ENGLISH-MEDICAL SURGICAL NURSING : 2 (PAPER SOLUTION): 31/07/2018 (Done)-UPLAOD no.10
PAPER SOLUTION NO.10-31/07/2018
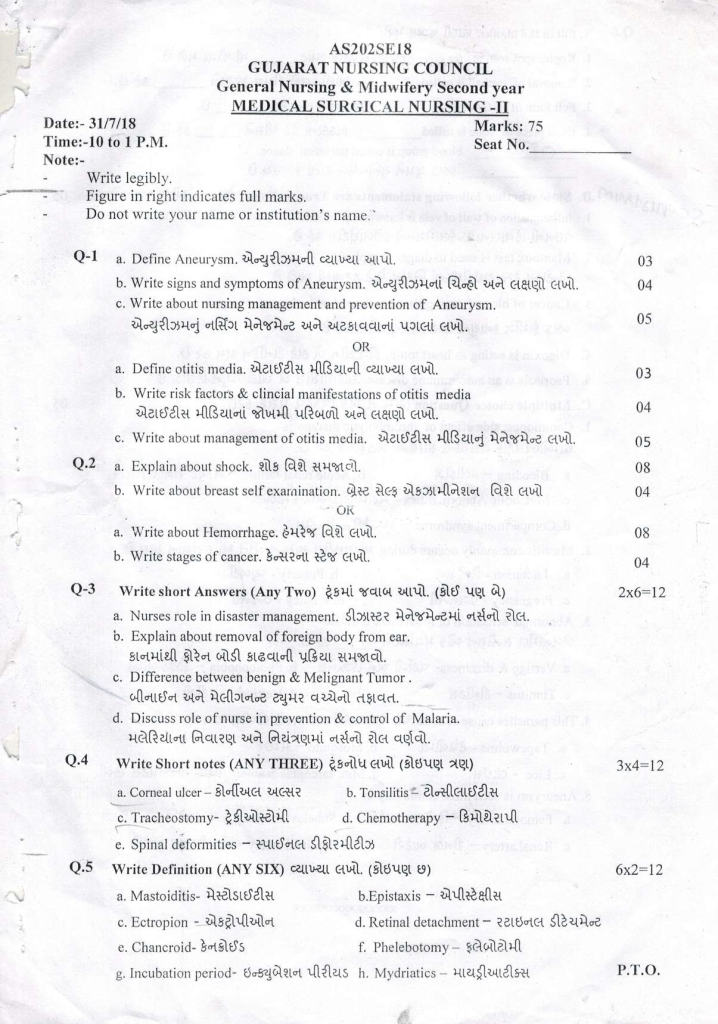
Q-1
a. Define Aneurysm., .03
Aneurysm is also known as ‘aneurysmal dilatation’. A localized bulging, ballooning or sac-like structure is seen at a weak point in the wall of a blood vessel, which is known as an ‘aneurysm’. Aneurysm is found in all sizes of arteries. Aneurysm is mainly found in the aorta. Apart from this, it is also found in the arteries supplying blood to the brain, heart, intestine, and back of the spleen. Due to aneurysm rupture, conditions like internal bleeding and stroke are seen, which is a fatal condition.
b. Write signs and symptoms of Aneurysm.04
The signs and symptoms of an aneurysm depend on the location of the aneurysm.
Cerebral aneurysm:
When a cerebral aneurysm is small, there are no symptoms. Cerebral aneurysm rupture causes the following signs and symptoms:
Sudden and severe headache (worst headache of one’s life)
Nausea and vomiting
Stiff neck
Blurred or double vision
Sensitivity to light
Seizures
Loss of consciousness
Drooping of eyelids
Confusion
Difficulty in speaking
Thoracic aortic aneurysm:
Chest pain (typically in the back and side)
Cuffing
Shortness of breath
Horsiness
Difficulty in swallowing
Abdominal aortic aneurysm:
Deep constant pain in the abdomen or on the side and back of the abdomen
Pulsating feeling near the Navel (navel)
Abdominal aortic aneurysm rupture causes the following symptoms:
Severe pain in abdomen and back
Nausea
Vomiting
Sweaty skin
Rapid heart rate when standing
Internal bleeding
Peripheral aneurysm:
Pain and swelling in limb
Pulsating lump in area of aneurysm
Cold fit, toss or finger
General symptoms:
Sudden and intense pain
Drop in blood pressure
Shock
Loss of consciousness
C. Write about nursing management and prevention of Aneurysm. 05
Nursing Management:
1) Vital Signs Monitoring:
Regular monitoring of the patient’s blood pressure, heart rate, respiratory rate and oxygen saturation is necessary. Any sudden change may indicate rupture.
2) Pain Assessment and Management:
Continuous assessment of the pain experienced by the patient and administration of analgesic medication as ordered.
3) Blood Pressure Control:
High blood pressure is a major risk factor for aneurysm rupture. Therefore, blood pressure should be controlled with antihypertensive medication.
4) Neurological Observation:
If the aneurysm is in the brain, monitor consciousness level, pupils, movement and seizure activity.
5) Pre-operative Care:
Advise the patient and family about the surgery, obtain informed consent, maintain a nil by mouth and complete necessary lab investigations.
6) Post-operative Care:
Monitor for bleeding, infection, reperfusion injury, urine output and signs of shock after surgery. Pay attention to patient mobilization and nutritional support.
7) Education and Psychological Support:
Provide information about aneurysm to the patient and his family members, explain the treatment process and provide psychological support for the mental distress caused.
Prevention:
1) Control of High Blood Pressure:
Hypertension is the main risk factor for aneurysm. Its control with regular monitoring and medication is essential.
2) Avoid Smoking:
Smoking damages blood vessels and is responsible for the development of aneurysm. Advise the patient to avoid smoking.
3) Adopt a Healthy Diet and Lifestyle:
Avoid fatty and cholesterol-rich foods, manage your weight, and be active daily.
4) Avoid Alcohol Abuse:
Alcohol is responsible for high blood pressure and vascular damage.
5) Screening for Family History:
If a patient has a family history of aneurysm, imaging tests such as ultrasound, CT scan, or MRI should be done periodically.
6) Regular Medical Check-up:
Screening and regular follow-up should be done for high-risk patients such as hypertensive, smokers, or old-age patients.
Aneurysm is a silent yet life-threatening condition. Regular monitoring, patient education, timely treatment and lifestyle modification can reduce the risk of aneurysm. The role of the nurse is to provide constant observation and holistic care of the patient so that potential complications can be avoided.
OR
a. Define otitis media. .03
Otitis media is made up of three words. Ot means ear, itis means inflammation and media means middle ear. Infection and inflammation of the middle ear is known as ‘otitis media’.
“Otitis” means:=inflammation of the Ear.
“Media”Means :=middle.
Infection and inflammation of the middle ear is called otitis media.
This inflammation spreads from a sore throat, (cold) cold or other upper respiratory tract infection to the middle ear and can be caused by viruses or bacteria and can be acute and chronic. In it, fluid accumulation occurs in the middle ear and due to this, bulging occurs and it causes pain.
type
1)Acute otitis media:
Acute otitis media is also called Acute suppurative otitis media or purulent otitis media. Acute otitis media is an acute infection and inflammation. It has an immediate onset and lasts for a short time. In this, the acute infection occurs in the middle ear and lasts for six weeks (6 weeks).
