ENGLISH-MEDICAL SURGICAL NURSING : 1 (MSN : 1)PAPER SOLUTION 22/03/2021-NO.13
22/03/2021 – PAPER SOLUTION -NO.13
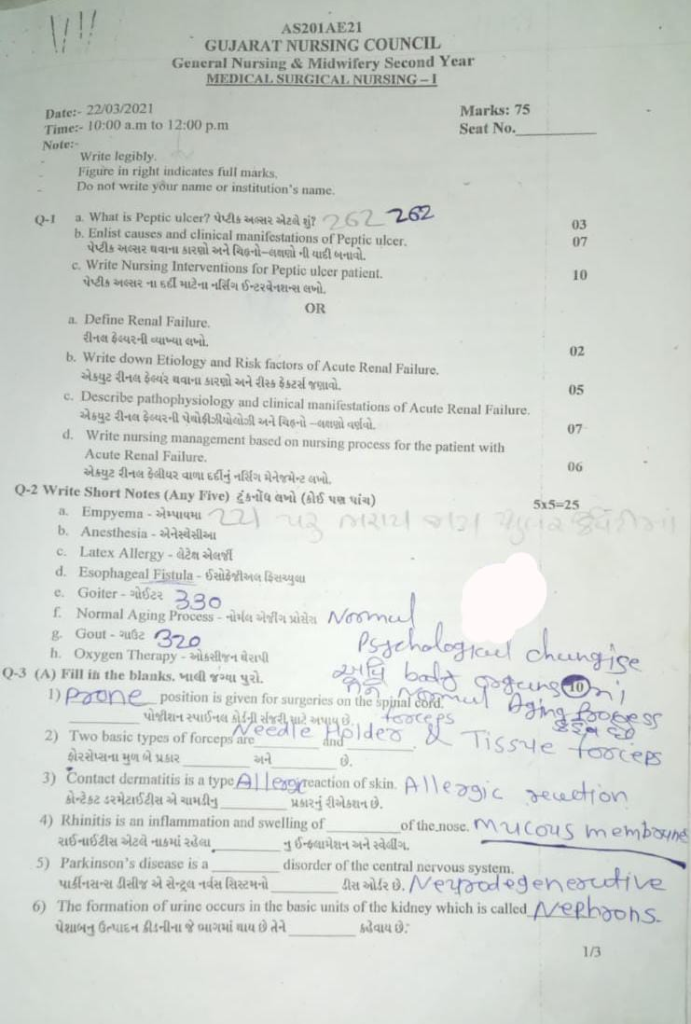
Q-1
a. What is peptic ulcer? What is peptic ulcer? 03
“Peptic ulcer” is a compound word.
1)”peptic “
2)” ulcer”
•••>
1)”peptic”
=> ” peptic” come from the Latin word “pepticus” ,
=> ” pepticus” Which come from the Greek word “peptikus” ,
=> “peptikus” Which come from the Greek word ” “peptein “
2)” ulcer” Which comes from the Latin word “ulcus”
=> ” ulcus” meaning a sore or a wound, an ulcer.
=> Peptic ulcer is an erosion or excavation ( hollow area ) formation in the mucosal lining of the stomach and the first part of the small intestine (duodenum) Peptic or duodenal ulcer.
=> In peptic ulcer, a sore or open sore develops in the mucosal lining of the stomach and the first part of the small intestine (duodenum). It is mainly caused by excessive secretion of acidic contents in the stomach. It is called peptic and duodenal ulcer.
•> If the peptic ulcer is in the “stomach”, it is called a “gastric ulcer”.
•> If the peptic ulcer is in the “small intestine”, it is called a “gastric ulcer”. If it is in the first part (duodenum) then it is called “duodenal ulcer”.
•> If the peptic ulcer is in the just upper part of the stomach i.e. in the “esophagus”, then it is called “esophageal ulcer”.
types of peptic ulcer. Types of peptic ulcer.
•> There are two types of peptic ulcer.
1)Acute peptic ulcer,
2)chronic peptic ulcer
•••>
1)Acute peptic ulcer,
=> Acute peptic ulcer is mainly superficial in which erosion of the superficial mucosal layer occurs.
=> Acute peptic ulcer heals within a short time but if left untreated So bleeding, perforation are seen in it.
2)chronic peptic ulcer
=> Chronic peptic ulcer has deep, sharp edges and a clean base.
=> In chronic peptic ulcer, there is also involvement of mucosa and submucosa.
=> If this ulcer penetrates into the stomach, it It also affects the nearby organ (pancreas) of the stomach.
b. Enlist causes and clinical manifestations of Peptic ulcer. List the causes and clinical manifestations of Peptic ulcer.07
Causes:
H.pylri (caused by Helicobacter pylori bacteria),
Regular use of pain-relieving mediation .
Ex:=
•>Aspirin ,
•>Ibuprofen,
•>Non steroidal anti •>inflammatory drug.
•>Ibuprofen,
•>Naproxen etc.
- Due to excessive production of stomach acid.
- Due to hereditary factors.
- Due to smoking.
- Due to alcohol consumption.
- Due to excessive stress.
- Irritating substances such as tea, coffee, spices, tobacco, Due to excessive use of things.
- Due to old age.
- Due to anxiety, worry.
Clinical manifestations (signs and symptoms):
- Inflammation in the stomach and the first part of the intestine (duodenum).
- Abdominal bloating.
- Abdominal burning.
- Pain in the upper middle part of the abdomen.
- nausea,
- vomiting,
- heart burn,
- Abdominal Bloating.
- belching (belching).
- weight loss.
- passing bloody, black, terry stools (hematochazia).
- bloody vomiting (hemetemesis).
- gastrointestinal bleeding.
- severe Abdominal pain.
- feeling of abdominal fullness.
c. Write Nursing Interventions for Peptic ulcer patient. Write Nursing Interventions for Peptic ulcer patient. 10
Nursing management (Nursing interventions):
1)pain related to gastric mucosa irritation.
