ENGLISH-GNM-SY-CHILD HEALTH NURSING (CHN)-PAPER SOLUTION-12/06/2025 (DONE)-NO.11
(CHN)-PAPER SOLUTION-12/06/2025 -NO.11
Q-1 a) Define pediatric nursing. Define pediatric nursing.03
PEDIATRIC NURSING:
Pediatric nursing is a branch of nursing. It provides holistic nursing care to children from CONCEPTION to adolescenceage. Its main goal is to ensure proper growth and development of children and to develop their physical, mental and social well-being. In pediatric nursing, preventive, promotive, curative and rehabilitative nursing care is provided to every child in this group.
b) Write qualities of pediatric nurse. Write the qualities of a pediatric nurse.04
Qualities of a Pediatric Nurse
A pediatric nurse is a nurse specially trained for the health care of children, who assists in the treatment and necessary healthcare services related to children from newborn to adolescence. The following are the main qualities that a pediatric nurse should have:
1. Compassion: Empathy and compassion
Compassion means caring deeply for the patient and trying to understand their suffering. Child patients are often unable to express their pain clearly, so it is very important for the pediatric nurse to understand their feelings and needs.
2.Patience: Patience and Calmness
Child patients are often scared, stressed, or uncooperative. Patience is a quality that helps the nurse remain calm in all situations. Being patient with children is essential for good treatment.
3. Communication Skills: Good communication skills
Communication skills are mandatory for a pediatric nurse. Nurses must be able to communicate clearly and effectively with child patients, their parents, and other healthcare professionals to facilitate the treatment process.
4. Observational Skills: Observational skills
Through observational skills, nurses can identify even the smallest symptoms of child patients. It helps in proper treatment by properly observing their respiration, temperature, body language, etc.
5. Clinical Knowledge: Scientific and medical knowledge
Clinical Knowledge is essential for a pediatric nurse. It covers topics like Developmental Stages, Immunization Schedule, Pediatric Dosing, and Emergency Response.
6. Adaptability: The ability to adapt to the situation
Adaptability is the ability where a nurse can work in rapidly changing situations. This quality is useful in making the right decisions when the health condition of a child patient can change rapidly.
7. Attention to Detail: Paying attention to every little detail
Attention to Detail means maintaining accuracy in medication dosage, symptom recording, reports, etc. Even a small mistake in a pediatric patient can cause a big problem.
8. Emotional Stability: Emotional balance
Through Emotional Stability, a nurse can work with a healthy mind even in stressful situations. When a patient’s health condition is poor, it becomes necessary to control one’s emotions.
9.Teamwork: Ability to work collaboratively
Teamwork is a quality in which nurses work together with doctors, other nurses, and healthcare staff. A good teamwork can make the patient’s treatment more effective.
10. Family-Centered Care Approach:
Family-Centered Care is a method in which the patient’s parents and family members are involved in the treatment process. Pediatric nurses educate parents about health and give them confidence.
Each of these qualities makes a pediatric nurse a suitable and better healthcare provider for the complete health care of a child patient.
c) Discuss nurse’s responsibilities in preventive pediatrics. 05
Nurse’s Responsibilities in Preventive Pediatrics:
Preventive Pediatrics aims to prevent, identify and control health problems that occur in the period before the birth of a child (antenatal period) to adolescence. Pediatric Nurses play a very important role in such preventive care. It is described in detail below:
1. Immunization Services:
Pediatric nurses help children get their immunizations on time. It provides information according to the correct schedule of the vaccine, the nurse administers the vaccine and provides information to the parents about its side effects.
2. Growth and Development Monitoring:
The nurse regularly observes the child’s weight, height and developmental milestones. If any delay is found, the parents and pediatrician are referred for timely diagnosis.
3. Parental Education:
The nurse provides education to parents about nutrition, hygiene, infection prevention, first aid, and home care. She teaches parents the proper methods of caring for a newborn baby.
4. Screening and Early Detection:
The nurse screens the baby for conditions such as visual defects, hearing loss, or congenital disorders. Early detection allows for early identification of serious conditions and timely treatment.
5. Nutritional Counseling:
Pediatric nurses provide appropriate nutritional counseling to parents and caregivers for problems such as malnutrition, obesity, and anemia. She explains the meal plan well and refers to the pediatrician when necessary.
6. Health Education:
Nurses involve children and parents in health education programs at schools and community levels. They provide information about personal hygiene, oral health, mental health, and sexual education.
7. Community Outreach and Follow-up:
Nurses reach out to children who cannot come to the health center. Through Community Outreach, nurses provide pediatric health services at home and follow-up on the results of previous treatments or referrals.
8. Infection Control and Hygiene Maintenance:
Nurses provide training and supervision in activities such as regular handwashing, sanitization, and proper waste disposal to prevent the spread of disease among children.
9. Mental and Behavioral Monitoring:
The nurse pays attention to the child’s behavior, emotional state, and mental response to education. Mental health issues such as anxiety, depression, ADHD, etc. are identified and referred in a timely manner.
10. Crisis Intervention:
Some children may have signs of domestic violence, bullying, or abuse. The nurse then performs appropriate crisis intervention and provides education for related safety and rehabilitation services.
Preventive Pediatrics is a field that is more than just treating illness – it is about taking measures before disease occurs. Pediatric nurses play a key role in bringing about positive change in this area. It provides long-term positive effects on the overall health and well-being of the child patient.
OR
a) Define growth and development of child. Define child growth and development.03
Growth
Growth is a physical maturation process in which the number and size of body tissues increase and the size or number of body organs increase. The increase in growth is due to cell division and the increase in the components inside the cells. The changes in the body due to growth are measured in inches/centimeters and pounds/kilograms. Growth is progressive and measurable, in which height and weight increase. Good nutrition helps in proper growth. Growth is seen according to age, so good food intake leads to good growth.
OR
Growth is the physical maturation in which the size and shape of various organs of the body increase. Which is seen due to the multiplication of cells and increase in intracellular substance. The change in growth can be measured in centimeters and kilograms.
