ENGLISH-MEDICAL SURGICAL NURSING-2(Paper Solution):10/12/2024 (Done-upload NO.09
MEDICAL SURGICAL NURSING-2–(Paper Solution No.9):10/12/2024
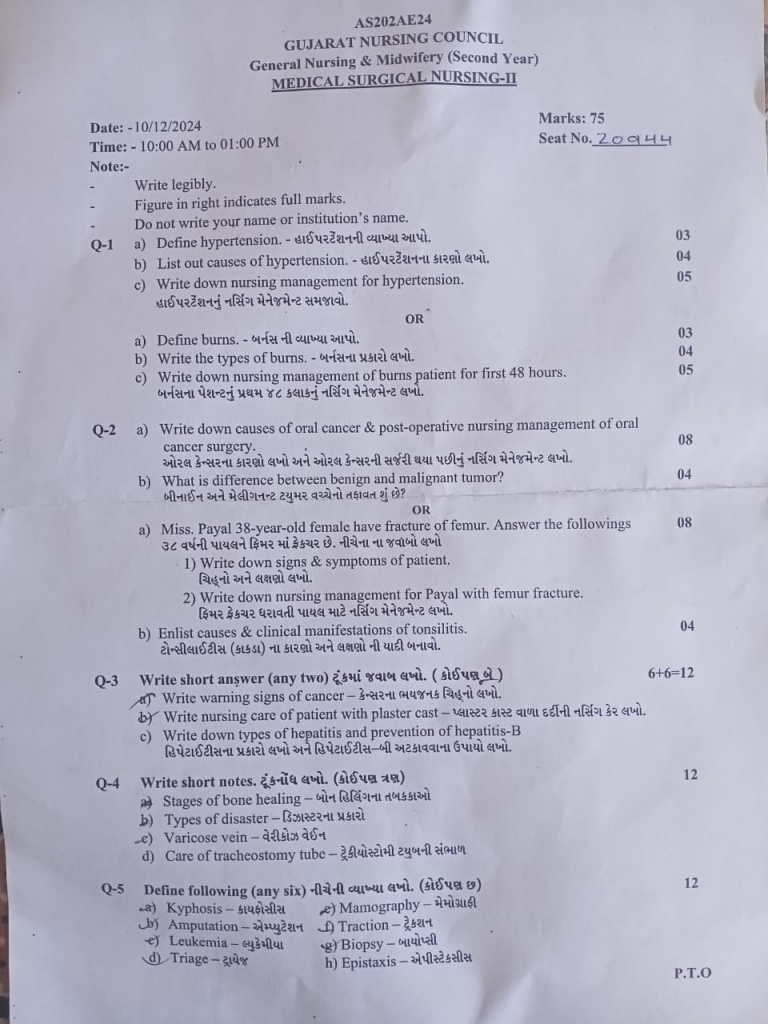
Q-1 a) Define hypertension. .03
Hypertension means high blood pressure. Hypertension is a common condition in which the pressure of blood against the artery walls is consistently high. When the systolic blood pressure is more than 140 mmHg and the diastolic blood pressure is more than 90 mmHg, it is known as hypertension. In short, hypertension means blood pressure is more than 140/90 mmHg.
Types of hypertension:
Hypertension is mainly divided into two types:
- 1) Primary hypertension
- 2) Secondary hypertension
1) Primary hypertension: Primary hypertension is also known as ‘essential hypertension’. This is the most common type of hypertension that can develop at any time. The exact cause of primary hypertension is unknown but hypertension is seen due to some factors. Such as age, unhealthy diet, lack of physical activity, overweight, obesity, smoking, alcohol consumption, stress, family history, diabetes, metabolic disorders
2) Secondary hypertension: Secondary hypertension is seen suddenly and due to some underlying condition. Such as kidney disease, adrenal gland tumor, thyroid problem (Cushing’s syndrome), pregnancy, use of oral contraceptive pill.
b) List out causes of hypertension. 04
Causes of Hypertension (High Blood Pressure)
Causes of Hypertension:
- Essential/Primary Causes of Hypertension:
(There is no specific cause in this type but the following factors are responsible)
- Increasing Age
- Hereditary (Heredity/Genetics)
- Obesity
- High salt intake
- Mental stress and anxiety
- Lack of physical activity
- Smoking and alcohol intake
- Adulteration and fast food
- Lack of sleep (Sleep apnea or inadequate sleep)
- Unhealthy lifestyle
- Secondary causes of hypertension:
(When there is an underlying medical cause for hypertension)
- Kidney diseases (e.g., renal artery stenosis)
- Adrenal disorders (e.g., pheochromocytoma)
- Thyroid dysfunction – Hypo/Hyperthyroidism
- Pregnancy (Pregnancy-induced hypertension)
- Certain medications (Steroids, NSAIDs, oral contraceptives)
- Congenital heart disease (Coarctation of aorta)
- Autoimmune diseases like lupus, scleroderma.
c) Write down nursing management for hypertension. 05
Nickel Assessment:
First, the patient’s physical, mental, and behavioral condition should be completely evaluated.
The patient’s Blood Pressure (BP) should be measured regularly in both arms.
Pulse, Respiratory Rate, and Body Mass Index (BMI) should be observed.
Check whether the patient has symptoms like Headache, Blurred Vision, Dizziness, or Epistaxis.
Collect information about the patient’s Dietary Habits, Exercise Pattern, and Stress Level.
- Monitoring and Observation:
Monitor BP in every shift.
