ENGLISH-FON UNIT 1-FUNDAMENTAL OF NURSING UNIT-1 PART-2
FUNDAMENTAL OF NURSING UNIT-1 (ફન્ડામેન્ટલ ઓફ નર્સિંગ યુનિટ -1)-part-2.
- f) Health care agencies – hospital and
- community service – types and
- function of hospitals health team.
- g) Modern approaches to nursing care
- including holistic nursing care
- h) Health and Disease
- Definition of health, determinants
of health status. - Basic human needs
💟 Health Care Agencies

- Health is a fundamental human right of every individual. Different health care agencies try to fulfill the health needs of the community by identifying them. The main departments of the health care agencies are as follows.
Community Level (કોમ્યુનીટી લેવલ):

- PHC – Primary Health Center
- CHC – Community Health Center
- UPHC – Urban Primary Health Center
- HAWC – Health and Wellness Center
- UHTC – Urban Health Training Center
- RHTC – Rural Health Training Center
Hospital

- Referral Hospital (FRU-First Referral Unit) (Referral hospital)
- District Hospital (District Hospital)
- Special Hospital (Special Hospital)
- Teaching Hospital (Teaching Hospital)
- ESIS Hospital (Employees’ State Insurance Hospital)
- AIIMS-super speciality hospital
- Private Agency (Private Agency) :-
- Private hospital (Private hospital)
- Nursing home (Nursing home)
- Dispensary (Dispensary)
- Clinic (Clinic)
- Other Agency :-
- Defence Service (Defence Service)
- Railway Hospital (Railway Hospital)
- Voluntary Health Agency (Voluntary Health Agency)
- WHO (World Health Organization)
- UNICEF (United Nation International Children Emergency Fund)
- Red Cross :-
- CARE (Co Operative American Relief Everywhere)
- UNESCO (United Nation Education Social and Culture Organisation)
- All the above health agencies solve the following health problems:
- Communicable Disease Control
- Nutritional Problem
- Environmental Sanitation Problem
- Medical Care Problem
- Communicable Disease Control
- Hospital :
- An institution for the care of patients and the treatment of people injured due to accidents etc. The word Hospital is derived from Hospus. Hospus means guest, meaning the patient who comes here is a guest and the institution that takes care of him is the hospital. The work of curing the sick people is done in the hospital.
- Hospital
- Definition

- It is an institution where sick or injured people are treated and cared for. A hospital has specialized medical equipment and doctors, nurses, and other healthcare staff who provide medical care and health services to patients.
- It has facilities for emergency care, surgery, diagnostic tests, and long-term care.
- Example:
The main departments of a hospital include OPD (Outpatient Department), ICU (Intensive Care Unit), Emergency Room, and Maternity wards. - or
- A hospital is an institution where more than one person works for the same goal. Our goal in a hospital is to work for health and where the disease of a sick person is diagnosed and comprehensive care is given to him. The team of people working here is called a health team. This health team includes doctors, nurses, social workers, servants and technicians. The hospital is a community agency. A person from any group of the society can come to the hospital for treatment and the health team provides treatment to every person without any discrimination of religion, caste, age etc.
- When a patient comes to the hospital, he is a guest of the hospital and he goes home after getting better. During this time, an image of the hospital is formed in him. If he has been given good treatment, then he takes a good image with him.
- Classification of Hospitals
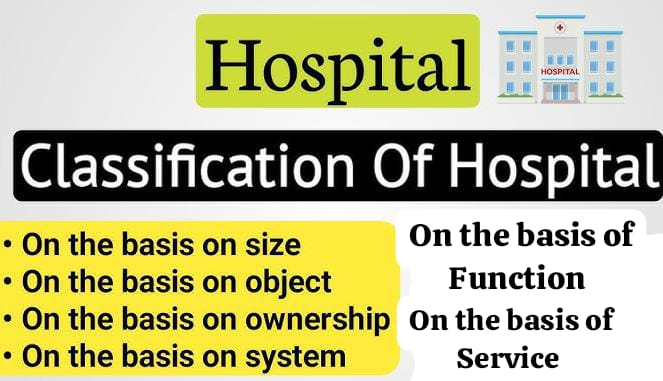
Ownership-based Classification
- Government Hospitals:
Run by the government to provide healthcare services at low or no cost. Example: Civil Hospital. - Private Hospitals:
Owned by individuals or organizations; typically charge higher fees for their services. Example: Apollo Hospitals. - Charitable Hospitals:
Operated by NGOs or trusts to offer community services. Example: Mission Hospitals. - Military Hospitals:
Provide healthcare exclusively for armed forces and their families. Example: Army Base Hospital. - Function-based Classification:
- General Hospitals:
Offer treatment for a wide range of diseases. Example: General Civil Hospital. - Specialty Hospitals:
Focus on specific specialties like cardiology, orthopedics. Example: Heart Institute. - Super-specialty Hospitals:
Provide advanced care in fields like neurology, oncology. Example: Tata Memorial Hospital. - Size-based Classification:
- Small Hospitals:
Typically have under 50 beds and serve small communities. - Medium Hospitals:
Have 50-200 beds, often multi-specialty. - Large Hospitals:
More than 200 beds with comprehensive facilities. - Service-based Classification:
- Teaching Hospitals:
Attached to medical colleges for training students. Example: AIIMS, Delhi. - Non-teaching Hospitals:
Focused only on patient care without educational activities. - Research Hospitals:
Dedicated to medical research along with patient care. Example: ICMR Centers. - Duration of Care:
- Short-term Hospitals:
Provide treatment for acute illnesses, often requiring short stays. - Long-term Hospitals:
Offer care for chronic diseases or rehabilitation. - Location-based Classification:
- Urban Hospitals:
Located in cities with advanced facilities. Example: Fortis Hospital. - Rural Hospitals:
Located in villages or remote areas, providing basic healthcare. - Access-based Classification:
- Open-access Hospitals:
Available to all patients without restrictions. - Closed-access Hospitals:
Restricted to specific groups like employees or military families. - Care Level-based Classification:
- Primary Care Hospitals:
Provide basic healthcare services and refer complex cases. - Secondary Care Hospitals:
Offer specialized treatments like surgeries. - Tertiary Care Hospitals:
Deliver highly specialized care like organ transplants or advanced therapies. - More information About government hospital

