ENGLISH-MSN 1 UNIT 1 INTRODUCTION ( THE HISTORY OF MODERN MEDICINE AND SURGERY)
THE HISTORY OF MODERN MEDICINE AND SURGERY (The History of Modern Medicine and Surgery):
INTRODUCTION (Introduction):
USEFUL TERMINOLOGIES:
ACUTE ILLNESS
Acute illness which has severe symptoms but is of short duration. It is also recovered in a short time.
cronic illness
These diseases occur over a long period of time. Due to this disease, a person’s ability to function gradually decreases. Which usually causes gradual changes in the body throughout life and results in a very serious illness and these diseases are usually irreversible (cannot be cured). Chronic diseases last for a long time and these diseases remain the same throughout a person’s life.
ACUTE INFLAMMATION (Acute Inflammation)
Acute inflammation is characterized by local vascular and exudative changes and usually lasts less than two weeks. The process of infection in any part of the body is called inflammation.
In this, redness, swelling, pain, and warmth (warmth) are seen in the inflamed part of the body. The main cause of inflammation in the body is pathogenic microorganisms.
ASEPSIS
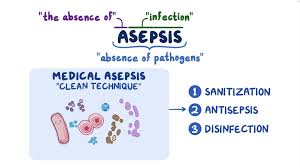
Asepticity is the state of being free from disease-causing microorganisms. (free from disease producing microorganisms).
DIESEASE

Disease is a condition in which the health of the body deteriorates. The health of a person does not remain normal, there are changes in the physiological functions of the human body. A person is unable to perform certain tasks and the vital functions of his body also deteriorate. Diseases are mainly caused by pathogenic microorganisms.
HEALTH

Health can be defined as complete physical, mental, social, and spiritual well-being, not merely an absence of disease and infirmity. (not merely the absence of disease or infirmity).
ILLNESS

People’s efficiency decreases during illness. People are unable to maintain any kind of physical and emotional balance and due to this, the efficiency of the person is disrupted.
INFECTON (Infection)
When any microorganism enters the body of a person and grows and multiplies (increases in number) and causes disease, it is called an infection.
MODE OF TRANSMISSION
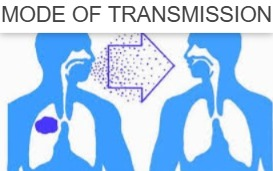
This is a type of transfer method in which microorganisms are carried from one place to another. Generally, the way in which a disease spreads is called the mode of transmission. For example. Direct contact, droplets etc.
PORTAL OF EXIT
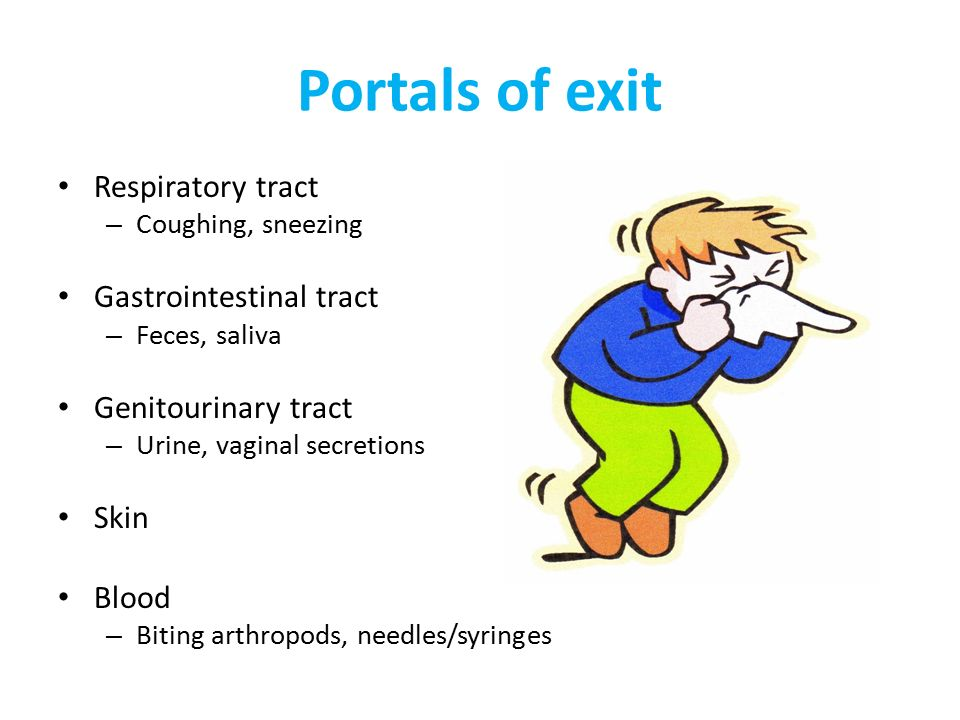
This is a place in the body where microorganisms in the body have a way to exit. E.g. Through urine and stool, through nose and oral cavity etc.
PORTAL OF ENTRY
This is the place in the body from where a microorganism enters the body of the host. For example, through the nose, oral cavity, broken skin and mucous membranes, microorganisms enter the body and spread the disease.
Reservoir

This is a place where any microorganism grows and develops. Multiplication can occur.
susceptible host
This is such a person That if microorganisms enter the person, they cannot fight them. Therefore, microorganisms develop and multiply (increase) and due to this, diseases occur and these people cannot resist those microorganisms.
Terminal illness
Terminal illness is a type of illness or disease that cannot be cured. It is fatal in which a person does not have a chance to live their life.
Trends

