluid intake.
If the patient is in pain, provide analgesic medicine.
Providing Mind Diversional Therapy to the patient.
Assessing the effectiveness of the patient’s medication.
Provide properly prescribed antibiotic medicine to the patient.
Advise the patient to maintain proper personal hygiene.
Advise patient to take adequate amount of rest.
To assess whether the patient has any other type of complication or not.
Advise the patient to follow up regularly.
Proper documentation of patient information.
Providing proper psychological support to the patient.
To provide work and comfortable environment to the patient.
Advise the patient to take a properly nutritious diet.
Advise the patient to follow up regularly.
Provide psychological support to patients.
To clear all the doubts of the patient.
To provide work and comfortable environment to the patient.
- Upper urinary tract infection
Upper urinary tract infection is called pyelonephritis. Upper urinary tract includes kidneys and ureters. Pyelonephritis involves involvement of kidneys, ureters, calyx and renal pelvis. Pyelonephritis is mainly caused by bacterial infection. In pyelonephritis, the bacteria mainly travel from the lower urinary tract (bladder and urethra) to the upper urinary tract (kidneys and ureters) and create infection and inflammation in the upper urinary tract.
Types of Pyelonephritis:
There are two types of pyelonephritis.
1) Acute pyelonephritis
2) Chronic pyelonephritis
1) Acute pyelonephritis,
Acute pyelonephritis develops rapidly and the onset of symptoms is sudden. Acute urinary tract infection is mainly
Seen from 24 to 48 hours to a week.
Etiology:
Causes of acute pyelonephritis:
Due to bacterial infection.
Escherichia coli.
Vesicourethral reflux
Due to urinary obstruction.
Due to impaired immune system.
Due to indwelling catheter.
Klebsiella.
Caused by Enterobacter species.
2) Chronic pyelonephritis:
Chronic pyelonephritis develops gradually and is mainly of extended period.
seen up to
Chronic pyelonephritis is mainly due to repeated episodes of acute pyelonephritis infection resulting in chronic pyelonephritis.
In chronic pyelonephritis
Renal inflammation
And due to fibrosis of tubules and interstitial tissues, it is seen in end stage renal diseases. Chronic pyelonephritis is mainly seen from 6 months to 1 year.
Chronic pyelonephritis is caused by recurrent or persistent renal infection, vesico-urethral reflux, and urinary tract obstruction.
Causes of chronic pyelonephritis.
Due to bacterial infection.
Due to neurogenic bladder.
due to hypertension.
Due to obstruction of urine flow.
Due to repeated infections.
Due to structural damage.
Kidney stone.
Due to urinary tract abnormality.
Symptoms and signs:
get a fever
Feeling cold.
Flank or back pain.
Urinary frequency increases.
Nausea and vomiting.
Painful urination.
Urinary frequency increases.
Costovertebral angle curvature.
Hematuria.
Fatigue.
Flank tenderness.
Malay.
Back pain.
Dysuria.
Confusion.
Diagnostic evaluation
History Collection,
Physical Examination,
Urinalysis.
Urine culture.
Sensitivity test.
Complete blood count test.
Blood culture.
Intravenous pyelography (IVP).
Kidney ultrasound.
CT Scan.
Voiding cytourethrography
Cytography
Renal biopsy.
MRI.
Medical management.
Provide antibiotic medicine to the patient.
Ex:=
Tobramycin,
Gentamycine,
Vancomycin,
Ciprofloxacine,
Norfloxacine, Trimethprim,
Sulfamethoxazole
Provide antipyretic medicine to the patient.
Ex:=Paracetamol.
Provide urinary antiinfective medicine to the patient.
Ex:=
Nitrofurantin,
Trimethoprime.
Provide urinary antiinfective medicine to the patient.
Ex:=
Tab Phenazopyridine.
Surgical management of patients with pyelonephritis:
1)Ureteroplasty:
In this procedure, strictures in the ureters are surgically removed or repaired.
2) Urethral reimplantation
Urethral reimplantation is performed to cure permanent vesicourethral reflux.
3) Urethral stent
Urethral stents primarily increase urine flow.
4) Percutaneous ultrasonic pyelolithotomy
Percutaneous ultrasonic paeolithotomy is mainly used to remove crush and stones.
Nursing Management
Properly of the patient
Making an assessment.
To assess the patient’s proper witer sign.
Advise the patient to have adequate fluid intake.
Provide intravenous to the patient.
To provide proper medicine to the patient.
Provide analgesic medicine to relieve the patient’s pain.
Advising the patient to take proper medication.
Maintain proper intake output chart of patient.
Advise the patient to maintain aseptic technique.
Advising the patient for proper follow up.
Advise the patient to take adequate rest.
Lower urinary tract infection:
In lower urinary tract infection, infection and inflammation occurs in the bladder and urethra, the lower part of the urinary system. Lower urinary tract infection occurs due to many reasons.
Like:
1) Urethral vesico reflux.
2) Due to bacterial infection in urinary tract.
Lower urinary tract etiology:
Due to bacterial infection.
Ex:
E.coli.
Klebsilla.
Enterococcus.
Staphylococcus saprophyticus.
Due to urinary tract abnormalities.
Due to a weakened immune system.
Urinary catheter.
Due to certain types of drugs.
Due to radiation.
Due to unhygienic condition.
Due to congenital deformity in urinary system.
Unprotected sexual intercourse.
Due to any other infection.
State the symptoms and signs:
Burning sensation during urination.
Urinary frequency increases.
Urgency in urination.
Passing small and frequent amounts of urine.
Nocturia.
Urinary incontinence.
Foul smelling urine.
Hematuria.
Discomfort in the pelvic area.
Back pain.
Pelvic pain.
Getting a low grade fever.
Nozia.
Vomiting.
Diagnostic Evaluation:
History Collection,
Physical Examination
Urine analysis.
Cytoscopy.