2)Chronic otitis media:
Cronic otitis media is also called chronic suppurative otitis media. In chronic suppurative otitis media, the infection of the middle ear is long-term and causes ear tissue damage and chronic otitis media is caused by repeated episodes of acute otitis media.
Chronic otitis media is caused by the accumulation of fluid in the middle ear. And middle ear infections also involve the mastoid bone.
b. Write risk factors & clincial manifestations of otitis media.04
Risk Factors:
Upper Respiratory Tract Infections (URTI)
Age < 3 years
Bottle Feeding in Supine Position
Allergies or Sinusitis
Exposure to Tobacco Smoke
Attending Day-care Centers
Cleft Palate or Craniofacial Abnormalities
Family History of Otitis Media
Clinical Manifestations
Ear Pain (Otalgia)
Fever
Hearing Loss
Irritability in Children
Ear Discharge (if perforation occurs)
Fullness or Pressure in Ear
Tugging or Pulling at Ear
Vertigo or Imbalance (in severe cases)
Mnemonic to Remember Symptoms: “HEAR FIST UP”
H – Hearing loss
E – Ear discharge
A – Appetite loss
R – Red tympanic membrane
F – Fever
I – Irritability
S – Sleep disturbance
T – Tugging at ear
U – Unsteady balance
P – Pain in ear
c. Write about management of otitis media. .05
Medical management of Otitis media.
If the patient has a condition of otitis media due to any bacterial infection, then give antibiotic medicine.
If the patient is in pain, provide analgesic medicine to relieve it.
If the patient has a fever, provide antipyretic medicine.
If the patient has any inflammatory condition, provide anti-inflammatory medicine.
If the patient has otitis media due to inflammation, instill antibiotic and corticosteroid ear drops to reduce inflammation and fight infection.
Provide gentle compression in the affected ear to relieve pain and discomfort.
Encourage the patient to drink adequate water to prevent dehydration.
surgical management of Otitis media.
1) Tympanocentesis:
In the tympanocentesis procedure, the fluid and pus present are aspirated through a needle. This procedure is mainly done when a small amount of fluid and pus has been collected.
2) Myringotomy/ Tympanotomy:
In this procedure, an incision is made in the tympanic membrane and then the debris and pus present in the middle ear are removed using forceps and tubing.
Name of the tube: Grommet tube.
3) Mastectomy:
This procedure is mainly performed when the infection in the middle ear becomes very severe. In mastectomy, an incision is made on the mastoid process and then the affected area of the middle ear is removed.
There are two types of mastectomy
1) Simple Mastectomy:
In this, only the affected area of the middle ear is removed.
2) Radical Mastectomy:
Radical mastectomy is performed to remove the three bones of the ear, the tympanic membrane and to close the opening of the Eustachian tube.
4) Otalum:
In the Otalum procedure, a small hole is made in the tympanic membrane using a laser. Otalum is an alternative method of myringotomy. In this procedure, debris present in the middle ear is removed.
Nursing management of Otitis media:
Properly assess the patient’s symptoms such as ear pain, irritability, fever, and assess the patient’s general health.
Observe the patient’s ear canal for any inflammation or swelling present and assess whether there is any redness in the tympanic membrane.
Properly assess the patient’s hearing acuity.
Use simple language, short sentences and speak slowly with the patient.
Examine the patient for any drainage in the ear canal.
If the patient is in pain, provide prescribed analgesic medicine.
Ex: Acetaminophen,
Ibuprofen.
Provide complete information to the patient and his family members about the patient’s disease condition, its causes, its symptoms and signs and its treatment.
Advise the patient to lie down on the affected side to reduce the pressure in the ear.
If the patient is experiencing pain and discomfort, perform proper comfort measures around the ear, such as warm compresses and gentle massage, to relieve the patient’s discomfort.
Assess the patient’s vital signs properly.
Provide antipyretic medication if the patient has a fever.
Advise the patient to maintain proper fluid intake to maintain hydration status.
Advise the patient to maintain proper hygienic conditions while handling the patient.
Advise the patient to have proper nutritional food intake.
Provide antibiotic medication and instill ear drops to the patient.
Provide a proper comfortable environment to the patient.
Q.2
a. Explain about shock .08
Shock is a condition in which blood, oxygen, and nutrition do not reach the vital organs due to low systemic blood pressure. As a result, the organs cannot work adequately and have to be overloaded to work, so the body goes into a state of shock.
☆ ☆Classification :
1)Decrese blood supply:=
a)cardiogenic shock
b) Hypovolemic shock
2)Abnormal blood supply:=
A) Septic shock
B) Allergic shock
C) Neurogenic shock
1)Decreased blood supply:=
A)cardiogenic shock: = In this type of shock, when the heart cannot work in the proper amount, due to which the blood does not reach all the parts of the body in sufficient quantity, due to which the condition of shock arises.
B)Hypovolemic shock: = In this condition, when due to excessive blood or fluid loss from the body due to any reason, the fluid content in the body decreases, due to which the condition of shock arises, it is called hypovolemic shock.
2)Abnormal blood supply:=
A)Septic shock:= This type of shock occurs when any germ enters any part of the body and infection occurs in that part of the body due to which the condition of Septic shock is seen.
B)Allergic shock:= This type of shock is seen due to allergic reaction.
C)Neurogenic shock:= This type of shock is seen due to any type of hemorrhage or damage in the nervous system.
2)Etiology:
☆malfunction of heart. ( Malfunction of heart)
☆myocardial infraction ( Myocardial infraction),
☆Angina pectoris ( Angina pectoris),
☆coronary aartery disease ( Coronary artery disease),
☆structure disease due to trauma( Structure disease due to trauma),
☆Cardiac arrest ( Cardiac arrest),
☆Abnormality of lungs,
☆Dysfunction of lungs( Dysfunction of lungs),
☆Pulmonary embolie( Pulmonary embolie),
☆Atlectasis( At lectasis),
☆Pneumonia( New monia),
☆Thoracic injuries ( Thoracic injury),
☆Reduction in blood volume due to burns,hemorrhage, diarrhea, vomiting, peritonitis. Etc
3)Clinical manifestation:
★ Reduce blood supply,
Anxiety,
★ Cynosis,
Rapid pulse,
Nausea,
Vomiting,
Cold, white and clammy skin,
Aspiration is Rapid or weak,
Pulse is Rapid and weak,
Pale face,
Low blood pressure,
Decrease urine output,
Metabolic acidosis.
4) Medical management: Give the patient oxygen.
Set up an IV line for the patient.
Give the patient intravenous fluid.
Give emergency drugs to the patient.
Provide blood supply to the patient. Give blood when there is a lot of blood loss to reduce dysrhythmia hypotension.
If necessary, give platelets and coagulant factors to the patient so that if there is a lot of blood loss, it works as a clotting factor.
Insert urinary catheter so that urine output can be determined.
Give the patient a supine position and keep the legs elevated. This position is contraindicated if there is a head injury.
5)Nursing management of patient with shock:=
Monitor the patient’s vital status.
