ENGLISH GNM-T.Y-Midwif& Gynecological-31/08/2020 (DONE-upload-paper-no.2)
GNM-T.Y-Midwif& Gynecological-31/08/2020

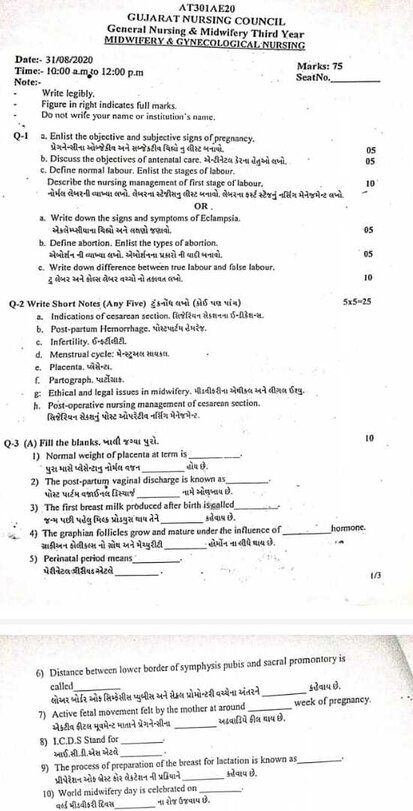
⏩Q-1
🔸 a. Enlist the objective and subjective signs of pregnancy, 05 Make a list of the objective and subjective signs of pregnancy.
List of objective and subjective signs of pregnancy:
First Trimester (1- 12(1-3 months) week):
Subjective Symptoms:
amenorrhea,
morning sickness,
Frequency of micturition,
breast discomfort,
fatigue
Amenorrhea:
Amenorrhoea in healthy married women during the reproductive period from 6 weeks after the last menstrual period is mostly due to pregnancy.
Morning sickness:
Most of the time the mother gets nausea and vomiting.
Frequency of Micturation:
In 8 to 12 weeks of pregnancy frequency of micturition is seen due to the pressure of the bulging uterus on the bladder.
Breast Discomfort:
Discomfort due to sensation of fullness in breast during 6 to 8 weeks.
Fatigue (feeling tired):
These symptoms are seen during early pregnancy and are experienced by many pregnant women.
Objective Sign:
breast changes,
Abdomen and Pelvic Changes on Changes,
Immunological test
Breast Changes:
Breast changes occur more clearly in primigravida.
These best changes happen during 6 to 8 weeks.
A delicate vein appears under the skin and the breast enlarges.
The nipple and primary areola are heavily pigmented.
Montgomery tubercle appears prominent.
And from 12 weeks of pregnancy, yellow secretion (colestrum) can be expressed.
On Abdominal Changes and Pelvic Changes:
On the abdomen:
The uterus is a pelvic organ until 12 weeks’ gestation and then the abdomen is felt as the suprapubic bulge (upper part) over the uterus.
Pelvic Changes:
These changes are varied and appear in different periods.
1) Jacquesmeier sign, Chadwick sign,
2) Vaginal sign (Ossander sign),
3) Cervical sign
(Goodell’s sign),
4) Uterine sign (Picksack sign),
5) Hagar sign,
6) Palmer’s sign.
1) Jackmier’s Sign:
The vaginal wall becomes hypertrophoid, edematous, and highly vascular.
Bluish discoloration of the vaginal mucosa due to increased venous blood supply to the vaginal wall is called Jacquemeier’s sign.
•> Chadwick Sign:
This sign is seen during the 8th week of pregnancy. Bluish discoloration of cervix, vagina and labia minora is seen due to local vascular changes. This is called “Chadwick’s sign”.
2) Vaginal sign (Ossander sign):
There is bluish discoloration of the anterior vaginal wall, anterior vaginal wall tenderness, and non-irritating mucoid discharge at 6 weeks.
It also has a palpation fill through the lateral fornix during 8 wks called “Ossander’s sign”.
3) Cervical sign
(Goodell Sign):
Cervical sign is observed during 6 weeks of pregnancy.
In which cervix is vacuolar, oedematous and hyperthyroid and hyperplasia.
Where the cervix becomes soft is called “Goodell’s sign”.
4) Uterine sign:
Size, Sap and Consistency:
6 The uterus is as large as a hen’s egg,
8 wickets equal to a cricket ball,
And 12 wicks are equal to the head of a fettle.
The pyriform sap in the nonpregnant stage of the uterus becomes globular during 12 weeks. The uterus becomes soft and elastic.
Piscak Sign:
If lateral implantation occurs in the uterus, symmetrical enlargement of the uterus may occur. This is called the “piscsec sign”, where one half is firmer (stronger) than the other.
5) Hagar Sign:
Hegar’s sign is seen at 6-10 weeks.
In which the upper body part of the uterus is enlarged due to growing fitters.
Lower segment of uterus becomes soft due to increased vascularity.
It causes cyanosis and softening of the cervix called “Hagar’s sign”.
6) Palmer Sign:
Palmer’s sign consists of regular and rhythmic contractions of the uterus on bimanual examination of the uterus from 4 to 8 weeks. It is called “Palmer’s sign”.
Immunological Test for Diagnosis of Pregnancy:
A pregnancy test depends on the presence of antigen (HCG) in maternal urine or serum.
Ex: Agglutination inhibition test
One drop of urine is mixed with one drop of human chorionic gonadotropin (HCG) antibody solution.
If human chorionic gonadotrophin is not present in the urine (the woman is not pregnant), the antibody will be free.
Now taking one drop solution containing latex particles coated with human chorionic gonadotrophin,
If agglutination occurs, the pregnancy test is negative.
Human chorionic gonadotrophin (HCG) binds to available antibodies when present in urine. Now administration of one drop solution containing latex particles coated with human chorionic gonadotropin trophin does not cause second agglutination as it binds the available antibody hence the pregnancy test is positive.
Ultrasonography:
Fetal viability and gestational age are determined by transvaginal sonography.
Second Trimester (13 to 28 weeks (4-7 months)):
Subjective Symptoms:
Often there is nosia, vomiting and frequency of micturition and amenorrhea is continuous.
New features appear such as quickening (women feel active fetal movement).
It usually occurs at 18 weeks i.e. about two weeks in advance in Multipara which gives accuracy to calculate the expected date of delivery.
A progressive enlargement of the lower utrust takes place.
Objective Symptoms:
1) General Examination,
2) Abdominal examination,
3) Vaginal examination,
4) Investigations.
1) General Examination:
a) In close: 24th week pigmentation is visible on forehead and cheek.
b) Breast Changes:
Breast enlargement with prominent veins.
Secondary areola appears during 20 th week.
16 th wk colostrum is thick and yellowish.
Striae are seen in varying degrees with advanced wicks.
2) Abdominal Examination:
a) Inspection,
b) Palpation,
c) Auscultation,
a) Inspection:
Linea nigra (brownish color pigmented line appears from symphysis pubis to encyform cartilage) from 20th week onwards.
The stria gravidarum is seen on the lower abdomen
b) Palpation:
Fundal height increases,
16 th week is the height of the uterus between the symphysis pubis and the umbilical.
At the 24th wick is at the umbilical level.
The uterus feels soft and elastic.
Uterus becomes ovoid shape.
Breakstone Hicks contractions occur.
Active fetal movement is felt from 20th week.
External balloting takes place from 20 th vic.
c) Auscultation:
18-20 wk fetal heart sound is heard with ordinary stethoscope. Its sound is like the tick of a watch, its location is according to the position of the fit, the rate is 110 – 160 / minute.
Vaginal Examination:
Bluish discoloration of the vulva, vagina and cervix occurs and the cervix is soft.
Internal balloting takes place during 16 to 18 weeks.
Investigations:
Sonography:
Routine sonography is performed between 18 and 20 weeks to assess fetal anatomy, placental site, and cervical canal integrity.
Radiography:
Radiography is done during the 16 th week in which the fetal skeletal shadow is visible.
Last/Third Trimester (29-40 Weeks/7-9 Months):
Subjective Symptoms:
amenorrhea,
feel tired,
Litigation (ie descent of the presenting part of the fetus into the lower uterine segment).
Resumption of frequency of micturition.
Increased fetal movement.
Objective symptoms:
Cutaneous changes become more prominent with increased pigmentation and striae.
Uterine sap changes from cylindrical to spherical after 36th week.
Fittal movement is easily filled.
Fundal height is as follows:
1) At 32th week: Fundal height at 32 weeks is seen up to the junction of upper and middle third.
2)At 36th wk: Fundal height comes up to encyform cartilage.
3) At 40 th wick:
Due to the engagement of the fitus, the fundal height comes up to a fundal height of 32 weeks.
