ENGLISH GNM-T.Y-Midwifery Third Year & Gynecological-13/09/2021 (DONE-paper no.૩)
GNM-T.Y-Midwifery Third Year & Gynecological-13/09/2021


Q-1 🔸a. Define Midwifery 02
Midwifery is a healthcare profession that not only provides care to child-bearing women during pregnancy, labor and childbirth, but also during the postpartum period (the period up to 6 weeks after the birth of a baby). is provided. It is called midwifery. However, midwifery also helps the mother with the care of the newborn and breastfeeding.
Those working in the profession of midwifery are known as midwives, the term is used to refer to both females and males, although most midwives are female.
A midwife is a trained health care personnel who provides support and care to women and newborns as well as provides proper education to women. They emphasize on natural child birth. and provide prenatal care to the mother to promote the well-being of the mother and child, provide assistance during labor and also provide maternal guidance on newborn care and breastfeeding to the mother.
b. Explain stages of labor. Explain the stages of labour.04
Stages of Labour:
The stages of labor are divided into four stages.
1) First Stage of Labour,
2) Second Stage of Labour,
3) Third Stage of Labour,
4) Fourth stage of labor
••>1) First Stage of Labor (Cervical Stage):
The first stage of labor is the initial phase of childbirth. In which the cervix gradually opens (dilate) and thins (effacement). Due to this, the baby can pass from the uterine cavity into the birth canal (vagina). In which regular and rhythmic uterine contractions are seen and the frequency, intensity and duration of uterine contractions gradually increases.
The first stage of labor starts with true labor pain and lasts until full dilatation of the cervix (10 cm). This stage is also called “cervical stage”.
The first stage of labor is further divided into 3 stages:
First Stage No Time Period:
Primigravida:=12-16 hours, and
Multigravida:=6-8 hours, no.
The first stage of labor is divided into three phases.
1) Latent Phase,
2) Active phase,
3) Transitional phase
1) Latent Phase,
The latent phase is known as “prodomal labor” or “pre-labor”.
Cervical dilatation of 1-4 cm centimeters occurs in this stage.
Contractions in this phase repeat every 15-30 minutes and last for 15-30 seconds.
In this phase the mother is talkative.
2) Active phase,
Active phase is also known as dilatation phase.
In this second phase, the cervix a
5 – 7 cm dilated. And the contractions are repeated every 3-5 minutes and
Seen for 45 – 60 seconds.
In this stage mother feels restlessness.
3) Transitional phase
In the transitional phase, the dilatation of the cervix is 8-10 cm.
Contractions are repeated every 2-3 minutes and last for 60 to 90 seconds.
The first stage of overall labor is the critical period in which, after the cervix opens, the uterus prepares for delivery by providing the proper position of the baby in the uterine cavity. Continuous monitoring by health care providers is important to improve the condition and well-being of the mother and fetus during this stage.
2) Second Stage of Labor (Expulsion of Fits):
The period from full dilatation of the cervix to the birth of the baby through the birth canal is called the second stage of labor.
its duration,
In primi gravida: 1-2 hrs
In multigravida: 20-30 minutes.
The second stage of labor is further divided into two phases:
1) Propulsive phase,
2) Explosive phase.
1) Propulsive Phase:
The propulsive phase starts from full dilatation of the cervix until the presenting part of the fitus descends to the pelvic floor (+4 +5 stations).
2) Explosive Phase:
This is the expulsive phase until the baby is completely expelled from the uterine cavity along with the mother’s bearing down efforts.
3) Third Stage of Labor (Expulsion of Placenta):
This stage is the period from the expulsion of the baby to the expulsion of the placenta and membranes is called the third stage.
Its time duration is 15 minutes in primi gravida and multigravida
4) Fourth Stage of Labor (Observation Stage):
The observation stage after the birth of the baby is called the 4th stage of labor. During this stage, the general condition of the mother and the condition of the newborn and the behavior of the uterus are carefully monitored.
Its time duration is 1 hour.
Thus, the time duration of all four stages of total labor (1st stage + 2nd stage + 3rd stage + 4th stage) is 13-15 hours in primigravida and 6-8 hours in multigravida.
c. Describe Physiological changes occur during pregnancy. 06 Know the physical changes that occur during pregnancy
Physiological changes during pregnancy
Pregnancy is a condition from the time of conception to the time of delivery. Physiological changes are observed in the mother’s body during pregnancy due to certain types of specific hormones. These changes occur to develop the fetus, prepare the mother’s body for labor, and produce the best milk during the periperium period.
1) Changes in reproductive system:-
A)Vulva:=
The vulva becomes more edematous and vacuolar.
Superficial varicosities (varicose vein := vein enlarged and swollen, usually seen in leg and also in pelvic area during pregnancy period) are also seen in multipara and labia minora becomes pigmented and its hypertrophy ( Organ size increases).
B)Vajaina:=
Vaginal wall is hypertrophoid,
becomes edematous and hypervascular.
Bluish discoloration of the vaginal mucosa due to increased venous blood supply to the vaginal wall is called “Jacquemeier’s sign”.
The length of the interior wall increases.
Vaginal secretions are highly acidic, thin and curdy white.
The acidic pH of vaginal secretions inhibits the multiplication of pathogenic microorganisms.
(C) Uterus:=
During pregnancy, the uterus grows more. During pregnancy, the weight of the uterus and its length also increases.
Weight of Uterus:
In the non-pregnant state, the weight of the uterus is about 60 gm, which increases to 900-1000 gm during pregnancy.
Length, Width and Thickness of Uterus:
of the uterus in the non-pregnant state,
Length := 7.5 cm,
Width:=5 cm and thickness:=2.5 cm.
During pregnancy (at term) of the uterus
Length := 30-35 cm,
Height:= 22.5 cm and
Thickness: = 20 cm.
Volume of Uterine Cavity: In non-pregnant state the volume of uterus is 10 ml which increases to 5 liters during pregnancy (at term).
Body of uterus: Growth and enlargement of the body of uterus.
Muscles
1) Outer:= longitudinal layer
2) Middle:= vascular layer
3) Inner:=circular layer
Hypertrophy (increase in size) and hyperplasia (increase in number) are seen in muscles.
After 20 weeks of pregnancy, the length of the uterine muscle fibers increases and the uterine wall becomes thinner due to which the uterus becomes softer and more elastic in pregnant condition than in non-pregnant condition.
Vascular System:
Blood supply begins to increase from 20 weeks onwards due to vasodilatation due to estradiol and progesterone.
The diameter of uterine artery doubles and blood flow increases and veins dilate.
During pregnancy the endometrium of the uterus is called decidua.
Braxton Hicks contractions:
Spontaneous contractions of the uterus early in pregnancy are irregular, infrequent, spasmodic and painless due to no effect on dilatation of the cervix until near term (37-42 weeks) they increase and finally merge with painful labor contractions. is
D) Isthmus:=
During pregnancy the lower segment of the uterus forms an isthmus.
The length of the isthmus in the nonpregnant state is 0.5 cm, which increases in length during pregnancy to a maximum of 7.5 cm-10 cm.
The muscle fibers of the isthmus are arranged circularly in the lower segment and form a sphincter-like structure which helps the fetus to stay in the uterus during early pregnancy. If this sphincter is incompetent, abortion can also occur.
E)Cervix:=
During pregnancy the cervix becomes vascular, oedematous and hypertrophoid and hyperplastic.
Cervix that becomes soft is called “Goodell’s sign”.
The length of the cervix doubles and its volume also increases.
F) Fallopian tubes:=
The length of the fallopian tubes is slightly increased. The tube becomes congested. Muscles hypertrophy and epithelium flattens.
G)overy:=
Ovulation remains at a standstill during pregnancy. The ovary is hypertrophied and vascularized.
In the usual menstrual cycle, the corpus luteum remains constant and enlarges by two 2.5 cm until the 8th week.
Colloid degeneration occurs and the uterus becomes calcified.Estrogen and progesterone hormones are produced by the corpus luteum and provide an environment to maintain the ovum until placental action begins.
H) Breast:=
Breast size, nodularity, and sensitivity increase with increased vascularity of the breast throughout pregnancy due to the effects of estrogen and progesterone.
The nipple becomes enlarged, dark and erectile.
Hypertrophy of 5 to 15 sebaceous glands that are invisible in the non-pregnant state is seen.
Called “Montgomery tubercles”. Its secretion around the nipple keeps the nipple and areola moist and healthy.
Areola that becomes dark and pigmented is called primary areola.
In the second trimester, another pigmented zone called the secondary areola forms around the primary areola.
In the first three months, the growth of the ductal system in the breast increases as the pregnancy progresses, its alveolar cells become secretory.
Total weight of breast is 0.4 kg.
The cyst enlarges due to alveolar proliferation and fat deposition and clear sticky fluid can be squeezed from the cyst at about 12 weeks.
At 16 weeks this clear sticky fluid becomes thick and yellow called colostrum which is an important sign of pregnancy.
Changes in other systems of the body.
1) Skin Changes:=
A) Face: Pigmentation is seen around the cheeks, forehead and eyes called “gravidarum in close” or “pregnancy mask” which disappears on its own after delivery.
B) Breast: Visible pigmentation changes occur in the breast.
