ENGLISH-MSN 1 : UNIT 2 HEALTH ASSESSMENT-UPLOAD
HEALTH ASSESSMENT :

USEFUL TERMINOLOGIES :
Acute Illness :
Severe symptoms are seen in this. Which are seen in short duration. A few days or weeks of illness are seen. Which occurs quickly. In which immediate treatment is provided. Its common cause is viral infection or injury. This illness also becomes normal in a short time.
Assessment :

Assessment is the systematic and intentional process of collecting information related to a patient’s health, which is called assessment.
Auscaltation :
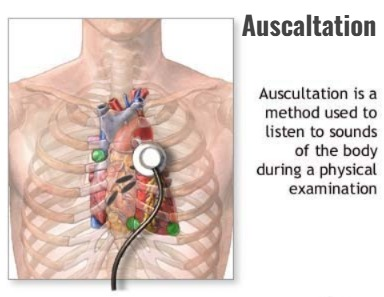
This is a physical examination method in which the body’s sounds are listened to through the ear or a stethoscope. In which sounds are heard from the heart, lungs, vessels, intestines, etc. In which the health care provider uses a stethoscope to listen to the sounds. This is also a diagnostic procedure.
Inspection :
This is also a method of physical examination in which all the data of the patient is taken through observation. In this method, health-related data is collected through the use of observation. For example, skin color, general appearance, etc.
Parcussion :
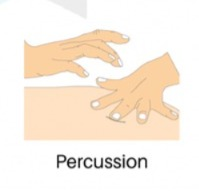
This is a method of physical examination. In which the density of body structures within a body cavity can be measured by collecting data from the sound produced by placing one hand on the body surface and tapping it with the fingers of the other hand. For example, The presence of air, fluid, etc. in the body structure is indicated by a change in the sound produced by tapping.
Palpation:
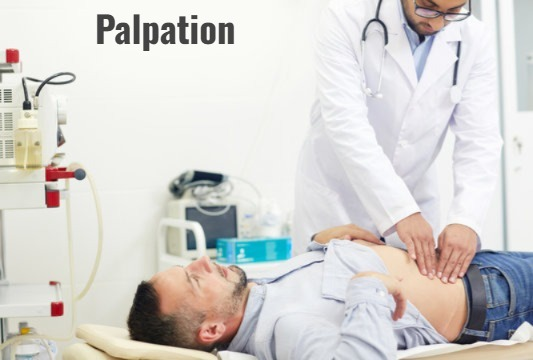
This is a method of physical examination. In which the size, shape or any abnormality is determined by pressing the organs or structures inside the body cavity with pressure.
Cheyne stoke respiration (Cheyne stoke respiration):
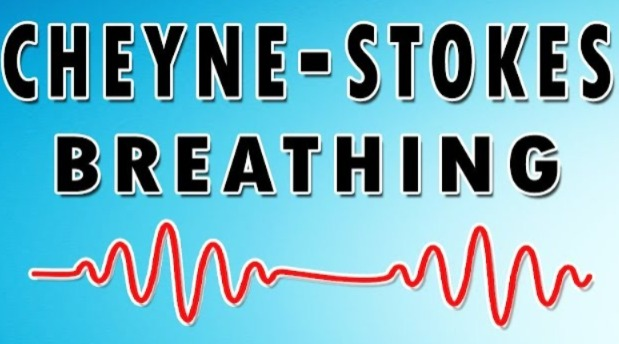
This is an abnormal pattern of breathing that is characterized by periods of apnea. In which the depth and frequency of respiration gradually increase after an episode of apnea.
Bradycardia:
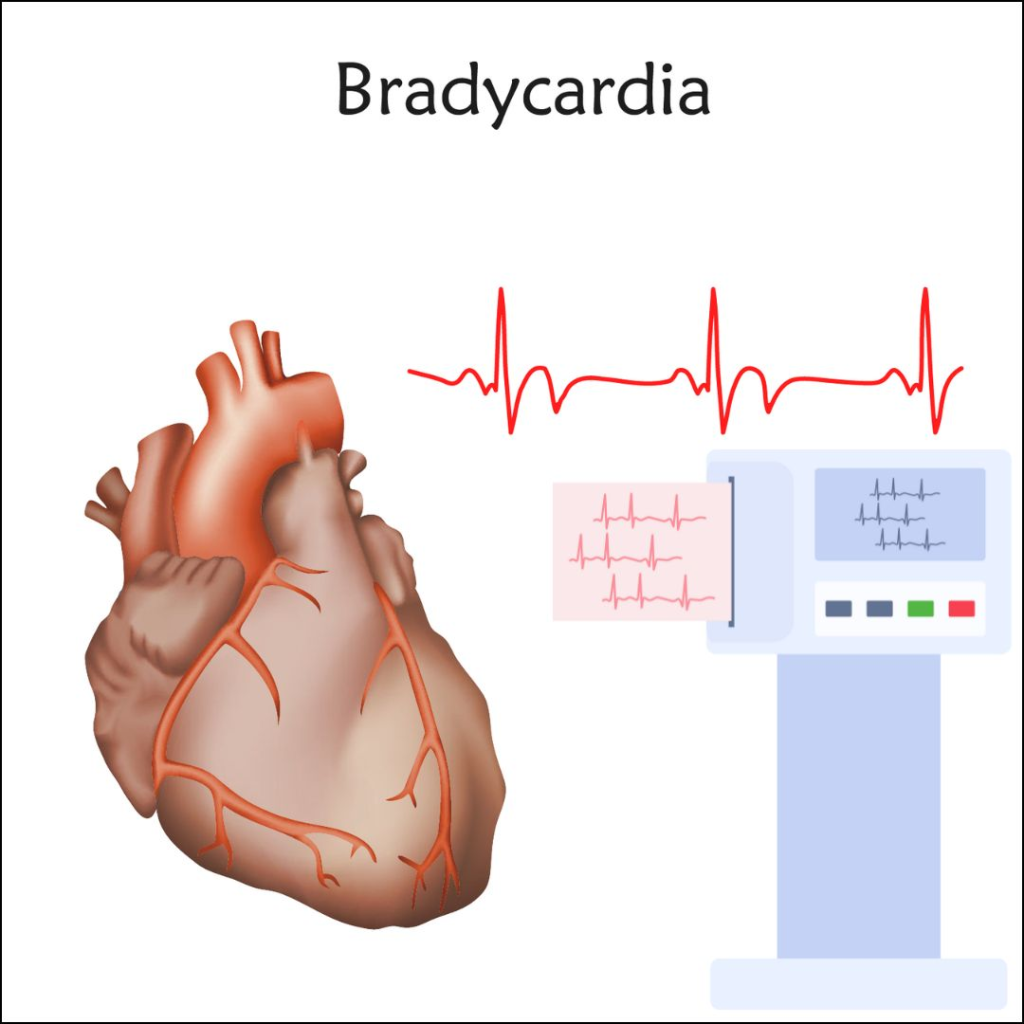
This condition is characterized by a slow heart rate. In adults, the heart rate is usually less than 60 bpm. This condition is called bradycardia. In this case, atropine is the first line of treatment. Which increases the heart rate in bradycardia.
Tachycardia (tachycardia) :
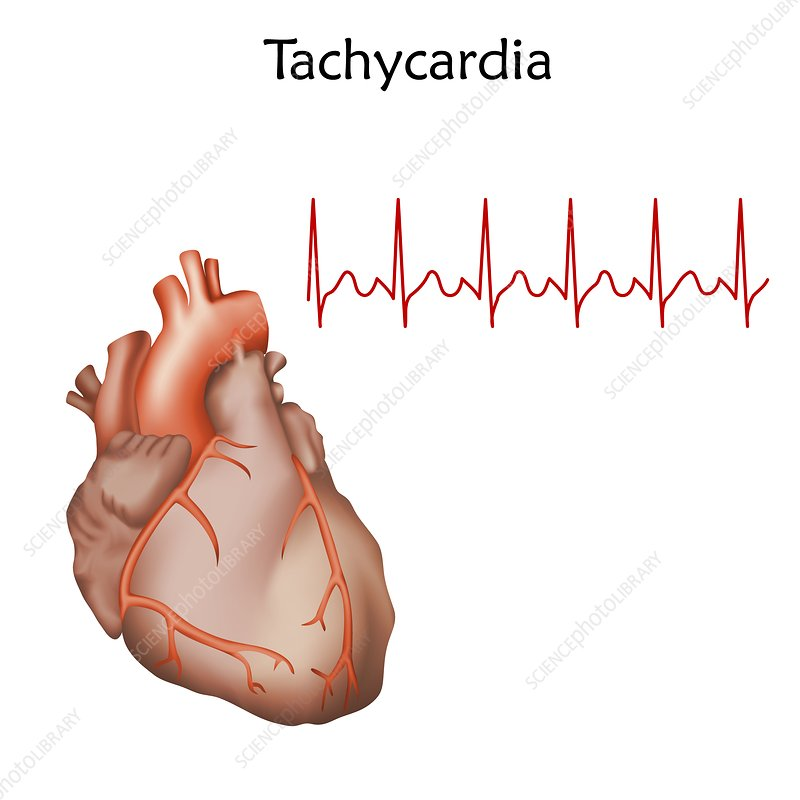
This condition is characterized by an increase in heart rate. In adults, the heart rate increases mainly by 100 bpm. This condition is called tachycardia.
Bradypnia:
This condition is characterized by an abnormally slow breathing rate. In which less than 12 respirations are observed.
Tachypnia:
This condition is characterized by an abnormal increase in breathing rate, with more than 24 respirations.
Disease:

The health of the body in this condition Disturbance is seen in the performance of vital functions. A disturbance in the function or structure of any organ or body part is called a disease.
Health:

According to WHO, “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
Illness:

Illness means illness. A person is unable to maintain physical and emotional balance. Which later causes disturbance in his ability to function is called illness.
kussmaul breathing (Kussmaul breathing):
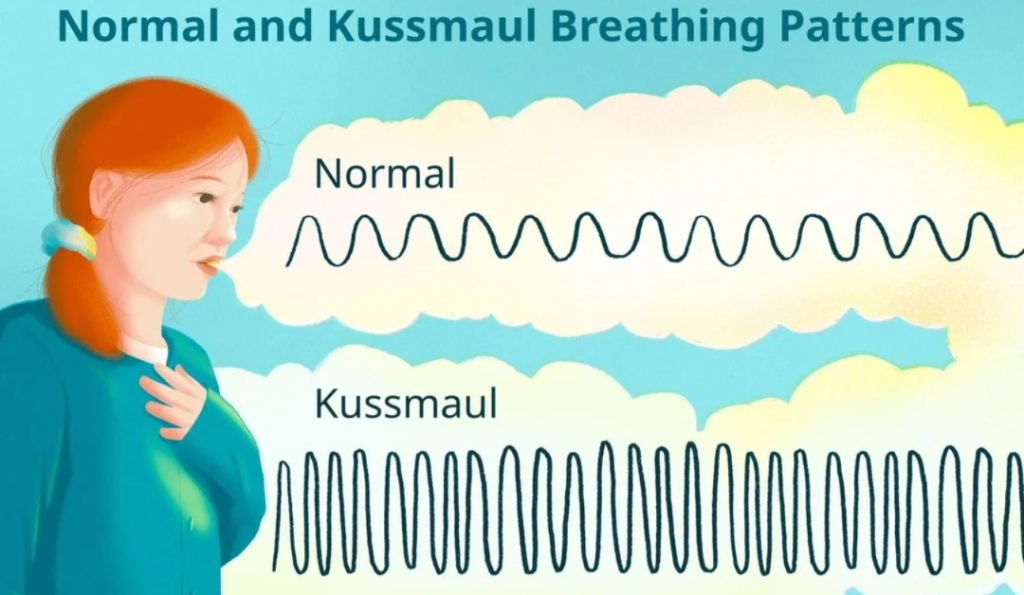
This is a type of abnormal respiration. In which an abnormal breathing pattern is seen. Rapid and deep breathing is seen. This is a sign of a medical emergency. In complications of diabetes and This condition is more common with coma.
Pursed lip breathing:
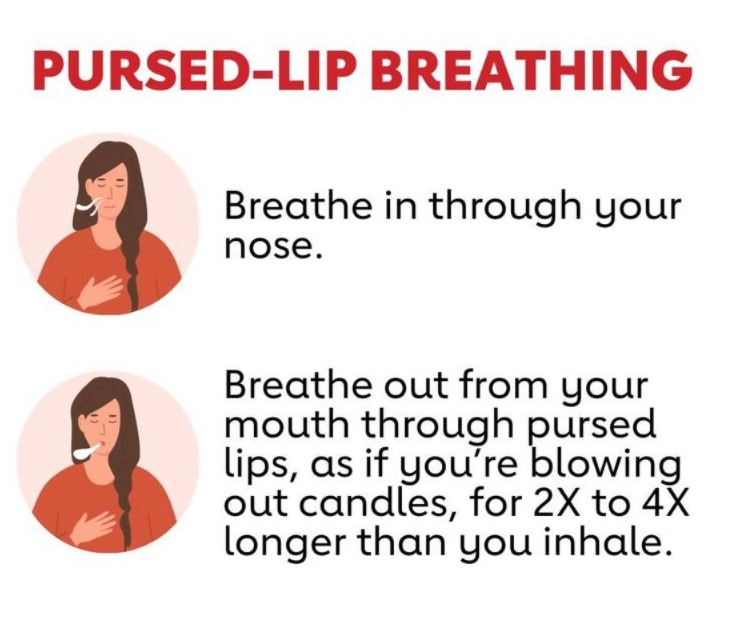
This is a breathing pattern in which the lips are partially closed. So that the air is exhaled slowly. It is used in patients with chronic obstructive pulmonary disease. In which the breath is taken in through the nose and exhaled through the mouth. This type of breathing provides relief in their breathing difficulty.
Terminal Illness (Terminal Illness) :

This infection or disease is an end-stage disease that is not treatable and can lead to death. This term is most commonly used in patients with cancer and chronic kidney or heart disease, etc., which cannot be cured and can lead to death. Such an illness is called a terminal illness. is.
Introduction:
- Different people have different perceptions of health. Some feel that a person is healthy when he is free from any disease or illness. While others believe that a person is healthy if he is capable of performing regular life activities.
- Health is a state of being strong in body, mind or spirit. Especially the absence of physical disease or pain.
- Health is a way of life. Which requires a desire to maintain healthy habits, including body functions and how to stay fit and healthy habits, including food and exercise. Health is a positive state of well-being when experienced physically, socially and spiritually.
Health Assessment :