Observe for complications like Urine Output, Edema, Chest Pain, or Shortness of Breath.
Follow up the patient’s laboratory reports like Serum Creatinine, Electrolytes, and ECG.
Maintain a Daily Fluid Intake and Output Chart for the patient.
- Lifestyle Modification Counseling:
Advise the patient to follow a low salt diet (less than 5 grams daily).
Encourage the patient to engage in regular physical activity (walking for 30 minutes daily, doing yoga).
Explain smoking cessation and alcohol avoidance.
Provide education on weight reduction, stress management, and healthy sleep patterns.
Provide information about the DASH Diet (Dietary Approaches to Stop Hypertension) to the patient.
- Medication Adherence:
Encourage the patient to take their antihypertensive medication regularly and at the right time.
Explain the side effects of medication such as postural hypotension, fatigue, or dizziness.
Create a Medication Reminder Chart to ensure that the medication is taken on time.
To make the patient understand that the medication should not be stopped prematurely.
5.Health Education:
Explain to the patient that Hypertension is a “Silent Killer”.
Inform about its complications such as Myocardial Infarction, Cerebrovascular Accident (CVA), and Renal Failure.
Teach the patient how to do Home BP Monitoring.
Involve the patient’s family members in Hypertension Management.
6.Observation and Prevention of Complications:
If Chest Pain, Sudden Weakness, Difficulty in Speech, Facial Droop etc. are observed, inform the doctor immediately.
Observe the patient for Fluid Retention, Oliguria, or Palpitations.
Keep Emergency Kit, Oxygen Supply, and Crash Cart available.
- Psychological Support:
After getting a diagnosis of hypertension, many patients may experience anxiety or depression.
Communicate with the patient empathetically.
Motivate them that their disease can be controlled.
Teach relaxation techniques such as breathing exercises.
- Follow-up and Home Care:
Ask the patient to go to OPD or PHC for regular follow-up.
Teach the patient home-based care such as rest, regular medication, and healthy diet.
Teach the patient’s family members BP Checking Techniques.
Hypertension is a lifelong condition, but it can be controlled. As a nurse, it is necessary to play a responsible role in all areas such as Assessment, Education, Monitoring, Emotional Support, and Lifestyle Modification for the patient.
Accurate Nursing Management
OR
a) Define burns.
Burn injuries occur due to direct contact with thermal, chemical, electrical and radiation. Injuries to the skin and tissues caused by contact with hot liquids, hot objects, streams, fire, sun, electricity and chemicals are known as ‘burn injuries’. Burn injuries occur due to the transfer of heat energy to the body as a heat resource. This heat is transferred through conduction and radiation. Human skin can tolerate temperatures up to 42-44 c. But when exposed to temperatures higher than this temperature, tissue destruction occurs. Burn injuries are a major global public health problem and have a physical, psychological, and financial impact on people. Most burns occur accidentally. Burn injuries occur in people of all ages and all socioeconomic groups.
OR
Burns are injuries to the skin and/or internal parts of the body caused by contact with hot objects or chemicals.
b) Write the types of burns. 04
Types & classification of burns
According to burn depth & severity of penetrate the skin surface
Burns are classified into first degree burns, second degree burns, third degree burns and fourth degree burns based on their depth.
The depth of the burn depends on the temperature of the burning object and the duration of exposure to it.
First degree burns / superficial partial thickness:
In first degree burns, the superficial layer of the skin, the epidermis, is affected and there is minimal tissue injury.
The burned area is pink to reddish in color and there is erythema, dryness, and pain. The area is hypersensitive (hyperesthesia).
Blister formation is not seen.
First degree burns heal within a week and scar formation is not seen.
First degree burns can also be treated at home.
Sunburn is an example of first degree burns.
Second degree burns / deep partial thickness:
Second degree burns are also known as ‘dermal burns’.
In second degree burns, the epidermis and dermis layers are affected and the epidermis layer is destroyed.
In addition, the hair follicles and sweat glands are also affected.
In this, redness, pain, swelling and blister formation are seen in the burned area.
Second degree burns heal within 2-3 weeks and scar formation is seen in it.
Third degree burns / full thickness:
In third degree burns, the epidermis, dermis and subcutaneous layer are affected. The epidermis and dermis layers are destroyed. In addition, bones, muscles, tendons and organs are often affected.
The burned area looks waxy white and charred, meaning that the area appears blackened by burning. The area appears firm and dry.
Pain and sensation are not seen due to destruction and damage to nerve endings. In addition, conditions like hematuria and shock are seen.
Deep scars are seen due to third degree burns, hence cosmetic or reconstructive surgery and skin grafts are used.
Third degree burns heal slowly.
Fourth degree burns:
Fourth degree burns extend to the fascia. Bones, muscles, tendons and organs are also damaged.
The affected area looks like dry char and the area is painless and eschar is also seen. (Dead tissue is seen on the skin due to burns. And it is seen to be shed off)
This type of burns is seen due to deep flame and electrical burns.
If the extremities are affected in the fourth degree, then amputation is required.
According to burn severity:
Burns are classified into minor burns, moderate burns and severe burns based on the severity of the burn and the amount of body surface area affected.
Minor burns:
In children, less than 10% of the total body surface area is affected and in adults, less than 15% of the total body surface area is affected.
Patients with minor burns can be treated on an outpatient basis.
All first-degree and second-degree burns are included in minor burns.
Moderate burns:
In moderate burns, 20 to 25% of the total body surface area is affected. In adults, 15 to 25% of the total body surface area is affected, while in children, 10 to 20% of the total body surface area is affected.
