ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING 03/07/2017 PAPER SOLUTION NO.9 (3RD YEAR) (Done)-UPLOAD
ENGLISH-MIDWIFERY AND GYNECOLOGICAL NURSING 03/07/2017 PAPER SOLUTION NO.9
GYNECOLOGICAL NURSING 03/07/2017 PAPER SOLUTION NO.9
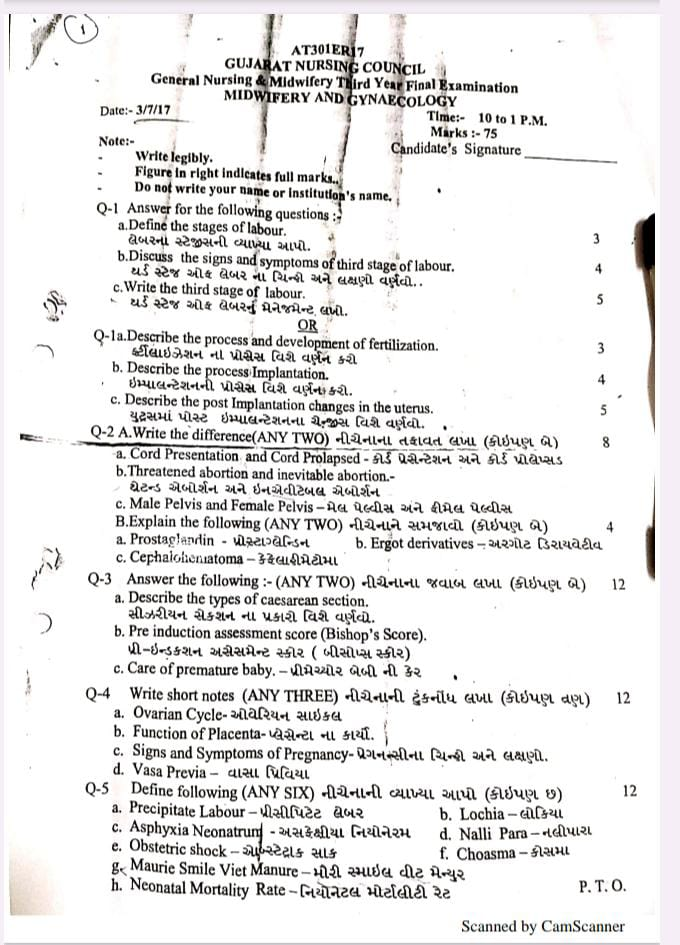
Q-1 Answer for the following questions:
a. Define the stages of labour. લેબરના સ્ટેજીસની વ્યાખ્યા આપો.
- Stages of Labor is an approach to divide the entire process from the onset of labor pain in the patient to the delivery of the placenta and the first hour thereafter into four stages. Specific physiological and clinical changes are observed in each stage.
- First Stage of Labor:
- This stage is the period from the onset of uterine contractions to the complete dilation of the cervical os to 10 centimeters.
- Second Stage of Labor:
- This stage begins after the completion of cervical dilation and continues until the complete delivery of the fetus.
- Third Stage of Labour:
- This stage is the period from the delivery of the fetus until the complete delivery of the placenta and membranes.
- Fourth Stage of Labour:
- This stage is the period up to the first hour after the delivery of the placenta, in which observation is important for the patient’s hemodynamic stability and complications such as postpartum hemorrhage.
b.Discuss the signs and symptoms of third stage of labour. થર્ડ સ્ટેજ ઓફ લેબર ના ચિન્હો અને લક્ષણો વર્ણવો.
- This stage starts with the expulsion of the fetus and the period till the expulsion of the placenta and membranes is called the third stage. Its duration is 15 minutes in primigravida and multigravida.
- The third stage of labor usually involves three phases.
- 1) Separation of the placenta from the uterine wall.
- 2) Descent down of the placenta.
- 3) Expulsion of the placenta
- 1) Separation of the placenta from the uterine wall:
- In this stage, the placenta starts to separate from the deep spongy layer of the decidua, the decidua basalis.
- Condition of the uterus before separation of the placenta:
- The uterus is discoid in shape.
- The uterus is firm.
- The uterus is below the umbilicus.
- It is non-bloatable.
- The fundal height is slightly below the umbilicus.
- Generally, two methods of separation of the placenta are involved.
- 1) Central Separation (Schultze Method)
- 2) Marginal Separation (Matthews Duncan Method)
- 1) Central Separation (Schultze Method) Schultze Mechanism:
- Usually the main factor for the separation of the placenta is uterine contraction and retraction, mainly due to the ability of the muscle fibers of the uterine cavity to retract, the separation of the placenta starts. Because with the expulsion of the fetus, the uterine cavity retracts. The discoid-shaped placenta does not remain attached normally in this retracted uterine cavity and due to this the placenta bends and its separation starts.
- Thus, in central separation, the placenta separates from the central part and with each uterine contraction and retraction, this separation increases, and the placenta bends and as the placenta separates from the central part, blood collection starts in the placenta and implantation site. This is called retroplacental hematoma. Because the accumulation of blood occurs in the posterior part of the placenta and the blood is not visible in it.
- 2) Marginal Separation (Matthews Duncan Method):
- Normally, the placenta is thin at its marginal site while it is thick at its central part. Due to the contraction and retraction ability of the muscle fibers, the margin of the placenta can be easily separated, so in marginal separation, with each contraction and retraction, the placenta starts to separate from the margin site and as the placenta starts to separate, blood becomes visible.
- Thus, there are generally two methods of placenta separation.
- 2) Descent down of placenta:
- After the separation of the placenta, due to uterine contraction and retraction, the placenta comes to the lower uterine segment or upper vaginal part and due to this, clinical signs of separation are seen:
- Signs of placental separation:
- Dark blood flows from each antrum.
- The umbilical cord protrudes 3 inches or more downward from the vaginal area and increases in length.
- The shape of the uterus changes from discoid to globular and contracts.
- 3) Expulsion of placenta:
- After the placenta has descended into the lower part of the uterine cavity, the placenta is expelled either by voluntary bearing down efforts of the mother’s abdominal muscles or by manipulative procedures.
C. Write the management of third stage of labour. થર્ડ સ્ટેજ ઓફ લેબરનું મેનેજમેન્ટ લખો.
- The management of the third stage is most crucial because it involves the separation and expulsion of the placenta from the uterine cavity and the third stage is to prevent complications of postpartum hemorrhage.
- The management of the third stage requires strict vigilance of the placenta, due to which complications of postpartum hemorrhage can be prevented.
- Stages of Management
- Currently, two methods are used in the management of the third stage.
