ENGLISH-GNM-SY-MENTAL HEALTH NURSING (MHN)-REPEATER PAPER SOLUTION-11/06/2025 (DONE)-NO.11
MHN)-REPEATER PAPER SOLUTION-NO.11-11/06/2025
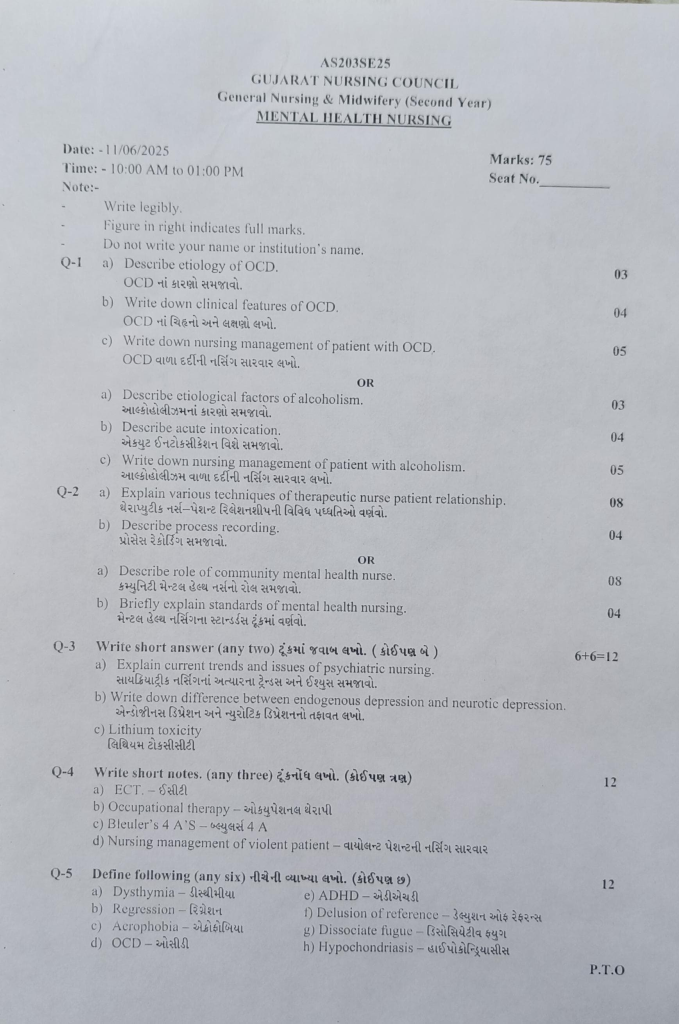
Q-1 a) Describe etiology of OCD.
Causes of OCD Explain.03
CAUSES OF OCD-(Causes of OCD)
Biological Factor:
- If Parents (Parents) or Siblings (Brothers and Sisters) have OCD (OCD), then the Possibility (Possibility) of it increases.
- Identical Twins have a higher Chance of OCD than Dizygotic Twins.
Brain Chemistry:
- Imbalance of Serotonin Neurotransmitter (Imbalance) Mood changes are seen.
Environmental Factor:
- Traumatic Events, Abuse and Stress cause OCD Symptoms.
Cognitive Factor:
- Certain Thought Patterns and Beliefs, such as Excessive Need for Control, result in OCD.
Neurological Factor (Neurological Factors):
- Abnormalities in Brain Structure and Function can cause OCD.
Infection:
- Streptococcal Infection can cause OCD.
b) Write down clinical features of OCD.04
Write down the signs and symptoms of OCD.
Unwanted Thoughts are repeated even though the person does not want them to be and all this happens in the Conscious State. This causes Anxiety and Fear.
Obsession:
- The person has frequent Thoughts of Germs or Contamination.
- Fear of Contamination
- Doubting
- Need for Order (Need for Order)
- Aggressive Thoughts
Compulsion:
Continuous Repetition of Purpose Actions, Without Desire, without Control
- Frequent Hand Washing.
- Checking whether the door is Locked or not.
- Washing/Cleaning
- Checking (e.g., Locks (Locks), Door
- Activity Repetition (e.g., Counting )
- Touching (e.g., repeatedly Touching Walls
c) Write down nursing management of patient with OCD.
Write the nursing treatment of a patient with OCD.05
Nursing Diagnoses for OCD Patients:
- Severe Anxiety
- Impaired Communication
- Altered Coping Ability (Altered Coping Ability)
- Impaired Judgment (Impaired Judgment)
- Disturbed Sleep Pattern (Disturbed Sleep Pattern)
- Lower Self-Esteem (Lower Self-Esteem)
1. Severe Anxiety:
Objectives:
- Reduce Anxiety.
- Minimize Compulsive Behavior.
Nursing Interventions:
- Observe Anxiety Levels and Establish Relationship with Respect, Warmth, and Empathy.
- Provide a Clean and Comfortable Environment.
- Motivate the Patient (Patient) to discuss their Anxiety (Anxiety).
- Identify Anxiety-Producing Situations (Anxiety-Producing Situations) and provide Psychological Support (Psychological Support).
- Encourage the Patient (Patient) to express their Feelings (Feelinggs) and work on alleviating their Fear (Fear).
- Discourage Compulsive Behaviors and administer Medications as per Prescription .
2. Impaired Communication:
Objectives:
- Improve Communication.
- Enhance Social Interaction.
Nursing Interventions:
- Provide a Trusting Environment.
- Help develop an Effective Relationship with the Patient.
- Discover the Source of Anxiety and observe for other Symptoms like Rigidity and Ambivalence.
- Motivate the Patient (Patient) to engage in conversations with others.
