ENGLISH GYNECOLOGY GNM UNIT 4
UNIT 4 PELVIC INFECTIONS.
Sexually Transmitted Diseases:
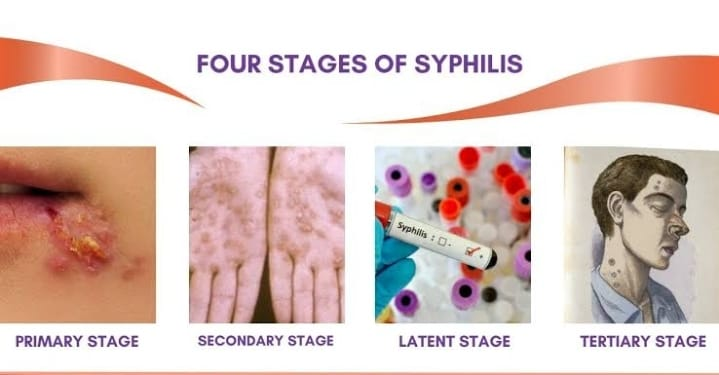
- Syphilis:
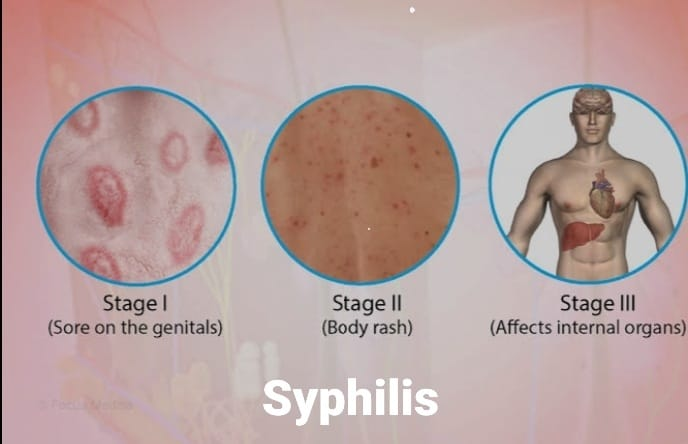
Syphilis is a sexually transmitted disease.
The causative organism of syphilis is the spirochete Treponoma palladium. This disease usually starts with syphilitic lesions in the genital tract and occurs mainly in the genitals, rectum and mouth. The disease is caused by direct contact with other persons who have primary or secondary syphilitic lesions. Its incubation period is 9-90 days. These symptoms are mainly seen in nine days and last up to three months.
Reasons:
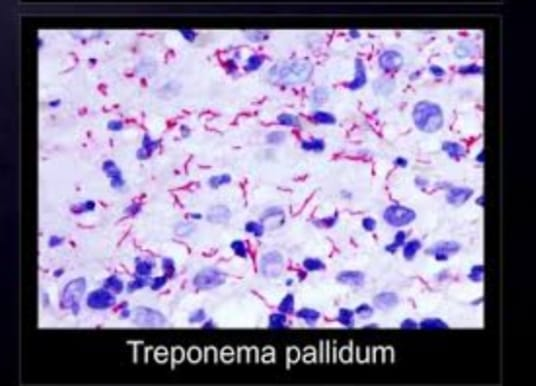
The spirochete Treponema pallidum,
Due to coming in contact with any infected person,
Unprotected sexual activity,
Due to contact with infected blood or bloody fluid.
Due to engaging in sexual activity with multiple partners.
Due to coming in contact with an infected partner.
Symptoms and signs:
The symptoms depend on the stage of syphilis. such as,
1) Primary stage
2) Secondary stage
3) Latent stage
4) Late stage
1) Primary Syphilis:
Primary syphilis occurs two to eight weeks after exposure to the bacteria. It starts with a small round sore called a chancry which is painless but highly infectious.
Small papule and lesion
A sore can be single or multiple.
Sore is also present on lips, tongue, hands, rectum and nipple.
A painless ulcer without any surrounding inflammatory reaction,
Inguinal gland enlargement.
2) Secondary Stage:
The secondary stage starts two to four weeks after the appearance of the sore and lasts for two to four years.
low grade fever,
headache,
loss of appetite,
weight loss,
anemia,
sore throat,
horseness,
Jaundice with or without hepatitis,
Pain in joints, muscles, long bones,
Cores, flat top, moist and necrotic lesions.
3) Latent Stage:
This is the third stage of syphilis. This stage lasts mainly for five to 20 years. It is mainly asymptomatic but can affect multiple organs.
Tumors occur in the skin, bones, and liver.
4) Late Stage:
This is the last stage of syphilis and about 15 to 30 percent of people who do not receive syphilis treatment enter this stage and the duration is very long and this last stage is a life threatening condition.
A tumor-like mass is created in this.
Damages the heart valves and blood vessels.
Meningitis (infection and inflammation of the meninges layer of the brain,
Paralysis.
There is no coordination.
Sleep is reduced.
Confusion.
Impaired judgment.
Slurred speech.
Difficulty seeing.
Deafness comes.
Mental Illness.
Memory decreases.
Diagnostic Evaluation:
History Collection,
Physical Examination
Blood test:
A blood test is done to see if any syphilis antibodies are present in the body.
Cerebrospinal fluid analysis.
vdrl test.
fta-abs (Fluorescent Treponomal Antibody Absorption) test is specific for treponoma palladium test.
Medical management
Treatment of syphilitic lesions is divided into three stages:
1.Early Syphilis: (Primary, Secondary and Early Latent Syphilis)
a Benzathine Penicillin G 2.4 Mega Unit I/ M Single Dose Itch Batak Ma. Half dose.
b. Procaine Penicillin G 600,000 units I/M daily for 10-14 days.
c. In penicillin hypersensitive cases, tetracycline or erthyromycin 500 mg orally 4 times a day for 14 days
- Late Syphilis: Benzathine Penicillin G 2.4 mega units I/ M weekly given for 3 wks.
3) Follow-up:
Serological tests are done 1, 3, 6 and 12 months after treatment of early syphilis.
In late symptomatic cases, for lifelong surveillance, serological tests are performed annually.
Nursing Management:
Treatment should be started as soon as the disease is detected.
The patient should be examined at 3rd, 6th, and 12 months to control the disease.
Avoid coming in contact with a person who has syphilis infection.
A detailed examination of the person who is suspected should be done.
Provide education to the patient on barrier method contraceptive use.
Treat the patient symptomatically.
Educating the patient to take proper treatment.
Continuous abstinence until recovery from syphilis or any sexually transmitted disease.
Provide patient education on using the barrier method as a contraceptive.
To maintain patient privacy and confidentiality.
Ask the patient to take regular follow-up.
Providing education to patients about sexual hygiene.
- Gonorrhea:

Gonorrhea is a common sexually transmitted venereal disease. Gonorrhea affects both men and women. The causative organism of gonorrhea is Neisseria gonorrhoea. This infection is mainly transmitted in the genitourinary system involving the genital organ, the rectum.
If this disease is not treated, fever and arthritic conditions can occur. If the hand is contaminated by this organism, there are chances of the infection spreading to the eye as well. Gonorrhea infection is mainly seen in the age group of 15 to 24 years. Gonorrhea is also known as “the clap” or “the drip”. Its incubation period is 3-7 days.
Causes of Gonorrhea:

Neisseria gonorrhoeae bacteria,
It is transmitted through vaginal, oral and anal sexual contact
If there is any prior history of gonorrhea.
Any other sexually transmitted infection.
If the hygienic condition of the genital area is not maintained properly.
If previously diagnosed with gonorrhea.
Sexual activity started early.
Have multiple sex partners.
If a pregnant mother has gonorrhea, she can transmit the infection to her baby.
State the symptoms and signs:
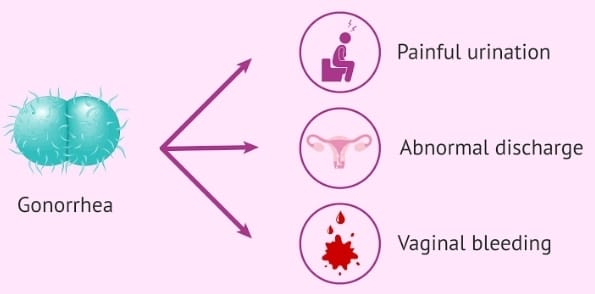
Man:
Burning sensation occurs during urination.
Purulent discharge from the penis.
Frequency of urination increases.
Pain, redness and soreness occur.
Urethral scarring.
Enlarge scrotum.
Pain and itching sensation during urination.
Inflammation of the prostate gland and testicles.
A yellow and green thick discharge comes out from the tip of the penis.
Female:
Purulent discharge.
Discomfort and aching pain over the abdomen.
Burning sensation.
There is urgency and frequency in urination.
There is difficulty in walking.
(Salpingitis: Infection and inflammation of the fallopian tubes).
fever,
vomiting,
low back pain,
Pain during intercourse,
Discharge from the vaginal area that is thin or thick yellow and green.