- It is the continuous and systematic collection of patient data in accordance with standard guidelines. It includes the patient’s perceived needs, health problem-related experiences, values, and lifestyle. Includes health history and physical assessment.
According to the American Nurses Association:
- “Assessment is a systematic, dynamic process by which the nurse collects and analyzes data about the patient through interaction with significant others and health care providers.
- Health assessment takes a health history Then there is a physical exam and assessment of the health status, which is done to detect diseases early in people who can see or feel them.
- A health assessment is a plan of care that identifies the patient’s needs and how those needs will be addressed by the health or skill nursing facility.
- Nursing Assessment is the collection of information about the patient’s physical condition. Information related to the psychological, social and spiritual condition is included in it.
In simple words, a health assessment collects data about the patient’s health status. It is a detailed study of the body to determine the general or mental condition of the body. - Assessment = Observation of the patient + Interview of the patient’s family and significant others + Examination of the patient + Review of medical records.
Purposes of Health Assessment :
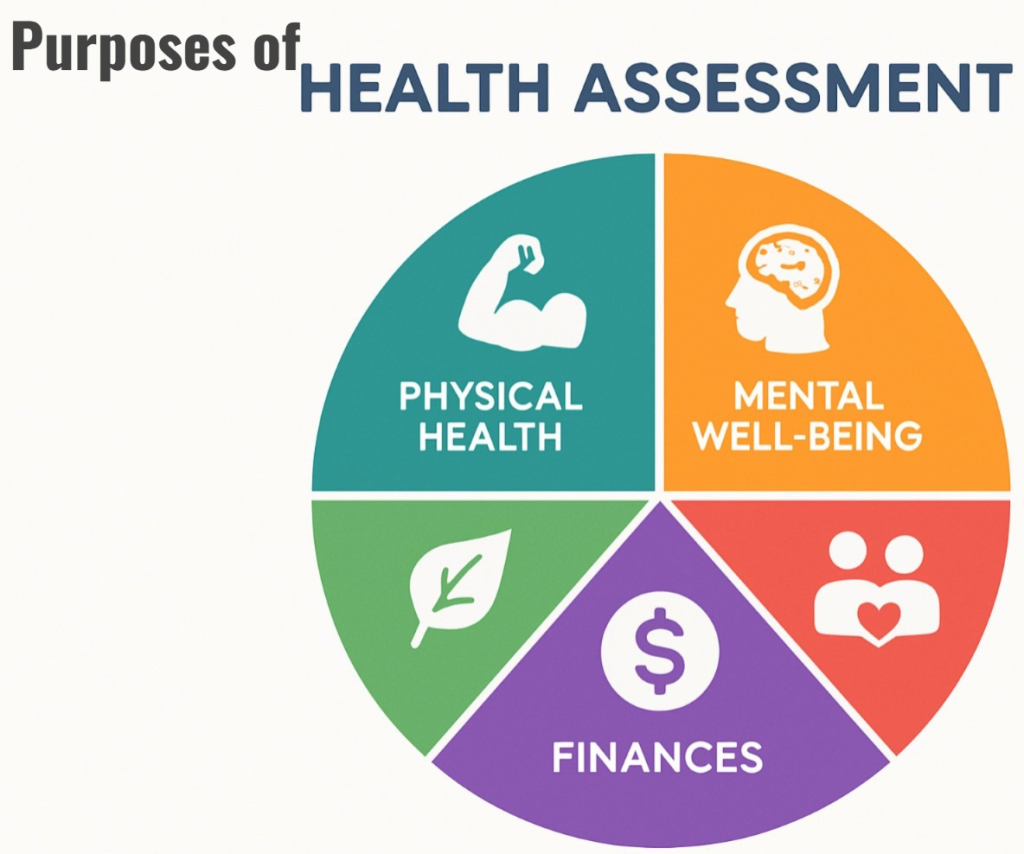
- To collect data about the patient’s physical, mental and social well-being.
- To identify the patient’s problem in the early stages.
- To determine the cause and extent (level) of the disease.
- To monitor changes in the patient’s health status.
- To determine the patient’s needs, nature of treatment, etc. For.
- To eliminate complications.
- To certify whether the patient is medically fit to resume duties.
- To contribute to medical research.
- To collect data systematically.
- To identify the patient’s strengths, weaknesses, knowledge, inspiration, support system, and coping ability.
- To compare the patient’s health status with the ideal state, including his age, ethnicity, culture, physical, psychological, and socioeconomic status.
Process of Health Assessment:
1. Health history (History of Health)
2.Physical Examination (Physical Examination).
1.Health history:
- Nursing Health History is a structured interview designed to collect specific data and obtain a detailed health record of the patient during the assessment phase.
- Health history is a collection of subjective data. Which includes information on both the patient’s past and current health status.
- Data Collection The primary focus of the interview is the health history. The health history is a review of the patient’s health pattern prior to the current contact with the health care agency. While the medical history focuses on the symptoms and progression of the disease, the nursing health history focuses on the patient’s response to changes in the health pattern.
- Health history records can be complete or focused. A complete health history includes biographical data, religion, current health status, past health status, detailed review of family history system, and psychological profile.
- Focus Health History focuses on the acute problem, so all your questions will be related to that problem.
Component of Health History:
1. Complete Health History:
Biographical data, reason for care, past health history, family history, review of systems, psychosocial profile, developmental considerations, current health status and analysis of symptoms
2. Focus Health History:
Biographical data, reason for care, past health history,
Family history only family history as it is related to the reason for specific care.
Psychosocial profile as it is related to the reason for specific care.
Developmental considerations as they will affect the acute problem
Ethnic considerations as they will affect the acute problem
Analysis of current health status and symptoms only related to the specific reason for seeking care.
Objectives of Health History:
To provide a subjective data base.
To identify the patient’s strengths.
To identify the patient’s health problems, both actual and potential, etc.
To identify the educational needs.
Identifying discharge need, identifying referral need.
Factors affecting subjective data collection:
Physical setting
Patient responsibility and his/her Behavior.
Communication skills.
Problems
Responsibility and behavior of a nurse
Nurses’ knowledge and skills.
Components of Nursing Health History
Biographic data
of health care Cause
History of present illness
Past health history
Family history
System review
Lifestyle
Sociocultural history
Psychosocial History
Occupational and Environmental History
Biographic Data:
Data is collected from the patient only when the nurse first talks to him/her. This information, which includes name, address, age, date of birth, gender, religion, bed number, ward, medical diagnosis, surgery, occupation, education, and type of health plan, can be useful in helping to understand the patient’s health.
Cause of Health Care:
- It is a brief statement of the patient’s problem. For which the patient seeks medical care. It is the primary reason why the patient is admitted or ill. The patient’s reason for seeking medical care should be described in the patient’s own words. The patient’s perspective is important. Because it explains what is important about the event from the patient’s point of view, it is necessary to determine the time of onset of symptoms as well as the complete symptom analysis.
- The patient’s statement should be written if there are many problems to indicate the priority of the patient’s complaint. Avoid using medical terminology. For example, the patient has had general weakness for a month, cough for two weeks, and fever for two days, and headache today. Headache × complains for one day.
Chief Complaint Fever × two days. Cough × 14 days and General Weakness × 30 days.
History of Present Illness :
- It includes Chief Complaint. It includes location, quality, quantity, setting, etc.
- Location is the area of the head where the headache occurs.
Quality is the gradual or sudden onset. Is the pain stabbing, dull, throbbing, and aching? Is the pain intermittent or constant? - Content Amount of fever Degree of pain using a pain scale.
- Chronology
When the symptoms started How often do they occur? - Setting Where were you when the symptoms appeared (e.g. home, hospital, job, etc.) Ask about associated factors (e.g. stress, fatigue, smoking, smoke inhalation) Factors that may cause the symptoms.
- Associated symptoms Are these symptoms similar to other parts of the body? Affects parts. The pattern of appetite and sleep is weakened. There is pain in the body.
- Exacerbating factors Are the occurrence of symptoms linked to activities such as smoking, talking loudly, eating, climbing, and changing body positions.
- Relieving factors How symptoms are reduced, i.e. meditation, rest, eating home remedies, and taking medications, etc.
- Past health history is information about a patient’s experience with any disease or surgery. It is very important to collect this information. It is an assessment of the patient’s health before the present illness because the previous illness may be related to the present illness. Which includes past health history.
- Ask the patient if he is suffering from any medical disease such as TB, anemia, stroke, hypertension, asthma, heart disease, glaucoma, etc.
- If the patient has this disease, ask him to what extent it affects his daily living activities. Is.
- To know the history of any previous surgery of the patient such as knee replacement, hysterectomy, valve replacement etc. To get complete information about the patient’s response to the surgery.
- Take note of the patient’s health history of any medicine, food or environmental allergies, including the name of the allergen, what type of reaction, and the substance.
Past health history:
Medical Disease:
Surgery :
Allergies:
Hospitalization:
- Ask if the patient has been hospitalized before, if so, why and for how long.
Injury or trauma:
- Ask the patient about the history of fractures, burns, changes in level of consciousness, abdominal trauma, etc.
Childhood illness or immunization:
- Whether the patient has received vaccines such as tetanus, hepatitis, diphtheria, measles, rubella, polio, etc.
Family history:
- Knowing if anyone in the family has a serious illness which can be acute or chronic.
- First of all in health, collect blood related and child related information because genetic and environmental factors are linked to diseases. Family health is very important.
- For example: Hypertension, Anemia, Diabetes, Mental Illnesses, Cancer, Seizures, Kidney Diseases etc. and write the health history of all family members and if all are alive then their age and gender.
Which is represented by a family tree.
Male: circle
Female: square box
Patient: indicate by arrow.
Lifestyle:
- Daily living activities, entertainment, hobbies, personal Habits etc. are included.
- Daily Living Activities are descriptions of self-care. This database includes nutrition, rest, sleep, and exercise.
Psychosocial History:
- This history includes the patient’s self-concept, self-esteem, sources of stress, and the patient’s capacity to cope.
In addition, when a crisis occurs, seek out sources of support such as family, religion, and support groups. - Ask the patient about their illness and whether it affects their sexual activity? This information should be collected last because by then the patient can be comfortable.
- The impact of the disease on their business, relationships with other people, the cause of AIDS can be identified from this.
- Psychosocial history includes obtaining information about the patient’s awareness about himself or his relationship with other humans, etc.
- The focus of obtaining information is the patient’s education, lifestyle, personal relationships, social relationships, marriage, school, siblings, etc.
Socio-cultural history:
- Inquiring about the socio-cultural history of the home environment, family situation, and the patient’s role in the family, etc., is essential.
- For example, a single parent may be the sole provider of a family of three children. Patient responsibility is essential so that the nurse can determine the impact of changes in his or her health status and plan for the most beneficial.
Occupational and Environmental History:
- The goal of collecting this history is to identify the critical factors in the environment or the substances that cause the disease.
- In which the patient’s occupation, job, life Style, environment etc. related information is collected.
- In which farms, factories, yards, heavy material, etc. can spread communicable diseases.
Physical Examination:
- The goal of a physical examination is similar to taking a health history.
A physical examination is an important part of a health assessment.
It provides objective data to diagnose and identify problems. - The goal of a physical examination is to assess any deviations from normal is. And to validate the information collected through interviews.
Measurement of baseline data and physical techniques are used to collect objective data. - Physical examination is included in nursing assessment. Signs and their measurement or observation are done. In which the patient experiences dizziness and vertigo.
- Techniques such as inspection, palpation, percussion, auscultation etc. can be used in physical examination.
What is baseline data? (What is baseline data) ?:
- Baseline data is the systematic organization of assessments obtained during a physical examination.
- A given point in time that forms the basis for comparison and evaluation to establish the patient’s condition. Height and weight are important for comparison with future measurements so that any changes can be identified.
Technique of Physical Assessment:
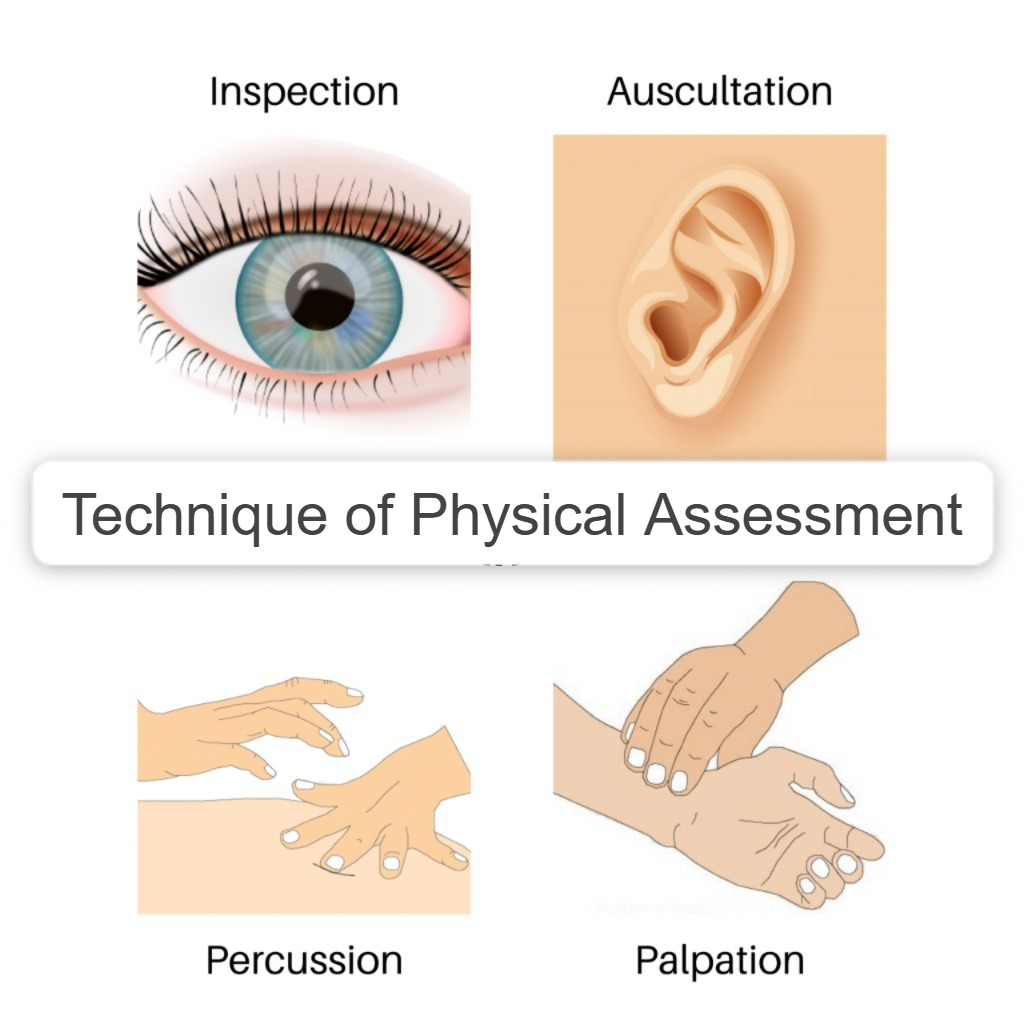
- Physical examination uses systemic assessment techniques and visual, auditory, tactile, and all-factorial senses. All of these senses will be used in specific assessment techniques.
- For example, it is often detected by changes in body odor and fluids.
Four specific techniques are used in physical examination. Including inspection, palpation, percussion, and auscultation.
1.Inspection:
- Inspection is a visual examination of the patient. And a visual examination of the body. In which the patient’s general appearance, body size, gait, height, shape, posture, etc. are carefully observed. This begins as soon as the nurse makes contact with the patient.
- During the inspection phase of the physical assessment, the nurse uses observation skills to systematically collect observable data.
This includes measuring the patient’s respiratory effort, skin color, and wound.
General Appearance:
- Expression: Concerned, Comfortable, alert, nervous.
- Body build: Thin, Fatty, Moderate.
- The patient’s words are also combined with body language.
For example, the patient’s pain experience is related to his body language. - Visualize the maximum area of the body during inspection and then compare it with the side of the other body.
- Compare the width of the right hand with the width of the left hand To do.
Adequate exposure of the body area is very important. In which color, texture, mobility, symmetry, nutritional status etc. should be observed.
2. Palpation:
- Palpation is the use of the hands and fingers to feel the texture, size, shape, placement, location, etc. of an organ. In which, specifically using the finger tips of the hand, assess the temperature, pulse, texture, moisture, mass, tenderness, and pain of the skin.
- Press 1 cm deep and gently palpate the skin, pulse, palpation, and tenderness.
- Then press 4 cm with both hands, which is deep palpation. With its help, determine the size of the organ and the deep organ (liver).
What to keep in mind when performing palpation? (What to keep in mind when performing palpation?):
- It is always very important to explain to the patient before performing palpation because touch is very important in our culture.
- Keep hands warm and nails short before performing palpation. The palmar surface of the finger is more sensitive than the finger tips, with the ulnar surface being more sensitive to vibration, and the dorsal surface being used for temperature.
- Palpation also helps in determining the size of the lymph node.
- Always proceed with gentle palpation first, then deep palpation. Because it can cause tenderness or fluid disruption.
- Using both hands, the size and shape of the kidneys and uterus are assessed between the finger tips and the organ.
Percussion:

- In simple words, it is called tapping. To get the quality of sound, sound is heard against the patient’s body by tapping with a finger. Which is used to reflect the density of the internal organ. Sound, vibration, and impedance which are produced with different densities. And it varies from organ to organ. And it is used to determine the size, shape, position, and also to detect fluid field organs.
- Percussion is a technique that physicians and nurses use to determine the consistency of tissue.
Percussion involves tapping on the body surface with short or sharp strokes to produce various palpable vibration sounds. - Percussion is used to detect the sound, location, size, shape, and size of many organs of the body. In which the examiner taps on the patient. To produce sound, the middle finger of the non-dominant hand is usually placed on the percussion area. And keep the middle finger of the dominant hand on the non-dominant.
- In which percussion is done in two ways.
Direct percussion:
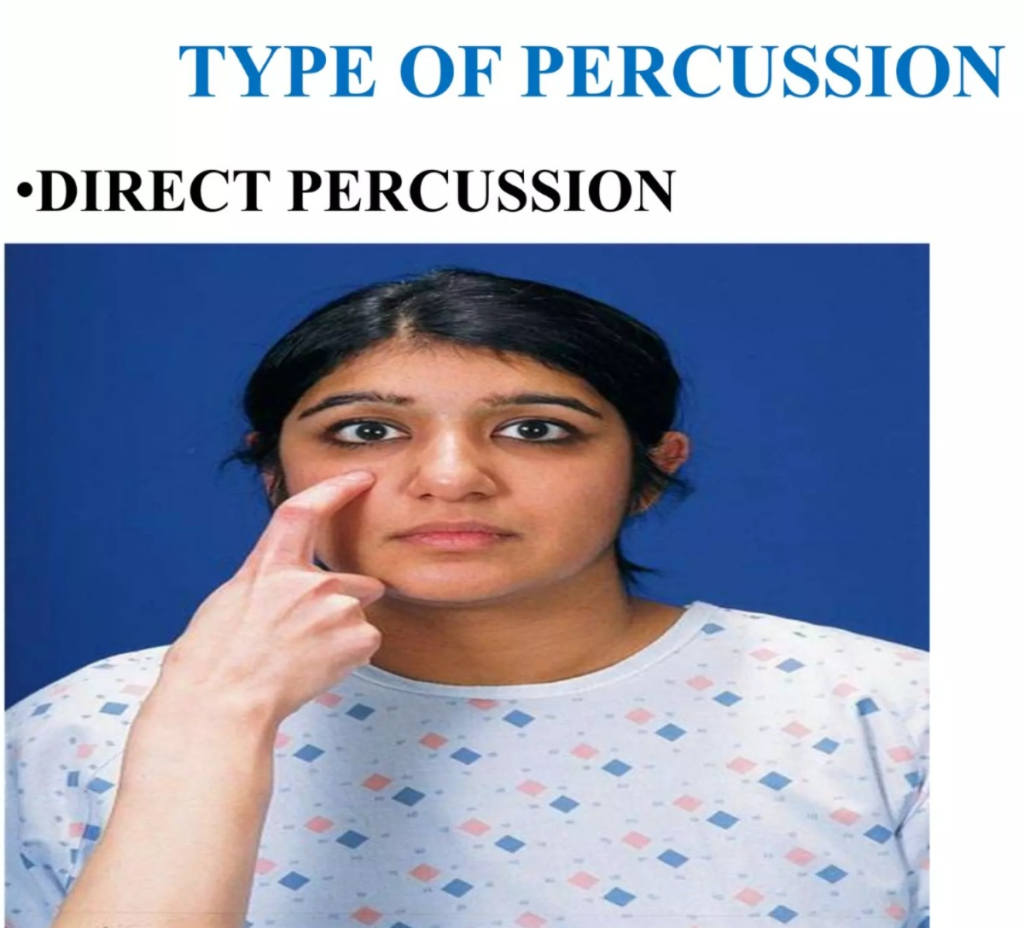
- This is used for the chest of infants and sinuses of adults. Tapping is done on specific parts of the body with the help of finger tips.
- In kidney tenderness. To listen to the vibrations created.
It is necessary to percuss two or three times on the same point before doing it on another. This is done to get an accurate reading. Strong percussion is required for fatty patients. - Percussion tones: Air (loud), fluid (dull) and solid area (soft).
Indirect percussion:
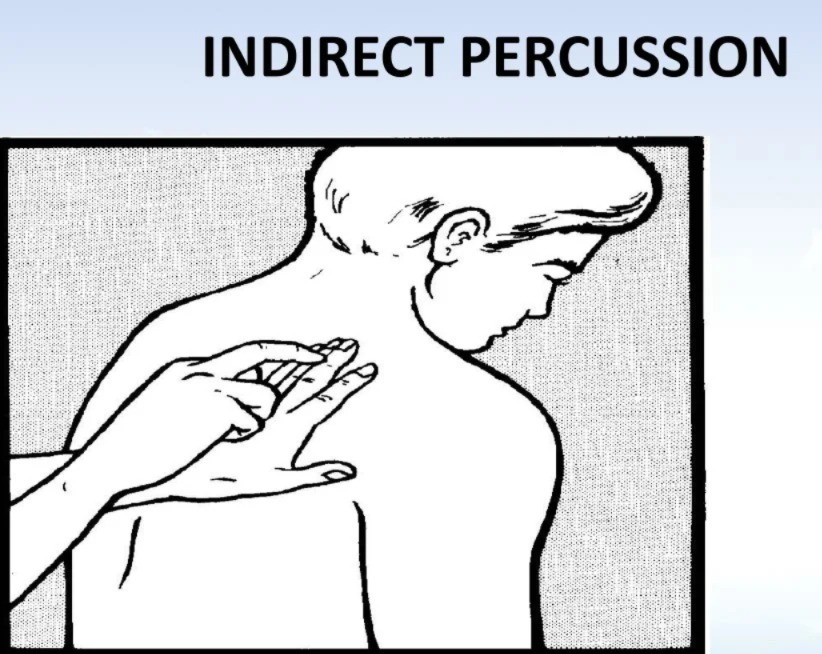
- This varies depending on the area, with the non-dominant hand palm down, fingers interlocked on the CVA and the dominant hand finger gently struck, e.g. T.. In the kidney….
_Thorax: The middle finger of the dominant hand strikes the interphalangeal joint of the non-dominant hand which is against the patient’s skin. - Percussion produces a sound which has many sounds and different characteristics.
Characteristics of sound:
- Tympanic (Tympany) It is usually heard over the abdomen.
- Resonance in normal lung tissue.
- Hyper resonance in inflated lungs.
- Dullness over the lungs.
- Flatness over the muscles.
Auscultation:
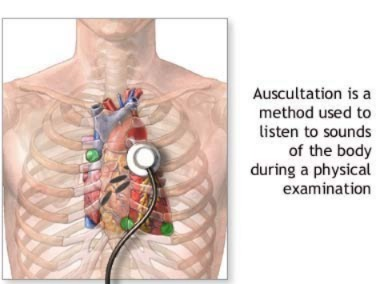
- Auscultation is usually performed with a stethoscope. A stethoscope is used to block out extraneous sounds while assessing the condition of the heart, blood vessels, lungs, pleura, and intestines.
- These include breath sounds, heart, vascular sounds, and bowel sounds.
- It is commonly used to detect the presence of abdominal sounds and assess their loudness, pitch, quality, frequency, and duration.
- The most common sounds heard include the heart, lungs, abdomen, and blood vessels. is.
- The chest is auscultated to hear heart sounds. Lung sounds are auscultated anteriorly and posteriorly for normal and abnormal lung sounds. The abdomen is auscultated for bowel sounds.
Characteristics of sound: ?
- Intensity: Loud, Medium, Soft.
- Pitch: Low, High, Medium.
- Duration: Short, long, medium.
- Quality: booming, hollow, dull and drum-like.
What is the order of physical examination? (Sequence of physical examination?) :
- Inspection
- Palpation (palpation)
- Purcussion (Percussion)
- Auscultation
Patient preparation :