- Communicate in a Simple and Concise manner, teaching Communication Skills.
3. Altered Coping Ability:
Objectives:
- Improve Coping Abilities.
- Help manage Obsessive-Compulsive Behaviors.
Nursing Interventions:
- Assess the Coping Abilities.
- Build a relationship with the Patient with Warmth and Respect.
- Fulfill the Dependency Needs (Dependency Needs) of the Patient and provide Positive Reinforcement.
- Accept the Patient’s Compulsive Behaviors initially.
- Gradually set Limits on Ritualistic Behavior.
- Do not punish the Patient for their Symptoms.
- Observe how many times the Patient engages in Hand Washing within an hour.
- Teach new Adaptation Skills to deal with Ritualistic Behavior .
- Use Cognitive and Modeling Therapy
OR
a) Describe etiological factors of alcoholism.
Explain the causes of alcoholism.03
CAUSES OF ALCOHOLISM:
Psychiatric Disorder
Psychiatric Disorder
Some patients with depression, anxiety and phobias will consume alcohol to elevate their mood.
Occupational Factors:
Some people associated with professions such as medical professionals, journalists, actors etc. consume alcohol.
Genetic Factors:
Some heavy drinkers have a family history of alcoholism. Which comes from one generation to another.
Biochemical Factors:
Due to alterations in dopamine and epinephrine, a person goes towards alcoholism.
Social Factors:
Sudden loss of property, unemployment, loss, injustice, peer group pressure, large family, broken homes, neglect, boredom, ignore, isolation.
Personality Factors:
Alcoholism is more common in people with anxious and anti-social personalities. is.
Psychological Factors:
They use alcohol to escape reality and avoid stress.
High Risk Groups:
If alcohol is easily available, it leads to alcoholism.
People suffering from chronic physical illness, business executives, Traveling sales personnel are likely to develop alcoholism. Boys, especially, follow their parents’ drinking patterns.
b) Describe acute intoxication.
Explain acute intoxication.04
Acute intoxication is a physical and mental condition that occurs when a patient’s body suddenly and in large quantities ingests a toxic substance. These substances typically include alcohol, drugs, chemicals, or other toxic substances. This condition is usually acute and its symptoms may appear within a short time.
According to (WHO),
“Acute Intoxication is a transient condition following the administration of alcohol or other psychoactive substances, resulting in disturbances in consciousness, cognition, perception, affect, or behavior.”
Main Causes:
- The main causes of acute intoxication include the following:
- Excessive alcohol Alcohol Consumption
- Inhalation, Injection, or Ingestion of Poisonous Chemicals
- Recreational Drug Use
- Overdose – Taking too much medication or drugs
- Accidental Intake – Especially in Children
Symptoms:
The symptoms seen in acute intoxication depend on the substance ingested, the amount, and the body response of the patient. Common symptoms include the following:
Central Nervous System (CNS) Symptoms
- Confusion
- Loss of Consciousness
- Slurred Speech
- Disorientation (Dizziness)
- May progress to Coma
Cardiovascular System:
- Tachycardia – fast heartbeat
- Hypotension – low blood pressure
- Arrhythmia – Irregular Heartbeat
Respiratory System:
- Respiratory Depression
- Breathing Difficulty
- Sometimes breathing may stop
Gastrointestinal System:
- Nausea and Vomiting
- Abdominal Pain
- Diarrhea – in some cases
Behavioral and Psychological Symptoms:
- Aggression
- Depression
- Hallucination
- Anxiety
Diagnosis:
- Acute Intoxication is diagnosed based on history and symptoms. Along with this, the following tests are useful:
- Blood Test – To find out the level of toxins
- Urine Analysis
- ECG – To check the cardiac status
- Imaging such as CT Scan: If the nervous system is affected
Treatment (Treatment):
- Acute intoxication requires immediate medical intervention.
1.Airway, Breathing, Circulation (ABCs) Management
- Oxygen Therapy
- Mechanical Ventilation: If Needed
- Intravenous Fluids: To manage dehydration and blood pressure
2. Detoxification
- Gastric Lavage: To remove the substance
- Activated Charcoal: To prevent absorption
- Antidotes: Antidotes suitable for a particular toxic substance
3. Psychological Support & Monitoring
- Continuous monitoring of the patient’s mental state and vital signs
- Nursing Observation 24×7
- Family Education and Counseling
Complications:
- Acute Intoxication can lead to severe complications if not treated in time:
- Brain Damage
- Liver Failure
- Multi-Organ Failure
- Coma or Death
- Acute Intoxication is an immediate and severe medical condition that can be life-threatening for the patient.
c) Write down nursing management of patient with alcoholism.
Nursing treatment of patient with alcoholism Write.05
Nursing Treatment of a Patient with Alcoholism:
Nursing Diagnosis:
- Increased Anxiety
- Altered Sleep Pattern
- Impaired Social Interaction
- Altered Nutrition Less Than Body Requirement
- Disturbed self-esteem
- Manipulative behavior
- Ineffective individual coping
- Risk for harming self and others
- Impaired social interaction
- decrease coping Abilities
1. Increased Anxiety
- Objectives: To help reduce the patient’s anxiety level.
Nursing Intervention
- Assess the anxiety level.
- Assist the patient with his/her Problems should be accepted.
- Establish a trustworthy relationship with the family and client.
- The patient should be helped to cope with his symptoms.
- Do not fight him by thinking that he is a drug addict.
- Encourage the patient to express his feelings and emotions.
- To support the patient Family members should be encouraged.
- Anti-anxiety medication should be given as prescribed.
2. Altered sleep patterns
- Objectives: To help the patient improve his sleep patterns.