The lie, presentation and position of the fetus can be determined by palpation of the fetal parts.
A fetal heart sound is audible.
Sonography can assess the growth of the fitus.
Assessment of amniotic fluid volume.
Fittal movement fills more.
b. Discuss the objectives of antenatal care, write the objectives of antenatal care. 05
Objectives of antenatal care:
The objectives of antenatal care are to improve the overall health of the fetus and the mother and to improve the well-being of the mother and the fetus and to prevent complications is a main aim.
1) Monitoring maternal health
Regular health checkups can monitor the mother’s overall health, such as blood pressure, weight gain, and overall well-being, etc., so that early identification of any complications can be done. And by treating it early, it can be prevented from happening further.
2) Monitoring fetal health
In antenatal care, assessment of the fetus including ultrasound scan, fetal heartbeat monitoring, and other tests can be done properly due to which the growth and development of the fetus can take place properly. If the child has any abnormality, it can be detected early and properly managed.
3) Health Education
Antenatal care provides an opportunity for appropriate education to expectant mothers, including pregnancy, child birth, breastfeeding, nutrition and parenting. This education can be helpful to the antenatal mother in making proper decisions.
4) Early detection of pregnancy related complications for proper management.
By visiting antenatal care, early detection of pregnancy related complications can be done and its timely management can be done. like,
gestational diabetes,
Preeclampsia, infection and other pregnancy related risks that can affect the pregnancy.
5) Preparation for Childbirth
Birth planning, preparation for labor, and delivery options are discussed in antenatal care sessions. By having this discussion, the mother and her family members can mentally and practically prepare for child birth.
6) Psychological support
Emotional and psychological changes are seen due to pregnancy. Antenatal care provides a supportive environment in which the expectant mother can discuss her anxiety, fear and doubts and clear them and reduce her anxiety and fear and feel emotionally well-being.
7) Prevention and Management of Maternal and Infant Complications
Antenatal care interventions include immunization, iron and folic acid supplementation, and preventive treatment to prevent pregnancy and childbirth related risks and complications.
8) Promotion of healthy behavior
Antenatal care provides education to promote behaviors such as smoking cessation, alcohol and drug avoidance, maintaining a balanced diet, and being physically active, which are important for healthy pregnancy outcomes.
9) Postpartum planning
Post-partum care is also discussed in antenatal care in which, post-partum care,
Breast feeding support and family planning options are discussed.
The objectives of overall antenatal care are to have a healthy pregnancy, properly manage any risks and complications, prepare the mother for child birth, and properly maintain the health of the mother and fetus during the throwout pregnancy.
c. Define normal labor. Enlist the stages of labor. Describe the nursing management of first stage of labor. 10 Write the definition of normal labour. List the stages of labour. Write the nursing management of fuscat stage of labour.
Normal Weber’s definition,
List of stages of labour,
Nursing Management of the First Stage of Labour:
Labor:
The series of events that take place in the genital organs to bring out the viable product of conception into the outer world through expulsion from the uterus (womb) is called “labour”.
A woman who is in labor is called a “parturient”.
And
The process of giving birth is called “Parturization”.
Normal labor is also called eutoshia.
Normal labor is said when the following criteria can be fulfilled.
1) The onset of labor should be spontaneous and at term (37 to 48 weeks).
2) Vertex presentation of fitus (the occiput of the head of the fitus is in the lower part of the uterine cavity and the chin of the fitus is tucked with its chest).
should be.
3) Duration of labor should not be long (ie if primary gravida mother then average duration of labor should be 12 hours and if multipara mother then average duration of labor should be 6 hours)
4) Birth should be natural with minimum assistance.
5) There should be no complications affecting the health of mother and baby.
••> List of Stages of Labour:
The stages of labor are divided into four stages.
1) First Stage of Labour,
2) Second Stage of Labour,
3) Third Stage of Labour,
4) Fourth stage of labor
••>1) First Stage of Labor (Cervical Stage):
The first stage of labor is the initial phase of childbirth. In which the cervix gradually opens (dilate) and thins (effacement). Due to this, the baby can pass from the uterine cavity into the birth canal (vagina). In which regular and rhythmic uterine contractions are seen and the frequency, intensity and duration of uterine contractions gradually increases.
The first stage of labor starts with true labor pain and lasts until full dilatation of the cervix (10 cm). This stage is also called “cervical stage”.
The first stage of labor is further divided into 3 stages:
First Stage No Time Period:
Primigravida:=12-16 hours, and
Multigravida:=6-8 hours, no.
The first stage of labor is divided into three phases.
1) Latent Phase,
2) Active Phase,
3) Transitional phase
1) Latent Phase,
-The latent phase is known as “prodomal labor” or “pre-labor”.
-Cervical dilatation of 1-4 cm centimeters occurs in this stage.
- Contractions in this phase are repeated every 15-30 minutes and last for 15-30 seconds. – Mother is talkative in this phase.
2) Active Phase,
-Active phase is also known as dilatation phase.
- In this second phase, the cervix dilates by 5-7 centimeters. -Then contractions are repeated every 3-5 minutes and last for 45-60 seconds. -In this stage mother feels restlessness.
3) Transitional phase
In the transitional phase, the dilatation of the cervix is 8-10 cm.
Contractions are repeated every 2-3 minutes and last for 60 to 90 seconds.
The first stage of overall labor is the critical period in which, after the cervix opens, the uterus prepares for delivery by providing the proper position of the baby in the uterine cavity. Continuous monitoring by health care providers is important to improve the condition and well-being of mother and fetus during this stage.
2) Second Stage of Labor (Expulsion of Fits):
The period from full dilatation of the cervix to the birth of the baby through the birth canal is called the second stage of labor.
its duration,
In primi gravida: 1-2 hrs
In multigravida: 20-30 minutes.
The second stage of labor is further divided into two phases:
1) Propulsive phase,
2) Explosive phase.
1) Propulsive Phase:
The propulsive phase starts from full dilatation of the cervix until the presenting part of the fitus descends to the pelvic floor (+4 +5 stations).
2) Explosive Phase:
This is the expulsive phase until the baby is completely expelled from the uterine cavity along with the mother’s bearing down efforts.
3) Third Stage of Labor (Expulsion of Placenta):
This stage is the period from the expulsion of the baby to the expulsion of the placenta and membranes is called the third stage.
Its time duration is 15 minutes in primi gravida and multigravida
4) Fourth Stage of Labor (Observation Stage):
The observation stage after the birth of the baby is called the 4th stage of labor. During this stage, the general condition of the mother and the condition of the newborn and the behavior of the uterus are carefully monitored.
Its time duration is 1 hour.
Thus, the time duration of all four stages of total labor (1st stage + 2nd stage + 3rd stage + 4th stage) is 13-15 hours in primigravida and 6-8 hours in multigravida.
••>Nursing Management of First Stage of Labour:
The first stage of labor is the critical period in which, after the cervix opens, the uterus prepares for delivery by providing the proper position of the baby in the uterine cavity. Continuous monitoring by health care providers is important to improve the condition and well-being of mother and fetus during this stage.
Nursing management of the first stage of labor involves the involvement of comprehensive care. Its aim is to support the mother physically, emotionally and educationally and the progress of labor.
1) Assessment
Properly monitor the progress of labor, condition of mother and also condition of fetus.
Inquire about when the labor pains started.
Any kind of liker should be inquired whether there is leakage or not.
Proper examination of the mother.
Perform proper obstetric examination.
Vaginal examination of the mother.
To properly check the antenatal records of the mother.
Maternal Assessment
Regular monitoring of the mother’s vital signs, such as
temperature,
pulse,
Respiration,
And to assess blood pressure properly.
To properly assess the intensity, frequency, duration, and resting tone of uterine contractions of pregnant women by palpation method.
Properly assess cervical dilatation and effacement by pervaginal examination.
Properly and accurately documenting and charting cervical dilatation and effacement.
Fetal assessment
Continuous monitoring of fetal heart rate by electronic fetal monitoring (EFM).
Properly assess the fetal heart rate pattern.
Proper documentation of fetal heart rate and any abnormality should also be properly documented.
2) Support and comfort measures
Providing a properly comfortable position to the mother due to which the comfort level of the mother can also increase and the labor process can also progress like walking, standing, sitting etc.
Advising the mother on relaxation techniques such as deep breathing exercises, and mind diversional therapy etc.
Provide emotional support, reassurance and psychological support to the mother to reduce her anxiety.
3) Hydration and nutrition
Advise the mother to have moderate fluid intake.
Continuously monitor the mother’s intake output chart to properly maintain the mother’s hydration status.
Advise the mother to take adequate amount of light food and take plain food to maintain the nutritional status of the mother.
Like plain water,
Salty Lemon Water,
Soup, and fruit juice etc.
