ENGLISH-GNM-SY-MSN-2-PAPER SOLUTION-10/06/2025 (DONE)-NO.11
GNM-SY-MSN-2-PAPER SOLUTION-10/06/2025 -NO.11
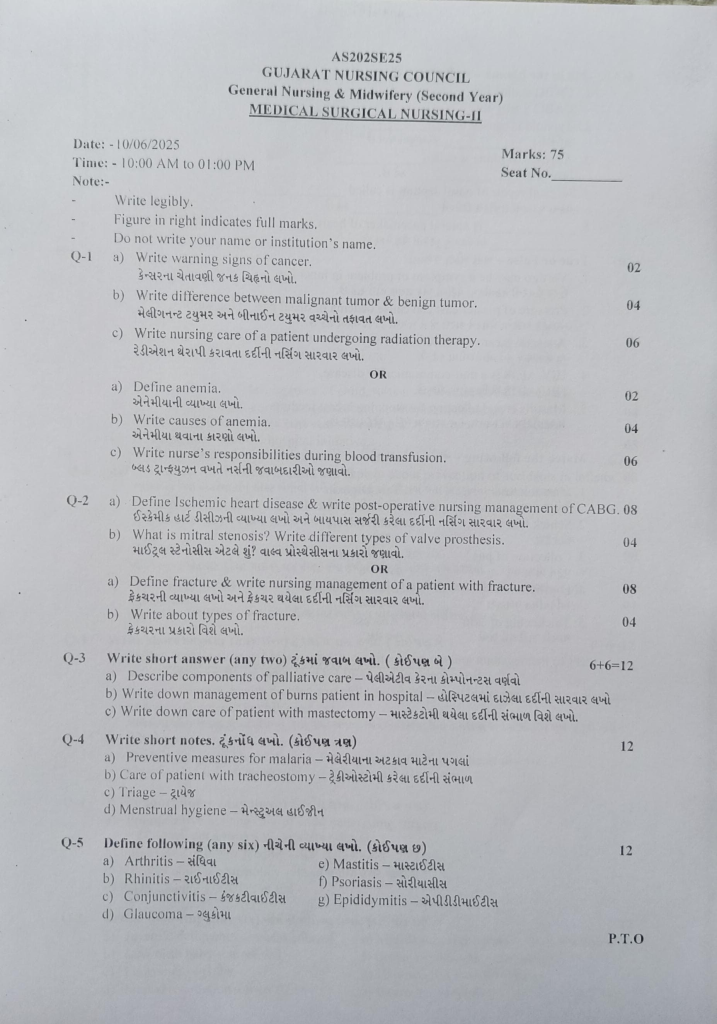
Q-1
a) Write warning signs of cancer..02
Warning sign of cancer:
CAUTION
1) C: change in bowel and bladder habit
2) A: A sore that does not cure
3) U: Unusual bleeding and discharge
4) T: Thickenin of lump in breast or any other parts
5) l: Indigestion and difficulty in swallowing
6) O: Obvious change in mole
7) N: Naging cough and soreness
- Change in bowel and bladder habit
- Description: In a normal person, the habit of bowel is one to two times.
It changes to 3 to 5 times.
Bladder: A normal person passes urine five to six times a day. It increases to 10 to 20 times.
1) Urine and stool change in consistency, size and frequency. Blood is present in urine and stool. - A sore that does not cure.
Description:
1): In this, the sore keeps getting bigger.
2): It is very painful.
3): Blood comes out of it.
In this, wherever the sore falls or an ulcer occurs in the body, it never heals, instead of healing, it increases and increases excessively.
3.Unusual bleeding and discharge.
Description:
1) : Blood comes from urine and stool.
2) : Blood comes from any part of the body such as 1) nipple, 2) penis.
Bleeding or discharge comes from any part of the body from any place. This is a sign of a type of cancer.
4.Thickening of lump and mass in breast or any other parts of the body.
Description: If there is a lump and mass, it never heals.
It gets bigger and bigger in its place.
And that lump and mass also becomes more painful and becomes like a lump.
5.Indigestion and difficulty in swallowing (difficulty in digesting food).
Description: In this, whatever is eaten is not digested and it is difficult to swallow food. As a warning for a person who has cancer, regurgitation of food occurs.
6.Obvious change in mole (any mole that has come back).
Description: If there is any mass or lump, its size changes.
The lump and mass become larger in the place where it decreases.
7.Necrosis, nagging cough and hoarseness (repeated cough).
Whenever coughing and nagging occurs, a hoarse sound is felt.
There is a change in the voice.
The voice becomes thick.
Blood comes out in the phlegm.
All these signs are warning signs of cancer.
b) Write difference between malignant tumor & benign tumor.04
Difference between Malignant Tumor and Benign Tumor
Benign Tumor:
Growth Rate:
- Grows slowly.
- Usually does not spread to surrounding tissues.
Shape:
- Has a well-organized, well-defined surface.
