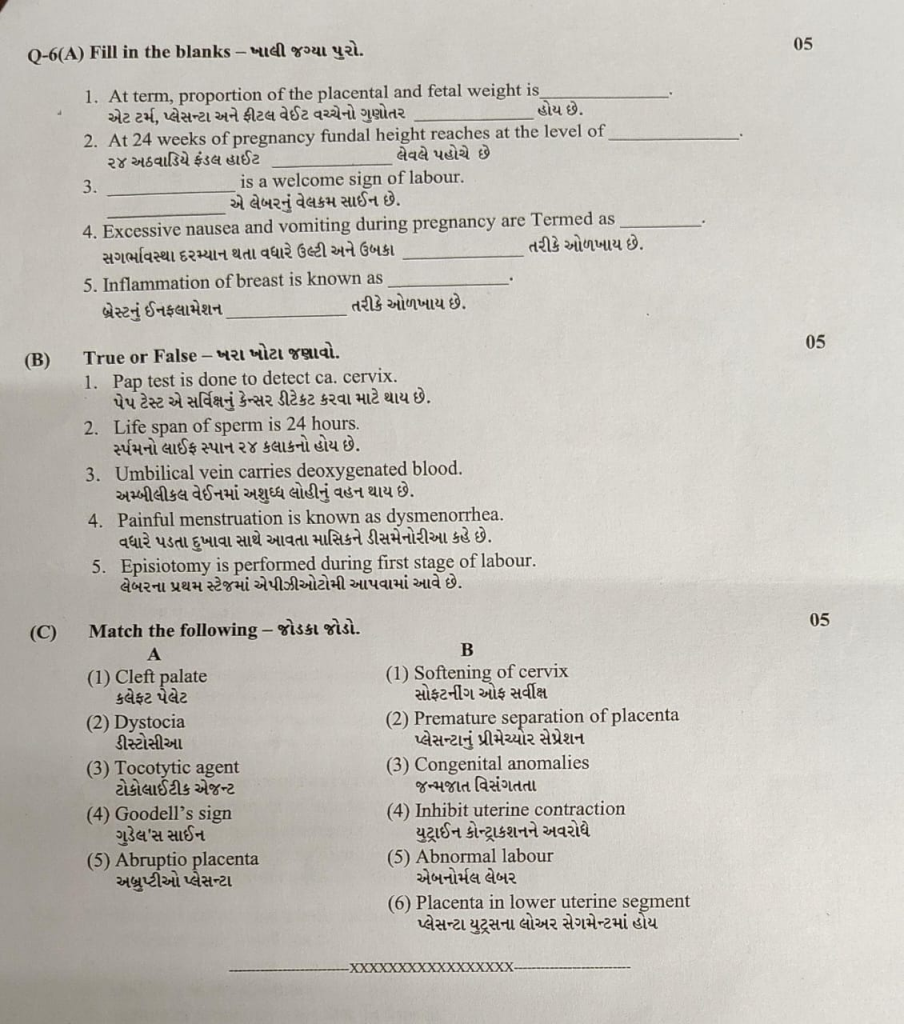
ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING (PAPER SOLTION : 07/07/2025)-Upload no.12
GNM-T.Y MIDWIFERY AND GYNECOLOGICAL NURSING (PAPER SOLUTION : No.12 07/07/2025)

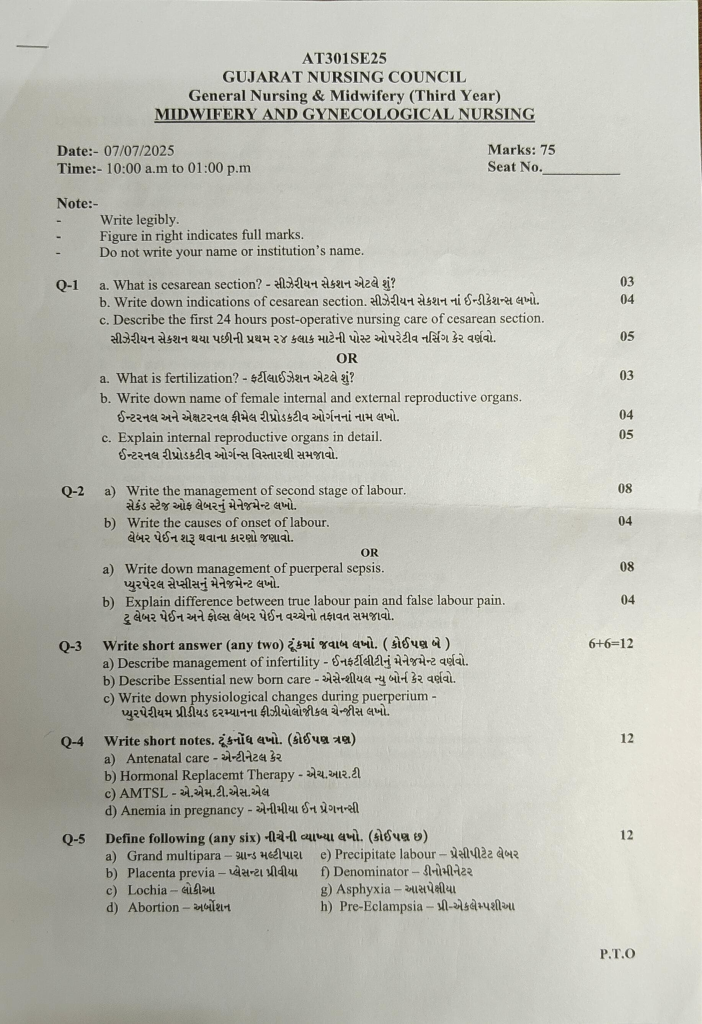
Q – 1 a. What is cesarean section? What is caesarean section? 03
Caesarean section is a surgical procedure in which an incision is made on the abdomen to deliver the baby from the uterus and the baby is delivered through it.
The types of caesarean section are as follows.
1.Based on the timing of delivery (According to the time of delivery):-
- Elective caesarean section:- In this type, caesarean It is already planned.
Indication – Previous Caesarean section, breech presentation, placenta previa etc… - Emergency Caesarean Section:-It is unplanned. Emergency caesarean section is performed when vaginal delivery is not possible.
Indication – Fetal distress, prolonged labour, uterine rupture…
2.Based on the uterine incision (uterine incision):-
- Lower segment caesarean section:- It is the most common type. In which a horizontal incision is made in the lower segment.
Advantages – It reduces blood loss, the chances of uterine rupture are less and healing also comes earlier. - Classical Cesarean Section:- In which a vertical incision is made in the upper segment.
Disadvantages – The chances of uterine rupture are higher.
3.Based on the approach of surgery (According to the approach of surgery)
open cesarean section:- In which A wide incision is made on the abdomen.
It is performed in patients with emergency pregnancy or multiple previous surgeries.
Minimal-invasive cesarean section :- In this, the baby is delivered through a minimally invasive technique on the abdomen.
b. Write Down indications of cesarean Section . Write down the indications of cesarean section. 04
Indications for Caesarean Section:
Indications for Caesarean Section are divided into two categories:
- 1)Absolute, (in which vaginal delivery is not possible)
- 2)Relative (in which vaginal delivery is possible but the mother and baby are Risk)
1) Absolute, (in which vaginal delivery is not possible):
- Central placenta previa,
- Severe degree contracted pelvis,
- Cervical or broad ligament fibroid,
- Vaginal atresia/obstruction,
- In advanced cervical carcinoma,
- Cephalopelvic disproportion,
- Obstruction due to pelvic mass,
- Fetus is dead.
2) Relative (in which vaginal delivery is possible but there is risk to mother and baby):
- Cephalopelvic Disproportion,
- Contracted pelvis,
- Previous cesarean delivery,
- Fetal distress,
- Abnormal uterine contractions,
- Large fetuses,
- Small Pelvis,
- Failed induction,
- Antepartum hemorrhage such as placenta previa, placental abruption.
- Malpresentation or abnormal lie (transverse lie).
- Bad obstetric history,
- Hypertensive disorders such as preeclampsia,
- Prolapse of Umbilical Cord,
- Elderly Primigravida,
- Medico-Gynecological Disorders:
- Chronic Hypertension,
- Chronic Nephritis,
- Diabetes,
- Heart Disease,
- Pelvic Tumor,
- Vaginal Atresia,
- Carcinoma of Cervix,
- Cervical Dystocia.
Common Indications for Cesarean Section
1) Failure to Progress in Labor: Prolonged labor in which the cervix does not dilate properly and the fetus does not descend properly into the birth canal, requiring a cesarean section.
2) Fetal Distress: Signs that the fetus is not able to tolerate labor properly, such as an abnormal fetal heart rate, indicate reduced oxygen supply to the fetus, requiring a cesarean section.
3) Malpresentation of Baby: When the baby is breech In presentation (buttocks as the presenting part), transverse position, due to which vaginal delivery becomes impossible and there is a need for cesarean section.
4) Placental abnormality:
Placenta previa:
In which the placenta is partially or completely implanted on the lower uterine segment, i.e. when the placenta is present as the presenting part.
Abruptio placenta
In which the placenta separates prematurely from the uterine wall, there is also a need for cesarean section.
5) Maternal health conditions
such as genital herpes,
heart disease,
severe hypertension,
conditions like .
6) Previous Cesarean Section: If a previous Cesarean Section has been performed, then the repeat Cesarean Section depends on the scar of the previous CS and the duration of the pregnancy.
7) Multiple Pregnancy: When there is a multiple pregnancy such as twins, triplets and the presenting part and position of the fetuses, there is a need to perform a Cesarean section is.
8) Umbilical Cord Prolapse: In which the umbilical cord slips down through the cervix, which can cut off the blood supply to the fetus.
9) Maternal Request: In some cases, the mother herself chooses a cesarean section due to personal and psychological reasons.
10) Emergencies During Labor:
To protect the health of the mother and baby due to complications during labor such as uterine rupture, severe bleeding, and maternal illness, and For their safety, an immediate cesarean section is required.
