ENGLISH GNM-T.Y-Midwifery & Gynecological-28/03/2022 (DONE-paper solution no.4)
GNM-T.Y-Midwifery & Gynecological-28/03/2022

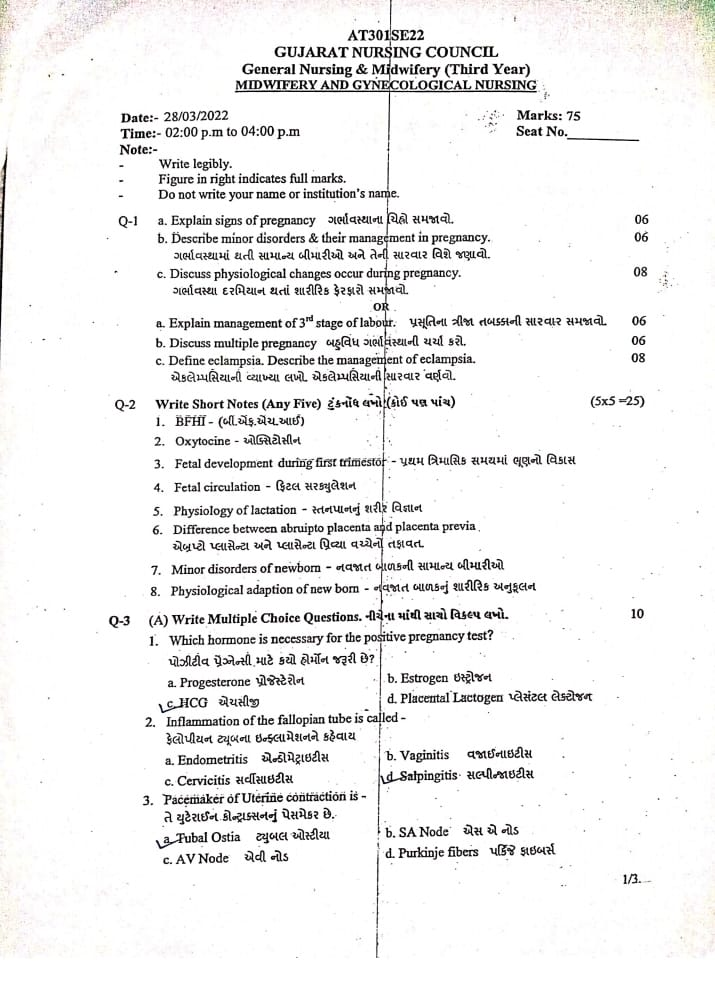
⏩Q-1 🔸a. Explain signs of pregnancy Explain signs of pregnancy 06
Tell the sign of pregnancy
Signs of pregnancy are as follows:
1) Presumptive sign,
2) Probable sign,
3) Positive sign.
1) Presumptive sign:– Mostly subjective i.e. the mother herself feels that she is pregnant while it may be due to another illness.
amenorrhea,
Nausea and Vomiting,
morning sickness,
Tingling sensation in 3 to 4 weeks,
Alarming of breast and nipple,
Appearance of Montgomery tubercles in the breast
Increased micturition,
Pigmentation (changes) in face and breast,
Quickening: The first movement of the mother and fetus occurs around 16 – 20 weeks.
2) Probable sign objective but definite conformation of pregnancy cannot be said.
Enlargement of the abdomen. Abdominal palpation can detect the signs of pregnancy.
Changes in the size and shape of the uterus and enlargement of the uterus.
External Ballotment and Internal Ballotment.
A positive pregnancy test means detection of human chorionic gonadotrophin (HCG) hormone in urine.
Occurrence of Jackmier’s sign or Chadwick’s sign (This sign appears during 8 weeks of pregnancy. Bluish discoloration of the cervix is called Chadwick’s sign, while bluish discoloration of the vagina is called Jackmier’s sign).
Occurrence of Hataman’s sign (This sign is seen from 1-3 months of pregnancy and involves slight bleeding at the time of implantation).
Finding Palmar sign (This sign is seen during 4-8 weeks of pregnancy. This sign shows regular and rhythmic contraction of uterus when bimanual examination is done).
Goodell’s sign (Goodell’s sign is a softening of the lower part of the cervix seen up to 6 weeks).
Hegar’s sign (this sign is seen during 6 to 10 weeks, in this the upper part of the uterus i.e. the body part of the uterus enlarges with the growing of fits and the lower part of the uterus becomes soft).
Piscak Sign:-
(This sign is seen during 6-8 weeks in which the uterus implants in the uterus and enlarges asymmetrically). •Ossander’s sign (This sign is seen during 6-8 weeks. In this sign, a pulsation is felt at the lateral fornix in the vaginal area.)
Braxton Hicks contractions (the uterus goes into spontaneous contractions early in pregnancy, is regular, infrequent, spasmodic, painless, has no effect on dilatation of the cervix, increases near term and finally merges with painful labor contractions). 3) Positive sign.
This sign pregnancy is a conformation.
Hear a vital heart sound,
Active movement of the fetus is felt,
Ultrasonography shows embryos up to 6 weeks followed by fetuses.
Radiological appearance of the skeletal system of Fittus.
Fetal movement and palpation of fetal parts.
Visualization of vital movement.
b. Describe minor disorders & their management in pregnancy. 06 Tell about common diseases in pregnancy and their treatment.
Minor disorders of pregnancy and their management:
1) Digestive System:
Nausea and Vomiting:
Nausea and vomiting are very common in primigravida and especially in women when they wake up in the morning.
Hormones like HCG, Oestrogen, Progesterone are responsible for nausea and vomiting.
Nausea and vomiting are usually more common in primigravida and first trimester.
Management
Dietary changes
Advise the mother to take dry toast, biscuits, salty crackers and protein rich food when she wakes up in the morning.
Advise the mother to take food in small and frequent amounts.
Advising the mother to take low fat food.
Advise the mother to avoid fried food and spicy food.
Advise the mother to take proper antiemetic medication.
Constipation
Constipation is the most common problem in pregnancy. Constipation is mainly seen during the second and third trimester.
Constipation is due to the effects of progesterone, decreased bowel tone and mobility, decreased physical activity,
Due to intake of iron supplement,
Constipation occurs due to the pressure of gravid uterus on the colon.
Management
Advise the mother to take high fiber foods.
Advising mother to intake adequate amount of vegetables and fruits.
Advise the mother to intake 6-8 glasses of water throughout the day.
Advising the mother to fill a glass of water in the morning activates the bowel movement.
Advise the mother to take frequent, small, and low-fat meals.
Advising the mother to do regular exercise.
Advise mother to take milk of magnesia in small amount.
Acidity and heart burn
Acidity and heartburn are commonly seen during pregnancy due to relaxation of the esophageal sphincter.
It is usually more common in mothers during the second and third trimesters.
ACIDITY AND HEART BURN Mostly acidity and heart burn conditions are seen due to increase in progesterone level, decrease in size of intestine, and displacement of stomach due to enlarged uterus.
Management
Advising the mother to eat in small and frequent amounts.
Do not give advice or overeating to the mother.
Advise pregnant women not to sleep immediately after eating. Athletes should remain in a sitting upright position for 30 minutes after eating.
Giving advice to avoid fatty and spicy food.
Advise mother to sleep in reclining position with support of five to six pillows.
Advising the mother to perform tailor sitting exercises.
Advise mother to take antacid medication prescribed by health care personnel.
Bleeding from gums, glossitis and gingivitis
. Bleeding can occur due to increased blood supply due to high levels of progesterone during pregnancy.
Management
Advising the mother to use a soft toothbrush.
Advising the mother to maintain oral hygiene.
Advise the mother to take vitamin-B complex, green leafy vegetables, yeast, eggs and cheese.
2) Circulatory system
Dizziness and fainting
It is mainly caused by the relaxation of the muscles of the blood vessels due to the effect of progesterone.
It subsides due to increase in blood volume.
Later, the pressure of the gravid uterus on the inferior vena cava causes less blood supply to the heart.
Management
Advise the mother to sleep less on her back in the last month. And giving advice to the mother to avoid standing for a long time.
Giddiness (dizziness)
Dizziness can also occur during pregnancy and due to this, loss of balance and the possibility of falling are also more common.
It is usually due to cardiovascular changes during pregnancy and low blood sugar levels and can also be caused by anemia.
Management
Advise the mother to take adequate rest.
Advise mother not to stay in standing position for long time.
Varicose vein
The condition of varicose veins is usually more common during the second and third trimester of pregnancy.
Varicose veins mainly in the lower extremities and vulva develop during pregnancy and hemorrhoids in the rectum also occur due to obstruction of venous return by the pregnant uterus.
Management
Advise the mother to wear supportive shoes.
An elastic crepe bandage and elevating the limb while performing movement in the varicose vein provides release in the symtoms.
Advise mother not to stay in sitting and standing position for long time.
After delivery, the condition of varicositis is relieved.
Complications like bleeding or prolapse are seen in hemorrhoids. Advise to use a small amount of laxatives to keep the bowels soft
Advise for local application of hydrocortisone ointment and replacement of prolapsed piles. Avoid surgical treatment as the condition reduces after delivery.
In ankle AD
Ankle AD usually occurs during the second and third trimesters.
It is usually vasodilatation,
Venous statis and uterine bellows are seen due to increased venous pressure.
Management
Properly marking the mother’s access to fluid is retention or how much weight is gained because fluid retention can also be caused by pregnancy induced hypertension (PIH).
Advise the mother to keep her legs elevated twice throughout the day.
Advising the mother to wear supporting stockings.
Advise the mother to avoid sitting and standing in one position for a long time.