Cell Characteristics:
- Benign cells appear normal and do not have mutations.
Capability to Spread:
- Does not metastasize (spread to other parts of the body).
Impact on Health:
- Usually not fatal, but may cause pressure, pain, and other symptoms if they are near vital organs.
Treatment:
- Can be easily removed by surgery and has a low chance of recurrence.
Malignant Tumor:
Growth Rate:
- Grows rapidly.
- Can invade surrounding tissues and organs.
Shape:
- Has a disorganized and irregular surface.
Cell Characteristics:
- Malignant cells are new and have mutations that cause them to grow uncontrollably.
Capability to Spread:
- Can metastasize to other parts of the body through lymph nodes and hemoglobin.
Impact on Health:
- Life-threatening and can cause significant health problems.
Treatment:
- High chance of recurrence and spread.
- Requires more extensive and aggressive treatment such as surgery, chemotherapy, radiation therapy, and targeted therapy.
c) Write nursing care of a patient undergoing radiation therapy. 06
☆ Nursingcare of a patient undergoing radiation therapy (Nursing management of radiation therapy):-
Inform the patient that the skin area should be covered.
Explain the procedure to the patient.
Tell the patient about the equipment needed for the procedure and the duration of the procedure.
Tell the patient and their relatives that when radiation therapy is being given, all persons except the patient should stay away from the area.
Tell the patient that small children and pregnant mothers should stay away from the area where the radiation is being given.
Educate the patient to eat small amounts of food and give the patient antidiarrheal medicine.
Insert the patient’s urinary catheter so that the bladder can be emptied properly.
Inform the patient not to use any type of oil or emollient.
Tell the patient not to go out in the sun.
Maintain proper oral hygiene.
Communicate with the patient and his/her relatives or by telephone.
If the patient has oral cancer, do not brush too vigorously, just maintain oral hygiene by taking it easy.
Maintain the patient’s hydration status.
Maintain the patient’s nutritional status.
Tell the patient to cover the cancerous area as much as possible.
Answer all the questions of the patient and his/her relatives correctly.
Tell the patient to be careful not to injure any part of the body as much as possible.
Tell the patient that hair loss is common while undergoing radiation therapy, so the hair will grow back, so there is no need for the patient to get depressed.
Provide psychological support to the patient.
Tell the patient to do some of his daily routine activities.
Provide the patient with different types of recreational therapy and mind diversion therapy.
Maintain good communication habits with the patient.
OR
a) Define anemia. .02
Anemia is a medical condition in which the level of hemoglobin or the number of red blood cells (RBCs) is lower than normal, which reduces the supply of oxygen to the body and causes symptoms such as fatigue, weakness, and shortness of breath.
b) Write causes of anemia.04
Main causes of Anemia:
Anemia is a condition in which the amount of hemoglobin in the body is low. Hemoglobin is a protein found in the red blood cells of the blood that carries oxygen to all the organs of the body. Decreased hemoglobin reduces the supply of oxygen in the body and symptoms of anemia are seen.
Below are the main scientific and treatment-related causes of anemia:
- Iron Deficiency
Iron Deficiency Anemia is the most common type of anemia. Iron is an essential mineral in the production of hemoglobin. Lack of iron reduces the production of hemoglobin.
Main Causes:
Menorrhagia (heavy or prolonged periods)
Internal bleeding such as peptic ulcer, hemorrhoids
A diet low in iron
Pregnancy, where the demand for iron increases
- Vitamin B12 or Folate Deficiency
Megaloblastic Anemia is a type of anemia caused by a deficiency of vitamin B12 and folate, in which the red blood cells become abnormally large and malformed.
Main Causes:
Lack of a nutritious diet
Malabsorption, such as pernicious anemia
Alcoholism
Increased requirements during pregnancy and breastfeeding
- Chronic Blood Loss:
Chronic Blood Loss Anemia: Small but continuous bleeding over a long period of time causes a slow deficiency of iron in the body.
Main Causes:
Diseases of the gastrointestinal tract such as Colon Cancer, Crohn’s Disease
Uterine Fibroids
- Congenital or Hereditary Blood Related Disorder:
Thalassemia and Sickle Cell Anemia are (Genetic) blood related problems that are caused by incomplete production of hemoglobin.
Thalassemia: A fixed part of hemoglobin is not formed, so blood is formed in small quantities.
Sickle Cell Anemia: Due to the sickle shape of red blood cells, they break down quickly and their oxygen carrying capacity is reduced.
- Hemolytic Type
Hemolytic Anemia is a type in which red blood cells break down prematurely. The body cannot make enough new blood.
Main Causes:
Autoimmune Disorders
Severe Infections
Certain Drugs or Toxins
- Bone Marrow Disorders
Aplastic Anemia is a condition in which the bone marrow stops making new blood cells.
