ENGLISH-MEDICAL SURGICAL NURSING : 1 PAPER SOLUTION 28/03/2022 -UPLOAD NO.12
28/03/2022 – PAPER SOLUTION NO.12
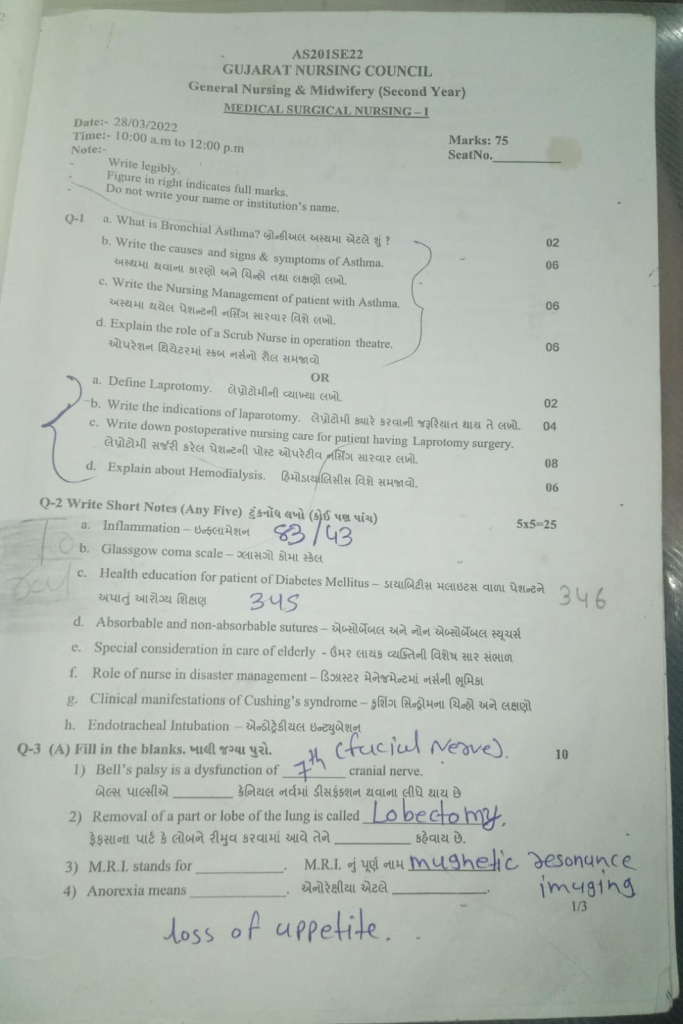
Q-1
a. What is Bronchial Asthma? What is bronchial asthma? 02
Bronchial asthma:
Bronchial asthma is a chronic inflammatory respiratory disorder. In which the airways (respiratory tract) become hyperresponsive to certain stimuli, due to which the airways become inflamed and narrowed, and due to mucus production, the airways become constricted and obstruction is seen in them. Asthma is reversible.
Due to some type of etiological factor, airway hyperresponsiveness occurs.
Due to this, inflammation is seen in the airways. Due to which hypersecretion of mucus, contraction of airway muscles and swelling of bronchial membranes are seen, due to which airways become narrowed. Due to this, cough, chest tightness, shortness of breath and wheezing sound are seen.
b. Write the causes and signs & symptoms of Asthma. Write the causes and signs and symptoms of asthma. 06
Etiology/causes of Bronchial asthma:
- Genetic factors,
- Family history,
- Respiratory infection
- Environmental factors: Exposure to allergens, air pollutants (dust, chemicals)
- Occupational factors,
- Hyperreactive airways
- Due to inhalation of certain types of irritant materials, such as cigarette smoking, strong odors of shops, and perfumes.
- Due to respiratory tract infection.
Clinical manifestation/Sign and symptoms of the Bronchial asthma:
- Dyspnea,
- Wheezing,
- Coughing with or without expectoration of sputum,
- Chronic cough,
- Shortness of breath,
- Tight feeling in chest,
- Increase respiratory rate,
- Child is pale, irritable, blurred vision,
- Chest pain,
- Breath sound is diminished,
- Headache,
- Muscle twitching,
- Confusion,
- Coma.
c. Write the Nursing Management of patient with Asthma. Write the nursing management of patient with asthma. 06
Impaired gas exchange related to altered oxygen supply, obstruction of airway
Improve gas exchange
- Monitor vital signs.
- Assess respiratory rate, rhythm and breathing pattern.
- Assess breath sounds and chest movement.
- Monitor pulse oximetry and arterial blood gas values.
- Provide the patient with a Fowler position and restrict his/her activity.
- Explain and encourage the patient about deep breathing and cuffing exercises.
- Provide the patient with knowledge about pursed lip breathing and diaphragmatic breathing.
- Encourage the patient to expectorate phlegm if secretions are present.
- If the SpO2 level is low, provide oxygen therapy.
- Provide nebulization to the patient.
- Administer the medicine (bronchodilator) prescribed by the doctor.
- Maintain records and reports.
Ineffective airway clearance related to obstruction from narrowed lumen Maintain patent airway (Maintain airway patent)
- Monitor vital signs.
- Assess respiratory rate, rhythm and breathing pattern.
- Assess breath sounds and chest movement.
- Monitor pulse oximetry and arterial blood gas values.
- Provide the patient with a Fowler position and restrict his activity.
- Explain and encourage the patient about deep breathing and cuffing exercises.
- Provide knowledge about pursed lip breathing and diaphragmatic breathing to the patient.
- Encourage the patient to expectorate phlegm if secretions are present.
- Provide oxygen therapy if SpO2 level is low.