- 1) Expectant (Watchful) Management
- 2) Active Management
- 1) Expectant (Watchful) Management
- In this management, the separation of the placenta and its descent into the vagina are allowed to occur spontaneously.
- For this management, minimal assistance is given for placental expulsion.
- In this stage, the mother is constantly watched, i.e. the mother should not be left alone even for a short time.
- If the mother is in a lateral position, then she should be given a dorsal position, due to which the signs of placental separation and the amount of blood loss can be properly observed.
- In this management, only the separation, descent and expulsion of the placenta are properly observed.
- One hand is placed on the fundus so that,
- a) the separation of the placenta can be observed.
- b) the state of uterine activity i.e. contraction and relaxation can be observed.
- Separation of Placenta
- The placenta starts separating from the uterine wall within a few minutes after the birth of the baby, so wait for 15 to 20 minutes for the placenta to separate on its own.
- No touch technique is used in this.
- In this, there is a “no touch policy” i.e. the placenta is expelled due to gravity in 15-20 minutes i.e. no massage on the fundus.
- Do not use any type of uterotonic and do not use any manual method for expulsion of the placenta.
- Expulsion of placenta
- When the placenta is expelled, the following points should be followed:
- Advise the patient to apply bear down forceps when the uterus becomes hard.
- The raised intra-abdominal pressure is important for the expulsion of the placenta.
- And the placenta can be expelled on its own.
- 2) Active Management
- 1) Use of Uterotonics
- Oxytocin is the drug of choice in the management of the third stage of labor.
- In the management of the third stage, 10 units of oxytocin should be provided IM (intramuscularly).
- Oxytocin enhances uterine contractions and helps in expelling the placenta.
- 2) CCT (Controlled Cord Traction)
- Controlled cord traction uses a manual method in which the umbilical cord is tracked and gently pulled downwards and backwards, which allows the placenta to separate from the uterine wall and then be expelled. However, controlled cord traction is performed by placing the hand on the suprapubic area when uterine contractions are present.
- 3) Fundal Pressure:
- Push the fundus downwards and backwards by placing four fingers behind the fundus and thumb in front of it. Apply pressure when the uterus is hard. If it is not hard, rub it gently to make it hard. Stop the pressure immediately when the placenta passes through the introitus. This method is more useful when the baby is macerated or premature as the tensile strength of the cord is low. If any clots are left inside, massaging the uterus helps in its expulsion.
- 4) Delayed Cord Cutting
- Wait for one to three minutes after delivery of the fetus and then cut the umbilical cord. This technique is more useful in term newborns. Because the newborn can receive adequate amount of blood from the placenta, due to which the condition of anemia can be prevented.
- But in preterm babies, the liver is immature and there is a high rate of breakdown of red blood cells and if the cord cutting is done, then the condition of hyperbilirubinemia (jaundice) can arise in the newborn.
- 5) Postpartum Vigilance
- After the delivery of the placenta, the placenta should be properly inspected, including the cotyledons, lobes, and the maternal and fetal sites and membranes. After the delivery of the placenta, fundal massage should be done, due to which the continuity of uterine contractions can be maintained and if there are retained bits of placenta, they can be expelled properly. And the condition of postpartum hemorrhage (PPH) in the mother can be prevented.
OR
Q-1.a.Describe the process and development of fertilization. કર્ટીલાઇઝેશન ના પ્રોસેસ વિશે વર્ણન કરો.03
- Introduction:
Fertilization is the fusion process of sperm and ovum to form a zygote. This process mainly takes place in the ampulla of the Fallopian tube. - Main stages of fertilization:
- Sperm Transport:
- During copulation, sperm is deposited in the vagina and reaches the fallopian tube through the uterus.
- Capacitation of Sperm:
- Sperm undergoes capacitation process with enzymes present in uterine and tubal fluids, which enables the sperm to cross the zona pellucida of the ovum.
- Acrosome Reaction:
- Hyaluronidase and other enzymes present in the acrosome break down the zona pellucida of the ovum.
- Penetration and Fusion:
- The sperm fuses with the plasma membrane of the ovum.
- The nucleus of the sperm fuses with the nucleus of the ovum and a diploid zygote is formed.
b. Describe the process Implantation. ઇમ્પાલન્ટેશનની પ્રોસેસ વિશે વર્ણન કરો.04
- Implantation is the process of the blastocyst implanting itself in the endometrium of the patient’s uterus and achieving compounding. This process usually occurs between the 6th and 10th day after fertilization. Proper implantation is important for the healthy development of the fetus.
- Main Stages of Implantation:
- Apposition:
- The blastocyst begins to settle on the endometrial lining.
- In this stage, the blastocyst finds a suitable location and stabilizes its position with the surface of the endometrium.
- Adhesion:
- Trophoblast cells fuse with endometrial cells.
- Molecules on the surface of trophoblast cells form a partial attachment to the endometrium.
- Invasion:
- Syncytiotrophoblast develops from trophoblast cells, which invades the endometrium.
- Lacunae form in the endometrial tissue, where maternal blood fills.
- Complete Embedding:
- The blastocyst completely fuses with the endometrium.
- In this stage, the blastocyst completely dissolves into the endometrium and begins the process of obtaining nourishment.
- Factors Facilitating Implantation:
- Uterine endometrium being in a receptive state (Maximum Receptivity around 20th-24th day of Menstrual Cycle).
- Appropriate hormonal support, especially the right amount of estrogen and progesterone.
- Having a good quality blastocyst.
c. Describe the post Implantation changes in the uterus. યુટ્રસમાં પોસ્ટ ઇમ્પાલન્ટેશનના ચેન્જીસ વિશે વર્ણવો. 05
- After implantation, various hormonal and cellular changes occur in the uterus and endometrium of the patient, which are essential for the stable development of pregnancy. These changes are collectively called decidual changes, which are important for the health of the patient and the nutrition of the fetus.
- Major Post-Implantation Changes:
- Decidual Reaction:
- Endometrial stroma cells differentiate into large, polyhedral and glycogen and lipid-rich decidual cells.
- These cells provide physical support to the uterus of the patient and lay the foundation for the nutrition of the fetus.
- Hormonal Changes:
- Trophoblast Cells secrete the hormone hCG (Human Chorionic Gonadotropin), which maintains the Corpus Luteum and increases the levels of Progesterone and Estrogen.
- This hormone makes the uterine endometrium richer and more nutritious.
- Uterine Vascular Changes:
- Spiral Arteries dilate and increase blood supply, so that adequate nutrition and oxygen are available to the Placenta and the developing fetus.
