ENGLISH-MSN-1-29/01/2024 (UPLOAD)-PAPER SOLUTION NO.08
29/01/2024- PAPER SOLUTION NO.08
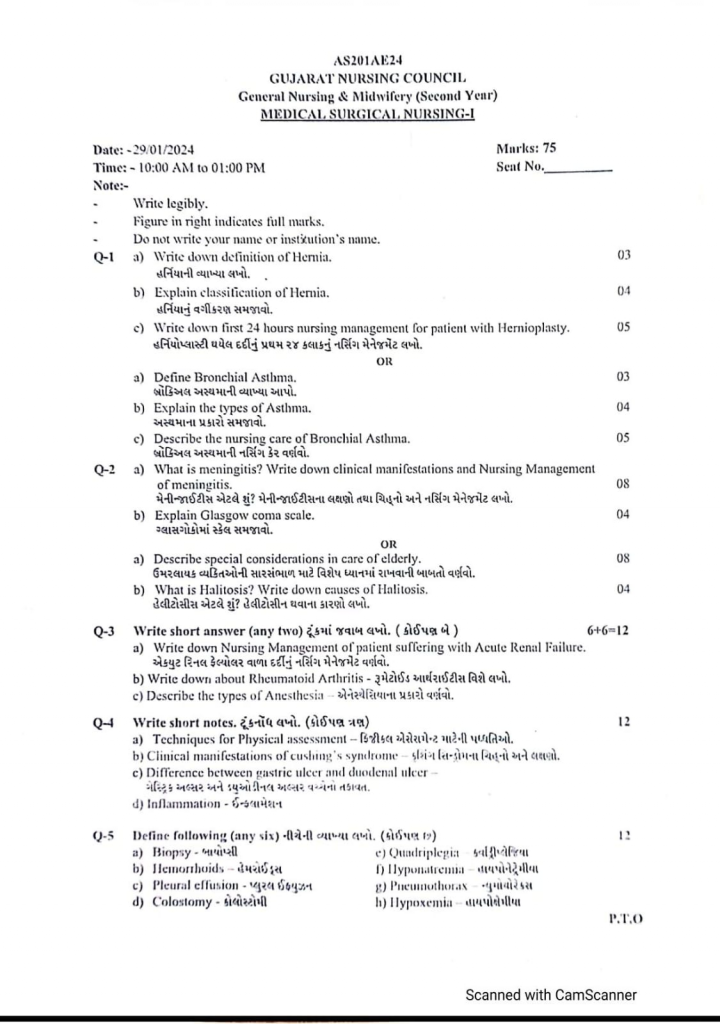
Q-1 a) Write down definition of Hernia. 03
Hernia is a condition in which a body organ or the muscular wall of the organ protrudes from its normal cavity.
The abdominal cavity has a muscular wall that plays an important role in supporting the abdominal organs.
When this muscular wall is bulging at some point, the abdominal organ protrudes from that bulging area into another cavity.
Hernia means that any organ protrudes from its normal cavity into another cavity, it is called a hernia.
Hernia := hernia may be defined as a protrusion of the organ from its normal body cavity to the other body cavity.
b) Explain classification of Hernia. 04
There are three types of hernias.
1)Reducibal hernia,
2)Irreducible hernia,
3)Strangulated hernia
1)Reducibal hernia,
=> A reducible hernia can be placed back in its normal place.
=> A reducible hernia can be returned to its normal place if the protruding organ is pushed back.
=> People with this type of hernia wear a special type of hernia belt so that the protruding organ remains in its normal place.
2) Irreducible hernia,
=> Irreducible hernia is a type of hernia in which the organ that has protruded cannot be placed back in its normal place.
=> This is mainly due to the fact that the organ is blocked by other intestines at the place where it has protruded.
=> Surgery is mainly required to treat an irreducible hernia.
3) Strangulated hernia
=> In a strangulated hernia, the organ that has protruded is mainly twisted in the intestines and the blood supply there is impaired.
=> This impaired blood supply leads to the formation of ischemia, necrosis and gangrene.
=> Immediate surgery is required in strangulated hernia.
Classification of the hernia. (Classification of hernia):
There are a total of ten classifications of hernia.
1)Inguinal hernia,
2)Femoral hernia,
3)umbelical hernia,
4)Incisional hernia,
5)Hiatal hernia,
6)Epigastric hernia,
7)Obturator hernia,
8)Spigelial hernia,
9)Ventral hernia,
10)Herniation of intervertebral disc
1)Inguinal hernia,
=> Inguinal hernia occurs mainly in the groin region (the area between the abdomen and thigh).
=> Inguinal hernia is mainly when the intestine protrudes from the week point of the inguinal canal and forms a triangle shape in the abdominal muscles near the groin region.
Mainly
•>Obesity,
•> Pregnancy,
•> Heavy lifting,
•> Straining during stool pass.
2) Femoral hernia,
=> Inguinal hernia is mainly found in the area between the abdomen and thigh.
=> Femoral hernia is mainly a bulge-like structure that appears in the upper part of the thigh.
=> Femoral hernia occurs in the lower part of the inguinal ligament.
=>Femoral hernia is mainly seen in women, pregnant women and obese people.
3)Umbelical hernia,
=> Umbilical hernia is mainly seen when the abdominal wall around the umbilical cord is weakened.
=> Umbilical hernia mainly protrudes from the umbilical cord and the area nearer to the umbilical cord.
=> Umbilical hernia is mainly seen in newborns, children and adults.
4)Incisional hernia,
=> Incisional hernia is mainly seen when the intestine protrudes from the surgical area after previous abdominal surgery, which is called Incisional hernia.
=>This hernia is mainly seen in elderly or over weight people.
5) Hiatal hernia,
=>Hiatal hernia is mainly an abdominal organ that protrudes from the abdominal cavity through the diaphragm muscles into the chest cavity.
=> Due to this, symptoms like heart burn and stomach acid are seen.
6) Epigastric hernia,
=> Epigastric hernia is mainly seen when the upper middle abdomen muscles are weak and the abdominal organ protrudes.
=> Epigastric hernia is mainly seen in men and is more common in women.
=> This is mainly seen in people between the ages of 20 and 50.
7) Obturator hernia,
=> Obturator hernia is mainly a protrusion of an abdominal organ through a gap in the front part of the pelvis and the bone.
8) Spigelial hernia,
=> In Spigelian hernia, the abdominal organ protrudes mainly through the spigelian fascia.
9) Ventral hernia
=> Ventral hernia is mainly a protrusion of an abdominal organ through a gap in the abdominal wall due to scar tissue developing in the abdominal wall, causing the abdominal wall to become weak and the abdominal organ to protrude through it.
10) Herniation of intervertebral disc
=> It is called a hernia due to increased pressure in the intervertebral disc.
=> Intervertebral disc herniation
c) Write down first 24 hours nursing management for patient with Hernioplasty. 05
Management of the patient after hernioplasty
Advise the patient to avoid heavy objects, weight lifting.