Relieve pain of the patient:
- Assess the patient’s pain level.
- Provide mind diversionary therapy to the patient To do.
- Provide the patient with prescribed analgesic medicine.
- Advise the patient to avoid beverages and caffeinated foods.
- Advise the patient on relaxation techniques.
2)Altered nutritional status less than body requirement related to the therapeutic regiments.
maintain nutritional status of the patient.
- Assess the nutritional status of the patient.
- Advise the patient to take liquid and semi-solid food.
- Advise the patient to avoid hot, spicy, and caffeine foods.
- Provide the patient with a bland diet To do.
- If the patient is experiencing heartburn, provide antacid medicine.
- If the patient is vomiting, provide antiemetic medicine.
3)Anxiety related to the disease condition
Relieve the anxiety level of the client
- Assess the patient’s anxiety level.
- Provide the patient with complete information about his disease condition, its causes and its treatment.
- Clear all the patient’s doubts.
- Provide a comfortable environment for the patient and his family members.
- Properly communicate with the patient in simple language Communication.
- Provide psychological support to the patient.
4)Risk for gastro intestinal bleeding related to the surgery.
monitoring the patient for the GI track bleeding.
- Monitor the patient’s vital signs.
- Monitor the patient’s hemoglobin level.
- Assess the patient for any conditions such as dizziness and nausea.
- Monitor the patient’s stool test.
- Monitor the patient’s urine output.
- Take immediate measures to stop bleeding if the patient is bleeding.
- The patient’s Continue monitoring.
OR
a.Define Renal Failure. Write the definition of renal failure.02
Renal failure :
Renal failure is also known as kidney failure. Renal failure is a condition in which the ability of the kidneys to remove waste products and perform filtration from the body is lost. Due to this condition, toxic materials accumulate in the body and electrolyte imbalance occurs in the body. Renal failure is a condition in which adequate kidney function fails.
There are two types of renal failure.
1. Acute Renal Failure
Acute renal failure is also known as acute kidney injury (AKI). In which kidney function declines suddenly and rapidly. Acute kidney failure is a condition in which the functional ability of the kidneys is suddenly impaired, due to which the kidneys cannot filter properly and urine output also decreases. (less than 1ml/ kg/ hr) and cannot maintain electrolyte balance and fluid balance in the body. Acute kidney failure occurs within 7 to 90 days. In acute kidney failure, mainly the glomerular filtration rate (GFR) decreases, the concentration of blood urea nitrogen increases, the amount of creatinine increases, urine output is less than 400ml throughout the day, the condition of hyperkalemia arises and sodium retention is seen in the body.
2.Chronic Renal Failure
This is an irreversible renal disease. In which there is progressive loss of renal function. Which is seen due to some other disease. In this condition, when acute renal disease is not treated on time, it is a chronic condition seen due to gradual decrease in kidney function. In which the kidneys fail to filter the blood and waste products accumulate in the blood.
b. Write down Etiology and Risk factors of Acute Renal Failure. 05
1) Pre Renal cause:
- Due to impaired blood supply to the kidneys. Due to dehydration.
- Diarrhea.
- Vomiting.
- Hemorrhage.
- Burn.
- Due to excessive use of diuretic medicine.
- Due to decreased cardiac output.
- Due to congestive heart failure.
- Due to cardiogenic shock.
- Due to acute pulmonary embolism.
- Due to constriction of blood vessels supplying blood to the kidneys.
- Due to dilation of blood vessels supplying blood to the kidneys.
2) Intrarenal:
- Intrarenal failure is mainly seen due to structural damage in the glomeruli, kidney tubules, and nephrons. Due to prolonged renal ischemia.
- Due to blood clot, cholesterol deposit around the veins and arteries.
- Due to infection.
- Due to hemolytic uremic syndrome.
- Due to severe transfusion reaction.
- Due to exposure to any nephrotoxic agent.
- Like:
- NSAID Drug,
- ACE inhibitor,
- Aminoglycoside Lupus,
- Multiple myeloma,
3) Postrenal:
- Due to obstruction of urine flow.
- Due to enlargement of the prostate gland.
- Due to kidney stones.
- Due to cancer of the urinary tract organs.
- Due to certain medications.
- Due to bladder stones.
- Due to enlargement of the prostate gland.
- Due to bladder cancer.
- Due to neurological disorders.
c. Describe pathophysiology and clinical manifestations of Acute Renal Failure. Describe the pathophysiology and signs and symptoms of acute renal failure.07
1.(Initiation Phase)
Features:
- This phase begins immediately after injury and usually lasts for hours to days. The cause may be ischemia, toxins, or sepsis.
- Urine output is normal or slightly decreased.
- Blood Urea Nitrogen and Creatinine levels are slightly elevated.
- Kidney damage can also be reversed with appropriate treatment.
2. Oliguric Phase
Features:
- This phase usually lasts for 1 to 2 weeks. Urine output is less than 400 mL/day.
- Glomerular Filtration Rate decreases.
- Fluid overload, electrolyte disturbances such as hyperkalemia, metabolic acidosis occur.
- The patient experiences symptoms such as muscle tension, sleep disturbances, nausea, vomiting, and high blood pressure.
- Life-threatening emergency states can also develop during this phase.
3.Diuretic Phase
Features:
- This phase marks the beginning of recovery.
- There is a significant increase in urine output (In some cases up to 3 to 5 liters/day).
- Now filtration increases, but tubular function has not yet completely recovered.
- Conditions such as dehydration, hypokalemia, and hypotension may arise.
- Careful fluid and electrolyte management of the patient is necessary.
4. Recovery Phase
Features:
- Duration: This phase can last from weeks to months.
- Normal urine output and BUN and creatinine levels begin to return to normal.
- Most patients recover completely, although some Patients are at risk of developing chronic kidney disease.