4) Antiseptic and aseptic
Applying proper antiseptic dressing on the genital area, due to which cleanliness can be maintained.
5) Education and Communication
To provide education to mother and her supporters about mother’s condition and progress of labour.
6) Care of Bowel
Provide proper enema to clear mother’s bowel and increase uterine contractions.
7) Care of Bladder
Advise pregnant women to empty the bladder frequently as a full bladder inhibits contracture.
8) Documentation
After assessing the condition of the mother and fetus, properly document it and maintain the partograph properly.
Properly documenting all assessments, interventions, observations, in the mother’s medical record.
Properly record maternal vital sign, uterine contraction pattern, cervical dilatation and effacement, fetal heart sound and labor progress.
9) Collaboration and Advocacy
Collaborating with other health care personnel such as obstetricians, midwives and nurses to properly communicate the condition of the mother’s labor and take decisions about the condition of the mother.
Thus, by properly managing the first stage of labor, complications in the mother and fetus can be prevented and the first stage of labor can be properly maintained.
🔸OR🔸
🔸a) Write down the signs and symptoms of Eclampsia. 05 Mention signs and symptoms of eclampsia
Symptoms and signs of eclampsia:
The symptoms and signs of eclampsia are divided into four stages:
1) Premonitoring stage (30 seconds),
2) Tonic stage (30 seconds),
3) Clonic stage (1 to 4 minutes),
4) Stage of coma
1) Premonitoring Stage (30 seconds):
In this patient is unconscious,
There is twitching of the muscles of the face, tongue and limbus,
The eyeball is rolled, turned to one side and then fixed.
This stage lasts for 30 seconds.
2) Tonic Stage (30 seconds):
This test In this stage the whole body goes into a tonic spasm,
Trunk = opisnotonys (abnormal body posture in which the head, neck, and spine are tilted backward.)
Limbus = Flex,
hand = clenched,
Respiration stops and the tongue protrudes between the teeth.
Cyanosis is seen,
The eyeball is fixed,
This stage lasts for 30 seconds.
3) Clonic stage (1 to 4 minutes):
All voluntary muscles undergo alternate contraction and relaxation,
Twitching starts from the face and involves the extremities of one site,
Tongue bites,
Breathing stearatorius,
A mouth full of blood-stained frothy secretions,
Cyanosis is gradually reduced,
Respiration is labored and noisy,
Temperature increases by 40°C due to fits.
This stage lasts from 1 to 4 minutes.
4) Stage of Coma:
After a fit, the patient goes into a coma stage that lasts from a few minutes to a few hours.
Deepcoma remains until another convulsion occurs.
In this the patient is seen in a state of confusion after a convulsion and the patient does not remember what happened to him.
If the fits occur consecutively, it converts to status epilepticus.
b. Define abortion. Enlist the types of abortion. 05 Write the definition of abortion. List the types of abortion.
Definition of Abortion,
Types of Abortion.
Definition of Abortion:
Abortion is a process in which pregnancy is terminated. In abortion, the product of conception is partially and completely separated and expelled from the uterine wall before the age of viability (28 weeks). This condition is called “abortion”.
Abortion if it occurs spontaneously is called “miscarriage” and if induced abortion is called “induced abortion”.
Majority abortions or miscarriages occur during the first trimester of pregnancy i.e. during the first 12 weeks of pregnancy, then it is called “early miscarriage”. And the miscarriage that occurs after 13 weeks of pregnancy is called “late miscarriage”.
Enlist the types of abortion:
The types of abortion are as follows.
1) Spontaneous abortion
A) Threatened abortion,
B) Inevitable abortion,
C) complete abortion,
D) Incomplete abortion,
E) Silent or missed abortion,
D) Septic abortion,
E) Recurrent abortion or habitual abortion,
2) Induced abortion
••>1)Spontaneous Abortion:
When abortion occurs naturally without any medical or surgical intervention, it is called spontaneous abortion. Its cause can be any genetic abnormality and maternal condition.
A) Threatened Abortion:
In threatened abortion, the process of abortion starts but the abortion does not reach the point where recovery is impossible, i.e. recovery can take place if proper care is taken.
B) Inevitable Abortion:
Inevitable abortion is a type of abortion in which the expulsion of the conceptus progresses with cervical dilatation. In this case, the pregnancy cannot be saved because most of the portion of the placenta is detached (from the uterine wall).
This is a clinical type of abortion in which the abortive changes have progressed to the point where continuation of the pregnancy becomes impossible.
C) Complete Abortion:
Complete Abortion A type of abortion in which the product of conception is expelled in the form of mass is called complete abortion.
D) Incomplete Abortion:
Incomplete abortion is a type of abortion in which the entire product of the conceptus does not exit the uterine cavity but a small part of it remains in the uterine cavity, then this abortion is called incomplete abortion.
E) Silent or Missed Abortion:
Silent or missed abortion is said when the fetus has died in the uterine cavity and is retained in it for more than 4 weeks, then this abortion is called silent or missed abortion.
D) Septic abortion:
When the abortion is accompanied by evidence of infection of the uterus and its contents, i.e. the abortion is due to any infection, the abortion is called a septic abortion.
E) Recurrent Abortion or Habitual Abortion:
When three or more spontaneous abortions occur in sequence before 20 weeks, it is called recurrent abortion.
Other causes include immunoglobulin G, hormonal deficiency, and cervical incompetence.
genetic factor,
infection,
Also caused by endocrine and anatomical abnormalities.
2)Induced Abortion:
Induced Abortion means any medical or surgical procedure to terminate a pregnancy at will is called induced abortion.
Medical Abortion:
A medical abortion involves the use of medication to terminate a pregnancy and
Medical abortion is effective up to 10 weeks of pregnancy.
Ex:= combination of Mifeprostone and misoprostol.
Surgical Abortion:
It involves performing a surgical procedure by health care personnel and terminating the pregnancy. It is called surgical abortion Ex: vacuume Aspiration.
Thus, the types of abortion are classified as follows
c. Write down the difference between true labor and false labor. 10 Write the difference between two labor and false labor.
Difference Between True Labor and False Labour:
1) Uterine contraction:
True Labour:
Contractions are always present.
Contractions are regular and increase in frequency, intensity and duration.
Its duration is up to 60 seconds.
It causes abdominal tightening (hardening of uterus), discomfort or pain.
The discomfort starts from the back and starts in the abdomen.
Walking increases the intensity of contractions.
The pain caused by it is not relieved by enemas or sedatives.
False Labour:
Uterine contractions are not always present in false labor.
It has irregular and inefficient uterine contractions.
Its time duration is for three to four minutes.
The contractions are not painful every day and the uterus is not hard.
The discomfort is primarily in the abdomen.
Its contractions can be relieved by walking.
Pain is relieved by providing it and sedatives.
2) Cervix
True Labour:
There is effacement and dilatation of the cervix.
False labor
Cervical changes are not seen in it.
3) Membrane:
True Labour: Tenses fill during contractions and a ‘bag of water’ is formed.
False labour: Tense does not fill and ‘bag of water’ does not form.
4) show:
True Labour: True Labour’s ma show is mostly present.
False Labour: False Labor is not a show to watch.
5) Fits:
True Labour: Fits a progressive descent in it.
False labor: in which the fitus does not descend progressively.
⏩Q-2 Write Short Notes (Any Five) 5×5=25
🔸 a. Indications of cesarean section,
Indications for caesarean section are divided into two categories:
1) Absolute, (in which vaginal delivery is not possible)
2) Relative (in which vaginal delivery is possible but risks to mother and baby)
1) Absolute, (in which vaginal delivery is not possible):
Central placenta previa,
Severe degree contracted pelvis,
Cervical or broad ligament fibroids,
Vaginal atresia/obstruction,
In advanced cervical carcinoma,
Cephalopelvic Disproportion,
Obstruction due to pelvic mass,
Fits a death.
2) Relative (where vaginal delivery is possible but risks to mother and baby):
Cephalopelvic Disproportion,
contracted pelvis,
Prevous cesarean delivery,
Fital Distress,
Abnormal uterine contractions,
large feet,
small pelvis,
fail induction,
Antepartum haemorrhage eg, placenta previa, abruptio placenta.
Malpresentation or abnormal lie (transverse lie).
Bad Obstetric History,
Hypertensive disorders such as preeclampsia,
Prolapse of umbilical cord,
Elderly primigravida,
Medico-gynecological disorders:
chronic hypertension,
chronic nephritis,
diabetes,
heart disease,
pelvic tumor,
vaginal atresia,
Carcinoma of cervix,
Cervical dystocia.
