ENGLISH-FON:UNIT : 6 (PART: 6)CARE PATIENT WITH BODY ELIMINATION DEVIATION-UPLOAD
Unit : 6 (part:6)Care of Patient with Body Elimination Deviation:
Definition and Introduction:
Elimination (Elimination – Elimination):
Elimination is a physiological process in which waste products are removed from the body. There are mainly two types of waste products in this process:
Urine: Urine is the liquid waste produced by the kidneys.
Stool: Stool is the solid waste left over from the digestive process.
When there is disruption, irregularity, or the body is unable to eliminate waste properly, it is called Elimination Deviation. is.
In this situation, the patient may experience physical, psychological and social disturbances. Therefore, it becomes essential to provide nursing care completely, proven (proven) and with a human attitude.
Major Types of Elimination Deviation:
A. Urinary Elimination Deviation:
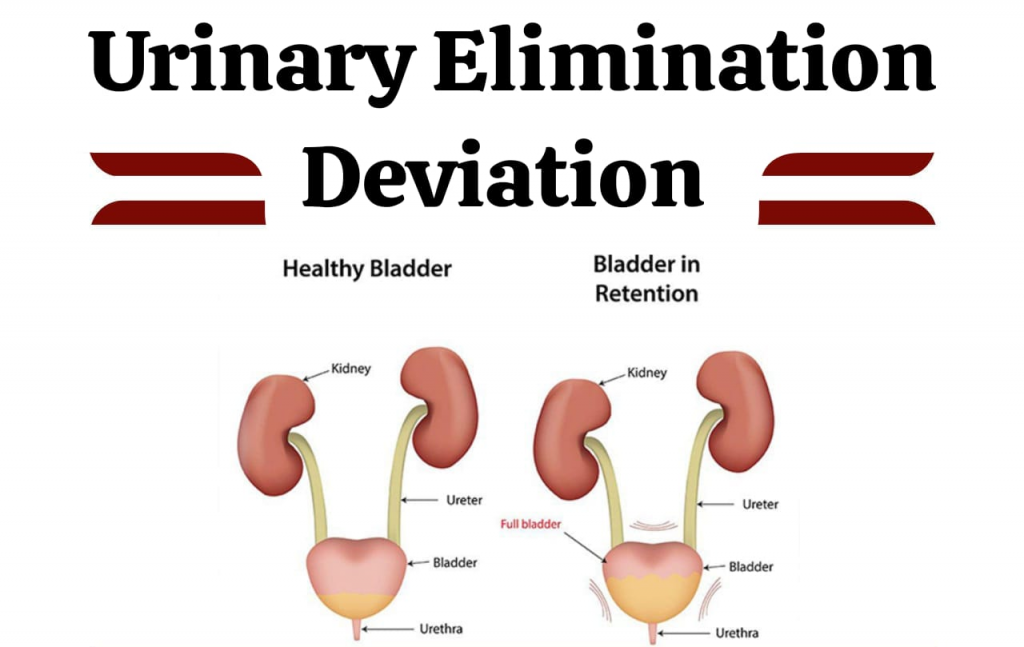
In this, the patient experiences difficulty or irregularity in urine elimination. The standard deviation is as follows:
Urinary Retention:Urine is produced but cannot be expelled from the urethra.
Urinary Incontinence: Loss of control over urine.
Urethral Stricture – Urethral stricture): Constriction in the urethra causes blockage of urine flow.
UTI (UTI): Infection in the urinary tract.
