ENGLISH NEW MIDWIFERY GNM TY UNIT 11 High Risk and Newborn
Unit: 11 High Risk and Newborn
Assessment of Newborn Baby:
Post-birth assessment of newborns is crucial to assess their overall health, well-being and development. Here are some aspects of newborn assessment:
1) General Appearance:
Color:
Assessing the color of the child’s skin, most children are pink or red in color. If there is cyanosis (bluish discoloration), it indicates breathing difficulties.
Posture:
Note the baby’s muscle tone. A healthy newborn baby has their hands slightly flexed and their feet slightly curved along the spine.
Activity:
Observation of spontaneous movement involving sucking reflex and grasping reflex.
2) Vital Sign:
Heart Rate:
The normal range is 120-160/minute.
Respiratory Rate:
Normal respiratory rate is 30-60 breaths.
Temperature:
A normal temperature is 36.5-37.5°C (97.7-99.5°F).
3) Head and Face:
Fontanelles:
Palpate the anterior fontanel (soft spot) and posterior fontanel of the newborn. To perform proper closure and tension of the fontanelles.
Ice:
Checking the ice for its cementation. Assessing red reflex (indicative of normal eye structure) and response to light.
Nose:
Assess the patency of the nose so that breathing can be appropriate.
4) Mouth and Neck:
Oral mucosa:
Assessing the presence of cleft palate, oral thrush and any lesions in the oral mucosa.
Neck:
Assess for any mass-like structures or abnormalities in the neck.
5) Chest and Lungs:
Breathing Sound:
Properly listening to the child’s breathing sound.
Chest Movement:
Properly assess whether the child’s chest rises symmetrically and falls down with breathing.
6) Heart and Abdomen:
Heart Sound:
Proper auscultation of heart sound to assess for any murmur type abnormal voice and abnormalities.
Abdomen:
Palpate the abdomen and auscultate bowel sounds to assess whether there is any mass-like structure in the child’s abdomen.
7) Genital Area and Anus:
Genital Area:
To assess whether the anatomical structure of the genital area of the child i.e. male (presence of testes in male child) and female (labial structure in female child) is proper or not.
Anus:
To assess the patency of the anus and to assess whether there is any abnormality or not.
Urine and Stool:
Urine is passed within 24 hours of birth and the first stool called miconium is greenish black in color which occurs in the first 48 hours three to four times a day for three to four days and then three to four times a day. Four days of transitional stools that are greenish brown.
8) Extremities:
Hand & Fits:
Counting the child’s fingers and toes. and to assess symmetry or to assess whether there are any abnormalities.
Movement:
Assess whether the child has spontaneous movement and the range of motion of the hands and legs.
9) Skin and Umbilicus:
Skin:
Assessing the child whether there are any birthmarks, lesions and rashes on their skin.
Umbelicus:
Provide proper cord care to the child and assess for any signs and symptoms of infection and bleeding.
10) Behavioral Assessment:
State of Alertness:
Properly assess the baby’s level of awareness and the amount of stimulus to provide a response.
Crying:
Properly assess whether the child is crying properly or not due to which the respiration status of the child can be properly assessed.
Additional Considerations:
Documentation:
To accurately record all findings in the newborn assessment chart.
Parenteral Education:
Provide education to parents about newborn care including proper breast feeding technique, maintaining hygiene, and to go to health care center immediately if any signs and symptoms of infection are observed in the child.
By proper observation of the child after birth, if there is any congenital abnormality in the child or any potential risk factor of any disease, it can be identified early and adequate measures can be taken and the child’s condition can be prevented from getting complicated.
- Management of the Newborn with Hyperbilirubinemia/Neonatal Jaundice:
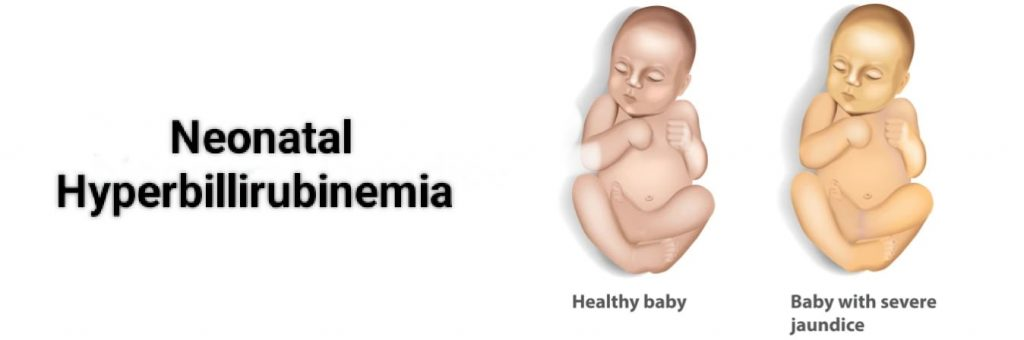
Definition:
When yellow discoloration of skin, sclera, and mucus membranes and body secretions due to accumulation of excessive bilirubin in body tissues is called “neonatal jaundice”/hyperbilirubinemia. Normal bilirubin is 0.1 to 0.8 mg/dl in blood. Now, when the level of bilirubin in the body is more than 5 mg/dl, it is called neonatal jaundice, it is also called icterus neonatrum or neonatal hyperbilirubinemia.

Incidence:
About 60% of full-term babies and 80% of preterm babies are seen in the first week of life. About 6% of term babies develop severe jaundice with bilirubin levels of 15 mg/dl or higher.
Type of Jaundice:
There are generally two types of jaundice namely,
1) Physiological Jaundice,
2) Pathological jaundice.
1) Physiological Jaundice:
Physiological jaundice is a non hemolytic jaundice caused by immaturity, in which the life span of neonatal RBC (red blood cells) is short and the conversion of urobilinogen is reduced. Defective uptake in liver cells from plasma, poor conjugation of bilirubin, increased enterohepatic circulation increases the load in the liver and causes defects.
Characteristic:
Jaundice usually appears 24-72 hours after birth.
Maximum yellow discoloration is observed on 4th – 5th day in full term baby and 6th – 7th day in preterm baby.
It usually disappears by 7 days in full term babies and by 14 days in preterm babies. Bilirubin level does not exceed 12 – 15 mg/dl.
It mostly does not require treatment and gets relieved on its own.
Cozies:
It is mostly seen due to excessive breakdown of RBC (red blood cells) due to short life span of red blood cells.
Inadequate enzymatic action of liver to convert bilirubin to soluble bilirubin due to hepatic immaturity.
Decreased conversion of bilirubin by the intestinal flora increases the amount of bilirubin in the circulation.
Treatment and Nursingcare:
There is no need to provide any specific treatment.
Provide adequate amount of fluid to the baby.
Careful observation of premature babies.
Advising the mother to provide adequate amount of breast feeding to her child.
If there is evidence of increased bilirubin levels to excessive amounts, treat by exchange transfusion.
Use phenobarbitone and phototherapy to treat this jaundice.
Providing proper daily routine or care to the child.
Careful observation of the child if there is any sign of complications.
Pathological Jaundice:
Definition:
Pathological jaundice occurs within 24 hours of birth. And if it is a mature baby it is usually seen for more than 1 week when
A pre-mature baby has mainly pathological jaundice for 2 weeks. Up to 5% of pathological jaundice occurs in the first 24 hours due to hemolytic disease and intrauterine infection.
Bilirubin in it increases at the rate of 5mg/100 ml in 24 hours.
Absolute bilirubin is greater than 15 mg/100 ml (250 μmol/L).
Reason:
Due to excessive hemolysis of red cells.
Due to defective conjugation of bilirubin.
Due to failure of excretion of conjugated bilirubin.
Due to Rh incompatibility.
Due to cephalohematoma.
ABO incompatibility.
Vitamin k therapy.
Congenital spherocytosis.
Due to glucose 6 phosphate dehydrogenase deficiency.
Due to reduced production of enzymes like glucuronyl transferase by immature liver cells due to prematurity.
Types:
Prolong unconjugated hyperbilirubinemia
Jaundice is mainly caused by hemolytic diseases of the breast mill.
Prolonged conjugated hyperbilirubinemia: It is mainly due to infection.
Clinical Features:
Yellow staining is seen on the face, trunk, palms and soles.
Urine staining is seen on the cloth.
The color of stool is clay, white or dark.
Bilirubin levels rise by 5 mg/dl/day.
Then Bija features symptoms like lethargy, drowsiness, poor sucking reflex, fever, infection etc.
Kernicterus (a pathological condition of the brain due to unconjugated bilirubin) develops when bilirubin develops above 15 mg/dl.
Its features include vomiting, high pitch cry, convulsions, opisthotonous position, nystagmus, hyperpyrexia, and spasticity.
Treatment:
The following methods are used to treat jaundice such as:
1) Phototherapy
2) Pharmacologic therapy
3) Exchange transfusion
Phototherapy:
Phototherapy is best used in moderate cases when the bilirubin level rises above (12 mg%). Phototherapy is stopped when the serum bilirubin level is around 10 mg%. A rebound increase in serum bilirubin may occur once phototherapy is stopped. It is important to maintain adequate hydration of the newborn. Spacial blue lamps with an output of 420 to 470 mm wavelength are most effective in treatment.
Phototherapy should be started as early as possible when maximum surface area can be exposed and ice shielding can be performed.
Phototherapy causes insensible fluid loss in newborns. Hydration is promoted by breastfeeding. Administering intravenous fluid therapy during phototherapy.
A phototherapy blanket protects the infant.
Phototherapy:
Phototherapy is a non-invasive, effective and simple and less expensive method to lower unconjugated bilirubin. Its light waves convert unconjugated bilirubin to a water-soluble non-toxic form by photooxidation that is readily excreted from the blood. Start phototherapy when bilirubin level reaches 15 mg/dl and 5mg/dl or higher in preterm babies.
Blue wave length is 450-460 nm. The tubelight and plexiglass are covered with a shield. A photo therapy unit is fixed over a crib or incubator. Fluorosonic or halogen lights can also be used.
Nursing Responsibilities in Phototherapy:
The baby should be completely exposed to the light source and the light should be kept at a distance of 45 cm.
Child’s head and genital area should be properly covered.
Advise the mother to provide frequent breast feeding to the child during photo therapy.
Provide feeding by intravenous infusion or nasogastric tube if extra fluid is required.
The position of the child should be changed every two hours and the position should be changed in such a way that it can get maximum light.
Keep checking the child’s temperature, pulse, and respiration (TPR) every two hours.
Continuously monitor the child for any side effects of phototherapy and have the serum bilirubin level tested every 12 hours.
Discontinue phototherapy when serum bilirubin level reaches 10 mg/dl.
Often phototherapy should be continued for 2-3 days. Or
6 hourly/day and,
Giving 2 hourly 3 times / day.
Involve the mother in the care of the baby.
It is important to give proper explanation, instruction and emotional support to the parents.
Complications and Side Effects of Phototherapy:
Immediate Problems:
Dehydration, hypothermia, hyperthermia,
loose stool/green stool,
Bronze baby syndrome (Bronze baby syndrome is a condition in which dark green-brown pigmentation of the child’s skin, mucus membranes and urine is observed after phototherapy is provided.)
skin lesions,
Hypocalcemia etc. are seen.
Long Term Problem:
Disturbance in endocrine and sexual maturation.
Skin cancer (rare condition).
Phenobarbital therapy:
Phenobarbital therapy induces hepatic microsomal enzymes and increases bilirubin conjugation and excretion. A dose of 5.8 mg/kg every 24 hours. is used. It takes 3-7 days to become effective. However, as a prophylaxis, it can be used in In which the mother is provided at a rate of 90 mg/dl two weeks before delivery.