As far as possible, pregnant women should not be given diuretics because the heel subsides on its own by resting and elevating the limbs.
Physiological ED or orthostatic ED does not require any treatment.
3) Musculo skeletal system
Becky
50% of the problem recurs during pregnancy.
Backache can occur during any stage of pregnancy but mostly occurs during the second and third trimester of pregnancy.
Backache is seen due to physiological changes such as joint ligaments laxity (relaxin and estrogen), weight gain, hyperlordosis, pelvis anterior tilt etc.
Another cause is faulty posture, high-heeled shoes, muscle spasm, constipation, and urinary infection etc.
Management
Advising the mother to take proper rest.
Advising mother to use correct body mechanism and improve body posture.
Advise the mother to keep the leg elevated while resting.
Advising the mother not to wear high heeled shoes.
Advise the mother to perform pelvic rocking and abdominal and breathing exercises.
A well-fitted pelvic girdle belt that corrects lumbar lordosis during walking.
Advising the mother to slip on a firm mattress.
Back muscle massage, analgesics and rest can reduce the pain caused by muscle spasm.
Leg cramps
Leg cramps usually occur during the second and third trimesters of pregnancy.
Leg cramps are usually caused by an altered calcium phosphorus balance.
And it can also be due to the pressure of the uterus.
Leg cramps may occur more commonly at night.
Deficiency of calcium and vitamin B12 can also cause leg cramps.
Management
Giving advice to properly massage the legs.
Advise the mother to do regular exercise, specially advise to do walking.
Advising the mother to apply local hits where the leg is painful.
Advise for oral intake of vitamin B1 and calcium.
4) Genito-urinary system
Vaginal discharge
Vaginal discharge that occurs from the first trimester to the third trimester.
It is usually seen due to hyperplasia of the vaginal mucosa and increased mucus production.
Management:–
Advising the mother on proper cleansing and maintaining hygiene.
Advise the mother to wear cotton undergarments and to avoid tight undergarments.
If there is any condition of vaginal infection then apply vaginal application metronidazole and miconazole as per doctor’s advice.
Urinary Urgency and Frequency:-
During the 12th week of pregnancy due to the pressure of the uterus and during the 3rd trimester of pregnancy due to the pressure of the fetal head, the frequency of maturation is observed which is relieved after delivery.
Management:-
Advise mother to intake adequate amount of fluid during the day.
Advise the mother to have a limited amount of fluid intake in the evening time.
Advise the mother to void at regular intervals.
Advise mother to sleep in side lining position while sleeping at night.
Advise the mother to wear a perinatal pad if necessary.
Advising the mother to perform the eagle exercise.
5) Intangimetry system:-
Etching:-
Body itching due to stria gravidarum, poor personal hygiene, heat, race, minor skin diseases.
Management:-
Advising the mother to bathe regularly and daily.
Advise the mother to apply calamine lotion.
Advise the application of talcum powder to provide a soothing effect to the mother’s skin.
Advising the mother to maintain proper hygiene condition.
6) Nervous System:-
Carpal Tunnel Syndrome:-
Fluid retention causes pressure in the ED and on the median nerve, leading to numbness in the mother and pins and needles sensation in the fingers and hands.
Management:-
Advising mother to increase salt intake in diet.
Advise the mother to keep her hand under the pillow.
Insomnia and Headache:-
Insomnia and headaches are usually more common during the second and third trimesters.
Management:-
Bathing with warm water properly while sleeping at night.
Advise the mother to sleep in a total and well ventilated room.
Advise the mother to lie down in lateral position with the support of a pillow.
Advising the mother to share her anxiety and fear.
Thus the minor aliments seen during pregnancy and their management are as follows.
c. Discuss physiological changes occur during pregnancy. 08 Explain the physiological changes that occur during pregnancy.
Physiological changes during pregnancy:-
Pregnancy is a condition from the time of conception to the time of delivery. Physiological changes are observed in the mother’s body during pregnancy due to certain types of specific hormones. These changes occur to develop the fetus, prepare the mother’s body for labor, and produce the best milk during the periperium period.
1) Changes in reproductive system:-
A)Vulva:=
The vulva becomes more edematous and vacuolar.
Superficial varicosities (varicose vein := vein enlarged and swollen, usually seen in leg and also in pelvic area during pregnancy period) are also seen in multipara and labia minora becomes pigmented and its hypertrophy ( Organ size increases).
B)Vajaina:=
Vaginal wall is hypertrophoid,
becomes edematous and hypervascular.
Bluish coloration of the vaginal mucosa due to increased venous blood supply to the vaginal wall is called “Jackemeier’s sign”.
The length of the interior wall increases.
Vaginal secretions are highly acidic, thin and curdy white.
The acidic pH of vaginal secretions inhibits the multiplication of pathogenic microorganisms.
(C) Uterus:=
During pregnancy, the uterus grows more. During pregnancy, the weight of the uterus and its length also increases.
Weight of Uterus:
In the non-pregnant state, the weight of the uterus is about 60 gm, which increases to 900-1000 gm during pregnancy.
Length, Width and Thickness of Uterus:
of the uterus in the non-pregnant state,
Length := 7.5 cm,
Width:=5 cm and thickness:=2.5 cm.
During pregnancy (at term) of the uterus
Length := 30-35 cm,
Height:= 22.5 cm and
Thickness: = 20 cm.
Volume of uterine cavity:
In the non-pregnant state, the volume of the uterus is 10 ml, which increases to 5 liters during pregnancy (at term).
Body of uterus: Growth and enlargement of the body of uterus.
Muscles:-
1) Outer:= longitudinal layer
2) Middle:= vascular layer
3) Inner:=circular layer
Hypertrophy (increase in size) and hyperplasia (increase in number) are seen in muscles.
After 20 weeks of pregnancy, the length of the uterine muscle fibers increases and the uterine wall becomes thinner due to which the uterus becomes softer and more elastic in pregnant condition than in non-pregnant condition.
Vascular System:
Blood supply begins to increase from 20 weeks onwards due to vasodilatation due to estradiol and progesterone.
The diameter of uterine artery doubles and blood flow increases and veins dilate.
During pregnancy the endometrium of the uterus is called decidua.
Braxton Hicks contractions:
Spontaneous contractions of the uterus in early pregnancy are irregular, infrequent, spasmodic and painless due to any dilatation of the cervix.
D) Isthmus:=
During pregnancy the lower segment of the uterus forms an isthmus.
The length of the isthmus in the nonpregnant state is 0.5 cm, which increases in length during pregnancy to a maximum of 7.5 cm-10 cm.
The muscle fibers of the isthmus are arranged circularly in the lower segment and form a sphincter-like structure which helps the fetus to stay in the uterus during early pregnancy. If this sphincter is incompetent, abortion can also occur.
E)Cervix:=
During pregnancy the cervix becomes vascular, oedematous and hypertrophoid and hyperplastic.
Cervix that becomes soft is called “Goodell’s sign”.
The length of the cervix doubles and its volume also increases.
F) Fallopian tubes:=
The length of the fallopian tubes is slightly increased. The tube becomes congested. Muscles hypertrophy and epithelium flattens.
G)overy:=
Ovulation remains at a standstill during pregnancy. The ovary is hypertrophied and vascularized.
In the usual menstrual cycle, the corpus luteum remains constant and enlarges by two 2.5 cm until the 8th week.
Colloid degeneration occurs and the uterus becomes calcified.Estrogen and progesterone hormones are produced by the corpus luteum and provide an environment to maintain the ovum until placental action begins.
H) Breast:=
Breast size, nodularity, and sensitivity increase with increased vascularity of the breast throughout pregnancy due to the effects of estrogen and progesterone.
The nipple becomes enlarged, dark and erectile.
Hypertrophy of 5 to 15 sebaceous glands that are invisible in the non-pregnant state is seen.
” Montgomery
They are called tubercles. They are located around the nipple and their secretion keeps the nipple and areola moist and healthy.
Areola that becomes dark and pigmented is called primary areola.
In the second trimester, another pigmented zone called the secondary areola forms around the primary areola.
In the first three months, the growth of the ductal system in the breast increases as the pregnancy progresses, its alveolar cells become secretory.
Total weight of breast is 0.4 kg.
The cyst enlarges due to alveolar proliferation and fat deposition and clear sticky fluid can be squeezed from the cyst at about 12 weeks.
At 16 weeks this clear sticky fluid becomes thick and yellow called colostrum which is an important sign of pregnancy.
Changes in other systems of the body.
1) Skin Changes:=
A) Face:
Pigmentation occurs around the cheeks, forehead, and eyelids called “gravidarum in close” or “pregnancy mask” which disappears on its own after delivery.
B) Breast:
Visible pigmentation changes occur in the breast.
C) Abdomen:
Laina nigra:-
Melanocyte stimulating hormone causes a brownish black line visible in the midline from the xiphisternum to the symphysis pubis called the linea nigra.
Straya gravidarum:-
Abdominal wall below the umbilicus and sometimes on the chest and breast is a depressed linear mask that is initially pink but turns glistening white after delivery called stria albicans or stria gravidarum.
Vacuolar spindle and palmar erythema are seen with high estrogen levels. Skin
Mild degree of hirsutism (excess hair) is seen and excess amount of hair is lost during purpureal period.
2) Weight Gain:-
Weight loss occurs during the early weeks of pregnancy due to nausea and vomiting. Weight gain remains progressive from the following months.
A healthy woman gains an average of 11 kg (24 lbs) of weight during pregnancy.
During 1st trimester: 1kg,
2nd trimester
During: 5kg,
During 3rd trimester: 5kg,
As the weight increases.
A) Reproductive weight gain:-
1) Weight of Fits: 3.3kg,
2) Weight of placenta: 0.6kg,
3) Weight of Liker: 0.8kg,
4) Weight of Uterus: 0.9kg,
5) Weight of breast: 0.4kg.
