ENGLISH-MENTAL HEALTH NURSING (GNM 2ND YEAR) 21/02/2018 PAPER SOLUTION-10 (Done)-UPLOAD
MENTAL HEALTH NURSING -21/02/2018 PAPER SOLUTION NO.10
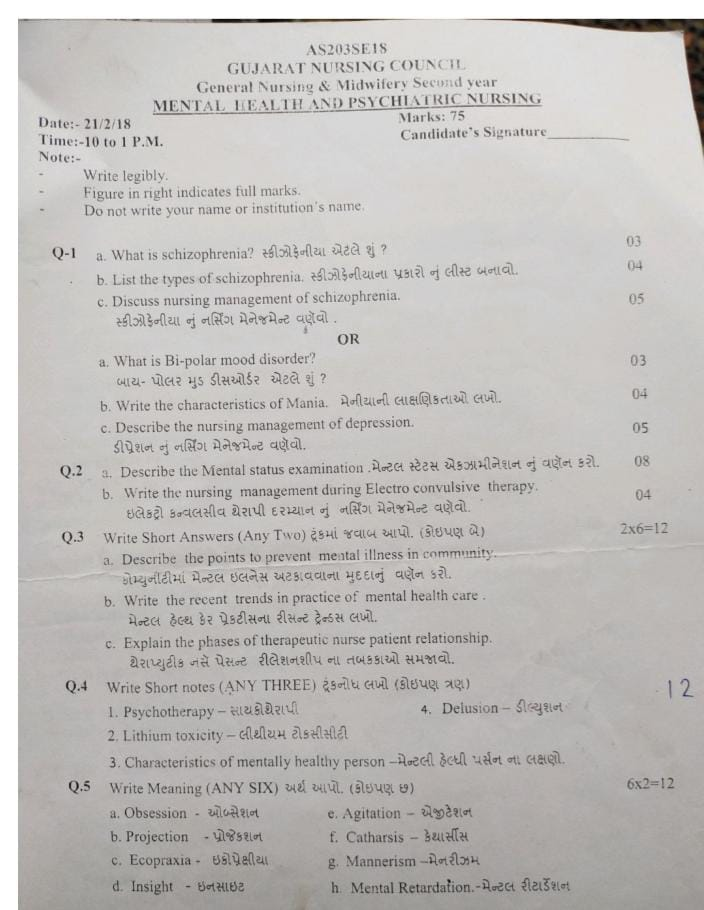
Q: 1 a. What is schizophrenia? What is schizophrenia?03
The term “schizophrenia” was coined by Eugen Bleuler in 1908.
The name derives from the Greek words “schizo-schizo” (split) and “phren-phren” (mind), meaning that this disorder is usually characterized by fragmented thinking.
Schizophrenia is a psychotic condition that affects the normal functioning of the brain. Affects the function, in which disturbances are seen in the thinking, emotion, and behavior function of the person. A person with schizophrenia experiences changes in behavior, perception, and thinking that can remove them from reality. When a person loses touch with reality, they experience psychosis.
Impaired Insight is a common feature of schizophrenia. The person who coined the term Schizophrenia is Eugen Bleuler.
b. List the types of schizophrenia.04
Types of schizophrenia
F 20-0 paranoid schizophrenia
F 20-1 hebephrenic schizophrenia
F 20-2 catatonic schizophrenia
F 20-3 undifferentiated schizophrenia
F 20-4 post – schizophrenic disorder
F 20-5 residual schizophrenia
F 20-6 simple schizophrenia
F 20-8 other schizophrenia
F 20-9 schizophrenia unspecified
Paranoid Schizophrenia
Paranoid Schizophrenia (Paranoid Schizophrenia)
This is the most common type. People of this type have delusions that they are being punished by others. Their thinking, speech and emotions, however, remain completely normal. Their onset is gradual. In some cases, acute is also seen. There is a good prognosis. Persecution and Grandeur Disorders are seen.
•Hebiphrenic Or Disorganized Schizophrenia
People with this type of schizophrenia are often confused and incoherent, and have jumbled speech. They have the worst prognosis. Their outward behavior is emotionless or inappropriate, acting silly or childlike. They cannot perform their daily activities properly. Hallucinations are also seen. The worst prognosis is seen after hebephrenic schizophrenia.
Catatonic Schizophrenia
Onset is acute and sudden. The most striking physical symptoms of this type are physical. People with catatonic schizophrenia are usually immobile and unresponsive to the world around them. They often become very rigid and rigid, they stay in one place and do not move. Their behavior is bizarre. They may repeat words spoken by another person. People with catatonic schizophrenia are at risk of malnutrition, and self-injury. They have the best prognosis. ECT and IV LORAZEPAM are their best treatments.
Undifferentiated Schizophrenia
This subtype is diagnosed when a person’s symptoms do not clearly represent one of the other three subtypes.
Post Schizophrenic Depression
A depressive episode resulting from schizophrenic illness where some low-level Schizophrenic symptoms may also be present.
Residual Schizophrenia
This Type I schizophrenia is chronic. Hallucinations, delusions and other symptoms may also be present but are significantly less common than when schizophrenia is diagnosed. Symptoms include eccentric behaviour, emotional blunting, excessive and illogical thinking.
Simple Schizophrenia
Insidious and progressive prominent negative symptoms are seen.