Main Causes:
Radiation or Chemotherapy
Viral infections such as Hepatitis
Autoimmune Disease
- Chronic Kidney Disease
A hormone called Erythropoietin is produced by the kidneys in the body, which signals the bone marrow to produce red blood cells. Kidney failure causes a decrease in this hormone, which causes anemia.
Anemia is not a single disease, but can be the result of many underlying conditions. Its proper diagnosis and treatment should be based on its root cause. If you feel tired, dizzy, have yellow skin, or have difficulty breathing, you should get an assessment done immediately.
c) Write nurse’s responsibilities during blood transfusion. 06
1.Patient Identification
Before starting blood transfusion, it is necessary to check the patient’s full name, hospital ID and blood group accurately. Two-person verification at the bedside is mandatory so that there is no mistake in the patient’s identification.
2.Blood Bag Verification
Check the donor number, expiration date, and blood component type written on the blood bag properly. If hemolysis, clot, or any abnormality is found, that blood should not be used.
- Checking Baseline Vital Signs
The patient’s temperature, pulse, blood pressure, and respiratory rate should be assessed before starting the transfusion, so that differences before and after can be observed.
- Close Monitoring at Start
The first 15 minutes of the transfusion are the most dangerous. Continuously observe the patient for signs of reactions such as dizziness, itching, fever, or breathing difficulty.
- Maintaining Transfusion Rate
Giving transfusion according to the specific flow rate according to the blood component, such as Packed RBCs (Packed Red Blood Cells) is usually given in 2-4 Hours. Giving it too quickly can cause problems like Fluid Overload.
- Taking immediate action against any adverse reaction (Immediate Response to Adverse Reaction)
If reactions like Anaphylaxis, Fever, Chest Pain, or Hypotension occur, stop the transfusion immediately, inform the Physician and keep Emergency Drugs available immediately.
- Post-transfusion Documentation
After the transfusion is completed, record the start time, end time, vital signs, and any side effects, if any, in the nursing notes.
- Proper Disposal of Waste Materials
Used blood bags and other materials should be disposed of according to the Biomedical Waste Destruction Protocol to avoid infection and legal problems.
Q-2 a) Define Ischemic heart disease & write post-operative nursing management of CABG.(08)
Definition of Ischemic Heart Disease:
Ischemic heart disease, also known as coronary artery disease or coronary heart disease, is a condition in which the heart muscles do not receive adequate blood and oxygen due to narrowed or blocked coronary arteries. This reduced blood flow, or ischemia, can lead to various problems including chest pain (angina), breathing difficulties, and potential heart attack.
OR
Ischemic heart disease is a condition in which the heart muscles do not receive adequate blood supply. The main cause is the narrowing or occlusion of the coronary arteries, due to which oxygen and nutrients cannot reach the heart properly. In this condition, the patient may experience angina, dyspnea, and in severe cases, myocardial infarction.
Post-operative Nursing Management of CABG:
Patient care after coronary artery bypass grafting (CABG) surgery is very important. The main responsibilities of nursing after CABG are as follows:
- Monitoring Vital Signs:
The patient’s temperature, pulse, blood pressure, and respiratory rate should be monitored regularly. Continuous ECG monitoring is essential for heart rate and rhythm.
- Pain Management:
After surgery, the patient may experience pain at the operative site. Analgesics and sedatives prescribed by the doctor are to be given to relieve it.
- Respiratory Support:
Guidance for Incentive Spirometry, Deep Breathing Exercise, and Coughing Technique to maintain the functional ability of the patient’s lungs after surgery.
- Maintaining Fluid and Electrolyte Balance:
Monitor the patient’s urine output, serum sodium, potassium, and other lab values to prevent dehydration or overhydration.
- Care of Incision Site:
Clean the chest incision and graft site, change the dressing, and monitor regularly for signs of infection such as redness, swelling, or discharge.
- Prevention of Thrombosis:
Do not allow the patient to remain lying down for long periods of time. Intermittent Pneumatic Compression, Stockings and Leg Range of Motion Exercise.
- Nutritional Support:
Adopt a Heart Healthy Diet that is low in sodium, low in fat, and high in fiber. Advise the patient to eat small frequent meals.
- Medication Administration & Observation:
Administer medications such as antiplatelet, antihypertensive, anticoagulant, and statin at the appropriate time and monitor for side effects.
- Psychological Support:
After surgery, the patient may experience depression, anxiety, or distress. The nurse should provide counseling to the patient and family to help them maintain a calm and confident environment.
- Discharge Planning and Home Care Instruction:
At the time of discharge, the patient and caregivers should be given complete guidance on medical follow-up, walking routine, regular use of medications, and diet.
Accordingly, nursing care after CABG surgery is extremely important for the patient to recover quickly and improve the recovery rate.
b) What is mitral stenosis ? Write different types of valve prosthesis.
.04
Mitral stenosis is a form of valvular heart disease in which the opening or orifice of the mitral valve is narrowed, restricting the flow of blood from the left atrium to the left ventricle, causing blood to pool in the left atrium.