C) Abdomen: Linea nigra A brownish black color line visible in the midline from xiphisternum to symphysis pubis is called linea nigra due to melanocyte stimulating hormone.
stria gravidarum
Abdominal wall below the umbilicus and sometimes on the chest and breast is a depressed linear mask that is initially pink but turns glistening white after delivery called stria albicans or stria gravidarum.
Vacuolar spindle and palmar erythema are seen with high estrogen levels. Skin
Mild degree of hirsutism (excess hair) is seen and excess amount of hair is lost during purpureal period.
2) Weight gain
Weight loss occurs during the early weeks of pregnancy due to nausea and vomiting. Weight gain remains progressive from the following months.
A healthy woman gains an average of 11 kg (24 lbs) of weight during pregnancy.
During 1st trimester: 1kg,
2nd trimester
During: 5kg,
During 3rd trimester: 5kg,
As the weight increases.
A) Reproductive weight gain
1) Weight of Fits: 3.3kg,
2)Weight of placenta: 0.6kg,
3)Weight of Liker: 0.8kg,
4) Weight of Uterus: 0.9kg,
5) Weight of breast: 0.4kg.
B) net maternal weight gain
1) Increase blood volume:=1.3kg,
2) Increase extracellular fluid:=1.2kg,
3) Fat and Protein:=3.5kg.
4) Cardio vascular system
A) Heart has to work more during pregnancy.
Cardiac volume increases by 10% but there is no change in ECG.
Cardiac output also increases due to increased heart rate and stroke volume.
Pulse rate also increases.
As the concentration rate increases from 40 to 45 mm, the platelet count decreases slightly.
B) Blood Pressure and Blood Volume:
Blood pressure remains within normal limits In some women, diastolic pressure drops by 5 to 10 mm during mid-pregnancy.
C) Venus pressor:
Femoral venous pressure increases by 10 cm due to the pressure of gravid uterus on the pelvic vein, then the blood volume also increases, the volume of red blood cells and plasma volume also increases in many parts of the body like uterus, pulmonary, renal, skin. , and blood flow to the mucosa increases.
4) Respiratory System:-
Hyperemia (increased blood flow) and congestion are seen in the upper respiratory mucosa.
Increased inspiration also increases oxygen intake and oxygen supply to the fetus.
Carbon dioxide is released due to increased exhalation, so the transfer of carbon dioxide from the fetus to the mother’s blood can be easily done due to low maternal carbon dioxide.
In the last weeks of pregnancy, due to the pressure of the gravid uterus on the diaphragm, there is a complaint of breathing difficulty which is relieved by lightening.
5) Digestive System:-
Due to the effect of progesterone, the muscle tone of the gastrointestinal system is reduced.
Relaxation of cardiac sphincter leads to regurgitation of stomach contents and heartburn.
As the gastric size decreases, it slowly empties and is continuous even in labor.
In many women, the gums become spongy and vascular and may bleed during brushing.
A decrease in the size of the intestine leads to better absorption of food and causes constipation.
6) Nervous System:-
Mood changes during pregnancy and periperium period are due to psychological conditions such as nausea, vomiting, mental irritability and sleeplessness.
Depression or psychosis may also develop in women.
Compression of the median nerve in the wrist leads to pain and paresthesia (tingling) in the hands and arms, which is called carpal tunnel syndrome and is seen in the last month of pregnancy as well as sensory loss due to compression of the cutaneous nerve.
7) Urinary Track:-
Frequent micturition is commonly seen in early and late pregnancy.
Stress incontinence can also occur.
Due to continuous dilatation of uterus and pelvis from early pregnancy to mid-pregnancy, urinary stasis occurs and infection can also occur. Renal function also increases in pregnancy.
8) Locomotor System:–
Backache is common during pregnancy due to relaxation of lordosis and joints due to relaxin hormone.
Due to weight gain in the sacral and lumbar plexus, leg cramps remain and difficulty in walking also occurs.
Thus, physiological changes are observed in women during pregnancy
d. Describe Antenatal care Describe care during pregnancy. 08
Care during pregnancy (antenatal care):
Definition:
Antenatal care is also called prenatal care in which comprehensive health care is provided to the pregnant woman from conception to childbirth.
This period is a crucial time for monitoring the mother and the developing fetus. Because if there are any potential health complications to the mother and the developing fetus, they can be managed by early identification. And the mother can be physically and emotionally prepared for childbirth and the postpartum period.
Systemic supervision (examination or advice) of women during pregnancy which is regular and periodic is called “antenatal or prenatal care”. Antenatal care starts from the beginning of pregnancy and ends when the baby is delivered.
Aim and Objectives of Antenatal Care:
Aim:
Screening of high risk cases.
To prevent complications as early as possible.
Antenatal care also helps in medical surveillance and prophylaxis.
To carry out ongoing assessment of mother and provide primary health care to her.
To improve the psychology by explaining the physiology of pregnancy and labor to the mother through demonstrations, charts, and diagrams by removing her fear.
Discussing time, space, mode and newborn care of delivery with the couple.
Encouraging couples for family planning and for medical termination of pregnancy
Give proper advice. Objectives:
The main objective is to deliver a healthy baby by a healthy mother with a normal pregnancy.
The first visit must be before the second missed period.
To assess the health status of mother and fetus.
For early screening of high risk pregnancy cases.
To formulate a plan for further management.
To promote, protect and maintain good physical and mental health of the mother during pregnancy.
Components of Antenatal Care:
1) Initial Assessment:
The first antenatal visit should be done early in pregnancy, ideally within the first 8 to 12 weeks of the last menstrual period.
During this assessment, the health care providers properly assess the woman in which the woman’s
Medical History, incl
previous pregnancy,
Medical condition, medication, and relevant family history are fully assessed.
This information is collected so that potential risk factors of the mother can be identified and appropriate care can be provided to the mother.
2) Physical Examination:
Physical assessment of the mother is done to assess the health status of the mother and the fetus during the throw out pregnancy period.
In this examination the mother’s blood pressure,
Weight, and urine tests are done due to which the mother can be identified early if she has the condition of gestational diabetes and preeclampsia.
Mother’s blood test is also done due to which mother’s hemoglobin level, blood group is done.
The mother is also screened for hepatitis and HIV infection.
3) Fetal Monitoring: Growth and development of the fetus is also monitored in antenatal care.
It involves assessment of the fetus through different methods such as ultrasound:
Ultrasound is done to confirm the pregnancy, to assess the gestational age, to assess the fetal growth and to identify any structural problems of the fetus i.e. malformations.
Fetal Doppler: Fetal heart rate is monitored by fetal doppler.
Kick Counting: Advise the mother to feel the fetal movement and count the number of fetal kicks throughout the day so that fetal well-being can be monitored.
4) Nutritional Guidance:
Proper nutrition is important for providing support to maternal health and fit development.
Antenatal health care providers provide guidance to the mother on a balanced diet along with proper weight maintenance and adequate amounts of vitamins and minerals.
Education is provided to pregnant women about the importance of taking (Ex: Iron and Folic Acid). And education is also provided to women that congenital birth defects in fetuses and anemia conditions in pregnant women can be prevented by taking adequate diet.
5) Health Education and Counselling: In antenatal care, education is provided to pregnant women about pregnancy related topics like,
1) Exercise: Safe physical activity and exercise are important to maintain the health of mother and fetus.
2) Labor and Birth Preparation: Information is provided to the mother about the stages of labor along with education about pain relief strategies and birth plan.
3) Breast feeding: Providing education to the mother about the technique, benefits of breast feeding.
4) Emotional and Mental Health: To properly assess the emotional and mental health of the mother and to provide adequate education and psychological support to the mother to relieve the fear and anxiety of the mother and to clear all the doubts of the mother.
6) Screening and Test: Proper genetic testing during the antenatal period of the mother so that any genetic complications can be identified.
Genetic Screening: In this, mother’s ultrasound and blood test are done, due to which genetic disorder risk can be identified (Ex: Ultrasound).
Screening for Infection: The mother is screened for identification of any sexually transmitted disease and any other infection that may affect the pregnancy.
Glucose tolerance test: Glucose test is done to identify if the mother has any gestational diabetes condition or not.
7) Preparation for Labor and Birth: Antenatal care includes discussion of birth preferences, options for management of labor pain, and preparation for potential complications.
8) Postpartum Planning: Antenatal care also includes planning for post partum care including breastfeeding support, education of the mother about newborn care. Thus, antenatal care is important for maintaining the health condition of the mother, for proper growth and development of the fetus and for early identification and management of potential risk factors.
OR
Q: 1(a) Ans
••>Preeclampsia
Definition:
Preeclampsia is a complication of pregnancy. In which its etiology is unknown but it is a multisystem disorder. In which high blood pressure is seen along with other organs are also damaged and most commonly liver and kidney are affected.
Preeclampsia occurs mainly after the 20th week of pregnancy and also differs in severity.
Among the main symptoms of preeclampsia,
1) Hypertension that increases above 140/90 mmHg (hallmark sign of preeclampsia),
2) Edema (mainly in hands, face, and legs) and excessive weight gain.
3) Proteinuria (excess amount of protein found in urine),
4) Albuminuria (albumin present in urine).
