ENGLISH-FON : UNIT : 6 (PART : 5)CARE OF PATIENT WITH PAIN-UPLOAD
Unit: 6( Part : 5)Care of patient with pain:

Introduction:

Pain is an unpleasant sensory and emotional experience that can be actual or Potential tissue damage resulting from trauma is a unique experience for an individual that may be difficult for the client to describe or explain and is often difficult for others to recognize and assess. It is an unpleasant feeling, which is entirely subjective and can be described or evaluated by the person experiencing it. Pain has a different meaning for each person, which can be different for some people at the same time.
Medical Definition:

Ac. to Carpenito,“Pain is defined as a state in which the individual experiences and reports severe discomfort or uncomfortable sensation”.
Ac. For Merskey & Bugdulk, “Pain is a complex multifactorial phenomenon that involves emotional experiences associated with the actual as well as the potential”.
Nursing Definition:
Acc. To McCaffey, “Pain is whatever the experiencing person says it is and existing whenever the person says it does”.
Types of pain:

Pain is categorized according to its duration, location and etiology.
A) General types of pain:
1) Acute pain
2) Chronic pain
1) Acute pain pain) :
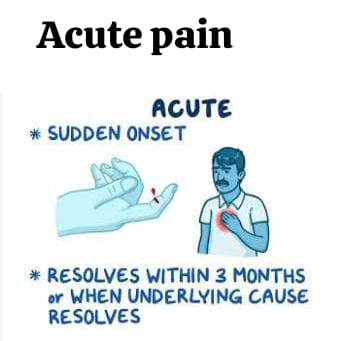
Acute pain is an episode of pain that lasts from seconds to less than 6 months. Acute pain is a very common occurrence, usually when an organic disease or injury is present, although healing may also occur. As healing progresses, the pain decreases and gradually disappears. Acute pain follows an acute injury, disease, or surgical intervention and is characterized by a rapid onset, varying in intensity, and a short duration, usually less than 6 months. Acute pain is usually accompanied by increased muscle tension and anxiety.
2) Chronic pain:
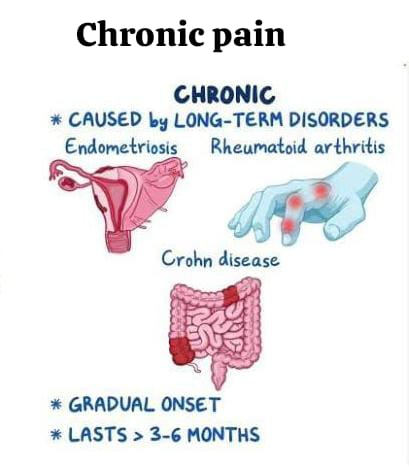
Chronic pain is an episode of pain that lasts for 6 months or more, whether intermittent or continuous. Its onset may be poorly defined and it is often difficult to treat because the cause of origin may be unclear.
B) Specific Type of Pain:

1) Nociceptive pain:
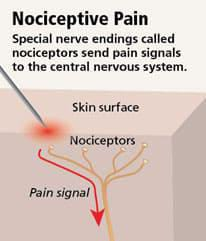
The normal process of stimulation that damages normal tissues or has the potential to do so for a long time, is usually responsive to non-opioids and/or opioids.
•Somatic pain:
Somatic pain is caused by stimulation of the somatic nervous system. It arises from the bones, joints, muscles, skin or soft tissues. The patient may describe it as a sharp diffuse, aching and/or throbbing pain that can be easily localized.
•Visceral Pain:
Visceral pain is caused by stimulation of the ANS (Autonomic Nervous System). Visceral pain arises from visceral organs such as the heart, GI tract (Gastrointestinal tract), and GU tract (Genitourinary tract). Visceral pain is diffuse, poorly localized, vague and dull pain.
2) Referred pain:
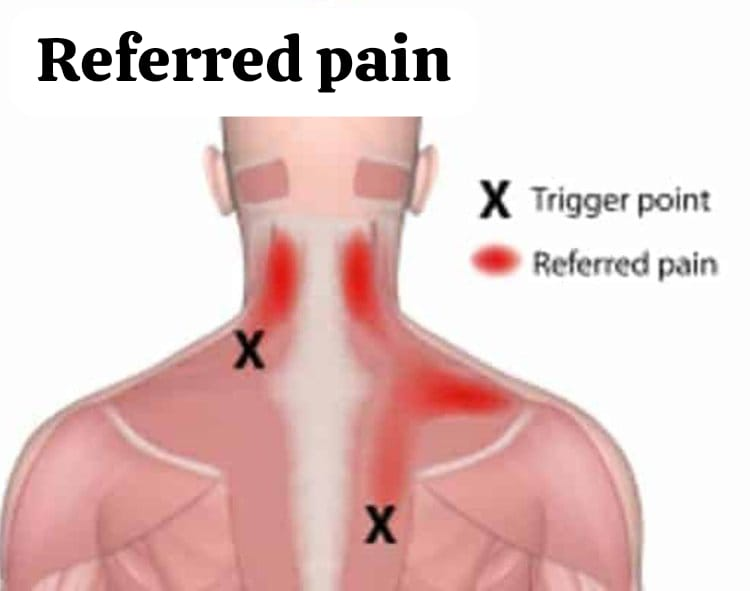
Referred pain is pain that occurs in an area that is far from its point of origin. Pain associated with myocardial infarction or heart attack is frequently referred to the neck, shoulder, or left arm.
Psychogenic pain is pain that is not physiological. It is believed to be primarily due to emotional factors rather than dysfunction. Psychogenic pain is a type of pain for which no physical cause can be identified.
4) Phantom pain:
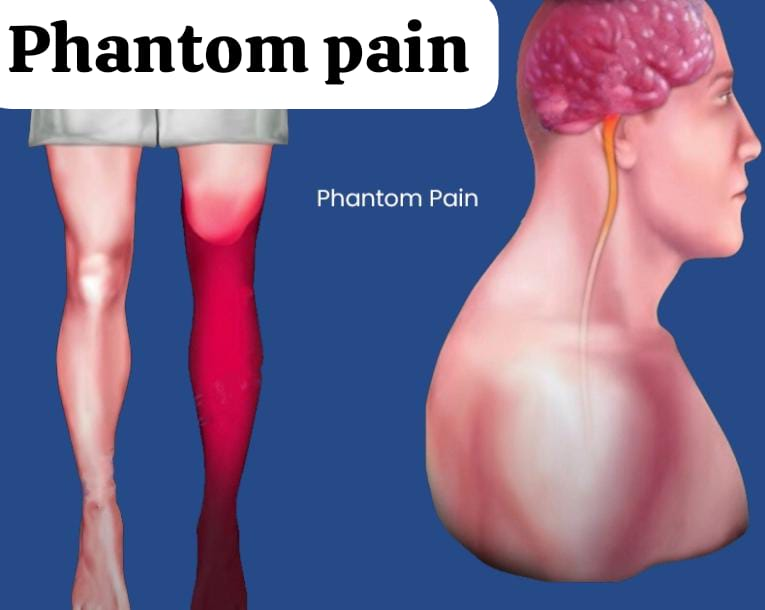
A sensation of pain without a demonstrable physiological or pathological substance; commonly seen after limb amputation. The painful sensation, which is usually intermittent, is described as shooting, stabbing, pricking, squeezing, throbbing, and burning. The missing limb may feel like a twist or cramp.
5) Neuropathic pain:

Neuropathic pain is caused by injury to or abnormal functioning of peripheral nerves or the Central nervous system. Injury to the peripheral nervous system can cause spontaneous paresthesia, numbness, pain during movement, tenderness of a partially denervated body part, and electric shock, burning, shooting, or tingling pain.
6) Superficial or Cutaneous pain:

Cutaneous pain is caused by stimulation of the skin. This pain is short-lived and localized.
Etiology and Precipitating Factor:
- Surgical & accidental trauma,
- Visual disorder, example sickle cell Anemia,
- Innovative diagnostic procedure,
- Excessive pressure
- Cancer
- Inflammation,
- Musculoskeletal disorder,
- Neuropathic and diabetes mellitus,
- Immunodeficiency syndrome as multiple series
- Visceral disorders, example myocardial infarction infarction)
Nursing Assessment of Pain:

Multiple pain assessment tools are available to determine the quality and quantity of a patient’s pain. Valid and reliable pain assessments are essential for clinical trials and effective management. The nature of pain makes objective measurement impossible.
1) Pain history:
When taking a pain history, the nurse should provide the client with the opportunity to express in their own words how they perceive the pain and the situation. This will help the nurse understand what the client understands about pain and how they cope with it. The initial pain assessment for a patient with severe pain may include only a few questions: assessing previous pain treatment and effectiveness, when and what analgesic medication was last taken, other medications being taken, and whether there are any allergies to medications.
2) Location:
Nurses need to ensure that the client is experiencing pain when. A pain chart, which is a drawing of the body and body parts, is a tool for determining the location of pain. The client marks the location of the pain on the drawing.
3) Intensity:
Since pain is a subjective experience, the nurse should remember that the most important indicator of the existence and intensity of pain is the client’s report of pain. Multiple pain assessment tools are available to determine the quality and quantity of the patient’s pain experience. Pain intensity scales are a quick and effective method for rating the intensity of pain for the client. This scale can be used in written or verbal form.
4) Precipitating Factors:
Physical and emotional stressors can also trigger pain. Emotional tension often brings on migraine headaches. Intense fear or physical exertion can cause angina. Environmental factors such as extreme cold or heat and humidity can affect certain types of pain.
5)Past pain experience:
Previous pain experience changes the client’s sensitivity to pain. People who have personally experienced pain or who have been exposed to pain in a close person are more likely to fear anticipated pain than those who have not experienced pain.
6) Physical Examination:
To determine the client’s physiological and behavioral response to pain, the nurse assesses the client’s vital signs and observes the client’s skin color, dryness, diaphoresis, facial expressions, and body gestures. Which reflects pain, discomfort and anxiety.
7) Physiologic Response:
The physiological response is different depending on whether the patient’s pain is acute or chronic. Acute pain stimulates the sympathetic nervous system and due to this, blood pressure, pulse rate, and respiratory rate increase and the patient becomes pale and diaphoresis and pupil dilation occurs.
8) Daily Pain Diary:
A daily pain diary can help the client and the nurse identify factors associated with pain. The client records various information such as time of onset of pain, activity of pain, level of pain intensity in pain-related conditions or behaviors, use of analgesic medications or other relief measures, duration of pain, time spent in relief activities, etc.
Management of Pain :
Introduction:
Pain is an unbearable feeling experienced as a result of any type of tissue damage or emotional distress in the body. Both pharmacological (with drugs) and non-pharmacological (without drugs) management are used for pain management.
Non-Pharmacologic Pain Relief Measures:
1.Physical Methods
a. Cold Therapy:
This method uses ice packs or cold compresses. They cause vasoconstriction and reduce swelling and inflammation, which provides pain relief.
b. Heat Therapy:
Hot packs or hot water bottles improve blood circulation, which causes muscle relaxation and reduces pain.
c. Massage Therapy:
Pressure or friction on the painful part of the body releases natural painkillers called endorphins, which reduce pain.
d. Transcutaneous Electrical Nerve Stimulation – TENS:
This is an electronic device that blocks pain signals by sending electrical impulses to the nerves under the skin.
2.Psychological Methods
a. Relaxation Techniques:
Methods such as guided imagery, deep breathing, and progressive muscle relaxation reduce stress hormones and help manage pain.
b. Cognitive Behavioral Therapy – CBT:
This is a talk therapy in which the patient identifies their negative thoughts and behaviors and changes them into positive thoughts, which reduces the experience of pain.
c.Distraction:
Distractions such as watching TV, listening to music, reading a book, etc., take the focus off the pain.
3.Complementary Therapies
a.Acupuncture:
A traditional Chinese treatment method in which needles are inserted at specific points on the body to reduce pain. It stimulates the nervous system.
b. Chiropractic Therapy:
Manual therapy is given to strengthen the spine of the body, especially useful for back pain and neck pain.