Surgical management of mitral stenosis
Repair of valve
Surgical repair of the valve is also known as ‘Commissurotomy’. In this, the fused leaflets are separated. The places where these leaflets meet are called commissures. Commissurotomy is performed by two methods: open commissurotomy and closed commissurotomy
Balloon valvuloplasty
Valvuloplasty is a minimally invasive procedure in which a deflated balloon attached to the tip of a catheter is inserted through the blood vessels, mainly in the groin area, and guided to the heart valve, where the balloon is placed and inflated. This widens the narrow or stenotic valve and enlarges the valve opening. This improves blood flow.
Valve replacement
Valve replacement is a surgical procedure used to manage severe valvular stenosis. In which the damaged heart valve is surgically removed and replaced with a mechanical or biological (bioprosthetic) valve.
OR
a) Define fracture & write nursing management of a patient with fracture.(08)
Explain /define fracture. (Definition of fracture):
Fracture is a break in the continuity of a bone.
A fracture is a break in the structure of a bone. A fracture involves the bone, its tissues, bone marrow, and periosteum.
A bone fracture can be either partial or complete.
Monitor the patient’s vital signs.
Assess the patient’s neurovascular status.
Check the patient’s pain level using a pain scale.
Maintain an intake output chart.
Check for any edema or swelling in the limb.
Elevate the affected extremity to reduce swelling.
Keep checking the tightness of the cast.
Check the patient for any signs of infection.
Provide the patient with a comfortable position.
Ask the patient to do some daily routine activities and exercise.
Ask the client to do deep breathing exercises.
Ask the patient to adopt relaxation techniques.
Ask the affected limb to be elevated to the level of the heart. So that venous return can be improved.
Use aseptic technique while dressing.
Ask the affected extremity to do range of motion exercises.
Give the patient knowledge about early ambulation and its benefits.
Ask the patient to take a diet rich in protein and calcium.
Provide education to the patient about assistive devices such as crutches, walkers, cranes, slings, etc.
Keep changing the patient’s position every two hours.
Provide reassurance to the client.
Provide antibiotics, analgesics, calcium supplements as prescribed by the doctor.
Maintain records and reports.
b) Write about types of fracture..04
1) Complete fracture:- In this, the bone breaks down in cross section. In a complete fracture, the bone is divided into two parts.
2) Incomplete fracture:- In this, the bone does not break down completely. In an incomplete fracture, the bone cracks but does not break down completely.
3) Closed fracture:- A closed fracture is also called a ‘simple fracture’. In this, the bone is broken. But it remains inside the skin, that is, the skin is intact, so the wound is not open or visible and the skin on the fracture side is intact.
4) Open Fracture:– Open fracture is also called ‘compound fracture’. In this, the bone breaks down and is visible from the skin. The fracture site is an interrupted skin. In an open fracture, bacteria can enter through the open site and create an infection.
5) Displaced Fracture:- In this fracture, the ends of the broken bone are separated from each other and this fracture is mainly seen due to falling.
6) Comminuted Fracture:- In this, the bone fragments are crushed and break down in many parts. This fracture is mainly seen in elderly people due to falling.
✓ Classification by fracture pattern:
1) Linear fracture: In this, the fracture is parallel to the long axis of the bone and this is mainly seen due to direct force applied to the bone.
2) Transverse fracture: In this, the fracture is seen at an angle of 90 degrees.
3) Oblique fracture: In this, the fracture is seen at an angle of 45° degrees. This fracture is mainly seen due to twisting force.
4) Spiral fracture: Spiral fracture is called ‘torsion fracture’. Which is mainly seen due to twisting force.
5) Depressed fracture: This fracture is mainly seen due to depression in the skull bone and facial.
6) Longitudinal fracture: It is mainly a fracture that occurs in the long axis of the bone. In this, the fracture line is longitudinal.
✓ Classification by type of fracture
1) Avulsion fracture: In an avulsion fracture, the bone segment breaks down from the ligament and tendon.
2) Compression fracture: Compression fracture is also called ‘crusted fracture’. This fracture occurs due to compression on the bone. In which the bone gets crushed.
3) Green stick fracture: In this, the bone breaks down from one side and the bone bends on the other side. Green stick fracture is more common in children.
4) Impact fracture: In an impact fracture, the continuity of the bone is lost.
5) Pathological fracture: Pathological fracture is mainly seen in bones that have become weak due to diseases such as osteoporosis, cancer.
6) Stress fracture: Stress fracture is seen due to repeated loading on a small cracked bone.
✓ Classification by eponym:
1) Cullis fracture: Cullis fracture is also called ‘broken wrist’. In which the radius bone is fractured from its articular surface of the wrist to about one centimeter.
2) Potts fracture: Potts fracture is mainly seen in the medial malleolus of the tibia and fibula.