The symptoms of preeclampsia are seen after the 20th week.
••> Eclampsia
Eclampsia Definition
Eclampsia is a life threatening complication that occurs during pregnancy in women.
The term eclampsia is derived from the Greek word “like a flash of lightning”. Tonic-clonic convulsions or coma as a complication of pre-eclampsia is called eclampsia.
While the condition of pre-eclampsia which,
Hypertension,
Edema (weight gain),
Proteinuria
(Protein in urine) and
If albuminuria (albumin present in urine) becomes complicated and converts to conditions like convulsion and coma, it is called “Eclampsia”.
This is an obstetrical emergency. It is important to take immediate measures to manage it.
🔸OR🔸
🔸 a. Define Pre-eclampsia and Eclampsia – Define Pre-eclampsia and Eclampsia 02
Causes of Eclampsia:
The exact cause is Unon.
Elderly or young primary gravida,
Due to hypertensive disorders during pregnancy: Ex: Preeclampsia,
Having a family history of hypertension,
Due to placental abnormalities like,
Hyperplacentosis: Excessive exposure of chorionic villi,
Ex: molar pregnancy, twins, diabetes,
Placental ischemia.
obesity,
Pre-existing vascular disease,
thrombophlebitis,
Complications with pregnancy like,
multifetal pregnancy,
hydatidiform pregnancy,
hydroamniosis,
Rh.Incomplicity,
Medical diagnoses like nephritis and diabetes mellitus,
Vasospasm: Dilator depression is due to increased sensitivity of circulating pressors such as angiotensin II and prostaglandins.
Dysfunction of endothelial cells reduces placental perfusion.
It can also be caused by immune complex diseases.
It can also be caused by not having enough protein, calcium, magnesium, vitamin E and A in the diet.
Due to genetic factor
Due to immunological factors.
Due to endocrine factor.
Due to environmental factors.
Due to chronic health conditions such as hypertension, gestational diabetes, kidney disease and autoimmune disorders
b. Write down causes of Eclampsia Lakhs 04
Symptoms and signs of eclampsia:
The symptoms and signs of eclampsia are divided into four stages:
1) Premonitoring stage (30 seconds),
2) Tonic stage (30 seconds),
3) Clonic stage (1 to 4 minutes),
4) Stage of coma
1) Premonitoring Stage (30 seconds):
In this patient is unconscious,
There is twitching of the muscles of the face, tongue and limbus,
The eyeball is rolled, turned to one side and then fixed.
This stage lasts for 30 seconds.
2) Tonic Stage (30 seconds):
This test In this stage the whole body goes into a tonic spasm,
Trunk = opisnotonys (abnormal body posture in which the head, neck, and spine are tilted backward.)
Limbus = Flex,
hand = clenched,
Respiration stops and the tongue protrudes between the teeth.
Cyanosis is seen,
The eyeball is fixed,
This stage lasts for 30 seconds.
3) Clonic stage (1 to 4 minutes):
All voluntary muscles undergo alternate contraction and relaxation,
Twitching starts from the face and involves the extremities of one site,
Tongue bites,
Breathing stearatorius,
A mouth full of blood-stained frothy secretions,
Cyanosis is gradually reduced,
Respiration is labored and noisy,
Temperature increases by 40°C due to fits.
This stage lasts from 1 to 4 minutes.
4) Stage of Coma:
After a fit, the patient goes into a coma stage that lasts from a few minutes to a few hours.
Deepcoma remains until another convulsion occurs.
In this the patient is seen in a state of confusion after a convulsion and the patient does not remember what happened to him.
If the fits occur consecutively, it converts to status epilepticus.
c. Write down signs and symptoms of Eclampsia. 04 Write the signs and symptoms of eclampsia.
Management of Eclampsia Medical and Nursing Management of Eclampsia
Aim of Management
To control fits of convulsions.
Controlling blood pressure.
Prevent complications.
Safe delivery of Fits.
Principles of Management
To maintain mother’s airway, breathing and circulation.
Properly administer 8-10 liters of oxygen to the mother.
Preventing maternal convulsions.
Provide proper ventilatory support to the mother.
Prevent injury to the mother.
All laboratory investigations of the mother should be done properly.
General Management
Hospitalization
Hospitalize the mother in a hospital with properly well equipped facilities.
Rest
Advise the mother to take adequate rest as well as advise to stop all activities and also restrict visitors.
Positioning
Advising mother to take rest in proper left lateral position due to which
History Collection
Collecting a complete history of the mother including the frequency and duration of the fits and taking a complete history of any medication the mother is taking or not.
Cideson and then General Examination
Provide proper drug to the mother and sedate her.
Ex:=phenobarbitone 15-30 mg (TDS)
Or
Diazepam 1.5 mg (TDS).
After the mother is properly sedated, do a general and abdominal examination of the mother properly and quickly.
Vital sign
To note the vital signs of the mother every half hour including,
temperature,
pulse,
Respiration,
and blood pressure.
If there is any disturbance in the vital sign or if the vital sign is raised above its normal range, treat it immediately.
Urinary output
Monitor mother’s urine output hourly.
Nutrition
Start the mother on 10% dextrose to maintain fluid, nutritional and caloric levels of the mother.
Fluid should not be increased in an amount more than 2 liters in 24 hours.
Additionally, 50 ml of 5% Dextrose should be provided to the mother at 8 hour intervals to maintain the caloric level of the mother.
Specific management or medical management
Eclampsia wadi mother can be treated by providing medication as follows:
a) Anticonvulsant,
b) Anti-hypertensive,
c) Sedatives,
d) Diuretic,
e) Antibiotics,
f) Other Medication.
a) Anticonvulsant,
Magnesium Sulphate A ( MgSO4 )
Acts as the drug of choice to treat the condition of eclampsia. Because it helps in preventing eclamptic fits in the pregnant mother.
Magnesium sulfate can be administered both IV (intravenously) and IM (intramuscularly).
Dose and route
•> IM (Intra Muscularly):
Initial dose:
Initially administer 4gm IV (intravenously) bolus, magnesium sulfate very slowly over 3-5 minutes.
Continuous Dose:
Administration of 5 gm magnesium sulfate IM (intra muscular) every four hours in alternate buttocks.
•>IV (Intra venously)
Initial dose:
Initial dose is 4-6 gm of magnesium sulfate administered slowly IV (intravenously) over 15-30 minutes.
Continuous Dose:
Administer 1-2 gm magnesium sulfate every hour IV (intravenously).
Magnesium sulfate is a toxic agent that can cause the condition of deep tendon reflux if not provided within therapeutic levels.
The therapeutic level of magnesium sulfate (MgSO4) is 4-7 mEq/L (milliequivalents per liter).
In case of overdose of magnesium sulfate (MgSO4), calcium gluconate is used as an antidote.
Magnesium sulfate when nitrogen is present,
Administer only when urine output increases above 30 ml/hr and respiratory rate above 12/min.
b) Anti-hypertensive,
Anti-hypertensives are used to control and reduce blood pressure.
Ex:
a) Hydralazine: 5 to 10 mg over 2 minutes.
b)Labetalol:
Initial dose: 20mg slowly over 2 minutes.
followed by 40-80 mg IV over 10 minutes.
The total dose should not exceed 300 mg.
c) Sedatives
Ex:=Diazepam
Dose:=5-10mg IV at the rate of 2-5mg/min.
Maximum dose: Do not increase more than 10mg dose.
d) Diuretic:
Diuretic medication should be provided during pregnancy only when pulmonary AD is present.
Ex:=Frusemide, Mannitol.
e) Antibiotics:
Antibiotics are provided as prophylaxis to reduce the complications of pulmonary and pleural infections.
Broad spectrum antibiotic medication is not used in these antibiotics.
f) Other Medication:
i) In case of pulmonary ED: Provide frusemide 40 mg IV followed by 10% mannitol.
ii) Heart Failure: Ex: Use of Lasix and Digitalis medication.
iii) Hyper pyrexia:
Antipyretic medication is not used.
Nursing Management of Eclampsia
Placing a pregnant woman with eclampsia in a side-padded side rail wada cot.
Keeping a padded tongue blade between the teeth.
Keeping the mother in lateral position can avoid aspiration.
During convulsions, keep the airways patent and provide oxygen to the mother in adequate amounts.
Properly monitoring the mother’s oxygen level by pulse oximetry.
Suction properly to remove oral secretions and any vomiting, if any.
Properly note the time, duration of the convulsions that the mother gets.
Provide proper and regular prenatal care to mothers with pregnancy induced hypertension.
Protect the mother from self-injury.
Keep the mother in a dark room to minimize stimuli such as bright lights, noise, and visitors.
Keeping the foot side of the bed slightly elevated will allow secretions to drain properly from the respiratory tract.
Assess mother’s vital signs, ED, fundus height, presentation and position of feet and fetal heart sound and test urine for protein.
Assessing mother’s urine output properly.
Provide intravenous infusion of glucose saline and Ringer’s lactate solution as prescribed to maintain mother’s fluid and nutritional levels.
Advising the mother to maintain her personal hygiene.
Providing properly prescribed medication to the mother.
Assess the mother’s uterine activity, cervical status and fetal status as the membranes may rupture and delivery may occur.