Exchange transfusion:
Exchange transfusion is commonly used to prevent kernicterus.
In which double volume exchange replaces up to 80% of red blood cells and helps reduce bilirubin levels by up to 50%.
Indication of exchange transfusion
The level of bilirubin in the body increases progressively (more than 1mg/dl/hour) despite taking phototherapy.
If the neonate has anemia and in cases of congestive cardiac failure.
If the newborn’s serum bilirubin level is greater than 20 mg/dl.
If cord blood hemoglobin is less than 12 g/dl and bilirubin level is more than 5 mg/dl.
- Neonatal hypoglycemia:
A plasma glucose level of less than 30 mg/dL (1.65 mmol/L) in the first 24 hours of life after birth of the fetus and less than 45 mg/dL (2.5 mmol/L) thereafter is termed “neonatal hypoglycemia”. comes
Neonatal hypoglycemia is the most common metabolic problem in the newborn. That is, if the blood sugar level of the newborn or neonate is low for some days after the birth of the fetus, the condition is called neonatal hypoglycemia.
Neonatal hypoglycemia is a metabolic disorder in which the blood glucose level of the neonate decreases from its normal level, then this condition is called neonatal hypoglycemia.
Normal blood glucose level
Normal levels in a one-day-old neonate are: 40-60 mg/dl.
In neonates older than one day: 50-90 mg/dl.
Etiology/ Causes:
1) Maternal diabetes: Children born to mothers with diabetes (especially if diabetes is poorly controlled) are at increased risk of neonatal hypoglycemia.
2) Prematurity: Premature infants often have an underdeveloped system for regulating blood sugar.
3) Intrauterine Growth Restriction (IUGR): Babies who are smaller than expected for their gestational age may have impaired glucose stores.
4) Birth asphyxia: A condition where oxygen levels decrease during birth can affect the regulation of blood glucose levels.
5) Infection: Infection can increase the risk of hypoglycemia by affecting the baby’s metabolism.
6) Hormonal deficiency: Issues with hormone production, such as adrenal insufficiency, can lead to conditions of hypoglycemia.
7) Metabolic Disorders: Sometimes inherited metabolic disorders can also cause the condition of hypoglycemia.
8) Hyperinsulinemia: In some newborns, the production of insulin is in excess amount due to which the condition of hypoglycemia can arise.
Other Causes:
Due to supply of low amount of glucose,
Due to inadequate storage of glycogen,
Due to birth defects and metabolic errors,
Due to impaired production of glucose,
Due to increased utilization of glucose due to hyperinsulinism,
liver disease,
Due to some deficiency during pregnancy time.
Symptoms and signs:
poor feeding,
lethargy look,
hypotonia,
bluish discoloration of skin (cyanosis),
apnea,
hyperthermia,
paler,
neurological damage,
grunting sound,
twitching,
nervousness,
Caesar,
Congestive heart failure,
hunger,
nozia,
Vomiting
Diagnostic Evaluation:
Serum and plasma glucose levels,
serum insulin,
For metabolic disorders
screening,
Urine test.
Management:
Treat the condition of hypoglycemia as early as possible to prevent neurological damage.
Advising the mother to provide early breast feeding to the newborn.
If the newborn needs extra formula feeding, provide it properly.
Continuously monitor the blood glucose level of the newborn.
Properly evaluate the newborn for lethargy and poor muscle tone.
Properly monitor newborns for feeding problems.
If the blood sugar level of the newborn is continuously low and in the condition that the newborn is not able to take breast feeding, provide dextrose solution continuously to the newborn.
In rare situations, when there is no improvement in the condition of the newborn despite providing the above treatment, there is a need to perform surgery to remove part of the pancreas, due to which the production of insulin can be reduced.
Complications:
neurological damage,
Heart failure (in rare conditions),
Scissors (occasionally).
- Hypothermia:

Hypothermia is a condition in which the body temperature of the newborn and infant is reduced from its normal physiological body temperature. It is usually reduced to 36.5 °C and 97.7 °F.
This condition is usually seen due to imbalance in hit production and hit loss conditions. Which is usually seen due to environmental factors, inadequate thermal production, and physiological issues. Due to this condition of hypothermia, serious complications can arise in the body such as metabolic disturbances, impaired organ functions, and increases the susceptibility to infection.
Hypothermia is a condition in which the body temperature i.e. core or internal body temperature falls below 95°F and 35°C.

Mode of Heat Loss in Newborn:
1) Evaporation: Evaporation of amniotic fluid from the child’s skin surface after birth.
2) Conduction: After birth due to child coming in contact with any cold object, cloth and tray.
3) Convection: A condition in which cold air from open windows and fans surrounding the baby is replaced by warm air.
4) Radiation: When the environment surrounding the newborn after birth is colder than the body surface, the heat in the body is passed through the radiation to the surroundings.
Temperature Range:
Normal Axillary Temperature : 36.5-37.4°C.
Cold stress: 36.0°C-36.4°C.
Moderate hypothermia: 32.0°C – 35.9°C.
Severe hypothermia: temperature less than 32.°C.
Etiology:
1) SITUATION CAUSES EXCESSIVE HEAT LOSS:
cold environment,
wet and naked baby,
cold linen,
During transport,
infusion,
Blood sampling.
Poor Ability to Hit Conserve:
Low Birth Weight (LBW),
Intra uterine growth retardation (IUGR).
Poor metabolic heat production:
Due to deficiency of brown fat,
CNS damage,
hypoxia,
hypoglycemia,
Sepsis.
Symptoms and signs:
Peripheral vasoconstriction:
cold extremities,
Decreased peripheral perfusion,
Acrocyanosis,
Increase Metabolism:
hypoglycemia,
hypoxia,
metabolic acidosis,
Increases pulmonary artery pressure:
distress,
tachypnea.
CNS depression:
bradycardia,
lethargy,
poor feeding,
apnea.
Chronic Sign:
weight loss,
Poor weight gain.
Management:
Mild hypothermia:
Properly covering the neonate after birth, specially covering the head, chest and its fit properly.
Properly ventilate the neonate using any of the following methods such as:
skin to skin contact,
Warm room and bed,
Radiant heaters and incubators.
Monitor the temperature every half hourly. After reaching 36.5 °C, monitor the temperature 1 hourly for the next 4 hours, then monitor the temperature every 2 hourly for 12 hours.
Moderate hypothermia:
Keep the room properly warm to prevent the newborn from hypothermia.
Keeping the child’s coat or bed properly warm.
Use of incubator to maintain normal temperature in newborn.
Proper use of radiant warmers.
Continuous warming until the temperature of the newborn reaches the normal range.
Monitor the temperature every 15 – 30 minutes.
Management of severe hypothermia (less than 32°C):
Warm the room properly with a room heater or a 200 watt bulb.
Use a properly air heated incubator (air temperature 35 – 36 °C).
Properly monitor the heart rate, temperature and glucose level of the neonate.
Take proper measures to minimize hit loss.
I.V. 10% dextrose 60-80 ml/ kg/ day to start.
Provide proper oxygenation to the neonate.
If the neonate is term then provide 1 mg vitamin K injection and if preterm neonate then 0.5 mg vitamin K injection.
Prevention:
The temperature of delivery room should be properly maintained like 28-32°c.
Clean and dry the baby immediately after the birth of the newborn and then properly cover the baby with a pre-warmed towel.
Properly covering the baby’s head and immediately assessing whether the baby’s head is properly clean and dry after birth.
Keep the baby close to its mother so that the baby gets warmth.
Start breastfeeding the child within 30 minutes after the birth of the baby.
If the baby has a low birth weight i.e. weight less than 2500 gm, then proper Kangaroo Mother Care (KMC) should be provided to it, due to which the temperature of the infant is maintained and best feeding is observed, due to which the bonding of mother and infant is improved. happens
- Neonatal Convulsion:
Neonatal Convolution is a very life threatening emergency that occurs due to cerebral and biochemical abnormalities in the newborn. This condition is more common in preterm babies and low birth weight (LBW) babies.
Definition:
Neonatal convulsions are paroxysmal behaviors caused by hypersynchronous discharges by groups of neurons. Neonatal convulsions occur from birth to 28 days after birth. It is usually caused by abnormal electrical activity in the brain. Due to which involuntary movement of the body, changes in muscle tone, and alterations in the level of consciousness are seen.
This condition of convulsions is seen due to various reasons such as metabolic imbalance, brain injury, infection, and congenital abnormalities.
Etiology (cause):
Causes of Convulsion:
1) Traumatic:
hypoxic ischemic injury,
Intracranial injury.
2) Biochemical:
hypoglycemia,
Carnicterus,
hypocalcemia,
hypercalcemia,
hyponatremia,
hypomagnesemia,
Pyridoxine Dependence
3) Infective:
high fever,
meningitis,
TORCH
(T: toxoplasmosis,
O: Other (includes various infections such as syphilis, varicella-zoster virus, and parvovirus B19).
R: Rubella
C: Cytomegalovirus (CMV)
H: Herpes simplex virus (HSV) infection.
Tetanus.
4)Iatrogenic:
respiratory stimulant,
Analeptic drugs,
drug toxicity,
Theophylline.
5) Others:
Cerebral Malformation
Classifications of Convulsion:
Convulsions are mainly classified into two types.
1) General Caesars
2) Partial and focal onset seizures.
1) General Caesars
There are six types of General Caesars.
1) Tonic – clonic seizures.
2) Absent Caesar.
3) Myoclonic seizures.
4) Tonic Caesar.
5) Atonic Caesar.
6) Clonic seizures.
2) Partial and focal onset seizures.
There are two types of partial and focal onset seizures.
1) Simple focal seizure.
2) Complex focal seizures.
1) General Caesars
There are six types of General Caesars.
In generalized seizures, there is involvement of both hemispheres of the brain, i.e. right and left hemisphere. That is, uncontrolled electrical discharges occur in the hemispheres on both sides of the brain. In this type of seizure, the neonate becomes unconscious. This seizure lasts for a few seconds. to rhythm and is observed for several minutes.
1) Tonic – clonic seizures.
Tonic clonic seizures are also called Grandmal seizures. In this seizure, the consciousness of the neonate is completely lost. And the neonate also falls on the ground.
In the tonic stage, the patient’s muscles stiffen and muscle tone increases.
In the clonic phase, the patient’s muscle tone is lost.
2) Absent seizures.
Absence seizures are also called petitmal seizures. This type of seizure is mainly seen in children.
These seizures are seen only for a few seconds. In these seizures, the patient has episodes lasting only a few seconds and the patient does not even know that he is having any kind of issue.
3) Myoclonic seizures.
In myoclonic seizure there is involvement of muscles and excessive jerking movement of the body. So in myoclonic seizure there is excessive jerking movement of the body.
4) Tonic Caesar.
In this seizure, the muscle tone increases suddenly and the body becomes stiff and the muscle tone increases greatly.
5) Atonic Caesar.
In this seizure, muscle tone is lost, so a drop attack is seen in this, i.e. the patient is
Standing up falls because in this seizure the patient’s muscle tone stops suddenly. In this seizure, the patient suddenly regains consciousness after a drop attack. In this seizure, the patient has a high risk of head injury.
6) Clonic seizures.
The neonate in a caesarean
No muscle stone is lost suddenly. In this the neonate is found unconscious and its muscle stone is also lost. A jerking moment of the limb and a jerking moment of the extremities are seen in this seizure.
2) Partial and focal onset seizures.