B) Net Maternal Weight Gain:-
1) Increase blood volume:=1.3kg,
2) Increase extracellular fluid:=1.2kg,
3) Fat and Protein:=3.5kg.
3) Cardio Vascular System:-
A) Heart has to work more during pregnancy.:-
Cardiac volume increases by 10% but there is no change in ECG.
Cardiac output also increases due to increased heart rate and stroke volume.
Pulse rate also increases.
As the concentration rate increases from 40 to 45 mm, the platelet count decreases slightly.
B) Blood Pressure and Blood Volume:-
Blood pressure remains within normal limits In some women, diastolic pressure drops by 5 to 10 mm during mid-pregnancy.
C) Venus pressor:-
Femoral venous pressure increases by 10 cm due to the pressure of gravid uterus on the pelvic vein, then the blood volume also increases, the volume of red blood cells and plasma volume also increases in many parts of the body like uterus, pulmonary, renal, skin. , and blood flow to the mucosa increases.
4) Respiratory System:-
Hyperemia (increased blood flow) and congestion are seen in the upper respiratory mucosa.
Increased inspiration also increases oxygen intake and oxygen supply to the fetus.
Carbon dioxide is released due to increased exhalation, so the transfer of carbon dioxide from the fetus to the mother’s blood can be easily done due to low maternal carbon dioxide.
In the last weeks of pregnancy, due to the pressure of the gravid uterus on the diaphragm, there is a complaint of breathing difficulty which is relieved by lightening.
5) Digestive System:-
Due to the effect of progesterone, the muscle tone of the gastrointestinal system is reduced.
Relaxation of cardiac sphincter leads to regurgitation of stomach contents and heartburn.
As the gastric size decreases, it slowly empties and is continuous even in labor.
In many women, the gums become spongy and vascular and may bleed during brushing.
A decrease in the size of the intestine leads to better absorption of food and causes constipation.
6) Nervous System:-
Mood changes during pregnancy and periperium period are due to psychological conditions such as nausea, vomiting, mental irritability and sleeplessness.
Women may also develop depression or psychosis.
Compression of the median nerve in the wrist leads to pain and paresthesia (tingling) in the hands and arms, which is called carpal tunnel syndrome and is seen in the last month of pregnancy as well as sensory loss due to compression of the cutaneous nerve.
7) Urinary Track:-
Frequent micturition is commonly seen in early and late pregnancy.
Stress incontinence can also occur.
Due to continuous dilatation of uterus and pelvis from early pregnancy to mid-pregnancy, urinary stasis occurs and infection can also occur. Renal function also increases in pregnancy.
8) Locomotor System:-
Backache is common during pregnancy due to relaxation of lordosis and joints due to relaxin hormone.
Due to weight gain in sacral and lumbar plexus, leg cramps remain and difficulty in walking also occurs.
Thus, physiological changes are observed in women during pregnancy.
🔸OR🔸
🔸 a. Explain management of 3d stage of labor. 06 Explain the treatment of third stage of labour
Management of 3rd Stage of Labour
Management of the third stage is most crucial because it involves separation and expulsion of the placenta from the uterine cavity, and to prevent complications of postpartum hemorrhage in the third stage.
Management of the third stage requires strict vigilance of the placenta to prevent complications of postpartum hemorrhage.
Stage of Management:– At present two methods are used in the management of the third stage.
1) Expectant (watchful) management
2) Active management
1) Expectant (watchful) management
In this management, separation of the placenta and its descent into the vagina is allowed to occur spontaneously.
For this management, placental expulsion is minimally assisted.
In this stage mother is constantly watched i.e. mother is not left alone even for a short period of time.
If the mother is in a lateral position, placing her in a dorsal position will allow a proper understanding of the sign of placental separation and the extent of blood loss.
In this management, only placenta separation, descent and expulsion are properly watched.
One hand is placed on the fundus so that,
a) Separation of placenta can be realized.
b) State of uterine activity i.e. contraction and relaxation can be understood.
Separation of placenta
The placenta begins to separate from the uterine wall within minutes of the baby’s birth, so wait 15 to 20 minutes for the placenta to separate on its own.
No touch technique is used in this.
Ama has a “no touch policy” ie the placenta is expelled by gravity within 15-20 minutes ie no massaging of the fundus.
Do not use any type of uterotonic and do not use any manual method for expulsion of placenta.
Expulsion of placenta
Following points to follow when placenta is expelled:
Advise the patient to apply beer down afters when the uterus becomes hard.
Raised intra-abdominal pressure is important to expel the placenta.
And the placenta may be expelled on its own.
2) Active management
1) Use of uterotonic:– Oxytocin is not the drug of choice in the management of third stage of labour.
Provide 10 units of oxytocin IM (intracellular) in management of third stage.
Oxytocin enhances uterine contractions and helps expel the placenta.
2) CCT (Control Cord Traction):– Manual method is used in Controlled Cord Traction in which the umbilical cord is tracked and gently pulled downwards and backwards due to which the placenta separates from the uterine wall and then expels it. Control coda traction is performed by placing the hand on the suprapubic area while uterine contractions are present.
3) Delay Coda Cutting:- Wait for one to three minutes after delivery of fits and then cut the umbilical cord. This technique is more useful in term newborns. Because the newborn can receive an adequate amount of blood from the placenta due to which the condition of anemia can be prevented.
But in pre-term babies, the liver is immature and the red blood cells break down in excess and if delayed coda cutting is done, due to this, the condition of hyperbilirubinemia (jaundice) may arise in the newborn.
4) Post Partum Vigilance:– Proper inspection of placenta after delivery of placenta including proper assessment of cotylodon, lobe and maternal and fetal site followed by fundal massage after delivery of placenta to ensure continuity of uterine contractions and if retained beats of placenta. So it can be expelled properly.
b. Discuss multiple pregnancy . 06
Multiple pregnancy
Definition:-
When more than one fetus develops in the uterus simultaneously and at the same time, it is called “multiple pregnancy”.
When two fetuses develop together in the uterus, they are called twins.
When three fetuses develop simultaneously in the uterus, they are called triplets.
When four fits develop simultaneously, they are called quadruplets.
Varieties and types of twin pregnancy
1) Dizygotic twins:
This commonest ie fertilization of two ova is the result of fertilization by two spermatozoa.
Two placentas are seen in this.
In this case, communication vessels are absent.
In this case, there may be two amnion and two chorion membranes.
Genetic features may be different in this.
They do not accept skin grafts.
2) Monozygotic twins:-
Monozygotic twins develop due to fertilization of this single ovum by a single sperm.
Communication vessels are present in this.
It contains two amnion membranes.
Monozygotic twins usually have the same sex.
Genetic features are also found to be the same.
Physical features like ice, hair color, ear sap, palmar crisis etc are seen in it.
He also accepts skin grafts.
etiology
Exit cause is unknown.
Due to maternal environmental factors such as:
Race: Highest found in Negrons.
Hereditary: This is mainly transmitted from the maternal side more commonly.
Advanced Age of Mother: Due to advanced age of mother like 30-35 years.
Due to Influence of Parity:
Mainly 5th gravida due to increased parity.
iatrogenic
This is due to drugs used in ovulation.
2) Superfecundation:- In which two different ova are released in the same cycle and fertilized in a short period of time by separate acts of coitus is called superfecundation.
3) Superfetation:- In this two ova are released through different menstrual cycles and fertilization takes place, it is called superfetation.
4) Fitters papyraces or compresses:- In this a placenta has died early and dead placentas have a flat end and compressed between the membrane of the living placenta and the uterine wall.
5) Fetal Acardiasis:– This is seen in uniovular twins.
Lie and Presentation:-
Common lie of feet:- is usually longitudinal but malpresentation is commonly seen.
Presentation:- Both vertex, first vertex and second breach, first breach and second vertex, both breach, first vertex and transverse, both transverse.
Diagnosis of Multiple Pregnancy
History Collection,
Physical Examination,
Assessment of symptoms
Excessive enlargement of the uterus,
Nausea and vomiting are more common in the early months.
Palpitations and shortness of breath are seen in the last months of pregnancy.
Swelling in the leg, varicose veins,
hemorrhoids,
Abnormal abdominal enlargement and excessive fetal movement.
General Examination
anemia,
Abnormal weight gain,
pre-eclampsia,
Abdominal examination
Inspection: Barrel sept and large abdomen.
Palpation: Increased height of uterus during amenorrhoea,
to fill the fundus of the uterus with a fit pole,
Increased abdominal girth,
Auscultation:-
Two fetal heart sounds are located at two different spots.
Investigation:-
sonography,
Biochemical tests such as maternal serum chorionic gonadotrophin,
Phytoproteins and unconjugated inst.
Management:-
Antenatal Management:-
Early diagnosis and proper detection of chorionicity, amnioticity, fetal growth pattern and congenital malformation if any.
Perform serial sonography, non-stress test and Doppler velocimetry for fitter surveillance.
advice
Advise mother to increase diet by 300 kcal/day.
Advising the mother to increase and moderate protein intake.
Supplement therapy:-
Iron therapy to mother 100 to 200 mg /day. And advising the mother to take additional vitamins, calcium and folic acid.
Advise the mother to take adequate rest to prevent pre-term labor and other complications.
Advising the mother to make frequent antenatal visits and giving advice to the mother to do antenatal checkup at regular intervals due to which early identification can be done if the mother has a condition of anemia, or complications of preterm and if there is a condition of preeclampsia.
Regular assessment of fetal growth by ultrasound at 2-3 week intervals.