- Formation of Decidua:
- The endometrium is divided into three parts:
- Decidua Basalis: Responsible for placenta formation.
- Decidua Capsularis: Covers the developing embryo.
- Decidua Parietalis: Covers the rest of the uterine cavity.
- Immune Modulation:
- The patient’s immune system is modified so that it does not react against foreign antigens such as fetal tissue.
- Decidual cells secrete special cytokines and growth factors.
- Formation of Placenta:
- The development of the placenta begins with the trophoblast cells, which will provide nutrition, protection, and metabolic support for the fetus.
- Post-implantation changes work to create a healthy and nutritious environment in the patient’s uterus, providing adequate support for the development of the fetus from the beginning of pregnancy throughout the pregnancy. These changes are essential for a successful pregnancy and a healthy delivery.
Q-2 A. Write the difference(ANY TWO) નીચેનાનો તફાવત લખો (કોઇપણ બે).08.
a. Cord Presentation and Cord Prolapsed-કોર્ડ પ્રેસેન્ટેશન અને કોર્ડ પ્રોલેપ્સડ
| Order | Points of Difference | Cord Presentation | Cord Prolapse |
|---|---|---|---|
| 1 | Definition | The umbilical cord is near the uterine os in front of the presenting part, but the membranes are intact. | After the membranes rupture, the umbilical cord comes out in front of the presenting part and into the vagina. 2. Membranes Status Membranes are intact Membranes are ruptured. 3. Risk There is little immediate risk to the fetus. There is a high risk of hypoxia and death to the fetus. 4. Diagnosis The cord is palpable on vaginal examination but not visible. The cord is visible and palpable up to the vagina. |
| 5 | Patient Symptoms | No special symptoms, only the cord is palpable. | Fetal Heart Rate is abnormal, the cord is visible outside, and the patient is panicking. |
| 6 | Management | The patient is given bed rest, positional therapy such as Trendelenburg Position, and attempts are made to prevent rupture of the membranes. | Immediate emergency medical management, relieving pressure on the cord, giving the knee-chest position, and expedited delivery, preferably emergency Cesarean Section. is done. |
b.Threatened abortion and inevitable abortion.થ્રેટેન્ડ એબોર્શન અને ઇનએવીટેબલ એબોર્શન
| Order | Points of Difference | Threatened Abortion | Inevitable Abortion |
|---|---|---|---|
| 1 | Definition | A condition in which the pregnancy can proceed despite bleeding and pain during pregnancy. | A condition in which the loss of the pregnancy is certain and cannot be prevented. |
| 2 | The cervical os | is closed. Is. | Open. |
| 3 | Bleeding | Spotting or light bleeding. | Heavy bleeding. |
| 4 | Pain | Usually mild pain or cramping. | Severe and constant pain, especially in the lower abdomen. |
| 5 | Viability of Pregnancy | With appropriate treatment, the pregnancy can survive. | The pregnancy cannot survive, it is essentially terminated. |
| 6 | Management | The patient may be given bed rest, sedatives, and hormonal support such as progesterone. | Preparation for delivery and medical or surgical procedures such as uterine evacuation may be necessary. |
c. Male Pelvis and Female Pelvis-મેલ પેલ્વીસ અને ફીમેલ પેલ્વીસ.
| Order | Points of Difference | Male Pelvis | Female Pelvis |
|---|---|---|---|
| 1 | Overall Structure | Heavy, Thick Bones and Strong Structure. | Light, Thin Bones and Soft Texture. |
| 2 | Shape | Heart Shaped Pelvic Inlet. | Oval/Round Pelvic Inlet. |
| 3 | Pelvic Cavity | Narrow and Deep. | Wide and Shallow. |
| 4 | Pelvic Outlet | Smaller and blocked. | Larger and open. |
| 5 | Pubic Arch Angle | Small, about 50°-60°. | Large, about 80°-85°. |
| 6 | Iliac Wings (Iliac Wings) Wings) | Vertical and close-in. | Very open and far-out. |
| 7 | Sacrum | Long, narrow and more curved. | Short, broad and less curved. |
| 8 | Pelvic Inlet | Heart-Shaped. | Oval or Round-Shaped. |
| 9 | Function of the Pelvis | More suitable for body support and walking. | For Childbirth Convenient. |
B.Explain the following (ANY TWO) નીચેનાને સમજાવો.(કોઇપણ બે). 4
a. Prostaglandin પ્રોસ્ટાગ્લેન્ડીન
- Introduction
- Prostaglandins are derived from prostaglandinic acid and act as local hormones. They were first described by von Euler in 1935.
- Prostaglandins are not hormones but autocolloids. They are derivatives of prostaglandin acid. They also act as local hormones. In general, prostaglandins are synthesized from an essential fatty acid, arachidonic acid, which is widely distributed throughout the body. In females, they are found in the menstrual fluid, endometrium, decidua, and amniotic membrane.
- Chemistry:
Prostaglandins are 20-carbon carboxylic acids containing a cyclopentane ring, which are made up of polyunsaturated fatty acids. - Varieties:
- There are many varieties of prostaglandins, the most commonly used prostaglandins are:
- such as,
PGE2-prostin E2 (dinoprostone),
PGF2α-prostin F2α (dinoprost tromethamine),
PGE1-misoprostol. - Indications:
- For induction of abortion,
- Medical termination of pregnancy,
- Termination of molar pregnancy,
- For induction of labor,
- For cervical ripening before abortion or induction of labor.
- For augmentation (acceleration) of labor.
- For management of atonic postpartum hemorrhage.
- For medical management of tubal ectopic pregnancy.
- For induction of labor when infra uterine fissuring has occurred.
- Contraindications:
- Absolute:
- Hypersensitivity to the compound,
- Asthma,
- Acute pelvic inflammatory disease (PID),
- Uterine fibrosis,
- Cervical stenosis,
- Pelvic surgery.
- Relative:
- Hypertension,
- Cardiovascular disease,
- Renal or hepatic disease,
- Peptic ulcer,
- Jaundice,
- Uterine scar,
- Active cardiac,pulmonary,
- Hypotension (PGE2).
- Route:
- Prostaglandins can be provided by different routes such as:
- Orally (misoprostol for ulcers),
- Vaginal (dinoprost for labor induction),
- Intravenously (e.g. epoprostenol for pulmonary hypertension),
- Intramuscular (e.g. alprostadil).
- Dosage:
- 1.Tablets – Contain 0.5 mg Prostin E2.
- Vaginal suppository – containing 20 mg PGE2 or 50 mg PGF2α.
- Vaginal pessary – containing 3 mg PGE2.
- Prostin F2α 1mg/ml, Prostin E2, 5 mg/ml are available in injectable ampoules or vials.