Development :
Development is the process by which a child’s body matures functionally and physiologically. Development involves an increase in skills and capacity to function. It involves psychological, emotional and social changes. It is difficult to measure development, but it can be measured.
b) Discuss factors influencing growth and development of child. State the factors affecting the growth and development of a child.04
Factors Affecting Growth and Development:
Some factors that promote or inhibit the process of growth. There are two factors. Environmental Factors
Hereditary Factors
(1) Hereditary Factors
Genetic factors are important factors that affect the growth and development of a child. They affect height, body structure, skin color, eyes, and hair.
Which depends on the genes of the parents. If the height of the parents is high, then the height of their child will also be high, if the parents are highly intelligent, then their child will also be highly intelligent, like some factors that affect the child.
Some genetic diseases that affect the growth and development of the child such as thalassemia, hemophilia.
So the child also has a chromosomal abnormality along with that disease, in which Down is seen.
In addition to this, gender also affects the growth and development of the child. While male babies are heavier and longer than female babies, girls mature earlier than boys. But their height and weight are less compared to boys.
In race and nationality, different races also grow and develop at different times, and their physical characteristics vary depending on the national group.
(2) Environmental Factors
Prenatal Factors
The intrauterine environment affects the growth and development of the fetus
Maternal Malnutrition
If the mother does not take a proper diet during pregnancy and if she is anemic, then the intrauterine growth Retardation is seen, low birth weight, preterm baby and disturbances in its growth and development in later life.
Maternal Infection
Some intrauterine infections such as HIV, hepatitis which are transmitted to the fetus through the placenta and affect its growth and development. Due to which congenital anomalies and congenital infections are seen.
Maternal Substance Abuse
Some teratogenic drugs, when taken during pregnancy, can cause congenital malformations, and smoking, tobacco, and alcohol also affect growth and development.
Maternal Illness
Conditions like hypertension, anemia, heart disease, hypothyroidism, diabetes, chronic renal failure, hyper pyrexia etc. which affect the growth of the fetus. If iodine deficiency is found in the mother, then the baby may suffer from mental retardation.
Miscellaneous
Prenatal conditions that affect the growth of the fetus. Which affects growth and development like uterine malformation, malposition of the fetus, bicornuate uterus, oligohydroamnios, polyhydramnios etc.
Postnatal Environmental Factors
Growth Pattern
Growth pattern is according to the size of the baby at birth. If the baby has a low birth weight, then complications may occur later.
Nutrition
Nutrition is very important for the growth and development of the baby. It should be quality and quantitative nutrition. It should contain protein, carbohydrates, vitamins, fats and minerals in sufficient quantities which help in the growth and development of the baby. If the baby is well nourished, then physical and mental growth is seen to be good.
Childhood Illness
Heart disease, kidney, liver malignancy, digestive disorders, metabolic disorders, etc. affect the growth and development of a child.
Physical Environment
Environmental conditions such as housing, living conditions, environmental sanitation, ventilation, fresh air, hygiene, safe water supply, etc. are essential for growth and Development
affects.
Psychological Environment
A good psychological environment such as a healthy family, a good relationship between the child and the parents, and healthy interactions with other family members helps in emotional, social, and intellectual development. If a child does not get the proper love, affection, and security, he or she becomes emotionally disturbed.
Cultural Influence
Culture affects growth and development. According to culture, its food habits, its beliefs, its living standard, education level, etc. affect growth and development.
Socioeconomic Status
Due to poor socio-economic status, a child cannot grow and develop properly and cannot get a proper nutritional diet.
Climate and Season.
Climate and season affect growth. Weight gain occurs in summer. Height increases in spring season compared to rainy season.
Play and Exercise
Play and exercise increase physiological activity and muscular development, as well as physiological, social, moral, intellectual development, and physical exercise improves health.
Intelligence
Which affects mental and social development. If a child has high intelligence, he will be able to adapt to the environment. If there is low intelligence, then it will not be able to be exhausted.
Hormonal Influence
Hormones greatly affect the growth and development of the child. Due to imbalance in them, problems are seen in growth and development.
c) Describe baby friendly hospital initiative. 05
B. F. H. I. is promoted by WHO and UNICEF for the promotion, protection and support of breastfeeding.
The main goal for this is to provide exclusive breastfeeding to the child for six months and continuous breastfeeding as complementary feeding until the child is two years old.
A baby friendly hospital should have a policy prepared for the successful promotion of breastfeeding. Which policy should be implemented by the hospital staff and the mother for the promotion of exclusive breastfeeding to the child. The steps should be in the return. These steps are as follows.
- B. F. H.I. in the hospital There should be a written policy for this and every staff should be aware of it.
- Every staff working in the hospital should be aware of this policy and should be trained to implement this policy.
- According to this policy, every pregnant mother should be given complete information about the advantages of breastfeeding and breastfeeding.
The mother should be helped to breastfeed the child within half an hour after the birth of the child. - The mother should be explained about all aspects of best feeding and the mother should be educated to maintain lactation for the child. should be given.
The mother should be made to understand that her child should not be given any food or water other than breast milk for a period of six months. - According to this policy, the mother stays with the child continuously, i.e. the practice of the mother and the child staying together completely is called rooming in. This practice should be promoted.
The mother should be encouraged to breastfeed only when the child demands it. - The child should not be given any artificial pacifiers for breastfeeding.
The mother should be introduced to a group that supports breastfeeding and arrangements should be made for such members to meet the mother during discharge.
Q-2 a) List out accidents occur in child and explain about prevention of accidents in infants. Make a list of accidents that occur in children and explain the steps to prevent accidents in infants.08
Common childhood accidents.
Drown:
In which a child can fall into any water-filled space inside the house or can drown by falling into any water-filled space around the house.
To burn and to be scorched:
You can get burned by fire while cooking and by any hot object falling on or touching your skin.
Getting anything stuck in the eyes, ears, nose, or throat:
Small parts of a child’s toys and any loose objects in the house can cause these types of injuries.
Falldown injury:
A child may fall while standing up and walking. It can fall from the steps, and it is common to fall from the bed and get injured.