Providing adequate knowledge about breast feeding and bottle feeding to the mother during the antenatal period so that the mother can feed her baby properly.
During Labour:-
Since twin pregnancy is a high risk pregnancy, admit the patient to a well-equipped hospital facility where available. Vaginal delivery can be performed when both or one fetus is in vertex presentation.
Care During First Stage of Labour:-
Taking additional precautions with normal conduction of singleton fetuses in the first stage.
Experience Obstetrician, Experience at Delivery,
An anesthetist, and a neonatologist should be present.
Ultrasound facility should be available in the labor room.
Adequate rest should be given to the mother to prevent early rupture of the mother’s membrane.
Limited use of analgesic drugs and epidural if required
Administer analgesia.
Careful monitoring of the fetus.
Check for cord prolapse by doing internal examination after membrane rupture.
Starting Ringer’s lactate solution in an intravenous line.
Cross-match, group and keep 1 unit of blood ready.
Delivery of First Baby:-
The conformational of the second stage is performed properly by vaginal examination.
Obstetricians, anesthetists and paediatricians must be present during delivery due to the increased risk of complications in multiple pregnancies.
Since multiple pregnancy is considered a high risk pregnancy, the operation theater should be properly prepared for caesarean section in case of emergency.
Continuously monitor the fetal heart sound until both babies are delivered.
Delivery of the first baby is usually spontaneous followed by a proper episiotomy.
Providing information to the mother about the sex of the first baby after delivery.
Then immediately provide the label to the baby as number 1.
Delivery of Second Baby:-
After delivery of the first baby, see the second baby in lie, presentation and fetal heart sound, abdominal examination or real time ultrasound.
Perform a vaginal examination to look for membrane and cord prolapse.
If the lie is longitudinal then look for low rupture of the membrane and again for cord prolapse.
If contractions are poor, add oxytocin to the infusion and administer to the mother.
The interval between two deliveries should be less than 30 minutes, if it is too late, interference has to be done. If the head is low down, forceps delivery, if there is no cephalopelvic disproportion in hiup, then do ventous delivery by doing internal version under general anesthesia.
Delivery of breech by breech extraction:-
If the lie of the fetus is transverse, bring the fetus into a longitudinal lie by external version and if that fails, internal version and perform breech extraction under general anesthesia.
Indications of Cesarean section for second twin:
Non cephalic presentation with larger twin,
Immediate closure of cervix after delivery of first baby,
Fits distress.
Third Stage:-
To prevent the condition of postpartum hemorrhage after delivery of the second baby, inject 10 international units (IU) IM or 20 international units (IU) oxytocin added to 500 ml of normal saline (NS) or Ringer’s lactate solution intravenously (IV). ) to administer to the mother.
Then deliver the placenta with Control Cord Traction (CCT).
Start oxytocin drip for at least one hour after delivery of second baby.
If there is excessive blood loss, give blood transfusion.
After the delivery of the mother, full care watch for two hours.
Providing additional support and health education to mothers for baby care.
Indications of Caesarean section:
Obstetric indication:-
placenta previa,
severe preeclampsia,
Previous caesarean section,
cord prolapse,
Abnormal uterine contractions,
Contracted pelvis.
For Twins:-
Both fits or having a non-cephalic presentation (breech, transverse) in the first fit.
Conjoint twins.
Having complications like intrauterine growth retardation.
c. Define eclampsia. Describe the management of eclampsia. 08 Write the definition of eclampsia. Describe the treatment of eclampsia.
Eclampsia Definition
Eclampsia is a life threatening complication that occurs during pregnancy in women.
The term eclampsia is derived from the Greek word “like a flash of lightning”. Tonic-clonic convulsions or coma as a complication of pre-eclampsia is called eclampsia.
While the condition of pre-eclampsia which,
Hypertension,
Edema (weight gain),
Proteinuria
(Protein in urine) and
If albuminuria (albumin present in urine) becomes complicated and converts to conditions like convulsion and coma, it is called “Eclampsia”.
This is an obstetrical emergency. It is important to take immediate measures to manage it.
Management of Eclampsia :-Medical and Nursing Management of Eclampsia
Aim of Management:-
To control fits of convulsions.
Controlling blood pressure.
Prevent complications.
Safe delivery of Fits.
Principles of Management
To maintain mother’s airway, breathing and circulation.
Properly administer 8-10 liters of oxygen to the mother.
Preventing maternal convulsions.
Provide proper ventilatory support to the mother.
Prevent injury to the mother.
All laboratory investigations of the mother should be done properly.
General Management:-
Hospitalization:-
Hospitalize the mother in a hospital with properly well equipped facilities.
Rest:-
Advise the mother to take adequate rest as well as advise to stop all activities and also restrict visitors.
Positioning:-
Advising the mother to rest in a proper left lateral position can reduce Venakawa compression and prevent heel pain.
History Collection: To collect a complete history of the mother including the frequency and duration of the fits and to take a complete history of any medication the mother is taking or not.
Siddeson and then General Examination:-
Provide proper drug to the mother and sedate her.
Ex:=phenobarbitone 15-30 mg (TDS)
Or
Diazepam 1.5 mg (TDS).
After the mother is properly sedated, do a general and abdominal examination of the mother properly and quickly.
Vital sign
To note the vital signs of the mother every half hour including,
temperature,
pulse,
Respiration,
and blood pressure.
If there is any disturbance in the vital sign or if the vital sign is raised above its normal range, treat it immediately.
Urinary Output: Monitor mother’s urine output hourly.
Nutrition:-
Start the mother on 10% dextrose to maintain fluid, nutritional and caloric levels of the mother.
Fluid should not be increased in an amount more than 2 liters in 24 hours.
Additionally, 50 ml of 5% Dextrose should be provided to the mother at 8 hour intervals to maintain the caloric level of the mother.
Specific management or medical management
Eclampsia wadi mother can be treated by providing medication as follows:
a) Anticonvulsant,
b) Anti-hypertensive,
c) Sedatives,
d) Diuretic,
e) Antibiotics,
f) Other Medication.
a) Anticonvulsant:- ,
Magnesium Sulphate A ( MgSO4 ):-
Acts as the drug of choice to treat the condition of eclampsia. Because it helps in preventing eclamptic fits in the pregnant mother.
Magnesium sulfate can be administered both IV (intravenously) and IM (intramuscularly).
Dose and route:-
IM (Intra Muscularly):
Initial Dose: Initially 4gm IV (intravenously) bolus, administer magnesium sulfate very slowly over 3-5 minutes.
Continuous dose: Administer 5 gm magnesium sulfate IM (intra muscular) every four hours in alternate buttocks.
•>IV (Intra venously):-
Initial Dose: Initial dose is 4-6 gm of magnesium sulfate administered slowly IV (intravenously) over 15-30 minutes.
Continuous Dose:
Administer 1-2 gm magnesium sulfate every hour IV (intravenously).
Magnesium sulfate is a toxic agent that can cause the condition of deep tendon reflux if not provided within therapeutic levels.
The therapeutic level of magnesium sulfate (MgSO4) is 4-7 mEq/L (milliequivalents per liter).
In case of overdose of magnesium sulfate (MgSO4), calcium gluconate is used as an antidote.
Magnesium sulfate when nitrogen is present,
Administer only when urine output increases above 30 ml/hr and respiratory rate above 12/min.
b) Anti-hypertensive: Anti-hypertensives are used to control and reduce blood pressure.
Ex:
a) Hydralazine: 5 to 10 mg over 2 minutes.
b)Labetalol:
Initial dose: 20mg slowly over 2 minutes.
followed by 40-80 mg IV over 10 minutes.
The total dose should not exceed 300 mg.
c) Sedatives:-
Ex:=Diazepam
Dose:=5-10mg IV at the rate of 2-5mg/min.
Maximum dose: Do not increase more than 10mg dose.
d) Diuretic: Diuretic medication should be provided during pregnancy only when pulmonary AD is present.
Ex:=Frusemide, Mannitol.
e) Antibiotics:
Antibiotics are provided as prophylaxis to reduce the complications of pulmonary and pleural infections.
Broad spectrum antibiotic medication is not used in these antibiotics.
f) Other Medication:
i) In case of pulmonary ED: Provide frusemide 40 mg IV followed by 10% mannitol.
ii) Heart Failure: Use of Ex:Lasix and Digitalis medication.
iii) Hyper pyrexia:
Antipyretic medication is not used.
Nursing Management of Eclampsia
Placing a pregnant woman with eclampsia in a side-padded side rail wada cot.
Keeping a padded tongue blade between the teeth.
Keeping the mother in lateral position can avoid aspiration.
During convulsions, keep the airways patent and provide oxygen to the mother in adequate amounts.
Properly monitoring the mother’s oxygen level by pulse oximetry.
Suction properly to remove oral secretions and any vomiting, if any.
Properly note the time, duration of the convulsions that the mother gets.
Provide proper and regular prenatal care to mothers with pregnancy induced hypertension.
Protect the mother from self-injury.
Keep the mother in a dark room to minimize stimuli such as bright lights, noise, and visitors.
Keeping the foot side of the bed slightly elevated will allow secretions to drain properly from the respiratory tract.
Assess mother’s vital signs, ED, fundus height, presentation and position of feet and fetal heart sound and test urine for protein.
Assessing mother’s urine output properly.
Provide intravenous infusion of glucose saline and Ringer’s lactate solution as prescribed to maintain mother’s fluid and nutritional levels.
Advising the mother to maintain her personal hygiene.
Providing properly prescribed medication to the mother.
Assess the mother’s uterine activity, cervical status and fetal status as the membranes may rupture and delivery may occur.
Obstetrical Management:
Most often when a woman has convulsions, labor is induced if labor has not started, labor is induced by artificial rupture of membranes, prostaglandins gel or oxytocin or caesarean section if the baby has died, spontaneous labor. Waited for.