A trend is a trend in a certain direction. Changes or amendments to any rule. New developments in any field are called trends.
Wound

Wound occurs in the body in which A breakdown or cut occurs in the continuity of the body’s cells, tissues and structures. This breakdown is caused by any kind of physical injury, internal or external, and is called a wound.
This unit includes the following topics.
a. BRIEF HISTORY OF EVOLUTION OF MODERN MEDICINE AND SURGERY.
b. THEORY OF ILLNESS AND ITS CAUSATION – ILLNESS AS HUMAN EXPERIENCE.
c. REVIEW OF NURSING PROCESS AND NURSING CARE PLAN.
A) BREIF HISTORY OF EVOLUTION OF MORDEN MEDICINE 💊 AND SURGERY (History of the evolution of medical and surgical procedures).
Medical surgical nursing:

When any patient comes to the hospital for any kind of The treatment of illness, inflammation or disease conditions that are cured using medicines is called the Medicine Branch, and when the condition cannot be treated through medical treatment and those people require surgical treatment (surgery), it is called the Surgical Branch. Thus, any patient is cared for through the use of medicine and surgery.
In these two branches, the care of a patient through the use of different types of nursing care is called Medical Surgical Nursing.
Evolution of modern medicine and surgery:
The history of medical science is considered as a part of the history of civilization. It logically began in Mesopotamia.
MEDICINE AND SURGERY IN THE ANCIENT WORLD:
- The first evidence of weaponry is the trapid skulls of the Stone Age.
- Some adults had holes in their skulls. It was probably performed on people with head injuries to relieve pressure on the brain.
- According to him, the treatment of injury and illness was a mixture of common sense and magic.
- People knew that falls broke bones and fires burned, and that wounds were caused by animal bites and anthropomorphic techniques.
- Primitive people believed that the causes of diseases were evil spirits or magic performed by enemies.
- The cure seemed to be to drive out the evil spirit.
ANCIENT EGYPT MEDICINE 💊:
- The curtain rose on Egyptian civilization around 3000 b.c.
- Some people in civilized society held specialized jobs.
- The first known doctor in history was Sheikh Anach. He healed the pharaoh’s nose.
- Another doctor we know of was Imhotep.
- Who was the pharaoh’s vizier or prime minister.
- He was also a doctor and was so famous that he was worshipped as a god after his death.
- Egyptian doctors used a wide range of medicines derived from herbs and minerals.
- They mixed it with wine or beer, or sometimes with dough, to make pills.
- Egyptian doctors also used ointments for wounds.
- The Egyptians believed that the human body was filled with canals that acted like irrigation canals, carrying blood, urine, feces, tears, and semen.
- The Egyptians knew that irrigation canals could sometimes become blocked, which could cause blockages in the human body. The Egyptians used laxatives and induced vomiting to open them. were.
- The Egyptians used clamps, suture, and cauterization.
- They had surgical instruments such as probes, saws, forceps, scalpels, and scissors.
- They also knew that honey was a natural antiseptic that helped prevent wounds from getting infected.
- They also dressed wounds with willow bark, which has a similar effect to honey.
Ancient Greek medicine
- The origins of modern medicine lie in ancient Greece.
- Most Greeks believed in (Asclepius), the god of healing.
- People who were sick would make sacrifices or offerings to the god.
- They would then spend the night in his temple.
- They believed that God would visit them in their sleep, i.e. in dreams, and that they would be cured when they woke up.
- At the same time, Greek doctors developed a rational theory of disease and discovered cures.
- The most famous Greek doctor was Hippocrates.
- Hippocrates emphasized that doctors should carefully observe and record the symptoms of patients.
- Hippocrates also believed that all magic He rejected this and believed in herbal medicine.
- A number of Greeks theorized that the human body was made up of elements. If those elements were in the right balance, a person was healthy, but if they were out of balance, they would become ill.
- Finally, Aristotle thought that the body was made up of four humors. These were phlegm, blood, yellow bile, and black bile.
- If a person had too much or too little of one humor, that person would become ill.
Roman medicine 💊 (Roman drugs)
Roman Empire Often Greek, Galen became a famous doctor during Roman times.
Galen believed in the theory of the four senses and also believed in the treatment of disease.
So if a patient had a cold, Galen would give him a hot substance like pepper.
The Romans suggested that small animals that caused the disease were carried through the air and entered through the nose and mouth. entered the body.
The Romans were great engineers and they created a public health system.
The Romans also knew that dirt promoted disease. They appreciated the importance of cleanliness. They made sponges to make clean water in towns.
Medicine in middle age:

Medicine flourished in the Islamic world.
In the 10th century, known as Al-Razi (Razez in the West), the Western doctor of this name was the first to distinguish between smallpox and measles. Abuqasis was the first to write about hemophilia.
Muslims established many hospitals and also discovered distillation and elixir. (purifying substances by changing them directly from a solid to a vapor without passing through a liquid state) .
In the Middle Ages, only monasteries had cleanliness. Streams provide clean water. The dirty water was used to clean the toilets which were in separate rooms.
Medicine in 16 th century:
Girolamo Fricastoro suggested that infectious diseases are caused by disease spores that are carried by the wind (droplets) or transmitted (spread) by touch (direct contact).
Leonardo da Vinci dissected the human body and made accurate drawings of what he saw, another great surgeon was Ambroise Pare.
In the 16th century, a surgeon applied oil to a wound. He made a mixture of egg whites, rose oil, and turpentine and found that it worked better than oil.
He also designed artificial limbs. In 1513, Eucarius Rosali published a book on childbirth, The Rosen Garden.
In 1540, an English translation titled The Birth of Mankind was published, which became a standard text. However, midwives were women. Syphilis was common in the 16th century.
17th century Medicine (Medicine in 17th century):
An Italian named Centorio invented the medical thermometer.
In 1628, William Harvey discovered how blood circulates around the body. Harvey realized that the heart is a pump that pumps blood out every time it contracts.
Blood circulates around the body. Harvey then estimated how much blood is pumped each time.
Finally, in 1683, Antoine Leuven I observed microorganisms.
Doctors discovered that the bark of the cinchona tree treated malaria because it contained quinine.
18 th century Medicine (Medicine in 18 th century):