There is discharge and irritation from the anal area. Bleeding occurs.
Tenderness is felt in the abdomen and pelvic area.
Diagnostic Evaluation:
historytaking,
Physical Examination,
swab test,
Culture from cervix, urethra, rectum or throat.
Urine Examination.
Nucleic acid test.
Gram staining.
Medical management
Specific treatment for gonorrhea is a single dose of any of the following medicines:
Ceftriaxone: 125 mg I/M
Ciprofloxacin: 500 mg orally.
Ofloxacin: 400 mg orally.
Cefixime: 400 mg orally.
Levofloxacin: 250 mg orally.
Conjunctivitis of the newborn is treated with a single dose of ceftriaxone (20-30 mg/kg) IM and gentamicin eye ointment (1%).
Follow-up: Culture should be done after 7 days of therapy. Repeat culture is done after 3 months at monthly intervals.
Nursing Management:
Taking a proper history of the patient.
Providing proper antibiotic medicine to the patient.
Perform serum examination for syphilis.
Provide proper education to the patient about personal hygiene.
Providing proper education to the patient about the disease condition.
Advise the patient to avoid multiple sex partners.
Educating the patient to use the barrier method of contraception.
Provide proper psychological support to the patient.
Providing antibiotic medicine to prevent infection.
Ask the patient to maintain personal hygiene.
Complications:
Pelvic Inflammatory Disease (PID),
infertility,
ectopic pregnancy,
dyspareunia,
Chronic pelvic pain, tubo-ovarian mass,
Bartholin gland abscess.
- AIDS (Acquired Immunodeficiency Syndrome):

Acquired Immunodeficiency Syndrome (AIDS) is a fatal illness. It is mainly transmitted by human immunodeficiency virus (HIV). Once a person is infected with HIV, it remains for life. H. HIV weakens a person’s immune system, so a person can easily get any infection in the body. So AIDS is not a single symptom but a set of many symptoms hence called a syndrome. Its incubation period ranges from 2 months to 4 years.
Reason:
Human immunodeficiency virus,
Hiv 1,
Hiv 2,
Sex worker
health care worker,
Due to contact with blood semen, cerebrospinal fluid, teats, saliva, breast milk, cervical or vaginal secretions of any HIV infected person.
Due to sexual activity with an HIV infected partner.
Due to injecting infected needle and syringe.
Transmission can occur through an infected mother to her child.
Due to contact/exposure to contaminated blood.
Blood transfusion.
Organ Transfusion.
Due to coming into contact with a person who already has syphilis or any other sexually transmitted disease.
Symptoms and signs:

weight loss,
diarrhea,
arthralgia,
Continuous cough for a month,
fever,
pharyngitis,
lymph node swelling,
Muscular system weakness,
dyspnea,
one head,
Liver enlargement.
Headache.
Sore throat.
Enlargement of the spleen.
Mouth Sore.
Nausea and vomiting.
Skin lesions.
feeling tired
Oral ulcers.
Loss of appetite.
Weight loss.
Sweating at night.
Swelling in the lymph nodes.
Diarrhea
Soreness in the mouth, anus and genital area.
Rashes falling into the skin. Neurological symptoms are seen.
Mode of Transmission:
Spread:
1) Sexual Transmission: HIV and AIDS are transmitted through sexual contact.
2) Transmission through blood:
Transmission of AIDS also occurs through the transmission of infected blood or by coming in direct contact with any infected blood.
3) Perinatal transmission:
Can be transmitted from infected mother to child.
Diagnostic Evaluation:
History Collection,
Physical Examination.
Recombinant DNA
t technique
PCR (Polymerase Chain Reaction).
ELISA (Enzyme Linked Immunosorbent Assay).
Viral isolation in culture.
Lymph node biopsy.
Rapid Hiv Antibody Test.
Western blot antibody testing.
Hiv viral load test.
Complete blood count.
CD4CELL Count.
Medical management
1) Nucleoside reverse transcriptase inhibitor (NRTI).
EX:= LAMIVUDINE
ZIDOVUDINE.
2)Non Nucleoside Reverse Transcriptase Inhibitor (NNRTI):
EX:= EFAVIREN
(SUSTIVA).
ETRAVIRINE
(INTELLENCE).
3) Protase inhibitors:
Ex:= ataxanavir.
Duranavir.
4) Entry or fusion inhibitor
EX:=enfuvirtide
(fuzeon),
Maraviroc
(selzentry).
5) Integrase inhibitors:
EX:=raltegravir
(isentress).
Nursing Management:
Provide proper position to the patient.
Advise the patient for deep breathing exercises.
Providing proper oxygen to the patient.
Maintain the patient’s hydration status.
Assessing the patient’s nutritional status.
Provide the patient with a diet that is high in protein and high in calories.
Providing fresh fruits, vegetables, whole gain and protein to the patient.
Provide easily digestible food to the patient.
Daily mouth care to the patient.
Providing food that the patient likes.
Maintaining social support of the patient.
Spend time with the patient.
Interacting properly with the patient and his family members.
Assessing the patient’s skin integrity.
Providing back care to patients.
Tell the patient about the importance of personal hygiene.
Keeping the patient away from the person who has the infection.
Patients using a barrier method as contraceptives.
If the patient is a smoker, give advice to avoid smoking.
Ask health care workers to maintain strict aseptic technique.
Prevention
Provide patient education to avoid unprotected sexual contact and use barrier method A contraceptive.
Avoiding pregnancy to a mother who has any sexually transmitted disease. Because that infection can also be transmitted to her child.
To provide advertisement in mass media and television to bring awareness about Sexual Health.
Any kind of blood or organ donation should not be done to a person who is infected with HIV.
Proper test should be done before blood transfusion.
Using streak sterilization practices in hospitals and clinics.
Do not use used needles and syringes.
Blood and body fluids of an infected person should not come in contact.
Provide proper education about AIDS to patients.
Provide antiviral treatment to the patient.
Providing psychological support to the patient.
HIV is a sexually transmitted disease.
Do not use used razors.
Do not use a used toothbrush.
Do not use used needle and thread.
Use disposable needles and syringes.
If the needle and series are to be reused, they should be used only after proper autoclaving.
Pregnancy should be avoided if a woman has AIDS or infection because there are chances of AIDS and HIV being transmitted to the newborn baby.
To provide education in human being about what steps can be taken for prevention of Aids and Hiv.
Using all types of mass media and technology to create awareness among individuals about the measures that can be taken for the prevention of HIV and AIDS.
Advise to avoid donation of blood and other body organs to persons who are at high risk of HIV and AIDS.
Screening for HIV and AIDS when blood is to be transfused or drawn.
Using sterilization techniques in hospitals and clinics.
Use disposable needles and syringes whenever possible.
If not possible, use sterilized needles and syringes.
Using zidovudine tablets as curative measures.
Avoid contact with infected blood and body fluids.
Medical personnel should observe universal precautions and use personal protective equipment (PPE) kits when blood and body fluids come into contact.
Take extreme precautions when doing injections and skin piercings.
Effective use of sterilization and disinfectants.
Provide education about AIDS to the person.
A=Avoidable,
I=Incurable,
D=Disease,
S=Syndrome. Providing health education about
To properly explain the AIDS disease to the student.
Also educating people that AIDS is not spread by any kind of fly or mosquito but through unprotected sexual contact.
Educating people that AIDS is not spread through clothes but through blood and body fluids.
Proper precautions should be taken by the staff members working in the hospital who do not have HIV and AIDS.
Giving antiretroviral therapy to a person who has HIV and AIDS.
- Genital Watts:
Definition:
Genital warts are small, non-cancerous growths or lesions that appear in the genital and anal area due to viral infections. It is caused by a specific type of human papilloma virus (HPV). These vats can differ in size and shape, and can be flat or raised. They are often transmitted through sexual contact and may be asymptomatic, but sometimes cause itching or discomfort.

Mode of Transmission:
sexual contact,
throw infant ((at delivery).
Symptoms and signs:
Small, flash colored and gray growths are seen in the genital area like vulva, penis and scrotum and anus region.
Cauliflower-like cluster warts can form large clusters with a cauliflower-like appearance.
Itching: Itching and irritation in the affected area.
Disc Comfort: Burning around watts and filling disc comfort.
Bleeding: Bleeding due to irritation and scratching from vats.
Diagnostic Evaluation:
cervical smear,
Colposcopy.
Treatment:
If vata occurs during pregnancy, no treatment is required
Because it can be treated after delivery.
2.Cryotherapy (to decrease size).
- Electrocauterization (to excise the wattles).
vulva
Vulvitis:
Definition:
Infection and inflammation of the vulva is called vulvitis.
Vulvitis usually occurs for three reasons:
Vulvitis due to specific infection.
Vulvitis due to sensitive reaction.
