ENGLISH NEW MIDWIFERY GNM TY UNIT 10 management of Complications of Purperium
Unit: 10 management of Complications of Purperium
Peripheral pyrexia A condition in which the body temperature increases to more than 100.4°F (38 °C) within 14 days after delivery is called “perperiral pyrexia”.
Or
When the oral temperature rises to 100.4°F (38°C) or higher on two separate occasions within 10 days after the first 24 hours of delivery, it is called “Peripheral pyrexia”.
Etiology:
unknown,
Genital: Peripheral sepsis.
Extra genital: ie,
Urinary tract infection (cystitis, pyelonephritis)
Breast infection (mastitis, breast abscess),
Intercurrent infections such as,
Malaria, pulmonary tuberculosis, respiratory infections, and fever.
Cesarean Section Wound Abscess,
Leg vein thrombosis
Other Causes:
mastitis,
pulmonary infection,
atelectasis,
pneumonia,
Septic pelvic thrombophlebitis,
malaria,
Pulmonary tuberculosis.
Symptoms and signs
fever,
chiles,
tachycardia,
uterine tenderness,
abdominal pain,
Foul smelling lokia,
Best Symptoms: Mastitis, localized pain, swelling and tenderness,
fatigue,
Decreased appetite.
Diagnostic Evaluation:
History Collection,
Physical Examination,
vital sign monitoring,
complete blood count,
blood culture,
Urine analysis, urine culture.
pelvic examination,
imaging studies,
Breast Examination
Management:
Carefully assess the site of infection.
Collecting complete history of the patient like headache, sneezing, cuffing, burning micturition, painful breast.
Complete physical examination of the patient including proper inspection and palpation of the uterus.
Look for nokia and perineum and examine the legs.
Send the throat swab, high vaginal swab, and midstream urine specimen to the laboratory and report the abnormality line to the physician.
Keeping records of patient’s vital signs and providing proper nursing care for febrile conditions.
Provide proper antipyretic medication to the patient.
Provide proper antibiotic medication to the patient.
- Peripheral sepsis

Infection in the genital tract as a complication of delivery is called puerperal sepsis. “Puerperal sepsis is infection of the genital tract during the first 6 weeks after delivery or abortion.”
Etiology:
endometritis,
endomyometritis,
endoparametritis,
or due to a combined infection of all three.
Causative Organism: Aerobic:
Staphylococcus pyogenes,
E. collie,
Klebsiella,
pseudomonas,
and non-hemolytic, Streptococcus,
Staphylococcus aureus,
Anaerobic: Involves:
Anaerobic streptococcus
Bacteroides fragilis
Clostridium welchii
Clostridium tetani
Predisposing factors:
Resistance to general or local conditions,
A condition that increases multiplication and virulence of the organism,
Due to introducing organism from outside,
Increasing prevalence of organisms resistant to antibiotics and chemotherapy.
Malnutrition and anemia,
Pre-eclampsia (antepartum factor),
Due to premature rupture of membranes,
Sexual intercourse during late pregnancy,
Due to chronic debilitating illness,
Introduction of sepsis into the upper genital tract during internal examination after rupture of membranes or during manipulative delivery.
Dehydration and ketoacidosis during labor,
Traumatic Operative Delivery,
Hemorrhage – APH or PPH,
Due to retained bits of placental tissues and membranes,
Placenta privya.
Mode of infection:
Mode of infection
Puerperal sepsis is specifically a wound infection. In this, the placental site, a laceration in the genital track, or a caesarean section wound can become infected.
Endogenous:
The organism is present in the genital tract before delivery, enters the genital organs through the blood stream or by the patient’s own.
Autogenous:
Here the organisms are present elsewhere in the body and are transmitted to the genital organs through the blood stream or droplet infection.
Streptococcus beta hemolyticus, E-coli, CL-welchii and Staphylococcus thus migrate from septic throat, physis and skin infections.
Exogenous:
Exogenous infection a
The infection is transmitted from some other source outside the patient. The organism is introduced by attendants, usually doctors or nurses. Infection may be in dust-borne or droplet form, during internal examination or through contaminated linen or blankets. Nowadays, Staphylococcus pyogenes is common.
Symptoms and signs
Local infection (wound infection):
The primary sites of infection are the perineum, vagina, cervix, and uterus.
Local wound infection can cause red, swollen and pus formation.
Slight temperature, malaise and headache can be seen and in acute infection rigor can be seen with high fever.