B. Bowel Elimination Deviation:
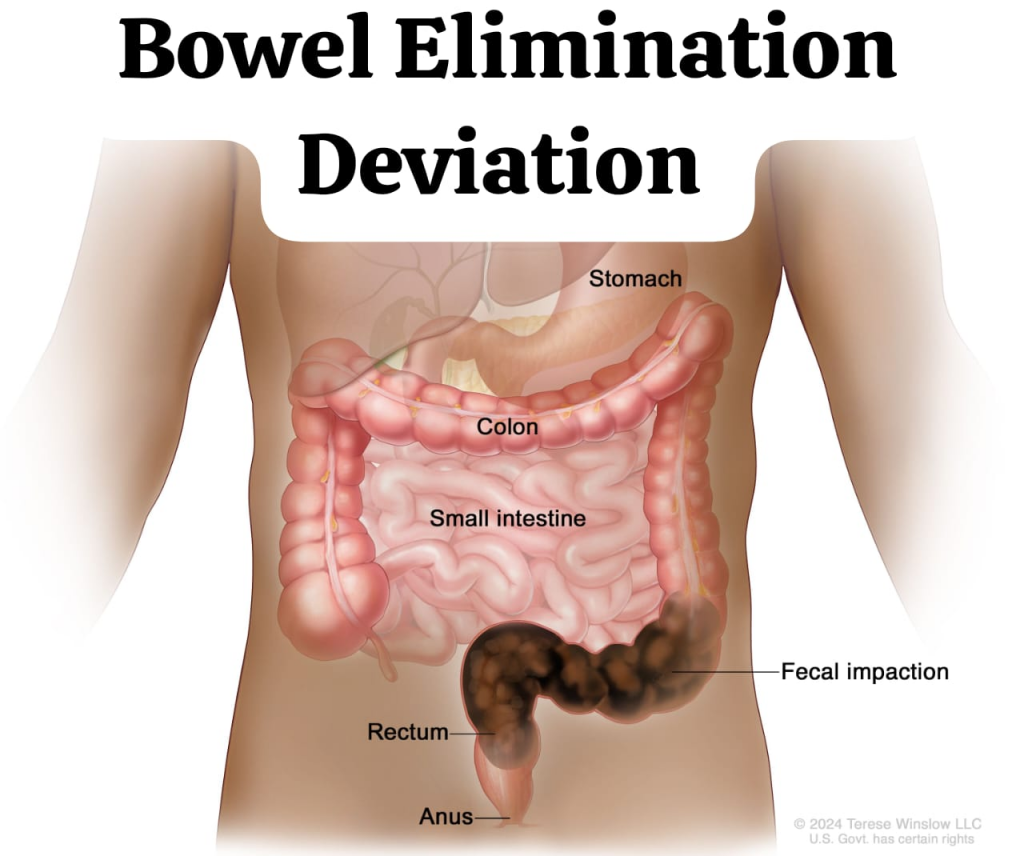
In this, there is an alteration in the elimination of stool. Alterations that may seem normal:
Constipation:Stools become hard or irregular.
Diarrhea: Frequent passing of loose stools.
Fecal Incontinence – Fecal incontinence): Loss of control over stool.
Obstipation (Obstipation): Severe constipation, stool cannot be expelled properly.
Comprehensive Nursing Interventions for Patient Care:

A. Nursing Care for Urinary Elimination Deviation:
1. Fluid Monitoring: Keep a record of how much fluid the patient takes in and how much urine is expelled daily.
2. Urine observation: Study the color, odor, amount, and frequency.
3. Catheterization (Catheterization): If the patient cannot expel urine, then the doctor should insert a catheter as per the order.
4. Aseptic Technique: To prevent infection during all actions.
5. Perineal Care: Maintain regular cleanliness and dryness of the perineal area.
B. Nursing Care for Bowel Elimination Deviation:
1. Diet Management: Give high fiber and light food.
2. Increase fluid intake: To keep stools soft.
3. Positioning: Place the patient in the proper position for defecation.
4. Laxatives and Antidiarrheals: Give medication as per the doctor’s advice.
5. Stoma Care: Maintaining the hygiene of the stoma area in patients with colostomy or ileostomy.
Psychological and Social Care:
- The patient may be feeling depressed or anxious due to loss of control over himself, hence Empathetic Communication is necessary.
- Psychological Counseling (Psychological Counseling): Provide when necessary.
- Support the patient to maintain independence.
- Family Education: Teach how to care for yourself at home.
Special Care in Case of Ostomy:
- If the patient has a colostomy or ileostomy:
- Stomach observation: Assess the color, size, and condition of the skin.
- Changing the stoma bag: Change it on time to prevent leakage.
- Skin protection: Protect the skin around the stoma from swelling or infection. Giving.
Documentation and Reporting:
- Record Maintenance of all nursing interventions.
- Report on patient progress, changes, and conditions.
