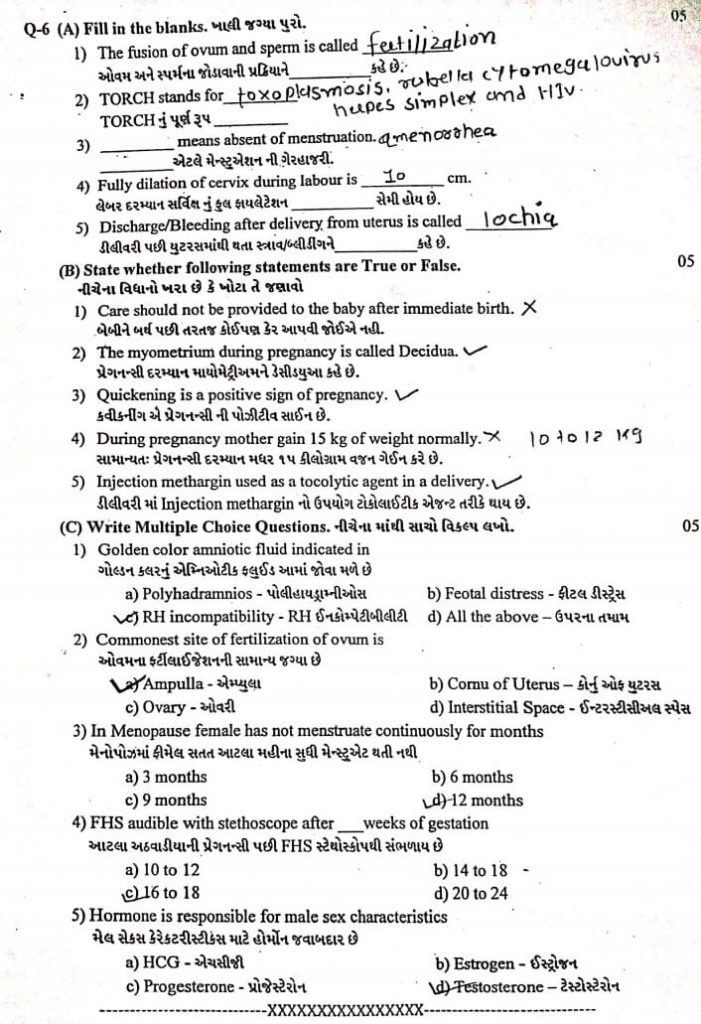
ENGLISH GNM-T.Y-Midwifery & Gynecological-12/09/2022 (DONE-paper no.5)
GNM-T.Y-Midwifery & Gynecological-12/09/2022

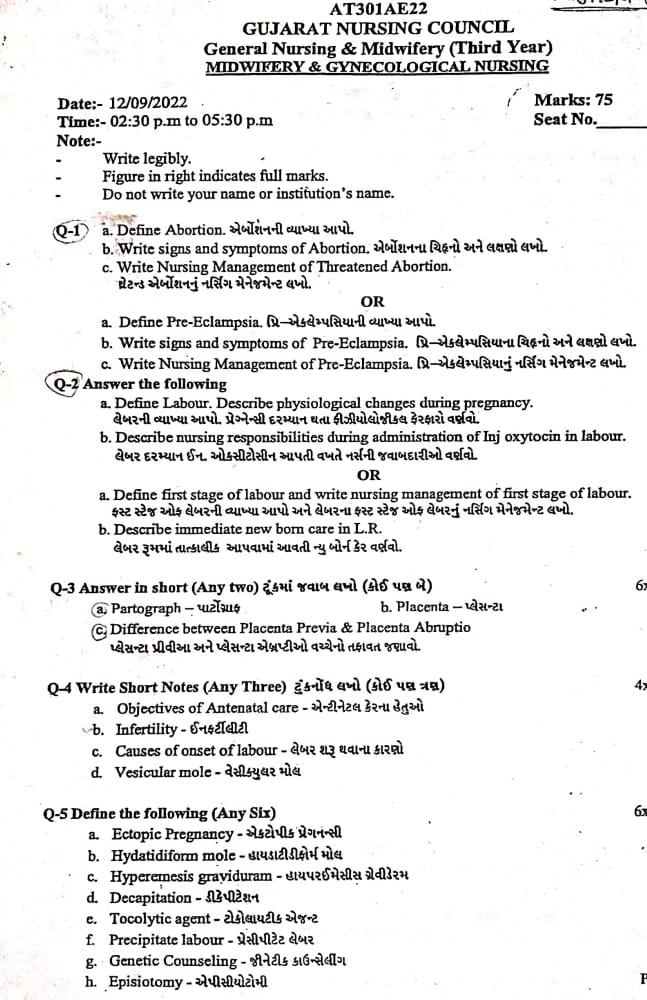
🔸 a. Define Abortion.Definition of abortion millions.
Abortion is a process in which pregnancy is terminated. In abortion, the product of conception is partially and completely separated and expelled from the uterine wall before the age of viability (28 weeks). This condition is called “abortion”.
Abortion if it occurs spontaneously is called “miscarriage” and if induced abortion is called “induced abortion”.
Majority abortions or miscarriages occur during the first trimester of pregnancy i.e. during the first 12 weeks of pregnancy, then it is called “early miscarriage”. And the miscarriage that occurs after 13 weeks of pregnancy is called “late miscarriage”.
The types of abortion are as follows.
1) Spontaneous abortion
A) Threatened abortion,
B) Inevitable Abortion,
C) complete abortion,
D) Incomplete abortion,
E) Silent or missed abortion,
D) Septic abortion,
E) Recurrent abortion or habitual abortion,
2) Induced abortion
b. Write signs and symptoms of Abortion. Write the signs and symptoms of aspiration.
Symptoms and signs of abortion are as follows.
1) Spontaneous abortion
A) Threatened abortion,
Vaginal erection,
Mild abdominal pain and cramping,
Bleeding to be slight,
Seeing blood no color bride red,
Mild abdominal pain,
Bleeding is painless,
mild back unite,
Dull pain in the lower abdominal area,
No fresh lump or expulsion of any kind,
having a closed cervix,
Seeing the discharge.
B) Inevitable Abortion,
Increased vaginal bleeding,
This bleeding occurs due to detachment of the placenta from the uterine wall,
Severe colicky lower abdominal pain,
No exfoliation of tissues of any kind,
Dizziness due to heavy blood loss,
Vital signs are normal in majority of cases but in some cases signs of shock are seen due to excessive bleeding.
Skin is cold and clammy,
A uterus felt firm (contracted),
Cervix is seen dilating.
C) complete abortion,
A history of expulsion of flaccid mass-like structures,
Decreased abdominal pain,
Vaginal bleeding is minimal or absent,
Uterus appears small during periods of amenorrhea,
Transvaginal ultrasonography showing empty ureteric VT
D) Incomplete abortion,
History of expulsion of small amount of mass like structure from vaginal area,
Colic pain in lower abdominal area,
During the internal examination..
Uterus appears small during periods of amenorrhea,
having vaginal bleeding,
Expulsion of incomplete mass like structure is seen during examination.
E) Silent or missed abortion,
Persistent brownish vaginal discharge,
Subsidence of pregnancy related symptoms,
Uterine growth arrest,
Absence of fetal heart sound,
Cervix becomes firm,
Fetal skeletal collapse in radiology,
Absent fetal movement.
D) Septic abortion,
Signs of infection such as,
fever,
feeling cold,
Riggers coming,
Foul smelling vaginal discharge and purulent vaginal discharge,
Infection is likely to be transmitted in the blood stream.
Abdominal pain and tenderness,
Tachycardia,
An increase in the pulse rate to more than 100-120 beats per minute indicates that the infection has spread to the uterine cavity.
Vaginal bleeding is observed,
Having a history of septic shock,
A history of jaundice, oligouria and anuria should be found.
E) Recurrent abortion or habitual abortion,
Absence of fetal heart sound,
Multiple spontaneous abortions (recurrent),
2) Induced abortion
Seeing the vaginal building,
Abdominal pain and camping,
To see an emotional reaction,
Like Guilt, Sadness etc.
c. Write Nursing Management of Threatened Abortion. Write the nursing management of threatened eruption.
Nursing management of threatened eruption
Proper assessment and monitoring of pregnant women in nursing management of threatened abortion.
To provide properly supportive care to women.
1) Assessment :-
Vital sign
To continuously monitor the mother’s vital signs. like,
pulse,
blood pressure,
temperature,
Respiration etc.
Bleeding assessment:- To assess the color, amount, intensity and consistency of vaginal bleeding.
History collection :- To collect proper history of mother including complete history about previous pregnancy and abortion.
2) Monitoring and Observation :-
Continuously observe the mother to assess whether she has any signs and symptoms of shock (hypotension, tachycardia, pallor).
Conduct proper investigations of mother including hemoglobin, hematocrit, ultrasonography, ABO & Rh grouping routinely.
3) Bed rest and physical activity :-
Advise the mother to take complete bed rest.
Advising the mother to do limited physical activity.
Advising mother not to do household work for one month.
4) Emotional Support :-
To provide emotional support and reassurance to the mother and her family.
To properly clear the doubts and queries of the mother and her family members.
Do not give false reasons to mother and her family members.
5) Education :- To provide education to the mother about the signs and symptoms of abortion such as increased bleeding, severe pain etc. and advice to seek immediate medical treatment if any such signs and symptoms are observed.
Provide education to mother to take proper follow up.
6) Hydration and Nutrition :-
Advise the mother to have adequate fluid intake.
Continuously monitor mother’s intake output chart.
Advising the mother to take a properly balanced diet.
Advise the mother to consume a high fiber diet to prevent constipation.
Providing supplements to the mother with good fitting.
Ex:= Ferrous Sulphate 200 mg( BD. ),
Folic acid 5 mg/day (TDS).
Provide mother with high protein and vitamin E diet.
7) Medication Administration :-
Providing prescribed meditation to the mother.
Provide medication to control bleeding and relieve pain.
Provide education to the mother about medication dosage, direction and side effects.