Pfropf Schizophrenia
There are types associated with mental retardation. They are called grafted schizophrenia.
c. Discuss nursing management of schizophrenia. Describe the nursing management of schizophrenia.05
1.TherapeuticNursing Management
- Giving the medicines prescribed by the psychiatrist
- Always remember the 5 rights before giving the medicine
- After giving the medicine, to observe its side effects or any changes in the patient and record them
- If the patient is to be given ECT, explain it and let him talk about his illness
2. Psychosocial Nursing Management
- Sit close to the patient
- Talk to the patient in a comfortable environment with a reliable communication so that his anxiety is removed
- Encourage the patient to talk about his problem
- Never criticize him while he is talking or being talked to
- Encourage the patient to talk
- Talk to the patient in a simple language that he can understand
- Listen calmly when the patient talks about his delusions and observe how it is reflected in his behavior
- Never validate his delusions but provide him with a safe environment
- Never talk about the patient’s hallucinations, talk about everything else
- Never ignore the patient, sometimes take a little time to talk to him Take a pose and use interview techniques like pinpointing, clarifying, reflecting, summarizing etc. during the conversation.
- Increase self-concept To increase the patient’s self-concept, he should be assigned some tasks like calling everyone for day activities, asking them to check whether everyone has eaten or not, asking them to clean up etc.
- Improve attention and judgment The nurse should play games like carrom, chess, ludo etc. with the patient. Small problems should be asked to solve them. The patient’s attention should be kept on the task.
- Improving family support A relative of the patient should always be with the patient who can help with his problem. The patient’s daily activities such as personal hygiene, diet, etc. can be of help.
3. Physical Needs Nursing Management
a) Provide protection :-
- Do not keep any sharp or injurious objects like knife, blade, rod, glass objects etc. near the patient until they are ready
- If the patient is quarreling with others and hitting each other, then he can be punished like not allowing him to participate in sports etc.
b) Help maintain personal hygiene
- Encourage the patient to brush
- Ensure the patient to empty his/her bowels and bladder completely as the patient can fill them
c) Help with sleeping
- Encourage the patient to go to bed early at night. I should switch off the light. Also, put a floor lamp on the bedside.
- If a patient is disturbing another patient, you should be separated.
- Give the patient a glass of warm milk to drink.
- Make the patient active during the day.
- Forbid the patient from taking naps in the afternoon.
d ) Nutritional Needs
- The next day, a balanced diet should be planned for the patient
- The patient should be served food that he likes and in his own container and he should eat it himself
- If the patient is skeptical about eating, first get his relative to test the food Should
- The patient should get food according to his needs
4. Recreational Needs Nursing Management
- The patient should be asked about his hobbies so that he can be given the recreational he likes
- The patient should be given a game like carrom board or ludo to play
- To use up energy, a game like badminton can also be given to the patient
- Initially, the patient No competitive games should be given or done
- If someone wins a competition, he should be congratulated
5. Spiritual Needs Nursing Management
- The patient should be encouraged to pray every day and separate arrangements should be made for him and all the upcoming festivals should be celebrated in a proper manner but no one can ever be forced to celebrate other religions or festivals
OR
a. What is Bi-polar mood disorder? What is Bi-polar mood disorder?03
Bipolar mood disorder is a chronic and recurring mental health condition characterized by unusual and extreme changes in the patient’s mood, energy levels, and activity patterns. Patients with this disorder switch between manic and depressive states, and the periods in between often seem normal, but they also have clinical value.
In bipolar mood disorder, the patient experiences a state of high mood called mania, in which there is excessive enthusiasm, overconfidence, and overactivity. When people experience negative emotions such as sadness, lethargy, lack of energy, and hopeless thoughts during a state of low mood or depression.
These mood swings are much more intense than the normal ups and downs of a normal person and can seriously affect the patient’s personal life, work, and social relationships.
b. Write the characteristics of Mania. 04
1. Euphoria:
- Symptoms:
- Mild elevation in mood is seen.
- The person feels Emotional and Physical Well-Being.
2. Elation:
- Symptoms:
- Moderate Mood Elevation occurs.
- The person experiences enjoyment and excitement.
3. Exaltation:
- Symptoms:
- Severe Mood Elevation occurs.
- Grandiosity Delusion occurs, in which the person considers himself grandiose and unique.
4. Ecstasy:
- Symptoms:
- Extreme Severe Elevation of Mood.
- The person experiences Extreme Joy, which is usually seen in Delirious Mania.
1. Psychomotor Activity:
- Increased Psychomotor Activity:
- The person becomes more active and hyper-agitated.
2. Speech and Thought Disturbances:
- Flight of Ideas:
- The person jumps from one thing to another, without a logical connection.
- Pressure of Speech:
- The person speaks more loudly and continuously, making it difficult to stop.
- Delusion of Grandiosity:
- The person begins to think of himself as Great or special.
- Delusion of Persecution:
- False belief that others will harm him (Harmful Intentions by Others).
- Distractibility:
- Lack of proper attention, easily distracted by surrounding objects.
- Poverty of Thought:
- Reduced Thought Variety, and thoughts pass through the brain very slowly (Slow Thinking).
Other Features of Mania
Behavioral Features:
- Impulsive Behavior: The person behaves in an unplanned and risky way.
- Action-Oriented Wishes: To do everything immediately Desire to Act Quickly.
- Positive Self-Image: The person sees themselves as Great or Superior.
- Tendency to Blame Others: Blame Others for their mistakes.
Cognitive Features:
- Exhibit Poor Judgment: Inability to Make Rational Decisions.
- Denial of Problems: Refuse to Acknowledge Problems.
- Poor Judgment (Poor Judgment): The habit of making Poor and Risky Decisions.
Physical and Social Features:
- Loudness: The way of speaking becomes more Loud and Intense.
- Hyperactivity: There is Excessive Activity both physically and mentally.
Productivity:
- Greater and more productive behavior (Increased Productivity), although it may not be appropriate.
Infatigability:
Not feeling tired (Inability to Feel Tired).
Biological Features:
- Increased Libido:
- Increased Sexual Desires.
- Insomnia (Insomnia):
- Difficulty Sleeping or not being able to sleep at all.
c. Describe the nursing management of depression. Describe the nursing management of depression.05
1.TherapeuticNeed Nursing Management
Provide a comfortable environment to the patient. And ask the patient’s relative to stay with him/her continuously
The doctor prescribed the medicine. Watch for its side effects and keep a record-report of it. Generally, give anti-depressant drugs
Do MSE of the patient This includes knowing and recording his/her suicidal thoughts and plans as well as how deadly they are.