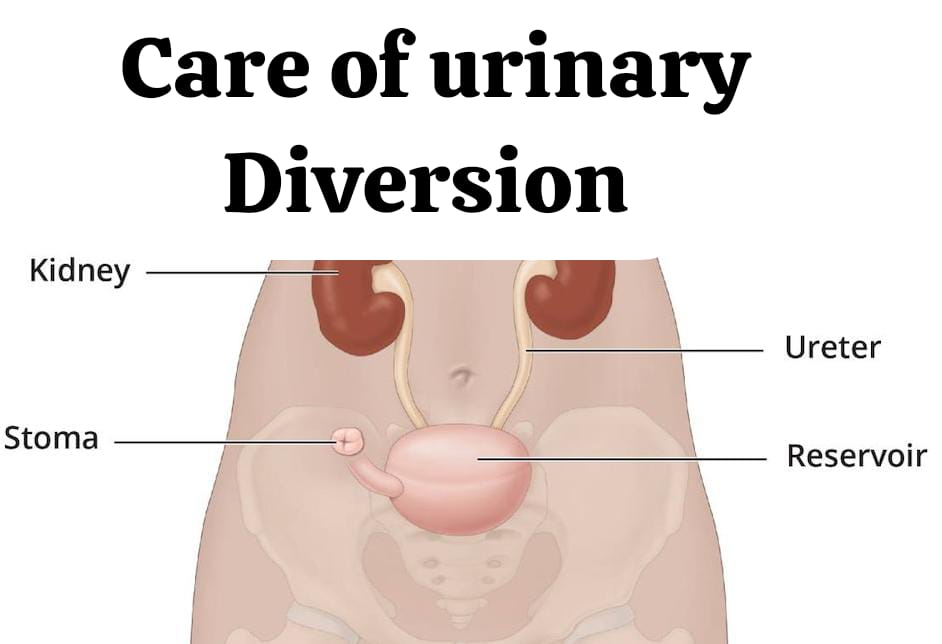
Care of urinary diversion:
Pre operative care:
Psychological care:
- A patient admitted for cystectomy and urinary diversion will already know the ward health team from the previous admission.
- Staff should establish rapport with the patient and provide the patient with Information should be provided in both verbal and written form to prepare for the physical effects of the operation, especially the formation of the stoma.
- It may be helpful for the patient and their family to arrange to meet with the person who has the stoma.
- There may be side effects of the surgery. Therefore, the nurse should discuss it with the patient and his family members.
- The patient should be advised to inform the doctor or visit the hospital if any problem arises while making challenging adjustments at home from the hospital or contact him on phone if any minor problem arises.
Physical care:
- The stoma will be located on the abdomen below the waist, usually on the right side. Considerations for choosing a specific side include:
- the patient’s build,
access for the surgeon
previous surgery
access for the patient following surgery
type of clothing to be worn after the surgery.
The following procedures are performed in preparation for surgery:
1. Bowel preparations The patient is placed on a fluid-only or low-residue diet.
2. The bowel is cleared of faeces. This can be done by enema or high colonic washout and is done two days before the operation. Bowel sterilization can be done with systemic and local antibiotic prescription.
3. The skin is shaved from nipple to knee.
4. The patient is helped to shower on the day of the operation.
5. The site chosen for the stoma is marked.
Post operative care:
Return From Theatre:
- A nasogastric tube will be in place for aspiration of gastric contents.
- Examination will reveal a midline incision, which will be covered by a surgical dressing and wound drain.
- The stoma, in the premarked position, It should have a moist red appearance and is covered by a collection bag fitted with a drainage tap.
- The infant feeding tube that forms a temporary splint at the ureteroileal anastomosis can be seen emerging from the stoma.
- The splints, one for each ureter and inserted during surgery, pass through the ideal loop and along the ureter at the junction of the anastomosis. The support of this splint reduces the risk of urine leakage from the anastomosis.
The Recovery period:
- The NG tube will remain in place for 24-48 hours or until bowel sounds return.
- The drainage may be removed when the discharge is less than 50 ml/24 hours, which is normal. Typically within 4-5 days.
Postoperatively:
- Removing splints from the stoma is usually done in 10-14 days and sutures in 10 days.
- Assessment and provision of a diet plan by a dietitian can help with wound healing and recovery. is.
- The nurse will teach the patient how to clean the stoma and how to change the bag and flange daily. The patient should be shown how to cut the flange to shape and fit it into position with the bag.
Discharge:
- 10-14 days after the operation, the patient and the nurse should plan for discharge, provided no complications arise.
- Follow-up appointments are usually scheduled after the operation. Then it will be scheduled for 6-8 weeks and then at longer intervals but it will be continuous for life.