- Provide nebulization to the patient.
- Administer prescribed medicine (bronchodilator) by the doctor.
- Maintain records and reports.
Ineffective breathing pattern related to bronchospasm Improving breathing pattern (Improving breathing pattern)
- Monitor vital signs.
- Assess respiratory rate, rhythm and breathing pattern.
- Assess breath sounds and chest movement.
- Monitor pulse oximetry and arterial blood gas values.
- Provide the patient with a Fowler position and restrict his/her activity.
- Explain and encourage the patient about deep breathing and cuffing exercises.
- Provide knowledge about pursed lip breathing and diaphragmatic breathing to the patient.
- Encourage the patient to expectorate phlegm if secretions are present.
- Provide oxygen therapy if the SpO2 level is low.
- Provide nebulization to the patient.
- Administer prescribed medicine (bronchodilator) by the doctor.
- Maintain records and reports.
Anxiety related to disease condition, hospitalization Reduce anxiety
- Assess the patient’s condition.
- Pay attention to the patient’s psychological needs and listen carefully to the patient.
- Encourage the patient to express his/her feelings, discomfort, and anxiety.
- To resolve all the doubts and queries of the patient.
- To provide knowledge to the patient about his condition and treatment so that his anxiety is removed and the patient becomes confident.
- To provide psychological support to the patient.
- To provide mind diversionary therapy and recreational therapy to the patient.
Activity intolerance related to fatigue, Dyspnea Increase activity level (increase activity level)
- Assess the patient’s condition.
- Check the patient’s activity level.
- Provide bed rest to the patient initially.
- Then gradually encourage the patient to do range of motion exercises.
- Assist the patient with his/her activity.
- Provide the patient with rest between 2 activities.
- Check whether the patient has any breathing difficulty during the activity.
- If breathing difficulty is found, stop the patient’s activity and provide rest.
d. Explain the role of a scrub nurse in operation theatre. Explain the role of a scrub nurse in an operation theatre.06
Responsibilities of a scrub nurse:-
- Welcoming patient
- Preoperative nursing assessment
- Checklist before scrubbing
- Scrubbing in
- Assembling instruments, counting before surgery
1)Welcoming patient:-
- Welcoming the patient
- Introducing yourself
- Getting the patient’s personal information
- Ask if the patient needs anything or help
- Give information about the surrounding environment
- Remove the patient’s jewelry
2)Preoperative nursing assessment:-
- Ask about the patient’s age, any allergies, and any infections present
- Check the patient’s vital signs
- Ask about any medications being taken, such as heparin, warfarin,
- Check nutritional status
- Check all reports of the patient To do
3) Checklist before scrubbing
- Check the patient’s consent
- Confirm about the surgical procedure
- Check instruments
- Check supplies
4) SCRUBBING IN”:-
Wash hands and arms thoroughly with antibacterial soap as usual. Then wear sterile mask, cap, gown and gloves so that infection does not occur when coming into contact with the patient’s body during surgery.
5) ASSEMBLE INSTRUMENTS : –
- Open the inner sterile set and place the sterile instruments on the myo tray and trolley Place
- Count all
- Place the surgical blade
- Prepare the sutures
6)ASSISTANCE DURING SURGERY:-
- Provide the surgeon with the necessary equipment in the correct position and safely
- Insert the scalpel into the kidney dish
- Keep the skin knife away from the working area
7) Assistance during surgery:-
- If necessary, retract the tissue
- Remove the artery tip as directed by the surgeon
- Cut sutures with scissors and help with suturing
- Assist with cautery
- Keep instruments, sutures, sponges ready before the surgeon asks for them
- Keep the sterile field clean
- Maintain strict aseptic technique
- Reduce air and if sneezing or coughing, go to the side
8)End of procedure:-
- When the surgeon completes the operation, count the sponges, sharp instruments
- Do wound dressing with non-touch technique
- Cover soiled instruments before placing in autoclave To do
- Remove gown and gloves.
OR
a. Define Laprotomy. Write the definition of laparotomy.02
Definition:
A laparotomy is a surgical procedure in which an incision is made in the abdominal wall to directly view the internal organs within the abdomen for examination, diagnosis, or treatment. This procedure is usually performed when the cause of an abdominal condition is unclear, and other diagnostic methods are not providing adequate information.
There are some cases of laparotomy in which any growth, infection, bleeding or organ damage is diagnosed through this incision and immediate treatment is given.
b. Write the indications of laparotomy. Write when laparotomy is required.04
Main Indications of Laparotomy:
1. Abdominal Trauma:
If there is a severe injury to the abdomen such as blunt trauma or penetrating injury, then laparotomy is necessary to check for internal bleeding and organ damage.
2. Unexplained Abdominal Pain:
When all the scans and tests fail to find a specific cause for the pain, a laparotomy is performed for live observation.
3. Internal Bleeding:
When bleeding occurs inside the abdomen, a laparotomy may be necessary to identify the source and control it.
4. Infection or Abscess:
Surgery may be necessary when there is a pus-filled area inside the abdomen, i.e. an abscess, and it is not clearing up with medication.
5. Diagnosis and Removal of Tumor or Mass:
When a growth, tumor or suspicious mass is found inside the abdomen, a laparotomy is performed for its biopsy or removal.
6. Gynecological Indications:
Such as ruptured fallopian tube (Rupture Ectopic Pregnancy), ovarian cyst or uterine fibroid.
7. For diagnostic purposes (Exploratory Purpose):
Exploratory laparotomy is performed to look inside when the cause of the disease is not fully known.