Severe burns:
Severe burns involve more than 20 to 25% of the total body surface area. In adults, more than 25% of the total body surface area is affected, while in children, more than 20% of the area is affected.
Inhalation and electrical burns are included in severe burns.
Third-degree burns and fourth-degree burns are included in severe burns.
c) Write down nursing management of burns patient for first 48 hours. 05
- Primary Assessment of the Patient:
The first 48 hours of the burn patient are the critical stages of the resuscitation phase.
The patient should be assessed immediately for three basic issues as per the ABC Protocol:
A – Airway: If the patient’s mouth, nose or throat is burned, then there is a high chance of airway obstruction. If necessary, the patient should be given Endotracheal Intubation.
B – Breathing: Observe the patient’s Respiratory Rate, Chest Movement, and SpO₂ (oxygen saturation).
C – Circulation: Check Pulse Rate, Blood Pressure, Capillary Refill Time and be alert for Hypovolemic Shock.
- Fluid Resuscitation:
The biggest risks in a burn patient are – Hypovolemia and Burn Shock.
Start Intravenous Fluid Therapy for the patient immediately – Ringer’s Lactate is usually used.
Determine the fluid rate according to the Parkland Formula:
👉🏻 4 mL × Body Weight (kg) × % TBSA (Total Body Surface Area)
👉🏻 50% of which should be given in the first 8 hours and the remaining 50% in the next 16 hours.
Monitor the patient’s urine output hourly to ensure that it is at least 0.5 mL/kg/hour.
3.Pain Management:
Burns patients have severe pain.
Give the patient intravenous opioids such as Morphine, Fentanyl.
Assess the patient’s pain every 2–4 hours and provide relief with medication according to the patient’s pain score.
Also provide emotional reassurance to the patient.
- Infection Control:
Since the patient’s skin remains open after burns, there is the greatest risk of sepsis.
Apply aseptic dressing of the wound area.
Apply topical antibiotic ointment such as Silver Sulfadiazine.
Maintain strict hand hygiene, barrier nursing technique and sterile environment for the patient.
If fever, pulse increases or pus is seen, take blood culture and start systemic antibiotics immediately.
- Wound Assessment and Documentation:
Regularly record the depth, color, exudate, odor of the wound in a daily note.
If photographic documentation of the wound is also done, wound healing can be tracked.
Use the Rule of Nine or Lund-Browder Chart for Burn Area Calculation.
6.Nutritional Support:
During the first 48 hours, the patient develops a hypermetabolic state.
If the patient is unable to eat, start Nasogastric Tube Feeding.
Give High Protein, High Calorie, Vitamin C, Zinc Supplements for wound healing.
Monitor the patient’s Electrolyte Levels, Serum Albumin, Blood Glucose.
7.Psychological Support:
Anxiety, Fear, Depression are common in burns patients.
Talk to the patient empathetically, explain the report, and be patient.
Counseling or Psychiatric Referral may also be done if necessary.
8.Preventing Complications:
Continuously monitor the patient for Hypovolemic Shock, Renal Failure, ARDS (Acute Respiratory Distress Syndrome).
Input-Output Charting, Vital Signs Monitoring, hourly monitoring for wound worsening or septic signs.
The first 48 hours of nursing management of a burns patient are the most critical stages in saving their life.
Airway, Breathing, Circulation, as well as Fluid Balance, Infection Control, Pain Relief, Nutrition, and Emotional Care – the role of a professional nurse in all these areas is essential for both the patient’s survival and wound healing.
Q-2 a) Write down causes of oral cancer & post-operative nursing management of oral cancer surgery. 08
Causes of Oral Cancer:
Oral cancer is a malignant tumor that occurs in places like mouth, tongue, lips, cheeks, inner layer of mouth (oral mucosa) and palate. Its main causes are given below:
- Smoking:
Regular consumption of cigarettes, bidis, cigars etc. causes carcinogenic substances to enter the cells of the mouth.
- Chewing Tobacco:
Continuous use of substances like tobacco, gutkha destroys the oral mucosa and cancer develops.
- Alcohol intake:
Drinking excessive amounts of alcohol reduces the protective function of mouth cells and increases the risk of cancer.
- Human papillomavirus (HPV) transmission:
Infection with HPV-16 in particular can cause cancer in the back of the mouth.
- Nutritional deficiency in food:
Deficiency of vitamins A, C and E in particular reduces the repair ability of cells, which increases the risk of cancer.
- Excessive sun exposure:
Ultraviolet (UV) rays from the sun are responsible for cancer, especially of the lips.
7.Poor Oral Hygiene:
Prolonged lack of proper dental cleaning or constant abrasion of the mucosa from broken teeth can be responsible for the development of cancer cells.
8.Genetic and Familial History:
Those whose family members have had oral cancer before are at higher risk.
Post-operative Nursing Management of Oral Cancer Surgery:
Nursing management is very important for the care of the patient after oral cancer surgery. Below is a detailed description of it:
1.Airway Management:
The patient may have undergone a tracheostomy after surgery.
Keeping the airway open, giving suction therapy.
Giving oxygen therapy if necessary.
- Pain Management:
The patient is in a lot of pain after surgery.
Give pain control medications (Analgesics) prescribed by the doctor on time.
Regular assessment of the patient’s pain level.
- Nutritional Management:
When the patient cannot eat by mouth, give a liquid diet through a nasogastric tube.
Give a high protein and calorie diet.
Make arrangements so that the patient can eat little by little.