These seizures are also called partial focal seizures and partial seizures. These seizures have unilateral hemisphere involvement.
It therefore affects whatever body activity is regulated by the involved hemisphere.
There are two types of partial and focal onset seizures.
1) Simple focal seizure.
In this type of seizure, the neonate may seem conscious, but there are unusual feelings and sensations.
In this, the usual feeling is that the child is very happy, very angry, or the neonate is suddenly sad or the feelings of nosia are seen suddenly and without any reason.
In this seizure there is involvement of only one hemisphere so the person has feelings of things that are not in reality.
2) Complex focal seizures.
In this seizure, the patient’s level of consciousness is altered or lost.
In this seizure, a person has a dream-like experience. In this type of seizure, the person does not even remember what he did properly. It is called complex focal seizure.
Symptoms and signs:
Temporary confusion.
Uncontrollable jerking moment of arms and legs.
Loss of consciousness.
Loss of awareness.
Temporary confusion may occur.
Numbness in body parts.
Loss of memory.
Visual changes occur.
Dizziness.
Tingling sensation in the chest.
Diagnostic evaluation:
History Collection,
Physical Examination,
Blood test.
Lumbar puncture.
Electroencephalogram.
Computerized tomography (CT scan).
Magnetic resonance imaging (MRI).
Positron emission tomography (PET test).
Single Photo Emission Computerized Tomography ( SPECT ).
Neuropsychological test.
Brain Mapping.
Management of Convolution Wada Neonate:
Maintain a properly safe environment to prevent injury to the neonate.
Keep the side rails up to prevent injury to the neonate.
Provide phenobarbitone 10 mg/kg body weight slowly over 3-5 minutes to control convulsions.
Do not put anything in the mouth of the neonate.
If the neonate is wearing anything around the neck, loosen it.
Not providing restraints to the neonate due to which injury cannot be prevented.
Provide a small pad under the head of the neonate.
If the neonate is vomiting, take proper care not to aspirate it.
Keep suction readily available and properly suction from the mouth and nose and keep the child’s airway patent so that breathing can be done properly.
Advise the child to take proper bed rest.
Provide intravenous (IV) fluids to the child.
Provide oxygen therapy to the neonate.
To provide proper working and comfortable environment to the neonate.
Advise the neonate to take proper medication.
Small for Date/Intrauterine Growth Retardation(IUGR)/Intrauterine Growth Restriction (IUGR) Dysmaturity/Chronic Placental Insufficiency:
Definition:
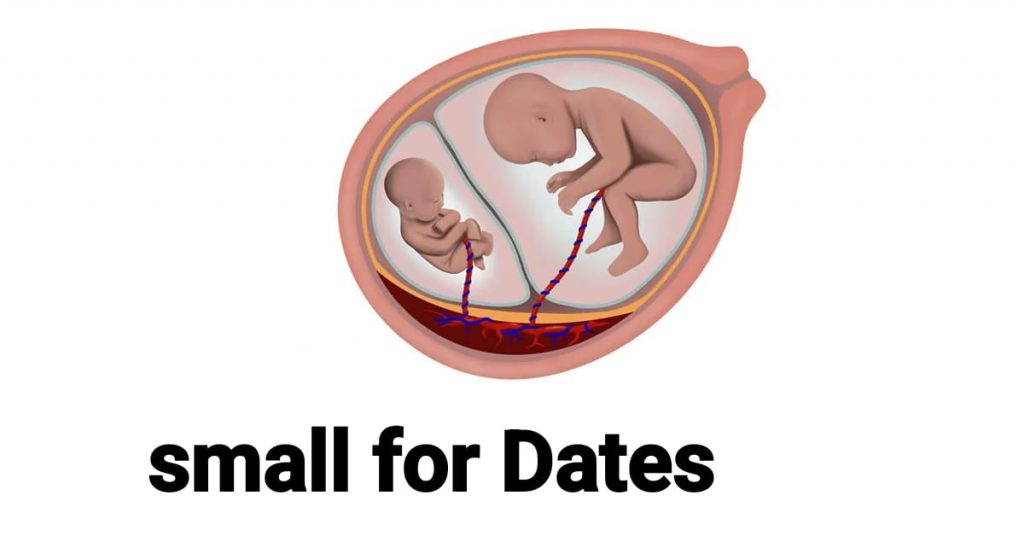
If a baby’s birth weight is less than the tenth percentile (10%) of its average gestational age, the condition is called intrauterine growth restriction/retardation (IUGR). Growth restriction/retardation can occur in preterm, term or post-term babies. can

Incidence of IUGR
Immaturity accounts for about 1/3 of low birth weight children.
Its overall incidence in developed countries is 2-8%.
Mothers of term babies – 5%,
In post-term babies – 15%.
Types: Small fits are divided into following two types based on clinical evaluation and ultrasound examination.
1) The fetus is small and healthy but its birth weight is less than the tenth percentile (10%) of its gestational age.
2) Growth restriction is due to pathological process so again it is divided into two parts viz.
(a)Symmetrical type I (20%),
(b)Asymmetrical type II (80%).
(a)Symmetrical Type I (20%):
- Uniformly small size.
- Ponderal Index (Birth Weight/Crown Hill Length): Normal.
3.HC(Head Circumference): AC(Abdominal Circumference) and Femur Length (FL):AC(Abdominal Circumference) ratio is normal. - Etiology: Due to genetic disease or infection.
5.Total Cell Number: Less, End Cell Size: Normal.
6.Poor prognosis with neonatal-complicated.
(b)Asymmetrical Type II (80%):
1.Head is bigger than abdomen.
- Ponderal Index (Birth Weight/Crown Hill Length): Low.
3.HC(Head Circumference):AC(Abdominal Circumference) and Femur Length (FL):AC(Abdominal Circumference) ratio are elevated. - Etiology: Due to chronic placental insufficiency.
5.Total Cell Number: Normal, Smaller Size.
6.Neonatal- mostly uncomplicated with good prognosis.
Etiology:
Fetal growth retardation is generally divided into four groups namely,
- Maternal,
2.Fittle, - Placental,
- Unknown.
- Maternal:
Constitutional: Small Women Due to maternal genetic and racial factors,
Due to maternal nutrition before and during pregnancy.
Due to poor-weight gain.
Cyanotic heart disease ma
Due to low blood oxygen level.
In-adequate substrate levels
Ex. Malabsorption syndrome.
Toxins like, alcohol, smoking, chronic renal failure, chronic urinary tract infection etc.
2.Fit:
In this, maternal blood contains enough substrates to cross the placenta but is not utilized by the fetus due to:
- Congenital Anomalies: Like, Cardiovascular, Renal and Other Factors.
2.Chromosomal Abnormalities: ie Trisomy 21, Trisomy 18 (Edward’s Syndrome) Trisomy 16, Trisomy 13 and Turner’s Syndrome. - Acceleration of the process of metabolism of the body due to torch agents.
- Due to multiple pregnancy.
- Placental: Due to poor uterine blood flow. Abruptio, circumvallate placenta, infraction
- Unknown. It is seen in about 40% of cases in unknown.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Clinical: Palpation of fundal height involves screening for fetal mass and volume Symphysis Fundal height after 24 weeks correlates with gestational age If it is 4 cm or less, it indicates growth restriction Abdominal girth if there is no maternal weight gain It does not increase.
Biophysical : HC, AC ration, femur length, amniotic fluid, anatomical survey ultrasound doppler parameters etc.
Biochemical markers: MSAFP and HCG levels are elevated in second trimester.
Physical Features at Birth:
Physical Features at Birth:
The birth weight deficit is about 600 gm less than the percentile standard.
Length is not affected.
Asymmetrical head circumference is greater than the body.
Dry and wrinkled skin, scaphoid abdomen, meconium-stained umbilical cord give the baby a “shriveled man” appearance. The cartilaginous ridges and plantar creses of the ear are well developed.
Baby is alert, active and cries normally, and keeps eyes open.
Reflexes are normal.
Management
Nursing management of the patient with intrauterine growth restriction usually occurs during the antenatal period, if possible.
Whenever a fit smaller than gestational age is suspected, a careful search is made to determine the presence of growth retardation by sonography.
When growth retardation is present, possible causes should be found out.
If growth retardation is present, the probable cause is identified.
If the fitus is symmetrical growth retardation, a meticulous search should be made to identify the fitus anomaly.
Fetus blood sampling and karyotyping to prevent unnecessary caesarean section in malformed babies.
The mother is given adequate rest in the pre-birth period, ie (in left lateral position).
Then there should be no after lunch for 2 hours and there should be a rest period of 8 hours during night time.
Provide balance diet in adequate amount to correct the condition of malnutrition to the mother. Like 300 extra calories should be provided.
A low dose of aspirin (50 mg) daily is helpful in selected cases
The patient should be properly hospitalized.
The condition of IUGR should be properly conformed.
To identify the patient for any congenital malformation and genetic disorder.
Any specific cause of intrauterine growth retardation should be treated first.
To check the fetal heart sound and mother’s condition regularly.
To check mother’s vital sign properly.
To provide proper support and reassurance to the mother.
Termination is done if the pregnancy is more than 38 weeks.
If the pregnancy is less than 38 weeks, the degree of IUGR should be checked.
If there is a condition of mild amount of retardation, advise the mother to take adequate amount of rest and provide adequate amount of supplementary therapy.
Assessing Lung Maturation of Fits in Severe Cases.
If maturity of lungs is achieved. It is assessed by L.S ratio (lecithin-sphingomyelin ratio), a value of L.S ratio greater than 2.0-2.5 is indicative of lung maturity. Delivery is done in such cases where growth of fitus cannot be improved by induction at 32-34 weeks followed by vaginal delivery/caesarean delivery.
If maturity of lungs is not achieved:
Maturity of the longus is evaluated.
Assay the level of phosphatidyl glycerol.
If the lungs are not mature, dexamethasone therapy is given and terminated.
Delivery can be made by:
Low rupture of membranes and followed by oxytocin
A casoma favorable for pregnancies of more than 34 wks is the cervix and the head is deep in the pelvis. If the cervix is favorable, prostaglandin gel can be used (PGE2).
Cesarean section is performed in unfavorable conditions.
During vaginal delivery the following are taken care of:
Delivery should take place in a well-equipped hospital where intensive intranatal monitoring is possible and has an intensive neonatal care unit.
Otherwise, the child should be transferred to a well-equipped hospital.
Precautions are taken during pregnancy.
The patient should be placed in the left lateral position.
If there is even slightly evidence of hypoxia (meconium staining and abnormal CTG), then immediate measures should be taken by caesarean section in the first stage and forceps in the second stage.
A pediatrician should also be available to care for the baby.
The baby should be cared for in an intensive neonatal care unit.
If there is a condition of hypoglycemia, special precautions should be taken for it.
To provide proper work and comfortable environment to mother.
- Birth asphyxia or asphyxia neonatorum:
Asphyxia neonatorum is failure to establish satisfactory pulmonary respiration at birth, meaning absence of pulse. Also defined clinically as failure to initiate and maintain spontaneous respiration within one minute of birth.
which leads to varying degrees of hypoxic and ischemic injury to body tissues and organs. It is accompanied by hypo ventilation, anaerobic glycolysis and lactic acidosis.
It is characterized by progressive hypoxia, hypercapnia, hypoperfusion and metabolic acidosis. It results in hypoxic ischemic encephalopathy with multi-organ dysfunction and neuromotor sequelae (neuromotor sequelae are long-term neurological and motor impairments due to brain injury or dysfunction).
Etiology:
Due to airway obstruction due to inhaled mucus or amniotic fluid.