Ultrasound.
x ray
Intravenous urography
Medical Management:
Provide antibiotic medication to the patient.
If the patient is in pain, give analgesic medicine.
Advise the patient to exercise properly.
Advise the patient to maintain personal hygiene.
Advise the patient to intake plenty of water.
State Nursing Management:
Take a complete history of the patient.
Take a proper history of what type of signs and symptoms the patient has.
Advising the patient to take proper medication.
to the patient’s pain
Provide antispasmodic medication to relieve.
If the patient has a condition of inflammation, provide aspirin medicine.
Advising the patient to perform a hit application.
Advise the patient to have plenty of fluid intake.
Advising the patient to avoid irritating substances like tea, coffee, cold drinks and spicy food.
Advise the patient to maintain proper personal hygiene.
To measure patient’s vital signs properly.
Advise the patient to have plenty of fluid intake.
Provide psychological support to patients.
To provide complete information to the patient about his disease condition, causes, symptoms and signs.
- Diabetes Mellitus:
Diabetes is a chronic metabolic disorder in which carbohydrate, protein and lipid metabolism is impaired. Diabetes is a group of metabolic disorders in which a person’s blood has high blood sugar levels. This mainly affects insulin secretion and insulin action in the body. If there is any impairment, high blood sugar level is seen in the body.
The “3 P” syndrome is predominantly seen in diabetes mellitus.
1)P: Polyuria (Frequent urination : passing urine frequently),
2)P: Polydipsia (increased thirst),
3)P: Polyphagia (Increased Hunger: Feeling very hungry).
Types of Diabetes Mellitus:
There are four main types of diabetes.
Type:1 (IDDM) Insulin Dependent Diabetes Mellitus.
type: 2 ( NIDDM )Non Insulin Dependent Diabetes Mellitus.
Type: 3 Diabetes Mellitus Associated Other Disease Conditions.
type:4 GDM Gestational Diabetes Mellitus.
Type: 1 (IDDM) Insulin Dependent Diabetes Mellitus:
This is a type of diabetes mellitus in which there is a total deficiency of insulin due to the destruction of the pancreatic beta cells in the body which are responsible for the production of insulin due to any autoimmune disease. It is taken by injection. This type of diabetes is mainly seen before the age of 30 years.
type: 2 ( NIDDM )Non Insulin Dependent Diabetes Mellitus.
Type 2 diabetes is mainly insulin resistance or is seen due to reduced sensitivity of insulin in which pancreatic cell produces insulin in inadequate amount. This type of diabetes is mainly due to taking proper diet. Due to this, due to exercising, making changes in life style and increasing physical activity, this diabetes can be prevented. This type of diabetes is mainly seen after the age of 30 years. Hence it is also called adult onset diabetes mellitus. If diabetes is not treated in this way, oral hypoglycemic agents are also taken.
Type: 3 Diabetes Mellitus Associated Other Disease Conditions.
In this, diabetes is also seen due to any other disease in the body.
type:4 GDM Gestational Diabetes Mellitus
This type of diabetes is mainly seen in women and even in women diabetes mellitus is seen during pregnancy due to glucose intolerance.
Etiology of Diabetes Mellitus:
Type: 1 (IDDM) Insulin Dependent Diabetes Mellitus:
inherited,
Environmental Factors
Due to some virus
type: 2 ( NIDDM )Non Insulin Dependent Diabetes Mellitus.
genetic factor,
Environmental Factors,
obesity,
Type: 3 Diabetes Mellitus Associated Other Disease Conditions.
Due to hormonal imbalance during pregnancy. Due to insulin deficiency.
Due to cell resistance to insulin despite insulin.
Due to too much sugar intake.
Due to sedentary life style.
Due to excess cholesterol in the body.
Symptoms and signs:
P: Polyuria (Frequent urination : passing urine frequently),
P: Polydipsia (increased thirst),
P: Polyphagia (increased hunger: feeling very hungry).
feeling tired
Weakness.
Difficulty seeing.
Tingling and numbness in hands and feet
Dry skin.
Soar is a slow hill
Frequent infections.
Nozia.
Vomiting.
Decreases wound healing
Weight loss.
Abdominal pain.
Diagnostic Evaluation:
History Collection,
Physical Examination,
1) Fasting blood sugar (FBS) This test is done without eating or drinking anything for at least eight hours. Its normal value should be less than 110 mg/dl mg/dl. And if the fasting blood glucose level is more than 125 mg/dl mg/dl then it is diagnosed as diabetes.
2)Random blood sugar (RBS) In this the sample is taken anytime there is no need to do any preparation. If the random blood glucose is more than 200mg/dl mg per desiclator then it is indicated as diabetes.
3) PP2bs (post prandial blood sugar) This test is done after 2 hours after taking a full meal. Normally the blood glucose level comes down to the fasting glucose level two hours after a meal, but if someone has smoked or drank caffeine, it is altered.
3) Glycosylated HB.
This test is done to assess how much glucose is attached to the blood molecule.
4) Glycocylated Albumin: Usually glucose is attached to albumin so glycosylated albumin is used to assay average glucose level.
5) Oral glucose tolerance test. In this, 150 mg of carbohydrate is provided to the patient for three days. After that, the fasting blood glucose level of the patient is checked. After that, the client is given 75 grams of glucose to drink, after which the glucose tolerance level of the patient is checked.
7) Ketonuria If there are ketones in the urine, it indicates that the body uses fat as a source of energy.
8) Proteinuria: If protein is present in the urine, it indicates that protein is used as a major source of energy.
9) Serum lipid profile
10)Serum BUN.
11) Serum creatinine.
Management of Diabetes Mellitus:
Principal of Management
To eliminate the symptoms of hyperglycemia.
To reduce microvascular and macrovascular complications of diabetes mellitus.
Reducing blood glucose levels.
The patient can achieve a normal life style as far as possible.