June Hunter invented tracheostomy.
Founded the treatment for scurvy by giving lemon juice.
Edward Zener found the smallpox vaccine.
19th century medicine (Medicine in 19th century):
Renlin invented the stethoscope.
Louis Pasteur developed a vaccine for rabies.
A vaccine for typhoid was also discovered. Rubber gloves were first used in surgery in 1890.
The banner show was greatly improved by Florence Nightingale and Mary Seacole.
who cared for soldiers during the Crimean War of 1854.
In the 19th century Great Ormond Street and Hospitals were established.
In 1864, Jean Henry Dunant founded the International Red Cross.
Women were allowed to become doctors in Britain from 1865.
20 th century Medicine (Medicine in 20 th century):

- Different blood types were identified.
- Insulin and EEG were also discovered.
- Alexander Fleming discovered penicillin.
- The polio vaccine was also discovered.
- The first heart and lung transplant was performed. was.
- Who eliminated the small box and CT scan and invented the M. R. I. (MRI).
- Gene therapy was introduced in the 1990s.
Evolution of surgery:
- Sushruta attained great mastery in the art of arms.
- His famous treatise, known as the Sushruta Samhita in 400 BC, is necessarily devoted to the art of arms.
- It contains a surgical text of Ayurveda and that too is clear.
- Vesical calculi, anal fistula (fissure, hemorrhoid), bone fractures (fractures), extraction of the fetus in abnormal labor (fetal Investigation), amputation, tumor removal, hernia repair, and cataract surgery, among other operations were performed.
- Rhinoplasty and plastic surgery were also performed.
- He mentioned knives and needles based on their use and the tissues involved.
- Thus modern medicine and surgery came into being.
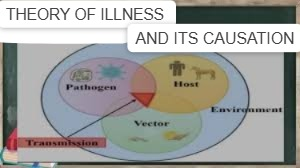
B) THEORY OF ILLNESS AND ITS CAUSATION – ILLNESS AS HUMAN EXPERIENCE.
Concept of Illness.

- Illness People’s ability to work decreases. A person cannot maintain a balance between any kind of physical and emotional status and due to this, a person’s efficiency is disrupted.
- Illness is a state of a person in which a person’s Emotional, intellectual, logical, social, religious, reduces the ability to work.
- Due to any illness, a person’s normal daily functioning also decreases and due to this, it affects the person a lot.
Two Types of illness (There are two types of illness).
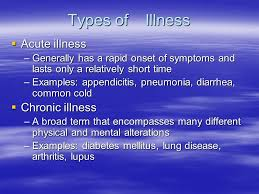
1) Acute illness (Acute Ilnesh)
2) chronic illness
1. Acute illness
This illness occurs suddenly. Due to this illness, the ability of a person to work decreases. In this illness, the speed of development of symptoms is very high and it occurs in a short period of time. These diseases are reversible (curable).
2. cronic illness
These illnesses occur over a long period of time. Due to this illness, a person’s ability to work gradually decreases. Which usually causes gradual changes in the body throughout life and results in very serious illnesses, and these illnesses are usually irreversible (cannot be cured). Chronic diseases last for a long time and these diseases remain the same throughout a person’s life.
concept of disease:
Disease is any disturbance in the normal functioning of the body. These diseases have a specific cause and their symptoms are mainly recognizable.
According to the Oxford English Dictionary Disease is defined as a condition of a part or organ of the body in which its functions are altered and from an economic point of view, it is defined as a disorder of the human life system with the environment of the disease.
Disease is a condition in which the health of the body is impaired. Due to this health, the human body cannot perform any important function, that is, its efficiency is reduced.
From the perspective of sociology Disease is considered as a social phenomenon. Which occurs in all societies and is defined in the context of a certain cultural group prevalent in the society. The simplest definition is that disease is the opposite of health which is any change from the normal functioning or state of complete physical or mental well-being because health and disease are mutually opposite conditions.
Who has defined health but not disease. The reason for this is that diseases have many sets of symptoms ranging from subclinical cases to severe overt illness. Some diseases start acutely. For example, food poisoning and some come on suddenly, for example, mental illness, arthritis, etc.
Some diseases have a carrier state. In which a person remains outwardly healthy and can infect others, for example, typhoid fever.
In some cases, a single organism can cause more than one disease. For example, streptococcus bacteria are present and how long they last. While some diseases can cause many illnesses, it is easy to determine the disease, but in many diseases, there is a border between normal and abnormal, like diseases like diabetes and hypertension. The final outcome of the disease is variable.
Causes of disease
Disease is an abnormal condition that affects the body of an organism. It has been interpreted many times. It is a clinical condition associated with specific symptoms and signs that can be caused by it. It can be caused by external factors such as infectious diseases or it can also be caused by internal problems.
causes of disease