Low alveolar surfactant causes lung expansion failure.
Administering morphine, pethidine and anesthetic agents to the mother in the prenatal and intra-natal period can cause asphyxia due to depression of the respiratory center of the baby.
Disturbance in the placental circulation leading to intrauterine hypoxia is the main cause of neonatal hypoxia. Such as anatomical changes in placenta, premature separation of placenta, post dated pregnancy, retro placental haemorrhage, pregnancy induced hypertension, and cord compression etc.
Due to birth trauma. Difficult forceps delivery, prolonged labour, contracted pelvis, breech delivery, oblique lie, occipito posterior position etc.
Due to weak respiratory muscles, immature respiratory center, and poor lung expansion in premature babies.
Congenital heart disease, blood loss, and circulatory collapse in shock.
Classification:
It is divided into two parts according to the intensity of clinical features viz:
1) Asphyxia Livida / Stage of Cyanosis/Blue Asphyxia
This is the primary condition of respiratory failure in which APGAR SCORE may be 4-6.
2) Asphyxia pallida/stage of shock/white asphyxia
This is a condition of respiratory and vasomotor failure with an APGAR SCORE of 0 – 3.
Clinical Features:
Clinical features of neonatal asphyxia vary according to degree of depression, duration of hypoxemia, plasma CO2 level and cause.
Muscle tone decreases in it.
Respiratory distress is observed.
Breathing difficulties are seen.
Irregular breathing is seen.
Cyanosis (Bluish discoloration of skin is seen especially around the lips and face.)
Abnormal heart rate (eg, bradycardia and tachycardia).
Reduced alertness and responsiveness.
Having a seizure.
Feeding difficulties.
Management:
Management of asphyxia neonatorum is divided into two parts viz.
1) Prophylactic management,
2) Definitive Management
1) Prophylactic Management:
To identify high risk during antenatal period itself.
Early fetal detection in high risk pregnancies. Because of this, if there is a condition of fetal distress, early identification can be done.
Use of electronic fetal monitoring during intrapartum period and scalp blood PH assessment as needed.
Proper use of anesthetic agents and anti-depressant medication during labour.
Definitive Nursing Management
Assess the baby’s APGAR score and provide proper treatment accordingly.
If APGAR score is between 7 – 10 then it is called normal.
If there is mucus in the baby’s oropharynges and laryngopharynges, clean them properly by suctioning.
Provide supplemental oxygen if needed.
Then reassess the condition of the neonate after five minutes, if normal, send the infant to the nursery.
If the baby’s APGAR score is between 4-6
Suction the baby’s mucus immediately from the oropharynx and nasopharynx by mucus suckers or suction operators.
After that, by providing the baby on a flat surface and head down position and turning his face to one side, due to which his mucus can be drained by gravitational force.
Simultaneously administer oxygen to the baby at a pressure range of 25-30 cm H2O through bag and mask.
Provide intermittent positive pressure ventilation to the infant if required.
Provide stimulus to infant on back and sole.
In majority of the cases, the baby can take independent respiration by using these simple measures.
After that, assess the APGAR score of the baby at five minutes, if it is satisfactory, then the infant should be given to the mother.
If the above measures fail,
Perform oral suction and start endotracheal intubation.
Connect an endotracheal tube to a resuscitation bag, through which O2 can be administered at a rate of 6-8 L/min.
Maintain Intermittent Positive Pressure Airway (IPPV) ventilation for 30 – 40/min.
Perform central external cardiac massage if heart rate is less than 60/min.
If the mother has a history of using a central depressant drug such as pethidine or morphine within 3 hours of delivery. A suitable antidote, e.g. Naloxone hydrochloride 60 mg/kg IM (single dose) or 10 µg/kg IV is given and may have to be repeated.
To combat acidosis, 8.4% NaHCO3 (sodium bicarbonate) 1 mEq/kg in 5% dextrose (diluted 1:1) is given very slowly (at a rate of 1 ml/min) in minimal doses through the umbilical or peripheral vein.
If the baby’s APGAR score is below 4,
Immediately perform tracheal intubation and start intermittent positive pressure ventilation.
If the mother has a history of using a central depressant drug such as pethidine or morphine within 3 hours of delivery. A suitable antidote, e.g. Naloxone hydrochloride 10 µg/kg IV is given to the neonate.
It is repeated every 2 – 3 minutes.
Complications:
respiratory distress syndrome,
cardiac failure,
respiratory infection,
septicemia,
Disseminated Intravascular Coagulation (DIC),
hyperbilirubinemia,
cerebral depression,
Failure to Thrive,
mental retardation,
cerebral palsy,
Convulsive disorder.
Introduction:
To prevent asphyxia by detecting risk factors and providing intensive intrauterine care.
Management of risk factors through necessary facilities or referrals.
Intranatal of fetal condition to detect fetal hypoxia
Assessment and management of fetal distress.
Preventing birth injuries through efficient management of malpresentation, contracted pelvis, instrumental delivery.
Careful use of anesthetic and depressant agents during the labor period.
Prognosis:
The prognosis of neonatal hypoxia depends on the maturity of the baby, duration and intensity of hypoxia, acidosis, and competent management.
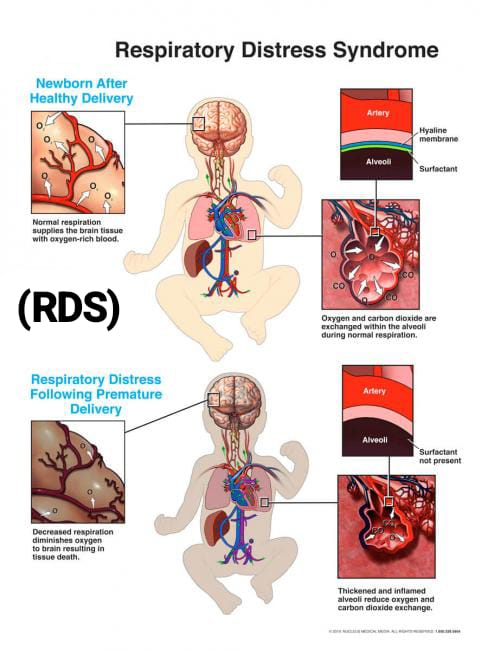
- Respiratory distress syndrome (RDS)
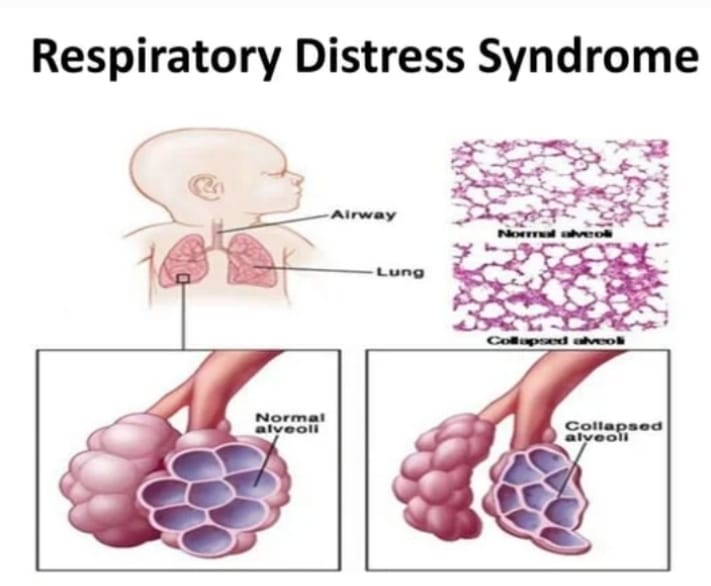
Definition:
Respiratory distress syndrome is a lung disease seen in newborns/neonates. It is mainly seen in premature babies, in neonates whose mothers are diabetic, in babies born by caesarean section or in breech delivery.
Respiratory Distress Syndrome (RDS) is usually seen due to the deficiency of Surfactant in the body of the neonate. The main reason for this is that when the newborn The child’s body cannot produce surfactant in adequate amount and due to lack of this surfactant in adequate amount the child’s lungs cannot function properly due to which gaseous exchange also does not take place due to which the amount of oxygen in the child’s body is reduced. Due to which conditions of hypoxia and acidosis arise.
Surfactant:
Introduction
Surfactant is a type of lipoprotein substance that is produced by combining phospholipids, mainly lecithin and sphingomyelin. And its ratio is usually (lecithin(L)):sphygomyelin(S)) of 2:1. Thus phospholipids called lecithin and sphingomyelin meet and produce surfactant.
function
Surfactant works to reduce the surface tension inside the alveoli, its functional unit inside the lungs in the body, due to which the lungs and alveoli do not collapse and gaseous exchange takes place within them properly.
production
Surfactant starts production at 20 weeks gestation period and its maximum production takes place during 37 weeks gestation period. A hormone called cortisol helps in the production of surfactant. Surfactant is produced by the alveolar type 2 epithelial cells of the lungs in newborns. And its storage takes place in the laminar bodies (LBS) of the alveolar cells. Maximum activity of surfactant to mature lungs occurs at 34 weeks’ gestation.
A child born before 37 weeks of gestation is called a preterm baby and is more likely to develop the condition of Respiratory Distress Syndrome (RDS) due to insufficient production of surfactant. Therefore, the condition of respiratory distress syndrome is seen in 50-80% of premature children.
Etiology:
pre maturity,
low birth weight baby,
asphyxia,
Maternal diabetes.
Symptoms and signs:
Rapid and slow breathing,
Respiratory rate to be 60/min,
Expiratory audible grating sound,
rib retraction,
Inter costal or sub costal retraction,
cyanosis,
in AD,
respiratory acidosis,
Electrolyte disturbance,
dyspnoea.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Chest X ray.
Management:
Aim of Treatment:
Provide surfactant replacement therapy.
Provide breathing support through a nasal continuous positive airway pressure (NCPAP) machine or a ventilator so that the infant can breathe properly.
Provide oxygen therapy.
Nursing Management:
If infants and neonates are suffering from Respiratory Distress Syndrome (RDS), provide them with artificial surfactant by inserting an artificial airway or breathing tube into the trachea/wind pipe so that the surfactant can enter the lungs directly.
Generally surfactant in the lungs of Fits starts to form from 24 weeks of gestation and is completely formed at 37 weeks of gestation, if adequate amount is not formed then there is a need to provide artificial surfactant.
Provide proper ventilatory support to the infant.
Infants with respiratory distress syndrome require the provision of ventilatory support through a mechanical ventilator connected to a breathing tube that passes through the infant’s mouth or nose into the wind pipe. to provide
Provide breathing support to the neonate by nasal continuous positive airway pressure (NCPAP).
To condition and treat hypoxia and acidosis in the neonate, warmed and humidified oxygen therapy is provided through positive pressure at 35% to 40% of endotracheal intubation.
Provide continuous positive airway pressure (CPAP) to the neonate if the arterial oxygen tension PO2 is not greater than 50 mm of Hg.
PO2, PCO2, and PH levels should be checked for early identification of any metabolic and respiratory acidosis conditions.
If condition of acidosis then administer sodium bicarbonate 4.2% (0.5 meq/ml Ex : 0.5 meq/ml amount to 1 meq/kg weight 1:1 with 5% glucose to provide minimum dose.)
Excessive use of alkaline can cause intra ventricular haemorrhage or even death in preterm babies.
Infants suffering from Respiratory Distress Syndrome (RDS) are treated with N. I. C. U. (NICU) and kept in a radiant warmer or incubator to keep them warm and reduce the risk of infection.
