ENGLISH-GNM-SY-MSN-1-REPEATER-PAPER SOLUTION-09/06/2025 (UPLOAD)-paper solution no.11
GNM-SY-MSN-1-REPEATER-PAPER SOLUTION-09/06/2025
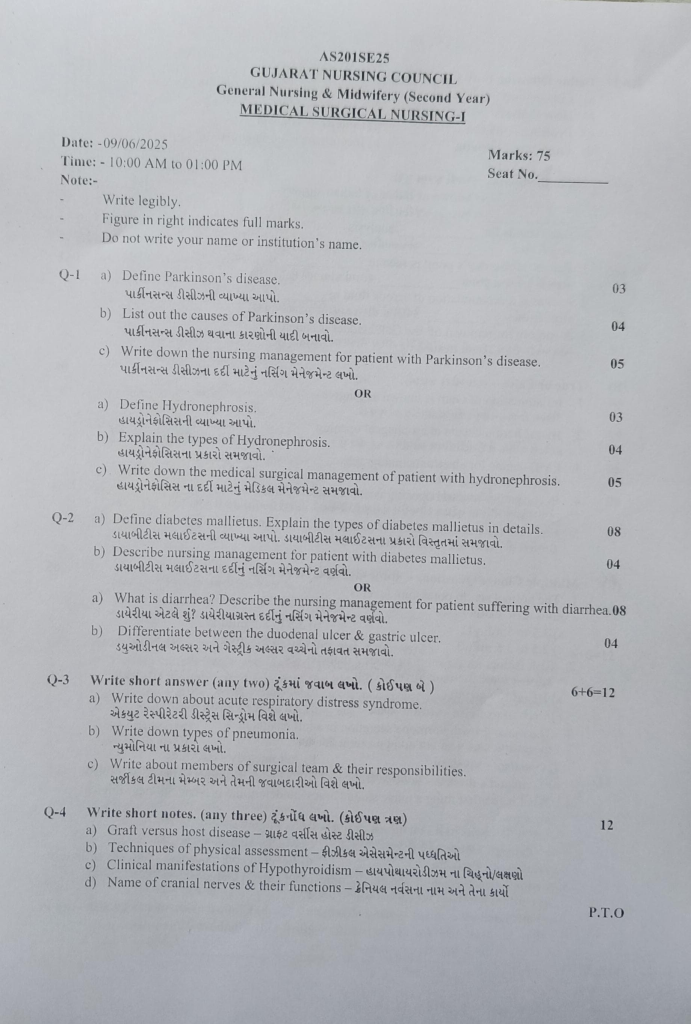
Q-1 a) Define Parkinson’s disease.
Parkinson’s disease is a disease in which the level of dopamine decreases, due to which there is obstruction of nerve impulse transmission and this is a neurodegenerative disorder. Parkinson’s disease is a chronic, progressive, neurological disorder in which muscle control, movement and balance are disturbed. Parkinson’s disease is a slow, progressive neurological movement disorder that also results in disability. Parkinson’s disease is a type of movement disorder. In which the muscle movement of a person is altered.
There are 3 main cardinal signs in Parkinson’s disease.
1) Tremor ( Tremor: Shaking) ,
2) Muscles Rigidity ( Muscles Rigidity: Stiffness),
3) Bradykinesia ( Bradykinesia)
••>
1) Tremor ( Tremor: Shaking) ,
Involuntary movements are seen in fingers, hands, feet etc. Tremor is mainly seen when a person is in a resting stage. But it is not seen when a person is on a task. Tremor occurs when a person is excited, tense and stressed.
2) Muscles Rigidity ( Muscles Rigidity: Rigidity),
In this, stiffness occurs in the limbs and trunk. This stiffness increases during movement. Due to rigidity, pain and ache occurs in the muscles.
3) Bradykinesia
In bradykinesia, voluntary movement is slow. Sometimes there is difficulty in movement. In bradykinesia, there is stiffness in the facial muscles, due to which a “Mask-Like” appearance is seen.
Thus, in Parkinson’s disease, Tremor, Muscles Rigidity and Bradykinesia are seen in the cardinal signs.
b) List out the causes of Parkinson’s disease.
Brain Infection
Encephalitis
Meningitis
Head Injury
Old Age
Genetic Factor
Environmental Factor
Due to the destruction of nerve cells that produce dopamine
Family History
Atherosclerosis
Due to Occurrence of viral Infection
Head Trauma
Due to chronic use of antipsychotic drugs
Due to deficiency of dopamine in the substantia nigra of the brain.
Due to use of Antipsychotic Drug
c) Write down the nursing management for patient with Parkinson’s disease.
Nursing management :-
Impaired Respiratory Function :-
Give high Fowler position.
Give steam inhalation if necessary.
Check SPO2 and give oxygen if less than 85.
If the patient is unconscious, suction should be done if necessary.
Anxiety:-
Provide a calm environment to the patient.
IPR should be maintained with the patient.
If possible, let them stay with other patients like them.
Before any procedure, the patient should be informed so that their anxiety can be reduced.
Fluid electrolyte imbalance:-
Iv infusion should be given as per the doctor’s order.
Maintain intake and output chart.
If necessary, give blood transfusion as per the doctor’s order.
If necessary, give electrolyte as per the doctor’s order.
Inadequate Nutrition:-
If there is no contraindication in the patient, then give a high protein and high calorie diet.
