ENGLISH – MIDWIFERY PRACTICAL SAMPLE TY GNM
SAMPLE VIVA TABLE
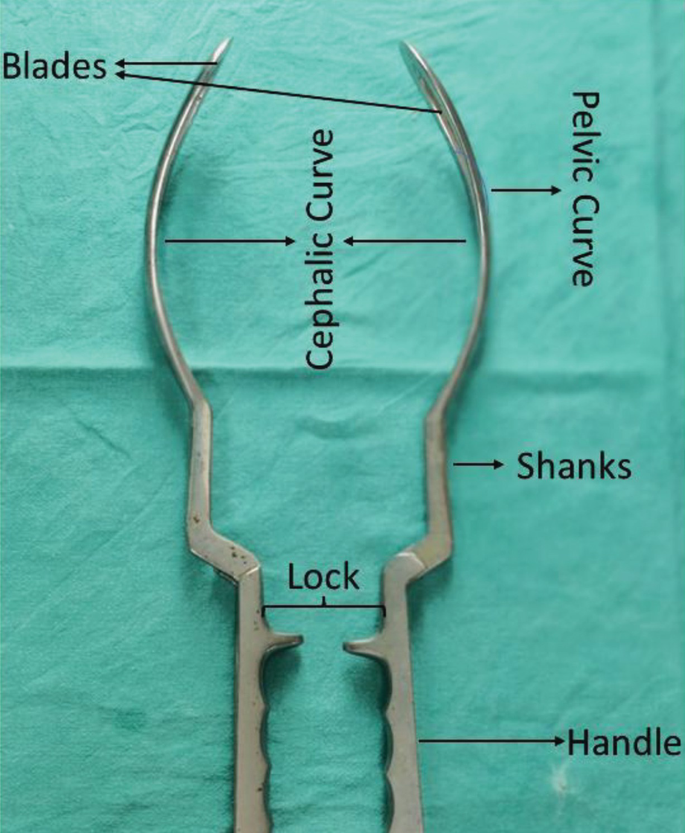
- OBSTRETIC FORCEPS

Definition: Obstetric forceps are specially designed instruments which are helpful for delivery of the head and delivery of the fetus through this instrument.
Varieties of -obstetric forceps: Three forceps are used in obstetric practice.
- Long curved forceps with or without axis traction device
- Short curved forceps
- Kielland’s forceps
acronym of forceps
F – Favorable head position and station
O – Open orifice
R – rupture membrane
C – Contraction present
E – Engage head
P – Pelvi Materi –(Major Cephalopelvic Dis Proportion)
S – Lithotomy Position
Characteristics
Blade — The blade is used to grip the fettle head nicely
There are two curves of the blade
a. Pelvic curve –– The pelvic curve is fixed in the birth canal and forms a circle with a radius of 17.5 cm.
b. Cephalic curve — The cephalic curve is a flat surface that articulates with the fetal head without compression of the fetal head and the radius of this curve is 11.5 cm.
Shank — The part between the blade and the lock, its length is 6.25 centimeters, it increases the length of the instrument and facilitates the outside of its lock valve.
Lock – There is a lock near the junction of the handle through which we can easily lock the instrument.
Handle — The handle is opposite to where the attachment of the blade is located and is 12.5 cm long and has screws attached to the end of the blade.
Use– long curved forceps are used by medical professionals for child birth during delivery when a complication arises and these forceps are carefully inserted inside the birth canal and held evenly around the baby’s head.
Kielland’ forceps is also used in an unrotated vertex or face presentation
Short curved -obstetric forceps are used in forceps delivery.
The sterilization process typically involves several steps:-
1.Cleaning –– Remove any debris, blood or any contamination from the forceps.
2.Disinfection –– After cleaning the forceps, the dish should be disinfected so that any micro-organisms present can be removed.
Glutaraldehyde is used for dish infections.
3.Sterilization — This stage is the last stage of sterilization in which all micro organisms and bacteria viruses and their spores are eliminated.
Methods like autoclave chemical sterilization, dry hit sterilization, etc. are used for sterilization.
- Placenta:
Definition:
The human placenta is ‘discoid’, ‘hemochorial’ and ‘deciduate’. The placenta is attached to the wall of the uterus and provides a connection between mother and fetus via the umbilical cord.
Placenta is a circular disc, spongy, flaky structure, thicker at the center and thin at the corners.
Placenta origin:
Placenta originates from the trophoblastic layer of the fertilized ovum.
It is closely linked with the mother’s circulation and helps the function of the fetus during intrauterine life.
Attachment of placenta:
The placenta is attached to the wall of the uterus and provides a connection between the mother and the fetus through the umbilical cord. It performs many functions and maintains pregnancy.
Development of placenta:
1.fetal component: The fetal side develops from the chorion frondosum.
2.maternal component: It is formed by decidua basalis.