Continuous start of hypertensive regimen as prescribed during post partum period.
Continuously monitor the mother for any other complications of eclampsia.
Advising the mother to follow up regularly.
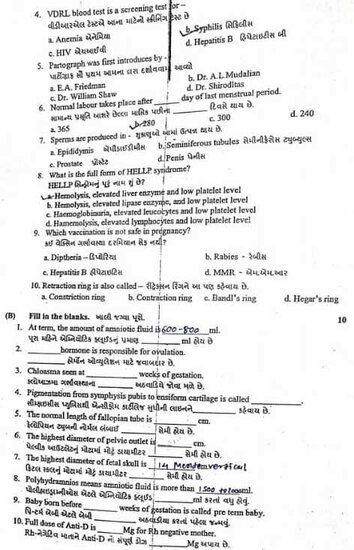
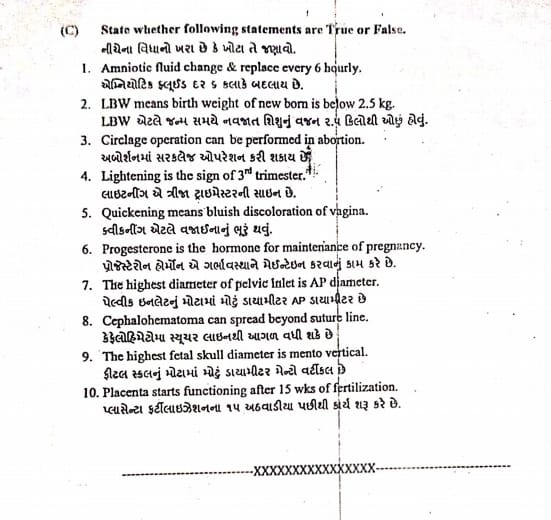
⏩Q-2 Write short Notes (Any Five) 5×5=25
1.BFHI-
BFHI := (BFHI)
Baby Friendly Hospital Initiative
The Baby Friendly Hospital Initiative is a global program launched in 1991 by the World Health Organization (WHO) and the United Nations International Children’s Emergency Fund (UNICEF).
Its main goal is to promote, protect and provide support to breastfeeding and to strengthen maternal practices so that the life of the newborn can start in the best way.
Objectives of BFHI (Baby Friendly Hospital Initiative):
To recognize and anchor hospitals and birthing centers that provide optimal level of care for infant feeding and mother-baby bond.
To properly implement the Ten Steps for Successful Breastfeeding in Maternal Facilities. Components of BFHI (Baby Friendly Hospital Initiative): The Baby Friendly Hospital Initiative has several components to promote, protect and support breastfeeding.
Here are the main 10 components of the Baby Friendly Hospital Initiative:
1) Have a written breastfeeding policy that is regularly communicated to all healthcare personnel.
2) Provide proper training to all healthcare staff in the necessary skills to effectively implement the breastfeeding policy.
3) To provide proper education to all pregnant women about the management of breast feeding and its benefits.
4) To properly help the mother to start breastfeeding the baby within one hour after the birth of the baby.
5) Show the mother how to breastfeed and how to maintain breastfeeding, even if the mother is separated from her child.
6) Do not give the newborn any food or drink other than breast milk unless medically indicated.
7) Practice rooming in- allowing mother and her baby to stay together for 24 hours a day.
8) Anchorage breast feeding on demand- Advising the mother to provide breast feeding whenever the baby shows signs of hunger.
9) Do not give artificial teats or pacifiers (also called dummies or soothers) to breastfeeding infants.
10) To promote the establishment of breastfeeding support groups and refer mothers to them on discharge from hospital or clinic.
This component forms the core of the BFHI and is designed to create an environment that supports breastfeeding as the best way to nurture the infant, promote mother-infant bonding, and improve health outcomes for both mother and infant. Supports and encourages.
Benefits of (Baby Friendly Hospital Initiative)
Health Benefits:
Best fitting provides many health benefits to both mother (reduced risk of breast and ovarian cancer) and baby (reduced risk of infection, reduced risk of allergies and chronic diseases).
Psychological benefit
Breast feeding promotes bonding between mother and infant.
Due to this, there is an emotional attachment between the mother and the infant.
Economic benefit
Breast feeding helps reduce the healthcare costs of health problems related to artificial feeding.
The Baby Friendly Hospital Initiative (BFHI) is a comparative initiative that aims to provide a supportive environment for breastfeeding in health care settings that can lead to improvements in maternal and child health.
🔸2.Oxytocin –
•>Introduction
Oxytocin is an octopeptide. Oxytocin is naturally produced in the hypothalamus but is stored and released in the posterior pituitary. Oxytocin has a half-life of 3-4 minutes and its duration of action is about 20 minutes.
It is rapidly metabolized and degraded by oxytocinase.
•>Mode of Action
Oxytocin helps the uterine muscles contract. Oxytocin’s main mode of action is contraction of the fundal part of the uterus and relaxation of the cervix.
Oxytocin also helps in the release of prostaglandins from the decidua and also helps in stimulating milk ejection from the breast.
•>Preparation used
1) Synthetic Oxytocin (Syntocin or Pitocin)
It has oxytocic effect apart from vasopressor action.
Syntocin is available in ampoules containing 5 IU/Ml.
Pitocin 5 IU/ml.
2) Syntometrine ( Sandoz): Combination of Syntocin 5 unit and Ergometrine 0.5 mg.
3)Desamino oxytocin: is not inactivated by oxytocinase and is 50-100% more effective than oxytocin. It is available in buccal tablets.
Contains 50 IU.
4) Oxytocin Nasal Solution: Contains 40 units/ml.
Indications: Oxytocin is used as a therapeutic and diagnostic test during pregnancy, labor and puerperium period.
1) Pregnancy:
Early pregnancy
Used to accelerate abortion and for induction of abortion with other abortifacient agents.
To stop bleeding after evacuation of uterus.
Late Pregnancy:
For induction of labour.
After expulsion of the placenta.
For cervical ripening.
2) Labor
Augmentation of Labour.
Uterine inertia.
During the active management of the third stage of labor.
Used after expulsion of placenta as an alternative to ergometrine.
To prevent and treat post partum haemorrhage.
3) Purperium or postpartum
To prevent and treat post partum haemorrhage.
To increase milk ejaculation.
•> Contraindication:
Pregnancy
Grand Multipara,
Contracted pelvis,
History of previous caesarean section,
hysterotomy,
Malpresentation.
During labor
All contraindications during pregnancy,
obstructed labour,
Incoordinate uterine contractions,
Fetal distress.
Its time
hypo volemic state,
Cardiac diseases.
•> Dangers/ Complications of Oxytocin:
Maternal
Uterine hyperstimulation
(over activity),
uterine rupture,
water intoxication,
hypotension,
antidiuresis,
Pituitary Soc.
fits
Fital Distress,
fetal hypoxia,
Increase incidence of neonatal jaundice.
•>Route and Dose of Oxytocin Administration
controlled intravenous infusion,
Bolus IV (intravenously),
IM (Intra Muscular),
Buccal tablets or nasal spray.
Induction or Augmentation of Labour:
IV (intravenously) Initial dose is started at a low rate (1-2 milliunits per minute) then the dose can be gradually increased to increase uterine contractions. A maximum of 20-40 munits/minute can be administered and is Every woman vice is different.
To increase uterine contractions and to prevent and treat post-partum haemorrhage:
IM (Intra Muscular)
If IM (intra muscular) administration is to be done, 10 IU is given immediately after delivery of the baby.
OR
If IV (intravenous) administration is to be done, 20 IU is administered in a pint of 500 ml of normal saline or Ringer’s lactate and then the infusion is provided.
•> Nursing Responsibilities
Administering injection oxytocin is a critical responsibility for the nurse Although oxytocin plays an important role in facilitating labor and managing labor progression, the nursing responsibilities for oxytocin administration are as follows.
1) Assessment and Preparation
assessment
Before administering injection oxytocin, the nurse should properly assess the pregnant woman’s labor progress, fetal heart rate, and uterine contractions and maternal vital signs. Due to which medication can be properly initiated and continued.
Preparation
Properly prepare oxytocin solution as per hospital protocols and as prescribed by health care personnel.
2) Monitoring
Uterine contractions
Continuously monitor uterine contractions by palpation method and assess whether urine contractions are regular and proper or not.
Fetal heart rate
Continuously monitor fetal heart rate and assess for signs and symptoms of fetal distress.
3) Administration
Initiation and Adjustment
Proper administration of medications prescribed by health care providers.
Keep the infusion rate low initially and then increase the infusion based on uterine contractions and labor progression.
4) Patient education
Explanation
Provide explanation to the mother and her support portion about the purpose of oxytocin infusion, its side effects, and continuous monitoring.
Expectations
Provide an explanation to the mother and her spotters about the expected increase in intensity and frequency of uterine contractions after administration of oxytocin.
5) Documentation
Charting
Documentation of oxytocin administration, including starting time, infusion rate, maternal vital signs, uterine contraction pattern, and continuous charting of fetal heart rate.
Response to treatment
Properly monitor uterine contractions and assess progress of labor to assess how effective oxytocin is after oxytocin infusion.
And any side of oxytocin
Assess whether there is an effect or not.
6) Communication
Communication with other healthcare personnel for oxytocin administration eg.
obstetrician,
Collaboration with midwife and other nurses.
Patient updates
Provide ongoing patient updates to the mother and her support person including information on labor progress, fetal well-being, and any changes after oxytocin administration.