Give the patient a comfortable position.
Provide the patient with a comfortable environment.
Maintain the patient’s oral hygiene.
Check the patient’s intake output.
Check the patient’s respiration.
Monitor the patient’s ECG.
Monitor the patient’s vital signs such as temperature, pulse, respiration, blood pressure.
If the patient has a safety concern, give them proper antibiotics and full environment.
Maintain the patient’s hydration status.
Maintain the patient’s nutritional status.
b. Write about breast self examination, .04
Breast self examination is done to see if there is any kind of abnormal mass, lump or nodule in the breast.
☆PURPOSES:
1) To see if there is any kind of abnormality in the breast.
2) To take early notice of breast cancer.
☆☆Time:
1) Breast self examination is usually done once a year in normal women.
2) If there is breast cancer, then it is done twice a year.
3) It is done once a month during menopause.
4) It is done once a month during the reproductive age.
☆☆There are total 5 steps for breast self-examination:
☆1)Step1: Stand in front of the mirror. Then look at the breast to see if there is any abnormality in it such as redness, discharge, abnormal size, inverted nipple, swelling, dimpling, bulging, etc. Thus, see if there is any abnormality in the breast.
☆Step2: In this step, keep your hands behind your head, then turn your head forward with your hands and look in the mirror to see if the size of the breast is symmetrical.
☆Step3: In this step, keep your hands on your waist, then lean forward and see if the size of the breast is symmetrical and if there is any lump.
☆Step4:
In this step, stand in front of the mirror.
Then raise your left hand.
Then palpate the left breast with the first three fingers of the right hand.
First of all, palpate in a circular motion.
Palpate from the outside to the inside.
Then quiz the nipple.
See if there is any discharge in it.
Now palpate the right breast in the same way.
Through this step, it is known whether there is any lump or mass in the breast.
☆Step5:
Then squeeze the nipple to see if there is any discharge in it.
Thus, through breast self examination, it is known from this step whether there is any abnormality in the breast and if breast cancer is to occur, it is known at the first opportunity.
OR
a write about Hemorrhage.08
Hemorrhage:- Hemorrhage means bleeding. In which blood loss occurs from damaged blood vessels. Which can be seen inside or outside the body.
Types of hemorrhage:-
Hemorrhage is mainly divided into two types:
1) External hemorrhage
2) Internal hemorrhage
1) External hemorrhage:- In external hemorrhage, bleeding is outside the body from a wound, abrasion or injury site and is visible.
2) Internal hemorrhage:- In internal hemorrhage, bleeding is seen inside the body. Which cannot be immediately visible like external hemorrhage. Which includes intracranial hemorrhage, gastrointestinal hemorrhage, pulmonary hemorrhage.
✓ Arterial Hemorrhage: – Bleeding seen in an artery is known as arterial hemorrhage. Which appears bright red in color. Arterial hemorrhage is severe and life threatening. Which is difficult to control (because the blood pressure in the artery is high).
✓ Venous hemorrhage: Bleeding seen in veins is known as ‘venous hemorrhage’. Which is seen in dark red color. Venous hemorrhage is less severe than arterial hemorrhage.
✓ Capillary hemorrhage: Bleeding seen in the smallest blood vessels capillaries is known as capillary hemorrhage. In capillary hemorrhage, small amounts of bleeding are seen from minor cuts and abrasions.
Causes of hemorrhage
Trauma or injury (accident, fall down, violence)
Medical condition (hemophilia, blood clotting disorder, liver disease)
Medication (blood thinner – warfarin, Aspirin)
Surgery
Aneurysm
High blood pressure
Cancer
Ulcer
Childbirth Signs and symptoms of hemorrhage
✓ External bleeding
Bleeding from open wound
Visible bleeding
Bruising
Discoloration of skin
Swelling around affected area
✓ Internal hemorrhage :
Intracranial hemorrhage :
Severe headache
Confusion or altered mental status
Vision problems
Seizures
Weakness or numbness on one side of body
Gastrointestinal hemorrhage :
Blood in vomiting
Blood in stool
Abdominal pain and swelling
Pulmonary hemorrhage :
Blood on phlegm
Chest pain
Breathing Difficulty
✓ General symptoms :
Rapid and shallow breathing
Rapid pulse
Hypotension
Pale or clammy skin
Weakness
Fatigue
Disease
Lightheadedness
Diagnostic evaluation of hemorrhage
History collection
Physical examination
Complete blood count
Coagulation study
Ultrasound
CT scan
MRI
Angiography
Endoscopy
Management of hemorrhage
Immediate first aid care :
Apply pressure: Apply pressure to the bleeding site using a clean cloth or bandage. This will help control the bleeding.
Elevate the area: If the bleeding is from a limb, elevate it to the level of the heart. This will reduce blood flow to that area.
Immobilize Area: Immobilize the injured area. So that further damage can be prevented.
✓ Medical Management:
Minor Hemorrhage:
Topical Hemostatic Agent: Apply a hemostatic agent with gauze to control minor bleeding.
Sutures or Staples: Small cuts and lacerations are cured with the help of sutures or staples.
Major Hemorrhage:
Tourniquet: In cases of severe limb bleeding, apply a tourniquet over the injury site. So that blood flow can be controlled.
Blood Transfusion: If necessary, replace the blood with a blood transfusion.
Intravenous Fluid: Administer intravenous fluid to maintain blood pressure and organ perfusion. Do.
Medication: Administering medicine such as tranexamic acid to control bleeding.
✓ Surgical intervention:
Ligation or clamping: Tying or clamping the bleeding vessel.
Repair of injured tissue: Surgically removing the damaged organ or tissue.
✓ Monitoring and support:
Vital sign monitoring: Continuously monitoring the patient’s blood pressure, pulse, respiratory rate, and oxygen level.
Critical care support: In severe cases, the patient is kept in the intensive care unit (ICU). So that the patient can be closely monitored and advanced interventions can be performed.
b. Write stages of cancer. .04
Introduction:
Cancer is a pathological condition in which the cells of the body divide in an uncontrolled manner and are invasive or metastatic in nature. The stages of cancer indicate the grade and extent to which the tumor has progressed, as well as the clinical classification. In addition to the staging system, stages are very important for treatment planning and prognosis.
1) Stage 0 (Stage 0 – Stage Zero):
Known as carcinoma in situ.
This stage is the earliest stage in which abnormal cells are confined to the originating tissue. There is no invasion of surrounding healthy tissue.
The cure rate is highest in this stage because the condition is localized.
2) Stage I (Stage I – Stage One):
This is called early-stage invasive cancer.
The tumor is small in size and has not spread to the lymph nodes.
Surgical removal and adjunct therapies can provide a successful outcome.
3) Stage II (Stage II – Stage Two):
The tumor is slightly larger and there is some infiltration of nearby tissues or initial lymphatic involvement.
There may be some infiltration, but there is no distant metastasis.
At this time, combination therapy is needed, such as chemotherapy + surgery.
4) Stage III (Stage III – Stage Three):
This is advanced local spread.
The tumor has spread extensively to nearby organs, structures, or lymph nodes.
In some cases, symptoms may also be severe.