- Government Hospital:-
- Government Hospital is managed by the government, all the employees working here are called government servants.
- State Government:-
- It comes under the state government.
- Central Government:-
- It comes under the central government.
- Semi Govt.Hospital:-
- It receives some percentage of government grants and some percentage is run with money given by industrialists and other donors. Often the staff in this hospital is also from the government.
- Municipal Hospital:-
- Municipal means that the municipality of the city and its staff are also appointed by it.
- E.S.I.S Hospital:-
- It is managed according to the central government and the staff is also according to it.
- Private Hospital (PRIVATE HOSPITAL) :-
- This type of hospital is managed by a single person and is owned by him. Often, a private hospital is run by a group of three or four people. Each group member is fully responsible for his research.
- Private Clinic (PRIVATE CLINIC):-
- It is owned by a single person or a clinic that is run by more than one person.
- Trust Hospital (TRUST HOSPITAL):-
In this hospital, some people form a trust together and it is managed by it. The board that forms this trust makes the rules and it is managed according to those rules. - Army Hospital (ARMY HOSPITAL) :-
This hospital is only for army men and the hospital is managed by the Central Government. It is in every state but it is managed by the Central Government only. - Industrial Hospital (INDUSTRIAL HOSPITAL) :-
Such a hospital is built for workers working in industries. For this, a hospital is built when the number of workers reaches a certain number. This hospital comes under the Industrial Act and is managed under this act and the workers are treated. - 💜 Function OF Hospital-Tell the functions of the hospital:-
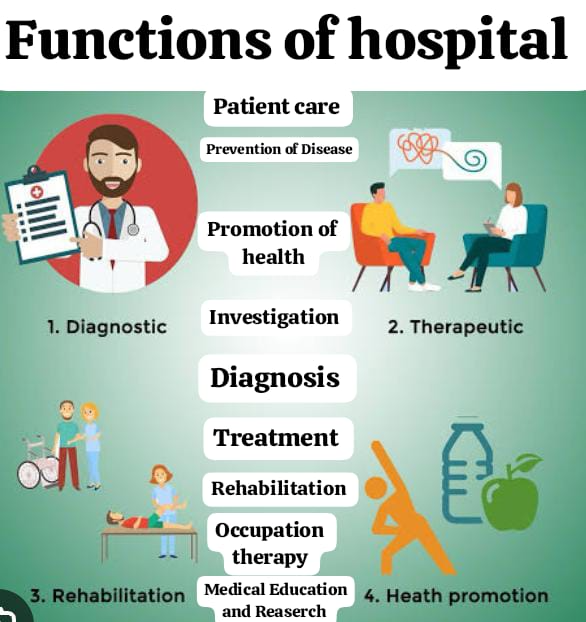
- 1.Patient care:-
All patients admitted to the hospital are given all kinds of care from admission to discharge, their nursing care and other needs are provided and in addition, 24-hour treatment is provided in emergencies. - 2.Prevention of Disease Prevention is better than Cure:-
The hospital doctors and staff nurses together with the patients prevent the disease. In order to prevent it from happening, it is done in advance. In addition, the necessary cleaning and other work is done by the hospital to prevent the disease from happening in the hospital. - 3.Promotion of Health:-
To improve the health of the patients admitted to the hospital, the hospital also gives them advice related to the disease. So that the patient can improve his health, health education is also given to his relatives and any person from the hospital associated with health can provide this type of health education.
- Investigation, Diagnosis and Treatment:-
Nowadays, there has been a huge progress in medical science. New inventions and related tools have also been invented for the diagnosis of every patient, so that the diagnosis of diseases can be done quickly. The patients admitted to the hospital are immediately investigated and their diagnosis is determined and accordingly the necessary treatment is started. This is an important function of the hospital. - Rehabilitation and Occupational Therapy:-
Every person admitted to the hospital who wants to recover and settle down in the society or profession again is given a specific type of guidance. For this, after getting his total history from the beginning, guidance is given according to his occupation till the last stage.
- Medical Education:-
All the activities running in the hospital include all types of education and it is provided by doctors, nurses, physiotherapists, pharmacies and technicians. In addition, planning is done for medical education where necessary.
In-service education is organized as per the requirement for the staff inside the hospital and everyone is trained and this type of education is given in accordance with new discoveries and new health programs etc.
- Medical Research:-
Different patients are admitted to the hospital, according to which many types of research can be done by knowing their problems. This work of research is as important as medical education, however, many types of research are done in many branches of the hospital and every person should know about it. Through new research, new skills can be acquired by knowing many types of skills. - Social Services:-
Social services i.e. social services are provided by the hospital for welfare and security. In this, social care is especially provided to the patients. For this, there is also a social welfare department where social workers give appropriate advice to everyone.
The hospital provides many types of certificates for security purposes such as physical fitness, age certificate, handicap certificate, widowhood certificate, etc. Along with this, certificates are provided for injured patients and dead certificates for deceased patients, reports for post-mortem of births and dead bodies are also provided.
- Administrative work of the Institute:-
The hospital is a huge institution, all the employees in it are managed by the administrative office of the hospital, records of each employee have to be kept. - Record:-
Many types of records are kept by the hospital, including records from admission to discharge of the patient, birth and death records, infectious disease records, in addition to some types of statistical information, written records of this matter are regularly sent to the necessary places, so this work is very essential for the hospital.
💖 Department of Hospital :

💖 What is OPD ?

- In which patients coming from outside are examined by a doctor and the necessary medicine and treatment are given from that department and only those patients who need it are admitted after planning. There are also different OPDs in OPD such as Medical OPD, Surgical OPD, Orthopedic OPD, Dental OPD, Skin OPD, E.N.T OPD etc.
💖 what is IN Patient Department

- This department has different wards in which patients are admitted and treated. Each ward has head nurses, staff nurses, etc. Apart from this, this department also has necessary offices like medical store inquiry office, etc.
From the ward perspective, this department has departments like medical ward, surgical ward, E.N.T ward, orthopedic ward, ophthalmic ward, pediatric ward, skin ward, isolation ward, etc. - 💖 List the different departments of Hospital. Make a list of the different departments of the hospital.

- 💖 List the different departments of Hospital. Make a list of the different departments of the hospital.
- Casualty Department: To provide emergency medical care
- Operation Theater (OT: operations theater): To perform surgical procedures.
- Intensive Care Unit (ICU): For special critical patients
- Anesthesiology Department: To provide anesthesia
- 💖Cardiology Department: For the heart
- ENT (Ear, Nose and Throat): For eyes, ears and throat
- Gynecology Department: For women’s diseases
- Pediatric Department: For children
- Neurology Department: For the treatment of central nervous system disorders
- Oncology Department: For cancer
- Ophthalmology Department: For the eyes
- Orthopedic Department: For the department of bones
- Urology Department: For urinary system related diseases
- Psychiatric Department: For mental illness Department
- Indoor Patient Department (IPD): For admitted patients
- Outdoor Department (OPD): For examining patients coming from outside by a doctor
- Nursing Department
- Pharmacy Department
- Laboratory Department
- Administrative Department
- 💖Laboratory Department:
- Laboratory is an important part of the hospital. Where blood, urine, serum, stool etc. are examined, there are also different types of laboratories, and expert doctors also work in them.
- Microbiology lab:
Microorganisms are studied in this section
Pathology:
Blood, stool, urine, sputum, etc. are examined in this department
Serology:
Serum, i.e. the water part of blood, is examined in this department
Blood bank:
Here blood is deposited and given as per the requirement and patient group
Histopathology:
Here, microscopic study of viscera (parts protruding from body parts) is done
💖 Nursing Department: - The main function of the nursing department is to provide all kinds of care to the patients in the hospital. The head of the nursing department is called a matron. There is a matron office for her in the hospital. Apart from this, there is also a day super room and a night super room. Each ward has a sister in charge room, staff nursing room, Student nurses etc. are doing the work.
- 💖Pharmacy Department:
- People who have studied pharmacy work in this department and they maintain and give all the medicines
- House surgeon:
He is the local surgeon of the surgery ward. - Honorary:
That is, an expert surgeon who provides free services.
Nursing staff:
Which includes staff nurses, head nurses etc. - Ward servant:
Which includes both male and female.
Sweeper:
There are male and female sweepers who work as sweepers. Apart from this, there are dressers, hospital assistants and other staff in the hospital. S.S.D (Central and Sterilization) plays an important role not only in supplying but also in improving the quality of their lives. - 💟 Health