Vulvitis due to vaginal discharge or urinary contamination
Vulvitis due to specific infection:
It can be of four types:
1.Bacterial:
a Pyogenic or non gonococcal
b tubercular
c Sexually transmitted diseases (gonorrhea, chancroid, lymphogranuloma venereum, syphilis, granuloma inguinal).
- Viral:
a Herpes genitalis
b Herpes zoster
c Condylomata acuminata
- Fungal:
a ring worm
b Moniliasis (Candida albicans)
- Parasitic :
a Pediculosis pubis
b Scabies
c thread worm.
Bacterial pyogenic or non-gonococcal:
- Vulval cellulitis,
2.Furunculosis,
3.Sebaceous and apocrine gland infections. - Impetigo
- Erysipelas
- Intertrigo.
- Infection due to trauma.
- Vulval Cellulitis:
It may be due to unhygienic conditions associated with small scratches on the vulva and due to this, severe cellulitis may occur.
Causative organism:
Staphylococcus aureus.
Symptoms and signs:
Vulva swollen, red and tender (severe pain on touch).
Severe pain
Severe etching.
Problems in micturition.
Excoriation of the skin (epidermis layer) due to scratching and laceration. Treatment:
systemic antibiotic,
Local Hot Compress,
Analgesic medication if there is a pain condition
2.Furunculosis:
An infection that affects the hair follicles of the mons and labia majora is known as folliculitis which in further infection is known as furunculosis.
Causative organism:
Staphylococcus aureus.
Treatment:
- Systemic and local antibiotics are given.
- Patient is advised to maintain cleanliness.
- Analgesics are provided for pain relief.
3.Sebaceous and Apocrine Gland Infection:
Sebaceous and apocrine gland infections show symptoms of boils (inflammation of sebaceous tissues).
Treatment:
Excision of the boil
- Impetigo:
It is a pustular infection caused by Staphylococcus aureus and/or Streptococcus.
Symptoms and signs:
Vulval region infection
The infection can spread to other parts of the body, the face or hands.
There is formation of pus.
In some cases, after the formation of pus, a crust may form.
- Blebs may form (extra growth). Treatment:
Systemic and local antibiotics are provided.
If blebs are present, they are excised.
If crust is present it is removed aseptically.
- Erysipelas:
This is a rare condition in which tissue becomes inflamed and transmitted to systemic disturbances upon infection.
Causative organism:
Beta hemolytic streptococcus.
Treatment:
A broad spectrum antibiotic is provided.
- Intertrigo:
It is due to irritation and infection of secretions retained in folds of skin, especially in obese patients. It can also be caused by the friction of under garments and sanitary towels.
Treatment:
Giving advice to properly maintain hygiene.
Provide antiseptic cream for local application.
Provide systemic antibiotics.
Dusting with starch or zinc oxide powder.
- Infection due to trauma
Infection of the perineum can occur after birth trauma or gynecological operations or through nail scratches.
Treatment:
Provide proper antibiotic medication as prescribed.
If pus is formed then provide local antiseptic dressing.
Viral infection:
Herpes zoster
Causative agent:
Varicella Zoster (VZV)
Symptoms and signs:
Inflammatory pain full eruption of groups of vesicles distributed or present on the skin.
Vesicles may rupture or dry up.
Treatment:
Provide analgesic medication to relieve pain.
Provide antibiotic medication to prevent secondary infection.
Acyclovir 800 mg (daily) given orally 5 times daily 1 wk or
7 days.
Acyclovir cream 5 percent is used locally for less severe infections.
Fungal infection:
Moniliasis:
Causative organism:
Candida albicans
Risk Factors:
diabetes mellitus,
Patients taking broad spectrum antibiotics,
Renal disorders during pregnancy.
Symptoms and signs:
vulval inflammation,
The inflamed area looks like raw beef.
Treatment:
Provide proper antibiotic medication to the patient.
If glycosuria is present, treatment of diabetes is necessary.
Instruct patient to wash vulva after micturition and maintain perineal cleanliness.
Ring Worm:
Causative organism:
Tinea cruris.
Symptoms and signs:
Bright red color license to see.
Treatment:
Clotrimazole/miconazole cream or ointment for local application.
Tablet Albendazole.
Tablet griseofulvin 500 mg for 1 month.
Parasitic infection:
Threadworm
Causative organism:
Oxyuris vermicularis. It is common in children and seen in stool.
Symptoms and signs:
Noctural perineal itchig
Perineal excoriation.
Treatment:
An anthelmintic drug such as mebendazole or local application of gentian violet is given.
Vulvitis due to sensitive skin Reaction of the skin:
The vulva is very sensitive to many agents or chemicals and can sometimes produce an allergic reaction or contact dermatitis. Such agents or chemicals are listed below:
Drugs used to treat pruritus-local application.
- Soap, detergent, powder.
- Contraceptive cream or jelly or foam tablet and condom etc.
Symptoms and signs:
Intense infection of the vulva or it is swollen.
Vesicles may appear.
Pruritis.
Treatment:
There is no specific treatment. It can be fixed in a few days.
Calamine lotion or cream is used.
Antihistamine meditation should be avoided.
Vulvitis due to vaginal discharge and contamination:
In case of continuous vaginal discharge, the area will become moist and cause the growth of this organism and eventually infection which can lead to inflammation of the vulva.
Causative organism:
candida albicans,
Trichomonas vaginalis.
Treatment:
Antibiotics are given to treat vaginal or UTI infections.
Check the patient for diabetes mellitus as it is a primary cause of infection.
Soothing lotion or calamine lotion can be applied.
- Bartholinitis:
Definition:
Bartholinitis: An infection and inflammation condition of Bartholin’s gland, an almond-shaped gland on the side of the vaginal opening. Their primary function is to produce mucus that helps lubricate the vaginal canal, infection and inflammation of the Bartholin’s gland is called Bartholinitis condition.
There are mainly four types of bartholinitis.
- Acute bartholinitis
- Recurrent bartholinitis
- Bartholin’s abscess
- Bartholin cyst
- Acute Bartholinitis: Sudden, severe infection and inflammation of one or both Bartholin’s land is called Bartholinitis.
Causative organism:
gonococcus,
E-coli,
staphylococcus,
Streptococcus and
Chlamydia trachomatis.
Symptoms and signs:
local pain,
discomfort,
Difficulty in walking and sleeping.
On examination the duct appears congested and tender.
Treatment:
Provide proper hot compresses to the patient.
Providing analgesic medicine to the patient to reduce the pain level.
Provide proper antibiotic medication to the patient.
Ex: Provide Ampicillin 500 mg orally 8 hourly.
- Recurrent Bartholinitis:
Periodic painful infection and inflammation of the Bartholin’s gland and if the condition occurs repeatedly, this condition is called recurrent Bartholinitis.
Symptoms and signs:
local pain,
discomfort,
Difficulty in walking and sleeping.
On examination the duct appears congested and tender.
Treatment: Excision of the inflamed duct and gland is done to reduce repeated infection and inflammation.
Provide proper hot compresses to the patient.
Providing analgesic medicine to the patient to reduce the pain level.
Provide proper antibiotic medication to the patient.
Ex: Provide Ampicillin 500 mg orally 8 hourly.
- Bartholin’s Abscess:
It is the formation of an abscess or pus in the duct that causes blockage in the duct resulting in accumulation of exudates in the duct and if left untreated the abscess may be transmitted to the lower vaginal wall.
Symptoms and signs:
fever,
Local pain and discomfort,
The patient cannot walk or sit.
Labia majora becoming tender.
Skin is red and oedematous.
Treatment:
If the patient has a pain condition, provide analgesic medication.
Hot compression is given.
Systemic antibiotics are given according to culture and sensitivity test to reduce infection. The most commonly used antibiotics are ampicillin and tetracycline.
The abscess is drained as soon as possible to prevent it from rupturing.
Marsupialization is carried out.
It is a procedure that helps in drainage of pus or cysts are removed.
The procedure is performed under general anesthesia.
An opening is made on the middle part of the labia minora to remove the cyst.
In this, the sac is incised and its edges are stitched.
- Bartholin cyst
A Bartholin cyst is a fluid-filled sac that blocks the Bartholin gland on either side of the vaginal opening. This gland secretes a fluid that helps lubricate the vagina. When the duct of the Bartholin gland becomes blocked, fluid collects, leading to cyst formation. Bartholin’s glands are usually painless and may not cause symptoms unless they become infected or enlarged.
Etiology:
infection,
trauma,
injury.
Symptoms and signs:
Swimming in Libya Majora,
local discomfort,
dyspareunia,
Skin a thin and signing,
Cysts are fluctuant and non-tender.
Treatment:
Marsupialization is the only treatment.
Vaginal infection
- Vaginitis:
Infection and inflammation of the vagina is called vaginitis.
Types:
There are seven types of infection:
- Vulvo vaginitis.
- Trichomoniasis.
- Moniliasis.
4.Vaginitis due to Chlamydia trachomatis. - Atrophic vaginitis.
6.Nonspecific vaginitis.