Bruises or cuts on the skin:
Such injuries can occur due to falling and hitting anything.
Poisoning:
If any non-edible items come within the reach of the child at home, the child can eat them and there is a possibility of poisoning.
To be bitten or injured by a bit:
A child can be bitten or injured by any snake, scorpion, or insect.
Electrical shock:
Electric shock can occur from electrical wiring and electrical appliances.
Fracture, dislocation, or sprain:
These types of injuries can occur when a child falls.
Suffocation or choking:
A child’s head gets caught in something and something is wrapped around their neck. This type of injury can occur due to falling.
Crush injury:
This type of injury can occur due to the child’s hands, feet and fingers getting stuck anywhere.
Sports injury:
Falls and hits during sports are common.
Road traffic accident ):
Child accidents can occur due to road traffic accidents and vehicle accidents.
- All the above accidents happen in children.
- Injuries like falls, electric shocks, burns, foreign body entrapment, drowning etc. are common during the infancy period.
- Toddlers and preschool children are Fall down injuries, sports injuries, road traffic accidents etc. are more common than injuries.
Measures for Accident Prevention.
- Inform the child’s parents about a safe environment so that they can take special care of things that can harm their children.
- Explain to the parents that as the child grows older, his/her mobility capacity will decrease. will increase and it becomes a high risk for any accident.
- Convince parents not to leave the child alone at any time and to supervise him/her constantly.
- Stay with the child during every activity of the child and assist him/her.
- Explain to take care that the electrical plugs and wiring in the house are not exposed.
- Explain to ensure that no small parts of the child’s toys are loose and that no other objects in the house are in a position that a small child can get into their hands so that foreign body exposure Risks can be reduced.
- Explain to be careful that no sharp objects are left lying around or lying around the house.
- Explain especially that hot items or cooking utensils should not be reached by the child.
- Explain especially that water containers are not full and that water tanks or tanks are not open around the house and in the house.
- Encourage the child to play in an open space or field for sports with supervision. Explain to the child not to play games in the home environment.
- Keep any cord or long objects that can get entangled in the child’s neck out of his reach.
- Never put any inedible or poisonous items in the food container and keep all these items under lock and key out of the child’s reach.
- If any container contains inedible items, label it with a danger label and explain to the child.
- Mother and father should take steps to prevent accidents in children and be safe Special education should be given for the environment. So that mortality and morbidity due to accidental injuries in children can be reduced.
b) Explain immunization schedule and nurse’s role in immunization. Explain immunization schedule and nurse’s role in immunization.04
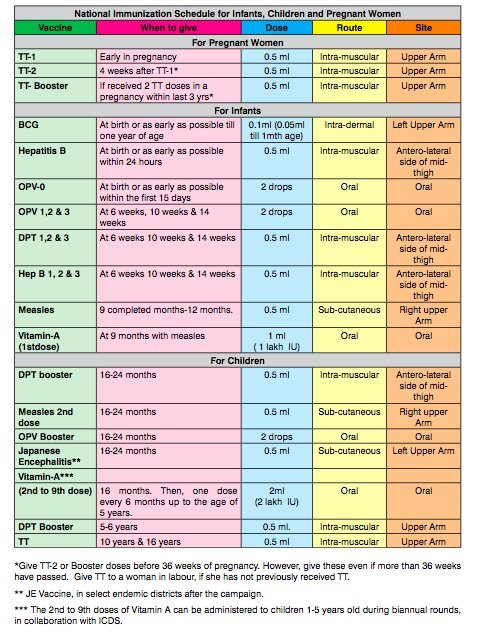
Nurse’s Role in Immunization:
Immunization is an important component of Preventive Healthcare, which is a key component of childhood immunization. Helps in preventing severe transmission of period diseases. Pediatric Nurse plays an important role in the successful implementation of the immunization program:
1. Vaccine Administration:
Nurses administer vaccines to children at the right age, in the right amount and through the right route. Such as using the intramuscular, subcutaneous or oral route. The necessary risks can be avoided by following sterile technique for each vaccine.
2. Guidance on Immunization Schedule:
The nurse provides information to parents about when to give the vaccine to their children according to the National Immunization Schedule or Universal Immunization Program (UIP) and reminds them not to miss any dose.
3. Vaccine Storage and Handling:
Vaccine To maintain effectiveness, it is necessary to store it according to the Cold Chain. The nurse stores the vaccine in the refrigerator at a temperature of 2°C to 8°C and maintains the potency of the vaccine by checking the Vaccine Vial Monitor (VVM).
4. Monitoring Adverse Reactions:
The nurse observes the child for adverse events following immunization (AEFI) such as fever, swelling, anaphylaxis, etc. Provides immediate intervention when necessary.
5. Health Education and Counseling:
The nurse explains to the parents the importance, advantages, and possible adverse effects of the vaccine. At the same time, the nurse reduces vaccine hesitancy by removing myths and misconceptions.
6. Record Maintenance:
The nurse keeps a record of the time, batch number, expiration date, etc. of each vaccine dose. Ensures tracking by updating the Immunization Card or digital record.
7. Participation in Mass Immunization & Outreach Services:
Pediatric nurses are extensively involved in national level camps like Pulse Polio Campaign, Measles-Rubella Drive etc. They help in delivering vaccines door to door by going out of the house.
8. Quality Assurance & Ethical Practice:
Nurses follow safety protocols and ethical standards at every step. Such as using scanned vaccines, using sterile needles, and ensuring informed consent from the patient.
Pediatric nurses act as a strong pillar in immunization. They not only provide vaccines but also play an important role in educating the family, maintaining safety and preventing the possibility of epidemics. A well-trained and responsible nurse can be a protection for the health of the child.
OR
a) Describe the impact of hospitalization on child and family. Describe the impact of hospitalization on a child and family. 08
Child reaction to hospital. (Child Reaction to Hospital).
- A child’s emotional reaction to the hospital depends on the type of stress and tension produced by the child’s illness and hospitalization.