To relieve the mother if she has problem of slip and anxiety
Tab. Diazepam, (5-10 mg before night meal),
Or
Tab.Calmpose, (5-10 mg before night meal),
Or
Tab.valium (5-10 mg before night meal),
to provide
Provide mild amount of laxative to mother at bed time for good ball activity.
Ex:= Milk of Magnesia.
Do not provide enema to the mother as enema is responsible for stimulating uterine contractions in the mother.
48 hours after the mother experienced signs and symptoms of threatened abortion
8) Consultancy and Referral :-
Collaborating properly with other health care personnel for care.
To provide timely referral services to the mother if required.
9) Documentation :- Timely documentation of mother’s assessment findings, interventions provided, and whether there are any changes in mother’s condition.
10) Follow up :– Giving advice to take regular follow up for mother’s progress and reassessment.
Nursing management of threatened abortion is usually provided to provide properly comprehensive care to the mother and to bring about improvement in the mother’s condition.
🔸OR🔸
🔸 a. Define Pre-Eclampsia
Preeclampsia :- Preeclampsia is a complication of pregnancy. In which its etiology is unknown but it is a multisystem disorder. In which high blood pressure is seen along with other organs are also damaged and most commonly liver and kidney are affected.
Preeclampsia occurs mainly after the 20th week of pregnancy and also differs in severity.
Among the main symptoms of preeclampsia are:-
1) Hypertension that increases above 140/90 mmHg (hallmark sign of preeclampsia),
2) Edema (mainly in hands, face, and legs) and excessive weight gain.
3) Proteinuria (excess amount of protein found in urine),
4) Albuminuria (albumin present in urine). The symptoms of preeclampsia are seen after the 20th week.
b. Write signs and symptoms of Pre-Eclampsia
Signs and symptoms of pre-eclampsia can vary by severity.
It may include the following:
Main symptoms:=
- High Blood Pressure (Hypertension): Blood pressure is persistently above 140/90 mm Hg.
- Proteinuria: Protein is detected in urine.
- Edema :- Edema, especially seen in hands, face or feet. While mild edema is normal during pregnancy, sudden or sudden edema, if accompanied by other symptoms and signs, may indicate pre-eclampsia.
4.Albuminuria :- Finding albumin in urine.
Alarmig symptoms:=
- Headache :- Often there is a severe and continuous headache which is not relieved even by treatment.
- Visual Disturbance :– This may include blurred vision, flashing lights or spots.
7.Pain in the upper part of the abdomen :– especially in the upper part of the right abdomen, which suggests involvement of the liver.
8.Decreased urine output :- Oliguria (reduced production of urine) Other symptoms :=
- Nausea and Vomiting :– Especially if it is persistent and heavy.
10 Shortness of breath:-especially if associated with fluid accumulating in the lungs (pulmonary edema).
11Hyperreflexia :- Exaggerated reflex response.
12 Thrombocytopenia: Low platelet count, which can lead to blood clotting problems.
- Decrease in movement of the feet:-
Less than normal movement by the fetus during that stage of pregnancy.
It is important to note that not all women with pre-eclampsia will experience all of these symptoms.
The presence of hypertension and proteinuria after 20 weeks of pregnancy in previously normotensive women are the primary diagnostic criteria for pre-eclampsia.
c. Write Nursing Management of Pre-Eclampsia. Write the nursing management of pre-eclampsia
Nursing management of pre-eclampsia involves closely monitoring the mother, preventing complications, and improving the well-being of the mother and fetus.
1) Assessment and Monitoring
Vital sign
Continuous vital sign monitoring of the mother including,
pulse,
blood pressure,
Respiration, etc
Temperature is involved.
Fluid intake output monitoring
Monitoring mother’s intake output chart. Because of this, kidney function and fluid balance can be monitored.
Fittal assessment
Assessing the fit’s heart rate and fit’s movement in fit assessment.
Assessment of symptoms
Regularly assessing the mother’s signs and symptoms
one head,
Visual Distance,
epigastric pain,
And to assess the condition of edema or not.
2) Bedrest and positioning
Advise the mother to rest on her left side to improve uteroplacental circulation and reduce vena cava compression.
Advising the mother to do limited mountain activity to prevent blood pressure from increasing.
3) Fluid management
Maintain the mother’s intravenous access so that her hydration status can be maintained and medication can be administered.
Continuously monitoring the intake output of the mother so that the hydration status of the mother can be maintained and fluid overloading of the mother can be prevented.
4) Medication administration
Providing the mother with medication properly prescribed by the healthcare provider.
like,
Antihypertensive drug to control blood pressure
Ex:=
labetalol
(Orally 100 mg (TDS)
I.V infusion :=1-2 mg / min.),
Hydralazine (Orly
100 mg/day in four divided doses).
If the mother has a condition of fluid overload, provide diuretic medication such as,
Ex: Lasix (Frusemide) (40 mg up to 5 days).
If the mother has a condition of convulsions, then provide anticonvulsive medication.
Ex:=Magnesium Sulphate.
Providing sedative meditation to the mother.
Ex:=
Diazepam 10-20 mg I.v. followed by:
Tab. Diazepam 5mg (TDS),
Tab.phenobarbitone 60 mg (hs).
If the mother has a condition of constipation, provide a mind laxative at bedtime.
Ex:= milk of magnesia.
Maintain mother’s progress chart in which,
Monitoring blood pressure four times during the day.
Daily weight monitoring of mother and condition assessment of edema.
Monitoring mother’s fluid intake and urine output.
Urine examination of mother including protein urea condition assay.
To do mother’s blood investigation in which mother’s
hematocrit,
platelet count,
uric acid,
creatinine level,
And liver function test (LFT) should be done once a week.
Ophthalmic examination of mother.
Continually assess fit’s wellbeing.
5) Monitor for complications
Assessing the mother for severe pre-eclampsia and warning signs and symptoms of eclampsia including,
Scissors, severe headache,
epigastric pain,
Assess for blurred vision.
Mother’s HELLP Syndrome:
(1)H :=hemolytic anemia,
(2) EL:=elevated liver enzymes,
(3) LP:= Low Platelet Count)
Assessing complications like
6) Patient education
Advising the patient and his family members for regular antenatal checkup of pregnant women so that the condition of pre-eclampsia can be detected early.
To provide complete information and education to pregnant women and their family members about the condition of pre-eclampsia, its causes, symptoms and signs, diagnosis, complications and its treatment.
Advise the pregnant woman and her family members to seek immediate medical treatment due to
The condition of pre-eclampsia can be prevented from developing excessively.
7) Emotional support
To provide proper reassurance and psychological support to the patient and his family members.
Giving advice to the patient and his family members to improve the coping mechanism properly.
8) Collaboration and Communication
Proper collaboration with other health care personnel for proper treatment of the mother including communication with obstetricians, neonatologists and anesthesia providers so that the mother can be properly cared for.
Proper communication and collaboration with other health care team members for mother’s care and providing proper treatment to mother.
9) Preparation for Delivery
Maternal pre-eclampsia condition,
Preparation for timely delivery to prevent complications to mother and baby based on gestational age and severity.
Keep all necessary emergency equipment ready like airway, catheterization equipment, oxygen, suction apparatus, emergency medicine tray and caesarean section tray etc. properly prepared.
10) Follow up and discharge planning
Planning the post partum care of the mother and properly planning how to recover the mother from the condition of pre-eclampsia.
Advise the client and his family members for proper follow-up of the client and for continuous monitoring of blood pressure.
Thus nursing management of pre-eclampsia is provided for continuous monitoring of pregnant women, timely intervention, comprehensive care and prevention of complications for mother and baby.
⏩Q-2 Answer the following
🔸 a. Define Labour. Describe physiological changes during pregnancy. Define labour. Describe the physiological changes that occur during pregnancy.
Labor
The series of events that take place in the genital organs to bring out the viable product of conception into the outer world through expulsion from the uterus (womb) is called “labour”.
A woman who is in labor is called a “parturient”.
And
The process of giving birth is called “Parturization”.
Normal labor is also called eutoshia.
Normal labor is said when the following criteria can be fulfilled.
1) The onset of labor should be spontaneous and at term (37 to 48 weeks).
2) Vertex presentation of fitus (the occiput of the head of the fitus is in the lower part of the uterine cavity and the chin of the fitus is tucked with its chest).
should be.
3) Duration of labor should not be long (ie if primary gravida mother then average duration of labor should be 12 hours and if multipara mother then average duration of labor should be 6 hours)
4) Birth should be natural with minimum assistance.
5) There should be no complications affecting the health of mother and baby.
Physiological changes during pregnancy
Pregnancy is a condition from the time of conception to the time of delivery. Physiological changes are observed in the mother’s body during pregnancy due to certain types of specific hormones. These changes occur to develop the fetus, prepare the mother’s body for labor, and produce the best milk during the periperium period.
1) Changes in reproductive system
A)Vulva:=
The vulva becomes more edematous and vacuolar.
Superficial varicosities (varicose vein := vein enlarged and swollen, usually seen in leg and also in pelvic area during pregnancy period) are also seen in multipara and labia minora becomes pigmented and its hypertrophy ( Organ size increases).
B)Vajaina:=
Vaginal wall is hypertrophoid,
becomes edematous and hypervascular.
Bluish coloration of the vaginal mucosa due to increased venous blood supply to the vaginal wall is called “Jackemeier’s sign”.
The length of the interior wall increases.
Vaginal secretions are highly acidic, thin and curdy white.
The acidic pH of vaginal secretions inhibits the multiplication of pathogenic microorganisms.
(C) Uterus: During pregnancy, the uterus grows excessively. During pregnancy, the weight of the uterus and its length also increases.
Weight of Uterus: In non-pregnant state, the weight of uterus is about 60 gm, which increases to 900-1000 gm during pregnancy.
Length, Width and Thickness of Uterus:
of the uterus in the non-pregnant state,
Length := 7.5 cm,
Width:=5 cm and thickness:=2.5 cm.
During pregnancy (at term) of the uterus
Length := 30-35 cm,
Height := 22.5 cm and
Thickness: = 20 cm.
