ENGLISH NEW MIDWIFERY GNM TY UNIT 12 Obstetrics Operations
Unit: 12 Obstetrics Operations
Induction of Labour
- Induction of Labour:
Induction of labor i.e. artificial initiation of uterine contractions after the period of viability of fits and before the spontaneous labor process starts, usually by medical, surgical or a combination of both methods to induce uterine contractions for vaginal delivery. It is called induction of labor.
Purpose of Induction of Labour:
Induction is done when continuation of the pregnancy may pose a risk to the health of the mother or the fetus. So in cases of safety of both, induction is indicated.
Indications of Induction of Labour:
There is a need for induction of labor when there is any deviation in the normal physiological process of child birth.
Maternal Indication:
Prolonged pregnancy,
Pre-eclampsia and Eclampsia,
Maternal medical complications like diabetes mellitus, chronic renal failure, cardiac disease, hypertension, cholestasis, postmaturity, intrauterine death,
intrauterine growth retardation,
APH specifically abruptio placenta,
Polyhydroamnios associated with maternal distress,
Oligohydroamnios,
Having a prior history of intrauterine death,
Premature Rupture of Membrane,
Due to congenital malformations in fitus.
Fital indication:
Intrauterine growth retardation (IUGR) due to chronic placental insufficiency,
Intrauterine fetal death,
Rh-isoimmunization,
unstable lie,
Due to congenital malformation of the fetus.
Contraindications:
contracted pelvis,
Cephalopelvic Disproportion (CPD),
malpresentation,
Prior classical caesarean section or hysterotomy,
vaginal bleeding,
Waza Privya,
placenta previa,
Active genital herpes infection,
High risk pregnancy, heart disease, pelvic tumor,
Obstetrics and medical complications with elderly primigravida,
Umbilical cord prolapse,
or cord presentation,
In cervical carcinoma,
HIV-positive women not receiving highly active antiretroviral therapy
In cervical carcinomas.
Risks due to Induction of Labour:
Mother:
psychological upset,
Tendency of prolonged labour,
The need for analgesics increases,
operative interference,
Morbidity.
Fits:
Iatrogenic prematurity,
hypoxia,
uterine dysfunction,
Protong Labor,
Operative delivery.
Method of Induction of Labour:
- Medical,
2.Surgical, - Combined.
Medical:
Prostaglandins PGE2 (prostaglandin), PGE1 (mizostol), oxytocin or mifepristone are used for medical induction.
Prostaglandins for medical induction (PGE2): Act locally on contiguous cells, thereby causing biomaterial contraction. But (PGE2) survival ripening while PGF2 is responsible for myometrial contractions. PGE2 dinoprostone intracervical application is used for cervical ripening. It is repeated after 6 hours, 3 to 4 doses can be given if needed. After the application, the patient should stay in bed for 30 minutes and monitor her uterine activity and fetal heart rate.
Misoprostol (PGE1): Currently used transvaginally or orally. 25 mg vaginally every four hours is used for cervical ripening and labor induction. A total of 6-8 doses can be given.
Oxytocin: Endogenous is uterotonic. It stimulates uterine contractions. It is given as an intravenous infusion when the cervix is ripe.
Mifepristone: It is a progesterone receptor antagonist and blocks progesterone and glucocorticoid receptors. Used vaginally for cervical ripening and labor induction.
Surgical induction:
1) Artificial Rupture of Membrane (ARM),
2) Stripping the membrane
Low Rupture of Membrane (LRM):
Procedure: A small amount of amniotic fluid is drained by rupturing the membrane below the presenting part and above the internal os. It is performed in the labor room or operation theater with full aseptic precautions followed by emptying of the bladder and lithotomy position with long couture forceps or amnion hook followed by placement of a sterile vulval pad and administration of antibiotics. After membrane rupture, amniotic fluid should be assessed for color, station of cervix, cord prolapse and fetal heart rate.
Indications: Anti-partum haemorrhage (APH),
Hydroamnios, severe preeclampsia, eclampsia.
Contraindications: Intra-uterine fetal death, maternal AIDS, genital active herpes infection.
Advantages:
Low blood pressure in pre-eclampsia and eclampsia,
Maternal distress is reduced in hydroamnios,
Leaker Omni can be assessed,
Internal fetal monitoring can be done,
Uterine CVD is assessed,
Blood sample taken from fetal scalp,
Catheter placement to measure intra-uterine pressure,
Bleeding is controlled in ante partum haemorrhage (APH) and
Abruption of the placenta and initiation of labor reduces tension.
Risk: Cord prolapse, excessive amniotic fluid escape, placental abruption, injury amnionitis etc.
Stripping the Membranes: This procedure is useful for cervical re-opening, before ARM and for induction of labour. Digital separation of the chorioamniotic membrane from the wall of the cervix and lower uterine segment is called stripping of the membrane. It causes the release of endogenous prostaglandin A from the membrane and decidua. This method is simple, safe and beneficial, its criteria being that the fetal head is applied to the cervix and the cervix should be dilated as far as the examiner’s finger can go.
Mechanical: Dilator
The membrane releases prostaglandins from the decidua for labor induction and survival ripening.
Transcervical balloon catheter (Follis catheter): Extra amniotic saline infusion is performed for cervical repair.