- Infection Control:
Keep the surgical site clean.
Give antibiotic therapy as per the doctor’s instructions.
Do wound dressing regularly.
- Communication Support:
If the patient is unable to speak after surgery, provide non-verbal communication tools such as a board, pen, etc.
Help teach the patient and family communication skills.
- Psychological Support:
The patient may experience depression or anxiety after surgery.
Talk to the patient lovingly and respect their feelings.
Assist in providing psychosocial counseling if needed.
- Oral Care:
Keep the patient’s mouth clean with a soft brush or medicated mouthwash.
Keep the mouth hydrated to prevent drying of the mucosa.
- Rehabilitation and Follow-up:
Refer the patient for Speech Therapy and Swallow Therapy.
Maintain regular follow-up for post-surgery check-ups.
Monitor for recurrence and metastasis.
Identify the causes of oral cancer in time.
b) What is difference between benign and malignant tumor? 04
Difference between Malignant Tumor and Benign Tumor
Benign Tumor:
Growth Rate:
- Grows slowly.
- Usually does not spread to surrounding tissues.
Shape:
- Has a well-organized, well-defined surface.
Cell Characteristics:
- Benign cells appear normal and do not have mutations.
Capability to Spread:
- Does not metastasize (spread to other parts of the body).
Impact on Health:
- Usually not fatal, but may cause pressure, pain, and other symptoms if they are near vital organs.
Treatment:
- Can be easily removed by surgery and has a low chance of recurrence.
Malignant Tumor:
Growth Rate:
- Grows rapidly.
- Can invade surrounding tissues and organs.
Shape:
- Has a disorganized and irregular surface.
- Cell Characteristics:
- Malignant cells are new and have mutations that cause them to grow uncontrollably.
Capability to Spread:
- Can metastasize to other parts of the body through lymph nodes and hemoglobin.
Impact on Health:
- Life-threatening and can cause significant health problems.
Treatment:
- Requires more extensive and aggressive treatment such as surgery, chemotherapy, radiation therapy, and targeted therapy.
- High chance of recurrence and spread.
OR
a) Miss. Payal 38-year-old female have fracture of femur.
1) Write down signs & symptoms of patient.
Clinical manifestation /sign and symptoms:
Pain,
Tenderness at site of fracture.
Swelling.
Increase body temperature.
Loss of function.
Diformity.
Blood loss.
Impairment in function.
Numbness.
Shortening of extremities.
Discolouration.
Impaired sensation.
Abnormal motility.
Diminized capillary refill.
Pallor.
2) Write down nursing management for Payal with femur fracture.
Monitor the patient’s vital signs.
Assess the patient’s neurovascular status.
Check the patient’s pain level using a pain scale.
Maintain an intake output chart.
Check for any edema or swelling in the limb.
Elevate the affected extremity to reduce swelling.
Check the tightness of the cast.
Check the patient for any signs of infection.
Provide the patient with a comfortable position.
Ask the patient to do some daily routine activities and exercise.
Ask the client to do deep breathing exercises.
Ask the patient to adopt relaxation techniques.
Ask the affected limb to be elevated to the level of the heart. So that venous return can be improved.
Use aseptic technique while dressing.
Ask the affected extremity to do range of motion exercises.
Give the patient knowledge about early ambulation and its benefits.
Ask the patient to take a protein and calcium rich diet.
Provide education to the patient about assistive devices like crutches, walker, crane, slings etc.
Keep changing the position of the patient every two hours.
Provide reassurance to the client.
Provide antibiotics, analgesics, calcium supplements as prescribed by the doctor.
Maintain records and reports.
b) Enlist causes & clinical manifestations of tonsilitis.
Etiology/causes of tonsillitis:
Tonsillitis is mainly caused by bacterial and viral infections. Group A Streptococcus bacteria is the main cause of tonsillitis. Common viruses include influenza virus, herpes simplex virus, cytomegalovirus, adenovirus, and Epstein-Barr virus.
Clinical manifestation/sign & symptoms of tonsillitis:
Swelling in the throat
Sore throat and throat pain
White and yellow patches on the tonsils,
Dysphagia (difficulty in swallowing),
Swelling in the lymph nodes in the neck
Referred pain in the ear (ipsilateral earache),
Bad breath and foul smelling (halitosis),
Fever,
Headache,
Chills,
Malas,
Discomfort,
Fatigue,
Sore throat,
Pain.
Difficulty in swallowing,
Fever,
Feeling cold,
Malas,
Redness.
Irritation,
Discomfort,
Sore throat.
Earache.
Fever.
Headache.
Bad breath.
Muscle pain.
Stiff throat.
Swelling in the lymph nodes of the neck.
Swelling of the eyes, mouth, and throat.
In severe cases, nausea.
Trouble sleeping.
Loss of appetite.
Vomiting.
Stomach pain.
Constipation.
Difficulty opening the mouth.
Headache.
Irritation and discomfort.
Q-3 Write short answer (any two) 6+6-12
A)Write warning signs of cancer
Warning sign of cancer:
CAUTION
1) C:= change in bowel and bladder habit
2) A:=A sore that does not cure
3) U:=Unusual bleeding and discharge
4) T:=Thickening of lump in breast or any other parts
5) l:=Indigestion and difficulty in swallowing
6) O:=Obvious change in mole
7) N:=Naging cough and soreness
Change in bowel and bladder habit
Description( Description ):= In a normal person, the habit of bowel is one to two times.
It changes to 3 to five times.