💚 WHO -definition

- “A person who is mentally, physically, socially or spiritually well and does not have any kind of disease or deformity is called a healthy person”.
- But when a person is physically, mentally or socially disturbed, he is called Sick or Patient. He cannot pay attention to his routine work due to his illness.
- That patient is sick, that is, not only himself is disturbed but the environment around him is also disturbed. Due to the patient’s illness, his family members are also disturbed.
Since the patient is sick, he cannot be present in any social event or society as before. Doctors and nurses should be careful while providing care to the patient.
The nurse who first comes in contact with the patient should do a good IPR with the patient and introduce other staff members. - It should also help in getting adjustment in the ward environment. The nurse should also develop good IPR with the patient’s relatives and give appropriate answers to the questions about the patient’s illness.
- There should be good communication to provide good nursing care. Otherwise, the patient feels lonely which affects his illness.
- 💚 To describe various changing concept of health

- 1.Biomedical concept
- According to this concept, health means “absence of disease”. If a person is free from disease, then he is considered a healthy person.
From the medical profession’s perspective, the human body is a machine. Disease means the machine’s ability to work breaks down and the only job of a doctor is to repair the machine. This concept has reduced the role of the environment to social, psychological and cultural determinants. - This concept does not address the main health problems like malnutrition, accidental drug abuse, mental diseases, chronic diseases, environmental pollution, population explosion, etc.
- Ecological concepts
According to this concept, there is a dynamic equilibrium between the human and its environment, and disease is a disorder of the human organism with the environment.
- Psychosocial concept
According to this concept, health is not only a biomedical phenomenon but also the influence of social, psychological, cultural, economic and political factors on the people concerned.
- Holistic concept
The holistic concept is a synthesis of all these concepts. It recognizes the strength of social, economic and political and environmental influences on health. It describes a multidimensional process that health means a healthy mind in a healthy body in a healthy family.
In a good environment, this concept suggests that all fields of society have an impact on health. Which are agriculture, animal husbandry, food, industry, education, housing, public works and other fields.
- Concept of well being
It suggests an improvement in the standard and quality of life. It refers to the standard of living which includes health education, food, consumption, clothing, housing, entertainment along with human rights and social safety.
- Quality of Life:
It is related to the individual’s feelings of satisfaction, happiness and sadness about the numerous problems of life, so increasing the standard and quality of life to achieve a feeling of well-being.
- 💟 Determination of Health Status:
- Every person has his own specific standard to check his health, which means that physically and mentally we are healthy but sometimes our health is disturbed, which is checked by knowing the right things.
- Whether there are symptoms of certain diseases in our body or not, e.g. (Pain), vomiting, (fever) etc. We decide that we are sick.
- People often feel good or bad about their health psychologically. For example, sometimes a person feels good about himself while sometimes he feels sick.
- In other ways, it is based on whether people are able to do their daily activities. For example, many people do their routing work every day.
To know the health status, not one but many issues should be considered, such as social, economic, cultural, patterns, etc. - To know the health status of any person, the current physical fitness is very important. Through it, is the person healthy or not? Why can it be known?
💟 According to Community Health (Determinat Of Health):
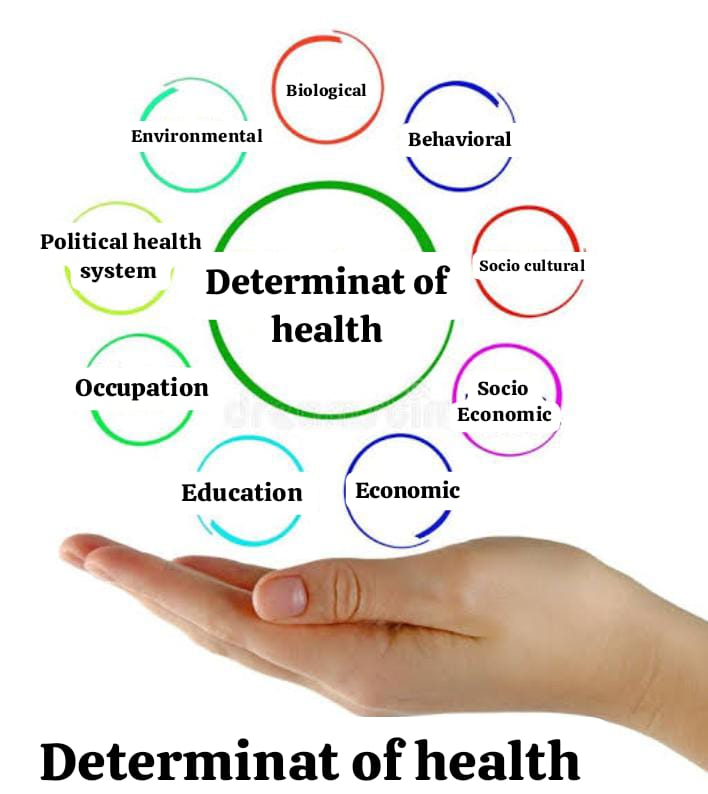
- Many factors affect health, in which the factors of the society in which the person lives affect.
- (1) Biological Determinant:-
- The physical and mental health of each person depends on the genes inherited by him. Many diseases are found to be hereditary. Such as diabetes, hypertension, mental retardation, etc.
- A person’s genes being healthy is an important factor for good health. Apart from this, viruses, bacteria, animals etc. present around a person also affect health as agents of diseases.
- (2) Behavioral and socio-cultural Determinant:-
- How a person behaves with family and society. It also affects health. Cultural and behavioral patterns and personal habits like smoking, alcoholism, etc. also affect health. A person’s parents, group, friends and mass media etc. also affect the lifestyle. A healthy lifestyle is necessary to stay healthy. Many problems are related to a person’s lifestyle. Eg: Coronary heart disease, drug addiction etc.
- In India where there is a traditional lifestyle, poor sanitation, poor nutrition, poor personal hygiene and customs and habits are responsible for the occurrence of diseases and deaths.
- (3) Environmental Determinant:-
- These are internal and external. Internal environment means body parts, cells, tissues etc. while external environment includes physical, mental, sociological.
- It is a fact that environment is directly related to physical, mental and social well-being. When we talk about the health status of the population, these three are related to each other. If the environment is conducive, then the physical and mental strength of the individual develops.
- (4) Socio-economic condition:-
- This is an important factor affecting human health, the health status of most people in the world can be known from their socio-economic condition. Nutrition, housing, education as well as the political system of the country,
- (5) Economic system:-
- In most developing areas, due to economic progress, the incidence of disease has decreased and life span has increased, and the quality of life has improved when it has improved their purchasing power, living conditions. The economic level of people is determined by how they live, the quality of life.
- (6) Education:-
- This is another important factor affecting health status. In the world where poverty, malnutrition, and high infant and child mortality rates are high, ignorance is more, this also affects health,
- (7) Occupation:-
- Those who do not have a job become the cause of health or death. Due to the decrease in work, income decreases, due to which social status decreases and its causes are psychological and social damages.
- (8) Political health system:-
- Health is also associated with the political system of the country. Political reasons are more responsible than technical for the implementation of health technology.
- (5) Health & family welfare services:-
- Health and family welfare services The purpose of health and family welfare services is to maintain the health of individuals and communities, treat people and prevent diseases. Health services are related to all these things and aim to maintain the health of people. For example, immunization of children provides protection against particular diseases.
- (6) Population:-
- 2/3 of which will be in developing countries. Most of them are in good health, but due to the rapid population growth and chronic diseases and disabilities, special attention needs to be given.
- (7) Gender:-
- Since 1990, more attention has been paid to females. Since 1993, there has been more awareness in making policies related to women’s health for nutrition, reproductive status, etc. Also, importance has been given to every plan related to its development.
- Other factors:
- We know that there has been a lot of progress in information and communication technology recently. Due to this revolution, people can easily get medical information. In this, the public gets the benefit of the services of many physicians, health professionals, biomedical, scientists and researchers from all over the world through mass media. Other health care systems also play a very important role in maintaining the health of the people.
💟 sick and well Introduction to the sick & well :
- Sick means a person who is disturbed somewhere. Patients who come to the hospital and are admitted come with many expectations and they have no idea how their relatives will admit them, how they will be received and how they will be treated. If the health of one person in the family deteriorates, it affects the entire family. When a patient comes to the hospital, he has many worries about his illness such as how many days he will have to stay in the hospital, the cost of medicine, when will he recover from the disease, etc.
Disease