If the patient is to be given ECT, then help and prepare for it.
2.Physical Needs Nursing Management
a. Safe Environment
- Keeping the patient under continuous observation is a The nurse should be there for his constant care
- Glass articles, ropes, pyjama and petticoat laces, net ties etc. should be removed from the room
Long bed sheets should also not be used as they can be used for hanging
Use paper dishes for food - Electric connections should not be kept open
- Medicine and instruments should be kept locked in the ward
- Care should be taken that the patient does not swallow more than one medicine Should
Give a room near the nursing station - Explain to him the different coping mechanisms of life
3.Personal hygiene:-
Encourage the patient to maintain his personal hygiene. Encourage him to change his clothes, take a bath, comb his hair, etc. Tell him that you look very good today
4. Nutritional lead
Ask to eat little and often
Give a whole grain diet with omelettes, salads, vegetables, etc.
Serve food at the same time as everyone else is eating
Ask the patient for their food preference
Record input and output
4.Psychosocial Need :-
Trusting Relationship
Talk to the patient, listen to him calmly, bring out the positive things in him, let the patient visit his relatives, try to create a positive attitude in him
Reduce suicidal ideation
Encourage the patient to talk about his suicidal ideation and how to commit suicide, etc. Find out what he believes to be used in suicide, how lethal it is, inform the patient of the consequences of his suicide, what will happen to your family members, etc.
Increase self-esteem
Call the patient by his name Praise his positive points and his positive achievements
Improve socialization
The patient should never be left alone Ask him to get out of bed gradually and meet people
Recreational needs
Identify the patient’s favorite hobby or game Give him enough time for outdoor games despite completing his hobby if he wins If you fail to give it credit, accept it without any disturbance. Spiritual Activities Q: 2 a. Describe the Mental Status Examination. 08. MSE is a standard structure or a whole process with the help of which a psychiatric patient A systematic assessment can be done.
In which the patient’s behavior, concentration, thought process, attention, and emotional function are examined, from which the patient’s mentality is concluded, which is called MSE.
DEFINITION :- Mental status examination means the evaluation of a person’s intellectual, cognitive ability, mood, and thought process.
Before MSE, it is necessary to assess vital signs.
(blood pressure, heart rate, respiratory rate, temperature)
• Topics are assessed in MSE :-
- 1) GENERAL APPEARANCE AND BEHAVIOR
- 2) SPEECH/TALKING PATTERN
- 3) MOOD/AFFECT
- 4) THOUGHT
- 5) PERCEPTION
- 6) COGNITIVE FUNCTION
- 7) MEMORY
- 8) INTELLIGENCE
- 9) INSIGHT
- 10) JUDGMENT
- 11) ATTENTION
1) GENERAL APPEARANCE AND BEHAVIOUR :- (General Appearance and Behavior)
Appearance :-Seeing how a person looks…. is old, young,…etc…
Conscious :-Is the person alert, drowsy (half asleep), stupor or comatose (कोमांटोस)….
Hygiene :-
- How does he keep his rice…..
- Does he keep it properly or not…..
Sleep (sleep) :-
- Does he sleep properly or not…
- How much Time sleeps…
Posture :-
- During the examination, to see what the person’s expression is like
- In which, does he talk openly or not….
- Does he answer the question asked or not….
- Does he sit with his head down or does he talk looking straight ahead…
Eye to eye contact :-Eye to eye contact Does he talk incessantly, for how long and when does he look away…
Gait (way of walking):- When the patient comes, how does he walk? Does he come confidently or does he come as if he is scared…
Facial expressions:- What kind of facial expressions do they give…
Eating pattern:- Does he eat properly or not and does he not eat too much…
2) SPEECH/TALKING PATTERN :-(Speech/Talking Pattern)
- Does the person start speaking very quickly or does he speak slowly…
- Does he respond to the question out of fear or not…
- Does he respond by shouting loudly…
- Does he answer the question correctly or incorrectly…
- Repeats one thing after another…..
- Mumbles…..
- Turns things around instead of directly..
- What are the thoughts of a person….
- positive (positive) / negetive (negative)
- Thoughts are fast and change frequently….
- Flights of ideas:-
- Thoughts come continuously but their direction keeps changing…….
- Vague thoughts:
- There is no external object/sound/smell/touch, but it feels like it is there
- Auditory, visual, olfactory, gustatory, tectile
- False perception of stimuli from outside occurs
- Deja vu (de-javu):-Feeling of having seen something in a previous life but never having met it in real life…..
- Jamais Vu (jamais vu):- Forgetting the people in the family with whom one lives…..
4) THOUGHT :- (Thought – Thought)
Neologism:- The use of new words that have no meaning.
5) PERCEPTION :- (Perception) :-
Hallucination :-
Illusion (illusion) :-
6) COGNITIVE FUNCTION :-
(Cognitive function) :-
- To know whether a person is conscious or not….
- Gives us replay slowly (stupor)
- Behaves like being in a coma….
- How does it give information about old things…. Do you know the whole thing or do you remember a little bit? Is….
- Does it have a concept of time, place, person, etc.?
7) MEMORY :-
immediate (immediate ) memory :-
- To ask someone to repeat something….
remote (remote) memory :-
- Do you remember your marriage date, your age, when and where you got your job…
recent (recent) memory :-
- To know whether you remember recent events or not…
- What did you eat in the morning, when did you eat, when did you wake up…
8) INTELLIGENCE :-(Intelligence) :-
- Can you read or write…and how was your school performance…..
9) INSIGHT :-
- Is the person aware of his condition or not….
- What is the internal intelligence like….