7) Emergency Response
If any type of side effect is observed during the administration of oxytocin and other symptoms are observed such as uterine hyperstimulation, then oxytocin should be discontinued immediately and supportive care should be provided.
Thus there is a need to perform this type of nursing responsibility while providing injectable oxytocin.
- Fetal development during first trimester
Fetal Development During the First Trimester
During pregnancy the first trimester i.e. 12 weeks (1-3 months) from conception to conception is a crucial part for the growth and development of the fetus as the fetus develops rapidly and from a critical stage.
1) First 1 to 4 wk (embryonic development):
Conception usually occurs within two weeks after the ovum is fertilized by a sperm.
This fertilized egg (zygote) undergoes multiple cell division and forms a ball-like structure of cells called blastocyte, after which the blastocyte is implanted in the uterine cavity through the fallopian tube at the end of 4 weeks.
Then the embryonic stage starts.
Primary development includes the formation of the placenta, umbilical cord, neural tube, heart, and basic layers of tissues.
- Vic 5-8 (Organogenesis)
Development of major organs and body systems takes place in organogenesis.
During the 5th week, the hard beating of the embryo starts and it can be detected in ultrasound.
Limb birds appear, facial features develop in the embryo, eye and ear structures develop.
Formation of organs like liver, kidney, and lungs starts.
Embryos after 8 weeks are called fetuses. It starts the formation of all major organs and external body structures.
3) Week 9-12 (Fetus Growth and Maturation)
Fits grow continuously and rapidly during this week.
In this, the facial features look more clear and the length of the legs also increases.
The fingers and toes of the feet separate and develop nails.
External genital organs are differentiated into male and female.
By the end of the first trimester (first 12 weeks of pregnancy), fits are 2.5-3 inches (6-7.5 cm) long and weigh 0.5-1 ounce (14-28 grams).
The placenta is fully functional, the placenta is fully developed to provide adequate nutrition and oxygen to the fetus and to accept waste products from the fetus.
Throw Out During the first trimester, the environment and maternal health have an effect on fitness.
Adequate prenatal care,
In which regular health checkup, proper screening, provides a healthy environment to the fit and early detection of any potential issues can be done.
- Fetal circulation-
Fetal circulation is a unique circulatory system that is present in the developing fetus. When the fetus is in the womb (uterus), it is formed to fulfill the need of oxygen and nutrients.
Separate fetal circulation in embryos starts during the 16 th post-fertilization day.
The fetal heart starts beating on the 21st day after fertilization. At the same time, the fetus obtains oxygen and nutrients from the placenta in utero because its lungs and alimentary track are functional, so fetal circulation is the circulation through which the fetus receives oxygen and nutrients from the placenta for its survival.
Features of fetal circulation
1) Umbilical Code:
There are two umbilical arteries and one umbilical vein in the umbilical cord.
Umbilical artery:
The umbilical artery transfers fetal waste products and deoxygenated blood from the fetus to the placenta.
Umbilical vein:
It transfers oxygenated blood and nutrients from the placenta to the feet.
2) Placenta:
The placenta acts as an interface between the circulatory system of the mother and the fetus.
The placenta works to exchange nutrients, oxygen and waste products between maternal blood and fetal blood.
As the placenta delivers oxygen and nutrients to the fetus through the umbilical vein and receives the deoxygenated blood and waste products of the fetus through the umbilical artery in the placenta.
3) Ductus Venous (vein to vein):
The ductus venosus is the conduit through which oxygenated blood passes from the umbilical vein to the inferior vena cava, bypassing the liver and digestive organs.
Because of this, oxygenated blood can reach the brain and heart of the fit in an adequate amount.
4) Foramen ovale (oval opening):
The foramen ovale is a fetal cardiac structure that is a small opening in the septum between the right atrium and the left atrium of the heart that acts as a conduit between the right atrium and the left atrium.
Due to this opening (sunt), the blood in the right atrium is shifted to the left atrium bypassing the fetal lungs.
This finding is important because the lungs of the fetus are functional during intrauterine life and are filled with fluid due to which the fetal lungs are not able to do their work properly.
5) Ductus arteriosus (artery to artery):
The ductus arteriosus is a fetal vascular connection that is the communication (shunt) between the pulmonary artery and the aorta.
Due to this ductus arteriosus sunt, blood from the right ventricles bypasses the lungs and flows into the systemic circulation through the sunt.
Vital Circulation:
Oxygen diffuses from the maternal blood into the choriodecidual space (placenta), thus the placental wall and vessels unite to form the umbilical vein.
The umbilical vein from the placenta travels through the umbilical cord to the fetus.
The umbilical vein passes through the umbilical wall to form two branches of the umbilical vein.
A branch of the umbilical vein joins with the portal vein of the liver of the fetus and provides nutrients and oxygen to the liver of the fetus. Blood is collected from the liver through the hepatic vein and enters the inferior vena cava.
The 2nd branch of the umbilical vein is the main vessel called the ductus venosus. It directly joins the inferior Venakawa.
Oxygenated blood in the umbilical vein mixes with deoxygenated blood from the lower leg and trunk in the inferior vena cava.
But Sirius does not affect the oxygen content of the ductus venosus.
Blood now enters the right atrium through the inferior vena cava.
Then the blood in the right atrium goes to the left atrium through the foramen ovale, which is between the right atrium and the left atrium.
Then the blood in the left atrium goes into the left ventricle through the mitral valve.
Blood then exits the heart through the aorta in the left ventricle.
The coronary vessels of the aorta (coronary artery, brachiocephalic trunk (right common carotid artery, right subclavian artery, left common carotid artery, left subclavian artery)) supply blood to the branches of the heart and head.
Blood from the head and neck enters the right atrium through the superior vena cava and crosses the inferior vena cava into the right ventricle through the tricuspid valve.
Most of the blood from the right ventricle through the pulmonary artery bypasses the lungs (since the lungs are inactive) and passes through the descending aorta through the ductus arteriosus (no shunt between the pulmonary artery and the aorta) to supply blood to the abdominal organs and the lower lens.
The descending aorta then forms the right and left internal iliac arteries.
The right and left internal iliac arteries again divide into two hypogastric arteries.
The hypogastric artery enters the umbilical cord to form two umbilical arteries.
These two umbilical arteries return deoxygenated blood to the placenta.
Fit blood circulates fast and is constantly renewed.
Mean cardiac output in fit is 350 ml/kg/min.
🔸5.Physiology of lactation – science of breastfeeding
Physiology of Lactation:
Lactation
Lactation is the process of breastfeeding through which the mammary gland produces and releases milk to provide nourishment to the child. It occurs through a complex interplay of hormones. In it, prolactin and oxytocin work as important hormones for main lactation.
The establishment and maintenance of lactation is generally determined by three factors:
1) Anatomical structure of mammary gland like development of alveoli, ducts, and nipple.
2) Initiation and maintenance of milk secretion.
3) Ejection or propulsion of milk from the alveoli towards the nipple.
The main two hormones responsible for lactase are:
Prolactin and oxytocin work as important hormones for lactation to occur.
1) Prolactin:
Prolactin hormone is secreted from the anterior pituitary gland.
It is the primary hormone for the stimulation of milk production (lactogenesis).
Estrogen and progesterone hormones are increased during pregnancy, these hormones prepare the breast for milk production but inhibit the production of lactase.
After the birth of a child, the level of estrogen and progesterone hormones decreases due to which the effect of prolactin hormone can be on the mammary gland and the secretion of milk increases.
2) Oxytocin:
Oxytocin is released from the posterior pituitary gland.
The release of oxytocin is crucial for milk ejection (the let-down reflex), which normally depends on the baby’s sucking and nipple stimulation.
Oxytocin is an important hormone for the contraction of the myoepithelial cells surrounding the alveoli (milk producing gland) causing milk to enter the duct from the alveoli and then from the duct to the nipple for best fitting.
•> Lactose is divided into four phases according to physiological base.
1) Mammogenesis (preparation of breast),
2) Lactogenesis (synthesis and secretion of milk from breast alveoli),
3) Galactokinesis (ejection of milk),
4) Galactopoiesis
(Maintenance of Lactation)
1) Mammogenesis (Preparation of Breast):
In this stage, the ductal and lobuloalveolar system of the breast grows during pregnancy in which the breast is prepared for the secretion of milk.
2) Lactogenesis (synthesis and secretion of milk from breast alveoli):
Some secretory activity (colostrum) is present during pregnancy and increases after delivery.
Actually milk secretion starts on the third or fourth day postpartum, during this period the breast feels engorged, tense, tender and warm.
Despite the high prolactin level during pregnancy, due to the effect of steroid estrogen and progesterone hormone, the breast tissue does not respond to the prolactin hormone and milk secretion does not occur, but after delivery, as the estrogen and progesterone levels fall down (decrease), the prolactin hormone decreases its milk secretion activity. In the mammary gland, prolactin and glucocorticoid hormones are important in this stage.
Secretory activity is increased directly or indirectly by growth hormone, thyroxine and insulin.
3) Galactokinesis (ejection of milk):
Milk is not only ejected by baby’s shaking but milk is ejected from the alveoli by a contractile mechanism.
Oxytocin hormone is the major galactokinetic (milk ejection) hormone.
Reflux is set up during the baby’s shaking.
Impulses from the nipple and areola then pass through the thoracic sensory and cause the synthesis of oxytocin in the hypothalamus and then reach the posterior pituitary gland to transport the oxytocin synthesized in the hypothalamus.
Oxytocin hormone is released from the posterior pituitary gland, which then causes contraction of the myoepithelial cells surrounding the alveoli (milk producing gland).
This process is called “milk ejection” or “milk let down reflex”.
Where milk is forced into the ampulla of the lactiferous duct, it is expelled either by the mother’s express or by the baby’s shuck.