The patient should be given iron supplement.
The patient is also given vitamin supplement. Teeth:- vit b complex.
Give mild laxative to relieve constipation.
In adequate Rest:-
If necessary, sedative can be given.
Give the patient a comfortable position.
The patient should be encouraged to get enough sleep.
Use dim light while sleeping at night.
Provide a quiet environment while sleeping at night.
OR
a) Define Hydronephrosis.
Hydronephrosis is a medical condition in which urine accumulates in the kidneys due to improper drainage, causing swelling or dilation of the kidneys. This condition can arise due to any problem in the ureter or urethra, such as obstruction, reflux, or stones. Hydronephrosis can occur in one or both kidneys and can be acute or chronic.
b) Explain the types of Hydronephrosis.
Types of Hydronephrosis:
Hydronephrosis is divided into different types based on the time of its onset, severity of the condition and age of the patient. Below are the main types of hydronephrosis:
1.Acute Hydronephrosis:
This type occurs suddenly and is usually caused by a sudden obstruction in the flow of urine. It causes symptoms like severe pain and urine retention in the patient.
2.Chronic Hydronephrosis:
This type develops slowly and over a long period of time. Chronic Obstruction is caused by causes like Vesicoureteral Reflux or Ureteral Stricture. Kidney Function can be reduced in the long term.
- Unilateral Hydronephrosis:
This type of hydronephrosis is called when only one kidney is affected. Obstruction or stone in the ureter is the common cause.
- Bilateral Hydronephrosis:
This type occurs when urine accumulation occurs in both kidneys. Usually problems like Bladder Outlet Obstruction, Urethral Stricture, or Prostatic Obstruction are the underlying causes.
- Antenatal Hydronephrosis:
This type is seen on ultrasound scans of the fetus during pregnancy. It is primarily caused by a congenital problem with the kidneys or urinary tract.
- Obstructive Hydronephrosis:
This type is known when there is a clear obstruction in the flow of urine, such as a stone, tumor, or stricture.
- Non-obstructive Hydronephrosis:
In this type, the flow of urine continues to flow back without obstruction, as occurs in vesicoureteral reflux.
All these types of hydronephrosis are diagnosed with appropriate imaging tests, such as ultrasound, CT scan, or MRI, and treatment is determined based on the patient’s condition and cause.
c) Write down the medical surgical management of patient with hydronephrosis.
Medical Management of the Patient for Hydronephrosis:
Hydronephrosis is a condition that arises due to the accumulation of urine in the kidneys due to obstruction of the external flow of urine. The aim of the medical management of the patient is to maintain the functionality of the urinary tract, treat the infection, control the pain and prevent damage to the kidneys. Appropriate medical management is done based on the patient’s condition as follows:
1.Antibiotic Therapy:
If the patient has a urinary tract infection, antibiotics are given. Broad-spectrum antibiotics are usually used such as Ceftriaxone, Piperacillin-Tazobactam, etc.
- Pain Management:
Analgesics and NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) such as Diclofenac or Ibuprofen are given to the patient when there is severe pain. Opioids can also be given in severe cases.
- Diuretic Therapy:
Diuretics such as Furosemide are sometimes used to promote urine excretion. However, it is essential to remove the obstruction before this treatment.
4.Fluid Management:
Intravenous fluids are given to keep the patient hydrated, especially if the patient is dehydrated. Acid-base and electrolyte balance are also monitored.
5.Monitoring Renal Function:
Renal function tests such as serum creatinine, blood urea nitrogen (BUN) should be checked regularly to monitor kidney function.
6.Blood Pressure Control:
Hypertension may occur in some patients with hydronephrosis. Therefore, antihypertensive drugs such as ACE inhibitors or calcium channel blockers can be given if needed.
- Stone Management:
If the cause of hydronephrosis is ureteral stone, then medical therapy can be given to dissolve the stone, in which allopurinol or potassium citrate is used.
Medical management is the first step in controlling the main causes of hydronephrosis. If the obstruction is not removed immediately, surgical intervention becomes necessary.
Surgical Management:
Ureterostomy or pyelostomy has to be done to remove the obstruction.
A nephrostomy tube is placed to drain urine directly from the kidney.
Ureteral stenting is used to drain urine by placing a tube in the ureter.
Pyeloplasty is a surgical treatment for pelvic-ureter junction obstruction.
If the stone is large, a procedure such as percutaneous nephrolithotomy or ureteroscopy may be required.
Q-2 a) Define diabetes mallietus. Explain the types of diabetes mallietus in details.
Diabetes mellitus is a chronic metabolic disorder in which carbohydrate, protein and lipid metabolism are impaired. Diabetes is a group of metabolic disorders in which a person’s blood has high blood sugar levels. This is mainly due to an impairment in insulin secretion and insulin action in the body.
“3 P” syndrome is mainly seen in diabetes mellitus.
1)P: Polyuria (frequent urination),
2)P: Polydipsia (increased thirst),
3)P: Polyphagia (increased hunger).
Types of diabetes mellitus:
There are four main types of diabetes.
- Type:1(IDDM) Insulin dependent diabetes mellitus.
- Type:2(NIDDM) Non-insulin dependent diabetes mellitus.
- Type:3 Diabetes mellitus associated with other disease conditions.
- Type:4 GDM Gestational diabetes mellitus.