Advise the patient to wear a supporting belt.
Monitor the patient regularly.
Provide proton pump inhibitor medicine to the patient.
Advise the patient to eat fruits and high fiber fruits.
Advise the patient to do nasogastric suctioning.
Provide analgesic medicine to relieve the patient’s pain.
Provide antibiotic medicine to the patient.
Properly assess the patient’s health.
Assess the type of hernia the patient has.
Assess the patient for any signs and symptoms of hernia.
Provide complete information about the surgical procedure to the patient.
Prepare the patient properly for surgery.
Provide analgesic medicine to relieve the patient’s pain.
Advise the patient to do daily routine activities in small amounts and frequent amounts.
Monitor the patient for redness, itching, infection in the surgical incision.
Conduct proper wound assessment of the patient.
Provide the patient with a high-fiber diet, high fluids, and stool softeners.
Assess the patient for any complications.
Provide proper psychological support to the patient.
Advise the patient to follow up regularly.
Properly dress the patient’s surgical area.
Provide a calm and comfortable environment for the patient.
Properly provide intravenous fluids to the patient.
Properly provide mind diversional therapy to the patient.
Advise the patient to engage in small amounts of physical activity.
Advise the patient to engage in small amounts of daily routine activity.
OR
a) Define Bronchial Asthma..03
Asthma is a chronic inflammatory respiratory disorder. In which the airways become hyperresponsive to certain stimuli, due to which the airways become inflamed and narrowed, and obstruction is seen in the airways due to mucus production.
Asthma is different from COPD because it is a reversible process.
b) Explain the types of Asthma. .04
Bronchial asthma is known as asthma and is classified into different types based on triggers, symptoms and mechanisms.
Here are some common types of asthma.
1) Allergic asthma: This type of asthma is caused by exposure to allergens such as pollen, pet dander, mold spores, and dust mites. This type is the most common form of asthma.
2) Non-allergic asthma: Unlike allergic asthma, non-allergic asthma is caused by triggers other than allergens, such as cold air, exercise (which causes bronchoconstriction), respiratory infections, smoke, strong odors, and air pollution.
3) Occupational asthma: This type of asthma is caused by exposure to certain substances in the workplace. Such as chemicals, dust, or fumes.
Occupational asthma can occur in people who did not have asthma before entering the occupation.
4) Exercise-induced asthma (EIA): This type of asthma is triggered by physical activity and exercise. This type of asthma occurs during and after exercise and is usually more common in people who already have asthma and a family history of asthma.
5) Childhood asthma: This type of asthma starts during childhood and can continue into adulthood.
Childhood asthma is caused by allergic triggers and can get worse or improve over time.
6) Adult-Onset Asthma: This type of asthma develops for the first time during adulthood and there is no history of childhood asthma. Adult-Onset Asthma can be triggered by respiratory infections, hormonal changes, or environmental factors.
7) Severe Asthma: Severe asthma is asthma that is difficult to control despite taking a lot of medication. People with severe asthma need specialized treatment and have frequent asthma attacks.
8) Brittle Asthma: This is a rare and severe form of asthma that causes unpredictable and sudden, severe asthma attacks.
9) Aspirin-induced asthma: Some people develop asthma symptoms after taking aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs).
10) Cough variant asthma: In this asthma, instead of typical asthma symptoms such as wheezing and shortness of breath, a persistent dry cough is the main symptom of asthma.
These types of asthma can overlap and a person may experience more than one symptom. Effective management usually involves identifying triggers and controlling asthma symptoms and preventing asthma attacks.
c) Describe the nursing care of Bronchial Asthma. .05
Impaired gas exchange related to altered oxygen supply, obstruction of airway
Improve gas exchange
Monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assess breath sounds and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide the patient with a Fowler position and restrict his/her activity.
Explain and encourage the patient about deep breathing and cuffing exercises.
Provide the patient with knowledge about pursed lip breathing and diaphragmatic breathing.
Encourage the patient to expectorate phlegm if secretions are present.
If the SpO2 level is low, provide oxygen therapy.
Provide nebulization to the patient.
Administer the medicine (bronchodilator) prescribed by the doctor.
Maintain records and reports.
Ineffective airway clearance related to obstruction from narrowed lumen Maintain patent airway (Maintain airway patent)
Monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assess breath sounds and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide the patient with a Fowler position and restrict his activity.
Explain and encourage the patient about deep breathing and cuffing exercises.
Provide knowledge about pursed lip breathing and diaphragmatic breathing to the patient.
Encourage the patient to expectorate phlegm if secretions are present.
Provide oxygen therapy if SpO2 level is low.
Provide nebulization to the patient.
Administer prescribed medicine (bronchodilator) by the doctor.
Maintain records and reports.
Ineffective breathing pattern related to bronchospasm Improving breathing pattern (Improving breathing pattern)
Monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assess breath sounds and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide the patient with a Fowler position and restrict his/her activity.
Explain and encourage the patient about deep breathing and cuffing exercises.
Provide knowledge about pursed lip breathing and diaphragmatic breathing to the patient.
Encourage the patient to expectorate phlegm if secretions are present.
Provide oxygen therapy if the SpO2 level is low.
Provide nebulization to the patient.
Administer prescribed medicine (bronchodilator).
Maintain records and reports.
Reduce anxiety related to disease condition, hospitalization
Assess the patient’s condition.
Pay attention to the psychological needs of the patient and listen to the patient carefully.
Encourage the patient to express his feelings, discomfort and anxiety.
Solve all the doubts and queries of the patient.
Provide the patient with knowledge about his condition and treatment so that his anxiety is removed and the patient becomes confident.
Provide psychological support to the patient.
Provide the patient with mind diversionary therapy and recreational therapy.
Activity intolerance related to fatigue, dyspnea Increase activity level (increase activity level)
Assess the patient’s condition.
Check the patient’s activity level.
Provide bed rest to the patient initially.
Then gradually encourage the patient to do range of motion exercises.
Assist the patient with his/her activity.
Provide rest to the patient between 2 activities.
Check whether the patient experiences any breathing difficulty during the activity.
If breathing difficulty is observed, stop the patient’s activity and provide rest.
Q-2 a) What is meningitis? Write down clinical manifestations and Nursing Management of meningitis.
Meninges: Meninges are the protective membranes of the brain and spinal cord that cover the brain and spinal cord. These meninges have three other layers.
1) Duramater (outer most layer),
2) Arachnoid mater (intermidiate layer),
3) Piamater (innermost layer)
Thus, there are three layers of meninges that cover and protect the brain and spinal cord.
Meningitis: If there is infection and inflammation in the meninges layer surrounding the brain and spinal cord, then that condition is called meningitis. This infection can be caused by bacteria, viruses and microorganisms.
{ Meningitis: infection and inflammation of the Meninges layer that should be cover to the brain and Spinal cord }
Causes of Meningitis
Due to bacterial infection.