- Misoprostol (PGE₁) 50 mg is given orally, vaginally or rectally every four hours for labor induction.
- Mechanism of action:
Both PGE2 and PGF2α have an oxygenating effect on the uterus. PGF2α acts mainly on the myometrium and PGE2 mainly on the cervix. - Side effects:
Nausea, vomiting, diarrhea, abdominal pain. - Uterine hyperstimulation: Excessive contraction of the uterus.
Headache.
Flushing: Skin redness and warmth.
Dyspnea: Changes in blood pressure.
Allergic reaction: Skin rashes.
Increased risk of bleeding. - Nursing Responsibilities:
- Properly assess the patient’s respiratory rate, rhythm, and depth.
- Indicate any vaginal discharge, itching, or irritation.
- Administer an antiemetic or antidiarrheal before providing the drug.
- When vaginal preparations are used, they should be placed in the vagina, but before that, they should be rinsed with warm water on the package.
- Note the length and duration of the contractions properly.
- If contractions are weak or absent, inform the doctor immediately.
- If the vaginal route is preferred, advise the patient to remain in the supine position for 10 to 15 minutes.
b. Ergot derivatives – અર્ગોટ ડિરાયવેટીવ
- Two of the ergot derivatives, ergometrine and metargine, are commonly used as oxytocics.
- Group:
- Classification: Uterotonic
- Type: Ergot alkaloid
- Chemistry: Ergometrine is an amine alkaloid. It is isolated from the fungus Claviceps purpurea, which grows on cereals such as rye and wheat.
- Indications:
- Therapeutic:
To stop atonic or eutonic uterine bleeding after delivery, abortion or expulsion of hydatidiform mole. - Prophylactic:
Used as a prophylaxis to prevent excessive hemorrhage after delivery. - Other Indications:
- Induction of abortion,
- For the prevention and treatment of PPH condition.
- Hydatidiform mole.
- Subinvolutions of uterus.
- Contraindications:
- Ergometrine/ Methergine: Pregnancy, 1st stage of labor, 2nd stage of labor and breech delivery before crowning of head.
- Suspected multiple pregnancy.
- In severe preeclampsia and eclampsia conditions.
- Cardiac disease.
- Hypertension.
- Severe liver and kidney disease.
- Rh – ve factors.
- In preeclampsia/ eclampsia conditions.
- Abruptio placentae.
- After delivery of 1st baby in cases of multiple pregnancy.
- Route:
- IM (intramuscular),
Oral - Dosage:
- Methylergometrine (methargine)
- Postpartum: 0.2 mg IM after delivery; may be repeated every 2-4 hours as needed (maximum 5 doses).
- Oral: 0.2 mg three times a day for 7 days for specific cases.
- Ergometrine (ergonovine)
- Dosage:
- Postpartum: 0.2 mg IM after delivery; may be repeated every 2-4 hours as needed.
- IV: 0.2 mg may be administered in acute situations, but IM is usually preferred.
- Mode of Action:
- There are certain types of receptors in the myometrium layer of the uterus. For example, serotonin (5 HT) and alpha adrenergic receptors stimulate it. Due to this, the level of calcium inside the cells starts increasing. That is, the number of calcium iron starts increasing. Due to this, strong and sustained uterine contractions are produced. Thus, when uterine contractions start, it helps in reducing the condition of postpartum hemorrhage (PPH) and also helps in uterine involution.
- Side effects:
- Nausea and vomiting,
- Headache,
- Blood pressure,
- Dysfunction,
- Diarrhea,
- Hypertension,
- Myocardial ischemia,
- Uterine rupture.
- Nursing Responsibility:
- 1.Monitoring:
- Properly monitor the patient’s vital signs.
- Properly monitor uterine tone and bleeding.
- Properly monitor for any advanced reactions.
- Immediately monitor the mother’s vital signs.
- Administer antiemetic medication if vomiting is uncontrollable.
- 2.Education:
- Properly monitor for any side effects.
- Properly monitor the patient for any signs and symptoms of severe chest pain, headache, and palpitations.
- 3.Administration:
- Properly provide medication to the patient.
- Administer intramuscular (IM) injections properly to the patient.
- 4.Documentation:
- Documentation is required to ensure that the patient has been properly provided with medication.
c. Cephalohematoma- કેફેલોહીમેટોમા
- Cephalohematoma is a subperiosteal hemorrhage caused by the accumulation of serum or blood between the periosteum and cranial bone of the skull bone of a newborn patient.
- Clinical Features:
- A soft, palpable, and clearly circumscribed swelling is seen on one or more bones of the skull of a newborn patient.
- This swelling is usually more common on the parietal bone.
- The swelling is more circumscribed than that of a caput succedaneum and does not cross suture lines.
- The patient is usually not in pain.
- Causes:
- Prolonged Labour.
- Forceps Delivery or Vacuum Extraction.
- Tight Natural Birth Canal.
- More Medical Interventions and Obstetrical Trauma.
- Difference:
- The main difference between Cephalohematoma and Caput Succedaneum is that Cephalohematoma does not cross the suture lines and has a late dissolution, while Caput Succedaneum crosses the suture lines and merges soon.
- Complications:
- Jaundice – Bilirubin levels increase due to the remnants of the blood clot.
- In rare cases, calcification and skull deformity.
- Anemia in extreme cases.
- Management:
- No specific treatment is usually required; this is self-resolving.
- Phototherapy may be given if the patient has high bilirubin levels.
- Antibiotic therapy may be given if the cephalohematoma is large and there are signs of infection.
- Aspiration may be required in rare cases.
- Conclusion:
Cephalohematoma is usually harmless and resolves within a short time. However, close observation of the patient and medical intervention when necessary are necessary.
Q-3 Answer the following:- (ANY TWO) નીચેના નો જવાબ આપો (કોઇપણ બે)12
a. Describe the types of caesarean section. સીઝેરીયન સેક્શન ના પ્રકારો વિશે વર્ણવો.
- What is Caesarean Section?
- Caesarean Section is a surgical procedure in which a cut is made on the patient’s abdomen and uterus and delivery is performed. This type of surgery is done when normal delivery is not possible. This process is done completely aseptically and under anesthesia.
- Types of Caesarean Section
- Lower Segment Caesarean Section (LSCS)
- This is the most common type. In it, a transverse incision is made on the lower uterine segment.
- In this type, bleeding is reduced, the wound heals faster and is also considered safer for future pregnancies.
- 2.Classical Caesarean Section
- In this type, a vertical incision is made on the upper uterine segment.
This is used in very few cases in today’s obstetrics — such as if the pelvis is very small, the placenta is anterior, or the fetal position is very abnormal.