Type:1(IDDM) Insulin Dependent Diabetes Mellitus:
This is a type of diabetes mellitus in which the beta cells of the pancreas in the body, which are responsible for producing insulin, are destroyed due to any autoimmune disease, resulting in a total deficiency of insulin. Due to the total deficiency of insulin in this, insulin is taken by injection. This type of diabetes is mainly seen before the age of 30.
Type: 2 (NIDDM) Non Insulin Dependent Diabetes Mellitus:
In type 2 diabetes, the amount of insulin in the body is usually normal, but the body’s cells become insensitive (insensitive) or resistant to insulin, due to which the metabolism of glucose or carbohydrates becomes uncontrolled. This causes diabetes.
This type of diabetes does not affect the amount of insulin in the body. For this reason, it is called non-insulin dependent diabetes mellitus. Therefore, it is not treated with insulin. This type of diabetes can be prevented by taking proper diet, exercising, making changes in lifestyle and increasing physical activity. This type of diabetes is mainly seen after the age of 30. Therefore, it is also called adult onset diabetes mellitus. If diabetes is not treated in this way, then oral hypoglycemic agents are also taken.
Type: 3 Diabetes mellitus associated with other disease conditions.
In this, diabetes is also seen due to any other disease in the body.
type: 4 GDM Gestational Diabetes Mellitus
This type of diabetes is mainly seen in women and even in those women, diabetes mellitus is seen during pregnancy due to glucose intolerance.
b) Describe nursing management for patient with diabetes mallietus.
1)Impaired nutritional status more than body requirement related to Disease Condition.
The primary goal of the diet plan is to control the glucose level, so assess the patient’s glucose level, and assess the patient’s lifestyle, cultural background, activity level, dietary habits and food preferences.
Ask the patient to take adequate amount of food and also ask him to take snacks in between.
Arrange extra meals before the patient does physical activity.
Administer insulin as per the doctor’s order.
2)Imbalance fluid volume related to increased stress hormone as evidenced by polyuria.
Assess the patient’s intake output chart.
Ask the patient to take oral fluids.
Provide the patient with intravenous fluids.
Check the patient’s serum electrolyte levels.
Check the patient’s vital signs.
3) Activity intolerance related to weakness as evidenced by limited activities.
Assess the patient’s activity level.
Plan the patient’s activity.
Provide the patient with analgesic medicine before resuming activity.
Instruct the patient to take rest between activities.
Provide the patient with prescribed medicine.
4) Knowledge deficit related to disease as evidenced by asking questions.
Assess the patient’s knowledge level.
Provide the patient with education about the diabetic diet.
Provide education to the patient about foot and nail care.
Provide education to the patient to cover their feet with soft shoes.
5)Fear related to insulin injection.
Monitor the patient’s blood glucose level.
Provide education to the patient about self-administration of insulin.
Provide education to the patient about complications of insulin therapy.
Provide education to the patient about signs and symptoms of hyperglycemia and hypoglycemia.
OR
a) What is diarrhea? Describe the nursing management for patient suffering with diarrhea.
Diarrhea is not a disease but a symptom. Diarrhea is a symptom of a disease of the digestive system. In diarrhea, the frequency of stool, its fluid content, and volume increases. Diarrhea is a condition in which liquid and more loose stools are passed more than three times in a day. Diarrhea is mainly caused by any bacterial, viral, and parasitic infection.
Nursing management of patients with the Diarrhea. (Nursing management of the patient with diarrhea):
1) Assessment
Take a complete history of the patient with diarrhea and perform a physical examination.
Monitor the patient’s vital signs.
Assess the patient for any signs and symptoms of dehydration.
2)Fluid and electrolyte balance
Maintain the patient’s intake output chart.
Provide oral rehydration solution to the patient.
Provide intravenous fluid to the patient to maintain the patient’s fluid and electrolyte balance.
3)Provide nutritional support to the patient
Advise the patient to follow a bland diet.
Advise the patient to avoid spicy food, fatty food, fried food.
Advise the patient to eat small and frequent meals.
4)Medication administrations
Provide the patient with prescribed antibiotics and antidiarrheal medicines.
5) Infection control measures
To control infection, advise the patient to maintain proper hygienic conditions.
Advise the patient to wash hands properly.
Advise the patient to maintain hygienic conditions in his/her home environment.
Advise the patient to consume warm water.
Advise the patient to consume properly cooked food.
Advise the patient to avoid fruits and vegetables.
Advise the patient to maintain proper personal hygiene.
b) Differentiate between the duodenal ulcer & gastric ulcer.
(Students should write the answer given here in the form of differences.)
Gastric ulcer and duodenal ulcer are two types of peptic ulcers that occur in different parts of the gastrointestinal tract.
Here are the main differences between gastric ulcer and duodenal ulcer:
- Location
Gastric ulcer Gastric ulcer occurs in the lining of the stomach.
Duodenal ulcer Duodenal ulcer occurs in the first part of the small intestine, known as the duodenum.
2) Symptoms:
Gastric ulcer Pain in these ulcers occurs immediately after eating, when the stomach is full.
The pain is not relieved after eating but it is more severe.
Other symptoms include nausea, vomiting and weight loss.
Duodenal ulcer
Pain in duodenal ulcer occurs two to three hours after eating and occurs when the stomach is empty, such as before meals or at night.
The pain of duodenal ulcer is relieved after eating because food temporarily neutralizes the stomach acid and acts as a cover around the ulcer.