- Acute renal failure is a severe condition in which kidney function is immediately reduced. It has four phases:
1.Initiation Phase: Initiation and injury
2.Oliguric Phase: Urine output decreases and electrolyte disturbances occur
3.Diuretic Phase: Urine output increases but irregularly
4.Recovery Phase: Kidneys gradually recover.
Signs and Symptoms (Clinical Manifestations of Acute Renal Failure):
1. Urinary changes:
Oliguria – low urine output (less than 400 mL/day)
Anuria – cessation of urine output
Seeing blood, mucus or dirt in the urine
2.Fluid retention:
Swelling of the body (edema)
Pulmonary edema
Increased blood pressure (hypertension)
3.Electrolyte imbalance:
Hyperkalemia → Irregular heartbeat
Hyponatremia (Hyponatremia)
Hypocalcemia
4. Gastrointestinal symptoms:
Vomiting
Anorexia
Abdominal cramps
Abdominal cramps
5. Neurological symptoms:
Confusion
Delirium
Weakness and fatigue
Coma if severe
6. Cardiac symptoms:
Uncontrolled heart rate (arrhythmia)
Slow or fast heart rate (bradycardia/tachycardia)
d. Write nursing management based on nursing process for the patient with Acute Renal Failure. Write the nursing management of a patient with acute renal failure.06
a) pain :-
- The patient is given analgesics as per the doctor’s orders.
- The patient should be given the right position.
- Other antibiotics should also be given to the patient at the right time.
- Severe In case of pain, the doctor should be informed immediately and opioids should be given if ordered.
b) fever:-
- The patient’s body temperature should be checked regularly
- If there is high fever, the patient should be given antipyretics.
- If the patient is feeling cold, an extra blanket should be given
- A wet cloth should be kept on the patient’s head.
c) Anxiety:-
- The patient should be treated with kindness
- The patient and their relatives should be informed about the hospital and ward setup.
- If possible, a relative should be allowed to stay with the patient at all times
- All the patient’s questions should be answered calmly and positively
D) Body fluid overload or electrolyte imbalance :-
- Antiemetics should be given for vomiting
- The patient should be checked for overhydration and edema and the severity of edema should be monitored.
- Give diuretic drugs to the patient as per the doctor’s order
- The patient should be encouraged to take small amounts of fluids
- The patient’s daily body weight should be checked and recorded
- The level of pitting edema in the patient should be recorded
- The patient’s intake and output chart should be maintained.
E) Altered Nutrition less than body requirement :-
- Based on the patient’s age, weight and blood glucose level as well as the nutritional requirements, a diet should be calculated and encouraged accordingly.
- The patient’s blood glucose level should be checked regularly
- The patient should be given a diet as follows:
- High calorie
- Low protein
- Low salt or no salt
- Low fluid
- The patient should be given vitamins and iron supplements.
F) prevent complication:-
- Regular observation of the patient should be done.
- The patient’s TPR and BP chart should be maintained
- The patient’s problem should be listened to carefully and signs of complication should be noted.
- If any type of complication is found in the patient, the doctor should be informed immediately.
- An emergency medicine tray should always be kept ready with the patient
G) Restlessness:-
- The patient should be given a comfortable position.
- If the patient has difficulty breathing, then oxygen therapy should be given
- Diuretic drugs should be given to the patient only in the morning and afternoon. They should not be given in the evening and at night, due to which, the patient experiences nocturia and due to which the patient cannot sleep
- If the patient has a catheter, it should be kept in the right position and the insertion site should be kept clean.
H) Unhygienic conditions:-
- If necessary, the patient should also be given diapers
- The patient should be helped to maintain personal hygiene.
- Appropriate water should be provided for bathing according to the season.
- If the patient is unable to do mouth care himself, then mouth care should be done
- If necessary, bed bath should also be given
Q-2 Write Short Notes (Any Five) 5×5 = 25
a. Empyema – Empyema
Empyema ( Empyema ) :
Empyema is a condition in which there is an accumulation of pus in the space between the lungs and the inner surface of the chest wall (pleural space). Abnormal collection of pus found in the pleural cavity is known as empyema. Empyema is also known as ‘pyothorax’ and ‘purulent pleuritis’ . Empyema is mainly seen as a complication of pneumonia and lung abscess.
Stage of Empyema:
Exudative stage: The exudative stage is the early stage of empyema. In which sterile serous fluid accumulates in the pleural space.
Fibropurulent stage:In this stage, the pleural fluid becomes purulent (pus-like) and the fibrous septa form pockets with localized pus.
Organizing stage: This is the last stage of empyema. In which fibrin and pus are organized in the pleural space and form a thick pleural pellicle.
Etiology/causes of empyema:
- Bacterial infection (Streptococcus pneumoniae)
- Viral infection
- Fungal infection
- Pneumonia
- Tuberculosis
- Lung abscess
- Trauma
- Chest wound
- Chest surgery
- Immunosuppression
clinical manifestations of Empyema:
- Dyspnea,
- Cough,
- Fever,
- Chest pain,
- Anemia,
- Movement on the affected side is diminished
- Shortness of breath
- Chest tightness
- Chest pain
- Persistent cough
- Weakness
- Fatigue
- Night sweats
- Anorexia
- Weight loss
Diagnostic evaluation of Empyema:
- History Collection
- Physical Examination
- X-ray
- CT Scan
- Ultrasound
- Sputum Analysis
- Thoracocentesis
- Blood Test
Management of Empyema:
Antibiotics Provide antibiotics to treat bacterial infections.
Pain Relievers (Analgesics)
Provide analgesic drugs to relieve pain.
Antipyretic
Provide antipyretic drugs to reduce fever. To do.
Mucolytic
Provide a mucolytic drug to break down and clear mucus.
Thoracocentesis In thoracocentesis, pus or fluid is aspirated by inserting a needle directly into the pleural cavity.
Chest tube drainage
In chest tube drainage, a chest tube (thoracostomy tube) is placed in the pleural space and the pus is drained.