In this, bleeding is more and recovery is also longer. - 3.Emergency Caesarean Section
- When the patient or fetus has a life-threatening condition, the operation is called an emergency caesarean.
Such as – fetal distress, breech presentation, abnormal results in cardiotocography, etc. - 4.Elective Caesarean Section
- This operation is planned and scheduled in advance.
- This type of Caesarean is done in cases such as – two previous Caesareans, Placenta Praevia, Uterine Abnormality, or Multiple Pregnancy.
- 5.Repeat Caesarean Section
- When the patient has already had one or more Caesareans and has to deliver again by Caesarean, it is called Repeat Caesarean.
- In this, the surgery is done keeping in mind the previous uterine scar.
- 6.Crash Caesarean Section
- This is an extreme emergency in which an immediate operation is required, such as in cases of placenta abruption or umbilical cord prolapse.
- Each type of Caesarean Section is selected by the Obstetrician, taking into account the medical condition of the patient and the well-being of the fetus. The right type of surgery and its proper management ensure safety for both the mother and the child.
b. Pre induction assessment score (Bishop’s Score). પ્રી-ઈન્ડકશન અસેસમેન્ટ સ્કોર (બીસીપ્સ સ્કોર)
- Bishop’s Score is a clinical scoring system used in Obstetrics to determine how ready a patient’s cervix is for “Induction of Labor”.
- Based on this score, the doctor can decide whether to medically induce labor in the patient or not. If the score is high, the cervix is considered mature and labor is more likely to begin successfully.
- Main Parameters – Parameters of Bishop’s Score
- Bishop’s Score is determined based on five main parameters. Each parameter is given a score of 0 to 3. The total score can range from 0 to 13.
- 1.Cervical Dilatation:
- This parameter gives an estimate of how open the cervix is.
- 0 cm = Score 0
- 1–2 cm = Score 1
- 3–4 cm = Score 2
- ≥5 cm = Score 3
- 2.Cervical Effacement
- A measure of how thin the cervix has become.
- 0–30% = Score 0
- 40–50% = Score 1
- 60–70% = Score 2
- ≥80% = Score 3
- 3.Cervical Consistency
- Indicates the texture of the cervix.
- Firm = Score 0
- Medium = Score 1
- Soft = Score 2
- 4.Cervical Position
- Indicates where the cervix is located in the uterus.
- Posterior = Score 0
- Mid-position = Score 1
- Anterior = Score 2
- 5.Fetal Station
- Evaluation of how low the fetal head is in the pelvis.
- -3 station = Score 0
- -2 station = Score 1
- -1/0 station = Score 2
- +1/+2 station = Score 3
- Interpretation – Evaluation of the score
- The Bishop’s Score is used to predict whether labor induction will be successful for the patient.
- ≥8 score: The cervix is fully mature. The success of induction of labor is very high.
- 5–7 score: The cervix is partially mature. Prostaglandin therapy can be used to induce labor.
- <5 score: The cervix is unfavorable. Cervical dilation is necessary first.
- Important Points
- Bishop’s Score has some relaxed scoring criteria for multiparous patients.
- The score indicates how prepared the patient’s body is for labor and based on this the doctor selects agents.
- It is very important to maintain sterile technique during scoring.
- Bishop’s Score is an important assessment tool in Obstetric Practice, which helps in determining the appropriate time and method for induction by assessing the cervical status of the patient. Based on this score, appropriate decisions are made for the safe management of the patient and the fetus.
c. Care of premature baby.-પ્રીમેચ્યોર બેબી ની કેર
- Premature Baby is a newborn infant who is born before 37 weeks. Since these babies are not completely developed, they need special care. They are more sensitive and their organs are not completely mature, so special neonatal care is required for these babies.
- 1.Thermal Regulation:
- Premature babies have less ability to regulate their skin temperature and brown fat.
- Keep the baby in a radiant warmer or incubator.
- Skin-to-Skin Contact (Kangaroo Care) is also very effective, which is called Kangaroo Mother Care.
- Maintain the room temperature between 25–28°C.
- 2.Respiratory Support (Respiratory Support):
- Respiratory Distress Syndrome (RDS) is seen in premature babies because the lungs are not fully developed.
- Oxygen Therapy should be given if necessary.
- In some cases, Continuous Positive Airway Pressure (CPAP) or Mechanical Ventilation may also be given.
- Surfactant Therapy is also given, which prevents the alveoli from collapsing.
- 3.Nutritional Support:
- Premature babies do not develop the ability to drink milk orally, so Gavage Feeding or Parenteral Nutrition is necessary in the beginning.
- Expressed Breast Milk (EBM) or Donor Human Milk is the safest.
- Milk is adjusted for its growth with Fortifiers.
- 4.Infection Prevention:
- Premature babies have an immature immune system, so they are more susceptible to infections.
- Maintain Strict Hand Hygiene.
- Use sterilized equipment.
- Perform Minimal Invasive Procedures.
- Adopt Barrier Nursing Techniques for parents and visitors as well.
- 5.Monitoring and Observation:
- Continuous monitoring of Heart Rate, Respiratory Rate, Oxygen Saturation (SpO₂).
- Daily weight checking.
- Observation of urine output, stooling and feed tolerance is necessary.
- 6.Parental Education and Emotional Support:
- Training parents about the baby’s condition, care and kangaroo care.
- Understanding the emotional needs of parents and supporting them.
- Counseling for home care after discharge is necessary.
- 7.Follow-up Care:
- Developmental Assessment of premature babies should be done at regular intervals.
- Vision Screening (ROP – Retinopathy of Prematurity)
- Hearing Test (Auditory Brainstem Response)
- Neurodevelopmental Evaluation. All these are necessary to prevent any long-term complications.
- Care for a premature baby should be very delicate and multi-disciplinary. It should be managed with complete coordination between expert doctors, nurses, and parents so that the overall development of the baby can be ensured safely.
Q-4 Write short notes (ANY THREE) નીચેનાની ટુંકનોંધ લખા (કોઇપણ ત્રણ)12
a. Ovarian Cycle- ઓવેરિયન સાઇકલ :
- Ovarian Cycle is a regular hormonal cycle in the female reproductive system, through which a mature ovum is released from the ovary. This system is controlled by the endocrine glands and is one of the main aspects of fertility.
- The Ovarian Cycle is usually 28 days long and is divided into three main stages:
- Follicular Phase:
- This stage begins on the first day of the cycle with menstruation and lasts until ovulation.
- During this phase, Follicle Stimulating Hormone (FSH) is secreted from the Pituitary Gland.