Bladder:= A normal person passes out the bladder five to six times a day. It increases to 10 to 20 times.
1) Urine and stool change in consistency, size and frequency. Blood is present in urine and stool.
A sore that does not cure.
( Description ):=
1):= In this, the sore keeps getting bigger.
2):= It is very painful.
3):= Blood comes out of it.
In this, wherever the sore falls or ulcer occurs in the body, it never heals, instead of healing, it increases and increases excessively.
Unusual bleeding and discharge.
( Description )
1) :=Blood comes from urine and stool.
2) :=Blood comes from any part of the body such as 1)nipple, 2)penis.
Bleeding or discharge comes from any part of the body, this is a sign of a type of cancer.
Thickening of lump and mass in breast or any other parts of the body.
( Description ):= If there is a lump and mass, then it never heals.
It gets bigger and bigger in its place.
And that lump and mass also causes more pain and becomes like a lump.
Indigestion and difficulty in swallowing.
( Description ):= In this, whatever is eaten is not digested and it becomes difficult to swallow food.
As a warning to a person who has cancer, regurgitation of food occurs.
Obvious change in mole.
( Description ):= If there is any mass and lump, its size changes.
The lump and mass become larger in the place where it decreases.
Necrosis, nagging cough and hoarseness.
Whenever coughing and nagging occurs, a hoarse sound is felt.
There is a change in the voice.
The voice becomes thick.
Blood comes out in the phlegm.
All these signs are warning signs of cancer.
b) Write nursing care of patient with plaster cast
Whenever there is a fracture in any bone, plaster of Paris bandaging is done to immobilize the fractured part. It is called a plaster cast.
With its help, the injured part can be immobilized.
After applying the plaster cast, it is very important to assess the patient’s plaster cast area. The plaster cast should be checked for neurological assessment of this area, pulse, skin color, swelling, etc.
If there is a lot of pain or irritation in the plaster cast area, it is necessary to rule out compartment syndrome.
If there is a change in the color of the skin in the cast area, it should be notified immediately.
This area is prone to skin infection, so special advice should be given to take personal hygiene measurements.
The cast should be applied so that it is not too tight or too loose, and it should be monitored after it dries.
If the plaster is not applied properly, there is a possibility of noise or infection in the area below it. Keep checking for that.
Advise to move the peripheral part beyond the plaster cast to improve blood circulation.
Rule out if there is a history of any allergic reaction while applying the cast.
Maintain cleanliness of the cast and maintain personal hygiene, do not apply any items on top of it.
Do not apply any powder, deodorant or chemical inside the cast.
Advise not to attempt to modify the cast yourself.
Do not place any heavy objects on it, do not break it, and do not lift anything from it.
c) Write down types of hepatitis and prevention of hepatitis-B
Types of Hepatitis:
Hepatitis is an inflammation of the liver. It is most often caused by a virus, but can also be caused by alcohol, drugs, autoimmune reactions, or toxins. There are five main types of hepatitis:
- Hepatitis A:
Transmitted by the fecal-oral route.
It is transmitted through contaminated food or water.
It is usually acute and not chronic.
Recovers without special treatment.
- Hepatitis B:
Transmitted through blood, body fluids, and mother-to-child transmission.
Can become chronic.
Long-term complications such as liver cirrhosis and hepatocellular carcinoma are possible.
- Hepatitis C:
Transmitted primarily through blood.
Many patients remain asymptomatic.
Can easily become chronic and cause long-term liver damage.
- Hepatitis D (Hepatitis D):
Only occurs in people who already have Hepatitis B.
Comes in the form of co-infection (Co-Infection) or super-infection (Super-Infection).
Can make the disease more serious.
- Hepatitis E (Hepatitis E):
Transmitted through the same fecal-oral route as Hepatitis A.
Pregnant Women are at higher risk.
(Prevention of Hepatitis B):
Hepatitis B is a severe viral infection. If not prevented on time, it can lead to chronic hepatitis, liver cirrhosis, or liver cancer. The following steps are very important to prevent it:
- Vaccination:
It is the most effective method of preventing Hepatitis B.
The first dose should be given within 24 hours of birth.
Vaccination is safe and effective for all ages.
- Use of Safe Blood & Instruments:
Selection of Screened Blood Donors.
Use of only sterile and single use needles and sharp objects.
- Safe Sex Practices:
Avoid unprotected sex.
Use condoms correctly.
- Prevent Perinatal Transmission:
Screening of the mother during pregnancy.
Newborns of positive mothers should be given Hepatitis B vaccine and Hepatitis B Immunoglobulin immediately after birth.
- Protection for healthcare workers:
Use of Personal Protective Equipment.
Prevent needlestick injury.
Q-4 Write short notes. 12
a) Stages of bone healing
Bone healing process is the process of repairing the injured bone and restoring its continuity to normal. In it, the structure of the bone is restored. In this, the injured bone part goes through some time and some phases, after which that part returns to normal condition.
The following stages are seen in the bone healing process.
Stage 1 Inflammation
Stage 2 Soft Callus Formation
Stage 3 Hard Callus Formation
Stage 4 Remodeling
Stage 1 Inflammation: This starts a few hours after the injury and reaches its peak level within 24 hours. It is seen for 7 days after 24 hours. This stage causes the hematoma that has accumulated in the injured area to coagulate and form a callus in the injured area.
Stage 2 Soft Callus Formation: The duration of this stage is 2 to 3 weeks. During this time, after the growth of connective tissue in the injured area, a soft callus develops which connects the two ends of the bone. This connection is not strong.