Ex:
Mycobacterium Tuberculosis ,
Streptococcus pneumoniae,
Neisseria Meningitidis,
Haemophilus influenzae,
Listeria monocytogenes.
Due to viral infection.
Mumps,
Herpis simplex virous,
Epstain barr virous,
Varicella-zoster virous,
Measles,
Influenza.
Due to fungal infection.
Due to Candida, Systemic Lupus Erythematosus (SLE),
Due to certain types of medication.
Due to head injury.
Due to trauma to the head and spinal cord.
Cancer.
Due to tobacco use.
Due to impaired immune system.
Due to overcrowding.
Due to brain surgery.
Symptoms and signs of meningitis
Headache,
Very high Fever,
Alternate mental status.
Confusion.
Altered consciousness.
Vomiting.
Photophobia ( An inability to tolerate light).
Irritability.
Drowsiness.
Confusion.
Altered consciousness.
Vomiting.
Sign of meningial irritation.
Nuchal rigidity ( Neck stiffness).
Headache.
Altered mental status.
Stunting.
Joint pain.
Muscle ache.
Positive Brudzinski Sign:
In Brudzinski sign, when the patient is provided with a supine position and his neck is flexed towards the chest, his hip and ankle automatically flex, which is called Brudzinski sign.
Kerning sign:
In Kerning sign, when the patient is provided with a supine position, after which the knee and hip of the patient are flexed, if the patient feels pain when the knee is extended again, it is called Kerning sign.
K:= Knee,
E:= Extention
R:= Resistense. That is, the patient feels pain when the knee is directly extended.
Diagnostic evaluation of a patient with meningitis
History taking and physical examination.
Blood culture.
Lumbar puncture.
Chest X-ray.
CSF examination.
CT scan.
Gram stain.
CSF culture.
MRI test.
Management of a patient with meningitis
If the patient has any bacterial infection, provide antibiotic medicine.
Ex:=
Rifampicin ,
Cefotaxime,
Vancomycin.
If the patient has any viral infection, provide antiviral medicine.
If the patient is in pain, provide analgesic medicine.
Ex:Acetaminophen, NSAID ( Non steroidal anti inflammatory drug).
Provide intravenous fluid to the patient.
If the patient has fever, provide antipyretic medicine.
If the patient has seizures, provide anticonvulsant medication.
Continuously monitor the patient closely.
Continuously monitor the patient’s vital signs.
If the patient has inflammation, provide corticosteroid medicine.
If the patient has meningitis, keep him properly isolated.
Properly monitor the patient’s hydration status.
Properly provide nutritional support to the patient.
Properly provide intravenous fluids to the patient.
Nursing management of the patient with meningitis
Properly assess the patient.
Continuously monitor the patient’s vital signs.
Properly assess the patient’s hydration status.
Maintain the patient’s proper fluid and electrolyte levels.
Provide analgesic medication if the patient is in pain.
Properly assess the patient’s neurological status.
Provide anticonvulsant medication if the patient is having seizures.
Provide proper nutritional support to the patient.
Provide proper psychological support to the patient.
Provide proper education to the patient about their disease, its causes, and its symptoms and signs.
Continuously monitor the patient’s intake output.
Continuously monitor the patient’s vital signs and neurological status.
Continuously monitor the patient’s level of consciousness.
Advise the patient to take medicine regularly.
Advise the patient to have regular follow-up.
Provide proper psychological support to the patient.
b) Explain Glasgow coma scale.
In the Glasgow Coma Scale, any type of stimulus is provided to the patient and the type of response the patient provides is assessed.
The Glasgow Coma Scale checks the patient’s level of consciousness.
Three main components are assessed in the GCS.
1) Eye opening
2) Verbal Response
3) Motor Response
1) Eye opening
A total of four scores are given in eye opening.
1) Spontaneous (= In this, the patient opens and closes his eyes on his own) := { 4 }
2) To voice (= In this, the patient is asked to open and close his eyes and the patient follows) := { 3 },
3) To pain (= In this, the patient is pinched in the body and the patient makes an eye expression) := { 2 }
4) No response (= If there is no response from the patient) := { 1 }
2) Verbal Response (Voice Response)
There are a total of five scores in Verbal Response.
1) Oriented (= if the person is asked about time, place and person and the person gives the correct answer) := { 5 } ,
2) Confused (= if the patient is asked about time, place and person and the patient is confused):= { 4 } ,
3) Inappropriate word (= if we ask the patient some question and the patient gives something else) := { 3 } ,
4) Incomprehensible sound (= if the patient is asked any question and he only makes sound through his mouth) := { 2 } ,
5) No response (= if no response is given) := { 1 }
3) Motor Response (= if the patient does not respond) Response)
Motor response mainly has six scores.
1) Obey command (= Whatever the patient is told to do, if the patient follows it properly) := { 6 } ,
2) Localized pain (= If the patient is pinched and the patient provides a response) := { 5 } ,
3) Withdraw pain (= If the patient is pinched and the patient tries to withdraw the hand) := { 4 } ,
4) Flexion (= When any mid-area of the patient’s body is pressed and the patient’s body flexes):= { 3 } ,
5) Extension (= If any stimulus is provided, the patient’s body extends):= { 2 } ,
6) No response (= If If the patient does not provide any response):= { 1 }
Thus, the Glasgow Coma Scale has a minimum score of 3 and a maximum score of 15.
result:
{ 3 } score achieve:= Then the patient has severe neurological damage.
{ 7 } score Achieve:= Then the patient is in a comatose state.
{ 8-12} score Achieve:= Then the patient has moderate neurological damage.
{ 13-14} score Achieve:= Then the patient has minor neurological damage.
{ 15 } score Achieve:= Then the patient is fully conscious and oriented.
Thus, the patient’s level of consciousness is assessed from the Glasgow Coma Scale.
OR
a) Describe special considerations in care of elderly.
1) Promotion of Self Respect and Dignity:-
In some institutes or groups, there are usually some restrictions on personal choice and independence.
The feelings of the elderly should be respected.
While the staff makes positive efforts to develop good relationships with the patients and gain their personal respect and friendship.
By developing good relationships, the group can be controlled and difficult situations can also be made easier.
2) Promotion of Comfort: Relaxation is necessary for physical and mental comfort. There are many factors that contribute to the comfort of the elderly such as skin care, care of bony structure, maintenance of temperature and fluid balance.
3) Safety:- Provide unpolished floors, good lighting, appropriate bed height, and proper walking aids
4) Daily Living Activities:- Encourage the patient to do as much daily activity as possible to prevent complications like dehydration, thrombosis, pressure sores, contractures, and ulcers.
5) Promotion of independence:- Encourage the patient to take self-care as much as possible and ask them to make their own decisions.
6) Encourage mobility and movement.
7) Ask them to take necessary medications and provide sufficient knowledge about those medications, such as side effects of the medication and its use.