Thus, a cesarean section is required in all these conditions.
c. Describe the First 24 Hours Post – operative nursing care of cesarian section. Describe the first 24 hours post – operative nursing care of cesarian section. 05
Post-operative Nursing Care:
First 24 hours (0 days):
Properly assess the patient’s vital signs such as pulse, blood pressure during the first six to eight hours of observation.
Record the amount of vaginal bleeding and the behavior of the uterus.
The patient’s Properly maintain hydration status, including continuous administration of sodium chloride (0.9%)/Ringer lactated drip up to 2-2.5 liters of solution.
If blood transfusion is required in an anemic mother, prepare for it.
Properly maintain the patient’s intake-output chart.
Drugs such as inj. Oxytocin 5 units IM/IV (slow) or Methergine 0.2 mg IM, followed by prophylactic antibiotics and analgesics as ordered.
Ambulation: If the patient’s general condition is good, she can sit up in bed and go to empty her bladder.
Encourage the patient to move her legs and ankles and take deep breaths.
Advise the mother to start breastfeeding within three to four hours when her pain has subsided and she is stable.
Also, keep monitoring the baby’s vital signs and general condition and refer immediately if any abnormalities are found.
OR
a. What is Fertilization? What is Fertilization? 03
Fertilization is the process of fusion of sperm and ovum, which forms a zygote. This process mainly takes place in the ampulla of the Fallopian tube.
Main stages of fertilization:
- Sperm Transport:
- During copulation, sperm is deposited in the vagina. And reaches the fallopian tube through the uterus.
- Capacitation of Sperm:
- The sperm completes the capacitation process with enzymes present in the uterine and tubal fluids, which enables the sperm to cross the zona pellucida of the ovum.
- Acrosome Reaction:
- Hyaluronidase and other enzymes present in the acrosome break down the zona pellucida of the ovum.
- Penetration and Fusion:
- The sperm fuses with the plasma membrane of the ovum.
- The nucleus of the sperm fuses with the nucleus of the ovum and a diploid zygote is formed.
b. Write down name of female internal and External Reproductive organs. Internal and External Female Reproductive Organs ना ना सम्मेल रेपडिक्षण. 04
1. External genitalia of female / VULVA / PUEDENDAM
- Mons pubis
- Labia majora
- Labia minora (labia minora)
- Clitoris
- Perineum
- Vestibule (Vestibule)
- Mammary gland
MONS PUBIS (Mons Pubis):
- The mons pubis is a cushion-like structure made of fat and skin. Which lies in front of the symphysis pubis.
- During puberty it becomes covered with hair and forms a horizontal margin.
LABIA MAJORA (Labia Majora):
- These are two thick folds on the front side. Which form the brim of the vulva. (The vulva is the external reproductive organ, also called the vulva).
- The labia majora are made up of skin, fat, areolar tissue, and smooth muscle. On the upper surface of which hairs are located. On the inner side of it are sebaceous glands.
The round ligament ends the labia majora. - The labia majora meet anteriorly near the mons pubis and posteriorly they meet near the skin of the perineum. Just as the male has the scrotum, the female has the labia majora.
LABIA MINORA:
- Labia minora are two small skin folds (which do not have fat or hair inside but have many sebaceous glands) that are located inside the labia majora.
- Their upper part meets the clitoris and forms the prepuce (prepuce – just like the foreskin on the penis in males, the cover of the clitoris in females), and the lower part forms the floor (frenulum) of the clitoris.
CLITORIS:
- It is of cylindrical (cylindrical) shape and triangular shape. It is made of erectile tissue (stimulating).
- It is like the penis in males, it is the clitoris in females.
It contains sensory nerve endings. It works as an arousal during sexual intercourse.
PERINEUM:
- This is an area that extends from the base of the labia majora to the anal canal. It is roughly triangular in shape.
- It is made up of connective tissue, fat, and muscle. It provides attachment to the muscles of the pelvic floor.
VESTIBULE:
- Vestibular glands (Bartholin glands) are 2 and are located on either side of the vaginal opening. They are about the size of a pea. They have ducts that open into the vagina and secrete mucous. This keeps the vulva moist and the vaginal cavity wet.
- INTERNAL REPRODUCTIVE ORGANS:
These organs are located inside the pelvic cavity. Which includes the following organs.
Internal reproductive organs are as follows.
- Vagina
- Uterus
- Uterine tube or Fallopian tube or Salpinges
- Ovaries
c. Explain internal reproductive organs in Detail.Internal reproductive organs in detail.05
INTERNAL REPRODUCTIVE ORGANS :
These organs reside within the pelvic cavity. They include the following organs.
Internal reproductive organs are as follows.
- Vagina
- Uterus
- Uterine tube or Fallopian tube or Salpinges /Sulfingus)
- Ovaries.
VAGINA:
- The vagina is a fibromuscular tube. Its lining is made up of stratified squamous epithelium cells. Which is the structure that connects the internal and external reproductive organs.
- It is located in front of the urinary bladder and behind the rectum. Its front wall is 7.5 cm and its back wall is 9 cm.
Structure of Vagina
The vagina has three layers
1.Outer Layer
2.Middle Layer Layer)
3.Inner Layer
1.Outer Layer :- The outer layer is made up of areolar tissue
2.Middle Layer :- The middle layer is made up of smooth muscles.
3.Inner Layer :- Made up of stratified squamous epithelium tissue. Which forms rugae (rugae – like projections).
It does not contain any secretions. It remains moist due to cervical secretions.
Between puberty and menopause, bacteria called lactobacillus acidophilus make the pH of the vagina acidic. Which is 4.9 to 3.5. Due to the acidic pH, infecting microorganisms do not enter the vagina.
Blood Supply:
Through the uterine artery and vaginal artery which are branches of the internal iliac artery.
The venous plexus is located in the wall of the muscles and drains into the internal iliac vein.
NERVE SUPPLY:
There are parasympathetic nerves, sympathetic nerves and somatic nerve supply
FUNCTIONS:
- The vagina allows the entry of the penis during intercourse.
- It holds the sperm until it moves to enter the uterus.
- It is an elastic structural part that helps the baby to come out during birth.
- The sensory nerve endings in the vagina provide the feeling of sexual pleasure.
- It acts as the outer opening of the urinary tract.
- Women experience monthly menstrual bleeding, in which blood from the uterus comes out through the vagina.
- The acidic pH of the vaginal cavity inhibits the growth of microorganisms.
UTERUS:
- The uterus is a hollow and muscular inverted pear-shaped organ. It is located within the pelvic cavity. Which is located between the urinary bladder and the rectum.
- In most women, the uterus is bent forward (anteflexion) and forward (anteversion) and is at a right angle (90°- right angle) to the vagina.
- Its anterior wall is attached to the bladder and forms the vesicouterine pouch. The pouch of peritoneum that forms between the bladder and the uterus is called the vesicouterine pouch.
- When the body is in an upright position, the uterus The length of the uterus is 3 inches, the width is 2 inches and the thickness is 1 inch. Its weight is 30 to 40 grams.
The parts of the uterus are as follows :
- Fundus:- It is dome-shaped. The uterine tube opens from its upper part.
- Body:- The body is the main part. The uterus becomes narrower as it goes down. It forms the internal os (mouth). Which continues forward to form the cervix.
- Cervix:- It is called the neck of the uterus. It opens or protrudes into the anterior part of the vagina. Its opening is called the external os (os).
STRUCTURE:
The uterus has 3 layers:
Perimetrium
Myometrium (myometrium)
endometrium (endometrium)
Perimetrium:
- This is a layer of peritoneum. It is spread around the uterus. On the front side, there is a fold of peritoneum on the fundus and body and on the upper side, there is a fold of peritoneum on the urinary bladder.
- The pouch of peritoneum that forms between the uterus and the bladder on the front side is called the vesico-uterine pouch while on the back side, the peritoneum reaches from the fundus to the cervix. The pouch that forms between the rectum and the uterus on the back is called the pouch of Douglas or the rectouterine pouch.
- Laterally (on the side) it is double folded. The layer of peritoneum forms the broad ligament and the round ligament on the side, which join the uterus to the pelvis.
MYOMETRIUM (myometrium):
- This is the thickest layer of the uterus. It contains a mass of smooth muscle and is accompanied by areolar tissue, blood vessels and nerves.
ENDOMETRIUM (Endometrium):
It is made up of columnar epithelium tissue and is lined by tubular cell glands that secrete mucus.
It has two layers in total.
- Functional layer (functional layer)
- Basal layer
1.Functional layer
- It is the upper layer. It is rich in blood vessels for the first 15 days or half of the cycle and if the ovum (egg) is not fertilized then this layer is shed (shed) and menstruation begins.
- If fertilized then it remains for 9 months (pregnancy) and then sheds and during 9 months it is called decidua.
2.Basal layer
This is the layer that lies in front of the myometrium. It is not shed during the menstrual cycle. This is the layer from which the new and fresh layer is formed.
The 2/3rd layer of the endometrium is made up of mucus membrane and the lower part is made up of stratified squamous epithelium up to the vagina.
BLOOD SUPPLY:
Arterial supply: – Blood reaches the uterus through the uterine artery and is a branch of the internal iliac artery.
Venous drainage: – Veins are similar to arteries but blood drains into the iliac vein.
Nerve Supply:
Parasympathetic nerve supply comes from the sacrum and sympathetic nerve supply comes from the lumbar region.
Supporting Structure:
The uterus is supported by surrounding organs. Which are in the pelvic cavity and there are ligaments. Which support the uterus. Like :-
- broad ligaments
- round ligaments
- Uterosacral ligaments
- Transverse cervical ligaments
- Pubocervical fascia
The above structures help the uterus maintain its shape and provide structural support.
FUNCTIONS OF UTERUS:
- The uterus helps in the fertilization of the ovum and sperm.
- After fertilization, it helps the zygote to implant in the inner wall of the uterus and maintains the pregnancy.
- During pregnancy, the content inside the uterus increases, which also increases the size of the uterus, so that the pregnancy can continue.
- It functions to provide nutrition to the fetus in the uterus during pregnancy.
- It helps the baby to come out during delivery by contracting the muscles of the uterus.