Blood glucose levels can be reduced using patient education, dietary management, exercise and pharmacological therapy.
Patient Education:
To provide proper health education to the patient and his family members.
In which to teach how to do self-monitoring of glucose.
Teach monitoring of urine ketones if type 1 diabetes mellitus.
Teach the patient how to administer insulin.
Teaching the management of hypoglycemia.
Providing education to patients about foot and skin care.
Teach management of diabetes before, during, and after exercise.
Providing education about patient’s life style modification.
Dietary Management:
Aim of Dietary Management:
To reduce the symptoms of hyperglycemia.
If treating hyperglycemia to reduce symptoms of hypoglycemia.
Lowering the overall blood glucose level of the body.
Avoiding diets that increase blood glucose levels.
Ask the patient to lose weight if he is obese.
Make the patient have regular food intake.
Ask the patient not to take sugar.
Ask to eat a diet that contains adequate amounts of protein, carbohydrates and fat.
Dietary Management:
The main goal of dietary management is to improve metabolic control in the diabetic client.
Improving the patient’s blood glucose level and lipid level.
Making a daily food intake plan of the patient.
Making a plan for weight management of the patient.
Provide adequate nutrition to the patient.
A person’s lifestyle and habits play an important role in controlling and managing the disease.
A balanced nutritional diet is very important in the patient.
Ask the patient to increase the protein intake in his diet. Excessive protein intake increases renal function. and glomerular filtration rate increases.
Maintaining the level of fat in the patient’s diet Maintain the daily cholesterol level in the diet and limit saturated fat and cholesterol.
Provide carbohydrates as per the patient’s body requirement.
Asking the patient to consume carbohydrates in an adequate amount to maintain the body’s energy requirements.
for type :1 diabetes special diet management includes In it breakfast should be taken after 1 hour after taking dose of morning insulin.
Then after three hours a small amount of carbohydrate should be taken.
Lunch should be taken four to five hours after taking the morning insulin.
Sugar content should not be taken in Ood.
Foods that are sweet and contain sugar should not be taken, such as cakes, ice creams, jams, etc.
Checking the patient’s blood glucose level regularly.
Carbohydrate should be taken in small amount before exercise.
The patient should be asked to check the amount of glucose, ketones and albumin in the urine and all these substances are observed during fasting.
Caloric restriction for obese clients.
Exercise:
Advise the patient to do regular exercise to prevent exacerbation of his disease condition.
Ask for regular walking.
Ask the patient to ride a regular bicycle.
Ask for adequate amounts of carbohydrates before and after exercise.
Pharmacological Management:
Pharmacological management is responsible for maintaining blood glucose levels.
If insulin is given above the abdomen, its absorption is fast. Absorption slows when given on arm and leg.
Time, Course:
1) Rapid Acting Insulin:
Ex:=Humalog.
Its onset is within 10 to 15 minutes.
2) Short Acting Insulin:
It is called regular insulin or R insulin (R insulin) or zink crystalline zinc insulin (czi). Its onset is 30 minutes.
3) Intermediate acting insulin:
It is also called regular R insulin and its onset period is after three to four hours and the patient is required to take food during this period.
Long Acting Insulin:
Ultra lente insulin or Peakless insulin.
Its onset of action is 6-8 hours and its action lasts 20 to 30 hours.
Insulin Dosage:
The starting dose of insulin is 0.5 unit /kg/day.
Insulin A 2/3 Rd dose in the morning
and 1/3rd in the evening. This dose may increase or decrease depending on food intake, exercise, and illness.
Insulin pump:
A small portable pump is used to administer insulin and its needle has to be changed daily.
Combine therapy:
The patient is provided with oral meditation insulin.
Oral Antidiabetic Agents:
1)sulfonyl urea,
2) meglitinides,
3) thiazolidinediones,
4)bigunides,
5) alpha glucoside inhibitor.
This therapy is primarily for patients with type 2 diabetes.
Nursing Management:
1) Impaired nutritional status more than body requirement related to intake excess of activity expenditure.
The primary goal of the diet plan is to control the glucose level, thereby assessing the patient’s glucose level, and assessing the patient’s lifestyle, cultural background, activity level, dietary habit and food preference.
Ask the patient to take food in adequate amount and also to take snacks in between.
Arrange for an extra mile before the patient engages in physical activity.
Administer insulin as per doctor’s order.
2) Imbalance fluid volume related to increased stress hormone as evidenced by polyuria.
To assess the patient’s intake output chart.
Ask the patient to take oral fluids.
Provide intravenous fluid to the patient.
Checking the patient’s serum electrolyte level.
To check patient’s vital sign.
3) Activity intolerance related to weakness as evidenced by limited activities.
Assess the patient’s activity level.
Activity planning of the patient.
Provide analgesic medication to the patient before resuming activity.
Ask the patient to rest between activities.
Providing patients and prescribed medicine.
4) Knowledge deficit related to cause and disease as evidence by asking questions.
Assessing the patient’s knowledge level.
Provide education to patients about diabetes diet.
Providing education to patients about foot and nail care.
Provide education to the patient or keep his feet covered with soft shoes.
5) Fear related to insulin injection.
Monitor the patient’s blood glucose level.
Provide education to patients about self-administration of insulin.
Provide patient education about complications of insulin therapy.
Provide education to patients about signs and symptoms of hyperglycemia and hypoglycemia.
- AIDS (Acquired Immunodeficiency Syndrome):
Acquired Immunodeficiency Syndrome (AIDS) is a fatal illness. It is mainly transmitted by human immunodeficiency virus (HIV). Once a person is infected with HIV, it remains for life. H. HIV weakens a person’s immune system, so any infection can easily occur in a person’s body. So AIDS is not a single symptom but a set of many symptoms hence called a syndrome. Its incubation period ranges from 2 months to 4 years.