8) Do rehabilitation in the patient according to his condition.
Additional Information:-
Skin care:-
Use mild soap
Bath once or twice a week
Hair care and brushing every day
Use moisturizers
Keep nails short
Use sunscreen, hat, long-sleeved clothing
Stay away from things like hot water bottles.
Pay attention to footwear so that sores do not occur
Avoid sun stroke
Supporting Changes in Bones and Joints:-
Do light exercise
Take precautions to avoid falls
Give a balanced diet that includes calcium and vitamin D supplements
Monitor and treat patient for pain
Give the patient more time because it may take more time to work.
Supporting Changes in Vision:-
Proper lighting should be provided to the patient
If necessary, the patient should be helped in choosing clothes
Natural tear products should be used.
The patient should be approached directly.
Supporting Changes to Hearing:-
While talking, reduce unnecessary noise.
Put yourself in the patient’s place so that the patient’s needs can be understood
Before speaking, make sure that the person’s attention is on you.
Get checked by a doctor and if necessary, get wax (mel) removed
Arrange for hearing assessment and if necessary, provide hearing aid.
5.Supporting Changes in Smell and Taste:-
Attractive meals should be prepared in which food with good smell should be prepared.
Spoiled food should not be given to eat
6.Supporting Changes in the Cardiovascular System:-
People get tired more easily due to cardiovascular changes, so they should be given more rest.
According to healthcare professionals, regular blood pressure monitoring should be done
If the person is unable to move on his own, he should be made to change positions frequently
Ask him to drink enough fluids and seek immediate medical help if the patient is dehydrated.
7.Supporting Changes in the Respiratory System:-
Short-term activities should be planned
More time is needed for rest.
If the person is unable to move on their own, they should be changed frequently
If the person is coughing continuously during or after meals, then ask them to consult a doctor
Keep the body alignment and position proper
Stay away from polluted air
Give oxygen therapy if necessary
8.Digestive Care:-
Maintain oral hygiene
Take appropriate treatment if there is tooth damage
Provide a comfortable environment for eating
Feed high fiber, high protein food with different tastes and textures.
Advise to drink more fluids
Give calcium and vitamin D supplements to prevent osteoporosis
9.Supporting Changes in Elimination:-
Maintain daily activities
Plan for the bathroom when going out
Reduce caffeine intake
Increase fiber intake
Do light exercise
Provide emotional support.
Everything should be given as needed.
- Urinary Care:-
Increase fluid intake
Drink less fluid before bedtime
Wear clothes that can be easily removed
Use absorbent pads
- Elderly care at home:-
If there is a wound, take care of it and get it dressed regularly
Monitor vital signs and give medicine on time.
Manage the patient if they are in pain or experiencing any discomfort
Help them with their daily hygiene needs.
b) What is Halitosis? Write down causes of Halitosis.
Halitosis is called bad breath.
=> In halitosis, an unpleasant odor is present when the breath is exhaled.
=> Halitosis is mainly seen due to dental decay, poor dental care, any gum disease, and bacterial infection.
State the reasons for patients with halitosis.
1) Due to taking certain types of food.
Ex:= Due to onion, garlic, fish, cheese, spices etc.
2) Due to tobacco products:=
=> Gum disease occurs due to smoking, due to which bad breath comes from the mouth.
3) Poor dental hygiene:=
=> If the mouth is not cleaned properly, then bad breath can come from the mouth.
4)Oral disease :=
=> Halitosis is also seen due to gingival dental decay, ulceration etc.
5)other cause:=
=> Due to chronic rhinosinusitis.
=> Due to tonsillitis.
=> Gastero esophageal reflux disease (GERD),
=> Due to lower respiratory tract infection.
=> Due to renal failure.
=> Due to nasal infection.
=> Due to renal infection.
=> Due to diabetes mellitus (smell of acetone breath).
Q-3Write short answer (any two)
a) Write down Nursing Management of patient suffering with Acute Renal Failure.
Nursing management of a patient with acute renal failure:
Properly assess the patient.
Properly monitor the patient’s vital signs.
Properly monitor the patient’s fluid balance.
Properly monitor the patient’s intake output chart.
Monitor the patient’s blood urea nitrogen level.
Assess the patient for any signs and symptoms of fluid overload.
Collaborate with health care team.
Monitor the patient’s electrolyte levels.
Properly provide medication to the patient.
Provide antihypertensive medication to the patient.
Properly provide nutritional support to the patient.
Advise the patient on fluid restriction.
Provide proper dialysis care to the patient.
Provide proper skin care to the patient.
Monitor the patient’s skin integrity properly.
Advise the patient on dietary restrictions.
Provide psychological support to the patient.
Advise the patient on maintaining proper hygienic conditions.
Collaborate with the patient’s health care team properly.
Monitor the patient’s intake output chart.
Monitor the patient’s daily weight.
Monitor the patient’s blood pressure properly.
Monitor the patient’s blood urea nitrogen level, creatinine and electrolyte levels.
Monitor the nutritional status of the patient.
Provide the patient with a high-calorie, low-protein, low-sodium, low-potassium diet and vitamin supplementation.
Provide the patient with small and frequent amounts of food.
Advise the patient to maintain strict aseptic technique.
Provide the patient with good oral care.
Monitor the patient’s heart activity properly.
b) Write down about Rheumatoid Arthritis
Rheumatoid arthritis is a chronic, systemic, autoimmune connective tissue disorder that causes inflammation of the tissues that line the joints, including the synovial membrane. It also causes destruction and proliferation of synovial members.
This results in joint destruction, ankylosis (stiffness of the joint), and deformity.
Autoimmune means that the body mistakenly identifies its own connective tissue and attacks it, primarily in the joints, causing pain, stiffness, and immobility in the joints.
Rheumatoid arthritis also affects other organs of the body, including the skin, eyes, lungs, and blood vessels.
Causes of Rheumatoid Arthritis:
The exact cause of rheumatoid arthritis is unknown.
Due to genetic factors (if a parent has this disease, there is a possibility of it in their child),
Due to stress.
Sex:=women are more likely to develop rheumatoid arthritis.
Due to any infectious agent.
It mainly occurs between the ages of 30 and 60.
Due to environmental factors.
Due to family history.
Due to hormonal effects.
Due to long-term smoking.
Due to metabolic and biochemical abnormalities.
Due to any bacterial, fungal, viral infection.
Due to immunological response.
Stages of Rheumatoid Arthritis
1) SINOVITIS,
2) Pannus formation
3) Fibrous tissues Ankylosis
4) Bony Ankylosis
1) Synovitis:
In this, when there is an infection in the body, the infection mainly affects the synovial membrane of the joint and due to this, infection and inflammation occurs in the synovial members and due to this, synovitis occurs and synovial fluid increases.
2) Pannus formation:
This synovial fluid becomes inverted and it becomes very thick and this fluid increases around the capsule of the joint.