- The endometrium, the inner wall of the uterus, breaks down during the menstrual cycle. This cycle continues every 26 to 30 days, and the chance of infection is reduced due to the influx of wbc.
FALLOPIAN TUBE/ SALPHINGES / MULERIAN DUCT / UTERINE TUBE (Fallopian tube, Salphinges, Mullerian duct, Uterine tube):
They are 2 in number. They are attached to the fundus and body and there is one on both sides of the fundus. They are 10cm long.
Its main parts are as follows.
- Interstitial:- This part is attached to the uterus. It is the part of the uterus that begins after the fundus.
- Isthmus:- This is narrow and is approximately 2.5 cm long.
- Ampulla:- The ampulla is the widest part of the tube. Here the ovum and sperm are fertilized.
- Infundibulum:- This is the last part of the fallopian tube and is shaped like a funnel.
At the end of this, finger-like projections are formed. These are called fimbriae. The fimbriae receive the egg cells. It has three layers
- Outer Layer (Outer Layer) which is made of peritoneum.
- Middle Layer (Middle Layer) which is made of muscles.
- Inner Layer (Inner Layer) which is made of mucus membrane and ciliated epithelium tissue.
Functions of FALLOPIAN TUBE:
- It causes the egg (ovum) to undergo peristalsis and reach the ampulla.
- The mucus secreted by it provides an ideal environment for the ova and sperm.
- The egg and sperm fertilize here and form a zygote.
- The fertilized zygote travels to the uterus.
Ovaries:
- The ovary is a female gonad. They are located on either side of the uterus in the ovarian fossa. They lie behind the broad ligament.
- They are 2 in number (pair of ovaries). It is homologous to the testis.
- It is attached to the pelvic wall by ovarian wall ligaments.
Location:
It is a structure surrounding the ovarian fossa (a fossa is a pit-like structure that contains an organ) in which it is located behind the ureters (back of the urinary tract), the obliterated umbilical The artery (which is an artery that disappears shortly after birth) is supported by
obturated intercostal muscles, vessels, and nerves in front and below.
Shape and Size:
The ovary is oval in shape. It is 3 cm long, 1.5 cm wide and 1 cm thick.
Surface And colour:
The ovary of young adults is pink in colour and smooth. In older women, it is rough, irregular, and gray in color because they have ovulated frequently.
Attachment:
Both ovaries are attached to the uterus at the top by the ovarian ligament and at the back by the broad ligament. It is called the mesovarium, blood vessels and nerves pass through the mesovarium.
Blood Supply:
It is supplied by the ovarian artery and is a branch of the abdominal aorta.
The vein is called the pampiniform plexus. It emerges from the ovary itself.
The right vein drains into the inferior vena cava and the left vein drains into the left renal vein.
Nerve Supply:
Sympathetic fibers that emerge from the T10 and T11 spinal ligaments.
Parasympathetic nerves emerge from the vagus nerve.
Histology Of Ovary:
- The ovary is oval in shape.
It is lined with a single layer of cuboidal epithelium cells. It is called the germinal epithelium. - It is lined with dense tissue. It is called the tunica albinia and is located inside the germinal epithelium.
It has a total of 2 parts.
Medula:- Made of connective tissue and connected by a network of blood vessels and made of elastic fibers.
Cortex:- It is made of the stoma and follicles of the ovary.
Q -2 a) Write the management of Second Stage of Labour. Write the management of Second Stage of Labour. 08
Second Stage of Labour Management:
- The transition from the first stage of labor to the second stage occurs due to the following features:
- Due to the increase in the intensity and frequency of uterine contractions.
- Due to the increase in the bearing down efforts of the mother.
- With the descent of the presenting part of the fetus, there is an urge to defecate.
- Complete dilation of the cervix occurs.
- Principles of the second stage of labor
- To facilitate the slow and natural expulsion of the fetus.
- To prevent perineal injury.
General measures:
- Advise the patient to lie down properly on the bed.
- Constantly observe the patient for the following signs:
- Continuous monitoring of fetal heart rate (FHR) at every five minute interval.
- Properly note the mother’s vital signs, mainly pulse and blood pressure, at 15 minute intervals.
- Proper reassurance should be provided to the mother so that her moral support can be properly maintained.
- Proper examination of the vaginal area at the beginning of the second stage to confirm the onset of labor and to prevent accidental coda prolapse.
- Properly assess the position and station of the fetal head.
Preparation for Delivery:
- When signs of “OS” dilation are observed, prepare the patient for delivery such as,
- Strong and frequent uterine contractions,
- Vulval gaping,
- Anus pouting,
- Thinning and bulging of the perineum.
- In primigravida, wait until the presenting part of the fetus is 4 to 5 cm into the vulva.
- Then provide the woman with a proper position.
- Wear gloves, gown and mask to maintain proper aseptic technique and then stand on the patient’s right side.
- Now the external genital organs should be properly painted with cotton swab and Dettol, then one sterile sheet should be placed under the patient’s buttocks and one sheet should be placed on the abdomen.
- Then to maintain aseptic technique, three “C” should be maintained properly such as,
- Clean hands,
- Clean surface,
- Clean cutting and ligature of cord.
- If the bladder is swollen, then catheterize it and empty it properly.
- Then check whether the membrane has ruptured or not, if not, then do Artificial Rupture of Membranes (ARM).
- Then conduct proper delivery, in which the main delivery is conducted in three phases:
- 1) Delivery of the head,
- 2) Delivery of the shoulder,
- 3) Delivery of the trunk
1) Delivery of the head:
- When delivering the head, the following principles should be followed, such as,
- Maintain proper flexion of the head.
- Prevent early extension of the head.
- The head should slowly escape out of the vulval outlet.
- If the mother’s uterine contractions are poor, then properly fit a venous line and then add 5 units of oxytocin in 5% dextrose and start its drips.
- Then advise the woman to apply bearing down forceps with each contraction and provide her with small amounts of water intake in between.
- Allow the fetal head to descend slowly before crowning.
- Perineal infiltration and episiotomy
- When the perineum is broad, tough and stretched, a proper episiotomy should be performed to prevent perineal tearing.
- When uterine contractions occur, administer 5 to 10 ml of 1% xylocaine to the perineum.
- Before the crowning stage, episiotomy is done by scissors starting from the midpoint of the forechest followed by mediolateral episiotomy at 7:30 clock (on the right side) or 4:30 clock (on the left side).
- After episiotomy, sudden escape of the head is prevented.
- Proper monitoring of slow delivery of the head between contractions is usually done by properly pushing the chin of the fetus with the right hand covered by a sterile piece of gauze and placing the right hand on the anococcygeal region and applying pressure on the occiput with the left hand.
- Then the forechest, nose, mouth and chin are born from the stretched perineum.
Care after delivery of the head:
- Immediately after delivery of the head, clean the head, mouth and fairings of the fetus with a liter finger covered with sterile gauze.
- Then clean the eyelids properly using a sterile and dry cotton swab, starting from the medial canthus and cleaning up to the lateral canthus to prevent contamination of the conjunctival sac.
- Then palpate the neck of the fetus and assess whether any loop of cord is present. Then, if the loop is present and loose, slip it off the shoulder and if tight, apply two cochlear forceps and then cut it in the middle.
Delivery of Shoulder:
- Do not rush while delivering the shoulder.
- Wait till uterine contractions and restitution and external rotation occur.
- Now, the anterior shoulder is seen below the pubis, then the head of the fetus is properly placed between the two pairs and lifted towards the mother’s abdomen, which first delivers the posterior shoulder and then the anterior shoulder.
- If the anterior shoulder is not free below the pubis, the head is depressed to bring the anterior shoulder below the pubis.
Delivery of Trunk:
- After delivery of the shoulder, insert the four fingers of both hands into the axilla and then deliver the trunk by lateral flexion.
- Immediate Care of Newborn After Delivery
- Immediate newborn care involves properly assessing and stabilizing the newborn.
- Immediate newborn care is crucial for the fetus to stabilize from intrauterine life to extrauterine life.
- Goals of Immediate Newborn Care
- 1) To establish, maintain and provide support to the newborn’s respiration.
- 2) To prevent the newborn from fever and hypothermia.
- 3) To prevent infection in the newborn.
- 4) To provide safety to the newborn and to prevent him from injury.
- 5) To provide immediate treatment by early identification of any actual and potential problems in the newborn.
- Immediate newborn care is provided.
- Immediate newborn care
1) Establishment of respiration
- When the newborn is received, the airway of the newborn should be immediately patent and the airway should be cleared properly. Due to which the newborn can breathe effectively.
- As soon as the newborn’s head is bent, wipe the mouth and nose and suck the mouth and nose so that the newborn can breathe properly. Suck first in the mouth and then in the nose so that secretions can be prevented from being aspirated.
2) Initiation of Cry
- Normally 99% of newborns cry immediately and spontaneously after delivery, this cry is known as a good sign for the newborn’s breathing.
- If the newborn does not cry properly, then follow the following steps:
- a) If the baby does not cry spontaneously or if the cry is weak, then simulate the baby to cry lightly.
- b) To stimulate the baby’s cry, rub the soles of his feet lightly instead of slapping his bottom. After removing the newborn’s secretions, stimulate the baby to start his cry.
- C) The cry of the newborn is usually loud and husky and if there is any of the following abnormal cries, then the newborn should be properly monitored such as,
- High pitched cry: = due to hypoglycemia and increased intracranial pressure,
- Weak cry: = prematurity,
- Hosacry: = laryngeal strider
3)Care of cord
- Cord care is an important immediate care of the newborn.
- The newborn’s cord should be clamped within 30 seconds of birth and then cut properly.
- After the newborn is delivered, place the newborn on the mother’s abdomen.
- Then clamp the cord properly from two opposite sites using a cord clamp.
- Apply the first clamp 5 cm away from the umbilicus, then apply the second clamp 2.5 centimeters from the first clamp.
- Then cut the cord properly between the two clamps.
- Do not apply anything to the cord, let it dry and fall naturally.
- The cord naturally falls off within seven to ten days after birth.
- Prevent the cord from getting wet with water and urine.
- If any kind of discharge and bleeding is present in the cord, then immediately assess the cord clamp and then loosen it properly.