3) Age and gender distribution:
Gastric ulcer
Gastric ulcer is usually more common in older adults, i.e. above 60 years of age. There is usually no gender difference in this.
Duodenal Ulcer
Duodenal ulcers are usually more common in young individuals, especially between the ages of 30 and 50.
Duodenal ulcers are more common in men than women.
4) Causes:
Common Causes for Both Ulcers:
Helicobacter pylori (H.pylori) infection: The major cause of both types of ulcers.
Non-steroidal anti-inflammatory drugs (NSAIDs): Such as aspirin and ibuprofen, which damage the stomach lining.
Lifestyle factors: Stress, smoking, excessive alcohol consumption, and certain types of diets are responsible for the development of ulcers.
Specific Differences: Gastric ulcers are more commonly associated with nonsteroidal anti-inflammatory drug (NSAID) use and are less commonly caused by Helicobacter pylori (H. pylori) infection, compared to duodenal ulcers.
5) Complications:
Gastric ulcers:
These have a higher risk of bleeding, especially if blood vessels are affected, and may also have a higher risk of becoming malignant (cancerous).
Duodenal ulcers:
These ulcers have a higher risk of perforation, where the ulcer creates a hole in the duodenal wall. The risk of malignancy is lower compared to gastric ulcers.
6) Diagnosis:
Both types of ulcers are diagnosed using similar methods.
1) Endoscopy
In this procedure, a thin, flexible tube with a camera is inserted through the mouth to visualize the stomach and duodenum.
2) Barium swallow X-ray
This procedure is currently used less frequently but is used to visualize whether an ulcer is present or not.
3) H. pylori test
This involves breath, blood, and stool tests, and a biopsy is also done at the time of endoscopy.
7) Treatment
There are general treatment approaches for both ulcers.
1) H. pylori eradication
If H. pylori is present, antibiotics should be provided.
2) Proton pump inhibitors (PPIs) or H2 receptor antagonists
to reduce stomach acid production and promote healing.
3) Discontinuation of non-steroidal anti-inflammatory drugs (NSAIDs)
if non-steroidal anti-inflammatory drugs (NSAIDs) are the cause.
4) Lifestyle modifications
such as dietary changes, reducing alcohol intake, stopping smoking, and managing stress.
Understanding the differences between gastric and duodenal ulcers helps in their diagnosis and management, as well as in getting appropriate treatment and reducing complications.
Q.3 Write short answer (any two)
a) Write down about acute respiratory distress syndrome.
ARDS (Acute Respiratory Distress Syndrome) is a life-threatening condition in which the alveoli of the lungs fill with fluid, obstructing gaseous exchange, causing difficulty in breathing, and a condition of hypoxemia due to acute deficiency of oxygen. This condition occurs as a result of a severe underlying condition such as infection, trauma, aspiration, or sepsis, and is treated with intensive care.
Causes:
The main causes of ARDS are as follows:
- Pneumonia: Infection in the lungs
- Sepsis: Severe infection in the bloodstream
- Trauma: Blunt or penetrating injury to the chest
- Aspiration: Aspiration of digestive fluids or vomit into the lungs
- Pancreatitis: Infection and inflammation of the pancreas
- Inhalation of toxic substances
Pathophysiology:
During ARDS, the alveolar-capillary membrane is damaged. As a result, fluid leaks from the capillaries and fills the alveoli. This impairs gaseous exchange (oxygen uptake) and carbon dioxide removal (carbon dioxide removal). This leads to severe hypoxemia.
Symptoms:
Severe shortness of breath
Rapid breathing
Cyanosis: Blue discoloration of the lips, tongue, or fingernails
Low oxygen levels
Confusion or fatigue
Low blood pressure
ARDS usually develops suddenly with other serious illnesses.
Diagnosis:
ARDS is diagnosed through history, physical examination, and the following tests:
Chest X-ray: bilateral infiltrates in the lungs
ABG – Arterial Blood Gas: very low oxygen saturation
Pulse oximetry: monitoring of oxygen levels
CT scan: more accurate evaluation of lung damage
Echocardiogram: to assess heart-related causes
Treatment:
There is no specific medicine for ARDS. Its management is supportive and immediate ICU care is required:
1.Mechanical Ventilation: Use of ventilator for oxygen support
2.Prone Positioning: Improve oxygenation by placing the patient on the stomach
3.Fluid Management: Reduce fluid in the lungs
4.Sedation & Analgesia: To keep the patient comfortable
5.Treat underlying cause: Such as treating sepsis with antibiotics
6.Nutritional Support: Provide adequate nutrition to the body for recovery from illness.
Complications:
Lung fibrosis: Hardening of the lung tissue
Multi-organ failure: Liver, kidney or heart also affected
Prolonged ventilation: Long-term stay on a ventilator
Nosocomial infections: Hospital-acquired infections
Acute Respiratory Distress Syndrome is a life-threatening but potentially reversible condition. If recognized early and aggressive supportive care is given, it is possible to save lives. ICU management, multidisciplinary team and continuous monitoring of the patient
b) Write down types of pneumonia.
Types of pneumonia:
Pneumonia is classified based on its cause, anatomical structure and its severity.
On the basis of Etiological Factors:
Bacterial Pneumonia:
Pneumonia caused by bacterial infection is known as bacterial pneumonia. Streptococcus pneumoniae, Mycoplasma pneumoniae and Haemophilus influenzae bacteria cause pneumonia.