8. Bowel Obstruction or Perforation:
In cases of intestinal blockage or rupture, immediate laparotomy is necessary.
Laparotomy is a surgical method used when the diagnosis of a disease is difficult or direct access is required for treatment. It can often be a lifesaving procedure in emergency conditions.
c. Write down postoperative nursing care for patient having Laprotomy surgery. Write the post-operative nursing care of a patient who has undergone laparotomy surgery.08
1. Regular monitoring of vital signs
It is necessary to regularly check blood pressure, pulse rate, respiratory rate and body temperature to assess the general condition of the patient. This monitoring helps identify early signs of possible complications such as infection, hemorrhage, or shock.
2. Monitoring and Care of the Incision Site
Daily monitoring of the surgical incision site for signs of infection such as redness, swelling, discharge, and pain is necessary. Dressing should be changed regularly using sterile technique.
3. Positioning and Mobilization of the Patient:
Initially keep the patient in Fowler’s position. Start active or passive mobilization within 24 hours after surgery to prevent complications like thrombosis and atelectasis.
4. Pain Management:
Give the patient analgesics according to the pain scale. Relaxation techniques should also be adopted to reduce pain.
5. Dietary Management:
A clear liquid diet should be given initially. If there are no symptoms of nausea, vomiting or abdominal distension, then gradually move towards a soft diet.
6.Respiratory Care:
The patient should undergo Incentive Spirometry and Deep Breathing Exercise to prevent pulmonary complications.
7.Urinary and Bowel Elimination Monitoring
Monitor urine output – low output may be a sign of worsening kidney function. Watch bowel movement patterns – delayed peristalsis may occur or bowel paralysis may occur.
8. Intravenous Fluid and Medication Administration:
Give the patient IV fluids to prevent dehydration and electrolyte imbalance. Antibiotics should be given on time to prevent infection.
9. Psychological Support:
The patient may experience depression, anxiety, or fear after surgery. Deal with the patient empathetically and provide emotional support.
10. Discharge Planning and Home Care Instruction:
Give the patient a clear understanding of incision care, medication regimen, follow-up appointments, and when to seek immediate medical attention before discharge. Prepare an action plan for home care.
The aim of all this nursing care is to ensure the patient gets a speedy recovery, avoid complications and enable safe discharge.
d. Explain about Hemodialysis. Explain about Hemodialysis. 06
Definition:- Hemodialysis is a method of removing excess waste from the body in cases of renal failure, in which excess waste is removed from the blood.
After removing harmful substances, pure blood is returned to the patient’s body.
Purpose :-
- Removing excess waste from the patient’s body To do.
- To make the body’s buffer system positive
- To remove excess fluid from the body
- To reduce water retention
- To prevent other complications
- To maintain the level of electrolytes in the body
Indications:-
- Acute Renal Failure
- Chronic Renal Failure
- Uremia
- Renal Encephalopathy
- Severe Edema
- Metabolic Acidosis
Procedure :-
Hemodialysis involves a machine (dialyzer) for purifying blood, in which blood is taken from one of the vessels of the patient’s body and sent to the dialyzer. The waste products in the blood are filtered and then pure blood is made, which is injected into the patient through other vessels.
In hemodialysis, a fistula is made. From where impure blood is taken out and pure blood is injected inside.
This fistula Can be made on wrist, arm and neck.
Complication:-
- Dehydration
- Hypovolemia
- Hypotension
- Hypovolemic shock
- Septicemia
- Death
Care during hemodialysis:-
- Check the patient’s weight and Record it.
- Written consent is obtained from the patient for dialysis.
- Explain the dialysis procedure to the patient so that they are less anxious
- Give the patient a comfortable position
- Ask the patient to stop taking antihypertensive and vasodilator medications before dialysis, if any, because dialysis causes hypotension
- Check vital signs and To monitor
- If there is any problem during dialysis, the patient should be asked about it and if necessary, the doctor should be informed immediately.
- Keep checking the patient’s fistula site regularly because due to the use of heparin during the procedure, the clotting process is slowed down and bleeding can occur The possibility increases.
- All emergency medicines should be kept ready with the patient
- The patient should be given the necessary medicines.
- After the completion of hemodialysis, the patient’s weight should be checked again
- After hemodialysis, the patient should Necessary medicines should be given.
Q-2 Write Short Notes (Any Five) Write short notes (any five) 5×5 = 25
a. Inflammation – Inflammation
Inflammation is a protective process in which the body’s white blood cells and chemical mediators (histamine/prostaglandin) that work to protect the body from viruses, bacteria, parasites, and other pathogens coming from outside and protect it from any type of irritant chemical is called inflammation. Inflammation is a good protective mechanism (physiology) of the body. And inflammation is a localized protective reaction of tissues in the body that occurs when any irritation, injury, or infection occurs in the body. And then certain types of characteristics are seen in the body such as pain, redness, and often the function of the body organ is also lost, which is called inflammation.
[ cardinal sign ( important sign) of inflammation is pain, Redness, warmth, swelling, exudate ( pus)].
type of inflammation.Type of inflammation
When inflammation occurs in the body, the body’s white blood cells release chemicals into the blood.
The release of these chemicals to remove foreign substances from the body increases blood flow in the body and due to this redness and warmth are seen and certain types of chemicals leak into the tissues and due to this swelling is seen. Due to this swelling, nerves are stimulated and it is responsible for creating pain.
there are three types of inflammation (according to time duration)
1)Acute inflammation,
2)chronic inflammation,
3)subacute inflammation
1)Acute inflammation,
Acute inflammation is a condition in which local vascular exudative changes are observed and is called acute inflammation.