Volume of uterine cavity:
In the non-pregnant state, the volume of the uterus is 10 ml, which increases to 5 liters during pregnancy (at term).
Body of Uterus:
Growth and enlargement of the body of the uterus.
Muscles
1) Outer:= longitudinal layer
2) Middle:= vascular layer
3) Inner:= Circular layer
Hypertrophy (increase in size) and hyperplasia (increase in number) are seen in muscles.
After 20 weeks of pregnancy, the length of the uterine muscle fibers increases and the uterine wall becomes thinner due to which the uterus becomes softer and more elastic in pregnant condition than in non-pregnant condition.
Vascular System:
Blood supply begins to increase from 20 weeks onwards due to vasodilatation due to estradiol and progesterone.
The diameter of uterine artery doubles and blood flow increases and veins dilate.
During pregnancy the endometrium of the uterus is called decidua.
Braxton Hicks contractions:
Spontaneous contractions of the uterus early in pregnancy are irregular, infrequent, spasmodic and painless due to no effect on dilatation of the cervix until near term (37-42 weeks) they increase and finally merge with painful labor contractions. is
D) Isthmus:=
During pregnancy the lower segment of the uterus forms an isthmus.
The length of the isthmus in the nonpregnant state is 0.5 cm, which increases in length during pregnancy to a maximum of 7.5 cm-10 cm.
The muscle fibers of the isthmus are arranged circularly in the lower segment and form a sphincter-like structure that allows the fetus to stay in the uterus during early pregnancy.
E)Cervix:=
During pregnancy the cervix becomes vascular, oedematous and hypertrophoid and hyperplastic.
Cervix that becomes soft is called “Goodell’s sign”.
The length of the cervix doubles and its volume also increases.
F) Fallopian tubes:=
The length of the fallopian tubes is slightly increased. The tube becomes congested. Muscles hypertrophy and epithelium flattens.
G)overy:=
Ovulation remains at a standstill during pregnancy. The ovary is hypertrophied and vascularized.
In the usual menstrual cycle, the corpus luteum remains constant and enlarges by two 2.5 cm until the 8th week.
Colloid degeneration occurs and the uterus becomes calcified.Estrogen and progesterone hormones are produced by the corpus luteum and provide an environment to maintain the ovum until placental action begins.
H) Breast:=
Breast size, nodularity, and sensitivity increase with increased vascularity of the breast throughout pregnancy due to the effects of estrogen and progesterone.
The nipple becomes enlarged, dark and erectile.
5 to 15 sebaceous glands that are invisible in the non-pregnant state show hypertrophy called “Montgomery tubercles”. Its secretion around the nipple keeps the nipple and areola moist and healthy.
The areola that becomes dark and pigmented is called primary areola.
In the second trimester, another pigmented zone called the secondary areola forms around the primary areola.
In the first three months, the growth of the ductal system in the breast increases as the pregnancy progresses, its alveolar cells become secretory.
Total weight of breast is 0.4 kg.
The cyst enlarges due to alveolar proliferation and fat deposition and clear sticky fluid can be squeezed from the cyst at about 12 weeks.
At 16 weeks this clear sticky fluid becomes thick and yellow called colostrum which is an important sign of pregnancy.
Changes in other systems of the body.
1) Skin Changes:=
A) Face: Pigmentation is seen around the cheeks, forehead and eyes called “gravidarum in close” or “pregnancy mask” which disappears on its own after delivery.
B) Breast: Visible pigmentation changes occur in the breast.
C) Abdomen:
Linea nigra A brownish black color line visible in the midline from xiphisternum to symphysis pubis is called linea nigra due to melanocyte stimulating hormone.
stria gravidarum
Abdominal wall below the umbilicus and sometimes on the chest and breast is a depressed linear mask that is initially pink but turns glistening white after delivery called stria albicans or stria gravidarum.
Vacuolar spindle and palmar erythema are seen with high estrogen levels.Skin
Mild degree of hirsutism (excess hair) is seen and excess amount of hair is lost during purpureal period.
2) Weight gain Weight loss occurs during the early weeks of pregnancy due to nausea and vomiting. Weight gain remains progressive from the following months.
A healthy woman gains an average of 11 kg (24 lbs) during pregnancy.
During 1st trimester: 1kg,
2nd trimester
During: 5kg,
During 3rd trimester: 5kg,
As the weight increases.
A) Reproductive weight gain
1) Weight of Fits: 3.3kg,
2)Weight of placenta: 0.6kg,
3)Weight of Liker: 0.8kg,
4) Weight of Uterus: 0.9kg,
5) Weight of breast: 0.4kg.
B) net maternal weight gain
1) Increase blood volume:=1.3kg,
2) Increase extracellular fluid:=1.2kg,
3) Fat and Protein:=3.5kg.
3) Cardio vascular system
A) Heart has to work more during pregnancy.
Cardiac volume increases by 10% but there is no change in ECG.
Cardiac output also increases due to increased heart rate and stroke volume.
Pulse rate also increases.
Platelets count is slightly decreased as the concentration rate increases from 40 to 45 mm.
B) Blood Pressure and Blood Volume:
Blood pressure remains within normal limits In some women, diastolic pressure drops by 5 to 10 mm during mid-pregnancy.
C) Venous pressure: Due to the pressure of the gravid uterus on the pelvic vein, the femoral venous pressure increases by 10 cm, then the blood volume also increases, the volume of red blood cells and plasma volume also increases. Many parts of the body like the uterus, Blood flow increases in the pulmonary, renal, skin, and mucosa.
4) Respiratory system
Hyperemia (increased blood flow) and congestion are seen in the upper respiratory mucosa.
Increased inspiration also increases oxygen intake and oxygen supply to the fetus.
Carbon dioxide is released due to increased exhalation, so the transfer of carbon dioxide from the fetus to the mother’s blood can be easily done due to low maternal carbon dioxide.
In the last weeks of pregnancy, due to the pressure of the gravid uterus on the diaphragm, there is a complaint of breathing difficulty which is relieved by lightening.
5) Digestive system
Due to the effect of progesterone, the muscle tone of the gastrointestinal system is reduced.
Relaxation of cardiac sphincter leads to regurgitation of stomach contents and heartburn.
As the gastric size decreases, it slowly empties and is continuous even in labor.
In many women, the gums become spongy and vascular and may bleed during brushing.
A decrease in the size of the intestine leads to better absorption of food and causes constipation.
6) Nervous system
Mood changes during pregnancy and periperium period are due to psychological conditions such as nausea, vomiting, mental irritability and sleeplessness.
Women may also develop depression or psychosis.
Compression of the median nerve in the wrist leads to pain and paresthesia (tingling) in the hands and arms, which is called carpal tunnel syndrome and is seen in the last month of pregnancy as well as sensory loss due to compression of the cutaneous nerve.
7) Urinary track
Frequent micturition is commonly seen in early and late pregnancy.
Stress incontinence can also occur.
Due to continuous dilatation of uterus and pelvis from early pregnancy to mid-pregnancy, urinary stasis occurs and infection can also occur. Renal function also increases in pregnancy.
8) Locomotor system
Backache is common during pregnancy due to relaxation of lordosis and joints due to relaxin hormone.
Due to weight gain in sacral and lumbar plexus, leg cramps remain and difficulty in walking also occurs.
Thus, physiological changes are observed in women during pregnancy.
b. Describe nursing responsibilities during administration of Inj oxytocin in labor. In during labor. Describe the nurse’s responsibilities when administering oxytocin.
Responsibilities of the nurse when administering injectable oxytocin during labor:
Administering injectable oxytocin during labor is a critical responsibility for the nurse.Although oxytocin plays an important role in facilitating labor and managing labor progression, nursing responsibilities for oxytocin administration are as follows.
1) Assessment and Preparation
assessment
Before administering injection oxytocin, the nurse should properly assess the pregnant woman’s labor progress, fetal heart rate, and uterine contractions and maternal vital signs. Due to which medication can be properly initiated and continued.
Preparation
Properly according to hospital protocols and as prescribed by health care personnel
2) Monitoring
Uterine contractions
Continuously monitor uterine contractions by palpation method and assess whether urine contractions are regular and proper or not.
Fetal heart rate
Continuously monitor fetal heart rate and assess for signs and symptoms of fetal distress.
3) Administration
Initiation and Adjustment
Properly administering medication prescribed by a health care provider.
Keep the infusion rate low initially and then increase the infusion based on uterine contractions and labor progression.
4) Patient education
Explanation
Provide explanation to the mother and her support portion about the purpose of oxytocin infusion, its side effects, and continuous monitoring.
Expectations
Provide an explanation to the mother and her spotters about the expected increase in intensity and frequency of uterine contractions after administration of oxytocin.
5) Documentation
charting
Documentation of oxytocin administration, including starting time, infusion rate, maternal vital signs, uterine contraction pattern, and continuous charting of fetal heart rate.
Response to treatment
Properly monitor uterine contractions and assess progress of labor to assess how effective oxytocin is after oxytocin infusion.
And any side of oxytocin
Assess whether there is an effect or not.
6) Communication
Communication with other healthcare personnel for oxytocin administration eg.
obstetrician,
Collaboration with midwife and other nurses.
Patient updates
Provide ongoing patient updates to the mother and her support person including information on labor progress, fetal well-being, and any changes after oxytocin administration.
7) Emergency Response
If any type of side effect is observed during the administration of oxytocin and other symptoms are observed such as uterine hyperstimulation, then oxytocin should be discontinued immediately and supportive care should be provided.
Thus there is a need to perform this type of nursing responsibility while providing injectable oxytocin.
🔸OR🔸
🔸 a. Define first stage of labor and write nursing management of first stage of labor.
First stage of labor
The first stage of labor is the initial phase of childbirth. In which the cervix gradually opens (dilate) and thins (effacement). Due to this, the baby can pass from the uterine cavity into the birth canal (vagina). In which regular and rhythmic uterine contractions are seen and the frequency, intensity and duration of uterine contractions gradually increases. The first stage of labor is also called the cervical stage which starts with true labor pain and ends with the cervix fully dilated to 10 cm.