A baby’s cry elicits a let-down reflex even without shaking.
The pressure of milk that builds up in the breast before the baby sucks is called “draft”. It is also produced by injecting oxytocin.
Breast engorgement occurs due to pain, breast engorgement in the milk ejection reflex If the ejection reflex is obstructed for more days after the start of milk secretion then breast engorgement occurs.
4) Galactopoiesis
(Maintenance of Lactation):
Prolactin is a single and important galactopolytic hormone.
Shaking is essential for effective and continuous lactation not only for the milk to come out of the gland but also for the release of prolactin.
Due to the pressure of milk in the breast, the production rate of milk decreases, so by periodic breast feeding, that pressure can be reduced and the secretion of milk is maintained.
A healthy mother produces 500-800 ml of milk to feed her baby.
Thus, according to this the physiology of lactation is divided into 4 phases.
- Difference between abruipto placenta and placenta previa
Difference between placenta previa and abruptio placenta:
1) Clinical features
•>Placenta previa
Nature of Bleeding
Painless, colicky and recurrent bleeding.
Bleeding is always visible.
Abruptio placenta
Bleeding due to painful, preeclampsia or trauma.
Bleeding can be a mix of visible and invisible bleeding.
•>Placenta previa
Character of blood
Bright red blood is seen.
Abruptio placenta
Blood is of dark red color.
•>Placenta previa
General condition and anemia
Anemia is characterized by visible blood loss.
Abruptio placenta
In this, the condition of anemia is seen more than the amount of visible blood loss.
•>Placenta previa
Features of preeclampsia
The condition of preeclampsia is not associated with placenta previa.
Abruptio placenta
Abruptio placenta features of preeclampsia are seen in 1/3 cases.
2) Abdominal examination
•>Placenta previa
Height of Uterus
The height of the uterus is seen according to the gestational age.
Abruptio placenta
In abruptio placenta, the height of the uterus is enlarged more than the gestational age.
•>Placenta previa
Fill of uterus
In placenta previa, the uterus feels soft and relaxed.
Abruptio placenta
Abruption of placenta ma uterus can be tense, tender and rigid.
•>Placenta previa
Malpresentation
Malpresentation is common in placenta previa and the head is high-floating.
Abruptio placenta
Abruptio placentae malpresentation is unrelated and may also involve the head.
•>Placenta previa
FHS (Fetal heart sounds)
A heart sound is often present in placenta previa.
Abruptio placenta
Heart sounds are often absent in abruptio placenta.
3) Placentography (USG)
•>Placenta previa
The placenta is found in the lower segment of the uterus.
Abruptio placenta
The placenta is found in the upper segment of the uterus.
4) Vaginal examination
•>Placenta previa
The placenta is implanted in the lower segment of the uterus.
Abruptio placenta
The placenta does not fill in the lower segment of the uterus.
🔸7.Minor disorders of newborn – common diseases of newborn child
Minor Disorders of Newborn:
1) Stuffy nose,
2) Sticky Ice,
3)Skin Races:
Types:
a)blotchy erythematous,
b) Napkin race (ammonia dermatitis),
c) Perianal dermatitis,
d) Intertrigo,
E) Oral thrush.
4) Congenital phimosis,
5) Genital crisis,
6) Birth marks,
7) Physiological Jaundice,
8) Constipation.
1) Stuffy Nose:
If there is a stuffy nose, due to this, the newborn has breathed through the mouth due to which the newborn swallows excessive air and due to this, conditions like abdominal distension and vomiting are seen in the newborn.
Treatment:
Nostril can be cleaned with a clean cotton soaked in normal saline.
2) Sticky Ice:
Sticky ice can be caused by a chemical irritant or bacterial conjunctivitis caused by streptococcus bacteria.
Treatment:
To treat sticky ice, use erythromycin eye ointment every six hours for seven to ten days.
3)Skin Races:
Types:
a)blotchy erythematous,
b) Napkin race (ammonia dermatitis),
c) Perianal dermatitis,
d) Intertrigo,
E) oral thrush,
a) Blochy erythematous:
Blotchy erythematous is localized on trunk, limbs and face and blotchy erythematous disappears within a day or two.
Treatment:
Blotchy erythematous can be treated by simply applying the powder after bathing the baby.
b) Napkin Race :
Napkin race is more common in artificially fed babies.
It is also called ammonia dermatitis.
Napkin Race a
diarrhea,
Frequent loose stools,
Strong ammoniacal urine,
Due to lack of cleanliness,
A wet nappy due to longer stay,
Due to fungal infection,
By using nylon or water tight plastic napkins.
A napkin race can happen.
Prevention:
Napkin race can be prevented by providing frequent care and attention to the napkin area and properly changing napkins when they become soiled.
This condition can be prevented by changing the wetted napkin immediately and keeping the skin dry.
Wash napkins properly with antiseptic solution.
c) Perianal dermatitis: Perianal dermatitis is situated around the anal opening.
The skin around the anus is red, indurated, excoriated. It is usually due to alkalinity of stool and is more common in artificially fed babies.
Treatment:
It can be prevented by changing weighted napkins promptly and keeping the skin dry.
Wash the napkin properly with an antiseptic solution.
Keep the napkin in air or sunlight and apply coconut oil or anti-fungal cream on the perianal region.
d) Intertrigo:
This is a variant of the napkin race with soreness in the groin area and flexors.
It also occurs where the neck folds.
In its cause, due to the two surfaces of the wet skin coming into contact and the air being cut off in this skin, it gradually gets infected.
Treatment:
Treatment involves exposing the infant’s buttocks to warm air to promote healing.
Advise the mother to avoid plastic pants as they prevent evaporation and increase skin damage from breakdown of urine.
E) Oral thrush: Oral thrush is an infection of the buccal mucus membrane and tongue caused by Candida albicans.
Treatment: Oral thrush is treated with 1% gentian violet solution or nystatin suspension (100,000 units/ml) applied to each side of the mouth 3-4 times a day with a cotton tipped swab.
4) Congenital phimosis: In this newborn the prepuce is a pinpoint due to which the newborn feels discomfort during micturition due to which the baby cries.
Treatment: Congenital phimosis is treated by dilatation using mosquito forceps.
5) Genital Crisis:
Genital crisis does not require any treatment. Only reasons are provided and the mother is assured and explained that the genital crisis resolves in a short period of time in which,
Mastitis Neonatal,
Hydrosil of Newborn,
Vaginal bleeding during first week.
etc. is involved.
- Birth Marks:
Introduction: The main cause of birth marks is unknown but it is less common in Asian people but more common in Spain, Italy and some Arab countries.
They believe that these birth marks are seen due to unsatisfied and unfulfilled desires of the pregnant mother.
Ex: If the antenatal mother has any twenties and her twenties are not fulfilled, birth marks are seen in the skin of her child. Birth Marks A benign regularity seen on the skin of a newborn at the time of birth or shortly after birth is called birth marks.
Birth marks are divided into two types.
a) Pigmented birth marks:
Pigmented birth marks are caused by excessive skin cells becoming pigmented which include,
Mall, cafe u latte spots, mongolian spot.
b) Vascular Birth Marks:
Vascular birthmarks are called red birthmarks which are usually seen due to increased blood vessels.
eg, muscular stain (salmon patches), hemangiomas, pot wine stain.
etc. Involvement Types of Birth Marks: 1) Cafe U Lat Spots:
This is a type of pigmented birthmark. This is one of the most common birth marks that are usually oval in shape and light brown to milky coffee in color.
These birthmarks are present at birth and sometimes present shortly after birth.
These birth marks do not fade with age.
b) Silver mark: This is seen as a silver strike on the right or left side, where the forefade and hairline meet. It is hereditary.
C) Port Wine Stain:
It is a vascular birthmark that presents as red and purple marks on the face and can be elsewhere on the body.
A port wine stain is caused by abnormal bleeding from blood vessels in the affected area. It is different in size. It is a few millimeters and it can also become dark if left untreated.
d)Salmon patches/stroke beats/telangiectatic nevus:
This is a vascular birthmark that usually presents as patches of slightly reddened skin on the face.
It is also found on nape of neck, upper eyelid, forehead, and nose. It gets relieved on its own within a few months.
e) Hemangiomas: These are vascular birthmarks and strawberrymarks. This is a red and raised mark.
Initially it is small and flat but it grows rapidly during four to five months of life and then fades.
f)Mongolian Spot:
This is a pigmented birthmark.
These Mongolian spots are harmless marks. Its color is bluish gray.
Mongolian spot A Down syndrome, irregular blue patches of skin pigmentation seen on the sacral area, and sometimes the back and extremities of a newborn baby resolves on its own between the ages of six months to one year.
G) Congenital melanocyte nevus: It is a pigmented birthmark that can be found anywhere on the body but usually more on the head and parts of the body. It is light brown to black in color, irregular in shape, flat raised and Lumpy.
It is often dark and hairy during puberty.
Treatment:
Most birthmarks are harmless and do not require treatment.
Pigmented marks tend to resolve on their own while vascular birthmarks have to be removed for cosmetic reasons.
H) Milia:
Many fine raised white or yellowish white sports called milia due to the retention of sebum on the nose, nasolabial folds, cheeks and fore head of the neonate.
Initially, it resolves on its own within a few weeks.
I) Epstein’s pearls: Epithelial cysts found in the lateral to midline of the hard plate called Epstein’s pearls require no treatment.
7) Physiological Jaundice:
Physiological jaundice is commonly seen in newborns also called neonatal jaundice.
In this condition, the skin of the new bone and its sclera turn yellow due to the increase in the amount of bilirubin in the body.
This jaundice appears during two to three days after birth and its peak level is seen at six to seven days.