- FSH is responsible for the growth of primary follicles inside the ovary.
- One follicle becomes dominant and develops into a Graafian Follicle.
- This follicle secretes the hormone Estrogen which stimulates the endometrium to thicken and proliferate.
- Ovulation Phase:
- This phase usually occurs in the middle of the cycle, around day 14.
- Estrogen levels peak, which stimulates the pituitary gland to release Luteinizing Hormone (LH).
- With the LH surge, the dominant follicle ruptures and a mature ovum is released — this is called ovulation.
- The ovum travels to the Fallopian Tube and is ready to be fertilized by a sperm.
- 3.Luteal Phase:
- After ovulation, the ruptured Graafian follicle converts into the Corpus Luteum.
- The Corpus Luteum secretes Progesterone and a little Estrogen.
- Progesterone makes the endometrium thicker and more secretory, which prepares it for embryo implantation.
- If fertilization occurs, the Human Chorionic Gonadotropin (hCG) hormone starts to be secreted and the Corpus Luteum remains active for a long time.
- If fertilization does not occur, the Corpus Luteum degenerates and the hormone level decreases, due to which the endometrium breaks down and menstruation begins.
- Hormonal Regulation:
- The activity of the ovarian cycle is mainly controlled by four hormones:
- 1.FSH (Follicle Stimulating Hormone)
- 2.LH (Luteinizing Hormone)
- 3.Estrogen
- 4.Progesterone
- This hormone directly affects the ovarian and uterine cycles.
- Clinical Importance:
- Disruption in the ovarian cycle i.e. hormonal imbalance, PCOS, lack of ovulation etc. can lead to infertility.
- This cycle can be controlled by using hormonal pinning or contraceptive pills.
b. Function of Placenta – પ્લેસેન્ટા ના કાર્યો.
- 1) Respiratory function:
The fetus receives oxygen and excretes carbon dioxide through the placenta.
Just as oxygen passes from the mother’s blood to the fetal blood, carbon dioxide in the fetus is transmitted to the maternal blood through the placenta. - 2) Nutritive function:
All types of nutrients such as amino acids, glucose, vitamins, minerals, lipids, water and electrolytes are transmitted from the mother to the fetus. - The food taken in the maternal diet reaches the placental side, where it becomes a simple form, after which the placenta selects the substances required by the fetus and transmits them to the fetus.
- 3) Storage function:
The placenta stores glucose, iron and vitamins. And the placenta provides it when the fetus needs it. - 4) Excretory function:
The waste products in the fetus are transmitted to the placenta. - 5) Protection:
The placental membrane has a limited barrier function. Some antibodies pass from the mother to the fetus, which provide immunity to the baby for three months after birth. - 6) Immunological function:
The antigens of the fetus and placenta act as foreign to the mother. However, graft rejection does not occur because the placenta provides immunological protection against rejection. - 7) Hormonal function:
- Steroid hormones:
Oestrogen,
Progesterone. - Protein hormones
HCG(Human Chorionic Gonadotropin),
HPL(Human Placental Lactogen),
Relaxin,
PAPPA(Pregnancy Associated Plasma Protein:= A). - •>HCG(Human Chorionic Gonadotropin):
HCG(Human Chorionic Gonadotropin) is produced by the cytotrophoblastic layer of the chorionic villi.
HCG(Human Chorionic Gonadotropin) is high during the 7th to 10th week of pregnancy and then decreases as the pregnancy progresses. It maintains the corpus luteum.
HCG(Human Chorionic Gonadotropin) is used in pregnancy tests because it is excreted in the mother’s urine. - HCG (Human Chorionic Gonadotropin) is detected in the blood 7 days after fertilization and in the urine 9 days after fertilization, which indicates a positive pregnancy test.
- •> HPL (Human Placental Lactogen):
HPL (Human Placental Lactogen) is produced by the placenta and is involved in the lactogenic and metabolic processes of pregnancy. When the level of human chorionic gonadotropin trophin decreases, the level of human placental lactogen (HPL) increases and continues throughout pregnancy. Human Placental Lactogen (HPL) acts as an anti-insulin which helps in increasing the glucose level in the blood and supplying glucose to the fetus. - •>Relaxin
Relaxin is produced by decidua cells. It softens the cervix and helps relax the pelvic ligaments and symphysis pubis during the labor process. - •>PAPPA (Pregnancy Associated Plasma Protein: A)
Pregnancy Associated Plasma Protein: A works as an immunosuppressant and works to maintain pregnancy. - •> Estrogen
Estrogen is produced by the placenta throughout pregnancy. It is essential for the well-being of the fetus.
Estrogen increases during labor, which helps in the release of oxytocin, which increases uterine contractions. - •> Progesterone
Progesterone is produced by the syncytial layer of the placenta and acts as a tocolytic agent and prevents uterine contractions, as well as acting as an immunosuppressant to help maintain pregnancy.
c. Signs and Symptoms of Pregnancy- પ્રેગનેન્સીના ચિન્હો અને લક્ષણો.
- There are three main signs of pregnancy which are as follows.
- Presumptive Signs
- Probable Signs
- Positive Signs
- Presumptive Signs:
- Mostly subjective i.e. the mother herself feels that she is pregnant when it could also be due to other illnesses.
- Amenorrhea,
- Nausea and vomiting,
- Morning sickness,
- Tingling sensation in 3 to 4 weeks,
- Enlargement of breast and nipple, Appearance of Montgomery tubercles in the breast.
- Increased urination, Colostrum expressed from the nipple.
- Pigmentation in the face and breast. (Chloasma, Linea Nigra, Striae Gravidarum),
- Quickening: The first movement of the mother and fetus is felt at about 16 – 20 weeks.
- Probable Signs:
- Probable signs are maternal physiological changes. They can be detected during examination. They are objective but cannot be said to be the exact confirmation of pregnancy.
- Enlargement of the abdomen. Pregnancy can be detected by abdominal palpation.
- Changes in the size and shape of the uterus and enlargement of the uterus.
- External and internal ectropion.
- A positive pregnancy test means the detection of the hormone human chorionic gonadotropin (HCG) in the urine. The following signs are seen in it:
- Jacquemier sign or Chadwick sign:
- This sign appears during the 8th week of pregnancy. In this, bluish discoloration of the vulva, vagina and cervix is called Chadwick sign, while bluish discoloration of the vagina is called Jacquemier sign.
- Heartman sign:
- This sign is seen between the 1st and 3rd month of pregnancy. In this, slight bleeding is seen when the fertilized egg implants in the uterine cavity.