In this, the infant’s air passage is cleaned periodically by endotracheal suctioning.
Continuous monitoring of heart rate, breathing and temperature through sensors taped on the infant’s body, apart from this, using sensors on fingers or toes to check the amount of oxygen in the infant’s blood.
Administer albumin or colloid solution to treat hypovolemic conditions as prescribed by pediatrician.
Treat anemia or electrolyte imbalance conditions properly.
Surfactant:
Introduction
Surfactant is a type of lipoprotein substance that is produced by combining phospholipids, mainly lecithin and sphingomyelin. And its ratio is usually (lecithin(L)):sphygomyelin(S)) of 2:1. Thus phospholipids called lecithin and sphingomyelin meet and produce surfactant.
function
Surfactant works to reduce the surface tension inside the alveoli, its functional unit inside the lungs in the body, due to which the lungs and alveoli do not collapse and gaseous exchange takes place within them properly.
production
Surfactant starts production at 20 weeks gestation period and its maximum production takes place during 37 weeks gestation period. A hormone called cortisol helps in the production of surfactant. Surfactant is produced by the alveolar type 2 epithelial cells of the lungs in newborns. And its storage takes place in the laminar bodies (LBS) of the alveolar cells. Maximum activity of surfactant to mature lungs occurs at 34 weeks’ gestation.
A child born before 37 weeks of gestation is called a preterm baby and is more likely to develop the condition of Respiratory Distress Syndrome (RDS) due to insufficient production of surfactant. Therefore, the condition of respiratory distress syndrome is seen in 50-80% of premature children.
Etiology:
pre maturity,
low birth weight baby,
asphyxia,
Maternal diabetes.
Symptoms and signs:
Rapid and slow breathing,
Respiratory rate to be 60/min,
Expiratory audible grating sound,
rib retraction,
Inter costal or sub costal retraction,
cyanosis,
in AD,
respiratory acidosis,
Electrolyte disturbance,
dyspnoea.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Chest X ray.
Management:
Aim of Treatment:
Provide surfactant replacement therapy.
Provide breathing support through a nasal continuous positive airway pressure (NCPAP) machine or a ventilator so that the infant can breathe properly.
Provide oxygen therapy.
Nursing Management:
If infants and neonates are suffering from Respiratory Distress Syndrome (RDS), provide them with artificial surfactant by inserting an artificial airway or breathing tube into the trachea/wind pipe so that the surfactant can enter the lungs directly.
Generally surfactant in the lungs of Fits starts to form from 24 weeks of gestation and is completely formed at 37 weeks of gestation, if adequate amount is not formed then there is a need to provide artificial surfactant.
Provide proper ventilatory support to the infant.
Infants with respiratory distress syndrome require the provision of ventilatory support through a mechanical ventilator connected to a breathing tube that passes through the infant’s mouth or nose into the wind pipe. to provide
Provide breathing support to the neonate by nasal continuous positive airway pressure (NCPAP).
To condition and treat hypoxia and acidosis in the neonate, warmed and humidified oxygen therapy is provided through positive pressure at 35% to 40% of endotracheal intubation.
Provide continuous positive airway pressure (CPAP) to the neonate if the arterial oxygen tension PO2 is not greater than 50 mm of Hg.
PO2, PCO2, and PH levels should be checked for early identification of any metabolic and respiratory acidosis conditions.
If condition of acidosis then administer sodium bicarbonate 4.2% (0.5 meq/ml Ex : 0.5 meq/ml amount to 1 meq/kg weight 1:1 with 5% glucose to provide minimum dose.)
Excessive use of alkaline can cause intra ventricular haemorrhage or even death in preterm babies.
Infants suffering from Respiratory Distress Syndrome (RDS) are treated with N. I. C. U. (NICU) and kept in a radiant warmer or incubator to keep them warm and reduce the risk of infection.
Properly maintaining the nutritional level of the child including intragastric feeding or intravenous administration of 10% glucose i.e. 70ml/kg body weight daily followed by breast milk and infant formula through feeding tube to prevent malnutrition.
Regularly monitor fluid intake to ensure fluid does not build up in the child’s lungs.
Complications:
Intra ventricular hemorrhage,
pulmonary hemorrhage,
Retrolental fibroplasia,
Neurological Abnormalities.
Prevention:
Administration of betamethasone to patients who are likely to deliver before 34 weeks.
Assessment of maturity of lungs before induction of pre-mature labor and delay in induction so as to minimize the risk to the fetus as much as possible.
If there is a diabetic mother, then to prevent the condition of hypoxia of the fetus.
- Umbilical sepsis:

Umbilical sepsis means infection and inflammation of the umbilical cord stump in neonates is called umbilical sepsis in which there is redness, swelling and discharge from the cord area.
Etiology:
Staphylococcus aureus,
Streptococcus species,
Escherichia coli,
Pseudomonas aeruginosa,
Klebsiella species.
Risk Factors:
poor hygiene,
premature birth,
low birth weight,
maternal infection,
Delay Umbilical Cord Care.
Symptoms and signs:
1) Local symptoms:
redness,
swallowing,
discharge,
Pain.
2) Systemic symptoms:
fever,
lethargy,
poor feeding,
irritability,
Sign of Apsis:
hypotension,
Tachycardia,
Abnormal breathing pattern
Diagnostic Evaluation:
History Collection,
Physical Examination,
Microbiological testing
Umbilical stump culture,
blood culture,
Laboratory test
complete blood count,
C-reactive protein,
imaging
Treatment:
1) Initial Assessment:
Clinical Evaluation Proper examination of umbilical cord and neonate.
2) Antimicrobial therapy:
Provide proper broad spectrum antibiotic medication to the child.
Provide proper intravenous antibiotic medication (IV medication) to the child like Cifotaxime, Ampicillin etc.
3) Local care:
Clinical
Gently clean the umbilical cord stump with sterile saline and antiseptic solution (Ex: Chlorhexidonel) Avoid using alcohol and iodine solution which can cause irritation.
Drying: Keeping the umbilical cord area dry can prevent further infection.
Wound Care: Apply a sterile dressing to the umbilical cord if needed.
4) Supportive Care:
Monitoring: To monitor the child’s proper vital signs including temperature, heart rate, blood pressure continuously.
Fluid Management: Provide intravenous fluids to maintain the child’s hydration status to properly balance hydration and electrolytes.
Nutritional support: Provide adequate feeding and nutritional support to the child.
5) Follow-up: Giving advice for regular follow-up to assess the child’s condition.
Prevention:
Proper aseptic precautions while cutting the umbilical cord
to follow.
- Low Birth Weight Preterm Baby OR Prematurity OR Premature Baby
Low birth weight means that the child’s birth weight is less than 2500 gm, then this condition is called low birth-weight baby (LBW).
In which, a very low birth weight baby means a child whose weight is 1500 grams or less is known as a very low birth weight baby.
Whereas, an extreme low birth weight baby means an infant whose birth weight is less than 1000 grams, then this condition is called an extreme low birth weight baby.
Preterm baby

A preterm baby is defined as a baby born before completing 37 weeks of pregnancy, calculated from the first day of the last menstrual period. These babies weigh 2500 grams or less.
etiology
Uterine Anomalies: Uterine anomalies such as malformation of uterus and cervical incompetence can be causes of prematurity.
Prior Obstetrical History:
Women who have a history of prior abortion and preterm delivery may develop the condition of premature baby.
Multiple Pregnancy: A condition of pre-maturity or low birth weight may arise when more than one fetus is growing in the uterine cavity.
Maternal Diseases in Pregnancy: Due to certain disease conditions during pregnancy such as preeclampsia, polyhydroamnios, ante partum haemorrhage (placenta previa, abruptio placenta).
Due to infection: genital tract infection, acute appendicitis, pyelonephritis
Chronic Disease: It involves the involvement of pregnancy associated diseases like conditions like diabetes, severe anemia, hypertension etc.
Fetal Cause: It involves the involvement of congenital anomalies due to which the condition of growth retardation may arise.
Classification:
preterm,
Small for Gestational Age (SGA)
Preterm:
Growth potential is normal and appropriate for the gestational period (10th to 90th percentile).
Small for Gestational Age (SGA):
Small for gestational age is intended to designate newborns with a birth weight below the 10th percentile.
It involves less than two standard deviations for gestational age. SGA fetuses may be constitutionally small or due to a pathologic process (fetal growth retardation).
Symptoms and signs
Weight should be less than 2500 grams.
Length should be less than 44 cm.
Head and abdomen should be large.
Skull bone is soft with wide suture and posterior fontanel is wide.
Head circumference increases more than chest circumference.
Ear pinna should be soft and flat.
Skin is red, thin and sinewy due to low amount of subcutaneous fat.
Plantar crises may not be visible before 34 wk.
The testes are undescended.
The labia minora is exposed because the labia majora are not in contact.
Nails are not properly grown into finger tips.
Complications:
asphyxia,
pulmonary syndrome,
cerebral hemorrhage,
fital shock,
heart failure,
edema,
infection,
Dehydration and acidemia,
anemia,
retrolental fibroplasia,
oligouria,
Anuria,
Jaundice.
Management:
The cord should be clamped immediately after the birth of the child, due to which the condition of hypervolemia can be treated. After that, the condition of hyperbilirubinemia can be corrected.
If there is a condition of hyperbilirubinemia and there is a need for exchange transfusion, keep the cord length long.
Clearing the child’s mouth and nose properly by sucking mucus.
Provide oxygen by properly using mask and nasal catheter.
Wrap the baby in a properly sterile towel.
Keep the child in a head down position on the proper cot.
Inj to prevent child from hemorrhagic condition. Vitamin. Provide K 1 mg I/M.
Handling Baby with Extreme Gentleness
Advise the baby to avoid bathing.
Keeping the child’s body temperature properly stable.
Preventing the child from atelectasis.
To prevent the child from getting an infection.
To provide proper nursing care to the child.
A preterm baby is functionally immature so special care should be provided.
- Rh Incompatibility:
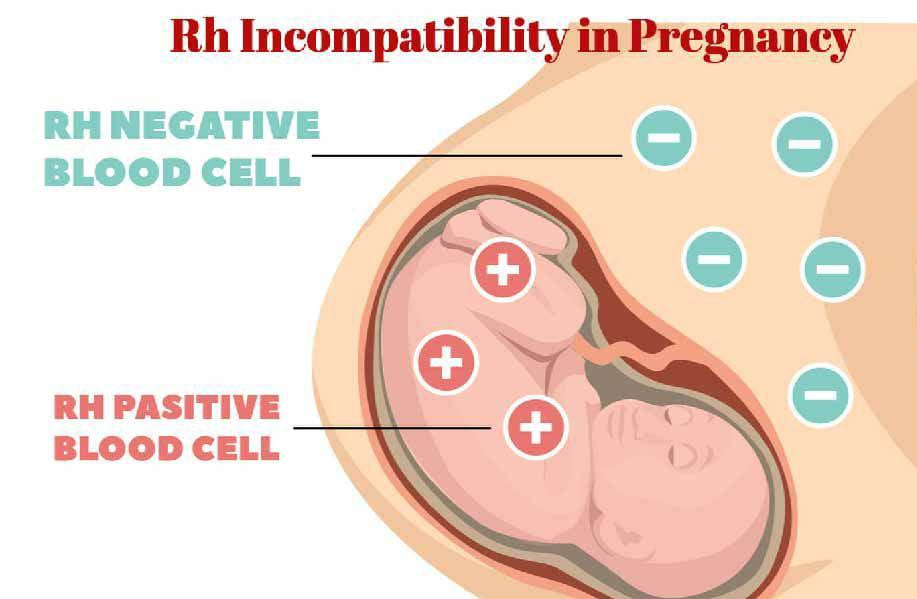
Rh factor:
Rh factor is a protein present on the surface of RBC (Red Blood Cell). which is called Rh positive and when this protein is not present on the RBC (red blood cells) surface then the condition is called Rh negative.