Uterine infection:
Temperature and pulse increase in mild infection.
Local discharge is thick and foul smelling.
The uterus is tender and subinvoluted.
In senior infection with high fever, rigor, lochia scanty and void, uterus may be tender, soft and sub involuted.
Extrauterine:
Pelvic tenderness (pelvic peritonitis),
Tenderness in Phoenix (parametritis),
In the pouch of Douglas, flesh (pelvic abscess) etc. can be seen.
Patients with pelvic peritonitis (pyrexia, lower abdominal pain, tenderness, pus),
General peritonitis,
thrombophlebitis,
Septicemia etc. can occur.
Diagnostic Evaluation:
History Collection,
Antenatal, intranatal and postnatal history
Physical Examination,
imaging studies,
Pelvic CT scan,
MRI (Magnetic Resonance Imaging),
Laboratory Tests:
Urine Examination,
WBCs (White Blood Cell Count),
cervical canal swab,
Intra Uterine Sampling of Uterine KVT Discharge,
Blood culture.
Management:
Antenatal
Improving the nutritional status of the mother and removing any infected areas in the body.
Intranatal
Surgical asepsis during delivery, screening for group B streptococcus in high-risk patients,
Antibiotics
Postpartum:
Initially a week of aseptic precautions, isolation and restricting visitors.
Treatment:
In general care, maintain isolation, give adequate fluids, calories, antibiotics and oral iron.
Properly maintain intake output chart of patient.
To properly monitor patient’s vital sign and maintain local discharge chart.
Surgical treatment: Relief of pus and pain in perineal wound.
Heparin IV 7-10 days in septic pelvic thrombophlebitis.
Debridement in colpotomy in pelvic abscess, laparotomy in unresponsive peritonitis.
If the patient is in septic shock, provide treatment.
- Thrombo-embolic disorder/venous thrombo-embolic disease:
Mainly 3 conditions are involved in venous thrombo-embolic disease.
1.Deep vein thrombosis.
- Thrombophlebitis.
- Embolism.
- 1.Deep vein thrombosis.
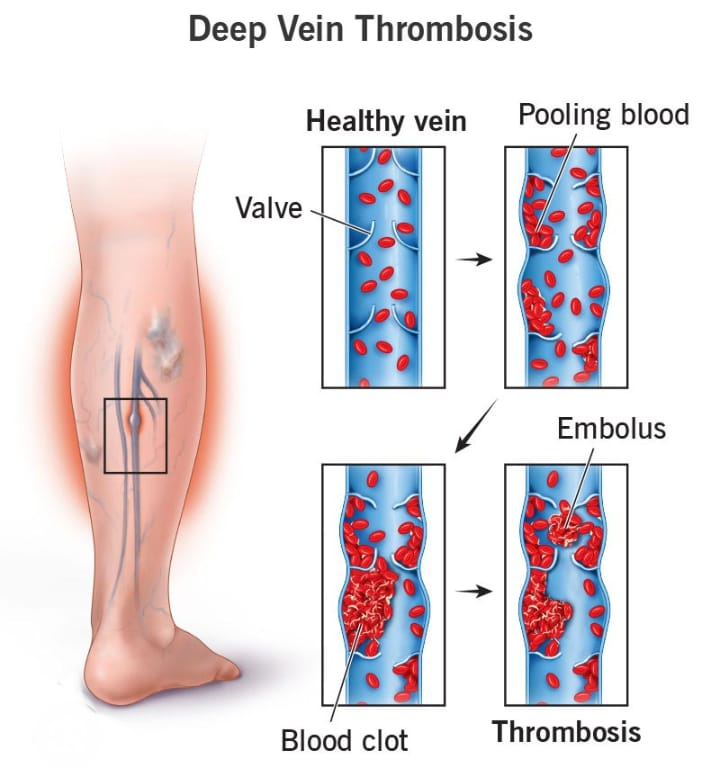
Deep Vein Thrombosis is a condition in which blood clot formation occurs in the venous system and mainly in the veins of the legs. This condition is called deep vein thrombosis. Thrombosis in pregnant women is significant because it increases the risk of pulmonary embolism. increases, and is a major cause of maternal death.

Etiology:
As the concentration of coagulation factor increases in normal pregnancy,
As the concentration of progesterone activity and platelet count increases,
By giving estrogen to suppress lactation.
Increased venous stasis due to pressure of gravid uterus on inferior vena cava and iliac vein.
