ENGLISH-FON:UNIT:6(PART:2)CARE OF PATIENT WITH ALTERED BODY TEMPERATURE-UPLAOD
Unit: 6 Therapeutic nursing care
Part: 2 : care of the patient with Altered body temperature (કેર ઓફ ધ પેશન્ટ વીથ અલ્ટર્ડ બોડી ટેમ્પરેચર):

Key terms(કી – ટર્મ્સ):
ફેબ્રીલ (Febril):

પેશન્ટ કે જે ફીવર માંથી સફર થતાં હોય તેને ફેબ્રીલ(Febril) તરીકે ઓળખવામાં આવે છે.
અથવા
પાઇરેક્સીયા માથી સફર થતા ક્લાઇન્ટ ને ફેબ્રીલ કહેવામાં આવે છે.
એફેબ્રીલ(Afebrile):
એવા ક્લાઇન્ટ કે જેનું બોડી નું ટેમ્પરેચર એ નોર્મલ રેન્જમાં હોય છે તેને એફેબ્રિલ(Afebrile) કહેવામાં આવે છે.
ફીવર/ પાઇરેક્સીયા (Fever / pyrexia):

બોડી નું ટેમ્પરેચર એ નોર્મલ રેન્જ કરતાં વધારે(More than normal range) હોય તેને ફીવર/પાયરેક્સિયા (Fever/ pyrexia)તરીકે ઓળખવામાં આવે છે.
હાઇપરથર્મીયા/ હાઇપરપાઇરેક્સીયા (Hyperthermia/Hyperpyrexia):
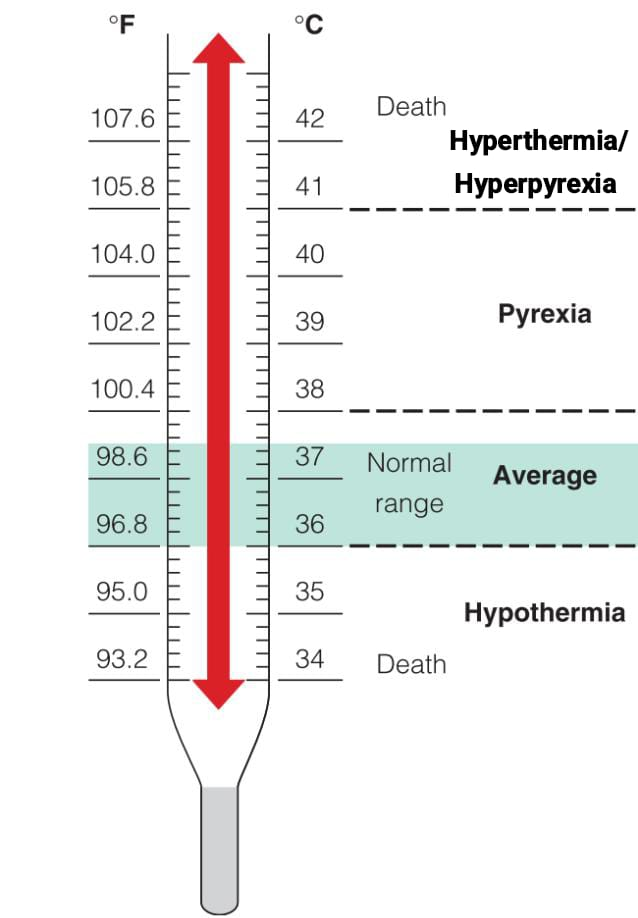
બોડી નું ટેમ્પરેચર ≥ 41°C/105.8°F ને હાઇપરથર્મીયા હાયપરપાયરેક્સિયા (Hyperthermia/Hyperpyrexia)તરીકે ઓળખવામાં આવે છે.
હાઇપોથર્મીયા(Hypothermia):
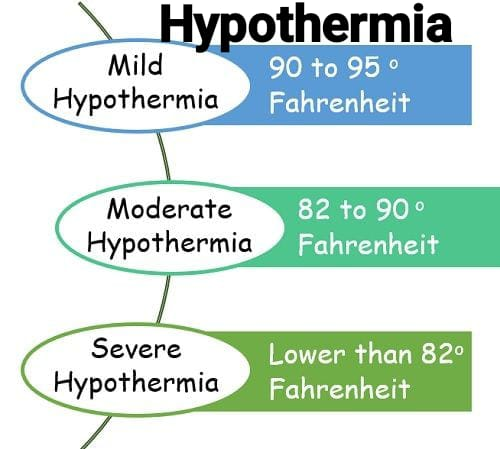
હાઇપોથર્મિયા એ એવી કન્ડિશન છે કે જેમાં બોડી ટેમ્પરેચર એ નોર્મલ વેલ્યુ કરતા ઓછું (Falls) હોય છે
Heat Stroke:
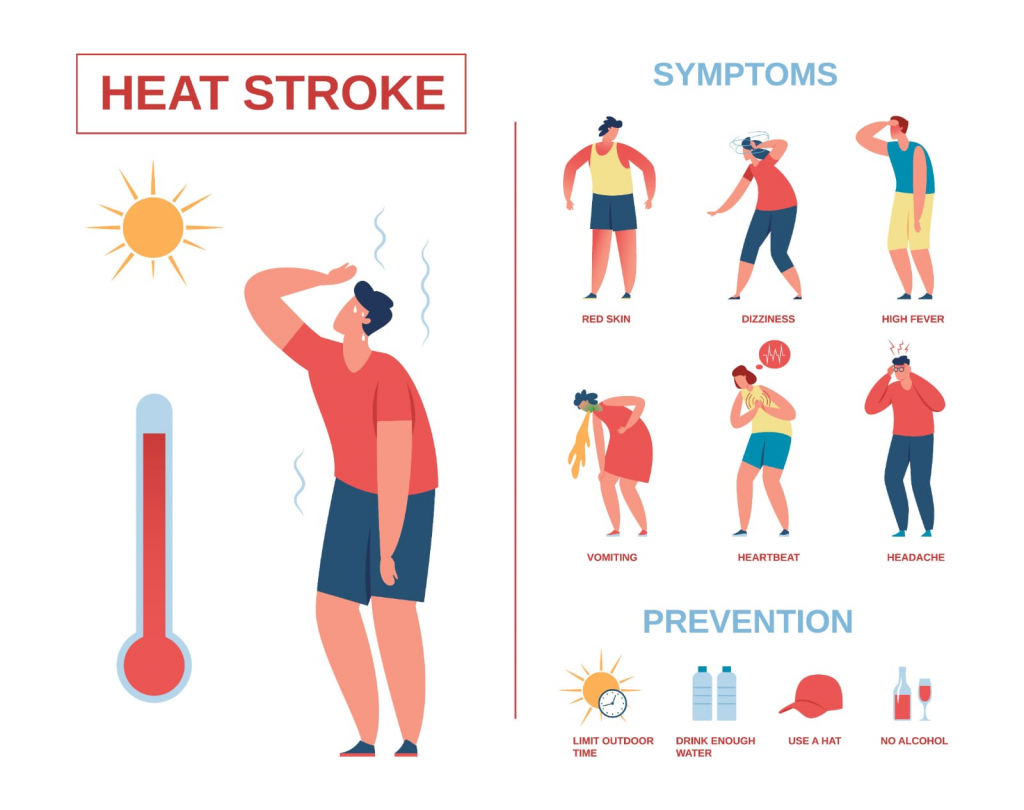
Heat stroke A one It is an emergency condition, which is characterized by elevated body temperature, which is caused by exposure to the sun or high environmental changes.
Fever Spike:
A rapid increase in temperature after normal temperature. The temperature returns to normal condition very quickly, i.e. within hours. This condition is known as Fever Spike.
Malignant Hyperthermia:
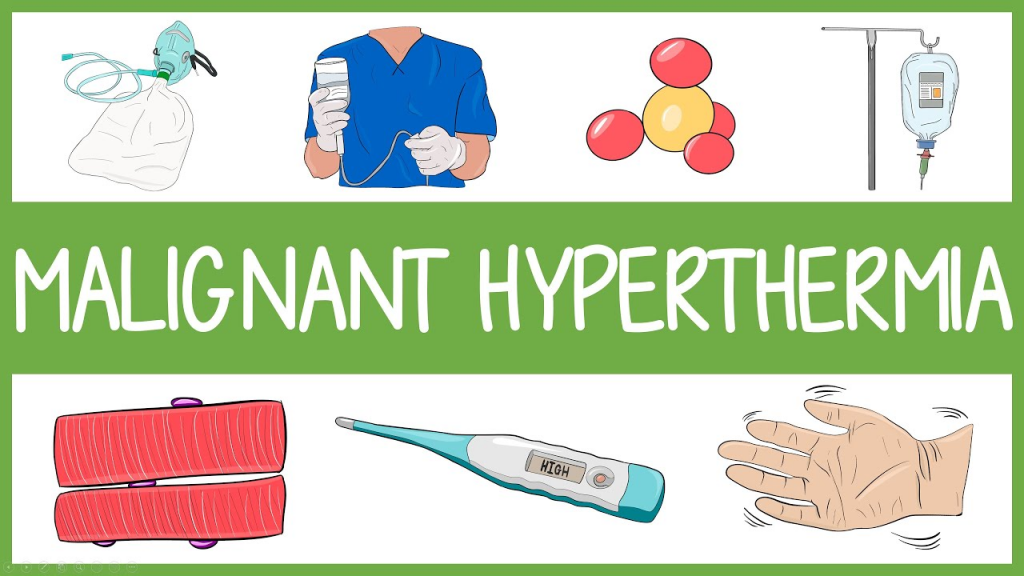
This is a hereditary condition of uncontrolled heat production, which occurs when the client receives anesthetic drugs.
Hot Application:

It is the application of dry/moist heat to the body parts for therapeutic purposes.
Cold Application:

It is the application of cold on body parts for therapeutic purposes.
Altered body temperature:
Introduction (Introduction):
Body temperature can vary for many reasons. The conditions associated with it are as follows:
Hyperpyrexia
Heat Stroke
Hypothermia
Hyperpyrexia:
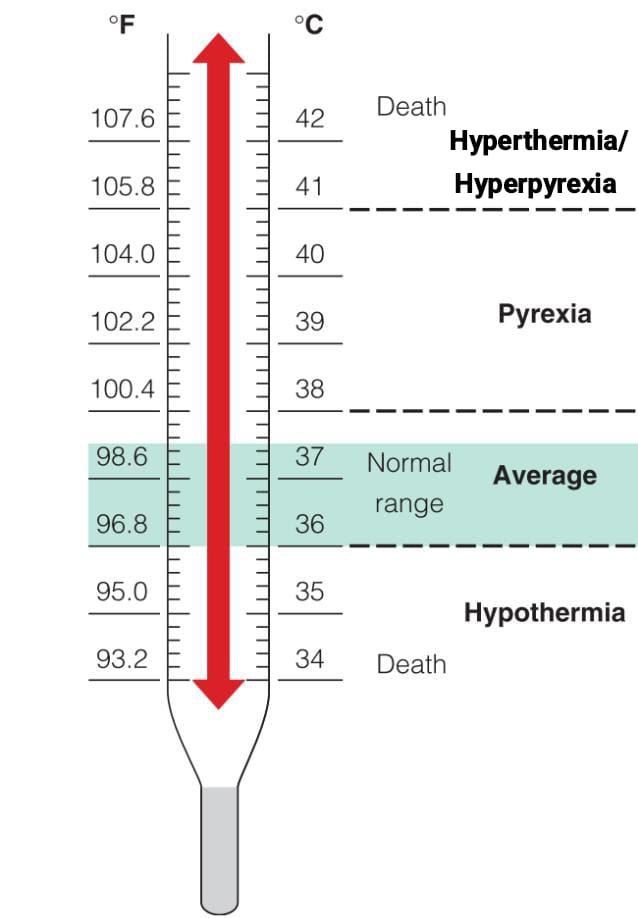
Hyperpyrexia is caused by changes in hypothalamic integration. Body temperature ≥ 41°C/105.8°F is known as Hyperthermia/Hyperpyrexia.
Pathophysiology:
- When a pyrogen (virus, bacteria) enters the body, it acts as an antigen and the immune system is simulated which increases the production of wbc. Then the antigen antibody reaction occurs and the hypothalamus is stimulated to raise the threshold.
- It takes hours for heat production and its conservation in the body and the body temperature to rise to a high threshold.
- During this time, the patient experiences chills, shivering, and cold despite the increase in body temperature.
- The chills will subside as soon as the body temperature reaches the new threshold. The patient feels warm and dry.
- With the body’s strong immunity or antibiotics, antigens such as bacteria and viruses will be destroyed.
- Then the new threshold of the hypothalamus will decrease.
- Then the loss of heat from the body starts.
- Warm and flushing of the skin (vasodilation) occurs.
- Then diaphoresis occurs.
- Fever is completely down.
- Afebrile condition occurs.
Clinical manifestations of fever:
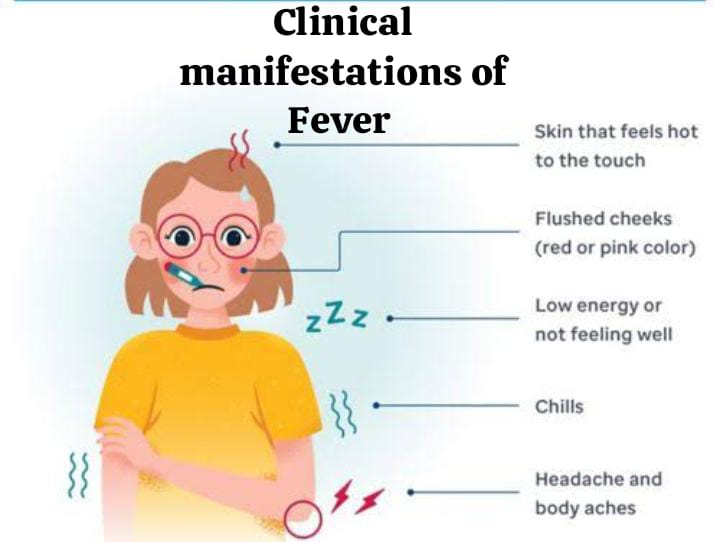
Initially:
Initially the following signs and symptoms are seen in the client such as,
- Increased heart rate.
- Complaint of cold. Complaint of feeling Cold. Increased Respiratory rate.
- Shivering, cold.
- Cyanotic nail beds.
- “Gooseflesh” on skin.
- Cessation of sweating.
During course of fever:
- Absence of chills.
- Warmth Feeling of Skin.
- Photosensitivity.
- Glassy eyed appearance.
- Increased pulse, Respiratory rate rate).
- Mild to severe dehydration.
- Drowsiness, Restlessness.
As fever subsides:
- Skin appears flushed.
- Sweating.
- Increased shivering.
- Dehydration.
- Increased thirst.
- Increased thirst.
- Loss Of Appetite.
- Muscles Aching.
- Weakness.
- Warmth Feeling of Skin.
Types of Fever:
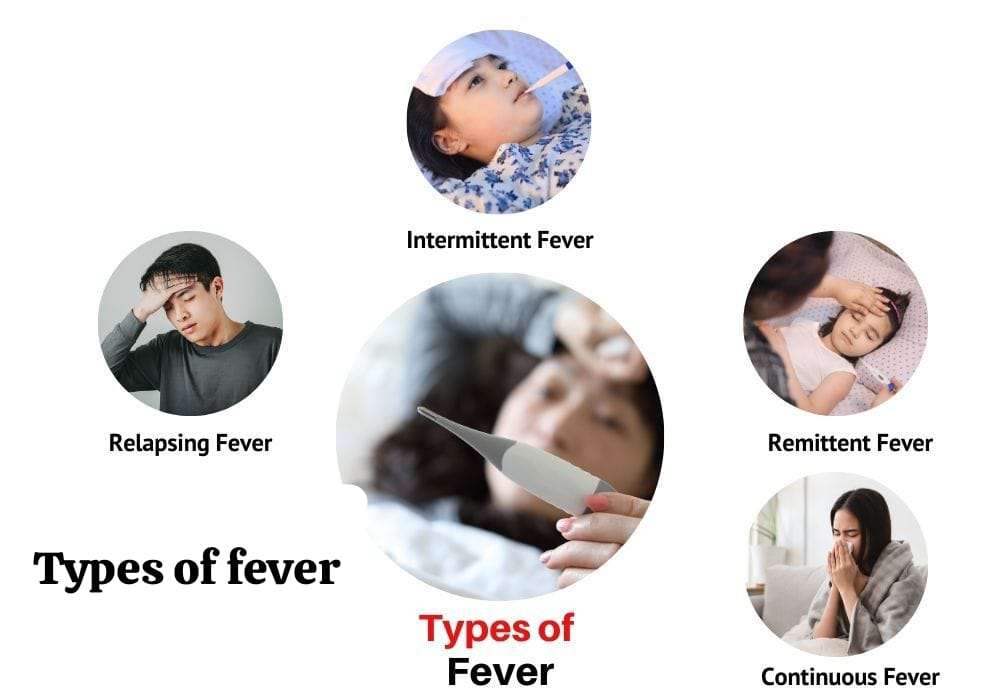
1) Intermittent Fever:
During this fever, the temperature is regular It alters at intervals and periods of normal or subnormal temperature are observed.
2) Remittent fever:
In this, the temperature fluctuates by more than 2°C in 24 hours. The temperature does not return to the normal range. The temperature in it always remains higher than the normal range.
3) Relapsing Fever:
There are short febrile periods for a few days. In which normal temperature is seen for 1-2 days.
4) Constant Fever:
In constant fever, temperature fluctuations are minimal but always remain above the normal range.
Nurse’s Action in Fever:

Nursing Assessment :
- Check the patient’s vital signs.
- Assess skin color and temperature.
- Properly check laboratory reports for WBC, hematocrit.
- Maintain room temperature according to client’s body temperature. Remove blanket when client complains of hot and warm sensation.
- Provide the patient with a blanket when the patient complains of severing or chilling.
- Provide the patient with a balanced diet and fluids.
- Maintain the patient’s intake-output chart.
- Maintain the client’s oral hygiene to keep the mucous membrane moist.
- Restrict the client’s activity level as it may cause Increases production.
- Provide sponge baths to enhance heat loss.
- Provide dry and clean clothing and bed linen.
- Provide prescribed analgesics and antipyretics to the patient.
Properly document.
Health protection Strategies:
Managing Fever:
- Rest.
- Maintain comfort and hygiene.
- Maintain hydration. Maintain.
- Maintain nutritional status.
Restorative Strategies
Measures to reduce heat production and facilitate heat loss:
Antipyretic Drug Therapy:
- Antipyretic drugs such as acetylsalicylic acid or acetaminophen are used to reduce the patient’s fever. These medications act on the heat regulating center but do not eliminate the cause of the fever.
- Rapid sponge bath,
Use of fan,
Hypothermia machine To use no.
Heat Stroke:
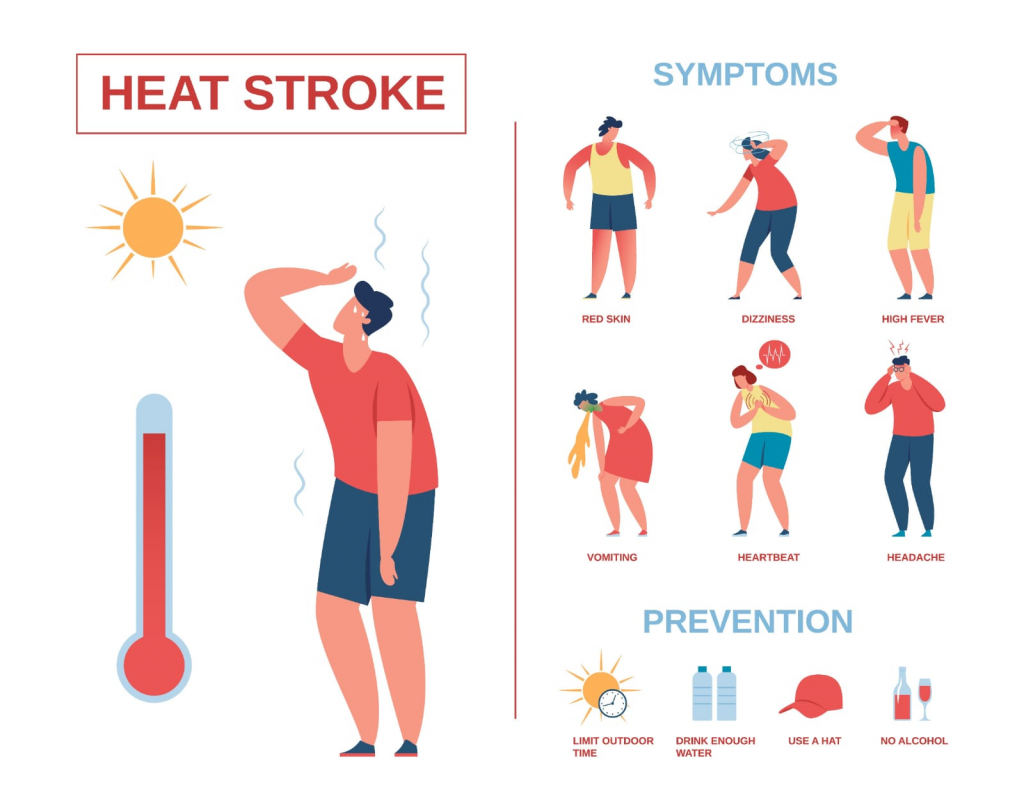
- Heat stroke is an emergency condition in which the body temperature is elevated due to prolonged exposure to the sun or excessive environmental changes.
- In some conditions, the body’s heat loss mechanisms are lost and the hypothalamus does not function properly. Heat stroke requires immediate medical attention. If not treated properly, it can increase the mortality rate.
- Risk Factors:
- Due to prolonged exposure to the sun.
- Age: Very young/old client.
- Clients who have cardiovascular disorders.
- Hypothyroidism, diabetes, alcoholics,
- Occupation of farmer, athletes, construction workers,
- Medications such as phenothiazines, diuretics,
- Amphetamines, anticholinergics.
- Clinical Manifestation:
- Giddiness,
Confusion,
Delirium,
Semiconcious – Conscious, - Gastrointestinal track: Excessive thirst, nausea, visual disturbances, non-reactive pupils, muscle cramps
- Skin: Hot, dry, no sweating, temperature 45°C, increased heart rate, increased blood pressure.
- If cooling measures are not taken, permanent neurological damage may occur.
- Nursing Action:
- Provide a total environment.
- Check the patient’s level of consciousness.
- Monitor the patient’s vital signs.
- Provide intravenous fluids to the patient.
- Monitor the patient’s intake-output record.
- As the client regains consciousness, collect a proper history of the client’s medical history, addictions, and previous medication intake.
- Monitor the patient’s intake-output.
- Provide cold compresses to the patient.
- Monitor the patient’s temperature.
- Document the assessment, actions taken, and the client’s reactions.
Hypothermia:
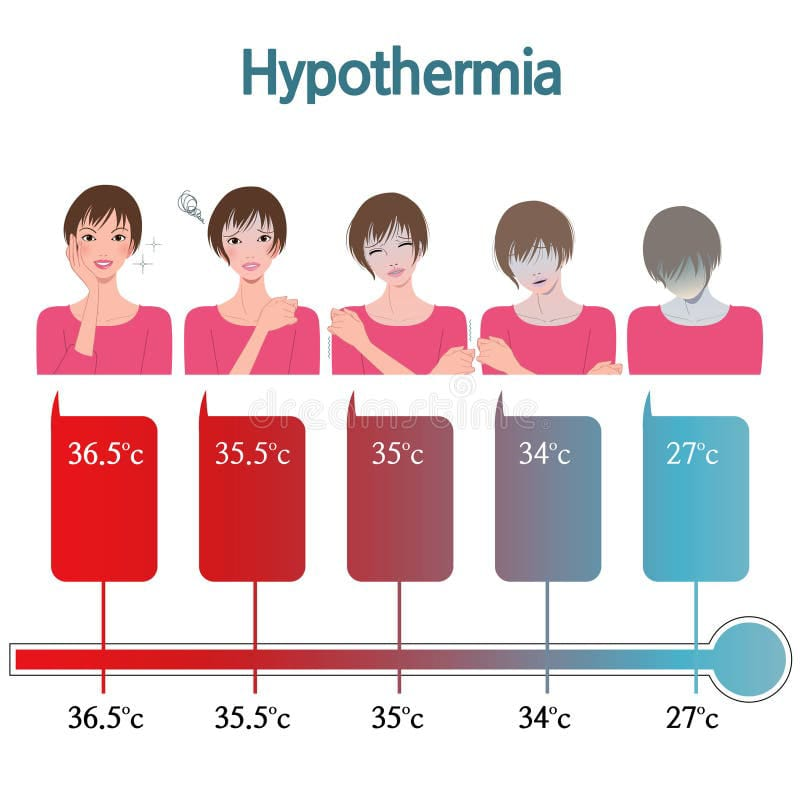
- It is a condition of altered temperature, where the body temperature falls below normal levels. It may be caused by an accidental falldown in a frozen lake. It can be induced during surgical procedures to reduce metabolic demand and the body’s O₂ needs.
- In severe hypothermia, the client may experience symptoms such as:
- Uncontrolled shivering,
- Loss of memory,
- Depression,
- Poor judgment,
- Loss of consciousness,
- Cardiac dysrhythmia,
- Cyanotic skin,
- Pulse and respiration falls
- Non-reactive to stimuli
- Extremely low respiration and pulse
Frost bite:
- This condition occurs when the body is exposed to subnormal temperatures. In this condition, ice crystals form inside the cells, causing permanent tissue damage. The most common areas are the ear lobes, tip of the nose, fingers, and toes. The affected area is white, waxy, firm to the touch, and non-sensitive.
- Nursing Action:
- Assessment.
- Warm the Client.
- Give prescribed analgesics.
- Protect injured tissue.
- Document.
- Normal body temperature:
- Oral temperature: 97-99°F (36.3 – 37.4° C).
- Axillary temperature: 96-98° F (35 .8-37° C).
- Rectal temperature: 98- 100° F.( 37- 38 ° C).
Formula:
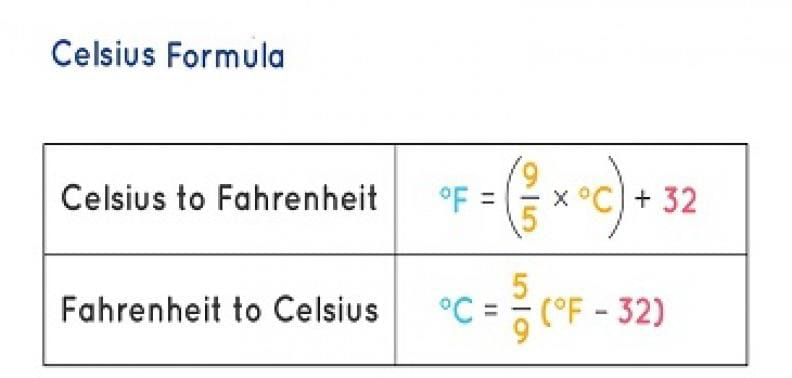
- C° → F° Formula
- F°= 9/5 × temperature C° + 32
- F° → C° Formula
- (Temprature F° – 32)× 5/9 = C°.
હોટ એન્ડ કોલ્ડ એપ્લીકેશન(hot and Cold Application):