Multimodal treatment is necessary, such as radiation therapy, chemotherapy, and sometimes immunotherapy.
5) Stage IV (Stage IV – Stage Four):
This is called metastatic cancer.
The cancer has spread to other organs of the body – such as the brain, liver, lungs, bones, etc.
Curative treatment is not possible, but palliation and symptom management are important.
Targeted therapy and supportive care can help maintain life span and quality of life.
Conclusion:
Cancer staging is the most important clinical step after diagnosis, which is the basis for treatment selection, patient counseling, and prognosis. Nurses, physicians, and oncologists have to schedule interventions according to staging.
Q-3 Write short Answers (Any Two). 2×6=12
a. Nurses role in disaster management.
The word disaster is derived from the word disaster or disaster. The meaning of which was compared to destruction by ancient people. These people believed that disaster was caused by an unfavorable position of the planet or the earth or by an unfavorable condition created by God.
According to the WHO, a disaster is any extraordinary event in any area of society that causes damage or loss, economic disturbances, loss of human life, damage to health and health services.
This is a condition in which there is a very large morbidity and mortality, and there is a lot of damage to property, roads, electrical lines and all infrastructure.
Disaster is a dangerous condition that is unpredictable and occurs suddenly and unexpectedly.
At this time, a person’s normal schedule is disrupted, and this is a major change in a person’s normal life.
Role of a nurse in disaster management.
The role of a nurse in disaster management is very important. In which it is especially necessary to take multi-disciplinary management steps as a nurse.
During a disaster, the affected population should be identified. They should be given care and should actively participate in disaster planning and management.
During a disaster, a nurse plays a key role in maintaining a holistic care approach. In which they work for the integration of everyone.
Nurses provide care to each person from physiological, psychological and spiritual aspects and maintain collaboration between each team member.
As a nurse, it is necessary to identify what type of event and what type of damage there is during a disaster. Then the main task is to identify the needs of the affected population.
After arranging the needs in priority setting, objectives and goals are set and resources and activities to fulfill the needs are planned through a collaborative approach.
During this time, they also contact government, non-government and many agencies to help them be as helpful as possible.
Nurses themselves need to be physically and psychologically prepared to work in disaster management. He should have the necessary training and professional preparation to do the job.
In this situation, the nurse tries to be helpful by maintaining communication between each team member.
Nurses also have a very important role in the disaster management plan and disaster prevention strategy in the community.
For this, the necessary strategy and training program should also be implemented. The people of the community can be made aware and informed about this matter through mock drills.
An evaluation plan is also prepared in a disaster. According to which, precautions can be taken in planning and implementation after assessment.
Efforts are also made to normalize the population affected by the disaster through a rehabilitation program.
It is also important to consider the basic needs of affected individuals and meet these needs at every stage of disaster planning.
b. Explain about removal of foreign body from ear.
Introduction:
Foreign bodies such as iron, pins, cotton, butterflies, live insects, etc. getting stuck in the ear are common, especially in children. If these objects are not removed in a timely and proper manner, infection, perforation or hearing loss can also occur in the ear.
Assessment required for removal:
Visual inspection of the ear with otoscopy to identify the exact location, size and type of foreign body.
History to know when the foreign body was stuck, attempt to remove before, ear pain or discharge.
Techniques of Removal of Foreign Body:
1.Manual Instrumentation:
Alligator forceps, Suction catheter or Hook are used for common non-living foreign bodies.
Pulling the foreign body slowly with direct visualization into the ear canal.
2.Irrigation:
For non-organic smooth objects, the method of washing the foreign body with a syringe using sterile warm saline or clean water.
Contraindicated if the tympanic membrane is perforated.
3.Chemical Immobilization:
If the foreign body is an insect, it is necessary to kill it first.
Therefore, mineral oil or lidocaine should be instilled to kill the insect and then removed.
4.Suction:
Low-pressure suction is used for smaller foreign bodies, especially beads or seeds that are round and smooth.
Precautions:
Keep the patient calm. If it is a child, then do proper immobilization.
Do not make aggressive attempts that may cause canal abrasion, bleeding, or perforation.
If repeated attempts for removal fail, then ENT consultation is necessary.
Role of Nurse:
Do proper assessment.
Keep sterile instruments ready.
Support the patient psychologically.
Maintain aseptic technique during the procedure.
Give post-procedure care such as topical antibiotic ear drops.
Referral if needed to ENT specialist.
Conclusion:
Foreign body removal from ear is a delicate procedure that should be performed by trained personnel. Nurses should play an active role in every stage from assessment to post-removal care so that complications can be prevented.
c. Difference between benign & Malignant Tumor.
Difference between Malignant Tumor and Benign Tumor
Benign Tumor:
Growth Rate:
- Grows slowly.
- Usually does not spread to surrounding tissues.
Shape:
- Has a smooth, well-defined surface.
Cell Characteristics:
- Benign cells appear normal and do not have mutations.
Capability to Spread:
- Does not metastasize (spread to other parts of the body).
Impact on Health:
- Usually not fatal, but may cause pressure, pain, and other symptoms if it is near vital organs.
Treatment:
- Can be easily removed with surgery and has a low chance of recurrence.
Malignant Tumor:
Growth Rate:
- Grows at a rapid rate.
- Can invade surrounding tissues and organs.
Shape:
- Has a disorganized and irregular surface.
Cell Characteristics:
- Malignant cells are new and have mutations that cause them to grow uncontrollably.
Capability to Spread:
- Can metastasize to other parts of the body through lymph nodes and hemoglobin.
Impact on Health:
- Is life-threatening and can cause significant health problems.
Treatment:
- Requires more extensive and aggressive treatment such as surgery, chemotherapy, radiation therapy, and targeted therapy.
- High likelihood of recurrence and spread.
d. Discuss role of nurse in prevention & control of Malaria.
Introduction:
Malaria is a serious parasitic disease caused by Plasmodium species and transmitted by the bite of female Anopheles mosquito. Nurses play an important role as frontline health workers in both prevention and control of malaria.
1.Surveillance and Early Detection:
Nurses identify suspicious fever cases and initiate immediate diagnostic process.
Detection is done through rapid diagnostic tests and peripheral blood smear.
Antimalarial therapy is given immediately to positive patients.
Referral to higher centers is ensured in serious or complicated cases.
2.Health Education and Awareness:
Nurses educate about malaria symptoms, transmission and complications at the community level.
Advises on the use of insecticide treated bed nets, mosquito repellents and protective clothing.
Conducts health education sessions in public places, schools and Anganwadis.
Motivates people to remove stagnant water and maintain cleanliness.
3.Vector Control Participation:
Nurses participate in both non-chemical and chemical methods for vector control.
Also works with trained persons in indoor residual spray, oiling of water surfaces and larviciding.
Nurses remain alert for identification and observation of vector breeding sites.
4.Chemoprophylaxis and Treatment Adherence:
Gives guidance on chemoprophylactic drugs such as doxycycline or mefloquine for high risk groups such as pregnant women, immunocompromised patients, and travelers.
Nurses ensure that patients complete the prescribed dose.
Keeps patients informed about side effects.
Monitors and counsels in cases of non-adherence.