Fibrinolytic therapy
In cases of fibropurulent empyema, a fibrinolytic agent such as plasminogen activator is instilled into the pleural space. It breaks down fibrin and helps in drainage.
Nursing management of pulmonary edema:
- Assess the patient properly and completely.
- Assess the patient’s respiratory status properly.
- Assess the patient’s vital signs completely.
- Assess the patient’s oxygen saturation properly.
- Continuously monitor the patient’s respiratory status and oxygen saturation to properly assess the patient’s condition.
- Continuously monitor the patient’s body temperature.
- Provide the patient with fluids in small amounts.
- Provide the patient with a properly comfortable position.
- Provide adequate oxygen to the patient to maintain the patient’s body oxygen saturation and provide respiratory support.
- Provide the patient with properly prescribed medication.
- Provide complete education to the patient and his/her family members about the patient’s condition, its causes, its symptoms and signs, and its treatment.
- Provide the patient with proper care and a comfortable environment.
b.Anesthesia
Definition:-
Anesthesia is a medical practice that prevents pain during surgery or other procedures. Anesthetic agents in anesthesia are a group of chemical agents that cause partial or complete loss of sensation. This anesthesia can prevent the patient’s discomfort and can help him/her cooperate.
The medicine given in anesthesia blocks the nerve signals so that the sensation of pain stops going to the brain and pain is not felt so that the surgical procedure can be done easily.
Purpose of Anaesthesia:-
- To get the patient’s cooperation
- To reduce or eliminate pain To do
- To keep the muscles of the body relaxed
- To perform the surgical procedure comfortably
There are three types of anesthesia.
1) Local anesthesia:-
This affects a limited area of the body (local part). This usually affects the part of the body where the surgery is to be performed or the part that needs to be numbed.
The following chemicals are used in local anesthesia.
- Xylocaine hydrochloride
- Lignocaine hydrochloride
- Amethocaine hydrochloride
- –>
- Procaine Hydrochloride
2) Spinal Anesthesia :-
There are two types of There are-
1)Epidural anesthesia:-
When anesthesia is injected into the epidural part of the spinal cord, it is called epidural anesthesia.
2)Spinal anesthesia:-
When anesthesia is injected into the subarachnoid space of the spinal cord, it is called spinal anesthesia.
Use of Spinal Anesthesia:-
- Orchidectomy
- Caesarean
- Hernia Surgery
- Hydrocele Surgery
- Penis Surgery
- Prostate Surgery
Complication :-
- Urinary Retention
- Meningitis
- CSF Leakage
- Hypotension
- Paralysis
- Allergy
3) General Anesthesia:-
When the sensation in the whole body is to be lost, the person is rendered unconscious. It is called general anesthesia. General anesthesia can be given as follows-
-
- Intravenously
-
- By inhalation
1.By intravenous:-
I.V. The following drugs are used in general anesthesia by injection: Thiopental sodium 2.5% Hexabarbitone 10% Methohexital sodium Propofol –>
- Midazolam
- Fentanyl
- Ketamine Hydrochloride
- Droperidol
2. Inhalation Anesthetics:-
This anesthesia is given through inhalation, which makes the patient unconscious.
Before administering this anesthesia, the patient is given some sedatives, then an endotracheal tube is inserted into the airway, and then this is given.
The following medicines are used in this.
- Sevoflurane
- Nitrous oxide
- Ether
- Cyclopropane
- Methoxyflurane
- Enflurane
- Panthrene
Responsibility of Nurse :-
- The work of administering anesthesia is done by the anesthesia doctor or anesthetist but the nurse assists in it and the responsibility of the nurse is as follows.
- First of all, the patient to be given anesthesia Identify by name
- Obtain written consent
- Answer questions asked by the patient about anesthesia The nurse should give it properly so that the patient’s anxiety can be reduced.
- Prepare the necessary equipment
- The nurse prepares the patient for anesthesia and provides gown, shoe cover, cap, etc.
- Clean the area where anesthesia is to be administered using aseptic technique
- Keep the necessary medications for anesthesia in the right place
- Continue to provide the patient with anesthesia during Observation
- Checking the patient’s vital signs
- Checking the patient’s level of consciousness
- The nurse should observe for complications due to anesthesia
- Preparing for surgery after anesthesia
- Maintain records and reports
- Clean the anesthesia machine after administering anesthesia.
C.Latex Allergy
Latex Allergy:
Latex allergy is an allergic reaction of the body’s immune system to natural latex, which is made from rubber. It is a hypersensitivity reaction that is obtained from the tree (Hevea brasiliensis). When latex comes into contact with objects, the body recognizes it as an allergen and mounts an immune response against it.
Symptoms:
- Latex allergy symptoms can appear within minutes or hours after contact. Common symptoms include:
- Itching on the skin
- Hives
- Swelling
- Runny Nose
- Watery or Red Eyes
- Difficulty Breathing
- In severe cases, life-threatening allergic reactions such as anaphylaxis may occur, which require immediate medical attention.
Types of Latex Allergy:
1. Type I Latex Allergy:
This is an IgE mediated allergic reaction in which there is an immediate Symptoms occur immediately and the possible outcome may be anaphylactic shock.
2.Type IV Delayed Hypersensitivity:
This type of allergy is T-Cell Mediated and symptoms may appear after 24–48 hours. Usually seen in the form of dermatitis.
Common Latex-Containing Items:
- Surgical Gloves
- Blood Pressure Cuffs
- Condoms
- Balloons
- Elastic Bands
- Catheters
Diagnosis:
- Skin Prick Test
Checks for the presence of IgE antibodies. - Serum Specific IgE Test
Blood to check for IgE against latex proteins Test. - Patch Test
Useful for Type-IV reactions.
Treatment & Management:
Avoidance of Latex:
Staying away from latex products is the most important step.
Antihistamines:
Useful for itching and redness.