1)Mechanical causes.
2)Biological causes.
3) Normative causes.
4)Nutritional causes.
5) Environmental Causes.
1)Mechanical causes
This causes damage to the structure of the body and any defect in the normal function of the body causes disease. For example. Injury, sprain, fracture etc.
2)Biological causes
Biological causes also affect the functioning of the body and result in genetic defects, agent infestation (organism), and infection (infection), changes in the immune system and changes in the secretion of normal organs.
3)Normative causes (normal Causes)
Common causes are psychological, but they involve the mind and body response (body-mind relationship). So due to these reasons, physical and mental problems arise.
4)Nutritional Causes
In developing countries, the main cause of diseases is due to the lack of nutrients and insufficient consumption of fruits and vegetables.
5)Environmental Causes
Environmental causes play a major role in the development of a person. Diseases include the following substances. Such as chemicals, acid aldehydes in cigarettes, allergens such as pollen, dust, mites, moisture, cat hair, etc. and pollutants produced by human activities such as sulfur oxides, nitrogen dioxide, carbon monoxide, or carbon dioxide, organic compounds carbon monoxide radioactive pollutants etc. and infectious agents such as viruses, bacteria etc. Many diseases are caused due to.
The causes of such diseases include mechanical causes, chemical causes, normative causes, nutritional causes, biological causes and environmental causes.
concepts of disease causation:
A. Germ theory of Disease:
Disease agent …… Man ……. Disease.
- In 1873, Pasteur put forward the germ theory of disease. This theory states that many diseases are caused by the presence and actions of specific microorganisms within the body. It is a guiding principle.
- The concept of theoretical causation embodied in the germ theory of disease is generally understood as a one-to-one relationship between the causative agent and the disease.
- The germ theory of disease was a revolutionary concept.
- It led many epidemiologists to adopt a one-sided view of the cause of disease.
- Before the germ theory, it was widely believed that disease was spread by noxious odors. Disease-causing conditions such as rotting meat, open sewers, and the like were often found in It was very smelly. Smell and disease were linked together.
- Thus, the germ theory shows that microorganisms play a major role in the causes of any disease.
Epidemiological Triad:
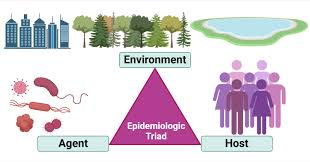
Agent (disease producing factors),
Host,
And
environment.
Epidemiological tried (Epidemiological triad):
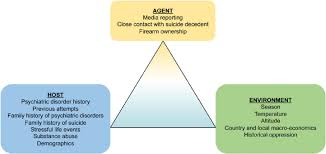
- The traditional model of the cause of infectious disease is known as the epidemiological triad.
- This triad includes external agents. The host and an environment. In which the agent, host and environment are the main factors in the spread of any disease.
- This epidemiological model has been in use for many years. It Helping epidemiologists focus on different classes of factors, especially in the context of infectious diseases. A classic example of a vector is the Anopheles mosquito.
- As the mosquito takes blood from an infected host, it ingests the parasite Plasmodium. Plasmodium is harmful to the host. However, after being stored in the salivary glands and injected into the host on which the mosquito feeds, Plasmodium can cause malaria in infected humans, acting as a vector for malaria.
Agent
- Agent Factors The first link in the chain of disease spread is the agent of the disease. A disease agent is defined as a substance. Living or non-living or active or dead, the excess presence or relative absence of which is necessary to perpetuate the disease process can start.
Host
- Host factors include various characteristics.
- Host factors are important to the extent that they affect.
- First:= Risk of exposure to the source of infection and
- Other := Host resistance or susceptibility to infection and disease.
- Host factors may include these.
- Age, sex, ethnicity ,group, nutritional status, socioeconomic status.
- Personal behavior: such as smoking, diet, drinking, sexual behavior, exercise, immunization status, or not vaccinated.
- Physical conditions: pregnancy, puberty, fatigue, immunosuppression, pre-existing diseases, etc.
Environment
- The study of disease is really the study of man and his environment.
- The external or macro environment is “all that is external to the individual human host, both animate and inanimate, and with which it constantly interacts”. Defined as, which includes air, water, food, shelter, etc.
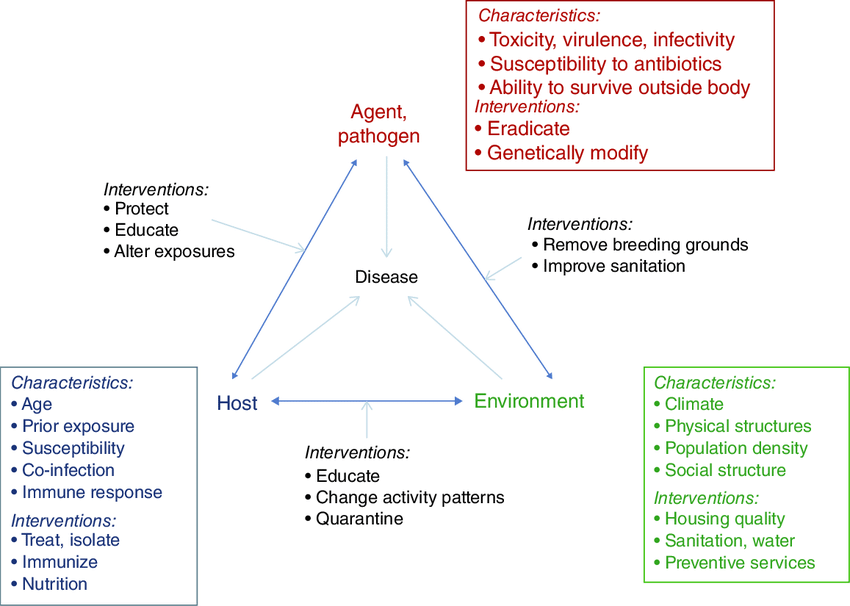
Agent factor
Nutritional agent, mechanical agent, chemical agent, physical agent, social agent, absence or Insufficiency or Excess, Biological agents.
Other causes for disease producing
Other causes also include diseases like heart disease, cancer etc.
Disease is when any microorganism enters the body of the host and those microorganism multiply and multiply. It causes disease in the host’s body. Thus, the agent, host and epidemiological agent act as a model for disease transmission.
C) review of nursing process and nursing care plan (Review of nursing process and care plan).