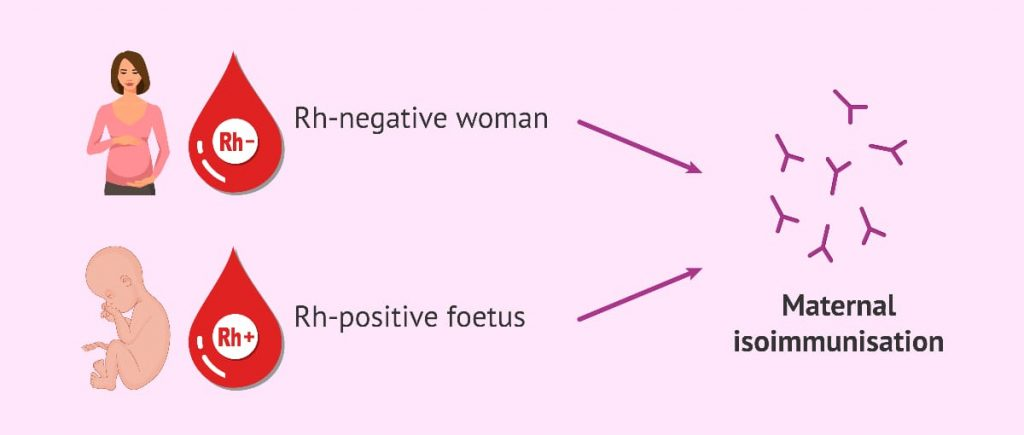
Rh Incompatibility:
The condition of Rh incompatibility is also known as Hemolytic Disease of Newborn (HDN).
The condition of Rh incompatibility arises when the blood group of the mother is Rh-ve (blood group) and the blood group of the child developing in her womb is Rh +ve, then the condition of Rh incompatibility is may arise.
Etiology:
When the mother’s blood group is Rh-ve and the father’s Rh+ve, the condition of Rh incompatibility can arise.
Having a history of transfusion.
Immune response.
Symptoms and signs:
The amount of bilirubin increases due to the breakdown of RBCs. And the condition of jaundice can arise.
hypotonia,
After birth the baby’s skin becomes yellowish and turns white.
lethargy,
Low muscle tone,
swallowing,
Edema.
Diagnostic Evaluation:
History Collection,
Physical Examination,
polyhydroamnios,
Finding more amount of bilirubin than normal infant,
blood type test,
Direct comb test,
Fetal Blood Typing,
ultrasound,
Middle cerebral artery Doppler.
Complications:
Carnicterus,
Hydrops fetalis (severe edema in unborn or newborn baby),
Problems like movement, hearing, speech etc.
Caesar.
Management:
Providing Rh immunoglobulin injection.
Proper blood transfusion should be done if the patient needs it.
Maintaining the proper hydration status of the patient, such as providing the patient with water, coconut water, fruit juice, which works to maintain the level of electrolytes in the body.
To keep the patient’s electrolytes properly maintained.
Providing the newborn with proper phototherapy.
Injury to the Navs to the Neonate:
- Facial Injury (Bell’s Palsy):
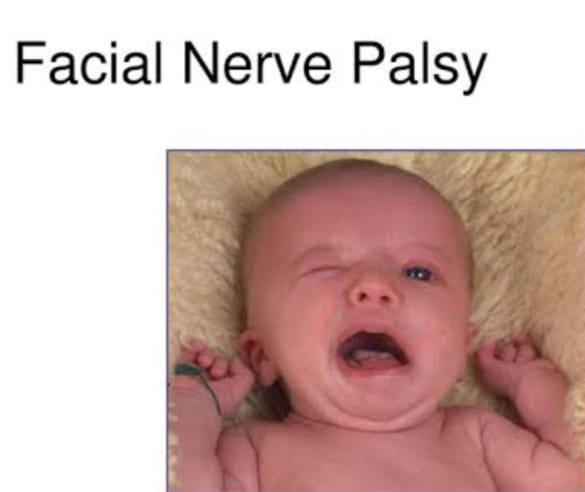
Facial palsy may occur due to pressure of direct forceps blade on the facial nerve and in normal delivery on the ramus of mandible side, facial palsy may occur. Its features include facial asymmetry (asymmetry), inability to close eyes, absent rooting reflux on the affected side and The angle of the mouth moves to the unaffected side while crying. Shaking reflex is good. Due to good regenerative power and short length of naves, recovery occurs in a few weeks Protecting eyes with antiseptic ointment as they remain open even during sleep.
Brachial Palsy:
Brachial palsy is caused by injury to the brachial plexus in shoulder distortion or traction on the shoulder or hyperextension of the neck in spontaneous vaginal delivery.
Clinical types of brachial palsy include Erb’s palsy and Klumpke palsy.
1) Erb’s palsy:
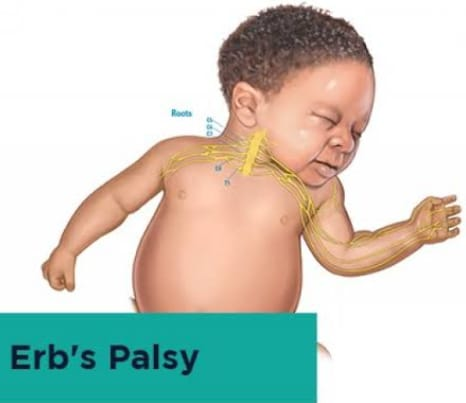
Erb’s palsy is caused by injury to the C5 and C6 nerve roots. Its clinical features include paralysis of the arm with extension of the elbow, pronation of the forearm and flexion of the wrist (waiter tip) on the affected side. Moro’s reflex is absent in the affected side. Permanent disability may occur in severe injuries. Treatment includes splinting of the arm, massage and passive movements. Most of the time, complete recovery comes in weeks or months.
2) Klumpke’s palsy: Damage to 7th, 8th cervical and 1st thoracic nerve roots causes Klumpke’s palsy. Its features include wrist drop and flaccid digits with paralysis of the forearm muscles. The arm is flexed from the elbow. Flaccid hand and flexed fingers with extension of the wrist. Damage to the cervical sympathetic chain of the 1st thoracic root causes meiosis ( Small, constricted pupil, tosis (drooping of the upper eyelid), anhidrosis (this is a rare condition in which the sweat gland does not produce sweat in a small amount or at all). , including placing a cotton ball in the baby’s hand to prevent contractions, and gentle massage and passive movements. Prognosis is good but severe laceration and hemorrhage may result in permanent deformity and if paralysis lasts for more than 3 months, neuroplasty is also required.

Injury to the bone:
Bone injuries can occur in the clavicle, humerus, and cervical spine. It is seen in difficult shoulder and breech delivery, green stick texture is common. Depressed fracture is seen in skull bone. Hip joint, joe, and cervical vertebra dislocation can occur so callus formation is necessary for excellent prognosis. Immediate identification and immediate management is important.
Injury to the Muscles: It is common in the sternomastoid muscles due to excessive lateral flexion of the neck in normal delivery, muscle injury is seen in difficult breech delivery and shoulder dystocia. Rupture of muscle fibers and blood vessels occurs on or after 7-8 days of birth. This leads to hematoma formation and presents as a tumor. The condition is complicated by contractions and torticollis (stiff neck with muscle spasm). No specific management required Mostly disappears within 6 months Stretching of neck muscles with gentle movement is helpful but massage is not required Torticollis persisting even after 1-2 years Requires surgical intervention.
Injury to the skin and subcutaneous tissue: Superficial abrasions, petechiae and bruising are seen after prolonged labor or forceps delivery. Spontaneous recovery occurs in 2-3 days. Local application of antibiotic lotion and hygienic practice leads to faster healing.
Injury to the viscera: Visceral injury can occur after difficult breech delivery and unskilled cardiac massage. Liver capsule laceration and spleen and adrenal hemorrhage may occur.Features of pallor, tachycardia, and shock are seen in the neonate.Correct hypovolemia and anemia to manage the condition. Surgical management of viscera repair. Prognosis is often poor.
Prevention of Birth Injury:
The incidence of birth injuries can be reduced with comprehensive antenatal and intranatal care.
Birth injuries can be prevented through skilled antenatal examination and identification and management of high risk cases in the skilled antenatal period.
Birth injuries can be prevented by the following practices during the intranatal period.
Do not stretch the neck unnecessarily during shoulder delivery in spontaneous vaginal delivery to prevent injury to the brachial plexus or sternomastoid muscles. Careful episiotomy to prevent scalp injuries. Continuous fetal monitoring to prevent cerebral anoxia. Precautionary measures to prevent birth injury in forceps delivery. Vaginal breech delivery to be performed by skilled personnel. Prolonged labor should be managed carefully.
- Caput Sucadenium:

Accumulation of serosanguineous fluid in the layers of the scalp causing edematous swelling is called caput sukkadenium. It is caused by the pressure of girdle of contact. It is either a bony pelvis, a dilating cervix or a vulval ring. Swelling and lymphatic drainage are seen due to low venous return.
Caput sucadenium is also seen at birth. And by pressing it, there is a hole in it. Swelling is bogey. And it crosses the suture line which disappears in 24-36 hours, mostly after membrane rupture.
- Cephalohematoma:
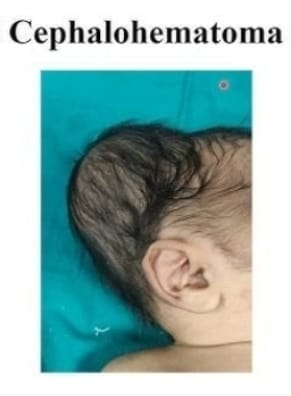
A cephalohematoma is a condition in which a collection of blood occurs under the pericranium and flat bones of the head that cover the skull bones, usually unilaterally and over the parietal bones. It is caused by rupture of a small emissary vein from the skull and may be associated with a fracture of the skull bone. This can occur due to forceps delivery but can also be seen after normal labor. Ventous application does not increase the incidence of cephalohematoma. It is never present at birth but develops slowly after 12-24 hours.
This swelling is limited by lines of sutures in the pericranium of the skull which are fixed to the margin of the bone, soft, fluctuant and incompressible.
It grows and disappears on its own after a few weeks i.e. approximately 6 weeks.
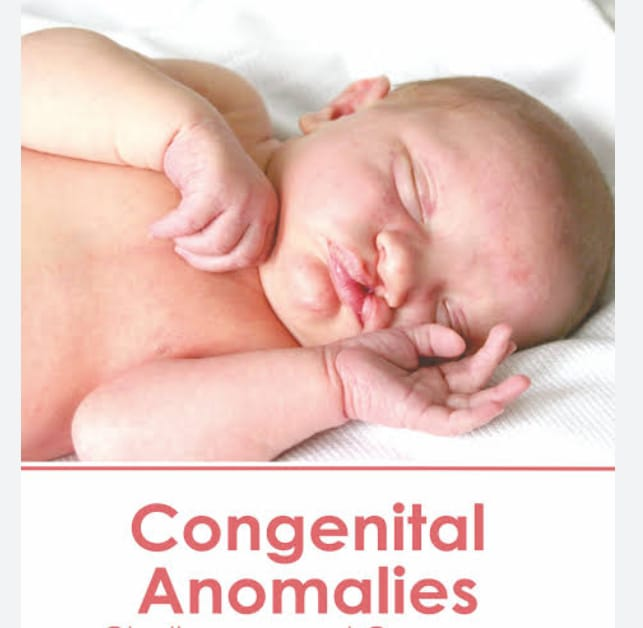
- Congenital anamolis
Congenital anamolis ne
Birth defect is also called. Congenital anamolis: That is, any metabolic, biochemical, structural, and functional disorder is present in the child at the time of birth. Congenital malformation When the child has only structural defect at the time of birth, it is called “congenital.” Malformation” is called.