- Illnesses that endanger the physical and mental development of children.
- Sickness restricts the child’s movement, prevents the child from sleeping properly, prevents the child from eating properly, and separates the child from the parents and home environment, which can lead to emotional distress in the child. Trauma occurs.
- Due to hospitalization and prolonged illness, the growth and development of the child also stops and adverse reactions are seen in the child. Child reaction to hospital depends on the age of the child.
1) Reaction of Neonate (Time from birth to 28 days)
- After the birth of the child, a different relationship is formed between the child and the mother. But when the child is hospitalized in the neonatal period, the relationship between the child and the mother is impaired.
- If the child is hospitalized in the neonatal period, the child does not have proper bonding with his family members.
- In the neonatal period, the child starts bonding with the people around him and if the child is hospitalized at the same time, then the bonding and trusting relationship also gets impaired.
- If the child is in the hospital, he stays away from his parents and due to being away, the parents lose love and affection for their child. Unable to provide care.
2) Reaction on infants (28 days to one year old)
- Separation Anxiety is seen in infants due to hospitalization.
- If an infant is hospitalized, the basic trust that should develop in the infant is disturbed.
- Emotional withdrawal and depression are seen in infants who are hospitalized.
- Growth and development in the child are delayed. Infants are afraid of strangers. Children cry excessively due to hospitalization.
- If a child is hospitalized during infancy, then the child becomes overly dependent on the mother.
3) Reaction to Toddler (Child aged one to three years)
- If a toddler is hospitalized, he protests against any object or procedure.
- The toddler’s hope is impaired and he tries to run away from anything.
If the toddler does not like a nurse during the hospitalization period, he cries so much on seeing the nurse that when the nurse comes to him to perform any procedure, the child starts crying. - At this time, the child keeps looking for his mother at any cost. If it is a toddler and he is hospitalized, the child shows anger and fear.
4) Reaction of Pre-school child (child from three to six years old)
- The emotional reaction of a pre-school child matches the emotional reaction of a toddler.
- Pre-school child shows regression, regression, projection, displacement, aggression, denial, withdrawal and fantasy.
5) Reaction of School aged children (6 to 12 years old child)
- In school age, children experience fear, anxiety, and various types of imagination, and children fear privacy.
- School age children use their defense mechanisms and react to hospitalization. Such as using defense mechanisms like repression and regression. Separation anxiety, negativism, depression, and phobia are seen in children.
6) Reaction of Adolescence (12 to 18 years)
- During adolescence, there is a lack of privacy and a fear of being separated from family and school. During this time, adolescents live in a state of insecurity.
- During adolescence, they get angry with anything, demand unwanted things, and reject treatment. Many people become depressed or refuse any kind of treatment.
Thus, different types of reactions are seen in children due to hospitalization.
a) Describe Impact of hospitalization on the Family of the child. (Impact of a child being hospitalized on his family and parents)08
Parents whose children are hospitalized not only feel separated from their children but also feel that other people are taking their place.
Furthermore, they feel a sense of inadequacy because other people are taking care of their children.
Due to the child being hospitalized, the unity of the family is also broken and the child is separated from his parents. The parents Anxiety and guilt are seen.
If a child is hospitalized, the stress level of their parents and family members increases.
1) Mainly due to many factors, the stress level of parents increases. Such as,
A) Parents do not have proper information or knowledge about what kind of illness their child has.
B) Parents are also afraid What kind of procedures are done with their child in the hospital.
C) Parents also fear what kind of treatment will be provided to their child.
D) Parents also fear what will happen to their child in the future, which increases the stress level of the parents.
E) When a child is hospitalized, the cost of his treatment can also be very high, due to which the financial burden comes on the parents, but the stress in the parents increases.
2) Many times parents feel guilty that their child’s illness is due to the parents not taking proper care of them and any kind of defect in the care of the child.
3) Parents of a child who is hospitalized feel anxiety, fear, disappointment, and the parents blame themselves.
4) When the child is treated, he is separated from his parents, due to which the parents feel helpless because they are not able to provide care to the child.
5) Many times, parents of hospitalized children also get angry with the health care personnel.
6) Parents also experience anxiety due to certain causes such as the strange environment of the hospital. Separation of parents and child. Child’s illness. Different types of procedures performed in the hospital. Unknown events and outcomes. Child suffering from any illness. Parents not being able to take care of their child.
b) Write down nurses’ role in preparation of child for diagnostic test/collection of specimens. 04
Nurses’ Role in Preparation of Child for Diagnostic Test / Collection of Specimens:
Diagnostic Test and Specimen Collection are very essential procedures for the diagnosis of a child’s disease. During this process, both the child and his parents are likely to be tense and afraid. The Pediatric Nurse then performs many important and professional responsibilities, through which the accuracy of the test results and the safety of the child are ensured.
1.Patient Education and Counseling
The nurse provides the child and parents with an advance understanding of which diagnostic test is to be performed, how it will be performed, and what its purpose is. To reduce fear and anxiety, the nurse speaks in simple language and also gives demos where necessary.
2. Physical Preparation before Test
Some tests require fasting (such as Fasting Blood Sugar, Lipid Profile), while some require drinking water or stopping stool excretion according to clear guidelines (such as Urine Culture, Stool Examination). The nurse ensures all this and provides timely guidance to the parents.
3. Preparation of Equipment and Supplies
The nurse keeps all the necessary equipment such as Syringes, Vacutainers, Sterile Containers, Swabs, etc. ready for the relevant test. Everything must be sterile and processed according to Aseptic Technique.
4. Emotional Support and Distracting Techniques
Diagnostic procedures can be frightening for a child when they are verbal or invasive. The nurse adopts distraction techniques such as putting on a play, telling a story or showing a video, etc. Along with this, they try to hide it by providing emotional support.
5.Proper Positioning and Assistance:
It is necessary to do proper positioning according to the age of the child and the type of test: such as Lateral Knee-Chest Position for Lumbar Puncture, Sitting Position for Throat Swab, etc. The nurse ensures the position and also involves the parents to keep the child under control.