Nursing process:
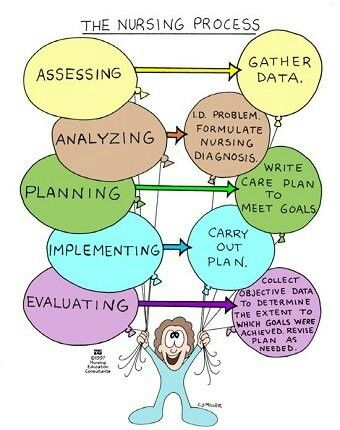
- The nursing process is a set of actions used to determine, plan, implement, and evaluate nursing care.
- The nursing process can be defined as a systematic approach to assessing a health condition, diagnosing appropriate care needs, developing a care plan, initiating the plan, and evaluating the effectiveness of the plan.
- The nursing process is a systematic and organized method of planning and providing quality and personalized nursing care. It is synonymous with a problem-solving approach. Which guides the nurse and client in determining the need for nursing care, planning and implementing care, and evaluating outcomes. It is a gosh approach to the efficient and effective provision of nursing care.
- The goal of the nursing process is to reduce and prevent actual or potential health problems. The nursing process can be applied to any action response. Which includes the nurse and the client.
Objectives of Nursing Process (Primary Objectives of Nursing Process)).
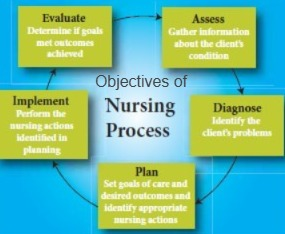
- The primary objective of the nursing process is to help the nurse manage the nursing care of each patient intelligently, scientifically and fairly.
- Helps maintain the patient’s health.
- Useful in protecting the client from illness.
- To identify the client’s clinical condition.
- To identify the client’s actual and potential health problems.
- To set priority for nursing procedures given to the client.
- To meet the identified needs of the client (need based).
- To provide adequate health care facilities to the client.
- To evaluate the nursing procedures provided to the client.
- To assist in the peaceful death of the client during terminal illness.
steps of nursing process (steps of nursing process):
Assessment (Assessment).
In this, information is collected about the patient’s condition.
Diagnosis.
In this, the patient’s problems are identified.
Planning.
This involves setting goals for the patient and planning the care of nursing interventions.
Implementation.
In this, the planned nursing intervention is implemented.
Evaluation.
In this, it is assessed to check whether the set goals and expected outcomes have been achieved or not.
Nursing assessment:
- Nursing assessment is the process of collecting or verifying data or information about a client.
- It is used to determine the level of health, well-being, and Helps establish a baseline about health habits, past illnesses, related experiences, and health care goals.
- It begins during the nurse’s first visit with a new patient and continues thereafter. This assessment includes asking about vital signs and performing a head to toe assessment. Ask questions about its signs and symptoms and listen carefully to the answers.
Nursing Diagnosis (NursingDiagnosis):

- Nursing diagnosis is the assessment of potential or actual problems in a client’s health condition.
- The treatment of which the nurse must be licensed and competent. This includes identifying these problems in the client, family, and significant others.
- The nurse creates a Nursing Diagnosis based on the nursing assessment.
Planning:

- Planning is the process of thinking about any nursing task before doing it.
- In it, nursing activities (Action) are planned to achieve any specific goal. And the client is planned according to which care is needed first.
Implementation:

- In A., the planned procedures are implemented.
- In this, the Plan of Action or Nursing Planning is implemented according to the patient’s needs. In this, actual care is provided to the patient.
Evaluation:

- In this, the implemented nursing processes are evaluated.
- In this, whether the goals have been achieved according to the goals we have set is evaluated.