Congenital anamolis affects any part of the body and results in physical and developmental disabilities. This congenital anomaly is usually caused by any genetic factor, environmental influences or a combination of both during the development of the child i.e. intrauterine life, genetic factors, chromosomal abnormalities, gene mutations, environmental influences, maternal infection, exposure to hazardous substances during pregnancy. (alcohol and certain types of medication), maternal health conditions such as diabetes, and obesity etc. and a combination of both.
Congenital anomalies involve central nervous system anomalies, cleft lip, cleft palate, heart disease, club foot, down syndrome and genetic syndrome.
Etiology:
Genetic factors include inherited genetic mutations and chromosomal abnormalities that are passed down from parents to their children.
Ex: Autosomal dominant disorder (Marfan syndrome),
Autosomal recessive disorder (cystic fibrosis),
X-linked genetic disorder (hemophilia),
and chromosomal abnormalities (Down syndrome).
Due to environmental factors
Some types of environmental exposures during pregnancy can increase the risk of congenital anamolysis, such as maternal infections during intrauterine life, especially STORCH (syphilis, toxoplasmosis, rubella, cytomegalovirus, herpes virus).
Due to mother’s exposure to teratogenic substances during pregnancy like alcohol, tobacco, smoking certain medicines, etc.
X-ray exposure of the mother during pregnancy.
Due to the mother taking certain types of drugs during pregnancy such as steroid hormones,
stilbestrol,
Anticonvulsants, folate antagonists, cocaine, lithium and thalidomide.
Due to maternal diseases like diabetes, obesity
Cardiac failure, malnutrition, iodine deficiency, folic acid deficiency etc.
Due to abnormal environmental environment like bicornuate uterus, septate uterus, poly hydroamnios, oligohydro amnios, fetal hypoxia etc.
Due to environmental pollution.
Symptoms and signs:
Physical Abnormalities
Many types of congenital anomalies are visible such as,
Cleft Leap,
cleft palette,
Limb deformities
(club foot),
Facial features being abnormal,
Abnormal growth pattern (microcephaly and macrocephaly) etc.
2) Developmental delay
Some children with congenital anomalies have delays in achieving developmental milestones.
motor skills,
language,
Speech development, cognitive abilities, social and emotional development etc. are involved.
3) Organ Dysfunction
Certain types of congenital anomalies cause dysfunction in internal organs and its signs and symptoms such as,
Congenital heart disease (cyanosis, rapid breathing,
poor feeding,
failure to thrive etc).
Gastero interstyle track ni anamolis (in it
feeding difficulties,
nozia,
vomiting,
abdominal pain, and failure to pass meconium etc.).
4) Neurological symptoms
Certain types of congenital anamnesis affect the central nervous system causing seizures,
Abnormal reflexes, muscle weakness,
Symptoms like paralysis, developmental regression, intellectual disabilities etc. are seen.
5) Respiratory symptoms
Certain types of congenital anamolis affect the respiratory system viz
Congenital diaphragmatic hernia,
Due to choenal atresia (narrowing of the nasal airway or tissues) respiratory symptoms such as respiratory distress,
Breathing Difficulty,
Rapid breathing and cyanosis may be observed.
6) Genitourinary abnormalities
Urinary tract abnormalities eg
genital abnormalities,
Problems with kidney function, its symptoms include urinary tract infection,
Difficulty in urinating,
Symptoms like abnormal genitalia etc. are seen.
7) Finding sensory impairment
Having congenital deafness,
Blindness.
List of Common Congenital Anomalies of Children
Common Congenital Anamolis Ma
1) Central Nervous System,
2) Congenital heart diseases,
3) Gastrointestinal system,
4) Respiratory system,
5) Genito-urinary system,
6) Musculoskeletal Abnormalities,
7) Blood disorders,
8) Metabolic disorders 9) Endocrine abnormalities,
10) Chromosomal Abnormalities
etc. the involvement of the system takes place.
1) Central Nervous System
Anencephaly in the central nervous system, spina bifida occulta, spina bifida cystica (meningocele,
meningomyelocele),
hydrocephalus,
Microcephaly, Macrocephaly,
Porencephaly etc.
2) Congenital heart diseases,
Congenital heart diseases include atrial septal defect (ASD), ventricular septal defect (VSD),
Tetralogy of Fallot (TOF),
Coarctation of Aorta (COA),
Patent Doctor’s Arteriosis (PDA),
Trans position of great artery.
aortic stenosis,
pulmonary stenosis,
Mitral or aortic regurgitation
etc. is involved.
3) Gastrointestinal system,
Gastrointestinal system: Cleft lip, cleft palate, tracheoesophageal fistula, esophageal atresia, congenital pyloric stenosis, duodenal atresia, congenital megacolon (Hisprung’s disease), exomphalus, umbilical hernia, anorectal malformation, diaphragmatic hernia, femoral hernia, Gertcher Cheese, Congenital Intestinal Obstruction etc Involvement takes place.
4) Respiratory system,
Respiratory system includes choanal atresia, tracheoesophageal fistula, congenital atelectasis, pulmonary agenesis, congenital stridor, congenital cyanosis etc.
5) Genito-urinary system,
Congenital hydronephrosis in the genitourinary system,
Congenital Polycystic Kidney,
Hosea Sue Kidney,
hypospadias,
Includes epispadias, congenital phimosis, congenital hydrocele, undescended testis, congenital inguinal hernia, ambiguous genitalia etc.
6) Musculoskeletal Abnormalities,
Musculoskeletal club foot, congenital dislocation of hip, developmental dysplasia of hip (DDH), osteogenesis imperfecta, polydactyly, syndactyly, Marfan syndrome, muscular dystrophy etc.
7) Blood disorders,
Thalassemia, Hemophilia, Sickle Cell Anemia, G6PD Deficiency etc.
8) Metabolic disorders
Metabolic disorders such as cystic fibrosis, phenylketonuria, G6PD deficiency, congenital lactose intolerance, galactosemia, Wilson’s disease, etc.
9) Endocrine abnormalities, congenital hypopituitarism (dwarfism) in endocrine abnormalities,
Congenital hypothyroidism (cretinism),
Congenital adrenal hyperplasia, congenital goiter, diabetes mellitus without involvement.
10) Chromosomal Abnormalities
Chromosomal Abnormalities Ma
Down syndrome (trisomy 21),
Edwards syndrome (trisomy 18), Patau syndrome
(Trisomy 13),
Turner syndrome (Xo),
Klinefelter syndrome (XXY, XXXY).
11) Other Anomalies
Congenital Anamolis include Congenital Cataract, Congenital Glaucoma, Rati no Blasto, Color Blindness, Congenital Deafness, Deaf and Dumb, Mental Retardation, Albinism, Hemangioma, Peder Willi Syndrome, Apert Syndrome etc.
Diagnostic evaluation
History Collection,
Physical Examination,
imaging studies,
Ultrasound during pregnancy,
x ray,
Magnetic Resonance Imaging,
computed tomography,
genetic testing,
Laboratory testing,
blood test,
Amniocentesis in early pregnancy (14 to 16 weeks),
Assay the maternal serum alpha phytoprotein (AFP),
antenatal screening,
Cardiac evaluation,
Neurological assessment,
Complications
Physical disability,
Limb deformity,
Health problems such as arrhythmias due to congestive heart defects,
heart failure,
Develop mental retardation,
Such as motor skills, language and cognitive impairment.
See the psychological challenge.
To have a psychological impact,
Seeing educational challenges due to developmental delay.
Management:
Children with congenital anomalies require regular medical monitoring and follow-up to monitor their growth development and overall health status. In which there is a need for regular physical assessment laboratory investigation, imaging studies etc.
Certain types of anomalies require appropriate surgical intervention to treat and alleviate symptoms. This surgical intervention is usually a cardiac anomaly, limb deformity, cleft lip and cleft palate, any anatomical structure requiring surgical intervention for reconstruction.
Medication treatment is needed to relieve certain types of congenital anomalies such as congenital heart effects with symptoms such as arrhythmias, heart failure, medication to prevent blood clotting.
Free habilitation therapy to treat certain types of congenital anaesthesia, including physical therapy, speech therapy, occupational therapy, etc., is required.
A child who has a condition of congenital anomaly needs to provide nutritious diet and feeding for proper growth and development of the child.
To provide adequate counseling and psychological support to children with congenital anomalies and their family members to cope with the condition.
To provide complete education to the child’s family members about the child’s disease, its causes, symptoms and signs, and its treatment.
To provide proper genetic counseling to the family members of the child and his parents.
Some types of congenital anomalies require life-long treatment, so all health care providers and family members should be properly collaborative and cooperative to provide proper treatment to the child.
To provide adequate comprehensive care to children with congenital anomalies.
To provide adequate psychological support to the parents of the child.
Preventive:
1) Preconception care
In preconception care, providing counseling and proper education to women who are in child bearing age so that women can take proper health care during pregnancy.
These generally include a healthy lifestyle, eating a balanced diet, maintaining an adequate weight, exercising regularly, avoiding harmful substances such as alcohol and smoking.
And if there is any medical health problem, its proper treatment is involved.
2) Prenatal care
There is a need for early and comprehensive prenatal care to properly assess maternal and child health. Due to prenatal screening, if the child has any congenital anomaly, its early detection and appropriate treatment is provided. It involves appropriate screening tests such as ultrasound and genetic testing and women are advised to have an adequate nutritious diet, adequate fluids, folic acid supplements to prevent neural tube defects, adequate sleep, smoking and alcohol avoidance. And giving advice not to come in contact with any hazardous substance.
3) Genetic counseling and testing
By providing genetic counselling, education is provided to women and couples whether the child is at risk of any type of congenital or anomalous or not, in which family history, genetic factors, and previous pregnancies are assessed and proper counseling is provided. Congenital anomalies in children can be prevented by providing genetic counseling to women and couples.
4) Avoidance of teratogenic exposure
To provide proper education to the pregnant woman that she should not be exposed to teratogenic substances and harmful substances and any kind of radiation exposure. Alcohol, tobacco, smoking, radiation, environmental toxins etc. are involved due to which there is risk of anomaly.
5) Optimizing Mother Health
The risk of congenital anomalies in the child can be prevented by providing appropriate health care before and during pregnancy, including proper treatment of any long-term diseases of the mother such as diabetes mellitus, hypertension, and thyroid diseases. .
If the mother has any kind of infection, treat her immediately.
Provide adequate food and vitamins supplements to the child if there is any nutritional deficiency.
6) Folic acid supplements
Adequate folic acid supplementation before pregnancy and during early pregnancy can prevent neural tube defects in the child. Like spina bifida, anencephaly etc. Women of child bearing age are advised to take daily supplements of 400 to 800 micrograms of folic acid ideally starting one month before conception and continuing till the first trimester after conception.
7) Environmental and Occupational Safety
A pregnant woman should not be exposed to any kind of hazardous chemicals and pollution due to which anomalies can be prevented. Occupational safety, guidelines and regulations should be followed regularly.