Nursing care in First 24 hours Following urinary Diversion:
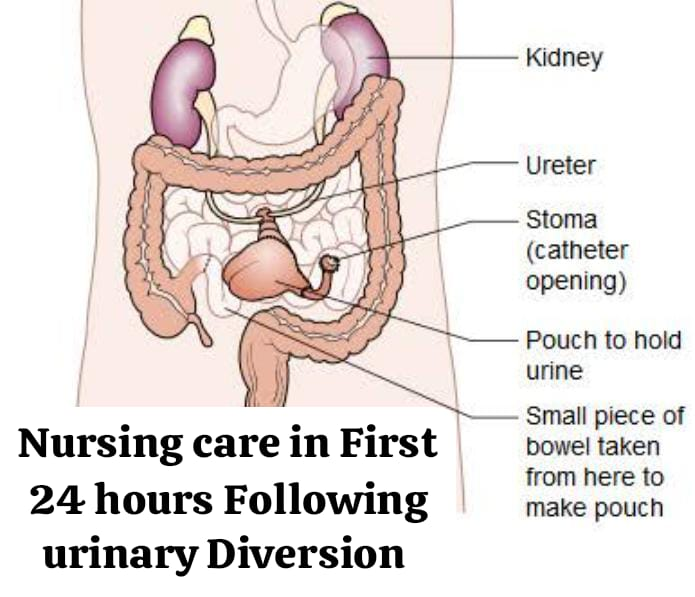
Potential Problem:
Hypovolemic shock due to cardiovascular instability and hemorrhage and pain
Action:
- Record vital signs and report any deviations from normal range.
- Monitor and mark visible blood loss on wound dressing.
- Report blood loss in drainage and if more than 100 ml/hour.
Potential Problems (Potential Problem):
Pain
Action:
- Observe the patient for disease.
- Administer the prescribed analgesic medication to the patient.
- Evaluate the effect of the medication 30 minutes after providing it.
Potential Problem:
Fluid and Electrolyte Imbalance
Action:
- Measure and record the patient’s urine output.
Balance all fluid output against all fluid input over 24 hours. - Observe for dyspnea and evidence of dehydration.
- Observe for vomiting.
Potential Problems (Potential Problem):
Paralytic ileus
Action:
- Keep the patient on NBM.
- Perform NG aspiration/free drainage hourly.
- Administer antiemetics as needed.
Potential Problem:
Deep vein thrombosis (DVT) Pulmonary embolism (PE)
Action:
- Preoperatively supply antiembolic stockings
- Encourage lower limb movement.
- Observe for evidence of DVT or PE.
Potential Problem:
Chest infection
Action:
- Encourage the patient to take deep breaths and cuffing.
- Refer to a physiotherapist.
- As much as possible, the patient Keep it upright
Potential Problem:
Wound infection
Action:
- Observe wound for leakage, check drainage hourly.
- Record temperature and report pyrexia.
Potential Problems (Potential Problem):
Development of Pressure Sore
Action:
- Leave the dressing undisturbed for 48 hours.
- Regularly change the patient’s position and observe for redness Do.
- Use a risk assessment scale to assess the patient’s needs.
- Make sure the skin is clean and dry.
- Use an air mattress if necessary.
Potential Problem:
Inability to perform personal hygiene tasks.
Action:
- Provide bed bath and mouth care.
- Discuss the patient’s concerns with him/her. Give information, but consider post-anesthetic drowsiness.
Potential Problem:
Anxiety
Action:
Given Evaluate patient’s understanding of information.
Bladder irrigation:
Definition:
Bladder irrigation involves inserting a catheter into the bladder through the urinary meatus and instilling a solution into the bladder and washing the urinary bladder.
Purposes:
- To ensure patency of the urinary drainage system.
- To cleanse the bladder of stagnant urine, bacteria, excess mucus, pus, and blood clots.
- To relieve congestion and pain in inflammatory conditions.
- To promote healing.
- To medicate the lining of the bladder.
- To stop bleeding.
- As a preoperative measure to prepare the bladder for surgery.
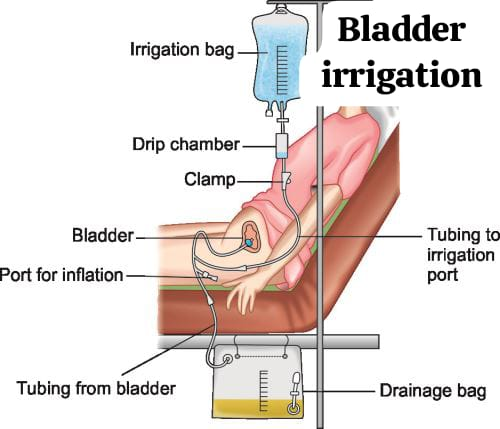
Types of irrigation procedure:
1) Open method:
It is done with an aseptic syringe in which the fluid is introduced into the urinary bladder and simultaneously drained out.
2) Closed Method:
This provides for frequent intermittent or continuous irrigation of the sterile catheter system without disruption. This is often done for patients undergoing genito-urinary surgery, where there is a risk of blood clots and mucus fragments occluding the catheter.