Physical Preparation :
- Assist the patient in sitting or assuming a position during the examination. Assist the patient in removing clothing as needed.
- Emptying the patient’s bladder relaxes the patient and increases easy palpation of the abdomen and pubic area. If urine test is required, collect urine in a urine container. If fasting is required, prepare the patient.
Psychological Preparation:
- When a patient is admitted to the hospital, he becomes worried and anxious and he is troubled by any problem.
- It is very important to know or understand the psychology of the patient
- To justify his questions.
- Explaining the procedure to the patient and the purpose of the examination is included in his psychological preparation.
- Making the patient relaxed and comfortable.
- Telling the patient the order of the examination.
Before starting the physical examination of the patient, it is necessary to prepare the unit to make the patient relaxed and comfortable. For which the following points should be taken into account.
- The time of the examination should be convenient for both the patient and the nurse because some important information is missed if done quickly.
- Light is necessary for the examination, so there should be light throughout the examination.
- Equipment: All equipment should be close by and in working condition before the examination. The patient should be able to sit or lie comfortably on a table or chair.
- Privacy: Privacy is an important part of the examination. When the doctor is examining the female, do not leave her alone. Always stay together because body exposure can be embarrassing.
- Temperature: The temperature in the room where the physical examination is performed should not be too hot or too cold. Provide a warm environment.
- Position: Many positions are used in physical examination, so there should be furniture so that the patient can take a comfortable position.
- Draping: Draping means covering the area near the exposure. Draping maintains privacy and prevents unnecessary heat loss.
General Assessment:
- Assessments can be comprehensive and focused. A comprehensive assessment is an initial assessment. Which is very sufficient and includes a detailed history and physical examination.
Skin (स्कीन) :
Ask about skin rashes, itching, dryness, oily skin, skin color changes, and changes in moles, etc.
Skin inspection:
- Color:Check the general skin color and check for uniformity.
- Pigmentation:Normal, hyperpigmentation, Hypopigmentation
- Moles: Excessive/normal sudden enlargement and irregular border of the mole. Changes in color: Itching, tenderness, pain, building up in the mole, changes in the surface of the mole.
- Vascularity: Abnormality: petechial, ecchymosis, purpura.
- Color: Pink, red, yellow, brown, black, green.
- Lesion: Types of lesions: macule, papule, scale, ulcer, and scar.
- Pattern: Annular, linear, clustered bull’s eye.
- Body area: Generalized, exposed areas, skin folds in the face, etc.
Palpation of the skin:
- Temperature – Normal, hyperthermia, hypothermia.
- Texture:Normal skin, soft, intake, minimal sweating, redness, scars, rough spots.
- Mobility:Normally, the skin moves easily when lifted and returns to its place immediately when released.
- Check for tenderness.
- Turgor: Mobility and moisture of the skin, if there is dehydration So poor turgor.
Nails:

- Inspection and palpation of the nail, checking the angle of the nail.
- Shape : Rounded, flat
- Texture : Smooth
- Color : Pinkish white.
- Thickness : Uniform
- Palpating the nail base. For the cleanliness and strength of nails.
Head inspection and palpation:
- Note size, shape, symmetry inspection, texture.
Listen to skin, palpate for any mass in the head, tenderness, swelling, and texture of hair.
Normally the head is non-cephalic. Skull is symmetrical and appropriate for body size. - Hair: Color texture quantity and distribution.
- Face: Facial expression: Depression, anxiety, anger, disgust. Facial Movement: Excessive blinking, continuous smiling.
- Facial Cementity: Puffy, sunken areas, trembling. Skin Color, Temperature and Pigmentation
Texture: Lissance in AD
Eye and Vision:
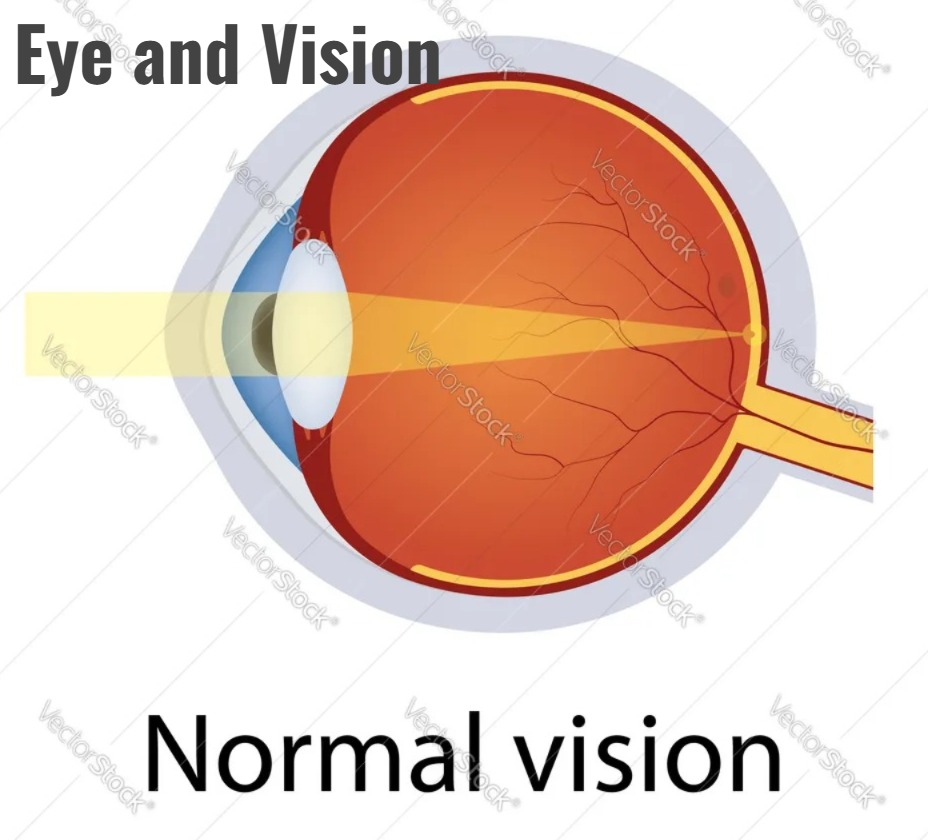
- Margin of the eye lid: Inspect for presence of secretion, redness, position of lacrimal glands.
- Lacrimal glands: Turned outward and distributed.
Conjunctiva: Check color (pink) Sclera: Check color (white)
Pupil: Check size, shape, symmetry, reaction to light. - Cornea: Normal (transparent).
- Vision: Check distance vision using Snellen or ‘E’ chart. Check near vision using Rosen Pom chart or cord with newsprint held 12 to 14 inches from the patient’s eyes.
- Eye Movement: Evaluate the main field of vision to obtain information about the movement within the eye. Ask the patient to follow your finger while drawing the letter H or z in the air.
- Corneal reflex: Gently touch the patient’s cornea with a cotton swab, causing the eye to blink.
NECK:
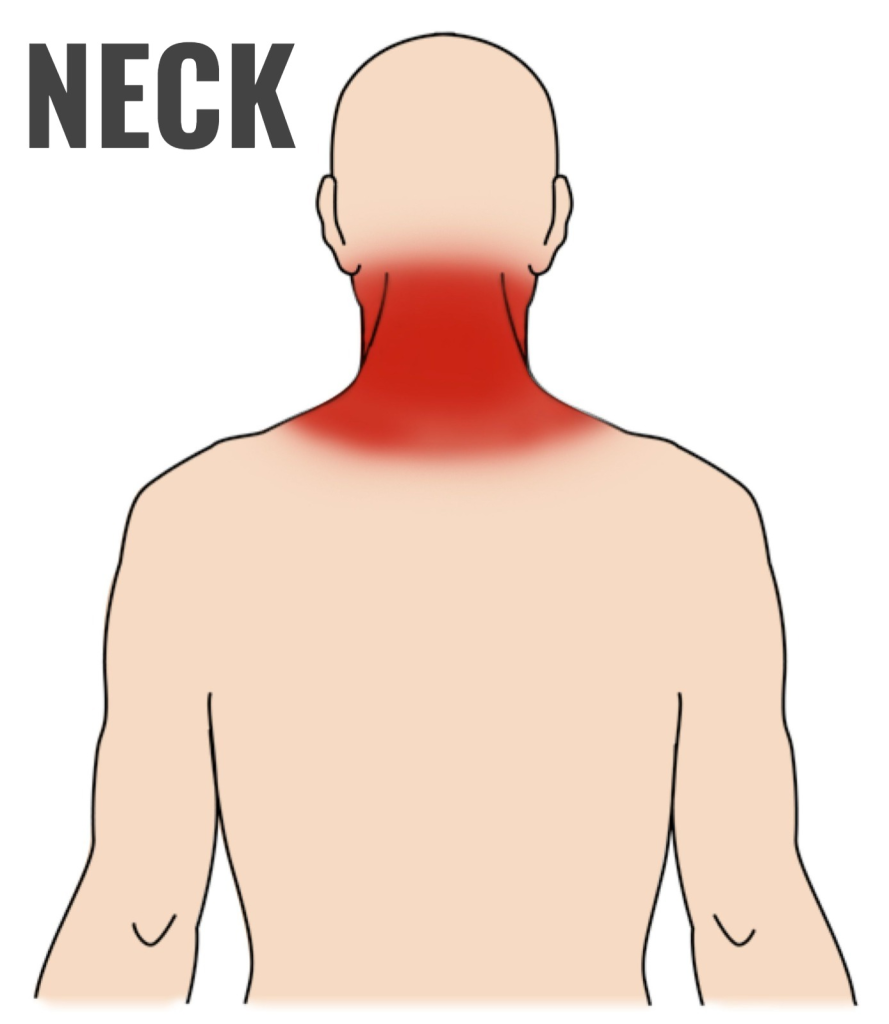
- Size and symmetry: Symmetrical
- Range of motion: Back, side to side. Position of the trachea
- Thyroid gland: Enlarged or non-enlarged.
Palpation:
1) Palpate the neck area for cervical nodes.
2) Distension of the jugular vein.
3) Tracheal ring, and cricoid cartilage, and thyroid cartilage.
4) Palpate the neck for carotid pulse.
Abnormal Finding:
- Tenderness and non-midline position.
- Lymphnode: Inspect superficial lymph node. In ED, palpate for redness, node size, mobility, border tenderness, and warmth.
- Position of the trachea: It is usually found on the midline.
- To check it, place the index finger on the suprasternal notch. Then slide it to the right and left so that both sides can be noted. Normally, the space between the trachea and the sternocleidomastoid muscles is the same on both sides.
Palpation of the lymph node (lymph node) Palpation):
- Assess all nodes.
Particular nodes: Use both hands on each side to compare findings. Submental nodes can be palpated well with one hand. - Supraclavicular nodes: Examine the patient with the shoulder forward and towards the flexed chain. This makes the node more accessible. Place the finger in the medial supraclavicular fossa and place it deep in the clavicle and in the sternocleidomastoid muscles. Ask the patient to take a deep breath while pressing deeply. Behind the clavicle because enlarged supraclavicular node can be easily felt during inspiration.
- Abnormality: Enlarged submental node, seen in facial acne.
- Enlarged supraclavicular node: Thoracic over abdominal pathology such as carcinoma, lymphoma, TB, and AIDS etc.
- Axillary node.
- Support the patient’s arm with your hand. Flex his elbow and place your forearm on his arm.
- Keep the palm of the examining hand flat in the axilla. Cup the fingers of the hand while examining the hand to insert it high into the axilla.
- When palpating the finger, the soft tissue will roll between the fingers. Rotate the fingers and palm and feel the node. Palpate the anterior, posterior, and lateral areas of the axilla.
Enlarge Lymphnode:
- Lymph drainage from the breast or systemic disorders such as Hodgkin’s disease, infection of the hand or finger, breast cancer, systemic syphilis.
Palpation of the node on the arm:
- Flex the patient’s arm 90 degrees.
Palpate the back of the elbow from the medical condyle of the humerus down. - Enlarged node: Ulcerative infection in the forearm in four to five fingers.
Groin region: Inguinal nodes in which,
Provide supine position to the patient. Palpate the inguinal ligament only on the inner aspect in the groin area using the finger pads.
This node is small, smooth, soft and mobile. - Enlarged, tender, warm, freely movable node: seen in inflammation.
Nose and paranasal sinuses:
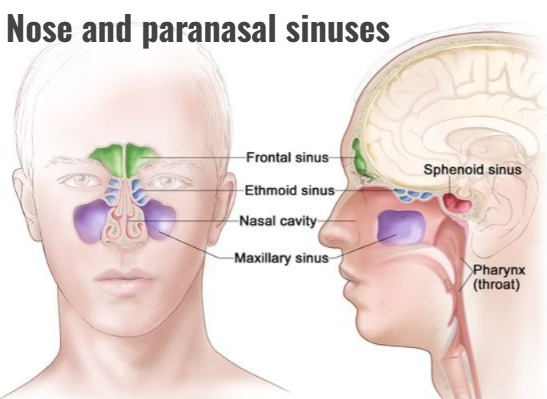
- Including inspection and palpation..
General appearance: Symmetric, midline symmetry If discharge present: Characteristic amount of discharge.
Paranasal sinuses: Whether there is swelling tenderness. - Nostrils: Dry, symmetrical, nose flaring
Internal nasal cavity: Patent or not patented.
Mouth (mouth) :