Epinephrine:
An immediate injection for anaphylaxis.
Medical Identification:
It is safe for people with latex allergies to wear a medical ID bracelet.
If you have a latex allergy, inform your doctor before undergoing any surgical or dental treatment so that latex-free instruments can be used.
d.Esophageal Fistula – Esophageal Fistula
Esophageal Fistula
Description:
Esophageal fistula is a medical condition in which an abnormal connection is formed between the esophagus – the food pipe – and another organ such as the trachea, bronchus, mediastinum, chest or skin.
This abnormal path can cause food or liquid to go directly to the lungs when swallowed, which can lead to aspiration pneumonia, sepsis, and severe respiratory complications.
Types:
1. Congenital Esophageal Fistula:
- Present at birth Is
- Mostly associated with Esophageal Atresia
- Requires proper surgical correction
2. Acquired Esophageal Fistula:
Develops throughout life, and can have the following causes:
- Cancer: Especially of the esophagus or lungs
- Trauma: For example, an injury or accident
- Infection: Diseases such as tuberculosis
- Surgery Post-Surgical Complications
- Radiation Therapy:After long-term cancer treatment
Common Types of Fistula:
1. Tracheoesophageal Fistula:
Connection between the esophagus and trachea: Most common Congenital type
2. Bronchoesophageal Fistula:
Connection between the bronchus and esophagus
Symptoms:
-
- Deep cough while eating
-
- In Infants – Coughing While Feeding)
-
- Recurrent respiratory infection or pneumonia
-
- Aspiration of food
-
- Breathing difficulty
-
- Nutritional deficiency
-
- Failure to thrive (especially in children)
Diagnosis:
1. Esophagography:
Barium Swallow Test to visualize the fistula
2. Endoscopy:
Direct observation of the esophagus
3. Bronchoscopy:
Inspection of the trachea and bronchi
4. Imaging:
CT Scan
MRI (Magnetic Resonance Imaging)
To identify complications and the location of fistulas
Treatment:
1.Surgical Repair:
Reconstruction of the esophagus by removing the connection
Immediate surgery is essential in congenital cases
2.Stenting:
Applied in fistulas caused by cancer or radiation Useful
3. Antibiotics:
To eliminate infection
4. Enteral Nutrition:
Giving nutrition through a nose or peg tube
5. Oxygen Therapy:
For respiratory support
Management (General Management):
- Immediate recognition and ICU transfer for high risk care
- Use of nasogastric tube or parenteral nutrition by stopping oral feeding
- Avoid infection with strict aseptic technique
- Ventilator Support
Multidisciplinary Team:
Pediatrician, Surgeon, Nutritionist, and Respiratory Therapist
Nursing Management:
1.Airway Management (Airway Management):
Keeping the patient’s airway open
Regular suctioning to remove mucus
2.Nutritional Support:
Avoiding oral feeding
Tube feeding with positioning
3.Infection Infection Prevention:
Hand Hygiene
Sterile Technique
4. Monitoring:
Regular monitoring of symptoms: temperature, respiratory rate, heart rate
Alert for signs of sepsis or pneumonia
5. Parental Support and Parental Support & Education:
Explaining the problem to parents
Giving guidance on how to take care at home
Risks and Complications:
- Aspiration Pneumonia: A respiratory infection caused by food entering the lungs
- Sepsis : Severe systemic infection
- Malnutrition : Severe nutritional deficiency
- Stricture Formation : Scar Tissue Formation in the Esophagus
- Mortality : Can be fatal if treatment is delayed
Esophageal fistula is a life-threatening medical condition that can be managed with prompt recognition, proper diagnosis, appropriate surgical intervention, and professional nursing management. Its timely care is extremely important, especially in newborns and cancer patients.
e. Goiter-
Goiter
Goiter is an abnormal enlargement or growth of the thyroid gland, which appears in the front of the neck. The thyroid is a butterfly-shaped endocrine gland that produces hormones for important functions in the body such as metabolism, energy production, heart rate, and temperature.
Goiter is not an independent disease, but can be an indicator of an underlying thyroid disorder – such as Hypothyroidism, Hyperthyroidism, or Euthyroid condition.
Types of Goiter:
1.Simple / Non-Toxic Goiter Goiter):
Gland enlargement despite normal thyroid hormone levels
Mainly due to Iodine Deficiency
2.Toxic Goiter:
Excessive production of thyroid hormone
Cause: Graves’ Disease or Toxic Nodular Goiter
3.Nodular Goiter:
One (Solitary Nodule) or more (Multinodular Goiter) nodules in the thyroid gland
Symptoms:
- A lump or deep lump in the neck
- Hoarseness
- Breathing Difficulty – Pressure on Trachea due to large goiter
- Difficulty Swallowing
- In patients with hypothyroidism: Fatigue, hair loss, extreme coldness
- In patients with hyperthyroidism: Heart palpitations, weight loss, restlessness
Diagnosis:
1.Physical Examination
Finding goiter and lump by neck palpation
2.Thyroid Function Test (TFT)
Measuring TSH, T3, T4 levels
3.Ultrasound
To know the size of the thyroid and nodules
4.Radioactive Iodine Uptake Scan
To see how the gland is functioning
5.Fine Needle Aspiration Cytology (FNAC)
To take cells from the lump and check for cancer
Treatment:
Iodine Supplementation
If goiter is caused by iodine deficiency
Thyroid Hormone Therapy
Levothyroxine – For Hypothyroidism
Antithyroid Drugs
Methimazole, Propylthiouracil – For Hyperthyroidism
Radioactive Iodine Therapy
To destroy thyroid tissue
Surgery (Thyroidectomy)
For large goiter, suspected cancer, or breathing difficulty
Nursing Management:
- Inform the patient about the cause of the goiter and its treatment
- Ensure that hormone therapy is being taken properly
- If there is breathing difficulty, give the patient Fowler’s position
- Monitoring the patient for pain, oral intake and hypocalcemia after surgery
- Signs of hypocalcemia: Check for tetany, Chvostak and Trousseau’s sign
- Also observe the patient’s vocal cords and voice changes
Complications:
- Pressure on Trachea
- Nodule turning into cancer
- Hypothyroidism / Hyperthyroidism
- Recurrent Laryngeal Nerve Injury – Voice Change
- Parathyroid Injury and Hypocalcemia
Goiter is often a common It may be a mild but serious medical condition. Proper diagnosis, timely treatment, and multidisciplinary management of the patient are essential. Thyroid-related adjustments and follow-up can completely benefit the patient.
f.Normal Aging process –
Normal Aging Process
Description:
Normal Aging Process is a sequential process of natural changes that occur in the body and brain over time. These changes affect almost every organ and its function.