- To know this, ask him questions about himself and based on his answers, decide whether insight is present or not….
10) JUDGMENT :-
- The information about this is based on the knowledge, education level of the person…
- Every person’s judgment is different….
11) ATTENTION / CONCENTRATION :- (Attention / Concentration) :-
You can ask about month, week, days…..
Ask a person to subtract 7 from 100, then he/she will ask To stay…(100-7 = 93, 93-7 = 86……..)
Or to do the reverse count……(100,99,98,97…..)
b. Write the nursing management during Electro convulsive therapy. Write the nursing management during Electro convulsive therapy.04
Conduct physical examination and necessary investigations like ECG, Hb, urine albumin/sugar, and X-ray.
Explain the procedure to the patient’s relatives and obtain written consent. Avoid directly informing the patient that they are going to receive ECT (એક્ટિ) until necessary.
Remove metallic articles (મેટાલિક અર્ટિક્લેસ) such as watch (વોચ), bangles (બેંગ્લેસ), rings (રીંગ્સ), and other ornaments (ઓર્નામેંટ્સ).
Keep the patient Nil by Mouth (NBM) (નિલ બાઇ મૌથ) for 6-8 hours before the procedure.
Remove artificial dentures (અર્ટિફિશિયલ ડેન્ચર) to prevent respiratory blockage (રીસપરેરીટીરી બ્લકેજ).
Remove hair oil (હેર ઓઇલ), lipstick (લિપસટીક્ષિ� (makeup), and nail polish (nail polish) to properly assess cyanosis status (cyanosis status).
Instruct the patient to empty bladder (bladder emptying) and bowel (bowel emptying).
Apply allergy/ID bands (allergy/ID bands) and avoid including fatty foods (fatty foods), meat (meat), or fried foods (fried foods) in their diet.
Encourage the patient to maintain personal hygiene (personal hygiene) and assess their anxiety level (anxiety level).
Remove tight clothes (tight clothes) and provide hospital clothes (hospital clothes).
Provide emotional support (emotional support) to reduce the patient’s fear (fear).
Administer muscle relaxants (muscle relaxants) as prescribed to reduce anxiety (anxiety).
Nursing Care During ECT:
Once the patient recovers from anesthesia, transfer them to the recovery room (recovery room).
Assist the patient in moving from the stretcher or wheelchair to the ECT table.
Position the patient in a comfortable dorsal position with a small pillow under the lumbar region.
Administer short-acting anesthetic drugs or muscle relaxants as prescribed.
Provide support for shoulders and arms (support the shoulders and arms) and restrain the thighs (thighs) to prevent fractures.
Monitor vital signs (vital signs) like blood pressure, pulse, and oxygen levels (oxygen levels).
Place a mouth gag (mouth gag) and tongue depressor (tongue depressor) to prevent tongue bite (tongue bite).
Clean the electrode placement area (electrode placement area) with alcohol swab or gel (alcohol swab or gel).
Support the patient’s head and hyperextend the chin (support the head and hyperextend the chin) to prevent jaw fractures.
Assist in placing electrodes (electrodes) and provide support to all major joints (major joints).
Monitor the voltage, frequency, and duration (voltage, frequency, and duration) as per prescription.
Use the cuff method to monitor seizure activity.
During seizure activity, administer 100% oxygen.
Nursing Care After ECT:
Position the patient in a side-lying position to prevent aspiration of secretions.
Monitor vital signs and provide side rails to prevent injury.
Continue oxygenation until spontaneous respiration. resumes.
Assess for confusion and restlessness.
Administer prescribed medications and monitor for side effects.
Document the procedure and any important events.
Q.3 Write Short Answers (Any Two) Write short answers. (Any two).2×6=12
a. Describe the points to prevent mental illness in community. Describe the points to prevent mental illness in community.
Describe the points to prevent mental illness in community:
Mental illness is a major challenge not only for individual but also for collective health. The following key points are necessary to prevent mental illness in the community:
1. Public Awareness and Education:
Creating awareness about mental health among the community, providing appropriate information about causes, symptoms and treatment. This allows individuals to seek timely treatment.
2. Early Detection and Timely Referral:
Identifying early symptoms and referring them to a primary health center or mental health specialist at the right time.
3. School and Workplace Mental Health Programmes:
Initiating activities such as stress management, counselling and relaxation techniques at schools and workplaces.
4. Strengthening Family Support System:
Creating a positive and supportive environment through family therapy, parental training and guidance for the patient’s family.
5. Substance Abuse Prevention:
Implementing comprehensive programs and public policies to avoid the abuse of substances such as alcohol, tobacco, and drugs.
6. Accessible Mental Health Services:
Providing counseling, psychiatric treatment, and rehabilitation services in every area.
7. Stress Management Techniques:
Teaching and promoting yoga, meditation, relaxation therapy and recreational activities.
8. Reduce Social Stigma (Changing society’s mindset about mental illness):
Increase empathy, understanding and acceptance in society for the patient, so that they can openly seek treatment.
b. Write the recent trends in practice of mental health care. Write the recent trends in mental health care practice.
Mental health has become one of the important priorities in the global health sector in the present times. Due to modern scientific developments and changes in the approach of health policies, many new trends are seen in mental health care practice. The following is a complete description of the recent important trends:
1. Community-Based Mental Health Services:
Today, instead of admitting patients to hospitals, the emphasis is on providing mental health services at the family and community level. Home-based care, Day-care centers, and Outreach Programs have now been developed to a greater extent.
2. Integration of Mental Health with Primary Health Care:
As per the guidance of WHO, mental health services are now being made an integral part of the Primary Health Care System. Hence, patients can get mental health care along with general health services.
3. Telepsychiatry and Digital Mental Health:
The use of Telepsychiatry and Mobile Health Applications is rapidly increasing to deliver mental health care to patients in remote areas. Patients can get mental health services through video calls, messaging or applications.