- Palpation of temporomandibular joint: tenderness and discomfort.
Note its odor on respiration. - Normal: No odor or slightly sweet.
Abnormal: Acetone odor is present if diabetic ketoacidosis is present. - Foul odor: If there is disease, poor dental care and inflammation in the sinuses.
Lips:

- Color: Pink normal or blue (respiratory or cardiac problem)
- Pallor: Anemia or shock
- Symmetry: Both vertically and laterally symmetrical.
- Moisture: Smooth and moist
- Check for the presence of crusts and lesions.
Teeth Teeth:

- Alignment: Protrude and number of teeth. Color: White ,yellow, gray, dark color in medication or caffeine intake.
- Surface: Smooth
- Check the teeth for caries, missing teeth, debris, etc.
- Palp the teeth for tooth stability.
Buccal Mucosa:

- Color: Pink and pale color with slight vascularity. Check for the presence of patches, ulcers, masses, etc.
Tongue inspection:

- Movement: Smooth and symmetrical.
Color: Pink moist. - Check for ulceration. Surface: Variation in swelling size.
Abnormal Finding:
- Atrophy of the tongue division on one side of the tongue is seen in neurological problems.
Small tongue: Malnutrition - Enlarged tongue: Mental retardation, acromegaly, hypothyroidism.
Smooth, red and swollen tongue: Vitamin B12 deficiency. - Patients with dentin: tenderness, lesions, and thickening of the gums. Fitting of dentures.
Palpation Of Tongue:
- Smoothness and Irregularity
- uvula and palate
- Inspection:
- Texture: Smooth, Immu Webelpalate
- Color: Pale Palate, and Soft Palate: Pink Surface Characteristics: Soft Palate failure and uvula deviation in use which is reflected in neurological problems.
- E.g. paralysis of the vagus nerve.
Pharynx :
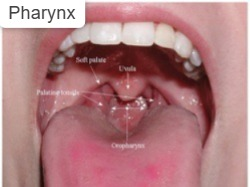
- Inspection of the fairings and posterior wall for any inflammation.
Ear:
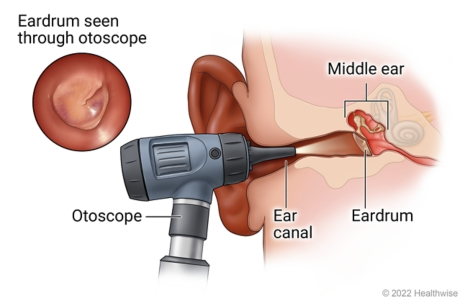
- Inspection of both ears
Alignment: Normal - Head position: Relation of eye size and outer canthus of septum normal.
Skin color: Blue: Cyanosis, Red: Full sing, pallor, frostbite.
Inspection:
- Pina: Inspection of size, shape, color, lesions, and mass.
External canal: Presence of discharge, mass of foreign body, and information. - Inspection of tympanic membrane.
Hearing assessment which involves two tests. - Weber Test:
Vibrate the tuning fork on the middle of the patient’s head. Then ask the patient if he hears the same in both ears or more in one ear than the other. - Rinnie Test:
Vibrate the tuning fork on the mastoid process and ask the patient when the sound is no longer heard. Then quickly reposition. Place the tuning fork on the front of the ear canal. Then ask the patient if he can hear the sound. When the sound is not heard, ask the patient to say it. Normally the patient will hear the sound twice for a long time through air conduction. such as by bone conduction.
Chest :
- Inspection
Breathing: Effortful, normal, or no effort. - Chest wall symmetry with anterior posterior angle: less than 90 degrees.
Barrel chest: costal angle greater than 90 degrees. - Breathing rate: normal, tachypnea, bradypnea, and apnea.
Breathing pattern: cello breathing or spontaneous.
Expansion of the chest.
Palpation:
- Chest wall: Pleural friction rub, crepitus.
Symmetry: Normal atelectasis reflex. - Asymmetry: Pneumonia, flail chest, pneumothorax.
Thoracic expansion
Curvature: Scoliosis and kyphosis. - Abnormal Findings: Increased fremitus, consolidation, lobar pneumonia, pleural effusion resulting in decreased normal lubrication.
Palpate the chest and check for tenderness, lumps, and any masses.
Percussion of the thorax:
- Tone: Resonance, hyper resonance, tympani
Intensity: Loud, soft, medium.
Pitch: Very low, low, or high pitch.
Duration Quality: Hollow ,Brumming
Percussion of heart border for heart size. - Auscultation (for breath sounds)
including broncho vesicular vesicular and bronchial, vocal sounds.
Heart:
- Inspect for cyanosis.
Palpate the pulse for regular or irregular rate.
Then palpate the apical pulse for location.
Duration: The apical pulse is located at the apex of the heart in the fifth intercostal space in an adult and the fourth intercostal space in a young child or infant. - Assessment of cardiac rate and rhythm
Auscultation of heart rate and rhythm The first heart sound is heard louder at the apex of the heart and the second heart sound is heard louder at the base of the heart. - Then identify additional heart sounds in both systole and diastole.
Heart sounds: s1,s2,s3,s4 and murmurs.
And also check the rate, rhythm, pitch, etc. in them.
Breast and axilla in females:
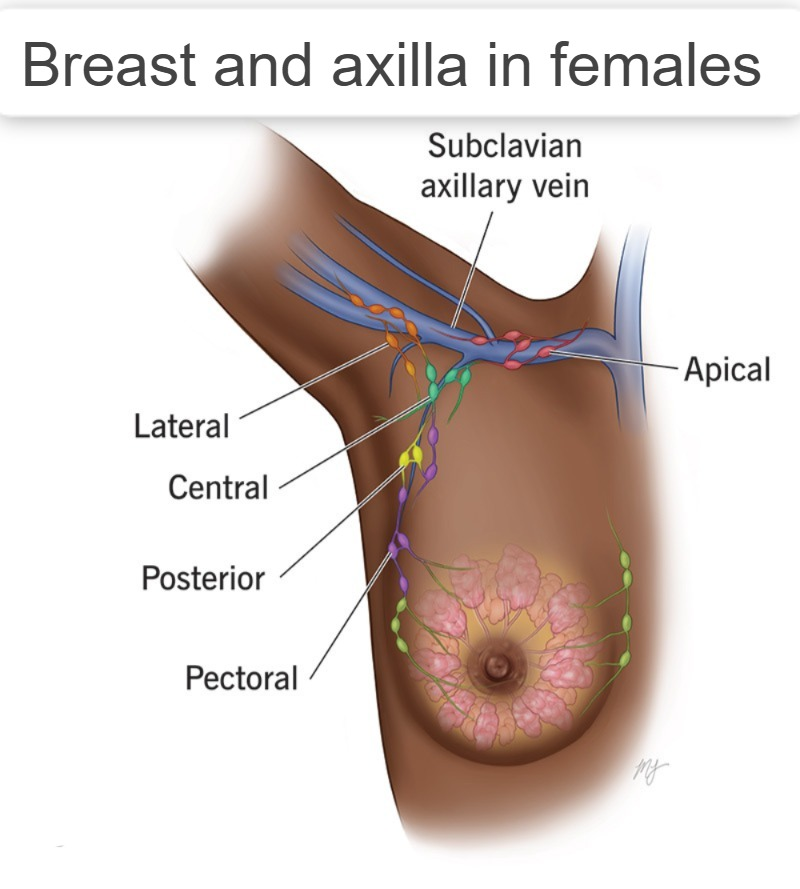
- Inspection
Breast size, shape, and cementation.
Skin of the breast: including appearance, color, pigmentation, vascularity, etc. - Areola: color and surface characteristics.
Nipple: including position, symmetry, discharge, bleeding, Lission, scaling, cracked nipples etc.
Axilla: Recess, Lission, Mass. - Palpation
Breast and axilla: including tenderness, nodules, and surface characteristics
Nipple: Discharge and surface characteristics.
Abdomen:
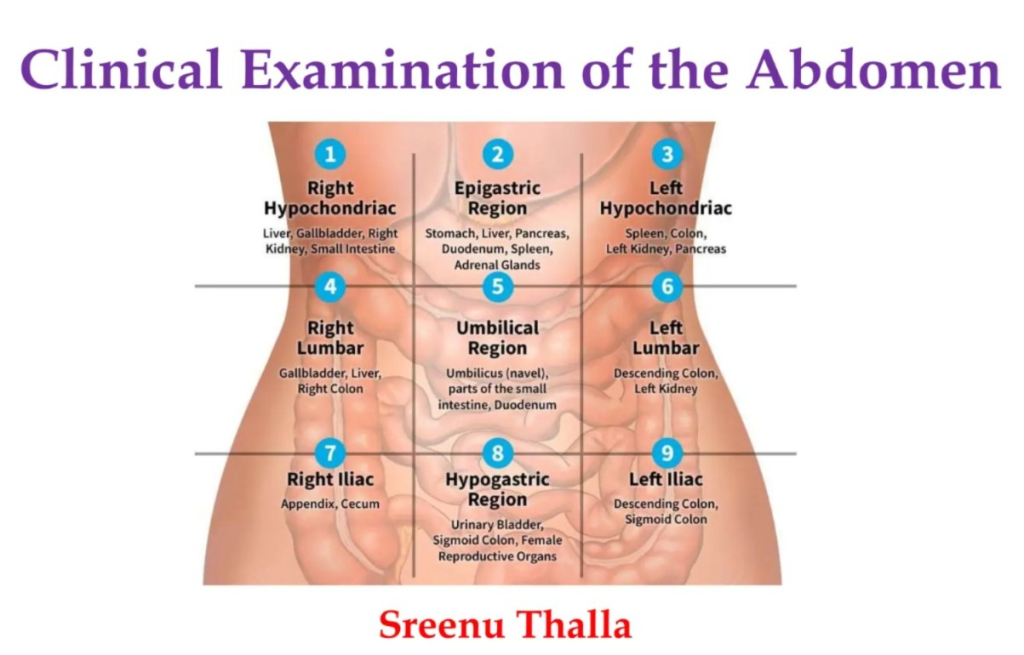
(A) Inspection:
- Skin color: redness, lichen, and discoloration. Cyanosis, rash pink purple or red.
Stryle: Abnormality. - Surface characteristics: Smooth
Umbelicus: Normally sunken contour with center. - Surface movement: Moves smoothly during respiration.
Abnormality: Peristalsis visible, grunting labored movement, restricted abdominal movement.
(b) Auscultation of Abdomen (Auscultation of the abdomen) :
- Bowel sound: High sound indicating diarrhea including use of laxatives and AGE.
Low sound: Inflammation, constipation - Vascular sound: Normally not hard.
‘Bruit’ which is an abnormal sound. - Which is heard in the aortic, renal, iliac and femoral arteries when the vessels become occluded.
(C) Percussion of Abdomen (Percussion of Abdomen):
- Tone, tympany, dullness
Liver: Enlarged liver: Cirrhosis and hepatitis. - Size of spill:
Stomach for tympany
Dullness: Liver
(D) Palpation of Abdomen:
- Tenderness: Present in peritoneal irritation.
Muscle tone: Relaxed
Surface characteristics: Smooth - Tenderness, mass, aortic, pulsation, local or general pain with deep palpation.
For a bulge around the umbilicus and the umbilical ring. - Liver and spleen: Border and tenderness
Normally the spleen is not palpable.
Palpation of the kidneys for tenderness at the costovertebral The angle is palpated. - Access the abdomen for abdominal reflexes. In which,
Fluid: shifting dullness, fluid wave
Pain: tenderness
Floating mass: two alloments.
Hip and Lower Limb:

(a) Inspection :
- For the strength of the patient’s feet and leg muscles.
Skin characteristics Hair distribution Superficial mass. - Vascularity and fracture.
Note any deformities in the toes, feet, nails, ankles and legs.
(b) Palpation of feet and lower legs
- Including temperature, pulse, tenderness, deformity, ED.
- Range of motion, Turgor Motor strength of both legs including toes, feet, ankles, knees, hips etc.
(Genitalia ):
- General inspection including lesions/scars.
- Discharge/Infection Voiding: Color of urine itself
Catheter or not.
Male:
- Any mass, hernia, Palpate the prostate gland for enlargement etc.
Female:
- Including discharge, swelling, redness, pelvic mass.
- Rectum: Inspection
- Patient, hemorrhoid, red Ness.
- Checking rectocele etc. in females.
Diagnostic Test (Diagnostic Test):

- x-ray : Study of the features present in it : e.g. Bone, Joint, Skull, Spine, Kidney, Uterus, Bladder.
- CT Scan
- MRI
- Positron Emission Magnetic Tomography: To determine the amount of blood flow in specific body tissues.
- Angiography: To assess blood flow using dye.
- Ultrasound
- Endoscopy: Direct visualization of body systems with a flexible tube equipped with a light.
Nutritional History:
- Know about nutritional status.
- Ask the patient about weight gain, loss, fatigue, etc.
- Ask about changes in skin color, texture, etc.
- Ask about night blindness and dryness in the eyes.
- Ask about constipation, diarrhea.
- Ask about heartburn, chest pain, abdominal discomfort, etc.
- Ask the patient about his eating habits, his method, eating time, etc. Ask about where they buy, food storage, cooking, etc.
- Ask about smoking/alcohol habits, if any illegal drugs are being taken.
- Ask about culture and religion.
- Ask about whether job timings affect eating habits, etc.
- Daily record of food intake etc.
General Clinical investigation:

- Microbiology: To detect microorganisms such as bacteria, viruses, fungi, and protozoa present in blood, urine, pus, body secretions, stool, pus, culture, etc.
Blood Study:

In which many types of investigations are done.
In which hematological blood analysis
- Hemoglobin: Male: 13 to 18 gm/dl , Female: 12 to 16 gm/dl
- Leukocyte count: Total 4500-11000 cumm
- Neutrophils: 45% to 73%
- Eosinophils: 0%-4%
- Basophil:0%-1%
- Lymphocyte: 20%-40%
- Monocyte: 2%-8%
- Platelet count: 150,000-450,000/cumm
- Hematocrit: male:42%-52% female:35%-47%
Coagulation Study (Coagulation Study):
- Potassium (k+): 3.5-5 meq/dl
Chloride (cl-): 97-107 meq/dl - Calcium (ca): 8.6-10.2 mg/dl
Amylase:111-296 u/L - Bilirubin: Total: 0.3-1.0 mg/dl ,
Direct bilirubin (conjugated): 0.0 to 0.3 mg/dl
Indirect bilirubin: (unconjugated):0.2 to 0.8 mg/dl - SGOT (Serum Glutamic Oxaloacetic Transaminase): male:10-40U/L
Female: 15-30 U/L
SGPT (Serum Glutamic Pyruvate Transaminase): male: 10-40U/L
Female: 8-35 U/L - Cholesterol: 150-200 mg/dl
Creatinine: 0.7-1.4 mg/dl - Glucose (fasting): 60 – 110 mg/dl
- Total protein: 6-8 gm/dl
Albumin: 3.5- 5.5 g/dl
Globulin: 1.7- 3.3 g/dl - Uric acid: 2.5 -8 mg/dl
Blood urea nitrogen: 10-20 mg/dl
Urine Examination:

1. Urine Color: Pale Yellow
2. Specific Gravity: 1.002-1.035
3. Osmolarity: 250-900msm/kg
4. Glucose: Negative
5. Protein: Negative
6.Bilirubin: Negative
7.WBC: 0-4
8.Bacteria: None
9.Casts and Crystals: None
10.Hemoglobin: Negative