- Palmar sign:
This sign is seen during 4-8 weeks of pregnancy. In this sign, regular and rhythmic contractions of the uterus occur when bimanual examination is done. - Goodell’s sign:
Goodell’s sign is seen up to 6 weeks and there is softening of the lower part of the cervix. - Hegar’s sign:
This sign is seen between 6 and 10 weeks and there is enlargement of the upper part of the uterus i.e. the body part of the uterus with the growth of the fetus and softening of the lower part of the uterus. In Hegar’s sign, there is cyanosis and softening of the cervix, there is a softening between the uterus and the cervical isthmus (Around 6-8 weeks). - Piskacek’s sign:
This sign is seen during 6-8 weeks in which the uterus enlarges asymmetrically due to lateral implantation in the uterus. - Osiander’s sign:
This sign is seen during 6-8 weeks. In this sign, pulsation is felt in the lateral fornix in the vaginal area. - Braxton Hicks Contractions:
In the beginning of pregnancy, the uterus contracts on its own. They are regular, infrequent, spasmodic, painless, due to which there is no effect on the dilation of the cervix. They increase closer to term and finally merge with the painful contractions of labor. The presence of a placenta in which,
Internal placentation and external placentation occur: - Internal placentation: After the sixteenth week, vaginal examination shows the presence of a body that moves on tapping and later returns to its place with a thud.
- External placentation: Around the 20th week of pregnancy, a placenta is felt in the uterus under the hand while palpating the uterus by hand. This is known as external placentation.
- Positive Signs: Positive signs confirm pregnancy. In which the examiner detects the placenta and documents it.
- Visualization of Fetus by Ultrasound: This test confirms pregnancy and also assesses the lie, presentation, fetal heart sound, location of placenta, amount and distribution of amniotic fluid and internal os. Fetal abnormalities such as encephalitis, spina bifida, myelomeningocele, etc., as well as uterine and ovarian abnormalities are detected by this method.
Routinely, the scan is recommended during the mid-trimester before the 20th week of pregnancy. In case of serious fetal abnormalities, the patient may be advised to terminate the pregnancy. - Pregcolor and pregcolor-card test: These are mostly used as home kits to confirm pregnancy. This color-changing card test is easy and can be done by the woman herself. The presence of 2 lines on the card test on the 5th day after missed periods confirms pregnancy.
- Hearing the fetal heart sound: The fetal heart sound is heard on the fetoscope after 20 weeks.
- Fetal movements: Fetal movements are felt at 22 weeks.
- Palpation of Fetal Parts: Fetal parts are palpable after 24 weeks
- Frequency of micturition: It is usually experienced at the end of term in which frequency of micturition occurs due to engagement of the fetal head.
- Radiography: It is not usually advocated in pre-conception practice.
Radiographic pelvimetry is rarely indicated in selected cases of suspected cephalopelvic disproportion. - Radioimmunoassay: This is a very sensitive method and can be used to detect the presence of hCG in maternal serum and urine 7-8 days after ovulation or at the time of implantation.
It confirms the presence of pregnancy 3 weeks after conception. The concentration of hCG in the mother’s serum doubles every 2-3 days until it reaches a peak value 2-3 months after conception (Blackburn 2007). - The embryo can be seen on ultrasonography by 6 weeks, after which the fetus can be seen.
- Radiological appearance of the fetal skeletal system.
- Visualization of the fetal skeleton on X-ray.
- Visualization of fetal movement in late pregnancy.
d. Vasa Previa – વાસા પ્રિવિયા
- Vasa previa is an obstetric complication in which the fetal blood vessels pass through or near the internal orifice of the uterus and are in front of the presenting part. When the supporting membrane ruptures, these vessels are at risk of rupture because they are unsupported by the umbilical cord or placental tissue. These complications can arise during labor and delivery.
- Etiology:
- Low-lying placenta may be due to uterine scarring resulting from previous miscarriages and D and C (dilation and curettage).
- Abnormally or unusually formed placenta can be a bilobed placenta or a succentrate-low placenta.
In-vitro fertilization pregnancies and multiple pregnancies (twins and triplets).
Due to velar insertion of umbilical cord. - Risk factors of vasa previa:
- Placenta previa,
Velamar insertion of umbilical cord,
Multilobed placenta,
Multiple pregnancies. - Symptoms and signs:
- Painless vaginal bleeding (2nd and 3rd trimester).
Darker red color blood (because baby’s blood is dark color, bright red blood means mother’s blood).
Fetal bradycardia. - Diagnostic evaluation:
- History collection,
Physical examination,
Ultrasonography:
Transvaginal sonography in combination with color Doppler helps detect vasa previa as early as the 16th week of pregnancy.
Note the triad of signs:
Painless vaginal bleeding,
Membrane rupture,
Fetal bradycardia or death. - Treatment:
- If blood vessels rupture, hospitalize the mother in the 3rd trimester to ensure rapid access to medical care.
- Cesarean section should be performed around 35 weeks of pregnancy.
- Healthy delivery by cesarean section is the only treatment plan to follow. Cesarean section should be planned as early as possible to avoid emergencies and late enough to prevent problems related to prematurity. Usually, a cesarean section is recommended at 35-36 weeks if the mother is normal without any risks.
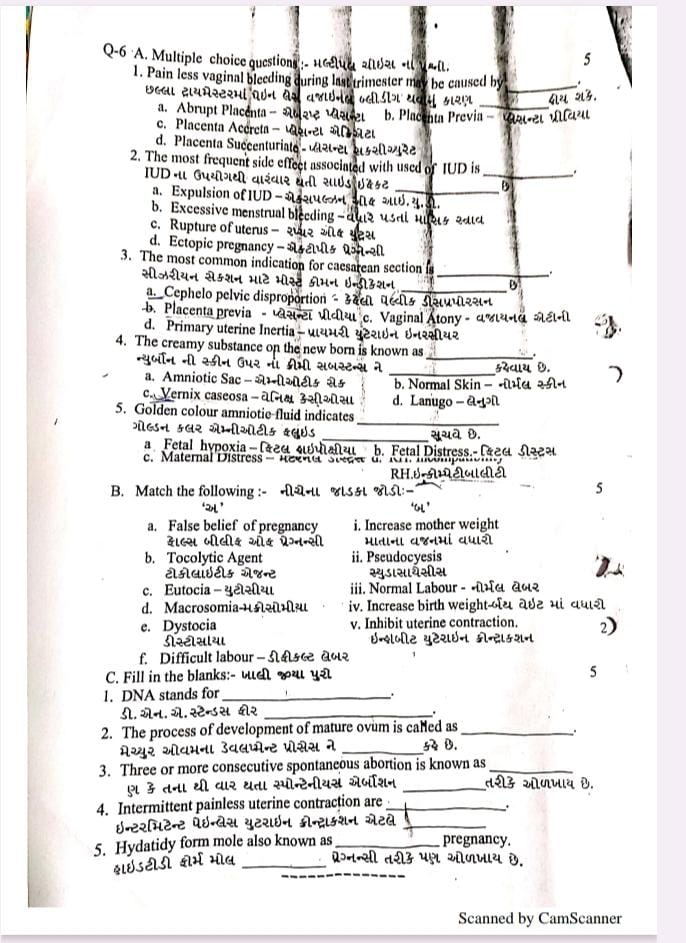
Q-6 A. Multiple choice questions :- મલ્ટીપલ ચોઇસ ના પ્રશ્નો.5
1.Pain less vaginal bleeding during last trimester may be caused by…… છેલ્લા ટ્રાયમેસ્ટરમાં પેઇન લેસ વજાઇનલ બ્લીડીંગ થવાનું કારણ……હોય શકે.