Combined Method: In this method both medical and surgical methods are used. Its advantages include being more effective than a single procedure, shortening the induction-delivery interval, thereby reducing infection, and shortening the observation period.
- Manual Removal of Placenta:
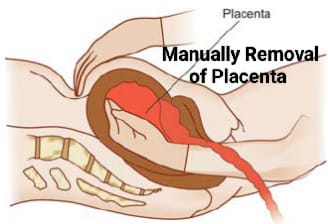

When the placenta is not delivered for 30 minutes after the birth of the baby and the placenta remains in the uterine cavity, in this condition there is a need to remove the placenta manually.
This procedure is done under general anesthesia and in emergency if there is no anesthetist, deep sedation is given.
It first involves providing the patient with lithotomy position, painting the operated area and covering the operated area with sterile linen.
Aseptic measures to catheterize the bladder.
Then hold the umbedical cord tightly with the left hand and make a cone shape of the right hand, dip it in antiseptic solution and introduce it in the direction of the cord in the instrument. Release when the placenta is located so that the fundus can be supported above the abdomen with the left hand.
Apply fundus steady pressure with abdominal hand, guiding finger movements until the placenta is completely separated from the uterine cavity.
After reaching the margin of the placenta separate the entire placenta with a slicing movement of the fingers between the placenta and the uterine wall.
When the placenta is completely separated, pull out the cord with the left hand and introduce the right hand to properly check for any retained bits of placenta.
Then give intravenous methargin 0.2 mg and continue massaging the uterus with the left hand and pull out the uterus with the right hand. Inspection for cervical-vaginal canal injury.
Then check the completeness of the placenta and membranes and whether the uterus is hard and contracted.
- version
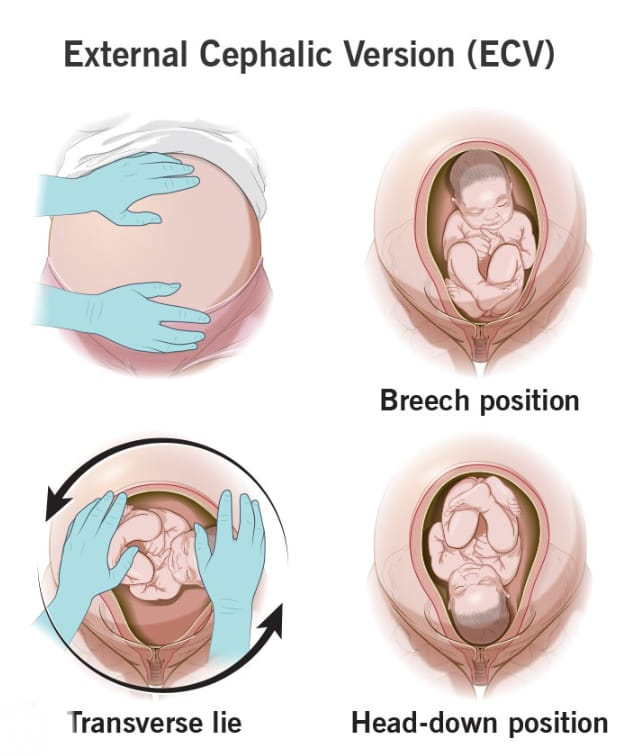
Definition:
The manipulative procedure of changing the lie of the fitus or bringing the favorable pole of the fitus to the lower pole of the uterus is called version. When the cephalic pole is brought to the lower pole of the uterus, it is called the cephalic version and when the podelic pole is brought to the lower pole of the uterus, it is called the podelic version.
Type:
1) Spontaneous,
2) External,
3) Internal,
4) Bipolar
1) Spontaneous version: This type of spontaneous version is more common in multipara, about 55% after 32 wks of breech presentation and about 25% after 36 wks.
2)External Version: In this type of version only the favorable cephalic or podalic pole is brought into the lower pole of the uterus by external manipulation (abdominal).
ECV (External Safelike Version):
In the external cephalic version, the cephalic pole of the fitus is brought into the lower pole of the uterus.
Advantages:
Incidence of breech presentation and breech delivery at term can be reduced.
Cesarean delivery can be reduced.
Maternal morbidity rates can be reduced by cesarean or vaginal breech delivery.
Vaginal breech delivery can reduce the risk of fits.
Contraindication:
Antepartum Haemorrhage (APH), Hyperextension of head, Large Fits, Major Congenital Anomalies, Dead Fits, Intra Uterine Growth Retardation (IUGR).
Multiple pregnancy, ruptured membrane, congenital malformation in uterus, contracted pelvis, prior cesarean section, obstructed complications, Rhesus isoimmunization.
Procedure:
External cephalic version (ECV) should be performed after 36 wks, as early reversion increases the chances. Tocolytic drugs are given to relax the uterus during external cephalic version.
Before the procedure real time USG is done to confirm the diagnosis and volume of amniotic fluid and non stress test is observed for well being assessment of fitus.
First empty the bladder. Then provide comfortable supine position to the patient. Then keep shoulders a little higher and do Thai flex. Then the back position, presentation, limbs, FHS etc. of the fetus are checked.
Then hold the podelic pole with the right hand and the cephalic pole with the left hand. Now version is done in opposite direction of head and breech till lie transverse, again fetal heart sound (FHS) is checked.
After bringing the fitus into a transverse lie, the arms are alternately crossed, and intermittent pressure is given until the head reaches the lower pole of the uterus.