Nursing assessment:

- Nursing assessment refers to the collection and interpretation of clinical information.
- It focuses on collecting data about the client’s health status, functional capacity, physical condition, and responses to actual and potential health problems.
- Nursing assessment involves the nurse assessing the patient.
- Nursing assessment involves the assessment of the client’s health problems. ,Related experiences, Health practices, Values and lifestyle, Health history.
- This involves observing the patient, interviewing the patient, his family, and other individuals, examining the patient, examining the patient’s records, and collecting information.
purposes of nursing assessment:
- To collect information about the client’s health For.
- To determine the client’s general functioning.
- To organize the information collected.
- To formulate possible hypotheses for the patient.
- To conduct an adequate investigation of the patient.
- To formulate a nursing diagnosis.
- To improve patient management skills and handle patient problems.
- To assess the patient’s health problems.
- To assess the client’s strengths.
- To assess the client’s health needs.
Type of assessment (Types of Assessment):
1.Initial assessment,
2.problem focused assessment,
3.Emergency assessment,
4)time lapsed assessment,
1.Initial assessment:
This assessment is done within a specific time frame after the patient is admitted.
2.problem focused assessment:
This assessment is done early to identify any specific problem.
For example, urination problem Intake output is assessed to know the status.
3.Emergency assessment (Emergency assessment):
This assessment is done immediately.
This assessment is done to do any physiological or psychological assessment.
This assessment is done to determine if the patient has a life It is done when there is a threatening condition.
Ex:=clients Airway, Breathing status, Circulation after cardiac arrest.
4)Time lapsed assessment:
This assessment is given to the client at a specific time. At that time, the client is assessed.
components of assessment:
1) collecting data,
2) organized data,
3) validating data,
4) recording data.
1)collecting data.
Collecting data is the process of gathering information about a client’s health status. In which the client’s health history, physical assessment, physical examination, laboratory tests, past history and present complaints of the patient are also collected in the data.
The collection of data should be systematic and continuous, no information should be forgotten.
The collection of data should be done keeping in mind the patient’s problem.
When collecting data, it should be descriptive, complete and accurate.
type of data
2 types of data
1) subjective data,
2)objective data.
1)subjective data: Subjective data includes symptoms.
Subjective data The client says it in his own words.
This information includes things like a client’s experience and emotions that he can only tell in his own words.
This information is also provided by family members and acquaintances of the client.
2)objective data: Objective data includes signs.
Objective data is collected by the health team Through observation, physical examination, laboratory tests, and measurements.
sources of data:
1)primary source:
- Primary sources include the client himself.
- Which includes the client’s subjective data that the client can say in his own words. This information is accurate because the client himself provides the information.
- The client provides his own accurate information.
- Which includes the client’s health needs, his lifestyle patterns, his past, and his present symptoms etc. The client says in his own words.
2)secondary source:
- This information is collected from the client’s family members and other significant people, the client’s medical records, charts, other members of the health team, and those who provide related care.
Family and relatives:These people Knows the client well.
- They can supplement the information provided by the client.
- They are the primary source of information for infants or children, seriously ill, mentally disabled, and unconscious clients.
Health care team: Every member of the health care team is a potential source of information. They can identify and communicate data and also verify information from other sources.
- They can collect client information from records, reports, laboratory investigations, etc.
- Thus, objective data can be obtained from the client’s family members, acquaintances, friends, records, reports, etc.
method of data collection:
1) Observation:
In this, information is collected by observing any patient or patient.
2) Interview:
Interviews are used to obtain information, identify problems, and evaluate changes. ,Teaching, or providing support or counseling requires interviewing the client.
3)Examination:
This involves collecting systematic data to identify health problems using measurements, physical examination, techniques, and interpretation of laboratory results.
E.g. cephalocodel:=head to toe assessment,
body system approach:= examining all the body systems.
review of system approach:= In this, only the specific affected area has to be examined.
2)organisation:
In this, the nurse arranges the information collected from the client in a specific order.
In this, the nurse arranges the information collected from the client in a specific order.
3)validating data:
- In simple word:=validating means cross checking the collected information
- (Validating means cross checking the collected information).
- This involves ensuring that the collected information is fact and true Cross-checking of data can be done in any of the following ways.
- Re-checking the client’s data, for example, re-checking pulse, blood pressure, etc.
- Confirming subjective data with objective data.
- Ask experts to re-check the collected information, for example, asking them to re-check the checked blood pressure.
- Re-checking the collected information.
- Verify with the client’s family members and their friends.
- Verify incorrect information as well.
- Also take the help of some kind of reference book including tax book, journal, research study.
4)Recording data:
- It is very important to record and report the information received from the client.
- The record should be accurate, complete, and in simple language, in an organized method.
- It is very important to record and report all the information properly. By doing this, no information is omitted (i.e. forgotten).
Nursing diagnosis:
- Nursing diagnosis is the second step of the nursing process. Then nursing assessment is done.
- In this phase, the data collected is analyzed and a nursing diagnosis is made based on the problem.
- North American Nursing Diagnosis Association (Nanda)
- Nursing diagnosis is made by collecting potential and actual information about the client.
- Nursing diagnosis is
- PES
- P:=PROBLEM,
E:=ETIOLOGY,
S:= SIGN AND SYMPTOMS /DEFINING CHARACTERISTIC.
PORPOSE OF NURSING DIAGNOSIS(Purpose of Nursing Diagnosis)::
- To analyze the collected information.
- To assess the normal functional status of the client.
- To identify the strength and weakness of the light.
- To make a diagnosis for the patient.
characteristic of nursing diagnosis.
1) Nursing diagnosis should be clear and concise.
2) Nursing diagnosis should be made according to the client’s evidence.
3) This should be based on planning.
4) Nursing care should be provided properly.
Type of nursing diagnosis (Types of Nursing Diagnosis):
1) Actual diagnosis,
2)High risk diagnosis,
3)wellness diagnosis,
4)syndrome diagnosis.
1) Actual diagnosis:
This diagnosis is made when the nurse assesses the client. The diagnosis is based on the actual need of the client.
- imbalance nutrition less than body requirement related to decreased appetite.
- Disturbed sleep pattern related to cough,fever and pain.
- Ineffective airway clearance related to viscous secretion.
- Acute pain related to cough secondary to Pneumonia.
- activity intolerance related to general weakness.
2)High risk diagnosis:
This problem describes a possible problem. It means that the client is more likely to develop the problem than other problems if they are in the same situation. It is a clinical judgment that the problem does not exist even if there are no signs and symptoms present.
Risk factors indicate that the problem is only likely to develop unless you intervene or do something about it.
For example, an obese classmate is undergoing hip replacement surgery so the nurse may make the following risk nursing diagnosis because the patient is on continuous bed rest.
- risk for Impaired skin integrity related to surgery.
- high risk for infection related to hospitalizations.
3)wellness diagnosis :
In this, a diagnosis is made about any specific wellness.
4)syndrome diagnosis :
In this, a nursing diagnosis is made about the syndrome of symptoms.
Ex:= rape, Trauma, Syndrome.
statement of nursing diagnosis :
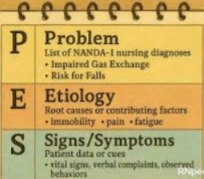
A nursing diagnosis statement has three parts.
1)problem,
2)Etiology,
3)definite characteristic .
1)problem:
In a problem, the client’s problems have to be stated and nursing diagnoses have to be made based on them.
Ex: knowledge deficit, Acute, Chronic, Ineffective, Altered, Decrease.
2)Etiology:
The etiology component of a nursing diagnosis identifies one or more causes of a health problem.
It guides the administration of nursing interventions.
It helps the nurse to provide individualized patient care because two patients may have the same problem but have different etiologies. may be.
3) Definite characteristic:
This involves the involvement of signs and symptoms of any problem. This includes subjective and objective data.
Ex:=fluid volume deficit related to decrease oral intake manifested by dry skin and mucus membrane.
2) risk for impaired skin integrity related to immobility manifested by redness on skin.
planning:

- Planning is the third important step in the nursing process.
- It is an important activity that involves the nurse’s thoughts on what to do, when to do it, where to do it, and who will do it.
- Planning involves interaction with the client, family, and health care team members.
- In planning Nursing care is planned by the nurse according to the patient’s needs and provided to the patient according to the patient’s needs.
- Planning is a deliberate systematic phase of the nursing process that involves decision-making and problem-solving.
- Planning is a nursing behavior that places the client at the center and plans interventions according to his or her needs to achieve a specific goal.
- Planning is a series of events that are carried out by the nurse to achieve a specific goal.
purposes of planning :
- To provide specific direction in the client’s activities.
- To maintain continuity of care for the client.
- To provide nursing care to the client according to his/her needs.
- To provide specific direction in the client’s activities.
- To maintain continuity of care for the client.
- To provide nursing care to the client according to his needs.
Types of planning (types of Planning):
1) Initial planning (initial planning)
2) ongoing planning (ongoing planning)
3) Discharge planning
1) Initial planning:
- This planning is done immediately after the patient is admitted.
- This planning has to be done very quickly and in a short duration because in this the hospital stay is less.
2) Ongoing planning:
- Ongoing planning is done by all nurses and provides care to the client.
- This planning has to be done every day and ongoing After assessment, planning has to be done.
3) Discharge planning:
- This planning is done about what kind of care the patient needs at home when he is discharged from the hospital.
- And what kind of environment has to be provided to the client at home and any special care given at home is planned for that is.
Phases of planning:
Planning is the process by which a nurse plans the type of care to be provided to a patient.
1)setting priority (setting priorities).
2)determine goal and expected outcome. (Setting goals and expected outcomes).
3)selecting the nursing strategies. (Selecting nursing strategies).
4) developing nursing care plan. (Creating a nursing care plan).
1)setting priorities:
Setting priorities is a decision-making process in which the nurse inquires about the patient’s problems and determines them in order. Priority is given to the nursing care that needs to be provided first.
A)High priority:
High priority includes problems that, if not solved, will cause great harm to the patient and can cause serious harm to the patient.
Ex:=ineffective Airways clearance after surgery related to abdominal Incision.
In this, it is very important to clear the patient’s airway.
Airway clearance is therefore a high priority in making a nursing care plan to improve the patient’s breathing pattern.
B)intermediate priority:
In this priority, even if there is a slight delay in providing nursing care, it does not indicate any kind of emergency, but care is provided as early as possible.
Ex:=pain related to Surgical process.
This includes the client’s pain It may take a while to remove, but it does not require immediate intervention.
C)low interventions:
Low priority includes nursing care that does not cause much harm to the patient, and it may take a while to remove, but it does not involve any kind of emergency.
Example:=definitely knowledge related to smoking cessation program.
2)determine goal and expected outcome:
The next step is to determine the goals or expected outcome.
The nurse should determine her goals and expected outcomes for each nursing diagnosis. Determines the outcome.
Goals are the goals set during a nursing intervention according to which care is provided to the client.
Purpose of goal :
To evaluate the client’s progress.
To see how effective the nursing intervention is.
Type of goals:
A)short term goal.
B)long term goal.
A)short term goal: This short time goal is to achieve a task in a short time. It has to be achieved within about a week, which requires immediate nursing care.
2) long term goal: This long term goal is to achieve a long term task. Which is usually achieved over weeks and months and can be achieved even after the patient’s discharge.
Expected outcome:
In this, the patient’s behavior that we want to achieve through nursing care is the expected outcome.
3) Selecting a nursing intervention:
Nursing intervention is a client are designed to achieve outcomes and have a specific approach.
Components of Nursing Interventions:
There should be a set of nursing interventions to achieve each outcome.
To be an effective nursing intervention, nursing interventions should be clear and concise.
Nursing interventions should be designed in consultation with the client, family members, consultants, etc.
Where is the nursing intervention? It should be clearly written when and how long it will take to complete.
4) Development of nursing care plan:
Writing a nursing care plan is the initial step in planning.
After assessing and diagnosing the patient, the nurse prioritizes each nursing diagnosis and forms a nursing care plan.
How to write a nursing care plan.
column:1
Includes the using assessment according to the priority.
column 2:=
Nursing diagnosis,
Expected outcome,
Column 3:=
includes nursing planning,
column:=4
Nursing interventions,
column:=5
contain evaluation.
Implementation:

- In simple terms, implementation is the process of putting planning into action.
- This is the fourth step of the nursing process.
- The nursing care plan is to be implemented by the client.
Purpose of implementation(Purpose of Implementation):
- To provide technical nursing care.
- To provide nursing care to prevent disease.
- To provide the client with the best level of health.
- To provide proper nursing care to the client.
Evaluation:

- Evaluation It is the fifth step of the nursing process.
- In this, the nursing intervention that has been implemented for the client is evaluated to see whether the goal that we have set has been achieved or not.
- In the evaluation phase, the nurse determines whether the goal of the nursing care that has been provided to the patient has been achieved or not.
- In simple terms, the nursing care that we provide to the client is done to see whether the proper client’s health has improved.
Purposes of evaluation
- To see whether the nursing care provided by the nurse is properly implemented.
- To see the client’s behavior towards the care provided by the nursing.
- To see whether the goals set by the nurse have been achieved.
- To see whether the client and family members are involved in the care provided by the nurse.
- To see how much the patient is cooperating with the nurse.
- To see if there is any mistake in the nursing intervention performed.
- To see how good the nursing care is.
Thus, in the nursing care plan
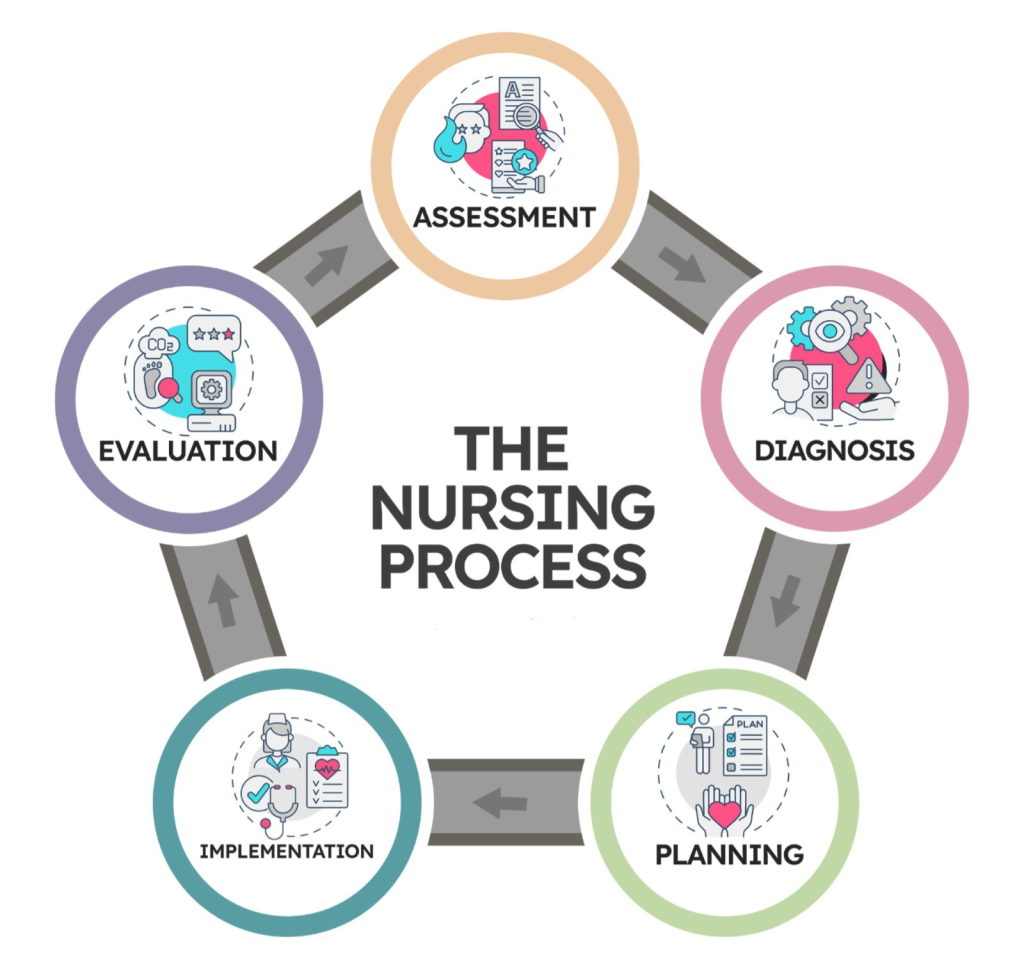
- assessment (Assessment),
- Diagnosis,
- planning
- implementation (Implementation),
- evaluation (Evaluation).
In this step, if a nurse provides care to any patient, the first step is the formation of a care plan.

FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
For unlocking 🔓 the full course or for more information, contact or whatsapp the following number.-
8485976407