✓ Classification by Anatomical Location:
1) Articular Fracture: In this type, the fracture is found in the articular surface of the joint. In this fracture, the articular cartilage is mainly damaged and along with it, the subchondral bone is also damaged.
2) Extracapsular Fracture: In this fracture, it is mainly found near the capsule of the joint but there is no involvement of the joint capsule and this type of fracture is mainly in the hip.
3) Intracapsular Fracture: This fracture is mainly found inside the joint capsule. It is mainly seen above the neck level and is seen on the head of the femur bone.
4) Epiphyseal Fracture: In this fracture, the fracture is mainly seen in the epiphyseal plate of the long bone. This fracture is also called Selter fracture.
Q-3 Write short answer (any two) 6 + 6 = 12
a) Describe components of palliative care
Components of Palliative Care:
- Physical Care:
Appropriate medical management is done to relieve the patient’s physical problems such as pain, nausea, dyspnea, and fatigue. - Psychological Support:
To help the patient overcome emotions such as depression, anxiety, fear, and stress. If necessary, provide support from a psychologist or psychiatrist. - Emotional Support: Emotional support:
Expressing emotional understanding and empathy to the patient and their family. Giving the patient the opportunity to express their feelings. - Spiritual Care: Talking about the patient’s spiritual questions, thoughts about the meaning of life, and fears about death, helping them to find peace and contentment. If desired, also take the help of a chaplain or religious guide.
- Social Support: Working collaboratively with the patient’s family. If necessary, seek the help of a Medical Social Worker or Counselor to help the patient with social issues such as employment, household responsibilities, etc.
- Ethical and Legal Support: Ethical and Legal Support: Educating the patient about their treatment options and rights. Providing guidance on legal matters such as Advance Directives, Wills, or Dignity in Death.
- Team-Based Care: Palliative care involves a multidisciplinary team such as a doctor, nurse, physiotherapist, Jointly care for the patient with a physiotherapist, psychologist, and social worker.
- Communication and Decision Making:
Maintain open and clear communication with the patient and his family and involve them in decisions regarding treatment as per the patient’s wishes.
b) Write down management of burns patient in hospital
- Primary Assessment of the Patient:
The first 48 hours of the Resuscitation Phase is an important stage for the burns patient.
The patient should be assessed immediately for three basic things as per the ABC Protocol:
A – Airway: If the patient’s mouth, nose or throat is burned, then there is a high chance of airway obstruction. If necessary, the patient should be given Endotracheal Intubation.
B – Breathing: Observe the patient’s Respiratory Rate, Chest Movement, and SpO₂ (oxygen saturation).
C – Circulation: Check Pulse Rate, Blood Pressure, Capillary Refill Time and be alert for Hypovolemic Shock.
- Fluid Resuscitation:
The biggest risks in burns patients are – Hypovolemia and Burn Shock.
Start Intravenous Fluid Therapy for the patient immediately – Ringer’s Lactate is usually used.
Determine the fluid rate according to the Parkland Formula:
👉🏻 4 mL × Body Weight (kg) × % TBSA (Total Body Surface Area)
👉🏻 50% of which should be given in the first 8 hours and the remaining 50% in the next 16 hours.
Hourly monitoring should be done to ensure that the patient’s urine output is at least 0.5 mL/kg/hour.
3.Pain Management:
Burns patients have severe pain.
Give the patient intravenous opioids such as Morphine, Fentanyl.
Assess the pain every 2–4 hours and provide relief by giving medication according to the patient’s pain score.
Along with this, give the patient emotional reassurance.
- Infection Control:
Since the patient’s skin remains open after burns, there is the greatest risk of sepsis.
Apply aseptic dressing of the wound area.
Apply topical antibiotic ointment such as Silver Sulfadiazine.
Maintain strict hand hygiene, barrier nursing technique and sterile environment for the patient.
If fever, pulse increases or pus is seen, take blood culture and start systemic antibiotics immediately.
- Wound Assessment and Documentation:
Regularly record the depth, color, exudate, odor of the wound in a daily note.
If photographic documentation of the wound is also done, wound healing can be tracked.
Use the Rule of Nine or Lund-Browder Chart for Burn Area Calculation.
6.Nutritional Support:
During the first 48 hours, the patient develops a hypermetabolic state.
If the patient is unable to eat, start Nasogastric Tube Feeding.
Give High Protein, High Calorie, Vitamin C, Zinc Supplements for wound healing.
Monitor the patient’s Electrolyte Levels, Serum Albumin, Blood Glucose.
7.Psychological Support:
Anxiety, Fear, Depression are common in burns patients.
Talk to the patient empathetically, explain the report, and be patient.
Counseling or Psychiatric Referral may also be done if necessary.
8.Preventing Complications:
Continuously monitor the patient for Hypovolemic Shock, Renal Failure, ARDS (Acute Respiratory Distress Syndrome).
Input-Output Charting, Vital Signs Monitoring, hourly monitoring for wound worsening or septic signs.
Nursing management of a burns patient is the most important stage in saving his life.