હીટ એપ્લીકેશન (Heat Application):

તેમાં થેરાપ્યુટિક પર્પઝ માટે ડ્રાય મોસ્ટ અથવા મોઇસ્ટ હીટ નું એપ્લિકેશન છે.
પર્પઝ ઓફ હોટ એપ્લિકેશન(purpose of hot Application):
- ક્લાઇન્ટ કમ્ફર્ટ ને પ્રમોટ કરવા માટે.
- એડીમાને રીડયુઝ કરવા માટે.
- પેઇન ને રીડયુઝ કરવા માટે.
- હાઇપોથર્મિયા માંથી સફર થતાં ક્લાઇન્ટ ને રીવાર્મ કરવા માટે.
ફીઝીયોલોજી(Physiology):
ફ્લુઇડ કલેક્શન થવાના કારણે એરિયામાં સ્વેલિંગ થાય છે(એડીમાં). આ સ્વેલીન્ગ થયેલા એરીયા મા હોટ એપ્લીકેશન કરવાથી વાઝોડાયલેટેશન થાય છે.ત્યારબાદ બ્લડ ફ્લો ઇન્ક્રીઝ થાય છે અને વેસ્ટ પ્રોડક્ટ રીમુવ થાય છે અને ફ્લુઇડ એ ઇન્ટ્રાસેલ્યુલર થી ઇન્ટ્રાવાસ્ક્યુલર સ્પેસ મા સીફ્ટ થાય છે.અને ઇન્ટ્રાસેલ્યુલર સ્પેસ મા ઓછા અમાઉન્ટ મા ફ્લુઇડ રહે છે.અને એડીમા રીલીવ થાય છે.
યુઝીઝ ઓફ હોટ એપ્લીકેશન(uses of Hot Application):
- હીટિંગ પેડ્સ, એક્વાથર્મિયા પેડ્સ, વાર્મ/હોટ સોકનો ઉપયોગ ક્લાયંટના કમ્ફર્ટ અને રીલેક્સેસન ને પ્રમોટ આપવા માટે થાય છે.
- મોઇસ્ટ હીટ જેમ કે વાર્મ / હોટ મોઇસ્ટ પેક, કમ્પ્રેસ ડીસ્પોઝેબલ હોટ પેક્સ અને સીટ્સ બાથ કે જે વાઝોડાયલેટેશન ને એન્હાન્સ કરે અને એડીમા ને રીડ્યુઝ કરે છે.
- હોટ ડ્રીંક્સ,ગેસ્ટ્રીક લવાજ, વાર્મ વોટર (107 ° F) કે જે ક્લાઇન્ટને રીવાર્મ કરવામાં હેલ્પ કરે છે.
- વાર્મ, હ્યુમીડીફાઇડ ઓક્સિજન એ બ્રિધીન્ગ દ્વારા લેવાથી ક્લાઇન્ટ રીવાર્મ થાય છે.
- પેરીટોનીયલ લવાજ(રીન્ગર લેક્ટેટ 107 ° C પેરીટોનીયલ કેવીટીમા)કે જે રીવાર્મીન્ગ ને એન્હાન્સ કરે છે.
- કાર્ડિયોપલ્મોનરી બાયપાસ ક્લાઇન્ટને મીકેનીકલી રીતે થેરાપ્યુટીકલી રીતે ઇન્ડ્યુસ હાયપોથર્મિયાને ફોલો કરવામાં રિવાર્ર્મિંગમાં ઇમ્પોર્ટન્ટ રોલ પ્લે કરે છે.
હોટ એપ્લીકેશન માટેના પ્રીકોસન્સ (precautionary measures to be taken for hot Application):

- Always be alert when applying hot applications. Because heat is a potential source of tissue damage, hot fluid leakage from the bottle pack can cause skin burns.
- Moist heat burns more than dry heat because water is a good conductor. The nurse should be alert to observe the client.
- Hot applications increase cellular activity and should never be applied to areas with malignant cell masses.
- The application of heat is different for each person. When applying heat, the client’s age, medical problems, and comfort level should be considered.
- Age: Infants and older people are more likely to suffer burns.
- Medical Problem: Clients with circulatory problems.
- Check the temperature of hot applications frequently to avoid inadequate or excessive heat.
- Always cover the hot pack with a cloth that protects the client’s skin from burns and discomfort.
- Collect subjective and objective information to detect the possibility of excessive heat or burning as well as inadequate heat.
- Monitor for signs of burning, such as pain and extreme redness.
- Explain the procedure and its rationale to the client.
- Always be aware of inaccuracies or malfunctions of mechanical equipment used for hot applications. Thus, assessment plays an important role to detect any fault.
Contraindications to hot application:

- 1) Malignancy: Heat can increase the metabolism of cells and the condition of the client with malignancy deteriorates.
- 2) Impaired Renal, Cardiac and Lung Functions: Hot application enhances vasodilation of cutaneous vessels, hence blood supply to vital organs may be affected.
- 3) Acutely inflamed areas such as acute appendicitis, tooth abscess, in such cases heat can rupture them and spread infection to the surrounding tissues.
- 4) Do not apply heat to an open wound as it may cause bleeding.
- 5) Heat application to the head may increase discomfort due to the vasodilation effect.
- 6) Use of hot applications may increase swelling associated with venous or lymphatic diseases. Therefore, heat should never be applied in such cases.
- 7) Do not apply heat to a client with pyrexia.
Application of Dry Heat:
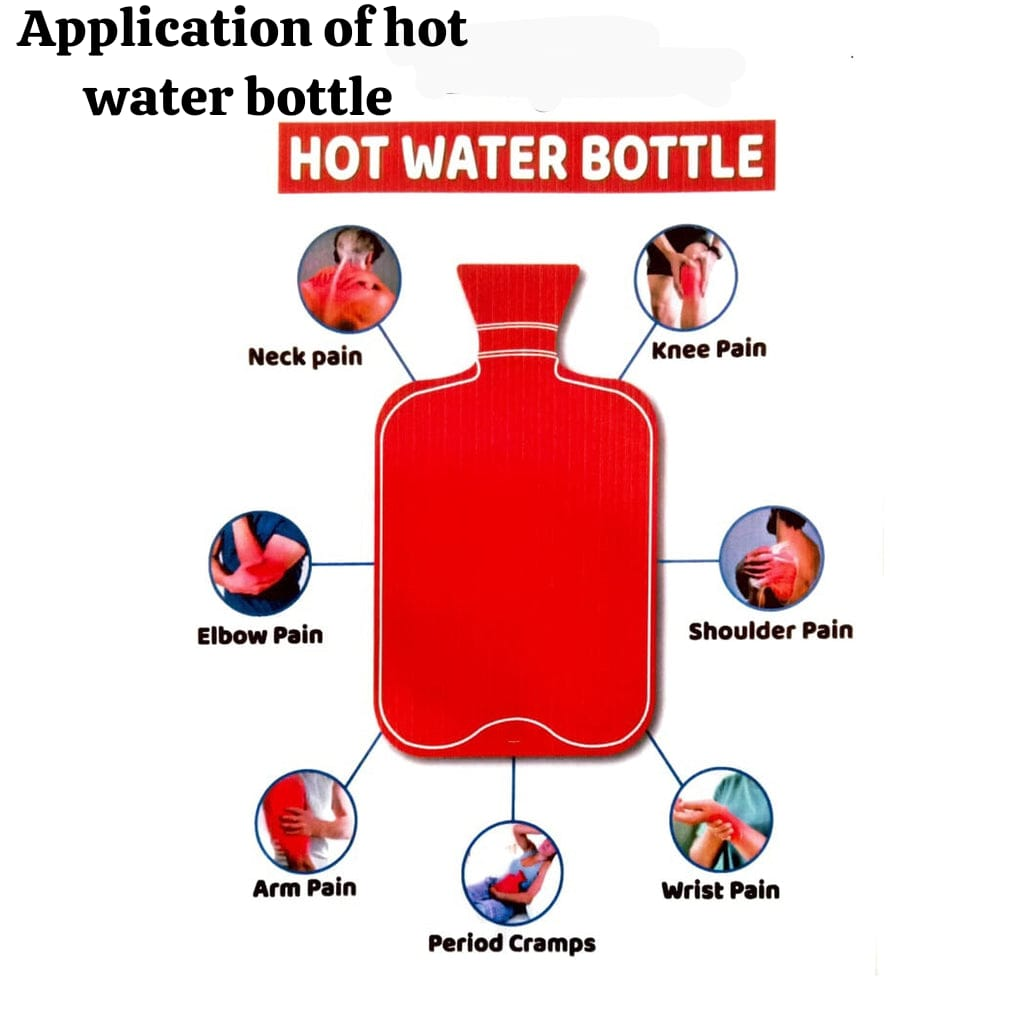
- This includes hot water bottles, heating pads.
- Preparations:
- Assess the client to identify needs.
- Check the physician’s order for dry heat application, type of equipment, temperature, frequency, and duration of each treatment.
- Detect disorders in the client that may be contraindicated for the use of hot applications.
- Detect the client’s health status, his consciousness, and his activity level.
- Collect all articles, properly check heat appliances such as hot water bottles for leaks.
- Articles:
- A Tray Containing:
- Hot water bag with Cover.
- Jug -2 (one for hot water and other for cold water).
- Duster-1 to dry the outside of bottle.
- Towel: 1 to insulate hot bottle from heat loss.
- Vaseline/oil/petroleum jelly-to apply skin in case of redness.
Procedure:
- Identify the client: To treat the right client.
- Explain the procedure to the client: To gain their confidence and cooperation.
- Provide privacy to the client if necessary.
- Drape the body part as needed and expose the required part.
- Provide the client with a comfortable position: To promote the client’s comfort.
- Wash hands properly: To prevent cross infection.
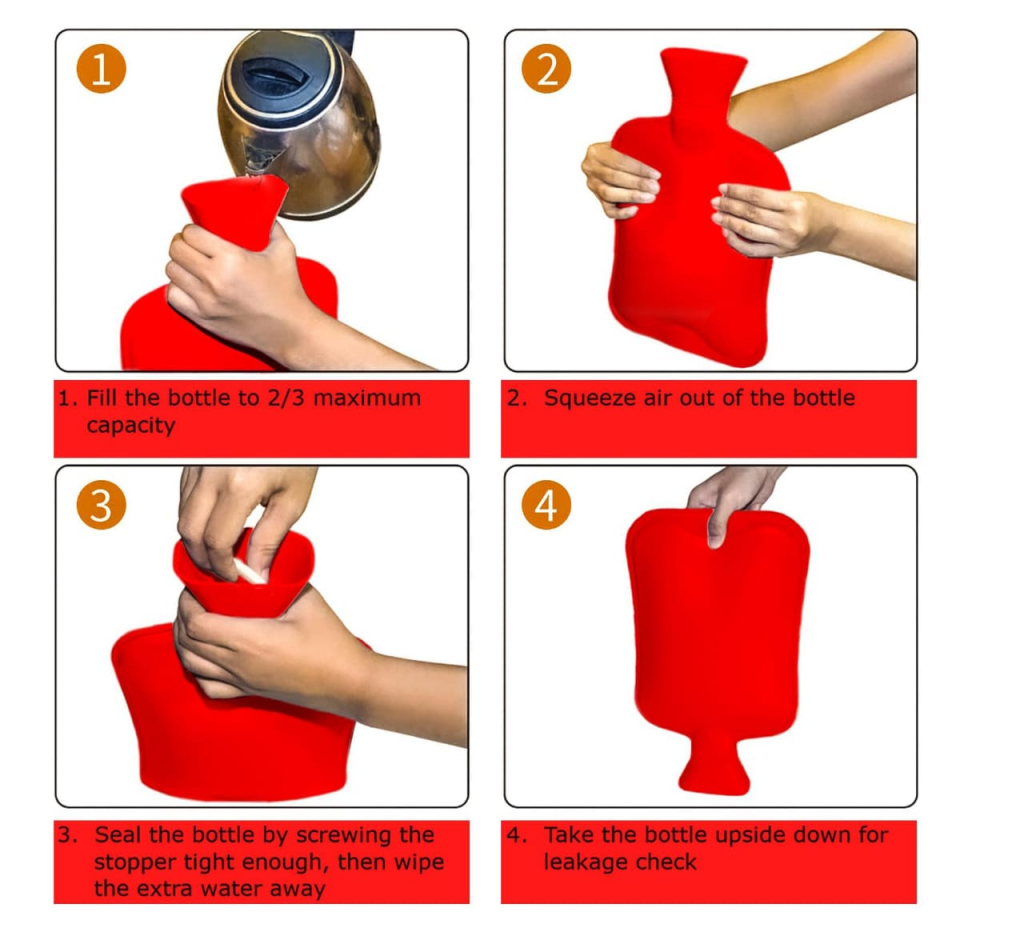
- Prepare the equipment by mixing hot and cold water and checking its temperature and its temperature should be 120 to 149 ° F (49 – 65 ° C) Celsius: To avoid burning the client.
- Pour hot water into the hot water bottle and remove it after 20-30 seconds: To warm the hot water bottle. With this, a little heat is used to warm the bottle and get the maximum benefit of heat application.
- Fill the bottle 2/3 – 1/2 with hot water: To avoid unnecessary weight. It is difficult to mold a full bag than a half-filled bag.