If a person has local vascular exudative changes and they last for less than two weeks (2 weeks or less than 2 weeks), then it is called acute inflammation.
2)chronic inflammation,
Chronic inflammation occurs when there is a long-term disease or pathogens remain in our body for a long time and it causes inflammation in the body or causes another disease condition, then it is called chronic inflammation and if acute inflammation is not treated, then it results in chronic inflammation for a long time.
Chronic inflammation is when an inflammation is present for more than 2 weeks or many months and many years.
3) Subacute inflammation
Subacute inflammation occurs during the period between acute and chronic inflammation. Subacute inflammation lasts from 2 weeks to 6 weeks and is called subacute inflammation.
b. Glasgow coma scale – Glasgow coma scale
# The patient’s level of consciousness is checked by the Glasgow coma scale.
There are mainly three components assessed in GCS.
1) Eye opening
2) Verbal Response
3) Motor Response Response)
••>
#1) Eye opening
There are a total of four scores in eye opening.
1) Spontaneous (= In this, the patient opens and closes his/her eyes on his/her own) := { 4 }
2) To voice
( To voice:= In this, the patient opens and closes his/her eyes If asked and the patient follows it) := { 3 } ,
3) To pain
( To pain := In this, if the patient is pinched in the body and the patient makes an eye expression, then it):= { 2 }
4) No response
( No response := If there is no response from the patient) := { 1 }
#2) Verbal Response
Verbal The response has a total of five scores.
1) Oriented (= if the person is asked about time, place and person and the person gives the correct answer) := { 5 } ,
2) Confused (= if the patient is asked about time, place and person and the patient is confused):= { 4 } ,
3) Inappropriate word
( Inappropriate word:= If we ask the patient some question and the patient gives something else) := { 3 } ,
4) Incomprahensuve sound ( Incomprahensuve sound := If the patient is asked any question and he only makes sound through the mouth) := { 2 } ,
5) No response
( No response := If no response is given) := { 1 }
#3) Motor Response
Motor response has six main scores.
1) Obey command
( Obey command:= Whatever the patient is told to do, if the patient follows it properly) := { 6 } ,
2) Localised pain ( Localised pain:= If the patient is pinched and the patient provides a response) := { 5 } ,
3) Withdraw pain ( Withdraw pain:= If the patient is pinched and the patient tries to withdraw his hand) := { 4 } ,
4) flexion
( Flexion:= When any mid-area of the patient’s body is pressed and the patient’s body flexes):= { 3 } ,
5) Extention:= If any stimulus is provided, the patient’s body extends):= { 2 } ,
6) No response
( No response:= If the patient does not provide any response):= { 1 }
Thus, the Glasgow Coma Scale has a minimum score of 3 and a maximum score of 15.
# result:
# { 3 } score achieve:= Then the patient has severe neurological damage.
#{ 7 } score achieve:= Then the patient is in a comatose state.
#{ 8-12} score achieve:= Then the patient has moderate neurological damage.
#{ 13-14} score Achieve:= Then the patient has minor neurological damage.
#{ 15 } score Achieve:= Then the patient is fully conscious and oriented.
Thus the patient’s level of consciousness is assessed using the Glasgow Coma Scale.
c. Health education for patient of Diabetes Mellitus – Health education for patient of Diabetes Mellitus
Introduction:
Diabetes Mellitus is a chronic metabolic disorder, in which the body does not produce or use insulin properly, due to which the blood glucose level increases.
Major Points of Health Education:
Major Points of Health Education:
1.(Dietary Management):
- Eat small meals at regular times
- Avoid sugar and refined carbohydrates
- Eat high-fiber foods like vegetables, whole grains
- Avoid oily and fried foods
- Drink enough water and control the amount of fruits
- Eat more beans, lentils and non-starchy vegetables
2. Regular Exercise:
- Walk or cycle for at least 30 minutes every day
- Exercise Blood Lowers glucose levels and improves insulin function
- Brisk Walk is the best for diabetes control
- Exercise provides great benefits without changing the level of diet
3.Regular use of medication (Medication Adherence):
- Take medicine or insulin injection as prescribed by the doctor
- Do not skip medicine and take it on time
- Be aware of the side effects of medicine
- Ask a doctor before taking over-the-counter medications
4.Blood Sugar Monitoring:
- Check your blood sugar level regularly
- Keep a glucometer at home
- Symptoms of Hypoglycemia (Hypoglycemia) – Low sugar: shakiness, hunger, dizziness
- Symptoms of Hyperglycemia (Hyperglycemia) : High sugar: increased thirst, frequent urination, Fatigue
5.Foot Care:
- Diabetes can cause nerve damage and circulation problems
- Check your feet daily – look for cracked skin, infection or cuts
- Wash and dry your feet thoroughly
- Cut nails straight
- See a podiatrist if there are any changes
6. Stress Reduction & Lifestyle Management:
- Stress can increase the level of diabetes
- Yoga, Meditation, Climate Change or Adopting a Hobby
- Completely Avoid Smoking and Alcohol
- It is necessary to get enough sleep (7–8 hours)
7. Regular Checkups & Complication Prevention:
- Get HbA1c test done every 3 to 6 months
- For eyes – Diabetic Retinopathy Screening
- For kidneys – Urine Protein Test
- Foot pulse, nerve sensation and heart checkup are also necessary
- Get lipid profile and blood pressure checked
Health education is the main tool for a diabetes mellitus patient to lead a healthy life. Proper diet, exercise, adherence to medication, and self-awareness – all of these together give a person the opportunity to manage diabetes well and prevent long-term complications.