Stage 3 Hard Callus Formation: The duration of this stage is 3 to 12 weeks. After the development of soft callus, after some time, that part becomes hard and is converted into a hard callus. In this stage, the union of the bone is seen clinically but it is not complete healing. In this, hardness develops due to increase in cellular volume and matrix.
Stage 4 Remodeling: This process takes 2 to 3 weeks but may take years to complete. In this stage, the lamellar structure of complete bone and medullary canal develop in the hard callus. In this, the hard callus is reabsorbed by osteoclast cells and the lamellar part of the bone develops by osteoblast cells. Remodeling is seen early in young people.
The healing of bone depends on the age of the person, his nutritional status, whether there is any disease condition or not, hormonal activity, whether there is any bad habit or not.
b) Types of disaster
There are mainly two types of disasters:
Natural disasters
Man-made disasters
Natural disasters
Natural disasters are also known as natural calamities. In which significant damage, loss of life and disruption are seen due to weather or environmental events.
Earthquake: Sudden and violent shaking of the ground is seen due to movement in tectonic plates. Due to which building collapse, infrastructure damage, landslides are seen.
Volcanic eruption: Explosive or effusive magma, ash and gas are released from a volcano which is known as a volcanic eruption. Which causes lava flow, ash cloud, pyroclastic flow, air travel disruption and health hazard.
Tsunami: A series of large waves in the ocean due to underwater disturbance. Due to which coastal flooding (flooding in coastal areas), infrastructure disruption, significant loss of life is seen.
Flood: Overflow of water on dry land. That is, land is covered with water. Due to which water damage, property destruction, water supply contamination occurs.
Cyclone, typhoon, hurricane: Powerful tropical storms are seen due to which high winds and heavy rainfall are seen.
Tornado: A tornado is a violently rotating column of air that is attached to the surface of the Earth and a cumulonimbus cloud.
Drought: A prolonged period of lack of rainfall leads to water shortages. This can lead to crop failure, water scarcity, and wildfires.
Landslides and mudslides: A downhill movement of rock, soil, and debris is known as a landslide. This can cause property damage, road blockages, fatalities, and injuries.
Wildfires: Uncontrolled fires in forests are known as wildfires. This can cause forest destruction, property loss, air quality degradation, and loss of life.
Blizzard and Snowstorm: Severe snowstorms are accompanied by high winds and low visibility. This can cause transportation disruption, hypothermia, and infrastructure damage.
Heatwave: Excessively high temperatures for a long period of time are known as heatwaves. This can cause heatstroke and agricultural damage.
Duststorm: Strong winds cause large amounts of dust in the air. This can cause reduced visibility and respiratory health issues.
Man-made disaster
Man-made disasters are known as anthropogenic disasters. These are events that occur as a result of human action and negligence. Due to which its significant impact on human health, infrastructure and environment is seen.
Industrial Accident: Accidents such as chemical spills, explosions, toxic releases have a significant impact on human life due to conditions like Bhopal gas tragedy (1984)
Nuclear Accident: Radioactive material is released due to the failure of a nuclear power plant. For example Chernobyl disaster – Ukraine
Environmental Pollution: Deforestation, improper waste disposal, air and water pollution cause long-term environmental degradation.
Transportation Accidents: Major accidents such as vehicle, train, ship and airplane accidents result in significant casualties and property damage.
Structural Failure: Buildings, bridges and other structures collapse due to design flaws, maintenance failures and poor construction. Such as the Morbi Bridge disaster
Conflict and Terrorism: Wars, acts of terrorism cause massive destruction, displacement and loss of life. Such as the Syrian Civil War, 11 attacks in the United States (2001)
c) Varicose vein
vericose vein (Define Varicose Vein)
Varicose veins are enlarged, twisted and swollen veins. They are mainly blue or dark purple in color.
They are mostly found in the legs and feet.
Varicose veins are caused by obstruction of blood flow.
causes and risk factors of varicose vein
Genetic
Age
Gender (Women are more likely to develop varicose veins)
Pregnancy
Obesity
Prolonged standing or sitting
Physical inactivity
Hormonal changes
Constipation
Signs and symptoms of varicose vein
Visible bulging veins
Veins that appear twisted or rope-like
Pain in the leg (especially after standing or sitting for a long period)
Swelling in the leg, stiff ankle
Heaviness or tiredness in the leg
Itching around the vein
Cramping or muscle spasms in Leg
Discoloration of skin
Diagnostic evaluation of varicose vein
History collection
Physical examination
Duplex ultrasound
Venography
CT venography
Management of varicose vein
Compression therapy: Compression therapy involves the use of elastic stockings, which apply pressure to the ankle and leg to improve venous blood flow.
Medication: There is no specific medicine to treat varicose veins, but medications are used for symptomatic management. Such as anti-inflammatory drugs to relieve pain and reduce inflammation.
Minimally invasive therapy:
Sclerotherapy: In sclerotherapy, a solution is injected into the varicose vein so that the vein collapses and fades.
Laser therapy: In laser therapy, a strong laser beam is directed at the varicose vein so that the vein fades and disappears.
Endovenous ablation therapy: In endovenous ablation therapy, the varicose vein is closed using laser energy or radio frequency.
Electrodesiccation: In electrodesiccation, the inner lining of the vessel wall is destroyed using an electric current.
Microphlebectomy: In microphlebectomy, the varicose vein is removed with a hook by making an incision.