Common Indications of Cesarean Section
1) Failure to Progress in Labour:
Prolonged labor in which the cervix does not dilate properly and the placenta does not descend properly in the birth canal, which necessitates a caesarean section.
2) Fetal Distress:
Signs that the fetus cannot tolerate labor properly, such as an abnormal fetal heart rate, indicate a reduced oxygen supply to the fetus, necessitating a cesarean section.
3) Malpresentation of Baby:
When the baby is in breech presentation (buttocks as presenting part), transverse position, vaginal delivery is impossible and caesarean section is required.
4) Placental abnormality:
Placenta previa:
In which the placenta is partially and completely implanted on the lower uterine segment i.e. when the placenta is present as the presenting part.
Abruptio placenta
In which, if the patient prematurely separates from the uterine wall, there is a need for caesarean section.
5) Maternal health condition
such as genital herpes,
heart disease,
severe hypertension,
condition like
6) Previous Caesarean Section:
If first caesarean section is done then repeat caesarean section depends on scar of privy cs and time duration of pregnancy.
7) Multiple Pregnancy:
When there are multiple pregnancies such as twins, triplets and based on the presenting part and position of the fetus, there is a need for caesarean section.
8) Umbilical cord prolapse:
In which the umbilical cord slips down through the cervix due to which the blood supply to the fetus is likely to be cut off.
9) Maternal Request:
In some cases, due to any personal or psychological reason, the mother herself selects caesarean section.
10) Emergencies during Labour:
Complications during labor such as uterine rupture, severe bleeding, and maternal illness necessitate an immediate caesarean section to protect the health and safety of the mother and baby.
Thus, in all these conditions there is a need to perform caesarean section.
b. Post-partum Hemorrhage
Postpartum haemorrhage is a condition that occurs from the birth of the baby to the end of the periperal period (after birth of baby up to 6 weeks period) from the genital tract in excessive amount which adversely affects the general condition of the mother. In which pulse rate increases as evidence and blood pressure falls down. So this condition is called Post Partum Haemorrhage (PPH).
If 500 ml or more after vaginal delivery,
1000 ml or more after caesarean section,
and ,
If there is blood loss of 1500 ml or more after caesarean hysterectomy, the condition is called post partum haemorrhage (PPH).
•>Types of Post Partum Haemorrhage (PPH).
There are two main types of postpartum hemorrhage:
1) Primary Postpartum Haemorrhage,
2) Secondary post partum haemorrhage.
1) Primary Post Partum Haemorrhage:
Bleeding that occurs within 24 hours after the birth of the baby is called primary postpartum hemorrhage, most often occurs in the first two hours after delivery.
It has two other types:
a) Third stage hemorrhage
b) True post partum haemorrhage
a) Third stage haemorrhage:
Third stage hemorrhage occurs before the placenta is expelled.
b) True post partum haemorrhage:
True postpartum hemorrhage occurs within 24 hours after the expulsion of the placenta.
2) Secondary post partum haemorrhage:
Bleeding in the peripartum period (occurring up to 6 weeks) after 24 hours after the birth of the baby is called delayed periperal hemorrhage, late periperal hemorrhage, or secondary postpartum hemorrhage.
•>1) Primary Post Partum Haemorrhage:
Bleeding that occurs within 24 hours after the birth of the baby is called primary postpartum hemorrhage, most often occurs in the first two hours after delivery.
It has two other types:
a)Third stage hemorrhage
b)True post partum haemorrhage
a) Third stage haemorrhage:
Third stage hemorrhage occurs before the placenta is expelled.
b) True post partum haemorrhage:
True postpartum hemorrhage occurs within 24 hours after the expulsion of the placenta.
Etiology of Primary Postpartum Haemorrhage:
1) Atonic uterus,
2) Traumatic,
3) Retained tissues,
4) Blood coagulation disorder.
1) Atonic uterus:
Up to 80% of postpartum hemorrhage is caused by an atonic uterus.
In it, the uterine sinus ruptures after the separation of the placenta, due to which the uterine muscles do not properly contract and retraction, the building continues continuously, which can lead to the condition of post-partum haemorrhage.
It is seen in the following conditions:
grandmultipara,
multiple pregnancy,
hydroamnios,
Due to over distension of uterus in large baby,
Malnutrition and anemia,
Antepartum haemorrhage, prolonged labour,
anesthesia,
have used oxytocin for induction or augmentation of labour,
Due to malformation of uterus,
Uterine Fibroids,
The third stage of labor is not properly managed,
Retained placenta
2) Traumatic:
Up to 20% of post partum haemorrhage (PPH) is bleeding after operative delivery in the genital tract after delivery and involves the cervix, vagina, perineum, periurethral region and rupture of the uterus.
3) Retained tissues:
Due to placental bits and blood clot remaining in the uterus, the condition of postpartum hemorrhage can occur.
4) Blood Coagulation Disorders:
Abruptio placenta, jaundice, thrombocytopenic purpura, HELLP syndrome, intra uterine death or sepsis.
Signs and Symptoms of Primary Postpartum Hemorrhage:
Vaginal bleeding is mostly external.
Effects due to blood loss depend on the predelivery hemoglobin level, the degree of hypervolemia, and the rate of blood loss.
Changes in the mother’s vitals, i.e. blood pressure, are seen after a blood volume loss of 20 to 25%. Rarely, rapid blood loss results in death within minutes.
On Abdomen Uterus:
Contracted in traumatic hemorrhage and flabby and massaged in atonic hemorrhage.
Management of Primary Postpartum Haemorrhage:
Postpartum hemorrhage is a major cause of maternal morbidity and mortality and is not always preventable but its incidence can be reduced by identifying risk factors.
Measures to prevent post partum haemorrhage:
Antenatal:
To improve the health status of women and make efforts to prevent anemia.
Delivery of high risk multipara in well equipped hospital.
Getting the blood group of each patient done.
Ultra sonography of previous cesarean delivery KM. R. I. By looking at the location of the placenta, placenta accreta can be detected.
Delivery in morbid adherent placenta to a senior obstetrician.
Intranatal:
Active management of the third stage can reduce postpartum hemorrhage by approximately 60%.
If induction or augmentation of labor is done with oxytocin, oxytocin infusion should be given to the athlete for one hour after delivery.
Observe for utero vaginal canal trauma after delivery in difficult labor or instrumental delivery.
After delivery, observe for about two hours to check whether the uterus is hard and contracted, and then send to the ward.
Administer local or epidural anesthesia in forceps, ventos or breech delivery.
Spontaneous separation and delivery of placenta in caesarean section.
Examination of placenta and membranes after delivery.
Antenatal Management:
Assessing the patient’s health status specially maintaining the patient’s hemoglobin level properly.
If the hemoglobin level is properly maintained, then any complications due to blood loss can be prevented.
Transfer the high risk mother to a well equipped hospital.
Intranatal Management:
Sedative and analgesic drug administration during internatal period.
Avoid Hasty Delivery After the baby’s head is delivered, it takes at least 2 to 3 minutes for the truck to deliver it.
Managing third stage care in high risk patients.
After the delivery of the placenta, properly assess whether the placenta has been delivered completely or not and assess whether any bits of the placenta are retained in the uterus or not.
Injection oxytocin is 10 unit / IM or if 20-40 unit oxytocin is added to 1000 ml of normal saline or Ringer lactate solution by infusion.
Exploration of the uterovaginal canal to note whether or not there is any trouma due to difficult labor or instrumental delivery.
Keep the athlete under observation for two hours after delivery of the patient.
Continuously note the mother’s vital signs during that time.
Nursing Management of Third Stage Building or True Postpartum Hemorrhage:
Calling health care personnel for extra health.
Intravenous cannula administration of two large doses.
Sending the blood to the laboratory for blood grouping and cross matching.
Adequate amount of intravenous fluid administration to the mother.
To note the vital sign of the mother properly.
If bleeding is due to an atonic uterus, gently rub the fundus with finger tips.
If soft and relaxed, gently massage the fundus in a circular motion so that the blood clots can be properly removed.
If bits of placenta or clots are retained in the uterine cavity, remove them properly.
Further repeat the injection oxytocin.
Administer methyl PGF2 intramuscularly or transabdominally into the myometrium to return the uterus to its tone and repeat as needed.
If the uterus is still atonic, perform manual compression.
Applying pressure on the placental side in manual compression can help control bleeding.
Tight intrauterine packing is performed under general anesthesia to control postpartum hemorrhage.
If the above measures fail then hysterectomy is done as a last option.
General Steps for Management of Postpartum Hemorrhage:
Starting intravenous therapy,
Catheterize the mother properly.
If necessary, start a blood transfusion.
To note whether the placenta has delivered properly and if the placenta has not delivered, to properly assess whether it is separated or unseparated.
Remove the placenta bimanually if the placenta has not separated.