Thrombophlebitis.
Other Risk Factors:
increase age,
multipara,
Operative Delivery,
obesity,
anemia,
heart disease,
Infection – pelvic cellulitis,
trauma,
immobility,
smoking,
Privy’s Deep Vein,
or,
Pulmonary embolism.
Symptoms and signs:
Pain in calf muscles,
fever,
Asymmetrical leg edema,
A positive Hohman sign (pain in the calf muscles when the foot is dorsiflexed), is seen.
Diagnosis:
History Collection,
Physical Examination,
Doppler ultrasound,
vinography,
Magnetic resonance imaging (MRI).
Management of Thromboembolic Diseases:
Preventing pregnancy and labor trauma, sepsis, dehydration and anemia.
Use of elastic compression stockings in surgery.
Advise for leg exercises and early ambulation after operative delivery.
Administration of low molecular weight heparin in high risk women.
- Thrombophlebitis:
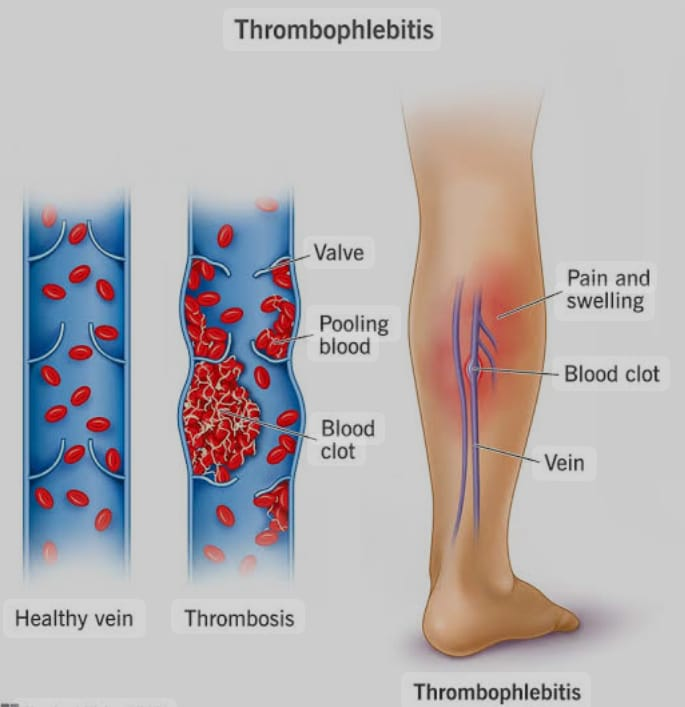
Thrombophlebitis is a condition in which blood clot formation occurs in the wall of vessels due to inflammation in the walls of the vessels. This condition is called thrombophlebitis. Postpartum thrombophlebitis occurs from a thrombosed vein at the placental site. When it is localized in the pelvis. It is called pelvic thrombophlebitis. It drains from the right ovarian vein to the lungs through the inferior vena cava and from the left ovarian vein to the left kidney. Sometimes retrograde extension into the iliofemoral veins results in “phlegmasia alba dolens” or white leg.
Etiology:
As the concentration of coagulation factor increases in normal pregnancy,
As the concentration of progesterone activity and platelet count increases,
By giving estrogen to suppress lactation.
Increased venous stasis due to pressure of gravid uterus on inferior vena cava and iliac vein.
Thrombophlebitis.
Other Risk Factors:
increase age,
multipara,
Operative Delivery,
obesity,
anemia,
heart disease,
Infection – pelvic cellulitis,
trauma,
immobility,
smoking,
Privy’s Deep Vein,
or,
Pulmonary embolism.
Symptoms and signs:
Most often occurs in the second week of purperium.
Rigor with fever mild to high,
Features of headache, malaise, tachycardia and toxemia may be seen.
The affected leg may appear swollen, painful, white and cold.
Pain in calf muscles,
fever,
Asymmetrical leg edema.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Doppler ultrasound,
vinography,
blood investigations,
Venus Ultrasound,
Computed Tomography (CT Scan),
Magnetic resonance imaging (MRI).
Management of Thromboembolic Diseases:
Preventing pregnancy and labor trauma, sepsis, dehydration and anemia.
Use of elastic compression stockings in surgery.
Advise for leg exercises and early ambulation after operative delivery.
Administration of low molecular weight heparin in high risk women.