3) Fibrous tissues Ankylosis:
In this, the synovial fluid increases greatly and it becomes stiff and it gets stuck around the joint and forms a hard structure.
4) Bony Ankylosis:
In this fibrous tissue forms a very hard structure and forms a bone-like formation and due to this the joint becomes immobilized and stiffness occurs in it.
Due to any etiological factor.
|
Infection of the synovial membrane occurs.
|
Inflammation of the synovial members occurs.
|
Synovial fluid is secreted from the synovial members.
|
This fluid progresses and accumulates in the bone.
|
And the bone becomes a very hard and stiff bone which is an immobilized bone.
|
Rheumatoid arthritis.
Symptoms and signs:
The affected joint becomes red, warm.
Joints become swollen and stiff and tender.
Joint pain.
Joint morning stiffness.
Arthritis occurs in more than three bones.
Joint becomes swollen (sponge like).
Arthritis occurs in the joints of the hands.
Firm bumps of tissues under the skin on arms.
Rheumatoid nodules form.
Rh factor positive.
Fluid accumulation in the ankles.
Joint loses its range of motion and becomes deformed.
Muscular atrophy around affected joint.
Ulnar deviation
In this, the finger deviates towards the ulnar surface.
Swan neck deformity
In this, the finger becomes a swan’s head.
Bouterine deformity
In this, the finger becomes bent.
Knock knee.
Difficulty in sleeping.
Numbness and tingling sensation.
Burning sensation in hand and foot.
Formation of lumps under the skin.
Burning sensation in the eyes.
Itching and discharge.
Dry mouth and eyes.
Chest pain.
Weakness.
Difficulty breathing.
Fatigue.
Loss of appetite.
Weight loss.
Low grade fever.
Malaise.
Depression.
Lymphadenopathy.
Inflammation of blood vessels.
Having involvement of multiple organs (pericarditis, osteoporosis, anemia, subcutaneous nodules, vasculities, neuropathy, fibrotic lungs disease).
Diagnostic Evaluation:
history taking and physical examination.
Rheumatoid factor test:= RA positive.
antinuclear antibody test.
erythrocyte sedimentation rate (ESR).
c-reactive protein (crp test).
complete blood count test.
Comprehensive metabolic panel (to monitor kidney and liver function).
synovial fluid analysis (synovial fluid changes from transparent to milky, cloudy, and dark yellow fluid).
arthroscopic examination.
X Ray.
joint ultrasound.
MRI.
Management of rheumatoid arthritis:
medical management
1)NSAID (NON STEROIDAL ANTI INFLAMMATORY DRUG) (This medicine is used to relieve pain and inflammation.)
Ex:= ibuprofen,
Naproxen sodium.
2)DMARDs (disease modifying antirheumatic drugs) :
These are mainly given in conditions such as moderate to severe rheumatoid arthritis.
Ex:=imuran,
Anti malarial medication,
Panicillamine and mithotrexate.
3) Antimalarial medication:
This medicine mainly uses hydroxyquloroquine along with methotrexate.
4) Corticosteroid:
Corticosteroids are mainly used to relieve inflammation.
5)Biological agent:
Tnf-a antagonist targets B cell, T cell.
Biological agent includes actemra,
Rituxan,
Remicade,
Enbrel,
Kindred,
.
6) Immunosuppressants:
These medications mainly weaken the immune system which is out of control in rheumatoid arthritis.
Ex:=azathioprine( imuran, azasan), Cyclosporine.
7)(tumor necrosis factor a):
These medications mainly inhibit the inflammatory chemical which is tumor necrosis factor.
Surgical management:
1) Joint fusion:
In this, surgical fusion of the joint is done to stabilize the joint.
2) Synovectomy:
This mainly involves removing the joint lining.
This is mainly used to remove the inflamed tissues that are causing pain.
Synovectomy is mainly used to reduce swelling and slow down joint damage.
3) Tendon repairs:
The tendons around the joint that are inflamed and damaged are loosened, so the surgeon repairs the tendons around the joint.
And keeps it stable.
4) Total joint replacement:
In joint replacement, the surgeon removes the damaged joint part and inserts a prosthesis that is made of metal or plastic in its place.
Nursing management:
Assess the patient’s pain level.
Assess the amount of morning stiffness the patient has.
Provide a comfortable position to the patient.
Encourage the patient to use non-pharmacological management.
Such as yoga, relaxation techniques, guided imagery, and rhythmic breathing.
Advise the patient on hot and cold applications.
Provide the patient with prescribed medications.
Instruct the patient to rest between activities.
Instruct the patient to rest frequently.
Instruct the patient to engage in physical activities such as walking, swimming, etc.
Instruct the patient to use assistive devices.
Instruct the patient to verbalize his or her feelings.
Provide complete education to the patient about the disease and its treatment.
Instruct the patient to maintain strict aseptic technique.
Provide education to the patient to participate in self care activities.
Encourage the patient to join self help groups and support groups.
c) Describe the types of Anesthesia
Anesthesia is a group of chemical agents that cause partial or complete loss of sensation.
There are three types of anesthesia.
1) Local anesthesia:-
This affects a limited area of the body (local part). It usually affects only the part of the body on which surgery is to be performed, which part needs to be numbed.
The following chemicals are used in local anesthesia.
Xylocaine hydrochloride
Lignocaine hydrochloride
Emethocaine hydrochloride
Procaine hydrochloride
2) Spinal anesthesia:-
There are two types of this-
1) Epidural anesthesia:- When anesthesia is injected into the epidural part of the spinal cord, it is called epidural anesthesia.
2) Spinal Anesthesia:- When anesthesia is injected into the subarachnoid space of the spinal cord, it is called spinal anesthesia.
Uses of Spinal Anesthesia:-
Orchidectomy
Caesarean
Hernia Surgery
Hydrocele Surgery
Penis Surgery
Prostate Surgery etc..
Complications:-
Urinary Retention
Meningitis
CSF Leakage
Hypotension
Paralysis
Allergies, Headaches etc.
3) General Anesthesia:- When there is a need to lose sensation in the entire body, the person is rendered unconscious. It is called general anesthesia. General anesthesia can be given as follows-
- Intravenously
- Inhalation
- Intravenously:-
The following drugs are used in general anesthesia through I.V. injection.
Thiopental sodium 2.5%
Hexabarbitone 10%
Methohexital sodium 1%
Propofol
Midazolam
Fentanyl
Ketamine hydrochloride
Droperidol
- Inhalation anesthetics:-
This anesthesia is given through inhalation, which makes the patient unconscious.
Before giving this anesthesia, the patient is given some sedatives, then an endotracheal tube is inserted into the airway, and then it is given through inhalation.
The following drugs are used in this.
Sevoflurane
Nitrous oxide
Ether
Cyclopropane
Methoxyflurane
Enflurane
Penthrene
Q-4 Write short notes.
a) Techniques for Physical assessment –
Physical examination uses systemic assessment techniques and visual, auditory, tactile, and olfactory senses. All these senses will be used in specific assessment techniques.