First Stage No Time Period:
Primigravida:=12-16 hours, and
Multigravida:=6-8 hours, no.
The first stage of labor is divided into three phases.
1) Latent Phase,
2) Active phase,
3) Transitional phase
1) Latent Phase,:-
The latent phase is known as “prodomal labor” or “pre-labor”.
Cervical dilatation of 1-4 cm centimeters occurs in this stage.
Contractions in this phase repeat every 15-30 minutes and last for 15-30 seconds.
Mother is talkative in this phase.
2) Active phase,
Active phase is also known as dilatation phase.
Cervix in this phase
5 – 7 cm dilated. And the contractions are repeated every 3-5 minutes and
Seen for 45 – 60 seconds.
In this stage mother feels restlessness.
3) Transitional Phase:-
In the transitional phase, the dilatation of the cervix is 8-10 cm.
Contractions are repeated every 2-3 minutes and last for 60 to 90 seconds.
The first stage of overall labor is the critical period in which, after the cervix opens, the uterus prepares for delivery by providing the proper position of the baby in the uterine cavity. Continuous monitoring by health care providers is important to improve the condition and well-being of mother and fetus during this stage.
••> Nursing Management of First Stage of Labour:-
Comprehensive care is involved in the nursing management of the first stage of labor. Its aim is to support the mother physically, emotionally and educationally and closely monitor the progress of labor.
1) Assessment:-
To properly monitor the progress of labor, the condition of the mother and the condition of the fetus.
Inquire about when the labor pains started.
Any kind of liker should be inquired whether there is leakage or not.
Proper examination of the mother.
Perform proper obstetric examination.
Vaginal examination of the mother.
To properly check the antenatal records of the mother.
Maternal Assessment:-
Regular monitoring of the mother’s vital signs, such as
temperature,
pulse,
Respiration,
And to assess blood pressure properly.
To properly assess the intensity, frequency, duration, and resting tone of uterine contractions of pregnant women by palpation method.
Properly assess cervical dilatation and effacement by pervaginal examination.
Properly and accurately documenting and charting cervical dilatation and effacement.
Fetal Assessment:-
Continuous monitoring of fetal heart rate by electronic fetal monitoring (EFM).
Properly assess the fetal heart rate pattern.
Proper documentation of fetal heart rate and any abnormality should also be properly documented.
2) Support and Comfort Measures:–
Providing a properly comfortable position to the mother due to which the comfort level of the mother can also increase and the labor process can also progress like walking, standing, sitting etc.
Advising the mother on relaxation techniques such as deep breathing exercises, and mind diversional therapy etc.
Provide emotional support, reassurance and psychological support to the mother to reduce her anxiety.
3) Hydration and Nutrition:-
Advise the mother to have moderate fluid intake.
Continuously monitor the mother’s intake output chart to properly maintain the mother’s hydration status.
Advise the mother to take adequate amount of light food and take plain food to maintain the nutritional status of the mother.
Like plain water,
Salty Lemon Water,
Soup, and fruit juice etc.
4) Antiseptic and Aseptic:-
Applying proper antiseptic dressing on the genital area, due to which cleanliness can be maintained.
5) Education and Communication:-
To provide education to the mother and her supporters about the mother’s condition and progress of labour.
6) Care of Bowel:-
Provide proper enema to clear mother’s bowel and increase uterine contractions.
7) Care of Bladder:-
Advise pregnant women to empty the bladder frequently as a full bladder inhibits contracture.
8) Documentation:-
After assessing the condition of the mother and fetus, properly document it and maintain the partograph properly.
Properly documenting all assessments, interventions, observations, in the mother’s medical record.
Properly record maternal vital sign, uterine contraction pattern, cervical dilatation and effacement, fetal heart sound and labor progress.
9) Collaboration and Advocacy
Collaborating with other health care personnel such as obstetricians, midwives and nurses to properly communicate the condition of the mother’s labor and take decisions about the condition of the mother.
Thus, by properly managing the first stage of labor, complications in the mother and fetus can be prevented and the first stage of labor can be properly maintained.
b. Describe immediate newborn care in L.R.
Immediate newborn care provided in the labor room
Immediate newborn care involves properly assessing and stabilizing the newborn.
Immediate newborn care is crucial for the stabilization of the fetus from intrauterine life to extrauterine life.
Goal of immediate newborncare
1) Respiration of newborn is done to establish, maintain and provide support.
2) To prevent the newborn from vomiting and hypothermia.
3) To prevent infection in the newborn.
4) To provide safety to the newborn and prevent him from injury.
5) To provide immediate treatment by early identification of any actual or potential problem in the newborn.
Immediate newborn care is provided.
•>Immediate Newborn Care
1) Establishment of Respiration:-
Immediately patent the newborn’s airway and clear the airway properly when the newborn is received. Due to which the newborn can effectively breathe.
As soon as the newborn’s head is born, wipe the mouth and nose and suction the mouth and nose so that the newborn can breathe properly. Saxon should be done through the mouth first and then through the nose to prevent aspiration of secretions.
2) Initiation of Cry :-
Normally up to 99% of newborns cry immediately and spontaneously after delivery, this cry is recognized as a good sign for the newborn’s breathing.
If the newborn does not cry properly, follow the steps below:
a) If the baby does not cry spontaneously or if the cry is weak then slightly simulating the baby to cry.
b) Lightly rub the soles of the baby’s feet instead of slapping them on the bum to stimulate the baby’s cry. Stimulate the baby to start crying after removing the newborn’s secretions.
C) Newborn’s cry is usually loud and husky and proper monitoring of newborn if there is any abnormal cry like,
•>Hypech cry:= due to hypoglycemia and increased intracranial pressure,
Weak cry:= prematurity,
Hosacry:= laryngeal stridor
3) Care of Koda:-
Cord care is important immediate care of the newborn.
A newborn’s cord should be clamped within 30 seconds of birth and then properly cut.
After the newborn is delivered, keep the newborn on the mother’s abdomen.
Then properly clamp the cord from two opposite sites by cord clamp.
The first clamp should be placed 5 cm from the umbilicus and the second clamp should be placed 2.5 cm from the first camp.
Then properly cut the cord between the two clamps.
Do not apply anything to the cord, let it dry and fall naturally.
The code folds down naturally within seven to ten days after birth.
Prevent the cord from getting wet by water and urine.
If any kind of discharge and bleeding is present in the cord, immediately assess the cord clamp and then loosen it properly.
Immediately if the following signs and symptoms are observed in the coda
To report such as,
Foul smell coming from the cord,
Seeing any discharge,
Redness around the cord,
The cord is wet,
If the cord does not fall down in 7-10 days,
inflammation,
Fever etc.
4) Maintain position of the newborn:-
During the first 12-18 hours after birth, the newborn is prone to choking, phlegm and gagging of mucus. So providing proper position to the newborn.
In which proper side lining position should be provided to the fitters due to which mucus can be removed and drainage can be done.
5) Identification and Banding:-
After the baby is born, proper identification band should be applied to the baby so that the baby can be properly identified.
6) Eyecare:-
Clean the newborn’s ice from inner canthers to outer canthers with properly sterile gauze.
Apply erythromycin or tetracycline ointment from the lower lead in ice if needed.
7) Attachment and Bonding:-
After the birth of the baby, placing the baby on the mother’s abdomen, due to which bonding with the mother and proper skin-to-skin contact can take place, due to which the attachment of the mother and the baby can occur and the baby can be prevented from hypothermia.
8)APGAR Score:-
APGAR score is the most important parameter of immediate newborn care.
APGAR score should be assessed at 1 minute and then 5 minutes after birth.
In APGAR score,
A:= Apperience
(skin color),
P:=Pulse (hotrate),
G:= grimace (reflux irritability),
A:=Activity
(muscle tone),
R:= Respiration (Respiratory Efforts)
is assessed.
APGAR score has a total score of 0-10.
APGAR score at 1 minute after birth:
If the Apgar score is 7-10 then it is called normal i.e. no depression in which the baby is provided with normal post delivery routine care.
If the APGAR score is between 4-6, it indicates mild depression in which the child requires assistance for breathing.
If the APGAR score is between 0-3, it indicates severe depression requiring resuscitation of the child.
APGAR score at 5 minutes after birth:
An APGAR score between 7-10 is considered normal, but if the Apgar score is below 7, the baby needs to be monitored for another half hour.
Thus, the immediate care of the newborn after birth is done as follows.
⏩Q-3 Answer in short (Any two) Write the answer in short (Any two)
Partograph
Definition:
Partograph A Cervical dilatation,
A graphic recording and tool for fetal head descent and labor progress and the condition of the mother and fetus. Partograph provides immediate and relevant information about the condition of the mother and fetus.
It recognizes the need to take action for appropriate time and timely referral. Morbidity and mortality rate of mother and fetus can also be improved through partograph.
Objectives or Advantages:
1) To record observations during labor properly.
2) To understand the latent and active phase of labour.
3) Interpreting the partograph to recognize any deviation from normal and take appropriate action.
4) To know the progress of labor so that action can be taken and referred at the right time.
5) Records can be seen at a glance in a single seat and easily handed over.
6) To avoid having to record the event of labor repeatedly.
7) To prolong labor and decrease the rate of education.
Observation Charted on Partograph:
1) Pregnant Woman Information:
A) Name,
B) GTPAL score
G: gravida,
T:=Tommy Birth,
P:=mercury,
A:= Abortion,
L:= Living Children.
C) Name of Hospital,
D) Hospital Registration Number,
E) Date and time of admission,
F) Time of membrane rupture,
G) Period of Gestation,
H) Date and time of labor onset.
2) Fittal condition:
A) Fetal heart rate,
B) amniotic fluid,
C) Molding.
3) Progress of Labour
A) Cervical dilatation,
B) Descent of head,
C) uterine contractions.
4) Maternal condition
A) Oxytocin, drugs and I.v. fluid administration
B) pulse,
C) blood pressure,
D) Temperature,
E) Urine volume, acetone and protein.