Reason:
Human immunodeficiency virus,
Hiv 1,
Hiv 2,
A sex worker
health care worker,
Due to contact with blood semen, cerebrospinal fluid, teats, saliva, breast milk, cervical or vaginal secretions of any HIV infected person.
Due to sexual activity with an HIV infected partner.
Due to injecting infected needle and syringe.
Transmission can occur through an infected mother to her child.
Due to contact/exposure to contaminated blood.
Blood transfusion.
Organ Transfusion.
Due to coming into contact with a person who already has syphilis or any other sexually transmitted disease.
Symptoms and signs:
weight loss,
diarrhea,
arthralgia,
Continuous cough for a month,
fever,
pharyngitis,
lymph node swelling,
Muscular system weakness,
dyspnea,
one head,
Liver enlargement.
Headache.
Sore throat.
Enlargement of the spleen.
Mouth Sore.
Nausea and vomiting.
Skin lesions.
feeling tired
Oral ulcers.
Loss of appetite.
Weight loss.
Sweating at night.
Swelling of the lymph nodes.
Diarrhea
Soreness in the mouth, anus and genital area.
Rashes falling into the skin. Neurological symptoms are seen.
Mode of Transmission:
Spread:
1) Sexual Transmission: HIV and AIDS are transmitted through sexual contact.
2) Transmission through blood:
Transmission of AIDS also occurs through the transmission of infected blood or by coming in direct contact with any infected blood.
3) Perinatal transmission:
Can be transmitted from infected mother to child.
Diagnostic Evaluation:
History Collection,
Physical Examination.
Recombinant DNA
t technique
PCR (Polymerase Chain Reaction).
ELISA (Enzyme Linked Immunosorbent Assay).
Viral isolation in culture.
Lymph node biopsy.
Rapid Hiv Antibody Test.
Western blot antibody testing.
Hiv viral load test.
Complete blood count.
CD4CELL Count.
Medical management
1) Nucleoside reverse transcriptase inhibitor (NRTI).
EX:= LAMIVUDINE
ZIDOVUDINE.
2)Non Nucleoside Reverse Transcriptase Inhibitor (NNRTI):
EX:= EFAVIREN
(SUSTIVA).
ETRAVIRINE
(INTELLENCE).
3) Protase inhibitors:
Ex:= ataxanavir.
Duranavir.
4) Entry or fusion inhibitor
EX:=enfuvirtide
(fuzeon),
Maraviroc
(selzentry).
5) Integrase inhibitors:
EX:=raltegravir
( isentress).
Nursing Management:
Provide proper position to the patient.
Advise the patient for deep breathing exercises.
Providing proper oxygen to the patient.
Maintain the patient’s hydration status.
Assessing the patient’s nutritional status.
Provide the patient with a diet that is high in protein and high in calories.
Providing fresh fruits, vegetables, whole gain and protein to the patient.
Provide easily digestible food to the patient.
Daily mouth care to the patient.
Providing food that the patient likes.
Maintaining social support of the patient.
Spend time with the patient.
Interacting properly with the patient and his family members.
Assessing the patient’s skin integrity.
Providing back care to patients.
Tell the patient about the importance of personal hygiene.
Keeping the patient away from the person who has the infection.
Patients using a barrier method as contraceptives.
If the patient is a smoker, give advice to avoid smoking.
Ask health care workers to maintain strict aseptic technique.
Prevention
Provide patient education to avoid unprotected sexual contact and use barrier method A contraceptive.
Avoiding pregnancy to a mother who has any sexually transmitted disease. Because that infection can also be transmitted to her child.
To provide advertisement in mass media and television to bring awareness about Sexual Health.
Any kind of blood or organ donation should not be done to a person who is infected with HIV.
Conduct proper test before blood transfusion.
Use of streak sterilization practices in hospitals and clinics.
Do not use used needles and syringes.
Blood and body fluids of an infected person should not come in contact.
Provide proper education about AIDS to patients.
Provide antiviral treatment to the patient.
Providing psychological support to the patient.
HIV is a sexually transmitted disease.
Do not use used razors.
Do not use a used toothbrush.
Do not use used needle and thread.
Use disposable needles and syringes.
If the needle and series are to be reused, they should be used only after proper autoclaving.
Pregnancy should be avoided if a woman has AIDS or infection because there are chances of AIDS and HIV being transmitted to the newborn baby.
To provide education in human being about what steps can be taken for prevention of Aids and Hiv.
Using all types of mass media and technology to create awareness among individuals about the measures that can be taken for the prevention of HIV and AIDS.
Advise to avoid donation of blood and other body organs to persons who are at high risk of HIV and AIDS.
Screening for HIV and AIDS when blood is to be transfused or drawn.
Using sterilization techniques in hospitals and clinics.
Use disposable needles and syringes whenever possible.
If not possible, use sterilized needles and syringes.
Using zidovudine tablets as curative measures.
Avoid contact with infected blood and body fluids.
Medical personnel should observe universal precautions and use personal protective equipment (PPE) kits when blood and body fluids come into contact.
Take extreme precautions when doing injections and skin piercings.
Effective use of sterilization and disinfectants.
Provide education about AIDS to the person.
A=Avoidable,
I=Incurable,
D=Disease,
S=Syndrome. Providing health education about
To properly explain the AIDS disease to the student.
Also educating people that AIDS is not spread by any kind of fly or mosquito but through unprotected sexual contact.
Educating people that AIDS is not spread through clothes but through blood and body fluids.
Proper precautions should be taken by the staff members working in the hospital who do not have HIV and AIDS.
Giving antiretroviral therapy to a person who has HIV and AIDS.
(STD)Sexually Transmitted Diseases:
- Syphilis:

Syphilis is a sexually transmitted disease.
The causative organism of syphilis is the spirochete Treponoma palladium. This disease usually starts with syphilitic lesions in the genital tract and occurs mainly in the genitals, rectum and mouth. The disease is caused by direct contact with other persons who have primary or secondary syphilitic lesions. Its incubation period is 9-90 days. These symptoms are mainly seen in nine days and last up to three months.