6. Proper Collection and Transport of Specimen:
The nurse collects specimens such as Blood, Urine, Stool, Sputum, Throat Swab, CSF (Cerebrospinal Fluid) etc. using the appropriate method and according to the requirement of the specimen. Then it helps in labeling it properly and sending it to the laboratory on time.
7.Universal Precautions and Infection Control:
During each test or specimen collection, the nurse follows Universal Precautions by wearing Gloves, Masks, Aprons, etc. Along with this, proper disposal of the used equipment is also done, so that cross-infection can be avoided.
8. Post-Procedure Care and Observation:
After the test, the child may feel tired, confused or unwell. The nurse immediately monitors vital signs and intervenes immediately if any adverse reaction is observed. Also explains to the parents what to watch out for.
9. Report Follow-Up and Parental Communication:
The nurse follows up on the test report and informs the doctor. The parents are also informed and understand the next steps.
The work of a pediatric nurse during diagnostic tests and specimen collection is not only technical, but also important at a social, emotional and educational level. An efficient nurse makes the experience more comfortable and safe for the child, as well as being helpful for accurate and timely diagnosis of disease.
Q-3 Write short answer (any two) Write a short answer. (any two) 6+6-12
a) Define Protein Energy Malnutrition and write down nursing management of PEM. Define protein energy malnutrition and write the nursing management of PEM.
Protein Energy Malnutrition (PEM)
Definition:
Protein Energy Malnutrition (PEM) is a nutritional problem in children, which was earlier known as protein calorie malnutrition (PCM), which is seen due to inadequate intake of protein and calories in the diet, resulting in impairment in the child’s growth, development and overall health.
The two main types of PEM are
1)Marasmus
2)Kwashiorkor
1)Marasmus:
PEM’s marasmus is caused by severe calorie deficiency, resulting in weakness, loss of muscle mass, and wasting of body tissues. Children with marasmus are usually very thin and have a “starved” appearance.
2) Kwashiorkor:
Kwashiorkor is a form of PEM that occurs due to severe protein deficiency despite adequate calorie intake.
Children with kwashiorkor have a swollen abdomen (edema) due to water retention, fatty liver, skin lesions, and stunted growth. Children with kwashiorkor are normal but have a higher body weight than those with marasmus.
Nursing management of PEM (Nursing of PEM) Management):
Management of a child with marasmus:
- Provide adequate nutritional supplements to the child,
- Provide adequate high calorie feeding to the child.
- Advise the child to consume nutritious food.
- Maintain adequate fluid and electrolyte levels of the child.
- Provide adequate ion supplements to the child.
- Advise the child to gradually increase his diet.
- Provide adequate antibiotic medicine if the child has any infection.
- Provide adequate psychological support to the child. Provide.
- Record the child’s weight daily.
- Advise the child to provide adequate breastfeeding.
- Provide nutritious food like green leafy vegetables, soup, banana, pulses, cereals, milk etc.
- Provide the child with a diet in small and frequent amounts.
- Provide adequate work and comfortable environment to the child.
Nursing Management of Kwashiorkor Child:
- Provide proper comprehensive support to the child.
- Properly assess the child’s nutritional status such as breast feeding, weaning, food habits, balanced diet,
Assess socioeconomic status. - Properly assess the child’s growth chart.
- Provide proper nutrition rehabilitation to the child. To do.
- Collaborate with other health care personnel for the child’s care.
- Advise the child’s parents to ensure adequate nutritious food intake.
- Properly maintain hydration status.
- Provide the child with properly prescribed medications.
- The child Provide proper psychological support.
- Provide complete information to the child’s parents about the causes of the disease, its symptoms and signs, and its treatment.
- Provide supplementary feeding to the child.
- Provide antibiotic medicine if the child has any infection.
- Provide adequate vitamins and mineral supplements to the child.
b) List out common health problems of children and discuss nursing management of diarrhea and vomiting occur in children. Make a list of common disorders seen in children and write the necessary nursing management for diarrhea and vomiting in children.
Common Health Problems in Children:
1. Diarrhea
2. Vomiting
3. Fever
4. Cold and Cough)
5.Ear Infection
6.Asthma
7.Allergy
8.Malnutrition
9.Skin Infection
10.Tonsillitis (Tonsillitis)
11. URI : Upper Respiratory Infection
12. Abdominal Pain
13. Conjunctivitis
14. Worm Infestation
Nursing Management of Diarrhea and Vomiting Vomiting in Children):
1. Maintain Hydration:
It is very important to maintain fluid balance in the child.
Give fluids in the recommended amount through ORS (Oral Rehydration Solution).
Give easily digestible fluids like Soup, Lemon Water, etc.
In moderate to severe cases, IVF (Intravenous Fluids) may be required.
2. Diet Management:
Give a bland diet such as khichdi, toast, rice.
If there is lactose intolerance, advise to avoid milk and dairy products.
Gently introduce the child back to normal food.
3.Monitoring:
Monitor Urine Output: Low urine output is a sign of dehydration.
Regular monitoring of temperature, pulse, and respiration is necessary.
Monitor whether the child is losing weight.
4. Rest and Comfort:
Provide a comfortable environment for the child.
If vomiting is continuous, maintain proper position to prevent aspiration.
5.Medication:
Give Anti-Emetic like Ondansetron as per doctor’s advice.
Give Anti-Diarrheal if necessary.
Give Zinc Supplementation for 10 to 14 days: As per WHO recommendation.
6. Infection Control:
Maintaining hand hygiene is very important.
Telling the child to keep used utensils, clothes, etc. separate and clean.
7. Parental Education:
Explaining to parents the symptoms of dehydration – such as dry tongue, less urine, shadows under the eyes, etc.
Giving guidance on how to give ORS, what to eat and what to avoid, etc.
8. Referral and Follow-up:
If severe symptoms such as continuous vomiting, bloody diarrhea (blood in loose motions) are observed, refer to the hospital immediately.
Schedule a time for a follow-up visit.