All this information is filled in a partograph.
Points to keep in mind while filling partograph:
1) Partograph maintenance should be started when the woman reaches the active phase of labor and the pregnant woman should not be left alone.
2) The fetal heart rate should be counted and recorded every half hour.
Fetal heart sounds should be counted for a full 1 minute and should be counted immediately after uterine contractions are detected.
3) Monitor uterine contracture frequency, intensity, duration, pulse, fetal heart rate every 30 minutes when dilatation of cervix is 4 cm or more.
4) Monitor blood pressure and cervical dilatation (in cm) every two hours.
5) Monitor descent of head and temperature every four hours.
Partograph
1) Patient Identification Data
In this, the woman’s name, age, GTPAL score, date and time of admission, registration number, time of rupture of membranes and time and date of onset of labor are marked.
2) Fittal condition
Counting and recording the vital heart rate every half hour.
To account for 1 minute of full heart rate.
To count fetal heart rate immediately after uterine contractions.
Fetal heart sound (FHS) < 120/Minutes or FHS > 160/Minutes indicates fetal distress. If there is a condition of fetal distress, immediate action should be taken.
A vertical column in each small box represents that half-hour interval.
2) Condition of membrane
Record condition of amniotic membrane and color of amniotic fluid every 30 minutes along with fetal condition.
A) Amniotic membrane is an intake if :=
I (Intect),
B) If liker is clear := C (Clear),
C) If Liker A is Absent := A( Absent) ,
D) If the amniotic membrane is ruptured := R (Rupture),
E) If there is meconium stained liquor:= M( meconium),
F) If blood is present in the liquid: B (Blood)
Thus, marking the condition of amniotic membrane and amniotic fluid in the partograph.
3) Molding (The bones of the fetal head are separated by sutures and fontanelles, but while passing through the birth canal, the bones of the fetal head overlap each other and the gap of the head changes for some time due to which the fetal head is a (This condition can easily pass through the birth canal is called molding.)
Moldings are recorded by grade to record.
A) 0 -> If bones are separated and sutures are easily felt.
B) + -> When the bones just touch each other.
C) ++ -> When bones are overlapping but easily separated.
D) +++ -> Bones are severely fixed when overlapping.
4) Progress of Labour
Start plotting labor progression on the partograph only after the woman is in active labor.
Active labor A cervical dilatation of 4 cm or greater and the athlete having two good contractions every 10 minutes should start plotting on the partograph.
Recording cervical dilatation in cm every four hours.
Record the onset of cervical dilatation starting from the left luteal line (when the mother is in active labour). Normally the graph line is continuous above the left alert line to show the proper time each time.
If the alert line is crossed i.e. if the graph moves to the right of the alert line then it indicates prolonged labor. Hence the midwife should be immediately alerted that there is something abnormal in the labour. Noting the time the alert line is crossed and immediately initiating measures for immediate treatment or referral.
When the graph crosses the action line i.e. if the action moves to the right side of the line, start treatment immediately or refer the mother to appropriate medical services.
The gap between alert and action line is 4 hours.
5) Uterine contractions
Recording uterine contractions every half hour Contractions twice in ten minutes indicate good uterine contractions.
Marking it as follows in the box of the partograph.
•••• -> Mild uterine contractions < 20 seconds,
///// -> Moderate uterine contractions 20 – 40 seconds,
■ ->Strong uterine contractions > 40 seconds.
6) Cervical dilatation and descent of fetal head
Descent of the fitter head occurs simultaneously with cervical dilatation throughout the labor process.
Until the cervix is 7 cm, the descent of the fetal head is assessed by abdominal palpation with the assessment of the fifth (5) number of the fetal head above the pelvic brim.
In the partograph, cervical dilatation is plotted by (x) while descent of the fetal head is plotted by (O).
7) Maternal condition
Maternal pulse every half hour
is recorded on the partograph and is plotted in the partograph by a dot(•).
Maternal blood pressure is recorded every 4 hours with both systolic blood pressure and diastolic blood pressure indicated by vertical arrows ( ↕ ) with the upper end of the arrow indicating systolic BP. While the arrow no lower end shows the diastolic blood pressure.
Recording the maternal temperature every four hours on a partograph.
Proper recording of maternal urine volume, urine acetone and protein level on partograph.
If any drug or oxytocin medication is given to the mother during the labor process, properly recording the dose route and time of administration.
Thus, early, quick and relevant information about labor progress and condition of mother and fetus can be obtained through Partograph.
b. Placenta –
Introduction
Placenta is a mass like structure. It usually develops in the anterior or posterior side of the upper uterine segment from two sources namely the fetal component chorion frondozum and the maternal component decidua basalis.
The placenta is connected to the fetus through the umbilical cord and the pregnancy is maintained. The placenta supports the life of the embryo by providing oxygen and food to the embryo and removing toxic materials.
Definition
The placenta has a “discoid shape” due to its septum.
It is “hemochorionic” because its chorion comes into direct contact with maternal blood, and it is “deciduous” because the placenta sheds off after birth.
Placenta origin
The placenta originates from the trophoblastic layer of the fertilized ovum.
The patient is closely linked to the mother’s circulation to properly perform functions that the fetus is unable to perform during intrauterine life.
The survival of the fetus depends on the integrity and efficiency of the placenta.
Attachment of placenta
The placenta is attached to the mother’s uterine wall and establishes a connection between the mother and the fetus through the umbilical cord.
Placenta at Fultma
At most the placenta is a disc-like spongy, fibrous structure that is flat and round or oval in shape. The placenta is thick in the center and thin at the edges.
Diameter and thickness of placenta
1)Average weight of placenta a:=
500 grams
2) Ratio between fetus and placenta := 1/6( 3kg / 500 gm).
3) Diameter of placenta a:= 15-20 cm.
4)Surface area of placenta:= 243 sq cm
(square centimeter).
5) Volume of placenta A:= 500 ml.
6) Placenta is thick in the center while thin at the edges.
Center Path of Placenta:=
2.5 to 3 cm.
Peripheral tract of placenta :=
1 to 1.5 cm
The umbilical cord connects the fetus to the placenta with an umbilical vein and
There are two umbilical arteries.
Part of placenta
The placenta has two surfaces.
1) Fetal surface (80%),
2) Maternal surface (20%)
1) Fetal surface (80%):
The fetal surface is smooth, sinuous and transparent, covered by a smooth and glistening amnion.
In which the umbilical cord is connected at the center.
Umbilical vessels are seen on this surface.
The fittal surface is bright red in color.
2) Maternal Surface (20%):
Maternal surface is “rough and spongy”.
It is dull red in color.
The maternal surface is divided into 15 to 30 cotyledons separated by sulci.
A small calcified infract appears on the maternal surface.
Structure of placenta
The placenta consists of two plates. The chorionic plate lies inward and is covered by the amniotic membrane. The umbilical cord attaches to this plate. On the maternal side there is a basal plate.
The intervillous space lies between the chorionic plate (fetal site) and the basal plate (maternal site).
In this intervillous space, the stem cell and its branches are located and the maternal blood is located in this space.
1) Amniotic membrane
Amniotic membrane is a single layer of cubical epithelium and connective tissues. And the amniotic membrane is loosely attached to the chorionic plate.
It has no part in placenta formation.
2) Chorionic plate
The chorionic plate is the seat of connective tissue. It contains branches of umbilical vessels. The chorionic plate is covered by the amniotic membrane at the fetal site.
Stem cells arise from the chorionic plate that forms the inner boundary of the choriodecidual space.
3) Basal plate.
The basal plate is formed from cytoblasts, syncytoblasts, and decidua basalis.
It is a compact and spongy layer.
A basal plate is present nearer the maternal surface.
The uterine artery and vein enter the intervillous space from the basal plate.
The basal plate forms the boundary at the maternal surface.
4) Intervillous space
It has chorionic plate on the inner side and basal plate on the outer side. There is a connection of two plates around.
Internally all sides are lined with syncytotrophoblasts and filled with slow flowing maternal blood.
In this intervillous space are the stem cells and their branches.
5) Stem branching
Stem cells arise from the chorionic plate and extend to the basal plate.
Primary, secondary and tertiary divisions are formed in progressive development.
The functional unit of the placenta is the fetal cotyledon or placentome. It is formed from major primary stem villus.
These major stem villi pass through the intervillous space and anchor in the basal plate. The functional subunit is called the lobule, which is formed from the tertiary villi.
There are about 60 stem cells in the human placenta. Hence each cotylodon (total :=15-20) has three to four major stem branches. Some villi anchor the placenta and some remain free in the intervalsal space called nutritive villi. The blood vessels in the villi do not connect with each other.
Circulation through the placenta There are two types of circulation in the placenta.
1) Phyto Placental Circulation,
2) Uteroplacental circulation
1) Phytoplacental Circulation,:- In phytoplacental circulation two umbilical arteries bring the impure blood from the placenta and enter the chorionic plate, each supplying 1/2 of the placenta.
The arteries break into small branches and enter the stem of the chorionic villi, which divide into primary, secondary, and tertiary vessels. Maternal and fetal blood flow side by side in opposite directions.
Fetal blood flow is 400 ml/minute which is mainly due to the pumping action of the fetal heart rate. Blood from the umbilical artery delivers carbon dioxide to the placenta and absorbs oxygen and returns to the fetus through the umbilical vein.
2) Uteroplacental Circulation (Maternal Circulation) :-
In the uteroplacental circulation, uterine arteries and veins enter the intervillous space through the basal plate and transmit blood and nutrients from the mother to the intervillous space.
Function of placenta
1) Respiratory function :-
The fetus receives oxygen through the placenta and excretes carbon dioxide. Just as oxygen from the mother’s blood passes into the fetal blood, the carbon dioxide in the fetus is transmitted to the maternal blood through the placenta.
2) Nutritive function:-
All types of nutrients such as amino acids, glucose, vitamins, minerals, lipids, water and electrolytes are transmitted from the mother to the fitters.
The food taken in the maternal diet reaches the placental side where it is converted into simple form, then the placenta selects the substances required by the fetus and transmits them to the fetus.