Obstetrical Management:
Most often when a woman has convulsions, labor is induced if labor has not started, labor is induced by artificial rupture of membranes, prostaglandins gel or oxytocin or caesarean section if the baby has died, spontaneous labor. Waited for.
Continuous start of hypertensive regimen as prescribed during post partum period.
Continuously monitor the mother for any other complications of eclampsia.
Advising the mother to follow up regularly.
d. Describe Management of Eclampsia. Describe the management of eclampsia 08
Indications of Caesarean section:
Indications for caesarean section are divided into two categories:
1) Absolute, (in which vaginal delivery is not possible)
2) Relative (in which vaginal delivery is possible but risks to mother and baby)
1) Absolute, (in which vaginal delivery is not possible):
Central placenta previa,
Severe degree contracted pelvis,
Cervical or broad ligament fibroids,
Vaginal atresia/obstruction,
In advanced cervical carcinoma,
Cephalopelvic Disproportion,
Obstruction due to pelvic mass,
Fits a death.
2) Relative (in which vaginal delivery is possible but risks to mother and baby):
Cephalopelvic Disproportion,
contracted pelvis,
Prevous cesarean delivery,
Fital Distress,
Abnormal uterine contractions,
large feet,
small pelvis,
fail induction,
Antepartum haemorrhage eg, placenta previa, abruptio placenta.
Malpresentation or abnormal lie (transverse lie).
Bad Obstetric History,
Hypertensive disorders such as preeclampsia,
Prolapse of umbilical cord,
Elderly primigravida,
Medico-gynecological disorders:
chronic hypertension,
chronic nephritis,
diabetes,
heart disease,
pelvic tumor,
vaginal atresia,
Carcinoma of cervix,
Cervical dystocia.
Common Indications of Cesarean Section
1) Failure to Progress in Labour:
Prolonged labor in which the cervix does not dilate properly and the placenta does not descend properly in the birth canal, which necessitates a caesarean section.
2) Fetal Distress:
Signs that the fetus cannot tolerate labor properly, such as an abnormal fetal heart rate, indicate a reduced oxygen supply to the fetus, necessitating a cesarean section.
3) Malpresentation of Baby:
When the baby is in breech presentation (buttocks as presenting part), transverse position, vaginal delivery is impossible and caesarean section is required.
4) Placental abnormality:
Placenta previa:
In which the placenta is partially and completely implanted on the lower uterine segment i.e. when the placenta is present as the presenting part.
Abruptio placenta
In which, if the patient prematurely separates from the uterine wall, there is a need for caesarean section.
5) Maternal health condition
such as genital herpes,
heart disease,
severe hypertension,
condition like
6) Previous Caesarean Section:
If first caesarean section is done then repeat caesarean section depends on scar of privy cs and time duration of pregnancy.
7) Multiple Pregnancy:
When there are multiple pregnancies like twins, triplets and based on the presenting part and position of the fetus, there is a need for caesarean section.
8) Umbilical cord prolapse:
In which the umbilical cord slips down through the cervix due to which the blood supply to the fetus is likely to be cut off.
9) Maternal Request:
In some cases, due to any personal or psychological reason, the mother herself selects caesarean section.
10) Emergencies during Labour:
Complications during labor such as uterine rupture, severe bleeding, and maternal illness necessitate an immediate caesarean section to protect the health and safety of the mother and baby.
Thus, in all these conditions there is a need to perform caesarean section.
Q-2 Write Short Notes (Any Five) 5×5=25
🔸 a. Indications of caesarian section-
Indications for caesarean section are divided into two categories:
1) Absolute, (in which vaginal delivery is not possible)
2) Relative (in which vaginal delivery is possible but risks to mother and baby)
1) Absolute, (in which vaginal delivery is not possible):
Central placenta previa,
Severe degree contracted pelvis,
Cervical or broad ligament fibroids,
Vaginal atresia/obstruction,
In advanced cervical carcinoma,
Cephalopelvic Disproportion,
Obstruction due to pelvic mass,
Fits a death.
2) Relative (where vaginal delivery is possible but risks to mother and baby):
Cephalopelvic Disproportion,
contracted pelvis,
Prevous cesarean delivery,
Fital Distress,
Abnormal uterine contractions,
large feet,
small pelvis,
fail induction,
Antepartum haemorrhage eg, placenta previa, abruptio placenta.
Malpresentation or abnormal lie (transverse lie).
Bad Obstetric History,
Hypertensive disorders such as preeclampsia,
Prolapse of umbilical cord,
Elderly primigravida,
Medico-gynecological disorders:
chronic hypertension,
chronic nephritis,
diabetes,
heart disease,
pelvic tumor,
vaginal atresia,
Carcinoma of cervix,
Cervical dystocia.
Common Indications of Cesarean Section
1) Failure to Progress in Labour:
Prolonged labor in which the cervix does not dilate properly and the placenta does not descend properly in the birth canal, which necessitates a caesarean section.
2) Fetal Distress:
Signs that the fetus cannot tolerate labor properly, such as an abnormal fetal heart rate, indicate a reduced oxygen supply to the fetus, necessitating a cesarean section.
3) Malpresentation of Baby:
When the baby is in breech presentation (buttocks as presenting part), transverse position, vaginal delivery is impossible and caesarean section is required.
4) Placental abnormality:
Placenta previa:
In which the placenta is partially and completely implanted on the lower uterine segment i.e. when the placenta is present as the presenting part.
Abruptio placenta
In which, if the patient prematurely separates from the uterine wall, there is a need for caesarean section.
5) Maternal health condition
such as genital herpes,
heart disease,
severe hypertension,
condition like
6) Previous Caesarean Section:
If first caesarean section is done then repeat caesarean section depends on scar of privy cs and time duration of pregnancy.
7) Multiple Pregnancy:
When there are multiple pregnancies such as twins, triplets and based on the presenting part and position of the fetus, there is a need for caesarean section.
8) Umbilical cord prolapse:
In which the umbilical cord slips down through the cervix due to which the blood supply to the fetus is likely to be cut off.
9) Maternal Request:
In some cases, due to any personal or psychological reason, the mother herself selects caesarean section.
10) Emergencies during Labour:
Complications during labor such as uterine rupture, severe bleeding, and maternal illness necessitate an immediate caesarean section to protect the health and safety of the mother and baby.
Thus, in all these conditions there is a need to perform caesarean section.
b. Fetal skull diameters
Diameter of femoral skull
Anterior posterior diameter
1) Suboccipito Bagmatic:=9.5 CM,
From the lower part of the nape of the neck to the center part of the bregma (anterior fontanel).
2)Suboccipito frontal:= 10 CM
From below the nape of the neck to the anterior end of the anterior fontanel or to the center part of the syncytium.
3) Occipito Frontal:= 11.5 CM
From the occipital eminence to the root of the nose i.e. to the glabella.
4)Mentovertical:= 14 CM
Mentovertical diameter from the midpoint of the chin to the highest point of the sagittal suture.
5) SUBMENTO VERTICAL:= 11.5 CM
Submentum vertical diameter from the junction of the floor of the mouth to the highest point of the sagittal suture.
6) Submento Pragmatic:= 9.5 CM
Submento bregma from the junction of the floor of the mouth to the center of the bregma (anterior fontanel).
Transverse diameter
1) Biparietal diameter:= 9.5 CM
Biparietal diameter is the diameter between the two parietal eminences.
2) Supra subparietal diameter:= 8.5 CM
From below the parietal eminence on one side to above the parietal eminence on the opposite side.
3) Bitemporal diameter:= 8.2 CM
Distance between anterior-inferior end of both coronal sutures.
4)Bimastoid diameter: 7.5 CM
The distance between the tips of both mastoid processes.
c. Breast Engorgement –
Breast engorgement is a perimenstrual complication that occurs due to venous and lymphatic congestion in the breast tissue.
Breast engorgement condition is mostly seen after the start of milk secretion in the peripartum period i.e. on the 3rd or 4th day postpartum.
Breast engorgement is usually caused by the accumulation of milk in the breast due to increased secretion of breast milk after child birth, causing the breast to become overfilled and congested. This condition is more common in breastfeeding mothers, especially in the early peripartum period when milk production and secretion are increased. This condition causes the breast to be full, firm and painful. And breast swelling and discomfort is called breast engorgement.
Etiology:
Due to normal venous and lymphatic engorgement in the breast prior to lactase, milk is not released from the lacteal system.
Due to increase in milk production during periperinal period,
Due to inadequate amount of breast milk being removed,
Due to the accumulation of milk in the breast due to not breastfeeding the baby properly.
Due to not providing proper position to the child during best feeding, adequate amount of breast milk cannot be removed.
Symptoms and signs
1) Swelling and firmness
Due to accumulation of milk in the breast, the breast becomes tight, firm and swollen.
2) Tenderness and pain
The breast is tender and painful and especially around the areola and nipple.
3) Skin changes
The skin on the breast is wrinkled and stretched.
4) Difficulty inbreast fitting
Child has difficulty in best fitting.
5) Fever and Malaise
Mother getting fever and feeling generalized body malaise and discomfort due to it.
Diagnostic evaluation
History Collection:
Assessment of symptoms in them,
onset and duration,
Prior History,
Medical History Collection.