Educating patients and families empowers them and they can manage their disease better.
d. Absorbable and non-absorbable sutures.
(A) Absorbable Materials:
They are self-dissolving.
(1) Catgut :-
It is made from the intestine of sheep. The sutures and ligatures used are sterilized with gamma radiation and do not need to be removed.
Type of Catgut :-
- Plain Catgut :-
This is natural which is made from tendon and fascia. And this gets absorbed in 10 days.
- Chromic Catgut:-
This is natural which is made from tendon and fascia. On this, chromic salt is applied on the plain catgut. Due to which its strength is maintained and irritation in the tissue can be reduced. This is absorbed in 20 to 40 days.
2) Poly glycolic acid :- ( P.G.A.)
This is a synthetic catgut and is also absorbable.
3) Living suture :-
This is made from the patient’s own tissues which are made from muscles and tendons. It is used especially in hernioplasty
B) Non Absorbable sutures:-
These cannot be dissolved
(a) Silkworm gut:-
These are made from the saliva of the silkworm. Which is made in the form of thread. Which is kept up to 12 inches in length and has different thicknesses.
This is not a purple or pink thread and is used in skin sutures.
B) Nylon thread or mono- filament:-
This is similar to silkworm gut.
C)Linen thread or Poly- filament:-
It is made from cotton. It is made of linen. This is especially used in gastrointestinal surgery and comes in numbers 90, 60, 35 and 25.
D) Silk thread :-
This is made from silk. It is especially used in skin, vascular, ophthalmic and oral surgery. It is available in different types.
E) Metal wire :-
It is made of silicone metal
It is used for herniorrhaphy, prolapse rectum and orthopedic surgery and is available in different sizes.
c. Special consideration in care of elderly.Special consideration in care of elderly.
1) Promotion of Self Respect and Dignity:-
Some institutions or groups usually have some restrictions on personal choice and independence.
The feelings and emotions of the elderly should be respected.
While the staff makes positive efforts to develop good relationships with the patients and gain their personal respect and friendship.
By cultivating good relationships, a group can be controlled and difficult situations can also be made easier.
2) Promotion of Comfort:
Relaxation is necessary for physical and mental comfort. There are many factors that contribute to the comfort of the elderly such as skin care, care of bony structure, maintenance of temperature and fluid balance.
3) Safety:
Provide unpolished floors, good lighting, appropriate bed height, and proper walking aids
4) Daily Living Activities:-
Encourage the patient to do as much daily activity as possible so that complications like dehydration, thrombosis, pressure sores, contractures, and ulcers can be avoided.
5) Promotion of independence:-
Encourage the patient to take care of themselves as much as possible and ask them to make their own decisions.
6)Encourage mobility and movement
7) Tell the patient to take the necessary medicines and provide sufficient knowledge about those medicines such as side effects of the medicine, its use.
8) If the patient is in a state of rehabilitation, do it according to his condition.
Additional information:-
1.Skin care:-
- Use mild soap Should
- Bathing should be done once or twice a week
- Hair care and brushing every day
- Using moisturizers
- Nails should be kept short
- Using sunscreen, hat, long-sleeved clothing
- Hot water bottle Stay away from things like.
- On footwear Sufficient attention should be paid so that sores do not occur
- Avoiding sun stroke
2.Supporting Changes in Bones and Joints:-
- Light exercise should be done
- Take precautions to avoid falls
- Give a balanced diet that includes calcium and vitamin D supplements
- If the patient is in pain, monitor him and give him appropriate treatment
- Give the patient more time because it may take them longer to work.
3.Supporting Changes in Vision:-
- The patient Proper lighting should be provided
- If necessary, the patient should be assisted in choosing clothing
- Natural tear products should be used.
- The patient should be contacted directly.
4. Supporting Changes to Hearing:-
- When communicating, reduce the extra noise.
- Put yourself in the patient’s shoes so that the patient’s needs can be understood
- Before speaking, make sure that Whether the person is paying attention to you or not.
- Get checked by a doctor and if necessary, get the wax (mel) removed
- Arrange a hearing assessment and provide hearing aids if necessary.
5.Supporting Changes in Smell and Taste :-
- Attractive meals should be prepared in which food with a good smell should be offered. Make.
- Spoilt food should not be given to eat
6.Supporting Changes in the Cardiovascular System:-
- People get tired more easily due to cardiovascular changes, so they should be given more rest.
- According to healthcare professionals, regular blood pressure monitoring should be done
- If the person is unable to move on their own, they should be repositioned frequently
- Advise the patient to drink plenty of fluids and seek immediate medical help if dehydration is observed.
7.Supporting Changes in the Respiratory System:-
- Give oxygen therapy if necessary
8.Digestive Care:-
- Maintain oral hygiene
- Get proper treatment if tooth damage occurs
- Provide a comfortable environment for eating
- Feed high-fiber, high-protein foods with a variety of tastes and textures.
- Advise to drink more fluids
- Give calcium and vitamin D supplements to prevent osteoporosis
9.Supporting Changes in Elimination:-
- Maintain daily activities
- Plan for the bathroom when you have to go out
- Reduce caffeine intake
- Abundant fiber in fruits Should be taken
- Light exercise should be done
- Provide emotional support.
- Everything should be given according to the need.
10. Urinary Care:-
- Increase fluid intake
- Consume less fluid before bedtime
- Wear clothes that can be easily removed
- Use absorbent pads
11. Elderly care at home:-
- If there is a wound, it should be taken care of and its regular dressing should be done
- To monitor vital signs and Administer medicine on time.
- Manage if the patient is in pain or experiencing any kind of discomfort.