If the placenta is undelivered but separated, assess where the placenta is present in the uterine cavity. That is, to assess whether it is present in the lower segment of the uterine cavity, in the part of the cervix or on the vagina.
If the placenta is present in the lower segment of the uterine cavity, remove it by controlled cord traction.
If control cold traction fails then perform bimanual compression and if that also fails then perform hysterectomy last.
If the separated placenta is on the cervix or vagina, grasp and remove it, if that fails, remove the placenta by bimanual compression and if that fails, perform hysterectomy last.
To properly remove retained bits of placenta in the uterine cavity if the placenta is delivered.
If placental clots cannot be removed, provide injection Syntocin 40 IU International Unit 1 Liter Intravenous Infusion. Due to which the patient’s clots can be removed.
Then complete vital sign assessment of the mother.
Provide a properly comfortable position to the mother and advise her to take proper rest.
To provide proper assurance to the mother.
2) Secondary post partum haemorrhage:
Bleeding in the peripartum period (occurring up to 6 weeks) after 24 hours after the baby’s birth is called delayed periperal hemorrhage, late periperal hemorrhage, or secondary postpartum hemorrhage.
The building in it can be done mostly during 8 to 14 days.
Etiology of Secondary Postpartum Haemorrhage:
If bits of cotyledon or membrane remain inside the uterine cavity,
Due to infection,
Due to endometritis,
If there is placental site subinvolution, due to
Due to caesarean section wound,
Due to estrogen therapy,
Due to carcinoma of the cervix,
Due to placental polyps,
Due to parietal inversion of uterus,
Signs and symptoms of secondary postpartum hemorrhage:
Heavy lochia discharge that appears bright red in color,
Local discharge being offensive,
fever,
Elevated pulse rate,
Subinvolution of uterus,
anemia,
sepsis,
Nursing Management of Secondary Postpartum Hemorrhage:
To properly assess the amount of blood loss.
To provide proper blood transfusion to the patient.
Properly identifying the causes of postpartum hemorrhage.
Administer 10 units of oxytocin IM (intracellular) or if intravenously (IV) to the patient by adding 20 units of oxytocin to 500 ml of normal saline or regurgitated solution to prevent post partum haemorrhage.
Provide proper antibiotic medication to the patient.
Advise the patient to take complete bed rest.
If the patient has any retained bits of placenta to remove it properly.
If the patient is bleeding even in a minor amount, do not ignore it as it can be an alarm symptom of post partum haemorrhage.
Properly remove retained product by sponge holding, ovum forceps or gentle curettage.
If bleeding is due to trauma to the cervicovaginal canal, control it with hemostatic sutures.
If the delivery of the patient took place in an unhygienic environment, then administration of anti-tetanus serum and anti-gangrene serum to the patient.
Provide blood transfusion if patient is anemic.
Properly monitor the patient’s vital signs including monitoring vital signs every four hours initially and then twice throughout the day.
Provide the patient with ferrous gluconate (300 mg TDS) or ferrous sulfate (200 mg TDS) orally.
Provide proper folic acid (5 mg) meditation to the patient.
To provide proper work and comfortable environment to the mother.
Advising mother to take proper follow up.
c. Infertility.
Definition:=
Infertility is a medical condition in which there is inability to conceive a pregnancy despite having regular and unprotected intercourse for 1 year or more, then such a condition is called infertility.
It affects approximately 10-15% of couples worldwide. Infertility can be due to various factors affecting male, female or both, and can be temporary or permanent.
Type of Infertility
There are generally two types of infertility.
1) Primary infertility,
2) Secondary infertility
1) Primary Infertility:
It is indicated for patients who have not been able to conceive a single pregnancy.
2) Secondary Infertility:
Thus, prior pregnancy indicates conception but subsequent failure to conceive is called secondary infertility.
Causes of Infertility
There are three main causes of infertility.
1) Fault in female,
2) Fault in Mail,
3) Combined factor.
1)Fault in Female:
A) Ovarian factor:
Ovulatory dysfunction is seen mainly for its three reasons as follows.
a) Anovulation/Oligoovulation:
Anovulation/oligoovulation is usually due to disturbances in the hypothalamopituitaryovarian axis.
Ovarian activity depends on gonadotrophin and normal secretion of gonadotrophin depends on GnRH (gonadotrophin releasing hormone) released from the hypothalamus.
(b) Lutenized unruptured follicle (LUF)
(Trapped Ovum):
This is seen due to inadequate growth and function of the corpus luteum.
(C) Trapped Uvam:
In this, the ovum is trapped inside the follicles, usually due to endometriosis or hyperproductemia.
2) Tubal Factors:
Infertility in this is usually due to tubopathy (tubal infection) due to which tubal functions are impaired.
Ex:= Defective ovum pickup followed by infertility.
3) Peritoneal factor:
One and the main factor of infertility is endometriosis.
4) Uterine factor:
These include certain factors that stop the implantation of the fertilized ovum into the endometrium.
These factors like,
a) Endometriosis,
b) fibroid uterus,
c)Uterine hypoplasia,
d) Congenital malformation of the uterus.
5) Cervical Factors:
In this due to second degree uterine prolapse,
Due to retroverted uterus,
And due to changes in the composition of the cervical nucleus.
6) Vaginal factor:
These include vaginal atresia,
Transverse vaginal septum, due to
2) Fault in Mail:
1) Due to defective spermatogenesis:
This leads to infertility and is usually due to the following:
orchitis,
undescended testes,
testicular toxins,
Primary testicular failure,
Due to genetic or chromosomal disorders such as, 47,XXY,
Due to endocrine factors such as thyroid dysfunction.
2) Obstruction of the efferent duct system due to:
These are found in two types.
1) Congenital:
As the vas deferens are absent.
2) Acquired:
This is usually due to some infection,
Occurs due to tuberculosis, gonorrhea, and surgical trauma (during herniorrhaphy).
3) Failure to deposit spam in Wajaina:
This is due to failure to deposit sperm in the vagina.
This is due to:
impotence,
Ejaculatory failure,
hypospadias,
Bladder neck surgery.
4) Due to error in seminal fluid:
Hence, due to immotile sperm,
Due to disturbance in sperm count,
Because of the low fructose count.
3) Combined Factor:
In this, infertility is seen due to the combined factors of both male and female.
Diagnostic Investigation:
Complete history collection and physical examination
This includes assessment of overall health, including reproductive health, history and identification of potential risk factors.
Ovulation Testing:
This includes monitoring the menstrual cycle and whether ovulation occurs regularly
Siemens Analysis:
In this, sperm count is evaluated and sperm size, morphology, and other parameters are assessed.
Imaging Testing:
This involves ultrasonography and hysterosalpingography to assess the uterus and fallopian tubes.
Hormonal test:
In this, hormonal levels are assessed to assess ovarian factor and other endocrine disorders.
Diagnostic Procedure:
For example, laparoscopy (to examine the affected organ), and genetic testing (to identify chromosomal abnormalities).
Treatment:
Treatment of infertility depends on its cause, duration and duration of infertility.
Medication
Fertility drugs are provided to stimulate ovulation in women and improve sperm production and function in men.
Surgery: Surgery is used to correct anatomical abnormalities such as tubal blockage, uterine fibroid, and varicocele (enlarged vein in scrotum).
Assisted Reproductive Techniques (ART)
Intra uterine insemination (IUI)
In this, sperm are placed directly into the uterine cavity during ovulation.
In Vitro Fertilization (IVF)
In this, the ovum and sperm are fertilized in the laboratory and then the embryo is transferred to the uterus.
Intra Cytoplasmic Sperm Injection (ICSI)
In this procedure, a single sperm is injected directly into the egg to cause fertilization.
Surrogacy
Surrogacy is done when it is not possible to carry the pregnancy to term.
General Nursing Management:
To take proper measures to improve the general health of the patient.
If the person is obese, give advice to reduce weight.
Advise the patient to avoid heavy smoking and alcohol.
Advise the patient to award tight and loose undergarments.
Advise the patient to take proper vitamin E, vitamin C, vitamin B12 and folic acid which improves spermatogenesis.
Provide proper psychological support to the patient.
Properly checking the patient’s body weight and calculating the body mass index which
Should be between 20-24.
Advising patients on proper stress management. In which giving advice to the patient to do yoga and meditation properly.
d. Menstrual cycle:
Definition:
Menstruation is derived from Mun. Menstrual cycle is a visible cyclical process of physiological changes in a fertile female that occurs in the endometrium of the uterus and through the interconnection of its hormones leading to vaginal bleeding. The HPO process
(H : hypothalamus,
P: Pituitary Gland,
O: Ovaris ) is caused by
H : Hypothalamus:
The hypothalamus secretes gonadotrophin releasing hormone (GnRH) which stimulates the anterior pituitary gland to release FSH (follicle stimulating hormone).