Reasons:
The spirochete Treponema pallidum,
Due to coming in contact with any infected person,
Unprotected sexual activity,
Due to contact with infected blood or bloody fluid.
Due to engaging in sexual activity with multiple partners.
Due to coming in contact with an infected partner.
Symptoms and signs:
The symptoms depend on the stage of syphilis. such as,
1) Primary stage
2) Secondary stage
3) Latent stage
4) Late stage
1) Primary Syphilis:
Primary syphilis occurs two to eight weeks after exposure to the bacteria. It starts with a small round sore called a chancry which is painless but highly infectious.
Small papule and lesions
A sore can be single or multiple.
Sore is also present on lips, tongue, hands, rectum and nipple.
Painless ulcers without any surrounding inflammatory reaction,
Inguinal gland enlargement.
2) Secondary Stage:
The secondary stage starts two to four weeks after the appearance of the sore and lasts for two to four years.
low grade fever,
headache,
loss of appetite,
weight loss,
anemia,
sore throat,
horseness,
Jaundice with or without hepatitis,
Pain in joints, muscles, long bones,
Cores, flat top, moist and necrotic lesions.
3) Latent Stage:
This is the third stage of syphilis. This stage lasts mainly for five to 20 years. It is mainly asymptomatic but can affect multiple organs.
Tumors occur in the skin, bones, and liver.
4) Late Stage:
This is the last stage of syphilis and about 15 to 30 percent of people who do not receive syphilis treatment enter this stage and the duration is very long and this last stage is a life threatening condition.
A tumor-like mass is created in this.
Damages the heart valves and blood vessels.
Meningitis (infection and inflammation of the meninges layer of the brain,
Paralysis.
There is no coordination.
Sleep is reduced.
Confusion.
Impaired judgment.
Slurred speech.
Difficulty seeing.
Deafness occurs.
Mental Illness.
Memory decreases.
Diagnostic Evaluation:
History Collection,
Physical Examination
Blood test:
A blood test is done to see if any syphilis antibodies are present in the body.
Cerebrospinal fluid analysis.
vdrl test.
fta-abs (Fluorescent Treponomal Antibody Absorption) test is specific for treponoma palladium test.
Medical management
Treatment of syphilitic lesions is divided into three stages:
1.Early Syphilis: (Primary, Secondary and Early Latent Syphilis)
a Benzathine Penicillin G 2.4 Mega Unit I/ M Single Dose Itch Batak Ma. Half dose.
b. Procaine Penicillin G 600,000 units I/M daily for 10-14 days.
c. In penicillin hypersensitive cases, tetracycline or erthyromycin 500 mg orally 4 times a day for 14 days
- Late Syphilis: Benzathine Penicillin G 2.4 mega units I/ M weekly given for 3 wks.
3) Follow-up:
Serological tests are done 1, 3, 6 and 12 months after treatment of early syphilis.
In late symptomatic cases, for lifelong surveillance, serological tests are performed annually.
Nursing Management:
Treatment should be started as soon as the disease is detected.
The patient should be examined at 3rd, 6th, and 12 months to control the disease.
Avoid coming in contact with a person who has syphilis infection.
A detailed examination of the person who is suspected should be done.
Provide education to the patient on barrier method contraceptive use.
Treat the patient symptomatically.
Educating the patient to take proper treatment.
Continuous abstinence until recovery from syphilis or any sexually transmitted disease.
Provide patient education on using the barrier method as a contraceptive.
To maintain patient privacy and confidentiality.
Ask the patient to take regular follow-up.
Providing education to patients about sexual hygiene.
- Gonorrhea:
Gonorrhea is a common sexually transmitted venereal disease. The causative organism of gonorrhea is Neisseria gonorrhoeae.
(neisseria gonorrhoea)
is This infection is primarily transmitted in the genitourinary system involving the genital organ, the rectum. If this disease is not treated, fever and arthritic conditions can occur. If the hand is contaminated by this organism, there are chances of the infection spreading to the eye as well. Gonorrhea infection is mainly seen in the age group of 15 to 24 years. Gonorrhea is also known as “the clap” or “the drip”. Its incubation period is 3-7 days.
Causes of Gonorrhea:
Neisseria gonorrhoeae bacteria,
It is transmitted through vaginal, oral and anal sexual contact
If there is any prior history of gonorrhea.
Any other sexually transmitted infection.
If the hygienic condition of the genital area is not maintained properly.
If previously diagnosed with gonorrhea.
Sexual activity started early.
Have multiple sex partners.
If a pregnant mother has gonorrhea, she can transmit the infection to her baby.
State the symptoms and signs:
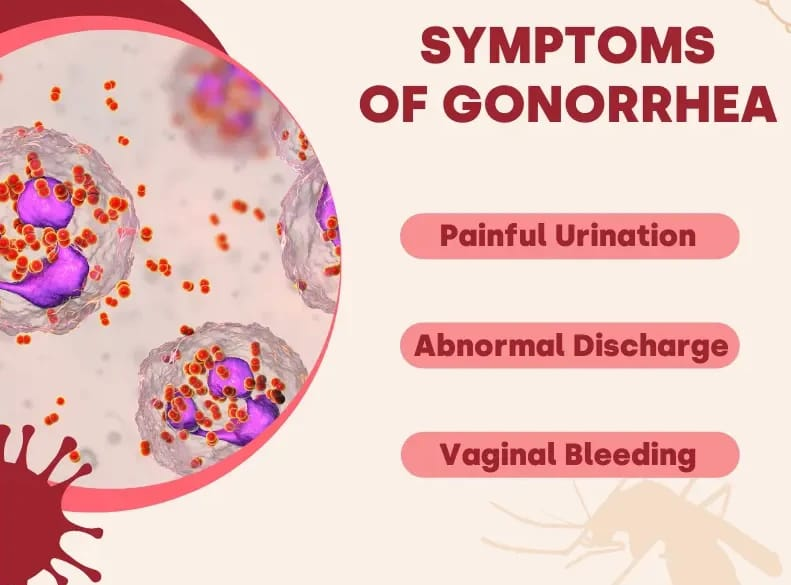
Man:
Burning sensation occurs during urination.