Observe the mother for 30 minutes after the procedure and check vital signs. Checking Fetal Heart Sound (FHS) and Non Stress Test (NST) of Fits Checking the mother for vaginal bleeding and membrane rupture.
Anti-D gammaglobulin 100 micrograms should be given to Rh negative women.
External version is easy in transverse lie. Its contracture is similar to placenta previa and congenital.
External podalic version: External podalic version is performed when external cephalic version fails in transverse lie and the second baby is a twin.
Complications of external version
Premature rupture of membranes, premature labor, abruptio placenta, bleeding, true knots in the cord, or cord wrapping around the fetal part, amniotic fluid embolism and increased phyto-maternal bleeding.
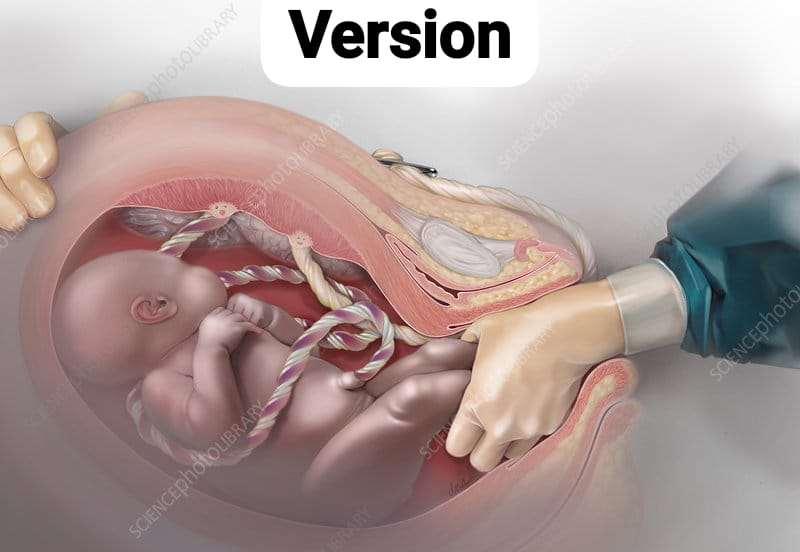
3) Internal version: In this type, version is performed by introducing one hand into the uterus and keeping the other hand on the abdominal. Internal version is always a podalic version and is completed with extraction of the fitus.
Conditions for internal version: Full dilatation of cervix, adequate liker amni and live fits.
Indications: Internal version is rarely indicated in singleton pregnancy and is only performed in twins when the second baby’s lie is transverse. However, in some cases such as caesarean section where there is no facility and transverse lie or cord prolapse with full dilatation of cervix, head high up and baby is alive, internal version is also performed in single pregnancy.
Contraindication:
Neglected Obstructed Labor.
Procedure:
First assessment of fitus ni lie, presentation and heart rate is done by an experienced obstetrician through abdominal palpation, vaginal examination and trans abdominal ultrasound examination. Internal versions are performed under general or epidural anesthesia such as,
First the patient is placed in dorsal lithotomy position, painting with antiseptic followed by draping and catheterization. If there is podelic pole of fitus in the left side of the mother then introduce the right hand and similarly if there is podelic pole of fitus in the right side then introduce the left hand making a cone shape of the hand so that its back side comes against the uterine wall approach to Podelic Pole.
Take the hind to the breech and Thai to catch the foot.
Now give steady traction to the leg, bring it down and push the cephalic pole upwards from outside with the other hand.
After bringing one leg down, there is no difficulty in delivering the other leg and delivery is completed by extraction of the breech during uterine contractions.
Check for utero vaginal canal injury or rupture of uterus after delivery.
Complications:
Maternal: Placental abruption, rupture of uterus, and increased morbidity rates.
Fetal risk: asphyxia, cord prolapse, intracranial haemorrhage, high perinatal mortality.
4) Bipolar version: In this version one or two fingers are introduced into the uterus and the other hand is placed on the abdomen. Its indications include low degree of placenta previa involving dead, deformed or viable fits, in which the cervix should be dilated to the extent of a list of two fingers and one leg should be brought downwards by pushing the hand towards one iliac fossa.
- Sterilization:
Permanent surgical contraception also called voluntary sterilization is a surgical method in which the reproductive function of an individual male or female is purposefully and permanently destroyed.
such as,
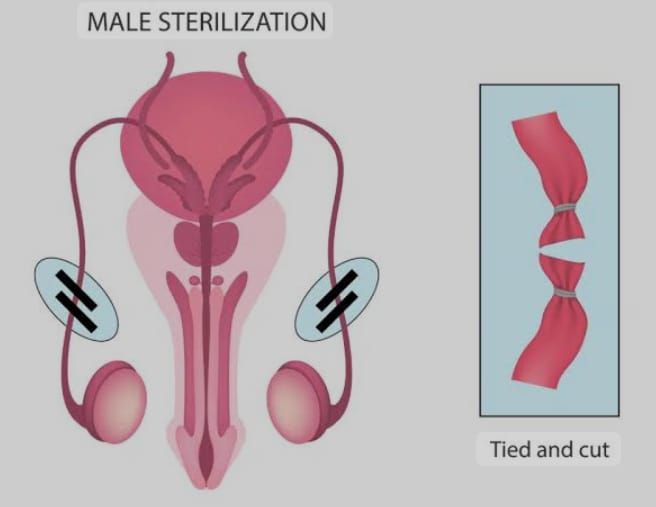
1)Male Sterilization: Vasectomy,
2) Female Sterilization: Tubectomy
1)Male Sterilization: Vasectomy: This is a permanent stylization operation performed in the male in which both sides of the vas deferens are resected and its ends are cut and ligated.