8) Screening and prenatal detection
Prenatal screening like ultra sound, maternal serum screening, and non invasive prenatal testing (NIPT) all these tests help in detecting any congenital anomalies and genetic abnormalities in the child. If early dissection takes place, adequate medical treatment can prevent congenital defects.
Congenital anomalies in the child can be prevented by using all these preventive measures.
- Newborn of HIV positive mother:

HIV / AIDS (Human immunodeficiency virus/acquired immunodeficiency syndrome) :
Acquired immunodeficiency syndrome is a disorder caused by the human immunodeficiency virus (HIV) in which there is a generalized dysfunction of the immune system. Cellular and humoral immunity is affected in it.
Mode of Action:
Two modes of transmission are mainly seen in the newborn.
1) Horizontal Transmission: Horizontal transmission of HIV occurs through intimate sexual contact or exposure to parenteral blood or contact with body fluids containing visible blood.
2) Vertical (Perinatal) Transmission: Vertical transmission is usually the transmission of the infection by an HIV infected pregnant woman to her fetus.
Symptoms and signs:
At birth, most children with HIV appear healthy and if not treated within 2-3 months may develop signs and symptoms of:
Early Sign of HIV:
Repeated fungal infections, mouth and oral thrush (oral cavity and posterior fairings).
Poor weight gain,
Lymphadenopathy (enlarged lymph node),
neurological problems,
Multiple bacterial infections,
hepatomegaly,
Pneumocystis carinii pneumonia (PCP) which usually occurs between 3 and 6 months.
Late sign of HIV:
diarrhea,
Failure to Thrive,
Developmental delay,
hepatosplenomegaly,
Chronic pneumonia, cough and lymphoid interstitial,
Chronic otitis media,
malays,
fatigue,
weight loss,
fever,
night sweat,
nephropathy,
Encephalopathy.
Diagnostic Evaluation:
History Collection,
Physical Examination,
ELISA (Enzyme Linked Immunosorbent Assay),
Western blot test (this detects the presence of HIV anti-bodies and is useful in children over 18 months of age),
P24 antigen: It is used to detect HIV antigen in children younger than 18 months. Two or more positive results are diagnostic for HIV infection.
CD4: It is used to evaluate the child’s immune status, risk for disease progression and the need for Pneumocystis carinii pneumonia (PCP) prophylaxis after 1 year of age.
Management:
Provide prophylaxis to infants born to HIV-infected women during the first year of life as prescribed against PCP.
Provide continuous prophylaxis to 12-month-old children diagnosed with HIV.
Providing antiretroviral therapy as a prescribed action of antiretroviral therapy is that it suppresses viral replication to preserve immune function and delay disease progression.
Providing the child with highly active antiretroviral therapy properly.
General Care:
Advising on proper hand washing.
If the child has conditions like weight loss, vomiting, diarrhea, malaise, altered activity level, oral lesions, the physician should be notified immediately.
Properly check whether the child has the condition of signs and symptoms of opportunistic infection.
Provide antiretroviral medication to the child as properly prescribed.
Keep the child properly isolated.
Keeping the child up to date immunized.
Keeping the child under proper monitoring and monitoring the child’s weight daily.
Provide proper calorie and protein rich diet to the child.
Keep food properly covered.
Wear gloves if you are in contact with body fluids while caring for the child.
Changing the child’s diaper frequently and wearing proper gloves while changing the diaper.
Fold soiled diapers inside out and dispose of in a tightly covered plastic container.
Clean up spills with a bleach solution (10:1 ratio of bleach to water).
Dispose of waste daily.
Immunization against common childhood illnesses is recommended for all children exposed to or infected with HIV.
Immunization of child with pneumococcal and influenza vaccine.
Administer Mumps, Measles and Rubella (M.M.R.) vaccine if the child is not severely immunocompromised.
- Newborn of a Diabetic Mother:
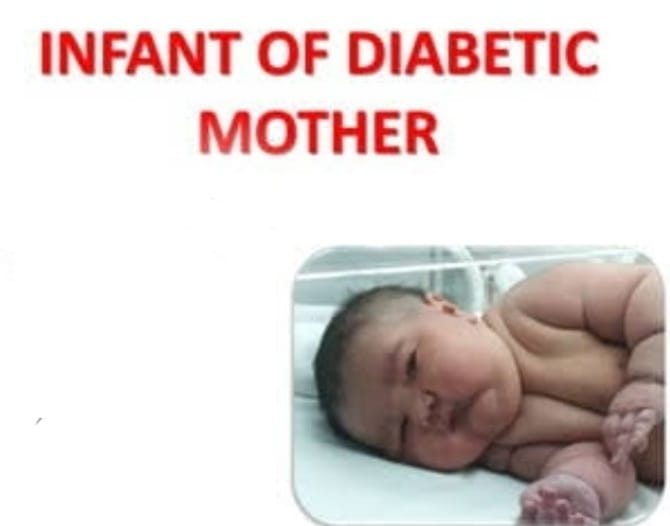
Newborn of a diabetic mother refers to a newborn or infant born to a diabetic mother. A mother who has diabetes, either preexisting (type 1 or type 2) or gestational diabetes (diabetes that develops during pregnancy). This condition can affect the baby’s health and development in several ways, requiring careful monitoring and management soon after birth to manage potential complications such as blood sugar, respiratory problems, jaundice and an increased risk of congenital anomalies.
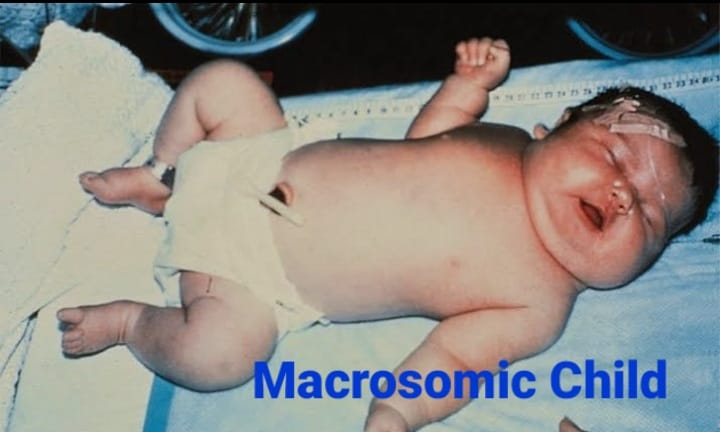
Generally two types of diabetes can occur during pregnancy viz.
1) Gestational diabetes,
2) Pre-gestational diabetes
1) Gestational Diabetes: This type of diabetes occurs during pregnancy as hormonal changes during pregnancy develop resistance to insulin. Here, the mother does not have diabetes before pregnancy.
2) Pre-gestational diabetes: In this condition the woman already has a diabetic condition such as insulin dependent diabetes.
Causes/ Etiology of Diabetes in Pregnancy:
The growing fetus is supplied with nutrients and water by the placenta. A number of hormones are produced to maintain pregnancy (cortisol, estrogen, human placental lactogen) that can block insulin. This usually occurs at 20-24 weeks of pregnancy.
On the other hand, with the growth of the placenta, there is also an increase in hormonal production due to which insulin resistance increases. Normally, the pancreas makes extra insulin to combat insulin resistance, but when insulin production is not enough to offset the effects of placental hormones, gestational diabetes occurs.
Women with pre-existing diabetes have an increased need for insulin, e.g. An insulin dependent mother may require more insulin as the pregnancy progresses.
Effects of gestational diabetes on fitness:
The effect of gestational diabetes on the fetus is of concern because the increase in maternal blood sugar levels during pregnancy is transferred to the fetus. This causes insulin to be secreted in greater amounts from the child’s body, causing tissue growth and deposition of fat, causing the newborn to be larger than expected for gestational age.
Newborns of diabetic mothers are at risk of congenital anomalies. Congenital anomalies such as heart, brain, spinal cord, urinary tract and gastrointestinal system problems can occur.
Other Conditions:
hypoglycemia,
macrosomia,
birth injury,
Respiratory distress.
Symptoms and signs:
Lazy size baby (due to excessive fat and glycogen accumulation in tissues),
In Face and Chikama AD,
Hyperbilirubinemia,
Signs of hypoglycemia:
twitching,
lethargy,
Caesar,
Difficulties in feeding,
apnea,
Cyanosis.
Signs of respiratory distress:
cyanosis,
nasal flaring,
grunting,
tachypnea,
Management:
Properly check for any signs and symptoms of respiratory distress.
Checking child’s bilirubin level properly.
Properly checking the child’s blood glucose level.
Monitoring the child’s weight properly.
To provide proper feeding to the child after the birth of the child.
Properly check whether the child has the condition of edema.
Properly assess whether the child has seizures and tremors.
Properly assess the child’s calcium level.
If the child has a condition of respiratory distress, provide oxygen properly.
Properly assess whether the child has any kind of birth injury.
- Levels of Care in NICU

Neonatal Intensive Care Unit (NICU):
Neonatal word is a compound word like:
NEW := new,
NATAL := Birth or Origin.
The Neonatal Intensive Care Unit (NICU) is called the Intensive Care Nursery (ICN) where infants and premature newborns, infants are properly cared for.
Level of care in n. I. C. U. ( NICU ):
N. I. C. (NICU) is mainly divided into four categories viz.
1) Level I : Well Newborn Nursery,
2) Level II : Special Care Nursery,
3) Level III : Neonatal Intensive Care Unit,
4) Level IV : Regional Neonatal Intensive Care Unit
1) Level I : Well Newborn Nursery:
Commonly referred to as a well baby nursery, this type of nursery has the ability to provide new resuscitation at each delivery.
In it, a healthy newborn infant is evaluated and properly cared for.
It provides proper care to neonates born between 35 and 37 weeks.
It provides neonatal care for neonates born below 35 weeks gestational age up to the time of transfer to appropriate neonatal care.
in it,
pediatrician,
family physician,
nurse practitioner,
And care is provided by another advanced practice registered nurse.
2) Level II : Special Care Nursery:
This is a special care nursery that involves the ability to provide all the care of a Level I nursery.
It usually provides care for neonates born at a gestational age of 32 weeks weighing 1500 grams or less and for newborns who are physiologically immature in a Level II special care nursery.
Infants who are able to feed and are in a recovery position after intensive care are cared for in a special care nursery.
Mechanical ventilation is provided for a brief duration and positive pressure is continuously maintained.
Infants born in less than 32 weeks of gestation and weighing less than 1500 grams are cared for in this special care nursery to stabilize them before being transferred to a neonatal intensive care facility.
in it,
neonatologist,
Neonatal Nurse Practitioner,
And
All Level I health care providers are involved.
3) Level III : Neonatal Intensive Care Unit:
It provides suspended life support care.
It provides comprehensive neonatal care.
It has immediate access to medical subspecialties, pediatric surgical specialties, pediatric anesthesiologists, and pediatric ophthalmologists.
It also has facilities to provide immediate ventilatory support and respiratory support.
In it, facilities of Computed Tomography (CT) scan, Magnetic Resonance Imaging (MRI), and Echocardiography are also available.
In it, all Level I and Level II care providers are available and in it,
Pediatric Surgeon,
Pediatric Medical Subspecialist,
Pediatric Anesthesiologist,
and Pediatric Ophthalmologist included.
4) Level IV : Regional Neonatal Intensive Care Unit:
This is a unit in which the highest level of neonatal care is provided.
In it, all the facilities of Level I, Level II and Level III care are available.
It also has facilities for Extracorporeal Membrane Oxygenation (ECMO) available.