Purulent discharge from the penis.
Frequency of urination increases.
Pain, redness and soreness occur.
Urethral scarring.
Enlarge scrotum.
Pain and itching sensation during urination.
Inflammation of the prostate gland and testicles.
A yellow and green thick discharge comes out from the tip of the penis.
Female:
Purulent discharge.
Discomfort and aching pain over the abdomen.
Burning sensation.
There is urgency and frequency in urination.
Difficulty in walking.
(Salpingitis: Infection and inflammation of the fallopian tubes).
fever,
vomiting,
low back pain,
Pain during intercourse,
Discharge from the vaginal area that is thin or thick yellow and green.
There is discharge and irritation from the anal area. Bleeding occurs.
Tenderness is felt in the abdomen and pelvic area.
Diagnostic Evaluation:
historytaking,
Physical Examination,
swab test,
Culture from cervix, urethra, rectum or throat.
Urine Examination.
Nucleic acid test.
Gram staining.
Medical management
Specific treatment for gonorrhea is a single dose of any of the following medicines:
Ceftriaxone: 125 mg I/M
Ciprofloxacin: 500 mg orally.
Ofloxacin: 400 mg orally.
Cefixime: 400 mg orally.
Levofloxacin: 250 mg orally.
Conjunctivitis of the newborn is treated with a single dose of ceftriaxone (20-30 mg/kg) IM and gentamicin eye ointment (1%).
Follow-up: Culture should be done after 7 days of therapy. Repeat culture is done after 3 months at monthly intervals.
Nursing Management:
Taking a proper history of the patient.
Providing proper antibiotic medicine to the patient.
Perform serum examination for syphilis.
Provide proper education to the patient about personal hygiene.
Providing proper education to the patient about the disease condition.
Advise the patient to avoid multiple sex partners.
Educating the patient to use the barrier method of contraception.
Provide proper psychological support to the patient.
Providing antibiotic medicine to prevent infection.
Ask the patient to maintain personal hygiene.
Complications:
Pelvic Inflammatory Disease (PID),
infertility,
ectopic pregnancy,
dyspareunia,
Chronic pelvic pain, tubo-ovarian mass,
Bartholin gland abscess.
- Tuberculosis During Pregnancy:
Tuberculosis is a serious infection caused by the bacterium Mycobacterium tuberculosis that mainly affects the lungs but can also spread to other areas of the body. Pulmonary tuberculosis is spread through air i.e. by coming into contact with the coughing or sneezing of an infected person.
Etiology of Tuberculosis:
Close contact with active tuberculosis patients
Weak immune system (HIV, organ transplantation, cancer, corticosteroid therapy)
Edge
Living in over crowded area
Malnutrition
Chronic health conditions
Symptoms and signs:
Persistent Cough (Cough present for more than three weeks)
blood in sputum,
chest pain,
fever,
feeling cold,
swollen gland,
fatigue,
night sweats,
loss of appetite,
weight loss,
Shortness of breath,
poor growth,
cuffing,
Diagnostic Evaluation:
History Collection
Physical Examination
Tuberculin skin test
x ray
Sputum test
Blood test
Management
Antibiotic therapy A combination of antibiotics is given as a treatment for tuberculosis. In which isoniazid, rifampin, ethambutol and pyrazinamide medications are given. A course of this medicine is done for six to nine months.
Directly Observed Treatment Short Courses (DOTs)
In DOTs therapy, the TB patient is supervised by a health care provider. The patient takes exactly the regular medicine and its effectiveness is observed. So it can be known whether the patient has completed the full course of treatment or not.
Isolation
TB positive patients are isolated. Because TB is a contagious disease and it is spread through air to each other. Hence the patient is isolated to prevent it from spreading.
Nutritional support
To provide adequate nutrition support to the patient with TB so that his immune system can be improved and weight gain can be achieved.
Education and counselling
Provide education and counseling to patients about tuberculosis. Explain infection control measures to the child and his family members.
Management:
To maintain the patient’s body temperature and provide proper antipyretic medication if the child has a fever condition.
Providing antibiotic drugs to treat bacterial infections.
Provide cough expectorant drug to expel cough.
Provide nasal decongestants to relieve congestion.
Adequate rest and plenty of fluid intake.
Avoid contact with irritants.
Properly and completely assess the patient.
Properly assess the patient’s respiratory status.
To assess patient’s vital signs completely.
Properly assess the patient’s oxygen saturation.
Continuous monitoring of the patient’s respiratory status and oxygen saturation to properly assess the patient’s condition.
Continuously monitoring the patient’s body temperature.
Advise the patient for continuous fluid intake to maintain the patient’s hydration status and keep the mucus thin.
Provide a properly comfortable position to the patient.
Provide adequate oxygen to the patient to maintain oxygen saturation of the patient’s body and provide respiratory support.
Provide properly prescribed medication to the patient.
To provide complete education to the patient and his family members about the child’s condition, its causes, its symptoms and signs and its treatment.
To provide proper working and comfortable environment to the patient.
A patient with tuberculosis does not require pregnancy termination.
Proper care should be provided to the antenatal mother during the antenatal period itself due to which the condition of maternal anemia and preeclampsia can be properly treated.
If the patient prefers hospital delivery, he should be admitted to the hospital two weeks before the properly expected date of delivery.
Advise the patient to take proper bed rest.
Maintain the patient’s nutritional and hydration status properties.
Advise the patient to perform proper breathing exercises.
Advise the patient to avoid fatty and spicy food.