Airway, Breathing, Circulation, as well as Fluid Balance, Infection Control, Pain Relief, Nutrition, and Emotional Care – the role of a professional nurse in all these areas is essential for both the patient’s survival and wound healing.
c) Write down care of patient with mastectomy
Care of Patient with Mastectomy:
- Wound Care:
After the operation, the patient’s wound should be regularly dressed. It is important to keep the wound clean and dry. If redness, pus, pain increases or fever occurs, contact a doctor immediately. Antibiotics can be given to prevent infection.
- Pain Management:
It is normal for the patient to feel pain after the operation. Analgesics should be given for pain relief. It is necessary to make the patient lie down in a comfortable position.
- Maintain Arm Movement:
After mastectomy, there is a possibility of lymphedema in the patient’s arms. Therefore, hand exercises should be done through physiotherapy.
- Psychological and Emotional Support:
The patient may experience feelings of depression, guilt, or shame after mastectomy. Counseling and support groups are helpful for the patient.
- Nutritional Care:
The patient should be given a high protein diet which is important for growth and tissue healing. In addition, the patient should also be given vitamin-C, iron, and folic acid.
- Follow-up Care:
The patient should be regularly referred to the oncologist and surgeon for examination. One should be alert for signs of recurrence.
- Maintain Hygiene:
It is very important for the patient to keep his body and wound clean. Maintaining hygiene can prevent infection.
Q-4 Write short notes. 12
a) Preventive measures for malaria
Introduction:
Malaria is a serious parasitic disease caused by Plasmodium species and transmitted by the bite of female Anopheles mosquito. Nurses play an important role as frontline health workers in both prevention and control of malaria.
1.Surveillance and Early Detection:
Nurses identify suspicious fever cases and initiate immediate diagnostic process.
Detection is done through rapid diagnostic tests and peripheral blood smear.
Antimalarial therapy is given immediately to positive patients.
Referral to higher center is ensured in serious or complicated cases.
2.Health Education and Awareness:
Nurses educate about malaria symptoms, transmission and complications at the community level.
Advises on the use of insecticide treated bed nets, mosquito repellents and protective clothing.
Conducts health education sessions in public places, schools and Anganwadis.
Motivates people to remove stagnant water and maintain cleanliness.
3.Vector Control Participation:
Nurses participate in both non-chemical and chemical methods for vector control.
Also works with trained persons in indoor residual spray, oiling of water surfaces and larviciding.
Nurses remain alert for identification and observation of vector breeding sites.
4.Chemoprophylaxis and Treatment Adherence:
Gives guidance on chemoprophylactic drugs such as doxycycline or mefloquine for high risk groups such as pregnant women, immunocompromised patients, and travelers.
Nurses ensure that patients complete the prescribed dose.
Keeps patients informed about side effects.
Monitors and counsels in cases of non-adherence.
5.Record Maintenance and Reporting:
Nurses properly document each positive case.
Maintains case register, line listing and daily reports.
Reports to higher health authorities on regular basis.
Analyzes trends and possible outbreaks from reported cases.
6.Training and Community Mobilization:
Nurses train ANMs, ASHAs and local health workers.
Collaborates with NGOs, local bodies and youth groups for community participation.
Conducts special awareness campaigns for parents and school children.
Nurses are not limited to clinical care only, they are a strong pillar of the public health support system. Surveillance, education, vector control, chemoprophylaxis, treatment adherence and reporting are critical steps in the prevention and control of malaria. Their efforts can significantly reduce both mortality and morbidity due to malaria.
b) Care of patient with tracheostomy
Tracheostomy is an emergency procedure, so do not waste time.
Strict aseptic technique should be observed before and after tracheostomy.
The tracheostomy tube should be of proper size and length.
Clear all doubts of the patient and his/her relatives and explain the procedure.
Closely monitor the patient before and after the procedure.
Nursing responsibilities:
Monitor and observe the patient.
Do not leave the patient alone for the first 48 hours.
Check if the patient has difficulty breathing.
Check the patient to make sure that the tube does not come out.
When the tube comes out, keep the following instruments ready:
Keep a suction catheter ready.
Maintain aseptic technique.
Give the patient a fowler position.
Do not attend the patient if any person has a respiratory infection.
Check if the patient develops any complications.
Inspire the patient or use a humidifier or filter.
Maintain the patient’s proper fluid intake and electrolyte balance.
Give the patient proper medications.
Take proper care of the patient’s oral cavity.
Dress properly.
Provide the patient with work and a comfortable environment.
Answer all questions from the patient and their relatives.
c) Triage
A)explain about triage: Triage is a system used during disasters.
It is designed to give priority to the patient vice hospital treatment
TRIAGE=SHORT/MINIMISE.
(USED DURING DISASTER)
S=SHORT
T=TRIAGE
A=AND
R=RAPID
T=TRANSPORT
Triage has three color codes through which the patient is categorized and then transported to the hospital as per the immediate need.