3) Storage function:– Placenta stores glucose, iron and vitamins. And the placenta provides it when the fetus needs it.
4) Excretory function:- The waste product in the fetus is transmitted to the placenta.
5) Protection:– Placental membrane has limited barrier function. Some antibodies that pass from the mother to the fetus provide immunity to the baby for three months after birth.
6) Immunological function:- Antigens of fetus and placenta act as foreign to mother. However, graft rejection does not occur because the placenta provides immunological protection against rejection.
7) Hormonal function:-
steroid hormones
estrogen,
Progesterone.
Protein hormones
HCG (Human Chorionic Gonadotrophin),
HPL (Human Placental Lactogen),
relaxin,
PAPPA (Pregnancy Associated Plasma Protein:= A).
•>HCG (Human Chorionic Gonadotrophin),
HCG (human chorionic gonadotrophin) is produced from the cytotrophoblastic layer of the chorionic villi.
HCG (human chorionic gonadotrophin) is high during 7 to 10 weeks of pregnancy then decreases as the pregnancy progresses it maintains the corpus luteum.
HCG (human chorionic gonadotrophin) is used in pregnancy tests because it is excreted in the mother’s urine.
HCG (human chorionic gonadotrophin) is detected in blood on day 7 and urine on day 9 after fertilization, which indicates a positive pregnancy test.
••> HPL (Human Placental Lactogen)
HPL (Human Placental Lactogen) is produced from the placenta and is involved in the lactogenic and metabolic processes of pregnancy. When the level of human chorionic gonadotropin trophin decreases, the level of human placental lactogen (HPL) increases and it continues in throwout pregnancy.
Human placental lactogen (HPL) works as an anti-insulin that increases blood glucose levels and helps supply glucose to the fetus.
••>Relaxin
Relaxin is produced by decidual cells. And it softens the cervix and helps the pelvic ligaments and symphysis pubis to relax the labor process.
••>PAPPA (Pregnancy Associated Plasma Protein:= A)
Pregnancy Associated Plasma Protein:= A works as an immunosuppressant and works to maintain pregnancy.
••> Estrogen
Estrogen is produced by the placenta in a throwout pregnancy. It is essential for welling of the phytoplacenta.
Estrogen increases during labour, which helps in the release of oxytocin, which increases uterine contractions.
••> Progesterone
Progesterone is produced from the synovial layer of the placenta which works as a tocolytic agent and prevents uterine contractions as well as works as an immunosuppressant to help maintain the pregnancy.
c. Difference between Placenta Previa & Placenta Abruptio Tell the difference between placenta previa and placenta abruptio.
Difference between placenta previa and abruptio placenta:
1) Clinical features
•>Placenta previa
Nature of Bleeding:-Painless, painful and recurrent bleeding.
Bleeding is always visible.
Abruptio Placenta:-
Bleeding caused by painful, preeclampsia or trauma.
Bleeding can be a mix of visible and invisible bleeding.
•>Placenta previa
Character of blood:- Bright red color blood is seen.
Abruptio Placenta:- There is blood of dark red color.
•>Placenta previa
General Condition and Anemia:- Anemia is seen in proportion to visible blood loss.
Abruptio placenta:- In this the condition of anemia is higher than the amount of visible blood loss.
•>Placenta previa
Features of preeclampsia:- The condition of preeclampsia is not associated with placenta previa.
Abruptio placenta:- Abruptio placenta with features of preeclampsia is seen in 1/3 cases.
2) Abdominal examination
•>Placenta previa
Height of Uterus:- According to the gestational age, the height of the uterus is seen.
Abruptio placenta:- In abruptio placenta the height of the uterus is enlarged more than the gestational age.
•>Placenta Previa:-
Feel of Uterus:- In placenta previa uterus feels soft and relaxed.
Abruptio placenta:- Abruptio placenta in uterus can be tense, tender and rigid.
•>Placenta previa
Malpresentation:- Malpresentation is common in placenta previa and the head is high floating.
Abruptio Placenta:-
Abruptio placentae malpresentation is unrelated and may also involve the head.
•>Placenta previa
FHS (Fetal heart sounds) :- Heart sound is mostly present in placenta previa.
Abruptio placenta:- Heart sound is mostly absent in abruptio placenta.
3) Placentography (USG)
Placenta Previa:- The placenta is found in the lower segment of the uterus.
Abruptio Placenta:- The placenta is found in the upper segment of the uterus.
4) Vaginal examination
Placenta Previa The placenta is implanted in the lower segment of the uterus.
Abruptio placenta The placenta does not feel in the lower segment of the uterus.
⏩Q-4 Write Short Notes (Any Three)
🔸 a. Objectives of Antenatal care –
The aim of antenatal care is to improve the overall health of the fetus and the mother and to improve the well-being of the mother and the fetus and to prevent complications.
1) Monitoring Maternal Health:- By doing regular health checkup, the overall health of the mother can be monitored, such as blood pressure, weight gain, and overall well-being etc. can be properly assessed, due to which the mother can be identified early if she has any kind of complications. And by treating it early, it can be prevented from happening further.
2) Monitoring Fetal Health:– Assessment of the fetus in antenatal care including ultrasound scan, fetal heartbeat monitoring, and other tests to be done properly due to which the growth and development of the fetus can take place properly. If the child has any abnormality, it can be detected early and properly managed.
3) Health Education:– Antenatal care provides the opportunity of appropriate education to the expectant mothers, which provides the opportunity of education about pregnancy, child birth, breast feeding, nutrition and parenting. This education can be helpful to the antenatal mother in making proper decisions.
4) Pregnancy :- Early detection of related complications for proper management.
By visiting antenatal care, early detection of pregnancy related complications can be done and its timely management can be done. like,
gestational diabetes,
Preeclampsia, infection and other pregnancy related risks that can affect the pregnancy.
5) Preparation for Childbirth:– Birth planning, preparation for labor, and delivery options are discussed in the antenatal care session. By having this discussion, the mother and her family members can mentally and practically prepare for child birth.
6) Psychological support:– Emotional and psychological changes are seen due to pregnancy. Antenatal care provides a supportive environment in which the expectant mother can discuss her anxiety, fear and doubts and clear them and reduce her anxiety and fear and feel emotionally well-being.
7) Prevention and Management of Maternal and Infant Complications:-
Antenatal care interventions include immunization, iron and folic acid supplementation, and preventive treatment to prevent pregnancy and childbirth related risks and complications.
8) Promotion of Healthy Behavior:– Education is provided to promote behaviors in antenatal care including smoking cessation, avoiding alcohol and drugs, maintaining a balanced diet, and being physically active, these behaviors are important for healthy pregnancy outcomes.
9) Postpartum Planning :- In antenatal care post partum care is also discussed in which, post partum care,
Breast feeding support and family planning options are discussed.
The objectives of overall antenatal care are to have a healthy pregnancy, properly manage any risks and complications, prepare the mother for child birth, and properly maintain the health of the mother and fetus during the throwout pregnancy.
b. Infertility
Definition:= Infertility is a medical condition in which there is inability to conceive a pregnancy despite having regular and unprotected intercourse for 1 year or more, then such a condition is called infertility.
It affects approximately 10-15% of couples worldwide. Infertility can be due to various factors affecting male, female or both, and can be temporary or permanent.
Type of Infertility
There are generally two types of infertility.
1) Primary infertility,
2) Secondary infertility
1) Primary Infertility:- It refers to patients who have not been able to conceive a single pregnancy.
2) Secondary Infertility:–
Thus, prior pregnancy indicates conception but subsequent failure to conceive is called secondary infertility.
Causes of Infertility
There are three main causes of infertility.
1) Fault in female,
2) Fault in Mail,
3) Combined factor.
1) Fault in Female:-
A) Ovarian factor:-
Ovulatory dysfunction is seen mainly for its three reasons as follows.
a) Anovulation/ Oligoovulation:-
Anovulation/oligoovulation is usually due to disturbances in the hypothalamopituitaryovarian axis.
Ovarian activity depends on gonadotrophin and normal secretion of gonadotrophin depends on GnRH (gonadotrophin releasing hormone) released from the hypothalamus.
(b) Lutenized unruptured follicle (LUF)
(Trapped Ovum):-
This is seen due to inadequate growth and function of the corpus luteum.
(C) Trapped Uvam:-
In this, the ovum is trapped inside the follicles, usually due to endometriosis or hyperproductemia.
2) Tubal Factors:-
Infertility in this is usually due to tubopathy (tubal infection) due to which tubal functions are impaired.
Ex:= Defective ovum pickup followed by infertility.
3) Peritoneal factor:-
One and the main factor of infertility is endometriosis.
4) Uterine factor:-
These include certain factors that stop the implantation of the fertilized ovum into the endometrium.
These factors like,
a) Endometriosis,
b) fibroid uterus,
c)Uterine hypoplasia,
d) Congenital malformation of the uterus.
5) Cervical Factors:-
In this due to second degree uterine prolapse,
Due to retroverted uterus,
And due to changes in the composition of the cervical nucleus.
6) Vaginal factor:-
These include vaginal atresia,
Transverse vaginal septum, due to
2) Fault in Mail:
1) Due to defective spermatogenesis:–
This leads to infertility and is usually due to the following:
orchitis,
undescended testes,
testicular toxins,
Primary testicular failure,
Due to genetic or chromosomal disorders such as, 47,XXY,
Due to endocrine factors such as thyroid dysfunction.
2) Obstruction of the efferent duct system due to:-
These are found in two types.
1) Congenital:-
As the vas deferens are absent.
2) Acquired:-
This is usually due to some infection,
Occurs due to tuberculosis, gonorrhea, and surgical trauma (during herniorrhaphy).
3) Failure to deposit spam in Wajaina:-
This is due to failure to deposit sperm in the vagina.
This is due to:
impotence,
Ejaculatory failure,
hypospadias,
4) Due to error in seminal fluid:-
Hence, due to immotile sperm,
Due to disturbance in sperm count,
Because of the low fructose count.