Nursing interventions
- The client’s sleep pattern should be assessed.
- The patient should be encouraged to get 6-8 hours of sleep during the night.
- Provide the client with a safe and calm environment.
- Encourage relatives to stay close to the patient.
- Give the patient a warm Provide a glass of milk.
- The patient should be given back massage and support.
- Ask the client to take a bath with warm water before sleep.
- Ask the patient to read books of his choice.
- Ask him to do some relaxation exercises.
- Play some music to have a smooth effect on the client’s mind. To do.
- Encourage the client to attend spiritual prayer.
- Give sedative medicine as prescribed.
3.Impaired Communication
Objectives: The patient’s communication improves and he interacts with people.
Nursing Intervention
- Assess the patient’s level of communication and social interaction.
- Maintain a friendly approach with the patient and communicate appropriately with the patient.
- Encourage them to participate in group therapy to promote their communication.
- Spend time with the patient and communicate with them in a language that is simple and understandable to the patient.
- Give them opportunities for social interaction and provide a friendly environment.
- The client should be motivated to engage in social interaction.
4. Reduces self-esteem and self-concept
Objectives:-The patient’s self-concept should be improved.
Nursing Intervention
- Give a brief explanation for the activity and help the patient identify their positive points.
- Increase their sense of self by giving attention, motivate the patient for activities that they can do with confidence.
- Anchor the client for positive physical habits.
- Respect the patient Teach exercises to increase.
- Do not put the patient in a difficult decision-making position and the relatives should also support the patient.
- The therapeutic relationship should provide opportunities to express feelings and emotions.
- Give medication as prescribed and check for potential side effects of medication.
- Rehabilitation of alcohol dependence syndrome (substance abuse patient) Rehabilitation)
- When the person needs to continue with social support in order to function and live a normal life.
- Available as inpatient units, comprehensive outpatient, day care centers, and drug de-addiction centers.
- Help them to quit the drug they are dependent on.
- Occupational and social rehabilitation, teaching relationships Technique, Religious Therapy
- Encourage them to be helpful and respectful.
- Encourage them to participate in self-help groups.
- Help them to lead productive and respectful lives.
Q-2 a) Explain various techniques of therapeutic nurse patient relationship. Explain various techniques of therapeutic nurse patient relationship.08
The therapeutic nurse-patient relationship is a professional and close mental relationship that aims to improve the physical, mental and emotional health of the patient. In this regard, the nurse behaves with the patient in an empathetic, respectful and trustworthy manner:
1. Active Listening:
- Active Listening is a method in which the nurse listens attentively and with full concentration to the patient.
- The patient’s sentences, tone and body language are observed.
- The patient is advised that his feelings and thoughts are important.
- Techniques such as “nodding”, “eye contact”, “verbal response” are included.
2. Empathy Expression:
- Empathy is the ability to understand and explain the patient’s feelings.
- The nurse tries to feel the patient’s pain, fear, or anxiety.
- This makes the patient feel safer, supported, and understood.
- Example: “I can understand how painful it must be for you.”
3. Clarification:
- Clarification is a technique used to clearly understand the patient’s message.
- If there is any ambiguity in the patient’s words, the nurse asks, “Do you mean to say that…?”
- This technique eliminates misunderstandings between the patient and the nurse.
4. Silence:
- Silence is a powerful tool to give the patient time to express their experience.
- A little silence is important when the patient is expressing a deep emotion.
- This technique allows the patient to process their inner thoughts.
5. Touch (Touch):
- Touch means that when the nurse gently touches the patient’s hand, he feels compassion and support. Touch must be used sensitively and ethically.
- A therapeutic bond develops with the patient through touch.
6. Open-ended Questions:
- Open-ended questions allow the patient to provide more information.
- Example: “What do you feel when you feel pain?”
- The patient speaks more openly and his true condition is understood.
7. Paraphrasing:
- Paraphrasing is when the nurse re-proposes what the patient says in her own words so that the patient understands that the nurse has heard and understood her.
- Example: “You say that you find it scary to be alone in the hospital, right?”
8. Stating Observations:
- Stating Observations are notes and descriptions of the patient’s behavior or emotional state.
- Example: “I can see that you seem a little more anxious today.”
- This also allows the patient to pay attention to their feelings.
9. Reinforcement:
- Reinforcement works to praise the patient’s positive behavior and efforts to participate in treatment.
- The patient’s mental confidence and motivation increase.
- Example: “You are following the diet very well to keep your blood sugar normal.”
10. Setting Boundaries:
- Setting Boundaries is useful for defining professional limits in a therapeutic relationship.
- Prevents personal relationship with patient.
- Maintains a healthy professional relationship between nurse and patient.
11.Summarization:
Summarization means repeating the main points of the conversation at the end.
It makes it clear what the conclusion of the conversation was.
The therapeutic nurse-patient relationship is not just about compassionate care, but is based on scientific and medical techniques. Through these methods, mental, emotional and physical support is provided to the patient, so that he can remain positive towards treatment and health recovery is speedy. Every nurse should use these methods regularly so that they can contribute to the collective development of the patient.
b) Describe process recording. Describe process recording.04
Process recording is a very important training technique in nursing education and when providing mental health services. In this process, the nursing student describes and writes down the conversation with the patient so that his/her perception, thoughts, feelings and understanding of responsibility can be deepened.
Purpose of Process Recording:
1. To improve communication skills.
2. To develop self-awareness.
3. To analyze the conversation with the patient.
4. Understand the patient’s mental status and emotional response.
5. Strengthen the nurse-patient relationship.
Key Components of Process Recording:
1. Data:
Information is provided about the patient’s personality, age, gender, medical diagnosis, and behavior.