7.Toxic shock syndrome
Vulvo vaginitis:
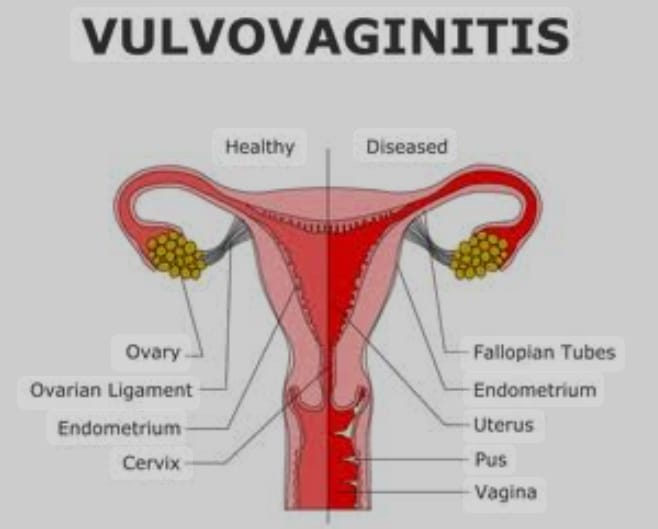
Vulvovaginitis means infection and inflammation of the vulva, (external female genitalia) and vagina is called vulvovaginitis.
Etiology
Fungal infections such as candida albicans.
Bacterial infections such as bacterial vaginosis.
Sexually transmitted infections such as gonorrhea, chlamydia and tracheomoniasis, gonococcal infections.
Chemical irritant substances,
allergens,
Hormonal changes like,
Pregnancy and menopause,
Due to presence of foreign body in vaginal area,
Thread worm infestation.
Symptoms and signs
Itching on the vulval and vaginal area,
pruritus,
Redness and swelling in the vulva,
Abnormal discharge,
Pain and burning sensation,
Sensitivity and soreness of the vulval area.
Pain and burning sensation.
Increased vaginal moisture.
Offensive vaginal discharge.
Painful micturition.
Labia minora small and red.
Diagnostic Evaluation:
Examination of vaginal discharge,
Culture and Media,
Stool examination.
Treatment:
In some cases the cause is unknown so simple perineal care helps.
If soreness is present, apply estrogen locally every night for 2 weeks.
Alternatively, tablet Ethinyl estradiol 0.01 mg OD is prescribed for 3 vaginal defenses.
Antibiotics are provided for culture and media.
Antihelminthic is provided for worm infestation.
Trichomoniasis:
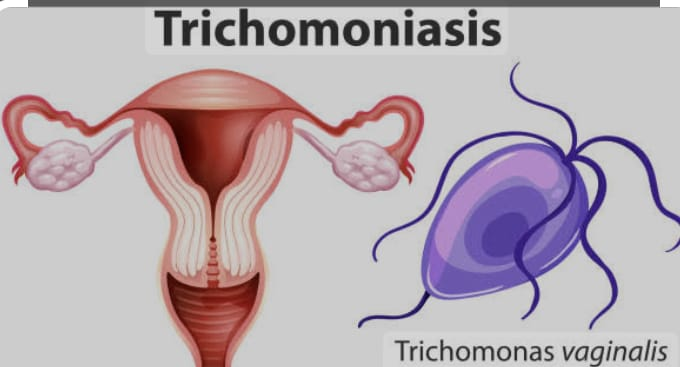
Vaginal trichomoniasis is an important cause of childbearing period.
Etiology:
It is transmitted by Trichomonas vaginalis through sexual contact or from one woman to another through toilet articles.
Symptoms and signs:
Sudden offensive profuse vaginal discharge,
Irritation and itching around the interstitials,
dysuria,
Frequency of Micturation,
On examination pass greenish yellow vaginal discharge.
Vaginal examination becomes painful.
Diagnostic Evaluation:
Vaginal discharge culture media.
Treatment:
- Tab. Metronidazole TDS for 1 vic.
2.Husband is also given the same treatment up to one week.
3.Advising couples to use barrier method during coitus act until wife is cured.
4.If symptoms persist, a second course of treatment is given after an interval of 7 days.
- In case of severe infection, a vaginal tablet containing Clotrimazole 100 mg is introduced into the vagina daily for continuous 6 nights.
- Local application is indicated in early pregnancy and lactation.
Moniliasis (Candida vaginitis):
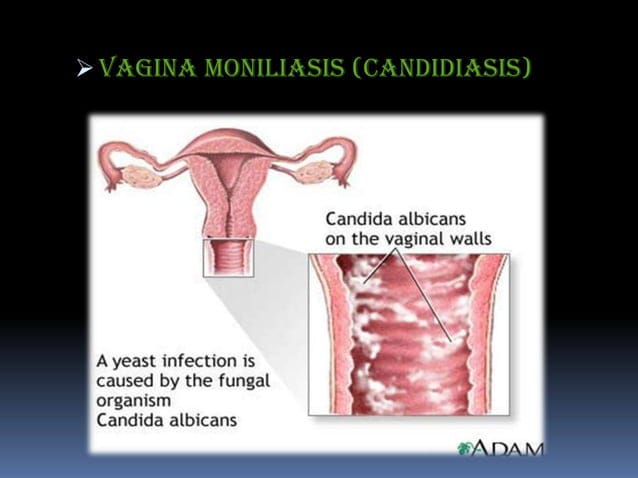
Moniliasis is caused by a Candida albicans infection caused by a gram-positive yeast like fungus.
Etiology:
Yeast infection occurs when there is a common environment change in the vagina.
Eg: Poor hygienic condition (dirty underwear and transfer of faecal yeast.
Prolonged use of antibiotics.
Use of oral contraceptives.
Transmitted through sexual contact.
Symptoms and signs:
Vaginal discharge.
Discharge is thick curdy white.
The vulva is red and swollen.
Pruritus.
Dyspareunia.
A white color flake should be present in the vajaina. Multiple wearing spots are seen removing white flakes.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Culture and Media,
Direct smear of discharge or flakes.
Treatment:
Use vaginal cream.
The patient is provided with fluconazole tablets 50 mg OD for 7 days.
Treatment should be done locally with nystatin ointment.
Advising couples to use contraceptive methods.
Treatment is continued even during menstruation.
Vaginitis due to Chlamydia trachomatis:

Vaginitis due to chlamydia trachomatis is a sexually transmitted disease that causes the condition of vaginitis and urethritis.
Etiology:
Chronic trachomatis infection
Symptoms and signs:
Irritant mucopurulent discharge,
Dysuria.
Diagnostic Evaluation:
Tissue culture serological test (VDRl)
Treatment:
Cap. Tetracycline 500 mg 4 times in a day is provided for up to 1 week.
Atrophic vaginitis (senile vaginitis):
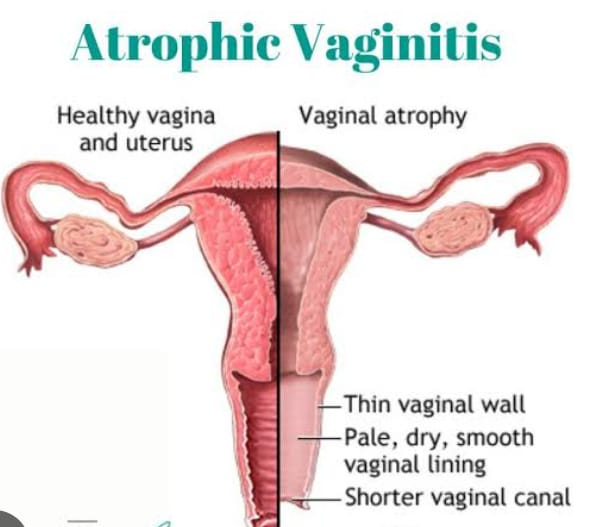
If the condition of vaginitis arises in post-menopausal women, this condition is called atrophic vaginitis.
Etiology:
Due to estrogen deficiency.
Symptoms and signs:
pruritus,
Vaginal wall inflammation,
Discomfort and soreness present in the vulva.
Having a painful vaginal examination.
Postmenopausal yellowish blood stained vaginal discharge.
Diagnostic evaluation:
History Collection,
Physical Examination,
Diagnostic curettage biopsy,
Pap smear.
Treatment:
Local application of estrogen vaginal cream.
Ethinyl estradiol 0.01 mg OD is provided for 3 weeks.
Nonspecific vaginitis:
Nonspecific vaginitis is due to a foreign body or infected body such as a (ring) pessary, tampons, IUD, child birth trauma, or vaginal operation.
Symptoms and signs:
Offensive vaginal discharge,
pruritus,
vulval irritation,
tender red swollen vaginal mucosa,
Diagnostic Evaluation:
History Collection,
Physical Examination
Treatment:
Improvement of general health.
Removal of foreign body.
Supply of bactericidal cream for 7 days.
Vaginal tablets inserted into the vagina are provided twice a day for 10 days.