Physical Examination:
It includes breast assessment,
skin assessment,
Nipple Examination,
Management of Breast Engorgement
1) Frequent and effective breastfeeding
Advising the mother to provide an adequate best fitting on the child’s demand to prevent milk from accumulating so that adequate amounts of milk can be removed from the best and the condition of breast engorgement can be prevented.
Providing education to the mother about the best feeding technique so that the mother can provide proper position to the child during breast feeding and correct amount of breast milk can be removed which can prevent breast engorgement.
2) Completely emptying of breast milk
At the time of best feeding of the child, education should be provided to the mother to get the best fitting of the child on the other breast only after complete breast feeding on the first breast, due to which adequate amount of milk can be emptied from both the breasts and the condition of engorgement can be prevented.
3) Breast massage and warm compression
Providing education to the mother or gently massaging the breast before best feeding can soften the engorged area.
Advise the mother to provide compresses on the breast through vam water before feeding which can relieve the discomfort.
4) Manual expression of milk
If the child is not able to breastfeed properly, it is best to remove excess milk from the breast by using a breast pump or expressing milk by hand to prevent breast engorgement.
5) Comfort measures
Advise the mother to avoid wearing tight fitting clothes.
To provide proper work and comfortable environment to the mother.
6) Pain Relieve
If the mother is in pain, provide analgesic medication to relieve the pain.
Ex:
Acetaminophen,
Ibuprofen.
d. Active management of third stages of labour- Active management of the third stage of labour
Active management of the third stage of labor
Active management of the third stage of labor involves the involvement of a set of procedures and interventions due to which the risk of post-partum haemorrhage (PPH) can be reduced and the placenta can be delivered properly.
Components of Active Management of Third Stage of Labor
1) Administration of uterotonic drug
Ex: Oxytocin
Timing
Administering the drug oxytocin (to stimulate uterine contractions) to the mother immediately after the birth of the baby, oxytocin is the drug of choice in the active management of the third stage.
Provide 10 units of oxytocin IM (intracellular) in third stage active management.
Oxytocin enhances uterine contractions and helps expel the placenta.
2) CCT (Control Cord Traction)
Control cold traction uses a manual method in which the umbilical cord is tracked and gently pulled downwards and backward to allow the placenta to separate from the uterine wall and then be expelled, but control cord traction is performed when uterine contractions are present. The hand is placed on the suprapubic area and then performed.
3) Delay code cutting
After delivery of fits, wait for one to three minutes and then cut the umbilical cord. This technique is more useful in term newborns. Because the newborn can receive an adequate amount of blood from the placenta due to which the condition of anemia can be prevented.
But in pre-term babies, the liver is immature and the red blood cells break down in excess and if delayed coda cutting is done, due to this, the condition of hyperbilirubinemia (jaundice) may arise in the newborn.
4) Post partum vigilance
Proper inspection of placenta after delivery of placenta including proper assessment of cotylodon, lobe and maternal and fetal site followed by fundal massage after delivery of placenta so that uterine contractions can be continued and if retained bits of placenta can be expelled properly. .
Benefit of Active Management
Reduce risk of hemorrhage
Active management of the third stage can reduce the risk of postpartum hemorrhage.
Faster delivery of placenta
Due to the active management of the third stage, the time duration of delivery of the placenta is reduced, due to which the time of the third stage can be reduced.
Lower incidence of retained placenta
Active management of the third stage can lead to delivery of a complete placenta, thereby reducing the incidence of retained placenta.
Improve Maternal Outcomes
Complications of excessive bleeding in the mother can also be reduced by reducing the time direction of the third stage.
Thus, active management of the third stage of labor is an evidence-based approach whose main aim is to reduce maternal morbidity and mortality rates by reducing the condition of post-partum haemorrhage in the mother. This management involves the use of uterotonic drugs, control cord traction, delayed cord cutting and watchful vigilance due to which the placenta can be delivered safely and properly and complications in the mother can be reduced.
🔸 e. Breech presentations
Definition
Breech presentation is a malpresentation of the fetus in the uterine cavity in which the lie of the fetus is longitudinal but the podalic pole (buttocks) is in the pelvic brim as the presenting part.
Attitudes/ Classification/ Varieties of Breach Presentation
There are mainly two types of breech presentation.
1) Complete (flexed breech),
2) Incomplete There are three other types of incomplete.
a) Breach with extended legs (Frank Breach).
b)Footling presentation.
C) Presentation of
1) Complete
(flexed breech),
A normal attitude of total flexion is maintained. In complete breech, the leg of the fit is flexed at the thigh and the foot is flexed at the knee and the foot is presented with the buttock of the fit.
In which as presenting part:
2 Butts,
external genitalia,
And 2 fits.
2) Incomplete
In Incomplete, there is varying degrees of extension of the legs in podelicpoles.
There are three other types of incomplete.
a) Breach with extended legs (Frank Breach).
b)Footling presentation.
C) presentation of the (knee).
a) Breach with extended legs (Frank Breach).
In this condition, the legs of the fit with the breech are extended i.e. the thigh of the fit is bent over the trunk of the fit and the leg is straight from the knee (knee).
The presenting part consists of 2 buttocks and external genitalia.
This condition is more common (70%) in primigravida.
b) Footling presentation:
A footling presentation occurs both and the leg is partially extended with one or both legs as the presenting part.
C) Presentation of the (knee):
In ni (knee) presentation the ni (knee) is presented in the brim as the thigh is extended but the ni is flexed.
etiology
Fault in passenger(fits):
in it,
Extended legs, prematurity,
twins,
hydrocephalus,
Dead fetuses.
Fault in passage (birth canal):
placenta previa,
hydroamnios,
Oligohydro amnios,
Due to less tone of uterus and abdomen.
Maternal factor
contracted pelvis,
placental malformation,
Scanty Liker Amni,
oligohydro amnios,
Uterine Abnormalities.
Diagnosis:
clinical,
sonography,
Radiological
Clinical:
Fundal Grip:
If there is no part of the head of the fetus, a hard global mass is felt.
Head Ballotment.
Lateral Grip:
The back side of the fetus is felt at one site and the irregular extremities are felt at the other.
Pelvic gripe::Pelvic gripe consists of a soft broad and irregular mass like structure.
Fetal Heart Sound: Fetal heart sound is heard around the umbilical cord.
Vaginal examination: Soft and irregular parts are felt during pregnancy.
Sonography
Sonography is used to confirm the clinical diagnosis.
If there are any congenital abnormalities in the fetus, it can be identified.
In sonography, the gestational age of the fetus and its approximate weight are measured.
Radiology: Radiology is done to confirm the diagnosis and note the position of the head and limbs.
Mechanism of Labour
In sacro anterior position
The principal movement takes place in three places.
1)Buttx,
2) Solder,
3) Head.
1) Buttocks:
Buttocks are engaged in any one of the oblique diameters of the pelvis.
Its engaging diameter by the trochanteric (10 cm) approaches the iliopubic eminence with the sacrum. A breech presentation is engaged when the diameter passes through the pelvic brim.
It continues to descend until the anterior buttocks touch the pelvic floor.
Then the internal rotation of the anterior buttocks is 1/8th of circular rotation behind the symphysis pubis. Along with this the trunk descends with lateral flexion of the trunk. And the anterior hip emerges first from below the symphysis pubis. Then the posterior hip is delivered.
This is followed by delivery and restitution of the trunk and lower limbs. In it the buttocks which were in the engaging oblique diameter come into position.
Solder:
The bisacromial diameter (12 cm) is engaged in the same oblique diameter of the pelvis immediately after delivery of the buttocks and trunk.
Internal rotation of the solder occurs in the anterior-posterior diameter of the pelvic outlet. With it, the external rotation of the trunk is 1/8th of the circle.
Then delivery of posterior shoulder with anterior flexion of delivered trunk followed by delivery of anterior shoulder.
Untwisting the trunk in restitution leads to the left sacro anterior (LSA) anterior solder to the right and the right sacro anterior (RSA) to the left.
Then 1/8 th of circle anterior rotation of occiput followed by external rotation of solder in the same direction.
Now the femoral trunk comes in a dorso-anterior position.
Head:
The suboccipitofrontal diameter of the head engages in the opposite oblique diameter or transverse diameter of the buttocks occupied.
Flexion increases with descent.
Occiput anteriorly 1/8th or 2/8th of circle internal rotation behind symphysis pubis. Next the subocciput continues to descend until it falls below the symphysis pubis.
Chin, mouth, fore head, vertex, occiput are delivered one after the other by flexion of the head.
Management of breech delivery
Assessment of cases for breech delivery, especially in primigravida, age of mother, complicating factors, size of baby, pelvic capacity, CT scan,
like this. Proper assessment of RI ultrasonography examination etc.
Delivery is planned by two methods when there is a breech presentation.
1) Elective caesarean section,
2) Spontaneous labor and vaginal breech delivery.
1) Elective Cesarean Section:
Indication:
bigbaby,
Hyperextension of the head, footling presentation, or preterm birth weight less than 1500 gm.
In obstetric or medical complications.