Advise the patient to take high protein.
Advise to keep the patient properly separated from her child after delivery and breastfeeding is contraindicated.
If the mother is recovering from an active disease, prophylactically provide the baby with T. Isoniazid 10-20mg/kg/day for 3 months.
As soon as possible the child should be given isoniazid Resist B.C.G. should be given
Proper feeding should be provided to the baby. Baby’s temperature should be maintained regularly.
The baby should be prevented from getting infected.
Patient should avoid pregnancy for 2 years.
Advise patient to avoid oral contraceptive medication while taking Rifampicin medicine.
If the patient’s family is complete, advise them for permanent sterilization method.
Multipara:
Definition:
Which is more than one of women
When Fitus has reached the stage of viability, the woman is called multipara.
Complications:
During pregnancy:
abortion,
Obstetrical hazards such as malpresentation,
multiple pregnancy,
Placenta privya.
Medical Disorders:
anemia,
hypertension,
Cardiovascular complications.
pre maturity,
During Labour:
cord prolapse,
Cephalopelvic Disorder (CPD),
obstructed labour,
ruptured uterus,
Post partum haemorrhage,
grief,
Precipitate Labour,
Prolabs umbilical cord.
During Purperium:
Increased morbidity rate due to intra natal hazard.
Subinvolution.
Falling lactation.
Management:
Multipara is considered in the highest category so the mother should be hospitalized immediately.
Proper antenatal care should be provided to the mother.
Delivery of multiparous women should be done in a hospital with a well-hospitalized facility.
The presentation and position of the fetus should be properly checked at the time of delivery.
After delivery, the mother should be properly assessed for post partum haemorrhage (PPH) condition.
- Heart disease during pregnancy
Heart disease during pregnancy refers to any cardiovascular condition that affects the heart or blood vessels and occurs or worsens during pregnancy. It involves preexisting conditions, such as congenital heart disease or valvular heart disease, as well as conditions that develop during pregnancy, such as gestational hypertension or peripartum cardiomyopathy. This condition can affect both the mother’s health and the developing fetus. The incidence of cardiac lesions in hospital deliveries is less than 1%. In common cardiac lesions the mood is rheumatic.
Etiology:
Advancing Age,
cardiac arrhythmia,
Left ventricular hypertrophy,
Previcious heart failure,
Due to risk factor appearance like infection, anemia, pre-eclampsia, severe weight gain, multiple pregnancy, inadequate supervision.
Classification of Heart Diseases:
Grade 1: Physical activity does not cause symptoms and is an uncompromised state.
Grade 2: Slightly compromised with some limitation in physical activity. The patient feels full at rest but remains uncomfortable with normal physical activity.
Grade 3: Markedly compromised in which the patient is comfortable at rest, but uncomfortable with less than normal physical activity.
Grade 4: Severely compromised in which the patient feels uncomfortable even at rest.
Diagnostic evaluation:
History Collection,
Physical Examination,
Chest x-ray,
ECG,
echocardiography,
Cardiac MRI,
Doppler flow studies.
Symptoms and signs:
Symptoms:
breathlessness,
nocturnal cough,
syncope,
Chest pain.
Sign:
chest murmur,
cardiac enlargement,
arrhythmia,
Chest radiography,
cardiomegaly,
Pulmonary vascular markings are increased,
Enlargement of pulmonary vein,
Dyspnea on exertion,
edema,
heart murmur,
Palpitation,
Bounding and collapsing pulse,
chest pain,
peripheral edema,
distended jugular vein,
Limitation of physical activity.
Aim of Management:
The aim of management is to maintain and improve the physical and psychological well-being of mother and offspring.
Measures to prevent maternal complications.
To detect high risk factors and prevent cardiac failure.
Management:
It is important to provide proper hospital care to the patient who has the condition of heart disease.
Antenatal Care:
Supervising patients with heart disease in a tertiary care hospital. Initial assessment should be done by a cardiologist.
Penidure LA 12 (Benzathine Penicillin) injection into puberium at four wk intervals in pregnancy.
Detect each risk factor during antenatal visit and provide proper treatment.
Properly assess whether the patient has dyspnoea and cough.
Properly auscultate for crepitation.
Hospitalize the patient if the heart rate is greater than 100/min.
Assess for anemia, weight and blood pressure.
Reevaluate the patient’s condition.
Screening for congenital abnormalities by sonography.
Antenatal advice: Advise the patient to take adequate bed rest.
Avoid excess excitement and stain.
Avoiding high calorie and spicy diet.
Giving advice to avoid low salt diet intake in food.
Advise the patient to consume a low carbohydrate diet.
Antenatal advice: Advise to take adequate rest, Advise to avoid excess excitement and strain, Advise to avoid high calorie and spicy food. Low salt, low carbohydrate and fat but high protein intake in kherak, correct anemia to do Avoiding colds and infections and maintaining adequate dental care
Anticoagulant: Congenital heart disease, pulmonary hypertension, artificial valve replacement/atrial fibrillation, anticoagulants are given. Instructions to give injection heparin 5000 units twice daily subcutaneously S up to 12 weeks of pregnancy, followed by warfarin tablets 3mg daily at the same time for 36 weeks. Then starting warfarin tablets after giving injection heparin for 7 days postpartum.
Indications for surgery in pregnancy: Medical treatment fails, intolerance symptoms, cardiac failure.
Admission/Hospitalization:
Grade-1: Two weeks before the expected date of delivery.
Grade-2: During 28 weeks in unfavorable social environment.
Grade-3&4: When pregnancy is diagnosed, hospitalize the patient throughout the pregnancy.
Management of Cardiac Failure in Pregnancy Proper care.
Labor: Spontaneous labor and delivery are usually without complications, and some obstetric indications are for labor induction (vaginal PGE2).
First Tage:
Position : Provide lateral recumbent position.
Oxygen: 5-6 L/min.
Analgesia: Epidural.