Treatment:
Physiological jaundice is relieved within a week.
Provide adequate extra fluid to the child.
Provide proper phototherapy to reduce the child’s bilirubin.
8) Constipation: Constipation is more common in artificially fed babies.
Treatment:
Properly correcting dietary errors.
Provide some fluid to the neonate.
Do not provide laxatives to neonates.
If the above measures fail, provide a small amount of milk of magnesia.
Avoid insertion of suppositories and catheters in neonates.
8.Physiological adaptation of new born-Physical adaptation of a newborn child
Physiological Adoption of Newborn:
Physiological adaptation in the newborn is important for survival of the fetus from intrauterine life to extrauterine life.
Physiological changes that occur in the newborn are as follows:
1) Respiratory System:
Fits to Neonate Transitions:
Before birth, the fetus receives oxygen from the placenta.
After birth, the lungs of the fetus expand and mature to oxygenate the blood.
Clearance of Lungs Fluid:
After the birth of the newborn, when the newborn takes its first breath, the fluid in the lungs is cleared and the lungs are transferred from the fetal circulation to the neonatal circulation.
Surfactant Production:
A surfactant is a substance that works to reduce the surface tension of the lungs. And prevents alveoli from collapsing due to which gas exchange can take place properly.
Closure of fetal sunt:
After birth, shunts in the newborn such as Doctor’s arteriosus (a shunt between the aorta and pulmonary artery) and foramen ovale (a shunt in the septum between the right atrium and left atrium) close and redirect blood to the lungs.
2) Cardiovascular Adaptation:
Circulatory Changes:
After birth, after clamping and cutting the umbilical cord, the umbilical vessels are constricted and the umbilical arteries and umbilical veins are closed.
Increases pulmonary blood flow:
After birth, the newborn lungs expand to be able to oxygenate the blood, thereby increasing the pulmonary circulation.
Closure of ductus arteriosus:
These blood vessels connect the pulmonary artery and the aorta, which close shortly after birth.
Closure of foramen ovale:
The foramen ovale is a hole in the septum between the right atrium and the left atrium that closes a few months after birth.
3) Thermoregulation:
Maintenance of Body Temperature:
Newborns have limited ability to regulate their body temperature and brown fat metabolism, vasomotor response (shivering), and being kept in a warm environment (incubator or skin-to-skin contact).
4) Gastrointestinal System:
Production of digestive enzymes:
After birth, the digestive enzymes of the fetus increase due to which the newborn can digest breast milk and formula milk.
Meconium Pass:
A few days after birth, the baby passes meconium (baby’s first stool) which indicates a normal digestive track.
5) Metabolism:
Glucose metabolism
Insulin secretion increases after the birth of the baby, which can decrease maternal blood glucose and thereby properly maintain fetal blood glucose levels.
Adjustment infeeding:
The gastrointestinal tract and metabolism of the fetus adjust to the transition from placental nutrients to the fetus.
6) Renal System:
Urine Production:
After the birth of the baby, the kidneys work to filter the fetal blood and produce urine.
Fluid Balance:
Fits’ urinary system adjusts to maintain fit’s fluid and electrolyte levels.
7) Immune System:
Passive Immunity:
A newborn receives antibodies through the placenta and through breast milk and works to increase immunity and fight against infection.
8) Neurological Adaptation:
Sensorimotor Integration:
New bone adjusts after birth to maintain coordination of sensory and motor responses to sensory stimuli.
Cephalocaudal Development:
A newborn develops head to toe after birth like lifting the head, grasping objects etc.
This adaptation takes place through hormonal, neural and metabolic processes through which the newborn can properly survive from intrauterine life to extrauterine life.
And this physiological adaptation is important for the proper growth and development of the newborn.
⏩Q-3 (A) Write Multiple Choice Questions. Write the correct option from the following. 10
- Which hormone is necessary for the positive pregnancy test? Which hormone is required for a positive pregnancy?
a. Progesterone – Progesterone
C. HCG
b. Estrogen-Estrogen
d. Placental Lactogen Placental Lactogen
2.Inflammation of the fallopian tube is called inflammation of the fallopian tube
a. Endometritis – Endometritis
c. Cervicitis- Cervicitis
d.Salpingitis- Salpingitis
b. Vaginitis – Vaginitis
3.Pacemaker of Uterine contraction is – It is a pacemaker of uterine contraction.
a. tubal Ostia- tubal ostia
c. AV Node
b. SA Node – S A Node
d. Purkinje fibers Purkinje fibers
- VDRL blood test is a serening test.
a. Anemia- Anemia
c. HIV – HIV
b. Syphilis- Syphilis
d. Hepatitis- b- Hepatitis B
- Partograph was first introduced by Partigraph
A. EA. Friedman –
c. Dr. William Shaw –
b. Dr. AL Modalian –
d. Dr. Shiroditas –
6.Normal labor takes —–place after day of last menstrual period. Normal delivery is approximately the day after the last menstrual period.
a. 365
c. 300
d. 240
b. 280
7.Sperms are produced in
c. Prostate-prostate
d. Penis – Penis
a. Epididyminh. – Epididymis
b. Seminiferous tubules – seminiferous tubules
- What is the fall form of HELLP syndrome? What is the full name of HELLP syndrome?
a. Hemolysis, elevated liver enzymes and low platelet level
b. Hemolysis, elevated lipase enzyme, and low platelet level
c. Haemoglobinuris, elevated leucocytes and low platelet level
d. Hemolysis, elevated lymphocytes and low platelet level
- Which vaccination is not safe in early pregnancy? Which vaccine is not safe during pregnancy?
c. Hepatitis B – Hepatitis b.
a. Diptheria- Diphtheria
b. Rabies – rabies
d. MMR – MMR
- Retraction ring is also called Retraction ring.
a. Constriction ring –
b. Contraction ring –
c. Bandi’s ring –
d. Hegar’s ring –
Q: (1) Ans
(C) HCG.
Q: (2) Ans
(d) Salpingitis.
Q: (3) Ans
(a) Tubal Ostia.
Q: (4) Ans
(b) Syphilis.
Q: (5) Ans
(a) E.A Friedman.
Q: (6) Ans
(b) 280 days.
Q: (7) Ans
(b) Seminiferous tubules.
Q: (8) Ans
(a) Hemolysis, elevated liver enzyme and low platelet level.
Q: (9) Ans
(d) MMR – MMR
Q: (10) Ans
(c). Bandl’s ring
⏩(b) Fill in the blanks 10
- At term, the amount of amniotic fluid is ———-ml. Amount of amniotic fluid throughout the month. ——– ml is.
600-800 ml.
2.—————-hormone is responsible for ovulation ———– – Hormone responsible for ovulation
Leutinizing hormone
(Luteinizing hormone) (LH),
- Chloarma seen at ———weeks of gestation. Chloazam is observed at ———–week of pregnancy.
16 weeks of gestation.
4.Pigmentation from symphysis pubis to ensiform cartilage is called———– The line from symphysis pubis to ensiform cartilage is called———-.
linea nigra
(Linea nigra).
5.The normal Imgth of fallopian tube is————-cm Normal length of fallopian tube ——cm.
Approximately 10-12 centimeters (cm).
- The highest diameter of pelvic outlet is ——-cm.
13 cm.
- The highest diameter of fetal skill is——–cm. The largest diameter of the fetal skull is —– cm.
14 cm
8.Polyhydramnios means amniotic fluid is more than ———–ml Polyhydramnios means amniotic fluid is more than ——- _ml.
2000 ml.
9.Baby Sorn before———-weeks of gestation is called pre term daby printers.
37 weeks.
10.Full dose of Anti-D is—— Mg for Rh negative mother. Rh negative mother is given full dose of anti-d —–mg.
0.3 Mg
⏩(C) State whether the following statements are True or False. 10 State whether the following statements are true or false.
1.Amniotic fluid change & replace every 6 hourly. Amniotic fluid is changed every 6 hours.
False
(Reason := Amniotic fluid is completely changed and replaced every three hours in which 300-400 ml/hr of amniotic fluid is changed and replaced).
- LBW means birth weight of new born is below 2.5 kg. LBW means birth weight less than 2.5 kg.
True.
- Circlage operation can be performed in abortion. Cerclage operation can be performed in abortion.
True
- Lightening is the sign of 3rd trimester. Lightening is a sign of the third trimester.
True
- Quickening means bluish discoloration of vagina. Quickening means browning of vagina.
False
(Reason:= Quickling is the first fetal movement that the mother feels.
And bluish discoloration of the vagina is called Jacquesmeier’s sign.
- Progesterone is the hormone for maintenance of pregnancy. Progesterone hormone works to maintain pregnancy.
True.
- The highest diameter of pelvic inlet is AP diameter. The largest diameter of the pelvic inlet is the AP diameter.
False
(Reseon:= The largest diameter of the pelvic inlet is not the AP diameter. But the transverse diameter.
Because the anterior posterior diameter is 11.5 cm and the transverse diameter is 13 cm.)
- Cephalohematoma can spread beyond suture line. Cephalohematoma may extend beyond the suture line
False
(Reseon:=Cephellohymato may not cross the suture line. But caput succidunum crosses the suture line.)
- The highest fetal skull diameter is mento vertical. The greatest diameter of the femoral skull is the mento vertical
True
- Placenta starts functioning after 15 weeks of fertilization. The placenta starts functioning after 15 weeks of fertilization.
True.
💪 💥☺ALL THE BEST ☺💥💪
Note :-MCQ ANSWER in unique pattern of APP in both languages is given below paper solution / click here. Clicking on “A” will change the language.
IF ANY QUERY OR QUESTION, REVIEW-KINDLY WATSAPP US NO. – 84859 76407