4. Use of Evidence-Based Psychotherapies:
Therapists are now increasingly using proven methods such as Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), and Mindfulness-based Therapy. These therapies are considered scientifically effective.
5. Focus on Preventive Mental Health:
To prevent mental illness before it occurs, emphasis is placed on Stress Management, Early Screening, and Psychoeducation in schools, workplaces, and communities.
6. Patient-Centered and Holistic Care:
Current approaches provide therapy that considers all aspects of the patient – physical, mental, social, and emotional. Emphasis is placed on patient rights, choices, and participation.
7. De-Stigmatization Initiatives:
To remove stigma and societal discrimination against mentally ill patients, large-scale awareness programs are organized by government and private organizations. Such as Mental Health Awareness Weeks, Social Media Campaigns, etc.
8. Rights-Based Approach to Mental Health:
Modern practice emphasizes the human rights, privacy and freedom of the patient. Laws like the Mental Healthcare Act, 2017 protect the rights of the patient.
9. Multidisciplinary Team Approach:
For successful treatment, medical doctors, psychiatrists, clinical psychologists, psychiatric nurses and social workers are now working together.
10. Focus on Vulnerable Groups:
Special therapy and support services are available for girls, the elderly, physically and mentally disabled patients and the LGBTQ+ community, so that their psychological needs can be met.
c. Explain the phases of therapeutic nurse patient relationship. Explain the phases of the therapeutic nurse-patient relationship.
PHASES OF THERAPEUTIC NURSE-PATIENT RELATIONSHIP:
The nurse-patient relationship is the end result of a planned, purposeful conversation between a nurse and a patient, through which behavior, thoughts, and feelings can be shared. Which has 4 Phases.
•1.Pre-Interaction Phase
•2.Orientation Phase
•3.Working Phase
•4.Termination Phase
1.Pre-Interaction Phase (pre-interaction phase)
The pre-interaction phase begins before the nurse first comes into contact with the patient. The nurse’s first task with the patient is investigation. This phase begins when the client is assigned.
Nurses may have misconceptions and prejudice about psychiatric patients. Many nurses express feelings of inadequacy, fear of hurting others, and fear of the patient’s abusive and violent behavior. Nurses should also recognize feelings of insecurity, approval-seeking behavior.
Self-analysis, which characterizes the Pre-interaction Phase, is a necessary task. To make it effective, the nurse needs to have a proper self-concept and self-esteem. They must have constructive relationships with others and face reality to help the patient in the same way.
“NURSES TASK”
~Identify your own feelings, fantasies, and fears.
~Analyze your own professional strengths and limitations.
~Obtain patient data.
First meeting with the client Plan.
“PROBLEMS”
~Difficulty in self-analysis and self-acceptance.
~Anxiety
~Depression
~Anger
~Boredom
“WAYS TO OVERCOME” (Methods of overcoming problems)
~Take help of colleagues and supervisors in self-analysis and face reality.
~Analyze yourself and identify your strengths and limitations.
2.Orientation Phase
The Orientation Phase is also called the Introductory Phase. This phase begins when Occurs when the nurse approaches the patient, introduces herself and receives an introduction about him. The nurse and patient, who are strangers, meet for the first time and become acquainted. The orientation phase ends when the nurse and patient begin to accept each other as unique human beings.
In this phase, the client and nurse come face to face for interaction. It is during this phase that the Termination Phase of the therapeutic relationship begins. During this phase, the goals of the therapeutic relationship are also discussed.
During this phase, the nurse and patient meet for the first time. One of the nurse’s primary concerns is to find out why the patient sought help.
It helps the nurse focus on the patient’s problems and determine the patient’s level of motivation.
“NURSES TASK”
~Build trust and rapport.
~Facilitate verbal expression of thoughts and feelings.
~Facilitate verbal expression of thoughts and feelings.
~Creating a therapeutic environment.
~Collect data including the patient’s feelings, strengths, and weaknesses.
~Establishing acceptable communication methods for both patient and nurse.
~Set priorities for nursing interventions.
~Initiating a therapeutic contract by determining the time, place, and duration of each meeting, as well as how long the relationship will last.
•Identifying the patient’s problems.
•Set specific goals.
“PROBLEMS”
~Not perceiving each other as unique individuals.
~Problems related to establishing an agreement between nurse and patient.
~Social class
~Anxiety
“WAYS TO OUTCOME”
The nurse shares the data collected from the patient with the supervisor. The supervisor should provide an environment in which the nurse feels free to express herself without any fear of criticism.
3.Working Phase
This phase begins when the nurse and patient are able to overcome the barriers of the orientation phase. During this phase, the nurse and patient actively work to achieve the goals that they set during the orientation phase. The characteristic of this phase is that the nurse is able to overcome anxiety and the patient’s fear of the unknown is also reduced. Reactions such as transference and countertransference also decrease.
Therapeutic work is done in this working phase. The goals set in the orientation phase are accomplished in this phase. Actual behavior change is the focus of this phase.
By connecting perceptions, thoughts, feelings, and actions, the nurse helps the patient reduce anxiety, increase independence, and develop coping mechanisms.
The patient usually shows resistance during this phase. The patient relaxes, trusts the nurse, and discusses mutually agreed-upon goals with the nurse as the assessment process continues and a care plan is developed.
~”NURSES TASK”
~Collect patient data and identify needs.
~Help identify patient problems.
~Use coping mechanisms To do.
~Promote positive self-concept.
~Facilitate behavior change.
~Give them opportunities to act in their own way.
~Develop a realistic plan of action.
~Implement the action plan.
~Evaluate the results of the action plan. To do.
~Nurses should provide information about the patient’s role in the treatment.
“PROBLEMS”
~The nurse is tested by the patient.
~Patient with mental illness may not progress quickly.
~There is difficulty in collecting data.
~Fear Of Closeness (Nurses work closely with patients so they have fear.