Advantages:
It has a simple operation technique and few complications.
The operation can also be done in camps and villages as an outdoor procedure.
Failure rate is 0.15% and success chance of reversal anastomosis operation is 50%.
Equipment, hospital stay, doctor training all costs are minimal.
Disadvantages:
Additional contraception is required for 2-3 months after the operation until the semen is sperm free.
Frigidity or impotence occurs which is mostly psychological.
Non Scalpel Vasectomy (NSV): This operation is provided under local anesthesia in which the vas is caught with specially designed forceps, then the stretched skin over the vas is punctured with the sharp point of the forceps without using a scalpel and then the vas is dissected, there is no need for sutures and the time is also less, there is a fast recovery, but the skill of the surgeon is much more required.
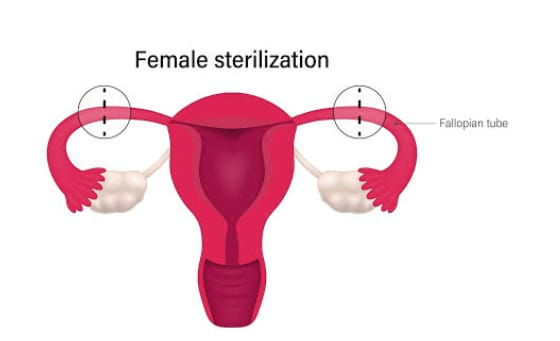
Female Sterilization/ Tubectomy:
Tubectomy is a method of permanent sterilization performed in females. It involves cutting the fallopian tubes and then ligation to block the passage of the ovum.
Time of Operation:
Postpartum Sterilization: Tubectomy can be done 24-48 months after delivery if the patient is healthy.
Internal Sterilization: When the operation is performed at any time other than child birth and abortion, it is called internal sterilization.
Traditional tubectomy: This method is also known as abdominal tubectomy. This method is usually performed under general anesthesia or spinal anesthesia in which an incision is made in the lower abdominal area and then the fallopian tubes are cut and tied or clamped. The abdominal lining is then closed. This usually works as a permanent contraceptive that blocks the passage of the ovum, which usually requires five to six days of hospitalization and sutures on the 5th day after the operation. Then it can be removed.
Post operative advice:
Heavy weight should not be lifted for 6 weeks.
Avoid heavy work for three months.
Sexual activity can be resumed 4 weeks after the operation.
Minilap operation: This is a minor form of abdominal tubectomy usually performed under local anesthesia in which a 2.5 to 3 cm incision is made in the lower abdominal area and then parts of the fallopian tubes are cut and clamped and The abdominal layer is then sutured again.This method is a very safe and effective method.This procedure can generally be performed at the primary health center (PHC) level and also in the campaign.This procedure acts as a good technique for postpartum sterilization. .
Advantage:
This technique is generally suitable for post partum sterilization.
This procedure is usually less traumatic than an abdominal tubectomy.
It usually has fewer complications.
Laparoscopic Sterilization: This laparoscopic sterilization technique is a very popular procedure of female sterilization in which the fallopian tubes are blocked or a rubber ring is placed in the fallopian tubes so that the ovum cannot reach the uterus before inserting a laparoscope into it. The abdomen is expanded with carbon dioxide, nitrous oxide, or air, then the laparoscope is inserted through the abdomen and the tube is visualized. After the tube is visualized, the fallopian tube is placed or a clip is applied to the fallopian tube. Due to which the tube is blocked then the laparoscope is removed and the lining of the abdomen is sutured and closed.
Advantage:
The incision is very small and the scar is also small.
It requires less time for operation.
This is a less expensive procedure.
Complications are minimal.
Hospital stay is short usually up to 48 hours.
Disadvantage:
It is not usually performed in the postpartum patient.
It is not suitable for patients who have medical disc order like heart disease, respiratory disease, diabetes and hypertension.
Complications:
pain,
stretching,
Irregular menstrual cycle,
Local infection.
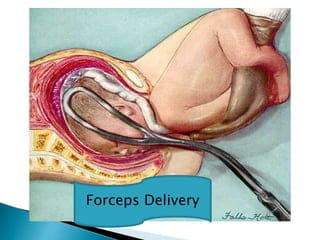
Forceps Delivery:
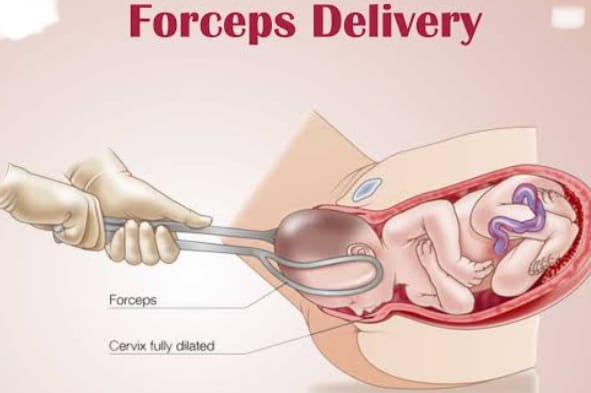
Obstetrics forceps were invented by doctors of the Chamberlain family in England in the 11th century. Obstetric forceps are a pair of instruments, and they are specially designed to extract the fetal head.