- WHO has given a definition of health but not of disease because…..
- It has many shades from symptomatic to dangerous manifest disease.
- Some diseases occur acutely and some chronically.
- Some diseases have a carrier state.
- In some cases, one organism causes more than one disease. (Streptococcus).
- And in some cases the same disease can be caused by more than one organism. (Diarrhea)
- Some diseases last for a short time and some for a long time.
- In some diseases, the borderline symptoms are unclear.
- The end point of the disease is variable such as disability or death of the host.
- The term “disease” means “without ease” when there is something wrong with the body’s function.
💚 To define the disease
- According to Webster’s…
A condition in which the health of the body is impaired. A change in the human body that occurs from the onset of a condition of health that interferes with the performance of important work. - According to the Oxford English Dictionary…
A condition of the body or of some part or organ of the body in which its function is impaired or distorted. - Ecological point of view…
A maladjustment of the human organism with the environment. - Other definition..
- Disease is the opposite of health, i.e. any deviation from the common function or state of complete physical or mental health.
- Disease means when a disease organism enters the body and succeeds in causing disease, it is called disease. When the body is disturbed, it is called illness.
- There are different theories for the concept of disease:
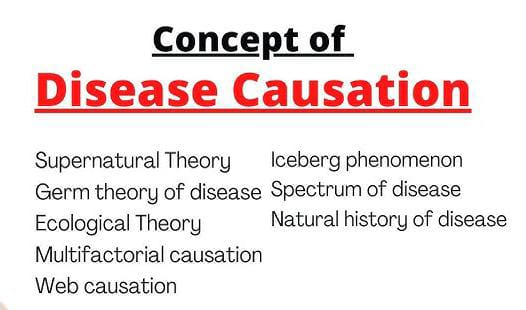
- (1) Super Natural Theory: –
- This theory talks about natural powers. In earlier times, diseases were believed to be caused by divine powers, for example, smallpox, chickenpox, leprosy, and were believed to be caused by sins committed in the previous time.
- (2) Germ Theory:
- It is believed that a disease is caused by some kind of germ (this theory was presented by a scientist named Pasteur from 1820 to 1895, in which he stated that the disease is caused by the entry of any bacteria or microorganism into the body.
- (3) Theory of Multiple Cause:
- In this, more than one cause is responsible for the disease. For example, if someone has tuberculosis, his economic status, etc. are responsible for it. In this way, more than one cause is responsible.
- Health and Illness Continuum
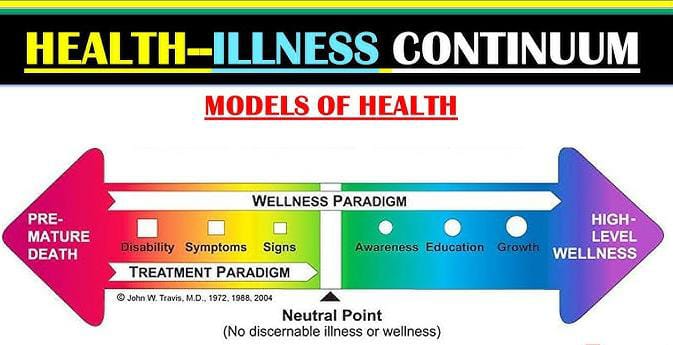
- Definition:
- The Health and Illness Continuum is a dynamic model, in which the health status of a person is shown as a range from Health to Illness. In this continuum, the health status of a person is not static; it always changes. Constantly changing.
- Key Points:
- Dynamic Process:
- The state between health and disease is constantly changing.
- Range:
- Optimal Health: The best physical, mental, and social condition.
- Severe Illness: When a person’s health capacity is greatly reduced.
- Reflection:
- A person’s lifestyle, genetics, and environment affect health.
- Stages of the Health and Illness Continuum:
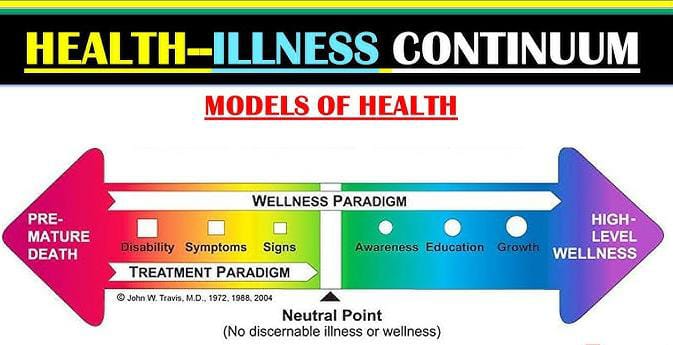
- High-Level Wellness:
Physical fitness, mental peace, and social balance.
Examples: Regular exercise, a nutritious diet, and a positive lifestyle.
- Neutral Zone:
A neutral state between health and disease.
Example: Common ailments such as the common cold.
- Mild Illness:
Symptoms are mild but require medical care.
Example: Diabetes or Hypertension.
- Severe Illness:
Physical or mental illness that affects lifestyle.
Example: Cancer, Heart Disease, or Depression.
- Terminal Illness:
When a person’s body organs lose their ability to function.
Elements of the Continuum:
- 1.Physical Health:
- Positive nutrition, fitness, and medical care.
- 2.Mental Health:
- Stress management and therapy.
- 3.Social Well-being:
- Positive connections in family and society.
- 4.Environmental Influence:
- Pollution, living conditions and workplace.
- Implications:
1.Preventive Focus:
Prevention of diseases through health promotion.
- Health Monitoring:
Regular check-ups help in improving physical and mental health.
3.Lifestyle Modification:
Nutrition, regular physical activity and mental rest.
Examples:
- Healthy Person:
A person who exercises regularly and follows a balanced diet is at the health end of the continuum.
- Ill Person:
A person with cancer or heart failure is at the disease end of the continuum.
- Neutral State:
A person with a cold or fatigue is in the middle of the continuum.
The Health and Illness Continuum is useful for understanding the dynamic process of health. It encourages individual and collective efforts for health promotion and disease prevention, allowing individuals to make the best decisions for their health.
Causes and Risk Factors for Developing Illness:
Illness is the result of an imbalance in the physical, mental, or social system. Various problems and risk factors are responsible for its development.
- Biological Factors:
- Genetic Mutations:
Genetic disorders such as Sickle Cell Anemia, Thalassemia, or Down Syndrome. - Weak Immune System:
Decreased immunity of the body, which causes infections. - Hormonal Imbalance:
Thyroid, diabetes, or PCOD.
- Lifestyle Factors:
- Poor Diet:
- Lack of fatty and nutritious food.
- Example: Obesity, heart disease.
- Smoking and Alcohol Consumption:
- Responsible for lung cancer and liver disease.
- Physical Inactivity:
- Responsible for weight gain and cardiopulmonary disease.
- Environmental Factors:
- Pollution:
- Air pollution, which is a risk factor for respiratory diseases such as asthma or bronchitis.
- Exposure to Pathogens:
- Bacteria, viruses, or fungal infections.
- Poor Hygiene:
- A major factor for epidemics and infections.
- Psychosocial Factors:
- Stress and Anxiety:
- Risk for depression and heart attack.
- Social Isolation:
- Mental illnesses and failure to cope mechanisms.
- Physical Factors:
- Physical Injury:
- Fractures or neurological diseases due to work or accidents.
- Excessive Strain:
- Overstraining that causes muscle injury or orthopedic problems.
- Epidemiological Factors:
- Age:
- Chronic diseases in old age such as arthritis or hypertension.
- Gender:
Osteoporosis in women or prostate cancer in men due to hormonal differences. - Ethnicity and Geography:
- Endemic Diseases that are found in a particular region.
- Genetic and Hereditary Factors:
- Family History:
- People at risk for heart disease, diabetes, or cancer.
- Other Factors:
- Drug and Chemical Exposure:
- Toxins that cause kidney or liver damage.
- Medical Negligence:
- Incorrect treatment or medical errors.
Preventive Measures:

- Adopting a healthy lifestyle:
Balanced diet, regular exercise, and healthy habits.
- Stress management:
Reducing stress through meditation, yoga, and counseling.
- Preventive screening:
Regular medical check-ups.
- Maintaining cleanliness:
Hand hygiene and safe food practices.
- Protection from pollution:
Using masks and a clean environment.
The causes and risk factors of illness are influenced by physical, mental, and environmental factors. Diseases can be prevented through preventive control of these factors and health promotion, which makes a person’s life healthier and better.
Types of Illness:
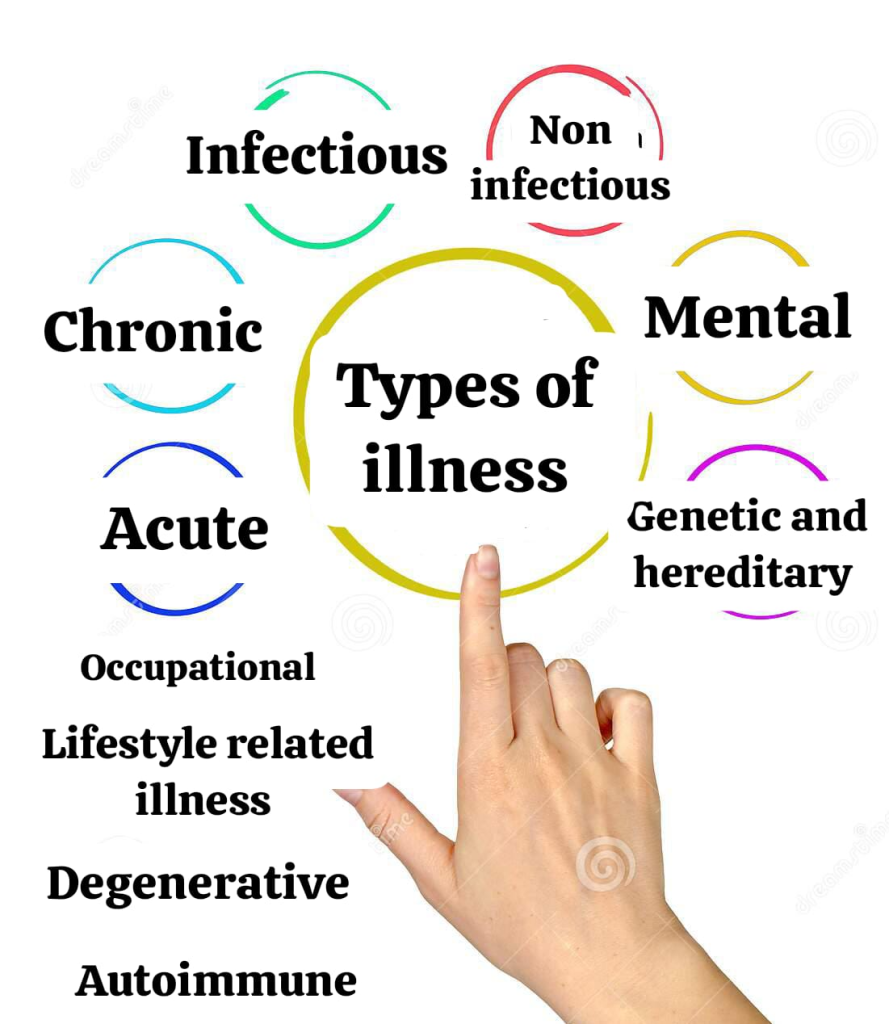
Illnesses affect a person’s physical, mental or social functioning. These types can be divided into different categories, ranging from short-term illnesses to long-term chronic diseases.
- Acute Illness:
- This type of illness starts suddenly and ends in a short period of time.
- Example:
- Common cold
- Flu
- Food poisoning
- Bronchitis
- Features:
- Sudden symptoms
- Short duration
- Quick recovery with medical treatment.
- Chronic Illness:
- These illnesses last for a long time and require annual or lifelong medical management.
- Example:
- Diabetes
- Heart disease
- Cancer
- Asthma
- Features:
- Persistent symptoms
- Can be controlled with medication and lifestyle changes.
- Infectious Illness:
- These types of illnesses are caused by bacteria, viruses, fungi, or parasites and can be spread from one person to another.
- Example:
- Malaria
- Tuberculosis (TB)
- HIV/AIDS
- Covid-19
- Features:
- Risk of Outbreaks
- Can be treated with vaccination and antibiotics.
- Non-Infectious Illness:
- This type of illness does not spread disease and is usually associated with the internal systems of the body.
- Example:
- Hypertension
- Arthritis
- Osteoporosis
- Depression
- Features:
- Individual factors or the environment are the cause.
- Requires long-term medical care.
- Mental Illness:
- This type of illness affects the mental state and personality of the patient.
- Example:
- Depression
- Anxiety Disorder
- Schizophrenia
- Bipolar disorder
- Features:
- Shows both physical and mental symptoms.
- Counseling and medical therapy are necessary.
- Genetic and Hereditary Illness:
- This type of illness is caused by a defect in the genetic code of a person and is passed down through generations.
- Example:
- Sickle cell anemia
- Thalassemia
- Hemophilia
- Down syndrome
- Features:
- Control is possible through medical management.
- A complete cure may never be possible.
- Occupational Illness:
- Illnesses that develop due to the work environment.
- Example:
- Silicosis (in factory workers)
- Hearing loss (due to loud noise)
- Carpal tunnel syndrome (Computer Operators)
- Features:
- Prolonged exposure causes effects.
- Preventive measures are necessary.
- Lifestyle-Related Illness:
- These types of illnesses are the result of an unhealthy lifestyle.
- Example:
- Obesity
- Heart attack
- Type 2 diabetes
- Alcoholic Liver Disease
- Features:
- Control is possible with diet and physical activity.
- It is necessary to improve lifestyle.
- Degenerative Illness:
- This type of illness gradually reduces the functionality of the body’s organs or systems.
- Example:
- Alzheimer’s
- Parkinson’s disease
- Multiple sclerosis
- Features:
- Medical care and physiotherapy are necessary.
- Symptoms become more severe in the progressive form.
- Autoimmune Illness:
- The body’s immune system attacks its own healthy tissues.
- Example
- Lupus
- Rheumatoid arthritis
- Psoriasis
- Illnesses can be of different types, depending on the individual’s lifestyle, genes, environment, and psychological state. Each type requires preventive and medical management to restore the patient to an optimal level of health.
Illness Behavior
Illness Behavior refers to the mental, physical, and social reactions that a person displays when faced with a disease or illness experience. This behavior depends on the severity of the disease, the person’s social barriers and beliefs, understanding of the disease, and access to health services.
Definition of Illness Behavior:
Illness Behavior is the behavior that a person displays when facing health-related problems or interacting with the health care system.
Components of Illness Behavior:

- Symptom Perception:
How a person recognizes symptoms of a health problem.
Examples: fatigue, pain, fever, etc.
- Health-Seeking Actions:
Steps taken to seek medical help, such as contacting a doctor.
- Exemption from Roles:
Release from daily responsibilities of an ill person, such as not going to work.
- Interaction with Professionals:
Contact with health care professionals for medical treatment and health advice.
Factors Influencing Illness Behavior:
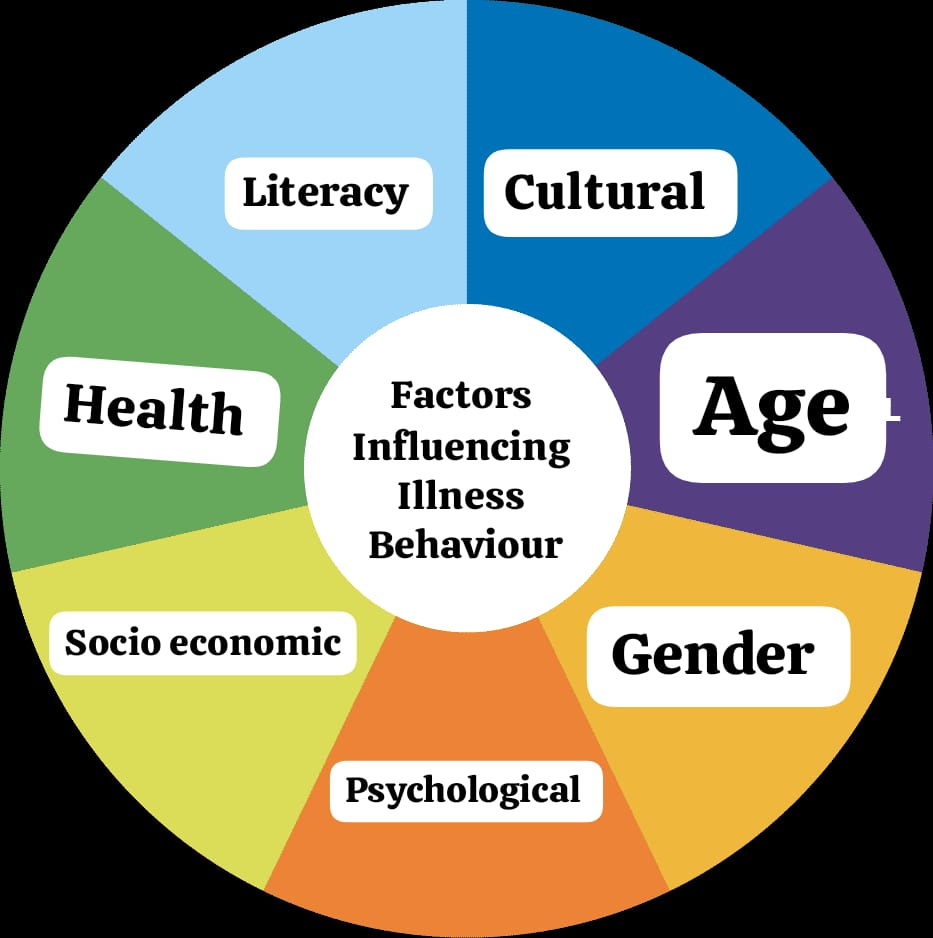
- Cultural Factors:
Beliefs and perspectives on disease in the person’s society.
Example: Some cultures ignore physical symptoms, while others seek medical help immediately.
- Gender and Age:
Children and the elderly seek health care more quickly.
Women generally take symptoms of illness more seriously.
- Psychological Factors:
Stress, depression, or tension can intensify the experience of symptoms.
- Socio-Economic Status:
People with higher economic status can easily seek health services.
The poorer classes are more likely to be misunderstanding health care.
- Health Literacy:
A person’s knowledge of the symptoms and treatment of the disease.
Stages of Illness Behavior:
- Symptom Recognition:
The patient experiences pain, fever, or discomfort in their body.
- Contact with Healthcare System:
Contact with a doctor or healthcare professional for diagnosis.
- Diagnosis and Treatment:
Medical treatment to determine the cause and cure the illness.
- Role Adjustment:
The patient changes their responsibilities, such as taking rest or leave.
- Recovery:
The stage of recovering from the illness and returning to daily life.
Types of Illness Behavior:

- Health-Seeking Behavior:
Urgently seeking medical advice or a medical checkup.
- Ignoring Symptoms:
The patient ignores the symptoms, which can lead to further progression of the disease.
- Self-Medication Behavior:
Attempting to treat by buying medicine from the pharmacy.
- Complication-Oriented Behavior:
Seeking medical treatment only when the symptoms of the disease become severe.
Examples:
- Positive Behavior:
- If a person experiences symptoms of diabetes, he/she immediately gets tested for diabetes.
- Negative Behavior:
- Despite having Chest Pain, the person does not seek medical help and considers it a normal ache.
- Challenges in Illness Behavior:
- Misconceptions:
- Patients often underestimate the severity of the illness.
- Fear of Healthcare:
- Fear of diagnosis or treatment.
- Financial Barriers:
- Inability to afford healthcare.
- Illness Behavior influences the relationship between the patient and the healthcare professional. Early recognition of symptoms and appropriate action can help reduce the severity of the illness and improve health.
Impact of Illness on the Patient and Family:

Illness not only affects the physical and mental health of the patient, but also the mental, social, and economic factors of his family. The severity, type, and duration of the illness determine the intensity of this impact.
Impact on the Patient:

- Physical Effects:
- Fatigue, pain, and loss of physical strength.
- Difficulty in activities of daily living, such as going to work or taking care of oneself.
- Sometimes disability or loss of control over leisure activities.
- Mental Effects:
- Stress and depression.
- The tension of living with the illness and worry about the future.
- Feelings of inadequacy due to one’s own inadequacy.
- Spiritual Effects:
- Concern about the meaning and purpose of life.
- Finding spiritual strength or loss of faith.
- Social Effects:
- The patient’s relationships and friendships may be disrupted.
- The ability to socialize and participate in social activities is reduced.
- Financial Effects:
- The need for money for medical expenses and treatment.
- Loss of ability to work, resulting in a decrease in income.
Impact on the Family:

- Emotional Stress:
- Development of anxiety, depression, or stress in family members.
- A state of constant worry among family members about the patient’s health.
- Changes in Daily Life:
- Dedicating time to caring for the patient, which disrupts their daily activities.
- Work hours may have to be reduced or given up.
- Financial Burden:
- The strain on the family’s finances due to medical bills, medications, and treatment costs.
- Additional costs to support the patient.
- Social Impact:
- Limitations in participation in social activities for family members.
- Impact on relationships with others.
- Role Adjustments:
- Family members may have to take on new responsibilities, such as becoming caregivers for the patient.
- Parenting roles for children change.
- Impact on Relationships:
- Relationships between the patient and family members may be strengthened or strained.
- Positive and Negative Impacts:
- Positive Impacts:
- Increases cooperation and unity in the family.
- Strengthens the spiritual beliefs of the patient and family members.
- Develops sensitivity and a sense of humanity for family members.
- Negative Impacts:
- Develops tension and conflict among family members.
- Economic stress and health-related fatigue.
- Lack of patient’s feelings and support.
- Steps to Reduce Impact:
- Emotional Support:
- Counseling services for the patient and family.
- Use of group therapy and search support groups.
- Financial Assistance:
- Use of health insurance or charitable funds.
- Planning medical expenses.
- Organization and Time Management:
- Create a schedule for patient care.
- Sharing responsibilities within the family.
- Education and Awareness:
- Health education for understanding the disease and appropriate treatment.
- Caregiver training for the patient.
- Spiritual Strength:
- Finding peace through religious or spiritual activities.
- Illness brings physical, mental, and financial challenges to both the patient and the family. With a positive approach, medical support, and emotional support, these challenges can be reduced and stability in life can be achieved.
Modern approaches to nursing care-including holistic nursing care