Note:
The main concern in diarrhea and vomiting is dehydration. Without timely diagnosis and proper nursing management, the condition of the child can become severe. Therefore, it is imperative to give proper attention at the primary level.
c) Explain congenital heart disease. Describe classification of heart disease. Define congenital heart disease. Describe the classification of heart disease.
Definition of Congenital Heart Disease:
Congenital Heart Disease is a heart condition that is present at the time of birth.These diseases are caused by impairment in the structures inside the heart, such as the ventricles, atria, valves, or blood vessels.
These types of diseases can cause obstruction, reverse flow, or overload in the normal blood flow of the heart. is.
Classification of Heart Disease:
Heart diseases are mainly of two types:
1.Congenital Heart Disease
This type of heart disease is present at birth.
Further Classification:
a) Acyanotic Heart Disease
Cyanosis is not seen in this type of heart disease.
Oxygenated Blood and Deoxygenated Blood are mixed in small amounts.
Examples:
- ASD (Atrial Septal Defect)
- VSD (Ventricular Septal Defect)
- PDA (Patent Ductus Arteriosus)
- Coarctation of Aorta
b) Cyanotic Heart Disease:
In this type of disease, cyanosis is seen due to oxygen deficiency in the body, especially as a bluish coating near the lips and nails.
Examples:
- TOF (Tetralogy of Fallot)
- Transposition of Great Arteries
- Tricuspid Atresia
- Total Anomalous Pulmonary Venous Return
2.Acquired Heart Disease:
This type of heart disease occurs in the later stages of life.
Its causes include infection, lifestyle, blood pressure or metabolic disorders.
Examples:
- Rheumatic Heart Disease
- Infective Endocarditis
- Myocarditis
- Cardiomyopathy
- Coronary Artery Disease (rare in children)
Congenital Heart Disease is a congenital disease of the heart, in which there are structural abnormalities. It is called Acyanotic and is classified as Cyanotic Heart Disease.
When Acquired Heart Disease develops during life and infection, diet, or lifestyle are responsible for it.
For Congenital Heart Disease, timely diagnosis, proper medical care, and if necessary, surgical intervention may be necessary.
Timely intervention makes normal development of the child possible.
Q-4 Write short notes. (any three) Write a short note (any three) 12
a) Pre-operative nursing care of child undergoing surgery – Pre-operative nursing care of a child undergoing surgery
Introduction:
When a child is admitted for surgery, the preparation before the surgery is very important.
Pre-operative Nursing Care is a nursing process in which the child is prepared physically, mentally and socially for the surgery.
This Care focuses on physical status, psychological preparedness, and family education from a surgical perspective.
Key Components of Pre-operative Nursing Care:
1. Complete Assessment:
- Asking about the child’s health history and allergies.
- To check vital signs such as pulse, temperature, blood pressure and respiration rate.
- To take samples for laboratory tests such as CBC, Blood Grouping, Clotting Time etc.
- Nursing Documentation should be complete and accurate.
2. Nil by Mouth (NPO – Nil Per Oral):
- The child should be stopped from eating and drinking for a certain period of time before surgery so that aspiration does not occur during anesthesia.
- Children are usually kept NPO for 6 to 8 hours before surgery.
3. Parental Counseling and Education:
- Giving parents complete information about the surgery – why the surgery is being done, how it will be done, how long it will take, etc.
- Giving information about anesthesia and surgical risks.
- Giving parents positive reassurance and listening to their questions and answering them.
4. Psychological Preparation:
- Managing the child’s feelings of fear, sleeplessness, crying, sadness, etc.
- Providing support for the emotional impact of pain or separation from the parent.
- Explaining the surgery to the family and child in simple language.
- Play therapy can be useful for young children.
5. Physical Preparation:
- Dress the child in a suitable hospital gown.
- Shave or clean the skin if necessary.
- Bath or skin cleansing to avoid the risk of infection.
- Mark the operative site (if (If there is an instruction).
- If necessary, I.V. Establishing a line.
6. Medication Management:
- Pre-medication is usually given as per the doctor’s order, usually sedatives or analgesics.
- There should be a clear order regarding whether to continue the previously taken medications (Routine Medications) or not.
7.Management of Valuables and Documents:
- Remove all jewelry, eyeglasses, dental appliances, etc.
- Fill in a consent form with the parents’ writings.
- Parental consent is usually mandatory for children.
8. Preparation for Transport:
- Make arrangements to transport the child to the operation theater properly.
- Send the necessary medication, documents and information with the parents.
- Pre-operative nursing care is a very important stage for the child which directly affects the outcome of the surgery.
Proper pre-operative preparation not only prepares the child physically but also mentally for the surgery and also reduces the recovery time. is.
b) Importance of breast feeding – Importance of breast feeding
Importance of Breastfeeding
Introduction:
Breastfeeding is the first and most important nutritional method of life for a newborn. It is scientifically called “Exclusive Breastfeeding” when the baby is given only breast milk for the first 6 months after birth and no water or food of any kind is given. Breastfeeding contains many important nutrients and immunological components.
Medical Benefits of Breastfeeding:
1.Benefits for the Infant:
Colostrum:
The thick yellow milk secreted in the first few hours and days after birth is called colostrum. This milk is rich in antibodies, which protect the infant from diseases like infection, diarrhea, and pneumonia.
Immunity:
The immunoglobulins, lactoferrin, lysozyme, etc. present in breast milk help in increasing the immunity of the infant.
Cognitive Development:
Research shows that neurological development is better in breastfed babies.
Lower risk of obesity and diabetes:
Breastfed babies are at a lower risk of type 1 and type 2 diabetes and childhood obesity.
2. Benefits for the Mother:
Uterine Contraction:
A hormone called oxytocin is released during breastfeeding, which quickly returns the uterus to its original size and helps in the contraction of the uterus after delivery. Reduces Postpartum Hemorrhage.
Lower risk of breast and ovarian cancer: Females who breastfeed for a long time have a reduced chance of developing this type of cancer.
Calorie Burn:
During breastfeeding, the mother burns approximately 500 calories per day, which is helpful in reducing weight after pregnancy.