~Nurses Life Stress
~Resistance Behaviour
“WAYS TO OUTCOME” (ways to overcome problems)
~The supervisor should communicate with experts and the help of other group members will be useful, and will help in interpreting the collected data.
4.Termination Phase.
The termination phase is called the resolution phase or the end phase. The termination phase begins with the orientation phase.
is the most important and most difficult phase of the therapeutic relationship. In this phase, the termination of the therapeutic relationship takes place.
The main goal of this phase is The relationship is to be brought to a therapeutic end.
This is a time to exchange feelings and memories and to evaluate the patient’s progress and whether the goal has been achieved.
“CRITERIA FOR TERMINATION”
~The patient’s present problems are relieved.
~The patient’s social function improves.
~The patient’s “ego” function is strengthened.
~The patient achieves the planned treatment goal.
“CAUSES OF TERMINATION”
~The patient leaves the ward on his own.
~The nurse terminates the relationship due to some reason Does.
~When the patient goes on “parole” and returns to the hospital.
~The therapeutic relationship is terminated when the patient is discharged.
~When the nurses’ duties change.
“PREPERATION OF PATIENT”
~Explain whether the goals of the Nurse Patient Relationship have been met.
~Explain whether the goals of the Nurse Patient Relationship have been met.
~Decision on termination.
~Inform the patient.
~The nurse should encourage the patient to talk about anxiety and fear.
~The patient should be sent on “parole” before discharge.
“NURSES TASK”
~End the relationship therapeutically.
~Establish the reality of separation.
~Review feelings about the relationship.
~Review progress of therapy and achievement of goals.
~Explore feelings of rejection, loss, sadness, and anger-related behaviors.
“PROBLEMS”
~Patient’s Angry Behaviour.
~Tries to Punish Nurse.
~Ignores Termination.
~Tries to Eliminate Nurses’ Faults.
“WAYS TO OUTCOME”
~The nurse should be aware of the patient’s feelings and deal with them appropriately.
~The nurse should give the patient a lot of weight to express their feelings about the termination.
~Discuss with the supervisor so that they can help.
Q.4 Write Short notes (ANY THREE) Write short notes (any three).12
1.Psychotherapy
Psychotherapy is a treatment method for emotional and personality problems.
Basic principles:
This therapy is based on the Therapist-patient relationship.
The therapist respects the patient and considers them as a human being.
Purpose of Psychotherapy:
To help the patient develop a sense of self-identity.
To develop interpersonal and intrapersonal skills using a combination of individual psychotherapy and group therapies. (Intrapersonal skills) to provide.
To help patients in cases like Mental illness, drug addiction.
Key Characteristics of Psychotherapy:
- A treatment method for emotional problems in which trained individuals modify and remove the patient’s symptoms.
- Designed to increase understanding of thoughts, feelings, social experiences and relationships.
- Helps gain insights by observing individual and family patterns.
Benefits of Psychotherapy:
- Helps improve self-awareness and emotional regulation.
- Develops social and interpersonal skills.
- Useful for long-term management of mental health issues is.
INDIVIDUAL PSYCHOTHERAPY
- This psychotherapy is conducted on a one-to-one basis.
- A therapist works with one client at a time. treat.
Definition:
Individual psychotherapy is a method in which a person’s feelings, attitudes, thinking, and behavior are explored and changed (Change) is attempted.
Purpose of Individual Psychotherapy:
- Emotional regulation.
- Self-awareness.
- Increase the individual’s To bring thoughts and behaviors in a positive direction.
Advantages:
- Personalized attention.
- Clients are given their Provides a safe environment to openly discuss issues.
- Therapist-client relationship is strengthened, which is helpful for healing.
Indication:
- Stress-related disorders
- Alcoholism
- Sexual disorders
Aims of Individual Psychotherapy (Goals of Individual Psychotherapy):
- Therapist understands client’s feelings.
- Modify
- Improve interpersonal relationships (IPR) and establish therapeutic relationship.
- Bring personal changes and provide consistent emotional support.
- Help client gain a greater understanding of their problems.
Nurse’s Role:
- Coordinate with other members of the team.
- Allow patients to make their own decisions.
- Explain treatment.
- Develop a trusting relationship.
- Nurses should encourage clients to involve in therapy.
2.Lithium toxicity
Introduction:
Lithium toxicity is a condition when Lithium levels in the patient’s blood increase and cause severe effects on the neurological, cardiac, and gastrointestinal systems. Lithium is a mood stabilizer, especially used for bipolar disorder, but its therapeutic index is very small, so even a small increase in dosage can lead to toxic effects.
Normal level of lithium:
Therapeutic level: 0.6 – 1.2 mmol/L
Toxic level: >1.5 mmol/L
Severe toxicity: >2.0 mmol/L
Types of lithium toxicity:
1.Acute Lithium Toxicity:
Occurs when a new patient takes a large amount of the drug. Symptoms are mainly gastrointestinal such as vomiting, nausea, diarrhea, etc.
2.Chronic Lithium Toxicity:
Occurs when the patient has been taking lithium for a long time and the lithium level gradually increases. Neurological symptoms are evident.
3.Acute-on-Chronic Lithium Toxicity:
It occurs when a patient has been taking lithium for a long time and suddenly takes a high dose for some reason. It has both gastrointestinal and neurological symptoms.