- Place the bag on a flat surface, remove air: (cover it tightly): Air interferes with the inside of the bag.
- Dry the outside of the bag. Check the bag for leakage. Keep the bag upside down: To prevent burning the client.
- Cover the bottle with a towel and take it to the client’s bedside: The towel is used to absorb the moisture. The risk of burns between the hot bottle and the skin increases because water is a good conductor. The towel will insulate the bag from heat loss.
- If necessary, dry the body area to receive the heat: To detect burning along with the therapeutic effect.
- Assess the client’s reaction initially and throughout the treatment period and observe for any signs of burning: If heat application is continued for more than 30 minutes, secondary effects may occur.
- Keep the bag in place for the appropriate time (20-30 minutes).
- Assessing the client and skin area: Changes in sensation or skin tone help determine the effectiveness of the treatment.
- Providing a comfortable position for the client: To enhance the feelings of well-being in the client.
- Covering the client with a sheet and removing any drapes: This shows respect and care for the client.
- Replacing all articles such as towels and dusters with laundry detergent. Wash the outside of the bag with soap and water, then empty the bag properly and hang it upside down. Storing it in a proper place after drying: This enhances the drying of the inside of the bag. It provides the facility of easy availability when needed.
- Proper hand washing: which decreases the spread of infection.
- Documenting procedures in the client’s record, including date and time, reason for treatment, type of heat, appearance of skin, and client’s reaction. Properly noting: Communication among members of the health team. Ensure safe nursing care is provided.
Sitz bath:
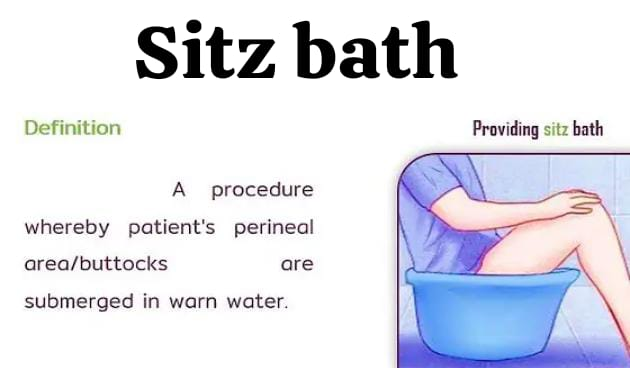
- Assess the client’s problem and assess the need for a sitz bath.
- Check the physician’s order to see if a sitz bath is prescribed and check its frequency, duration, and how many days of treatment to provide, as well as whether any medications are to be provided.
- Clean the tub with a disinfectant solution.
- Wash hands properly.
- Collect all equipment including tub for sitz bath, towels, clean clothes, inflating ring. Collect this equipment.
- Solution used for sitz bath: I KMNO4 1: 5000, II Eusol solution, III Boric acid: 1 dram to 1 pint.
Procedure :