c. Yoga and Meditation:
Yoga and meditation are very effective for pain control, they reduce the activity of the sympathetic nervous system and activate the parasympathetic nervous system.
4.Lifestyle Modification
Proper Sleep Sleep): Sufficient sleep relaxes the body and helps control pain.
Balanced Diet: A nutritious diet promotes supportive recovery processes in the body.
Regular Exercise: The amount of blood increases and endorphins are released, which reduce pain.
Non-pharmacologic pain relief measures are given to the patient in addition to medication. Provides pain relief without side effects. It is based on a holistic and evidence-based method. Selective planning of appropriate methods according to the patient’s needs proves to be very beneficial for long-term pain management.
Pharmacologic Pain Relief Measures for Patient:
Introduction:
Pharmacologic Pain Relief Measures are Pharmacological measures are those in which the main objective of relieving the patient from pain is achieved through medication. These medications affect the nervous system, block pain sensation or reduce its proportion, and provide comfort to the patient. Such remedies are given in standardized, scientific and controlled manners, so that the patient gets physical and mental peace.
1. Analgesics
Medications that reduce pain and keep the patient conscious.
Type:
Type:
Opioids:
Opioid analgesics work on synaptic transmission in various parts of the central nervous system. By binding to natural opioid receptors, they inhibit the ascending pathway of pain perception and activate the descending pathway. Narcotic analgesic medications are available only with a doctor’s prescription and are used for more severe pain, such as cancer pain.
Examples: Morphine, Pethidine, Fentanyl
Non-Opioids:
Used for mild to moderate pain. Non-opioid analgesic medications include common over-the-counter medications such as aspirin, acetaminophen, (Tylenol), ibuprofen (Advil), piroxicam, and ketorolac. Damaged tissue releases enzymes that stimulate local pain receptors. Non-opioid analgesics interfere with these enzymes and reduce inflammation and pain. These are mostly used for mild or moderate pain, but there are some prescription-strength medications in this class.
Example: Paracetamol, Ibuprofen
2. Sedatives and Tranquilizers:
These drugs calm the patient’s state of mind, reduce anxiety and make the experience of pain tolerant.
Example: Diazepam, Lorazepam
3. Anesthetics:
These are medications that completely block pain and sometimes even make the patient unconscious. is.
Subtype:
A. Local Anesthesia
Used to numb a small part of the body.
Example: Lidocaine, Bupivacaine
B. Regional Anesthesia Anesthesia)
Used to block pain in large areas of the body.
Epidural Analgesia:
It is most commonly used to provide immediate pain relief, especially post-operative pain, especially for thoracic, abdominal, orthopedic, vascular surgery, labor and delivery pain, and chronic pain situations. Epidural analgesia is administered into the spinal epidural space. The doctor inserts a blunt tip needle into the layer of the vertebral interspace near the area requiring analgesia. Epidural analgesia is very effective during childbirth.
Spinal Anesthesia:
Has a fast and powerful effect on pain.
C. General Anesthesia
Prepares the patient for major surgery by making him completely unconscious.
Example: Thiopental, Propofol
4. Nerve Blocks
These In this method, anesthetic medication is injected around the nerves to block pain sensation.
Example: Pudendal Nerve Block
5. Patient Controlled Analgesia
In this method, the patient controls the administration of the medication. Drugs such as opioids are administered through a pump. Medication can be given to the patient in controlled amounts according to their needs. This method is especially useful for post-operative pain management.
6) Placebo Response:
The word placebo comes from the Latin word meaning “I shall please”. It consists of an inactive substance that is often given to satisfy a person’s demand for the drug. A person unaware of the properties of a placebo may find it effective for pain relief. Placebo reduces anxiety. (A placebo is an inactive substance or treatment given to a patient, mainly to please them or to satisfy their expectation of treatment, even though it has no therapeutic effect).
Pharmacologic Pain Relief Measures for Patients are a scientifically integrated, effective and safe approach to pain management. The choice of appropriate medication and appropriate method should be made based on the patient’s physical condition, level of pain and health history. These measures lead to a comfortable, pleasant experience and quick recovery for the patient.