Viral Pneumonia:
Pneumonia caused by viral infection is known as viral pneumonia. Viruses such as influenza, coronavirus, adenovirus and respiratory syncytial virus are responsible for causing pneumonia.
Fungal Pneumonia:
Pneumonia caused by fungal infection is known as fungal pneumonia.
On the basis of Anatomical Structure:
Pneumonia is classified as follows on the basis of anatomical structure
Lobar Pneumonia:
In lobar pneumonia, infection is seen in one or more lobes of the lungs.
Broncho Pneumonia:
In broncho pneumonia, infection is seen in multiple lobes as well as the bronchi.
Interstitial Pneumonia:
In interstitial pneumonia, the interstitial tissue and alveolar septa are infected.
On the basis of broad classification:
Community Acquired Pneumonia:
Pneumonia that occurs in the community is called community acquired pneumonia.
Hospital Acquired Pneumonia:
Pneumonia that occurs after 48 hours of hospitalization is called hospital acquired pneumonia.
Ventilator Associated Pneumonia:
Pneumonia that occurs due to endotracheal intubation or mechanical ventilation is called ventilator associated pneumonia.
Aspiration Pneumonia:
Pneumonia that occurs due to aspiration of endogenous or exogenous substances is called aspiration pneumonia.
c) Write about members of surgical team & their responsibilities.
A trained and coordinated surgical team is essential for every surgery to be successful. This team consists of different medical professionals who perform their specific roles and responsibilities during the operation. Below is information about the main members of the surgical team and their exact responsibilities:
- Surgeon
Responsibility:
The surgeon is the main leader of the operation. He/She manages the patient’s condition pre-operatively, intra-operatively and post-operatively. He/She assesses the patient’s surgical needs, selects the appropriate surgical technique and performs the operation. The surgeon also leads the entire team during the operation.
2.Anesthesiologist
Responsibility:
Anesthesiologist provides anesthesia to the patient and continuously monitors his vital signs such as heart rate, blood pressure, oxygen saturation, etc. during the operation. This keeps the patient pain-free during the operation and ensures his safety during the surgery.
3.Surgical Assistant
Responsibility:
Surgical Assistant assists the surgeon during the operation. They control bleeding, handle instruments, and perform technical tasks such as suction and tissue retraction. The assistant may be a physician or a specially trained non-physician.
4.Scrub Nurse
Responsibility:
The Scrub Nurse maintains a sterile field in the operation theater. She sterilizes instruments before the operation and provides the surgeon with sterile instruments, sutures, and other surgical supplies during the operation. She confirms the instrument and sponge count after the operation.
5.Circulating Nurse:
Responsibility:
The Circulating Nurse provides support to the surgery by staying outside the sterile zone. She does documentation, brings additional supplies, assists in patient positioning and acts as a bridge for communication. Her role is important for the safety and coordination of the operation theater.
6.Surgical Technologist
Responsibility:
The Surgical Technologist sterilizes instruments and equipment, sets up the operation theater and also acts as a scrub nurse. During the operation, the surgeon is given instruments efficiently and helps maintain a sterile environment.
- Post Anesthesia Care Unit Nurse – PACU Nurse
Responsibility:
The PACU Nurse observes the patient in the recovery room after the operation. She monitors vital signs, provides pain management, and provides close monitoring until the patient regains consciousness. Her role is important in recovering from anesthesia.
The surgical team is multidisciplinary and each member supports the surgery according to their role and responsibility. Successful surgery is not possible without perfect coordination of everyone — surgeon, anesthesiologist, nurses, and technologist.
Q-4 Write short notes. (any three)
a) Graft versus host disease
Graft versus host disease occurs when an immunodeficient patient receives a transplant of immunocompetent cells. Graft versus host disease occurs when the human leukocyte antigen (HLA) of the donor and recipient do not match.
GRAFT VERSUS HOST DISEASE occurs after:
1)blood transfusion,
2)liver, kidney and bone marrow transplantation,
3)after fetal thymus transplantation,
GRAFT VERSUS HOST DISEASE occurs within 100 days of transplantation.
It mainly affects the
Skin,
Liver,
and the gastrointestinal tract.
sign and symptoms/clinical manifestation of GRAFT VERSUS HOST DISEASE.
macula popular rashes on the skin,palms,hands and soles of feet.
These rashes spread throughout the entire body.
Abdominal pain,
nausea,
vomiting,
diarrhea,
malabsorption,
mild jaundice and elevated liver enzymes,
bacterial and fungal infections,
If symptoms are limited to the gastrointestinal tract and skin, the prognosis is good, but if multisystem involvement is present, the prognosis is not very good.
Treatment of GVHD:
Provide corticosteroid medicine to the patient.
Provide the patient with immunosuppressive agents (methotrexate, Cyclosporine).
When blood transfusion is to be done, do a proper assessment.
Assess the patient for any adverse reactions.
Assess the patient for skin redness, erythema, swelling.
Provide the patient with immunosuppressive therapy.
If the patient has any other signs and symptoms, inform the doctor immediately.
b) Techniques of physical assessment
Physical examination uses systemic assessment techniques and visual, auditory, tactile, and olfactory senses. All these senses will be used in specific assessment techniques.
For example.. It is often detected by changes in body odor and fluid.
Four specific techniques are used in physical examination. Which include inspection, palpation, percussion, and auscultation.