a. Abrupt Placenta – એબરપ્ટ પ્લેસન્ટા
b. Placents Previa – પ્લેસેન્ટા પ્રિવિયા
c. Placenta Accreta- પ્લેસન્ટા એક્રિએટા
d. Placenta Succenturiata –
પ્લેસન્ટા સકસીચ્યુરેટ
2.The most frequent side effect associated with used of IUD is……
IUD ના ઉપયોગથી વારંવાર થતી સાઇડઇફેક્ટ……છે.
a. Expulsion of IUD – એકાપલ્ઝન ઓફ આઇ.યુ.ડી.
b. Excessive menstrual bleeding – વધારે પડતાં માસિક સ્ત્રાવ
c. Rupture of uterus – રપ્ચર ઓફ યુટ્રસ
d. Ectopic pregnancy – એક્ટોપીક પેગ્નેન્સી
3) The most common indication for caesarean section is …… સીઝરીયન સેક્શન માટે મોસ્ટ કોમન ઇન્ડીકેશન……છે.
a. Cephelo pelvic disproportion – કેફેલી પેલ્વીક ડીસપ્રપોરશન
b. Placenta previa – પ્લેસન્ટા પ્રીવીયા
c. Vaginal Atony – વજાયનલ એટીની
d. Primary uterine Inertia – પ્રાયમરી યુટેરાઇન ઇનરસીયર
4.The creamy substance on the new born is known as …… ન્યુર્બોન ની સ્કીન ઉપર ના ક્રીમી સબસ્ટન્સ ને …… કહેવાય છે.
a. Amniotic Sac – એમ્નીઓટીક સેક
b. Normal skin -નોર્મલ સ્કીન
c. Vernix caseosa – વેનિક્સ કેસીઓસા
d. Lanugo – લેનુગો
5.Golden colour amniotic fluid indicates …… ગોલ્ડન કલર એમ્નીઓટીક ફ્લુઇડ …….છે.
a. Fetal hypoxia –
ફિટલ હાઇપોક્સીયા
b. Fetal Distress –
ફિટલ ડીસ્ટ્રેસ
c. Maternal Distress –
મેટરનલ ડીસ્ટ્રેસ
d. R.H. incompatibility –
R.H. ઇન્કોમ્પેટીબીલીટી
B. Match the following:- નીચેના જોડકા જોડો : –
‘ અ ‘ ‘ બ ‘
a. False belief of pregnancy i. Increase mother weight – માતાના વજનમાં વધારો
b. Tocolytic Agent ટોકોલાઇટીક એજન્ટ ii. Pseudocyesis સ્યુડોસાયેસીસ
c. Eutocia – યુટોસીયા iii. Normal Labour – નોર્મલ લેબર
d. Macrosomia-મેક્રોસોમીયા iv. Increase birth weight – બર્થ વેઇટ માં વધારો
f. Difficult labour-ડીફીકલ્ટ લેબર e. Normal Dystocia નોર્મલ ડીસ્ટોસીયા
v. Inhibit uterine contraction – ઇન્હીબીટ યુટેરાઇન કોન્ટ્ર્રાક્શન
✅ Correct Matching:
| ‘અ’ (Column A) | ‘બ’ (Column B) | Explanation |
|---|---|---|
| a. False belief of pregnancy | ii. Pseudocyesis | Pseudocyesis – False pregnancy belief without actual conception. |
| b. Tocolytic Agent (ટોકોલાઇટિક એજન્ટ) | v. Inhibit uterine contraction | Tocolytic agents are drugs that suppress uterine contractions to prevent preterm labor. |
| c. Eutocia (યૂટોસિયા) | iii. Normal Labour | Eutocia refers to normal and uncomplicated labor. |
| d. Macrosomia (મેક્રોસોમિયા) | iv. Increase birth weight | Macrosomia means the fetus has a birth weight of more than 4000-4500 grams. |
| f. Difficult Labour (ડિફિકલ્ટ લેબર) | e. Normal Dystocia | Dystocia indicates difficult or obstructed labor. |
C. Fill in the blanks:- ખાલી જગ્યાઓ પુરો.05
1.DNA stands for …… ડી. એન. એ. સ્ટેન્ડસ ફીર …… ➡️ Deoxyribonucleic Acid
Explanation: DNA is the genetic material found in the nucleus of cells responsible for heredity and genetic information.
2.The process of development of mature ovum is called as……મેચ્યુર ઓવમના ડેવલમેન્ટ પ્રોસેસ ને …… કહે છે. ➡️ Oogenesis
Explanation: Oogenesis is the process by which the female gametes (ova) develop in the ovaries.
3.Three or more consecutive spontaneous abortion is known as …… ત્રણ કે તેના થી વાર થતા સ્પોન્ટેનીયસ એર્બોશન……છે. ➡️ Recurrent Abortion
Explanation: Recurrent abortion (also called Recurrent Pregnancy Loss) is defined as three or more consecutive pregnancy losses before 20 weeks of gestation.
4.Intermittent painless uterine contraction are …… ઇન્ટરમીટન્ટ પેઇનલેસ યુટેરાઇન કોન્ટ્રાક્શન એટલે …… ઓળખાય છે. ➡️ Braxton Hicks Contractions
Explanation: These are false labor contractions that are irregular, painless, and usually occur after the mid-second trimester.
5.Hydatidy form mole also known as …… Pregnancy. હાઇડટીડી ફોર્મ મોલ …… પ્રેગ્નન્સી તરીકે પણ ઓળખાય છે. ➡️ Molar Pregnancy
Explanation: Molar pregnancy is a gestational trophoblastic disease characterized by abnormal growth of trophoblastic tissue instead of a viable pregnancy.