Toxic Shock Syndrome (TSS):
It is seen in menstruating women between 15-30 years.
Symptoms and signs:
fever,
Vomiting and diarrhoea,
hypotension,
races,
Acute respiratory distress syndrome.
Diagnostic Evaluation:
blood culture,
Serum electrolytes
Treatment:
Supportive treatment is provided.
Hypovolemia is corrected.
The condition of hypotension is corrected.
Corticosteroids are provided by the parenteral route.
Tab. Cloxacillin is provided for 2 wk.
- Metritis:
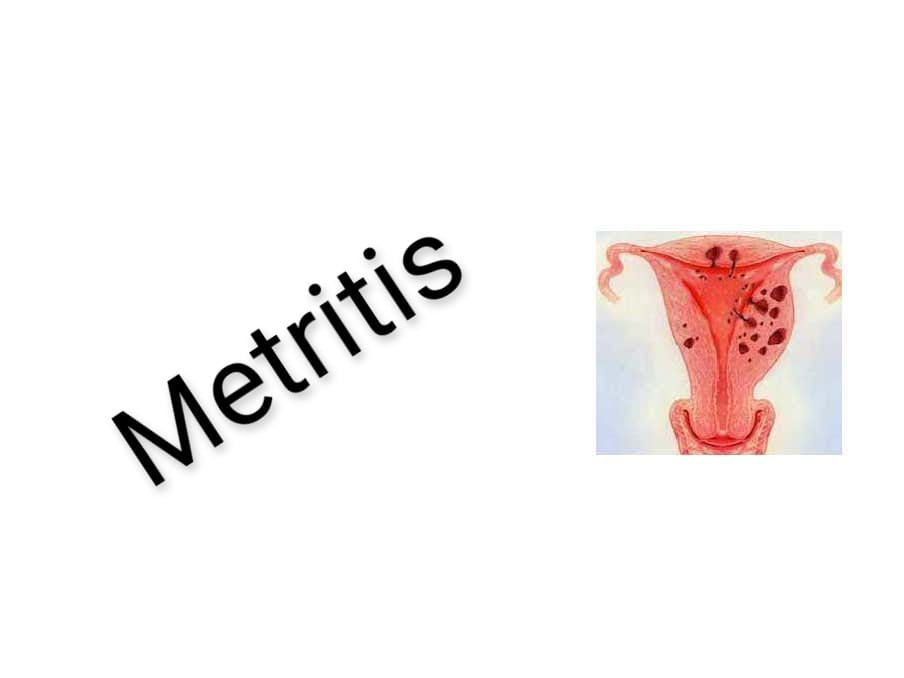
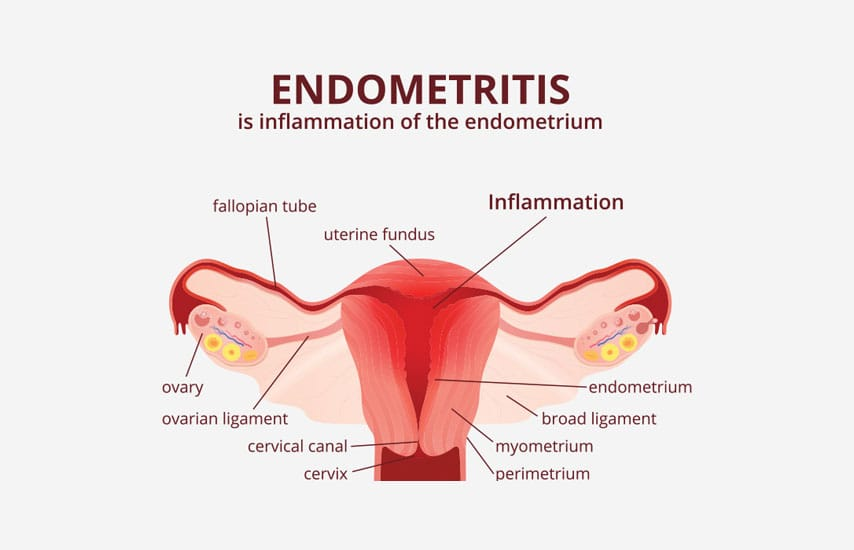
The condition of infection and inflammation in the wall of the uterine cavity is called metritis. Generally there are three layers of uteride KVT viz.,
The outer most layer is called 1) Perimetrium. Middle layer which is called 2) myometrium and innermost layer which is called 3) endometrium thus infection and inflammation occurring in any of these three layers of the uterus is called metritis.
If infection and inflammation occurs in the outer most layer of the uterus such as perimetrium, then the condition is called perimetritis. If infection and inflammation occurs in the middle layer of the uterus such as myometrium, then the condition is called myometritis. If the inner most layer of the uterus such as If infection and inflammation occurs in the endometrium, the condition is called endometritis.
Types of Metritis:
Generally there are three types of metritis namely,
1) Acute metritis
2) Chronic metritis
3) Atrophic or senile endometritis
1) Acute metritis:
The condition of acute metritis usually arises after abortion or child birth.
Etiology:
Organisms can generally be endogenous or exogenous.
Placental site (organisms can multiply easily due to open wound).
Lokia.
Symptoms and Signs:
fever,
pelvic pain,
Profuse offensive vaginal discharge,
Local discharge present,
Abdominal pain and cramps.
Rapid pulse and increased heart rate,
Chronic Metritis:
It is a rare condition but if it occurs, it is due to cyclic shedding of infected endometrium and constant drainage of infected material.
Etiology:
Infected endometrium due to growth of organisms,
Due to IUCD infection,
Infected polyps,
retained polyps,
fibroid uterus,
tubercular infection,
Endometrial burns caused by caustics or radiation (especially with radium).
Diagnostic evaluation:
History Collection,
Physical Examination,
USG,
blood testing,
Cervical culture,
endometrial biopsy,
laparoscopy,
Hysteroscopy.
Symptoms and signs:
Dysmenorrhea (painful menstruation),
dyspareunia,
Abnormal vaginal discharge,
Discomfort during bowel movements,
fever,
general discomfort,
malays,
Pain in lower abdominal and pelvic region,
purulent vaginal discharge,
The uterus becomes slightly bulky and enlarged and the condition of heavy menorrhagia arises.
Treatment:
Provide proper antibiotic medication after culture and sensitivity test.
Advise for hysterectomy if the patient is in menopausal condition.
Atrophic or senile metritis:
Atrophic or senile metritis usually arises due to estrogen deficiency which reduces the immunity of the uterocervical vaginal canal.
Symptoms and Signs:
offensive vaginal discharge,
Blood stained vaginal discharge,
Uterus enlarges, becomes soft and tender,
Purulent discharge escaping from the cervix.
Diagnostic Evaluation:
History Collection,
Physical Examination,
Histological examination,
Performing diagnostic curettage in the condition of pyometra.
Atrophic or senile endometritis is always confused with CA Cx, all tests should be done to exclude CA Cx.
Treatment:
Estrogen supplements are given in the form of ethinyl estradiol 0.01 mg OD for 4 wk or 1 month. It will help in healing of endometrium.
In pyometra, drainage of pus is done with simple cervical dilatation and after 2 weeks, diagnostic curettage is done under coverage of antibiotics.
In unresponsive cases, hysterectomy is performed and the specimen is sent for histological examination.
Assessing the level of infection.
Use of aseptic technique for abortion.
Use of sterile articles to prevent infection.
Properly assess if there is endometrial burn due to radiation.
Advise on handwashing before any procedure.
Advise the patient to maintain personal hygiene.
Encouraging the patient to properly clean the genital area after defecation and urination.
Provide a comfortable position to the patient.
If the patient has an infection, then provide antibiotic medication and if there is a pain condition, analgesic medication should be provided as per the prescription.
If the patient has fever then provide antipyretic medication.
- Salpingitis:
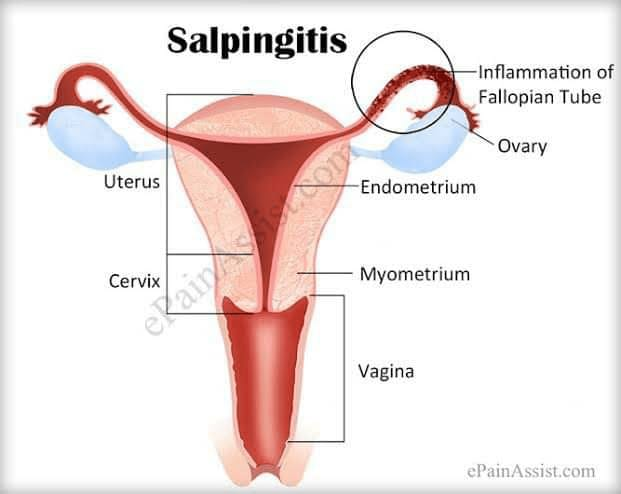
Salpingitis is a gynecological condition in which infection and inflammation of the fallopian tubes is called salpingitis. It is often caused by a sexually transmitted infection (STI) and can cause symptoms such as pelvic pain, fever and abnormal vaginal discharge. If left untreated, salpingitis can lead to complications such as infertility or ectopic pregnancy.