Fluid: Provide not more than 75ml/hour.
Colorfully Watch: To properly assess the patient’s pulse and respiration rate. If the pulse rate rises above 110/min, give intravenous digoxin 0.5 mg. Properly monitoring vital signs through cardiac monitoring. Central venous pressure monitoring should be done if necessary.
prophylactically
Provide antibiotics.
Second stage: Advise to avoid maternal pushing and ventous delivery is preferred over forceps, and perform it without lithotomy position. Do not administer after intravenous ergometrine delivery.
A caesarean section is not required.
Third stage: Slightly blood loss is not bad, if excessive, give oxytocin by infusion and give frusemide along with it.
Purperium: Keep the patient under close observation in the first 24 hours, record oxygen, pulse, BP and respiration, give diuretic if needed. Unless the patient is in failure, breast feeding is not contraindicated.
Teenage Pregnancy:
Teenage pregnancy is pregnancy in women between the age of 13 to 19 years. It usually involves young women who are still in their adulthood and may face social, emotional and health challenges as a result. Teenage pregnancy can affect the educational, economic stability and health of the mother as well as the health and development of the child. The teenage mother is at risk of complications such as gestational hypertension, cephalopelvic disproportion anemia and nutritional deficiency. The incidence of sexually transmitted diseases is high in those people. Infants born to teenage mothers may have complications such as prematurity, birth asphyxia, and low birth weight.
Etiology:
Fear of reporting sexual activity to parents.
Limited use of contraceptives
Low education level.
Low knowledge of ability to conceive.
Due to early marriage.
Less use of contraceptives.
Because of being rapped.
Due to sexual abuse.
Diagnostic Evaluation:
Positive pregnancy test, ultrasonography.
Treatment:
Adequate caloric intake in the diet, so that the growing adolescent and his/her fitness gets adequate support.
Educate clients for proper prenatal care and to report potential problems to health care providers.
Drugs: If there is an STD then give antibiotics.
Nursing Diagnoses:
Deficient knowledge (maternal) about pregnancy and related responsibilities.
Nutrition less than body requirements.
Interrupted family processes.
Planning and Goals:
Knowledge about pregnancy and fix responsibilities in the patient is increased.
Advise the patient to take nutritional diet.
To provide proper support to the patient and his family members.
Implementation:
Monitoring nutritional deficiency and the amount of weight gain the patient has.
Blood pressure for gestational hypertension and for gestational diabetes
Monitoring glucose level properly.
Properly monitoring the patient’s fundal height.
Properly assessing the patient’s knowledge.
Regular antenatal checkup of the patient.
Providing proper education to the patient about options like pregnancy termination, continuation, etc.
Allowing the patient to explain his feelings and promoting his mental and emotional well-being.
Providing proper health education to patients.
- Osteomalacia:
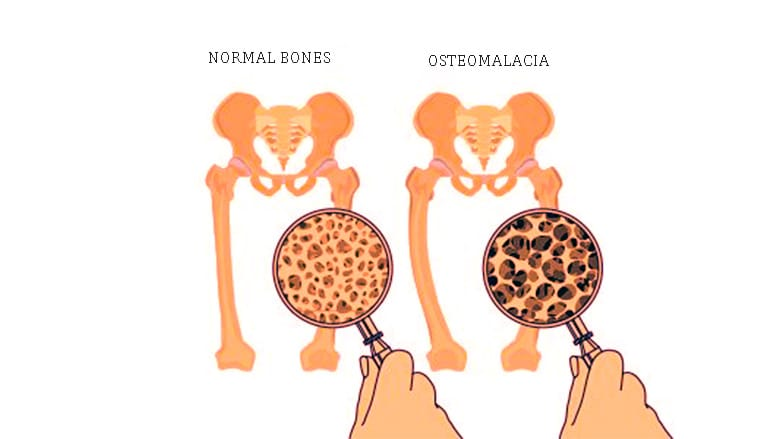
Bones need calcium and phosphorus to stay healthy and strong, but the body also needs vitamin D for absorption of the two minerals. Without this vitamin, bones can become soft and flexible. After the growth plate closes, this softening is called osteomalacia. Osteomalacia is usually a softening of the bone due to vitamin D deficiency. The affected bone is soft bone. Osteomalacia is caused by a deficiency of vitamin D in the body which can be caused by conditions that interfere with the absorption of vitamin D in the body, e.g. Intestinal disorders.
Etiology:
Due to vitamin D deficiency.
celiac disease,
kidney or liver disease,
Due to certain types of surgery,
Due to malnutrition during pregnancy,
Due to certain types of drugs.
Symptoms and signs:
Bone pain that spreads to the lower back, pelvis, hips and ribs.
Tenderness in arm, leg and spine.
Low calcium levels cause muscle spasms and cramps.
Low calcium in the body causes tingling and numbness sensation in the extremities or around the mouth.
Bone fractures can happen very easily.
Muscle weakness.
Diagnostic evaluation
History Collection,
Physical Examination,
Diagnosis of osteomalacia is done through a few blood investigations such as:
Vitamin D level: This is assessed in cases of osteomalacia.
Calcium level: This is assessed in cases of osteomalacia.
Phosphorus level: This is assessed in cases of osteomalacia.
Alkaline phosphatase isoenzyme level: Here the level is indicative of osteomalacia.
Parathyroid hormone level: An increased level means an adequate amount of vitamin D in the body.
X-rays and other imaging tests: These will show small cracks in the bone throughout the body (loose transformation zone).
Bone biopsy is rarely done.
treatment
In cases of osteomalacia, early oral supplementation of vitamin D, calcium and phosphorus is prescribed by the doctor.
Intravenous vitamin D is indicated in cases of absorption problems due to intestinal injury or surgery.
Staying in sun exposure is advised.
C comes in for antenatal checkup from time to time.
Advising the patient properly to deliver the patient in a well-equipped hospital.