2) Spontaneous Labor and Vaginal Breech Delivery:
Indication:
Average Featal Weight,
flexed fetal head,
Adequate pelvis,
Absence of obstetric or medical complications,
Emergency caesarean section and continuous labor monitoring are facilitated with presence of experienced obstetrician.
Management of vaginal breech delivery:
First stage
Management is generally the same as normal labor except that the onset of spontaneous labor increases the chance of vaginal delivery.
Perform pelvic assessment and vaginal examination after membrane rupture as there are chances of cord prolapse.
Start an intravenous line to the mother and provide lactated Ringer’s solution.
Do not give to mother for oral intake.
Then send for blood group and cross matching.
Monitor fetal status and progress of labor and provide oxytocin infusion for labor augmentation.
First, cesarean section is indicated if there are any complications during labor, labor not progressing, fitus distress, code presentation or prolapse.
Second stage
There are three methods of vaginal breech delivery:
1) Spontaneous
Expulsion of the fetus with little assistance is not the preferred method.
2) Assisted breech
It helps in the delivery of the fetus from start to finish.
3) Breach extraction
It involves delivery of a portion of the fetus or the entire body by obstetricians.
This method is rarely used as it causes trauma to the fetus and the mother.
Assisted breech delivery
A breech delivery should be performed by a skilled obstetrician.
For that, the neonatologist should keep the anesthetist, assistant instrument and suture material, resuscitation equipment for the baby ready.
steps
When the anterior buttock of the fetus is visible, lift the patient onto the labor table and provide the patient with lithotomy position as the buttock distends the perineum.
After doing antiseptic cleaning and emptying the bladder through catheter.
Administer pudendal block to the patient. Episiotomy, when necessary, is given when the perineum is distended.
Then advise the patient to wear bearing down afores.
Then do not touch the feet until the buttocks slip with the leg in the flex breech and deliver to the umbilical.
After the delivery of the trunk to the umbilical cord, take the umbilical cord downwards to one side, if the back is on the posterior side, rotate the trunk and bring it to the anterior side.
DELIVERY OF ARMS
To prevent extension of the arm, the assistant should keep his hand on the fundus and give steady pressure during uterine contractions, note the position of the hand when the scapula is visible, when the axilla is visible, deliver the arm one after the other by simple locking with a finger in each elbow and At that time, cover the baby’s legs with a stylish towel and never pull them down to hold them.
Delivery of the after coming head
The preferred time between umbilical to mouth delivery is five to ten minutes and is a more crucial stage. Following are the general methods for delivery of fitus:
1)Burn Marshall Method
This method involves letting the baby hang on its own weight and asking the assistant to apply suprapubic pressure with the hand in a downward and backward direction.
So the head flexes more and the pelvic cavity has a favorable diameter, when the nape of the neck is visible below the pubic arch, hold the baby with a finger between the two ankles.
Then keep steady traction and keep the trunk in upward and forward direction During this time hold the perineum with the left hand and allow the face and brow to be delivered from it one after the other After delivery of the mouth remove the secretion with a mucus shaker for the delivery of the rest of the head Depress the trunk.
2) Forceps delivery
In forceps delivery, the head should be in the pelvic cavity for delivery of the after coming head in the breech, Das or specially designed piper forceps are used in ordinary forceps.
3) Malar Flexion Shoulder Traction (Modified Mauriceau and Smiley Weight Technique):
Place the baby on the supinated left forearm and let the limbus hang down on either side.
Place the middle and index fingers of the left hand on the malarbone on either side. This will maintain the flexion of the head.
Then place the ring and little fingers of the pronated right hand on the child’s right shoulder, the index finger on the left shoulder and the middle finger on the occipital region.
Apply traction in a downward and backward direction until the nape of the neck is visible below the pubic arch. and have the assistant apply suprapubic pressure to maintain flexion and
Then, by moving the baby in an upward and forward direction towards the mother’s abdomen, the face, brow will be delivered and finally the occiput and vertex will be delivered by depressing the trunk.
Resuscitate the baby immediately if there is asphyxia after delivery.
🔸f. Essential New bom care –
properly assessing and stabilizing the newborn.
Essential newborn care is crucial for the fetus to stabilize from intrauterine life to extrauterine life.
Goal of Essential Newborncare
1) Respiration of newborn is done to establish, maintain and provide support.
2) To prevent the newborn from vomiting and hypothermia.
3) To prevent infection in the newborn.
4) To provide safety to the newborn and prevent him from injury.
5) To provide immediate treatment by early identification of any actual or potential problem in the newborn.
Immediate newborn care is provided.
Essential Newborn Care
1) Establishment of Respiration
Immediately patent the newborn’s airway and clear the airway properly when the newborn is received. Due to which the newborn can effectively breathe.
As soon as the newborn’s head is born, wipe the mouth and nose and suction the mouth and nose so that the newborn can breathe properly. Saxon should be done through the mouth first and then through the nose to prevent aspiration of secretions.
2) Initiation of Cry: Normally 99% of newborns cry immediately and spontaneously after delivery, this cry is known as a good sign for newborn’s breathing.
If the newborn does not cry properly, follow the steps below:
a) If the baby does not cry spontaneously or if the cry is weak then slightly simulating the baby to cry.
b) Lightly rub the soles of the baby’s feet instead of slapping them on the bum to stimulate the baby’s cry. Stimulate the baby to start crying after removing the newborn’s secretions.
C) Newborn’s cry is usually loud and husky and proper monitoring of newborn if there is any abnormal cry like,
•>Hypech cry:= due to hypoglycemia and increased intracranial pressure,
Weak cry:= prematurity,
Hosacry:= laryngeal stridor
3) Care of Code
Cord care is important immediate care of the newborn.
A newborn’s cord should be clamped within 30 seconds of birth and then properly cut.
After the newborn is delivered, keep the newborn on the mother’s abdomen.
Then properly clamp the cord from two opposite sites by cord clamp.
The first clamp should be placed 5 cm from the umbilicus and the second clamp should be placed 2.5 cm from the first camp.
Then properly cut the cord between the two clamps.
Do not apply anything to the cord, let it dry and fall naturally.
The code folds down naturally within seven to ten days after birth.
Prevent the cord from getting wet by water and urine.
If any kind of discharge and bleeding is present in the cord, immediately assess the cord clamp and then loosen it properly.
Immediately if the following signs and symptoms are observed in the coda
To report such as,
Foul smell coming from the cord,
Seeing any discharge,
Redness around the cord,
The cord is wet,
If the cord does not fall down in 7-10 days,
inflammation,
Fever etc.
4) Maintain position of the newborn
During the first 12-18 hours after birth, the newborn is prone to choking, phlegm and gagging of mucus. So providing proper position to the newborn.
In which providing the fitters with a proper side lining position due to which the mucus is removed
5) Identification and banding
After the baby is born, proper identification band should be applied to the baby so that the baby can be properly identified.
6) Eyecare
Clean the newborn’s ice from inner canthers to outer canthers with properly sterile gauze.
Apply erythromycin or tetracycline ointment from the lower lead in ice if needed.
7) Attachment and Bonding
After the birth of the baby, placing the baby on the mother’s abdomen, due to which bonding with the mother and proper skin-to-skin contact can take place, due to which the attachment of the mother and the baby can occur and the baby can be prevented from hypothermia.
8) APGAR score
APGAR score is the most important parameter of immediate newborn care.
APGAR score should be assessed at 1 minute and then 5 minutes after birth.
In APGAR score,
A:= appearance (skin color),
P:=Pulse (hotrate),
G:= grimace (reflux irritability),
A:=activity (muscle tone),
R:= Respiration (Respiratory Efforts)
is assessed.
APGAR score has a total score of 0-10.
APGAR score at 1 minute after birth:
If the Apgar score is 7-10 then it is called normal i.e. no depression in which the baby is provided with normal post delivery routine care.
If the APGAR score is between 4-6, it indicates mild depression in which the child requires assistance for breathing.
If the APGAR score is between 0-3, it indicates severe depression requiring resuscitation of the child.
APGAR score at 5 minutes after birth:
An APGAR score between 7-10 is considered normal, but if the Apgar score is below 7, the baby needs to be monitored for another half hour.
9) Vitamin K:
A newborn’s intestine is sterile for some time after birth i.e. the bacteria responsible for manufacturing vitamin K is not present in the intestine which is why the newborn cannot manufacture vitamin K i.e. vitamin K is a clotting factor. The factor responsible for this is that if this vitamin K is not present in the body of the newborn, then there are chances of building in the newborn, so as a preventive measure, artificial injection of vitamin K is provided to the newborn baby.
Dose:=
In pre term:=0.5 ml,
Full term:= 1 mg.
Intra muscularly (IM) is provided on the vastus lateralis (lateral anterior thigh).
Thus essential newborn care after birth is provided accordingly.
🔸g. Placenta Previa
When the placenta partially or completely implants near or above the internal os of the lower segment of the uterus it is called “placenta previa”. 1/3 of cases of antepartum hemorrhage are due to placenta previa.
Etiology:
The exact cause of placenta implantation in the lower uterine segment is unknown.
Some theories are given below:
Dropping Down Theory:
According to this theory, the fertilized ovum drops down into the lower uterine segment.
Persistence of chorionic activity
It explains the formation of the capsular placenta from the chorion coming in contact with the decidua vera of the lower segment of the uterus.