1) Emergency 😡(Red color): In this, the person needs immediate treatment. For that, the sooner they are sent to the hospital for treatment, the better.
Example:=severe respiratory depression ,
BRAIN HEMORRHAGE
2)URGENT🙁 (YELLOW Color): In this, the person does not need to be taken to the hospital immediately like in red color. If a person gets any injury, it will be okay even if they are taken to the hospital for treatment for one to two hours late, so this yellow color will work even if the patient gets treatment a little late.
3)Delay🤢(Green colour): In this, the person in green colour does not need immediate treatment like red and yellow colour. In this, even if the person gets treatment late for one to three hours, there is no emergency.
4)Death ⚰️(Black colour): In this, the person is in a very serious condition or is in a condition like death. So according to this color code, we can give treatment according to the needs of the injured person.
2)system:
1)Identification of victim:= In this, the victim is identified such as name, address and what is the need of the victim and treatment is given.
2)Relief work:= In this, treatment is given according to the needs of the person such as ECG, RBS, CPR, etc.
3) Rehabilitation/Recovery:= In this, if the patient is treated, he/she becomes rehabilitated and returns to his/her previous health condition.
So, according to triage, we can take any person who needs treatment to the hospital according to how much he/she needs.
d) Menstrual hygiene
Menstrual hygiene:
1) In menstrual hygiene, when a girl gets her menstrual period every month after 12 to 16 years, the kind of cleanliness that needs to be maintained is called menstrual hygiene.
2) When a girl goes to school, she needs to have complete information about the menstrual cycle.
3) When periods start, sanitary pads should be used.
4) Sanitary pads should be changed every six to seven hours.
5) When periods start, one should take a bath once or twice a day.
6) Take adequate rest during periods.
7) Drink plenty of water during periods.
8) Eat foods rich in iron and vitamin C.
9) Wash hands properly before and after using sanitary pads.
10) Change sanitary pads frequently.
11) Wrap the used pads in cloth or paper and throw them in the dustbin.
12) Wash hands properly after using the pads.
13) It is very important to maintain hygiene during periods.
14) Take a bath once or twice a day during periods and wear clean clothes.
15) After toilet and urination, private parts should be washed properly with water.
16) Always use cotton undergarments.
17) Do not use wet undergarments.
18) When using sanitary pads, cover them properly and throw them in the dust bin.
19) If you are not using sanitary pads and are using household cloths, change them frequently.
20) Clean the cloth with soap and water.
21) Then dry it properly in sunlight.
22) Only then use that cloth.
23) When sitting down to eat, clean your hands with soap and water.
In this way, proper hygiene should be maintained during your period.
Q-5 Define following (any six) 12
a) Arthritis
Arthritis is a medical condition that mainly affects the joints and its main symptoms include inflammation (swelling), pain and reduced mobility.
The common types are Osteoarthritis – which is a degenerative joint disease and Rheumatoid Arthritis – which is an autoimmune disorder. Symptoms of arthritis include stiffness, warmth and redness. It becomes more common with age and is treated with anti-inflammatory drugs, physical therapy and sometimes surgery to control symptoms.
b) Rhinitis
Inflammation and swelling of the mucous membrane inside the nose is called rhinitis. In which running nose, sneezing, nasal congestion and itchy nose are seen. Which has its types in allergic rhinitis, non-allergic rhinitis and infectious rhinitis etc.
c) Conjunctivitis
Conjunctivitis is the inflammation or infection of the conjunctiva – the mucous membrane that lines the white part of the eye and the inner surface of the eyelids. Symptoms include redness, itching, discharge, watering, and pain. The main causes are viral, bacterial, and allergic infections. Treatment includes antibiotic eye drops or antihistamines.
d) Glaucoma
Glaucoma is an eye disorder in which the pressure of the fluid inside the eye increases. That is, the intraocular pressure is abnormally high, optic nerve dystrophy occurs, and peripheral visual field loss occurs. In this condition, the intraocular pressure is more than 25 mm Hg. If this pressure remains high for a long time and glaucoma is not treated, the optic nerve becomes permanently damaged, visual field loss occurs, and finally blindness occurs.
e) Mastitis
The condition of infection and inflammation in the breast tissue is called mastitis. One of the complications of mastitis is the condition of breast abscess.
f) Psoriasis
Psoriasis is a non-infectious, recurrent, chronic (long-term) inflammatory disorder. It is characterized by increased keratin synthesis. It is characterized by red and round plaques, scaly, erythematous, silvery white patches. When these silvery white scales are removed, bleeding is seen at pin points, which is called the ‘auspitz phenomenon’.
Types of psoriasis:
1 – Psoriasis vulgaris
2 – Generalized psoriasis
3 – Localized psoriasis
4 – Erythematous psoriasis
Psoriasis vulgaris is caused by streptococcal pharyngitis.