The infection is usually polymicrobial in nature and usually affects both fallopian tubes. The ovary is usually involved in the inflammatory process and is therefore called salpingo-oophoritis.
Types of salpingitis:
There are usually two types of salpingitis:
1) Acute salpingitis,
2) Chronic salpingitis
1) Acute salpingitis
: This type of acute salpingitis starts suddenly and is often associated with bacterial infections, such as those caused by sexually transmitted pathogens such as gonorrhea or chlamydia.
Among its symptoms, the fallopian tube is red and swollen and the inner wall of the fallopian tube sticks to each other and sometimes the fallopian tube can rupture.
2) Chronic salpingitis:
If acute salpingitis is not treated properly, it can lead to chronic salpingitis.
Etiology of salpingitis:
Sexually Transmitted Infection (STI):
Chlamydia trachomatis
Neisseria gonorrhoea
Other bacterial infections:
Mycoplasma species Ureaplasma species
Escherichia coli (E. coli),
staphylococcus,
Streptococcus
Post surgical and post abortion infections:
Pelvic surgery or abortion Abortion infection
Tuberculosis:
Mycobacterium tuberculosis
Chronic pelvic inflammatory disease (PID):
Due to prolonged or repeated infections
Autoimmune conditions:
Sometimes seen due to autoimmune disorders.
Symptoms and signs:
lower back pain,
Abnormal vaginal discharge,
Painful sexualintercourse,
spotting between periods,
painful menstruation,
Pain during ovulation,
fever,
Nausea and vomiting,
Abdominal pain on both sides,
Frequent urination,
Painful urination.
Diagnostic evaluation:
Diagnostic evaluation of salpingitis usually includes the following:
History Collection,
Physical Examination
Laboratory Test Complete Blood Count (CBC): To check for elevated white blood cell count indicative of infection.
Cervical culture to identify sexually transmitted infections (STIs) such as chlamydia and gonorrhea.
Nucleic acid amplification tests (NAATs) to assay Chlamydia trachomatis and Neisseria gonorrhoeae.
Imaging studies Transvaginal ultrasound to visualize the tube and look for any abnormalities or fluid collections.
Pelvic ultrasound advises imaging to assess the reproductive organs.
Laparoscopy is a minimally invasive procedure in which the fallopian tubes are visualized and abnormalities are identified to identify abnormalities of the fallopian tubes.
Treatment:
Treatment of salpingitis usually includes treatment of the following:
- Antibiotic medication: Empirical antibiotics: Provide broad-spectrum antibiotics to cover common pathogens including chlamydia, gonorrhea and anaerobes. Examples include doxycycline with azithromycin or ceftriaxone.
- Pain Management:
Provide nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pelvic pain and complications.
3.Treatment of sexual partner:
Giving advice for treatment and appropriate diagnosis of sexual partner to prevent reinfection and transmission of sexually transmitted infection (STI).
4.Surgical Intervention:
Laparoscopy: In severe or complicated cases, for direct treatment or removal of abscess.
- Follow-up care of infection
Advise for regular follow-up to assess and observe for any complications, such as chronic pelvic pain or infertility.
- Supportive Measures:
Advise the patient to maintain proper hydration and nutritional status. And giving advice for safe sexual practices to prevent future infections.
Complications:
infertility,
ectopic pregnancy,
chronic pelvic pain,
Tubo Ovarian Abscess,
Recurrent infection.
- Ophoritis:
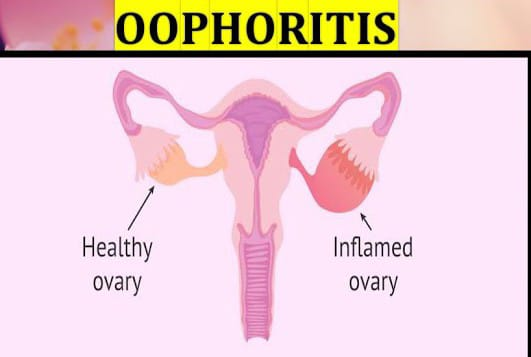
Definition: The condition of infection and inflammation of the ovary is called oophoritis. If there is infection and inflammation in one or both ovaries in the female reproductive system, this condition is called oophoritis.
Etiology of Oophoritis:
Sexually Transmitted Infection (STI):
Chlamydia trachomatis
Neisseria gonorrhoea
Other bacterial infections:
Mycoplasma species Ureaplasma species
Escherichia coli (E. coli),
staphylococcus,
Streptococcus
Viral infection:
such as mumps
Post surgical and post abortion infections:
Pelvic surgery or abortion infection
Tuberculosis:
Mycobacterium tuberculosis
Chronic pelvic inflammatory disease (PID):
Due to prolonged or repeated infections
Autoimmune conditions:
Sometimes seen due to autoimmune disorders.
Symptoms and signs:
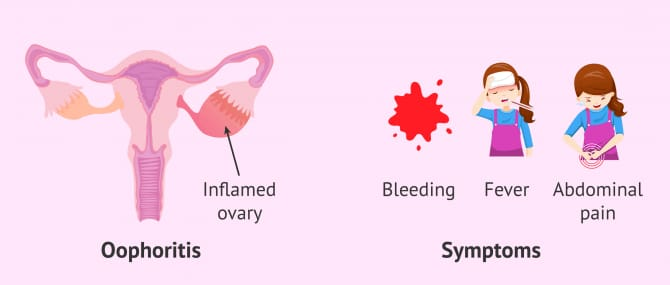
pelvic pain,
Hot and tender vajaina,
lower back pain,
Abnormal vaginal discharge (purulent and bloody discharge),
Painful sexualintercourse,
painful menstruation,
Pain during ovulation,
fever,
Nausea and vomiting,
Lower abdominal pain,
Frequent urination,
Painful urination.
Diagnostic evaluation:
History Collection,
Physical Examination
Laboratory Test Complete Blood Count (CBC): To check for elevated white blood cell count indicative of infection.
Culture A cervical or vaginal culture to identify a bacterial or fungal infection.
Serological test: to identify a viral infection such as a condition such as mumps.
Imaging studies Transvaginal ultrasound to visualize the ovaries and inflammation,
To identify infection, abscess and cyst if present
Pelvic Ultrasound Pelvic ultrasound is performed to assess the reproductive organs.
Laparoscopy is a minimally invasive procedure in which the ovaries are visualized and abnormalities are identified to identify ovarian abnormalities.
CT scan: In complicated cases, a computed tomography (CT) scan may be used to see the pelvis in more detail.
Treatment:
Treatment of oophoritis usually includes treatment of the following:
- Antibiotic medication: Empirical antibiotics: Provide broad-spectrum antibiotics to cover common pathogens including chlamydia, gonorrhea and anaerobes. Examples include doxycycline with azithromycin or ceftriaxone.
Antiviral Medication: Antiviral medication should be provided as supportive treatment if the patient is diagnosed with a viral infection.
- Pain Management:
Provide nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pelvic pain and complications.
4.Treatment of sexual partner: Giving advice for treatment and appropriate diagnosis of sexual partner to prevent reinfection and transmission of sexually transmitted infection (STI).
5.Surgical intervention: Drainage or surgery: In severe or complicated cases, to treat or remove the abscess.
- Follow-up care: of infection
Advise for regular follow-up to assess and observe for any complications, such as chronic pelvic pain or infertility. - Supportive measures: Advise the patient to maintain proper hydration and nutritional status. And giving advice for safe sexual practices to prevent future infections.
Complications:
infertility,
chronic pelvic pain,
Tubo Ovarian Abscess,
Recurrent infection,
Menstrual irregularity.
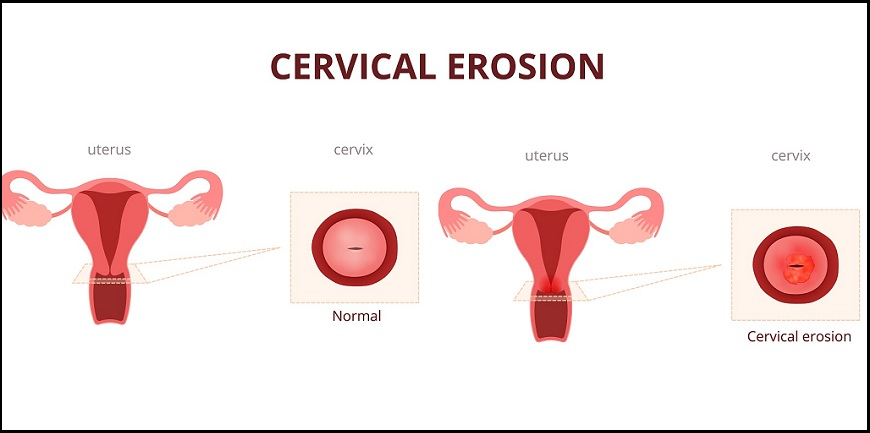
- Cervical Erosion and Cervical Ectopy:

Cervical erosion also known as cervical ectopy is a condition in which the squamous epithelium of the ecto-cervix is replaced by a columnar epithelium that is continuous with the endo-cervix.