Simple Classification:
1) Conventional traction forceps
Short: Wrigley’s, Simpson’s Short, Elliott. Generally, short forceps are used.
Long:
a) Without axis traction E.X. Simpsons Long, Elliotts Long, Das Forceps.
b) E X with with axis traction.Milne Murray, Barnes-Neville, Hague-Ferguson.
2) Rotational forceps: Killand, Moolgaoker, Barton.
3) Special forceps: Piper’s forceps for posterior head in breech, Hale forceps for LSCS, New rubberized forceps (Greenberg).
Classification or Types of Forceps Application:
1) High forceps:
Application of forceps to the head of the fitus involves involvement where the biparietal diameter has not passed through the plane inlet of the pelvis (non-engaged head).
In high forceps the head is not engaged.
2)Mead Forceps Operation:
Application of forceps involves involvement where the biparietal diameter has passed through the plane of the inlet but has not passed the level of the ischial spines. It has a fittal head a engage but and station +2 above.
It also has two sub-types:
1) High Mead,
2) Low Mead.
1) High Mead:
The biparietal diameter passes through the plane of the inlet but remains above the level of the ischial spines. Manual rotation performed using forceps is an example of such a forceps operation.
2) Low Mead:
The biparietal diameter is passed through the plane of the inlet and lies to the level of the ischial spines. Therefore, the lower pole lies below the level of the ischial spine.
3) Low forceps operation:
When the biparietal diameter of the fetal head has passed the ischial spine and forceps are applied, it is called low forceps operation.
Fetal skull +2 cm station or higher, but not reaching the pelvic floor.
Rotation is 45 degrees or less and greater than 45° in the anterior or posterior position.
4)Outlet forceps:
It is a variant of the low forceps operation, where forceps are applied to the head of the fistula on the perineum and the head is visible in the introitus between contractions. The sagittal suture should lie in the anterior-posterior diameter of the outlet. Thus, while all outlet forceps are low forceps, not all low forceps are outlet forceps operations.
The scalp should be exposed above the introitus except for separating the labia in the outlet forceps. Fetal skull is above pelvic floor, sagittal suture is direct antero-posterior diameter or right/left occiput in anterior or posterior position, fetal head is above perineum and rotation is greater than 45°.
Forceps have the following fundamental parts:
Blades: Each blade is mostly fenestrated but can also be solid. The fenestrated blade is light for rotation and its grip is good for traction. Each blade has two cusps.
1) Safelike Curve: Its curve is flat and fits over the fittal head.
2)Pelvic curve: Its curved part is above the rim and fits over the maternal pelvis.
Shank: The portion between the blade and the lock is called the shank and can be parallel or overlapping.
Lock: A lock is also available in forceps.
Handle: This is a long metal rod with finger grips on the outside and an Axis Traxon mechanism in the Traxon forceps.
Measurement:
Cephalic Covered Radius: 11.5 cm,
Pelvic Covered Radius: 17.5 cm,
Distance between two blades: Maximum 8.5 Cm and Minimum: 1.5 to 3.5.
Shank 6.25cm.
Handle: 12.5cm.
Functions of Forceps
Traction: About 20 kg of traction force is required in primigravida and about 13 kg of traction force in multipara.
Rotation: Kiland forceps are best for rotation of the head. But simple long forceps can also be used.
Compression: The forceps are the first type of lever. If the forceps are placed correctly in a biparietal, bilamar placement, their impact on the cranium is minimized.
Stimulation of Uterine Action: Traction should be given only when uterine contractions are present.
Protective Cage: Works as a protective cage to protect the premature baby’s head from the pressure of the birth canal.
The risk of sudden decompression in delivery of after-coming head in breech remains low.
Indications
Maternal:
The second stage of labor is prolonged when the mother is unable to bear down and to reduce the strain on the mother in some obstetric and medical conditions.
Pregnancy induced hypertension, eclampsia in obstetrics
Medical: Valvular heart disease, pulmonary tuberculosis, second lung disease, liver and kidney disease, general debility, anemia, diabetes etc.
Fetal: Fetal distress in second stage of labor or failure to progress, malrotation, large fits, cord prolapse with full dilatation of cervix, postmaturity, and aftercoming head in breech.
Contraindications: Incomplete dilatation of cervix, moderate or severe degree of contracted pelvis, malpresentation, contracting ring, pelvic tumor.
Pre-requisites:
After coming head (favorable presentation) in vertex presentation, China anterior or breech delivery in face presentation, fitus head +2, K + 3 station or 0/5 palpable above symphysis pubis (engage head), adequate pelvis, full dilatation of cervix, Rupture membrane, empty bladder and rectum, adequate anesthesia, episiotomy and resuscitation facilities for the baby are the primary requirements.
Low Forceps Application:
First of all consult the patient and his family members.
Provide proper lithotomy position to the patient. Then painting and draping.
Then administer anesthesia properly.
Emptying the bladder through a simple catheter.