2. Setting:
A description of where the conversation took place – such as a hospital room, OPD, or consultation room.
3. Objective:
What is the purpose of the conversation – to establish a trusting relationship with the patient, to help him relax, etc.
4. Actual Verbatim Conversation:
A literary account of what was said between the patient and the nursing student.
Example:
Nurse: “How is your mood today?”
Patient: “My mood is very bad…”
5. Analysis:
The meaning, emotion, and behavior of each dialogue are interpreted.
For example: The patient says “I am in a bad mood”, the possibility of depression or anxiety can be discussed.
6. Feelings of Nursing Student:
What feelings did the nursing student have? Did they feel fear? Or empathy?
7. Evaluation:
Was the objective achieved? How meaningful were the patient’s answers? Did the patient open up or not?
8. Future Plan:
What to do next? When to hold the next session? What issues to work on?
Benefits of Process Recording:
Self Reflection: Nursing student reflects on his/her own approach and behavior.
Professional Growth: Understanding current interactions can lead to better service in the future.
Patient Needs Assessment: What he/she feels from the patient’s interactions, There is an opportunity to understand.
There is an opportunity to develop a therapeutic relationship.
Process Recording is not just a written document but a tool in nursing education through which students develop their communication skills, mental understanding, and the art of effectively interacting with patients. It is an educational tool through which students can learn in depth about their professional development and the psychosocial aspects of patients.
OR
a). Describe role of community mental health nurse. Explain the role of a community mental health nurse.08
Nurses play an important role in providing community mental health services.
Nurses play many roles while providing community mental health services.
- Care provider
- Educator
- Leader
- Domiciliary role
- Liaison
- Counselor
- Coordinator
- Administrator
- Advocate
- Research work
- Care provider : (Care Provider)
- A nurse provides care to a mentally ill patient and provides guidance to family members on how to care for the mentally ill patient at home.
- Educator:
- A nurse provides education to people in the community on how to promote mental health.
- A nurse educates people in the community about misconceptions about mental health in the community. Aware.
- Goes to the community and organizes various programs and educates people there about the promotion of mental health and prevention of mental illness.
- Laision:
- Liision means contact
- The nurse works as a liaison officer and acts as a link between the patient, his family members, the mental health care team, and other members.
- Domiciliary :(Domiciliary)
- A nurse provides domiciliary services.
- She visits the community and knows the status of the people in the community.
- If a person with mental illness is detected, she provides care to him and refers him to a psychiatrist.
- Counselor : (Counselor)
- A nurse provides counseling services to patients, their family members, and the community.
- Provides counseling services to patients, their family members, and the community, such as those who have experienced a stressful situation or life event.
- Coordinator: (Coordinator) A nurse coordinates the work of the mental health team among the various members of the mental health team so that good care can be provided to the community and people can use it.
- Advocator : (Advocate) A nurse works as an advocate. She helps the patient make decisions and fights for the patient’s rights.
- Administrator :(Administrator) A nurse plays the role of an administrator. Such as where to program in the community and how to program and provide resources for that.
- Evaluator : (Evaluator) – Evaluates various programs implemented in the community and knows about the impact it has on people.
- Research: Nurses play an important role in research work, observing the diagnosis and treatment of patients and conducting research on them.
b) Briefly explain standards of mental health nursing. 04
Standards of Mental Health Nursing:
The Standards of Mental Health Nursing are professional guidelines that provide guidance to nurses on how to provide quality, ethical and safe care when providing mental health care. Adherence to these standards ensures patient-centered and evidence-based practice.
The following is a description of each standard:
1. Assessment and Diagnosis
The nurse conducts a broad assessment of the patient’s psychological, biological, and social needs.
Clinical assessment is used to identify mental disorders such as schizophrenia, bipolar disorder, etc. Clinical Observation and Interview Techniques are used.
2. Care Planning
Prepares a personalized care plan according to the patient’s individual needs.
The plan involves medication management, therapeutic communication, and crisis intervention.
3. Therapeutic Relationship Relationship)
The nurse develops a trustful and empathetic relationship with the patient.
Provides psychological support by maintaining boundaries.
4. Medication Administration
The nurse appropriately administers mental health drugs such as antidepressants, antipsychotics, and mood stabilizers.
Side Effects and Adverse Reactions Continuous monitoring for adverse reactions.
5. Ethical and Legal Aspects
Works in accordance with the Mental Health Act and Patient Rights.
Maintains confidentiality and informed consent.
6. Multidisciplinary Collaboration
Works as a team with a psychiatrist, clinical psychologist, social worker and occupational therapist.
Promotes integrated care.
7. Health Education and Rehabilitation
The nurse provides training to the patient and his family on Mental Health Awareness, Stigma Reduction and Coping Mechanisms.
Through Rehabilitation Programs Reestablishes employment, housing, and social life.
8. Documentation and Reporting
Maintains accurate documentation of each clinical activity.
Fills out Progress Notes, Incident Reports, and Care Plan Updates in a timely manner.
9. Evidence-Based Practice
New Research and Clinical Provides treatment according to Clinical Guidelines.
Participates in Continuous Professional Education.
10. Safety and Risk Management:
Conducts risk assessments for patient and staff safety.
Adheres to policies such as Suicide Prevention, Violence Management, and Restraint Use.
These Standards of Mental Health Nursing guide nurses towards Clinical Excellence, Moral Responsibility, and Patient Mental Well-Being.
It is essential for every nurse to adhere to these standards for their profession.
Q-3 Write short answer (any two) 6+6-12
a) Explain current trends and issues of psychiatric nursing. Explain the current trends and issues in psychiatric nursing.