For example.. It is often detected by changes in body odor and fluid.
Four specific techniques are used in physical examination. Which include inspection, palpation, percussion, and auscultation.
- Inspection:
Inspection is a visual examination of the patient. And it is a visual examination of the body. In which the patient’s general appearance, body size, gait, height, shape, posture, etc. are carefully observed. This begins as soon as the nurse makes contact with the patient.
During the inspection phase of the physical assessment, the nurse uses observation skills to systematically collect observable data.
This includes measuring the patient’s respiratory effort, skin color, and wound.
General appearance
Status of consciousness
Personal grooming
Expression: worried, comfortable, alert, nervous. Body build: thin, fat, moderate. This also involves linking the patient’s words with body language.
For example, the patient’s pain experience is related to his body language.
During inspection, the maximum area of the body is visualized and then compared with the side of the other body.
Comparing the width of the right hand with the width of the left hand.
Adequate exposure of the body area is very important. In which color, texture, mobility, symmetry, nutritional status etc. are observed.
- Palpation:
Palpation means using the hands and fingers to feel the texture, size, shape, placement, location, etc. of the organ. In which specially using the finger tips of the hand to assess the temperature, pulse, texture, moisture, mass, tenderness and pain of the skin.
Gentle palpation is done by pressing 1 cm deep to assess the skin, pulse, palpation, and tenderness.
Then press 4 cm with both hands which is deep palpation. With its help, the size of the organ and the deep organ (liver) are determined.
What should be kept in mind while doing palpation?
It is always important to explain to the patient before palpation because touch is very important in our culture.
Keep the hands warm and nails short before palpation. The palmar surface of the finger is more sensitive than the finger tips, with the ulnar surface being more sensitive to vibration and the dorsal surface being used for temperature.
Palpation also helps in determining the size of the lymph nodes.
Always proceed with gentle palpation first and then with deep palpation. This can cause tenderness or fluid disturbance.
Using both hands, the size and shape of the kidneys and uterus are assessed between the finger tips and the organ.
- Percussion:
In simple words, it is called tapping. To get the quality of sound, the sound is heard against the patient’s body by tapping with a finger. Which is used to reflect the density of the internal organ. The sound, vibration and resistance that are produced with different densities and vary from organ to organ and are used to know the size, shape, position, and also to detect the fluid field of the internal organ.
Percussion is a technique that the physician practices to determine the consistency of the tissue.
In percussion, tapping is used to produce various palpable vibration sounds with short or sharp strokes on the body surface.
Percussion is used to detect the sound, location, size, shape, and size of many organs of the body. In which the examiner taps on the patient. To extract the sound, the middle finger of the non-dominant hand is usually placed on the percussion area. And the middle finger of the dominant hand is placed on the non-dominant.
In which percussion is done in two ways.
- Direct percussion
This is used for the chest of an infant and the sinuses of an adult. Specific parts of the body are struck with the help of finger tips.
In kidney tenderness. Listen for the vibrations created.
It is necessary to select the same point two or three times before doing another. This is done to get an accurate reading. Strong percussion is needed for fatty patients.
_Percussion tones: Air is soft, fluid is dull and solid is soft.
- Indirect percussion
This varies according to the area in which the non-dominant hand is placed palm down and the fingers of the dominant hand are gently struck on the CVA, e.g. in the kidney….
_Thorax: The middle finger of the dominant hand strikes the interphalangeal joint of the non-dominant hand which is against the patient’s skin.
Percussion produces sounds which have many sounds and different characteristics.
Characteristics of the sounds
Tympanic usually heard over the abdomen.
Resonance which is in normal lung tissue.
Hyper resonance which is in dilated lungs.
Dullness over the lungs.
Flatness over the muscles.
Auscultation
Auscultation is usually performed with a stethoscope. A stethoscope is used to block out extraneous sounds while assessing the condition of the heart, blood vessels, lungs, pleura, and intestines.
These include breath sounds, heart vascular sounds, and bowel sounds.
It is commonly used to detect the presence of abdominal sounds and assess their loudness, pitch, quality, frequency, and duration.
The most commonly heard sounds include the lungs, heart, and abdomen and blood vessels.
The chest is auscultated for heart sounds. Lung sounds are auscultated anteriorly and posteriorly for normal and incidental lung sounds. The abdomen is auscultated for bowel sounds.
Characteristics of the sound:
Intensity: Loud, medium, soft.
Pitch: Low, high, medium.
Duration: Short, long, medium.
Quality: Booming, hollow, dull, and drum-like.
b) Clinical manifestations of cushing’s syndrome
Body weight increases.
Upper body obesity occurs and hands and feet become thin.
The patient’s face becomes round and red.
Fatty buffalo hump in the neck region.
Its growth is also slow in children.
Skin changes are:=
Skin infections are seen.
Acne is seen in the body.
Straie (white colour stretch marks on the abdominal skin) are seen on the skin of the abdomen, thigh, and Breast.
Skin with easy brushing (bruising of the skin).
Skin becomes thin, fragile.
Muscles and bone changes include:=
Backache while doing routine activities.
Pain and tenderness in the bones.
Difficulty climbing stairs due to proximal muscle weakness.
Collection of fat between the two shoulders (buffalo hump).
Fractures in the ribs and spinal cord due to thinning of the bones.
Muscle weakness.
Women with Cushing syndrome often have:
Excessive growth of hair on the face, neck, chest, thighs (hirsutism) due to Cushing syndrome in women.
Irregular menstrual cycle.
Men may have:
Decrease or no desire for sexual activity.
Impotence
( ejaculatory failure).
Other symptoms of Cushing syndrome are:
Psychological problems:
Depression, anxiety and behavioural changes are seen.
Blood pressure increases.
Bone loss.
Sleep disturbances are seen.
Excessive catabolism of protein occurs.
Muscle wasting is seen.
Sodium and Water retention occurs.
The patient has a moon face appearance.
The patient has a condition of hyperglycemia.
Polyuria (increased frequency of urination).
Polydypsia (Increase thirst).
c) Difference between gastric ulcer and duodenal ulcer-
(Students should write the answer given here in the form of differences.)
Gastric ulcer and duodenal ulcer are two types of peptic ulcers that occur in different parts of the gastrointestinal tract.
Here are the main differences between gastric ulcer and duodenal ulcer:
- Location
Gastric ulcer Gastric ulcer occurs in the lining of the stomach.
Duodenal ulcer Duodenal ulcer occurs in the first part of the small intestine, known as the duodenum.
2) Symptoms:
Gastric ulcer Pain in these ulcers occurs immediately after eating, when the stomach is full.
The pain is not relieved after eating but it is more severe.
Other symptoms include nausea, vomiting and weight loss.
Duodenal ulcer
Pain in duodenal ulcer occurs two to three hours after eating and occurs when the stomach is empty, such as before meals or at night.