Diameter and thickness of placenta:
1.Diameter : 15-20 cm
2.Thickness: 3 cm
- Weight : 500 g
4.Surface area: 243 sq.cm - Volume : 500 ml
Surface:
Fetal surface:
Maternal surface
Peripheral margin
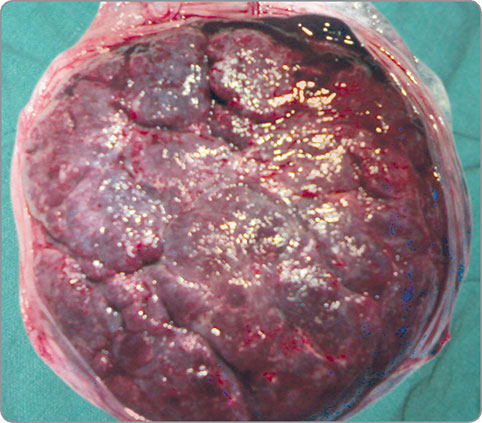
1. fetal surface

The fetal surface is smooth and covered with glistening amnion. In its center is the umbilical cord
Umbilical vessels are visible below the amnion.
Amniotic membrane to chorionic
Can be separated from the plate but not from the umbilical cord.
4/5th placenta is of fetal origin.
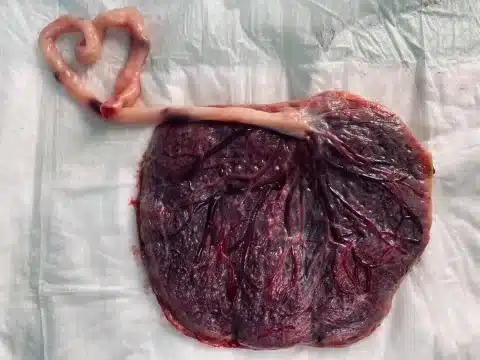
2.maternal surface
Maternal surface is rough and spongy.
Maternal blood causes its dull red appearance.
It consists of 15 to 20 maternal cotyledons which are separated by sulci.
Many small gray colored sports are visible due to calcium deposition.
Its share is 1/5.
3.peripheral margin
It is formed by the fusion of the basal and chorionic plates
It is continuous with chorion leave and amnion
Attachments
Placenta is attached anteriorly or posteriorly to the upper part of the uterus.
Circulation
1.maternal circulation
2. fetoplacental circulation
1.maternal circulation
Maternal circulation is not fully established until the end of the first trimester.
First theory:
During that trimester, endovascular trophoblasts migrate up the decidual spiral arteries so that maternal blood perfuses into the placental intervelar space.
The second theory:
The tophoblast invades the decidual spiral arteries and forms the trophoblastic plug.
The trophoblastic plug prevents maternal blood flow into the intervillous space until the first trimester.
The plug then loosens and permits maternal blood flow into the continuous intervillous space.
The volume of mature placenta is 500 ml.
Of which 350 ml is in the villi system and 150 ml in the intervillous space.
The blood in the intervillous space is completely replaced three to four times a minute.
The intervalsal space has a pressure of 10 to 15 mmHg during uterine relaxation and 30 to 50 mmHg during uterine contraction.
Blood in maternal sinus remains unclotted by fibrinolytic enzyme.
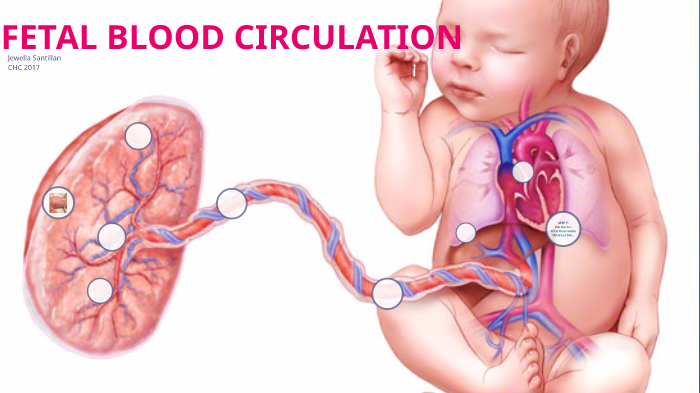
2. fetoplacental circulation
Umbilical arteries carry impure blood from the fetus and supply the placenta.
Arteries divide into small branches and form primary secondary and tertiary vessels.
Blood passes through the terminal capillaries into the venous system.
Due to this, gas exchange takes place between the blood of the mother and the fetus.
Fetal blood moves to the placenta at a minute flow of 400 ml.
Function of placenta
Fetal respiratory function
Fetal alimentary function
Fetal endocrine function
Fetal barrier function
Enzymatic function
Immunological function
Respiratory function
Pulmonary exchange of gas does not occur during intrauterine life. Fetal respiratory function is by simple diffusion.
Oxygen travels from the placenta through the umbilical cord to the fetus by diffusion.
Fetal alimentary function
All nutrients such as glucose, amino acids, lipids, vitamins, water and electrolytes pass through the maternal sinus into the fetal circulation.
Glucose is transferred by facilitated diffusion.
Fatty acids and triglycerides are freely transported.
Cholesterol is made by the fetus.
Water soluble vitamins are actively transported.
Fat soluble vitamins are slowly transported.
Water and electrolytes cross by simple diffusion.