- Help the patient fulfill daily hygienic needs.
f. Role of nurse in disaster management- Role of nurse in disaster management.
Nurses role in disaster management. Role of Nurses in Disaster Management.
- The word disaster is derived from the word disaster or disastro. The meaning of which people of old times used to compare it with destruction. These people believed that disasters were caused by the unfavorable position of the planet or the earth or by an unfavorable condition created by God.
- According to the WHO, a disaster is any extraordinary event that occurs in any area of society that causes damage or loss, economic disturbances, loss of human life, or damage to health and health services.
- This A condition in which there is a very large amount of morbidity and mortality, and there is a lot of damage to property, roads, electrical lines and all infrastructure.
- A disaster is a dangerous condition that cannot be predicted, is unknown to everyone and occurs suddenly.
- At this time, the normal schedule of the person is disrupted, and this is a major change in the normal life of the person.
Role of the nurse in disaster management.
- The role of the nurse in disaster management is very important. In which it is especially necessary to take multi-disciplinary management steps as a nurse.
- During the time of disaster, the affected population has to be identified. They have to be given care and have to actively participate in disaster planning and management.
- During the time of disaster, the nurse plays a key role in maintaining a holistic care approach. In which she works for the integration of everyone.
- The nurse provides care to each person from physiological, psychological and spiritual aspects and she maintains collaboration between each team member.
- As a nurse, you have to identify what kind of event and what kind of damage there is during a disaster. Then, the main task is to identify the needs of the affected population.
- After arranging the needs in priority setting, setting objectives and goals helps in planning the resources and activities to fulfill the needs through a collaborative approach.
- During this time, you also help in contacting government, non-government and many agencies to be as helpful as possible.
- To work in disaster management, the nurse must be physically and psychologically prepared. He should have the necessary training and professional preparation to do the work.
- During this situation, the nurse tries to be helpful by maintaining communication between each team member.
- Nurses also play a very important role in disaster management plans and disaster prevention strategies in the community.
- For this, the necessary strategies and training programs should also be implemented. The people of the community can be made aware and informed about this matter through mock drills.
- An evaluation plan is also prepared in a disaster. According to which, precautions can be taken in planning and implementation after assessment.
- Efforts are also made to normalize the population affected by the disaster through rehabilitation programs.
- It is also important to keep in mind the basic needs of the affected persons at every stage of disaster planning and fulfill these needs.
g. Clinical manifestations of Cushing’s syndrome Symptoms and signs of Cushing’s syndrome.
- Clinical manifestation/sign and symptoms of cushing syndrome.
- Body weight increases.
- Upper body obesity and thin hands and feet.
- Patient’s face becomes round and red.
- Fatty buffalo hump in the neck region.
- Slow growth is also seen in the patient.
- Skin changes are seen.
- Skin infection is seen.
- One is seen in the body.
- Striae (white color stretch marks on the abdominal skin) are seen on the skin of the abdomen, thighs, and breasts.
- Skin with easy bruising (bruising of the skin).
- Skin becomes thin, fragile.
- Muscle and bone changes.
- Back pain while doing routine activities.
- Bone pain and tenderness.
- Difficulty climbing stairs due to proximal muscle weakness.
- Fat accumulation between the two shoulders.
- Fractures in the ribs and spinal cord due to bone thinning.
- Muscle weakness.
Other symptoms of Cushing’s syndrome:
- Psychological problems Depression, anxiety and behavioral changes are seen.
- Blood pressure increases.
- Bone weakness.
- Sleep disturbances are seen.
- Excessive catabolism of protein occurs.
- Muscle wasting is seen.
- Sodium and water retention occurs.
- The patient has a moon face appearance.
- The patient has a condition of hyperglycemia
- Polyuria (increased frequency of urination).
- Polydipsia (increased thirst).
h. Endotracheal Intubation – Endotracheal Incubation.
Endotracheal Intubation
Endotracheal Intubation is an important and life-protective medical procedure in which a tube called an endotracheal tube is placed in the patient’s trachea. This procedure is done to keep the airway open, deliver the right amount of oxygen, and remove carbon dioxide.
Indications for Endotracheal Intubation:
Endotracheal intubation is performed in the following situations:
- When the patient is unable to breathe spontaneously
- During general anesthesia
- Respiratory failure
- Trauma, blunt head injury, brain injury
- Cardiac arrest
- Airway obstruction
- Risk of aspiration
- Hypoxemia or hyperventilation
Equipment:
Endotracheal tube
Laryngoscope
Stylet (Stylet)
Sedatives and Paralytics
Oxygen Supply System
Suction Machine
Capnography Monitor
Ambu Bag
Stethoscope
Tube Fixation Devices (Strap or Tape)
Step-by-Step Procedure:
1. Pre-Oxygenation:
The patient is given 100% oxygen for 3-5 minutes to reduce the risk of hypoxia.
2. Medication Administration:
Sedative Etomidate, Midazolam or Propofol
Paralytic Agent: Succinylcholine or Rocuronium
3. Positioning:
The patient’s head is placed in the “Sniffing Position” so that the trachea is in a straight line.
4. Visualization with a Laryngoscope (Laryngoscopy):
The glottis and vocal cords are visualized using a laryngoscope.
The glottis and vocal cords are visualized using a laryngoscope.
5.Intubation of endotracheal tube:
The tube is carefully inserted into the trachea between the vocal cords.
6.Tube Placement Confirmation:
Check the presence of CO₂ through capnography
Check the movement of the chest on both sides and listen for breathing sounds with a stethoscope Chest X-ray Conforming Placement
7. Fixing the Tube (Tube Fixation):
The tube is fixed with tape or strap so that it does not slip.