Current Trends in Psychiatric Nursing
1. Technology-Based Mental Health Care:
Telepsychiatry and telehealth services are growing rapidly in psychiatric nursing.
Specialty:
- Treatment of remote patients through video consultation.
- Use of digital therapy, mobile apps and electronic health records.
2. Holistic & Personalized Treatment:
Psychiatric nursing is now only pharmacology (Pharmacology) will not be based on.
Flow:
- Medicine + Therapeutic Models (Models) — such as CBT (Cognitive Behavioral Therapy), DBT (Dialectical Behavioral Therapy).
- The physical, emotional, social and spiritual aspects of the patient are taken care of.
3. Interprofessional Team Approach (Interprofessional Team Approach):
The treatment now involves a multidisciplinary team more.
The team consists of:
Psychiatrist, Psychologist, Nurse, Occupational Therapist, Social Worker, etc.
4. Evidence-Based Practice:
Psychiatric nursing now adopts scientific research-based methods.
Example:
New medication protocols
Therapeutic interventions such as Exposure Therapy, EMDR (Eye Movement Desensitization and Reprocessing)
5. Culturally Sensitive Care:
Nursing is now done according to the patient’s cultural beliefs, language and lifestyle.
Specialty:
- Interpreting the patient’s mental states according to culture.
- Strengthening the therapeutic alliance.
6.Continuous in Nursing Education (Continuous Education in Nursing):
It is important to stay updated on new medications, mental health disorders, and treatment methods.
Resources:
- E-learning Platforms
- Webinars, Simulation Tools, Certificate Courses
Current Issues in Psychiatric Nursing:
1. Workload & Burnout
Psychiatric nurses work long shifts with high-risk patients.
Difficulties:
- Mental fatigue
- Overshift work
- Burnout and feelings of fatigue
2. Safety & Risk of Violence
Patients in psychiatric settings can often become aggressive or violent.
Concerns:
- Lack of personal safety
- Risk of physical and verbal assault
3. Inadequate Compensation & Recognition
Compared to other nursing fields, psychiatric nurses receive less recognition and pay.
Results:
- Staff turnover
- In motivation खत
4. Ethical Dilemmas
Nurses have to make ethical decisions regarding involuntary treatment, restraint, and the patient’s capacity.
Example:
How to obtain consent when a patient is in a state of psychosis?
5. Stigma & Lack of Support:
Psychiatric nursing is still not actively accepted in some societies.
Effect:
- Nurses feel less valued about their careers.
- Less focus on mental health in nursing education
6. High Complexity in Addiction Cases
Patients have a dual diagnosis with Substance Use Disorder (SUD).
Concerns:
- Relapse rates are high
- Withdrawal Management is difficult
7. Low Nurse-to-Patient Ratio:
When there are more patients and less nurses, the quality of care is affected.
Impact:
- Less time for individual consultation
- Incomplete Documentation
8. Documentation and Legal Responsibility:
Psychiatric cases have more legal implications.
Requirements:
- Accurate Documentation
- Legal Knowledge
Trends in psychiatric nursing are patient-centric, tech-enabled, and culturally inspired, while issues include nurse safety, morale pressure, and lack of resources. Continuous education and professional support for every nurse is essential for effective nursing care.
b) Write down the difference between endogenous depression and neurotic depression. Write the difference between endogenous depression and neurotic depression.
1.Based on Origin:
Endogenous Depression:
This type of depression is caused by internal physical or neuro-biological causes, such as chemical imbalance in the brain.
Neurotic Depression:
This type of depression is usually caused by external factors such as tension, problems with close relationships, or ups and downs in life. occurs.
2. Severity of Symptoms:
Endogenous Depression:
Symptoms are very severe, including sleeplessness, loss of appetite, loss of interest in life, and thoughts of suicide.
Neurotic Depression:
Symptoms are usually mild to moderate and the person expresses their sadness.
3. Mood Mood Reactivity:
Endogenous Depression:
The person’s mood does not react. That is, the mood does not improve even with good news or a good environment.
Neurotic Depression:
The person’s mood can change according to the situation. In a good environment, the mood improves for a while.
4. Insight into the disease:
Endogenous Depression:
Often a person does not have a complete understanding of the disease. He cannot consider himself sad.
Neurotic Depression:
The person can explain the reason for his sadness and understands that he is depressed.
5.Treatment:
Endogenous Depression:
Anti-depressant drugs are usually required.
Neurotic Depression:
Psychotherapy, counseling and stress management more Effective.
6. Family History:
Endogenous Depression:
A family history of depression is common.
Neurotic Depression:
There is usually no family history but personal life events affect it.
Endogenous depression depends on internal and body-related factors, while neurotic depression is caused by external stress and life events. Occurs due to events. The symptoms and treatment of both are different.
c) Lithium toxicity Lithium toxicity:
Lithium toxicity:
Introduction:
Lithium toxicity is a condition where the level of lithium in the patient’s blood increases and it causes severe effects on the neurological, cardiac and gastrointestinal systems. Lithium is a drug used as a mood stabilizer, especially for bipolar disorder, but since its therapeutic index is very small, even a slight increase in dosage can cause toxic effects.
Normal level of lithium:
Therapeutic level: 0.6 – 1.2 mmol/L
Toxic level: >1.5 mmol/L
Severe toxicity: >2.0 mmol/L
Types of lithium toxicity:
1.Acute lithium toxicity:
Occurs when a new patient is taking a high dose of the drug. Symptoms are mainly gastrointestinal such as vomiting, nausea, diarrhea, etc.
2. Chronic Lithium Toxicity:
It occurs when the patient has been taking lithium for a long time and the lithium level gradually increases. Neurological symptoms are evident.