- Inspection:
Inspection is a visual examination of the patient. And it is a visual examination of the body. In which the patient’s general appearance, body size, gait, height, shape, posture, etc. are carefully observed. This begins as soon as the nurse makes contact with the patient.
During the inspection phase of the physical assessment, the nurse uses observation skills to systematically collect observable data.
This includes measuring the patient’s respiratory effort, skin color, and wound.
General appearance
Status of consciousness
Personal grooming
Expression: worried, comfortable, alert, nervous. Body build: thin, fat, moderate. This also involves linking the patient’s words with body language.
For example, the patient’s pain experience is related to his body language.
During inspection, the maximum area of the body is visualized and then compared with the side of the other body.
Comparing the width of the right hand with the width of the left hand.
Adequate exposure of the body area is very important. In which color, texture, mobility, symmetry, nutritional status etc. are observed.
- Palpation:
Palpation means using the hands and fingers to feel the texture, size, shape, placement, location, etc. of the organ. In which specially using the finger tips of the hand to assess the temperature, pulse, texture, moisture, mass, tenderness and pain of the skin.
Gentle palpation is done by pressing 1 cm deep to assess the skin, pulse, palpation, and tenderness.
Then press 4 cm with both hands which is deep palpation. With its help, the size of the organ and the deep organ (liver) are determined.
What should be kept in mind while doing palpation?
It is always important to explain to the patient before palpation because touch is very important in our culture.
Keep the hands warm and nails short before palpation. The palmar surface of the finger is more sensitive than the finger tips, with the ulnar surface being more sensitive to vibration and the dorsal surface being used for temperature.
Palpation also helps in determining the size of the lymph nodes.
Always proceed with gentle palpation first, then deep palpation, as it may cause tenderness or fluid disturbance.
Using both hands, the size and shape of the kidneys and uterus are assessed between the finger tips and the organs.
- Percussion:
In simple words, it is called tapping. To get the quality of sound, sound is heard against the patient’s body by tapping with a finger. Which is used to reflect the density of the internal organ. The sound, vibration and resistance that are produced with different densities and vary from organ to organ and are used to know the size, shape, position, and also to detect the fluid field of the internal organ.
Percussion is a technique that determines the consistency of the tissue by the physician.
In percussion, tapping is used to produce various palpable vibration sounds with short or sharp strokes on the body surface.
Percussion is used to detect the sound, location, size, shape, and size of many organs of the body. In which the examiner taps on the patient. To extract the sound, the middle finger of the non-dominant hand is usually placed on the percussion area. And the middle finger of the dominant hand is placed on the non-dominant.
In which percussion is done in two ways.
- Direct percussion
This is used for the chest of an infant and the sinuses of an adult. Specific parts of the body are struck with the help of finger tips.
In kidney tenderness. Listen to the vibrations created.
It is necessary to select the same point two or three times before moving on to another. This is done to get an accurate reading. Strong percussion is needed for fatty patients.
_Percussion tone: Air la ute, fluid dull and solid area soft.
- Indirect percussion
This varies according to the area in which the non-dominant hand is placed palm down and the fingers of the dominant hand are gently struck on the CVA, e.g. in the kidney….
_Thorax: The middle finger of the dominant hand strikes the interphalangeal joint of the non-dominant hand which is against the patient’s skin.
Percussion produces sounds which have many sounds and different characteristics.
Characteristics of the sound
Tympanic is usually heard over the abdomen.
Resonance which is in normal lung tissue.
Hyper resonance which is in dilated lungs.
Dullness on the lungs.
Flatness on the muscles.
Auscultation
Auscultation is usually performed with a stethoscope. A stethoscope is used to block out extraneous sounds while assessing the condition of the heart, blood vessels, lungs, pleura, and intestines.
These include breath sounds, heart vascular sounds, and bowel sounds.
It is commonly used to detect the presence of abdominal sounds and assess their loudness, pitch, quality, frequency, and duration.
The most commonly heard sounds include the lungs, heart, and abdomen and blood vessels.
The chest is auscultated for heart sounds. Lung sounds are auscultated anteriorly and posteriorly for normal and incidental lung sounds. The abdomen is auscultated for bowel sounds.
Characteristics of the sound:
Intensity: Loud, medium, soft.
Pitch: Low, high, medium.
Duration: Short, long, medium.
Quality: Booming, hollow, dull, and drum-like.
c) Clinical manifestations of Hypothyroidism
Hair loss.
Brittle nails.
Dry skin.
Numbness and tingling of fingers.
Deepening of voice.
Disturbances in menstrual cycle.
Menstrual disturbances.
Subnormal temperature and pulse.
Patient gains weight.
Skin thickness.
Face becomes expressionless.
Child becomes irritable and tired.
Child’s speech slows down.
Tongue enlarges, hands and feet increase in size.
Deafness is observed.
Complaints of constipation are observed.
Inadequate ventilation.
Pleural effusion.
Respiratory muscles weaken.
Serum cholesterol levels increase and coronary artery disease occurs.
Myxedema coma.
Fatigue.
d) Name of cranial nerves & their functions
CRANIAL NERVES:
There are 12 pairs of cranial nerves
These cranial nerves are related to the cranial cavity i.e. the brain
These cranial nerves contain sensory, motor and mixed nerves.
These cranial nerves are as follows.
- Olfactory Nerve:
This nerve is a sensory nerve which carries the sensation of smell to the brain.