- Evidence-Based Practice (EBP):

- Evidence-Based Practice (EBP) is the integration of scientific evidence, patient-centered preferences, and clinical expertise in nursing care and health services to provide the best health services.
- Features:
- Scientific Basis:
Relying on recent research for care. - Use of Clinical Expertise:
Utilizing the experience and skills of practitioners. - Patient-Centered Approach:
Taking into account the patient’s aspirations and needs. - Standard Guidelines:
Implementation of policies and guidelines in health services. - Elements of EBP:
- Best Evidence:
Evidence derived from modern research. - Clinical Expertise:
The use of medical professionals’ experience in health services. - Patient Preferences:
Prioritizing the patient’s values, beliefs, and preferences. - Process of EBP:
- Formulating a Question:
Clarifying and investigating a patient’s question or problem. - Searching for Evidence:
Collecting information from articles, research papers, and databases such as CINAHL, PubMed, and the Cochrane Library. - Appraising the Evidence:
Examining whether the evidence found is strong or not. - Applying the Evidence:
Planning treatment based on strong evidence and patient aspirations. - Evaluating the Outcome:
Seeing the results of care or treatment and making necessary adjustments. - Benefits of EBP:
- Improved Patient Outcomes:
Successful treatment based on strong evidence and best practices. - Standardized Care:
Consistent health services through guidelines. - Enhanced Treatment:
Adopting new discoveries and techniques. - Professional Excellence in Nurses and Health Services:
The use of research and development in nursing practice. - Examples:
- Surgical Wound Care:
Medical research shows that moist wound dressings help surgical wounds heal faster. - Diabetes Management:
Nutritional Planning-based treatment with insulin therapy. - Fall Prevention:
Research-based multifactorial interventions for older patients. - Barriers to EBP:
- Time Constraints:
Less time available to medical staff for research. - Lack of Knowledge:
Health workers unaware of new research. - Limited Access to Research:
Limited access to libraries or databases. - Evidence-Based Practice (EBP) is an important tool for modern nursing care, which helps in providing quality health services. It improves the quality of health services through Patient-Centered Care and Science-Based Solutions.
Palliative Care

- Palliative Care is a comfortable and quality of life service for patients who are terminally ill or dying, which takes care of the physical, emotional, social, and spiritual aspects. Its main goal is to reduce the painful symptoms of the patient and his family with compassionate care.
- Key Features:
- Pain Management:
The use of pain killers and drugs such as morphine to control the painful symptoms of the patient. - Emotional Support:
Providing psychological comfort to the patient and his family. - Spiritual Care:
Meeting the religious and spiritual needs of the patient. - Improved Quality of Life:
Focusing on making the remaining life of the patient more comfortable and pleasant. - Patient and Family Involvement:
The role of the patient and their family in treatment decisions. - Goals of Palliative Care:
- Relieve symptoms of the patient.
- Ensure quality of life.
- Provide psychological support to the family.
- Prepare the patient physically and mentally for the final stages of death.
- Benefits:
- Pain Relief:
Relieve symptoms of the patient through morphine or pain management therapy. - Trust and Compassion:
Provide psychological comfort to the patient. - Family Support:
Help prepare the family for the time after death. - Optional Treatment:
Provide emergency treatment where necessary. - Interventions and Therapies:
- Physical Care:
- Resolving the patient’s distressing symptoms, such as shortness of breath, psychological stress, etc.
- Psychological Support:
- Reducing mental stress through counseling.
- Spiritual Therapy:
- Providing spiritual comfort to the patient through prayer, meditation, and religious activities.
- Diet Management:
- Proper diet for the patient’s nutrition.
- Examples:
- Cancer Patients:
- Morphine and relaxation therapy for pain management as part of palliative care.
- Terminal Illness:
- Psychological support and medical care for patients with long-term illness.
- End-of-Life Care:
- Physical and mental comfort to patients in the final stages of death.
- Palliative Care in Indian Context:

- In India, various Cancer Institutes and Hospices are functioning to provide palliative care for short-term illnesses such as cancer, terminal stage diseases.
- Palliative Care is compassionate, purposeful and comfortable care for the patient and their family, which only addresses the symptoms of the patient.
- Patient-Centered Care:
- Patient-Centered Care is a way of healthcare where the patient is kept at the centre of healthcare. It respects the physical, emotional and social aspects of the patient along with their values, beliefs and preferences.
- Key Features:
- Individualized Care:
- Providing care that is tailored to the characteristics and needs of each patient.
- Respect for Patient Preferences:
- Involving the patient in decisions about their treatment.
- Patient-Doctor Collaboration with Healthcare Providers:
- Open communication and involvement between the patient and the healthcare team.
- Transparency:
- Providing the patient with complete information about their condition and treatment.
- Involvement of Family:
- Involving family members in the patient’s treatment.
- Emotional Support:
- Empathetic approach to reducing the patient’s psychological distress.
- Process:
- Assessment:
- Evaluating the patient’s symptoms and needs.
- Learn about the patient’s lifestyle, medical history, and preferences.
- Communication:
- Communicate openly and clearly with the patient.
- Inform the patient about treatment and care options.
- Treatment Planning:
- Develop a care plan based on patient input.
- Set short-term and long-term goals.
- Collaboration:
- Coordinate with each member of the healthcare team.
- Collaborate to achieve the best possible outcome for the patient’s treatment.
- Feedback and Evaluation:
- Improve services based on patient feedback.
- Review patient treatment outcomes.
- Benefits:
- Improved Quality of Care:
A patient-centered approach helps improve the quality of healthcare. - Patient Satisfaction:
Patients are more satisfied when they are involved in their treatment decisions. - Better Health Outcomes:
Patient engagement makes treatment more effective. - Increased Trust:
Increased trust and transparency between the patient and the healthcare professional. - Examples:
- Diabetes Management:
A diet plan and fitness program as per the patient’s choice. - Pregnancy Care:
A delivery plan for a pregnant patient with the guidance of a professional according to their wishes. - Chemotherapy patient:
A patient’s lifestyle should be considered along with medical and psychological support for their treatment. - Role of Policies and Documentation:
- Patient Rights:
Every patient has the right to receive appropriate information and make choices about treatment. - Care Plan Documentation:
A record of the programs chosen by the doctor and nurse for the patient’s treatment. - Standard Protocols:
A treatment plan for the nursing and medical team. - Patient-Centered Care improves the quality of healthcare and increases patient satisfaction. It focuses not only on the patient’s pathology but also on their entire lifestyle, which makes it more impactful and positive for the healthcare system.
Technology-Based Nursing