3) Combined Factor:-
In this, infertility is seen due to the combined factors of both male and female.
Diagnostic Investigation:-
Complete history collection and physical examination
This includes assessment of overall health, including reproductive health, history and identification of potential risk factors.
Ovulation Testing:-
This includes monitoring the menstrual cycle and properly assessing whether ovulation occurs regularly.
Siemens Analysis:-
In this, sperm count is evaluated and sperm size, morphology, and other parameters are assessed.
Imaging Testing:-
This includes ultrasonography and hysterosalpingiography to assess the uterus and fallopian tubes.
Hormonal test:– In this hormonal level is assessed to assess ovarian factor and other endocrine disorders.
Diagnostic procedures:– Like, laparoscopy (to examine the organ), and genetic testing (to identify chromosomal abnormalities).
Treatment:– Treatment of infertility depends on its cause, duration and duration of infertility.
Medication:– Fertility drugs are provided to stimulate ovulation in women and improve sperm production and function in men.
Surgery:- Surgery corrects anatomical abnormalities like tubal blockage, uterine fibroid, and varicocele (enlarged vein in scrotum).
Assisted Reproductive Techniques (ART)
Intra uterine insemination (IUI)
In this, sperm are placed directly into the uterine cavity during ovulation.
In Vitro Fertilization (IVF)
In this, the ovum and sperm are fertilized in the laboratory and then the embryo is transferred to the uterus.
Intra Cytoplasmic Sperm Injection (ICSI)
In this procedure, a single sperm is injected directly into the egg to cause fertilization.
Surrogacy
Surrogacy is done when it is not possible to carry the pregnancy to term.
General Nursing Management:
To take proper measures to improve the general health of the patient.
If the person is obese, give advice to reduce weight.
Advise the patient to avoid heavy smoking and alcohol.
Advise the patient to award tight and loose undergarments.
Advise the patient to take proper vitamin E, vitamin C, vitamin B12 and folic acid which improves spermatogenesis.
Provide proper psychological support to the patient.
Properly checking the patient’s body weight and calculating the body mass index which
Should be between 20-24.
Advising patients on proper stress management. In which giving advice to the patient to do yoga and meditation properly
c. Causes of onset of labor
Reasons for onset of labor:
No exact cause of labor is known but it is said that many factors are responsible for the onset of labor such as,
1) Mechanical Cause,
2) Hormonal causes,
3) Neurological causes
1) Mechanical Cause,
ama,
Heightened reflex irritability of the uterus,
uterine distention,
Menstrual Period Suppression,
Prolonged pressure of fits.
2) Hormonal causes:
1) Phyto-placental contribution
Fetal hypothalamus is triggered to produce releasing factors.
The anterior pituitary gland releases adrenotrophic hormone due to these factors
( ACTH) is stimulated to produce.
Adrenotrophic hormone
(ACTH) stimulates the fetal adrenal gland to secrete cortisol.
Cortisol causes changes in placental hormones.
Ex:=
Estrogen levels increase,
Progesterone levels decrease.
2) Estrogen hormone: Estrogen increases the chances of mechanism as follows:
1) Increases release of oxytocin from maternal pituitary.
2) Stimulates myometrial receptors to synthesize oxytocin, prostaglandins.
3) Synthesis of prostaglandins by decidual and amnion cells is increased.
4) Myometrial contraction stimulates the synthesis of the protein actomyosin.
3) Progesterone
Progesterone has a relaxant effect on the uterus.
Progesterone is produced first by the corpus luteum and then by the placenta.
It inhibits uterine contractility.
Fetal production of dehydroepiandrosterone sulfate (DHEA-S) and increased cortisol inhibits the conversion of fetal pregnenolone to progesterone.
Hence progesterone levels fall down before labor while estrogen levels rise.
Then the progesterone level falls down which is associated with the synthesis of prostaglandin.
4) Oxytocin:
The hormone oxytocin is released from the mother’s posterior pituitary gland.
As the level of estrogen increases, it helps in increasing the level of oxytocin.
Oxytocin receptors in the decidual vera are increased at the end of pregnancy. Oxytocin acts directly on the myometrium and causes contraction of the uterus.
It also acts on endometrial tissues to release prostaglandins.
5) Prostaglandins
The major sites of prostaglandin formation are the placenta, fetal membranes, decidual cells and myometrium.
It is said that the release of estrogen causes the uterine decidua to release prostaglandins, which act on the uterine muscles causing the uterine muscles to contract.
3) Neurological causes
Labor can be initiated through a nerve pathway.
Both ‘α’ and ‘β’ adrenergic receptors are present in the myometrium.
Estrogen acts on the ‘α’ receptor and progesterone acts on the ‘β’ receptor.
1)’α’:=’α’ adrenergic receptor Stimulate ‘α’ receptor.
2)’β’:=’β’ adrenergic receptor Stimulate ‘β’ receptor.
A contractile response from the ‘α’ receptors of the prostaglandin nerve fibers located in and around the uterus and in the lower part of the uterus is initiated when progesterone reduces.
So the reasons for starting this labor are as follows.
d. Vesicular mole
Definition
A vesicular mole is also called a hydatidiform mole (H.mole).
This is an abnormal condition of the placenta. In which few degenerative and few proliferative changes occur in the young chorionic villi and due to this cluster (lump like shape) is formed in the cyst. And because it resembles a hydatid cyst, it is called a hydatidiform mole or vesicular mole.
When the chorionic villi transforms into a mass of translucent vesicles, it forms a bunch-like structure called a hydatidiform mole.
etiology
Its exact cause
is unknown,
Due to ovular defect,
It can also be due to the following reasons:
Hemorrhagic pregnancy,
In most teenage pregnancies,
In women over 35 years of age,
Due to faulty nutrition habits such as low protein intake,
Due to low calorie intake in the diet,
Due to disturbed maternal immune mechanism,
Because of the history of hydatidiform mole,
Women whose ovulation is simulated by clomiphene,
Have poor socioeconomic condition.
Type of vesicular mole
There are two types of vesicular mole:
1) Complete Mall,
2) Incomplete Mall
1) Complete Mall:
Complete or classic H. mole forms when fertilization occurs in an egg whose nucleus has been lost and inactivated.
In this the mole resembles a bunch of white grapes.
In this case, the fluid-filled vesicles grow rapidly, causing the uterus to become larger than the expected duration of pregnancy.
Complete mole involves the fetus, placenta and amniotic membrane.
A complete mole can also progress to carcinoma and does not contain an embryo.
2) Incomplete Mall
These contain embryonic or fetal parts and an amniotic sac is present.
Congenital anomalies are present in these.
These contain underdeveloped embryos that fail to survive.
Signs and Symptoms
Abnormal vaginal bleeding,
Bleeding is brownish and watery as the blood mixes with the fluid from the ruptured system giving the appearance of a discharge.
Thus, painless vaginal bleeding occurs during the fourth and fifth months of pregnancy.
Lower abdominal pain.
The patient appears to be ill without any reason.
Hyperemesis gravidarum occurs.
Early features of pre-eclampsia are seen at periods less than 20 weeks.
Pulmonary embolism causes dyspnoea.
The uterus appears larger during the gestation period.
Thyrotoxic features are observed such as,
Tremors, and anxiety etc.
Fetal heart sound and fitus patas are absent.
Expulsion of grape-like vesicles from the vaginal area.
USG:=Snow storm apparition can be seen.
Diagnostic evaluation
full blood count,
ABO and Rh grouping and blood clotting test,
Hepatic, renal and thyroid function tests,
sonography,
Straight X-ray Abdomen,
Pelvic Angiography,
CT scan and MRI.
Management
Provide proper supportive therapy to the mother so that the lost blood can be restored.
When a vesicular mole is diagnosed, the risk of choriocarcinoma can be prevented by evacuating it by suction and surgical curettage as early as possible.
To test ABO and Rh in mother’s blood investigation.
Start a fluid infusion to the mother immediately.
Provide blood transfusion to the mother if excessive amount of blood has been lost.
Emptying the uterus through a suction procedure means suctioning the mole.
After the end of suction, when no vesicles enter the suction cannula and the uterine cavity contracts, start by adding 10 units of oxytocin to the glucose drip and introduce 0.2 mg of methargin into the drip.
Oxytocin should be avoided during the Sachsen procedure because it causes embolization of vesicles in the patient’s venous channel.
Curating gently and properly from the uterine cavity by blunt curettage.
After curating, the vesicles should be properly sent to the laboratory for histological examination.
To properly monitor the mother’s vital signs like pulse rate, respiration, and blood pressure every half hour.
Administer 10 units of oxytocin to the mother intramuscularly (IM) or, if intravenously (IV), 20 units of oxytocin in 500 ml of normal saline or Ringer’s lactated solution to the patient to prevent postpartum hemorrhage.
Advise the patient to undergo hysterectomy if the patient is above 40 years of age.
Advising the mother to follow up regularly.
Administer Anti D immunoglobulin 100 microgram (IM) if mother is Rh negative.
Advising women to use contraceptive method properly.
Advising the mother to avoid pregnancy for one year.
Advising the mother to follow up for at least two years. Its aim is choriocarcinoma
Find out.
Advising women to take follow-up every three months after 4 to 6 weeks of follow-up and athlete for 2 years includes assessment of women’s history collection, clinical examination.
⏩Q-5 Define the following (Any Six)
🔸 a. Ectopic Pregnancy –
When a fertilized ovum implants and develops outside the normal endometrial cavity, it is called an ectopic pregnancy.
Anatomical site of implantation of ectopic pregnancy:
Tubal pregnancy is more common, normally occurring in the right fallopian tube more often than in the left fallopian tube.
The ampulla in the fallopian tube is the most common site of implantation of an ectopic pregnancy.
If an ectopic pregnancy occurs at the isthmus of the fallopian tube, it is considered a dangerous site that can also lead to tubal rupture.
b. Hydatidiform mole –
Definition
A hydatidiform mole (H.mole) is also called a vesicular mole.