Minerals such as ions calcium and phosphorus are actively transported.
fetal endocrine function
The main job of the placenta is to produce hormones that maintain the pregnancy.
Placenta acts as an additional endocrine gland.
It produces protein hormone and steroidal hormone.
A. protein hormone
1.human chorionic gonadotrophin
It is produced from the cytotrophoblastic layer.
2. human placental lectogen
It is also produced by the placental.
Through it, the metabolic process takes place during pregnancy.
B. steroidal hormones
1. Progesterone
It is produced by the placenta.
It maintains the pregnancy.
Progesterone levels drop during labor.
2. Estrogen
It is produced in large amounts during pregnancy.
Estrogen also maintains pregnancy.
fetal barrier function
Fital membrane performs a protective function.
It protects the body from many harmful agents.
It does not allow substances of large molecular size to reach the fetus.
At the end of pregnancy, small antibodies can reach the fetus.
Protects the fetus from some harmful substances like tubercle bacilli, poliomyelitis virus etc.
enzymatic function
Many placental enzymes are involved in hormone synthesis and metabolism.
such as oxytocin.
immunological function
Placenta is an allograft for the uterus.
However, no graft rejection is observed in pregnancy.
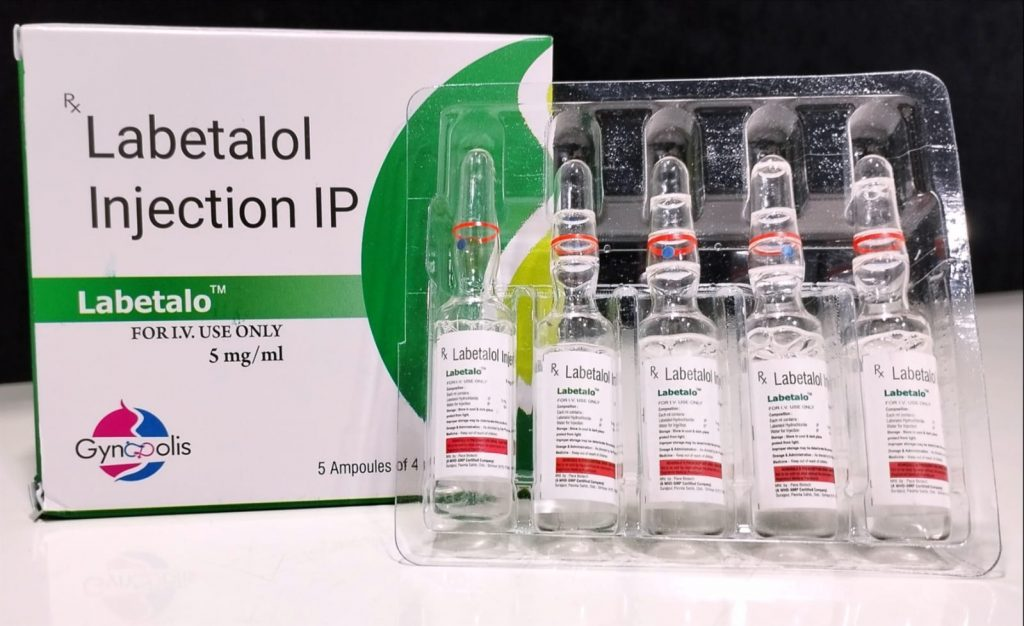
- Labetalol :-

Group:- Alpha (alpha) and beta (beta) adrenergic antagonist
Dose :- 1ml -5mg, 20mg/4ml
Route :- intravenously (lv only), ORAL
Mode of action :-
Labetalol combines both selective competitive alpha one blocking and non-selective beta receptor blocking activity in a single substance.
Labeta Lol is a beta blocker medication that relaxes blood vessels and slows the heart rate, decreasing blood flow and blood pressure.
Use :- High blood pressure in pregnancy can cause complications for mother and baby.
Labetalol is a blood pressure medication used to lower blood pressure during pregnancy.
Indication:-
High blood pressure
preeclampsia
Eclampsia
Contraindications :-
Bronchial asthma
Cardiac failure
Cardiogenic shock
Severe bradycardia
Severe hypotension
Hypersensitivity
Side effects:-
Labetalol affects the growth of the baby in the womb.
Affects the baby’s blood sugar level.
Patient feels dizzy, sleepy and weak.
Head one
Cold fingers or toe
Nausea or vomiting.
diarrhea (diarrhoea)
Stomach pain
•√. Labetalol first line choice in pregnancy :-
Because reduces hypertension during pregnancy with every prescribed antihypertensive drug, but labetalol reduces hypertension, protein urea, and fetal/newborn death rates.
Nursing responsibility:-
To maintain the seven rights of the patient.
Right route
Right dose
Right client
Right time
Right drug
Right information to client
Right to refuse
Monitor blood pressure and pulse frequently during dose adjustment and periodically during therapy.
See the patient for complications.
Patient receiving i/v labetalol must be in supine position 5. Patient recommended supine position after three hours of drug administration.
Monitor patients intake and output chart and weight chart daily.
Watch for out come of drug administration.
(TO READ FULL VIVA CONTENT PLEASE TAKE SUBSCRIPTION)