- Identify the client.
- Explain the procedure.
- Provide privacy.
- Fill the tub 1/3rd-1/2 with water.
- The water should cover the rectal and perineal areas and keep its temperature between 100 – 110 °F.
- Use the back of your hand to check the temperature of the water.
- Place an inflated ring on the bottom of the tub. This ring acts as a cushion between the bottom of the tub and the skin to enhance the client’s comfort.
- Add medication to the water, if prescribed. Provide instructions to the client to empty their bladder.
- Remove dressing and clean the perineal area. Inspect: Dressings may become loose and obstruct drains and interfere with water cleaning action.
- Assist client in sitting position in tub: Weakness, poor balance may make sitting difficult.
- Assist client in sitting position in tub: To minimize risk of falldown.
- Check client’s condition during sitz bath if client has condition of weakness, faintness, or weakness Remove the client from the tub immediately.
- Help the client out of the sitzbath after 10-20 minutes: Maximum effect can be achieved within 10-20 minutes.
- Allow the area to dry and apply the prescribed sterile dressing (if ordered) after assessment: Dressing is necessary in cases where the wound is susceptible to infection through open skin surfaces. This promotes comfort and shows respect for the person. Prevents cross-infection.
- Help the client get dressed.
- Provide the client with a comfortable position. And ask the client if they have any complaints.
- Clean the seats and bath tub for next use.
- Replace all articles.
- Wash hands properly.
- Treatment on client’s record: time, date, observations and client’s reactions, any education given. Informing the physician in case of any problem: Communication with health team members verifies the appropriateness of nursing care.
Cold Application:

Cold application on the skin causes constriction of blood vessels, decreases sensation, reduces blood supply, and decreases metabolism of affected cells.
Types of cold application:
- સ્પોન્જ બાથ(Sponge bath)
- કૉલ્ડ પેક્સ(Cold packs)
- આઇસ પેક(ice packs)
- કોલ્ડ કોમ્પ્રેસ(Cold compresses)
- ક્રાયોથેરાપી(Cryotherapy)
- કોલ્ડ વોટર મા ઇમર્શન (immersion in cold water)
- પર્પઝ ઓફ કોલ્ડ એપ્લિકેશન(purposes of Cold Application):
- 1) પેઇન ને રિડ્યુસ કરવા માટે
નર્વ ઇમ્પલ્સીસ ના કન્ડક્શન ને રીડ્યુસ કરીને.
આર્ટેરીયોલ્સ ના સ્પાઝમ ને રીલીવ કરીને.
સ્પ્રેઇન થયેલું હોય તો તેવા કેસીસ માં કન્જેશન ને રીલીવ કરીને. - 2) ઇન્ફ્લામેશન અને એડીમા ના ફોર્મેશન ને રીડ્યુસ કરવા માટે. કોલ્ડ એ બ્લડ સર્ક્યુલેશન ને ડીક્રીઝ કરી ફ્લુઇડ ના કન્જેશન ને પ્રિવેન્ટ કરે છે.
- 3) હેમરેજ ને કન્ટ્રોલ કરવા માટે.
- 4) બેક્ટેરિયાના ગ્રોથ ને ચેક કરવા માટે કોલ્ડ નો યુઝ એ ટીશ્યુસ ના ટેમ્પરેચર ને રિડ્યુસ કરે છે, એન્વાયરમેન્ટ ને માઇક્રોઓર્ગેનીઝમ ના ગ્રોથ માટે લેસ કન્ડક્ટીવ(Less conductive) બનાવે છે.
- 5) કન્ડક્શન, કન્વેક્શન્સ અને ઇવાપોરેશન માટે બોડી ટેમ્પરેચર ને રિડ્યુસ કરવા માટે.
- 6) ટીશ્યુસ ની સેન્સીટીવીટી ને ડિક્રીઝ કરીને એનેસ્થાઇઝ કરવા માટે.જેના કારણે શોર્ટ ટાઇમ માટે નમ્બનેસ નું સેન્સેસન આવે છે.
પ્રીકોશનરી મેઝર્સ ટુ બી ટેકન( સાવચેતીના પગલાં લેવા )(Precautionary measures to be taken):
- ટ્રીટમેન્ટ ની ઇફેક્ટીવનેસ ને ચેક કરવા માટે ક્લાયંટનું ટેમ્પરેચર એ ફ્રીક્વન્ટલી ચેક કરવું.
- ટીશ્યુસ ને ડેમેજ ન થાય તે માટે હંમેશા કોલ્ડ પેક અને સ્કીન વચ્ચે કાપડ રાખવું.
- શીવરીન્ગ, હાઇપોથર્મિયા ના કેસીસ માં કોલ્ડ એપ્લીકેશન ને સ્ટોપ કરવું.
- ક્લાઇન્ટ ને પ્રોસીઝર હંમેશા એક્સપ્લેઇન કરવી.
- કોલ્ડ એપ્લીકેશનમાં ઉપયોગમાં લેવાતા ઇક્વિપમેન્ટ્સ માં માલફંક્શનીન્ગ સર્જાવાની શક્યતાને હંમેશા ધ્યાનમાં રાખવી.
- પ્રોસીઝર સ્ટાર્ટ કરતા પહેલા, હંમેશા ટેમ્પરેચર ની એપ્રોપ્રિએટનેસ ને ચેક કરવું.
કોલ્ડ એપ્લીકેશન માટેના કોન્ટ્રાઇન્ડીકેશન્સ (Contraindications to cold applications):
- એવા ક્લાઇન્ટ કે જે શોક અને કોલેપ્સ સ્ટેટ મા હોય.
- એડીમાં, મસલ્સ સ્પાઝમ.
- એવા પેશન્ટ કે જેને નંબનેસ ની સેન્સેસન હોય.
- સીવરીન્ગ અને હાઇપોથર્મિયા માંથી સફર થતાં હોય તે પેશન્ટ મા.
- જો ક્લાયન્ટને ઇન્ફેક્ટેડ વુન્ડ હોય જે પસ દ્વારા ડ્રાય થયેલ હોય.
કોલ્ડ સ્પંજ બાથ (Cold Sponge bath):

Articles :
- Basin with water
- Wash Clothes
- Towel
- Sheet: To cover the body.
- Client’s thermometer
Procedure:

- Assess and identify clients’ needs To do.
- Assess the client’s condition and see if cold application is contraindicated.
- Properly wash hands.
- Collect all articles.
- Identify the client.
- Explain the procedure to the client.
- Provide privacy.
- Assess the client’s temperature: To assess baseline data.
- Fill the basin with water:
Tepid bath: 80-90°F
Cold bath: 65-80°F
Water with alcohol 85-95°F: Since the water temperature is lower than body temperature, heat loss can occur through conduction. - Remove the client’s clothes and cover them with a sheet : Provide privacy to expose body surface area for bathing and evaporation.
- Start with wet skin on the face and do not dry it: Wet skin causes heat loss through evaporation.
- Apply cool and moist cloth to axilla and groin. Then remoisten as it warms: To enhance heat loss through conduction.
- Avoid applying heat to chest and abdomen: Sponging increases severing in the chest and abdomen.
- Sponging should be stopped if the temperature falls within 2°F of the temperature.
- Assess temperature, pulse, and respiration every ten minutes.
- Bathing should be continued for 20-30 minutes.
- Dry the client after bathing: Drying the skin after bathing reduces friction.
- Provide comfortable positions for the patient and advise on wearing clean clothes: To promote client comfort and show respect and care for the person.
- Replace articles: To minimize cross-infection.
- Proper hand washing.
- Document nursing activities including time, date, body temperature, water temperature, client’s actions: To verify the appropriateness of nursing care. For.
- Assess temperature in 30 minutes for one hour and then 1-2 hour intervals.
Complications of hot application:

- Pain,
- Burns,
- Maceration With moist heat,
- Red Skin,
- Pale colour because of Secondary effect of hot,
- Hyperthermia (Hyperthermia)
Complications of Cold Application:

- Pain,
- Blister,Skin break Down,
- Maceration with moist Cold.
- Grey / Blue Skin.
- Cold Red colour of skin because of Secondary effect of cold,
- Hypothermia,
- Shivering