3. Acute-on-Chronic Lithium Toxicity:
It occurs when the patient has been taking lithium for a long time and suddenly takes a high dose for some reason. It has both gastrointestinal and neurological symptoms.
Symptoms:
- Gastrointestinal:
- Vomiting
- Loss of appetite
- Stomach pain
- Diarrhea
- Neurological:
- Confusion
- Ataxia – Unsteadiness in walking
- Tremor
- Seizure
- Coma
- Cardiac:
- Arrhythmia
- Bradycardia
- Effect on Urinary System:
- Polyuria
- Dehydration
- Acute Kidney Injury
Causes:
- If you take too much lithium
- Impaired kidney function Occurrence
- Dehydration
- Concomitant use of drugs such as Thiazide Diuretics, NSAIDs, ACE Inhibitors
- Overdose
Diagnosis:
Measuring blood lithium levels
Checking electrolytes, creatinine
Knowing the condition of the heart through ECG
Neurological assessment
Treatment:
1. For mild toxicity:
- Stopping lithium
- Improve hydration (by oral or IV fluids)
- Close monitoring of blood levels
2. For moderate to severe toxicity:
- Stopping lithium
- Give IV Normal Saline
- Perform hemodialysis – especially when lithium levels are >2.5 mmol/L, or neurological symptoms are serious
Prevention:
- Check lithium dosage regularly
- Advise patient to stay hydrated
- Monitor kidney function
- Avoid interacting medications
- Monitor lithium levels regularly To do
Lithium toxicity is a serious condition that can be avoided if recognized promptly and treated appropriately. Regular follow-up of the patient, blood monitoring and proper medical supervision are essential.
Q-4 Write short notes. (any three) Write a short note. (any two)12
a) ECT.- ECT
Introduction:
Electroconvulsive Therapy (ECT) – Electroconvulsive therapy is a medical mental health treatment in which a controlled electrical current is passed through the patient’s brain to induce a therapeutic seizure. This therapy is mainly used for patients who have mental health conditions such as severe depression, bipolar disorder, schizophrenia or catatonia and have not been relieved by other treatments.
History and uses:
ECT was first developed in Europe in 1938. Before that, options for severe mental disorders were very ineffective. Today, ECT is administered in a safer, more controlled, and more modern manner, using general anesthesia and muscle relaxants.
Procedure:
1. Pre-evaluation:
Before starting ECT, the patient’s medical history, physical examination, blood tests, ECG, (ECG), and often brain imaging tests (such as MRI) are taken.
2. Anesthesia and Muscle Relaxant:
The patient is placed under general anesthesia so that he does not feel any pain. Muscle relaxants are also given so that the muscular movements of the body are controlled during the seizure.
3. Placement of electrodes: Electrodes are placed on the scalp – either bilaterally or unilaterally.
4. Electrical stimulation: A controlled electrical current (such as 70-120 volts for 0.7 seconds) is given. As a result, the patient’s brain experiences a known and therapeutic seizure.
5. Post-procedure Monitoring: The patient is monitored in the recovery area after ECT, keeping in mind the condition. The patient wakes up in a very short time.
Frequency of Sessions:
A typical ECT consists of 6 to 12 sessions, which are given two or three times a week. In special cases, maintenance ECT may also be given, in which treatment is continued over the long term.
Indications:
- Treatment-resistant Depression
- Severe Suicidal Tendency
- Severe Catatonia
- Psychotic Depression
- Atypical Response to Therapy
Benefits:
- Rapid treatment results
- Immediate effect in severe cases
- Improvement in patient’s mood, expectations and behavior
- Possibly less need for medical drugs
Possible Side Effects:
- Immediate loss of orientation or disorientation
- Temporary memory loss, especially for recent events
- Headache
- Vomiting or nausea
- Fatigue
Rare Complications:
- Heart Rhythm Abnormalities (Cardiac Arrhythmia)
- Respiratory Depression
These complications are very rare and are mainly seen in high risk patients.
Myths vs Reality:
- Many people believe that ECT is atrocious, but today’s method is very safe and medically acceptable.
- ECT causes permanent memory loss – this is also a misconception. Most patients are able to lead normal lives.
- Electroconvulsive Therapy (ECT) is a modern medical psychiatric intervention that often proves to be a turning point in the patient’s life.
b) Occupational therapy Occupational therapy
Definition:
Occupational therapy is the art and science of selected activities. It is designed to restore and enhance a person’s functional abilities using goal-oriented activities for the assessment and treatment of individuals with psychological, physical, or developmental disabilities. Occupational therapists Works with individuals, families, groups, and communities.
Goals of Occupational Therapy:
- Promote recovery.
- Prevent hospitalization.
- Develop good work and leisure habits.
- Boost self-confidence.
Indications for Occupational Therapy (Uses):
- Depression
- Chronic schizophrenia
- Anxiety disorders
- Manic disorders
- Paranoid schizophrenia Schizophrenia)
- Catatonic schizophrenia
- Antisocial personality disorder
- Dementia
- Substance abuse
- Childhood disorders (Childhood Disorders)
Classification of Activities:
1. Diversional Activities (Diversional):
- Organized games (organized games).
2. Remedial Activities:
- Specific muscle groups.
- Examples:
- Physiotherapy.
- Basket making.
- Basket making.
- Candle making (Candle making).
- Weaving (weaving work).
- Tailoring (tailoring).
- Gardening (Gardening).
Principles of Occupational Therapy (Key Principles):
- Select activities that are based on the client’s interests, IQ level, strengths, and abilities.
- Utilize available resources.