This is an abnormal condition of the placenta. In which few degenerative and few proliferative changes occur in the young chorionic villi and due to this cluster (lump like shape) is formed in the cyst. And because it resembles a hydatid cyst, it is called a hydatidiform mole or vesicular mole.
When the chorionic villi transforms into a mass of translucent vesicles, it forms a bunch-like structure called a hydatidiform mole.
Type of vesicular mole
There are two types of vesicular mole:
1) Complete Mall,
2) Incomplete Mall
1) Complete Mall:
Complete or classic H. mole forms when fertilization occurs in an egg whose nucleus has been lost and inactivated.
In this the mole resembles a bunch of white grapes.
In this case, the fluid-filled vesicles grow rapidly, causing the uterus to become larger than the expected duration of pregnancy.
Complete mole involves the fetus, placenta and amniotic membrane.
A complete mole can also progress to carcinoma and does not contain an embryo.
2) Incomplete Mall
These contain embryonic or fetal parts and an amniotic sac is present.
Congenital anomalies are present in these.
These contain underdeveloped embryos that fail to survive.
c. Hyperemesis graviduram –
Severe type of nausea and vomiting in pregnancy which adversely affects the health of the mother including dehydration, weight loss and electrolyte imbalance of the mother and also impairment in the daily routine activities of the mother is called “hyperemesis gravidarum”.
Hyperemesis gravidarum (HG) usually occurs more frequently during the first trimester of pregnancy, usually starting around 4–6 weeks of pregnancy and symptoms persist until around 9–13 weeks. This period corresponds to the time when pregnancy hormones, especially human chorionic gonadotropin (hCG), are at their highest levels. In most cases, the symptoms of hyperemesis gravidarum begin to improve by the end of the first trimester, although some women in severe cases may experience symptoms that persist into the second trimester or throw out pregnancy.
d. Decapitation –
Decapitation is a destructive delivery.
This type of destructive delivery is performed when the womb (uterus) itself has died and to expel the dead fetus from the womb through the vaginal canal in which some body of the dead fetus is removed. Parts are reduced. Due to which dead fetuses can be easily delivered from the birth canal.
In decapitation delivery, the head of the fetus that has died in the womb (uterine cavity) is cut from its trunk and then the fetus is delivered with the extraction of the trunk of the fetus. This procedure is called decapitation.
🔸 e. Tocolytic agent –
A tocolytic agent is a type of medication used to inhibit uterine contractions during pregnancy. This medication is used to delay pre-term labor and prevent premature birth.
A tocolytic agent is provided to stop or slow down temporary uterine contractions when a woman experiences preterm labor (uterine contractions starting before 37 weeks). Due to which other types of interventions can be taken like providing corticosteroids for maturation of the lungs of the fetus and transferring the mother to well equipped hospital facilities for the care of premature newborns etc.
Type of Tocolytic Agent:
1) Beta agonists: such as terbutaline which work to relax urinary smooth muscles.
2) Calcium channel blockers: such as nifedipine, these medications block the entry of calcium into the smooth muscles of the uterine cavity, thereby reducing uterine contractions.
3) Magnesium Sulphate: Magnesium Sulphate acts on motor and plate of cell membrane.
4) Prostaglandin inhibitors: eg, indomethacin
which reduces the synthesis of prostaglandin. and reduces uterine contractions.
5) Oxytocin Receptor Antagonists:
For example, atosiban, which blocks oxytocin receptors in the myometrium, also inhibits the entry of intracellular calcium and inhibits the release of prostaglidins, thereby inhibiting myometrial contraction.
Tocolytic agents can be administered I.V. or orally, which usually depends on the specific medication, clinical situation, gestational age, health of the mother, health of the fetus, and contraindications to the medication.
Thus, tocolytic agents play a crucial role in obstetric care by delaying premature birth and improving outcomes for both mother and baby in high-risk pregnancies.
🔸f. Precipitate labor –
Precipitate labor is called “rapid labor” and “rapid childbirth”.
Precipitate labor is that in which the total duration of the first and second stages of labor is less than two hours. Due to this, the infant is expelled rapidly and spontaneously.
It is commonly seen in multipara women.
Having a relaxed pelvic or perineal floor with multipara,
Multipara also has usefully strong, forceful contractions
And due to the painful sensation not being filled during labor, immediate birth is not reported due to which precipitated labor is seen.
🔸g. Genetic Counseling –
Genetics: The science dealing with heredity and variation is called genetics and the science of studying the structure and behavior of genes is called genetics.
Genetic counseling
Genetic counseling is a process in which family history and medical records are evaluated, genetic tests are ordered, and the results of these genetic tests are evaluated to help parents understand what decisions to make next. .
Genetic counseling is a process carried out by medical experts in which genetic tests are done and family history is taken and medical records are reviewed by experts with the aim of preventing parents from having any type of genetic disorder in their child. A genetic disorder can be identified whether or not there is a possibility of passing it on.
Genetic counseling provides education to parents about genetic disorders.
as well as psychological to them
Support is provided and information on support groups and services is provided.
The main aim of genetic counseling is to enable couples to make decisions for the future management of the pregnancy.
Its objectives include providing information, assisting in counseling, and helping couples adjust to problems.
Thus reducing the chances of birth of genetically defective babies is the main aim of genetic counselling.
h. Episiotomy –
A surgical plan incision is made over the perineum and posterior vaginal wall during the second stage of labor (2nd stage) called an “episiotomy”.
Episiotomy is performed to widen the vaginal opening for spontaneous or manipulative easy and safe delivery of fits.
An episiotomy is performed to reduce overstretching and rupture of the perineal muscles and fascia and to reduce stress and strain on the fetal head.
Type of episiotomy
There are generally four types of episiotomy viz.
1) Medio-lateral
2) Median
3) Lateral
4)’J ‘ Sep
1) Medio-Lateral: In this the midpoint of the forehand is placed downwards (downward) and outwards (outward) on the right or left side.
It is placed 2.5 cm centimeters away from the anus.
2) Median: In this the incision is started from the center of the forechit and extended posteriorly 2.5 cm in the midline.
3)Lateral: In this the incision is started 1 cm from the center of the forechit and extended laterally with the possibility of injuring the Bartholian gland.
4) ‘J’ Sep: In this the incision starts from the center of the forechit and 1.5 cm posterior to the midline and then downwards and outwards.
5 or 7 o’clock position is placed to avoid anal sphincter.
⏩Q-6 (A) Fill in the blanks. Vacancy filled 05
1) The fusion of ovum and sperm is called
(Fertilization).
2) TORCH stands for_——— Full form of TORCH——–
T: Toxoplasmosis O: Other (includes various infections such as syphilis, varicella-zoster virus, parvovirus B19, and hepatitis B or C) R: Rubella (German measles)
C: Cytomegalovirus (CMV)
H: Herpes simplex virus.
3) ———– means absence of menstruation. ————means absence of menstruation.
Amenorrhea (Amenorrhea).
4) Fully dilation of cervix during labor is —————– cm. Full dilatation of cervix during labor is——-cm.
10 cm
5) Discharge/Bleeding after delivery from uterus is called
Lochia
⏩(B) State whether the following statements are True or False. 05
1) Care should not be provided to the baby after immediate birth. X Baby should not be given any care immediately after birth.
False :-
(Reason := After the birth of the baby, it is necessary to provide immediate care to the baby for its health and well-being.)
2) The myometrium during pregnancy is called Decidua. ✓ Myometrium during pregnancy is called Decidua.
False :-
(Reason := Myometrium of uterus is a muscular layer which helps in uterine contraction during labor but during pregnancy endometrium (innermost layer) of uterus is called decidua.)
3) Quickening is a positive sign of pregnancy. ✓ Quickening is a positive sign of pregnancy.
True :-
4) During pregnancy mother gain 15 kg of weight normally. Generally, a mother gains 15 kilograms of weight during pregnancy.
False :-
(Reason := An average pregnant woman usually gains about 11 kg of weight during pregnancy which
During 1st trimester :=1 kg,
During 2nd trimester :=5kg,
During 3rd trimester :=5 kg, thus, total weight gain is 11 kg.)
5) Injection methargin used as a tocolytic agent in a delivery. Injection methargin is used as a tocolytic agent in delivery.
False :-
(Reason:= Methergine is not used as a tocolytic agent during delivery but Methergine is used after delivery to prevent the condition of post partum haemorrhage by increasing uterine contractions and preventing bleeding, on the other hand as a tocolytic agent. It inhibits uterine contractions and is used to prevent pre-term delivery.).
⏩(C) Write Multiple Choice Questions. 05
1) Golden color amniotic fluid indicated in Golden color amniotic fluid is seen in this
a) Polyhadramnios -Polyhydramnios
c) RH incompatibility – RH incompatibility
b) Feotal distress
d) All the above
2) Commonest site of fertilization of ovum is
2) Ampulla – Ampulla
b) Cornu of Uterus – Cornu of Uterus
c) Ovary
d) Interstitial Space – Interstitial Space
3) In Menopause female has not menstruated continuously for months
A female in menopause does not menstruate continuously for so many months
a) 3 months
b) 6 months
c) 9 months
d)-12 months
4) FHS audible with stethoscope after weeks of gestation
FHS is heard with a stethoscope after this week’s pregnancy
a) 10 to 12
b) 14 to 18
c) 16 to 18
d) 20 to 24
5) Hormone is responsible for male sex characteristics
The hormone is responsible for male sex characteristics
a) HCG – HCG
c) Progesterone – Progesterone
b) Estrogen – Estrogen
d) Festosterone – Testosterone
(C) Write Multiple Choice Questions.
Q: (1) Ans
(C)RH incompatibility-
(RH incompatibility).
Q: (2) Ans
(a)Ampulla.
Q: (3) Ans
d) 12 months.
Q: (4) Ans
c) 16 to 18
Q: (5) Ans
d) Testosterone
💪 💥☺ALL THE BEST ☺💥💪
Note :-MCQ ANSWER in unique pattern of APP in both languages is given below paper solution / click here. Clicking on “A” will change the language.
IF ANY QUERY OR QUESTION, REVIEW-KINDLY WATSAPP US NO. – 84859 76407