Stimulates to secrete LH(Luteinizing Hormone).
P : Pituitary Gland :
FSH (follicle stimulating hormone) from pituitary gland
LH (luteinizing hormone) is secreted. He works on Overies.
O: Overies:
Pituitary gland secretes FSH (Follicle Stimulating Hormone) which causes maturation of ovarian follicle, secretion of estrogen and ovulation.
While LH (Luteinizing hormone) promotes development of corpus luteum and secretion of progesterone.
Hormone secretion during the menstrual cycle is regulated by a negative feedback mechanism.
The hypothalamus responds to changes in blood levels of estrogen and progesterone. As hypothalamus is depressed by high blood levels of estrogen and progesterone while hypothalamus is stimulated by low levels of estrogen and progesterone.
The average length of menstruation cycle is 28 days.
Menstruation Cycle:
Menstruation cycle has two phases.
1) Ovarian phase
2) Uterine phase
1) Ovarian Phase:
Further two phases are involved in ovarian phase.
a) Follicular phase,
b) Luteal phase
a) Follicular phase:
The follicular phase starts from the first day of menstruation and ends with ovulation. This phase is usually up to 14 days.
In this phase follicles grow due to follicle simulating hormone (FSH).
One of these follicles (dominant follicle) becomes mature.
This mature follicle becomes the Graafian follicle. It releases estrogen.
Estrogen then acts on both follicle stimulating hormone (FSH) and luteinizing hormone (LH).
Estrogen suppresses follicle stimulating hormone (FSH) and stimulates luteinizing hormone (LH).
Then the luteinizing hormone (LH) ruptures the Graafian follicle which is formed from the dominant follicle and the ovum is released and then the work of the corpus luteum increases.
b) Luteal Phase:
The luteal phase is the cycle from ovulation to the start of the next menstrual cycle, usually lasting 14 days.
During this phase the corpus luteum develops, which forms from the remaining ovarian follicle after ovulation.
The corpus luteum produces progesterone that prepares the lining of the uterine cavity for implantation of a fertilized egg.
The luteal phase can have two possibilities:
I : Fertilization absent
II : Fertilization present
I : Fertilization absent
If fertilization is absent, the corpus luteum converts to the corpus menstrualis.
Corpus menstrualis converts to corpus albicans and then disappears on day 28.
II : Fertilization present
If fertilization is present, the corpus luteum converts to the corpus luteum verum, which also contains the hormone progesterone and lasts for three months.
Progesterone hormone suppresses the mother’s immunity, so growth of the fetus in the uterine cavity can occur and the condition of abortion is prevented.
2) Uterine Phase:
The uterine phase is further divided into three phases:
1) Bleeding phase (4 days)
2) Proliferative phase (10 days)
3) Secretarial phase (14 days)
1) Bleeding phase (4 days):
When the ovum is not fertilized, the increased level of progesterone hormone in the blood causes vasoconstriction of the blood vessels of the endometrium (innermost layer of the uterus).
Due to this, the blood supply to the endometrium layer of the uterine cavity decreases.
And the condition of hypoxia arises.
This causes necrosis and death of endometrium layer cells and tissues.
Now, due to necrosis and death of these cells and tissues, the condition of hematometra (collection of blood in the uterine cavity) arises.
Due to this condition the nerve supply goes to the hypothalamus where it stimulates the pituitary gland. The pituitary gland releases oxytocin which is responsible for causing uterine contractions.
Due to this uterine contraction, blood flow to the vaginal site becomes visible. And menstruation starts. It contains endometrial gland, endometrial cells, capillary blood and unfertilized ovum.
When the level of reduced progesterone reaches a critical level, the second ovarian follicle is stimulated by follicle-stimulating hormone (FSH) and the proliferative phase begins.
2) Proliferative phase (10 days):
The proliferative phase is also called the follicular phase.
In this stage, follicle simulating hormone (FSH) causes ovarian follicles to grow and mature to produce estrogen.
Estrogen stimulates the proliferation of the endometrium and prepares it to receive a fertilized ovum.
Thus the endometrium becomes thick (2 to 3 mm) due to rapid cell multiplication.
And due to the increase of mucus secreting gland and blood capillaries, at the end of this phase due to the effect of luteinizing hormone (LH), ovulation occurs and the production of estrogen decreases.
3) Secretarial Phase (14 days):
This phase is also called the luteal phase.
Immediately after ovulation, the lining cells of the ovarian follicle are stimulated by luteinizing hormone (LH) and form the corpus luteum.
Now this corpus luteum produces progesterone.
Due to the effect of this progesterone hormone, the endometrium of the uterine cavity secretes more mucus from the secretory gland and becomes edematous i.e. thick (5 to 6 mm) and the endometrium provides a favorable environment for implantation of the fertilized ovum.
Thus, the menstrual cycle is explained in two phases namely ovarian phase and uterine phase.
🔸 e. Placenta,
Introduction
Placenta is a mass like structure. It usually develops in the anterior or posterior side of the upper uterine segment from two sources namely fetal component chorion phrondosum and maternal component decidua basalis.
The placenta is connected to the fetus through the umbilical cord and the pregnancy is maintained. The placenta supports the life of the embryo by providing oxygen and food to the embryo and removing toxic materials.
Definition
The placenta has a “discoid shape” due to its septum.
It is “hemochorionic” because its chorion comes into direct contact with maternal blood, and it is “deciduous” because the placenta sheds off after birth.
Placenta origin
The placenta originates from the trophoblastic layer of the fertilized ovum.
The patient is closely linked to the mother’s circulation to properly perform functions that the fetus is unable to perform during intrauterine life.
The survival of the fetus depends on the integrity and efficiency of the placenta.
Attachment of placenta
The placenta is attached to the mother’s uterine wall and establishes a connection between the mother and the fetus through the umbilical cord.
Placenta at Fultma
At most the placenta is a disc-like spongy, fibrous structure that is flat and round or oval in shape. The placenta is thick in the center and thin at the edges.
Diameter and thickness of placenta
1)Average weight of placenta a:= 500 gm
2) Ratio between fetus and placenta := 1/6( 3kg / 500 gm).
3) Diameter of placenta a:= 15-20 cm.
4)Surface area of placenta:= 243 sq cm (square centimeter).
5) Volume of placenta A:= 500 ml.
6) Placenta is thick in the center while thin at the edges.
Center area of placenta:=2.5 to 3 cm.
Peripheral area of placenta := 1 to 1.5 cm
The umbilical cord connects the fetus to the placenta with an umbilical vein and
There are two umbilical arteries.
Part of placenta
The placenta has two surfaces.
1) Fetal surface (80%),
2) Maternal surface (20%)
1) Fetal surface (80%):
The fetal surface is smooth, sinuous and transparent, covered by a smooth and glistening amnion.
In which the umbilical cord is connected at the center.
Umbilical vessels are visible on this surface.
The fittal surface is bright red in color.
2) Maternal Surface (20%):
Maternal surface is “rough and spongy”.
It is dull red in color.
The maternal surface is divided into 15 to 30 cotyledons separated by sulci.
A small calcified infract appears on the maternal surface.
Structure of placenta
The placenta consists of two plates. The chorionic plate lies inward and is covered by the amniotic membrane. The umbilical cord is attached to this plate. On the maternal side there is a basal plate.
The intervillous space lies between the chorionic plate (fetal site) and the basal plate (maternal site).
In this intervillous space, the stem cell and its branches are located and the maternal blood is located in this space.
1) Amniotic membrane
Amniotic membrane is a single layer of cubical epithelium and connective tissues. And the amniotic membrane is loosely attached to the chorionic plate.
It has no part in placenta formation.
2) Chorionic plate
The chorionic plate is the seat of connective tissue. It contains branches of umbilical vessels. The chorionic plate is covered by the amniotic membrane at the fetal site.
Stem cells arise from the chorionic plate that forms the inner boundary of the choriodecidual space.
3) Basal plate.
The basal plate is formed from cytoblasts, syncytoblasts, and decidua basalis.
It is a compact and spongy layer.
A basal plate is present nearer the maternal surface.
The uterine artery and vein enter the intervillous space from the basal plate.
The basal plate forms the boundary at the maternal surface.
4) Intervillous space
It has a chorionic plate on the inner side and a basal plate on the outer side. There is a connection of two plates around.
Internally all sides are lined with syncytotrophoblasts and filled with slow flowing maternal blood.
In this intervillous space are the stem cells and their branches.
5) Stem branching
Stem cells arise from the chorionic plate and extend to the basal plate.
Primary, secondary and tertiary divisions are formed in progressive development.