- Plan short-term activities that boost self-confidence (Helps to increase self-confidence).
- Provide reinforcement even for small achievements.
- Design activities that provide new experiences and improve daily living skills.
Nurse’s Role in Occupational Therapy:
- Diagnose strengths, abilities, and talents.
- Select appropriate activities in coordination with other therapeutic team members.
- Educate clients to develop new skills.
- Identify problems that demand change.
- Promote socialization and help develop positive interests in the client.
c) Bleuler’s 4 A’S – Bleuler’s
Bleuler’s 4 ” A “:
1. Associative disturbance or looseness: This is a thought disorder. Such a person cannot think logically. 2. Affect disturbance: In this, there is disturbance in the patient’s mood, i.e. the patient’s mood is flat or blunt. 3. Ambivalence: Showing opposite feelings and desires towards the same person, thing or situation. 4. Autistic thinking: This is a thought disorder. In this, the person gets lost in dreams and is not aware of the surrounding environment.
d) Nursing management of violent patient
Nursing Management of Violent Patient:
1. Assessment of Patient Behavior:
-
- Assessment of the patient’s behavior to identify signs of aggression, anger, and violent behavior. Identify the level.
-
- Note trigger factors and previous violent history.
-
- Complete assessment of the patient’s mental and physical condition.
2. Therapeutic Communication:
-
- Talk to the patient in a calm, gentle and clear voice.
-
- Building a trusting relationship (Therapeutic Relationship).
-
- Avoiding negative tone and punishing language.
3. De-escalation Techniques:
-
- Maintaining personal space and trying to control the patient by giving them choices.
-
- Calm the patient through communication.
-
- If the situation worsens, quickly inform the helper staff.
4. Use of Medication:
-
- Give medication like sedatives or antipsychotics under medical advice.
-
- On the patient To observe the effectiveness of medication.
5. Physical Restraint and Safe Environment:
-
- If necessary, use physical restraint and a secure environment.
-
- All measures must be taken under legal and medical guidance.
6.Monitoring and Documentation:
- Continuous monitoring of patient behavior, interventions, and responses.
- Properly documenting each action.
7.Communication with Family:
- Maintain cooperative communication with the patient’s family.
- Provide information about therapeutic interventions.
8. Final Objective:
- Understand the patient’s violent behavior, calm it down, and provide humane and safe care.
Q-5 Define the following (any six)12
a) Dysthymia:
Dysthymia, also known as Persistent Depressive Disorder, is a chronic mood disorder in which a person experiences mild but persistent symptoms of depression such as apathy, fatigue, loss of energy, and Lack of energy, and loss of self-confidence. It is not as severe as clinical depression (Major Depressive Disorder) but affects the quality of life in the long run. Treatment includes anti-depressants and psychotherapy.
b) Regression – Regression:
regression is an immature way of responding to stress Some people are unable to face life’s challenges courageously. At such times, they reduce anxiety by behaving like people younger than their age. In this, the person behaves as if he or she is at the next developmental level instead of reality.
Some regressions are normal, such as tears coming from overly emotional reactions. Extreme forms and degrees of regressions result in psychosis.
Ex. After the birth of a new born baby in the family, due to less attention being given to the child, this child starts doing infantile behavior like bed wetting.
c) Acrophobia – Acrophobia:
Acrophobia is a specific phobia in which a person feels unbearable and excessive fear of heights, due to which the person experiences panic attacks and activities to avoid high places. This fear is more than the intensity of the actual danger and if not treated properly, it can affect the quality of life. Cognitive Behavioral Therapy, Exposure Therapy and Anti-Anxiety Medication can be useful in its treatment.
d) OCD:
Thoughts are repeated despite the person’s unwillingness and all this happens in the waking state. Which causes Anxiety and Fear. For example, a person has frequent thoughts of contamination by insects and despite not wanting to, they constantly repeat purposeless actions and cannot control them.Example: washing hands frequently, checking whether the door is locked or not.
OR
OCD stands for Obsessive Compulsive Disorder. This is a long-lasting disorder in which the patient has uncontrolled and repeated thoughts and these thoughts are seen in the form of action, that is, in their behavior. For example, a person washes their hands frequently after touching something because they think they have germs on their hands.
e) ADHD – ADHD:
ADHD stands for Attention Deficit Hyperactivity Disorder, which is a neurodevelopmental disorder. It is characterized by symptoms of inattention, hyperactivity, and impulsivity. This condition affects the educational, social, and occupational lives of children and adults. Treatment includes behavioral therapy, parent training, educational support, and stimulant medication.
F) Delusion of reference:
Delusion of reference is a delusional condition in which a person believes that common events, television shows, newspaper articles, or other people’s actions are specifically about or refer to them, even though they have no such connection. This delusion is commonly seen in mental illnesses like schizophrenia, delusional disorder.
g) Dissociate fugue:
Dissociative fugue is a rare but severe dissociative disorder in which a person unintentionally engages in travel behavior to an unknown place and forgets their identity and past. In this condition, the person has no memory of what they did or where they went. The person can usually adopt a new identity at this time. This condition is usually caused by severe mental trauma and may be associated with schizophrenia or other severe mental disorders. Medical and psychotherapy-based treatment is essential for dissociative fugue.
h) Hypochondriasis:
Hypochondriasis is a psychiatric condition in which a person has a false and persistent belief that they have a serious and life-threatening physical disease, when no such disease is found in medical assessment. The person perceives normal physical symptoms as signs of a serious illness and repeatedly seeks medical assessment, but is unable to find a solution. This condition is now known in modern medical terminology as Illness Anxiety Disorder. Hypochondriasis is commonly seen as part of the anxiety spectrum and affects a person’s daily life, behavior, and social interactions. Cognitive Behavioral Therapy is considered important for its effective treatment and sometimes anti-anxiety medication is also used.