✓ Surgical Intervention:
Vein Stripping and Ligation: In this procedure, the affected area of the vein is cut and removed through a small incision and the ends of the vein are tied.
Ambulatory Phlebectomy: In ambulatory phlebectomy, small varicose veins are removed by making small punctures in the skin using local anesthesia.
✓ Lifestyle Modification:
Exercise regularly to improve blood circulation.
Ask the patient to walk daily.
Ask the patient not to stand or sit for long periods of time.
Ask the patient to maintain a healthy weight to avoid pressure on the veins.
Ask the patient to elevate the leg to the level of the heart. This will facilitate venous return and reduce swelling.
Ask the patient to avoid smoking.
Ask the patient to make lifestyle modifications.
Ask the patient to maintain a healthy weight.
Ask the patient to exercise regularly.
Ask the patient to eat a high-fiber, low-salt diet.
Avoid prolonged standing or sitting.
Advise the patient to elevate the leg.
Avoid wearing tight clothing.
d) Care of tracheostomy tube
Tracheostomy is a surgical procedure in which a direct opening is made in the trachea and a tracheostomy tube is placed in it. This tube provides air to the patient, especially when it is difficult to breathe normally through the nose or mouth. Proper care of the tracheostomy tube is essential for the patient’s safety, comfort, and protection from infection.
- Cleaning of the Tube:
The tracheostomy tube must be cleaned daily so that mucus and other secretions do not accumulate there.
Remove the inner cannula and wash it in sterile water or saline.
Gently clean the tube with a brush.
After washing and drying it completely, insert the inner cannula again.
Clean the external housing as well.
- Suctioning:
Suctioning is necessary when the patient cannot expel mucus by breathing on his own.
Use sterile technique.
Remove secretions from the trachea using a suction catheter.
Do not take more than 10 to 15 seconds.
Check oxygen support after each suction.
- Stoma Site Care:
Clean the skin where the stoma tube is placed regularly.
Clean with sterile gauze and normal saline.
Report any redness, swelling or discharge around the stoma immediately.
Apply dry gauze and change it daily.
- Tube Fixation and Stability:
Check the tube fixation properly to ensure that it is not loose.
Adjust the neck strap so that the patient does not feel pressure and the tube does not come out.
Check the fixation status in every shift.
- Humidification:
It is necessary to provide humidified air as the patient breathing through the tracheostomy tube feels dry.
Use a humidifier.
Sometimes HME (Heat Moisture Exchanger) is also used.
- Emergency Preparedness:
Always be prepared for conditions like tube blockage or accidental dislodgement.
Second, keep sterile tubes, obturators, suction machines, and oxygen readily available.
Staff and caregivers should be given advanced training.
- Assessment and Documentation:
Monitor the patient’s respiratory status, respiratory rate, oxygen saturation, etc.
Document each activity and observation properly.
- Patient and Caregiver Education:
Train the patient and their family members in tube care, cleaning, suction, and emergency management.
Provide written and demonstration guidance.
Proper care of the tracheostomy tube is very important for the patient’s life. Regular cleaning, hygiene, suctioning, and continuous monitoring protect the patient from infection and ensure that their breathing pattern is working properly.
Q-5 Define following (any six) 12
a ) Kyphosis
Kyphosis is an abnormality of the spine in which the spinal cord is curved outwards.
The spinal cord is rounded or hunchbacked. In kyphosis, the convexity of the spine increases outwards.
b) Amputation
Amputation comes from the Latin word amputare. Its meaning is “to cut off”.
The injured or deformed part is completely removed (cut).
c ) Leukemia
Leukaemia is a malignant (cancerous) disease that affects the blood and blood-forming organs such as the bone marrow, lymph, and spleen. In Leukemia, there is an abnormal increase in the formation of leukocyte cells, which affects the formation of normal red blood cells, which causes anemia.
d) Triage – Triage
A)explain about triage: Triage is a system used during disasters.
It is designed to give priority to the patient in the hospital
TRIAGE=SHORT/MINIMISE.
(USED DURING DISASTER)
S=SHORT
T=TRIAGE
A=AND
R=RAPID
T=TRANSPORT
Triage has three color codes, through which the patient is categorized and then transported to the hospital as per the immediate need.
1) Emergency 😡(Red colour): In this, the person needs immediate treatment. For this, the sooner they are sent to the hospital for treatment, the better.
Example:=severe respiratory depression ,
BRAIN HEMORRHAGE
2)URGENT🙁 (YELLOW Color): In this, the person does not need to be taken to the hospital immediately like in red color. Even if the person who has any injury is taken to the hospital for treatment for one to two hours late, this yellow color works even if the patient gets treatment a little late.
3)Delay🤢(Green color): In this, the person in green color does not need very immediate treatment like in red and yellow color. In this, the person gets treatment even if the person gets treatment for one to three hours late. There is no emergency in this.
4)Death ⚰️(Black color): In this, the person is in a very serious condition or is in a condition like death. So according to this color code, we can give treatment according to the needs of the injured person.
2)system:
1)Identification of victim:= In this, the victim is identified such as the name, address and the need of the victim and treatment is given.
2)Relief work:= In this, treatment is given according to the needs of the person such as ECG, RBS, CPR, etc.
3)Rehabilitation/recovery:= If the patient is treated in this, he/she becomes rehabilitated and returns to his/her previous health condition.