- If the following signs and symptoms are seen from the cord, then immediately
- report such as,
- Foul odor coming from the cord,
- No discharge,
- Redness around the cord,
- The cord is wet,
- The cord does not fall down in 7-10 days,
- Inflammation,
- Fever etc.
4) Maintain position of the newborn
- The newborn is usually prone to choking, coughing and gagging during the first 12-18 hours after birth. Therefore, the newborn should be provided with proper position.
- In which the fitters should be provided with proper side lining position so that mucus can be removed and drained.
5) Identification and Banding
- After the baby is born, apply proper identification band to the baby so that the baby can be properly identified.
6) Eye Care
- Clean the eyes of the newborn properly from the inner canthus to the outer canthus with sterile gauze.
- If necessary, apply erythromycin or tetracycline ointment to the eyes from the lower lid.
7) Attachment and warmth (bonding)
- After the baby is born, placing the baby on the mother’s abdomen allows for bonding with the mother and proper skin-to-skin contact, which helps the mother and baby bond and prevents the baby from hypothermia.
8) APGAR Score
APGAR score is the most important part of immediate newborn care.
APGAR score is assessed at 1 minute and then at 5 minutes after birth.
In APGAR score,
A:= Appearance (skin color),
P:=Pulse (heart rate),
G:=Grimes (reflux irritability),
A:=Activity (muscle tone),
R:=Respiration (respiratory efforts)
are assessed.
The total score of APGAR score is 0-10.
APGAR score at 1 minute after birth:
If the Apgar score is between 7-10, it is considered normal, meaning there is no depression, in which the baby is provided with normal post-delivery routine care.
If the APGAR score is between 4-6, it indicates mild depression, in which the child requires assistance for breathing.
If the APGAR score is between 0-3, it indicates severe depression, in which the child requires resuscitation.
APGAR score at 5 minutes after birth:
If the APGAR score is between 7-10, it is considered normal, but if the Apgar score is below 7, the baby needs to be monitored for another half an hour.
9) Vitamin K:
The intestine of a newborn is sterile for some time after birth, that is, the bacteria that are responsible for manufacturing vitamin K are not present in its intestine, due to which the newborn cannot manufacture vitamin K, that is, vitamin K is responsible for a clotting factor. If this vitamin K is not present in the body of the newborn, then there are chances of it building up in the newborn, so as a prophylactic measure, artificial injection of vitamin K is provided to the newborn baby.
Dose:=
In pre-term:=0.5 ml,
Full term:= 1 mg.
Intra muscularly (IM) is provided on the vastus lateralis (lateral anterior).
Immediate newborn care after birth is provided as follows.
Then cover the baby with proper cloth to prevent hypothermia and apply proper identification band and then transfer the baby to the nursery for further care and observation.
2) Delivery of the shoulder,
3) Delivery of the trunk
b) Write the causes of Onset of Labour. 04
Causes for the onset of labor:
No specific cause for labor is known but it is said that many factors are responsible for the onset of labor such as,
1) Mechanical causes,
2) Hormonal causes,
3) Neurological causes
1) Mechanical causes,
These include,
Heightened reflex irritability of the uterus,
Uterine distension,
Menstrual period suppression,
Prolonged pressure of fetuses.
2) Hormonal causes:
1) Feto-placental contribution
Fetal hypothalamus is triggered to produce releasing factors.
Due to these releasing factors, anterior pituitary gland is stimulated to produce adrenotrophic hormone
(ACTH).
Adrenotrophic hormone
(ACTH) stimulates fetal adrenal gland to secrete cortisol.
Due to cortisol, changes occur in placental hormones.
Ex:=
Estrogen level increases,
Progesterone level decreases.
2) Estrogen hormone: Estrogen increases the possibility of the following mechanisms:
1) The release of oxytocin from the maternal pituitary increases.
2) Oxytocin stimulates myometrial receptors to synthesize prostaglandins.
3) Prostaglandin synthesis increases by decidual and amnion cells.
4) Myometrial contraction stimulates the synthesis of the protein actomyosin.
3) Progesterone
Progesterone has a relaxant effect on the uterus.
Progesterone is first produced by the corpus luteum and then by the placenta.
It inhibits uterine contractility.
The conversion of progesterone from fetal pregnenolone is inhibited due to increased fetal production of dehydroepiandrosterone sulfate (DHEA-S) and cortisol.
Therefore, before labor, progesterone levels fall while estrogen levels rise.
Then, progesterone levels fall, which is associated with the synthesis of prostaglandins.
4) Oxytocin:
Produced by the mother’s posterior pituitary gland Oxytocin hormone is released.
As estrogen levels increase, it helps in increasing oxytocin levels.
Oxytocin receptors increase in the decidua vera at the end of pregnancy. Oxytocin acts directly on the myometrium and causes contraction of the uterus.
In addition, it also acts on the endometrial tissue to release prostaglandins.
5) Prostaglandins
The major sites of prostaglandin production are the placenta, fetal membrane, decidual cells and myometrium.
It is said that due to the release of estrogen, the decidua releases prostaglandins and its action on the uterine muscles causes the uterine muscles to contract.
3) Neurological causes
Labor can be initiated through a nerve pathway.
Both ‘α’ and ‘β’ adrenergic Receptors are present in the myometrium.
Estrogen acts on the ‘α’ receptor and progesterone on the ‘β’ receptor.
1)’α’:=’α’ adrenergic receptor stimulates ‘α’ receptor.
2)’β’:=’β’ adrenergic receptor stimulates ‘β’ receptor.
Contractile response from ‘α’ receptors of prostaglandin nerve fibers located in and around the cervix and in the lower part of the uterus starts when progesterone is reduced.
Thus, the reasons for starting this labor are as follows.
OR
a) Write the Management of Puerperial Sepsis. Write the Management of Puerperial Sepsis. 08
Improve the nutritional status of the antenatal mother and eliminate any infection in the body.
Surgical asepsis during intranatal delivery, screening of group B streptococcus in high risk patients, antibiotics
Postpartum:
Initially one week of aseptic precautions, isolation and restriction of visitors.
Treatment:
Maintain isolation in general care, adequate fluid, calories, antibiotics and oral iron.
Maintain the patient’s intake output chart properly.
Properly monitor the patient’s vital signs and maintain a local discharge chart.
Surgical treatment: Remove pus and pain in the perineal wound Do.
Heparin IV 7-10 days in septic pelvic thrombophlebitis.
Debridement in pelvic abscess by colpotomy, laparotomy in unresponsive peritonitis.
Provide treatment if the patient is in septic shock.
b) Explain The difference between true labour pain and False Labour pain. Explain the difference between true labor pain and false labor pain.04
Difference between true labor and false labor:
1) Uterine contractions:
True labor:
- Contractions are always present in it.
- Contractions are regular and increase in frequency, intensity and duration.
- Its duration is up to 60 seconds.
- There is abdominal tightening (hardening of the uterus) discomfort or pain.
- The discomfort starts from the back and comes to the abdomen.
- Contractions from walking The intensity increases.
- The pain is not relieved by enemas or sedatives.
False Labor:
- In false labor, uterine contractions are not always present.
- It involves irregular and inefficient uterine contractions.
- Its duration is three to four minutes.
- The contractions are not painful every day and the uterus does not become hard.
- The discomfort is primarily in the abdomen.
- The contractions can be relieved by walking.
- The pain is relieved by giving an enema and sedatives. is.
2) Cervix
True Labor:
- Effacement and dilation of the cervix occur.
- False Labor
- Cervical changes are not seen in it.
3) Membrane:
True Labor: During contractions, tension is felt and a ‘bag of water’ is formed.
False Labor: Tensile strength is not felt and the formation of ‘bag of water’ does not occur.
4)show:
True Labor: In true labor, the show is mostly present.
False Labor: In false labor, the show is not noticeable.
5) Fit:
True Labor: In it, fit is progressively descending.
False Labor: In it, fit is not progressively descending.
Q- 3 Write Short Answer (Any two) Write Short Answer (Any two) 6+6=12
a) Describe management of infertility.- Describe the management of infertility.
Treatment modalities of infertility: Treatment modalities of infertility vary and generally depend on the cause of infertility.
1) Lifestyle modifications:
- Weight management By achieving a healthy body mass index (BMI) through an adequate diet and regular exercise. Exercise can improve fertility.
- Smoking and Alcohol Cessation: Smoking and alcohol consumption in excessive amounts both negatively impact fertility. Therefore, it should be avoided.
- Stress Reduction: Yoga, meditation, and counseling techniques help reduce stress and it affects fertility.
2) Medical Treatment:
- Ovulation induction Women who have an ovulatory disorder (polycystic ovary syndrome) are given medications such as clomiphene citrate, letrozole, or gonadotrophins that stimulate ovulation.
- Hormonal therapy Correcting hormonal imbalances that affect fertility, such as thyroid disorders and hyperprolactinemia.
- Treatment of infection If pelvic If there is a condition of infection such as PID, the patient should be provided with adequate antibiotic medication to treat the infection that affects fertility.
3) Surgical Intervention:
- Laparoscopic surgery is used to treat conditions that affect fertility such as endometriosis, pelvic adhesions, and fibroids.
- Tubal Surgery Tubal surgery is used to repair blocked or damaged fallopian tubes that prevent sperm from reaching the egg.
4) Assisted Reproductive Technologies (ART):
- Intrauterine Insemination (IUI): Intrauterine insemination is a process to improve fertilization in which sperm is inserted directly into the uterine cavity at the time of ovulation. Comes.
- In Vitro Fertilization (IVF) In the in vitro fertilization process, ovum and sperm are fertilized outside the body, i.e. in a laboratory.
In the steps of which, - Ovarian stimulation is the use of medication that stimulates the ovaries to produce multiple eggs.
- Egg retrieval A surgical procedure to collect eggs from the ovaries.
- Fertilization Eggs and sperm are mixed in a laboratory dish and then the embryos are cultured.
- Embryotransfer Now more than one embryo is transferred into the uterine cavity.
- Intracytoplasmic injection In this procedure, sperm is directly introduced into the egg to improve fertilization.