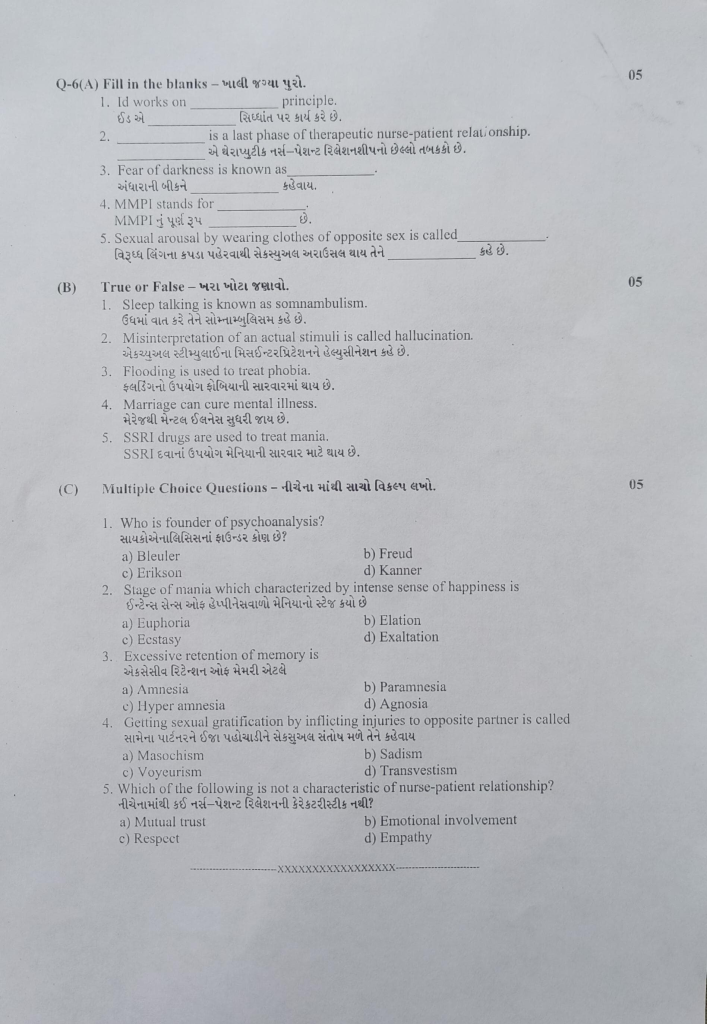
Q-6(A) Fill in the blanks – Fill in the blanks.05
1.Id works on……… principle. The id operates on the principle of pleasure.
2………….is a last phase of therapeutic nurse-patient relationship.Termination
3.Fear of darkness is known as……….. Fear of darkness is known as……… : Nyctophobia
4.MMPI stands for……… The full form of MMPI is…… : Minnesota Multiphasic Personality Inventory
5.Sexual arousal by wearing clothes of opposite sex is called…….. Sexual arousal by wearing clothes of opposite sex is called……… : Transvestism
B) True or False – Tell the truth. 05
1.Sleep talking is known as somnambulism. Sleep talking is called : ❌ False. Sleep talking is called Somniloquy, while Somnambulism means sleepwalking (sleepwalking upside down).
2.Misinterpretation of an actual stimuli is called hallucination. : ❌ False .This is called Illusion, not hallucination. Hallucination is perception without external stimulus.
3.Flooding is used to treat phobia. Flooding is used to treat phobias :✅ True. Floodingis a behavioral therapy technique used for phobia by exposing the person directly to the feared object.
4.Marriage can cure mental illness. Marriage improves mental illness :❌ False Marriage is not a treatment or cure for mental illness. It may help support but cannot replace therapy or medication.
5.SSRI drugs are used to treat mania. SSRI drugs are used to treat mania. : ❌ False SSRIs (Selective Serotonin Reuptake Inhibitors) are primarily used for depression and anxiety, not for treating mania.
(C) Multiple Choice Questions Write the correct option from the following.05
1. Who is the founder of psychoanalysis? Who is the founder of psychoanalysis?
a) Bleuler
b) Freud
c) Erikson
d) Kanner
✅ Correct Answer: (b) Freud
Explanation: Sigmund Freud is considered the father of psychoanalysis.
2.Stage of mania which characterized by intense sense of happiness is What is the stage of mania characterized by intense sense of happiness?
a) Euphoria
b) Elation
c) Ecstasy
d) Exaltation
✅ Correct Answer: (a) Euphoria
Explanation: Euphoria is a mood state of exaggerated well-being often seen in early mania.
3.Excessive retention of memory is
a) Amnesia
b) Paramnesia
c) Hyperamnesia
d) Agnosia
✅ Correct Answer: (c) Hyperamnesia
Explanation: Hyperamnesia refers to abnormally vivid or complete memory recall.
4.Getting sexual gratification by inflicting injuries to opposite partner is called injury to opposite partner Getting sexual satisfaction by reaching out is called
a) Masochism
c) Voyeurism
b) Sadism
d) Transvestism
✅ Correct Answer: (b) Sadism
Explanation: Sadism is a paraphilia involving pleasure from hurting others.
5.Which of the following is not a characteristic of nurse-patient relationship? Which of the following is not a characteristic of the nurse-patient relationship?
a) Mutual trust
b) Emotional involvement
c) Respect
d) Empathy
✅ Correct Answer: (b) Emotional involvement
Explanation: Therapeutic relationship should avoid deep emotional involvement to maintain professionalism.