5.Record Maintenance and Reporting:
Nurses properly document each positive case.
Maintains case register, line listing and daily reports.
Reports to higher health authorities on regular basis.
Analyzes trends and possible outbreaks from reported cases.
6.Training and Community Mobilization:
Nurses train ANMs, ASHAs and local health workers.
Collaborates with NGOs, local bodies and youth groups for community participation.
Conducts special awareness campaigns for parents and school children.
Nurses are not limited to clinical care only, they are a strong pillar of the public health support system. Nurses play a critical role in every step of malaria prevention and control — surveillance, education, vector control, chemoprophylaxis, treatment adherence, and reporting. Their efforts have enabled significant reductions in both mortality and morbidity from malaria.
Q.4 Write short notes (ANY THREE) 3×4=12
a. Corneal ulcer
Introduction:
Corneal Ulcer is an inflammatory or infectious lesion in the epithelial layer of the cornea and the underlying stromal layer. Such an ulcer is primarily of microbial origin, but sometimes non-infectious causes can also be responsible.
Etiology:
Corneal ulcer is usually caused by the following pathogens:
1.Bacterial ulcer:
Most common cause; especially Pseudomonas aeruginosa, Staphylococcus aureus, etc. More common in contact lens users.
2.Viral ulcer:
Mainly caused by Herpes Simplex Virus and Herpes Zoster Ophthalmicus.
3.Fungal ulcer:
Especially caused by Fusarium and Aspergillus species.
4.Acanthamoeba keratitis:
Protozoan parasite.
5.Non-infectious causes:
Severe dry eye, exposure keratopathy, neurotrophic keratopathy, etc.
Pathophysiology:
During corneal ulcer, there is a break in the corneal epithelium and microbial agents cause stromal invasion. As a result, the release of inflammatory mediators by neutrophils and cytokines leads to tissue necrosis.
Clinical Features:
Severe ocular pain
Redness
Photophobia
Lacrimation
Foreign body sensation
Decreased visual acuity
Purulent discharge
Diagnosis:
- Slit Lamp Biomicroscopy – to see ulcer size, depth, infiltrate, hypopyon.
- Fluorescein staining – to diagnose epithelia defect.
- Corneal scraping and culture – to identify the causative organism.
- Confocal Microscopy – to see the presence of fungal or Acanthamoeba.
Treatment:
Medical Management:
Broad-spectrum antibiotics: such as Fluoroquinolones or fortified Cefazolin + Tobramycin
Antiviral agents: such as Acyclovir for Herpetic ulcer
Antifungal drugs: such as Natamycin or Voriconazole
Cycloplegics: such as Atropine – to reduce pain
Lubricating drops: for supportive care
Surgical Management:
Tarsorrhaphy – for non-healing ulcer
Therapeutic Penetrating Keratoplasty – for perforation or refractory ulcer
Complications:
Corneal perforation
Secondary glaucoma
Endophthalmitis
Permanent vision loss
Corneal opacity
Prevention:
Strict hygiene during contact lens handling
Prompt treatment of ocular trauma
Avoid self-medication with steroids
Regular ophthalmic follow-up
Conclusion:
Corneal ulcer is a vision-threatening ophthalmic emergency. It requires timely and appropriate microbiology-guided treatment.
b. Tonsilitis
Tonsils are masses of lymphatic tissue located in the throat. Their function is to protect the body from microorganisms and toxic substances of the organism.
When the tonsils become infected and inflamed, it is called tonsillitis. This is a painful condition, because foreign substances or toxins of microorganisms are deposited in these tonsils, due to which this condition is more painful.
When the tonsils become inflamed, they appear swollen, red, and tender.
This area also has a gray and white color appearance.
Due to infection in the tonsils, swelling is also seen in the lymph nodes around the neck.
Tonsillitis is generally seen in two types.
Acute Tonsillitis..
In this condition, symptoms of infection are seen in a very short period of time and infection occurs quickly.
The main cause of it is bacteria and viruses.
Chronic Tonsillitis..
If episodes of acute tonsillitis are seen repeatedly, this condition converts into chronic tonsillitis due to long-term untreated.
Group A beta streptococcal microorganism is responsible for the main cause of tonsillitis.
Etiology/causes of tonsillitis:
Tonsillitis is mainly seen due to bacterial and viral infections. In which tonsillitis is mainly seen due to group A streptococcus bacteria. Common viruses include influenza virus, herpes simplex virus, cytomegalovirus, adenovirus, and Epstein-Barr virus.
Clinical manifestation/sign & symptoms of tonsillitis:
Swelling in the throat
Sore throat and throat pain
White and yellow patches on the tonsils,
Dysphagia (difficulty in swallowing),
Swelling in the lymph nodes in the neck
Referred pain in the ear (ipsilateral earache),
Bad breath and foul smelling (halitosis),
Fever,
Headache,
Chills,
Malas,
Discomfort,
Fatigue,
Sore throat,
Pain.
Difficulty in swallowing,
Fever,
Feeling cold,
Malas,
Redness.
Irritation,
Discomfort,
Sore throat.
Earache.
Fever.
Headache.
Bad breath.
Muscle pain.
Stiff throat.
Swelling in the lymph nodes of the neck.
Swelling of the eyes, mouth, and throat.
In severe cases, nausea.
Trouble sleeping.
Loss of appetite.
Vomiting.
Stomach pain.
Constipation.
Difficulty opening the mouth.
Headache.
Irritation and discomfort.
Diagnostic evaluation of Tonsilitis:
History collection
Physical examination
Complete blood count
Throat culture (rapid strip test)
Medical management of tonsillitis:
Antibiotics:
If tonsillitis is caused by a bacterial infection, antibiotic drugs should be given to treat it.
Pain relievers (analgesics):
Provide analgesic medicine to relieve pain.
Corticosteroid:
In selected cases, corticosteroid drugs should be given to reduce inflammation.
Antipyretics:
Use antipyretic drugs to reduce fever.
Fluids:
Provide the patient with plenty of fluids. This can prevent dehydration.
Rest:
Provide adequate rest to the patient.
Surgical management of tonsillitis:
Tonsillectomy:
Tonsillectomy is performed in patients with recurrent or chronic tonsillitis, i.e. the tonsils are surgically removed.
Nursing management of Tonsilitis:
Ibuprofen is specifically given as an analgesic to relieve pain for the management of this condition. It also reduces pain, inflammation and swelling.
Antibiotic therapy is given to treat this condition.
The patient should be advised to drink plenty of fluids and eat green leafy vegetables and fruits.
Medications such as aspirin and acetaminophen can be given to the patient to relieve throat pain and inflammation.
The patient should be advised to rest especially in this condition.
Ask him to avoid any irritating substances.
Advise him to gargle with warm water by adding salt to warm water.
Some herbal and home remedies can also be prescribed to the patient to get relief from this condition, such as galsemium.
In cases of chronic tonsillitis, tonsils are removed by surgery. Special peri-operative care should be taken for these patients.
After the operation, the patient should be advised to rest, avoid physical activity as much as possible and refrain from going out. Precautions are especially taken for children.
After the operation, a liquid diet should be given for some time to reduce the pain and then a semi-solid diet can be started gradually. Spicy food should be avoided and hard food should also be avoided.