The functional unit of the placenta is the fetal cotyledon or placentome. It is formed from major primary stem villus.
These major stem villi pass through the intervillous space and anchor in the basal plate. The functional subunit is called the lobule, which is formed from the tertiary villi.
There are about 60 stem cells in the human placenta. Hence each cotylodon (total :=15-20) has three to four major stem branches. Some villi anchor the placenta and some remain free in the intervalsal space called nutritive villi. The blood vessels in the villi do not connect with each other.
Circulation through the presenta
There are two types of circulation in the placenta.
1) Phyto Placental Circulation,
2) Uteroplacental circulation
1) Phyto Placental Circulation,
Two umbilical arteries in the phytoplacental circulation bring impure blood from the placenta and enter the chorionic plate, each supplying 1/2 of the placenta.
The arteries break into small branches and enter the stem of the chorionic villi, which divide into primary, secondary, and tertiary vessels. Maternal and fetal blood flow side by side in opposite directions.
Fetal blood flow is 400 ml/minute which is mainly due to the pumping action of the fetal heart rate. Blood from the umbilical artery delivers carbon dioxide to the placenta and absorbs oxygen and returns to the fetus through the umbilical vein.
2) Uteroplacental Circulation (Maternal Circulation)
In the uteroplacental circulation, uterine arteries and veins enter the intervillous space through the basal plate and transmit blood and nutrients from the mother to the intervillous space.
Function of placenta
1) Respiratory function
The fetus receives oxygen and excretes carbon dioxide through the placenta.
Just as oxygen from the mother’s blood passes into the fetal blood, carbon dioxide in the fetus is transmitted to the maternal blood through the placenta.
2) Nutritive function
All kinds of nutrients like amino acids, glucose, vitamins, minerals, lipids, water and electrolytes are transmitted from the mother to the fitters.
The food taken in the maternal diet reaches the placental side where it is converted into simple form, then the placenta selects the substances required by the fetus and transmits them to the fetus.
3) Storage function
Placenta stores glucose, iron and vitamins. And the placenta provides it when the fetus needs it.
4) Excretory function
The waste product in the fetus is transmitted to the placenta.
5) Protection
Placental membrane has limited barrier function. Some of the antibodies passed from the mother to the fetus provide immunity to the baby for up to three months after birth.
6) Immunological function
Antigens from the fetus and placenta act as foreign to the mother. However, graft rejection does not occur because the placenta provides immunological protection against rejection.
7) Hormonal function
steroid hormones
estrogen,
Progesterone.
Protein hormones
HCG (Human Chorionic Gonadotrophin),
HPL (Human Placental Lactogen),
relaxin,
PAPPA (Pregnancy Associated Plasma Protein:= A).
•>HCG (Human Chorionic Gonadotrophin),
HCG (human chorionic gonadotrophin) is produced from the cytotrophoblastic layer of the chorionic villi.
HCG (human chorionic gonadotrophin) is high during 7 to 10 weeks of pregnancy then decreases as the pregnancy progresses it maintains the corpus luteum.
HCG (human chorionic gonadotrophin) is used in pregnancy tests because it is excreted in the mother’s urine.
HCG (human chorionic gonadotrophin) is detected in blood on day 7 and urine on day 9 after fertilization, which indicates a positive pregnancy test.
••> HPL (Human Placental Lactogen)
HPL (Human Placental Lactogen) is produced from the placenta and is involved in lactogenic and metabolic processes of pregnancy. When the level of human chorionic gonadotropin trophin decreases, the level of human placental lactogen (HPL) increases and it continues in throwout pregnancy.
Human placental lactogen (HPL) works as an anti-insulin that increases blood glucose levels and helps supply glucose to the fetus.
••>Relaxin
Relaxin is produced by decidual cells. And it softens the cervix and helps the pelvic ligaments and symphysis pubis to relax the labor process.
••>PAPPA (Pregnancy Associated Plasma Protein:= A)
Pregnancy Associated Plasma Protein:= A works as an immunosuppressant and works to maintain pregnancy.
••> Estrogen
Estrogen is produced by the placenta in a throwout pregnancy. It is essential for welling of the phytoplacenta.
Estrogen increases during labour, which helps in the release of oxytocin, which increases uterine contractions.
••> Progesterone
Progesterone is produced from the synovial layer of the placenta which works as a tocolytic agent and prevents uterine contractions as well as works as an immunosuppressant to help maintain the pregnancy.
🔸f. Partograph,
Answer of partograph is in the next paper solution.
Paper: 13/09/2021,
No Q: 2 Write short notes answer to Q: (h).
🔸g. Ethical and legal issues in midwifery, midwifery ethical and legal issues.
Ethical and Legal Issues of Midwifery:
Ethical Issues of Midwifery:
1) Autonomy and Informed Consent:
Respect for Autonomy:
Midwives should respect women’s rights to make informed decisions about their care.
Informed Consent:
It is important to ensure that women understand their options, risks and benefits of the intervention.
2) Non Malefficiency (Do No Harm):
Midwives should strive to avoid actions that may harm the mother or child during childbirth.
3) Beneficence (promoting mood):
It is the duty of the midwife to actively promote the well-being of the mother and child during the process of pregnancy and childbirth.
4) Justice:
To provide adequate, equitable and proper health care facilities to all women irrespective of their socio-economic status and background.
5) Confidentiality:
Maintaining privacy and confidentiality of patient information is important in health care practices.
6) Cultural Sensitivity and Respect:
Midwives should be aware of and respect the cultural, spiritual and religious beliefs of the women they care for.
Legal Issues in Midwifery:
1) Problem in medication.
2) Failure and Inadequate Client Monitoring.
3) Failure to adequately assess the client.
4) Fair to report change in the patient.
5) Abortion.
6) Nursing Care of New Born.
1) Problem in Medication:
A nurse is authorized for the administration of medication with many medication-related allegations.
Ex: Improper client identification,
Failure to monitor the dose, time and side effects of meditation.
2) Failure and Inadequate Client Monitoring:
According to the condition of the client, the nurse has to monitor it at appropriate time intervals. In labor and delivery, they have to monitor both the client i.e. the mother and the baby. In the prenatal, natal and postnatal period to prevent complications in the mother and the child, their monitoring is done by the nurse. There is legal responsibility.
3) Failure to adequately assess the client:
Nurses should have higher level assessment skills in all specialty areas.
Proper assessment of the client’s health status such as prenatal assessment, fetal monitoring and assessment of labor progress is essential.
If there is failure to properly assess the client, complications are missed and inappropriate care is received by the patient.
4) Fair to report change in the patient:
When the nurse assesses the client’s condition and reports any changes in the client’s condition immediately to the consult physician. As a patient advocate, if the nurse fails to notify the doctor, the client gets delayed in getting care and the client may suffer injury and problems.
And there can be legal issues too.
5) Abortion:
Legal issues regarding the midwife’s role in abortion care can vary widely depending on local laws and regulations. This also involves the involvement of legality, informed consent and adherence to protocols.
A nurse has the right to refuse to assist in an abortion but not the right to stop it.
6) Nursing Care of New Born:
It is important to provide immediate nursing care of the newborn, which involves assessment of the newborn, proper monitoring, and proper stabilization of the newborn.
There are some legal requirements for providing nursing care to newborns such as properly identifying the infant-mother pair through finger prints, foot prints and wrist bands and taking blood samples for phenylketonuria (PKU) testing if applicable.
Providing a clear airway is standard of practice.
Camping of the umbilical cord.
Apply antibiotics.
Keeping the infant warm and minimizing stress in dressing etc.
Resuscitation equipment should be kept in the delivery room.
The nurse should keep records of all delivery events.
Fulfilling legal requirements through careful documentation in the delivery room.
When newborns are not provided with standard care, complications can arise and legal issues can also arise due to this.
🔸 h. Post-operative nursing management of cesarean section. Post-operative nursing management of cesarean section.
Postoperative Nursing Management of Cesarean Section:
First 24 hours (day 0):
Immediate Care
In the post operative management of caesarean section during the first day of caesarean i.e. 6 to 8 hours on the first day keeping the mother under proper close observation.
To properly monitor the mother’s vital signs on the first day such as,
Monitor the temperature every two hours,
pulse,
Respiration,
Monitoring blood pressure every 15 minutes,
etc. to note properly.
The wound should be properly inspected every half hour and ashed to see if any blood loss has occurred.
The amount of vaginal building means assessing the condition of the lochia and properly assessing the condition of the uterus.
Provide proper left lateral position to mother or provide recovery position.
Fluid:
Provide adequate amount of fluid to the mother.
Administer sodium chloride (0.9%) / Ringer’s lactate drips to the mother continuously up to 2-2.5 liters.