Etiology:
The etiology of cervical erosion is generally divided into two types of etiology:
- Congenital,
- Acquired
- Congenital: Congenital cervical erosion is usually present at birth.
- Acquired:
Acquired cervical erosion is usually caused by increased levels of the hormone estrogen.
Other Causes:
Infections such as chronic cervicitis,
trauma.
Symptoms and signs:
Cervical erosion is usually asymptomatic but in some cases the following symptoms are observed:
Vaginal discharge may be mucopurulent, offensive, and irritating because the infection is present. And blood may be stained due to premenstrual congestion.
pelvic pain,
Becky,
Contact bleeding is seen especially during pregnancy.
Rarely infertility
Sign:
During internal examination a bright red area surrounding the external OS is seen. And multiple oozing sports or sharp bleeding is observed if rubbed through the gougepiece.
Diagnostic evaluation:
History Collection,
Physical Examination,
speculum examination,
blood test,
Cytological examination of cervical smear to assess the condition of dysplasia and malignancy,
colposcopy,
Cervical biopsy.
Management:
- In asymptomatic cases, routine examination and active treatment should be withheld.
- In symptomatic cases:
If it occurs during pregnancy and early puparium, treatment should be withheld for at least 12 wk postpartum.
If there are pill users, advise to stop the pill and use the barrier method.
If continuous erosion and discharge is present, treat it surgically such as:
i Thermal cauterization
ii. Cryosurgery
iii Laser vaporization.
Surgical Treatment:
i Thermal cauterization (two to three wicks for the procedure)
ii. Cryosurgery (total freezing)
iii Laser vaporization.
- Pelvic abscess
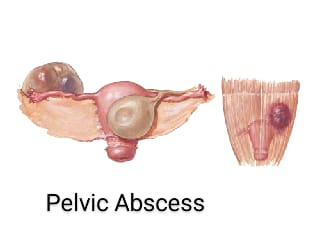
Pelvic abscesses can be caused by complications of pelvic inflammatory disease (PID) in which infected fluid or pus collects in the pouch of Douglas, fallopian tubes, ovaries, uterus, bladder, rectum, or parametric tissues (tissues in the perimetrium layer of the uterus). A pelvic abscess is a localized collection of pus that forms in the pelvic region due to infection or inflammation. It can be caused by various conditions, such as pelvic inflammatory disease, appendicitis, or complications from surgery.
Etiology:
- Pelvic Causes:
Post-abortal and due to peripheral sepsis,
Acute salpingitis,
Infected uterus due to septic abortion,
After a disturbed tubal pregnancy,
After abdominal or vaginal surgery,
Due to irritant peritonitis,
Due to contamination of urine by bile meconium during caesarean section,
Due to ovarian cyst rupture,
Due to use of iodine rich diet in hysterosalpingography.
Extra Pelvic Causes:
diverticulitis,
Rupture Goal Bladder,
Perforated pelvic ulcer
Other Causes:
Pelvic Inflammatory Disease (PID),
induce abortion,
Due to failure to maintain sterile technique during surgical procedures,
chlamydia,
gonorrheal infection,
Risk Factors:
multiple sexual partners,
Sexually Transmitted Diseases (STDs),
Intra uterine device (IUD),
diabetes mellitus,
Vic Immune System
Symptoms and signs:
Elevation of body temperature.
Getting a fever.
Pain in the perineal area.
Retention of urine.
Redness.
Swelling.
Tenderness.
Movement of the cervix becomes painful.
Movement of tender masses in the Pouch of Douglas.
Diagnostic evaluation:
History Collection,
Physical Examination,
sonography,
biopsy,
CT scan,
MRI (Magnetic Resonance Imaging),
1.Mass like structural filling in pelvic region near rectum.
2.Rarely the pus can be pointed above the inguinal region.
- If the abscess ruptures in the peritoneal cavity, a life threatening condition arises.
Treatment:
If the patient has pain condition then provide analgesic medication.
Use of antibiotic medication to destroy aerobic and anaerobic bacterial infections.
Advise the patient to bathe properly.
Provide proper intravenous (I.V.) fluid to the patient.
If there is a collection of pus, drain it properly.
Colpotomy Drainage: An incision is made in the vagina and the pus that has collected is drained.
Performing laparotomy in the setting of pelvic abscess.
Providing the patient with broad spectrum antibiotic medication like gentamicin, clindamycin ceftriaxone etc.
Nursing Management:
To monitor patient’s vital signs properly.
Provide proper position to the patient.
Advise the patient to take adequate bed rest.
If vaginal discharge is present, note its color and amount properly.
Provide education to the patient to maintain personal hygiene and safe sexual activity.
- (PID)Pelvic Inflammatory Disease:
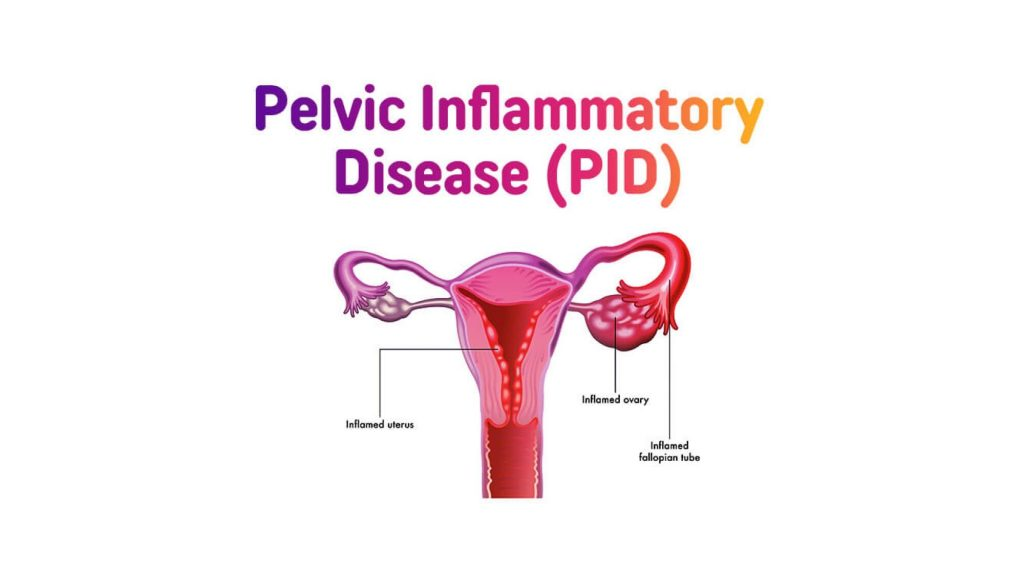
PID (Pelvic Inflammatory Disease) In which infection and inflammation occurs in the upper genital tract organs of the female reproductive system, this condition is called pelvic inflammatory disease. This infection is usually responsible for sexually transmitted diseases. The bacteria are transmitted vaginally in an ascending (downward to upward) manner in the upper genital tract. Because of this, the condition of infection and inflammation arises in the reproductive organs of the female. This infection can involve the organs of the mother, vagina, cervix, uterus, fallopian tube, ovary etc.
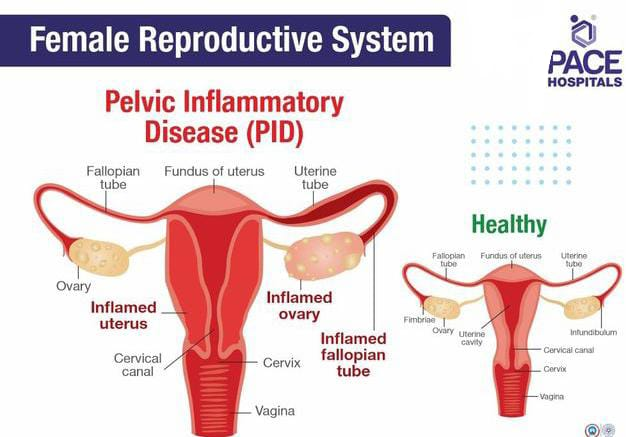
If the infection is in the vagina, it is called vaginitis.
If the infection is in the cervix, it is called cervicitis.
If the infection is in the uterus, it is called metritis.
If the infection is in the fallopian tubes, it is called salpingitis.
If the infection is in the ovary, it is called oophoritis.
Types of Inflammatory Disease:
Pelvic inflammatory diseases are generally divided into two types,
- Acute pelvic inflammatory disease
2.Chronic pelvic inflammatory disease
1.Acute Pelvic Inflammatory Disease
: Acute Pelvic Inflammatory Disease means if severe symptoms are seen in a short time then this condition is called Acute Pelvic Inflammatory Disease.