Defective decidua
In this the chorionic villi are spread over a large area of the uterine wall to receive nourishment.
During this process, not only does the placenta become membranous but implantation in the lower part of the uterus may occur.
Large Surface Area of Placenta:
Because of the big surface area like twins, the placenta implants in the lower segment.
High Risk Factors:
Multipara.
Increase maternal age
( > 35).
Having a history of privy lower segment caesarean section (L.S.C.S).
If any other scar is present in the uterus due to it.
Big Placental Size and Abnormalities,
Placental hypertrophy due to smoking,
Privy curettage.
Types of placenta previa:
There are four types of placenta previa depending on the degree of extension of the placenta into the lower segment of the uterine cavity.
1) Type I (lateral placenta previa),
2) Type II (Marginal placenta previa),
3) Type III (Incomplete placenta previa),
4) Type IV (Complete placenta previa)
1) Type I (Lateral placenta previa):
In this type no major part of the placenta is attached to the upper segment but only the lower margin enters the lower segment but does not reach the os.
2) Type II (Marginal placenta previa):
In this type the placenta only reaches the margin of the internal os but does not cover it.
If the placenta is anterior, vaginal birth is possible, blood loss is average, risk of fetal hypoxia is higher than maternal shock.
3) Type III (Incomplete placenta previa):
The placenta covers the internal os not centrally but partially when in late pregnancy the cervix begins to efface and dilate, causing bleeding due to the lower stretch.
4) Type IV (Complete placenta previa):
In this the placenta covers the internal os even when it is fully dilated. Severe haemorrhage occurs and caesarean section is required to save the life of mother and baby.
Sign and Symbols
symptoms
vaginal bleeding,
Bleeding is sudden.
Bleeding is painless.
Bleeding is causeless.
Bleeding is recurrent.
Bleeding is unrelated to activity and often occurs during sleep and the patient is alarmed upon waking to find himself in a pool of blood.
In placenta previa, the blood is bright red because of bleeding from a separated ytero-placental sinus.
Sign
The patient has evidence of late pregnancy.
Evidence of blood loss is also seen such as shock, anemia depending on the degree of haemorrhage.
Abdomen
In this, the size of the utrust is according to the gestational period.
Uters feel soft, relaxed, and elastic.
A breech, transverse, unstable lie shows malpresentation.
The head is floating.
A fetal heart sound is often present.
Bright red blood is seen in placenta previa.
Diagnostic evaluation:
Diagnostic evaluation is done by two methods:
1) Placentography,
2) Clinically
1) Placentography:
a) Sonography:
I trans abdominal
Ultra sound
(TAS).
II trans vaginal
Ultra sound
(TVS).
III Transperineal
Ultra sound.
Magnetic Resonance Imaging (MRI),
radiography,
radioactive isotope,
2) Clinically:
By Internal Examination (Double Setup Examination),
Direct visualization daring cesarean section,
Management of placenta previa:
Principles of management of placenta previa
To prevent injuries to the fitus,
To reduce the risk of infection,
To control vaginal bleeding,
To promote health and reduce anxiety.
Management of placenta previa:
Provide adequate amount of antenatal care to the patient to improve the health status of the mother.
Perform an ultrasound at 20 wks followed by a repeat 34 wk ultrasound to confirm the type of placenta previa.
Instruct the pregnant woman to rest in bed and then gently palpate the uterus for tenderness and tone.
To properly assess the amount of blood loss.
Color of bleeding and complete blood count (CBC) test.
Inj to patient as per hospital policy and prescription. Provide Morphine 15 mg IM.
Properly assess the amount of blood loss the client has suffered.
To properly note the client’s vital signs like, temperature, pulse, respiration, blood pressure.
To properly assess whether the client has an anemic condition or not.
To check the fetal heart sound regularly and frequently.
Abdominal examination of the pregnant woman followed by note of fetal heart sound and properly note whether any tenderness is present in the uterus.
Do not perform vaginal examination in the condition of placenta previa as it may increase bleeding.
Properly monitoring pregnant women for continuous or intermittent bleeding.
Arrangements should be made to shift the pregnant woman to another well equipped hospital having blood transfusion facility, caesarean section facility and neonatal care unit if required.
If the client has a hemorrhagic condition, start intravenous dextrose normal saline drips.
Advise the client to avoid stress and advise to take complete bed rest.
When the client is admitted to the hospital follow the following treatment viz.
Providing immediate attention,
Then properly planning what type of treatment is required.
In the immediate assessment, the amount of blood loss the client has suffered, his general condition, his pallor, pulse rate and blood pressure should be properly noted.
Send blood samples immediately to the laboratory for cross-matching and assessment of hemoglobin levels.
Start an infusion of normal saline to the patient.
Keeping blood ready to hand for transfusion after cross matching of blood.
Perform gentle abdominal palpation to assess the presence of any active bleeding.
Formulation of line of treatment:
In this, proper treatment should be provided according to the condition.
Hemoglobin level should be properly estimated and should be 10 gm or more.
Expectant treatment should be provided till 37 weeks are completed.
Termination in any of the following conditions viz:
Recurring hemorrhage,
dead fits,
Fetus is a congenital malformation,
India If there is uterine growth retardation (IUGR), termination is performed in such conditions.
Specific treatment is started after admission to the hospital. like,
Vaginal examination is performed in the operation theater to properly prepare for caesarean section.
After examination the membrane is artificially ruptured then oxytocin is started then delivery is conducted as per condition.
If the labor process is progressing satisfactorily without any bleeding, perform vaginal delivery.
If the bleeding is continuous, the pregnant woman should undergo caesarean section.
Assess presentation if baby is malformed or dead, ventous delivery if vertex presentation and breech delivery if breech.
🔸 h. Partograph
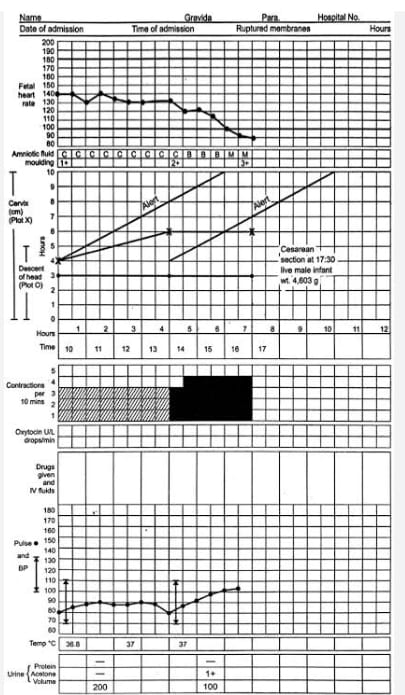
Partograph
Definition:
Partograph A Cervical dilatation,
A graphic recording and tool for fetal head descent and labor progress and the condition of the mother and fetus. Partograph provides immediate and relevant information about the condition of the mother and fetus.
It recognizes the need to take action for appropriate time and timely referral. Morbidity and mortality rate of mother and fetus can also be improved through partograph.
Objectives or Advantages:
1) To record observations during labor properly.
2) To understand the latent and active phase of labour.
3) Interpreting the partograph to recognize any deviation from normal and take appropriate action.
4) To know the progress of labor so that action can be taken and referred at the right time.
5) Records can be seen at a glance in a single seat and easily handed over.
6) To avoid having to record the event of labor repeatedly.
7) To prolong labor and decrease the rate of education.
Observation Charted on Partograph:
1) Pregnant Woman Information:
A) Name,
B) GTPAL score
G: gravida,
T:=Tommy Birth,
P:=mercury,
A:= Abortion,
L:= Living Children.
C) Name of Hospital,
D) Hospital Registration Number,
E) Date and time of admission,
F) Time of membrane rupture,
G) Period of Gestation,
H) Date and time of labor onset.
2) Fittal condition:
A) Fetal heart rate,
B) amniotic fluid,
C) Molding.
3) Progress of Labour
A) Cervical dilatation,
B) Descent of head,
C) uterine contractions.
4) Maternal condition
A) Oxytocin, drugs and I.v. fluid administration
B) pulse,
C) blood pressure,
D) Temperature,
E) Urine volume, acetone and protein.
All this information is filled in a partograph.
Points to keep in mind while filling partograph:
1) Partograph maintenance should be started when the woman reaches the active phase of labor and the pregnant woman should not be left alone.
2) The fetal heart rate should be counted and recorded every half hour.
Fetal heart sounds should be counted for a full 1 minute and should be counted immediately after uterine contractions are detected.
3) Monitor uterine contracture frequency, intensity, duration, pulse, fetal heart rate every 30 minutes when dilatation of cervix is 4 cm or more.
4) Monitor blood pressure and cervical dilatation (in cm) every two hours.
5) Monitor descent of head and temperature every four hours.
Partograph
1) Patient Identification Data
In this, the woman’s name, age, GTPAL score, date and time of admission, registration number, time of rupture of membranes and time and date of onset of labor are marked.
2) Fittal condition
Counting and recording the vital heart rate every half hour.
To account for the full 1 minute of the fittal heart rate.
To count fetal heart rate immediately after uterine contractions.
Fetal heart sound (FHS) < 120/Minutes or FHS > 160/Minutes indicates fetal distress. If there is a condition of fetal distress, immediate action should be taken.