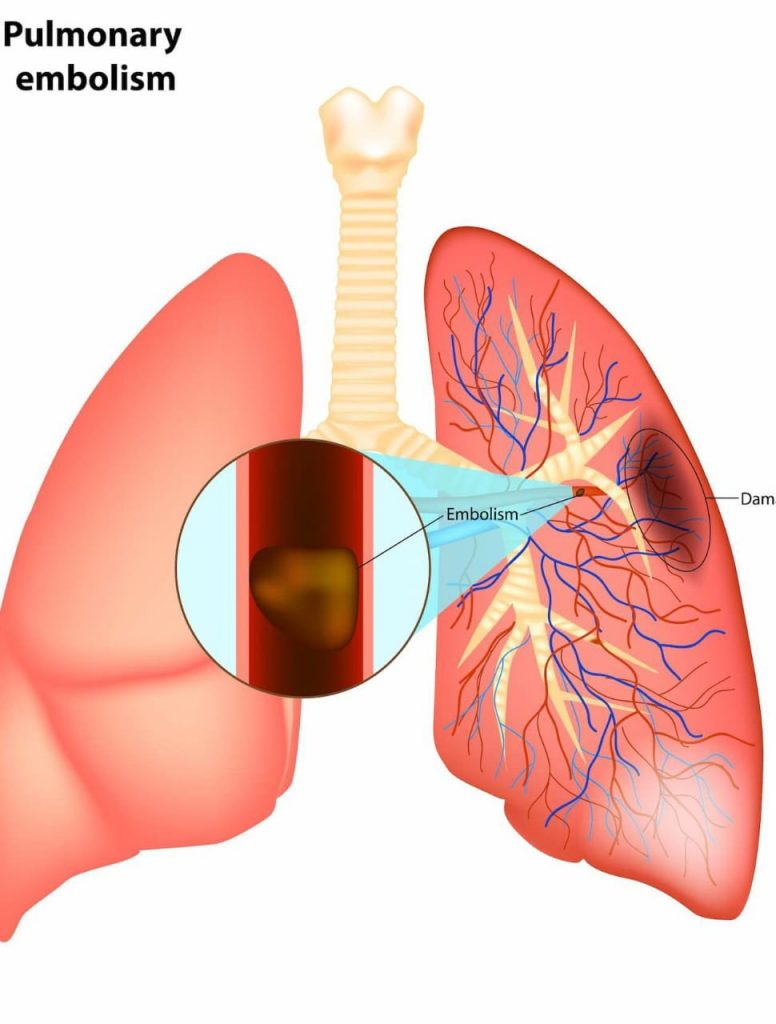
- Pulmonary embolism:

Pulmonary embolism involves obstruction and blockage of one or more pulmonary arteries due to thrombus (blood clot) formation. This thrombus originates in the vascular system or right heart and travels to the pulmonary artery.
Thus, when a large clot breaks loose from a thrombus vein and enters the pulmonary circulation, pulmonary embolism is seen. It is a leading cause of maternal death.

Etiology:
deep vein thrombosis,
Hypercoagulation,
venus statis,
Due to trauma,
Due to inherited or acquired clotting disorders,
Due to infection.
Prolonged immobilization
Heart failure
Heart disease
Hormonal factor
Advanced Edge
Obesity
Symptoms and signs:
Rapid onset of dyspnoea,
Shortness of Brith,
Pleuritic chest pain,
Tachycardia,
diaphoresis,
Blood in cough (haemoptysis),
cyanosis,
fever,
fainting,
Calf & thigh pain.
Diagnostic evaluation
History Collection,
Physical Examination,
Chest x-ray,
ultra sound,
Magnetic Resonance Imaging,
pulmonary angiography,
ventilation perfusion scan,
D dimer test,
electrocardiogram,
Doppler ultrasound,
Lungus scan.
Management:
Anticoagulant therapy
Provide anticoagulant drug for treatment of pulmonary embolism. Which prevents the formation of blood clot and helps dissolve the clot. Giving heparin, low molecular weight heparin medicine as anticoagulant drug.
Thrombolytic therapy
Providing thrombolytic therapy to rapidly dissolve the clot in life threatening and emergency conditions. which breaks down clots. For example tissue plasminogen activator (tPA)
Inferior vena cava filter
Inferior vena cava filters are used when anticoagulant therapy is contraindicated or ineffective. In which an inferior vena cava filter is placed which prevents the clot in the lower area of the body from traveling to the lungs and depositing in the filter there.