If the mother is anemic, provide adequate blood transfusion to the mother to improve post-operative recovery.
Maintaining patient no intake output chart.
Drugs:
Administer injectable oxytocin medication slowly 5 units IM/IV to the mother.
or providing methargine 0.2 mg IM as prescribed.
Providing prophylactic antibiotic medication to the mother in the first 48 hours after caesarean section.
Provide analgesic medicine to mother as ordered.
Ambulation:
If the mother’s general condition is good, she can sit in bed and even go to the toilet to empty her bowels and bladder.
Anchoring the patient to move legs and ankles and deep breathing.
In 3 to 4 hours when the mother is stable and her pain level is reduced, advise the mother to start breastfeeding the neonate.
Along with this, keep monitoring the baby’s vital signs and general condition and if any abnormalities are found, immediately refer them to a hospital with well-equipped facilities.
Second Day:
On the second day after caesarean section, provide oral feeding to the mother in the form of electrolyte, water and some tea.
Then advise the mother to provide adequate breastfeeding to the baby.
If for any reason the baby is not able to shake properly, then advise the mother to provide milk to the baby by manually expressing it.
Third Day:
Providing light solid diet to mother as per mother’s choice.
If the mother does not pass stool spontaneously and properly, then provide 4-6 teaspoons of milk of magnesia to the mother at bed time.
Or
Give 3-4 teaspoons of lactulose solution.
Six or Seventh Day: Skin stitches to be removed on day 6 to 7 of a cesarean section.
Discharge:
When the patient is discharged on the next day after removal of stitches, providing discharge advice such as taking adequate amount of nutrition, maintaining proper hygiene, and explaining the proper care of the baby.
⏩Q-3 (A) Fill the blanks -10
1) Normal weight of placenta at term is.
500 gm
2) The post-partum vaginal discharge is known as ——–
lochia.
3) The first breast milk produced after birth is galled.
Colostrum
4) The graphian follicles grow and mature under the influence of —– hormone. Growth and maturity of Graafian follicles is due to ——-hormones.
follicle-stimulating hormone (FSH).
(follicle stimulating hormone).
5) Perinatal period means ———- Perinatal period means———–
28 weeks of gestation to 7 days of life
6) Distance between lower border of symphysis pubis and sacral promontory is called ———- Distance between lower border of symphysis pubis and sacral promontory is called.
diagonal conjugate
(Diagonal Conjugate)
7) Active fetal movement felt by the mother at around ———– week of pregnancy. Active fetal movement is felt by the mother during the first trimester of pregnancy.
18-20 weeks.
8) I.C.D.S Stand for———– I.C.D.S stands for————
ICDS:
Integrated Child Development Services
9) The process of preparation of the breast for lactation is known as
Lactogenesis
10) World midwifery day is celebrated on ———— World midwifery day is celebrated on ————.
5th May
⏩B) State whether the following statements are True or False. 10 State whether the following statements are true or false
1) Puerperium period is following child birth up to 6 months. The period from birth to six months is called purperium period.
False
(Reason: The puerperium period, also known as the postpartum period, usually refers to the first 6 weeks after childbirth, not 6 months.)
2) Reduce amniotic fluid volume is associated with asymmetrical I.U.G.R.
True
3) The baby born after completion of 46 weeks of gestation is known as post maturity. A baby born after 46 weeks of gestation is called postmaturity.
True
4) Fetal distress occurring by any cause indicates immediate LSCS. Fetal distress for any reason is an indication for cesarean section.
True
5) Prostaglandin helps in softening and ripening the cervix. Prostaglandins help the cervix to soften and ripen.
True
6) Uterine fibroid is the most common cancerous tumor of female uterus. Uterine fibroid is a common cancerous tumor in women’s uterus.
False
7) Best time for giving intravenous ergometrine is after third stage of labor. The best time to give intravenous ergometrine is after the third stage of labor.
True
8) Mal presentation means the fetus breech part present in maternal pelvis. Mal presentation means part of the fetal breech in the maternal pelvis.
False
(Reason:
Uterine fibroids are non-cancerous (benign) tumors that usually develop in the uterus. It is the most common type of tumor found in the female reproductive system.
which affects many women during their reproductive years.
9) Primary PPH occurs within 6 weeks of post-partum period. Primary PPH occurs by the sixth week of the postpartum period.
False
( Reason : Primary postpartum hemorrhage (PPH) involves excessive bleeding that occurs in the first 24 hours after child birth. If it occurs within the first 24 hours, it is usually classified as primary PPH, and if it occurs within 24 hours to 6 weeks is secondary PPH. Therefore, primary PPH occurs within the first 24 hours, not within 6 weeks of the postpartum period.)
10) Manual removal of placenta is done under anesthesia. Manual removal of placenta is done under anesthesia.
True
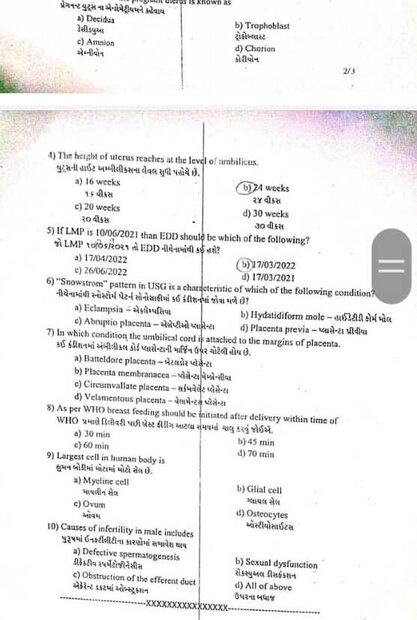
⏩(C) Write Multiple Choice Questions.
1) Ovulation occurs.
a) 14 days before next menstruation 14 days before next menstruation
b) 14 days after menstruation 14 days after menstruation
c) Within 16 hours of LH surge
d) 16 days before next menstruation 16 days before next menstruation
2) At term the volume of amniotic fluid is around. At term amniotic fluid volume is approx.
a) 1200 ml
b) 800 ml
c) 600 ml
d) 300 ml
3) Involution of the uterus is completed by involution of utes
a) 8 weeks after delivery
c) 6 weeks after delivery
b) 12 weeks after delivery
d) 16 weeks after delivery
4) Fetal compromise is assessed by all these except. Fetal compromise is assessed by all of the following.
a) FHS 120-160/min FHS 120-160/min
b) Presence of meconium
c) Pathological CTG
d) Poor fetal blood sampling results
5) Episiotomy is performed when the perineum is bulged and is
a) 2-3 cm in diameter
b) 4-5 cm in diameter
c) 6-7 cm in diameter
d) 3-4 cm in diameter
6) Most common feature of Ectopic pregnancy is the most common sign of Ectopic pregnancy.
a) Abdominal pain – Stomach pain
c) Fainting attack – Fainting attack
b) Amenorrhoea – Amenorrhoea
d) Vaginal bleeding – vaginal bleeding
7) Oral contraceptives are contraindicated in Oral contraceptives cannot be given in this
a) Hypertension – Hypertension
b) Fibroid – Fibroid
c) Menorrhagia – Menorrhagia
d) all of the above – all of the above
8) Commonest cause of Rupture of uterus is Rupture of uterus.
a) Obstructed labor Obstructed labor
b) Post cesarean gestation – Post cesarean gestation
c) Shoulder presentation Solder presentation
d) None of the above
9) Bishop scoring is based on
a) Dilatation of cervix Dilatation of cervix
b) Effacement of cervix
c) Uterine contraction
d) Station of Head Station of Head
10) This is not an Assisted Reproductive Technique. This is not an assisted reproductive technique.
a) G.I.F.T
b) ZIFT
c) IVF Embryo Transfer IVF Embryo Transfer
d) Artificial insemination into uterus Artificial insemination into uterus
Q: (1) Ans:
a) 14 days before next menstruation
14 days before next menstruation.
Q: (2) Ans
b) 800 ml
Q: (3) Ans
c) 6 weeks after delivery
Q: (4) Ans
d) Poor fetal blood sampling results
Q: (5) Ans
(C) 6-7 cm in diameter
Q: (6) Ans
d) Vaginal bleeding
(Vaginal bleeding).
Q: (7) Ans
d) all of the above.
(All of the above).
Q: (8) Ans
a) Obstructed labor
Q: (9) Ans
a) Dilatation of cervix
Q: (10) Ans
(b)ZIFT
(Z. IFT)
💪 💥☺ALL THE BEST ☺💥💪
Note :-MCQ ANSWER in unique pattern of APP in both languages is given below paper solution / click here. Clicking on “A” will change the language.
IF ANY QUERY OR QUESTION, REVIEW-KINDLY WATSAPP US NO. – 84859 76407