5) Donor Gametes:
- Couples who have severe fertility issues and whose infertility is genetic can use donor eggs or donor sperm for fertility.
- Donor eggs Donor eggs are fertilized with the partner’s or donor’s sperm through IVF.
- Donor sperm is used when there is severe infertility in the male. And due to the genetic risk of male infertility, donor sperm is also used.
6) Surrogacy:
- In surrogacy, another female (surrogate) carries and delivers a child for individuals or couples who are unable to conceive or carry a pregnancy to term:
- Gestational surrogacy In gestational surrogacy, both the desired woman’s egg and the desired male’s sperm (surrogate gametes) are collected, subjected to in vitro fertilization in a laboratory, and transmitted to the surrogate mother.
- 7) Psychological Support
Infertility is emotionally challenging. Counseling, support groups, and therapy are important for individuals and couples to cope with the condition of infertility. - Thus, the treatment for infertility depends on the different causes in each individual. In which reproductive endocrinologists, urologists, surgeons and mental health professionals provide adequate treatment to each infertile couple according to their cause and their needs.
b) Describe Essential New Born Care. – Describe Essential Newborn Care.
Essential Newborn Care:
Essential Newborn Care involves properly assessing and stabilizing the newborn.
Essential Newborn Care is crucial for the fetus to transition from intrauterine life to extrauterine life.
Goal of Essential Newborn Care
- 1) To establish, maintain and provide support to the newborn’s respiration.
- 2) To prevent the newborn from fever and hypothermia.
- 3) To prevent the newborn from getting infections.
- 4) To provide safety to the newborn and prevent him from injury.
- 5) To provide immediate treatment for any actual or potential problems in the newborn by early identification.
- Immediate newborn care is provided.
>Essential Newborn Care
1) Establishment of Respiration
When the newborn is received, immediately patent the newborn’s airway and properly clear the airway. Due to which the newborn can breathe effectively.
As soon as the newborn’s head is turned, wipe the mouth and nose and suction the mouth and nose so that the newborn can breathe properly. Suction should be done first through the mouth and then through the nose, which can prevent aspiration of secretions.
2) Initiation of Cry: Normally 99% of newborns cry immediately and spontaneously after delivery, this cry is considered a good sign for the newborn’s breathing.
If the newborn does not cry properly, follow the following steps:
- a) If the baby does not cry spontaneously or if the cry is weak, then lightly simulate the baby to cry.
- b) To stimulate the baby’s cry, instead of slapping his bottom, lightly rub the soles of his feet. After removing the secretions of the newborn, stimulate the baby to start crying.
- C) The cry of the newborn is usually loud and husky and if there is any abnormal cry as follows, then the newborn should be properly monitored such as,
- Cord care is an important immediate care of the newborn.
- The newborn’s cord should be clamped within 30 seconds of birth and then cut properly.
- Delivering the newborn After this, place the newborn on the mother’s abdomen.
- Then clamp the cord properly at two opposite sites using cord clamps.
- Apply the first clamp 5 cm away from the umbilicus, then apply the second clamp 2.5 centimeters from the first clamp.
- Then cut the cord properly between the two clamps.
- Do not apply anything to the cord, let it dry and fall off naturally. Devi.
- The cord naturally falls off within seven to ten days after birth.
- Prevent the cord from getting wet with water and urine.
- If any kind of discharge or bleeding is present in the cord, immediately access the cord clamp and then loosen it properly.
- If the following signs and symptoms are seen in the cord, then immediately
- Reporting such as,
- Foul odor coming from the cord,
- Seeing no discharge,
- Redness around the cord,
- The cord should be wet,
- The cord should not fall down in 7-10 days,
- Inflammation,
- Fever etc.
•>High pitched cry:= Due to hypoglycemia and increased intracranial pressure,
Week Cry:= Prematurity,
Hosacry:= Laryngeal Strider
3)Care of Cord
4) Maintain Position of the Newborn
A newborn is usually prone to choking, coughing and gagging during the first 12-18 hours after birth. Therefore, the newborn should be provided with a proper position.
In which the fitters should be provided with a proper side lining position so that mucus can be removed and drained.
5) Identification and Banding
After the baby is born, a proper identification band should be applied to the baby so that the baby can be properly identified.
6) Eye Care
Clean the newborn’s eyes properly from the inner canthus to the outer canthus with sterile gauze.
If necessary, apply erythromycin or tetracycline ointment to the lower lid of the eye. Apply from the side.
7) Attachment and warmth (bonding)
After the birth of the baby, place the baby on the mother’s abdomen so that bonding with the mother occurs and proper skin-to-skin contact can occur, which causes attachment of the mother and the baby and prevents the baby from hypothermia.
8) APGAR score
APGAR score is the most important part of immediate newborn care.
APGAR score is assessed 1 minute after birth and then at 5 minutes.
In APGAR score,
A:= Appearance (skin color),
P:= Pulse (heart rate),
G:= Grimace (reflux irritability),
A:= Activity (muscle tone),
R:= Respiration (respiratory efforts)
are assessed.
The total score of the APGAR score is 0-10.
The APGAR score is given at 1 minute after birth:
- If If the Apgar score is between 7-10, it is considered normal, meaning there is no depression, and the baby is provided with normal post-delivery routine care.
- If the APGAR score is between 4-6, it indicates mild depression, in which the child requires assistance for breathing.
- If the APGAR score is between 0-3, it indicates severe depression, in which the child requires resuscitation.
- APGAR score at 5 minutes after birth:
- If the APGAR score is between 7-10, it is said to be normal, but if the Apgar score is below 7, then the baby needs to be monitored for another half hour.
9) Vitamin K:
The intestine of a newborn is sterile for some time after birth, which means that the bacteria that are responsible for manufacturing vitamin K are not present in its intestine, due to which the newborn cannot manufacture vitamin K, i.e. vitamin K is responsible for a clotting factor. If this vitamin K is not present in the body of the newborn, then there is a possibility of blood clots forming in the newborn, so as a preventive measure Newborn babies are provided with artificial injection of vitamin K.
Dose:=
In pre term:=0.5 ml,
Full term:= 1 mg.
Intra muscularly ( IM ) is provided on vastus lateralis (lateral anterior).
Thus essential newborn care after birth is provided as follows.
C) Write Down Physiological Changes During Puperium
Physiological changes during the puerperium period:
- Puerperium:
Puerperium is the period of 6 weeks (42 days) after childbirth in which the tissues of the body, especially the pelvic organs, return to their pre-pregnancy stage both anatomically and physiologically. It is called puerperium. - Duration:
Puerperium begins with the expulsion of the placenta. It is about 6 weeks from the time of expulsion, during which the uterus becomes almost non-pregnant in size.
The period is roughly divided as follows:
• Immediate: Within 24 hours,
• Early: Up to 7 days,
• Remote: Up to 6 weeks
1) Physiological Changes in Reproductive System in Puerperium Period:
- ( a ) Involution of Uterus: Involution is the process in which the bulky uterus during pregnancy progressively returns to its normal pre-pregnant state after delivery. This is called involution of uterus.
- Anatomical Considerations After delivery of the placenta, healing of the placental site into the endometrium occurs. After delivery, the uterus alternates Firms and tightens with hardening and softening.
The size of the uterus during pregnancy is approximately,
Length: 20 cm, Breath: 12 cm,
Thickness: 7.5 cm.
And the weight of the uterus is 900-1000 gm.
Which,
At the end of the puerperium period i.e. 6 weeks after childbirth, the uterus returns to its pre-pregnant state, such as, the size of the uterus during the puerperium period is
Length: 7.5 cm, Breath: 5 cm ,
Thickness:2.5 cm is about.
And the weight of the uterus is 60 gm.
Reduction of the size and position of the uterus:
- After 24 hours, it is at the level of the umbilicus. The uterus descends into the pelvic cavity at a rate of 1.25 cm/hr and is not palpable abdominally above the symphysis pubis after 10 days.
Consistency of the uterus: Due to repeated strong myometrial contractions, the blood flow to the uterus is controlled, making it hard. Its consistency can be felt by palpation. It should feel firm and round. If the funds are soft, it is called a boggy uterus. It indicates that the contractility is inadequate and blood loss is ongoing.
( b )Involution of Cervix:
- After delivery, the lower uterine segment and cervix remain loose, thin and stretched.
- It may be edematous, bruised and have small tears and lacerations. It takes a few weeks for the isthmus to return to its normal shape and size.
- The consistency of the first post partum day service remains normal enough to admit two fingers. Then at the end of the first week it remains as long as the tip of the fingers can be admitted. The evolution of the cervix continues for 3-4 months. But the parous cervix never acquires the appearance of a non-parous cervix. The external os which initially looked like a dimple now looks like a slit.
(C) Vaginal canal: It takes about 4 to 8 weeks for the distensible vagina to involute. After delivery the vaginal canal appears swollen and smooth, gradually becomes small and firm but never reaches its pre-pregnancy size. The introitus remains permanently large and the hymen is lacerated. Represented in the form of nodular tags.
(d) Perineum: The muscles of the perineum floor become stretched, swollen and bruised, with a scar resembling an episiotomy.
(e) Broad ligaments and round ligaments: The broad ligaments and round ligaments take some time to recover from stretching. Initially the ligaments are stretched but by the end of the puerperium period the ligaments return to their non-pregnant length.
( f ) Pelvic floor and pelvic fascia: The pelvic floor and pelvic fascia take a long time to involute due to the stretching effect.
( f ) Lochia:
- The vaginal discharge that occurs during the first 15 days during the puerperium period is called lochia, which is the uterine body, Comes from the cervix and vagina.
- It contains blood vessels, decidual tissue, epithelial cells of vaginal mucus, bacteria, membrane fragments and small clots.
- Odor of lochia
- The odor (smell) of lochia is fishy.
Types of lochia:
There are three types of lochia.
- 1) Lochia rubra ,
- 2) Lochia syrosa,
- 3) Lochia alba
1) Lochia rubra :
- Lochia Rubra is the first phase of lochia. In which the discharge is red and bloody and lasts for 1 to 4 days after childbirth.