Keeping the IV line properly patent by properly introducing the IV line to the patient.
Assessment of cervix, membranes and pelvic outlet by internal examination.
Steps of Operations:
First separate the right and left blades by articulating the blades in front of the patient. Then introduce the left blade first. Hold it vertically in the left hand and then introduce two fingers or the entire right hand into the vagina to depress the posterior vaginal wall. Insert the blade posteriorly into the hollow of the sacrum. Pushing with the thumb of the right hand. Pushing it upwards by the guidance of the fital head and internal fingers. Swing the handle downwards and backwards.
When correctly applied, the blades will be directed upward over the parietal eminence, the shank in contact with the perineum, and the superior surface of the handle. Then, by the guidance of internal fingers, rotate the blade and bring it to the left side of the maternal pelvis.
Now change the hand and hold the right blade in the right hand and bring it in front of the left blade from the same manor.
Then locking by depressing the blade, if proper application then locking is not difficult.
Give steady but intermittent traction during contractions after checking for proper application of the blades. Depending on the station of the head in the low forceps, push the head in a downward and backward direction until the head rests on the perineum, then push horizontally towards the operator until the crown is reached. After this slowly move the head in an upward and forward direction towards the mother’s abdomen to deliver the head from extension. Then remove the blades one by one and remove the right blade first.
After head delivery, the same procedure as for normal delivery should be done. And the patient should be given Inj. Methagin 0.2 mg given after delivery of anterior shoulder. Repair the episiotomy and check for tar and take next steps.
Complications:
Maternal: Birth canal, bowel, bladder can be injured and in rare cases bone can also be injured. Haemorrhage, infection, obstetric shock, uterine rupture and anesthetic complications can also occur.
Fit: Scalp injury, facial nerve injury, cephalohematoma, birth asphyxia, intracranial hemorrhage, linear or depressed skull fracture.
Nursing Interventions:
When the obstetrician decides to collect the forceps and prepare for their application.
To check record and report of fetal heart rate before applying forceps.
Providing psychological support to the patient and giving information about the procedure.
After forceps application to check the record and report of fetal heart rate before re-applying traction.
Observation of mother and baby for signs and symptoms of complications after the procedure.
To record forceps deliveries and monitor vital signs of mother and baby.
Advantages of Delivery
Forceps are more effective when rapid delivery is needed, such as fetal distress.
Forceps are most effective when moderate traction is required.
Safer for premature babies as the fetal head remains within a protective cage.
Ventos are useful in cases where they are contraindicated such as anterior face or aftercoming head in breech presentation.
Less frequently than Ventos occurs in neonatal scalp trachea, hemorrhage, jaundice, or cephalohematoma.
Vaginal delivery is more successful than Ventos.
If the vacuum is not maintained in the ventos, the problem of cups falling off does not occur after correctly applying the blades.
Forceps for outlet, mid-cavity or rotational delivery are available.
- Ventos/Vacuum Extractor:
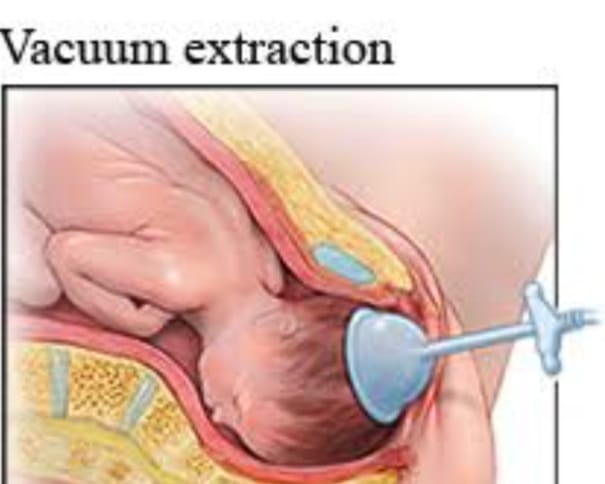
Ventos was introduced in 1956 by Malmstorm. Ventos are instrumental devices designed to assist delivery by creating a vacuum between the device and the fetal scalp.
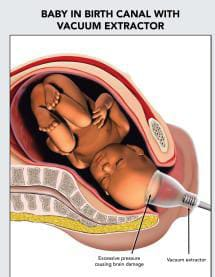
It involves the following components:
1.Suction cup with 4 sizes (30, 40, 50, 60 mm) made of metal.
- A vacuum pump with a manometer attached (modern vacuum extractors have an electrical pump).
3.Traction rod device.
4.Rubber tubing is available with chain in center.
Parts of instruments
Parts involve suction cups-4 sizes (30,40,50,& 60 mm) vacuum generator and traction tubing.
Initially, metal cups were used, but with soft cups, silk cups (silicone rubber/disposable plastic cups), better attachment to the scalp is achieved. These cups can be folded and introduced into the game without any difficulties and there is no risk of trauma or injury. There is less chance of aspiration while rigid plastic cups are safe and effective for rotational delivery.
The cup is connected to the pump by a thick-walled rubber tube to empty the air.
Vacuum is created by hand pump or electric pump.
Indications:
Atuate pelvis with dip transverse arrest.
If there is a second baby of twins and the head is high and the descent is delayed in the condition.
Fetal distress or prematurity.
In conditions of delayed first stage in the condition of uterine inertia or primary cervical dystocia.