Aging is not a disease, but a process of physical and mental adaptation. Some physical abilities slow down, but many patients can remain completely healthy from the inside if a proper lifestyle is adopted.
Normal Physiological Changes of Aging:
1. Nervous System:
Changes:
In the normal aging process, the size of the brain decreases and neurons gradually degenerate. Due to which symptoms like memory loss, slow reaction and dementia are seen. Both sensory and motor function are affected.
2. Cardiovascular System
Changes:
Heart rate slows down and elasticity of veins and arteries decreases. Atherosclerosis increases, which increases the risk of heart attack and high blood pressure.
3.Respiratory System:
Changes:
The elasticity of the lungs decreases, and the ability of the alveoli to inflate decreases. Due to reduced oxygen uptake, fatigue, low energy and low stamina are observed.
4. Digestive System:
Changes:
Secretions of digestive juices slow down, which causes hard stools and constipation. The function of the pancreas and liver also gradually decreases.
5. Urinary System
Changes:
The filtering function of the kidneys decreases. Blood urea nitrogen and creatinine levels may increase. Urinary incontinence occurs, which reduces the ability to hold urine.
6.Endocrine System
Changes:
The levels of major hormones such as insulin, thyroid and adrenal hormones decrease. The risk of diabetes increases due to the slowing of insulin response.
7. Reproductive System
Changes:
In women, estrogen levels decrease after menopause. In men, testosterone gradually decreases. Both reproductive ability and sexual function are affected.
8. Musculoskeletal System
Changes:
Bone density decreases (osteoporosis). Cartilage decreases, which causes osteoarthritis. Tissues shrink, which is called Muscle Atrophy.
9. Integumentary System
Changes:
The skin becomes thin, dry, and less elastic. Collagen and elastin decrease. Hair turns white and hair also decreases due to the decrease in the number of follicles.
10. Immune System
Changes:
The activity of T-cells and B-cells decreases, due to which the body does not get protection from viruses and bacteria. Transmission of diseases is more and feedback on vaccination is also less.
There is a gradual decline in physical capacity with aging, but a person can live a beautiful life with a good diet, regular exercise, social participation and medical checkups.
It is important to understand the difference between normal aging and pathological aging.
Normal aging process is a natural process occurring in the body which is inevitable for every person. If a person improves his lifestyle on time, maintains physical and mental fitness, then aging can lead to a comfortable and active life.
g. Gout :
Definition:-
Gout is a recurrent attack of inflammatory arthritis. In which red color, swelling, heat are seen in the joint. Which is seen due to the increase in uric acid in the blood. Uric acid crystals are deposited in the joints, tendons and surrounding tissues.
Etiology:-
- Medullary cystic kidney disease in genetic causes
- After surgery
- Diabetes mellitus
- Metabolic syndrome
- Hemolytic anemia
- Hypertension
- Chemotherapeutic drugs
- Taking immunosuppressive drugs
- Renal disease
- Use of diuretics
Clinical Manifestation:-
- Inflammatory arthritis in which the part is red, swollen, hot is seen mainly on the Big Toe in which it is seen in the metatarsal phalangeal
- Fatigue and fever are seen along with joint pain
- Tophy is seen
- Hyperuricemia
Diagnostic test :-
- In blood test. Uric acid above 6mg/dl is found
- X-ray joint
- E. SR
- Kidney function test
- Electrolyte
- Blood count
Treatment:- acute gout
- NSAIDS with calciquine & Steroids are given.
Drugs:- Ibuprofen.
- Drugs like allopurinol and febuxostate are given to reduce uric acid levels.
- Steroids are given into the joint for swelling.
1. Manage pain of patient.:
- Elevate the affected joint and provide a comfortable position
- Give medications as per doctor’s order
- Immobilize the affected joint
- To prevent the weight of the bedclothes from falling Use of bed cradle or footboard
- The patient’s activity and disability should be checked regularly
2. Explain to the patient about diet precautions, including taking 2-3 liters of fluid per day.
3. Explain to the patient to stay away from alcohol.
4. The patient should be given necessary instructions for a healthy lifestyle.
5. Explain to take a proper balanced diet.
6. Explain the importance of rest and exercise.
h. Oxygen Therapy – Oxygen Therapy
Oxygen Therapy : Oxygen Therapy
Definition:
Oxygen Therapy is a treatment method in which oxygen is administered from an external source to maintain the oxygen concentration in the patient’s body at a normal or required level.
This therapy is especially necessary when the patient has hypoxemia: a lack of oxygen in the blood. The level drops. If oxygen is not supplied in time, it can lead to hypoxia, which is a condition in which the oxygen supply to the body’s organs decreases.