8. Starting Ventilation (Mechanical Ventilation):
The patient is started on oxygen with a ventilator or an ambu bag.
Complications (Complications):
- Tracheal Injury
- Dental Trauma
- Hoarseness
- Sore Throat
- Aspiration (Aspiration)
- Hypoxia if delayed
- Endobronchial Intubation
- Infection
Endotracheal intubation is an essential, life-saving procedure that is performed to provide immediate oxygen support to a patient who is unable to breathe. This procedure should only be performed by a properly trained healthcare professional, as it is very sensitive and requires timely resolution of the risks involved.
Q-3
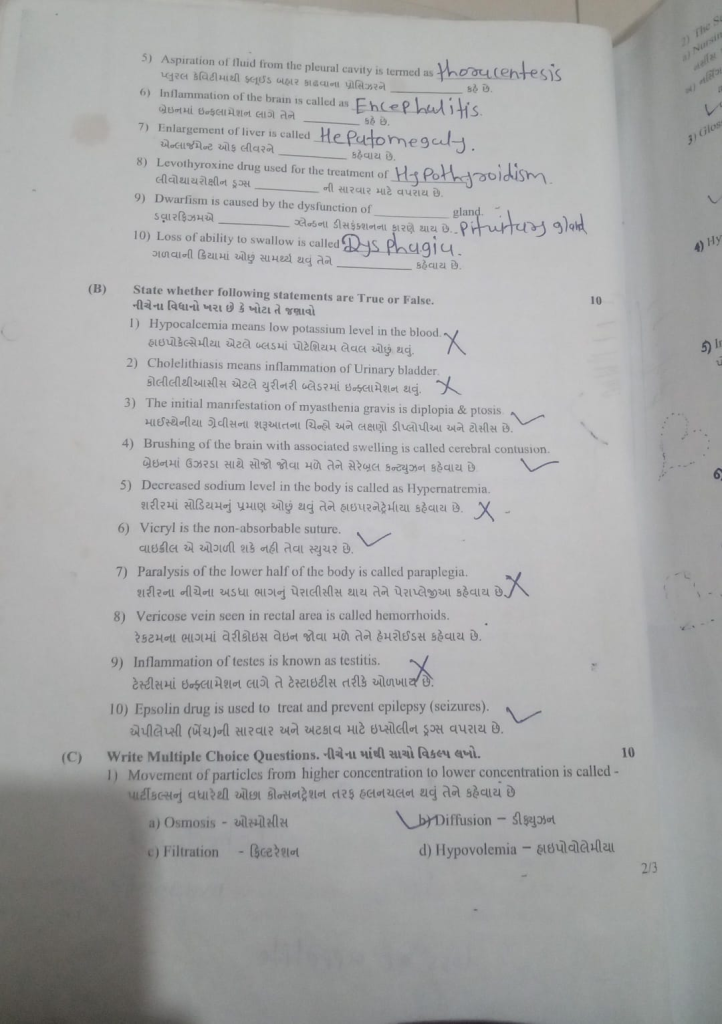
(A) Fill in the blanks, fill in the blanks. 10
1) Bell’s palsy is dysfunction of … Cranial nerve. Bell’s palsy is caused by dysfunction of … Cranial nerve. 7th (Seventh) Cranial nerve.
Bell’s palsy is caused by dysfunction of the Seventh (Seventh) Cranial nerve.
2) Removal of a part or lobe of the lung is called …. Removal of a part or lobe of the lung is called …. It is called. Lobectomy.
The removal of a part or lobe of the lung is called lobectomy.
3) M.R.i. stands for M.R.I. The full name is …. Magnetic Resonance Imaging
M.R.I. The full name of is – Magnetic Resonance Imaging.
4) Anorexia means …. Loss of appetite.
5) Aspiration of fluid from the pleural cavity is termed as …. The procedure of removing fluid from the pleural cavity is called …. Says. Thoracentesis.
The process of removing fluid from the pleural cavity is called thoracentesis.
6) Inflammation of the brain is called as …. Inflammation of the brain feels like …. It is called. Encephalitis.
When inflammation occurs in the brain, it is called encephalitis.
7) Enlargement of liver is called …. Enlargement of liver is called …. Hepatomegaly.
Swelling or enlargement of the liver is called hepatomegaly.
8) Levothyroxine drug used for the treatment of …. લેવોથીરોક્ષિન ડ્રુગ્સ …. It is used to treat hypothyroidism. Levothyroxine is used to treat hypothyroidism.
9) Dwarfism is caused by the dysfunction of …. gland. Dwarfism is …. It is caused by the dysfunction of the gland. Pituitary gland.
Dwarfism Pituitary gland is caused by the dysfunction of the gland.
10) Loss of ability to swallow is called …. Loss of ability to swallow is called …. It is called. Dysphagia.
Inability or difficulty in swallowing is calleddysphagia.
( B ) State whether following statements are True or False. State whether the following statements are True or False (10)
1) Hypocalcemia means low potassium level in the blood. Hypocalcemia means low potassium level in the blood. False
Hypocalcemia = Low calcium level in the blood, not potassium.
(Low potassium is called hypokalemia.)
2) Cholelithiasis means inflammation of Urinary bladder. Cholelithiasis is inflammation of the urinary bladder. False
Cholelithiasis = Presence of gallstones in the gallbladder, not urinary bladder.
(Cystitis is inflammation of the urinary bladder.)
3) The initial manifestation of myasthenia gravis is diplopia & ptosis The early signs and symptoms of myasthenia gravis are diplopia and tosis. True
Common early signs include double vision (Diplopia) and drooping eyelids (Ptosis).