Important Medical Recommendations: World Health According to the World Health Organization (WHO), a baby should be given only breast milk for the first 6 months after birth.
Complementary feeding should be started after 6 months and breastfeeding should be continued for at least 2 years.
Breastfeeding is not just a nutrition method, but the beginning of a healthy lifestyle for both mother and child. The nutrients, antibodies and hormones it contains contribute significantly to the physical and mental development of both. Every mother should encourage breastfeeding under medical guidance.
c) National child labour policy – National Child Labour Policy
National Child Labour Policy
Introduction:
National Child Labour Policy i.e. National Child Labour Policy – National Child Labour Policy Child Labour Policy is an important policy implemented by the Government of India in 1987. The main objective of this policy is to prevent child labour in the country and to provide children with proper education, health, and a happy childhood.
What is Child Labour?
Child labour is a condition in which children below the age of 14 are forced to do work that is harmful to their physical, mental, and social development. Such children are exploited and deprived of compulsory education.
Key Features of the National Child Labour Policy:
1. Prohibition of Child Labour:
According to this policy, it is completely prohibited for children below 14 years of age to work in hazardous industries (Hazardous Occupations).
For this, the Child Labour (Prohibition and Regulation) Act, 1986 was implemented.
2.Direct Action Plan:
In areas where the incidence of child labour is high, Special Schemes are implemented such as –
National Child Labour Project – NCLP (National Child Labour Project).
3. Education and Rehabilitation:
Special schools, healthcare, nutrition, and skill development are provided for children released from labor.
4. Awareness Campaigns:
Media Campaigns, Voluntary Organizations, and the government are working together to create awareness against child labor. Integrated programs are being implemented.
Recent Amendments:
According to the Child Labour (Prohibition and Regulation) Amendment Act, 2016, children below the age of 14 are now prohibited from all types of work, except if they help in non-hazardous work of the family.
Furthermore, the law has been made stricter to keep adolescents between the ages of 14 and 18 away from Hazardous Work.
The National Child Labour Policy is not just a legal policy, but an effort to secure the future of India’s children. Every child has fundamental rights to education, health and nutrition. This policy reflects the commitment of the Government of India to completely eliminate child labour and ensure a safe, healthy and educated future for every child.
d) ICDS functions – ICDS – Functions of ICDS
Functions of ICDS – Integrated Child Development Services
(Integrated Child Development Services):
ICDS stands for Integrated Child Development Services – implemented by the Government of India, which aims to provide comprehensive care to children aged 0 to 6 years, breastfeeding mothers and pregnant women. Ensuring nutritional, health and educational development.
Supplementary Nutrition:
Supplementary nutrients are given to pregnant women, breastfeeding mothers and children to prevent nutrient deficiencies. This includes key nutrients like protein, carbohydrates, vitamins and iron, which are very important for the health of the child.
Anganwadi Services:
Nutritious diet, health assessment and pre-school education are provided to children at Anganwadi centres. The programs here are designed for educational and social development.
Health Check-up and Early Detection:
Regular health assessments are conducted for children, pregnant women, and breastfeeding mothers. Among them, early diagnosis of fever, anemia, motor development disorders etc. is done and arrangements are made for referral.
Immunization:
Immunization is given to children and pregnant women at fixed times to provide protection from diseases like Polio, Measles, DPT, Tetanus etc. This work is done in coordination with the health department.
Health and Nutrition Education:
Breastfeeding mothers and other community members are provided with awareness and training on nutrition, infant feeding, lactation, nutrition, and hygiene. So that they can better manage their own and their child’s health.
Early Childhood Care and Education:
A framework for school readiness is created for children aged 3 to 6 years through play-based learning activities, stories, and educational toys. Special attention is paid to the mental and social development of the child.
Referral Services:
When a child or a breastfeeding mother is seriously ill or suffers from Severe Acute Malnutrition (SAM), they are immediately referred to a health center or high-level hospital for treatment.
Convergence with multiple departments for holistic child development:
ICDS offers various It creates a coordinated structure for the overall development of the child by coordinating with departments like Health, Education, Sanitation, Women & Child Development, Rural Development etc.
Q.5 Define following (any six) Write the following definition. (Any six) 12
a) Juvenile deliquency – Juvenile Delicacy
Juvenile delinquency is one of the most common problems of society.‘Juvenile’ means childhood and ‘delicacy’ means antisocial behavior or criminal behavior
Juvenile delinquency is a type of A criminal act that is usually committed by children and teenagers who are under the age of 18. Juvenile delinquency is illegal or antisocial repetitive behavior by a child that is usually committed by individuals under the age of 18. This juvenile delinquency can range from relatively minor crimes such as vandalism, shoplifting to more serious crimes including assault, drug offenses, and property crimes. This juvenile delinquency behavior involves lying, stealing, stealing from home, running away from school, running away from home, disobeying someone, fighting, looting, sexual assault, etc.
b) Low Birth Weight baby – Low Birth Weight baby Baby:
Low birth weight means that the weight of the child at the time of birth is less than 2500 gm, this condition is called low birth-weight baby (LBW).
In which, very low birth weight baby means that the weight of the child is 1500 grams or less, it is known as very low birth weight baby.
While, extreme low birth weight baby means that the weight of the infant is less than 1000 grams, this condition is called extreme low birth weight baby.
c) Leukemia – Leukemia:
Leukemia is the most common type of childhood malignancy. It is usually a cancer of the blood and bone marrow. It is characterized by persistent and uncontrolled production of immature and abnormal WBCs. This disease is usually caused by abnormal proliferation and maturation of the bone marrow, which interferes with the production of normal red blood cells, white blood cells, and platelets. Leukemia is a major neoplastic disease of childhood.
d) Mental retardation Mental retardation:
Mental retardation is also called “intellectual disabilities”. Mental retardation is the most severe condition in which a child’s cognitive and problem-solving skills are impaired. Also known as cognitive developmental delay. In which there are limitations in the child’s intellectual function and adaptive behavior. Mental retardation is a condition in which a child has difficulties in learning, thinking, problem-solving, reasoning, and understanding concepts compared to other children. These limitations can range from mild to profound. They can cause impairment in the child’s communication, socialization, and daily routine activities. Such a child needs continuous care and support to survive.