- Technology-Based Nursing makes nursing practice and patient care more efficient through the use of modern technology and digital tools. Its aim is to provide more accurate data management, faster diagnosis, and better health services.
- Key Features:
- Telehealth:
Video Consultation and monitoring services for remote patients. - Electronic Health Records (EHR):
Digital Database of patient health history. - Mobile Health Apps:
For patients’ medical security and self-monitoring. - Sensors and Monitoring Devices:
Heart Rate Monitor, Blood Pressure Machine, and Glucose Monitor. - Digital Communication:
Data Sharing and Online Updates among Healthcare Teams. - Robotics in Nursing:
Robotic Assistance for Patient Care, such as delivering medications or monitoring patients. - Applications of Technology-Based Nursing:
- Telehealth and Remote Care:
- Video Consultation for sick patients.
- Diagnosis of patient symptoms through Telemedicine.
- Mobile Health:
- Fitness Trackers and Digital Reminders for Patients.
- Emergency Care:
- Use of Technology for Electronic Alarm Systems.
- Ambulance Tracking Systems.
- Medical Machine Learning in Medicine:
- Artificial Intelligence (AI) to guide treatment.
- Big Data Analysis to identify disease patterns.
- Virtual Reality:
- Simulation Programs to teach nursing.
- VR Therapy to increase mental relaxation for patients.
- Benefits:
- Accurate and Fast Information:
- Fast access to patient medical records and symptoms.
- Time-Saving:
- Technology makes routine processes faster.
- Patient Safety:
- More accurate monitoring of patient symptoms and treatment.
- Cost-Effective:
- On-demand services, such as telehealth, reduce costs.
- Remote Care:
- Technology assists patients in providing care without having to go to the hospital.
- Examples:
- Telemedicine:
- Remote Medical Guidance for remote patients.
- ICU Monitoring System:
- Digital machines to monitor a patient’s vital signs.
- Medical Robots:
- Robotic Assistance during surgery.
- Medication Delivery for patients.
- Wearable Devices:
- Apple Watch that tracks blood oxygen and heart rate.
- Challenges:
- Technology Adaptation:
- Need to teach healthcare workers new technologies.
- Cost:
Modern equipment is often expensive. - Privacy and Data Security:
Ensuring the security of patient data. - Technology-Based Nursing makes nursing practice more efficient and patient-centered. It ensures accurate data, rapid treatment, and remote connectivity. While there are some challenges, the widespread use of technology in the medical field opens up new directions for healthcare.
Community-Based Care:

- Community-Based Care is a health service designed to meet the health needs of all members of the community. It provides health services to patients based on their home and taking into account social factors.
- Key Features:
- Primary Health Services:
- Immunization, Nutrition Programs, and First Aid.
- Disease Control:
- Control programs for epidemics.
- Special services for TB, Malaria, HIV/AIDS.
- Community Participation:
- Organization of work by ASHA Workers and Anganwadi Workers.
- Care at the Point of Need:
- Providing health services to patients where they need them.
- Community-Based Health Education:
- Camps and workshops to spread awareness about healthcare.
- Community Research:
- Data collection in rural areas to find out various problems.
- Objectives:
- Cultural Relevance:
- Providing services according to the cultural beliefs of the patient.
- Accessibility and Affordability:
- Making health services available to all.
- Promoting Preventive Care:
- Health promotion for the patient and the community.
- Long-Term Care:
- Nutritional care for the elderly or those with chronic diseases.
- Types of Community-Based Care:
- Home-Based Care:
- Health care provided to the patient at home.
- Example: Visiting nurse or home caregiver.
- Rural Health Care:
- Primary Health Centers (PHCs) in villages.
- Maternal and Child Health (MCH):
- Health laboratories for pregnant women and screening for children.
- Epidemic Control:
- Health activities for epidemics such as malaria, dengue.
- Community Rehabilitation:
- Rehabilitative services for people with disabilities or patients.
- Applications:
- Sanitation Campaigns:
- Awareness programs for clean villages.
- Immunization Drives:
- Immunization programs for children and mothers.
- Health Awareness Campaigns:
- Education programs for HIV/AIDS, TB, and diabetes.
- Dietary Guidance:
- Guidelines for nutritious food in poor communities.
- Benefits:
- Accessibility:
- Health services in remote areas.
- Preventive Care:
- Health activities to reduce epidemics.
- Comfort for Patients:
- Health services to patients in their homes.
- Community Involvement:
- Cooperation with local voluntary organizations and health workers.
- Examples:
- ASHA Workers:
- Health and nutrition guidance for pregnant women.
- Immunization Camps:
- Free polio drops and hepatitis vaccines in villages.
- Maternal Care:
- Safe delivery service through primary health centers.
- Disease Control:
- DOTS therapy program for TB.
- Challenges:
- Limited Community Resources:
- Lack of adequate services for medicines and technology.
- Lack of Training:
- Lack of proper training for health workers.
- Time for Outcomes:
- Health outcomes take longer to be seen.
- Community-Based Care improves access and quality of health services for remote areas and rural communities. It is a health system that is patient-centered and prioritizes preventive care. These services can be made more effective through community-based models and governmental schemes.
Holistic Nursing Care

- Holistic Nursing Care is a healthcare system that provides health care to the patient in a holistic manner, based on the physical, mental, emotional, social, and spiritual aspects.
- Key Features:
- Patient-Centered Approach:
- Fully respects the patient’s needs and preferences.
- Places the patient at the center of their treatment.
- Comprehensive Support:
- Focuses on the patient’s entire life, not just the disease.
- Empathetic Care:
- Building a relationship of empathy and trust with the patient.
- Inclusion of Alternative Therapies:
- Meditation, Yoga, Massage Therapy, and Art Therapy.
- Multi-Disciplinary Approach:
- Teamwork with doctors, nurses, counselors, and spiritual guides.
- Aspects of Holistic Nursing Care:
- Physical:
- Management of the patient’s physical symptoms, such as pain management and physical comfort.
- Mental:
- Counseling to reduce stress and depression.
- Emotional:
- Creating a positive environment in the patient’s family.
- Social:
- Helping to improve the patient’s relationships and social connections.
- Spiritual:
- Supporting religious beliefs and spiritual needs.
- Goals of Holistic Nursing Care:
- Improvement in Overall Health:
- A stress-free state of the patient’s body and mind.
- Enhanced Quality of Life:
- Not just treatment, but lifestyle changes.
- Boost in Morale of the patient and family:
- Respect and psychological support for the patient.
- Nutrition and Comfort:
- Nutritious diet and comfortable environment.
- Process of Holistic Nursing Care:
- Holistic Assessment:
- Assessment of the patient’s physical, mental, emotional, social and spiritual needs.
- Empathy and Comfort:
- Allocating time for communication with the patient.
- Use of Complementary Therapies:
- Use of meditation, massage, yoga etc. for patient comfort.
- Creating a Care Plan:
- Making individual efforts to benefit from treatment.
- Feedback and Adjustments:
- Revise the care plan based on patient and family feedback.
- Benefits:
- Comprehensive Care:
- Physical and mental comfort for the patient.
- Improved Outlook:
- Improvement in the patient’s approach to life.
- Integrated Treatment:
- Integration of medical and alternative therapies.
- Effective Treatment:
- Not just treating the disease, but improving the lifestyle.
- Examples:
- Cancer Patients:
-Meditation and massage therapy with chemotherapy. - Mental Health Patients:
-Mental comfort through counseling and yoga therapy. - Geriatric Patients:Comfortable lifestyle with religion and counseling activities for the elderly.
- Holistic Nursing Care is not just a method of making patients disease-free, but focuses on supporting them to live a completely healthy and balanced life. This method of healthcare provides the best healthcare to the patient by incorporating all aspects of the patient.