Even after the operation, the patient complains of pain for some time. To remove that complaint, advise him to take pain relief medicine.
Advising the patient to use an ice collar after a particular operation, in which putting ice in a bag and placing that bag on the side of the neck provides great relief to the patient and also reduces the bleeding tendency.
After the operation, the patient also complains of bleeding. As soon as this bleeding is noticed, he is placed in an upright position and an ice collar is applied to his neck. And immediate hospitalization is also advised.
Complication of tonsilitis
Peritonsillar abscess is seen as a complication of tonsillitis.
Peritonsillar abscess is also known as ‘Quency’.
In which pus collection is seen in the peritonsillar space.
c. Tracheostomy
Tracheos=trachea
Otomy=opening
In tracheostomy, an artificial opening is made in the trachea. And a tube is inserted through this opening. And oxygen is artificially given to the patient. Tracheostomy is done to keep the patient’s airway patent.
Classification: Tracheostomy is classified into types based on the situation:=
1) According to situation:
A)In emergency: In this, tracheostomy is done to relieve respiratory distress when the patient is in respiratory distress.
B)Prophylactic: In this, it is done when the patient is in mild respiratory distress so that the patient’s condition does not worsen severely.
2)According to duration:
A)Temporary: In this, an opening is made in the trachea for a short time.
B) Permanent: In this, an opening is made in the trachea for life. To keep the airway patent.
3) According to Incision:
A) High: In this, the incision is placed above the isthmus of the thyroid gland.
B) Low: In this, the incision is placed below the isthmus of the thyroid gland.
Indication:
1) If there is any obstruction of the air passage due to any tumor.
2) If there is stenosis or swelling in the trachea and larynx.
3) If there is any foreign body in the trachea.
4) If there is any unconscious patient.
5) If there is any patient who is in respiratory distress, it is done to keep the airway patent.
6) Tracheostomy is done when the patient has undergone mouth or neck surgery.
7) Tracheostomy is done when the patient has trauma to the larynx and trachea or is paralyzed.
8) It is done when the patient has undergone any radiation therapy.
9) Tracheostomy is done when the patient has difficulty breathing for a long time.
10) Tracheostomy is done when the patient has accumulation of secretion in the lower respiratory tract.
11) It is done when the patient is intubated for a long time after the operation.
12) It is done to provide oxygen from outside when the patient is not able to breathe naturally.
13) It is done when there is any kind of injury to the airway.
Complications:
1) Ventilation is reduced due to the insertion of a tracheobronchial tube.
2) The tube may come out suddenly when the patient is coughing, sneezing, and suctioning.
3) Lower respiratory tract infection occurs.
4) Infection occurs in the area where the tube is inserted.
5) There is also a chance of pulmonary infection.
6) There is also a chance of tracheoesophageal fistula.
7) Prolonged suctioning can cause hypoxia and cardiac arrest.
8) Hemorrhage occurs at the tracheostomy site and can also enter the respiratory tract.
9) The patient also gets choked because food and water also enter.
10) Injury occurs in the wall of the trachea when rough handling is done.
General instruction:
1) Always keep in mind that tracheostomy is an emergency procedure so do not waste time.
2) Maintain strict aseptic technique before and after tracheostomy.
3) The tracheostomy tube should be of proper size and length.
4) Clear all doubts of the patient and his/her relatives and explain the procedure.
5) Closely monitor the patient before and after the procedure.
5) Nursing responsibilities :=
1) Monitor and observe the patient closely.
2) Do not leave the patient alone for the first 48 hours.
3) Check if the patient is having difficulty breathing.
4) Watch the patient to make sure that the tube does not come out.
5) Keep the instrument ready when the tube comes out, as follows:
6) Keep the suction catheter ready.
7) Maintain aseptic technique.
8) Give the patient a fowler position.
9) Do not attend the patient if any person has a respiratory infection.
10) Check if the patient has any complications.
11) Inspire the patient or use a humidifier or filter.
12) Maintain the patient’s proper fluid intake and electrolyte balance.
13) Give the patient proper medications.
14) Pay close attention to the patient’s oral or VT.
15) Dress appropriately.
16) Provide the patient with a comfortable environment to work in.
17) Answer all questions from the patient and their relatives.
d. Chemotherapy
Chemotherapy is a therapy to kill abnormal cancer cells in a cancer tumor in the body. Chemotherapy is a treatment to destroy cancer cells with chemical agents.
This chemical agent is a treatment to prevent the reproduction and cellular function of abnormal cancer cells by disturbing them and preventing them from multiplying and spreading from one place to another.
This therapy is sometimes used along with radiation therapy.
This therapy is specifically given to reduce the size of the tumor before surgery.
This therapy first affects the cancer cells that have spread throughout the system in every part of the body and finally acts to reduce its size in the main place where the cancer is located.
The chemical agents given in this therapy are very important in destroying the malignant cancer cells and using this agent in combination with other agents gives very effective results.
Detailed information about chemotherapy (Chemotherapy in Detail):
How chemotherapy works (How Chemotherapy Works):
Chemotherapy treatment is given in the body through injection or oral medicine. This treatment spreads throughout the body through the blood circulation and destroys fast-growing cancer cells. Chemotherapy effectively reduces the size of the cancer tumor and destroys cells that have spread to other parts.
Different types of chemotherapy (Types of Chemotherapy):
Adjuvant Therapy:
- It is given after surgery to remove the main tumor, so that the remaining cancer cells are destroyed.
Neoadjuvant Therapy:
- It is given before surgery, so that the size of the tumor is reduced and it becomes easier to remove it.
Metastatic Therapy:
- This method is used when the cancer has spread, which destroys the tumor and prevents its spread.
Chemotherapy Treatment (Chemotherapy Drugs): Several types of treatment are used for chemotherapy. Some of the common treatments include cyclophosphamide, methotrexate, doxorubicin, and paclitaxel. Treatment is given alone or as a combination therapy.
Side Effects of Chemotherapy: Chemotherapy treatment is very powerful and it destroys rapidly growing cells. This can cause some side effects, such as:
Myelo suppression: Most chemotherapy drugs suppress the bone marrow, which reduces the production of blood cells.
Fatigue: The cause of this is unknown, but anemia, weight loss, and sleep patterns are seen due to disturbed sleep patterns.
Nausea and vomiting: These are the most common side effects
Mouth infection occurs due to cytotoxic drugs, which is called stomatitis.
Cardio toxicity
Alopecia, which means hair loss. Changes in taste and smell are seen.
Leukemia
Skin changes: In which hyperpigmentation, infection, disheveled nail coloration, ulcers, and photosensitivity are seen.
Pulmonary toxicity
Diarrhea and constipation, loss of appetite.
Renal toxicity: In which nephrotoxicity and renal failure are seen.
Neuro toxicity: In which CNS damage and peripheral nerve damage are seen.
Testicular and ovarian function is altered.
Weakness, fatigue, and weight loss occur.
Nursing Care of Patient During Chemotherapy:
Nursing management of the patient during chemotherapy should be done very carefully. Which includes the following points.
Before starting chemotherapy, it is necessary to completely review any patient. In which the description of the drug, what type of drug it is, what agent it is, what is its dosage, what is its route of administration, all this information needs to be reviewed.