Its receptors are located in the nasal mucosa and when stimulated, the sensation of smell is carried to the temporal lobe of the brain through the olfactory track and the smell is perceived.
- Optic Nerve:
This is a sensory nerve. The optic nerve is the site where the sensation of vision is taken from the retina of the eye, passes through the optic foramen, passes through the optic track, and enters the thalamus first and from there the sensation is taken to the occipital lobe of the cerebral cortex where its interpretation takes place.
- Oculomotor Nerve:
This is a motor nerve whose nerve fibers originate from the midbrain
It also contains autonomic nerve fibers and supplies nerves to the intrinsic and extrinsic muscles of the eyeball, due to which the accommodation of the eye i.e. focusing on any nearby object can be done and different movements of the eyeball can be done.
- Trochlear Nerve:
It originates from the midbrain and supplies the superior oblique muscles of the eye.
- Trigeminal Nerve:
This is a mixed type of nerve and has three branches:
- Ophthalmic Nerve
- Maxillary Nerve
- Mandibular Nerve.
The nerve fibers of this nerve are connected to the pons veroli and are also involved in supplying the muscles that help in mastication.
- Abducent Nerve:
Its nerve fibers emerge from the pons veroli and are involved in supplying the lateral rectus muscles of the eye.
- Facial Nerve:
It emerges from the lower part of the pons. It supplies the muscles of the face, scalp and neck.
The motor nerve fibers of the facial nerve work for facial expression.
Its sensory nerve fibers are connected to the posterior tongue which provides the perception of taste.
- Vestibulocochlear Nerve:
It is also called the auditory nerve. It is a sensory nerve. It has 2 branches.
- Cochlear nerve. It conveys the impulses of hearing. It is connected to the organ of Corti of the cochlea of the inner ear.
- Vestibular nerve.. It conveys impulses of equilibrium. It is connected to the semicircular canal, sacculus in the inner ear and carries impulses to the pons veroli and cerebellum.
- Glossopharyngeal Nerve:
It is a mixed type of nerve.
It is associated with the secretion of saliva.
Its sensory nerve fibers carry impulses of taste from the tongue to the medulla and function in reporting the taste.
It also functions for the swallowing process and gag reflex.
- Vagus Nerve:
It is a mixed nerve.
Its sensory nerve fibers supply impulses to the pharynx, larynx, trachea, heart, bronchi, esophagus, stomach, small intestine and gall bladder.
Motor nerve fibers help in the swallowing process.
It is the longest branch of all the cranial nerves. And it is the main branch of the parasympathetic nervous system.
- Accessory Nerve:
It is a motor nerve.
Its nerve fibers emerge from the medulla and help in the swallowing process.
- Hypoglossal Nerve:
It is a motor nerve.
It emerges from the medulla.
Its nerve fibers help with tongue movement and the swallowing process during speech.
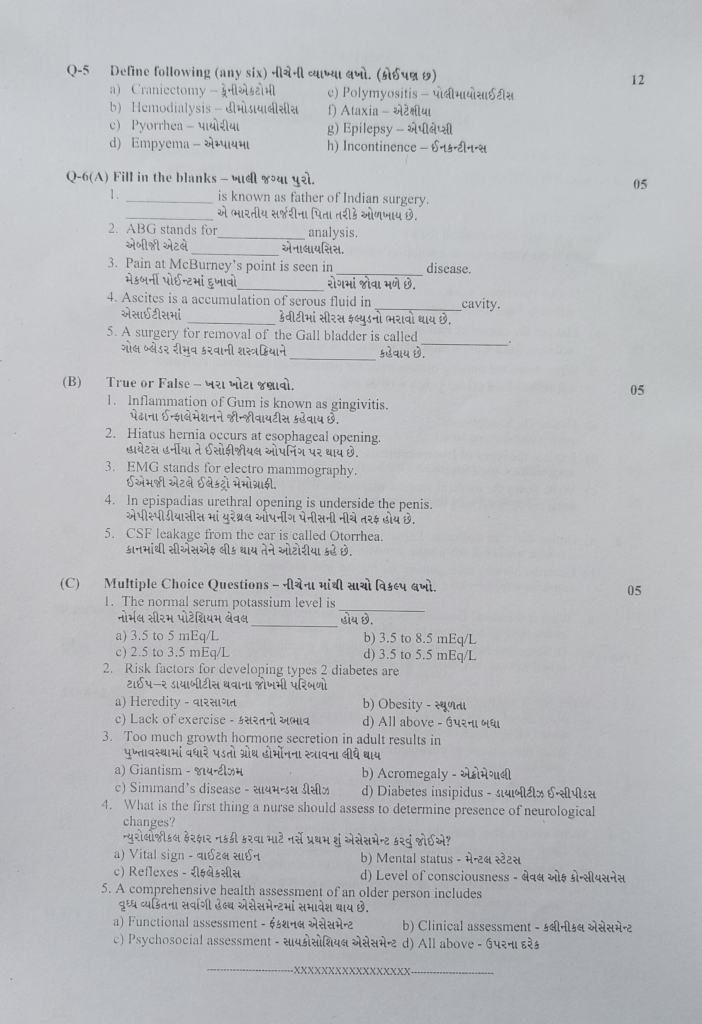
Q-5 Define following (any six)
a) Craniectomy
A craniectomy is a surgical procedure in which a part of the skull (cranium) is permanently removed to relieve pressure on the brain, such as during a head injury, stroke, or brain swelling (edema).
b) Hemodialysis
Hemodialysis is a method of removing excess waste from the body in cases of renal failure, in which excess waste is removed from the blood. After removing harmful substances, the clean blood is returned to the patient’s body.