- Lochia rubra contains
blood,
fetal membrane, decidua,
vernix caseosa and lanugo.
2) Lochia seroosa:
- Lochia seroosa is the second phase of lochia. Which is seen as yellowish pale or pale brownish in color.
- Lochia seroosa lasts for 5 to 9 days.
It contains less red blood cells but a higher amount of leukocytes,
wound exudate,
survival mucus,
and microorganisms.
3) Lochia alba:
- Lochia alba is the third phase of lochia. It is usually pale white in color.
- Lochia alba is visible for 10-14 days.
- In it,
- Increased decidual cells,
- Leukocytes,
- Mucus,
- Cholesterol crystals,
Amount: The average amount of lochia is about 250 ml during the first 5 to 6 days.
- (2) Breast and lactation:
- Breasts develop during pregnancy due to hormonal stimulation. For a few days after delivery, both feeding and non-feeding breasts secrete colostrum. Colostrum is the creamy yellow precursor to milk. This makes the breasts soft and non-tender.
- After three days, prolactin levels increase and the breasts become firm and tender. Then milk secretion starts. Due to increased blood flow, venous and lymphatic congestion, the breast becomes distended, hard and warm. This is called physiological engorgement.
- It lasts for 24 to 48 hours and then resolves on its own. Milk production is stimulated by the baby’s sucking. The breast feels firm, full and tender until it is empty.
Normal duration: The normal duration of lochia is up to three weeks if three weeks If it persists, it may be a local lesion.
Clinical Importance of Local Discharge: Lochia provides information about the mother’s perinatal state, so it is important to assess lochia.
Odor (Smell): May be due to offensive infection.
Odor: Scanty or absent may be due to infection.
Amount: Scanty or absent infection May be due to.
Color: Continuous red color lochia may be due to subinvolution.
Duration: If lochia persists for three weeks or more, it may be a local lesion.
Breasts
Lactation:
- Lactation is the process of breastfeeding that is based on the interplay of hormones, instinctive reflexes, and learned behaviors of the mother and newborn.
- Lactation is particularly under the control of the hormones prolactin and oxytocin and is maintained by three factors:
- 1)Anatomical structure of mammary gland, development of alveoli, ducts and nipple.
- 2) Initiation and maintenance of milk secretion.
- 3) Milk ejection or propulsion of milk from alveoli to nipple.
Milk production: A healthy mother produces 500 to 800 ml of milk to feed her baby.
- (3) Cardiovascular Changes:
Blood Volume The blood volume that increased during pregnancy decreases and the circulatory system returns to its prepregnancy state.
Cardiac Output Due to diuresis and diaphoresis, excess water in the body is removed from the body and cardiac output returns to its normal range.
Hemoglobin and hematocrit levels: Due to blood loss during pregnancy, hemoglobin and hematocrit levels initially decrease but within a few weeks the blood stabilizes within its normal range.
4) Respiratory function: After delivery, the abdominal pressure decreases and the diaphragm descends, which improves lung expansion and ventilation, but there are no noticeable changes in respiratory rate.
- (5) Endocrine Changes:
Hormone Shift: Pregnancy related hormones such as estrogen, progesterone and human chorionic gonadotropin (HCG) hormone are reduced.
The level of prolactin hormone is elevated to maintain breast feeding.
- (6) Renal Changes
Diuresis Urine output increases due to which the fluid accumulated in the body during pregnancy is excreted from the body.
Bladder Function The bladder regains its tone and function, although some temporary issues such as urinary retention or urinary incontinence may occur.
- (7) Gastrointestinal Changes:
Bowel Function
Bowel function takes some time to normalize but due to its motility being reduced, a condition of constipation is seen.
Appetite in women becomes normal in some time but bowel changes are seen in some women for some time.
- (8) Musculoskeletal Changes:
Abdominal Muscles Abdominal Muscles The tone of the vagina regains over time, while the pelvic floor muscles also return to normal over time, but Kegel exercises are important in strengthening the pelvic floor muscles.
(9) Psychological Changes Hormonal fluctuations, physical recovery, and the demands of newborn care impact emotional well-being. It is also common to experience mood swings such as the “baby blues”. And some women also experience post-partum depression.
Thus, such physiological changes are seen in women during the post-partum period.
Q- 4 Write Short notes. Write short notes (any three) 12
a) Antenatal care
Antenatal care is also called prenatal care, in which comprehensive health care is provided to pregnant women from conception to the birth of a child.
This period is a crucial time for monitoring the mother and the developing fetus. Because it allows for early identification and management of any potential health complications in the mother and the developing fetus. And the mother can be prepared physically and emotionally for childbirth and the postpartum period.
Systematic supervision (examination or advice) of a woman during pregnancy which is regular and periodic is called “antenatal or prenatal care”. Antenatal care starts before pregnancy and ends when the baby is delivered.
•> Aim and Objectives of Antenatal Care:
Antenatal Care Aim:
The aim of antenatal care is to improve the overall health of the fetus and mother and to improve the well-being of the mother and fetus and to prevent complications.
1) Monitoring Maternal Health
Regular health checkups can monitor the overall health of the mother, such as properly assessing blood pressure, weight gain, and overall well-being, so that any complications in the mother can be identified early. And they can be treated early and prevented from happening further.
2) Monitoring Fetal Health
Assessment of the fetus in antenatal care, which includes ultrasound scans, fetal heartbeat monitoring, and other tests, so that the fetus’s growth and development can be properly monitored. If the child has any abnormality, it can be detected early and managed properly.
3) Health Education
Antenatal care provides the opportunity for appropriate education to expectant mothers. It provides the opportunity for education about pregnancy, childbirth, breastfeeding, nutrition and parenting. This education can be helpful for the antenatal mother in taking proper decisions.
4) For early detection and proper management of pregnancy related complications
Antenatal care visits can help in early detection of pregnancy related complications and timely management. Such as,
gestational diabetes,
preeclampsia, infection and other pregnancy-related risks that can affect the pregnancy.
5) Preparation for Childbirth
In the antenatal care session, birth planning, preparation for labor, and delivery options are discussed. By doing this discussion, the mother and her family members can prepare mentally and practically for the birth of a child.
6) Psychological Support
Emotional and psychological changes are observed due to pregnancy. Antenatal care provides a supportive environment in which the expectant mother can discuss and clear her anxieties, fears and doubts and can reduce her anxiety and fear and feel emotionally well-being.
7) Prevention and Management of Maternal and Infant Complications
Antenatal care interventions include immunization, iron and folic acid supplementation, and preventive treatment to prevent pregnancy and childbirth-related risks and complications.
8) Promotion of Healthy Behavior
Education is provided in antenatal care to promote behavior, including smoking cessation, avoiding alcohol and drugs, maintaining a balanced diet, and being physically active. These behaviors are important for a healthy pregnancy outcome.
9) Postpartum Planning
Postpartum care is also discussed in antenatal care, including postpartum care, breastfeeding support, and family planning options.
The objectives of overall antenatal care are to have a healthy pregnancy, properly manage any risks and complications, prepare the mother for childbirth, and properly maintain the health of the mother and fetus during the throwout pregnancy.
Objectives:
The main objective is to deliver a healthy baby by a healthy mother with a normal pregnancy.
The first visit should be before the second missed period.
To assess the health status of the mother and fetus.
For early screening of cases of high-risk pregnancy.
To formulate a plan for further management.
To promote, protect, and maintain good physical and mental health of the mother during pregnancy.
•> Components of Antenatal Care:
1) Initial Assessment:
The first antenatal visit should be done early in pregnancy. Ideally, it should be done within 8 to 12 weeks of the last menstrual period.
During this assessment, health care providers properly assess the woman, which includes a complete assessment of the woman’s medical history, including previous pregnancies, medical conditions, medications, and relevant family history.
This information is collected to identify the mother’s potential risk factors and to provide appropriate care to the mother.
2) Physical Examination: A physical assessment of the mother is done to assess the health status of the mother and fetus during the throw out pregnancy period.
In this examination, the mother’s blood pressure,
weight, and urine tests are done, due to which if the mother has a condition like gestational diabetes and preeclampsia, it can be identified early.
The mother’s blood test is also done, due to which the mother’s hemoglobin level, blood group, are done.
The mother is also screened for hepatitis, and HIV infection.
3) Fetal Monitoring: The growth and development of the fetus is also monitored in antenatal care.
Fetal assessment is done through various methods such as, Ultrasound: Ultrasound is done to confirm pregnancy, assess gestational age, assess fetal growth and identify any structural problems i.e. malformations in the fetus. Fetal Doppler: Fetal heart rate is monitored through fetal Doppler. Kick counting: Advise the mother to feel the fetal movement and count the number of fetal kicks throughout the day, which can monitor fetal well-being.
4) Nutritional guidance: Proper nutrition is important to provide support to maternal health and fetal development.
Antenatal health care providers provide guidance to the mother about a balanced diet, as well as education to pregnant women about the importance of maintaining proper weight and taking adequate amounts of vitamins and minerals (Ex: iron and folic acid). And education is also provided to women that taking an adequate diet can prevent congenital birth defects in the fetus and the condition of anemia in pregnant women.
5) Health Education and Counseling: In antenatal care, pregnant women are provided with education on pregnancy-related topics. Such as,
Exercise:
Safe physical activity and exercise are important for maintaining the health of the mother and the fetus.
Labor and Birth Preparation:
Information is provided to the mother about the stages of labor, along with education about pain relief strategies, and birth plans.
Breastfeeding:
Providing education to the mother about the techniques and benefits of breastfeeding.
Emotional and Mental Health:
Properly assess the emotional and mental health of the mother and provide adequate education and psychological support to the mother to relieve her fear and anxiety and clear all the doubts of the mother.
6) Screening and Test:
Properly conduct genetic testing during the mother’s antenatal period so that any genetic complications can be identified. Genetic Screening:
In this, ultrasound and blood tests are done on the mother so that if there is a risk of genetic disorders, it can be identified. (Ex: Ultrasound). Screening for Infection:
The mother is screened to identify any sexually transmitted diseases and any other infections that may affect the pregnancy. Glucose Tolerance Test:
A glucose test is performed to identify whether the mother has any gestational diabetes.