Symptoms:
- Gastrointestinal:
- Vomiting
- Loss of appetite
- Stomach pain
- Diarrhea
- Neurological:
- Confusion
- Ataxia – Unsteadiness in walking
- Tremor
- Seizure
- Coma
- Cardiac:
- Bradycardia
- Effect on the urinary system:
- Polyuria
- Dehydration
- Acute kidney injury (Acute Kidney Injury)
Causes:
- If you take too much lithium
- Kidney function deteriorates
- Dehydration
- Thiazide Diuretics, Enacides Taking with drugs like (NSAIDs), ACE Inhibitors
- Overdose
Diagnosis:
Measuring blood lithium level
Checking electrolytes, creatinine
Knowing the condition of the heart through ECG
Neurological assessment
Treatment:
1. For mild toxicity:
Discontinue lithium
Improve hydration (by oral or IV fluids)
Close monitoring of blood levels
2. For moderate to severe toxicity:
Stop lithium
Give IV normal saline
Hemodialysis – especially when lithium levels are >2.5 mmol/L, or neurological symptoms are serious
Prevention:
Lithium dose Check regularly
Instruct the patient to stay hydrated
Monitor kidney function
Avoid interacting medications
Monitor lithium levels regularly
Lithium toxicity is a serious condition that can be avoided if recognized promptly and treated appropriately. Regular follow-up of the patient, blood monitoring and proper medical supervision are very essential.
3.Delusion- Delusion
Introduction:
Delusions are psychological symptoms in which the patient has unrealistic beliefs that are clearly false but are persistently believed to be true by the patient, and these beliefs cannot be changed by any logical explanation or evidence. Delusions are typically seen in mental illnesses such as Paranoid Disorder, Schizophrenia, Schizoaffective Disorder, Major Depressive Disorder, and Bipolar Disorder.
Definition of Delusion:
A delusion is a fixed, false belief that is contrary to the patient’s cultural or religious background and that has no realistic basis but which the patient believes to be absolutely true and which the patient maintains despite being confronted with evidence to the contrary. is.
Types of Delusion:
1. Paranoid Delusion:
The patient believes that someone wants to harm him, is plotting, or is being tracked.
2. Grandiose Delusion:
The patient believes that he is a very special person, like God. Avatar, famous scientist or person with great power.
3. Erotomanic Delusion:
The patient believes that a famous person or someone else loves him.
4. Nihilistic Delusion:
The patient believes that the world has now ended or that his body or internal organs no longer exist.
5. Somatic Delusion:
The patient believes that there is a serious illness in his body, which in fact is not the case.
6. Delusion of Reference:
The patient believes that news, TV, journalism, etc. are directly related to him.
Pathophysiology:
The causes behind the delusion The mechanism involves dopamine, specifically excessive dopamine activity in the mesolimbic pathway. Sometimes, the dysfunction of the cervical temporal lobe and prefrontal cortex is also responsible for delusions.
Diagnosis:
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), there are specific criteria for delusional disorder.
Clinical Interview
Mini Mental State Exam (MMSE)
Ruling out organic causes (such as brain tumor, neurological disorders, etc.)
Neuro imaging (CT/MRI) when necessary
Treatment:
1.Pharmacotherapy:
Antipsychotic drugs such as Risperidone, Olanzapine, Aripiprazole (Aripiprazole)
Mood Stabilizers if bipolar disorder
Antidepressants if depression
2.Psychotherapy:
Cognitive Behavioral Therapy
Reality Orientation
Family Therapy
3.Hospitalization:
Necessary if the patient is aggressive, suicidal or high risk
Delusion is a serious psychological condition that affects the patient’s daily life, relationships and functioning. With timely diagnosis and appropriate treatment, significant improvement in the patient’s symptoms is possible. A multidisciplinary team approach to mental health is necessary so that the patient can return to a normal life.
4..Characteristics of a mentally healthy person.
The characteristics of a mentally healthy person are as follows.
1. He has his own philosophy of life:
A mentally healthy person formulates his own values keeping in mind the demands of society. This philosophy guides him in his various activities of life.
2. A proper sense of self-evaluation:
A well-adjusted person knows about his abilities, motives, strong points and limitations. He carefully evaluates his behavior and admits his mistakes.
3. Emotionally mature:-
He is emotionally mature and stable and expresses his feelings well and uses them with proper control.
4.A balanced self-regarding sentiment. (Balanced self-regarding sentiment):-
He has a proper sense of personal respect. He thinks that he is an important member of the social group and can contribute something to its progress and welfare.
5. . Socially adjustable (. Socially adjustable):-
We are all social beings. This social life refers to the reality of Give & Take. A mentally healthy person knows the art of living a social life and does social give and take
6. A realistic approach:-
: His approach to various problems in life is realistic. He is not afraid of imaginary dangers or difficulties that may arise.
8. Intellectually sound:He has sufficiently developed intellectual powers. This enables him to think independently and take the right decision at the right time.
9. Emotional maturity. (Emotion Maturity):
Emotions like fear, anger, love, etc. are commonly seen in our social life. Such a person has mature emotion behavior. He has control over them and expresses them according to accepted social norms.
10. Bravery facing failures (Courage to face failures):
Life is a see-saw game. If we aim for success, we sometimes face failures. A person with complete mental balance has enough courage and endurance to face the failures in his life.
11. Punctuality:
A person with mental health has desirable social and healthy habits. He does not forget his commitments and is regular and punctual in fulfilling his duties.
12. Self-judgment:
Self-determination is one of the important characteristics of such a person. He uses it to solve his problems. He does not rely on the judgment of others.
Common Characteristics of a Mentally Healthy Person:-
They feel good about themselves.
They are not overwhelmed by emotions like fear, anger, love, jealousy, guilt, or anxiety.
They have stable and satisfying personal relationships.
They feel comfortable with other people.
They can laugh at themselves and with others.
They have respect for themselves and others even if there are differences.
They are able to accept life’s disappointments.
They can meet the demands of life and manage their problems when they arise.
They make their own decisions.
They shape their environment whenever possible and Adjusts it when necessary.