Preliminary assessment:
- Assess the function of the catheter drainage system.
- Type of catheter in place.
- Length of time/duration of catheter.
- Bladder Distention.
Procedure:
General instructions
- Maintain strict aseptic technique.
- Administration only after obtaining a doctor’s order To do.
- Maintain an accurate record of the fluid used for irrigation.
- The fluid should be instilled gently and allowed to drain back out by gravity.
Articles (Aarticles):
- Sterile bulb for attaching the catheter Syringe/Asepto Syringe: To introduce irrigating fluid into the bladder.
- A kidney tray: To collect waste.
- A 2-pint measuring cup containing the required solution at a temperature of 104°F: To irrigate the bladder.
- A sterile measuring glass containing medicine, if ordered: To instill at the end of treatment.
- A Macintosh with paper lining: To protect bed linen.
- Distilled water (normal saline): To avoid irritation of the sensitive mucus lining of the bladder.
- Sodium Nitrate 1:8000 : To prevent clot formation.
- Boric Acid 2%
Potassium Permanganate 1:10000
Acriflavine 1 in 10000 : Mild antiseptic and non-irritating.
Silver Nitrate 1 in 5000
Acetic Acid 400 in 1 : Astringent
For the treatment of Pseudomonas infection.
A weak aqueous solution should be used for irrigation:
Solution:
Procedure:
Steps:
- Explain the procedure to the patient: To promote cooperation and decrease anxiety.
- Place a Macintosh and towel under the patient’s buttocks: To protect the bed linen.
- Place the female patient in the dorsal recumbent position: For easy access to the perineal area.
- Fold back the top bedclothes and drape the patient with a bath blanket, exposing the perineal area: Reduces body exposure and reduces the possibility of embarrassment to the patient.
- Wash hands and wear sterile gloves: Helps prevent cross-contamination.
- Place a sterile basin/kidney tray between the patient’s legs near the perineal area: To receive the solution from the catheter.
- Fill the irrigating solution into the urinary bladder by gently pinching the bulb: To introduce the irrigating solution.
- Detach the syringe from the catheter in the pinched bulb position and allow it to drain into the kidney tray: Prevents the bladder’s mucus membrane from sucking and helps in reviewing the return flow.
- Repeat the process until the solution is clear: Prevents any remaining waste from being released into the bladder.
- If the solution does not come back, turn the patient to the nurse’s side: Repositioning facilitates drainage.
- Open the sterile set at or between the patient’s thighs using sterile technique: Convenient for performing the steps.
- Wear gloves: To prevent infection.
- Place a sterile towel under the end of the catheter: To keep the catheter sterile.
- Clamp the drainage tubing distally to the irrigation part: To prevent the irrigation solution from flowing into the drainage bag.
- Remove the cap from the needle and draw the irrigation solution into the syringe: To maintain the sterility of the syringe and solution.
- Using a three-way Foley catheter or Y connector, expel air from the tubing connected to the irrigation bag: To prevent bladder spasms and pain.
- Connect one end of the three-way catheter to the irrigating tubing, which is connected to the irrigation solution in the bag: To ensure correct tube connection.
- Connect the other end of the catheter to the drainage tubing and bag and the third end to the catheter balloon.
- Open the flow clamp on the drainage tubing: To obtain proper inflow and outflow of fluid.
- Adjust the flow using the clamp on the irrigation tubing to maintain 40 to 60 drops per minute: To prevent undue force of fluid into the cavity.
- Unclamp the drainage tubing so that the solution flows out of the bladder through the catheter and tubing: To drain the fluid.
- Repeat the irrigation process until the purpose of the irrigation is achieved: To cleanse the bladder of bacteria and blood clots.
- Measure the amount of urine and subtract the amount of solution used from the volume of fluid in the bag: To maintain the intake output chart.
- Assess the color, clarity, and any abnormal constituents of the drainage: To judge the effectiveness of the treatment.
- Assess the flow of urine through the catheter and tubing: To assess the functioning of the drainage system.
After care of the patient and articles:
- Provide a comfortable position for the patient.
- Clean the equipment and keep it in its proper place.
- Wash hands properly.
- Record the treatment on the patient chart, including,
Date and time,
Purpose of irrigation,
Amount of solution used,
Amount of drainage drained from the bladder,
Properly report any complications.
Complications of bladder irrigation:
- Infection,
- Tissue trauma,
- Urethral irritation: Urinary infection due to the presence of a catheter.
- Muscular Spasm.