7) Preparation for Labor and Birth: Antenatal care includes discussions about birth preferences, options for managing labor pain, and preparation for potential complications.
8) Postpartum Planning: Antenatal care also includes planning for postpartum care, including breastfeeding support, newborn care, and education for the mother. Thus, antenatal care is important for maintaining the health condition of the mother, for the proper growth and development of the fetus, and for the early identification and management of potential risk factors, if any.
b) Hormonal Replacement Therapy – HRT
Hormonal Replacement Therapy (HRT)
Introduction:
Hormonal Replacement Therapy is a medical therapy in which hormones are given from an external source to replace a patient’s hormone levels when they are deficient. HRT is given, especially in females after menopause or after hysterectomy, when there is a deficiency of female hormones such as estrogen and progesterone.
When is hormonal replacement therapy given? (Indications for HRT):
1. Menopause – When a woman’s menstrual cycle stops completely and estrogen levels in the body drop.
2. Premature Ovarian Insufficiency – When estrogen levels drop before the age of 40.
3. Post-hysterectomy – When the patient’s uterus and sometimes ovaries are removed.
4. Hypogonadism (Hypogonadism) – When the patient’s body has low biological hormone production.
5.Transgender Hormone Therapy – Hormone therapy for transgender patients for gender reassignment.
Types of HRT:
1.Estrogen-only Therapy – Only estrogen is given, which is considered safe only for patients who do not have a uterus.
2.Combined Estrogen and Progesterone Therapy Progesterone Therapy – If the uterus is still present, progesterone should be given along with estrogen to reduce the chances of endometrial hyperplasia.
3.Local (Vaginal) Estrogen Therapy – Mainly useful for local symptoms like vaginal dryness, itching or pain.
Routes of Administration:
1.Oral Tablets
2.Transdermal Patches
3.Gels and Creams
4.Vaginal Rings or Tablets
5.Injectables
Benefits of HRT):
- Relieves Vasomotor Symptoms such as hot flashes, night sweats.
- Relieves problems affecting the vagina such as dryness and pain.
- Reduces the risk of osteoporosis.
- Helps with mood swings and sleep problems.
Risks and Precautions:
- Long-term use of HRT may increase the risk of Breast Cancer, Deep Vein Thrombosis, Stroke, and Heart Disease.
- A complete medical evaluation is required before starting HRT.
- Regular follow-up of the patient, Mammography, and Pelvic Examination (Pelvic examination) is mandatory.
Who should not be given (Contraindications):
Patients with a history of breast cancer or endometrial cancer.
Liver disease, irregular uterine bleeding.
History of thrombosis or stroke.
Hormonal Replacement Therapy (HRT) is It is a tool that, when used correctly and in the right patient, can be very beneficial. It improves the patient’s quality of life, but it should be used only under the advice and supervision of a doctor. HRT must be personalized for each patient to ensure that it is safe and effective. Increased risk of breast enlargement, bloating, breast tenderness.
Testosterone-related:-
Acne, oily skin. Risk of sleep apnea. Possible effects on fertility.
Contraindications absolute:
Active or history of breast or endometrial cancer.
Undiagnosed vaginal bleeding. active thromboembolic disorders.severe liver disease.
History of cardiovascular disease, controlled hypertension.Monitoring and follow-up Regular follow-ups to monitor hormone levels, side effects and therapeutics efficiency. Regular check-ups for breast and endometrial health.Bone density monitoring for osteoporosis.
c) AMTSL – A. M. T. S. L.
AMTSL – Full Form: Active Management of Third Stage of Labour
The third stage of labour is the period after the birth of the baby, which lasts until the complete expulsion of the placenta and membranes. This stage is extremely important for the health of the mother and usually lasts for 5 to 30 minutes.
Management of the Third Stage of Labor:
Currently, two methods are used in the management of the third stage.
1) Expectant (Watchful) Management
2) Active Management
1) Expectant (Watchful) Management
In this management, the separation of the placenta and its descent into the vagina are allowed to occur spontaneously.
In this management, minimal assistance is given for placental expulsion.
In this stage, the mother is constantly watched, i.e. the mother is not left alone even for a short time.
If the mother is in a lateral position, then she should be given a dorsal position, due to which the signs of placental separation and the amount of blood loss can be properly recognized. Can.
In this management, only the separation, descent and expulsion of the placenta are properly watched.
One hand is placed on the fundus so that,
a) The separation of the placenta can be seen.
b) The state of uterine activity i.e. contraction and relaxation can be seen.
The placenta starts separating from the uterine wall within a few minutes after the birth of the baby, so wait for 15 to 20 minutes for the placenta to separate on its own.
In this, no touch technique is used.
In this, there is a “no touch policy” i.e. the placenta is expelled within 15-20 minutes due to gravity i.e. no massage on the fundus.
Do not use any type of uterotonics and do not use any manual method for expulsion of the placenta. Do not use either.
Expulsion of placenta
When the placenta is expelled, the following points should be followed:
Advise the patient to apply a beer down forceps when the uterus is hard.
The raised intra-abdominal pressure is important for the expulsion of the placenta.
And the placenta It can be expelled spontaneously.
2) Active Management
1) Use of Uterotonics
Oxytocin is the drug of choice in the management of the third stage of labor.
In the management of the third stage, 10 units of oxytocin should be provided IM (intramuscularly).
Oxytocin stimulates uterine contractions It helps in expelling the placenta by enhancing it.
2) CCT (Controlled Cord Traction)
Controlled cord traction uses a manual method in which the umbilical cord is tracked and gently pulled downwards and backwards, due to which the placenta separates from the uterine wall and can then be expelled. However, controlled cord traction is performed when uterine contractions are present by placing the hand on the suprapubic area.
3) Fundal Pressure:
Push the fundus downwards and backwards using the uterus as a piston by placing four fingers behind the fundus and the thumb in front. Apply pressure when the uterus is hard. If it is not hard, rub gently to make it hard. When the placenta passes through the introitus, stop the pressure immediately. When the baby is macerated or premature This method is more useful when the tensile strength of the cord is low. If there are any clots left inside, massaging the uterus helps in their expulsion.
4) Delayed cord cutting
Wait for one to three minutes after the delivery of the fetus and then cut the umbilical cord. This technique is more useful in term newborns. Because the newborn has an adequate amount of placenta from the placenta. The mother can receive blood, which can prevent the condition of anemia.
But in preterm babies, the liver is immature and there is a high rate of breakdown of red blood cells and if the cord cutting is done late, then due to this, the condition of hyperbilirubinemia (jaundice) can arise in the newborn.
5) Postpartum vigilance
After the delivery of the placenta, the placenta should be properly inspected, including the cotyledons, lobes, and the maternal and fetal sites and membranes. Proper assessment and then fundal massage after delivery of the placenta can ensure continuity of uterine contractions and if there are retained bits of placenta, it can be expelled properly. And the condition of postpartum hemorrhage (PPH) in the mother can be prevented.
d) Anemia in Pregnancy
Anemia is the most common blood disorder seen in women during pregnancy. It is generally more prevalent in areas with poor socioeconomic conditions. Anemia is a condition in which the circulating red blood cells and hemoglobin levels are lower than their normal levels (reduced number). Due to this, the oxygen carrying capacity of the red blood cells decreases. It is usually seen due to various reasons such as nutritional deficiency (iron, vitamin B12, or folate), chronic disease, genetic condition, and blood loss.
Normal Hb in females: 12-16 gm/ dl.
If the hemoglobin level in females is between 10 gm/ dl – 11.9 gm/ dl, it is called mild anemia.
If the hemoglobin level in females is between 7 gm/ dl – 9.9 gm/ dl If it is in between, it is called moderate anemia.
If the hemoglobin level in a female is less than 7 gm/dl, it is called severe anemia.
Classification:
1. Physiological anemia.
2. Pathological anemia.
1. Physiological anemia: In pregnancy, plasma volume, red blood cell (RBC) volume and hemoglobin mass increase, so pregnancy demands special attention. The extra demand for iron increases in the first trimester and even with an adequate amount of diet, it is not met, so physiological iron deficiency occurs during pregnancy. Therefore, hemoglobin concentration falls down in pre-pregnancy due to the effect of hemodilution and negative iron balance.
2.Pathological anemia:
Deficiency anemia: Due to iron deficiency, folic acid deficiency, vitamin B 12 deficiency, protein deficiency, etc.
Hemorrhagic:
Acute: Due to bleeding in the early months or antepartum hemorrhage (APH).
Chronic: Hookworm infestation, bleeding piles, etc.
Hereditary: Thalassemia, Sickle Cell Hemoglobinopathy, Other, Hemoglobinopathy, Hereditary Hemolytic.
Bone Marrow Insufficiency: Hypoplasia or aplasia due to radiation, drugs (aspirin, indomethacin.
Anemia of infection (malaria, tuberculosis).
Chronic disease (renal) or neoplasm.
Etiology:
Due to nutritional deficiency.
Chronic disease Due to.
Genetic factors.
Blood loss.
Infection.
Bone marrow disorders.
Vitamin deficiency.
Impaired production of red blood cells.
Excessive blood loss.
Decreased production of red blood cells.
Symptoms and signs:
Fatigue,
Weakness,
Pale skin, conjunctiva and mucous membranes,
Shortness of breath,
Dizziness Headache, rapid and irregular heartbeat, cold hands and feet. Brittle nails. Poor concentration. Cognitive difficulties. Growth and development delays. Loss of appetite. Dizziness. Tachypnea. Tachycardia. Palpitations. Diarrhea and vomiting. Cardiac enlargement with murmur. In some cases, jaundice, petechiae and ecchymosis may also be present. Hepatomegaly may occur. Diagnostics Evaluation
History taking,
Physical examination,
Complete blood count test.
Peripheral blood smear.
Additional blood tests.
Bone marrow aspiration and biopsy.
Imaging tests.
X-ray.
CT scan.
M .R .I.
Genetic testing.
Stool examination
Management:
Assess the cause of anemia in the woman.