Supplemental Oxygen Provide supplemental oxygen to maintain adequate oxygen levels.
Embalectomy An embolectomy involves the surgical removal of a clot (embolism).
Nursing management of pulmonary embolism
The nurse plays an important role in assessing women for signs and symptoms of pulmonary embolism, including:
Sudden chest pain, shortness of breath, rapid heartbeat,
May include coughing and fainting.
To provide a properly comfortable position to women.
To check the vital sign of the woman, specially to monitor the respiratory rate and breath sound.
Properly assess the woman for signs and symptoms of respiratory distress.
Properly assess whether the mother is in a condition of hypoxia.
Adequate intravenous fluids to the patient.
Continuously monitor the woman’s oxygen level.
The nurse should prioritize stabilizing the woman’s condition by ensuring adequate oxygenation, providing oxygen as needed, and initiating cardiac monitoring. Depending on the severity of symptoms, administer intravenous fluids to maintain hemodynamic stabilization.
Proper collaboration with other health care personnel for proper care of women
Giving the woman proper medication, usually including anticoagulants (such as heparin or low molecular weight heparin) to prevent further clotting, and providing thrombolytics medication.
To provide complete education to the woman, and her caregivers, about the woman’s condition, its causes, symptoms and signs, and its treatment.
Properly monitoring how effective the treatment provided to women is.
To provide adequate emotional and psychological support to women and their family members.
To provide proper work and comfortable environment to women.
Providing education to women to take medication regularly.
- Breast Engorgement:
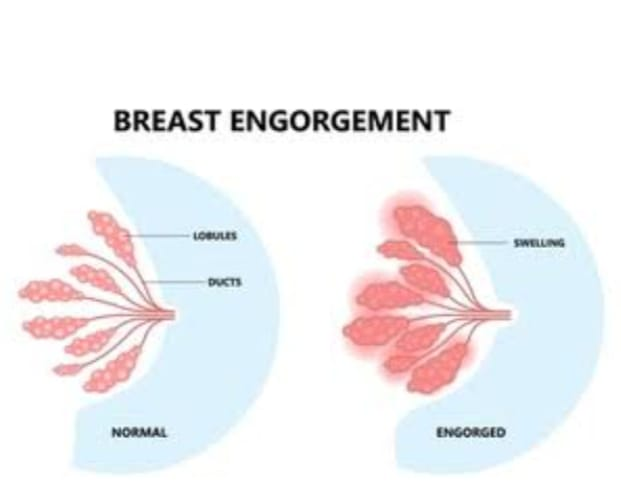
Breast engorgement is a complication of perimenopause that occurs due to venous and lymphatic congestion in the breast tissue. Breast engorgement condition is mostly seen after milk secretion starts in the peripartum period i.e. 3rd or 4th day postpartum. Breast engorgement is usually an overfilled breast due to increased secretion of breast milk after child birth due to accumulation of milk in the breast. And congested.
This condition is more common in breastfeeding mothers, especially in the early peripartum period when milk production and secretion are increased. This condition causes the breast to be full, firm and painful. And breast swelling and discomfort is called breast engorgement.
Etiology:
Due to normal venous and lymphatic engorgement in the breast prior to lactase, milk is not released from the lacteal system.
Due to increase in milk production during periperinal period,
Due to inadequate amount of breast milk being removed,
Due to the accumulation of milk in the breast due to not breastfeeding the baby properly.
Due to not providing proper position to the child during best feeding, adequate amount of breast milk cannot be removed.
Symptoms and signs
1) Swelling and firmness
Due to the accumulation of milk in the breast, the breast becomes tight, firm and swollen.
2) Tenderness and Pain Breasts are tender and painful and especially around the areola and nipple.
3) Skin changes
The skin on the breast is wrinkled and stretched.
4) Difficulty inbreast fitting
Child has difficulty in best fitting.
5) Fever and Malaise
Mother getting fever and feeling generalized body malaise and discomfort due to it.
Diagnostic evaluation
History Collection,
Assessment of symptoms in them,
onset and duration,
Private History,
Medical History Collection.
Physical Examination:
It includes breast assessment,
skin assessment,
Nipple Examination,
ultrasound,
Management of Breast Engorgement
1) Frequent and effective breastfeeding
Advising the mother to provide an adequate best fitting on the child’s demand to prevent milk from accumulating so that adequate amounts of milk can be removed from the best and the condition of breast engorgement can be prevented.