Objectives of Oxygen Therapy:
- Supply sufficient oxygen to vital organs such as the brain and heart
- Maintain cellular metabolism
- Avoid life-threatening conditions such as hypoxia
- Reduce respiratory distress
- SpO₂ (oxygen saturation) level ≥95% Maintain
Indications:
- Oxygen therapy is useful in the following conditions:
- Chronic Obstructive Pulmonary Disease (COPD)
- Pneumonia
- Asthma Attack
- Anemia
- Carbon Monoxide Poisoning
- Heart Failure
- During Recovery After Trauma or Surgery
- Cerebral Hypoxia
Methods of Oxygen Administration:
1. Nasal Cannula:
- The simplest method of oxygen delivery
- 1 to 6 liters per minute
- 24% to 44% FiO₂
2.Simple Face Mask:
- For medium flow delivery
- 5 to 10 liters/minute
- 40% to 60% FiO₂
3.Non-rebreather Mask (Non-Rebreather Mask):
- For severely hypoxic patients
- 10 to 15 liters/minute
- 90% to 100% FiO₂
4. Venturi Mask:
- A specific oxygen source is provided
- Especially useful for COPD patients
5. Oxygen Tent:
- For light oxygen requirements for children
6. Mechanical ventilation (Mechanical Ventilation):
- When the patient’s natural breathing stops
Precautions and Monitoring:
- Continuous monitoring of oxygen levels through SpO₂ monitoring (Pulse Oximetry)
- The patient’s ABG (Arterial Blood Gas) test Assess pH, PaO₂, PaCO₂
- Humidify when giving oxygen at ≥4 L/min
- Handle oxygen bottles/cylinders safely as they are flammable
- Give oxygen slowly and in a controlled manner, especially for COPD patients, as excess oxygen poses a risk of carbon dioxide retention.
Side Effects:
- Dry nasal mucosa
- Oxygen toxicity: Can occur from prolonged exposure to high levels of oxygen
- Retinopathy of Prematurity: Risk in newborns
- Hypoventilation: Especially in COPD patients
Oxygen therapy is an effective and life-saving treatment method, which is important in maintaining the necessary oxygen supply to the respiratory system and the entire body.
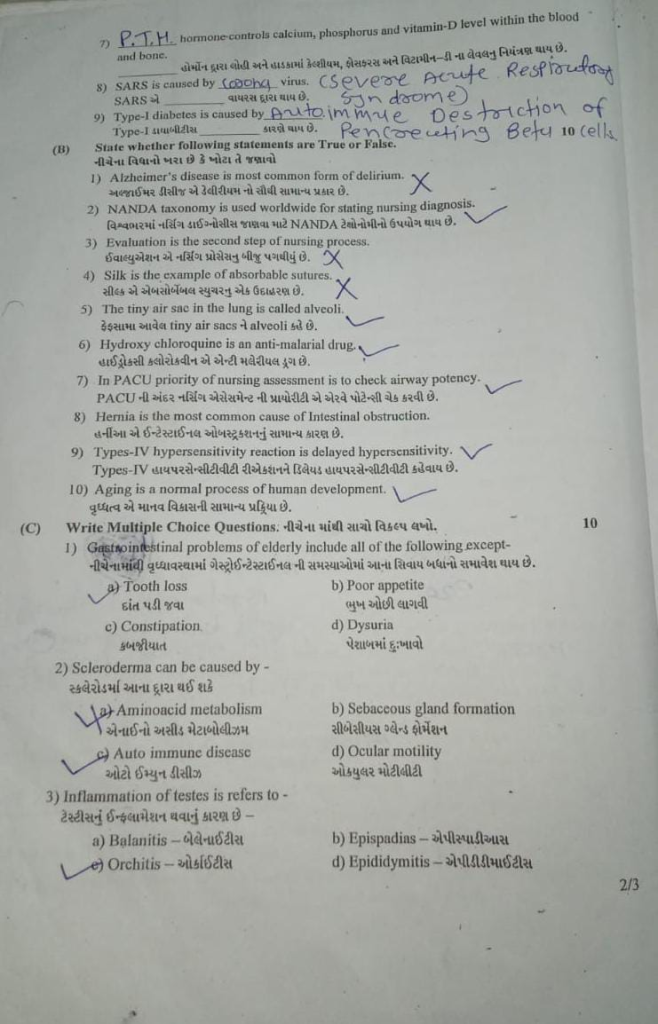
Q-3 (A) Fill in the blanks, 10
1) …… Position is given for Surgery on the Spinal cord…… Position is given for Surgery on the Spinal cord. Prone
2) Two basic types of forceps are …… and ….. The basic types of forceps are …… and ……. Tissue and Hemostatic
3.Contact dermatitis is a type ……. reaction of skin. Contact dermatitis is a type of ……. reaction of the skin. Hypersensitive
4.Rhinitis is an inflammation and swelling of …… of the nose. Mucosa
5.Parkinson’s disease is a …… disorder of the central nervous system. Parkinson’s disease is a …… disorder of the central nervous system.Neurodegenerative
6) The formation of urine occurs in the basic units of the kidney which is called …… The part of the kidney that produces urine is called ……. Nephron
7) …… hormone controla calcium, phosphorus and vitamin-D level within the blood and bone ……. The hormone controls the levels of calcium, phosphorus and vitamin D in the blood and bones.Parathyroid
8) SARS is caused by …… Virous. SARS is caused by …… virus. Corona virus
9) Type-1 diabetes is caused by …… Type 1 diabetes is caused by ……. Autoimmune destruction of beta cells
B) State whether following statements are True or False. 10
1) Alzheimer’s disease is the most common form of delirium. Alzheimer’s disease is the most common type of dementia, not delirium. Delirium is an acute confusional state.
2) NANDA taxonomy is used worldwide for stating nursing diagnosis. NANDA taxonomy is used to identify nursing diagnoses worldwide. ✅ True
NANDA (North American Nursing Diagnosis Association) provides standardized nursing diagnoses globally.
3) Evaluation is the second step of nursing Process. ❌ False
Evaluation is the last (fifth) step of the nursing process. The second step is nursing diagnosis.
4) Silk is the example of absorbable sutures. Silk is an example of an absorbable suture. ❌ False
Silk is a non-absorbable suture material.
5) The tiny air sac in the lung is called alveoli. The tiny air sacs in the lungs are called alveoli.