A vertical column in each small box represents that half-hour interval.
2) Condition of membrane
Record condition of amniotic membrane and color of amniotic fluid every 30 minutes along with fetal condition.
A) If Amniotic Membrane is Intect :=I (Intect),
B) If liker is clear := C (Clear),
C) If Liker A is Absent := A( Absent) ,
D) If the amniotic membrane is ruptured := R (Rupture),
E) If meconium stained liquor:= M( meconium),
F) If blood is present in the liquid: B (Blood)
Thus, marking the condition of amniotic membrane and amniotic fluid in the partograph.
3) Molding (The bones of the fetal head are separated by sutures and fontanelles, but while passing through the birth canal, the bones of the fetal head overlap each other and the gap of the head changes for some time due to which the fetal head is a (The condition can easily pass through the birth canal is called molding.)
Moldings are recorded by grade to record.
A) 0 -> If bones are separated and sutures are easily felt.
B) + -> When the bones just touch each other.
C) ++ -> When bones are overlapping but easily separated.
D) +++ -> Bones are severely fixed when overlapping.
4) Progress of Labour
Start plotting labor progression on the partograph only after the woman is in active labor.
Active labor A cervical dilatation of 4 cm or greater and the athlete having two good contractions every 10 minutes should start plotting on the partograph.
Recording cervical dilatation in cm every four hours.
Record the onset of cervical dilatation starting from the left luteal line (when the mother is in active labour). Normally the graph line is continuous above the left alert line showing the proper time each time.
If the alert line is crossed i.e. if the graph moves to the right of the alert line then it indicates prolonged labor. So the midwife is immediately alerted that there is something abnormal in the labor. Noting the time the alert line is crossed and immediately initiating measures for immediate treatment or referral.
When the graph crosses the action line i.e. if the action moves to the right side of the line, start treatment immediately or refer the mother to appropriate medical services.
The gap between alert and action line is 4 hours.
5) Uterine contractions
Recording uterine contractions every half hour Contractions twice in ten minutes indicate good uterine contractions.
Marking it as follows in the box of the partograph.
-> Mild uterine contractions < 20 seconds,
-> Moderate uterine contractions 20 – 40 seconds,
->Strong uterine contractions > 40 seconds.
6) Cervical dilatation and descent of fetal head
Descent of the fitter head occurs simultaneously with cervical dilatation throughout the labor process.
Until the cervix is 7 cm, the descent of the fetal head is assessed by abdominal palpation with the assessment of the fifth (5) number of the fetal head above the pelvic brim.
In the partograph, cervical dilatation is plotted by (x) while descent of the fetal head is plotted by (O).
7) Maternal condition
Maternal pulse every half hour
is recorded on the partograph and is plotted in the partograph by a dot(•).
Maternal blood pressure is recorded every 4 hours with both systolic blood pressure and diastolic blood pressure indicated by vertical arrows ( ↕ ) with the upper end of the arrow indicating systolic BP. While the arrow no lower end shows the diastolic blood pressure.
Recording the maternal temperature every four hours on a partograph.
Proper recording of maternal urine volume, urine acetone and protein level on partograph.
If any drug or oxytocin medication is given to the mother during the labor process, properly recording the dose route and time of administration.
Thus, early, quick and relevant information about labor progress and condition of mother and fetus can be obtained through Partograph.
Q-3 (A) Fill in the blanks,
1) Average length of menstrual cycle is——–days. An approximate menstrual cycle is of ——days
28 days.
2) HELLP syndrome stands for———– Give the full name of HELLP syndrome————
HELLP:
Hemolysis, Elevated Liver enzymes, and Low Platelet count
3) Increase amniotic fluid (1500-2000ml) in pregnancy is called
polyhydramnios
(Polyhydramnios).
4) Assessment of labor done by ————– Assessment of labor is done by ——-.
partograph
(partograph)
5) Premature separation of placenta is called.
abruptio placentae (abruptioplacenta).
6) Cyanosis and softening of cervix seen in —— sign. Sinusosis and soft ning of cervix are seen in —–sine.
Hegar sign
7) Abortion with clinical evidence of infection of uterus is called —-.
septic abortion (septic abortion).
8) —————immunogiobulin present in breast milk ————– Immunoglobulin is found in mother’s milk
IgA (Immunoglobulin A).
9) Excessive vaginal bleeding at normal interval of menses is called
menorrhagia (menorrhagia).
10) A Pregnancy continues beyond 2 weeks of EDD is termed as ————-
Postmaturity or
Post term Pregnancy (Postmaturity or Post Term Pregnancy)
(b) state whether following statemenos are true or false 10 State whether the following statements are true or false
1) HCG hormone is responsible for the positive pregnancy test. HCG hormone is responsible for a positive pregnancy test.
True.
2) Oxytocion is a hormone produced by adrenaline gland. Oxytocin is produced by the hormonal adrenal gland.
False
(Reason := Oxytocin is produced from the hypothalamus and stored in the posterior pituitary gland and releases oxytocin).
3) “Crowning” seen during fourth stages of labor. In the fourth stage of labor, the council is observed.
True
4) Vertex fetal position is most favorable for birth. Vatancus fetal position is most favorable for birth.
True
5) Permanent cessation of menstruation is called menopause. Permanent cessation of menstruation is called menopause.
True
6) Rooming in promotes maternal and infant bonding. Rooming in can enhance mother-child bonding
False
(Reason := When the combined duration of the first and second stages of labor is more than 18 hours, it is called prolonged.)
7) Prolonged labor means total time of 1″ and 2nd stage of labor is more than 8 hours. If the total time of first stage and second stage of labor takes more than eight hours, it is called prolonged labor.
False
(Reason := Anterior fontanel which is called bregma closes during 16 to 18 months after birth.)
8) Anterior fontanel closes at 6 weeks. The anterior fontanel closes at six months.
True
9) Syphilis is a systemic disease caused by Treponema pallidum. Syphilis is a systemic disease. which is caused by pallidum in Treponema.
True
10) Post partum hemorrhage means more than 300ml blood loss occurs after delivery. Blood loss of more than 300 ml after delivery is called PPH.
False
(Reason := Post partum haemorrhage is called when,
Whereas if vaginal delivery is done and blood loss is more than 500 ml and if cesarean section is done and blood loss is more than 1,000 ml then it is called postpartum haemorrhage.)
(C) Write Multiple Choice Questions.
1) What is the normal color of amniotic fluid?
a) Clear
c) Brownish
b) Greenish Chinese
d) Golden
2) In the second stage of labor which of the following injection is given to improve uterine contraction. Which of the following injections are given to increase uterine contractions during the second stage of labour?
a) Prostaglandin Prostaglandin
c) Phenergan Rang
b) Oxytocin
d) Diazepam Diazepam
3) Endometrium of the pregnant uterus is known as
a) Decidua
c) Amnion
b) Trophoblast Trophoblast
d) Chorian
4) The height of uterus reaches at the level of umbilicus.
a) 16 weeks
c) 20 weeks
b) 24 wocks 24 weeks
d) 30 weeks
5) If LMP is 10/06/2021 than EDD should be which of the following? If IMP 10/b/021 then EDD will be which of the following?
a) 17/04/2022
c) 26/06/2022
(6)17/03/2022
d) 17/03/2021
6) “Snowstrom” pattern in USG is a characteristic of which of the following condition Snowstop pattern sonography is seen in which of the following conditions?
a) Eclampsia -Eclampsia
c) Abruptio placenta abrupt placenta
b) Hydatidiform mole Hydatidiform mole
d) Placenta previa – Placenta previa
7) In which condition the umbilical cord is attached to the margins of placenta.
a) Batteldore placenta – Batteldore placenta
b) Placenta membranaces- Placenta membonsea
e) Circumvallate placenta – Circumvallate placenta
d) Velamentous placenta
8) As per WHO breast feeding should be initiated after delivery within time of WHO best feeding should be started after delivery.
a) 30 min
c) 60 min
b) 45 min
d) 70 min
9) Largest cell in human body is the largest cell in human body
a) Mycline cell
c) Ovum
b) Glial cell
d) Osteocytes
10) Causes of infertility in male include causes of infertility in male
a) Defective spermatogenesis
c) Obstruction of the offerent duct
b) Sexual dysfunction
d) All of above
Write Multiple Choice Questions.
Q: (1) Ans
a) Clear.
Q: (2) Ans
b) Oxytocin.
Q: (3) Ans
a) Decidua (Decidua).
Q: (4) Ans
(b) 24 weeks.
24 Vic
Q: (5) Ans
(b) 17/03/2022
Q: (6) Ans
b) Hydatidiform mole (Hydatidiform mole).
Q: (7) Ans
Battledore placenta ( Battledore placenta).
Q: (8) Ans
(a) 30 minutes
Q: (9) Ans
(c) Ovam
Q: (10) Ans
d) All of the above.
💪 💥☺ALL THE BEST ☺💥💪
Note :-MCQ ANSWER in unique pattern of APP in both languages is given below paper solution / click here. Clicking on “A” will change the language.
IF ANY QUERY OR QUESTION, REVIEW-KINDLY WATSAPP US NO. – 84859 76407