As an adjunct to symphysiotomy.
In the condition that the second stage of labor is prolonged.
In rotation of caput from posterior to anterior.
Contraindication
Presentation other than vertex (like face, brow, breech etc.)
face presentation,
Preterm fits (< 34 weeks), suspected fetal coagulation disorder, suspected fetal macrosomia (> 4 kg),
unengaged fital head,
Suffelo Pelvic Disproportion,
Fetal Bleeding Disorder,
Premature chance of scalp avulsion or sub-aponeurotic hemorrhage is high.
Prerequisite Sides: Primary requirements such as forceps application only if cervix less than full dilatation and no head rotation can be applied Other conditions include vertex presentation, term fetus, fetal head athlete 0 station and more than 2/5 above symphysis pubis Should not be palpable. Uterine contractions are helpful but not necessary. Keeping obstetric forceps ready for use.
Procedure:
Advise the patient to assume proper lithotomy position.
Maintain proper aseptic technique or precautions while handling the patient.
Advising to empty the bladder properly.
Give perineal in-filtration or pudendal block depending on the station of the fetal head.
Perform a pervaginal examination.
Application of the cup
Select the largest possible cup according to the dilatation of the cervix.
Insert the cup by retracting the perineum with the fingers of the other hand.
Place the cup near the occiput (flexion point) in the fittal head so that the knob of the cup will be towards the occiput. This will flex the head and show the degree of knob rotation.
Apply betadine antiseptic solution over the rim of Malstrom Metal Co. Then introduce a vacuum of 0.2 kg/cm² in two minutes with a pump.
Checking for cervical or vaginal tissue in the cup.
Pressure 0.1 kg / cm² to create an effective vacuum of 0.8 kg / cm² in 10 minutes.
An artificial scalp is produced by sucking the scalp into a cup.
It disappears in a few hours.
Principles of Traction:
Traction should come at a right angle to the cup It should be consistent with uterine contractions If descent does not occur even after three pulls, operative vaginal delivery should be abandoned Traction should not be given for more than 30 minutes.
After the head is delivered open the screw release valve to remove the vacuum and release the cup then complete the delivery as per normal procedure.
Complications:
Maternal:
Injuries are usually minor, but injuries to soft tissues such as the cervix or vagina can occur.
Failure rate is high.
Neonate: Superficial scalp aberration and in cephalo hematoma, intracranial haemorrhage, retinal haemorrhage, jaundice etc.
Advantages:
It is easy to use and requires less anesthesia.
It can be used even if the cervix is dilated less than full dilatation. But in modern obstetrics it is applied after full dilatation.
Ventos are used in unrotated or malrotated heads. They help in autorotation.
Forceps do not occupy space like blades do.
Traction force is ( 10 kg ), which is less than forceps and because of the safety factor, the cup comes out due to vacuum break due to high pressure.
If applied correctly, maternal tissue is not injured. Perineal injury is minimized so it is the instrument of first choice.
Postpartum maternal discomfort is less than with forceps.
- Difference Between Forceps Delivery and Vacuum Delivery:
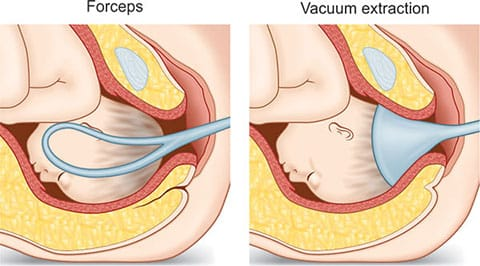
1) Forceps delivery:
In forceps delivery, the baby is delivered using forceps.
Obstetric forceps are a pair of instruments specially designed to extract the fetal head.
Forceps delivery does not require maternal afters.
Equipment in forceps delivery is less complex.
The incidence of cephalohematoma in forceps delivery remains low.
Forceps delivery is safer for premature babies because the fetal head remains within a protective cage.
Ventos delivery is performed using forceps in contracted cases such as anterior face or breech presentation.
Used in non-sephalic presentation.
Full dilatation of the cervix is necessary to apply the forceps.
For the application of forceps, the athlete’s femoral head should be at +2, +3 station.
Adequate anesthesia remains essential in forceps delivery.
In this the blade of the forceps will be directed upwards on the parietal eminence, the shank in contact with the perineum and the handle on the superior surface.
Forceps delivery is associated with third and fourth degree perineal lacerations.
The blades of the forceps hold the spot.
Maternal tissues are injured.
In case of conditions like fetal distress, it provides a quicker delivery with less time consumption.
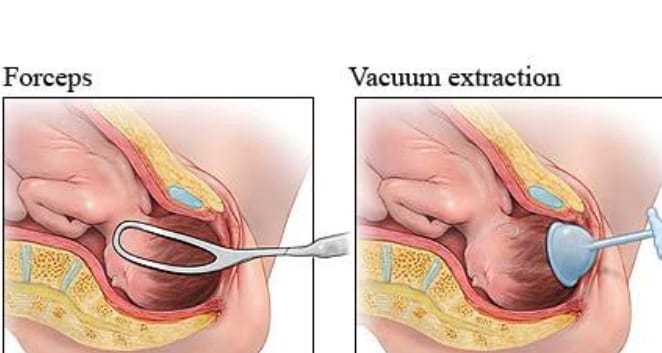
2) Vacuum delivery:
In vacuum delivery, the baby is born through a vacuum.