4) Brushing of the brain with associated swelling is called cerebral contusion. Swelling of the brain with bruising is called cerebral contusion. True
Cerebral contusion = Bruising of brain tissue often accompanied by swelling.
5) Decreased sodium level in the body is called as Hypernatremia Decreased sodium level in the body is called as Hypernatremia. False
Low sodium = Hyponatremia
(High sodium = Hypernatremia)
6) Vicryl is the non-absorbable suture. Vicryl is a non-dissolvable suture. False
Vicryl = Absorbable synthetic suture.
7) Paralysis of the lower half of the body is called paraplegia. Paralysis of the lower half of the body is called paraplegia. True
Paraplegia = Paralysis of both lower limbs.
8) Varicose vein seen in rectal area is called hemorrhoids. Varicose veins found in the rectal area are called hemorrhoids. True
Hemorrhoids = Dilated (vericose) veins in rectal/anal area.
9) Inflammation of testes is known as testitis. Inflammation of the testicles is known as testitis. False
Correct term = Orchitis
(Testitis is not a medically accepted term.)
10) Epsolin drug is used to treat and prevent epilepsy (seizures). Epsolin (Phenytoin) drugs are used to treat and prevent epilepsy (seizures). True
🔹 Epsolin (Phenytoin) is an anticonvulsant used in epilepsy management.
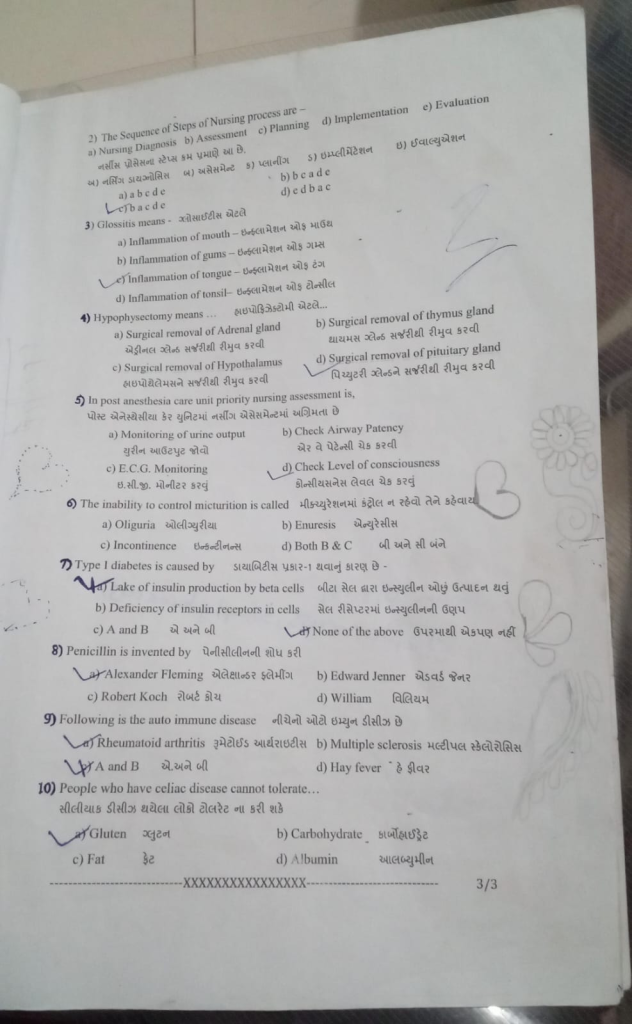
( C ) Write Multiple Choice Questions. Write the correct option from the following. 10
1) Movement of particles from higher concentration to lower concentration is called – Filtration
d) Hypovolemia – Hypovolemia
2) The Sequence of Steps of Nursing process are …. The steps of the nursing process are as follows….
a) Nursing Diagnosis
b) Assessment
c) Planning
d) Implementation
e) Evaluation
A) Nursing Diagnosis
B ) Assessment
C ) Planning
D) Implementation
E) Evaluation
a) abcde
b) bcade
C) bacde
d) edbac
3) Glossitis means – Glossitis means…
a) Inflammation of mouth – Inflammation of mouth
b) Inflammation of gums – Inflammation of gums
c) Inflammation of tongue – Inflammation of tongue
d) Inflammation of tonsil Inflammation of tonsils
4) Hypophysectomy means … Hypophysectomy means….
a) Surgical removal of Adrenal gland. Surgical removal of adrenal gland
b) Surgical removal of thymus gland. Surgical removal of thymus gland
c) Surgical removal of Hypothalamus. Surgical removal of hypothalamus
d) Surgical removal of pituitary gland. Surgical removal of the pituitary gland.
5) In post anesthesia care unit priority nursing assessment is,
a) Monitoring of urine output
b) Check Airway Patency
c) E.C.G. Monitoring E.C.G. Monitor
d) Check Level of consciousness.
6) The inability to control micturition is called…
a) Oliguria
b) Enuresis
c) Incontinence
d) Both B & C
7) Type I diabetes is caused by … Type I diabetes is caused by –
a) Decreased insulin production by beta cells
b) Deficiency of insulin receptors in cells
c) A and B
d) Lets None of the above
8) Penicillin is invented by … Penicillin was invented by…
a) Alexander Fleming
b) Edward Jenner
c) Robert Koch
d) William
9) Following is the auto immune disease
a) Rheumatoid arthritis
b) Multiple sclerosis
c) A and B
d) Hay fever
10) People who have celiac disease cannot tolerate … Fate
d) Albumin Albumin