The pain of duodenal ulcer is relieved after eating because food temporarily neutralizes the stomach acid and acts as a cover around the ulcer.
3) Age and gender distribution:
Gastric ulcer
Gastric ulcer is usually more common in older adults, i.e. above 60 years of age. There is usually no gender difference in this.
Duodenal Ulcer
Duodenal ulcers are usually more common in young individuals, especially between the ages of 30 and 50.
Duodenal ulcers are more common in men than women.
4) Causes:
Common Causes for Both Ulcers:
Helicobacter pylori (H.pylori) infection: The major cause of both types of ulcers.
Non-steroidal anti-inflammatory drugs (NSAIDs): Such as aspirin and ibuprofen, which damage the stomach lining.
Lifestyle factors: Stress, smoking, excessive alcohol consumption, and certain types of diets are responsible for the development of ulcers.
Specific Differences: Gastric ulcers are more commonly associated with nonsteroidal anti-inflammatory drug (NSAID) use and are less commonly caused by Helicobacter pylori (H. pylori) infection, compared to duodenal ulcers.
5) Complications:
Gastric ulcers:
These have a higher risk of bleeding, especially if blood vessels are affected, and may also have a higher risk of becoming malignant (cancerous).
Duodenal ulcers:
These ulcers have a higher risk of perforation, where the ulcer creates a hole in the duodenal wall. The risk of malignancy is lower compared to gastric ulcers.
6) Diagnosis:
Both types of ulcers are diagnosed using similar methods.
1) Endoscopy
In this procedure, a thin, flexible tube with a camera is inserted through the mouth to visualize the stomach and duodenum.
2) Barium swallow X-ray
This procedure is currently used less frequently but is used to visualize whether an ulcer is present or not.
3) H. pylori test
This involves breath, blood, and stool tests, and a biopsy is also done at the time of endoscopy.
7) Treatment
There are general treatment approaches for both ulcers.
1) H. pylori eradication
If H. pylori is present, antibiotics should be provided.
2) Proton pump inhibitors (PPIs) or H2 receptor antagonists
to reduce stomach acid production and promote healing.
3) Discontinuation of non-steroidal anti-inflammatory drugs (NSAIDs)
if non-steroidal anti-inflammatory drugs (NSAIDs) are the cause.
4) Lifestyle modifications
such as dietary changes, reducing alcohol intake, stopping smoking, and managing stress.
Understanding the differences between gastric and duodenal ulcers helps in their diagnosis and management, as well as in getting appropriate treatment and reducing complications.
d) Inflammation
Definition.
Inflammation is the local response of living cells to injury to the body by any agent (microorganism).
Inflammation is the response of the body to an antigen that has entered.
The process of inflammation causes a malfunction in the body’s immune system.
Inflammation is a process in which the body’s white blood cells and chemicals protect the body from foreign substances or infectious agents.
It is a protective reaction of localized tissue, which causes localized pain, redness, swelling and sometimes loss of function.
Damaged tissue due to injury stimulates the entire process of inflammation. Which is a local response given by the skin and other tissues. Due to which redness, heat, swelling are seen. Due to the increase in blood supply, that area is also seen as hot.
All these elements are caused by the activity of immune cells
Types of Inflammation (Type of Inflammation).
Acute Inflammation (Acute Inflammation).
Acute inflammation is seen as rapid onset (progressing quickly). In which local vascular and exudative changes are seen. Its duration is less than two weeks. Immediate response is seen in acute inflammation. When the injurious agent (microorganism) is removed, inflammation subsides and healing begins with the return of normal function. Eventually, the structure returns to normal.
Chronic Inflammation.
Chronic inflammation occurs when the agent continues to cause injury. Symptoms persist for a long period of time, lasting months or years.
Chronic inflammation is characterized by proliferative changes at the site of injury. This cycle involves cellular infiltration, necrosis, and fibrosis, leading to permanent tissue damage.
Sub Acute Inflammation.
Sub acute inflammation is a phase between acute inflammation and chronic inflammation. In which elements are activated like in the acute phase and repair occurs like in the chronic phase.
Etiology.
Exogenous factors
(1) Physical factors
Mechanical agents
Inflammation occurs due to fractures, foreign substances
Thermal agents
Inflammation occurs due to burns, freezing
Chemical agents
Inflammation occurs due to chemicals such as toxic gases, acids, bases, drugs and venoms
(2) Biological factors
Inflammation occurs due to bacteria
Viruses
Parasites and fungi
Endogenous factors
Circulation Disorders
Thrombosis
Infarction
Hemorrhage
All of the above causes inflammation.
Systemic and Local Signs of Inflammation
Redness _Vasodilation causes blood to pool more, causing redness.
Warmth _Vasodilation increases blood flow, causing local area to warm.
Edema (swelling). _Edema occurs when leukocytes and fluid enter the circulatory system. Swelling occurs because of increased blood supply to the area of inflammation and limited venous return from that area.
Purulent exudate
Pain. _ Local area swelling due to compression of nerve endings.
Loss of function
Fever
Weakness
Increased respiration
Increased pulse
Increased WBC count
Treatment of Inflammation.
Inflammation is the body’s short-term or long-term response to a stimulus. During this response, it is necessary to take treatment to minimize the changes and discomfort that develop in the body. The following treatment is given during inflammation.
Non-steroidal anti-inflammatory drug (NSAID)
This drug inhibits the production of prostaglandins from the cells
Medicines such as paracetamol, ibuprofen etc. can be given for this.
Corticosteroids
Steroids inhibit the formation of prostaglandins and inhibit the function of white blood cells that play an important role in the inflammatory process. They also suppress the body’s temporary immunity so that the body’s resistance can be minimized.
Antihistamines
Histamine is a chemical that is produced by WBCs and connective tissue cells, such as basophils and mast cells, which secrete histamine in an allergic response. Antihistamines can reduce symptoms of local inflammation by blocking the production of basophils and mast cells.
Hot and cold therapy
Cold therapy causes blood vessels to narrow, which blocks inflammation, reduces pain, and cools the area.
Hot applications increase symptoms of inflammation but can help with muscle spasms or cramps.
Nursing Management of Inflammation..
Assessment
Ask the client about risk factors, nutrition, medication use, location, duration, redness, pain, swelling.
Check the movement and circulation of the injured part and check for any discharge.
Nursing Management
Pain
Assess the level of pain using a pain scale.
Provide comfort measures such as back rubs, comfortable positions, and mind diversional activities.
Administer analgesics and anti-inflammatory drugs as ordered by the doctor.
Encourage rest.
Apply hot and cold applications to relieve pain.
Elevate the inflamed part if possible.
Tissue Integrity
Provide nutritional food for the healing process
Check the circulation in the affected part and the skin of the surrounding area.
Use sterile water or normal saline to clean the inflamed part.
Clean and dry the inflamed area. Keep it open to air so that healing is good.
Prevent infection
Check the wound, whether there are any signs of infection in it such as pus, slow healing, bad smell, etc. If pus is found, send it for culture.