A vacuum is an instrumental device designed to assist delivery by creating a vacuum between the device and the fetal scalp.
A small amount of maternal aftertaste is required in vacuum delivery.
It can be done even if there is little expertise in it.
In it, the incidence of cephalohaematogen may be higher.
Contraindicated for premature babies because the fetal head is soft.
Contraindicated in non-vertex presentation (face, brow, breech).
It is not used in non-selflike presentations.
Vacuum delivery can be used even if the cervix is less dilated than full dilatation. But in modern obstetrics it is applied after full dilatation.
For the application of vacuum, the femoral head should be at the athlete’s zero station.
Vacuum delivery requires less anesthesia.
A vacuum cup is placed in the fetal head near the occiput.
Vacuum delivery is associated with solder dystocia and cephalohematoma.
A vacuum does not occupy space like forceps blades.
If the vacuum is applied correctly, it does not injure the maternal tissues.
The failure rate of vacuum is high.
- Destructive Surgeries:
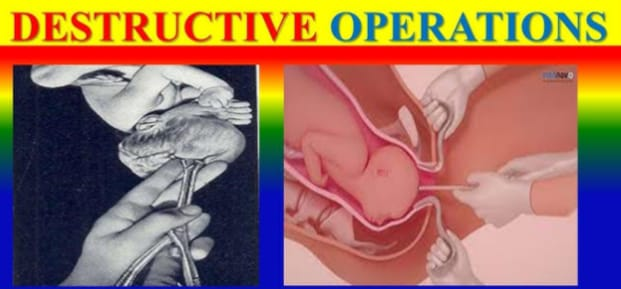
Definition:
Destructive surgery is performed when the fetus has died during intrauterine life and to expel this dead fetus from the uterine cavity through the vaginal canal and reduce the bulk of the fetus for easy delivery. is
There are four types of surgery that can be done such as,
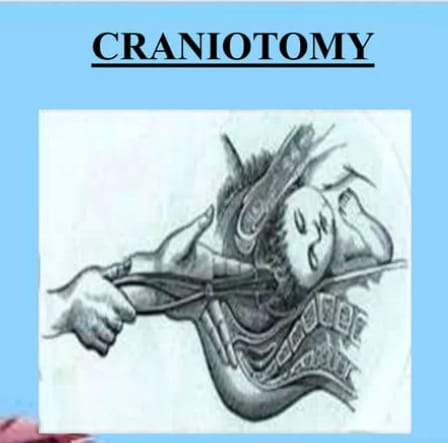
1.Craniotomy,
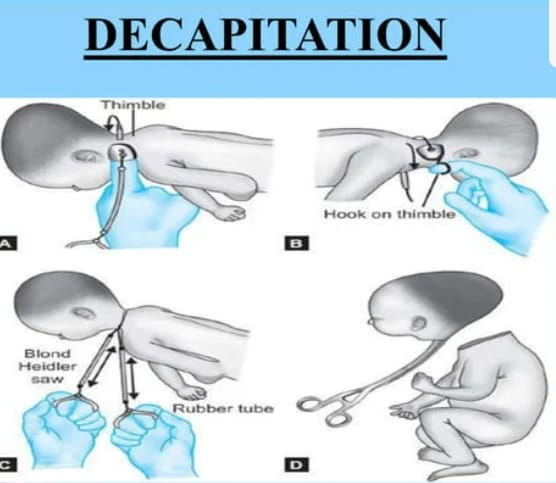
- Decapitation,
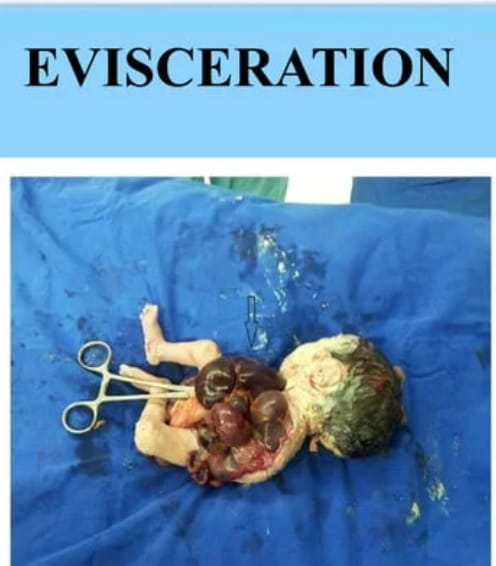
3.Evisceration, - Clidotomy.
1.Craniotomy: The operation to expel the fetus from the uterine cavity by perforating the head of the fetus is called craniotomy.
Decapitation: In this type of operation the fetal head is cut from the trunk and delivery is completed with extraction of the trunk. This operation is performed in dead fits with neglected solder presentation and interlocking heads of twins.
3.Evisceration: The contents of the thoracic and abdominal cavities are opened and delivered. This operation is performed in dead fits, neglected solder presentations and fit malformations.
Clidotomy: In this type of operation, one or two clavicles are divided and part of the shoulder girdle is reduced. It is performed only when there is shoulder dystria with dead fitters.

Complications: Injury to utero vaginal canal and viscera (bladder),
Rupture of uterus,
Post partum haemorrhage,
grief,
Peripheral sepsis, etc.