Q.5 Write Meaning (ANY SIX) Give the meaning. (Any six).6×2=12
a. Obsession
A recurring and persistent thought, impulse, or image that is caused by distressing emotions such as anxiety, fear, or disgust is called an obsession.
b. Agnosia -Agnosia
Agnosia is the inability to recognize the sensations and stimuli of an object, person, or sound.
b. Projection
This is a frequently used defense mechanism. In this, rejected thoughts, impulses, desires, etc. are transferred to others. In this, the person blames his own mistakes and others. When projection is used, problems arise in our relationships.
If an ex-student fails an exam, he blames the examiner for not being able to check the paper properly.
C. Ecopraxia
Ecopraxia is a neurological symptom in which a person consciously imitates the movements of others. These types of actions are usually involuntary and may be associated with conditions such as Autism Spectrum Disorders, Schizophrenia, or Tourette Syndrome.
d. Insight
Insight is the awareness and understanding of a person’s own mental state, illness, or problem. When a person has an understanding of and accepts their abnormal behavior and symptoms, that person is said to have good insight.
e. Agitation – Agitation
Agitation is a mental and physical state of restlessness in which a person is very anxious, restless, and restless. This symptom is seen in various mental illnesses such as Mania, Dementia, or Delirium.
f. Catharsis – Catharsis
Catharsis is a mental process in which suppressed emotions are released through words, tears, or other expressions to relieve stress. This method is applied in therapy where a person freely expresses their inner pain and emotions.
g. Mannerism
Mannerism is a pathological behavioral pattern in which a person displays involuntary repetitive, inappropriate, and unusual gestures, facial expressions, or body movements that have no apparent functional purpose. Mannerism is commonly seen in schizophrenia, autism spectrum disorder, and other neuropsychotic conditions.
h Mental Retardation.- Mental Retardation
Mental Retardation is a neurodevelopmental disorder in which there are significant limitations in a person’s intellectual functioning (i.e. intellectual ability) and adaptive behavior (i.e. social and practical skills of daily life). Mental retardation usually develops before the age of 18 and is assessed by an Intelligence Quotient, or IQ, with a score of approximately 70 or less. It adversely affects a person’s abilities such as problem-solving, reasoning, planning, judgment, academic learning, and practical understanding. According to international medical standards, this condition is now known as Intellectual Disability instead of Mental Retardation, which is a more humane and modern definition.
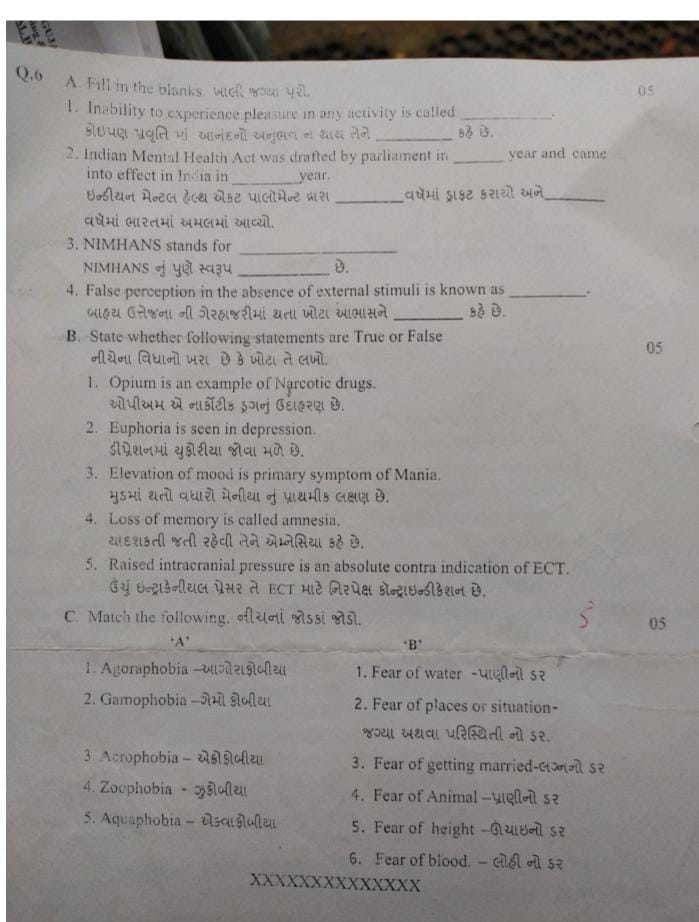
Q.6 A. Fill in the blanks, fill in the blanks.05
1.Inability to experience pleasure in any activity is called…..Anhedonia
2.Indian Mental Health Act was drafted by parliament in……year and came into effect in India in…..year. The Indian Mental Health Act was drafted by the Parliament in the year …… and came into force in India in the year …….1987,1993
The Indian Mental Health Act was drafted by the Parliament in the year _1987_ and _1993_ and _1993_ .
3.NIMHANS stands for…… Pune version of NIMHANS…… National Institute of Mental Health and Neuro Sciences_
4.False perception in the absence of external stimuli is known as…… State whether the following statements are True or False.05
1.Opium is an example of Narcotic drugs. OPM is an example of a Narcotic drug:✅ True
2.Euphoria is seen in depression. Euphoria is seen in depression:❌ False
Euphoria is usually seen in mania, while depression is characterized by apathy and negative emotions.
3.Elevation of mood is primary symptom of Mania. Elevation of mood is the primary symptom of Mania:✅ True
4.Loss of memory is called amnesia. Loss of memory is called amnesia:✅ True
5.Raised intracranial pressure is an absolute contra indication of ECT. Raised intracranial pressure is an absolute contra indication of ECT:✅ True
C. Match the following. Connect the following pairs 05
A B
1.Agoraphobia 1.Fear of water
2.Gamophobia 2.Fear of places or situation Fear of
3.Acrophobia 3.Fear of getting married
4.Zoophobia – Zoophobia 4.Fear of Animal
5.Aquaphobia – Aquaphobia 5.Fear of height
6.Fear of blood
✅(Answer):
1 → 2
2 → 3
3 → 5
4 → 4
5 → 1