It is necessary to identify the patient who is to be given chemotherapy.
Assessing the patient and checking his blood reports to monitor whether he has any kind of problem is very important before starting chemotherapy.
It is especially important to review the patient’s anxiety level and psychological status. Explain all the processes to him so that his anxiety can be removed.
After starting chemotherapy, the patient will see some side effects, which should be explained and prepared in advance.
Chemotherapy agents are given in very specific doses and after taking all precautions.
It is necessary to take great care while preparing medicine and medicine for chemotherapy patients.
Any disposable items left after giving the dose of medicine or unused drug should be properly discarded.
If any medicine is spilled while giving chemotherapy to the patient, it is necessary to manage the spill properly.
It is necessary to take steps to protect the patient and the staff, for this, precautions should be taken to ensure that the medicine does not spill and does not fall on the skin.
While preparing this chemotherapeutic agent for the patient, the staff should take complete precautions. Special care should be taken to ensure that the medicine does not come into contact with the staff through inhalation.
After giving chemotherapy to a patient, all the details should be recorded and reported systematically. Like the name of the chemical agent, dose, route, time, premedication, postmedication, if there is any complaint, it is necessary to document everything properly.
Post-Chemotherapy Care:
Post-chemotherapy care requires the doctor’s comfort and advice. Lifestyle changes such as relaxation techniques, exercise, and maintaining mental health are essential.
Chemotherapy is a highly effective and necessary treatment that can improve the lives of cancer patients.
e. Spinal deformities
Introduction:
Spinal deformities are conditions in which there is an unusual bend, crookedness, or angularity in the natural alignment of the spine, or vertebral column. There are generally three types of natural curves in the spine – cervical, thoracic, and lumbar. When these curves become excessive or diminished, or the spine becomes sideways, it is called a deformity. This condition can affect not only the postural but also the neurological, respiratory, cardiovascular, and psychological systems.
Main types of Spinal Deformities-:
- Scoliosis:
Scoliosis is a deformity in which the spine curves sideways and forms an ‘S’ or ‘C’ shape. It can manifest as unbalanced shoulder and hip height, pelvic tilt, and rib hump. This condition is especially common in adolescent patients and is known as idiopathic scoliosis.
- Kyphosis:
Kyphosis is a deformity caused by a deep forward curve in the thoracic spine. Normally, there is a curve of 20-45 degrees in the thoracic region, but when it increases to 50 degrees or more, it is considered pathological. The patient may have a hunchback appearance, back pain, and respiratory distress.
3.Lordosis:
Lordosis is an excessive inward curve in the lumbar region, also known as a hollow back. The patient appears to have a rounded back and a forward-thrust pelvis. The main cause may be muscular dystrophy, obesity, or herniated discs.
Etiology of Spinal Deformities:
Congenital: Congenital bone deformity
Neuromuscular: Neuro-muscular conditions such as cerebral palsy, muscular dystrophy
Degenerative: Age-related changes such as osteoarthritis
Traumatic: Due to accident or injury
Infectious & Tumoral: Tuberculosis or metastatic cancer
Idiopathic: Deformity that develops without a clear cause
Clinical Features:
Chronic pain in the back, neck or waist
Difficulty walking or balance
One shoulder or hip appearing higher
Postural imbalance
Respiratory congestion or difficulty breathing
Nerve Symptoms of impairment such as numbness or tingling sensation
Diagnosis:
Physical Examination: Adam’s Forward Bend Test
Radiograph (X-ray): Cobb Angle to measure the curve angle
MRI: To check for nerve involvement
CT Scan: Assessment of bone disc deformity
Pulmonary Function Test: To measure respiratory impact
Management and Treatment:
- Conservative:
Orthotic brace: Given in teenage patients to prevent growth
Physiotherapy: For posture and back muscle strengthening
Analgesics and Analgesics & Anti-inflammatory Drugs: For pain management
2.Surgical Treatment:
Spinal Fusion: To achieve stability by fusing two or more vertebrae together
Pedicle Screw Instrumentation: To provide mechanical support to the spine
Osteotomy: To correct abnormal bone spurs
Complications:
Spinal cord injury
Paralysis
Infection
Hemorrhage
Circulatory and Respiratory Disturbance
Postural and muscular Abnormalities
Spinal deformities It is not just a question of physical appearance, but can have serious neurological and musculoskeletal effects. It is very important to make an individual diagnosis and treatment plan for each patient. With the help of surgical and non-surgical treatment options, the patient’s lifestyle can be improved and in the long run, they can be enabled to lead a normal life.
Q.5 Write Definition (ANY SIX) .6×2=12
a. Mastoiditis
Mastoiditis is a serious bacterial infection that occurs in the air cells of the mastoid bone. This bone is part of the skull and is located behind the ear. Mastoiditis usually develops after otitis media, or middle ear infection, when the infection spreads from the middle ear to the mastoid bone. In this condition, the patient experiences signs such as pain behind the ear, swelling, redness, fever, headache, hearing loss, and sometimes ear discharge. If not treated promptly, the infection can spread to the facial nerve, meninges, or brain, leading to life-threatening complications. Medical management of mastoiditis involves high-dose intravenous antibiotics and, when necessary, surgical intervention such as mastoidectomy.
b Epistaxis
Epistaxis means nose bleed or nasal hemorrhage Bleeding from the nostril or nasal cavity due to rupture of vessels in any area of the mucous membrane in the nose is known as epistaxis.
OR
Epistaxis means nose bleed or nasal hemorrhage Bleeding from the nostril or nasal cavity due to rupture of vessels in any area of the mucous membrane in the nose is known as epistaxis.
Epistaxis is also known as nose bleed. This is a condition in which active bleeding occurs from the nostril, nasal cavity or nasopharynx. This occurs when the blood vessels inside the nose are damaged or injured. The process of bleeding from the front or back of the nose is called nosebleed or epistaxis.
c. Ectropion
Ectropion is an abnormal position of the lower eyelid in which the eyelid turns outward, exposing the conjunctiva of the eye and leading to problems such as dryness, irritation, watery eyes, and recurrent infections. This condition is usually caused by aging, paralysis, trauma, scarring, or surgical complications in elderly patients. Treatment for ectropion depends on its cause and severity, and may include lubricant eye drops, temporary taping, or corrective surgery.
d. Retinal detachment
1)Definition: Retinal detachment is an eye disorder in which the pigmented cells of the retina detach from the sensor cells. If not treated properly, the entire retinal detachment occurs, causing vision loss and blindness.
2)Types: a)Rhegmantogeneous,
B)Tractional
C)Exudative
D)Both rhegmantogeneous and tractional.
1) Regmantogenious: In this type of retinal detachment, when there is a hole in the small wall of the retina, the vitreous humor fluid leaks between the sensory rods and cones, causing the epithelial wall to separate and causing retinal detachment.
2)Tractional: In this, when the retinal rod and cone separate from the pigmented epithelium due to tumor or injury and retinal detachment occurs.
3)Exudative: In this, when there is accumulation of fluid due to any type of infection or inflammation and due to this detachment of the retina occurs, the epithelium is separated from the surface.