Providing education to the mother about the best feeding technique so that the mother can provide proper position to the child during breast feeding and correct amount of milk can be removed due to which breast engorgement can be prevented.
2) Completely emptying of breast milk
At the time of best feeding of the child, education should be provided to the mother to get the best fitting of the child on the other breast only after complete breast feeding on the first breast, due to which adequate amount of milk can be emptied from both the breasts and the condition of engorgement can be prevented.
3) Breast massage and warm compression
Providing education to the mother or gently massaging the breast before best feeding can soften the engorged area.
Advise the mother to provide compresses on the breast through vam water before feeding which can relieve the discomfort.
4) Manual expression of milk
If the child is not able to breastfeed properly, it is best to remove excess milk from the breast by using a breast pump or expressing milk by hand to prevent breast engorgement.
5) Comfort measures
Advise the mother to avoid wearing tight fitting clothes. Provide proper work and comfortable environment to the mother.
6) Pain Relieve
If the mother is in pain, provide analgesic medication to relieve the pain.
Ex:
Acetaminophen,
Ibuprofen.
- Breast abscess
Breast abscess is a condition in which pus/abscess collects in the breast tissue due to infection and inflammation in the breast tissue, this condition is called breast abscess.
etiology
Bacterial infections such as Staphylococcus aureus, including methicillin-resistant strains (MRSA).
Lactation: Blocked milk is often seen in breast feeding women due to milk duct or mastitis.
Trauma: Injury to breast tissue can introduce bacteria.
Skin conditions: Skin conditions like eczema, psoriasis can occur.
Vic Immune System.
Diabetic patient.
Due to surgery or invasive procedures.
Chronic condition.
Symptoms and signs:
localized pain,
Swelling,
redness,
Warmthness fill,
Getting a fever.
Diagnostic evaluation
History Collection,
Physical Examination,
ultrasound,
mammography,
Fine needle aspiration,
Culture and sensitivity test,
blood test,
Complete blood count (CBC) test.
Management:
Treatment consists of incision and drainage or serial percutaneous needle aspiration. To prepare the patient for the operative procedure.
Start breast feeding on the uninvoluted side.
Mechanically empty the infected breast every hour.
After the condition is treated, start breast feeding on the involved side.
Provide instructions to the patient on antibiotics and analgesics.
Midwives and doctors should wash their hands before handling the mother and baby.
Taking proper preventive measures to prevent breast abscess from occurring.
- Peripartum Psychosis/ Postpartum Psychosis
Peripartum psychosis or postpartum psychosis is a term that covers a group of mental illnesses characterized by the sudden onset of psychotic symptoms in women after childbirth. In which women may experience irritability, mood swings, hallucinations.
Peripheral psychosis is a severe form of mental illness occurring in approximately 1-2 cases in 1000 women with an onset as early as the first 48-72 hours after delivery and most often within 2-3 weeks due to increased hormonal changes. (such as a sudden drop in estrogen levels after birth).
etiology
The causes of perinatal psychosis are not yet known but are common in women with a history of bipolar disorder or who experience postnatal psychosis after a previous birth.
Risk Factors:
Having a family or personal history of psychiatric illness,
Past history of postnatal psychosis,
After birth of first baby.
Symptoms and signs
Signs and symptoms appear as early as 48 hours to 2 weeks after a child’s birth.
Symptoms like mania, depression or schizophrenia illness are seen in patients with postnatal psychosis.
Symptoms of mania such as,
Hyperactivity, euphoria, flights of ideas, insomnia, delusions, extreme excitement, restlessness, irritable, full of energy.
Hypomania with delusions, hallucinations (auditory), mutism, stupor or transient swings with severe depression.
Bizarre behavior,
Some mothers switch from depression to mania while others switch from mania to depression.
Typical features are confusion, extreme fear and ecstasy, perplexity, transient delusional ideation.
Management:
Psychiatrist is immediately consulted for management and the patient is admitted to the hospital.
Treat severe overactivity and delusions with antipsychotic drugs.
Drugs include chlorpomazine and sublingual estradiol to start, and lithium is given in manic depressive psychosis.
Providing electroconvulsive therapy in unresponsive or depressive psychosis.
Do not give breast feeding.
Supervision of the patient in cases of suicidal, infanticidal impulses.
Psychosocial treatment includes counselling, psychotherapy, cognitive behavioral therapy, family focus intervention and international focus intervention and social support is provided in the Postnatal Illness Association.