6) Hydroxy chloroquine is an anti-malarial drug. Hydroxychloroquine is an antimalarial drug. ✅ True
Hydroxychloroquine is used to treat malaria as well as autoimmune diseases like rheumatoid arthritis.
7) In PACU priority of nursing assessment is to check airway potency. The priority of nursing assessment within the PACU is to check airway patency. ✅ True
Maintaining airway patency is always the first priority in post-anesthesia care.
8) Hernia is the most common cause of Intestinal obstruction. Hernia is a common cause of intestinal obstruction. ❌ False
Adhesions (scar tissues) are the most common cause of intestinal obstruction, not hernia.
9) Types-IV hypersensitivity reaction is delayed hypersensitivity. Types-IV hypersensitivity reactions are called delayed hypersensitivity. ✅ True
Type IV hypersensitivity is also called delayed-type hypersensitivity, involving T-cell mediated responses.
10) Aging is a normal process of human development. Aging is a natural, progressive, and universal process in human development. ✅ True
Aging is a natural, progressive, and universal process in human development.
( C ) Write multiple choice questions. Write the correct option from the following. 10
1) Gastrointestinal problems of elderly include all of the following except-
a) Tooth loss
b) Poor appetite
c) Constipation Constipation
✅ d) Dysuria – painful urination
-> Dysuria is a urinary problem, not a gastrointestinal one.
2) Scleroderma can be caused by -Scleroderma can be caused by –
a)Aminoacid Amino metabolism
b) Sebaceous gland formation
✅ c) Auto immune disease –
d) Ocular motility
->Scleroderma is an autoimmune connective tissue disorder.
3) Inflammation of testes is refers to- –>
b) Epispadins – Epispadias
✅ c) Orchitis – Orchitis
d) Epididymitis – epididymitis
->Orchitis means inflammation of the testes.
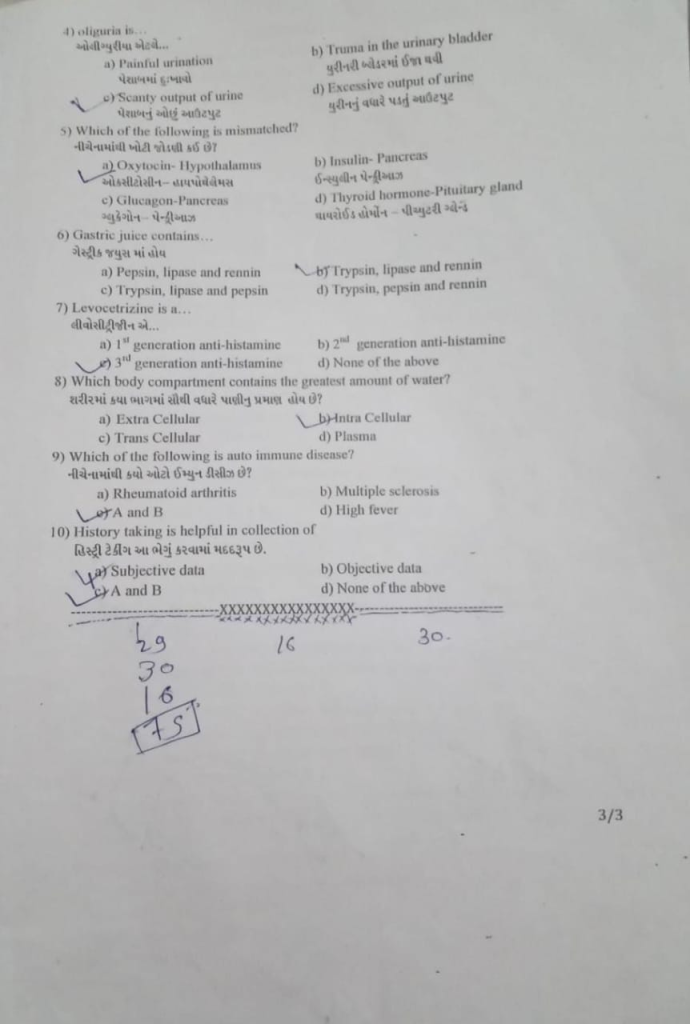
4) oliguria is……
a) Painful urination
b) Trauma in the urinary bladder
✅ c) Scanty output of urine – low output of urine
d) Excessive output of urine
-> Oliguria is defined as low urine output, typically less than 400 mL/day in adults.
5) Which of the following is mismatched? Which of the following is the incorrect spelling?
a)Oxytocin-Hypothalamus
b) Insulin- Pancreas Pituitary Gland
-> Thyroid hormone is produced by the thyroid gland, not the pituitary.
6) Gastric juice contains…Gastric juice contains
✅ a) Pepsin, lipase and rennin
b) Trypsin, lipase and rennin
c) Trypsin, lipase and pepsin
d) Trypsin, pepsin and rennin
-> These are the primary enzymes in gastric juice.
7) Levocetrizine is a…Levocetrizine is a…
a) 1st generation anti-histamine
✅ b) 2nd generation anti-histamine
C) 3rd generation anti-histamine
d) None of the above
-> Levocetirizine is a second-generation antihistamine used in allergy treatment.
8) Which body compartment contains the greatest amount of water? Which part of the body has the highest water content?
a) Extra Cellular
✅ b) Intra Cellular
c) Trans Cellular
d) Plasma
-> Around 2/3 of body water is present in the intracellular compartment.
9) Which of the following is auto immune disease? Which of the following is an auto immune disease?
a) Rheumatoid arthritis
b) Multiple sclerosis
✅ c) A and B (Rheumatoid arthritis and Multiple sclerosis)
d) High fever
->Both are classic autoimmune disorders.
10) History taking is helpful in collection of…..History taking is helpful in collection.
✅ a) Subjective data
b) Objective data
c) A and B
d) None of the Above
-> History includes patient’s personal experiences and symptoms, which are subjective data.