So according to triage, we can take any person who needs treatment to the hospital according to the extent.
e) Mammography –
Mammography is a special X-ray imaging technique used for the initial diagnosis of breast cancer, in which a mammogram is performed to obtain a clear and high-resolution image known as a mammogram. In this procedure, photographs are taken from both sites by gently pressing the breast tissue so that tumors, microcalcifications, or other abnormalities can be easily identified. Mammography is of two types, Screening Mammography and Diagnostic Mammography, in which screening is for patients who have no symptoms, while diagnostic is for patients with symptoms. Mammography is considered a highly effective and reliable method for the prevention and early therapy of breast cancer.
f) Traction
Traction is a therapeutic method in which a broken body part is pulled and kept in the proper position, especially when the bone is broken. This method helps in reducing muscle spasm, controlling pain and stabilizing the fracture (fragment).
g) Biopsy.
Biopsy is a medical procedure in which a sample of tissue or cells is taken from a suspected part of the body so that it can be examined under a microscope to obtain specific information about the disease. This procedure is especially used for the diagnosis of diseases such as cancer. The main types of biopsy involve needle biopsy, excisional biopsy, incisional biopsy and endoscopic biopsy. This procedure is usually performed under anesthesia and provides necessary and reliable information for the treatment of the patient.
h) Epistaxis
Epistaxis means nose bleed or nasal hemorrhage. Bleeding from the nostril or nasal cavity due to rupture of vessels in any area of the mucous membrane in the nose is known as epistaxis. Epistaxis is also called nose bleed. This is a condition in which active bleeding occurs from the nostril, nasal cavity or nasopharynx. This occurs when the blood vessels inside the nose are damaged or injured. The process of bleeding from the front or back of the nose is called nose bleed or epistaxis.
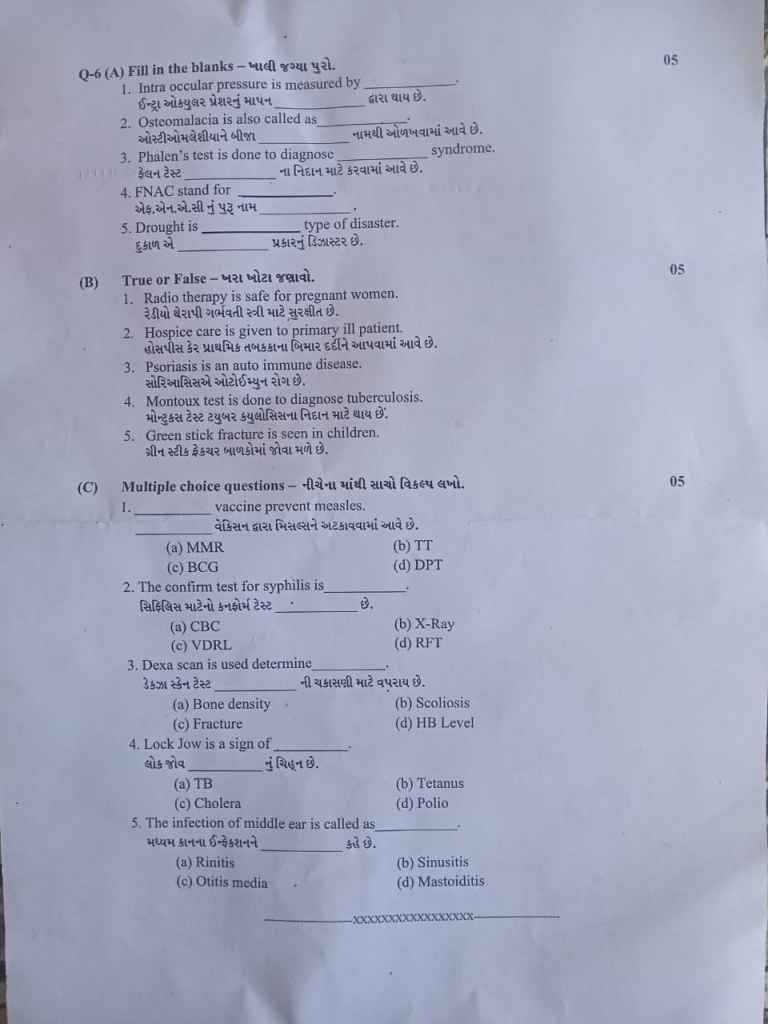
Q-6 (A) Fill in the blanks – 05
1.Intra occular pressure is measured by……… (Intraocular Pressure, IOP)
2.Osteomalacia is also called as………….. (Rickets)”
3 .Phalen’s test is done to diagnose …………….syndrome (Carpal Tunnel Syndrome)
4.FNAC stand for ………………… Fine Needle Aspiration Cytology.
5.Drought is …………….type of disaster. (Natural)
B) True or False – 05
1.Radio therapy is safe for pregnant women. ❌
2.Hospice care is given to primary ill patient. ❌
3.Psoriasis is an auto immune disease. ✅
4.Montoux test is done to diagnose tuberculosis. ✅
5.Green stick fracture is seen in children. ✅
(C) Multiple choice questions05
1…………vaccine prevent measles.
(a) MMR
(b) TT
(c) BCG
(d) DPT
2.The confirm test for syphilis is ……………
(a) CBC
(b) X-Ray
(c) VDRL
(d) RFT
3.Dexa scan is used determine…………….
(a) Bone density
(b) Scoliosis
(c) Fracture
(d) HB Level
4.Lock Jow is a sign of…………….
(a) TB
(b) Tetanus
(c) Cholera
(d) Polio
5.The infection of middle ear is called as…………………..
(a) Rinitis
(b) Sinusitis
(c) Otitis media
(d) Mastoiditis