Classification of mental retardation.
There are four classifications of mental retardation.
1) Mild mental retardation,
2) Moderate mental retardation,
3) Severe mental retardation,
4) Profound mental retardation .
••>
1) Mild Mental Retardation:
In mild mental retardation, the child’s Iq level is 51 to 70.
In this case, the child is capable of doing his work under supervision.
He is also capable of doing school work.
In mild mental retardation, if proper training is provided to him, he can also do simple jobs. And can also earn.
2) Moderate Mental Retardation:
Moderate Mental The Iq level of a child with mental retardation is 39 to 50.
If proper training is provided to a child with moderate mental retardation, he can eat on his own, wear clothes on his own, and if toilet training is provided, he can perform his daily routine activities.
In moderate mental retardation, the child has difficulty in communicating. In this, if the child is provided with proper training, the child is able to do his work himself under supervision.
3) Severe Mental Retardation:
In severe mental retardation, the Iq level of the child is between 21 and 35.
In this, the child is not able to fulfill his physical needs.
In this, if the child is provided with training, he can do the simplest work.
In this, the child needs more supervision.
Severe mental retardation is identified during the early time of the child. In which the child’s motor development is poor, speech is delayed and communication skills are impaired.
4) Profound Mental Retardation:
In profound mental retardation, the child’s IQ level is below 20.
e) Mid-day meal program – Mid-day meal program:
Midday meal program (MDMP)( Mid-day meal Program)
The Mid-Day Meal Program is also called “School Lunch Program”. This program was introduced in the throwout country in 1961. Its main objective is to attract more children to school and reduce school dropout and improve the nutritional status and literacy rate of the child.
Beneficiaries:
Schoolgoing children
Aim of Mid-Day Meal Program:
1) To increase the child’s attention to school.
2) To reduce school dropout.
3) To improve the child’s nutritional status and health status.
4) To fulfill 1/3 of the child’s nutritional requirement.
5) To improve the child’s interest in school.
6) To reduce the child’s school dropout.
7) To attract more children to school.
Objective:
To enhance the child’s admission to school.
To improve the child’s attraction towards school.
To enhance the child’s attention in school.
To improve the child’s literacy rate.
To improve the child’s nutritional status.
To improve the child’s health status.
f) Down’s syndrome:
Down Syndrome is a genetic disorder, in which a person’s cells Cells have an extra copy of chromosome number 21, called Trisomy 21. This chromosomal abnormality affects the development of the brain and body. It usually causes intellectual disability, special facial symptoms, and developmental delays. It can also cause congenital heart defects and respiratory problems. This condition is congenital and has no diagnosis, but early intervention and special education can improve the quality of life.
g) Hypospadias:
Hypospadias is a congenital defect found in males. Hypospadias occurs when the opening of the urethra is on the underside of the penis instead of the tip. This can range from mild curvature to a more severe form where the opening is closer to the scrotum.
h) Enuresis – Enuresis:
Enuresis (bedwetting) is a common pediatric problem in which a child experiences frequent involuntary urination while sleeping. The condition of frequent involuntary urination while sleeping, when voluntary urine control should normally be achieved, is called enuresis and this condition is seen in a child even after 5 years. Enuresis (bedwetting) is also called nighttime incontinence.
Q-6(A) Fill in the blanks – Fill in the blanks. 05
1.Baby born with teeth it is known as……………. Answer : Natal teeth.
2.Infection of the middle ear is known as ………………… Answer: Otitis media
3.Mother’s first milk is called ……………….. Mother’s first milk is called……… Answer: Colostrum Colostrum is called.
4.World children’s day is celebrated on ……………………. World children’s day is celebrated on…………… day. Answer: It is celebrated on 14th November.
5.Oral thrush caused by…………….microorganism. Oral thrush is caused by the organism Candida albicans.
(B) Multiple Choice Questions – Write the correct option from the following. 05.
1. Commonly the vaccines are preserved at the temperature of
a) 2 to 8°C
c) -2 to -8°C
b) 8 to 10°C
d) 0 to 2°C
✔️ Correct Answer: a) 2 to 8°C
2. Rickets disease occurs in the children due to deficiency of
a) Vitamin A
b) Vitamin B
c) Vitamin C
d) Vitamin D
✔️ Correct Answer: d) Vitamin D
3. Weaning diet can be started from month of
a) 4 Months
b) 6 Months
c) 9 Months
d) 12 Months
✔️ Correct Answer: b) 6 Months
4. BCG vaccine should be given to the baby by this route
a) Intramuscular
b) Intravenous
c) Subcutaneous
d) Intradermally
✔️ Correct Answer: d) Intradermally
5. Anorexia nervosa commonly seen in
a) Male
b) Toddler
c) Female
d) Adolescent girl
✔️ Correct Answer: d) Adolescent girl
(C) Match the following.05
A B
- Tetanus 1.Interruption of flow of speech
- Stuttering 2.Lock jaw
- Xerophthalmia 3.Kernictus
- Anencephaly 4.Neurotubular defect
- Neonatal jaundice 5.Vitamin A deficiency
- Absent of cranial vault
✅ (C) Correct Answer (05)
| A | B | Correct Match |
|---|---|---|
| 1. Tetanus | 2. Lock jaw | 1 → 2 |
| 2. Stuttering | 1. Interruption of flow of speech | 2 → 1 |
| 3. Xerophthalmia | 5. Vitamin A deficiency | 3 → 5 |
| 4. Anencephaly | 6. Absent of cranial vault | 4 → 6 |
| 5. Neonatal jaundice | 3. Kernicterus | 5 → 3 |
🟢 Final Matching:
- Tetanus → Lock jaw
- Stuttering → Interruption of flow of speech
- Xerophthalmia → Vitamin A deficiency
- Anencephaly → Absent of cranial vault
- Neonatal jaundice → Kernicterus