4)Rhegmantogeneous and Tractional both: In this, retinal detachment occurs due to the formation of a hole or due to both tumor and injury.
e. Chancroid
This is a sexually transmitted disease caused by the gram-negative Haemophilus duke bacilli. It causes papules (fluid-filled blisters) and pustules (pus-filled blisters) to form and then increase in number, along with painful, irregular, deep genital ulcers. It is often associated with lymphadenopathy and HIV.
f. Phelebotomy-
Phlebotomy is a medical procedure in which an opening is made in a vein. In which a needle is inserted into the vein and blood is removed.
This procedure is mainly done for diagnostic purposes, treatment (therapeutic purposes), blood donation, or blood collection.
It is also called venipuncture in another language.
In this, blood is removed using a needle.
This procedure is used to diagnose and treat many medical conditions.
There are two types: vein puncture and capillary puncture
g. Incubation period
The period between exposure to an infectious agent (bacteria, virus) and the first signs and symptoms are seen is known as the incubation period. For example:-
Influenza: 1-4 days
Covid 19: 2-14 days
Chickenpox: 10-21 days
h.Mydriatics
Mydriatics are pharmacological agents that increase the diameter of the pupil, i.e., dilate the pupil. These drugs are commonly used to properly visualize the fundus and retina during an ophthalmic examination, or during a surgical procedure. Some mydriatics are intended for temporary pupillary dilation, while in some cases the effect is long-lasting. The main mydriatic drugs include atropine, tropicamide, and phenylephrine. They must be used with caution for safety and efficacy.
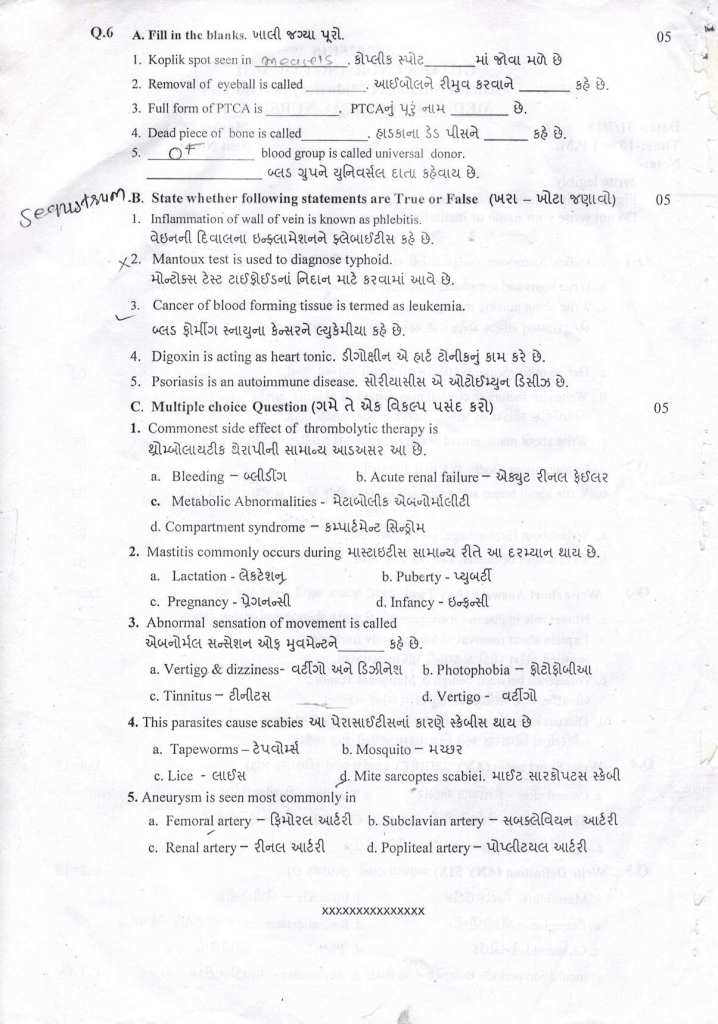
Q : 6 A. Fill in the blanks. 05
1.Koplik spot seen in ______ .✅ Measles
2.Removal of eyeball is called ______ . ✅ Enucleation
3.Full form of PTCA is_______ . ✅ Percutaneous Transluminal Coronary Angioplasty
4.Dead piece of bone is called ______ .✅ Sequestrum
5.______ blood group is called universal donor.✅ O negative
B. State whether following statements are True or False 05
1.Inflammation of wall of vein is known as phlebitis. વે✅ True
✔️ Phlebitis is indeed the inflammation of a vein wall, usually due to infection, trauma, or IV infusion.
2.Mantoux test is used to diagnose typhoid. ❌ False
✖️ Mantoux Test is used for diagnosing Tuberculosis (TB), not Typhoid.
🧪 For Typhoid, Widal test is commonly used.
3 Cancer of blood forming tissue is termed as leukemia. ✅ True
✔️ Leukemia is a malignancy of blood-forming tissues, especially white blood cells.
4.Digoxin is acting as heart tonic. ✅ True
✔️ Digoxin is a cardiac glycoside that improves heart contraction and is often called a “heart tonic” in clinical terms for congestive heart failure and arrhythmias.
5.Psoriasis is an autoimmune disease. ✅ True
✔️ Psoriasis is a chronic autoimmune skin disease that speeds up skin cell growth, leading to scaly and inflamed skin patches.
C. Multiple choice Question 05
1.Commonest side effect of thrombolytic therapy is
a.Bleeding –
b. Acute renal failure –
c.Metabolic Abnormalities
d. Compartment syndrome –
✅ a. Bleeding
✔️ Thrombolytics dissolve blood clots, which increases the risk of internal or external bleeding.
🔍 Explanation: Most feared complication due to their clot-dissolving action.
➡️ Correct Answer: a. Bleeding –
2.Mastitis commonly occurs during.
a Lactation –
b. Puberty
c. Pregnancy –
d. Infancy –
✅ a. Lactation –
✔️ Mastitis is an infection of the breast tissue, most common during breastfeeding (especially in first few weeks postpartum).
➡️ Correct Answer: a. Lactation –
3.Abnormal sensation of movement is called.
a. Vertigo & dizziness –
b. Photophobia
c. Tinnitus –
d. Vertigo –
✅ d. Vertigo –
✔️ Vertigo is the sensation of spinning or abnormal movement when no movement is happening.
➡️ Correct Answer: d. Vertigo –
4.This parasites cause scabies.
a. Tapeworms –
b. Mosquito –
c. Lice –
d. Mite sarcoptes scabici –
✅ d. Mite Sarcoptes scabiei –
✔️ Scabies is caused by a tiny mite called Sarcoptes scabiei, which burrows into the skin.
➡️ Correct Answer: d. Mite Sarcoptes scabiei –
5.Aneurysm is seen most commonly in…
a. Femoral artery-
b. Subclavian artery –
c. Renal artery –
d. Popliteal artery –
✅ d. Popliteal artery –
✔️ While aortic aneurysms are most common, popliteal artery aneurysms are the most common peripheral arterial aneurysm.Aneurysms are most commonly seen in the popliteal artery (after the aorta).
➡️ Correct Answer: d. Popliteal artery –