2.Chronic Pelvic Inflammatory Disease
: If the attacks of acute infection in Chronic Pelvic Inflammatory Disease occur frequently, this condition converts into Chronic Pelvic Inflammatory Disease.
Etiology:
Bacteria such as chlamydia and gonorrhea,
Viral infections such as herpes simplex,
Due to parasitic infection,
Due to fungal infection
Risk Factors:
Due to low socio economic status,
Due to multiple sexual partners,
Due to past history of PID,
cigarette smoking,
Due to low immunity,
Because of abortion,
Due to using IUD (Intra Uterine Device).
Symptoms and signs:
Lower abdominal pain,
fever,
one head,
Irregular menstrual bleeding,
nozia,
vomiting,
anorexia,
tenderness,
vaginal discharge,
Pain during periods,
Pain during voiding and defecation.
Diagnostic evaluation:
History Collection,
Physical Examination,
Complete Blood Count (CBC) test,
Ultrasonography (USG),
Cervical and vaginal swab cultures,
urine test,
CT scan (CT scan),
MRI,
Endometrial biopsy.
Medical Management:
The aim of medical management is to prevent infection and further transmission and to prevent complications arising.
If the patient has a bacterial infection, provide broad spectrum antibiotic medicine such as
ceftriaxone,
metronidazole,
tetracycline,
Erythromycin.
Advise the patient to take proper rest.
Advise patient to intake adequate amount of oral fluid.
If the patient has an intra-uterine device (IUD) inserted, remove it properly.
Provide the patient with a proper semi-fowler position.
Advise the patient to avoid sitz baths if they have an acute infection.
To continuously monitor the patient’s vital signs.
To provide analgesic medicine to relieve the patient’s pain.
Advise the patient to apply a hitting pad on the abdomen to relieve the pain if the patient has abdominal pain.
Advise patients to use proper barrier contraceptive methods to reduce the risk of pelvic inflammatory disease.
Advise the patient to seek medical treatment if he/she has any symptoms of pelvic inflammatory disease.
Advise the patient to avoid sexual activity during peripartum period after delivery, abortion.
Advise the patient to maintain personal hygiene.
Surgical Management:
This surgical management is done when the infection usually involves the fallopian tubes and ovaries.
Laparoscopy: A small incision is made in the abdominal wall and then a laparoscope (thin flexible tube with a camera and light) is inserted so that any infection and inflammatory conditions in the reproductive tract can be visualized on the screen.
Salpingectomy: This involves the surgical removal of the fallopian tubes.
- Pelvic tuberculosis
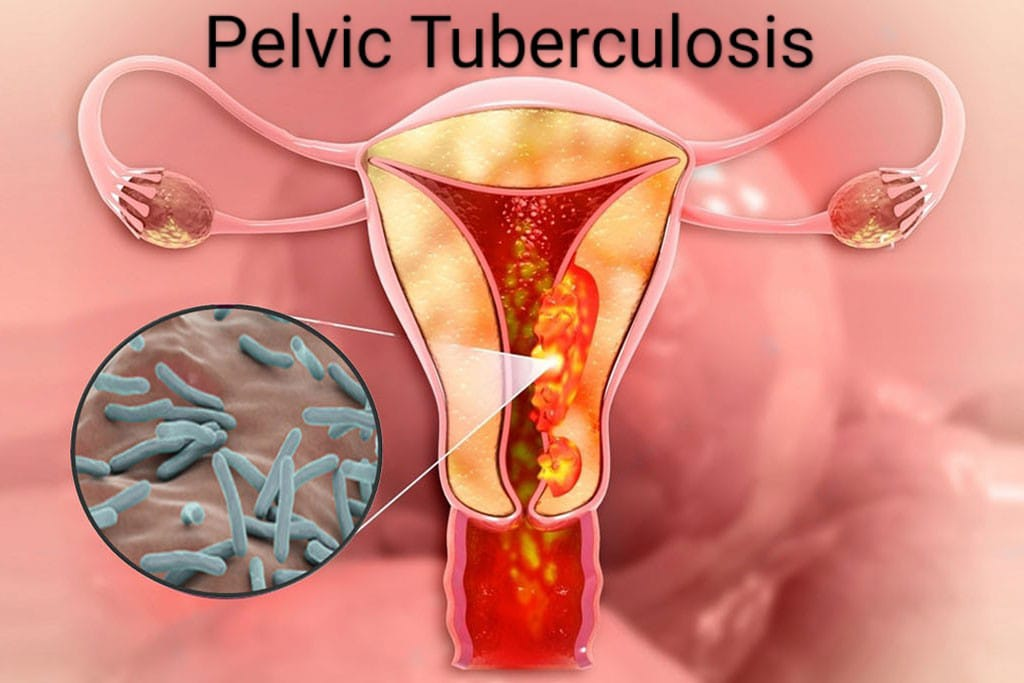
Pelvic tuberculosis is a serious infection caused by the bacterium Mycobacterium tuberculosis that mainly affects the lungs but can spread as a secondary infection to other organs in the body, such as lymph nodes, bones, joints, and the urinary tract and pelvis. Transmission can occur in the region. If the organisms of tuberculosis spread to the pelvic region and cause infection there, it is called pelvic tuberculosis. It involves the uterus, fallopian tubes, ovaries.
Etiology:
Close contact with active tuberculosis patients
Weak immune system (HIV, organ transplantation, cancer, corticosteroid therapy)
Edge
Subtons abuse
Living in over crowded area
Malnutrition
Chronic health conditions
Symptoms and signs:
fever,
feeling cold,
swollen gland,
fatigue,
night sweats,
loss of appetite,
weight loss,
Shortness of breath,
poor growth,
cuffing,
Abdominal swallowing,
infertility,
Menstrual problems like,
Amenorrhea, oligomenorrhea, menorrhagia, metrorrhagia,
Postcoital bleeding,
Poor general health,
pelvic pain,
vaginal discharge,
dyspareunia,
Abdominal mass and pelvic mass,
abdominal tenderness,
pelvic tenderness,
Ascites (abdominal distension),
Uterus enlargement,
pyometra,
Fistula
Diagnostic evaluation
History Collection
Physical Examination
Tuberculin skin test
x ray
Sputum test
blood test,
Endometrial curettage,
ultrasonography,
Histologic examination,
hysterosalpingiography,
endoscopy,
laparoscopy,
Biopsy collection of lesions in the external genitalia, vagina, cervix, and pelvic cavity
Management of Tuberculosis:
Antibiotic therapy
A combination of antibiotics is given as a treatment for pulmonary tuberculosis. In which isoniazid, rifampin, ethambutol and pyrazinamide medications are given. A course of this medicine is done for six to nine months. Which depends on the severity of tuberculosis.
Drug therapy
It is as follows:
A regimen of 6 months or 4 medications for 6 months is provided initially.
It involves:
- Isoniazid (INH)
- Rifampin (RIF)
3.Pyrazinamide (PZA) - Ethambutol (EMB) or Streptomycin (SM)
This medication is an antitubercular therapy that is very effective in killing bacteria. Treatment can be continued for 6-9 months. Initial therapy with 4 drugs viz (INH+RIF+PZA+EMB) is given for 2 months followed by 2 drugs provided in next 4 months (isoniazid and rifampicin).
Pyridoxine is added wherever INH is prescribed.
Directly Observed Treatment Short Courses (DOTs)
In DOTs therapy, the TB patient is supervised by a health care provider. The patient takes exactly the regular medicine and its effectiveness is observed. So it can be known whether the patient has completed the full course of treatment or not.
Isolation
TB positive women are isolated. Because TB is a contagious disease and it is spread through air from one to another. Hence women are isolated to prevent it from spreading.
Nutritional support
Provide adequate nutrition support to women with TB to improve their immune system and gain weight.
Education and counselling
Providing education and counseling to women about tuberculosis. Explain infection control measures to the child and his family members.
To maintain the woman’s body temperature and to provide proper antipyretic medication if the woman has a condition of fever.
Providing antibiotic drugs to treat bacterial infections.
Provide cough expectorant drug to expel phlegm.
Provide nasal decongestants to relieve congestion.
Adequate rest and advice for plenty of fluid intake.
Avoid contact with irritants.
To assess women properly and completely.
Properly assess respiratory status of women.
To assess vital sign of woman completely.
To properly assess the woman’s oxygen saturation.
Continuously monitoring the woman’s respiratory status and oxygen saturation to properly assess the woman’s condition.
Advise the woman for continuous fluid intake to maintain hydration status and keep mucus thin.
To provide a properly comfortable position to women.
To maintain oxygen saturation of the woman’s body and to provide adequate oxygen to the woman to provide respiratory support.
Providing properly prescribed medication to women.
To provide complete education to women and their family members about the condition, its causes, symptoms and signs and its treatment.
To provide proper work and comfortable environment to women.
Surgical Treatment:
When chemotherapy does not provide a response, bilateral salpingo-oophorectomy with total hysterectomy is advised.