Check vital signs such as temperature, pulse, BP, respiration
Get WBC count test done and complete blood examination done.
Give fluids and a nutritional diet
If there is a wound, dress it with aseptic technique.
Wash hands before touching the inflamed area and wash hands after touching it
Foods rich in vitamin C
Q-5 Define following (any six) (12)
a) Biopsy
A biopsy is a medical procedure in which a small sample of tissue is collected from the body for examination under a microscope.
This is done to diagnose diseases, usually to determine whether a tumor is benign or malignant (cancerous).
A biopsy can be done on any part of the body and is usually done using a needle, but sometimes a surgical procedure is required.
The collected tissue is examined by a pathologist, who provides a detailed report on the presence, type, and severity of any abnormalities found.
b) Hemorrhoids
Hemorrhoids are enlarged blood vessels that are located in the anus and rectum.
They can develop both internally and externally in the anus and rectum.
Common symptoms include pain, itching, swelling, and bleeding.
Hemorrhoids are caused by increased pressure on the lower anus due to chronic constipation or diarrhea, obesity, pregnancy, and heavy lifting.
c) Pleural effusion Pleural effusion
Pleural effusion is the accumulation of excess fluid between the layers of the pleura outside the lungs. The pleura is a thin layer that covers the inside of the lungs and chest cavity and helps to facilitate the movement of the lungs during breathing.
When excess fluid accumulates in the pleural space, it can cause symptoms such as chest pain, difficulty breathing, and coughing.
d) Colostomy Colostomy
A colostomy is a surgical procedure in which a portion of the large intestine (colon) is removed to create a stoma (opening) in the abdominal wall, called a colostomy.
This opening is used to drain fecal matter, or stool, into a pouch connected to the stoma.
e) Quadriplegia
Quadiplegia is a medical condition in which there is complete paralysis of both upper arms and both legs.
This condition is usually caused by damage to the cervical (upper) spinal cord, resulting in loss of motor and sensory function below the level of injury.
f) Hyponatremia
Hyponatremia is a medical condition characterized by a lower than normal amount of sodium in the blood.
Sodium is an essential electrolyte that helps regulate water balance, nerve function, and muscle function.
The normal value of sodium levels in the blood is usually between 135 and 145 milliequivalents (mEq/L). Hyponatremia occurs when its level falls below 135 mEq/L.
g) Pneumothorax
Pneumothorax, commonly known as a collapsed lung, is a medical condition in which air enters the pleural space, the space between the lung and the chest wall.
Pneumothorax is the accumulation of air in the pleural space.
The pressure of this air causes the lung to collapse, leading to problems with lung function.
h) Hypoxemia
Hypoxemia is a medical condition characterized by a lower than normal amount of oxygen in the blood.
A lower than normal oxygen level, especially in arterial blood, is called hypoxemia.
It is a critical condition because the body’s cells and tissues need oxygen to function properly.
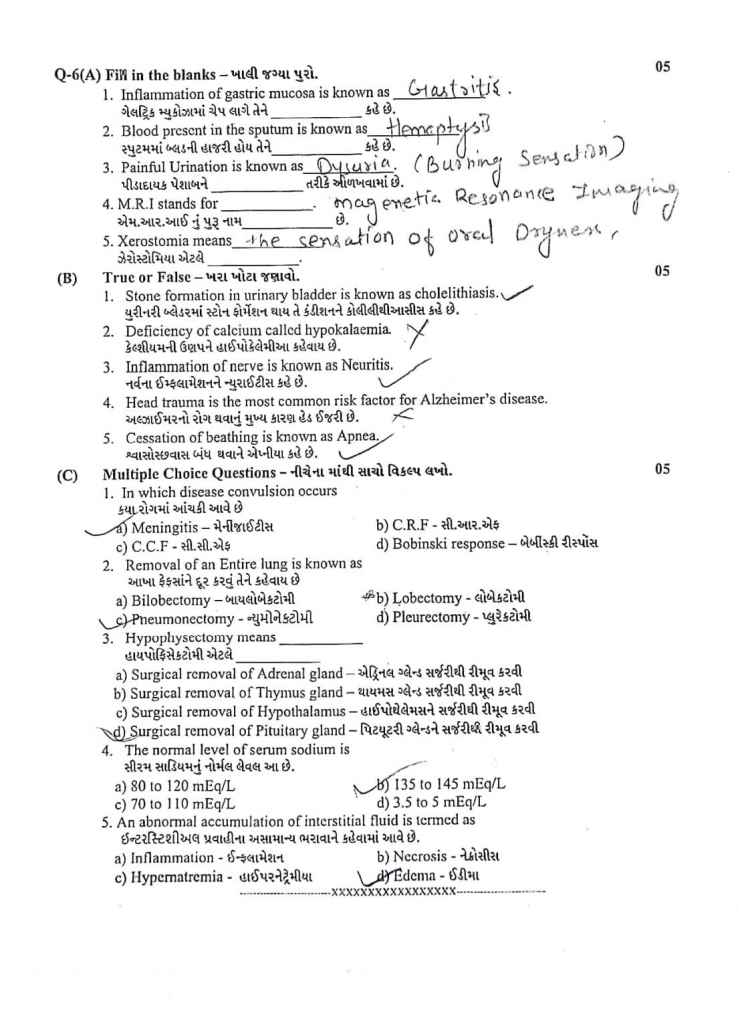
Q-6(A) Fill in the blanks .05
1.Inflammation of gastric mucosa is known as………….gastritis
2. Blood present in the sputum is known as…………hemoptysis
3.Painful Urination is known as ………………… Dysuria
4.M.R.I stands for …………..Magnetic Resonance Imaging.
5.Xerostomia means ……………………Dryness of Mouth
(B) True or False –
1.Stone formation in urinary bladder is known as cholelithiasis. .❌
2.Deficiency of calcium called hypokalaemia. .❌
3.Inflammation of nerve is known as Neuritis. .✅
4.Head trauma is the most common risk factor for Alzheimer’s disease. ❌
5.Cessation of beathing is known as Apnea. ✅
(C) Multiple Choice Questions –
1.In which disease convulsion occurs
a) Meningitis –
b) C.R.F –
c) C.C.F
d) Bobinski response –
2.Removal of an Entire lung is known as
a) Bilobectomy
c) Pneumonectomy –
b) Lobectomy –
d) Pleurectomy
3.Hypophysectomy means
a) Surgical removal of Adrenal gland –
b) Surgical removal of Thymus gland
c) Surgical removal of Hypothalamus –
d) Surgical removal of Pituitary gland –
4.The normal level of serum sodium is
a) 80 to 120 mEq/L
c) 70 to 110 mEq/L
b) 135 to 145 mEq/L
d) 3.5 to 5 mEq/L
5.An abnormal accumulation of interstitial fluid is termed as
a) Inflammation –
b) Necrosis
c) Hypernatremia –
d) Edema –