Generalized psoriasis and localized psoriasis require hospitalization and symptoms such as fever, chills, hypocalcemia, and joint pain are seen. It is characterized by a history of erythematous and scaly lesions.
Erythematous psoriasis presents with red lesions all over the body. It is accompanied by difficulty in maintaining body temperature and hypoalbuminemia (low levels of albumin in the blood), ED, and high cardiac output due to inflammatory vasodilation.
Psoriatic arthritis is a complication of psoriasis.
g) Epididymitis
The epididymis is a coiled tube that lies above and behind the testicles and plays an important role in storing and transporting sperm. Infection and inflammation of the epididymis is called epididymitis. The condition of epididymitis is mainly caused by any infection or inflammation, which causes redness, warmth, and swelling in the scrotum (sac containing the testicles).
If the condition of epididymitis (inflammation) spreads to the testicles, it is called epididymo-orchitis.
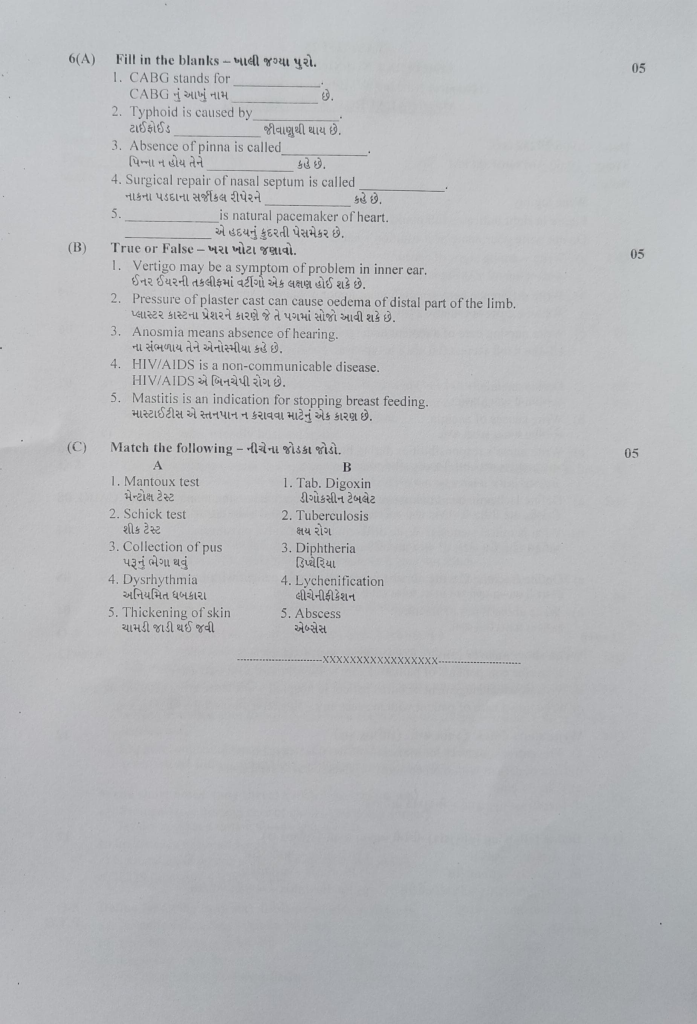
6(A) Fill in the blanks – 05.
1.CABG stands for……….. 👉 Coronary Artery Bypass Grafting
2.Typhoid is caused by………. 👉 Salmonella typhi
3.Absence of pinna is called…… .👉 Anotia
4.Surgical repair of nasal septum is called………👉 Septoplasty
5……….is natural pacemaker of heart.…………. 👉 SA Node (Sinoatrial Node)
(B) True or False – 05.
1.Vertigo may be a symptom of problem in inner ear. ✅ True
📌 Inner ear disorders like labyrinthitis or vestibular neuritis can cause vertigo.
2.Pressure of plaster cast can cause oedema of distal part of the limb. ✅ True
📌 Tight casts may impede circulation, leading to swelling or edema distal to the cast.
3.Anosmia means absence of hearing.❌ False
📌 Anosmia means loss of smell, not hearing. Loss of hearing is called anacusis.
4.HIV/AIDS is a non-communicable disease. ❌ False
📌 HIV/AIDS is a communicable disease transmitted through blood, sexual contact, or from mother to child.
5.Mastitis is an indication for stopping breast feeding.❌ False
📌 In most cases, breastfeeding is encouraged during mastitis to help drain the breast and relieve infection.
(C) Match the following 05
| A | B | Answer |
|---|---|---|
| 1. Mantoux test – | 2. Tuberculosis | ✅ 1 → 2 |
| 2. Schick test – | 3. Diphtheria | ✅ 2 → 3 |
| 3. Collection of pus – | 5. Abscess | ✅ 3 → 5 |
| 4. Dysrhythmia | 1. Tab. Digoxin | ✅ 4 → 1 |
| 5. Thickening of skin – | 4. Lichenification – | ✅ 5 → 4 |