Purpose :
To remove excess waste from the patient’s body.
To make the body’s buffer system positive.
To remove excess fluid from the body.
To reduce water retention.
To prevent other complications.
To maintain the level of electrolytes in the body.
c) Pyorrhea
Pyorrhea is also known as periodontitis. Periodontitis is a condition in which the bones and ligaments that support the teeth become inflamed due to infection. Pyorrhea is a serious gum infection in which the soft tissue and bones that support the teeth are destroyed.
d) Empyema –
Empyema is a condition in which there is an accumulation of pus in the space between the lungs and the inner surface of the chest wall (pleural space).
Abnormal collection of pus found in the pleural cavity is known as empyema. Empyema is also known as ‘Pyothorax’ and ‘Purulent Pleuritis’. Empyema is mainly seen as a complication of pneumonia and lung abscess.
OR
Purulent material accumulates (accumulates) in the pleural space and is called empyema. It is also called pyothorax.
e) Polymyositis
Polymyositis is a chronic, progressive and inflammatory myopathy (muscle disease) that affects the tissues of skeletal muscles and causes gradual swelling and weakness within them. It is an autoimmune disorder in which the body’s immune system damages its own muscle tissue. Polymyositis usually occurs in adults and affects females more. The main symptoms include gradual increase in tissue weakness, fatigue, sometimes difficulty swallowing due to the affected tissues, and sometimes difficulty breathing. Blood tests, muscular biopsy, MRI, and electromyography are used for diagnosis. Treatment mainly involves corticosteroids and immunosuppressant medications.
f) Ataxia
Ataxia is a neurological condition in which a person’s balance and coordination in voluntary movement is impaired, such as the inability to walk, pick up objects or speak, and this condition is mainly caused by dysfunction of the cerebellum or its pathways.
g) Epilepsy
If the patient has repeated episodes of seizures, then that condition converts into epilepsy. Epilepsy is a mental abnormality in which the electrical impulses of neurons in the brain of a person are greatly disturbed, due to which abnormal electrical activity is seen in the neurons and the condition of epilepsy occurs due to which jerking movements arise in the body.
h) Incontinence
Incontinence is a medical condition in which a person loses voluntary control over urine or stool, that is, there is no bladder or rectal control within the body. In this condition, a person may have urinary incontinence or fecal incontinence. Urinary incontinence is a condition in which there is no control over urine and urine leaks involuntarily. Fecal incontinence is a condition in which stool is passed involuntarily. This problem is usually caused by medical conditions such as nervous system abnormalities, pelvic muscle weakness, bladder or bowel dysfunction. Incontinence affects a person’s daily life, mental health and social health and requires proper medical diagnosis and treatment.
Q-6(A) Fill in the blanks 05
1…………is known as father of Indian surgery.Sushruta
2.ABG stands for……… analysis.Arterial Blood Gas
3.Pain at McBurney’s point is seen in……… disease.Appendicitis
4.Ascites is a accumulation of serous fluid in…….. cavity peritoneal
5.A surgery for removal of the Gall bladder is called…Cholecystectomy
B) True or False – 05
1.Inflammation of Gum is known as gingivitis.✅ True
2.Hiatus hernia occurs at esophageal opening. .✅ True
3.EMG stands for electro mammography.❌ False
4.In epispadias urethral opening is underside the penis.❌ False
5.CSF leakage from the ear is called Otorrhea. ❌ False
(C) Multiple Choice Questions 05
1.The normal serum potassium level is…..
a) 3.5 to 5 mEq/L
c) 2.5 to 3.5 mEq/L
b) 3.5 to 8.5 mEq/L
d) 3.5 to 5.5 mEq/L
✅d) 3.5 to 5.5 mEq/L
📌 Explanation: Normal potassium levels are 3.5 to 5.5 mEq/L. Below 3.5 is hypokalemia, and above 5.5 is hyperkalemia.
The normal potassium level is 3.5 to 5.5 mEq/L.
2.Risk factors for developing type 2 diabetes are
a) Heredity
b) Obesity
c) Lack of exercise
d) All above
✅ d) All above
📌 Explanation: Type 2 diabetes is associated with heredity, obesity, and lack of physical activity.
3.Too much growth hormone secretion in adult results in
a) Giantism
b) Acromegaly
c) Simmand’s disease
d) Diabetes insipidus
✅ b) Acromegaly
📌 Explanation: In adults, excess growth hormone causes Acromegaly (enlarged hands, feet, jaw). In children, it causes Gigantism.
4.What is the first thing a nurse should assess to determine presence of neurological changes?
a) Vital sign
b) Mental status
c) Reflexes
d) Level of consciousness
✅ d) Level of consciousness – Level of whiteness
📌 Explanation: Level of consciousness (LOC) is the first indicator of neurological status.
Instead of LOC, neurological deterioration can be detected early.
5.A comprehensive health assessment of an older person includes
a) Functional assessment
b) Clinical assessment
c) Psychosocial assessment
d) All above
✅ d) All above
📌 Explanation: Functional, Clinical, and Psychosocial assessments are all part of geriatric evaluation.
All types of assessments are essential for proper screening of the elderly.