If the woman’s anemia condition is due to nutritional deficiency, provide the child with adequate nutritional supplements such as iron, vitamin B 12 and folate.
Provide the woman with a nutritious diet containing iron.
Provide the woman with adequate supplementary diet according to the nutritional deficiency.
If the woman’s anemia condition is due to any infection or chronic disease, then the woman’s condition should be treated immediately.
If the woman has a condition of severe anemia, then do proper blood transfusion.
Monitor the woman regularly.
If the woman’s anemia condition is due to excessive blood loss, then stop it and start intravenous infusion immediately.
Provide complete education to the woman and her family members about her condition, its causes, its symptoms and signs and its treatment.
Do all the laboratory investigations of the woman.
Do regular screening of the woman to prevent her from the condition of anemia.
Q – 5 Define Followings (Any Six) Write the definition below (any six) 12
a) Grand Multipara – Grand Multipara
Grand Multipara is when a woman has given birth to four or more viable children before.
b) Placenta previa – Placenta previa
When the placenta partially or completely Implantation near or above the internal os of the lower segment of the uterus is called “placenta previa”. 1/3rd of antepartum hemorrhage cases are due to placenta previa.
Types of placenta previa:
There are four types of placenta previa based on the degree of extension of the placenta into the lower segment of the uterine cavity.
- 1) Type I (lateral placenta previa),
- 2) Type II (marginal placenta previa),
- 3) Type III(Incomplete Placenta Previa),
- 4) Type IV(Complete Placenta Previa)
1) Type I (Lateral Placenta Previa):
In this type, the major part of the placenta is attached to the upper segment but only the lower margin enters the lower segment but does not reach the OS.
2) Type II (Marginal Placenta Previa):
In this type, the placenta is only It reaches the margin of the internal os but does not cover it.
If the placenta is anterior, vaginal birth is possible. Blood loss is average. The risk of fetal hypoxia is higher than that of maternal shock.
3) Type III (Incomplete Placenta Previa):
The placenta partially but not centrally covers the internal os. Bleeding occurs due to lower stretching when the cervix begins to efface and dilate in late pregnancy.
4) Type IV (Complete Placenta Previa):
In this, the placenta covers the internal os. It covers even when fully dilated. Severe hemorrhage occurs, requiring a cesarean section to save the life of the mother and baby.
c) Lochia
- The vaginal discharge that occurs during the first 15 days of the puerperium period is called lochia. It comes from the uterine body, cervix and vagina.
- It contains blood vessels, decidual tissue, epithelial cells of vaginal mucus, bacteria, membrane fragments and small clots.
- Odor of lochia
- The odor (smell) of lochia is fishy. (fishy) like.
Types of lochia:
There are three types of lochia.
- 3) Lochia Alba
1) Lochia Rubra :
- Lochia Rubra is the first phase of lochia. In which the discharge is red and bloody and lasts for 1 to 4 days after childbirth.
- Lochia rubra contains
blood,
fetal membrane, decidua,
vernix caseosa and lanugo.
2) Lochia seroosa:
- Lochia seroosa is the second phase of lochia.
Which is seen as yellowish pale or pale brownish in color. - Lochia seroosa lasts for 5 to 9 days.
It contains less red blood cells but a higher amount of leukocytes,
wound exudate,
survival mucus,
and microorganisms.
3) Lochia alba:
- Lochia alba is the third phase of lochia. It is usually pale white in color.
- Lochia alba is visible for 10-14 days.
- In it,
- Increased decidual cells,
- Leukocytes,
- Mucus,
- Cholesterol crystals,
- Fatty and glandular epithelial cells,
- And microorganisms are found in it.
–>
Amount: The average amount of lochia is about 250 ml during the first 5 to 6 days.
Normal Duration: The normal duration of lochia is up to three weeks. If it persists beyond three weeks, then there may be local lesions.
Clinical Importance of Lochia Discharge: Since lochia provides information about the mother’s perinatal state, it is important to assess lochia.
Odor (Smell): May be due to offensive infection.
Odor: Scanty or absent may be due to infection.
Amount: Scanty or absent may be due to infection.
Color: Continuous red color Nokia may be due to subinvolution.
Duration: If lochia persists for three weeks or more, it may be a local lesion.
d) Abortion
Abortion is a process in which pregnancy is terminated. In abortion, the product of conception is partially or completely separated and expelled from the uterine wall before the age of viability (28 weeks). This condition is called “abortion”.
If abortion occurs spontaneously, it is called “miscarriage”. And if it is done on purpose, it is called “induced abortion”.
Majority abortion or miscarriage occurs during the first trimester of pregnancy, that is, during the first 12 weeks of pregnancy, it is called “early miscarriage”. And a miscarriage that occurs after 13 weeks of pregnancy is called a “late miscarriage”.
The types of abortion are as follows.
1)Spontaneous abortion
A)Threatened abortion,
B)Inevitable abortion,
C) Complete abortion,
D) Incomplete abortion,
E) Silent or missed abortion,
D) Septic abortion,
E) Recurrent abortion or habitual abortion,
2)Induced Abortion
e) Precipitate Labour – Precipitate Labour
Precipitate labour is also called “rapid labour” and “rapid childbirth”. Precipitate labour is when the total duration of the first and second stages of labour is less than two hours. This results in rapid and spontaneous expulsion of the infant. It is commonly seen in multipara women. Multipara has a relaxed pelvic or perineal floor, multipara usually has strong, forceful contractions and does not feel painful sensation during labor, so immediate birth is not reported, due to which precipitated labor is seen.
f) Denominator – Denominator
The denominator is the bony part of the fetus that is the presenting part in relation to the various quadrants of the maternal pelvis.
For example,
- Face Presentation has the occiput as the denominator.
- Mentum (chin).
- Brow presentation has the frontal eminence as the denominator.
- Breech presentation has the sacrum as the denominator.
- Solder presentation has the acromian process of the scapula of the seller as the denominator.
g) Asphyxia
Asphyxia is a condition in which the body does not get enough oxygen, which causes difficulty in breathing and if not treated immediately, unconsciousness or death can also occur.
h) Pre – Eclampsia
Preeclampsia is a condition of pregnancy that occurs when the body does not get enough oxygen, causing difficulty in breathing and can lead to unconsciousness or death if not treated immediately. It is a complication whose etiology is unknown but it is a multisystem disorder. In which blood pressure is high, other organs are also damaged and most commonly the liver and kidneys are affected.
Preeclampsia is mainly seen after the 20th week of pregnancy and it also differs in severity.
The main symptoms of preeclampsia are,
- 1) Hypertension that increases to more than 140/90 mmHg (hallmark sign of preeclampsia),
- 2) Edema (mainly in the hands, face, and in the legs) and excessive weight gain,
- 3) Proteinuria (excess amount of protein in the urine),
- 4) Albuminuria (albumin present in the urine).
These symptoms of preeclampsia are seen after the 20th week.
Q – 6 Fill in the Blanks – fill in the blank space. 05
1. At term preportion of the placenta and fetal weight is…….At term placenta and fetal weight ratio is: 1:6.🔸 At term placenta and fetal weight ratio is 1:6.
2.At 24 weeks of pregnancy fundal height reaches at the level of …… 24 weeks of pregnancy fundal height reaches at the level of …… 24 weeks of pregnancy fundal height reaches at the level of …… : umbilicus.🔸 24 weeks of pregnancy fundal height reaches at the level of umbilicus.
3……. is a Welcom sign of labour. …… is a Labor’s Welcome Sign : Show 🔸 Show is a Welcome sign of labour.
4.Excessive nausea and Vomiting during pregnancy are termed as …… Excessive nausea and vomiting during pregnancy are termed as …… : Hyperemesis Gravidarum.
🔸 Excessive vomiting and nausea during pregnancy is known as Hyperemesis Gravidarum.
5. Inflammation of Breast is Known as …… Inflammation of Breast is known as …… : Mastitis.🔸 Inflammation of Breast is known as Mastitis.
(B) True or False – Tell true false. 05
1.Pap test is done to detect ca. cervix. Pap test is used to detect cervical cancer : ✅ True
Explanation: Pap smear is used to screen for cervical cancer (Ca. cervix).
2.Life Span of Sperm is 24 hours. Sperm has a lifespan of 24 hours. : ❌ False
Explanation: Sperm can live up to 3–5 days in female reproductive tract, not just 24 hours.
3. Umbelical vein Carries deoxygenated blood. Umbelical vein carries deoxygenated blood. : ❌ False
Explanation: Umbilical vein carries oxygenated blood from the placenta to the fetus.
4. Painful Menstruation is Known as Dysmenorrhea. Menstruation that comes with excessive pain is called Dysmenorrhea. : ✅ True
Explanation: Dysmenorrhea refers to painful menstruation.
5.Episiotomy is Performed during first stage of Labour. Episiotomy is usually done during the second stage of labour to assist delivery. : ❌ False
Explanation: Episiotomy is usually done during the second stage of labour to assist delivery.
(c) Match the Followings – Match the Pairs. 05
A B
(1) Cleft palate (1) Softening of Cervix
Cleft palate (1) Softening of Cervix
Cleft palate (1) Softening of Cervix
(2) Dystocia (2) Premature Sepration of placenta
Dystocia Premature Separation of Placenta
(3)Tocolytic agent (3) Congenital Anomalies
Tocolytic agent (3) Congenital Anomalies
(4)Goodell’s Sign (4) Inhibit Uterine Contraction
(5)Abruptio Placenta (5) Abnormal Labour
Abruptio Placenta Abnormal Labour
(6) Placenta in lower uterine Segment
Placenta in lower uterine segment Be in a segment
(c) Correct Match :
| A (pair A) | B (pair B) | Correct Match (: A → B) |
|---|---|---|
| (1) Cleft palate | (3) Congenital Anomalies | (1) → (3) |
| (2) Dystocia | (5) Abnormal Labour | (2) → (5) |
| (3) Tocolytic agent | (4) Inhibit Uterine Contraction | (3) → (4) |
| (4) Goodell’s Sign | (1) Softening of Cervix | (4) → (1) |
| (5) Abruptio Placenta | (2) Premature Separation of Placenta | (5) → (2) |
